MECHANICAL VENTILATION INDICATIONS FOR MECHANICAL VENTILATION RULE 1





- Slides: 74

MECHANICAL VENTILATION
INDICATIONS FOR MECHANICAL VENTILATION RULE 1. The indication for intubation and mechanical ventilation is thinking of it. RULE 2. Intubation is not an act of personal weakness. RULE 3. Initiating mechanical ventilation is not the "kiss of death
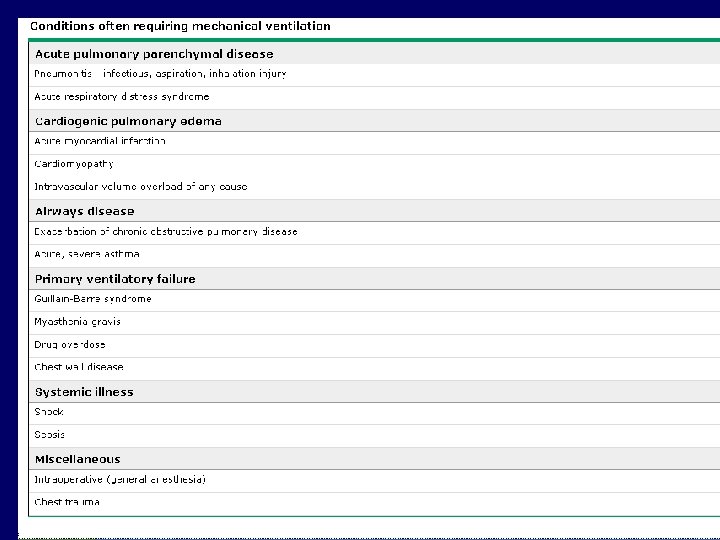
Indications Relieve respiratory distress Rest respiratory muscles Decrease work of breathing Improve oxygenation Prevent or reverse atelectasis Improve ventilation Decrease O 2 consumption Permit sedation Stabilize chest wall Prevent complications
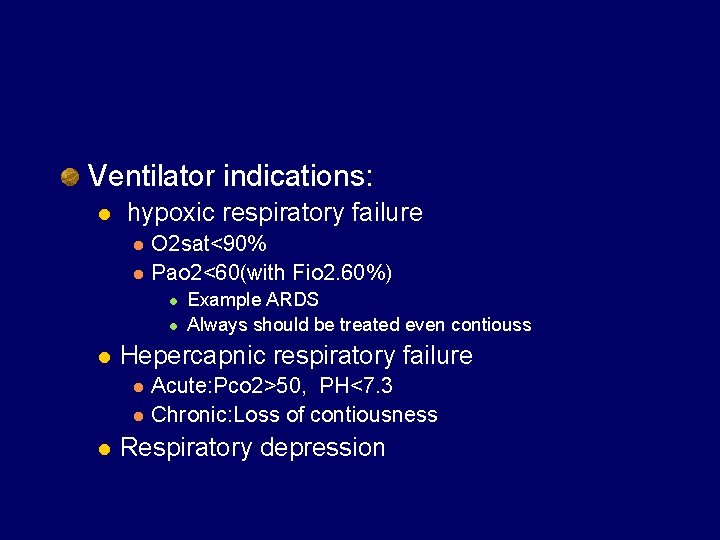
Ventilator indications: l hypoxic respiratory failure l l O 2 sat<90% Pao 2<60(with Fio 2. 60%) l l l Hepercapnic respiratory failure l l l Example ARDS Always should be treated even contiouss Acute: Pco 2>50, PH<7. 3 Chronic: Loss of contiousness Respiratory depression
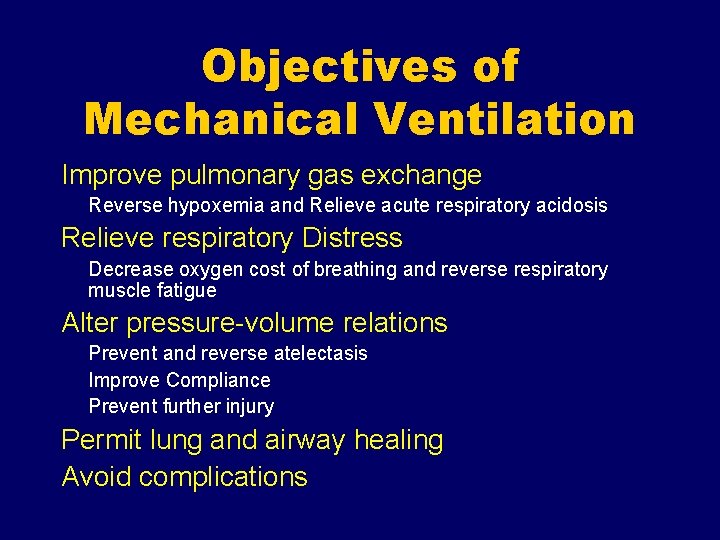
Objectives of Mechanical Ventilation Improve pulmonary gas exchange Reverse hypoxemia and Relieve acute respiratory acidosis Relieve respiratory Distress Decrease oxygen cost of breathing and reverse respiratory muscle fatigue Alter pressure-volume relations Prevent and reverse atelectasis Improve Compliance Prevent further injury Permit lung and airway healing Avoid complications
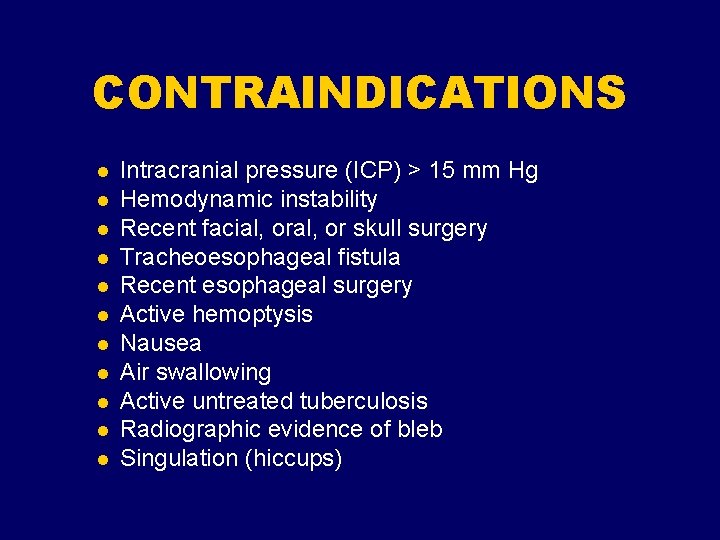
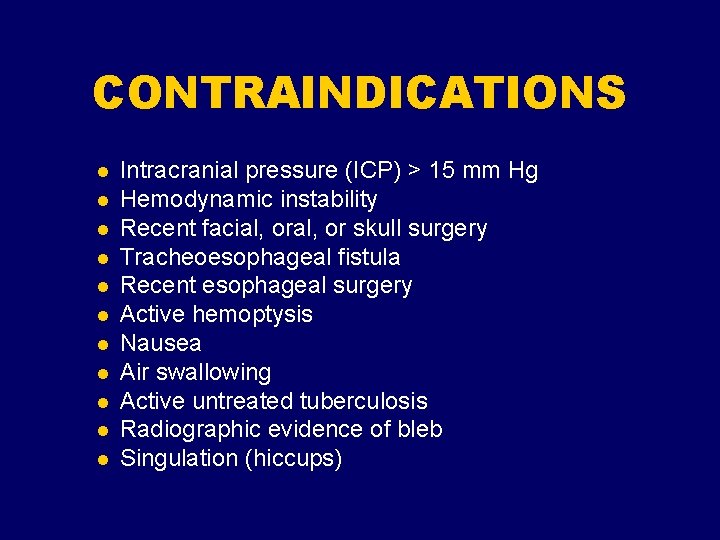
CONTRAINDICATIONS l l l Intracranial pressure (ICP) > 15 mm Hg Hemodynamic instability Recent facial, or skull surgery Tracheoesophageal fistula Recent esophageal surgery Active hemoptysis Nausea Air swallowing Active untreated tuberculosis Radiographic evidence of bleb Singulation (hiccups)
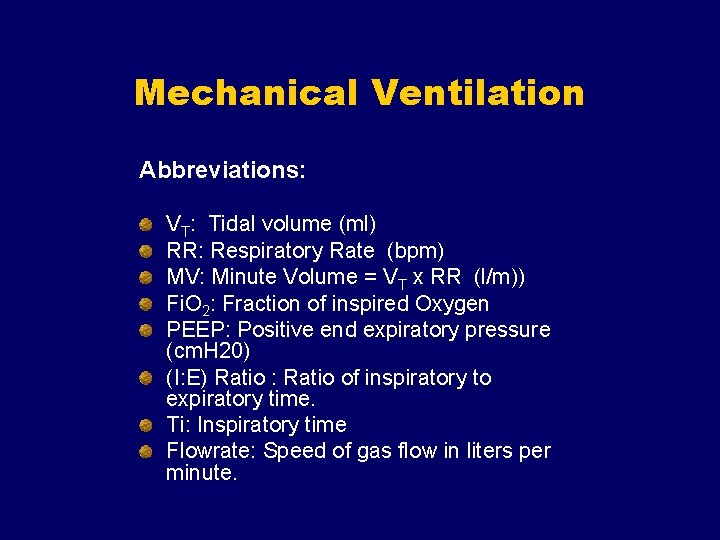
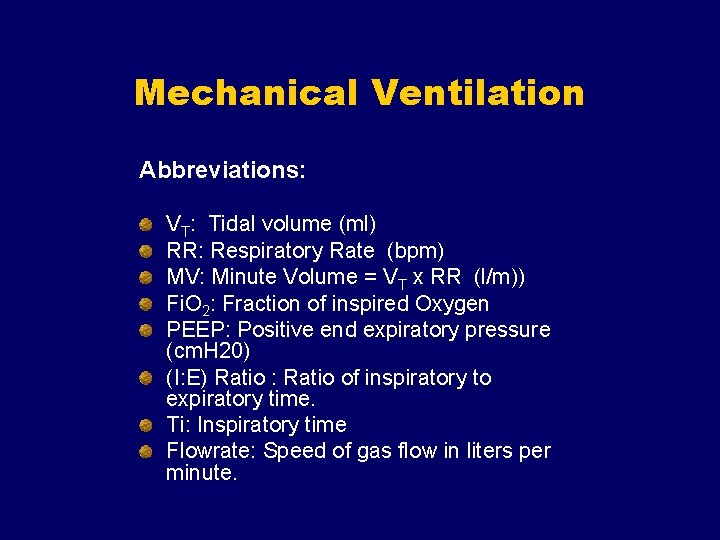
Mechanical Ventilation Abbreviations: VT: Tidal volume (ml) RR: Respiratory Rate (bpm) MV: Minute Volume = VT x RR (l/m)) Fi. O 2: Fraction of inspired Oxygen PEEP: Positive end expiratory pressure (cm. H 20) (I: E) Ratio : Ratio of inspiratory to expiratory time. Ti: Inspiratory time Flowrate: Speed of gas flow in liters per minute.
