Ventilation 1212022 Ventilation 1 Pulmonary Ventilation Tidal volume


- Slides: 98
Ventilation 1/21/2022 Ventilation 1
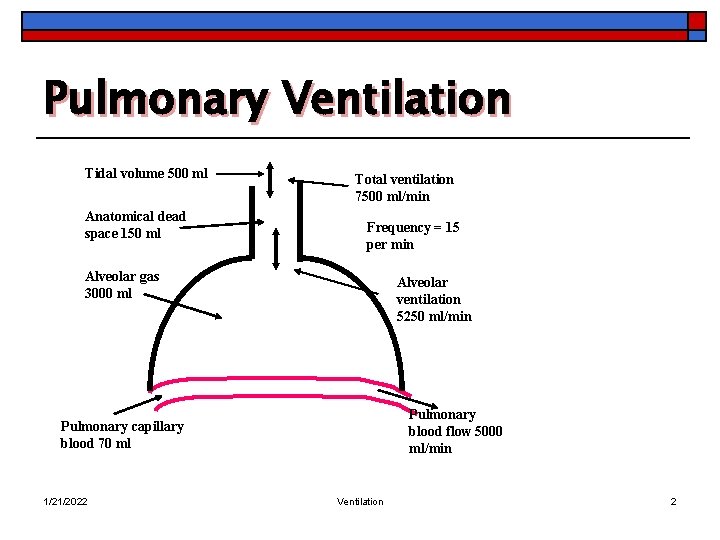
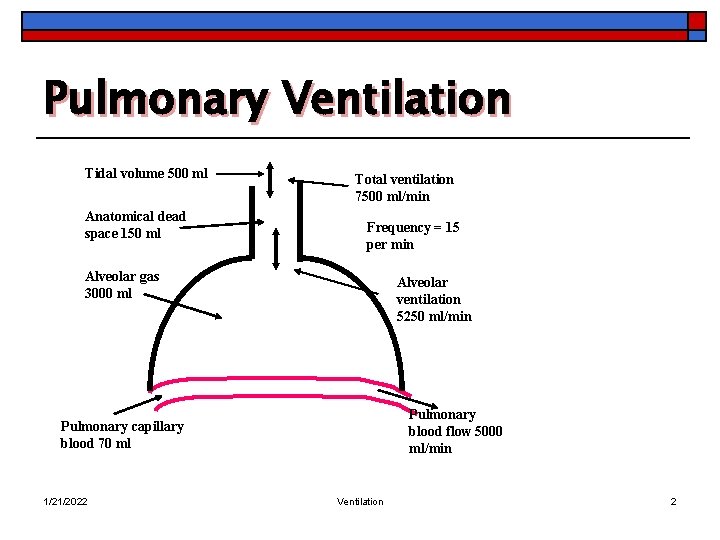
Pulmonary Ventilation Tidal volume 500 ml Anatomical dead space 150 ml Total ventilation 7500 ml/min Frequency = 15 per min Alveolar gas 3000 ml Alveolar ventilation 5250 ml/min Pulmonary blood flow 5000 ml/min Pulmonary capillary blood 70 ml 1/21/2022 Ventilation 2

Pulmonary Ventilation o Minute ventilation (VE) n Volume of air inspired or expired per minute o o n 1/21/2022 Depends on the frequency (f) Depth of breathing (tidal volume, VT) VE = ( VT * f) Ventilation 3
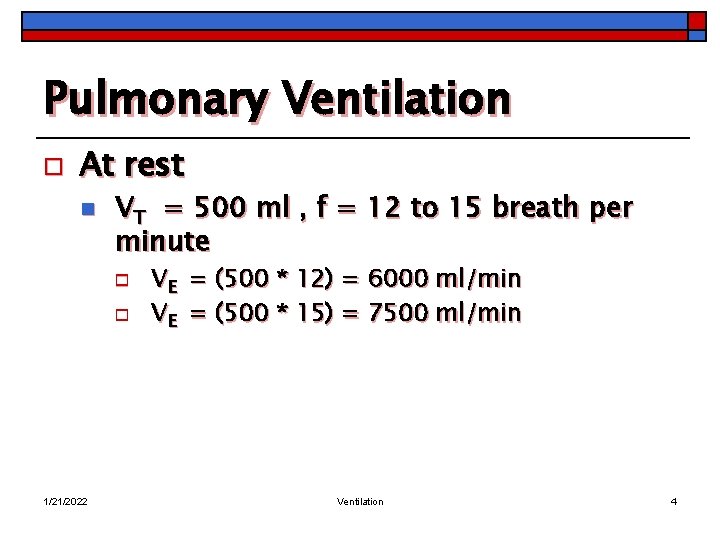
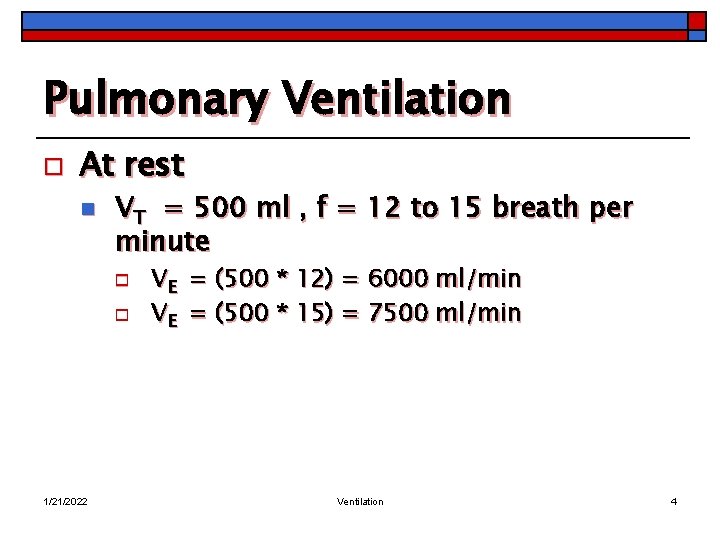
Pulmonary Ventilation o At rest n VT = 500 ml , f = 12 to 15 breath per minute o o 1/21/2022 VE = (500 * 12) = 6000 ml/min VE = (500 * 15) = 7500 ml/min Ventilation 4
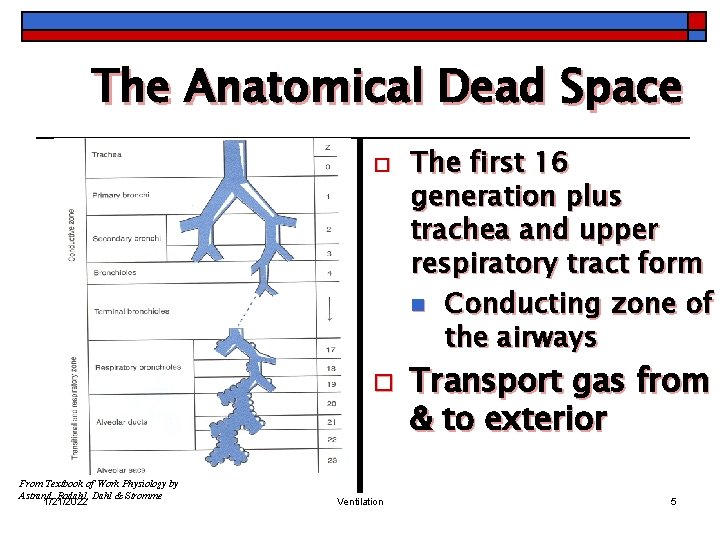
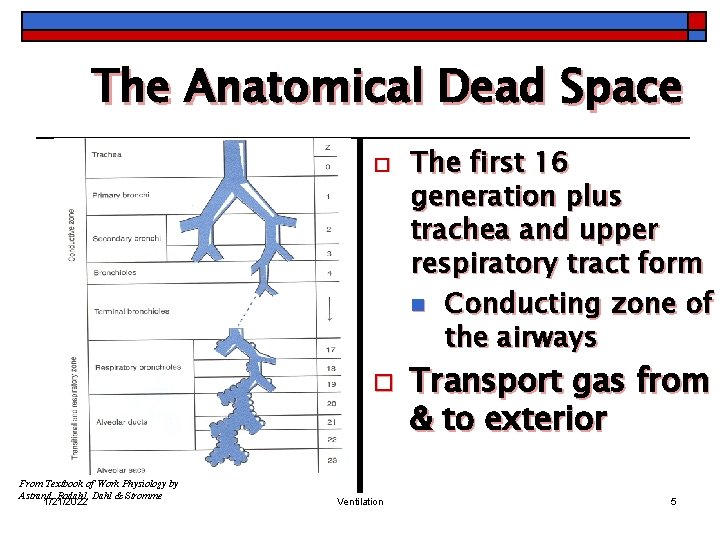
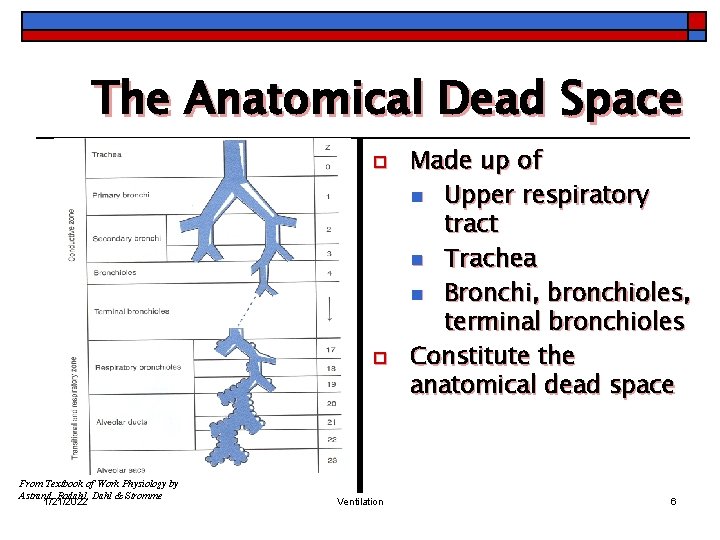
The Anatomical Dead Space o o From Textbook of Work Physiology by Astrand, Rodahl, Dahl & Stromme 1/21/2022 Ventilation The first 16 generation plus trachea and upper respiratory tract form n Conducting zone of the airways Transport gas from & to exterior 5
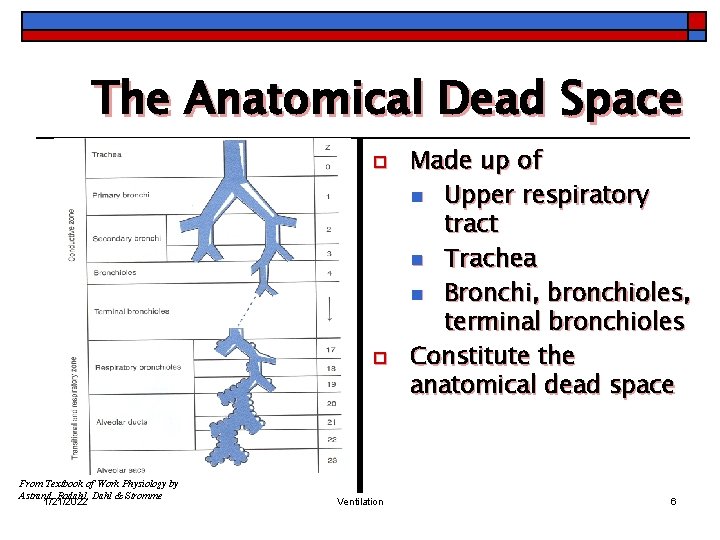
The Anatomical Dead Space o o From Textbook of Work Physiology by Astrand, Rodahl, Dahl & Stromme 1/21/2022 Ventilation Made up of n Upper respiratory tract n Trachea n Bronchi, bronchioles, terminal bronchioles Constitute the anatomical dead space 6
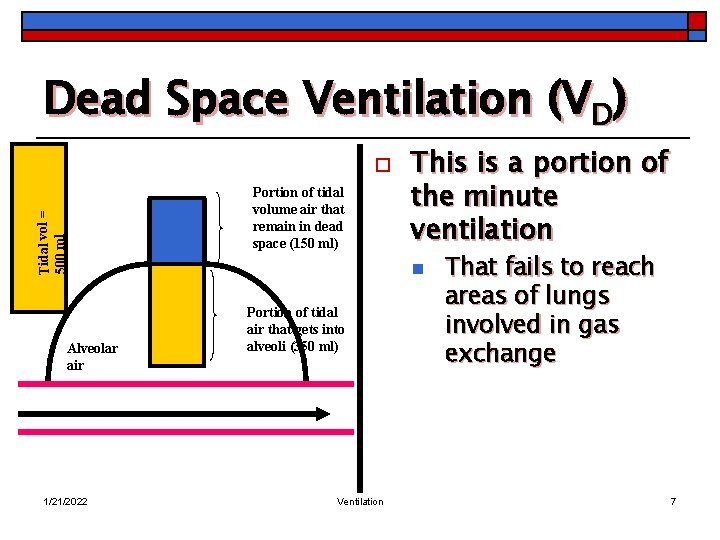
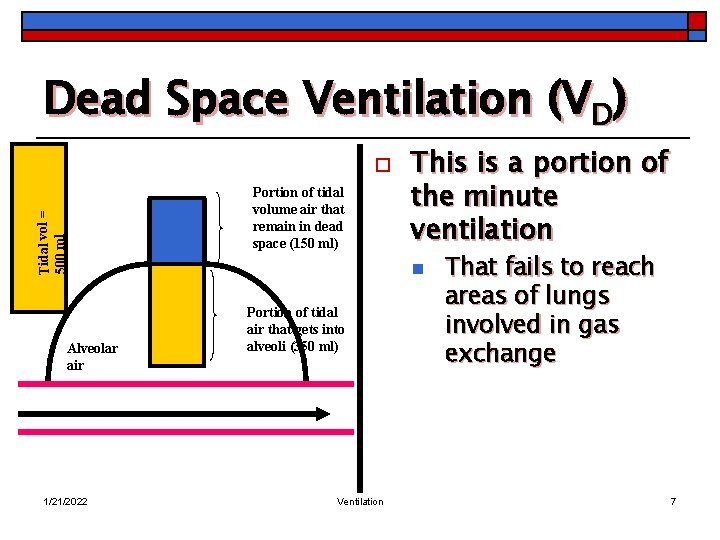
Dead Space Ventilation (VD) Tidal vol = 500 ml o Alveolar air 1/21/2022 Portion of tidal volume air that remain in dead space (150 ml) This is a portion of the minute ventilation n Portion of tidal air that gets into alveoli (350 ml) Ventilation That fails to reach areas of lungs involved in gas exchange 7
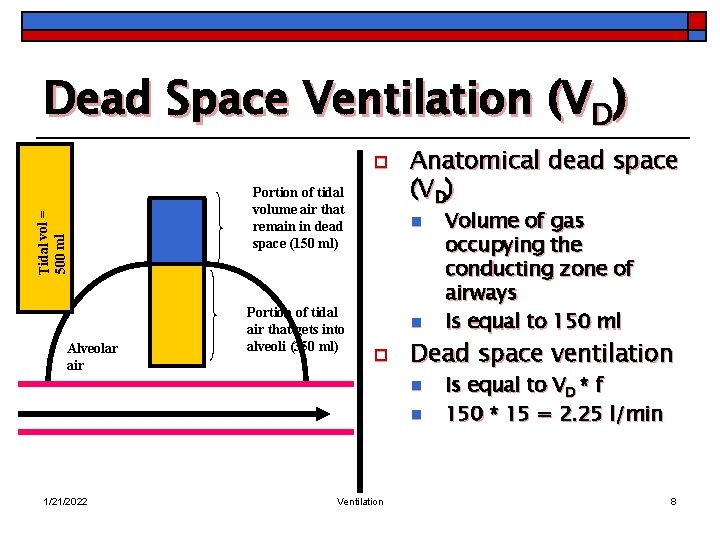
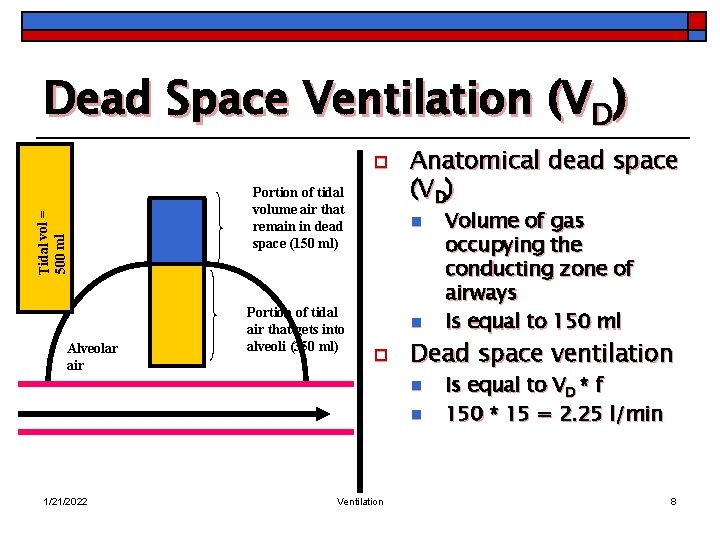
Dead Space Ventilation (VD) Tidal vol = 500 ml o Alveolar air Portion of tidal volume air that remain in dead space (150 ml) Portion of tidal air that gets into alveoli (350 ml) Anatomical dead space (VD) n n o Dead space ventilation n n 1/21/2022 Ventilation Volume of gas occupying the conducting zone of airways Is equal to 150 ml Is equal to VD * f 150 * 15 = 2. 25 l/min 8
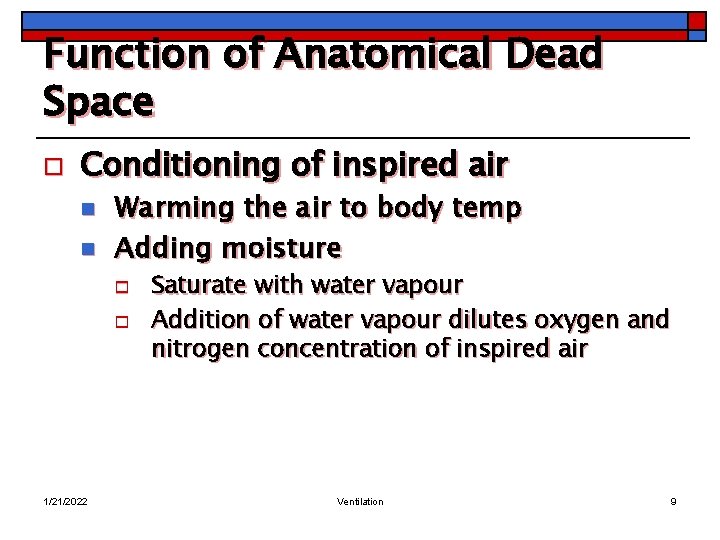
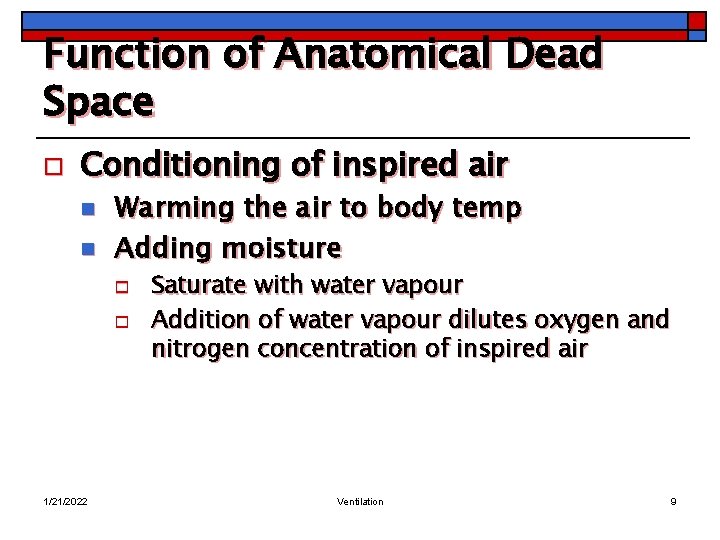
Function of Anatomical Dead Space o Conditioning of inspired air n n Warming the air to body temp Adding moisture o o 1/21/2022 Saturate with water vapour Addition of water vapour dilutes oxygen and nitrogen concentration of inspired air Ventilation 9
Function of Anatomical Dead Space o o Removal of foreign material Foreign particles n n n o Filtered by nose Impacted in lower airways Dissolved on moist surface of airways Small particles (soot, pollen) n 1/21/2022 Impact on the surface of the airways Ventilation 10
Function of Anatomical Dead Space o Impaction n Stick to mucus lining o Carried in the mucus towards the mouth n n o Mucus is propelled upwards towards the mouth n 1/21/2022 Expectorated Swallowed Cilia of the respiratory epithelium Ventilation 11
Function of Anatomical Dead Space o Foreign materials in inspired gas (cigarette smoke, smog) n Stimulate irritant receptors in the airways o o o 1/21/2022 Cause coughing Increase secretion of mucus Hypertrophy of mucus glands Ventilation 12
Function of Anatomical Dead Space o Prolonged breathing air containing foreign material o 1/21/2022 Cause chronic bronchitis n Increase airway resistance, difficult in breathing Ventilation 13
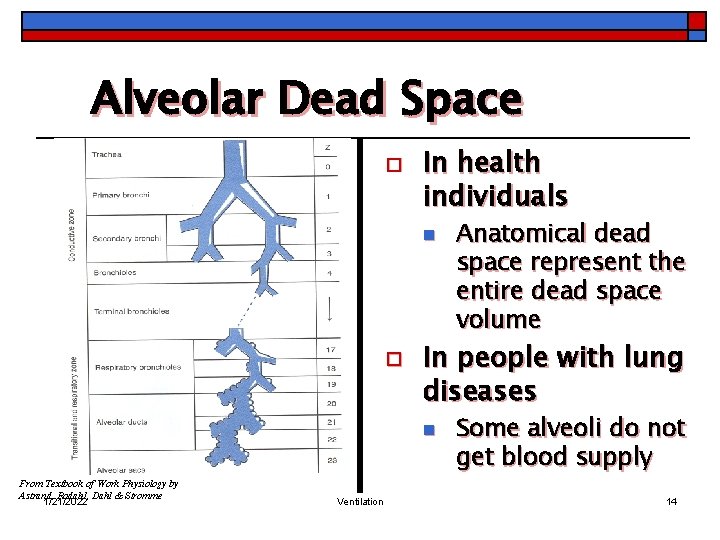
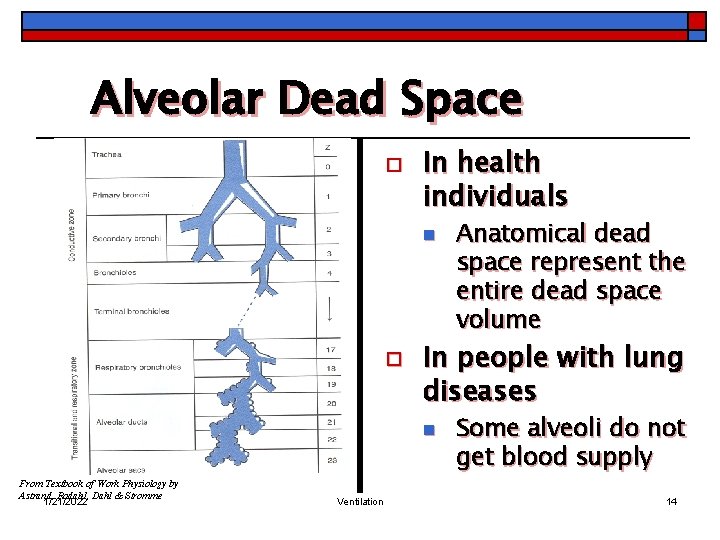
Alveolar Dead Space o In health individuals n o In people with lung diseases n From Textbook of Work Physiology by Astrand, Rodahl, Dahl & Stromme 1/21/2022 Ventilation Anatomical dead space represent the entire dead space volume Some alveoli do not get blood supply 14
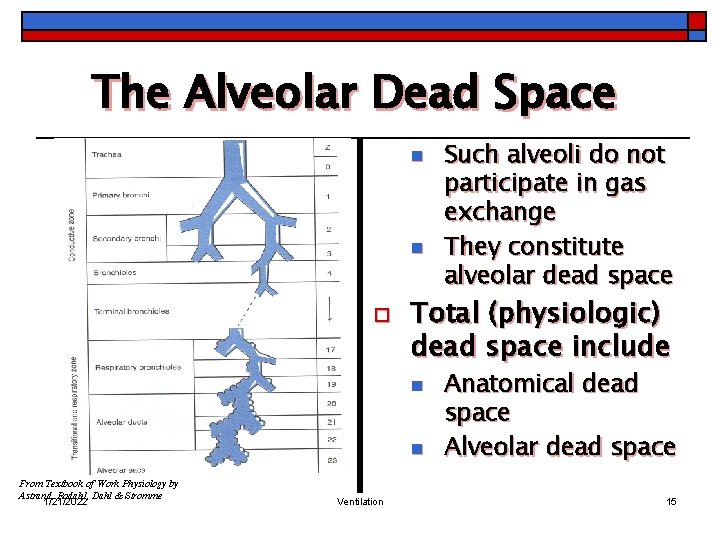
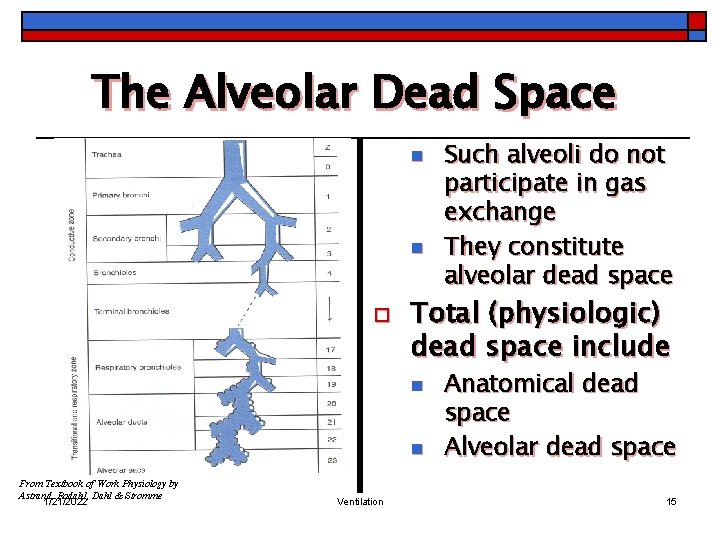
