Mechanical ventilation in Acute severe asthma status asthmaticus



















- Slides: 66
Mechanical ventilation in Acute severe asthma (status asthmaticus) Acute respiratory distress syndrome (ARDS) Neuromuscular diseases Dr Arthur Chun-Wing LAU Associate Consultant Dept of Medicine (Respiratory and Critical Care Medicine) and Dept of Anaesthesia (Intensive Care Unit) PYNEH April 2005
Acute respiratory distress syndrome (ARDS)
ARDS: pathophysiology l Formation of protein-rich alveolar edema after damage to the integrity of the lung’s alveolar-capillary barrier l Can be initiated by physical or chemical injury or by extensive activation of innate inflammatory responses

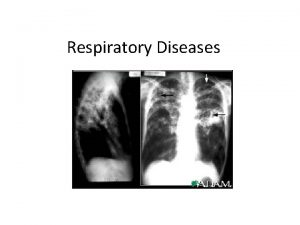
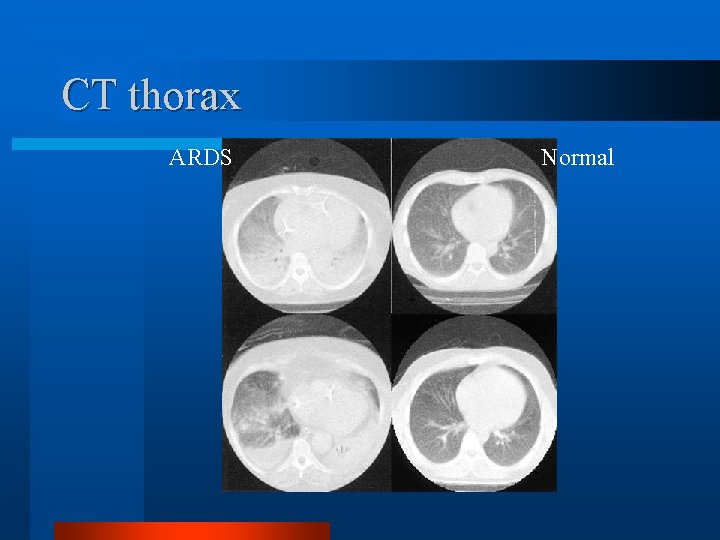
ARDS: radiology
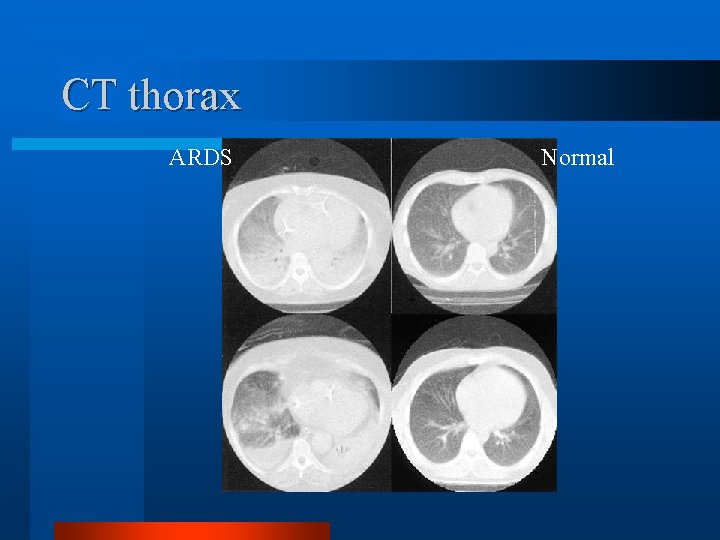
CT thorax ARDS Normal
Physiological derangements in ARDS l Ventilation-perfusion mismatch l Alveolar ventilation impairment by excluding oxygenation (Intrapulmonary shunt) l Inactivates surfactant leading to atelectasis l Decreases lung compliance (stiff lung)


ARDS Most studies of ventilatory strategies for ARDS and acute lung injury (ALI) have shown no benefit in terms of mortality. l Exceptions for so-called “lung protective strategy” studies: – Amato et al 1998 (N= 53), and – The ARDSnet mechanical ventilation study 2000 (N = 861) • better outcome in the low tidal volume (6 ml/kg predicted body weight) group l

Tidal volume l Important to avoid over-distension of alveoli in the relatively normal parts of lung – start at 6 -7 ml/kg predicted BW (to maintain plateau pressure <30 -40 cm H 2 O) – allow PCO 2 to rise slowly (i. e. giving kidneys time to compensate for respiratory acidosis), aim to keep p. H > 7. 25 (instead of aiming for a target PCO 2, but advisable to not to allow Pco 2 to rise above 20 k. Pa)

Positive end-expiratory pressure (PEEP) l Optimal PEEP – improves gas exchange by maintaining alveolar patency (open lung approach) – reduces the Fi. O 2 required (high oxygen concentrations are toxic to the lung) l Too high PEEP will cause lung injury and impairs cardiac output