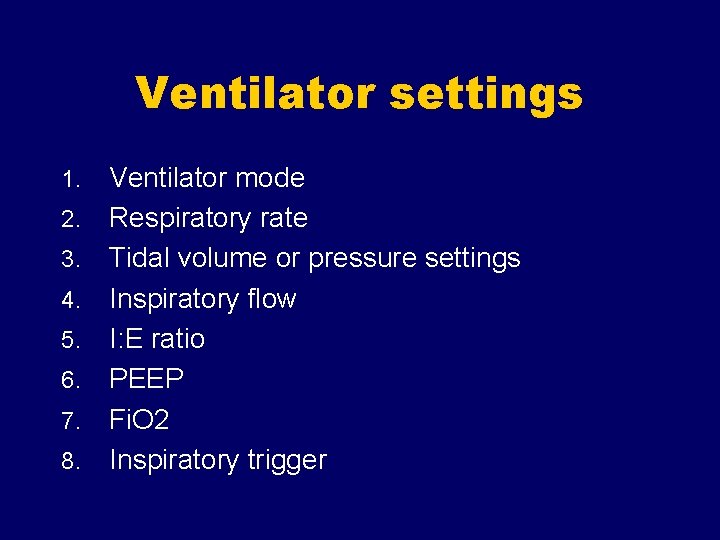
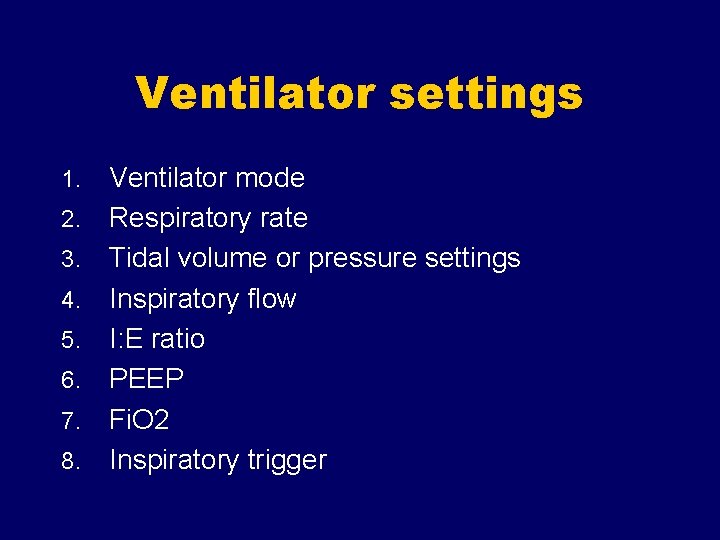
Ventilator settings 1. 2. 3. 4. 5. 6. 7. 8. Ventilator mode Respiratory rate Tidal volume or pressure settings Inspiratory flow I: E ratio PEEP Fi. O 2 Inspiratory trigger
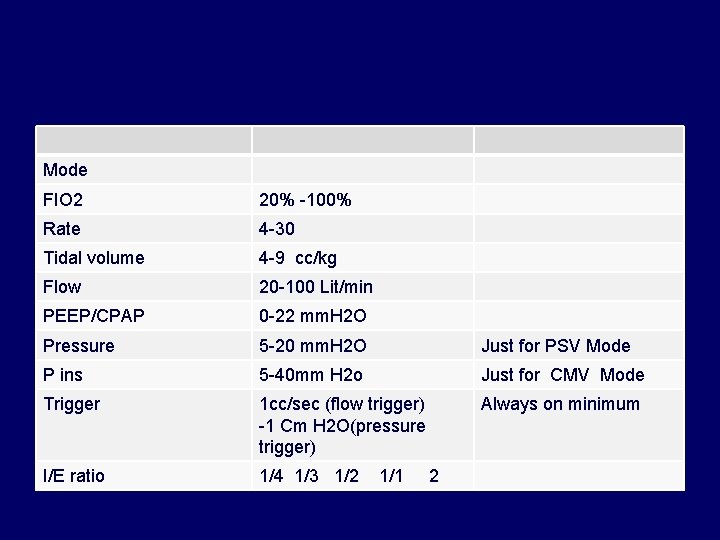
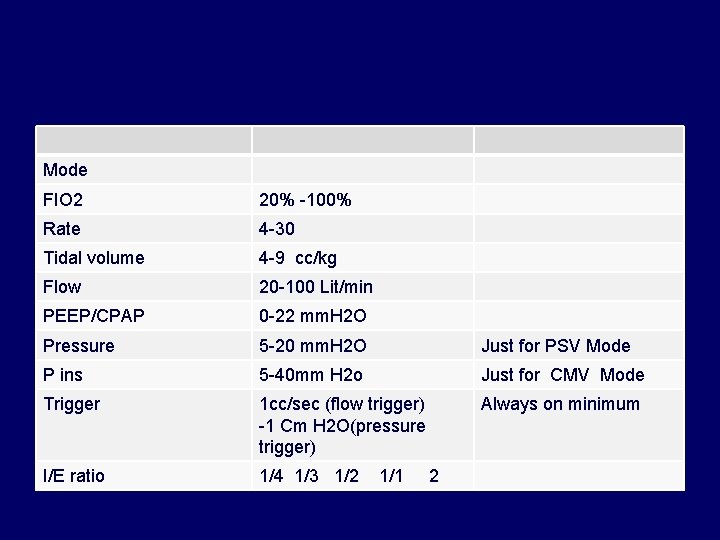
Mode FIO 2 20% -100% Rate 4 -30 Tidal volume 4 -9 cc/kg Flow 20 -100 Lit/min PEEP/CPAP 0 -22 mm. H 2 O Pressure 5 -20 mm. H 2 O Just for PSV Mode P ins 5 -40 mm H 2 o Just for CMV Mode Trigger 1 cc/sec (flow trigger) -1 Cm H 2 O(pressure trigger) Always on minimum I/E ratio 1/4 1/3 1/2 1/1 2
Respiratory Rate
Tidal Volume or Pressure setting Maximum volume/pressure to achieve good ventilation and oxygenation without producing alveolar overdistention Max cc/kg = 10 cc/kg Some clinical exceptions
Tidal Volume Vt > TLC can result in over-distended lung and lung injury TLC reduced in lung disease TLC plateau pressure = 30 – 35 cm. H 2 O
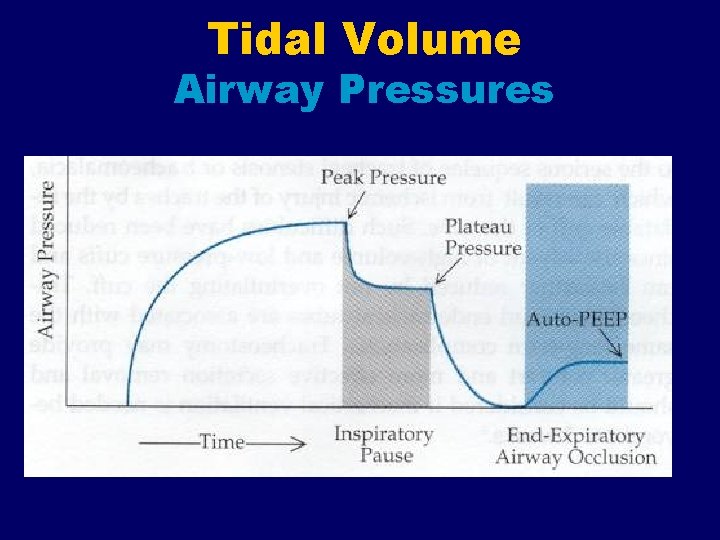
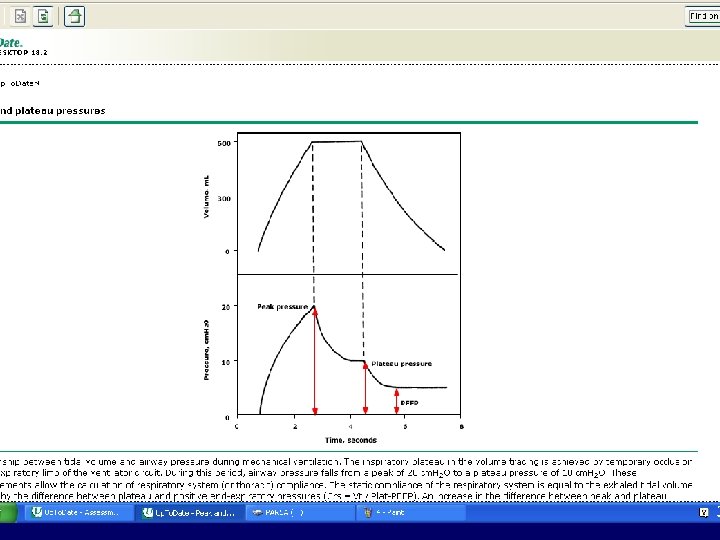
Tidal Volume Airway Pressures
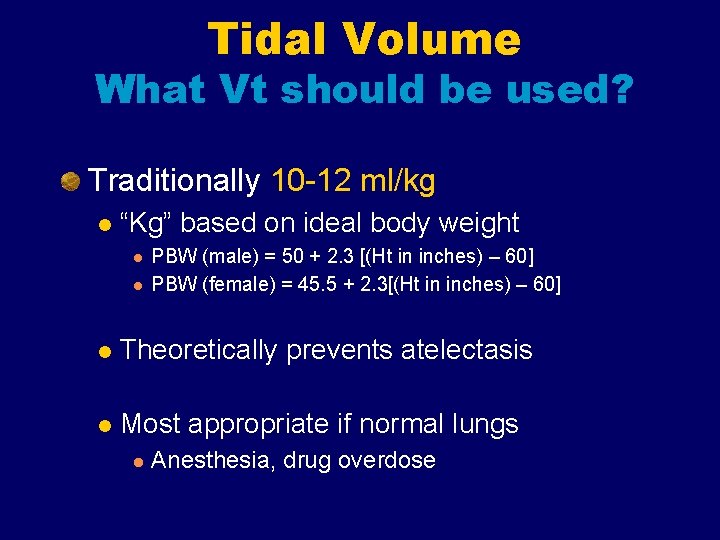
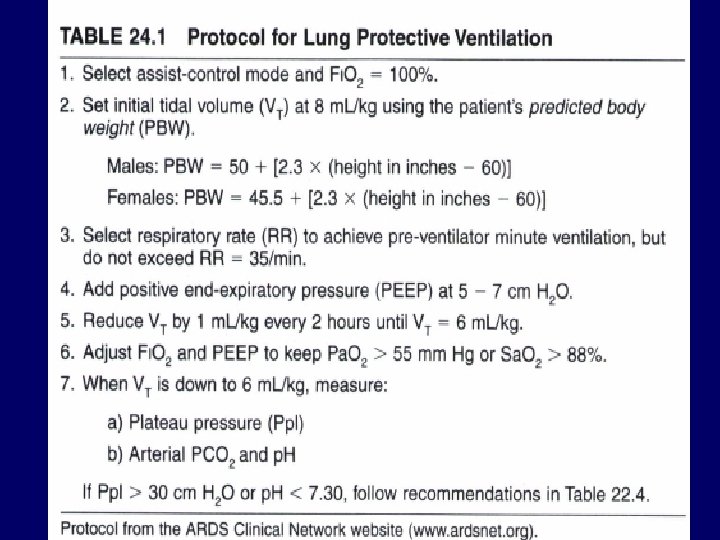
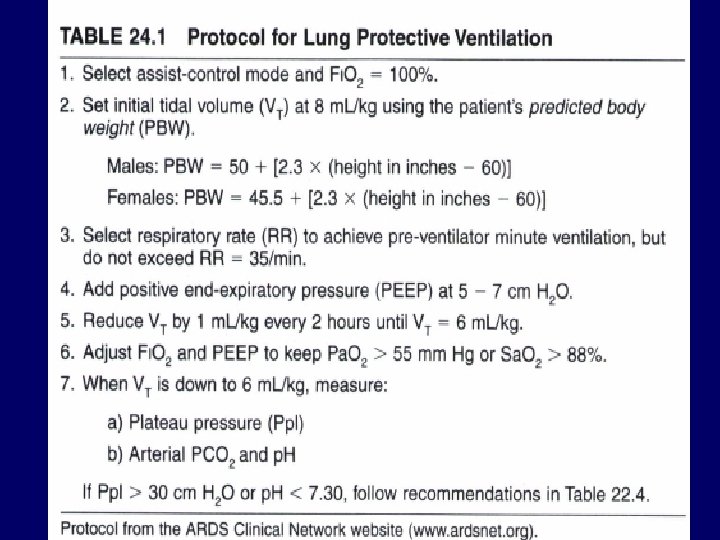