The Alveolar Dead Space n n o Total (physiologic) dead space include n n From Textbook of Work Physiology by Astrand, Rodahl, Dahl & Stromme 1/21/2022 Ventilation Such alveoli do not participate in gas exchange They constitute alveolar dead space Anatomical dead space Alveolar dead space 15
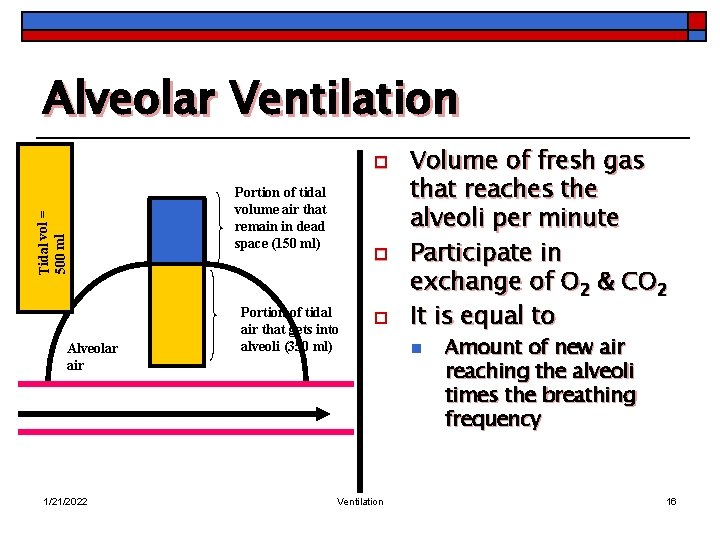
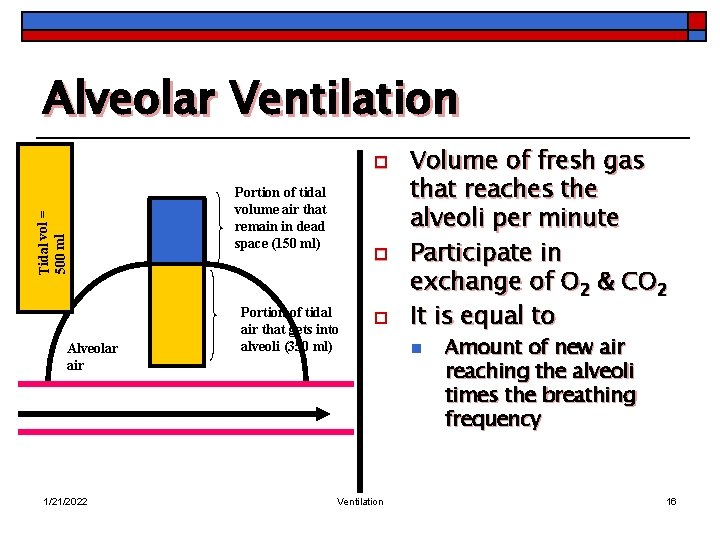
Alveolar Ventilation Tidal vol = 500 ml o Alveolar air 1/21/2022 Portion of tidal volume air that remain in dead space (150 ml) o Portion of tidal air that gets into alveoli (350 ml) o Ventilation Volume of fresh gas that reaches the alveoli per minute Participate in exchange of O 2 & CO 2 It is equal to n Amount of new air reaching the alveoli times the breathing frequency 16
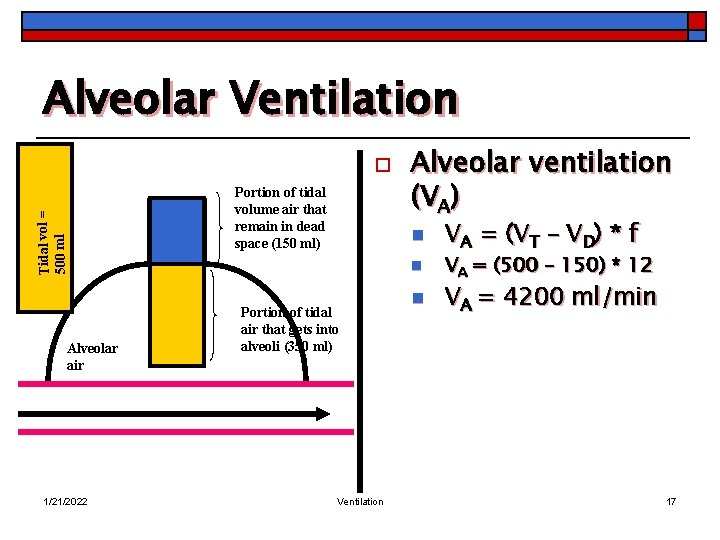
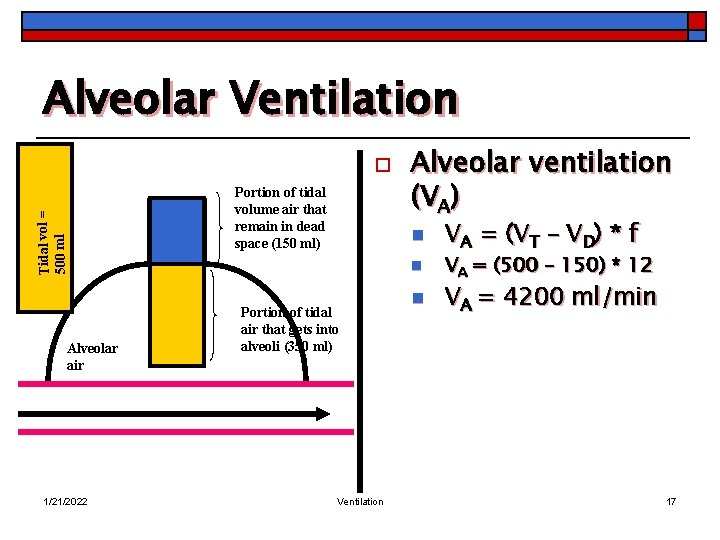
Alveolar Ventilation Tidal vol = 500 ml o Alveolar air 1/21/2022 Portion of tidal volume air that remain in dead space (150 ml) Alveolar ventilation (VA) n n Portion of tidal air that gets into alveoli (350 ml) Ventilation n VA = (VT – VD) * f VA = (500 – 150) * 12 VA = 4200 ml/min 17
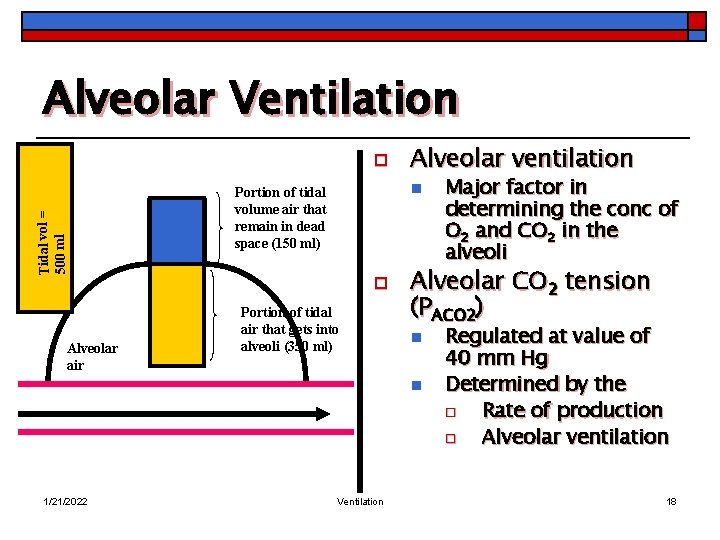
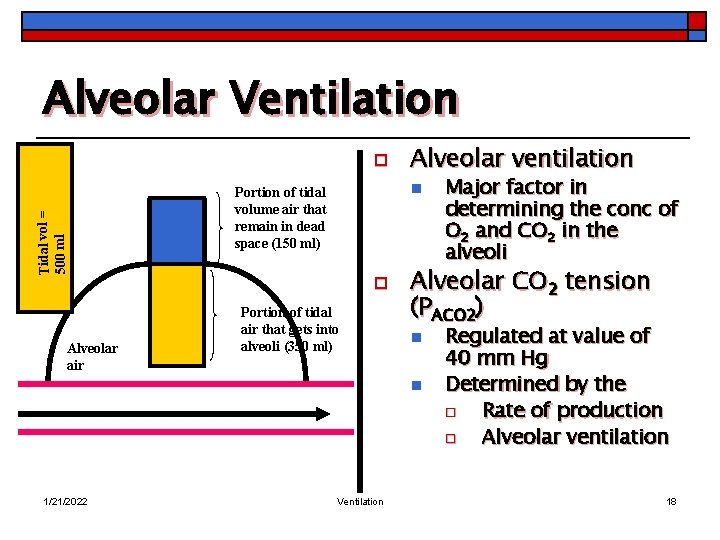
Alveolar Ventilation Tidal vol = 500 ml o Alveolar air Alveolar ventilation n Portion of tidal volume air that remain in dead space (150 ml) o Portion of tidal air that gets into alveoli (350 ml) Alveolar CO 2 tension (PACO 2) n n 1/21/2022 Ventilation Major factor in determining the conc of O 2 and CO 2 in the alveoli Regulated at value of 40 mm Hg Determined by the o Rate of production o Alveolar ventilation 18
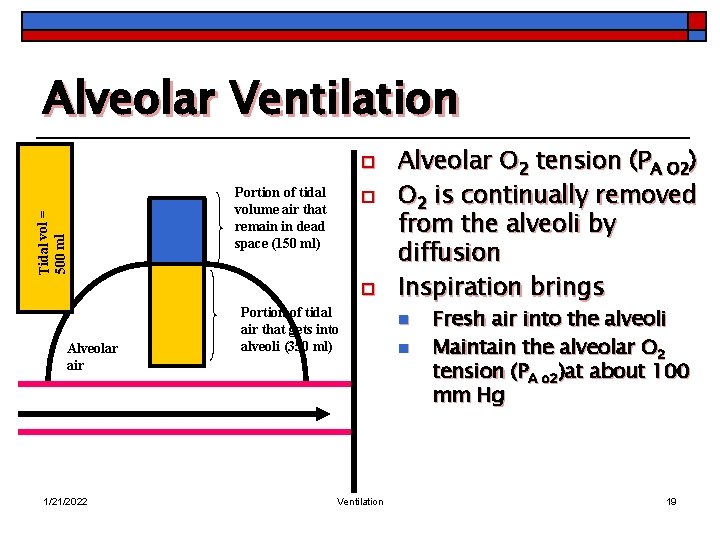
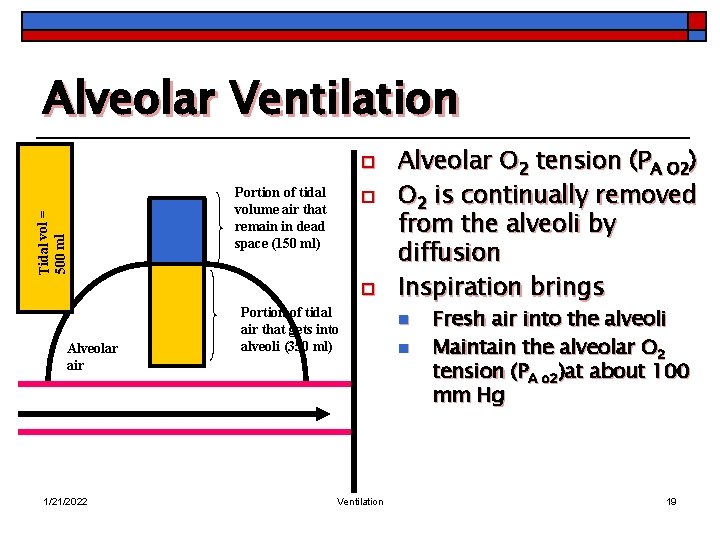
Alveolar Ventilation Tidal vol = 500 ml o Portion of tidal volume air that remain in dead space (150 ml) o o Alveolar air 1/21/2022 Portion of tidal air that gets into alveoli (350 ml) Ventilation Alveolar O 2 tension (PA O 2) O 2 is continually removed from the alveoli by diffusion Inspiration brings n n Fresh air into the alveoli Maintain the alveolar O 2 tension (PA o 2)at about 100 mm Hg 19
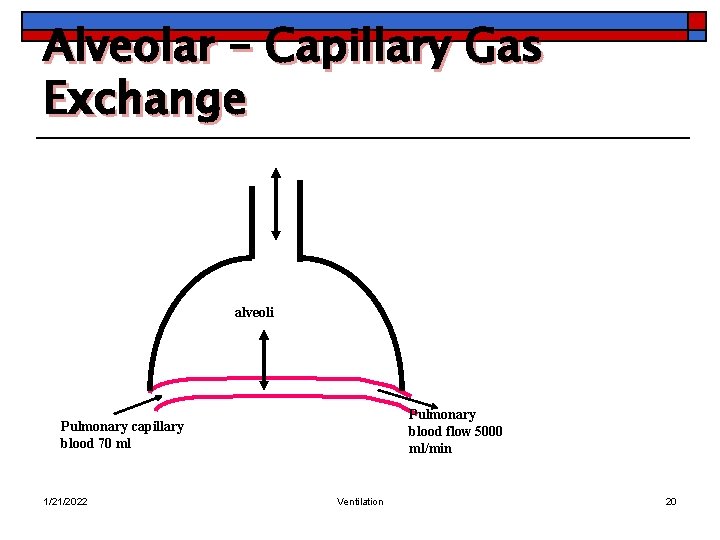
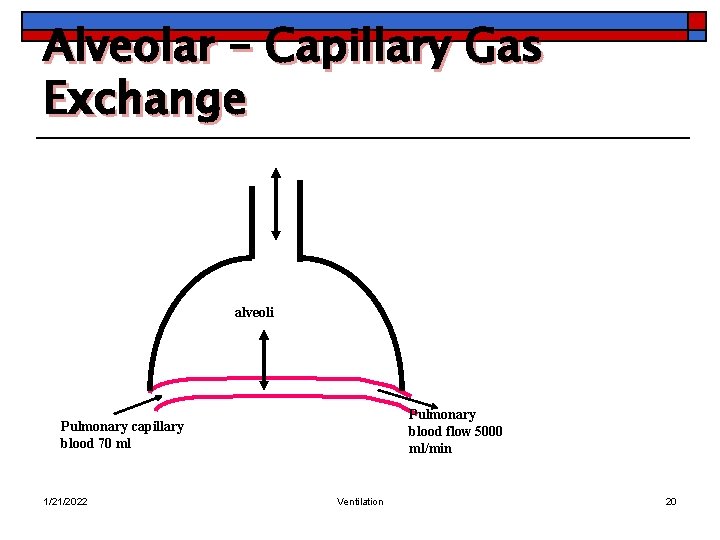
Alveolar – Capillary Gas Exchange alveoli Pulmonary blood flow 5000 ml/min Pulmonary capillary blood 70 ml 1/21/2022 Ventilation 20
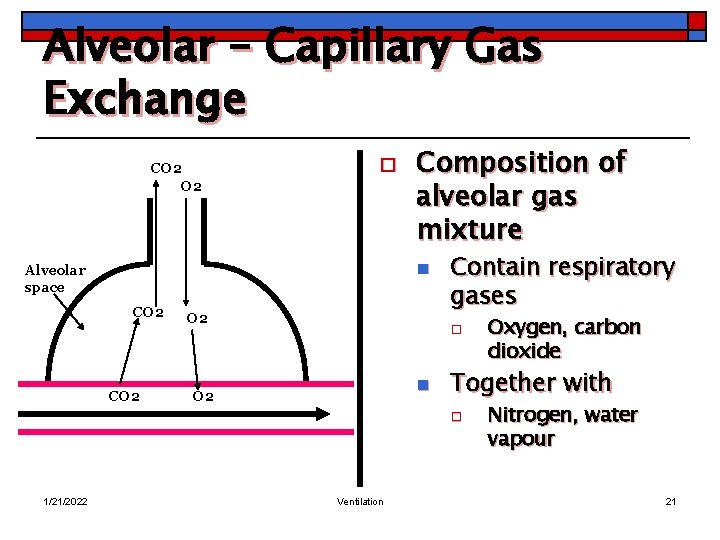
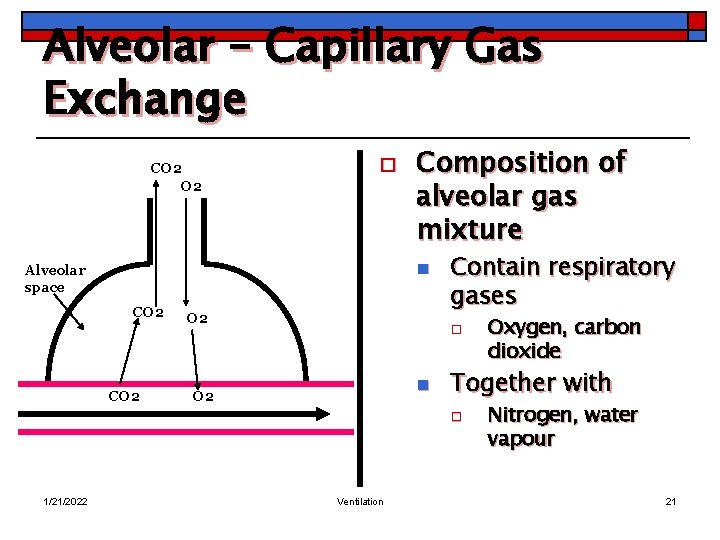
Alveolar – Capillary Gas Exchange CO 2 o Composition of alveolar gas mixture n Alveolar space CO 2 O 2 Contain respiratory gases o n O 2 Together with o 1/21/2022 Ventilation Oxygen, carbon dioxide Nitrogen, water vapour 21
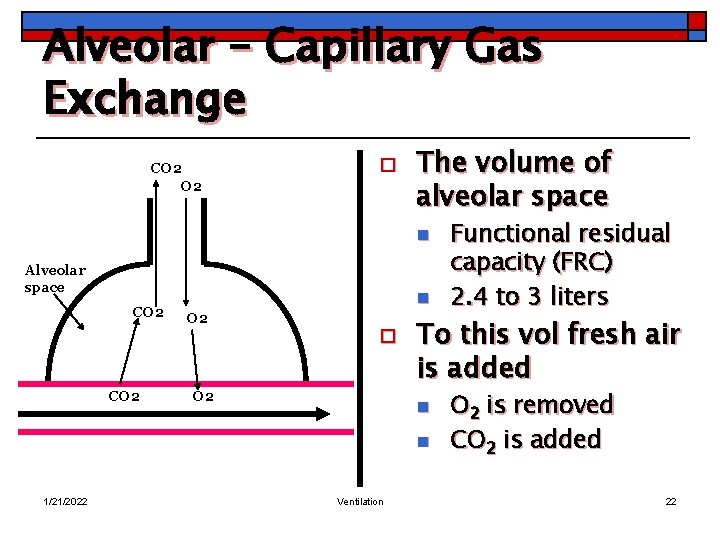
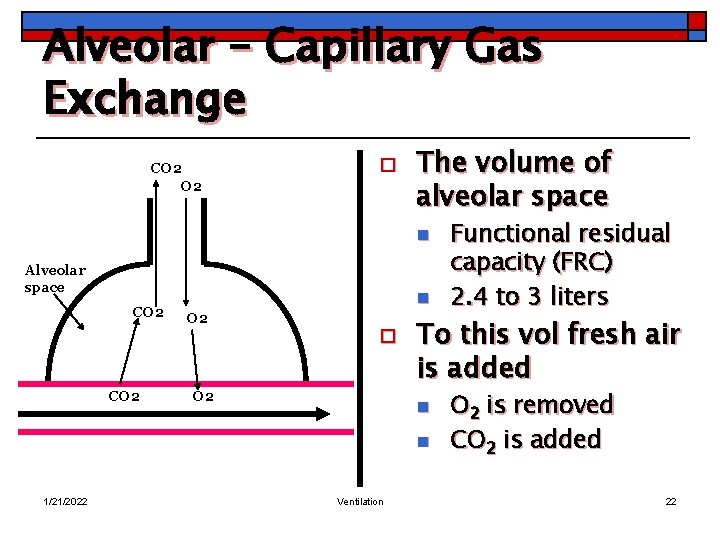
Alveolar – Capillary Gas Exchange CO 2 o The volume of alveolar space n Alveolar space CO 2 n O 2 o O 2 To this vol fresh air is added n n 1/21/2022 Ventilation Functional residual capacity (FRC) 2. 4 to 3 liters O 2 is removed CO 2 is added 22
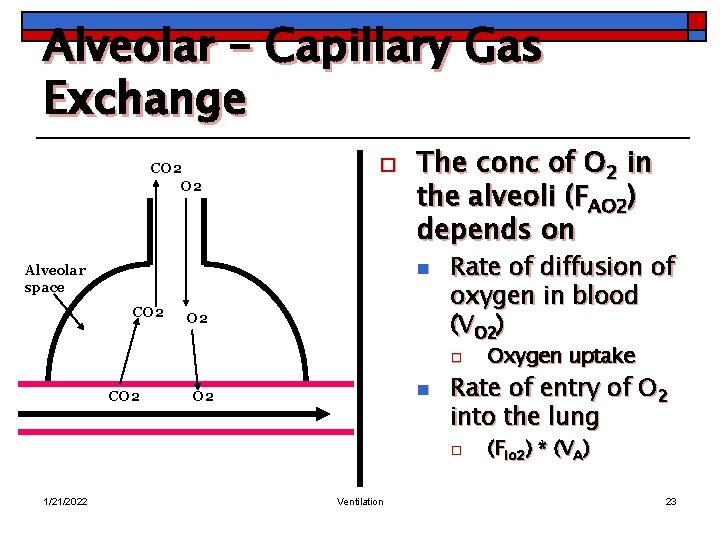
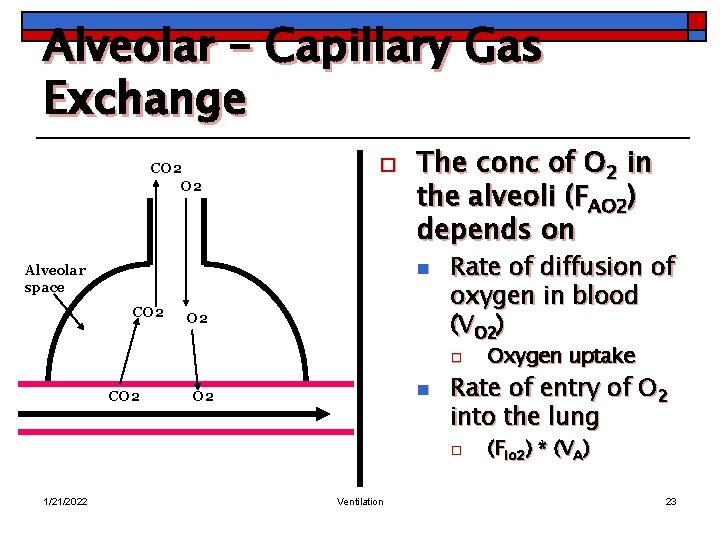
Alveolar – Capillary Gas Exchange CO 2 o The conc of O 2 in the alveoli (FAO 2) depends on n Alveolar space CO 2 Rate of diffusion of oxygen in blood (VO 2) o CO 2 n O 2 Rate of entry of O 2 into the lung o 1/21/2022 Ventilation Oxygen uptake (FIo 2) * (VA) 23
Alveolar – Capillary Gas Exchange CO 2 o n n Alveolar space CO 2 1/21/2022 Where O 2 (FIO 2) is the conc of O 2 in inspired air (VA) is alveolar ventilation O 2 Ventilation 24
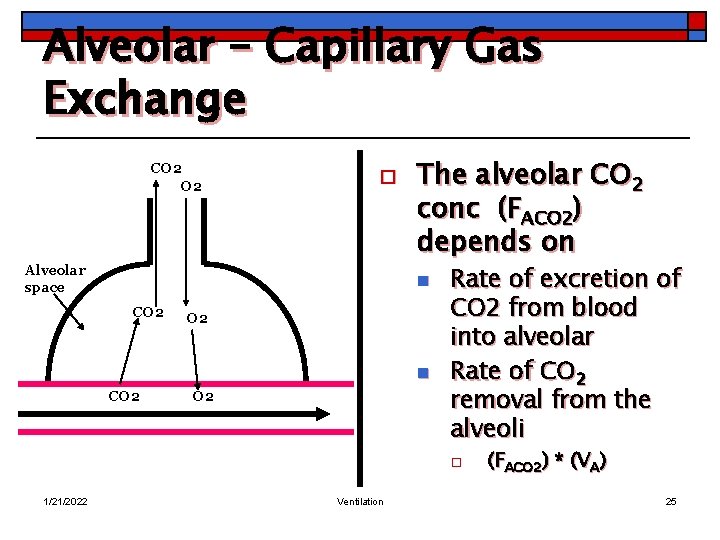
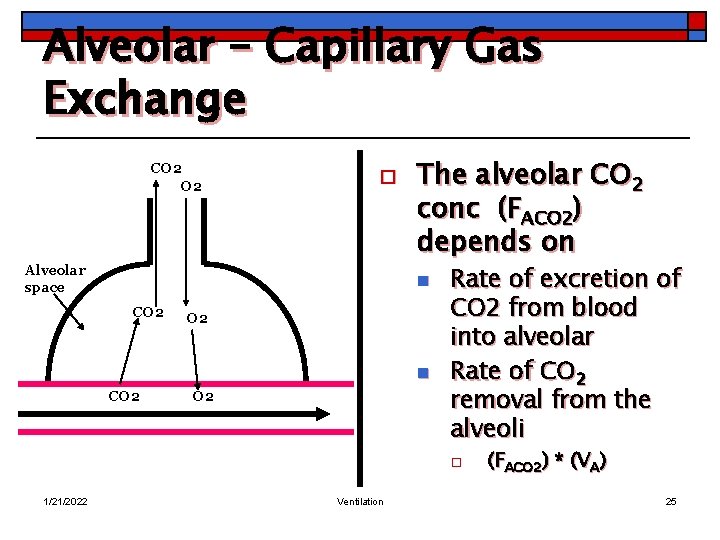
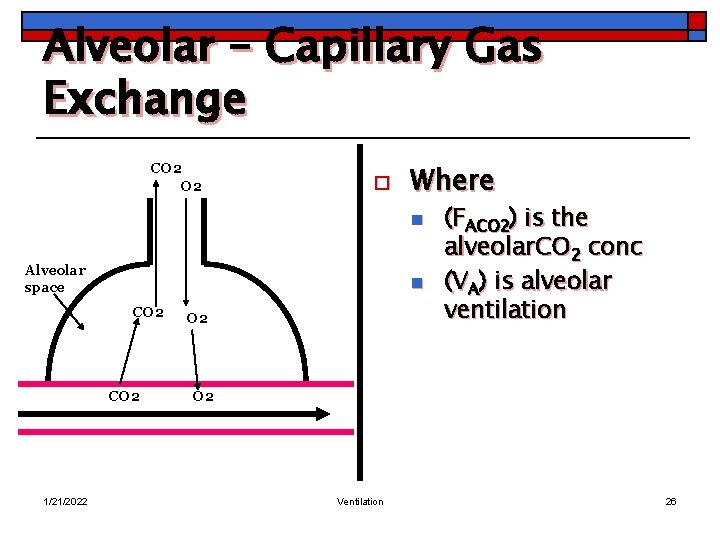
Alveolar – Capillary Gas Exchange CO 2 o Alveolar space The alveolar CO 2 conc (FACO 2) depends on n CO 2 O 2 Rate of excretion of CO 2 from blood into alveolar Rate of CO 2 removal from the alveoli o 1/21/2022 Ventilation (FACO 2) * (VA) 25
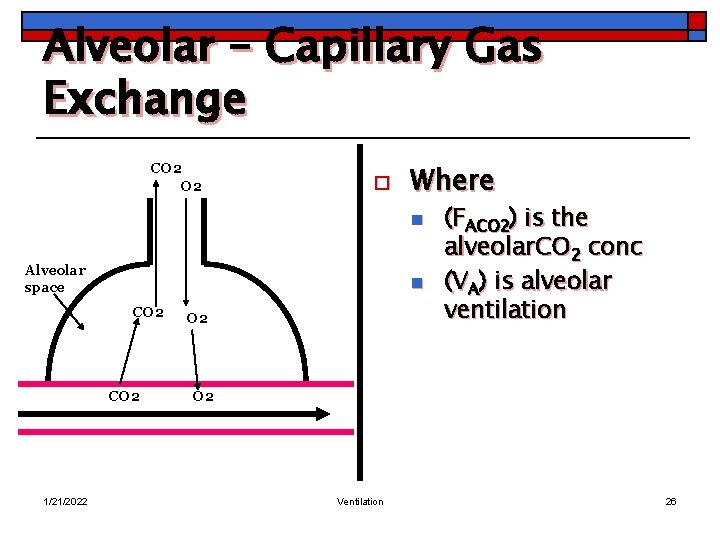
Alveolar – Capillary Gas Exchange CO 2 o Where n Alveolar space n CO 2 1/21/2022 O 2 (FACO 2) is the alveolar. CO 2 conc (VA) is alveolar ventilation O 2 Ventilation 26
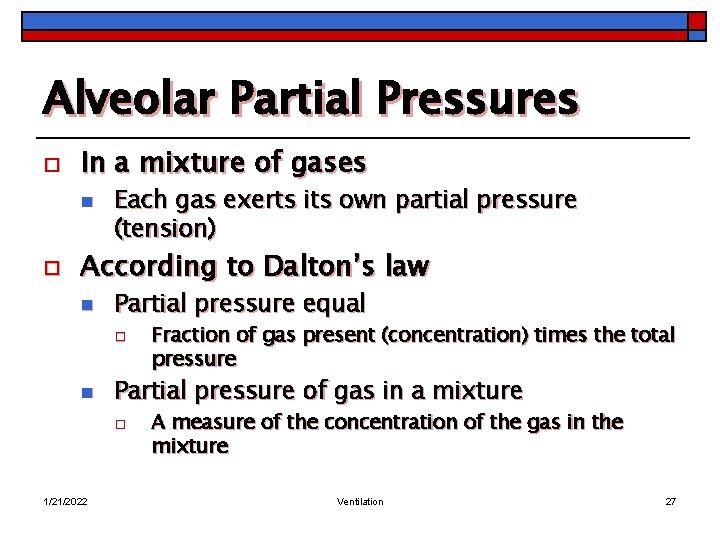
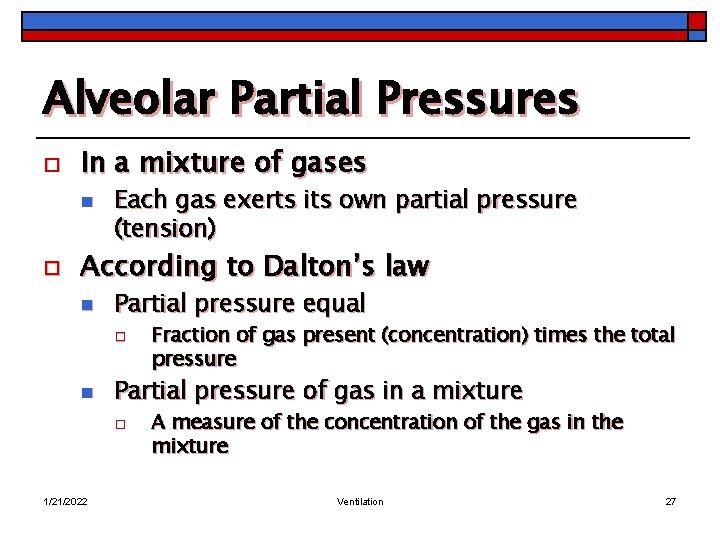