Total PEEP levels applied in recent studies on protective mechanical ventilation Black: study patients White: control patients
PEEP: setting l no optimal way to assess "best PEEP" – PEEP is added in increments of 2 -5 cm until the "best/optimal PEEP" is obtained, choose the level which provides the highest static compliance and the lowest airway plateau pressure – PEEP above lower inflection point on static P-V curve l PEEP over 20 cm is rarely beneficial and usually results in additional pressureinduced lung injury
Respiratory rate l if possible use rates <30/min to decrease risk of dynamic hyperinflation l Rates up to 35/min were used in ARDSnet study l N. B. Minute volume = RR x TV

Ventilator mode at equivalent inspiratory times PCV has the advantage of higher mean airway pressure compared to constant flow volume controlled ventilation or the addition of inspiratory pause l Decelerating flow volume controlled ventilation has a similar airway pressure profile to PCV but with constant volume delivery. l ARDSnet study used volume preset assist control l
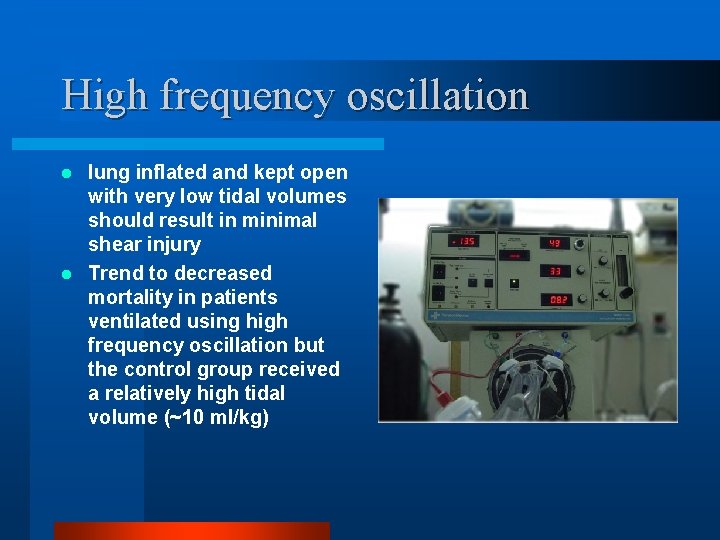
High frequency oscillation lung inflated and kept open with very low tidal volumes should result in minimal shear injury l Trend to decreased mortality in patients ventilated using high frequency oscillation but the control group received a relatively high tidal volume (~10 ml/kg) l
Airway pressure release ventilation variation of inverse ratio ventilation l lung volume and hence oxygenation is maintained by continuous positive airway pressure l CO 2 clearance is achieved by the transient release of circuit pressure allowing gas to escape and lung volume to fall l CPAP is then re-established to the previous level, allowing the entry of fresh gas into the system patient may breathe throughout the respiratory cycle also known as BIPAP l
Inverse ratio ventilation (IRV) l I: E ratio > 1 can improve oxygenation in patients who remain hypoxic despite PEEP – not all patients benefit from this strategy – muscle relaxants often required when I: E ratios of > 2: 1 are used – small risk of causing haemodynamic compromise
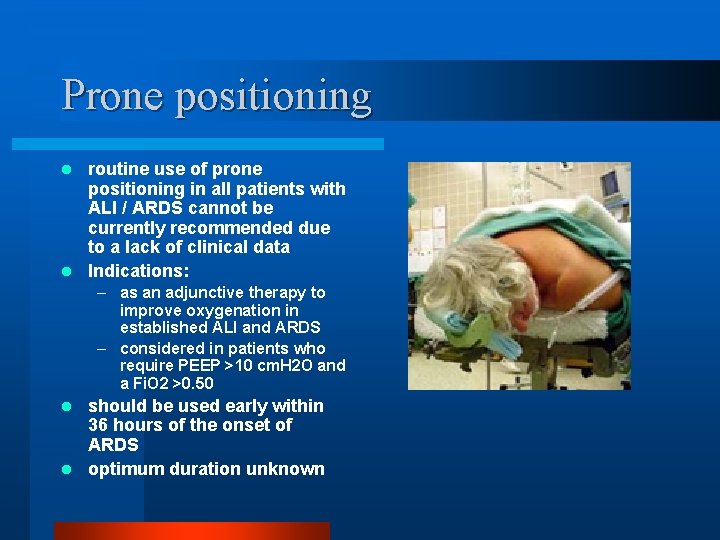
Prone positioning routine use of prone positioning in all patients with ALI / ARDS cannot be currently recommended due to a lack of clinical data l Indications: l – as an adjunctive therapy to improve oxygenation in established ALI and ARDS – considered in patients who require PEEP >10 cm. H 2 O and a Fi. O 2 >0. 50 should be used early within 36 hours of the onset of ARDS l optimum duration unknown l
Prone positioning physiological effects improvement in oxygenation has been reported in 58 to 100 % of patients l Respiratory mechanics: initial decrease in respiratory system compliance which subsequently improves during the prone period and increases when returned to supine l with more prolonged prone ventilation there is improvement in CO 2 clearance which is related to improvement in alveolar ventilation in well-perfused areas l
Prone positioning: mechanism l The mechanism of improvement in oxygenation with prone positioning is multifactorial – less dependent atelectasis and ventilation is more homogeneous – more effective alveolar recruitment at a lower endinspiratory pressure and de-recruitment will be minimized at lower end-expiratory pressure – reduction in ventilation and perfusion mismatch and a reduction in intrapulmonary shunt. – Changes in the distribution of secretions and extravascular lung water
Lung recruitment manoevres l designed to improve oxygenation and reduce shear injury by reopening alveoli thought to reduce shear injury at the interface between collapsed and open alveoli l N. B. there are no clinical trials supporting the use of recruitment maneouvers

