HYPOCALCEMIA Hasan AYDIN MD Hasan AYDIN Yeditepe University



- Slides: 43
HYPOCALCEMIA Hasan AYDIN, MD Hasan AYDIN Yeditepe University Medical Faculty Department of Endocrinology and Metabolism
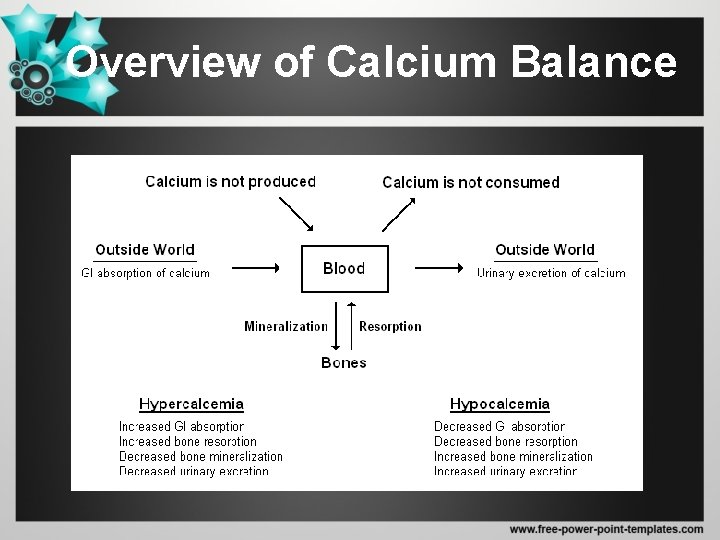
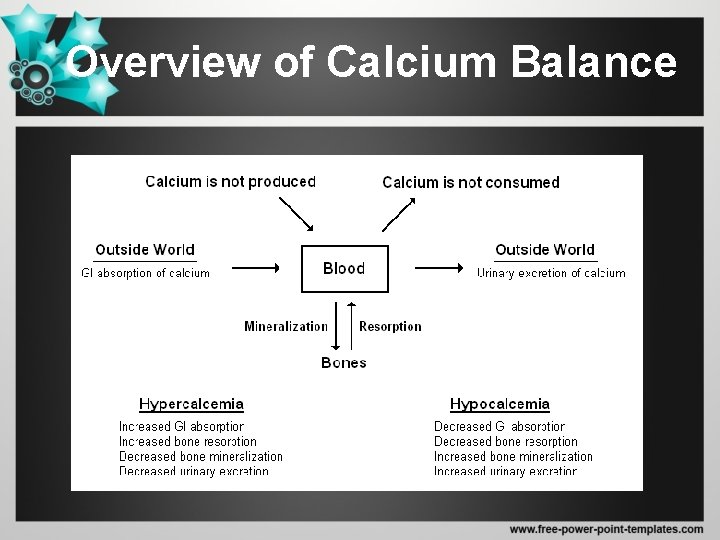
Overview of Calcium Balance
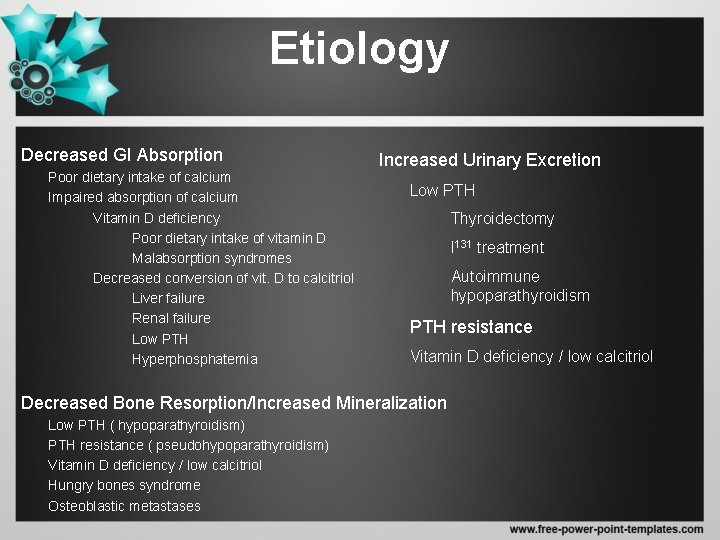
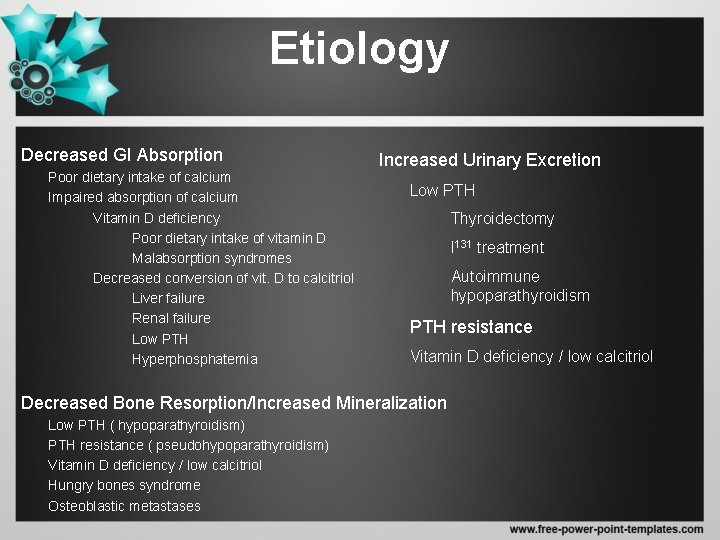
Etiology Decreased GI Absorption Poor dietary intake of calcium Impaired absorption of calcium Vitamin D deficiency Poor dietary intake of vitamin D Malabsorption syndromes Decreased conversion of vit. D to calcitriol Liver failure Renal failure Low PTH Hyperphosphatemia Increased Urinary Excretion Low PTH Thyroidectomy I 131 treatment Autoimmune hypoparathyroidism PTH resistance Vitamin D deficiency / low calcitriol Decreased Bone Resorption/Increased Mineralization Low PTH ( hypoparathyroidism) PTH resistance ( pseudohypoparathyroidism) Vitamin D deficiency / low calcitriol Hungry bones syndrome Osteoblastic metastases

Parathyroid Related Disorders – Absence of the parathyroid glands or of PTH • Congenital – – Di. George’s syndrome X-linked or autosomally inherited hypoparathyroidism Autoimmune polyglandular syndrome type I PTH gene mutations • Postsurgical hypoparathyroidism • Infiltrative disorders – Hemachromatosis – Wilson’s