Alveolar Partial Pressures o In a mixture of gases n o Each gas exerts its own partial pressure (tension) According to Dalton’s law n Partial pressure equal o n Partial pressure of gas in a mixture o 1/21/2022 Fraction of gas present (concentration) times the total pressure A measure of the concentration of the gas in the mixture Ventilation 27
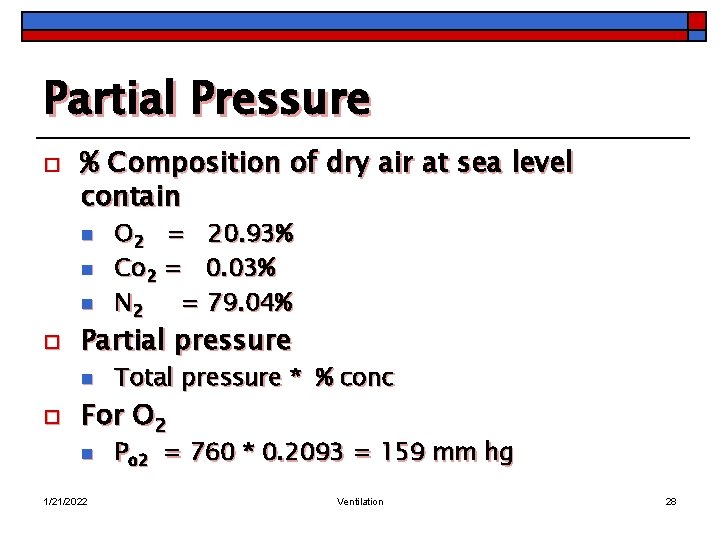
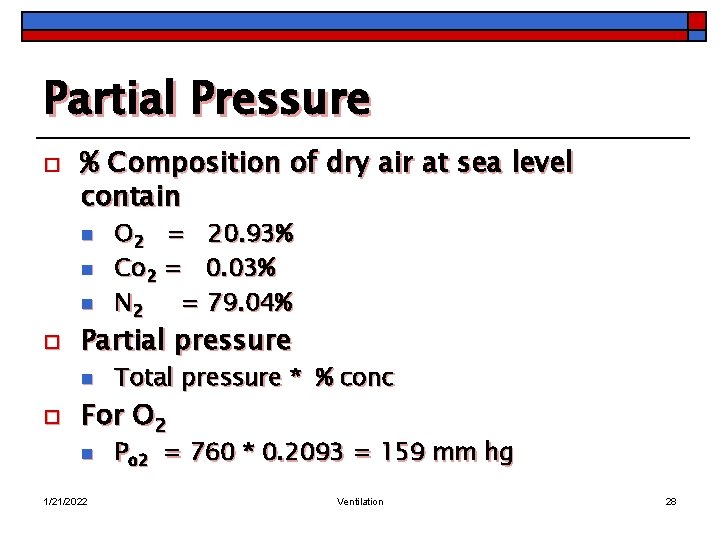
Partial Pressure o % Composition of dry air at sea level contain n o Partial pressure n o O 2 = 20. 93% Co 2 = 0. 03% N 2 = 79. 04% Total pressure * % conc For O 2 n 1/21/2022 Po 2 = 760 * 0. 2093 = 159 mm hg Ventilation 28
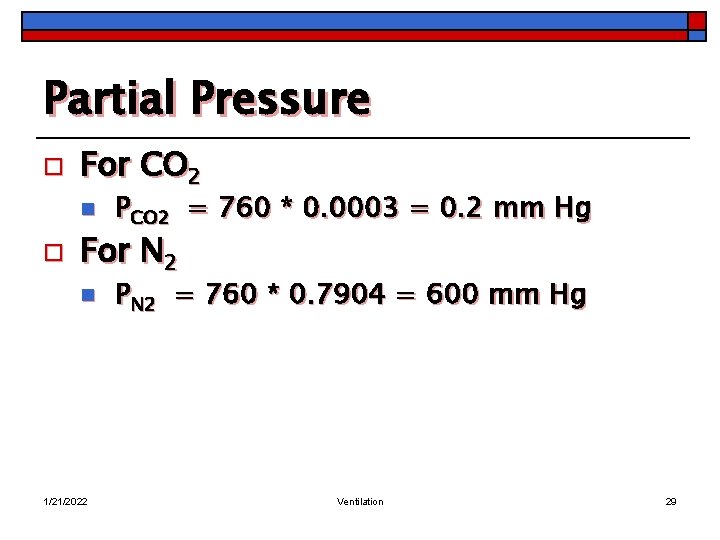
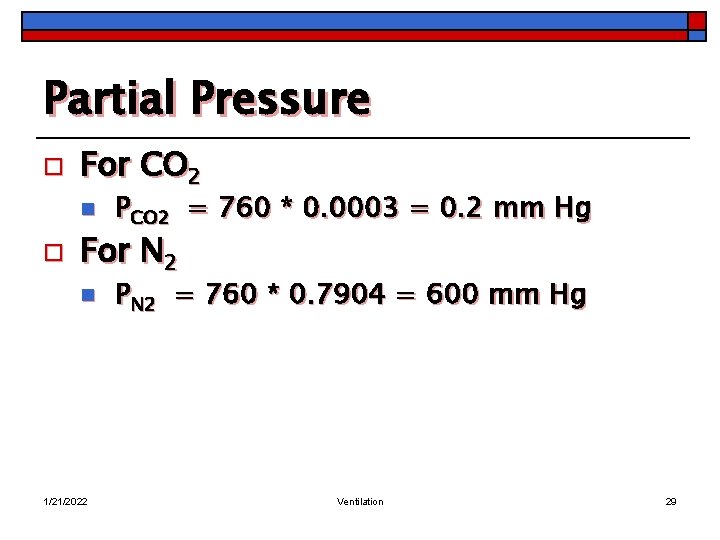
Partial Pressure o For CO 2 n o PCO 2 = 760 * 0. 0003 = 0. 2 mm Hg For N 2 n 1/21/2022 PN 2 = 760 * 0. 7904 = 600 mm Hg Ventilation 29
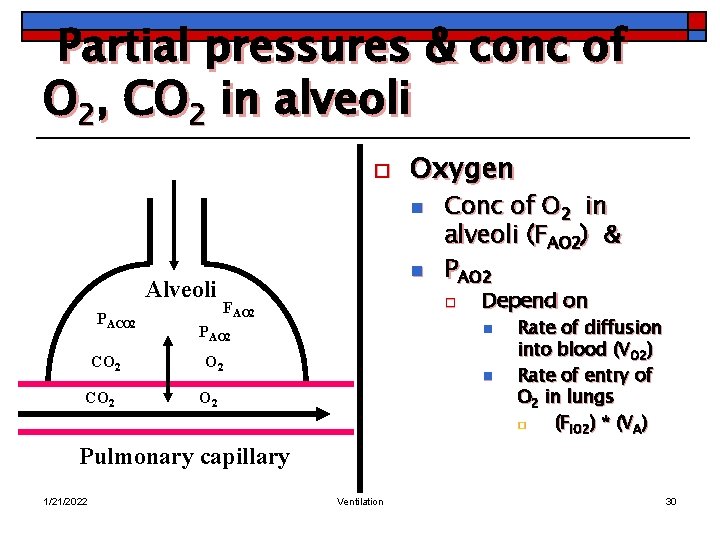
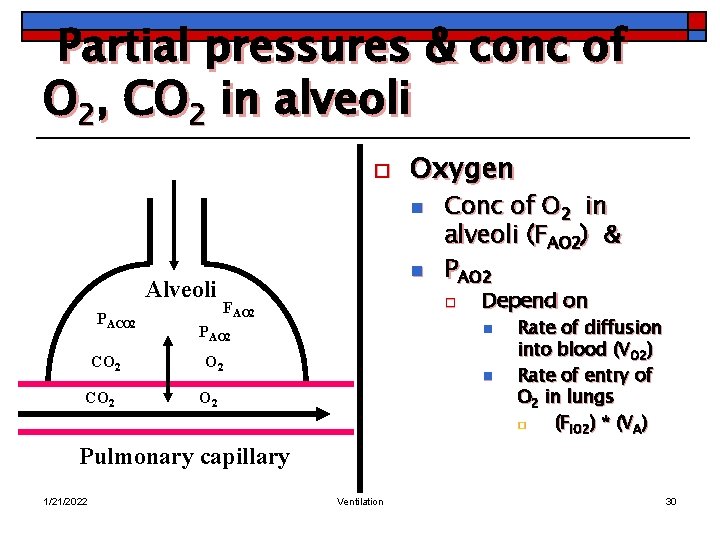
Partial pressures & conc of O 2, CO 2 in alveoli o Oxygen n Alveoli PACO 2 n Conc of O 2 in alveoli (FAO 2) & PAO 2 o FAO 2 Depend on n PAO 2 n O 2 Rate of diffusion into blood (VO 2) Rate of entry of O 2 in lungs o (FIO 2) * (VA) Pulmonary capillary 1/21/2022 Ventilation 30
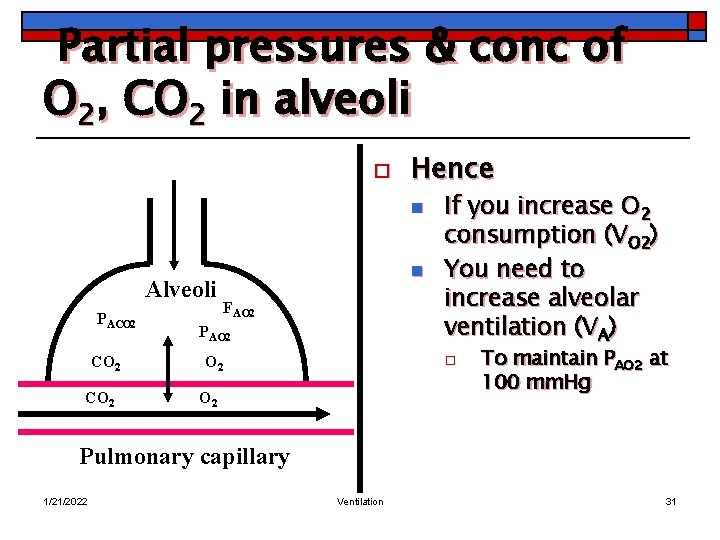
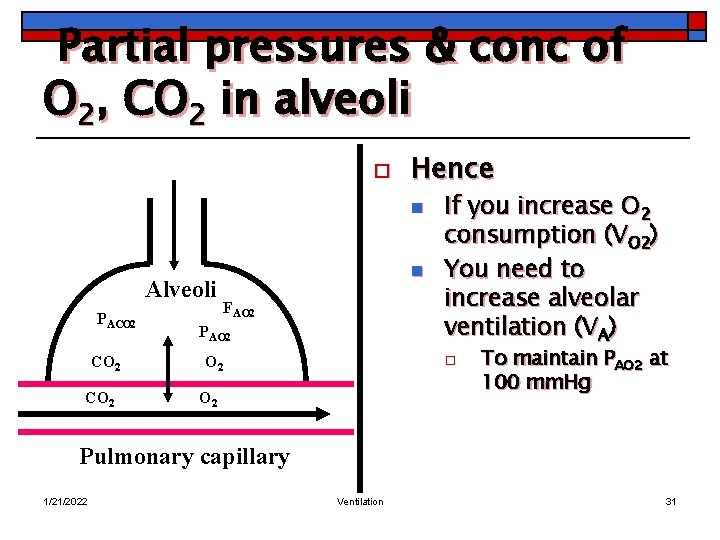
Partial pressures & conc of O 2, CO 2 in alveoli o Hence n Alveoli PACO 2 n FAO 2 PAO 2 If you increase O 2 consumption (VO 2) You need to increase alveolar ventilation (VA) o O 2 To maintain PAO 2 at 100 mm. Hg Pulmonary capillary 1/21/2022 Ventilation 31
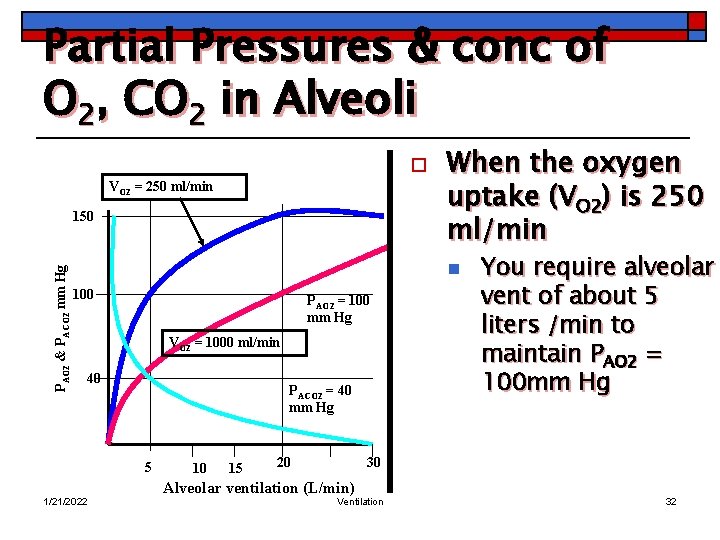
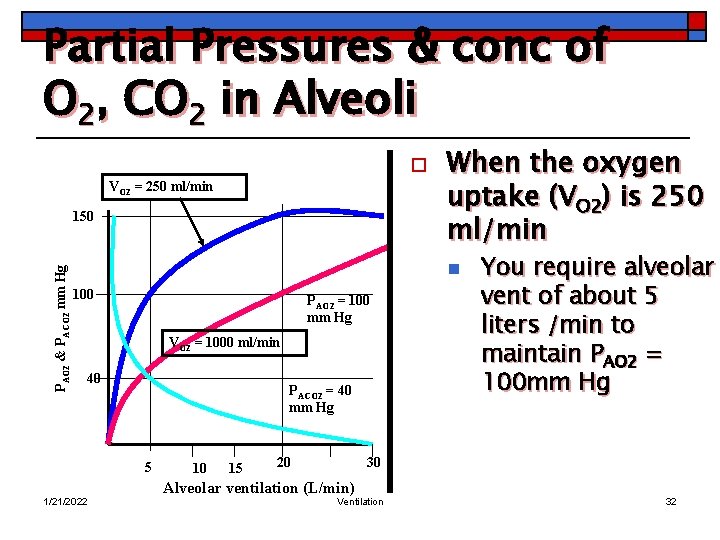
Partial Pressures & conc of O 2, CO 2 in Alveoli o VO 2 = 250 ml/min PAO 2 & PACO 2 mm Hg 150 When the oxygen uptake (VO 2) is 250 ml/min n 100 PAO 2 = 100 mm Hg VO 2 = 1000 ml/min 40 PACO 2 = 40 mm Hg 5 1/21/2022 10 15 20 You require alveolar vent of about 5 liters /min to maintain PAO 2 = 100 mm Hg 30 Alveolar ventilation (L/min) Ventilation 32
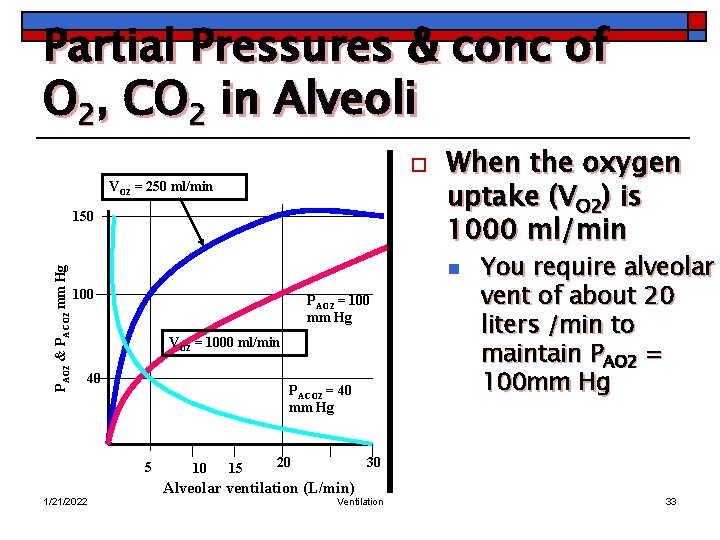
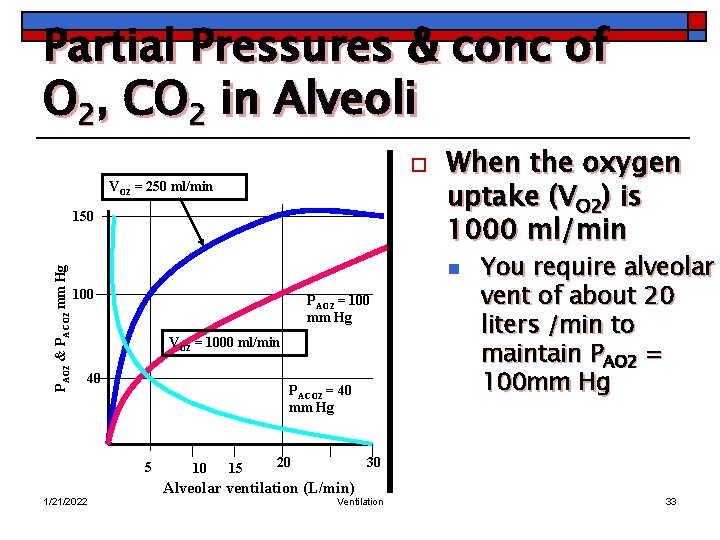
Partial Pressures & conc of O 2, CO 2 in Alveoli o VO 2 = 250 ml/min PAO 2 & PACO 2 mm Hg 150 When the oxygen uptake (VO 2) is 1000 ml/min n 100 PAO 2 = 100 mm Hg VO 2 = 1000 ml/min 40 PACO 2 = 40 mm Hg 5 1/21/2022 10 15 20 You require alveolar vent of about 20 liters /min to maintain PAO 2 = 100 mm Hg 30 Alveolar ventilation (L/min) Ventilation 33
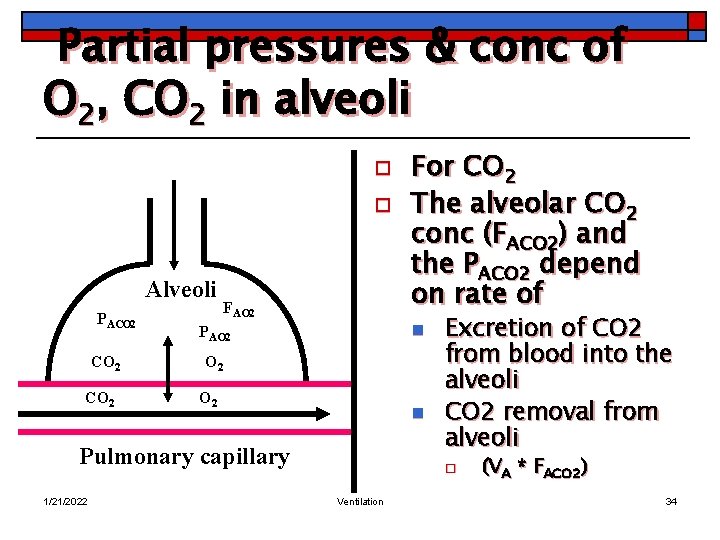
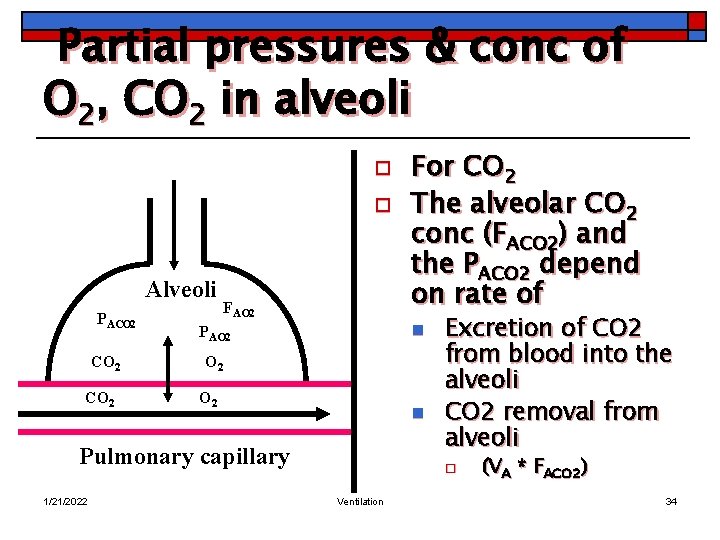
Partial pressures & conc of O 2, CO 2 in alveoli o o Alveoli PACO 2 FAO 2 n PAO 2 O 2 n Pulmonary capillary 1/21/2022 For CO 2 The alveolar CO 2 conc (FACO 2) and the PACO 2 depend on rate of Excretion of CO 2 from blood into the alveoli CO 2 removal from alveoli o Ventilation (VA * FACO 2) 34
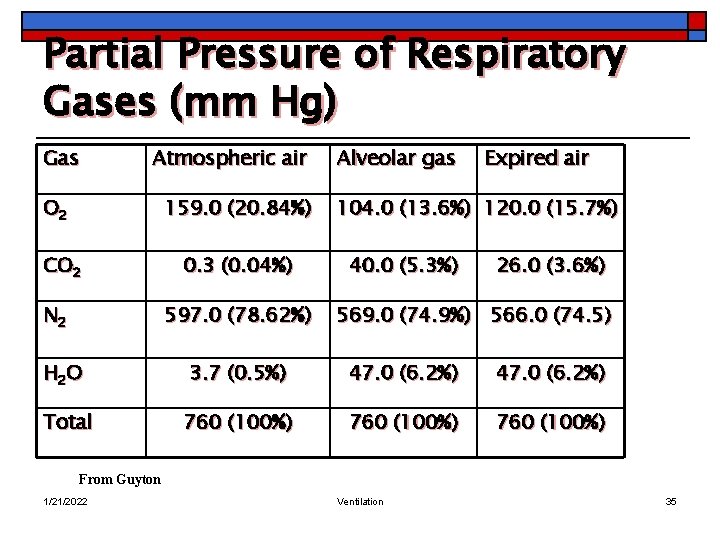
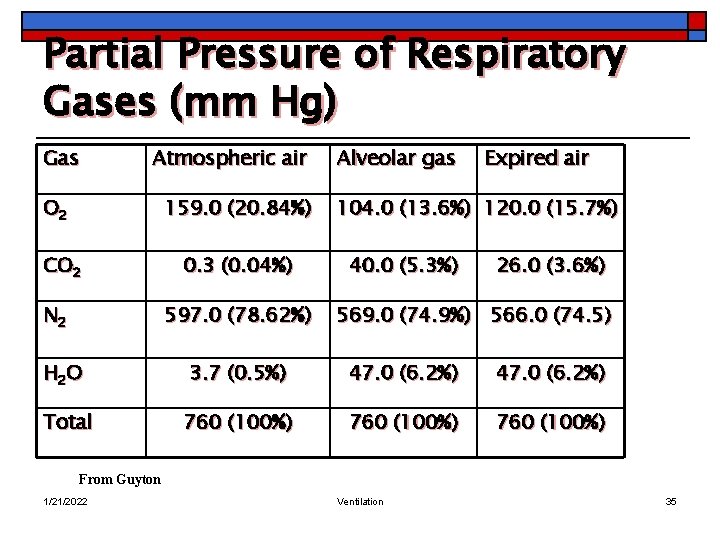
Partial Pressure of Respiratory Gases (mm Hg) Gas Atmospheric air O 2 159. 0 (20. 84%) CO 2 N 2 0. 3 (0. 04%) 597. 0 (78. 62%) Alveolar gas Expired air 104. 0 (13. 6%) 120. 0 (15. 7%) 40. 0 (5. 3%) 26. 0 (3. 6%) 569. 0 (74. 9%) 566. 0 (74. 5) H 2 O 3. 7 (0. 5%) 47. 0 (6. 2%) Total 760 (100%) From Guyton 1/21/2022 Ventilation 35
Diffusion 1/21/2022 Ventilation 36
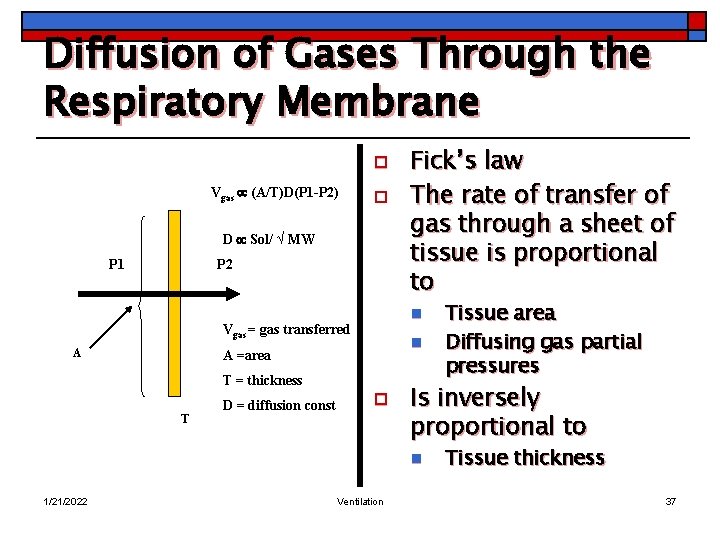
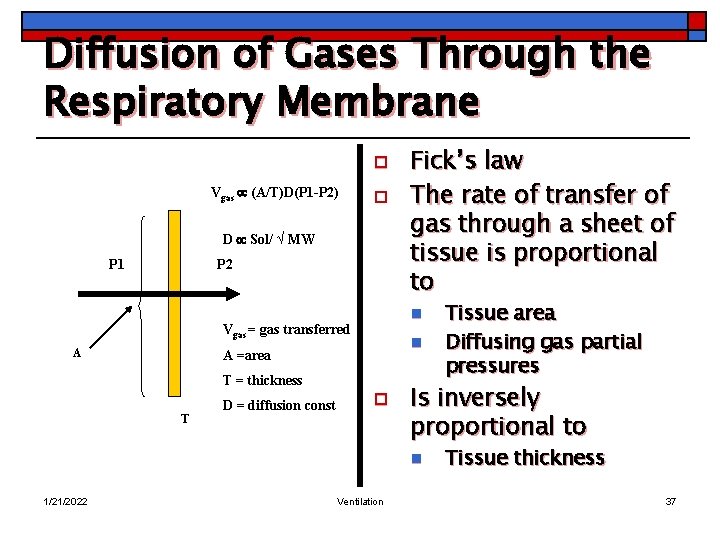
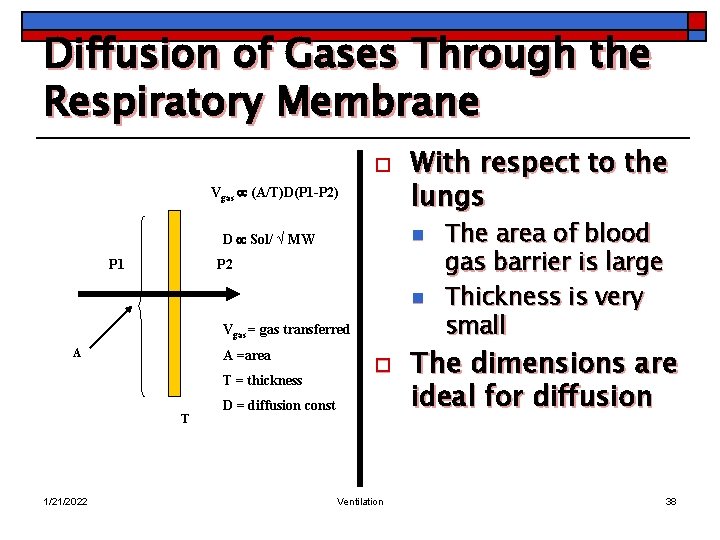
Diffusion of Gases Through the Respiratory Membrane o Vgas (A/T)D(P 1 -P 2) o D Sol/ √ MW P 1 P 2 n Vgas = gas transferred A n A =area T = thickness T D = diffusion const Fick’s law The rate of transfer of gas through a sheet of tissue is proportional to o Is inversely proportional to n 1/21/2022 Ventilation Tissue area Diffusing gas partial pressures Tissue thickness 37
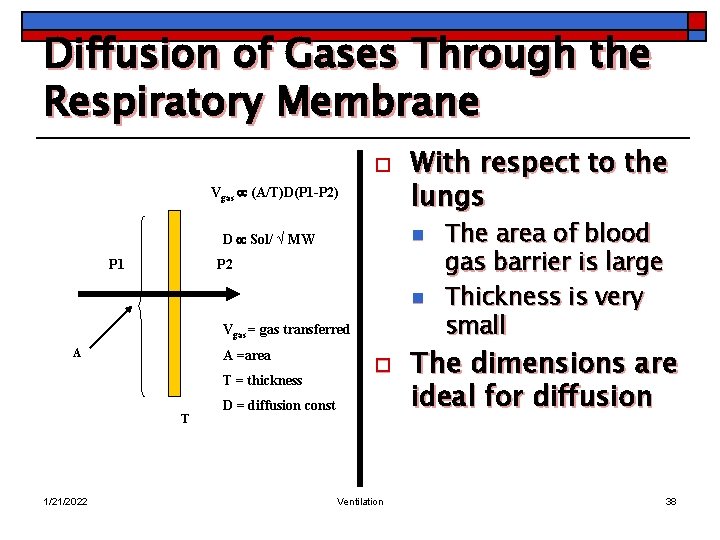
Diffusion of Gases Through the Respiratory Membrane o Vgas (A/T)D(P 1 -P 2) n D Sol/ √ MW P 1 With respect to the lungs P 2 n Vgas = gas transferred A A =area T = thickness T 1/21/2022 o D = diffusion const Ventilation The area of blood gas barrier is large Thickness is very small The dimensions are ideal for diffusion 38
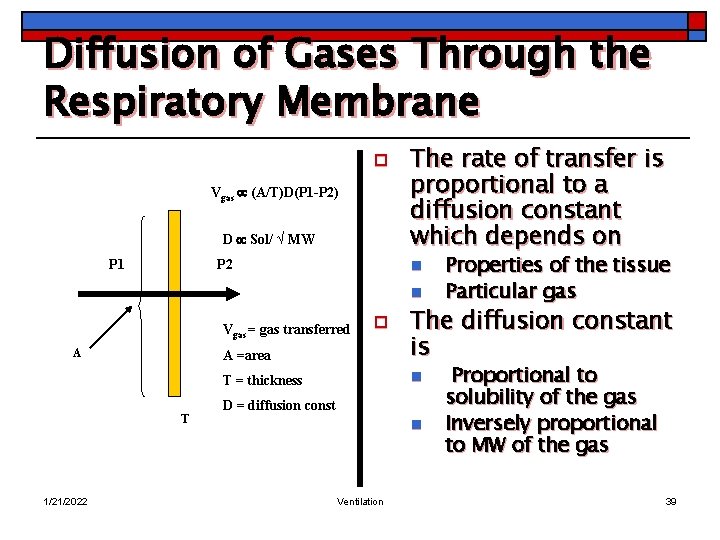
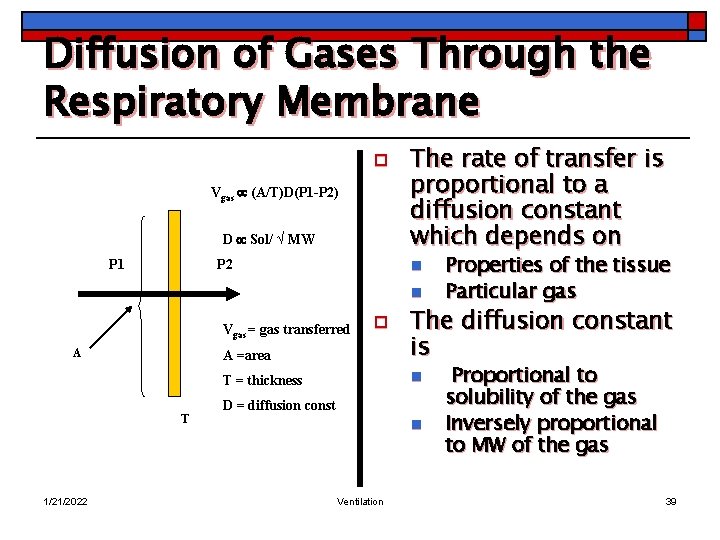