Recruitment maneuvers: methods incremental levels of PEEP with constant peak airway pressure inspiratory pressure, or l prolonged increase in pressure (eg 40 -50 cm. H 2 O) either as single maneuver (lasting 40 -50 secs) or with stepwise increase in pressure with return to baseline between each increase, or l pressure control ventilation at high inspiratory pressures either with stepwise increases with return to baseline between each increase or single maneuver lasting 120 secs, or l BIPAP may be useful as a recruitment maneouver in patients who are taking spontaneous breaths l
Recruitment manoevres: Haemodynamic consequences l fall in cardiac output l rise in pulmonary artery pressure l fall in blood pressure l transient long term significance unknown
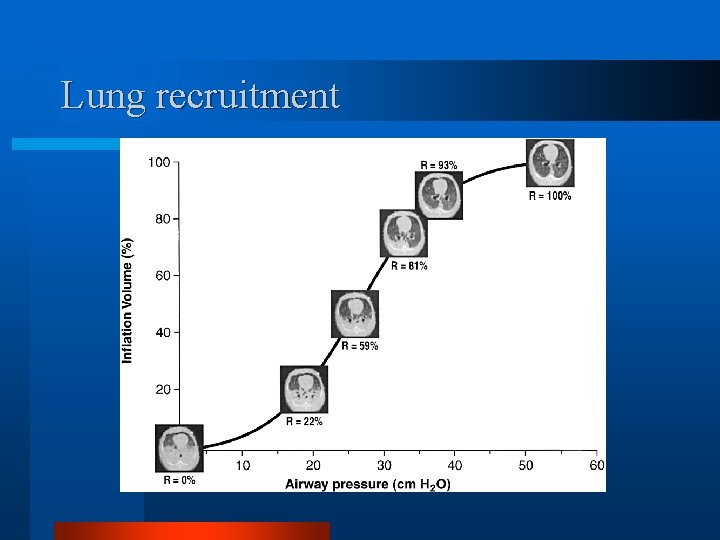
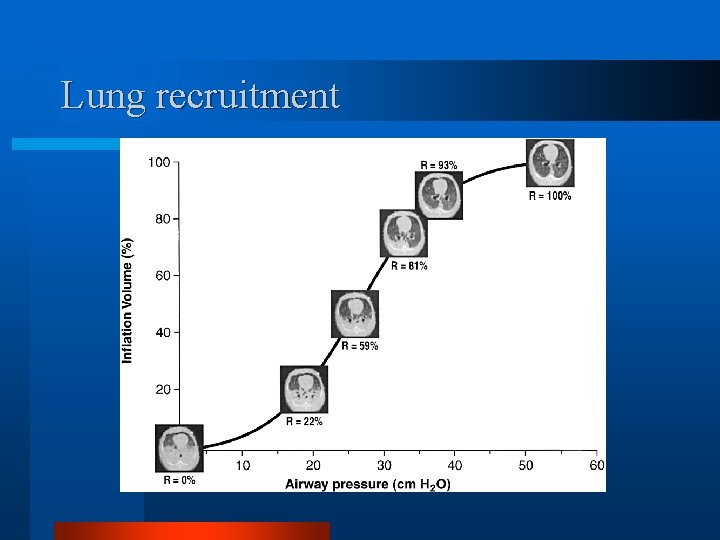
Lung recruitment
Tracheal gas insufflation l l l an adjunctive ventilatory technique enhance CO 2 elimination efficiency Method – During expiration, fresh gas insufflated through the TGI catheter washes out the CO 2 that remains in the dead space proximal to the catheter tip higher flows causing a greater reduction in Pa. CO 2 l Benefit l – less CO 2 is inhaled during inspiration (enhances CO 2 removal) – has the potential to make ventilation with a lower VT more efficient
Aspiration of gas from the dead space (ASPIDS) l a new principle l gas rich in CO 2 during late expiration is aspirated through a channel ending at the distal end of the tracheal tube. l Simultaneously, fresh gas injected into the inspiratory line fills the airway down to the same site.