Tidal Volume What Vt should be used? Traditionally 10 -12 ml/kg l “Kg” based on ideal body weight l l PBW (male) = 50 + 2. 3 [(Ht in inches) – 60] PBW (female) = 45. 5 + 2. 3[(Ht in inches) – 60] l Theoretically prevents atelectasis l Most appropriate if normal lungs l Anesthesia, drug overdose
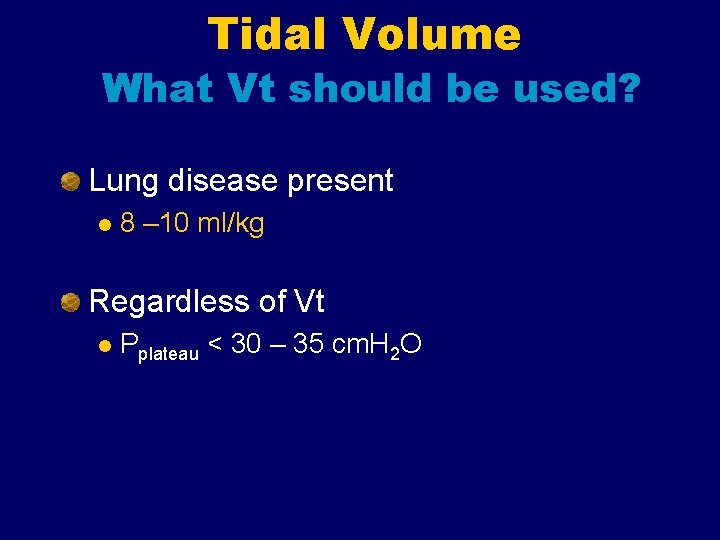
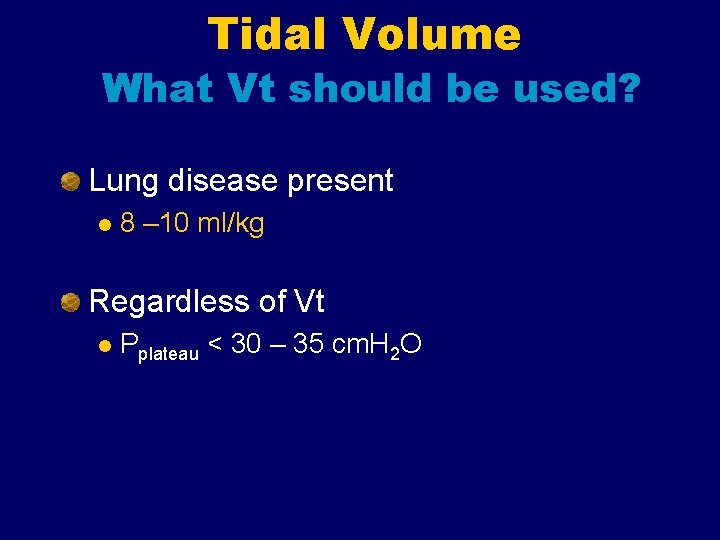
Tidal Volume What Vt should be used? Lung disease present l 8 – 10 ml/kg Regardless of Vt l Pplateau < 30 – 35 cm. H 2 O
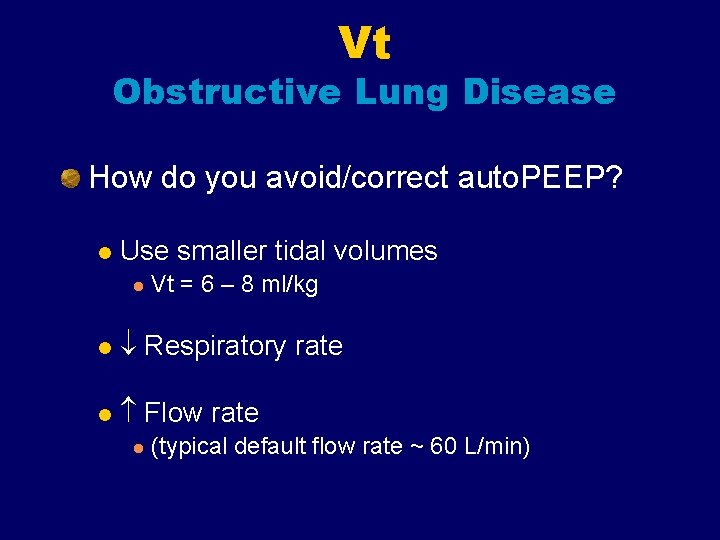
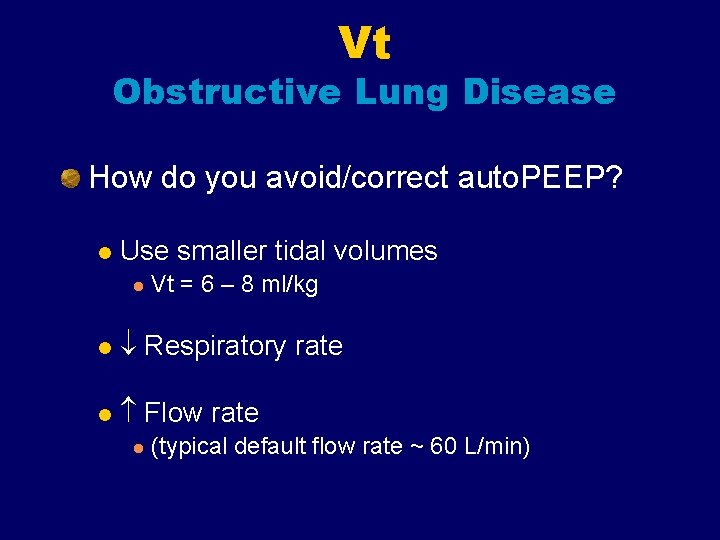
Vt Obstructive Lung Disease How do you avoid/correct auto. PEEP? l Use smaller tidal volumes l Vt = 6 – 8 ml/kg l Respiratory rate l Flow rate l (typical default flow rate ~ 60 L/min)
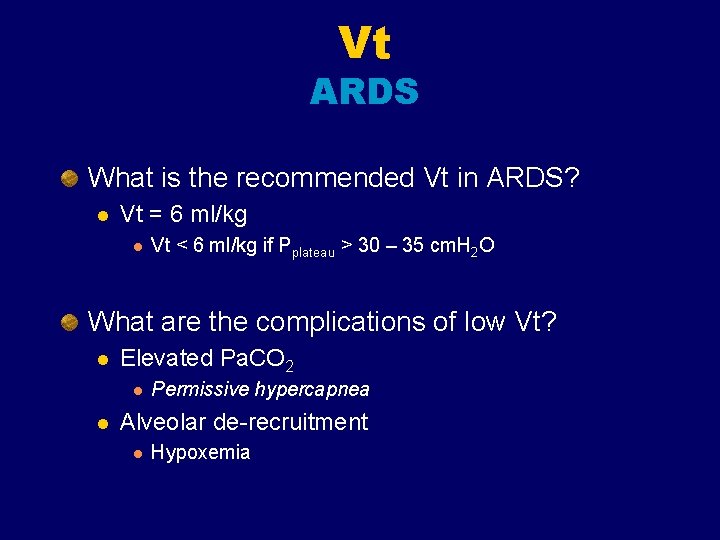
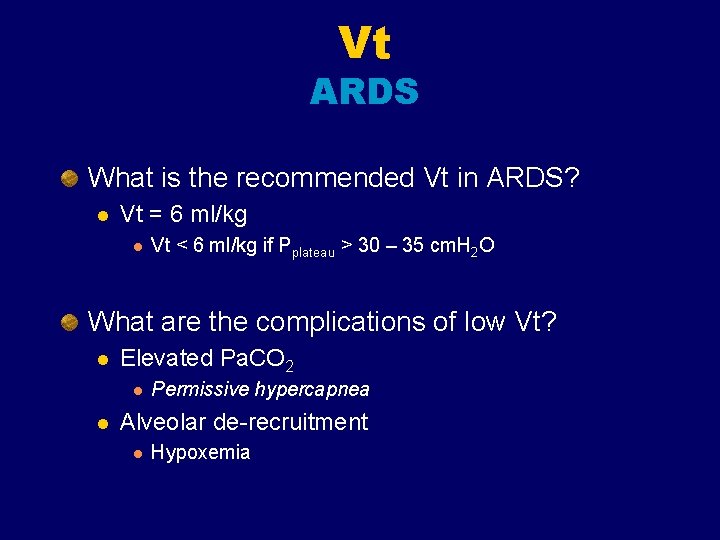
Vt ARDS What is the recommended Vt in ARDS? l Vt = 6 ml/kg l Vt < 6 ml/kg if Pplateau > 30 – 35 cm. H 2 O What are the complications of low Vt? l Elevated Pa. CO 2 l l Permissive hypercapnea Alveolar de-recruitment l Hypoxemia
Double-checking the selected tidal volume Once a tidal volume is selected, the peak airway pressure necessary to deliver a single breath should be recorded. As tidal volume increases, the pressure required to force that volume into the lung also increases. During mechanical ventilation, a persistent breath-tobreath peak pressure higher than 45 cm water is a risk factor for barotrauma.