Diffusion of Gases Through the Respiratory Membrane o Vgas (A/T)D(P 1 -P 2) D Sol/ √ MW P 1 P 2 The rate of transfer is proportional to a diffusion constant which depends on n n A =area The diffusion constant is T = thickness n Vgas = gas transferred A T 1/21/2022 Properties of the tissue Particular gas o D = diffusion const n Ventilation Proportional to solubility of the gas Inversely proportional to MW of the gas 39
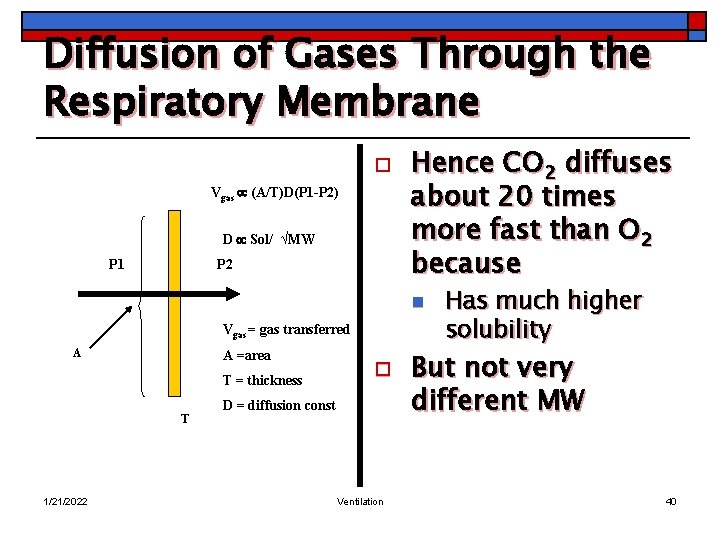
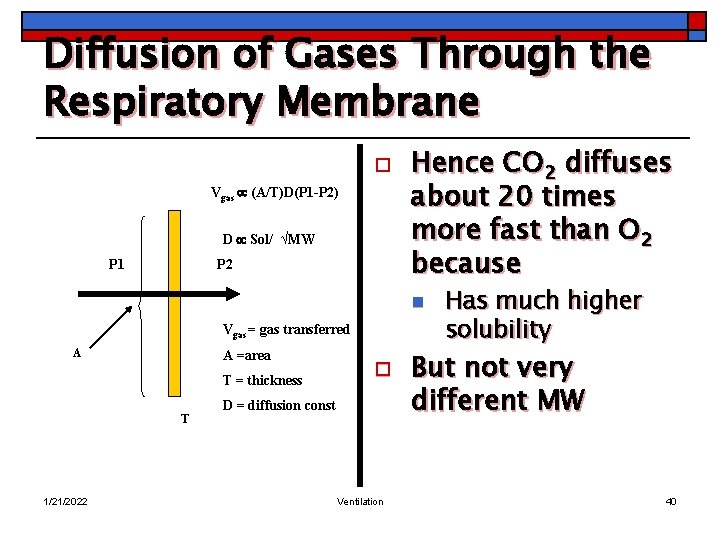
Diffusion of Gases Through the Respiratory Membrane o Vgas (A/T)D(P 1 -P 2) D Sol/ √MW P 1 P 2 Hence CO 2 diffuses about 20 times more fast than O 2 because n Vgas = gas transferred A A =area T = thickness T 1/21/2022 o D = diffusion const Ventilation Has much higher solubility But not very different MW 40
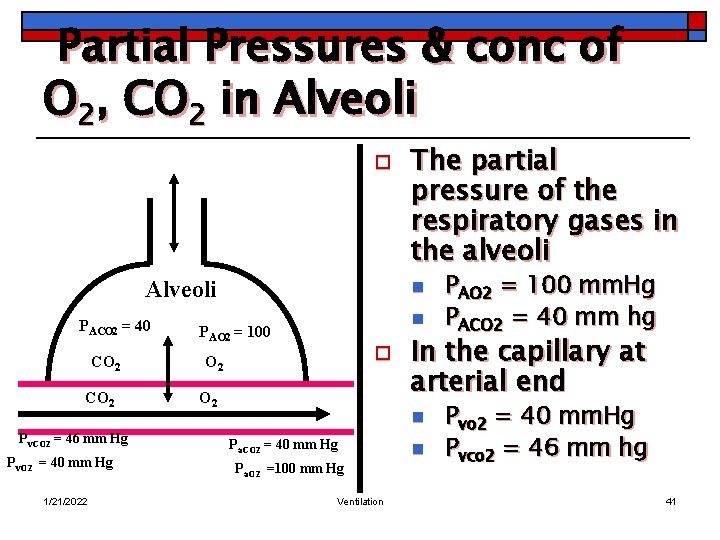
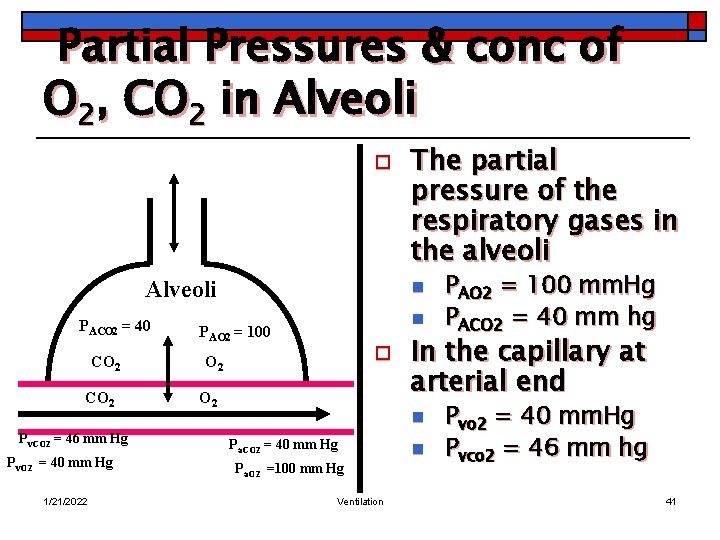
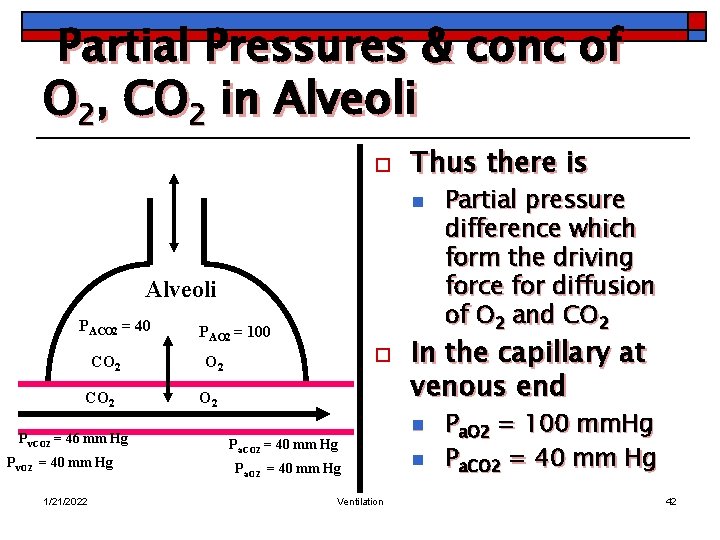
Partial Pressures & conc of O 2, CO 2 in Alveoli o Alveoli PACO 2 = 40 CO 2 Pv. CO 2 = 46 mm Hg Pv. O 2 = 40 mm Hg 1/21/2022 The partial pressure of the respiratory gases in the alveoli n n PAO 2 = 100 o O 2 In the capillary at arterial end n Pa. CO 2 = 40 mm Hg Pa. O 2 =100 mm Hg Ventilation PAO 2 = 100 mm. Hg PACO 2 = 40 mm hg n Pvo 2 = 40 mm. Hg Pvco 2 = 46 mm hg 41
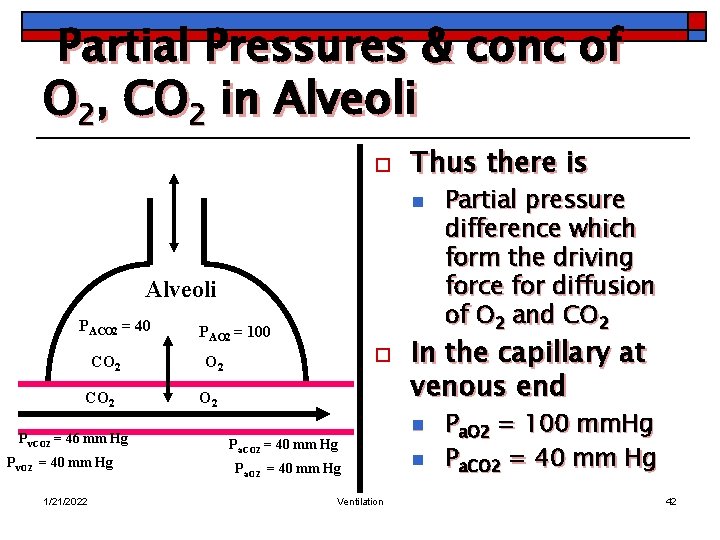
Partial Pressures & conc of O 2, CO 2 in Alveoli o Thus there is n Alveoli PACO 2 = 40 CO 2 Pv. CO 2 = 46 mm Hg Pv. O 2 = 40 mm Hg 1/21/2022 PAO 2 = 100 o O 2 In the capillary at venous end n Pa. CO 2 = 40 mm Hg Pa. O 2 = 40 mm Hg Ventilation Partial pressure difference which form the driving force for diffusion of O 2 and CO 2 n Pa. O 2 = 100 mm. Hg Pa. CO 2 = 40 mm Hg 42
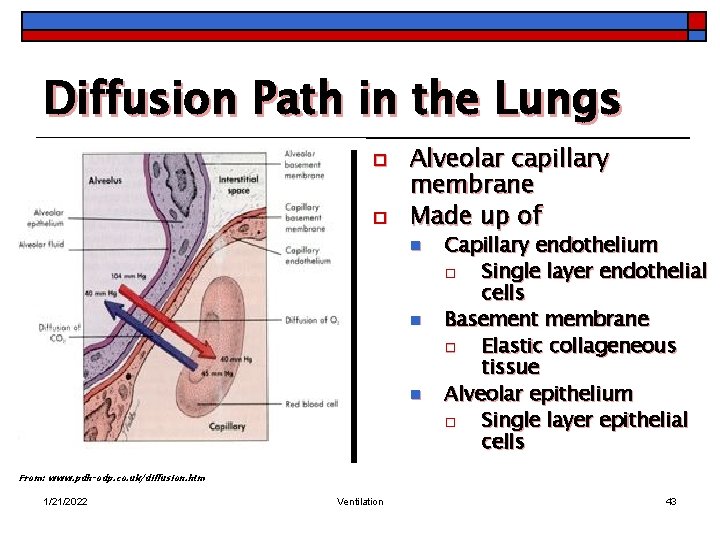
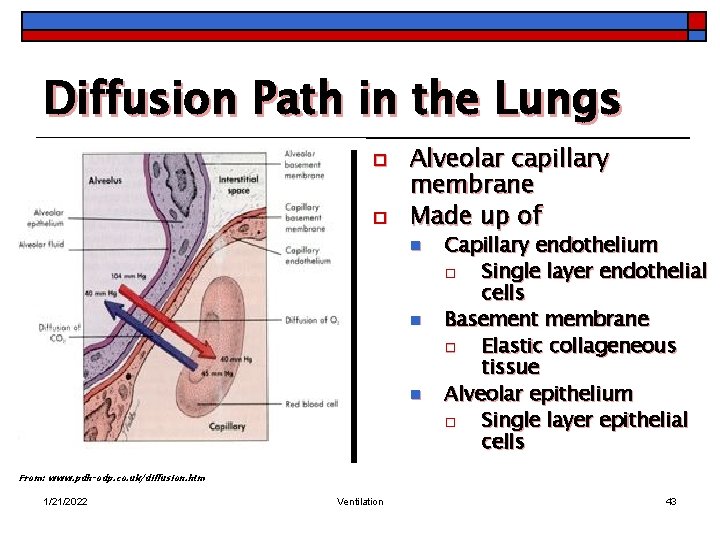
Diffusion Path in the Lungs o o Alveolar capillary membrane Made up of n n n Capillary endothelium o Single layer endothelial cells Basement membrane o Elastic collageneous tissue Alveolar epithelium o Single layer epithelial cells From: www. pdh-odp. co. uk/diffusion. htm 1/21/2022 Ventilation 43
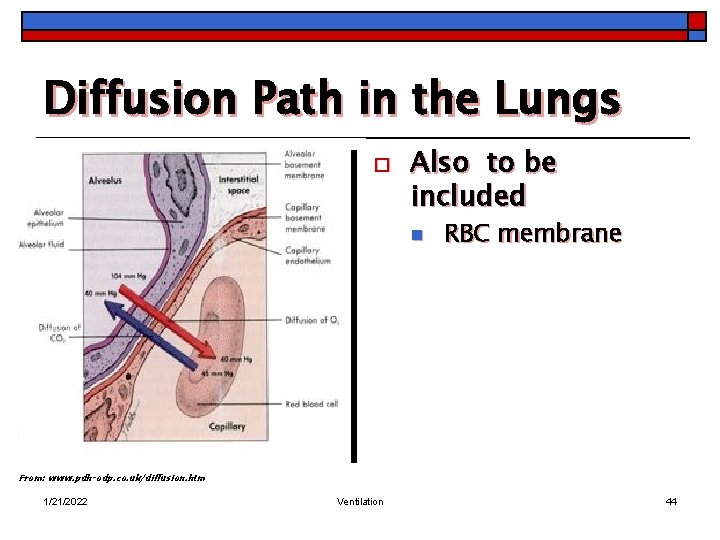
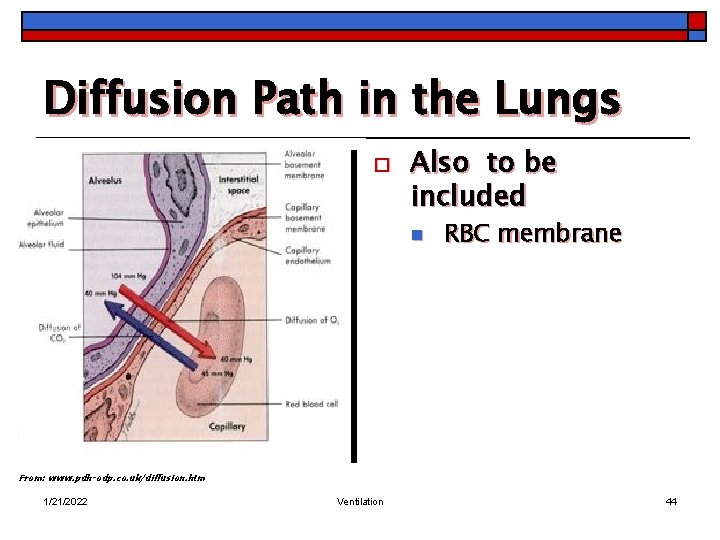
Diffusion Path in the Lungs o Also to be included n RBC membrane From: www. pdh-odp. co. uk/diffusion. htm 1/21/2022 Ventilation 44
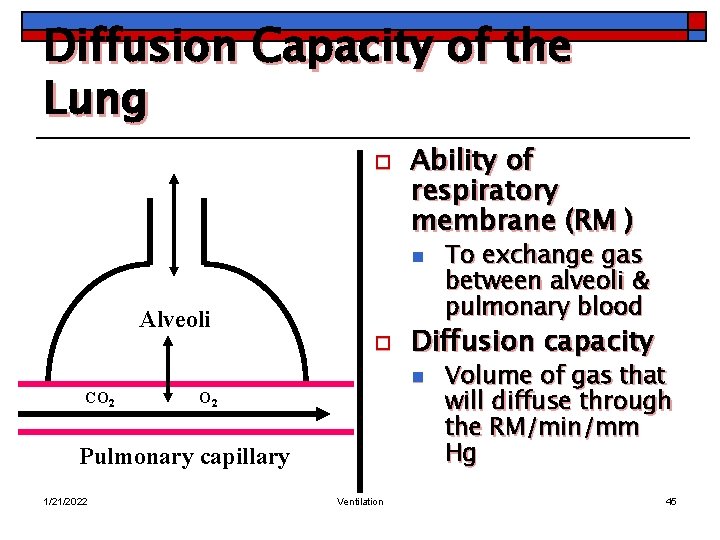
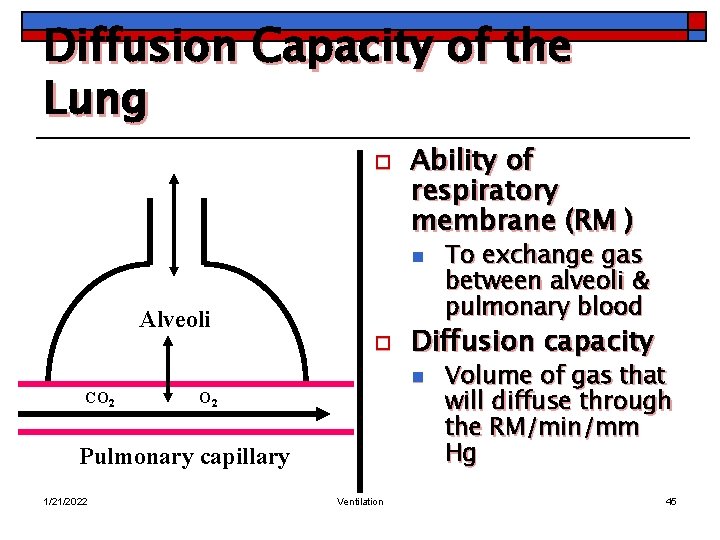
Diffusion Capacity of the Lung o Ability of respiratory membrane (RM ) n Alveoli o Diffusion capacity n CO 2 Pulmonary capillary 1/21/2022 Ventilation To exchange gas between alveoli & pulmonary blood Volume of gas that will diffuse through the RM/min/mm Hg 45
Diffusion Capacity of the Lung o Factors affecting diffusing capacity of the lung include n n o Membrane component Blood component Membrane component n Pulmonary diseases may affect diffusion process by o o 1/21/2022 The SA (destruction of alveoli) Diffusion distance (oedema) Ventilation 46
Diffusion Capacity of the Lung o Reducing the partial pressure gradient for the diffusion of gases n 1/21/2022 Ventilation/perfusion abnormalities Ventilation 47
Diffusion Capacity of the Lung o Blood component n Chemical combination of gases with Hb require finite time o o n 1/21/2022 In Hb conc enhances the transfer of gases Anaemic individuals would have impaired diffusion capacity Increase in cardiac output (C. O) enhance diffusion capacity Ventilation 48
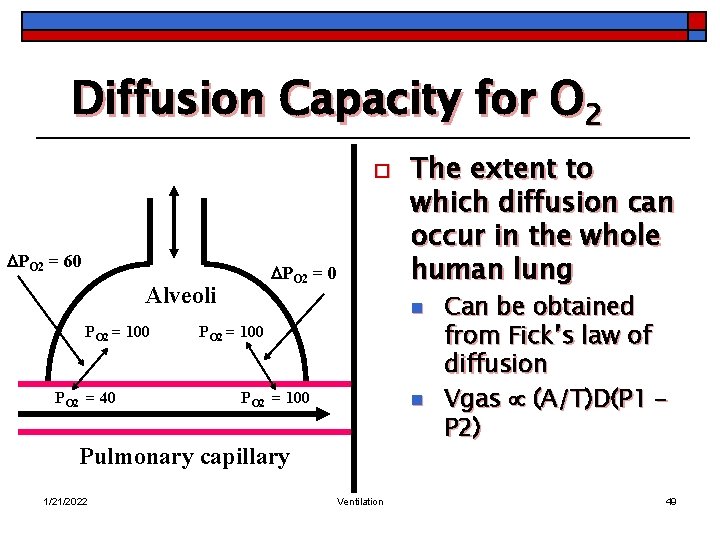
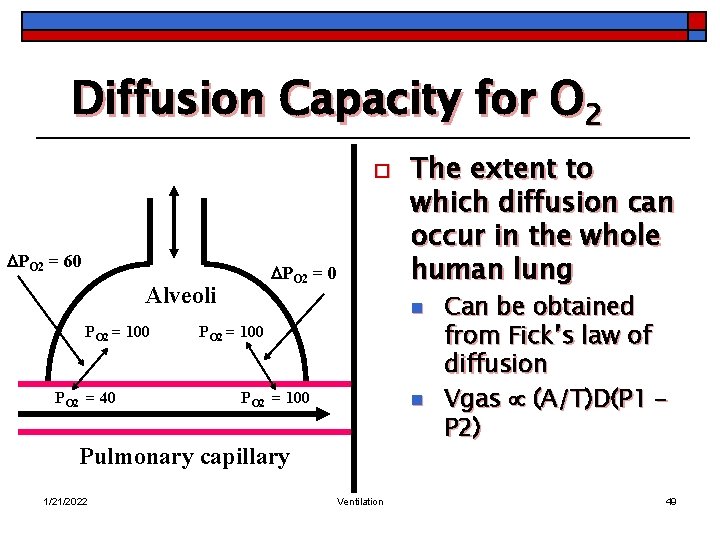
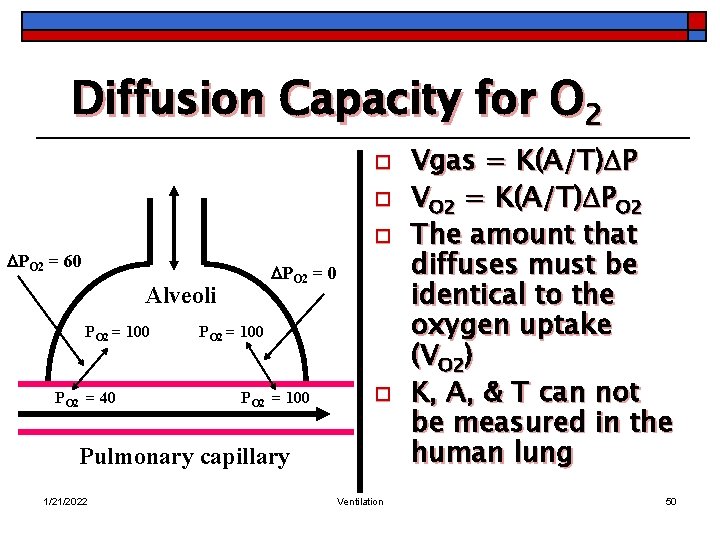
Diffusion Capacity for O 2 o PO 2 = 60 PO 2 = 0 Alveoli PO 2 = 100 PO 2 = 40 n PO 2 = 100 n Pulmonary capillary 1/21/2022 The extent to which diffusion can occur in the whole human lung Ventilation Can be obtained from Fick’s law of diffusion Vgas (A/T)D(P 1 – P 2) 49
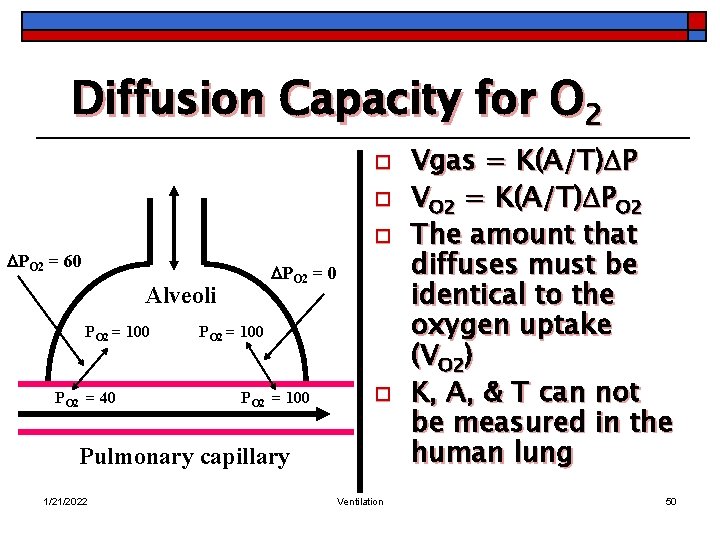
Diffusion Capacity for O 2 o o o PO 2 = 60 PO 2 = 0 Alveoli PO 2 = 100 PO 2 = 40 PO 2 = 100 o Pulmonary capillary 1/21/2022 Ventilation Vgas = K(A/T) P VO 2 = K(A/T) PO 2 The amount that diffuses must be identical to the oxygen uptake (VO 2) K, A, & T can not be measured in the human lung 50
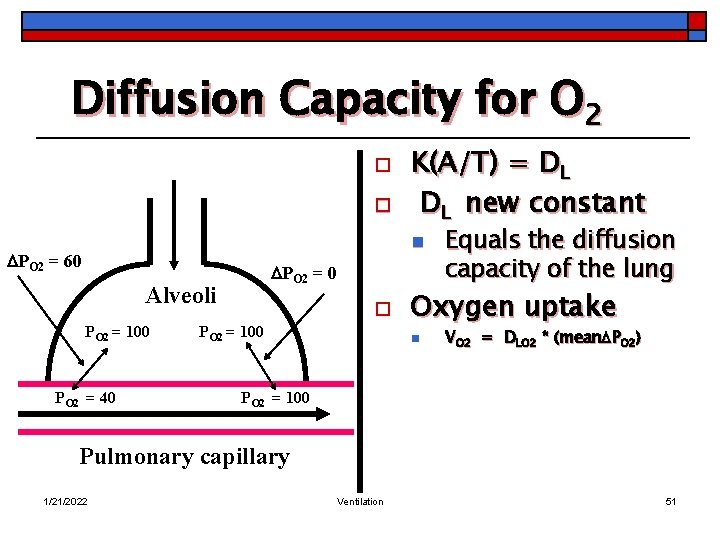
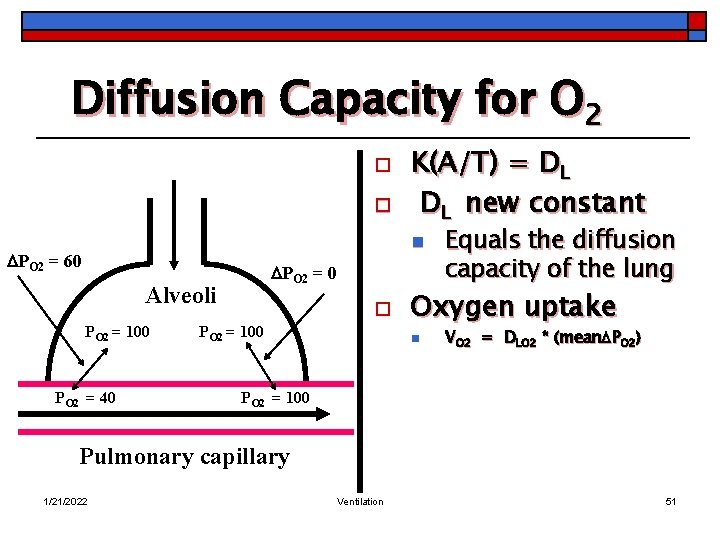
Diffusion Capacity for O 2 o o K(A/T) = DL DL new constant n PO 2 = 60 PO 2 = 0 Alveoli PO 2 = 100 PO 2 = 40 o PO 2 = 100 Equals the diffusion capacity of the lung Oxygen uptake n VO 2 = DLO 2 * (mean PO 2) PO 2 = 100 Pulmonary capillary 1/21/2022 Ventilation 51