Extracorporeal membrane oxygenation (ECMO) l very expensive not associated with improved survival
Partial liquid ventilation l involves filling the lungs with a fluid (perfluorocarbon, also called Liquivent or Perflubron) which has – very low surface tension, similar to surfactant – high density, oxygen readily diffuses through it – may have some anti-inflammatory properties l l The lungs are filled with the liquid, the patient is then ventilated with a conventional ventilator using a protective lung ventilation strategy. Liquid will help the transport of oxygen to parts of the lung that are flooded and filled with debris, help remove this debris and open up more alveoli improving lung function.
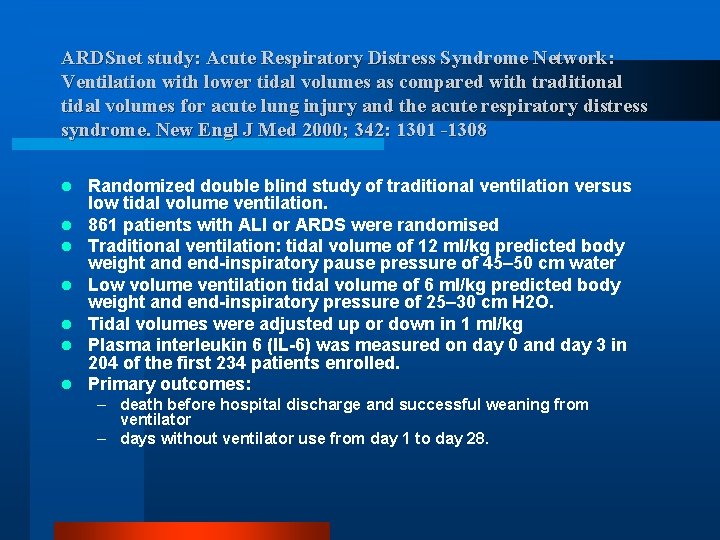
ARDSnet study: Acute Respiratory Distress Syndrome Network: Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. New Engl J Med 2000; 342: 1301 -1308 l l l l Randomized double blind study of traditional ventilation versus low tidal volume ventilation. 861 patients with ALI or ARDS were randomised Traditional ventilation: tidal volume of 12 ml/kg predicted body weight and end-inspiratory pause pressure of 45– 50 cm water Low volume ventilation tidal volume of 6 ml/kg predicted body weight and end-inspiratory pressure of 25– 30 cm H 2 O. Tidal volumes were adjusted up or down in 1 ml/kg Plasma interleukin 6 (IL-6) was measured on day 0 and day 3 in 204 of the first 234 patients enrolled. Primary outcomes: – death before hospital discharge and successful weaning from ventilator – days without ventilator use from day 1 to day 28.
Outcomes l Trial stopped after enrollment of 861 patients because mortality was lower in the lower tidal volume group than in traditional tidal volume group – Mortality: Low volume (LV) ventilation (31%), Traditional ventilation (TV) 39. 8%, p = 0. 007 l No of days without ventilator use during the first 28 days greater in LV 12+/- 11 days vs TV 10 +/- 11 days, p<0. 001
Conclusion l Lung protective strategies – Low tidal volume (6 ml/kg PBW) – High PEEP (similar outcome for lower PEEP if small TV is used) – Low plateau pressure (<30 cm. H 2 O) – Permissive hypercapnia – Inverse ratio ventilation if necessary l Adjunctive – Prone positioning – Recruitment manoevres l Experimental – ECMO – Partial liquid ventilation – High frequency ventilation
Status asthmaticus
Status asthmaticus: pathophysiology l Severe obstructive airway problem from bronchospasm and airway edema l Presence of bronchial casts