Sighs Because a spontaneously breathing individual typically sighs 6 -8 times per hour to avoid microatelectasis, giving periodic machine breaths of 1. 5 -2 times the preset tidal volume 6 -8 times per hour was once recommended. Often, the peak pressure needed to deliver such a volume would predispose the patient to barotrauma. Today, sighs are usually not used if the patient is receiving tidal volumes of 10 -12 m. L/kg or requires the use of positive end-expiratory pressure (PEEP).
I: E Ratio 1: 2 Prolonged at 1: 3, 1: 4, … Inverse ratio
FIO 2 The usual goal is to use the minimum Fio 2 required to have a Pa. O 2 > 60 mmhg or a sat >90% Start at 100% Oxygen toxicity normally with Fio 2 >60%
Inspiratory flow Varies with the Vt, I: E and RR Normally about 40 -60 l/min Can be majored to 100 - 120 l/min
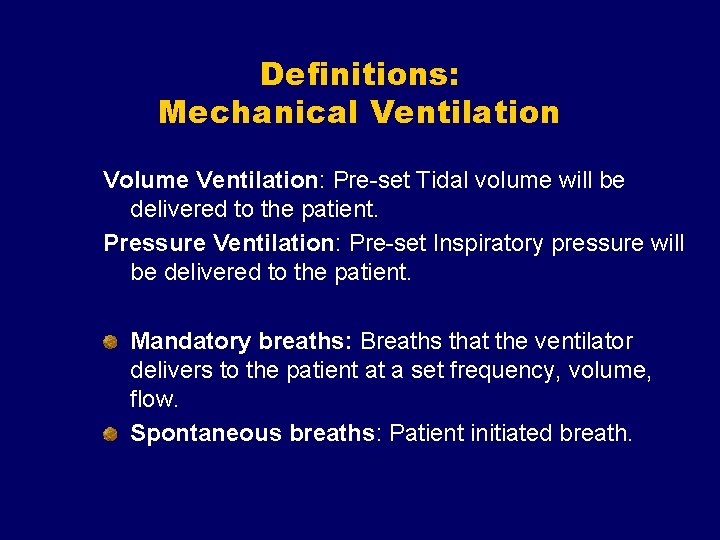
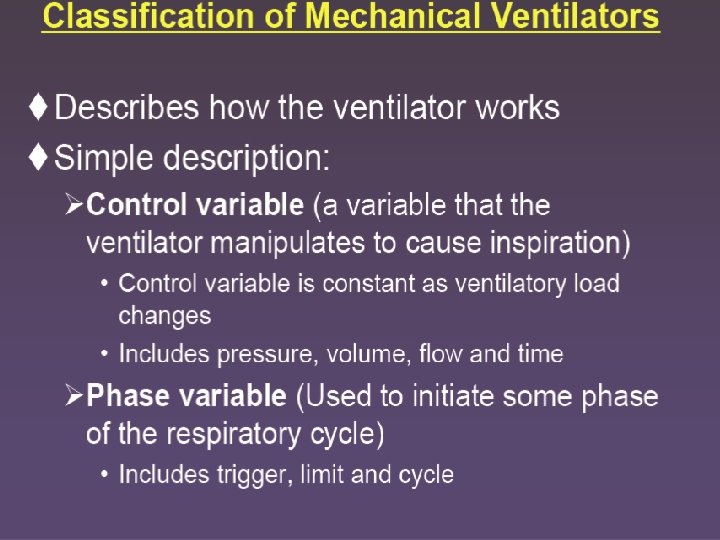
Definitions: Mechanical Ventilation Volume Ventilation: Pre-set Tidal volume will be delivered to the patient. Pressure Ventilation: Pre-set Inspiratory pressure will be delivered to the patient. Mandatory breaths: Breaths that the ventilator delivers to the patient at a set frequency, volume, flow. Spontaneous breaths: Patient initiated breath.
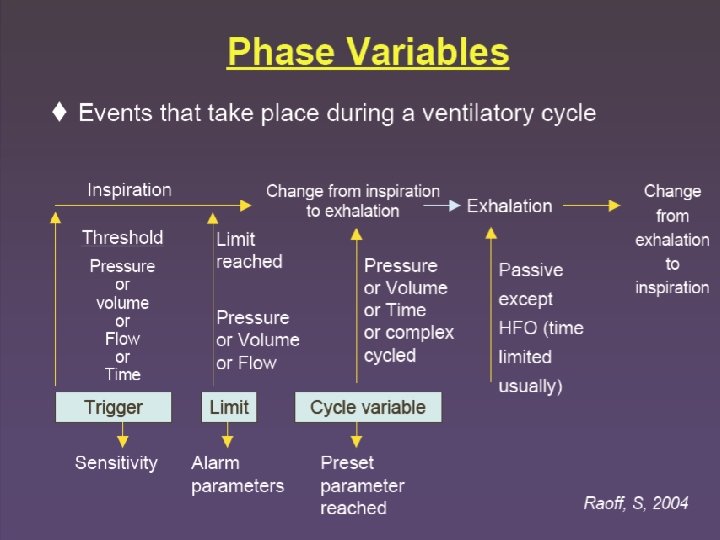
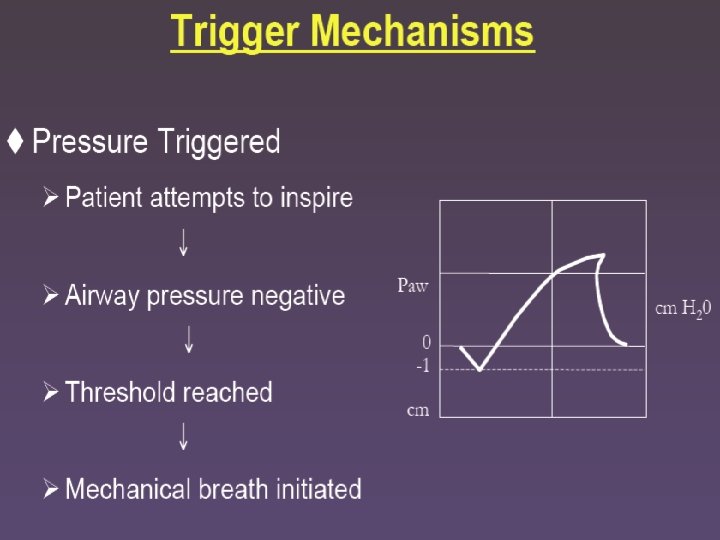
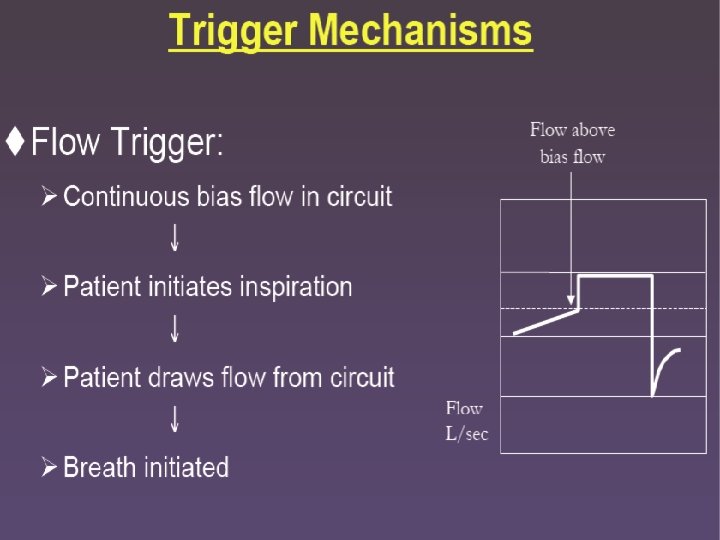
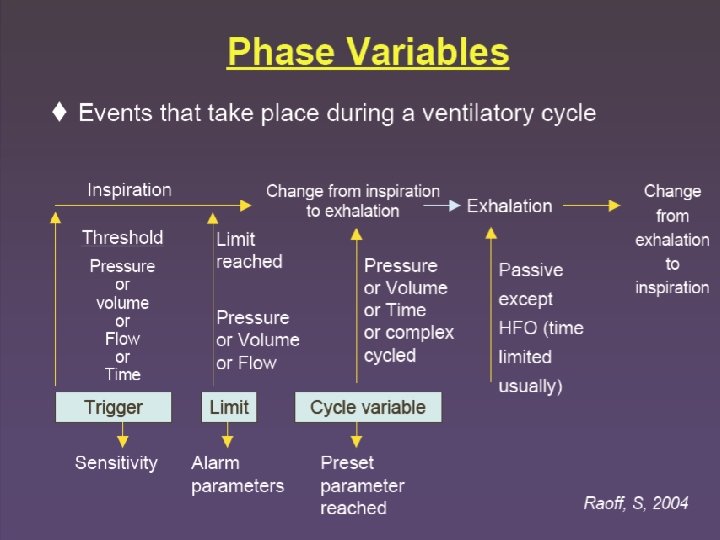
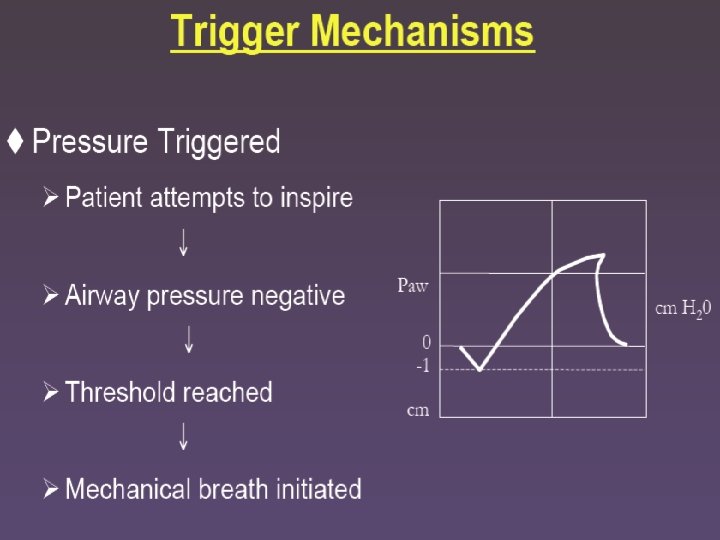
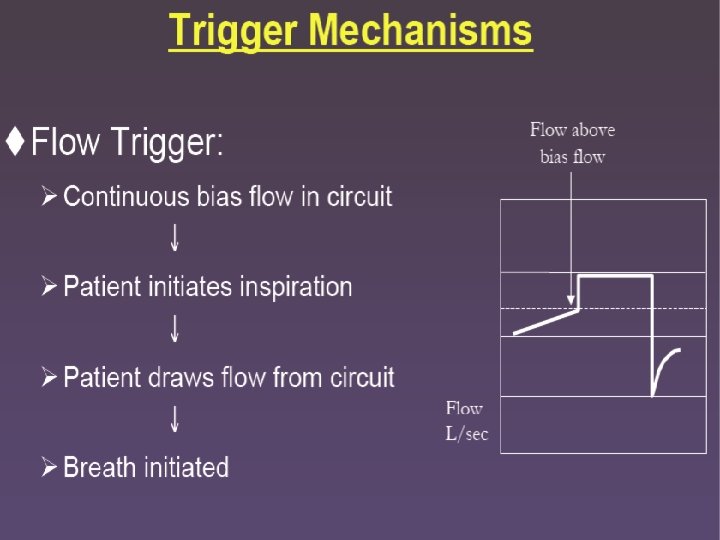