disease – Metastases • Hypoparathyroidism following radioactive iodine thyroid ablation – Impaired secretion of PTH • Hypomagnesemia • Respiratory alkalosis • Activating mutations of the calcium sensor – Target organ resistance • Hypomagnesemia • Pseudohypoparathyroidism (Type I and II)
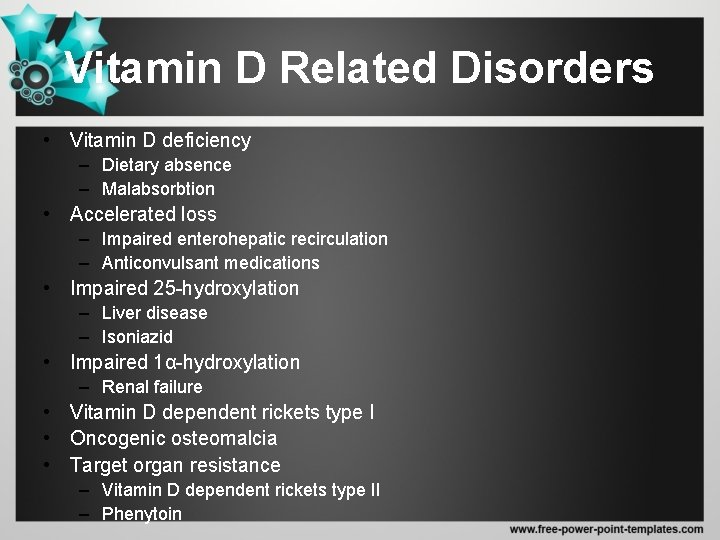
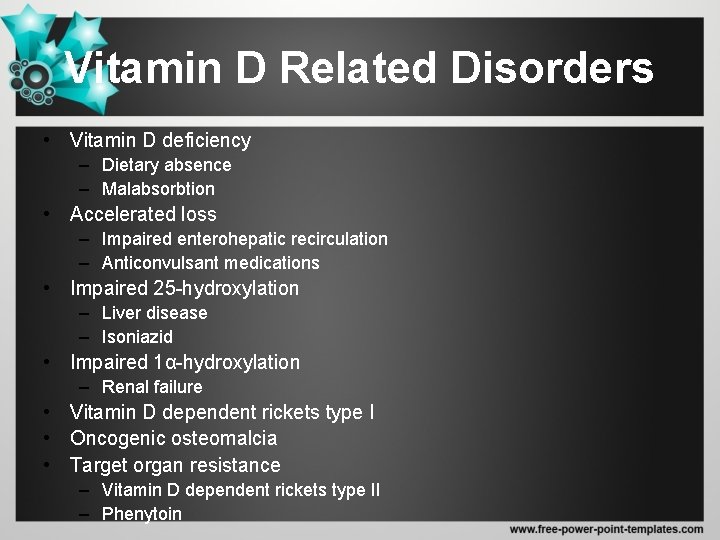
Vitamin D Related Disorders • Vitamin D deficiency – Dietary absence – Malabsorbtion • Accelerated loss – Impaired enterohepatic recirculation – Anticonvulsant medications • Impaired 25 -hydroxylation – Liver disease – Isoniazid • Impaired 1α-hydroxylation – Renal failure • Vitamin D dependent rickets type I • Oncogenic osteomalcia • Target organ resistance – Vitamin D dependent rickets type II – Phenytoin
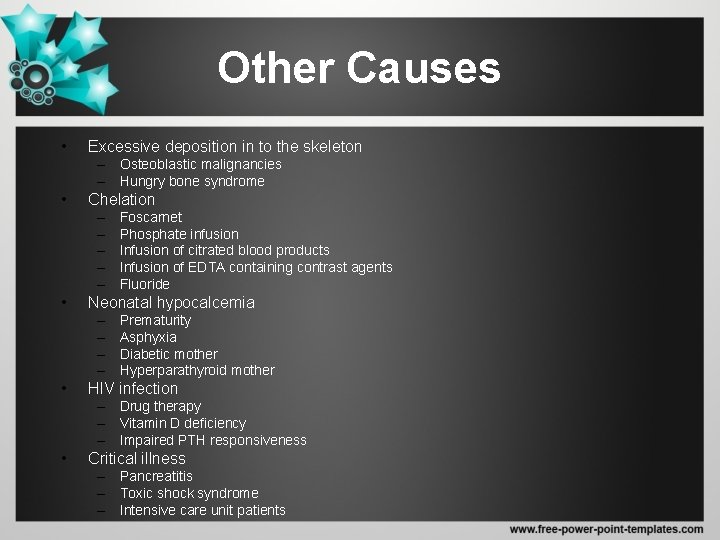
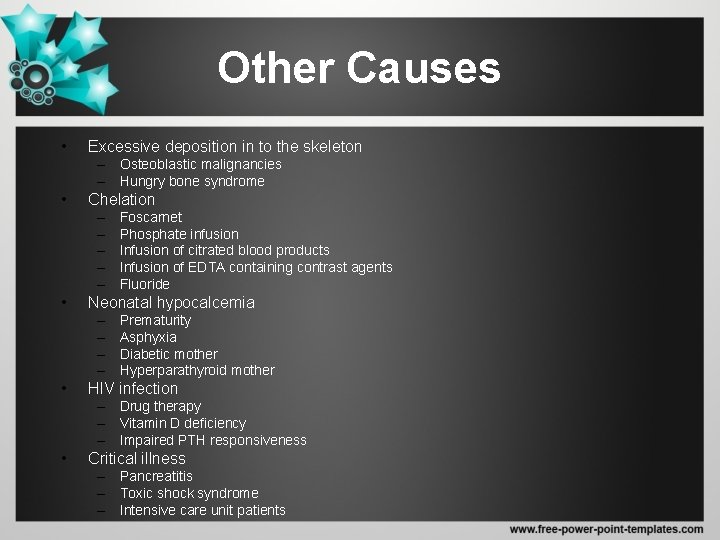
Other Causes • Excessive deposition in to the skeleton – Osteoblastic malignancies – Hungry bone syndrome • Chelation – – – • Neonatal hypocalcemia – – • Foscarnet Phosphate infusion Infusion of citrated blood products Infusion of EDTA containing contrast agents Fluoride Prematurity Asphyxia Diabetic mother Hyperparathyroid mother HIV infection – Drug therapy – Vitamin D deficiency – Impaired PTH responsiveness • Critical illness – Pancreatitis – Toxic shock syndrome – Intensive care unit patients