Bronchial cast


Non invasive l insufficient data to recommend this form of ventilation in acute asthma l available data suggests that it is probably safe
Invasive l When to ventilate, complex decision which needs to be based on a number of factors – rate of deterioration – monitor p. H and Pa. CO 2 – respiratory rate – clinical signs of exhaustion – likely response to treatment
Goals of mechanical ventilation l The ideal ventilator setting is to reduce dynamic hyperinflation (DHI) – limited minute ventilation (MV), using low tidal volume (Vt) and respiratory rate to result in tolerable level of gas exchange (permissive hypercapnia) – extended expiratory time (TE) – Aim at the lowest positive inspiratory pressure (PIP) and the lowest expiratory lung volume, avoiding intrinsic positive end expiratory pressure (PEEP)
Ventilator modes volume controlled mode: guarantees reproducible VT despite variations of airways resistance but then, the consequent rise of pressure must be limited l pressure controlled mode: variations of resistance induce important variations of VT. A continuous monitoring of ventilation is always indicated (inspiratory and expiratory parameters of the ventilator, saturation, capnography, transcutaneous p. CO 2, ABG) l Assisted and spontaneous mode are not indicated l
Neuromuscular blockade l Indicated in patients who, in spite of sedation, continue to breath in a desynchronized manner
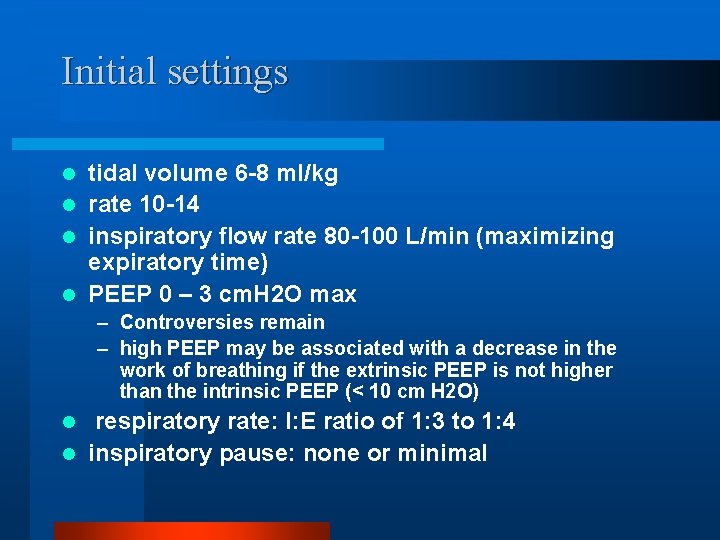
Initial settings tidal volume 6 -8 ml/kg l rate 10 -14 l inspiratory flow rate 80 -100 L/min (maximizing expiratory time) l PEEP 0 – 3 cm. H 2 O max l – Controversies remain – high PEEP may be associated with a decrease in the work of breathing if the extrinsic PEEP is not higher than the intrinsic PEEP (< 10 cm H 2 O) respiratory rate: I: E ratio of 1: 3 to 1: 4 l inspiratory pause: none or minimal l
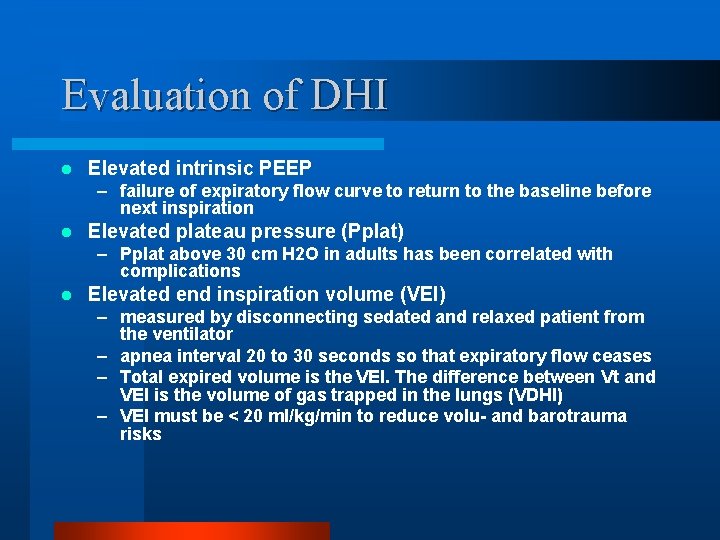
Evaluation of DHI l Elevated intrinsic PEEP – failure of expiratory flow curve to return to the baseline before next inspiration l Elevated plateau pressure (Pplat) – Pplat above 30 cm H 2 O in adults has been correlated with complications l Elevated end inspiration volume (VEI) – measured by disconnecting sedated and relaxed patient from the ventilator – apnea interval 20 to 30 seconds so that expiratory flow ceases – Total expired volume is the VEI. The difference between Vt and VEI is the volume of gas trapped in the lungs (VDHI) – VEI must be < 20 ml/kg/min to reduce volu- and barotrauma risks
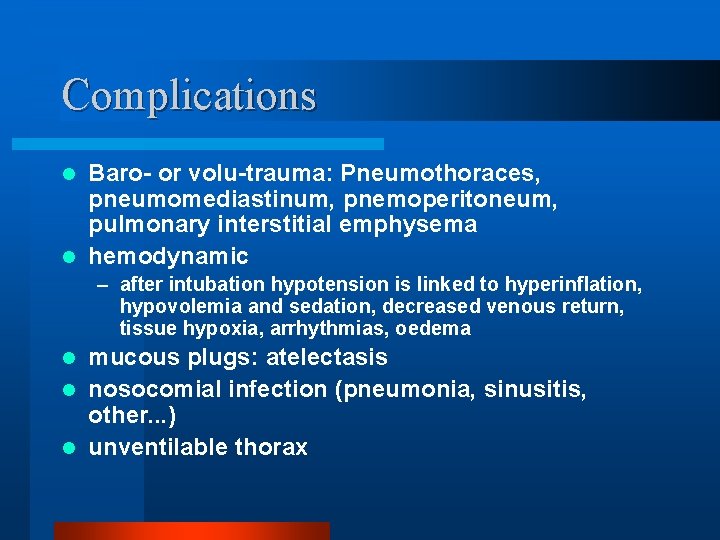
Complications Baro- or volu-trauma: Pneumothoraces, pneumomediastinum, pnemoperitoneum, pulmonary interstitial emphysema l hemodynamic l – after intubation hypotension is linked to hyperinflation, hypovolemia and sedation, decreased venous return, tissue hypoxia, arrhythmias, oedema mucous plugs: atelectasis l nosocomial infection (pneumonia, sinusitis, other. . . ) l unventilable thorax l
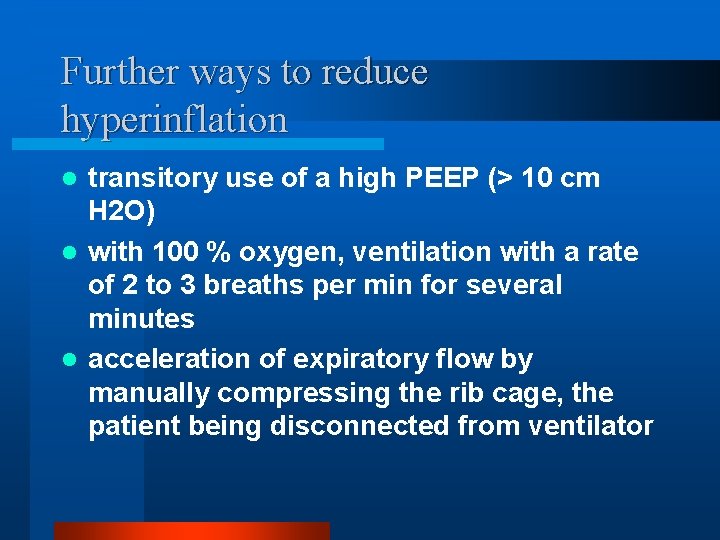
Further ways to reduce hyperinflation transitory use of a high PEEP (> 10 cm H 2 O) l with 100 % oxygen, ventilation with a rate of 2 to 3 breaths per min for several minutes l acceleration of expiratory flow by manually compressing the rib cage, the patient being disconnected from ventilator l