Definitions: (Cont’d) Triggering: The sensitivity of the ventilator to the patient’s respiratory effort. Either flow or pressure setting that allows the ventilator to detect the patient’s inspiratory effort. Allows the ventilator to be in synchronization with the patient’s spontaneous respiratory efforts improving patient comfort during mechanical ventilation.
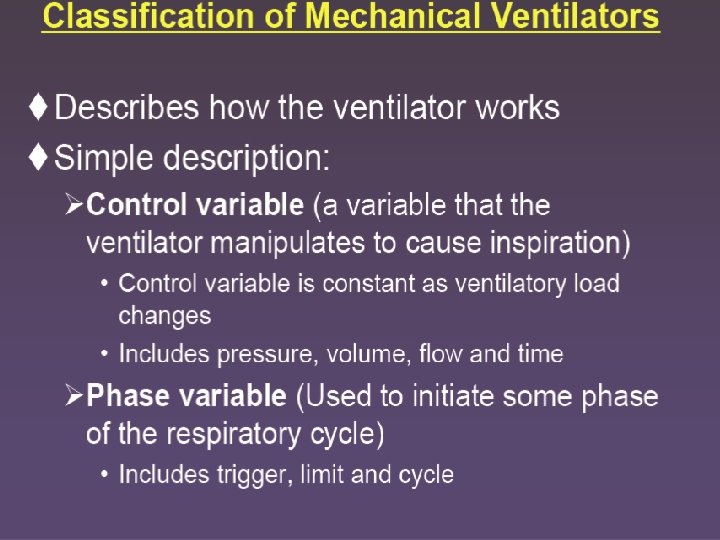
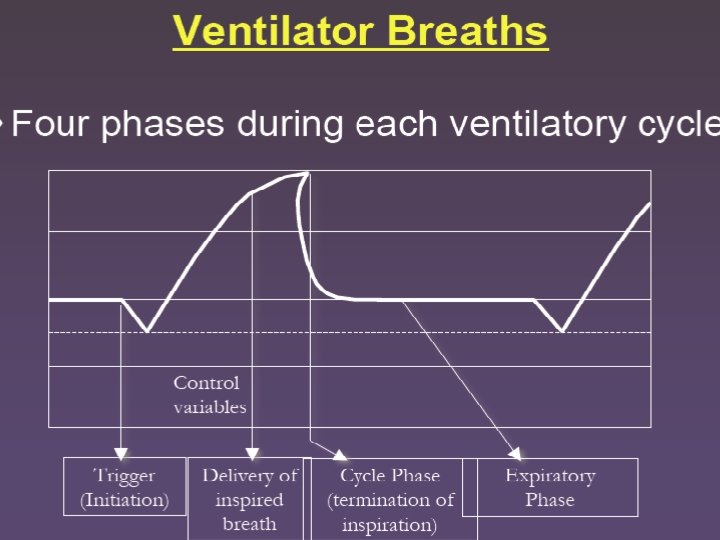
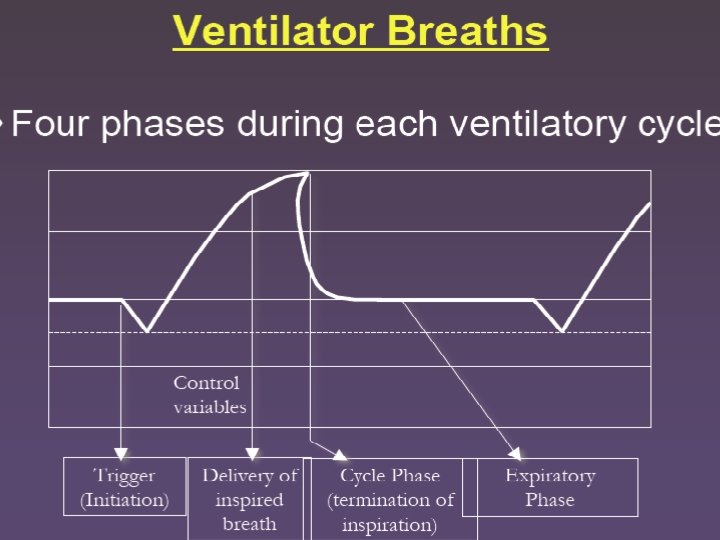
Ventilators are programmed with a trigger, which opens the inspiratory valve and initiates gas flow a limit, the factor that regulates the rate/amount of gas flow cycling, the parameter that ends gas flow and opens the expiratory valve.
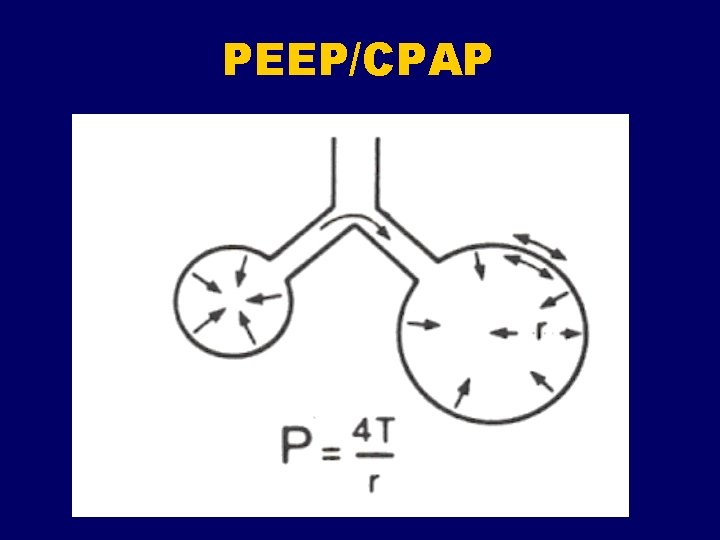
Positive end-expiratory pressure PEEP is a mode of therapy used in conjunction with mechanical ventilation. At the end of exhalation (either mechanical or spontaneous), patient airway pressure is maintained above atmospheric pressure by exerting a pressure that opposes complete passive emptying of the lung. This pressure is typically achieved by maintaining a positive pressure flow at the end of exhalation.
Positive end-expiratory pressure PEEP therapy can be effective when used in patients with a diffuse lung disease that results in an acute decrease in functional residual capacity (FRC). In many pulmonary diseases, FRC is reduced because of the collapse of the unstable alveoli. This reduction in lung volume decreases the surface area available for gas exchange and results in intrapulmonary shunting. If the FRC is not restored, a high concentration of inspired oxygen may be required to maintain the arterial oxygen content of the blood at an acceptable range.