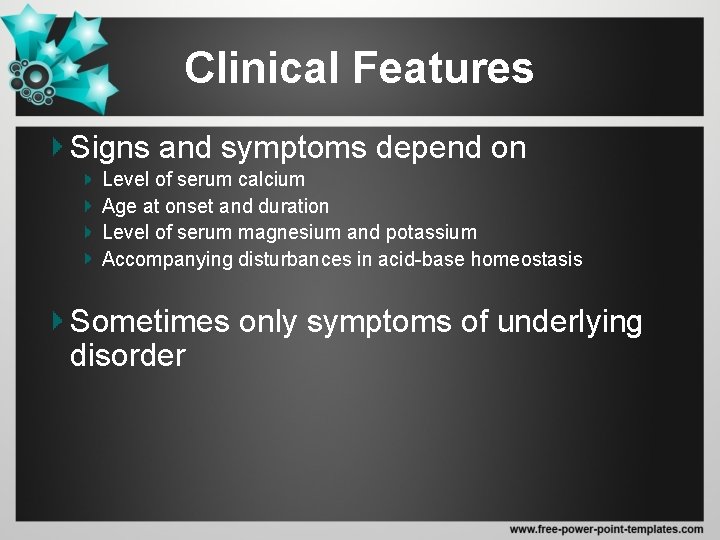
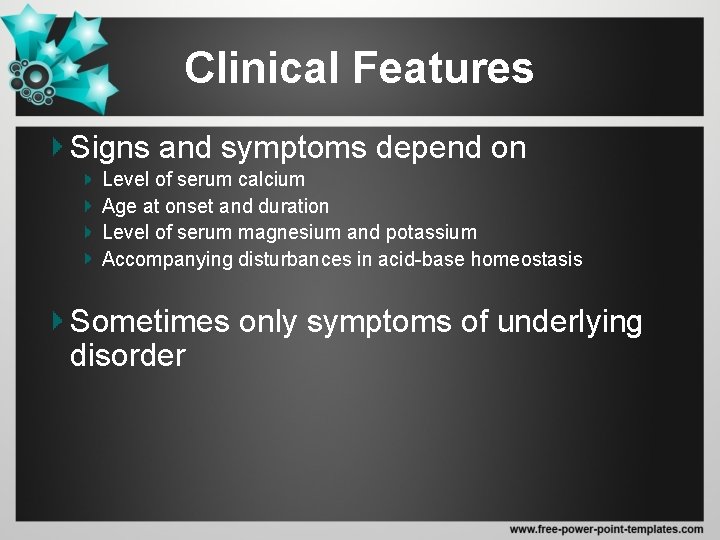
Clinical Features Signs and symptoms depend on Level of serum calcium Age at onset and duration Level of serum magnesium and potassium Accompanying disturbances in acid-base homeostasis Sometimes only symptoms of underlying disorder
Symptoms and Signs • Systemic – Confusion – Weakness – Mental retardation – Behavioral changes
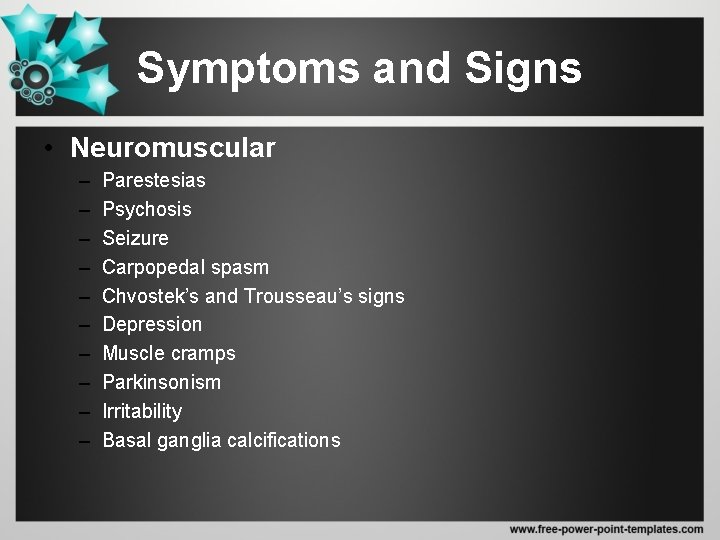
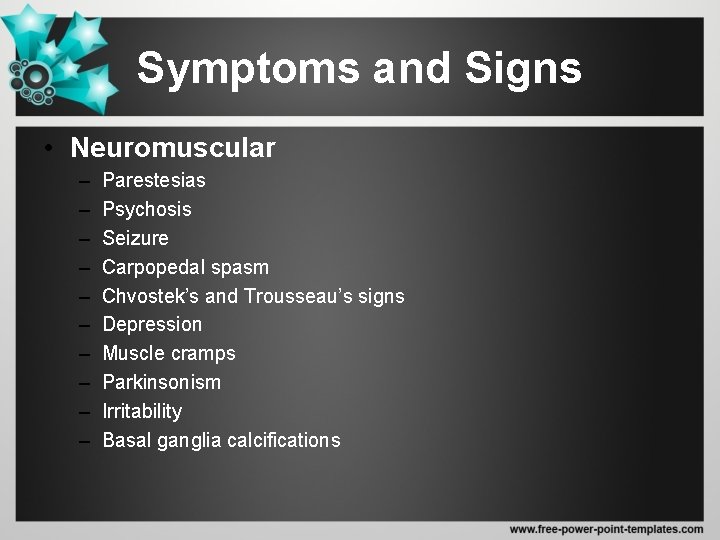
Symptoms and Signs • Neuromuscular – – – – – Parestesias Psychosis Seizure Carpopedal spasm Chvostek’s and Trousseau’s signs Depression Muscle cramps Parkinsonism Irritability Basal ganglia calcifications
Syptoms and Signs • Cardiac – Prolonged QT interval – T wave changes – Congestive heart failure l Ocular Cataracts
Syptoms and Signs • Dental – Enamel hypoplasia of teeth – Defective root formation – Failure of adult tooth to erupt l Respiratory Laryngospasm Bronchspasm Stridor
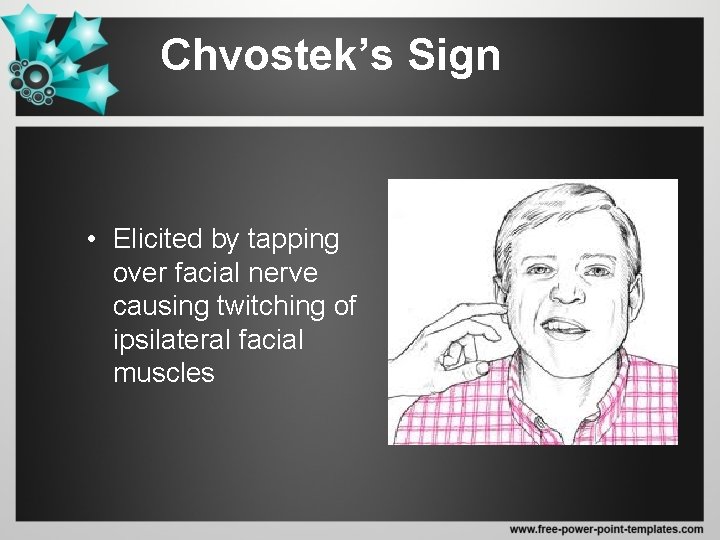
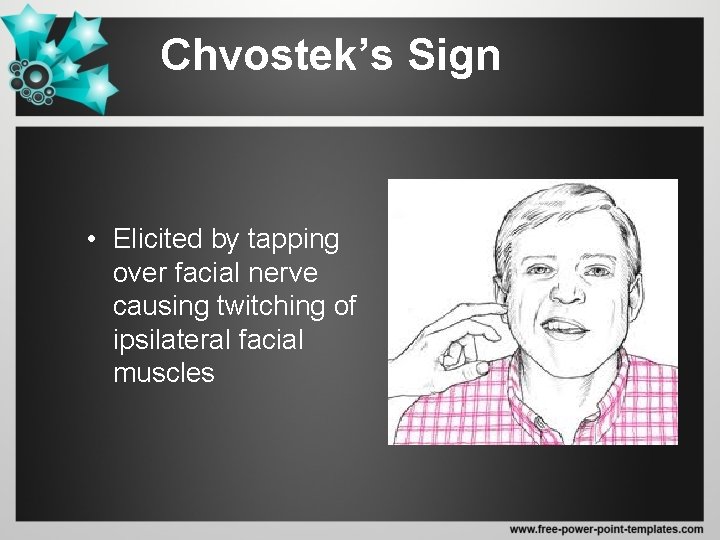
Chvostek’s Sign • Elicited by tapping over facial nerve causing twitching of ipsilateral facial muscles
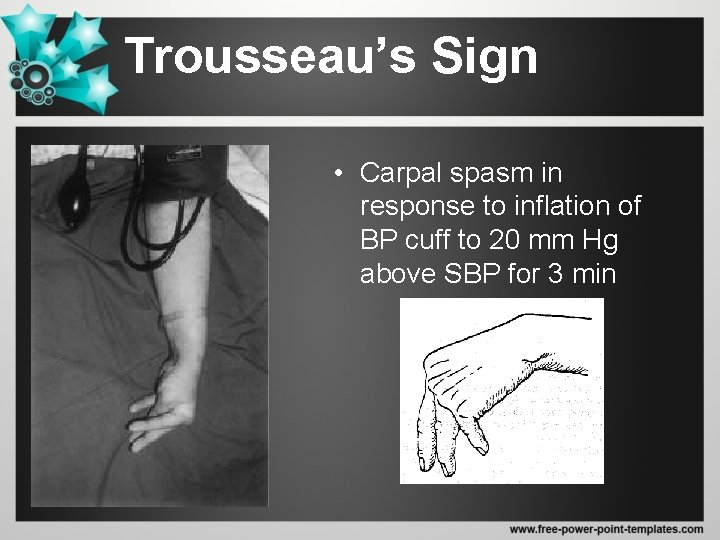
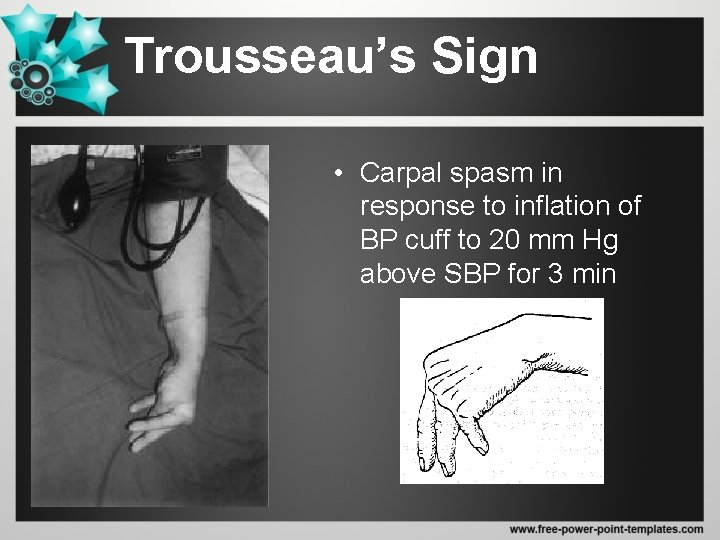