Neuromuscular disease
Problems l Removal of secretions l Ventilatory pump failure l Progressive atelectasis l Increasing oxygen requirement l Decreasing MIP and VC
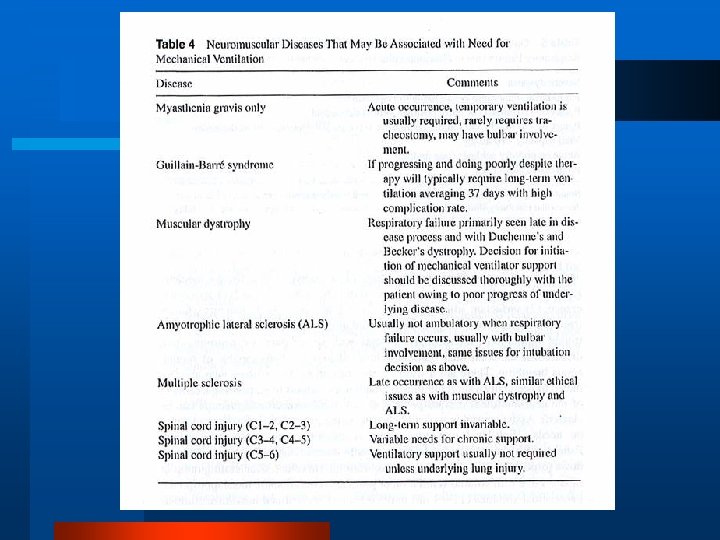


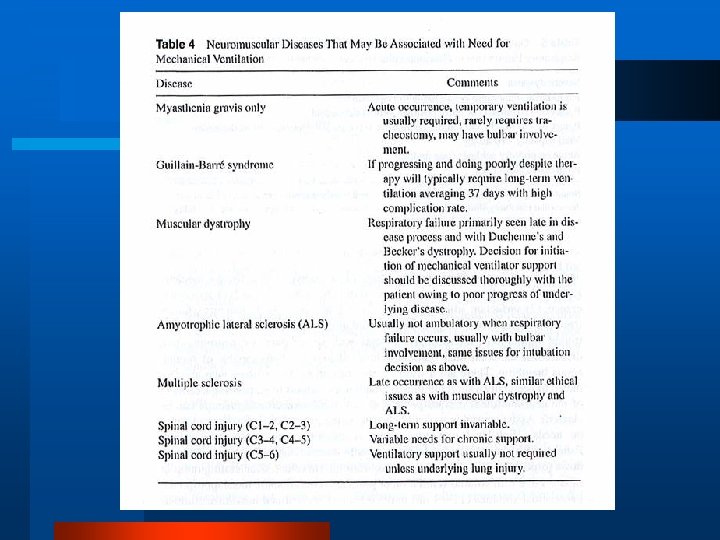
Choice of ventilatory support l Noninvasive positive-pressure ventilation – If reversibility is expected over hours to days, e. g. mild LRTI in chronic neuromuscular disease as polymyositis or MG – Problem: secretion retention l Intermittent positive pressure ventilation via endotracheal tube
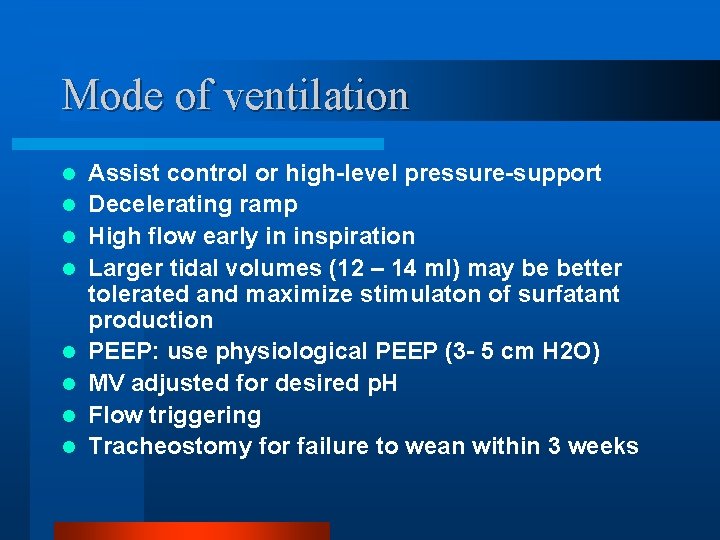
Mode of ventilation l l l l Assist control or high-level pressure-support Decelerating ramp High flow early in inspiration Larger tidal volumes (12 – 14 ml) may be better tolerated and maximize stimulaton of surfatant production PEEP: use physiological PEEP (3 - 5 cm H 2 O) MV adjusted for desired p. H Flow triggering Tracheostomy for failure to wean within 3 weeks
Myasthenia gravis
Myasthenia gravis l 1/20 000 adults - females >> males - peak incidence in 3 rd decade in women, in 6 th in men - associated with other auto-immune diseases, particularly other organspecific auto-immune diseases
MG: clinical features l l l Facial muscle weakness (drooping eyelids, double vision) Muscle weakness in the arms or legs Difficulty in breathing, talking, chewing or swallowing Fatigue brought on by repetitive motions Sequelae – – – aspiration due to bulbar involvement nosocomial pneumonia Atelectasis acute respiratory failure cardiac arrest