Positive end-expiratory pressure Applying continuous positive pressure at the end of exhalation (eg, PEEP, continuous positive airway pressure [CPAP]) causes an increase in alveolar pressure and an increase in alveolar volume. This increase in lung volume increases the surface area by reopening or stabilizing collapsed or unstable alveoli. This “splinting” or “propping open” of the alveoli with positive pressure may provide a better matching of ventilation to perfusion, thereby reducing the shunt effect.
Positive end-expiratory pressure Once a true shunt is changed to a ventilation/perfusion mismatch, lower concentrations of oxygen can be used to maintain an adequate Pa. O 2. PEEP therapy has also been effective for improving lung compliance. When the FRC and lung compliance are decreased, more energy and volume are needed to inflate the lung. By applying PEEP, the lung volume at the end of exhalation is increased, which decreases the work of breathing because the lung is already partially inflated; therefore, less volume and energy are needed to inflate the lung.
Positive end-expiratory pressure In summary, when used to treat patients with a diffuse lung disease, PEEP should improve compliance, decrease dead space, and decrease the intrapulmonary shunt effect. The most significant benefit of PEEP is that the patient can maintain an adequate Pa. O 2 at a lower and safer concentration of oxygen (<60%), thereby reducing the risk of oxygen toxicity.
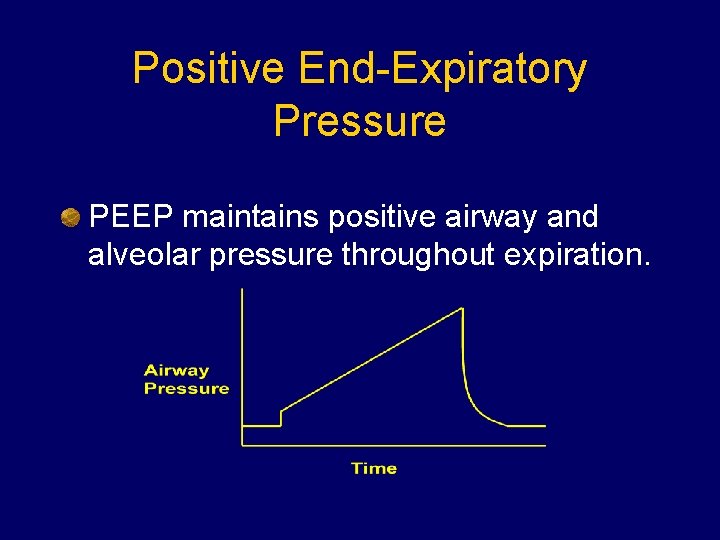
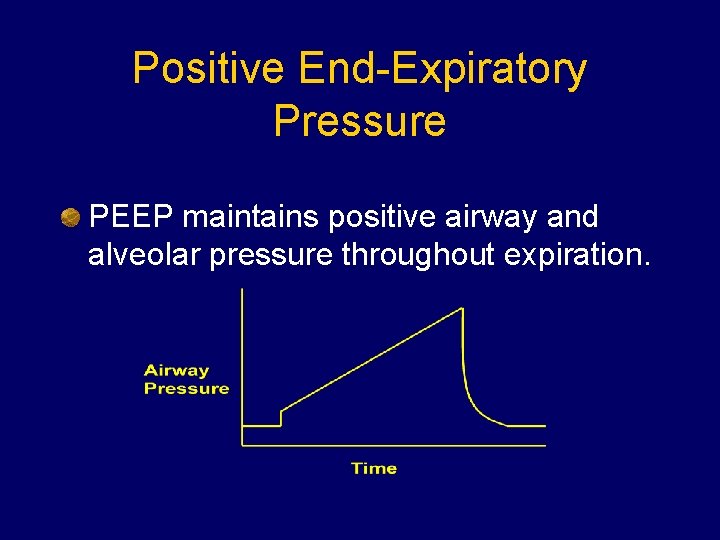
Positive End-Expiratory Pressure PEEP maintains positive airway and alveolar pressure throughout expiration.

PEEP/CPAP Indications Refractory hypoxemia Pa. O 2/FIO 2 < 150 l Prototypic disease = ARDS l COPD with air-trapping “Physiologic” PEEP
PEEP/CPAP Where do you start? l PEEP = 5 – 7 cm. H 2 O l Increase in increments of 2 -3 cm. H 2 O Where do you stop? l Goals: Adequate oxygenation l FIO 2 reduced to acceptable level l l No upper limit exists
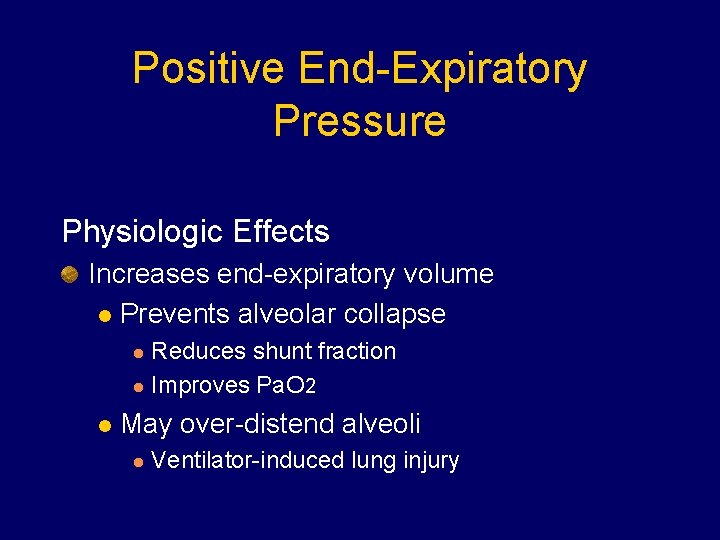
Positive End-Expiratory Pressure Physiologic Effects Increases end-expiratory volume l Prevents alveolar collapse Reduces shunt fraction l Improves Pa. O 2 l l May over-distend alveoli l Ventilator-induced lung injury