Trousseau’s Sign • Carpal spasm in response to inflation of BP cuff to 20 mm Hg above SBP for 3 min
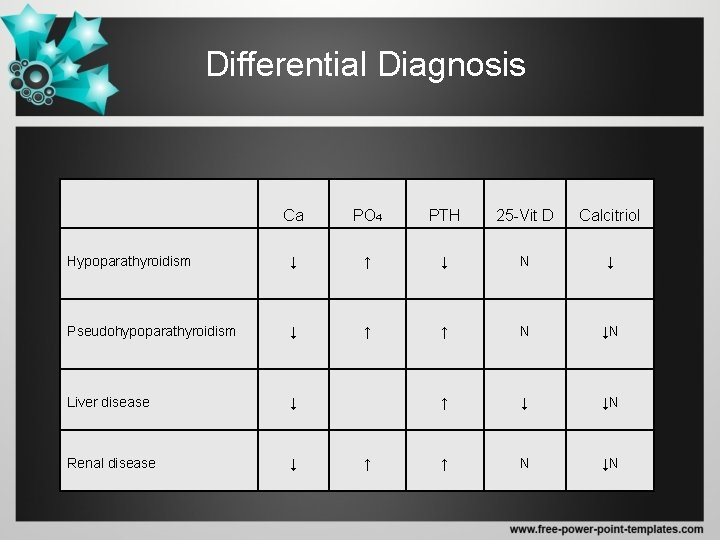
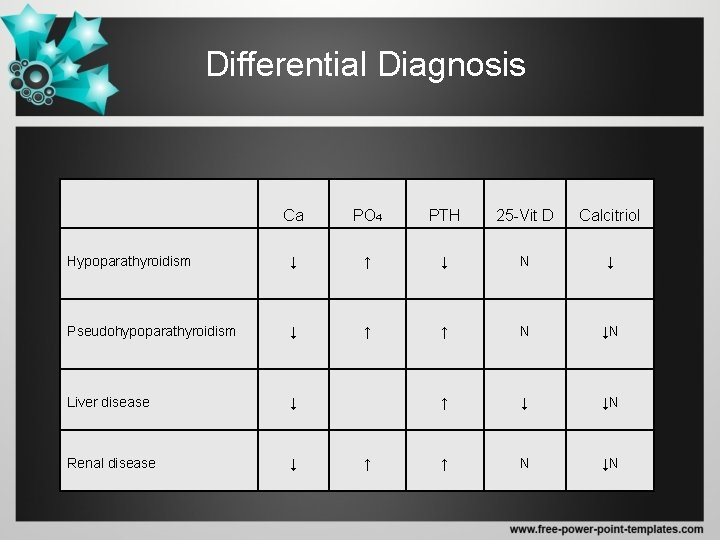
Differential Diagnosis Ca PO 4 PTH 25 -Vit D Calcitriol Hypoparathyroidism ↓ ↑ ↓ N ↓ Pseudohypoparathyroidism ↓ ↑ ↑ N ↓N Liver disease ↓ ↑ ↓ ↓N Renal disease ↓ ↑ N ↓N ↑
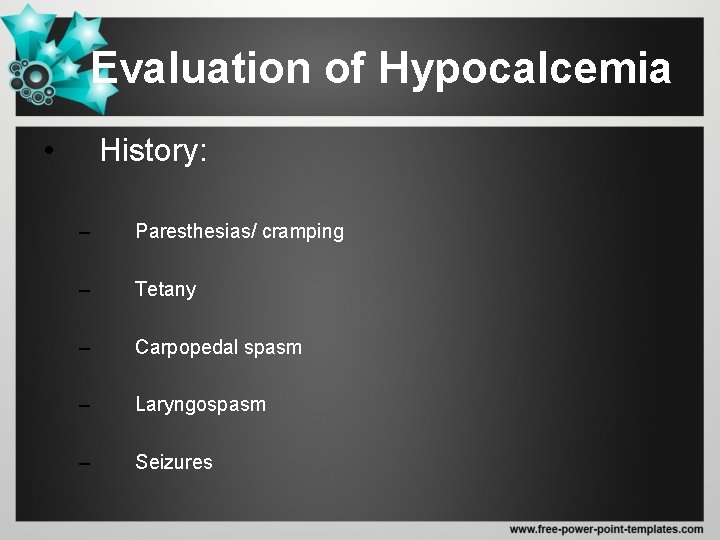
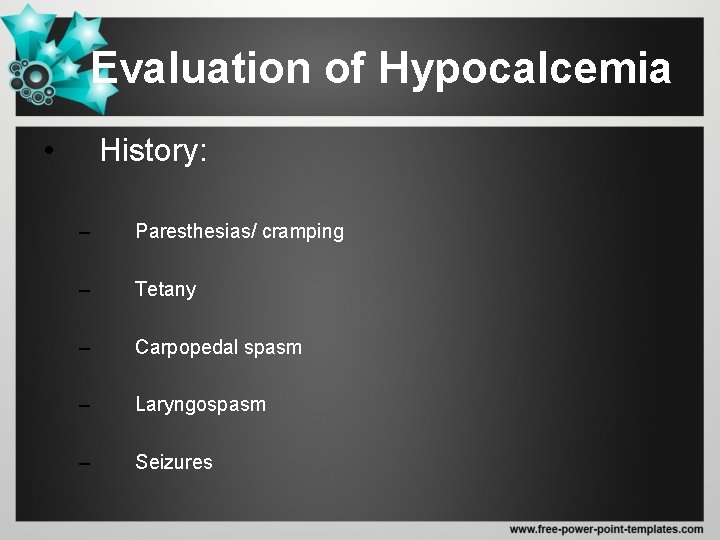
Evaluation of Hypocalcemia • History: – Paresthesias/ cramping – Tetany – Carpopedal spasm – Laryngospasm – Seizures
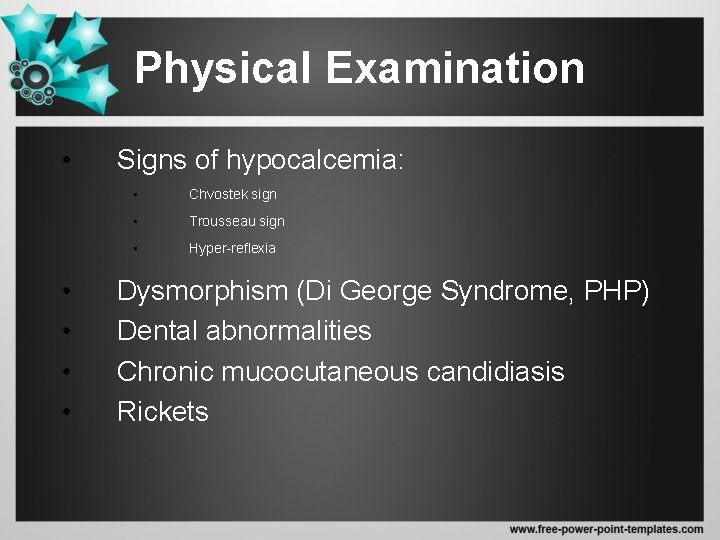
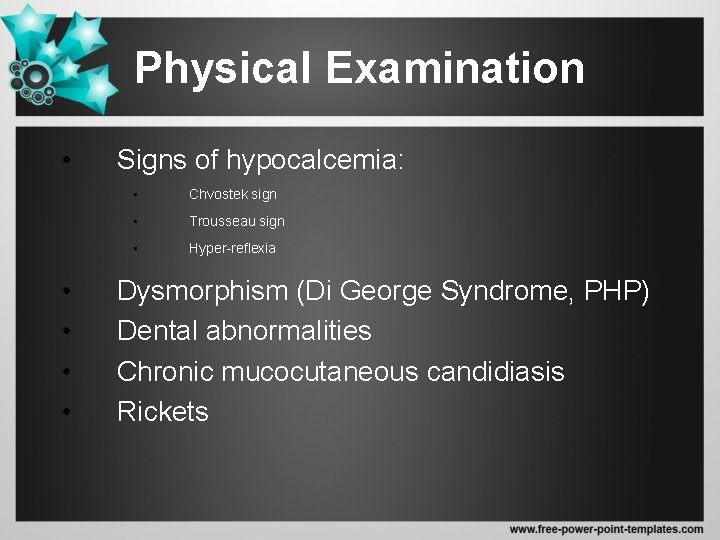
Physical Examination • • • Signs of hypocalcemia: • Chvostek sign • Trousseau sign • Hyper-reflexia Dysmorphism (Di George Syndrome, PHP) Dental abnormalities Chronic mucocutaneous candidiasis Rickets
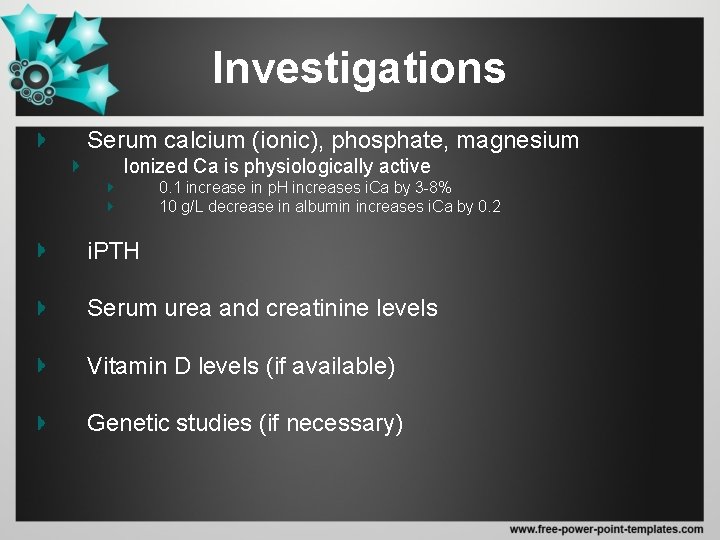
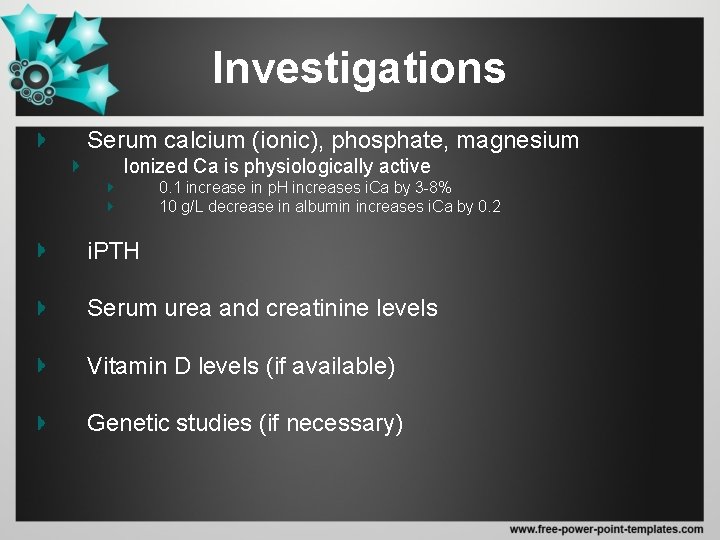
Investigations Serum calcium (ionic), phosphate, magnesium Ionized Ca is physiologically active 0. 1 increase in p. H increases i. Ca by 3 -8% 10 g/L decrease in albumin increases i. Ca by 0. 2 i. PTH Serum urea and creatinine levels Vitamin D levels (if available) Genetic studies (if necessary)
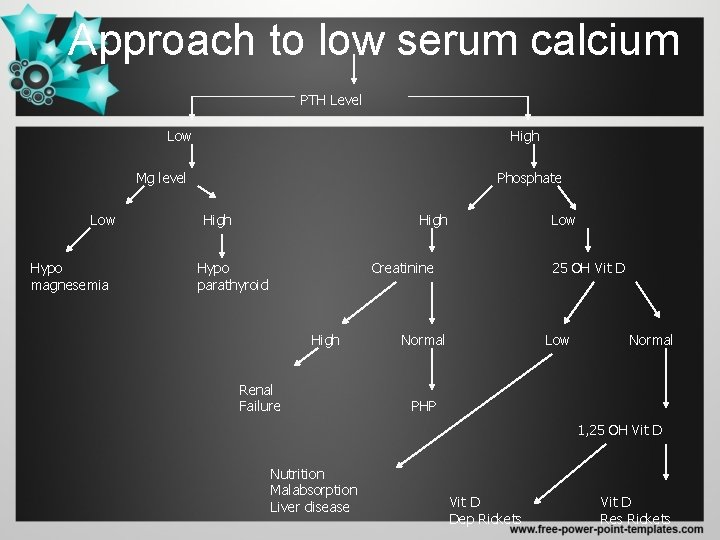
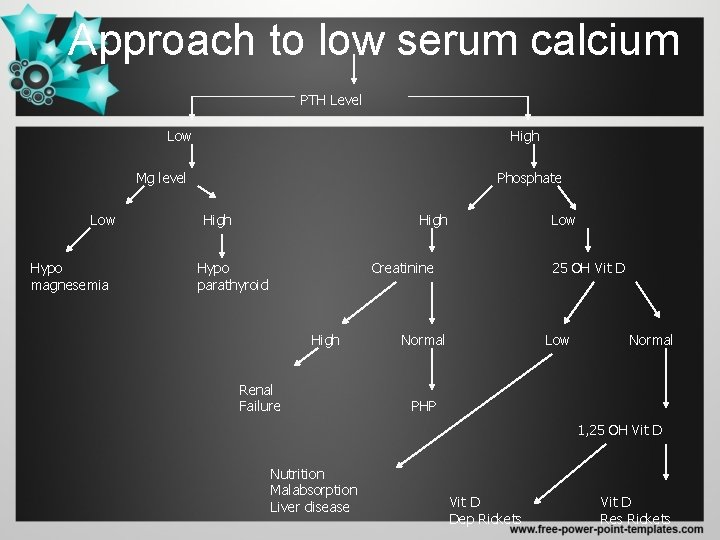