MG: pathophysiology auto-immune antibodies to post-synaptic ACh receptor in 90% (Usually Ig. G), and skeletal muscle unable to synthesize receptors at a sufficiently high rate to maintain normal neuromuscular function l myeloid cells within thymus have ACh receptors on their surface which serve as a source of autoantigen to trigger an immune response l – thymic hyperplasia in 70% (tend to be younger patients) – thymomas in 10 – 15% (tend to be elderly) l as disease progresses pre-synapatic receptor may become involved
Myathenic crisis l Predominant problem is neuromuscular respiratory failure l Incidence increases markedly with age
Precipitating factors intercurrent infection l Pregnancy l drugs: antibiotics (aminoglycosides, polymyxins, tetracycline), anti-arrhythmics (quinidine, quinine, procainamide), local anaesthetics (procaine, lignocaine), muscle relaxants, analgesics (morphine, pethidine) l
Management l l Intubate when VC falls below 15 ml/kg Aims of ventilation – Rest patient – Prevent collapse and atelectasis – Consider witholding anticholinergics while patient is intubated – Plasmaphoresis and/or IV Ig – Steroids l Duration of mechanical ventilation is usually short-term unless there is infective complication

Gullain-Barre syndrome
Gullain-Barre: clinical features l l progressive motor weakness of > 1 limb with areflexia Clinical (in order of importance) – initial rapid progression of weakness but no further progression by 4 weeks – symmetry seldom absolute but if one limb is affected opposite one is likely to be affected – mild sensory symptoms and signs – facial weakness common (especially in axonal degeneration form) and frequently bilateral. – Other cranial nerves may be involved, particularly those innervating tongue, muscles of deglutination and extraocular muscles – recovery usually start 2 -4 weeks after progression stops – sinus tachycardia, other arrhythmias and labile BP absence of fever at onset of neuritic symptoms
GB: pathophysiology l postinfectious immune-mediated disease – Many of the identified infectious agents are thought to induce antibody production against specific gangliosides and glycolipids, such as GM 1 and GD 1 b, distributed throughout the myelin in the peripheral nervous system, e. g. Campylobacter jejuni infections l Result: Demyelination +/- axonal disruption
Respiratory dysfunction l l l impaired expiratory effort (cough) weakness of tongue and retropharyngeal muscles causes positional airway obstruction inspiratory muscle weakness increased risk of aspiration due to weakness of laryngeal and glottic muscles ventilatory drive and CO 2 response generally normal
Assessment of respiratory function l respiratory dysfunction may be compromised before clinical signs are clinically obvious l ventilatory muscle insufficiency may not correlate well with general neuromuscular examination

GB: serial assessment l l l l l respiratory rate paradoxical abdominal movement frequent changes in breathing pattern to alternate between major and accessory respiratory muscles use of accessory muscles during quiet breathing cough ability nasal speech difficulty with protruding tongue and difficulty swallowing (indicate bulbar involvement) atelectasis or pulmonary infiltrates on CXR maximum inspiratory force – < 20 cm H 2 O associated with high risk of ventilatory insufficiency – FVC < 15 ml/kg associated with increased risk of ventilatory failure – < 10 indicative of ventilatory failure ABG: changes occur late
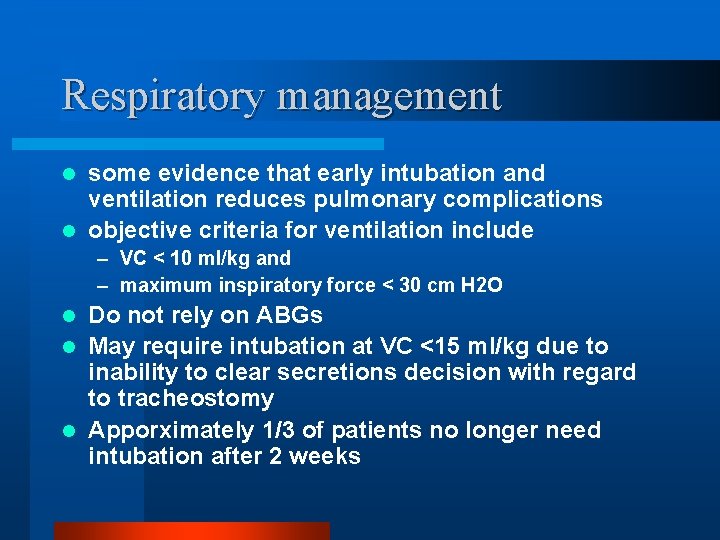
Respiratory management some evidence that early intubation and ventilation reduces pulmonary complications l objective criteria for ventilation include l – VC < 10 ml/kg and – maximum inspiratory force < 30 cm H 2 O Do not rely on ABGs l May require intubation at VC <15 ml/kg due to inability to clear secretions decision with regard to tracheostomy l Apporximately 1/3 of patients no longer need intubation after 2 weeks l