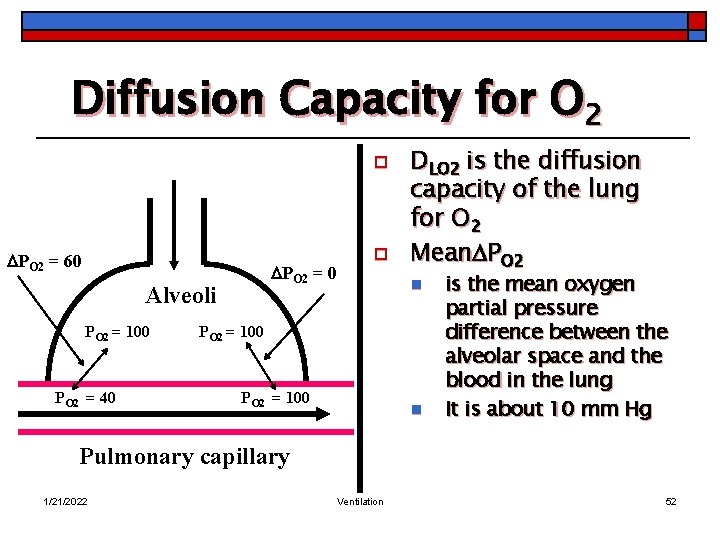
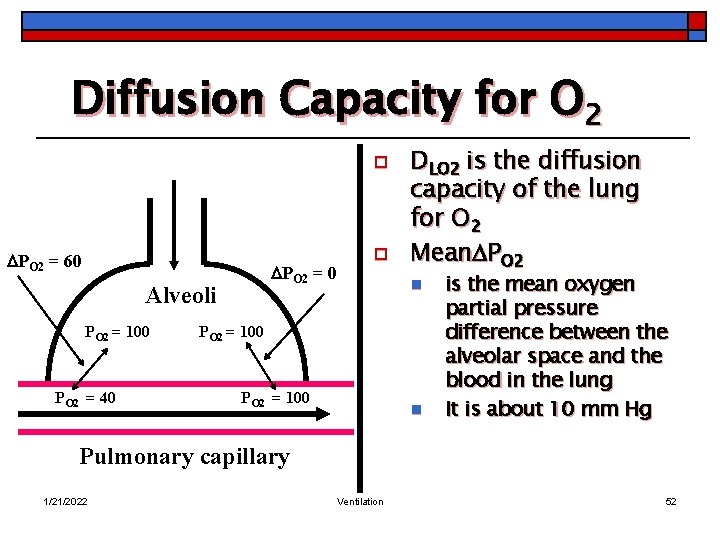
Diffusion Capacity for O 2 o PO 2 = 60 PO 2 = 0 Alveoli PO 2 = 100 PO 2 = 40 o DLO 2 is the diffusion capacity of the lung for O 2 Mean PO 2 = 100 n is the mean oxygen partial pressure difference between the alveolar space and the blood in the lung It is about 10 mm Hg Pulmonary capillary 1/21/2022 Ventilation 52
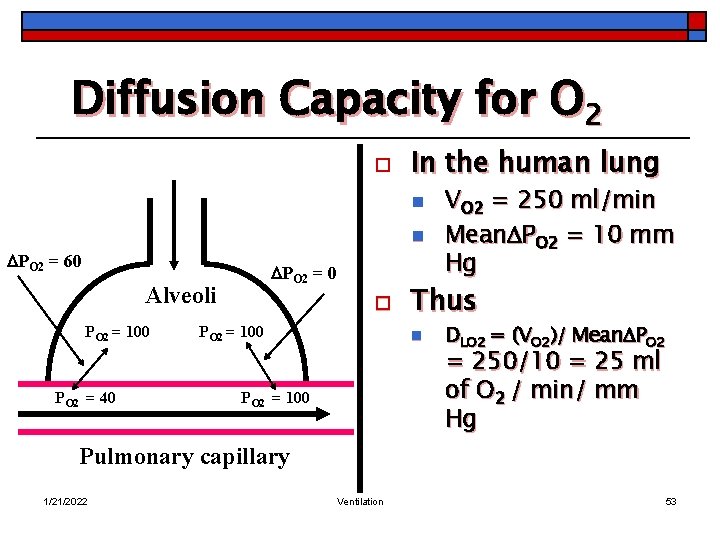
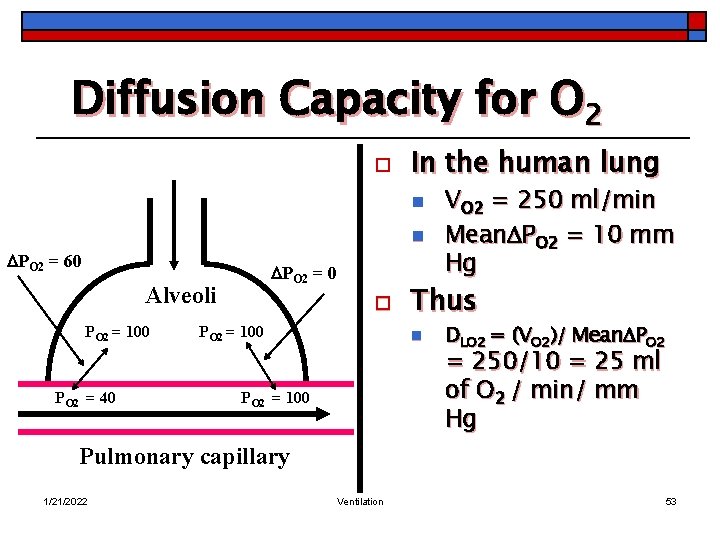
Diffusion Capacity for O 2 o In the human lung n n PO 2 = 60 PO 2 = 0 Alveoli PO 2 = 100 PO 2 = 40 o PO 2 = 100 Thus n PO 2 = 100 VO 2 = 250 ml/min Mean PO 2 = 10 mm Hg DLO 2 = (VO 2)/ Mean PO 2 = 250/10 = 25 ml of O 2 / min/ mm Hg Pulmonary capillary 1/21/2022 Ventilation 53
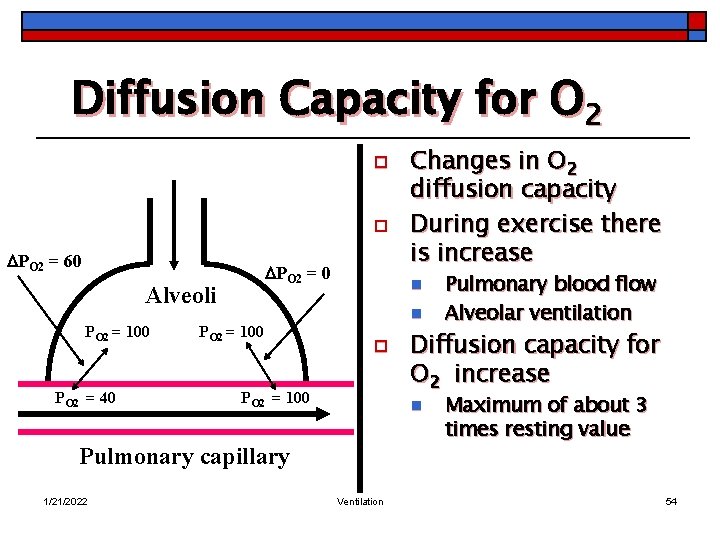
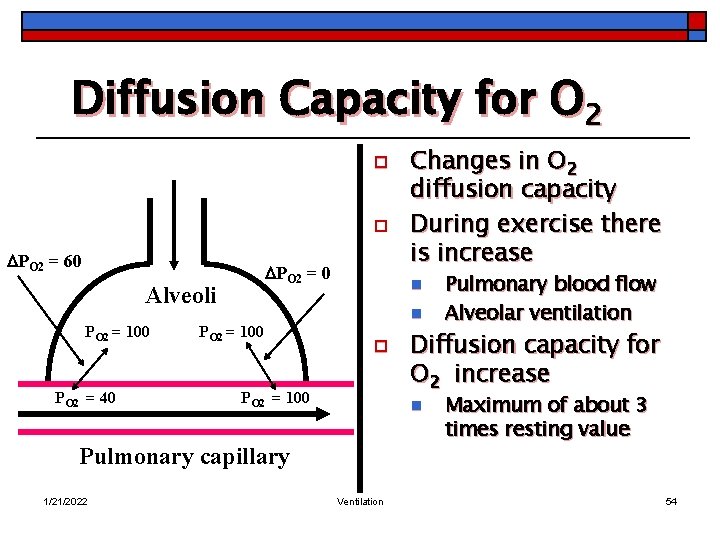
Diffusion Capacity for O 2 o o PO 2 = 60 PO 2 = 0 Alveoli PO 2 = 100 PO 2 = 40 PO 2 = 100 n n o PO 2 = 100 Ventilation Pulmonary blood flow Alveolar ventilation Diffusion capacity for O 2 increase n Pulmonary capillary 1/21/2022 Changes in O 2 diffusion capacity During exercise there is increase Maximum of about 3 times resting value 54
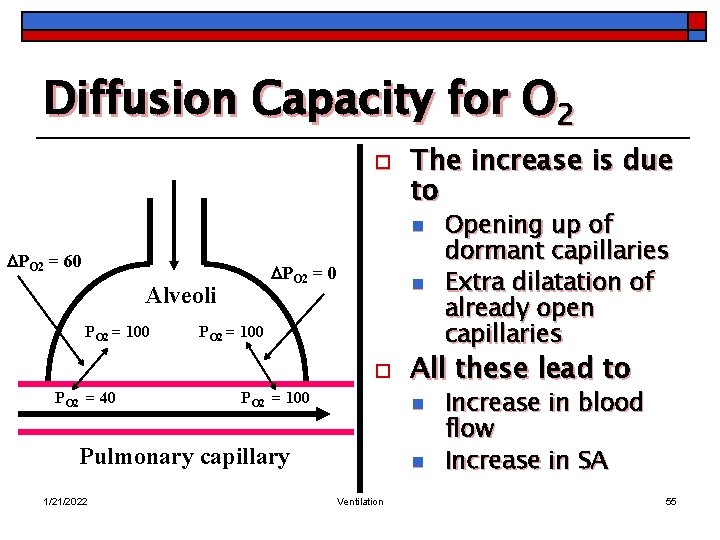
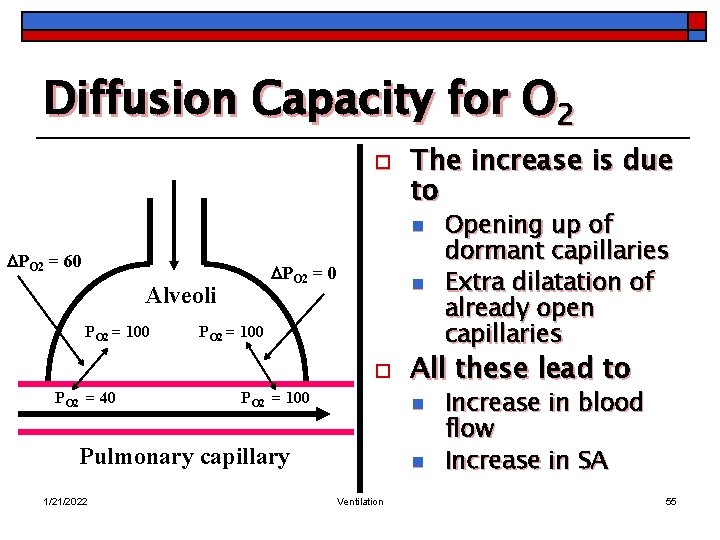
Diffusion Capacity for O 2 o The increase is due to n PO 2 = 60 PO 2 = 0 Alveoli PO 2 = 100 n PO 2 = 100 o PO 2 = 40 PO 2 = 100 1/21/2022 All these lead to n Pulmonary capillary n Ventilation Opening up of dormant capillaries Extra dilatation of already open capillaries Increase in blood flow Increase in SA 55
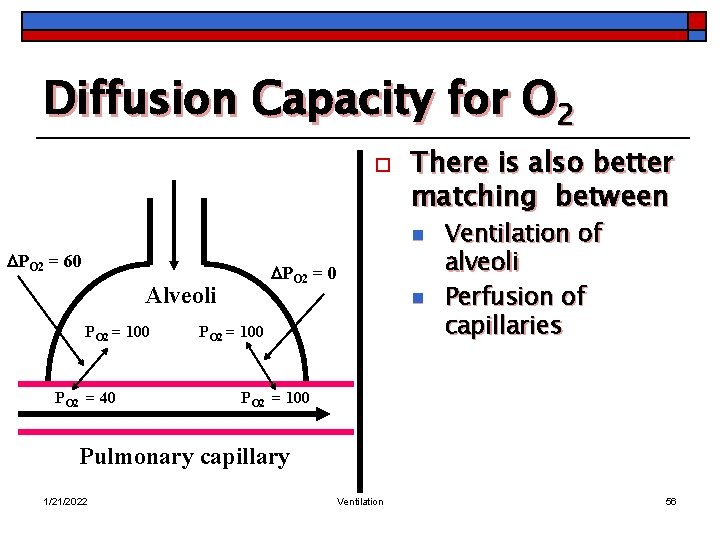
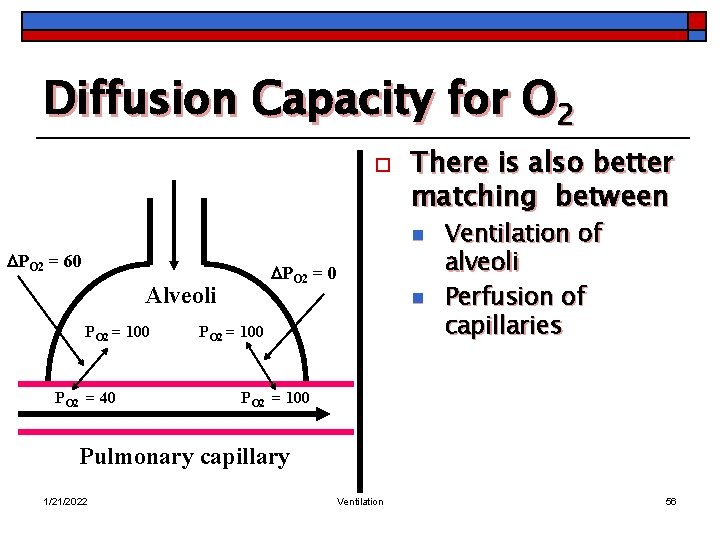
Diffusion Capacity for O 2 o There is also better matching between n PO 2 = 60 PO 2 = 0 Alveoli PO 2 = 100 PO 2 = 40 n PO 2 = 100 Ventilation of alveoli Perfusion of capillaries PO 2 = 100 Pulmonary capillary 1/21/2022 Ventilation 56
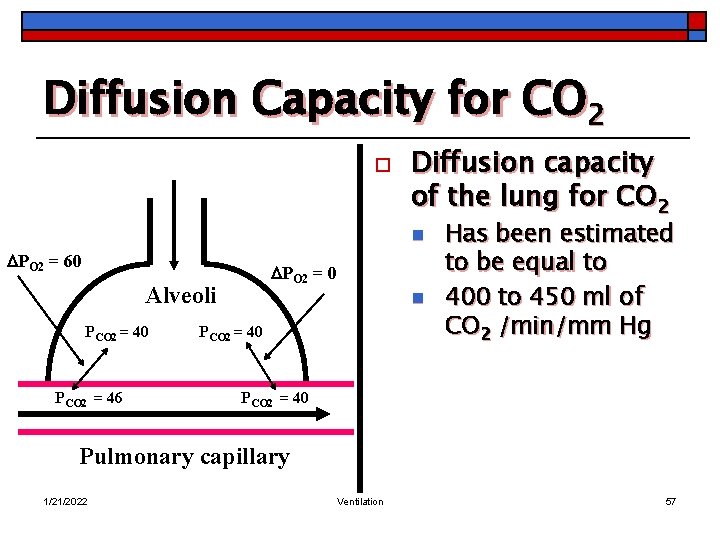
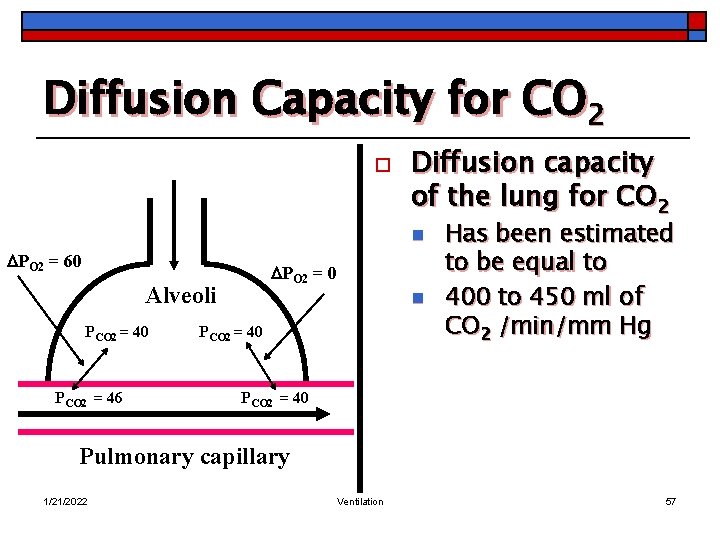
Diffusion Capacity for CO 2 o Diffusion capacity of the lung for CO 2 n PO 2 = 60 PO 2 = 0 Alveoli PCO 2 = 40 PCO 2 = 46 n PCO 2 = 40 Has been estimated to be equal to 400 to 450 ml of CO 2 /min/mm Hg PCO 2 = 40 Pulmonary capillary 1/21/2022 Ventilation 57
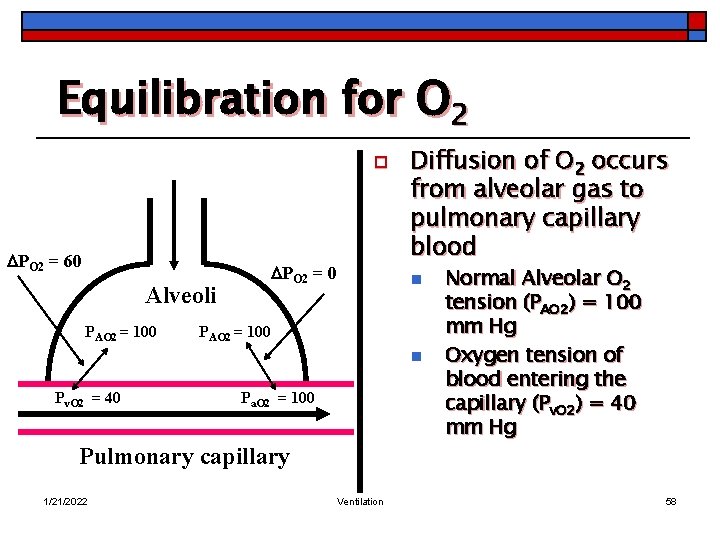
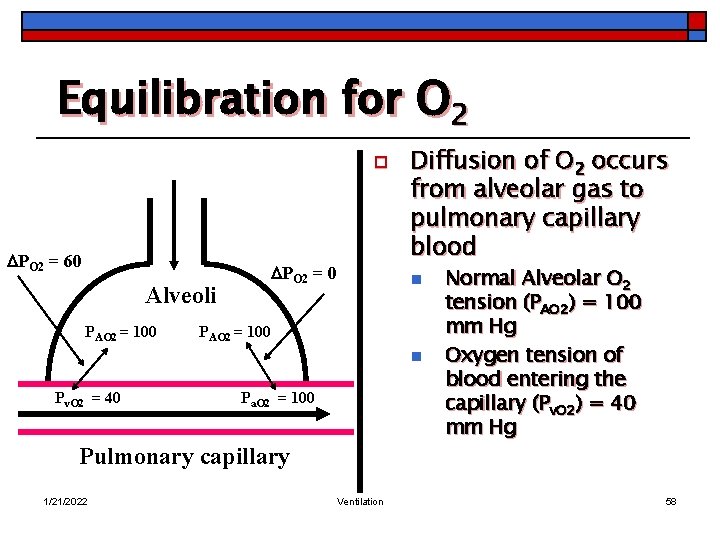
Equilibration for O 2 o PO 2 = 60 Alveoli PAO 2 = 100 PO 2 = 0 Diffusion of O 2 occurs from alveolar gas to pulmonary capillary blood n PAO 2 = 100 n Pv. O 2 = 40 Pa. O 2 = 100 Pulmonary capillary 1/21/2022 Ventilation Normal Alveolar O 2 tension (PAO 2) = 100 mm Hg Oxygen tension of blood entering the capillary (Pv. O 2) = 40 mm Hg 58
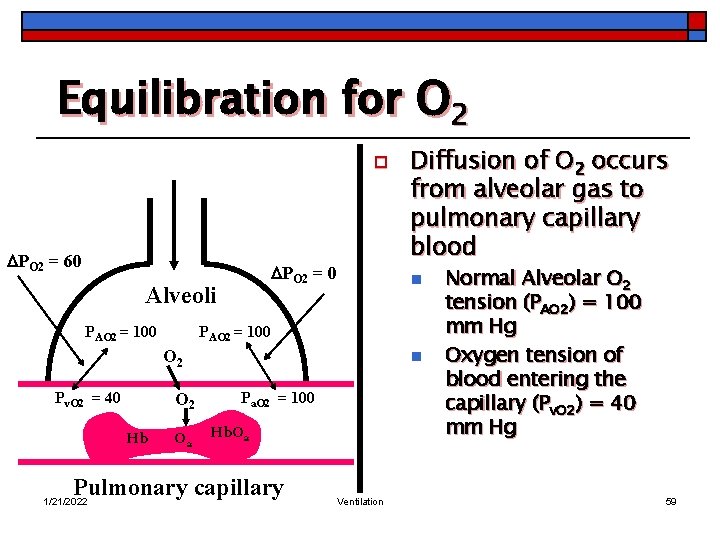
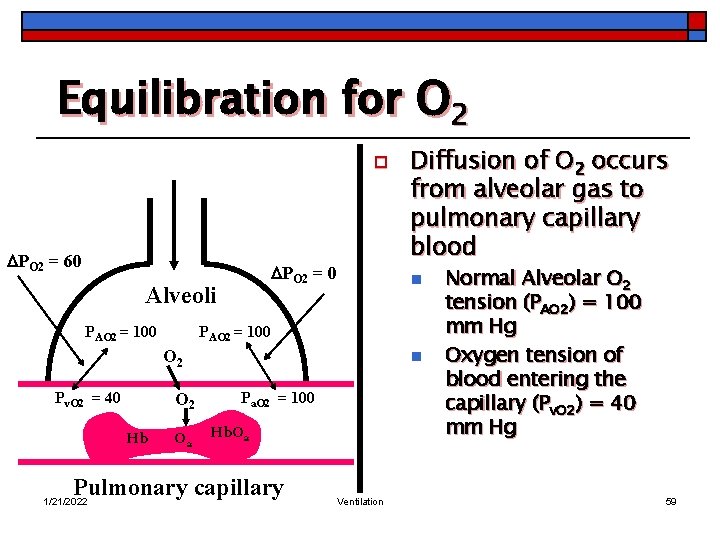
Equilibration for O 2 o PO 2 = 60 PO 2 = 0 Alveoli PAO 2 = 100 n PAO 2 = 100 O 2 Pv. O 2 = 40 O 2 Hb O 2 n Pa. O 2 = 100 Hb. O 2 Pulmonary capillary 1/21/2022 Diffusion of O 2 occurs from alveolar gas to pulmonary capillary blood Ventilation Normal Alveolar O 2 tension (PAO 2) = 100 mm Hg Oxygen tension of blood entering the capillary (Pv. O 2) = 40 mm Hg 59

Equilibration for O 2 o PO 2 = 60 PAO 2 = 100 n PO 2 = 0 Alveoli After crossing the alveolar/capillary membrane n PAO 2 = 100 O 2 Pv. O 2 = 40 O 2 Hb. O 2 Pulmonary capillary 1/21/2022 n Pa. O 2 = 100 Ventilation O 2 diffuse in plasma Raising plasma O 2 tension Cause O 2 to diffuse into RBC 60
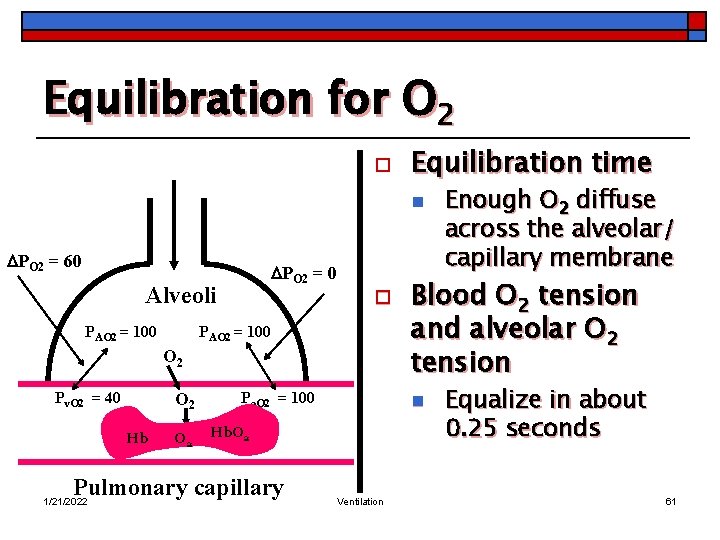
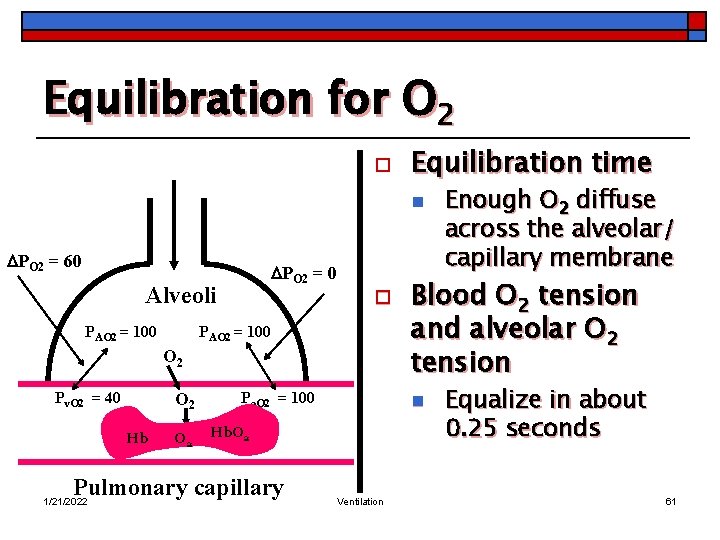
Equilibration for O 2 o Equilibration time n PO 2 = 60 PO 2 = 0 Alveoli PAO 2 = 100 o PAO 2 = 100 O 2 Pv. O 2 = 40 O 2 Hb O 2 Pa. O 2 = 100 Pulmonary capillary 1/21/2022 Blood O 2 tension and alveolar O 2 tension n Hb. O 2 Ventilation Enough O 2 diffuse across the alveolar/ capillary membrane Equalize in about 0. 25 seconds 61
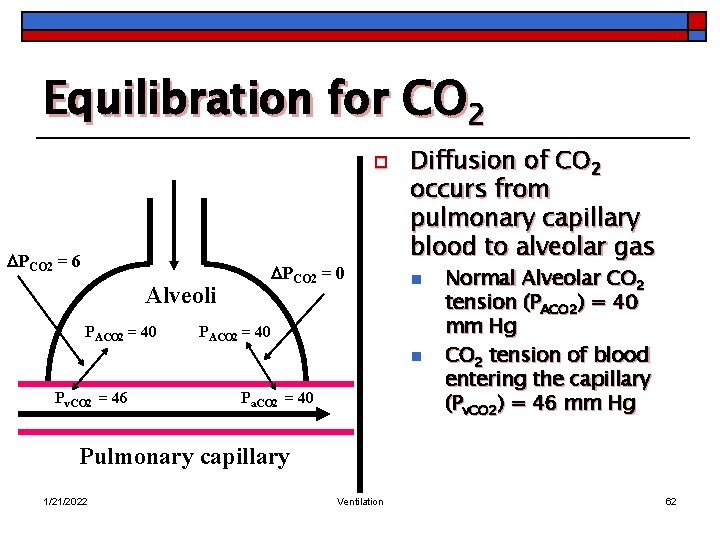
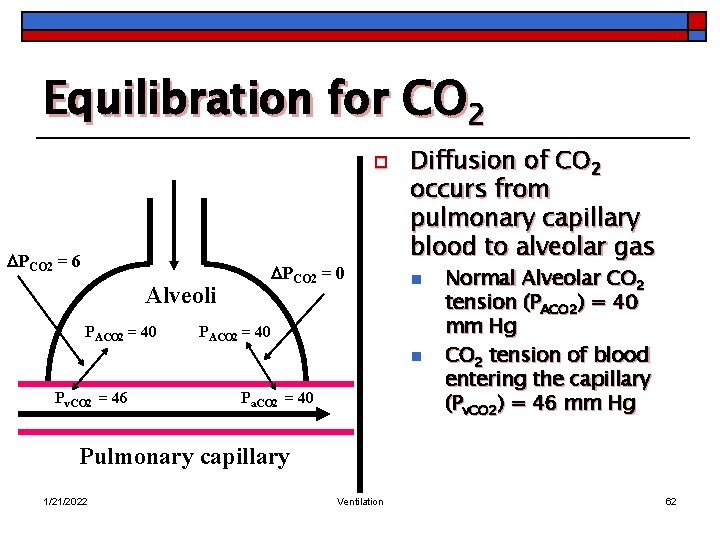
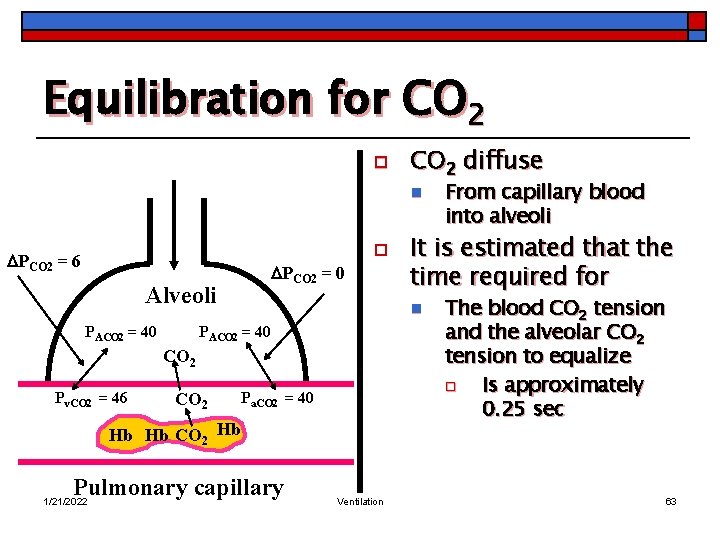
Equilibration for CO 2 o PCO 2 = 6 PCO 2 = 0 Alveoli PACO 2 = 40 Diffusion of CO 2 occurs from pulmonary capillary blood to alveolar gas n PACO 2 = 40 n Pv. CO 2 = 46 Pa. CO 2 = 40 Normal Alveolar CO 2 tension (PACO 2) = 40 mm Hg CO 2 tension of blood entering the capillary (Pv. CO 2) = 46 mm Hg Pulmonary capillary 1/21/2022 Ventilation 62