Positive End-Expiratory Pressure Physiologic Effects Increases pleural (intra-thoracic) pressure l Reduces venous return l Reduces cardiac output and DO 2
PEEP What are the secondary effects of PEEP? Barotrauma l Diminish cardiac output l Regional hypoperfusion l Na. Cl retention l Augmentation of ICP? l Paradoxal hypoxemia l
PEEP Relative Contraindications: Barotrauma l Airway trauma l Unilateral lung disease l Hemodynamic instability l Hypovolemia l ICP? l Bronchopleural fistula l
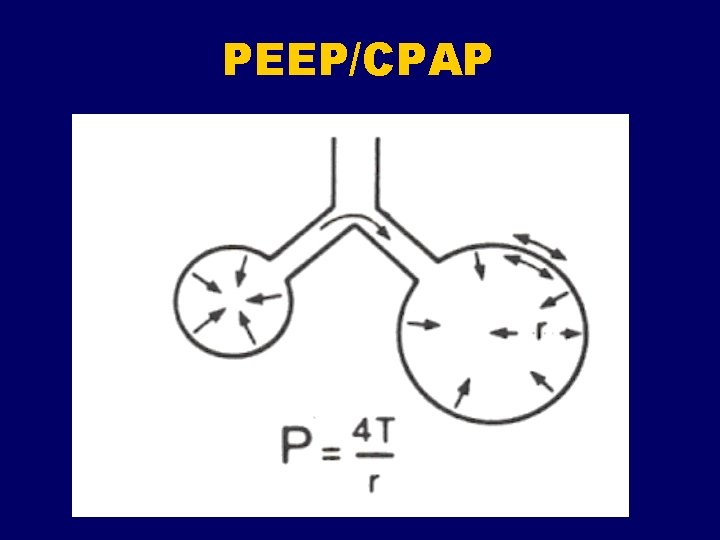
PEEP/CPAP Why might PEEP worsen hypoxemia in unilateral lung disease? l Effects of PEEP go to normal alveoli and not diseased alveoli
PEEP/CPAP
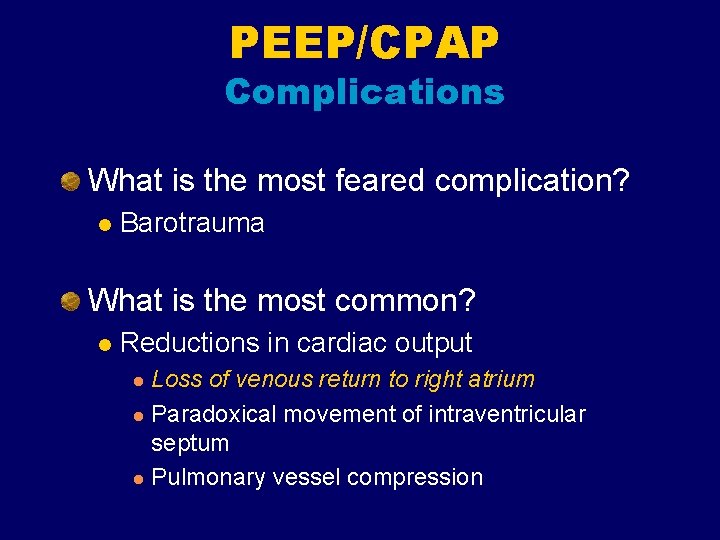
PEEP/CPAP Complications What is the most feared complication? l Barotrauma What is the most common? l Reductions in cardiac output Loss of venous return to right atrium l Paradoxical movement of intraventricular septum l Pulmonary vessel compression l
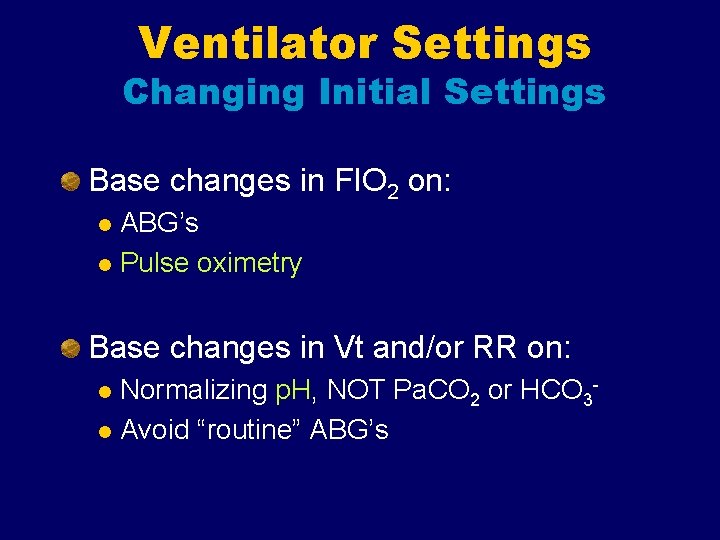
Ventilator Settings Changing Initial Settings Base changes in FIO 2 on: ABG’s l Pulse oximetry l Base changes in Vt and/or RR on: Normalizing p. H, NOT Pa. CO 2 or HCO 3 l Avoid “routine” ABG’s l
Oxygenation decisions With the target Pa. O 2 identified, the FIO 2 can be adjusted using the following formula: New FIO 2 = (old FIO 2 X desired Pa. O 2)/measured Pa. O 2
Ventilation Decisions New rate = (old rate X measured PCO 2)/desired PCO 2

Assist-control, volume Ingento EP & Drazen J: Mechanical Ventilators, in Hall JB, Scmidt GA, & Wood LDH(eds. ): Principles of Critical Care
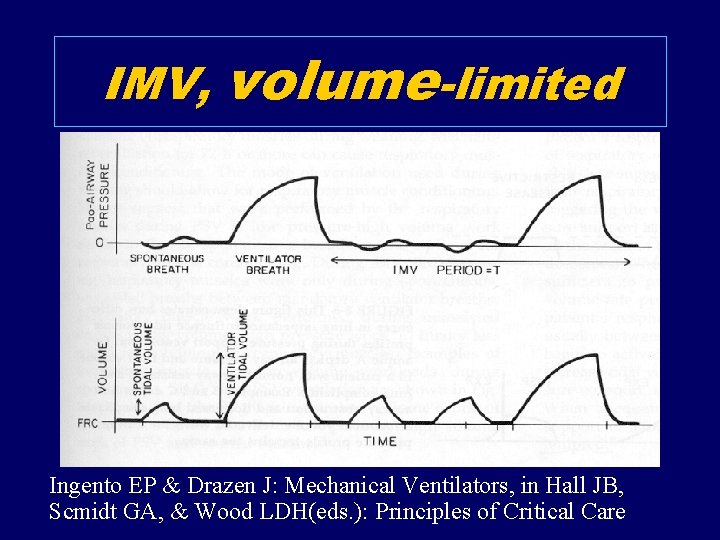
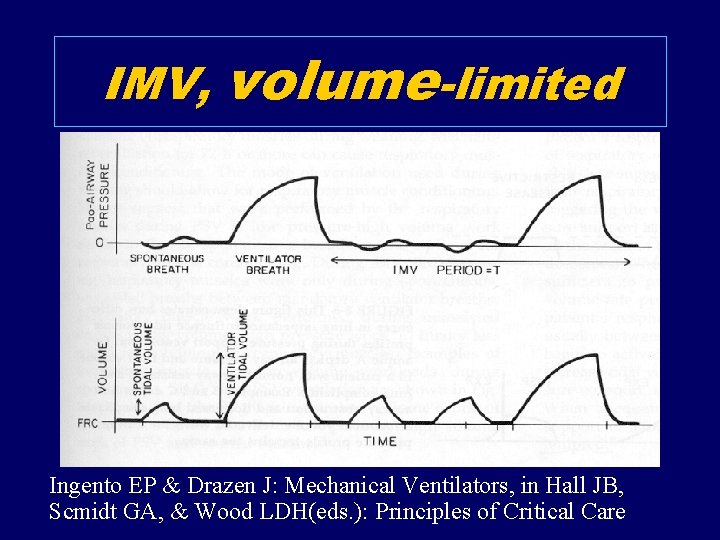
IMV, volume-limited Ingento EP & Drazen J: Mechanical Ventilators, in Hall JB, Scmidt GA, & Wood LDH(eds. ): Principles of Critical Care
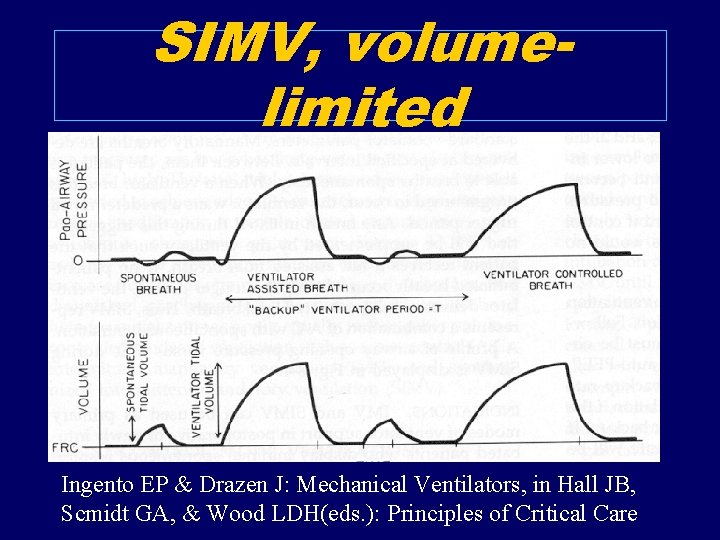
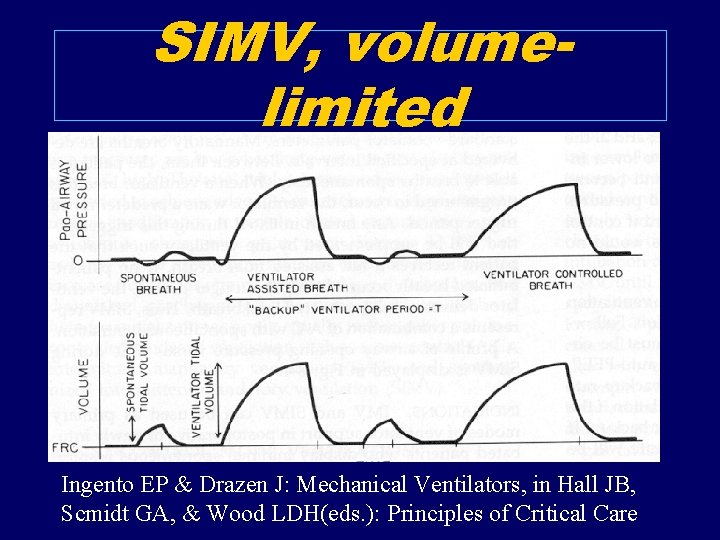
SIMV, volumelimited Ingento EP & Drazen J: Mechanical Ventilators, in Hall JB, Scmidt GA, & Wood LDH(eds. ): Principles of Critical Care
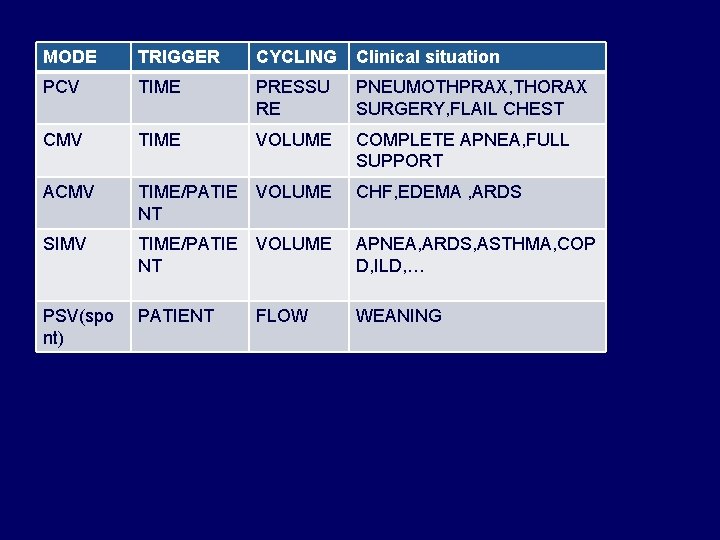
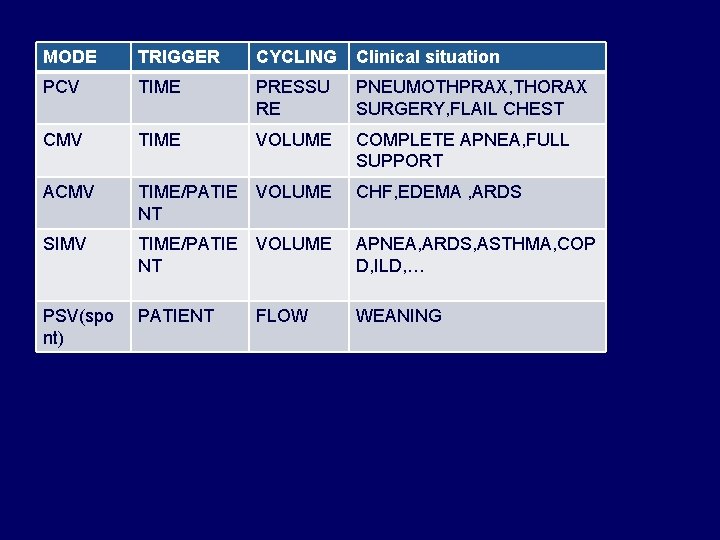
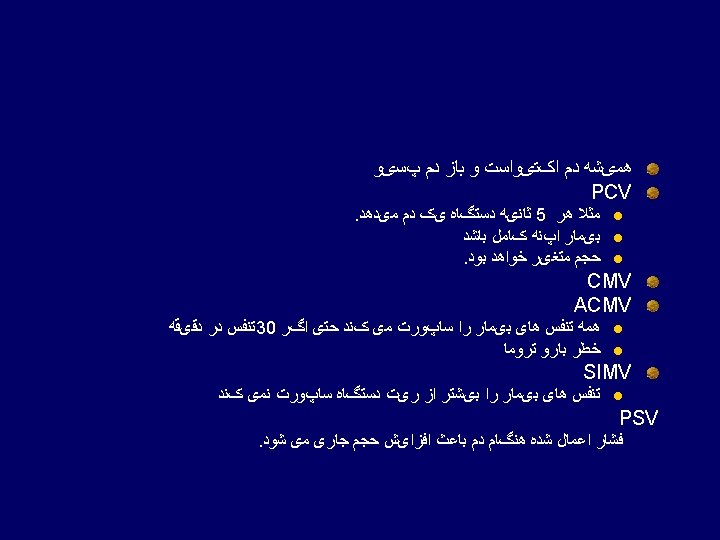
MODE TRIGGER CYCLING Clinical situation PCV TIME PRESSU RE PNEUMOTHPRAX, THORAX SURGERY, FLAIL CHEST CMV TIME VOLUME COMPLETE APNEA, FULL SUPPORT ACMV TIME/PATIE NT VOLUME CHF, EDEMA , ARDS SIMV TIME/PATIE NT VOLUME APNEA, ARDS, ASTHMA, COP D, ILD, … PSV(spo nt) PATIENT FLOW WEANING