Approach to low serum calcium PTH Level Low High Mg level Low Hypo magnesemia Phosphate High Hypo parathyroid Low Creatinine High Renal Failure 25 OH Vit D Normal Low Normal PHP 1, 25 OH Vit D Nutrition Malabsorption Liver disease Vit D Dep Rickets Vit D Res Rickets
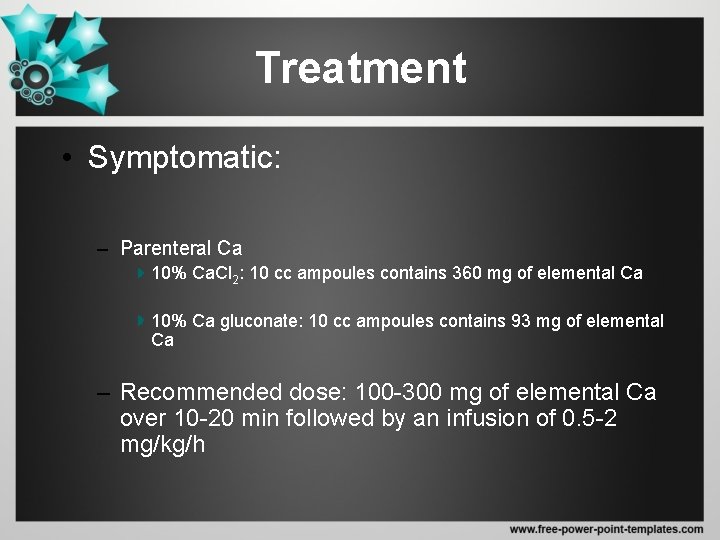
Treatment • Symptomatic: – Parenteral Ca 10% Ca. Cl 2: 10 cc ampoules contains 360 mg of elemental Ca 10% Ca gluconate: 10 cc ampoules contains 93 mg of elemental Ca – Recommended dose: 100 -300 mg of elemental Ca over 10 -20 min followed by an infusion of 0. 5 -2 mg/kg/h
Treatment • Side effects: – Nausea – Vomiting – Flushing – Hypertension – Bradycardia, heart block (patients should be monitored)
Treatment • Asymptomatic – Oral Ca supplementation • 1 -4 g/day in divided doses • If patient has concurrent hypomagnesemia, Ca replacement alone will not correct hypocalcemia unless Mg is also replaced (2 -4 g IV for symptomatic patients)
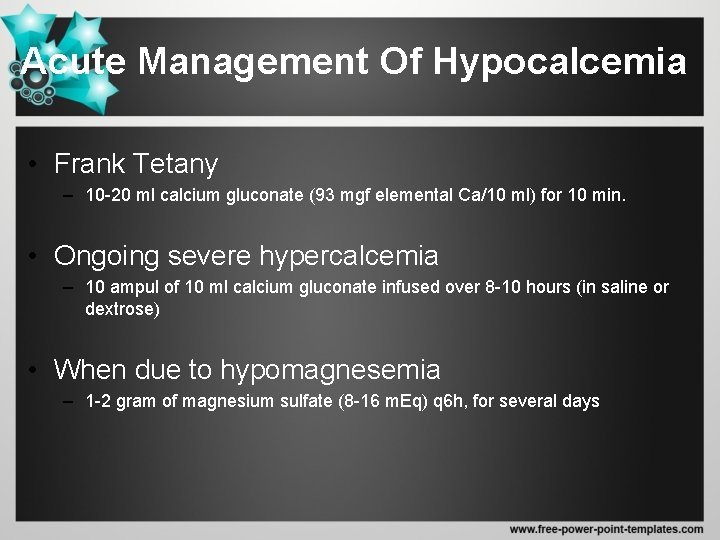
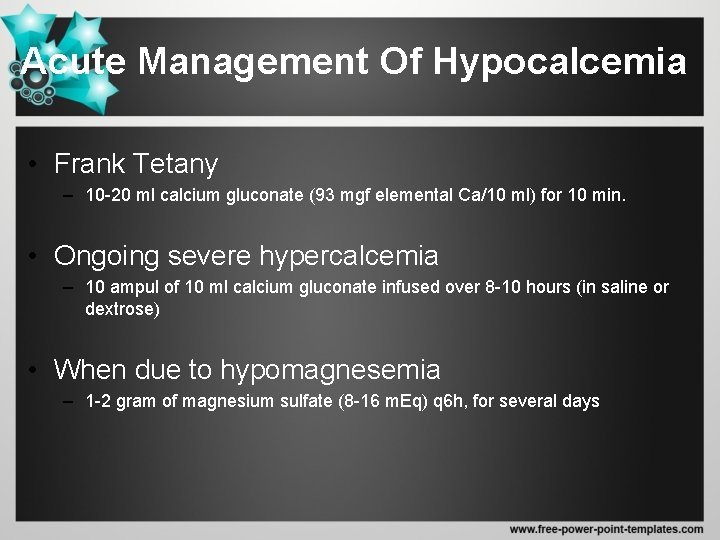
Acute Management Of Hypocalcemia • Frank Tetany – 10 -20 ml calcium gluconate (93 mgf elemental Ca/10 ml) for 10 min. • Ongoing severe hypercalcemia – 10 ampul of 10 ml calcium gluconate infused over 8 -10 hours (in saline or dextrose) • When due to hypomagnesemia – 1 -2 gram of magnesium sulfate (8 -16 m. Eq) q 6 h, for several days
SPECIFIC CAUSES OF HYPOCALCEMIA