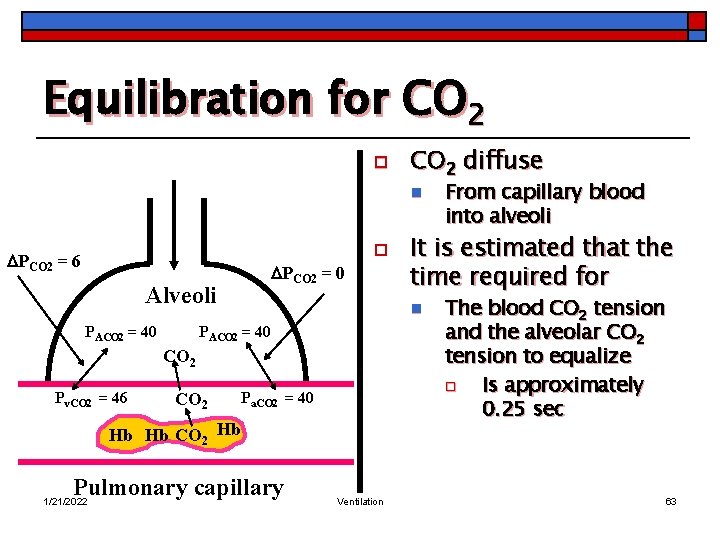
Equilibration for CO 2 o CO 2 diffuse n o PCO 2 = 6 PCO 2 = 0 Alveoli PACO 2 = 40 CO 2 Pv. CO 2 = 46 CO 2 Pa. CO 2 = 40 Hb Hb CO 2 Hb Pulmonary capillary 1/21/2022 It is estimated that the time required for n PACO 2 = 40 Ventilation From capillary blood into alveoli The blood CO 2 tension and the alveolar CO 2 tension to equalize o Is approximately 0. 25 sec 63
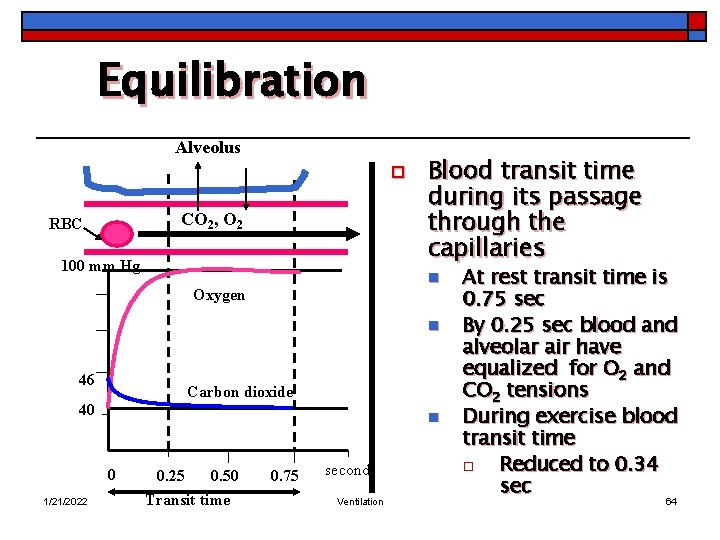
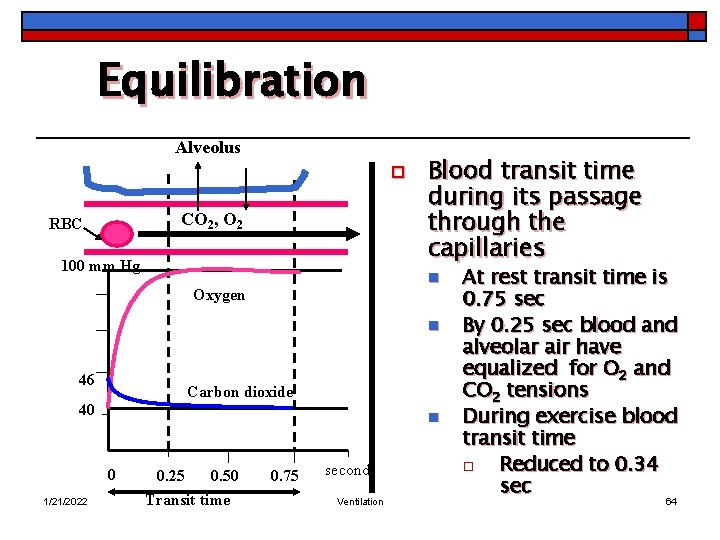
Equilibration Alveolus o CO 2, O 2 RBC 100 mm Hg Blood transit time during its passage through the capillaries n Oxygen n 46 Carbon dioxide 40 n 0 1/21/2022 0. 25 0. 50 Transit time 0. 75 seconds Ventilation At rest transit time is 0. 75 sec By 0. 25 sec blood and alveolar air have equalized for O 2 and CO 2 tensions During exercise blood transit time o Reduced to 0. 34 sec 64
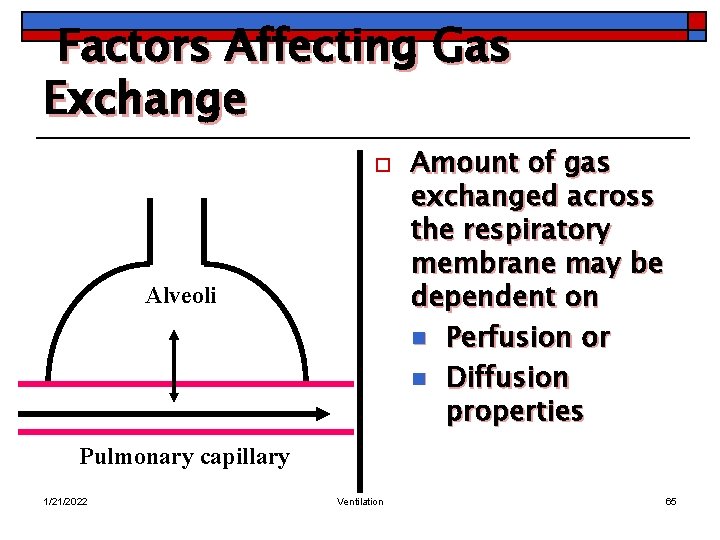
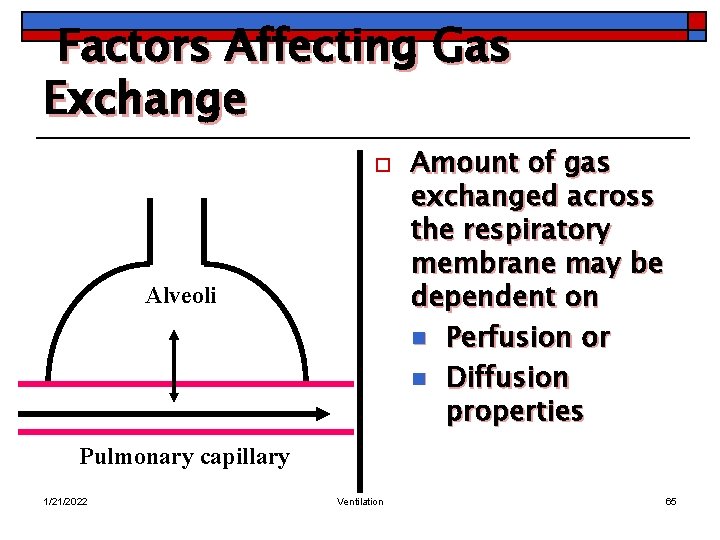
Factors Affecting Gas Exchange o Alveoli Amount of gas exchanged across the respiratory membrane may be dependent on n Perfusion or n Diffusion properties Pulmonary capillary 1/21/2022 Ventilation 65
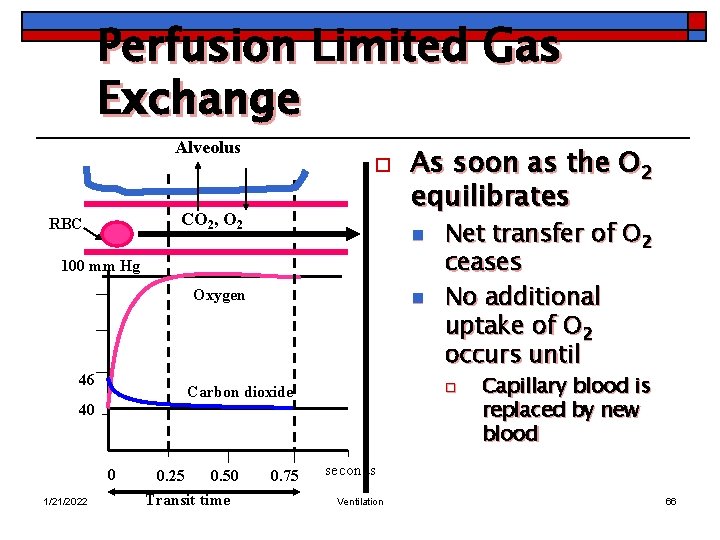
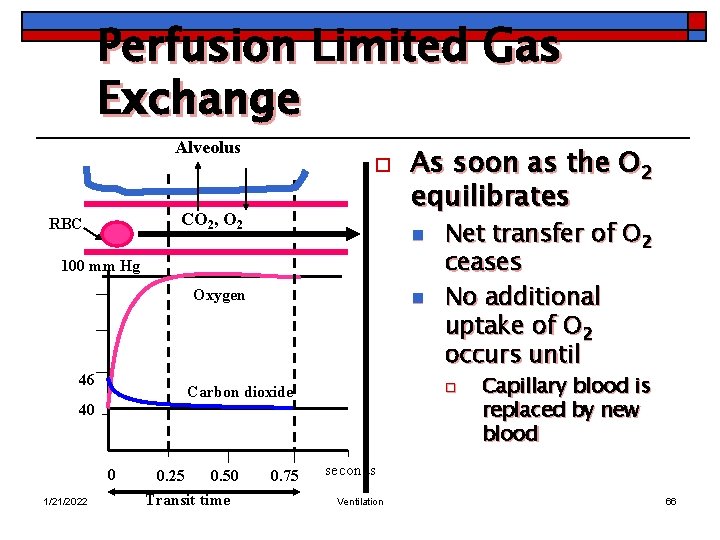
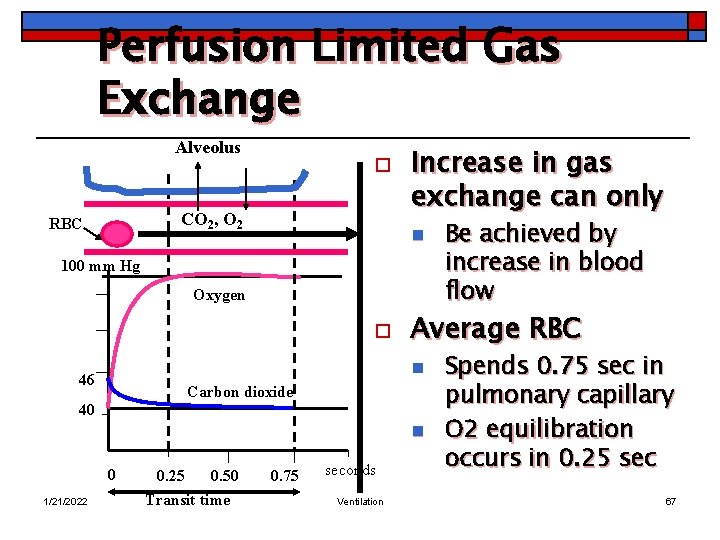
Perfusion Limited Gas Exchange Alveolus o CO 2, O 2 RBC As soon as the O 2 equilibrates n 100 mm Hg Oxygen 46 n o Carbon dioxide 40 0 1/21/2022 0. 25 0. 50 Transit time 0. 75 Net transfer of O 2 ceases No additional uptake of O 2 occurs until Capillary blood is replaced by new blood seconds Ventilation 66
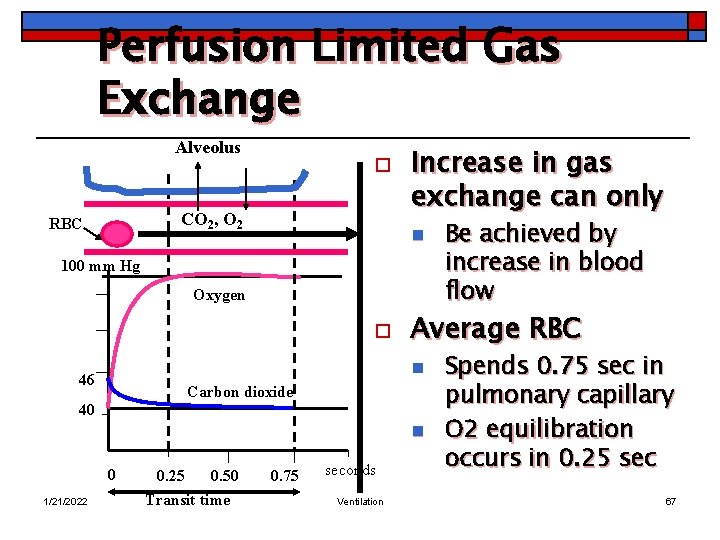
Perfusion Limited Gas Exchange Alveolus o CO 2, O 2 RBC Increase in gas exchange can only n 100 mm Hg Oxygen o Average RBC n 46 Carbon dioxide 40 n 0 1/21/2022 0. 25 0. 50 Transit time 0. 75 seconds Ventilation Be achieved by increase in blood flow Spends 0. 75 sec in pulmonary capillary O 2 equilibration occurs in 0. 25 sec 67
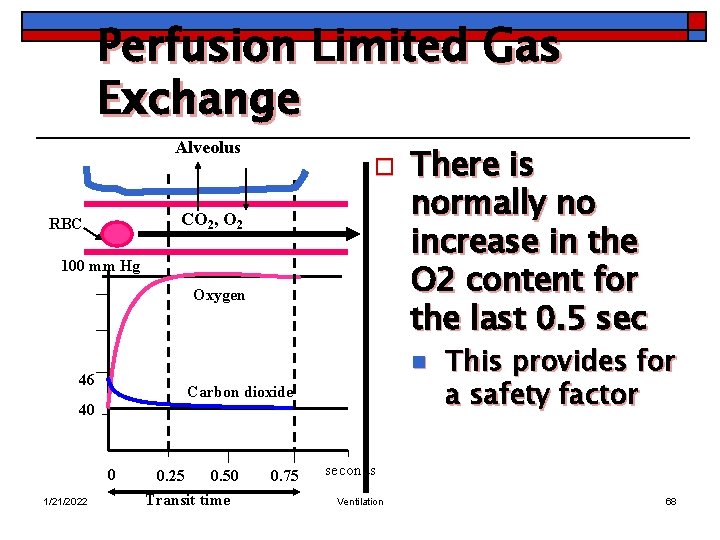
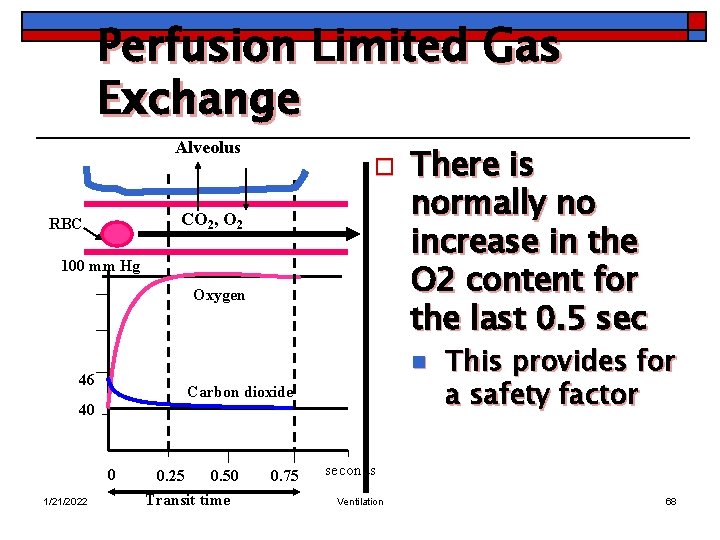
Perfusion Limited Gas Exchange Alveolus o CO 2, O 2 RBC 100 mm Hg Oxygen n 46 Carbon dioxide 40 0 1/21/2022 There is normally no increase in the O 2 content for the last 0. 5 sec 0. 25 0. 50 Transit time 0. 75 This provides for a safety factor seconds Ventilation 68
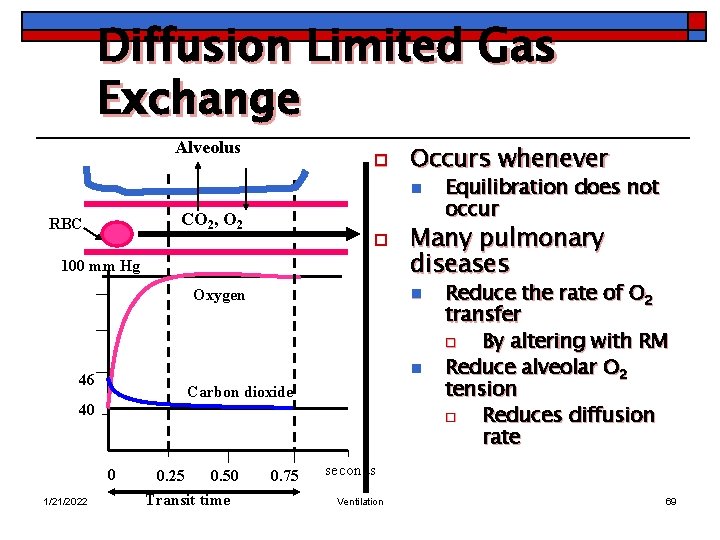
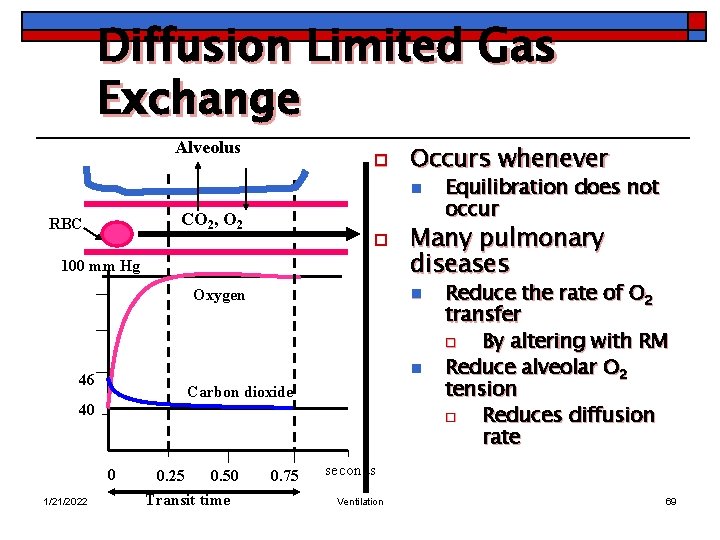
Diffusion Limited Gas Exchange Alveolus o Occurs whenever n CO 2, O 2 RBC o 100 mm Hg n 46 Carbon dioxide 40 0 1/21/2022 Many pulmonary diseases n Oxygen 0. 25 0. 50 Transit time 0. 75 Equilibration does not occur Reduce the rate of O 2 transfer o By altering with RM Reduce alveolar O 2 tension o Reduces diffusion rate seconds Ventilation 69
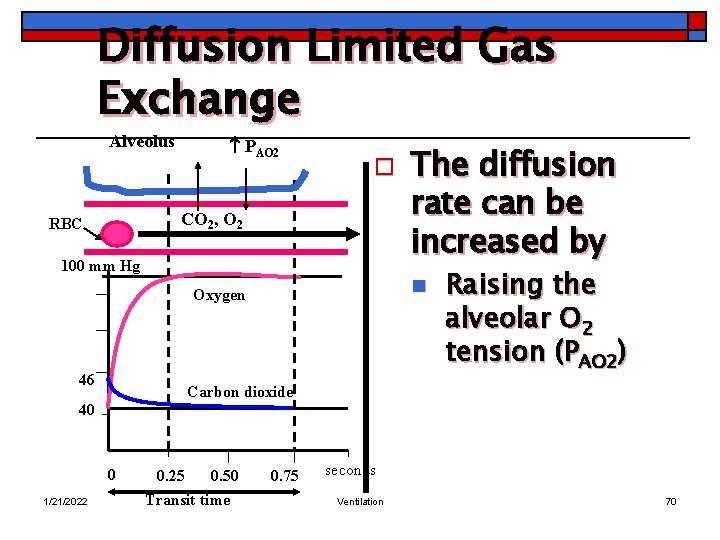
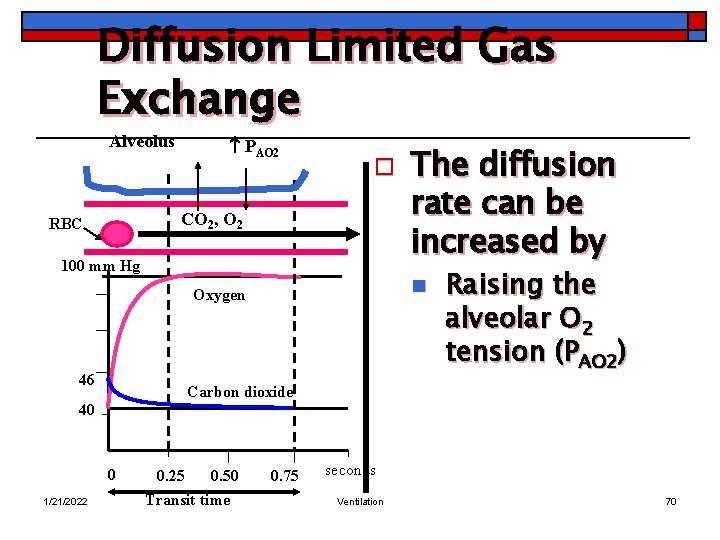
Diffusion Limited Gas Exchange Alveolus PAO 2 o CO 2, O 2 RBC 100 mm Hg n Oxygen 46 The diffusion rate can be increased by Raising the alveolar O 2 tension (PAO 2) Carbon dioxide 40 0 1/21/2022 0. 25 0. 50 Transit time 0. 75 seconds Ventilation 70
Blood Flow Q 1/21/2022 Ventilation 71
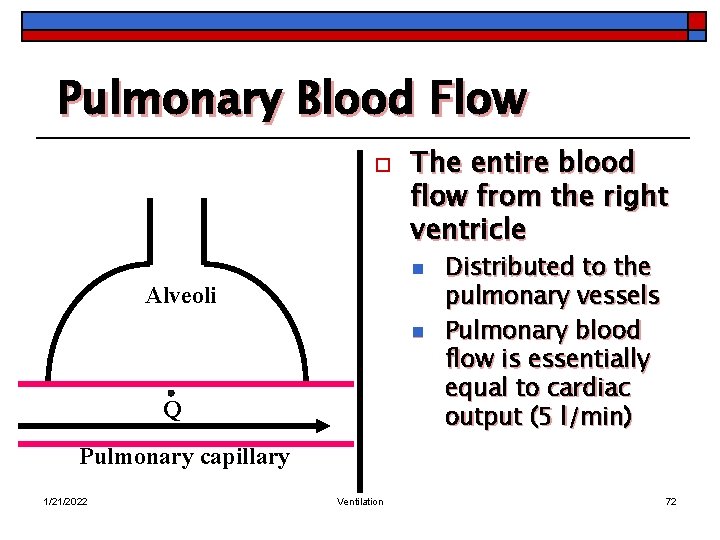
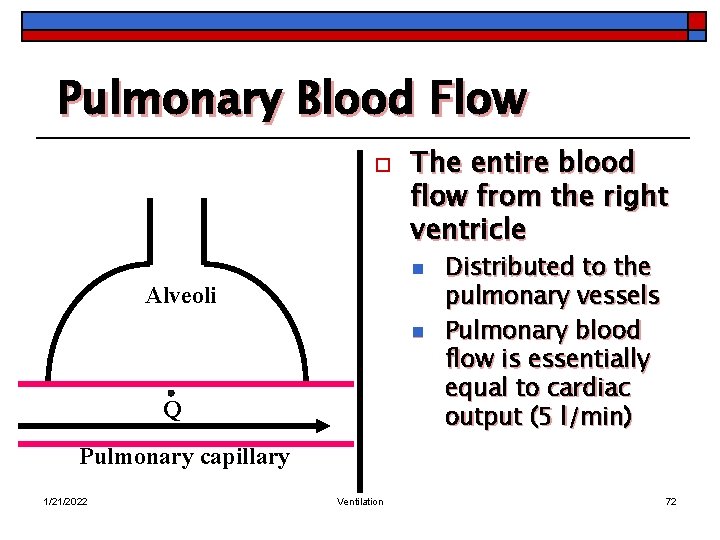
Pulmonary Blood Flow o The entire blood flow from the right ventricle n Alveoli n Q Distributed to the pulmonary vessels Pulmonary blood flow is essentially equal to cardiac output (5 l/min) Pulmonary capillary 1/21/2022 Ventilation 72
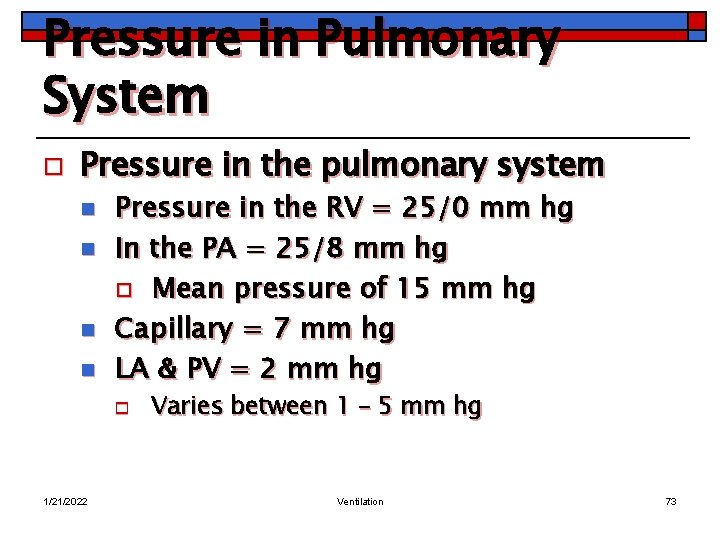
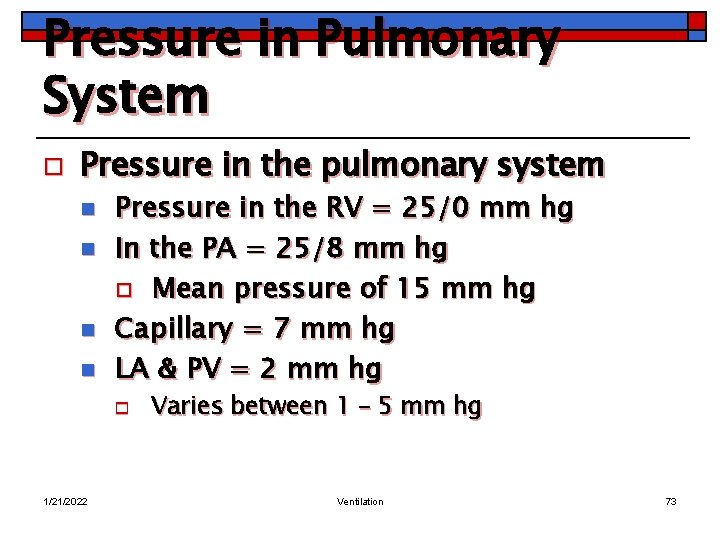
Pressure in Pulmonary System o Pressure in the pulmonary system n n Pressure in the RV = 25/0 mm hg In the PA = 25/8 mm hg o Mean pressure of 15 mm hg Capillary = 7 mm hg LA & PV = 2 mm hg o 1/21/2022 Varies between 1 – 5 mm hg Ventilation 73
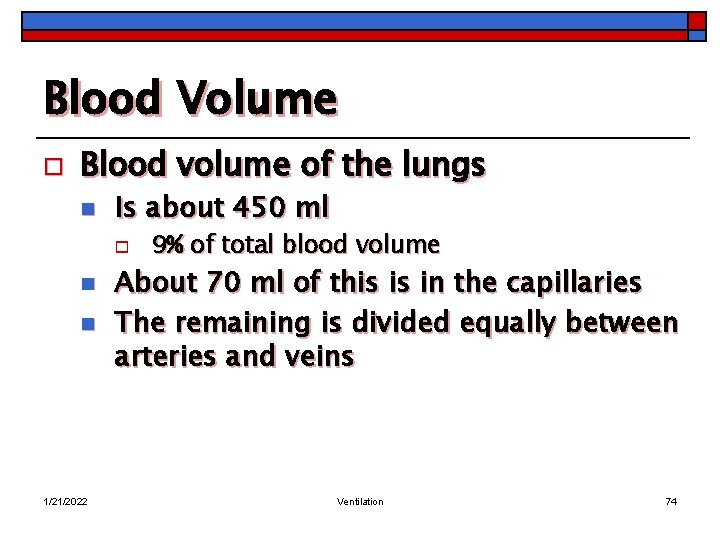
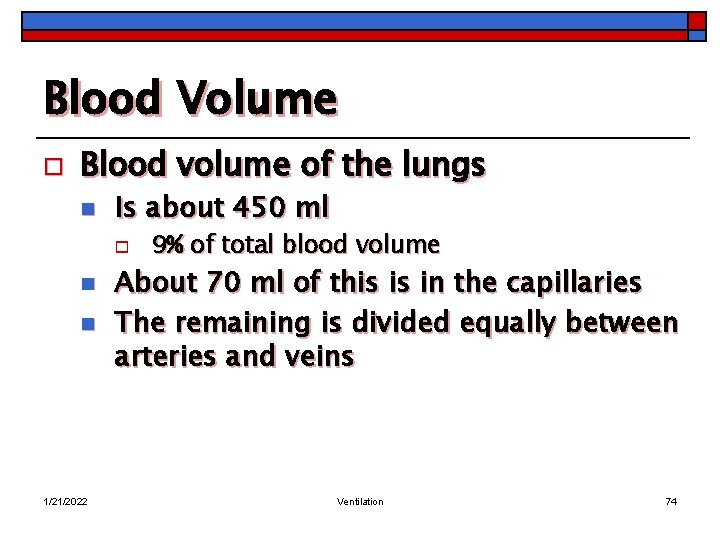
Blood Volume o Blood volume of the lungs n Is about 450 ml o n n 1/21/2022 9% of total blood volume About 70 ml of this is in the capillaries The remaining is divided equally between arteries and veins Ventilation 74
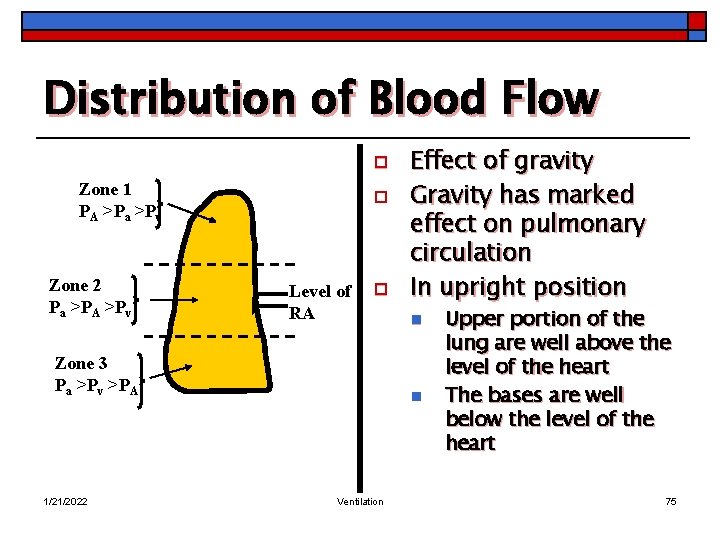
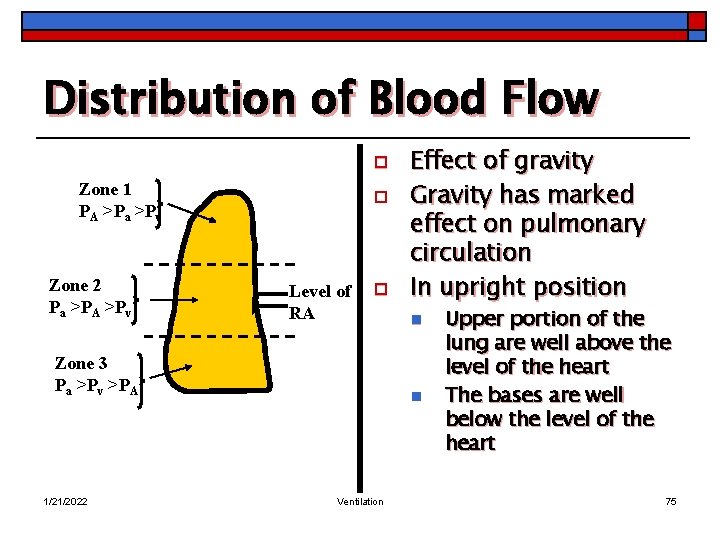