Thank you
 Berotec nebs
Berotec nebs Status asthmaticus
Status asthmaticus Pathophysiology definition
Pathophysiology definition Vent modes
Vent modes International severe asthma registry
International severe asthma registry Mild moderate severe asthma exacerbation
Mild moderate severe asthma exacerbation What is life
What is life Mild moderate severe asthma exacerbation
Mild moderate severe asthma exacerbation Unmet needs in severe asthma
Unmet needs in severe asthma Mild moderate severe asthma exacerbation
Mild moderate severe asthma exacerbation Malnutrition case presentation
Malnutrition case presentation Mechanical ventilation learning package
Mechanical ventilation learning package Mechanical ventilation indications
Mechanical ventilation indications Pip and peep
Pip and peep Mechanical ventilation 101
Mechanical ventilation 101 Peep in ventilator
Peep in ventilator Transairway pressure
Transairway pressure Tactical ventilation
Tactical ventilation Malampti
Malampti Iron lung
Iron lung Dope in mechanical ventilation
Dope in mechanical ventilation Actual mechanical advantage vs ideal mechanical advantage
Actual mechanical advantage vs ideal mechanical advantage Bouncing ball in scratch
Bouncing ball in scratch Wmo severe weather
Wmo severe weather Dka criteria
Dka criteria Mild moderate severe dehydration
Mild moderate severe dehydration Severe hypocalcemia
Severe hypocalcemia Severe combined immunodeficiency
Severe combined immunodeficiency Severe obesity
Severe obesity Severe dehydration
Severe dehydration Severe npdr definition
Severe npdr definition A 23 year old male experienced severe head trauma
A 23 year old male experienced severe head trauma Fluid of choice in severe dehydration
Fluid of choice in severe dehydration Severe weather safety precautions worksheet
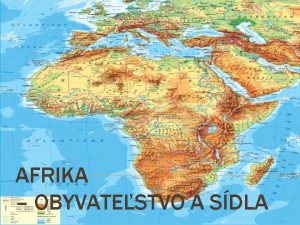
Severe weather safety precautions worksheet Najredšie osídlené oblasti afriky
Najredšie osídlené oblasti afriky Potassium dose calculation
Potassium dose calculation Wmo severe weather
Wmo severe weather Dehydration in malnutrition
Dehydration in malnutrition Chapter 16 section 1 water in the air answer key
Chapter 16 section 1 water in the air answer key Severe hypocalcemia
Severe hypocalcemia Bowl in medical term
Bowl in medical term Match the description with the example whmis
Match the description with the example whmis Bill nye thunderstorms
Bill nye thunderstorms Carbonic anhydrase use
Carbonic anhydrase use Severe angle blocking
Severe angle blocking What causes metabolic acidosis
What causes metabolic acidosis Katrine zhiroff
Katrine zhiroff Hyponatremia correction formula pdf
Hyponatremia correction formula pdf Cholera
Cholera Vce stress
Vce stress Severe weather data inventory
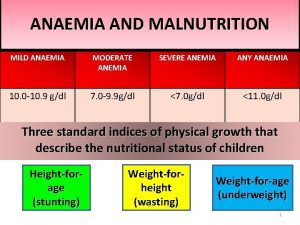
Severe weather data inventory Severe anemia
Severe anemia Chapter 20 weather patterns and severe storms
Chapter 20 weather patterns and severe storms Chapter 20 weather patterns and severe storms
Chapter 20 weather patterns and severe storms Anxiety headache
Anxiety headache Domina severe
Domina severe Severe pong game cards
Severe pong game cards Anemia tibc ferritin iron
Anemia tibc ferritin iron Serum osmolality
Serum osmolality Mild moderate severe dehydration
Mild moderate severe dehydration Laxative effect
Laxative effect Severe dehydration
Severe dehydration Severe adjective
Severe adjective Severe weather graphic organizer
Severe weather graphic organizer Severe ms heart
Severe ms heart Severe preeclampsia criteria
Severe preeclampsia criteria Phidian style
Phidian style