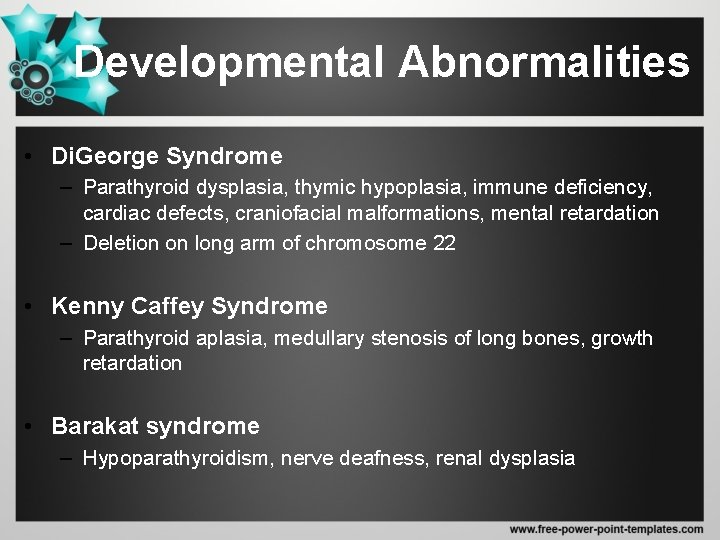
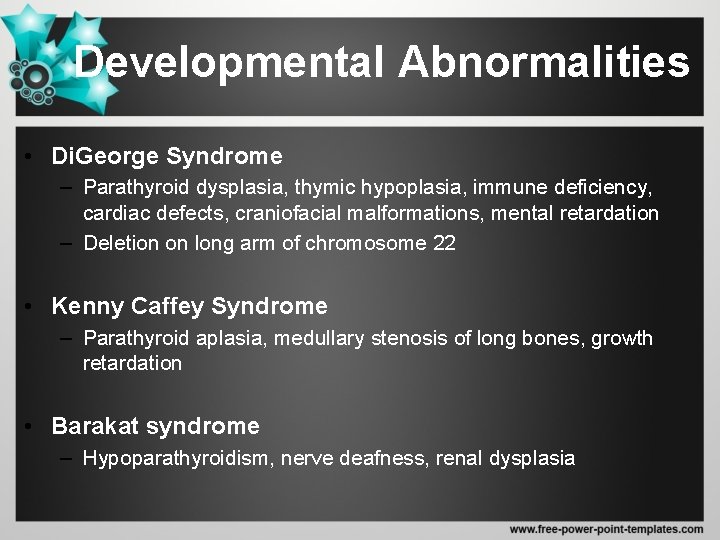
Developmental Abnormalities • Di. George Syndrome – Parathyroid dysplasia, thymic hypoplasia, immune deficiency, cardiac defects, craniofacial malformations, mental retardation – Deletion on long arm of chromosome 22 • Kenny Caffey Syndrome – Parathyroid aplasia, medullary stenosis of long bones, growth retardation • Barakat syndrome – Hypoparathyroidism, nerve deafness, renal dysplasia
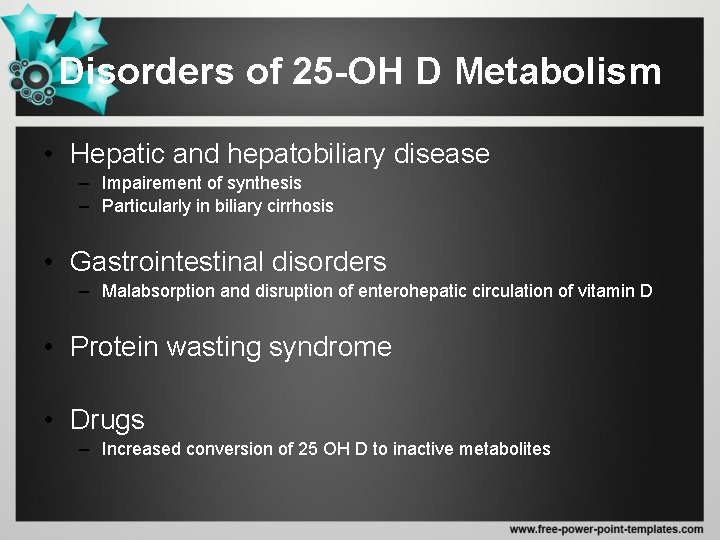
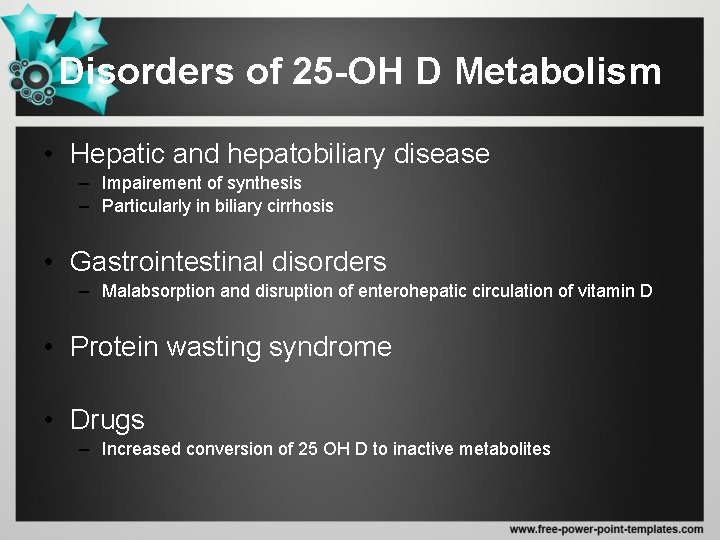
Disorders of 25 -OH D Metabolism • Hepatic and hepatobiliary disease – Impairement of synthesis – Particularly in biliary cirrhosis • Gastrointestinal disorders – Malabsorption and disruption of enterohepatic circulation of vitamin D • Protein wasting syndrome • Drugs – Increased conversion of 25 OH D to inactive metabolites

Disorders of 1, 25 -OH D Metabolism • Vitamin D dependent rickets type II • Vitamin D resistant rickets and osteomalacia • Hypercalciuric hypophosphatemic rickets • Tumor induced osteomalacia
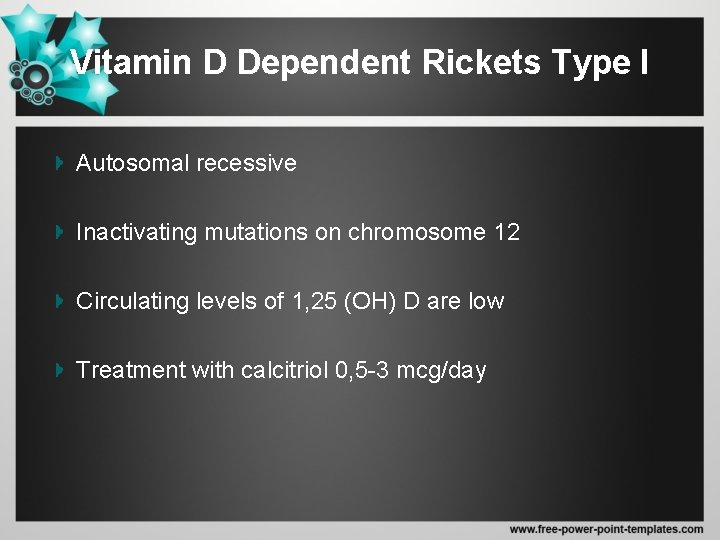
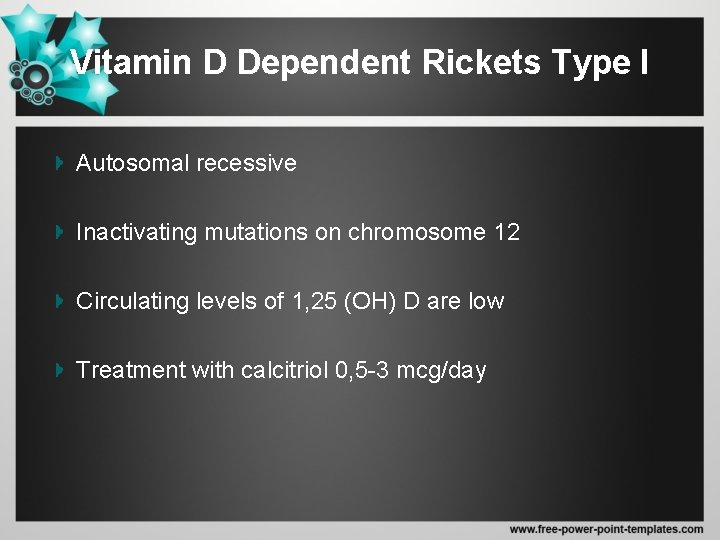
Vitamin D Dependent Rickets Type I Autosomal recessive Inactivating mutations on chromosome 12 Circulating levels of 1, 25 (OH) D are low Treatment with calcitriol 0, 5 -3 mcg/day