Distribution of Blood Flow o Zone 1 PA >Pa >Pv Zone 2 Pa >PA >Pv o Level of RA o Zone 3 Pa >Pv >PA 1/21/2022 Effect of gravity Gravity has marked effect on pulmonary circulation In upright position n n Ventilation Upper portion of the lung are well above the level of the heart The bases are well below the level of the heart 75
Distribution of Blood Flow o Zone 1 PA >Pa >Pv There are marked pressure gradients n Zone 2 Pa >PA >Pv Level of RA In the pulmonary arteries from top to bottom of the lung Zone 3 Pa >Pv >PA 1/21/2022 Ventilation 76
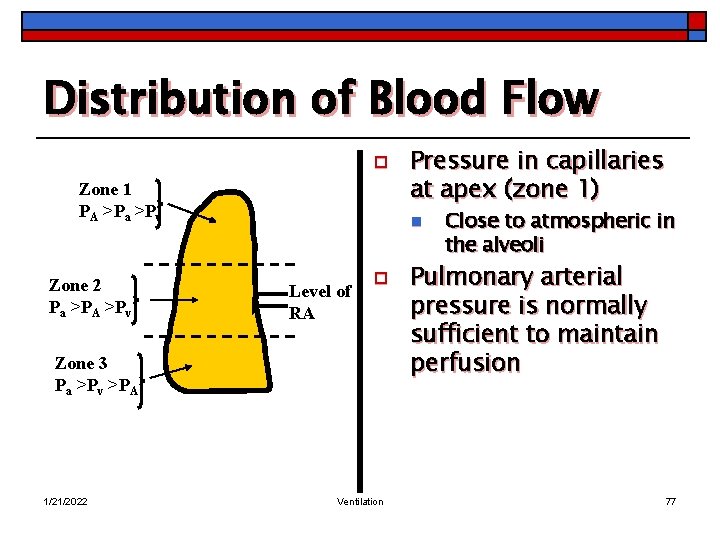
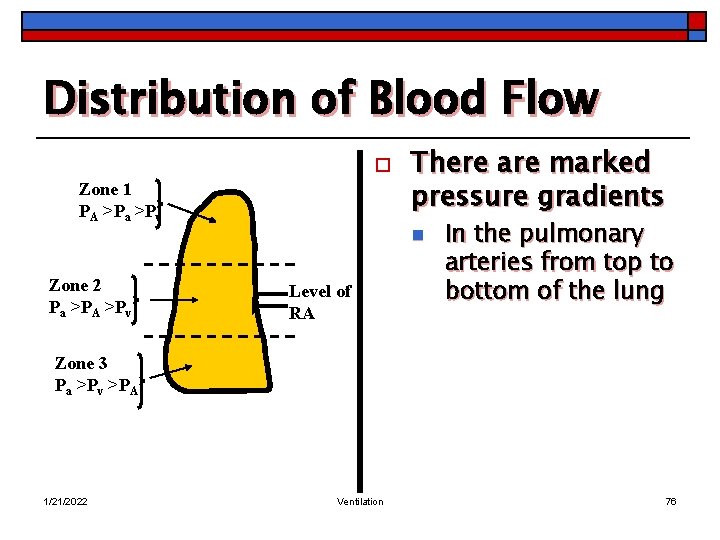
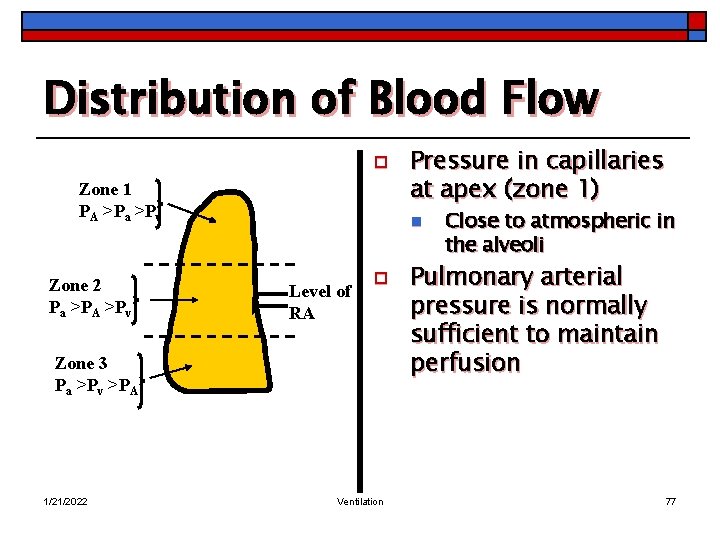
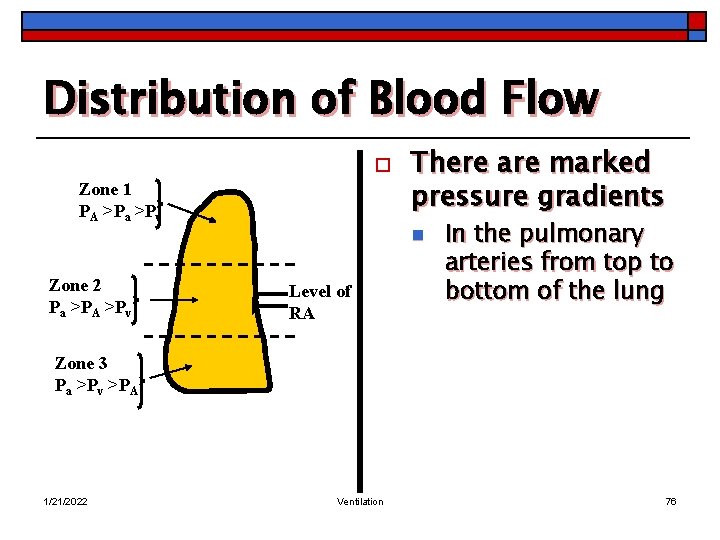
Distribution of Blood Flow o Zone 1 PA >Pa >Pv Zone 2 Pa >PA >Pv n Level of RA o Zone 3 Pa >Pv >PA 1/21/2022 Pressure in capillaries at apex (zone 1) Ventilation Close to atmospheric in the alveoli Pulmonary arterial pressure is normally sufficient to maintain perfusion 77
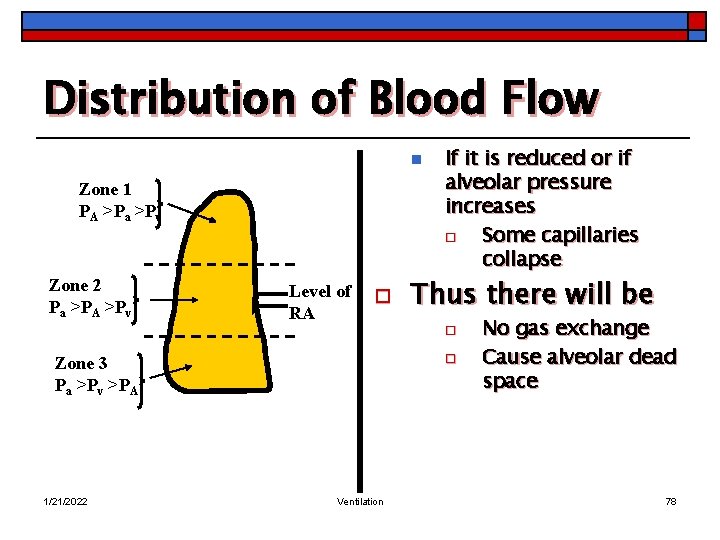
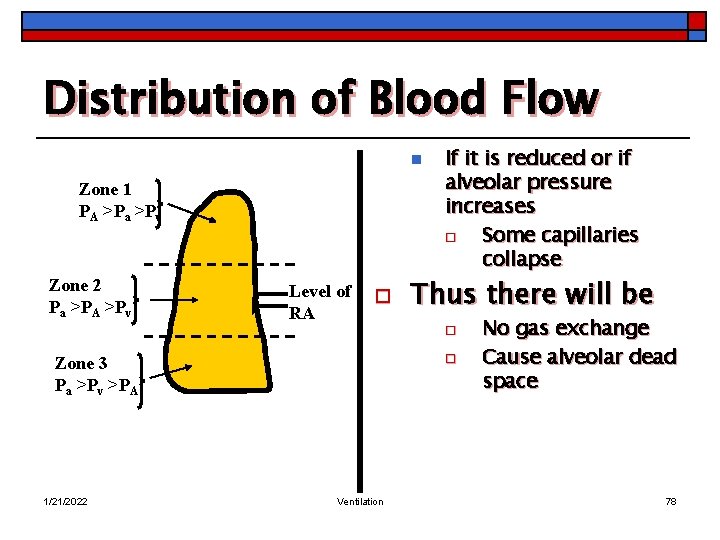
Distribution of Blood Flow n Zone 1 PA >Pa >Pv Zone 2 Pa >PA >Pv Level of RA o If it is reduced or if alveolar pressure increases o Some capillaries collapse Thus there will be o o Zone 3 Pa >Pv >PA 1/21/2022 Ventilation No gas exchange Cause alveolar dead space 78
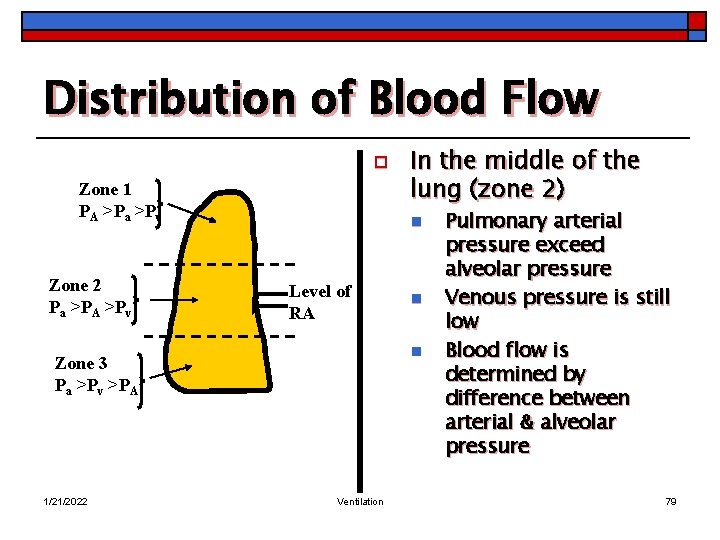
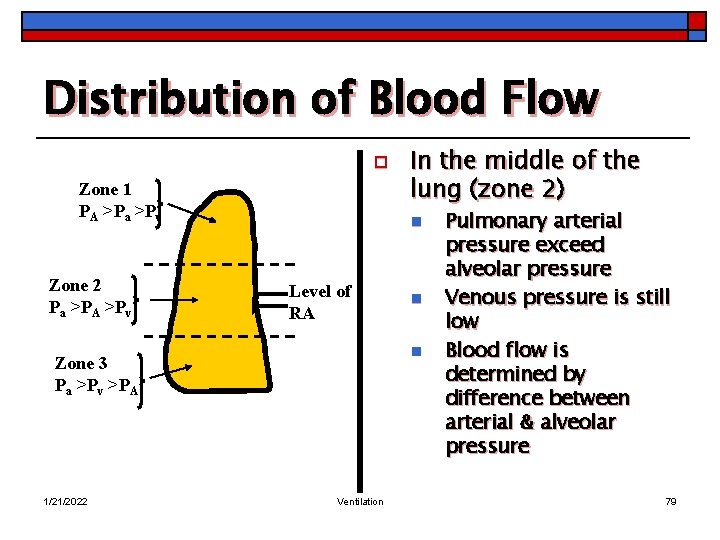
Distribution of Blood Flow o Zone 1 PA >Pa >Pv Zone 2 Pa >PA >Pv n Level of RA n n Zone 3 Pa >Pv >PA 1/21/2022 In the middle of the lung (zone 2) Ventilation Pulmonary arterial pressure exceed alveolar pressure Venous pressure is still low Blood flow is determined by difference between arterial & alveolar pressure 79
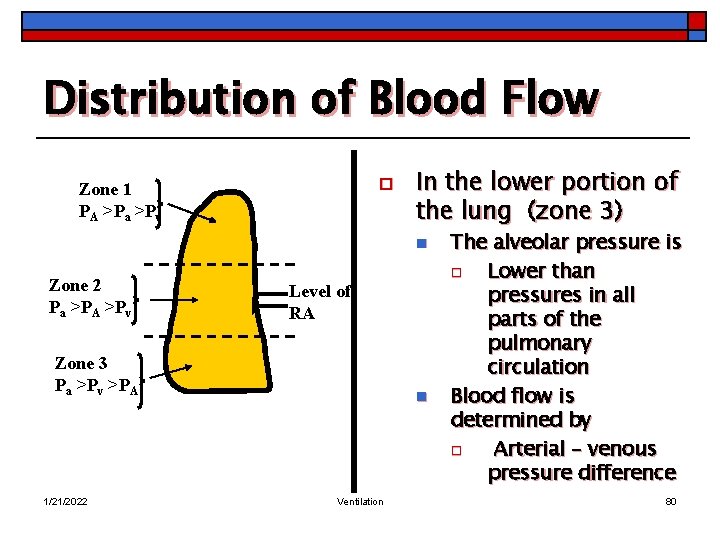
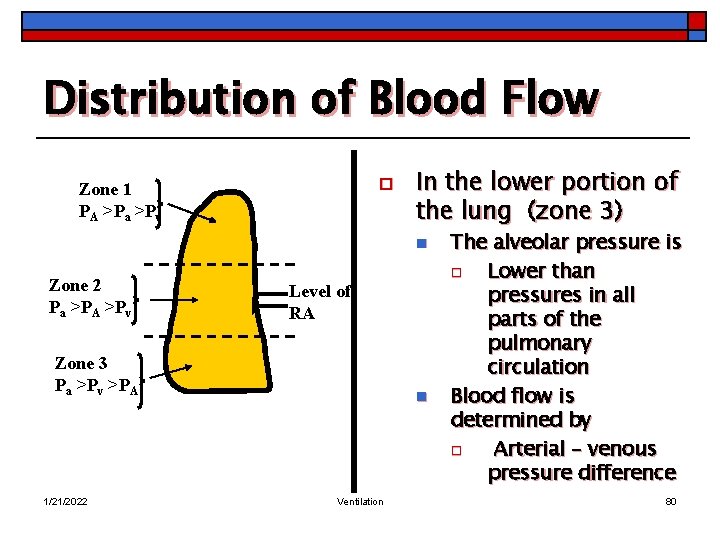
Distribution of Blood Flow o Zone 1 PA >Pa >Pv In the lower portion of the lung (zone 3) n Zone 2 Pa >PA >Pv Level of RA Zone 3 Pa >Pv >PA 1/21/2022 n Ventilation The alveolar pressure is o Lower than pressures in all parts of the pulmonary circulation Blood flow is determined by o Arterial – venous pressure difference 80
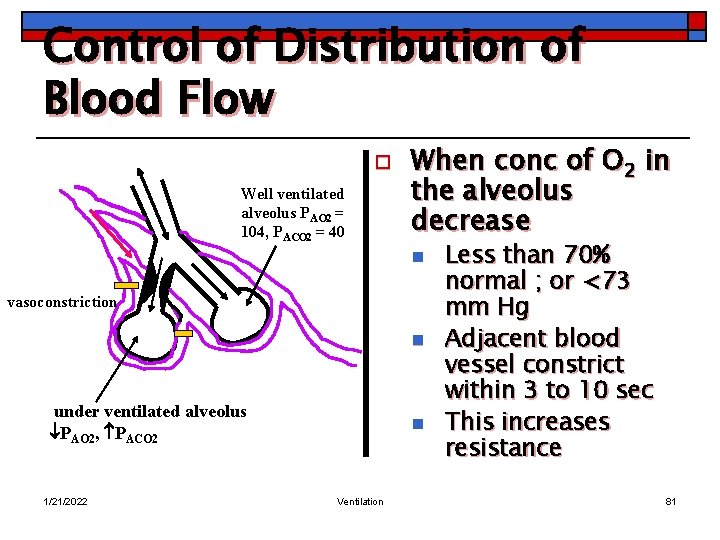
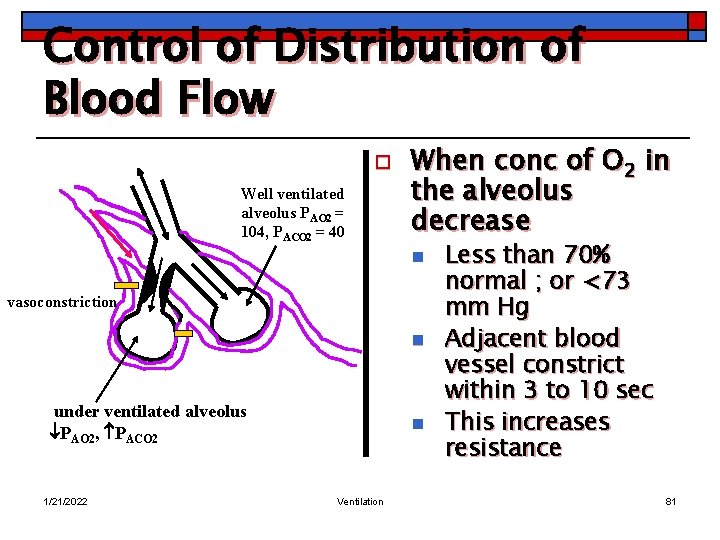
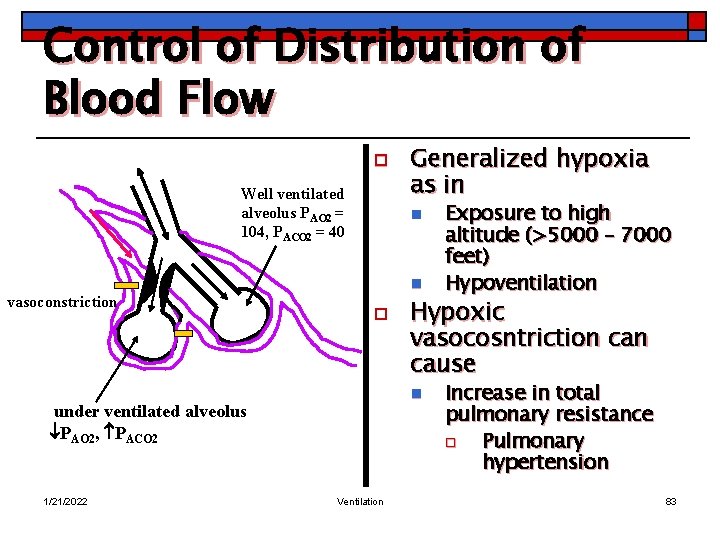
Control of Distribution of Blood Flow o Well ventilated alveolus PAO 2 = 104, PACO 2 = 40 When conc of O 2 in the alveolus decrease n vasoconstriction n under ventilated alveolus PAO 2, PACO 2 1/21/2022 n Ventilation Less than 70% normal ; or <73 mm Hg Adjacent blood vessel constrict within 3 to 10 sec This increases resistance 81
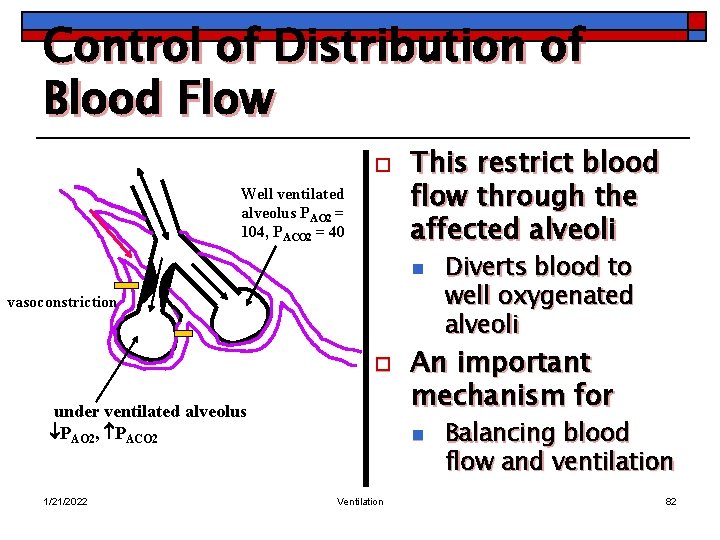
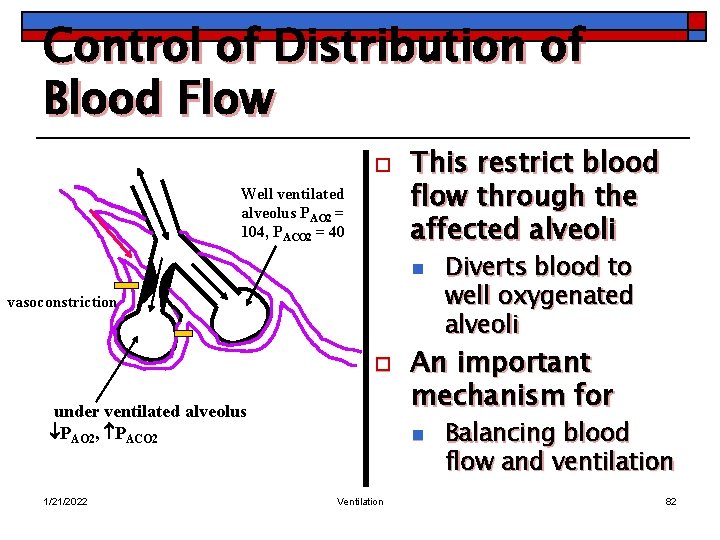
Control of Distribution of Blood Flow o Well ventilated alveolus PAO 2 = 104, PACO 2 = 40 This restrict blood flow through the affected alveoli n vasoconstriction o under ventilated alveolus PAO 2, PACO 2 1/21/2022 An important mechanism for n Ventilation Diverts blood to well oxygenated alveoli Balancing blood flow and ventilation 82
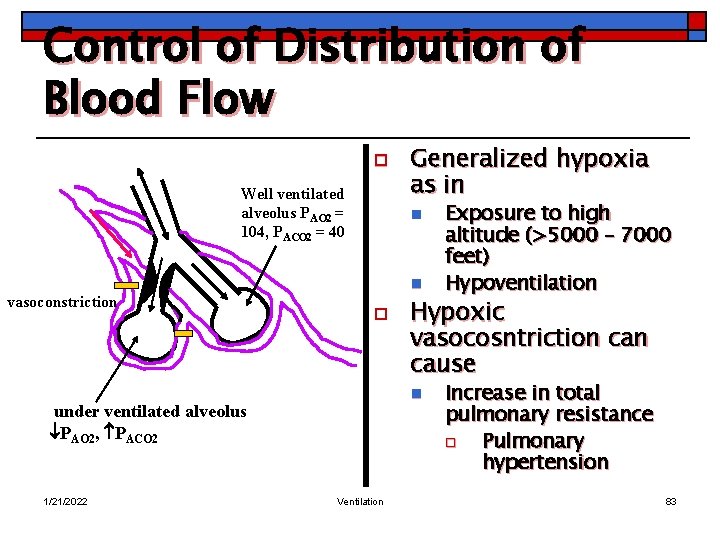
Control of Distribution of Blood Flow o Well ventilated alveolus PAO 2 = 104, PACO 2 = 40 vasoconstriction n n o Ventilation Exposure to high altitude (>5000 – 7000 feet) Hypoventilation Hypoxic vasocosntriction cause n under ventilated alveolus PAO 2, PACO 2 1/21/2022 Generalized hypoxia as in Increase in total pulmonary resistance o Pulmonary hypertension 83
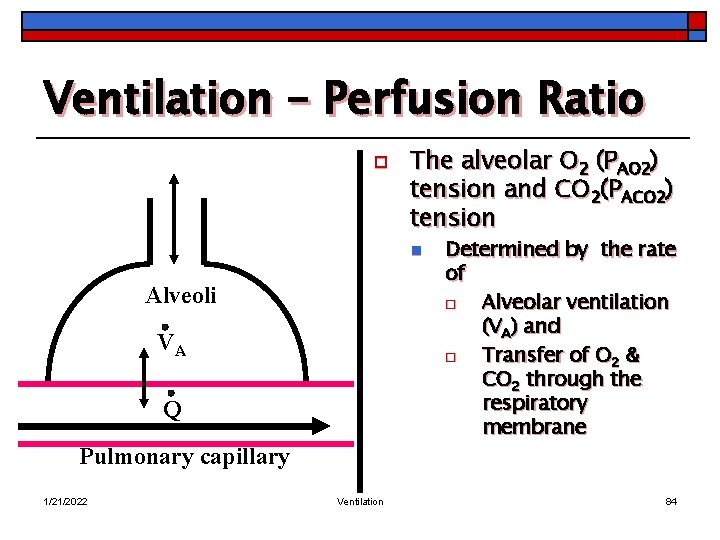
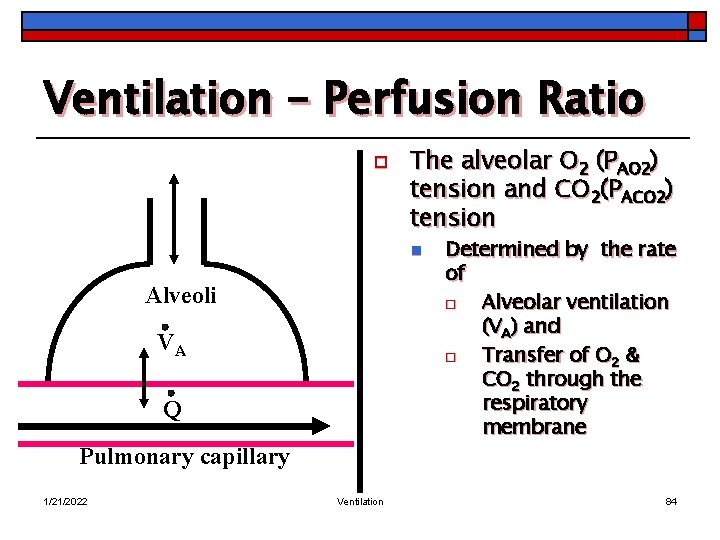
Ventilation – Perfusion Ratio o The alveolar O 2 (PAO 2) tension and CO 2(PACO 2) tension n Alveoli VA Q Pulmonary capillary 1/21/2022 Ventilation Determined by the rate of o Alveolar ventilation (VA) and o Transfer of O 2 & CO 2 through the respiratory membrane 84
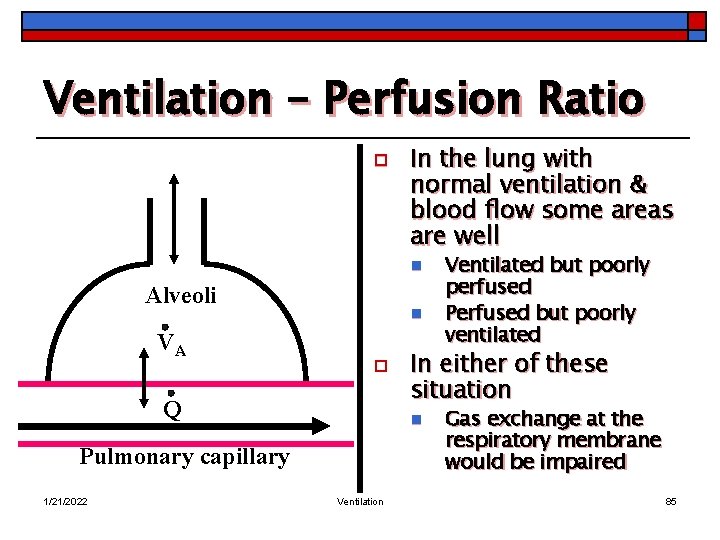
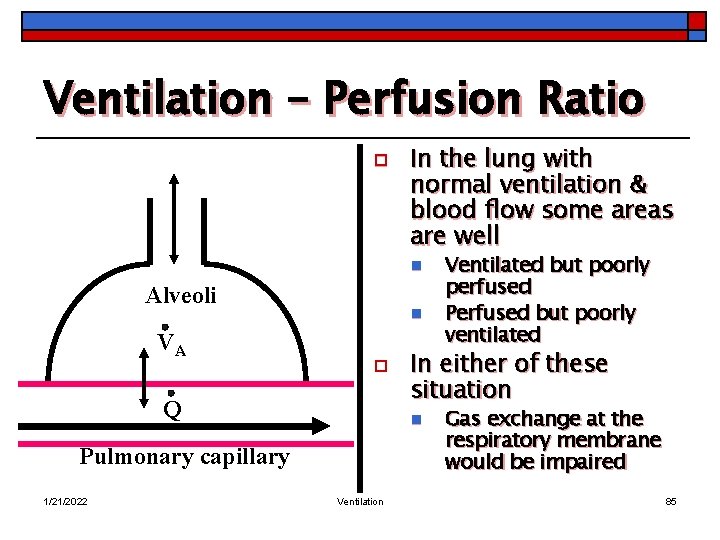
Ventilation – Perfusion Ratio o In the lung with normal ventilation & blood flow some areas are well n Alveoli VA n o Q 1/21/2022 In either of these situation n Pulmonary capillary Ventilation Ventilated but poorly perfused Perfused but poorly ventilated Gas exchange at the respiratory membrane would be impaired 85
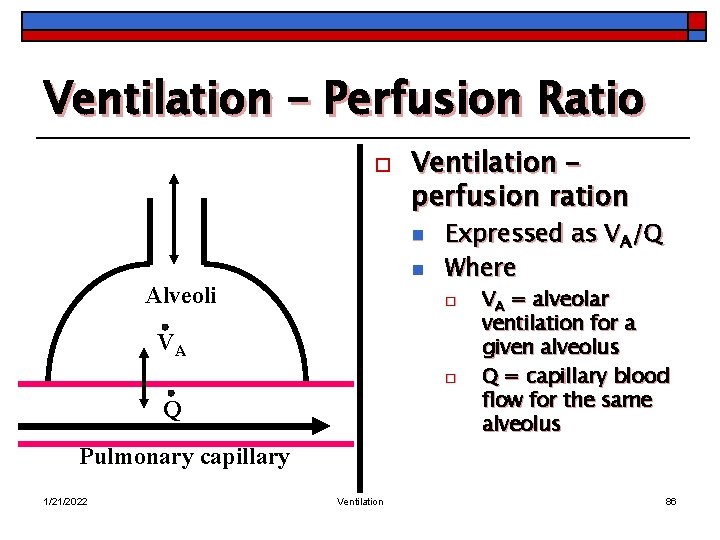
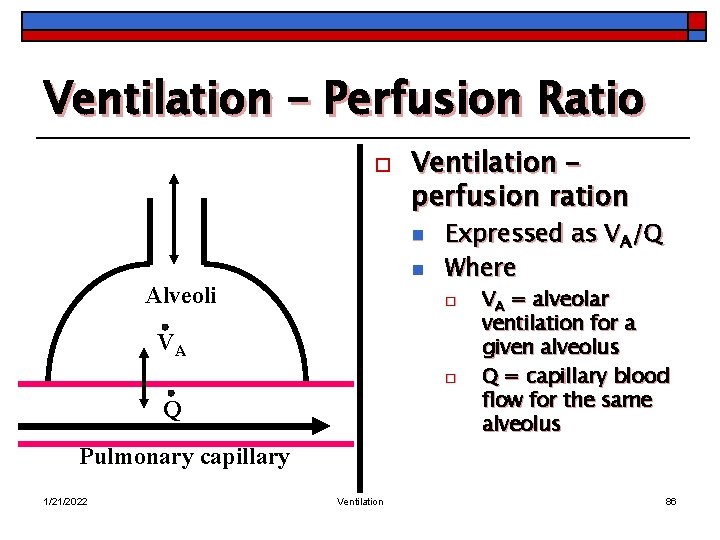