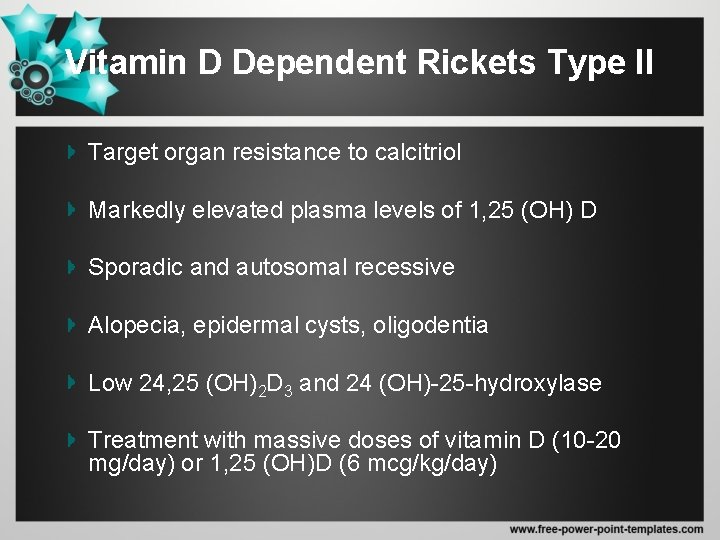
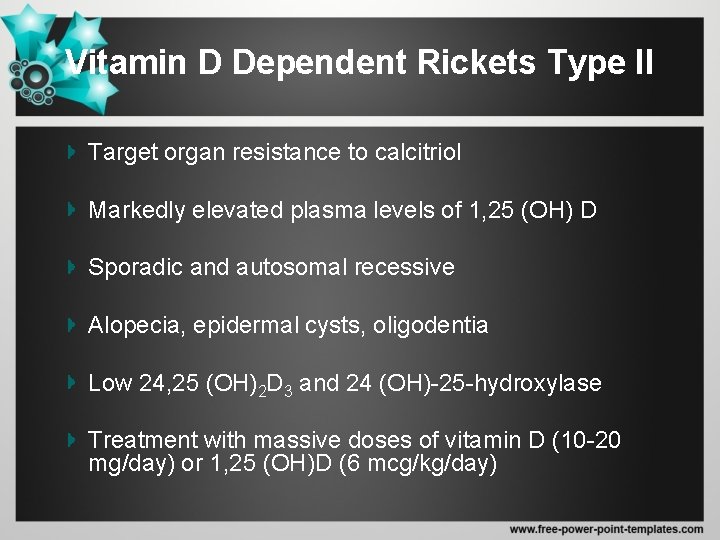
Vitamin D Dependent Rickets Type II Target organ resistance to calcitriol Markedly elevated plasma levels of 1, 25 (OH) D Sporadic and autosomal recessive Alopecia, epidermal cysts, oligodentia Low 24, 25 (OH)2 D 3 and 24 (OH)-25 -hydroxylase Treatment with massive doses of vitamin D (10 -20 mg/day) or 1, 25 (OH)D (6 mcg/kg/day)
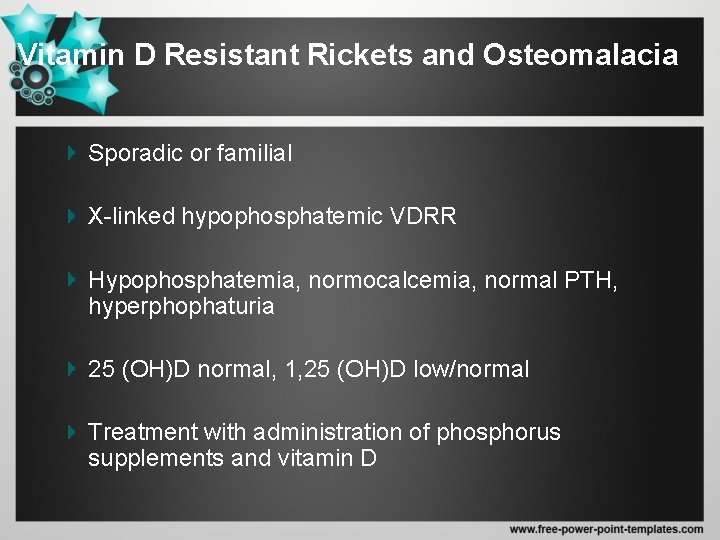
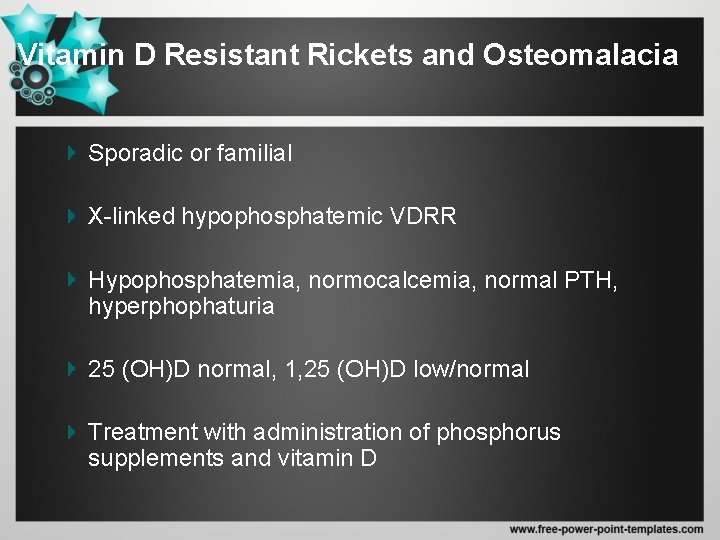
Vitamin D Resistant Rickets and Osteomalacia Sporadic or familial X-linked hypophosphatemic VDRR Hypophosphatemia, normocalcemia, normal PTH, hyperphophaturia 25 (OH)D normal, 1, 25 (OH)D low/normal Treatment with administration of phosphorus supplements and vitamin D
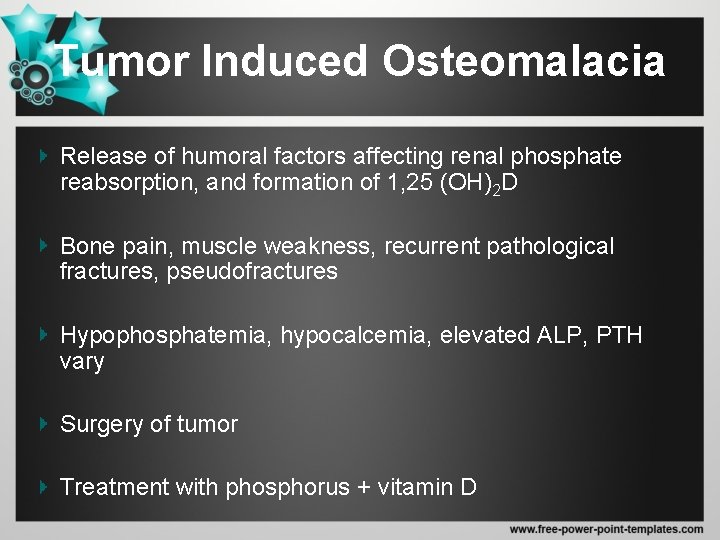
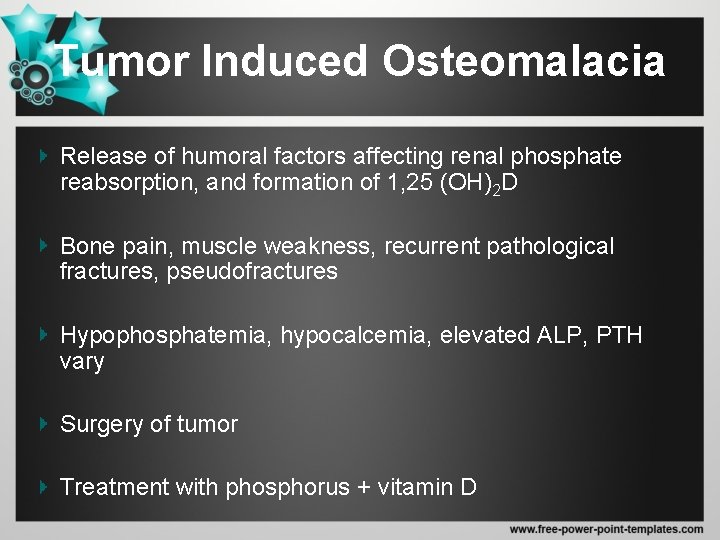
Tumor Induced Osteomalacia Release of humoral factors affecting renal phosphate reabsorption, and formation of 1, 25 (OH)2 D Bone pain, muscle weakness, recurrent pathological fractures, pseudofractures Hypophosphatemia, hypocalcemia, elevated ALP, PTH vary Surgery of tumor Treatment with phosphorus + vitamin D
Hypoparathyroidism • Clinically – Symptoms of neuromuscular hyperactivity • Biochemically – hypocalcemia, – hyperphosphatemia, – diminished to absent circulating i. PTH.
Etiology • Surgical hypoparathyroidism (most common) • Familial hypoparathyroidism • Idiopathic hypoparathyroidism • Functional hypoparathyroidism
Functional Hypoparathyroidism • long periods of hypomagnesemia – selective gastrointestinal magnesium absorption defects – generalized gastrointestinal malabsorption – alcoholism. • Serum PTH low • Hypocalcemia • Mg is required for PTH release • Mg is probably also required for the peripheral action of PTH
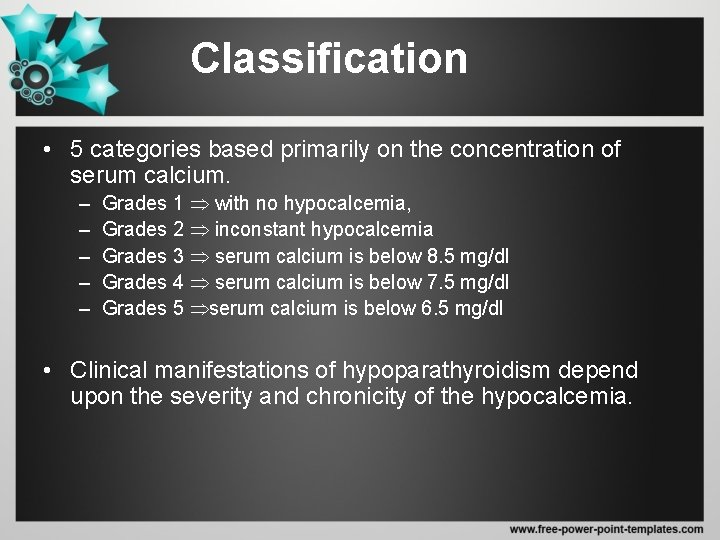
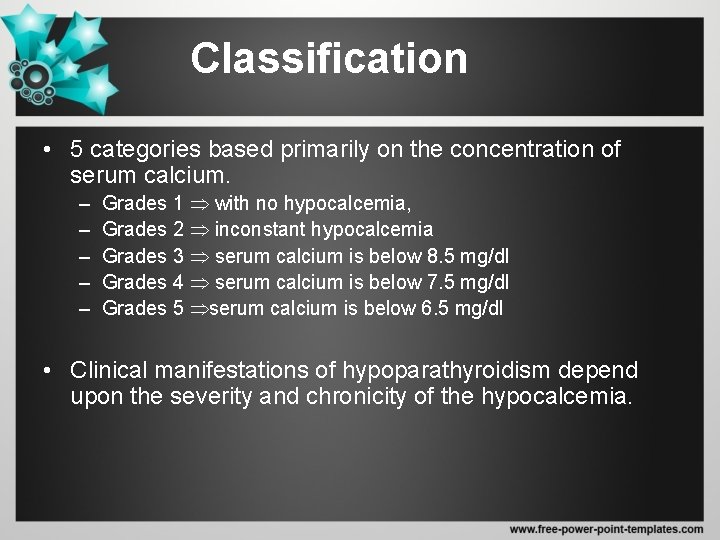
Classification • 5 categories based primarily on the concentration of serum calcium. – – – Grades 1 with no hypocalcemia, Grades 2 inconstant hypocalcemia Grades 3 serum calcium is below 8. 5 mg/dl Grades 4 serum calcium is below 7. 5 mg/dl Grades 5 serum calcium is below 6. 5 mg/dl • Clinical manifestations of hypoparathyroidism depend upon the severity and chronicity of the hypocalcemia.
Treatment • Physiologic replacement of PTH. • Pharmacologic doses of vitamin D – (ergocalciferol or its more potent analog dihydrotachysterol, in combination with oral calcium administration) • Diets low in phosphate (restriction of dairy products and meat) and oral aluminum hydroxide gels
PTH Resistance Syndromes
Etiology of Pseudohypoparathyroidism • abnormal target tissue responses – receptor binding of the hormone – final expression of the cellular actions of PTH • resistance to several other hormones (vasopressin, glucagon). • secretion of a biologically inert form of PTH, • circulating inhibitors of PTH action, • an intrinsic abnormality of PTH receptors, • autoantibodies to the PTH receptor,
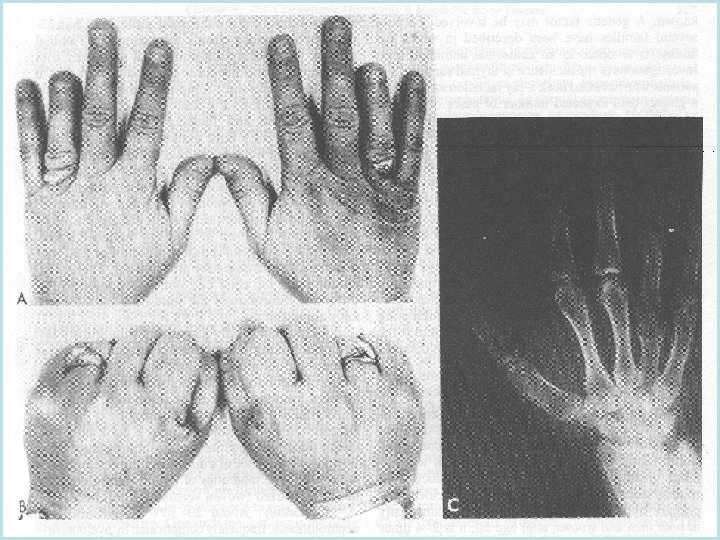
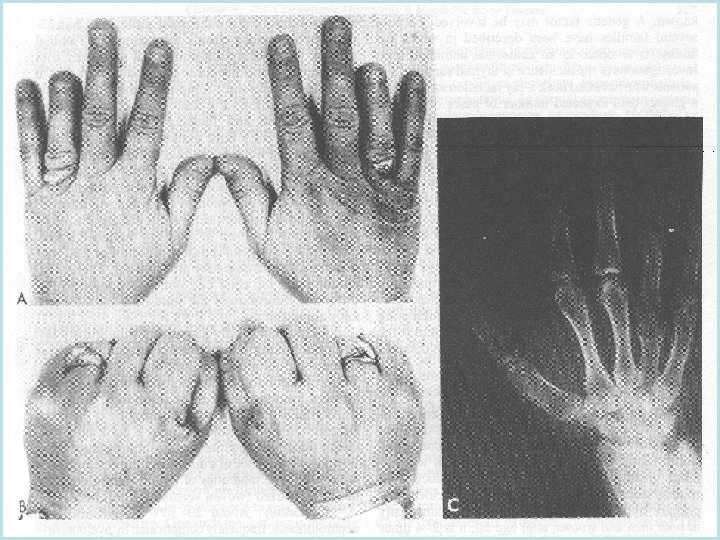
Pseudohypoparathyroidism • Rare familial disorder • Target tissue resistance to PTH, • Hypocalcemia, hyperphosphatemia • Increased parathyroid gland function, • Short stature and short metacarpal and metatarsal bones.
Ps. HP Type Ia (Albright Syndrome) • Hypoparatrhyroidism, short stature, round facies, obesity, brachydactily, neck webbing, sc calcifications • Defect in the function of Gs protein • TSH, Glucagon, Gonadotropin resintance • Autosomal dominant • Intermittant hypocalcemia, elevated PTH, low urine Ca
Pseudopseudohypoparathyroidism • developmental defects • without the biochemical abnormalities of pseudohypoparathyroidism. • lack evidence of PTH resistance • 50% reduction in Gs alpha function • Autosomal dominant
Pseudoidiopathic hypoparathyroidism • Structurally abnormal form of PTH present • Fail to respond to own PTH • Normal response to exogenous PTH