Ventilation – Perfusion Ratio o Ventilation – perfusion ration n n Alveoli Expressed as VA/Q Where o VA o Q VA = alveolar ventilation for a given alveolus Q = capillary blood flow for the same alveolus Pulmonary capillary 1/21/2022 Ventilation 86
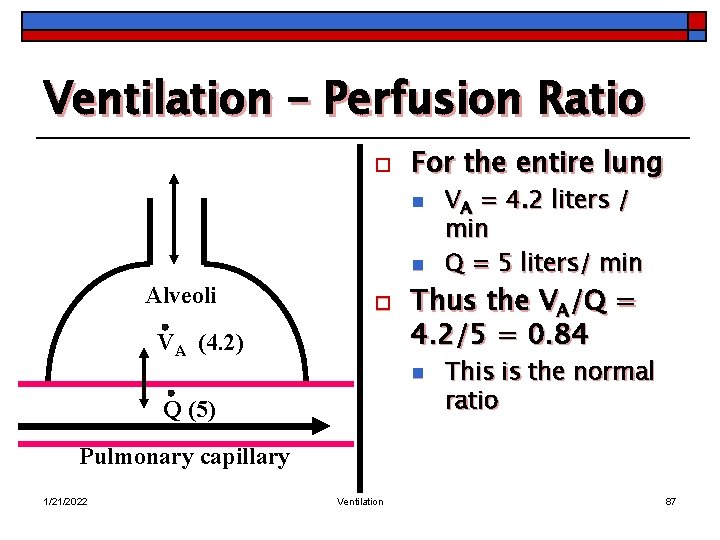
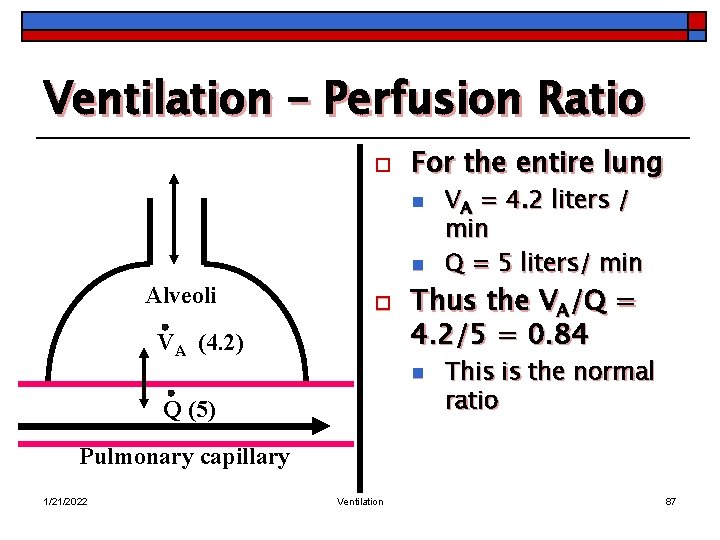
Ventilation – Perfusion Ratio o For the entire lung n n Alveoli o VA (4. 2) Thus the VA/Q = 4. 2/5 = 0. 84 n Q (5) VA = 4. 2 liters / min Q = 5 liters/ min This is the normal ratio Pulmonary capillary 1/21/2022 Ventilation 87
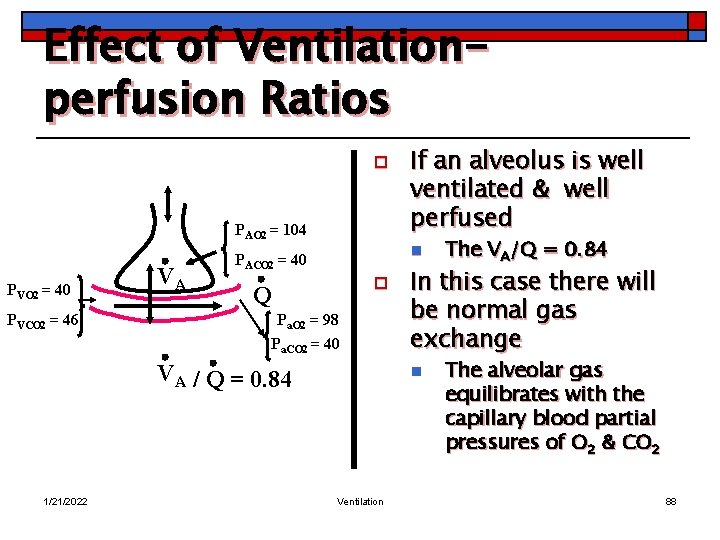
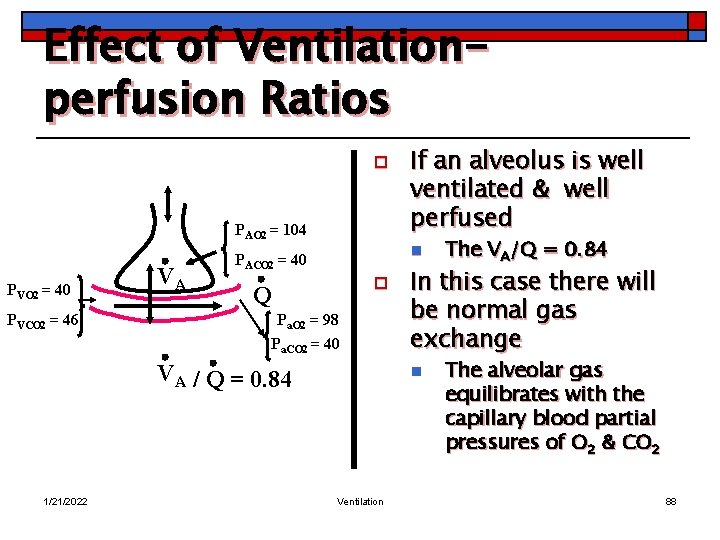
Effect of Ventilationperfusion Ratios o PAO 2 = 104 PVO 2 = 40 PVCO 2 = 46 VA n PACO 2 = 40 o Q Pa. O 2 = 98 Pa. CO 2 = 40 VA / Q = 0. 84 1/21/2022 If an alveolus is well ventilated & well perfused In this case there will be normal gas exchange n Ventilation The VA/Q = 0. 84 The alveolar gas equilibrates with the capillary blood partial pressures of O 2 & CO 2 88
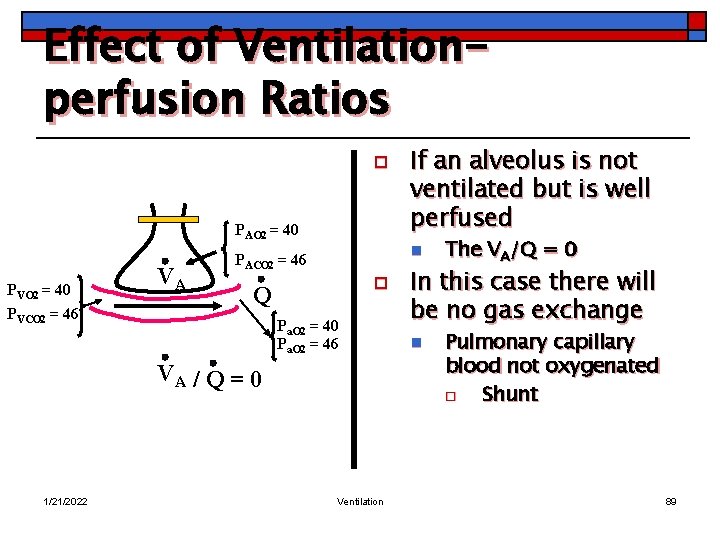
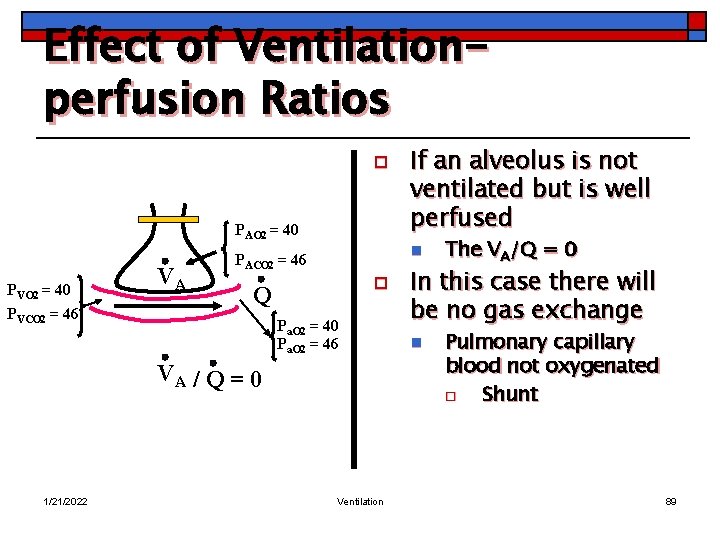
Effect of Ventilationperfusion Ratios o PAO 2 = 40 PVCO 2 = 46 VA n PACO 2 = 46 o Q Pa. O 2 = 40 Pa. O 2 = 46 VA / Q = 0 1/21/2022 If an alveolus is not ventilated but is well perfused Ventilation The VA/Q = 0 In this case there will be no gas exchange n Pulmonary capillary blood not oxygenated o Shunt 89
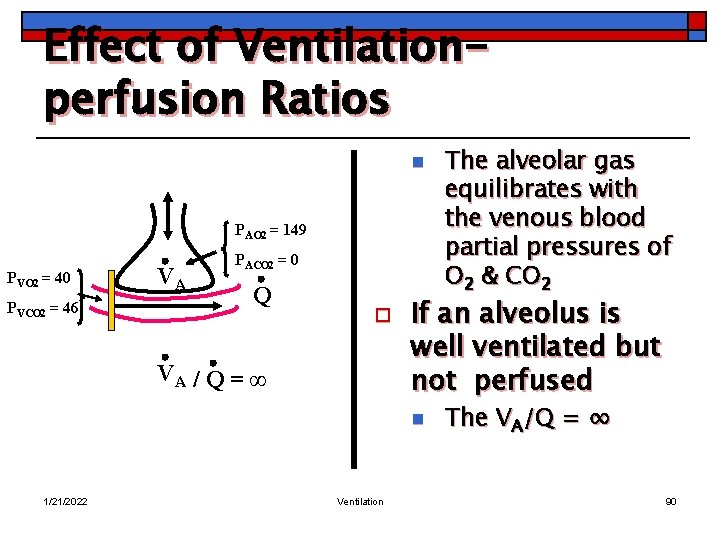
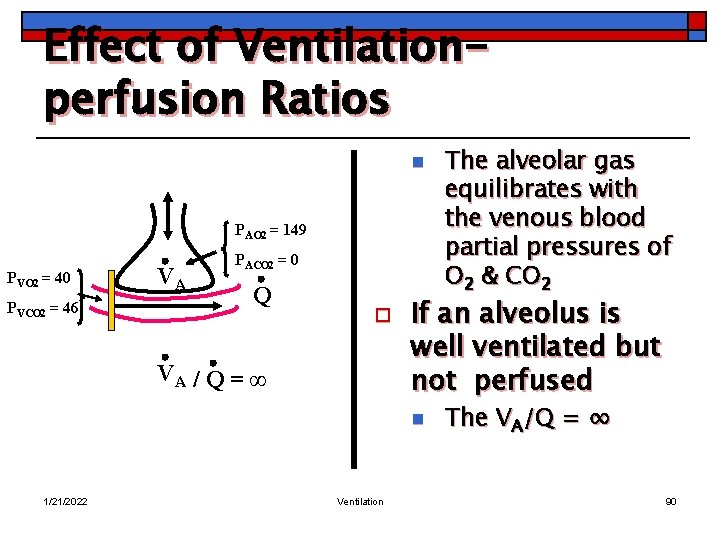
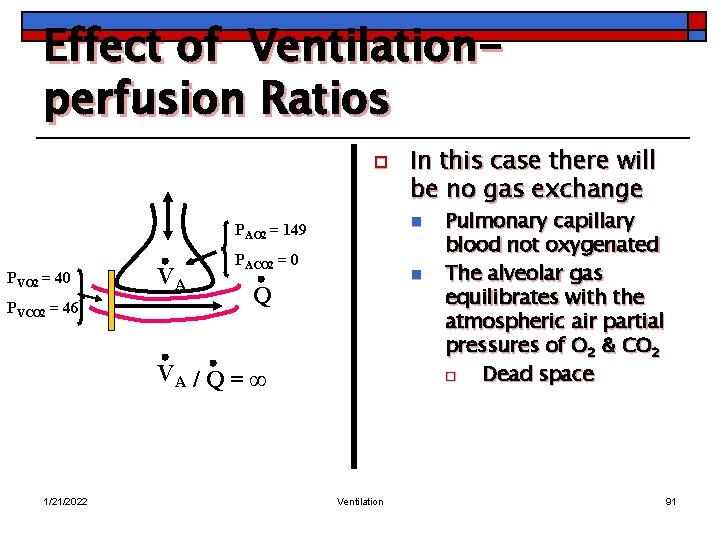
Effect of Ventilationperfusion Ratios n PAO 2 = 149 PVO 2 = 40 PVCO 2 = 46 VA PACO 2 = 0 Q o VA / Q = ∞ If an alveolus is well ventilated but not perfused n 1/21/2022 Ventilation The alveolar gas equilibrates with the venous blood partial pressures of O 2 & CO 2 The VA/Q = ∞ 90
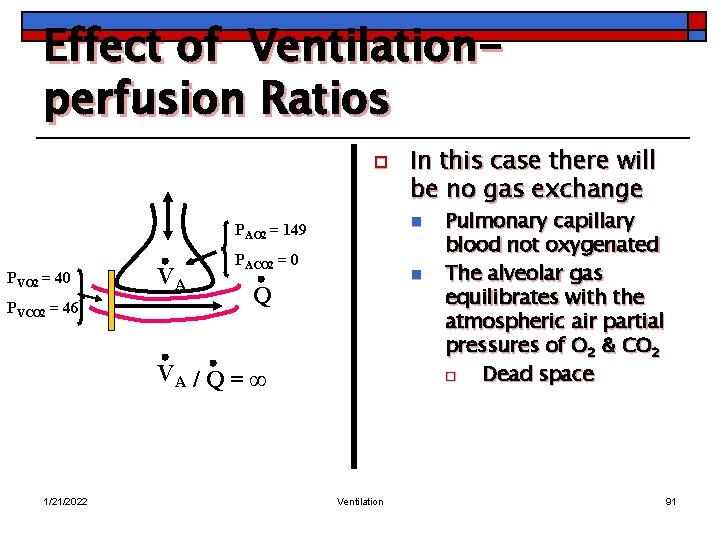
Effect of Ventilationperfusion Ratios o n PAO 2 = 149 PVO 2 = 40 PVCO 2 = 46 VA PACO 2 = 0 n Q VA / Q = ∞ 1/21/2022 In this case there will be no gas exchange Ventilation Pulmonary capillary blood not oxygenated The alveolar gas equilibrates with the atmospheric air partial pressures of O 2 & CO 2 o Dead space 91
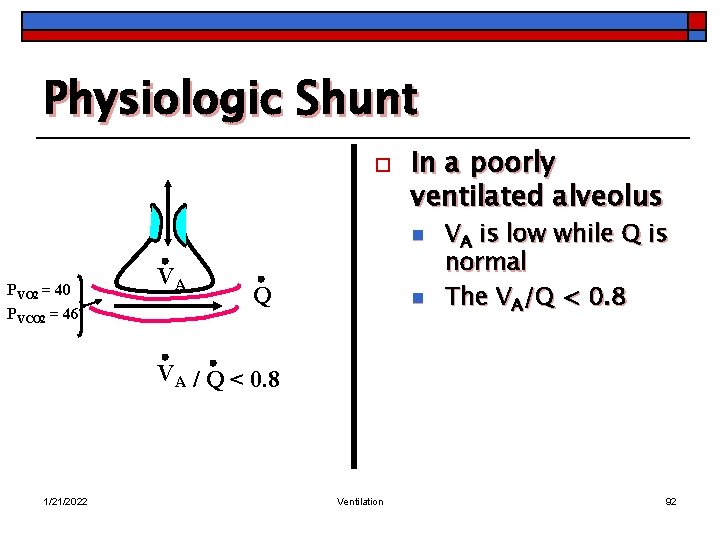
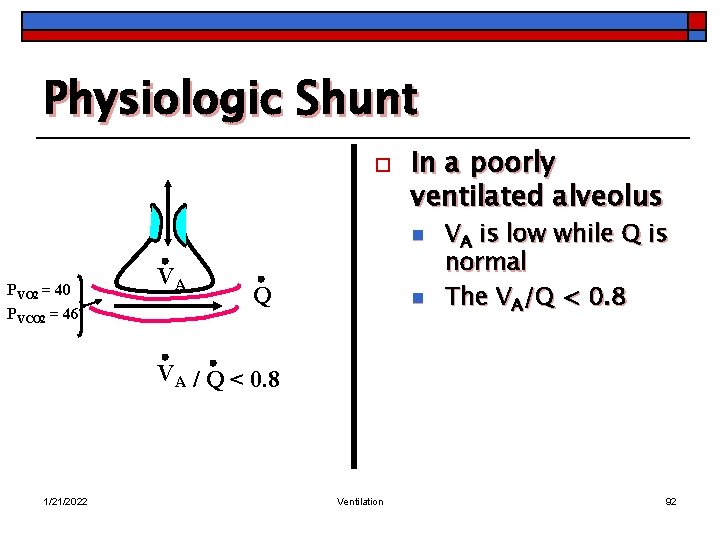
Physiologic Shunt o In a poorly ventilated alveolus n PVO 2 = 40 PVCO 2 = 46 VA Q n VA is low while Q is normal The VA/Q < 0. 8 VA / Q < 0. 8 1/21/2022 Ventilation 92
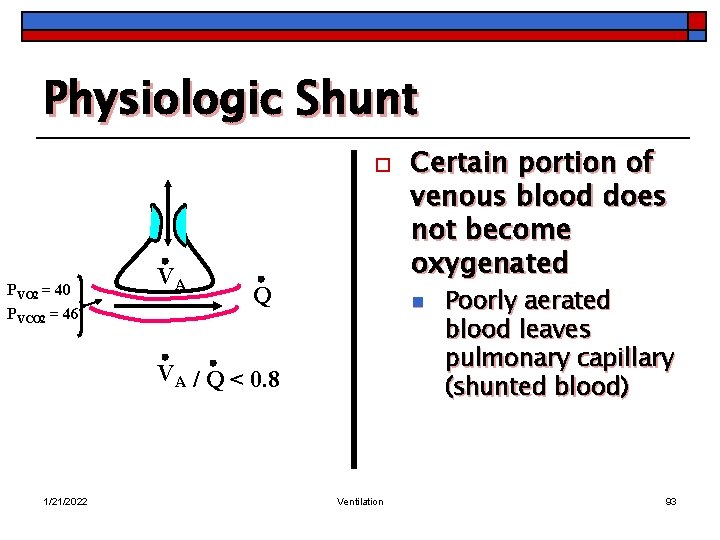
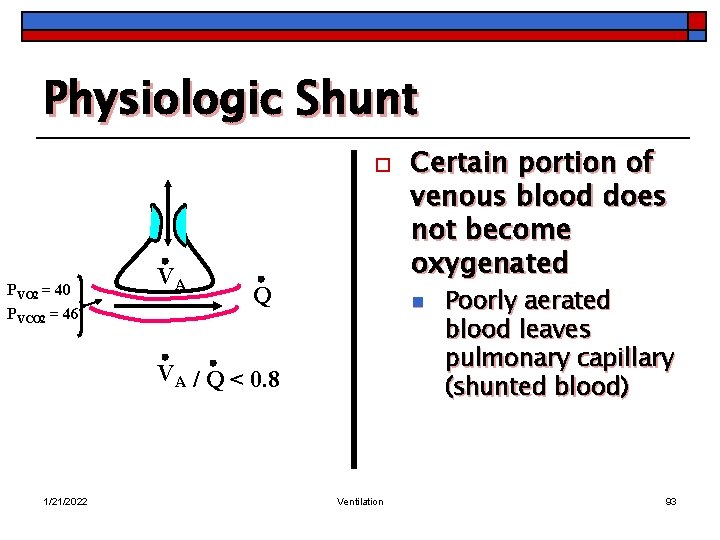
Physiologic Shunt o PVO 2 = 40 PVCO 2 = 46 VA Q n VA / Q < 0. 8 1/21/2022 Certain portion of venous blood does not become oxygenated Ventilation Poorly aerated blood leaves pulmonary capillary (shunted blood) 93
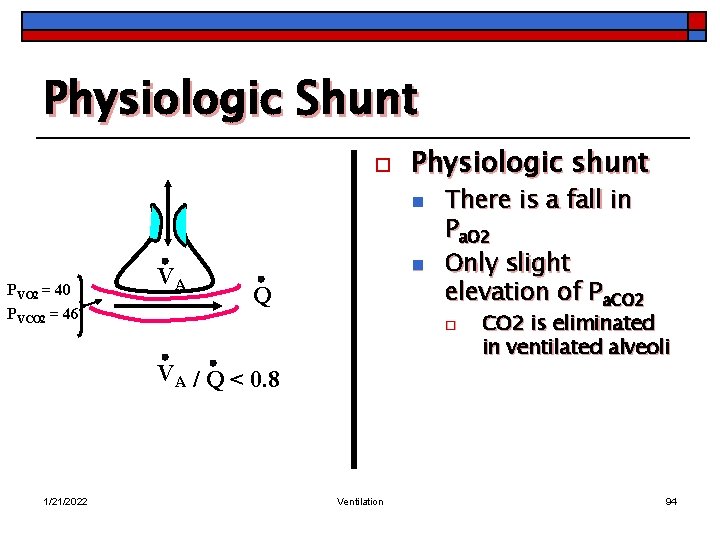
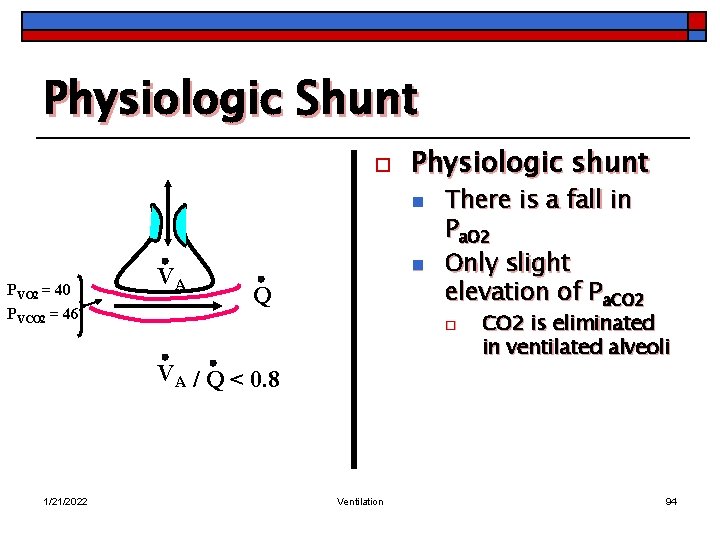
Physiologic Shunt o Physiologic shunt n PVO 2 = 40 PVCO 2 = 46 VA n Q o VA / Q < 0. 8 1/21/2022 There is a fall in Pa. O 2 Only slight elevation of Pa. CO 2 Ventilation CO 2 is eliminated in ventilated alveoli 94
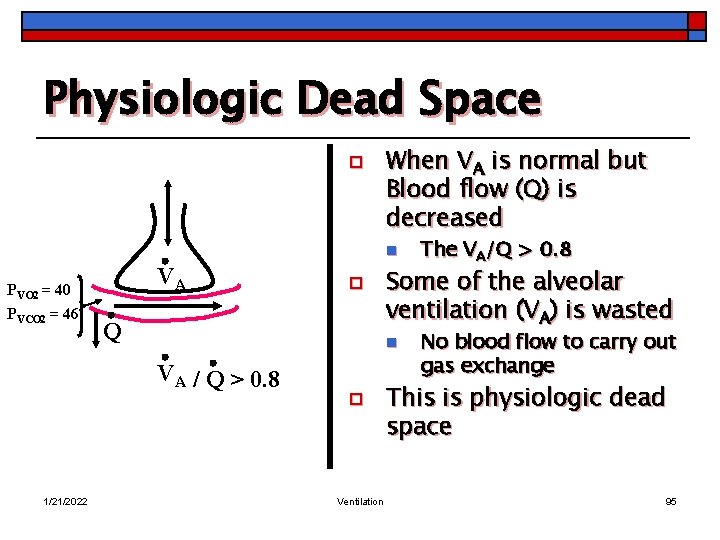
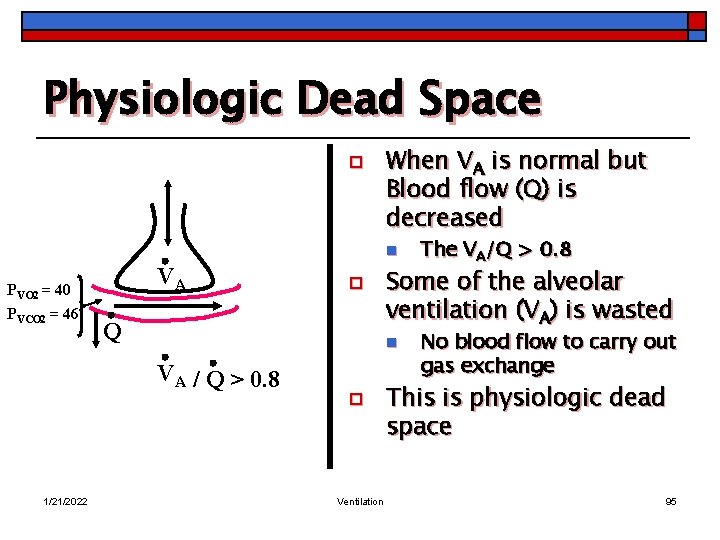
Physiologic Dead Space o When VA is normal but Blood flow (Q) is decreased n PVO 2 = 40 PVCO 2 = 46 VA Q Some of the alveolar ventilation (VA) is wasted n VA / Q > 0. 8 1/21/2022 o o Ventilation The VA/Q > 0. 8 No blood flow to carry out gas exchange This is physiologic dead space 95
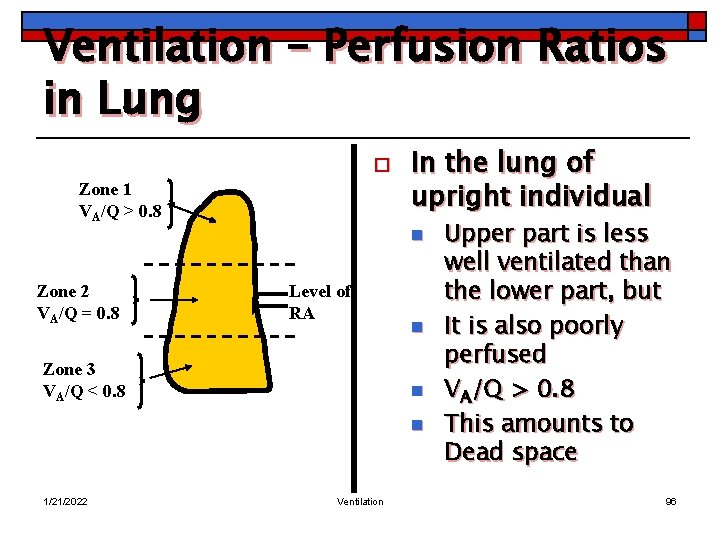
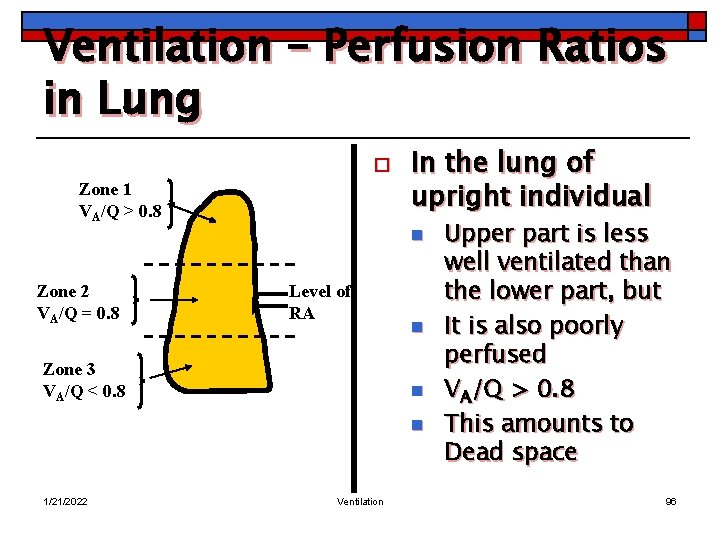
Ventilation – Perfusion Ratios in Lung o Zone 1 VA/Q > 0. 8 In the lung of upright individual n Zone 2 VA/Q = 0. 8 Level of RA Zone 3 VA/Q < 0. 8 n n n 1/21/2022 Ventilation Upper part is less well ventilated than the lower part, but It is also poorly perfused VA/Q > 0. 8 This amounts to Dead space 96
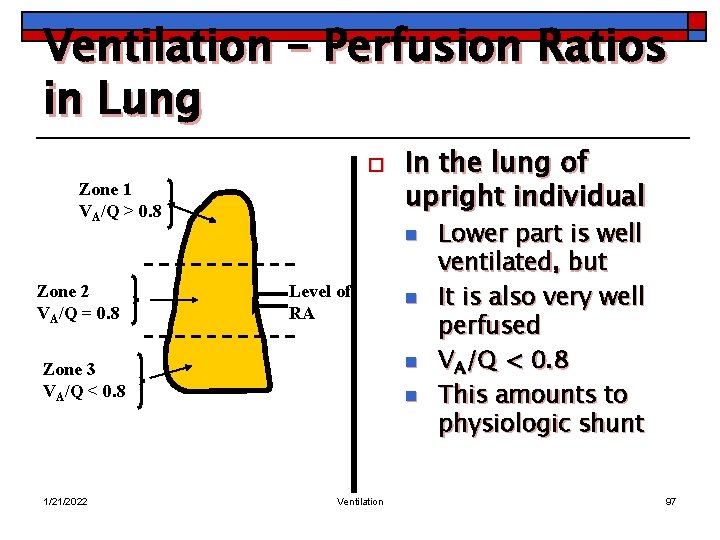
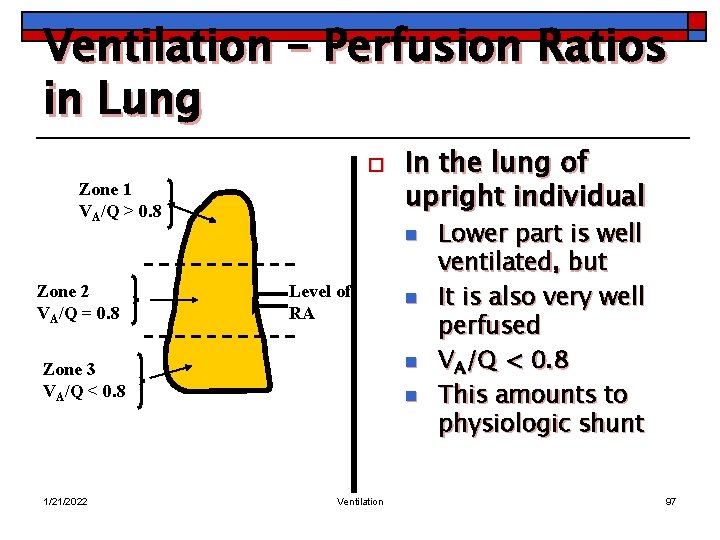
Ventilation – Perfusion Ratios in Lung o Zone 1 VA/Q > 0. 8 In the lung of upright individual n Zone 2 VA/Q = 0. 8 Level of RA n Zone 3 VA/Q < 0. 8 1/21/2022 n n Ventilation Lower part is well ventilated, but It is also very well perfused VA/Q < 0. 8 This amounts to physiologic shunt 97
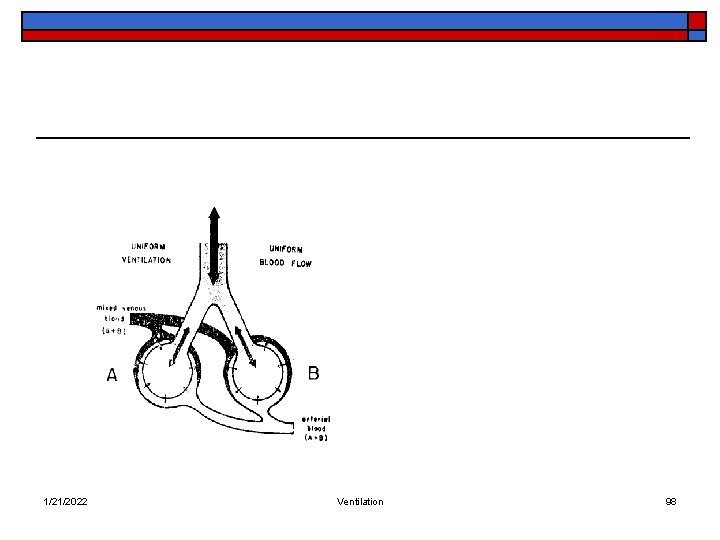
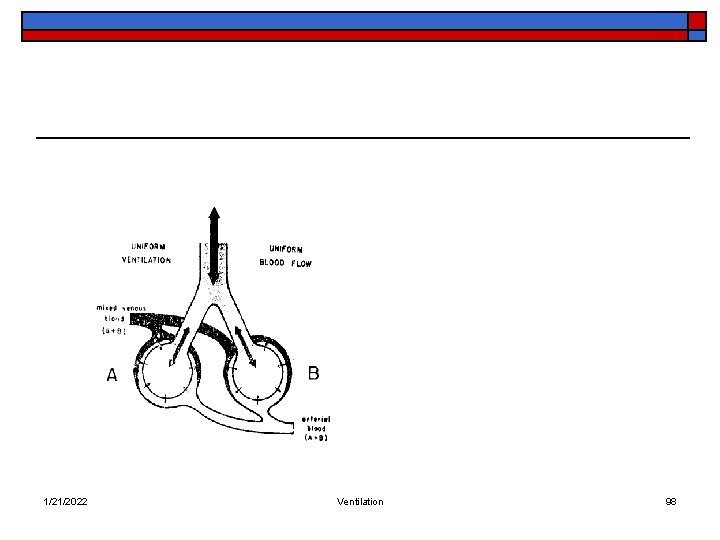
1/21/2022 Ventilation 98