PCV: pressure controled Ventilation CMV: controled mode ventilation ACMV: Assist controled mode ventilation SIMV: spontanous intermittent mandatory ventilation PSV: pressure support ventilation ASV: asssist spontanous ventilation
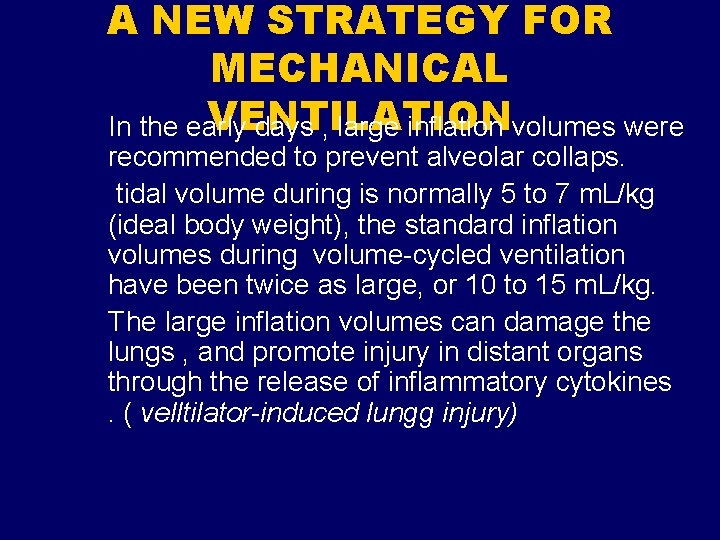
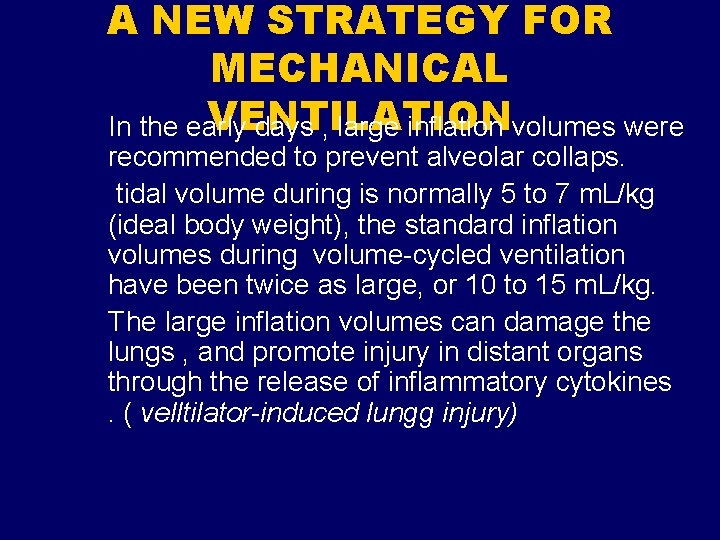
A NEW STRATEGY FOR MECHANICAL VENTILATION In the early days , large inflation volumes were recommended to prevent alveolar collaps. tidal volume during is normally 5 to 7 m. L/kg (ideal body weight), the standard inflation volumes during volume-cycled ventilation have been twice as large, or 10 to 15 m. L/kg. The large inflation volumes can damage the lungs , and promote injury in distant organs through the release of inflammatory cytokines. ( velltilator-induced lungg injury)
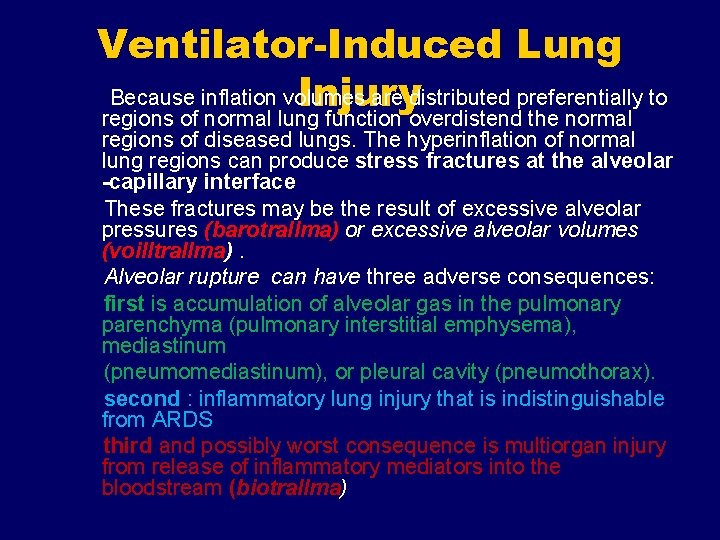
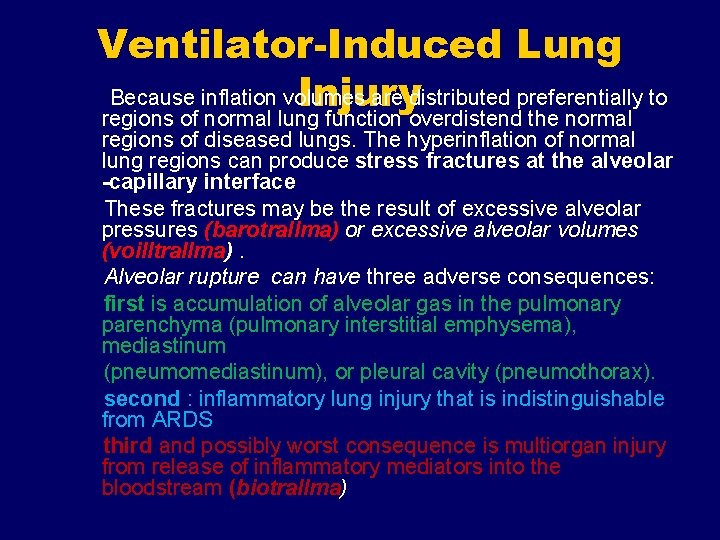
Ventilator-Induced Lung Because inflation volumes are distributed preferentially to Injury regions of normal lung function overdistend the normal regions of diseased lungs. The hyperinflation of normal lung regions can produce stress fractures at the alveolar -capillary interface These fractures may be the result of excessive alveolar pressures (barotrallma) or excessive alveolar volumes (voilltrallma). Alveolar rupture can have three adverse consequences: first is accumulation of alveolar gas in the pulmonary parenchyma (pulmonary interstitial emphysema), mediastinum (pneumomediastinum), or pleural cavity (pneumothorax). second : inflammatory lung injury that is indistinguishable from ARDS third and possibly worst consequence is multiorgan injury from release of inflammatory mediators into the bloodstream (biotrallma)
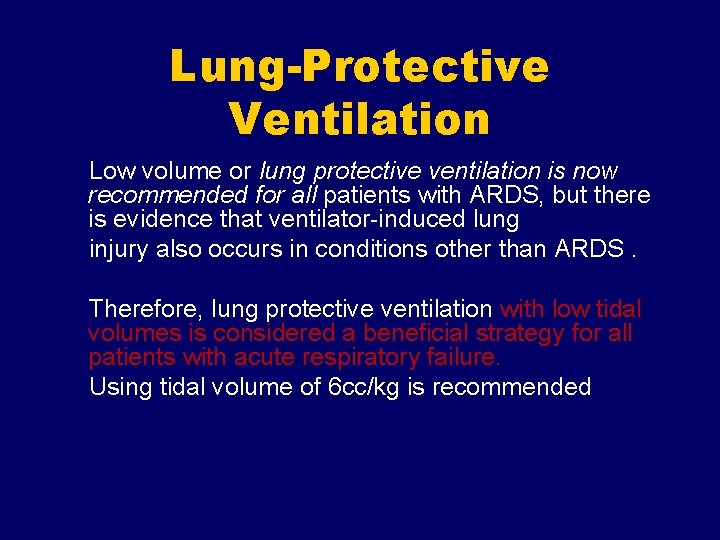
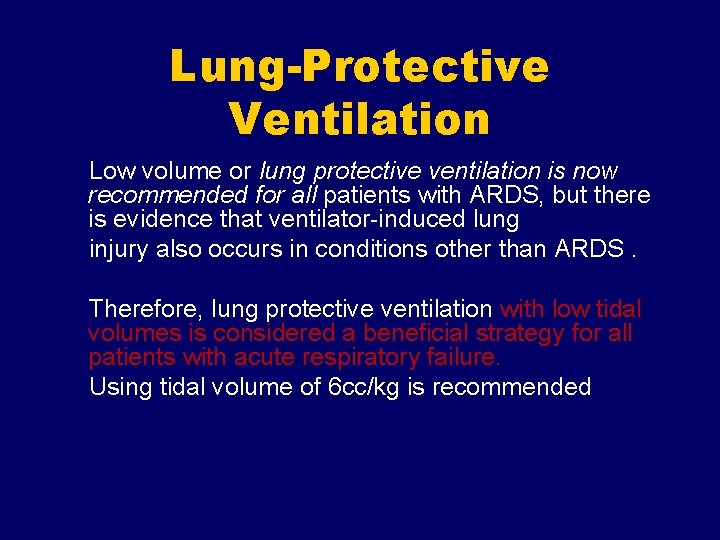
Lung-Protective Ventilation Low volume or lung protective ventilation is now recommended for all patients with ARDS, but there is evidence that ventilator-induced lung injury also occurs in conditions other than ARDS. Therefore, lung protective ventilation with low tidal volumes is considered a beneficial strategy for all patients with acute respiratory failure. Using tidal volume of 6 cc/kg is recommended
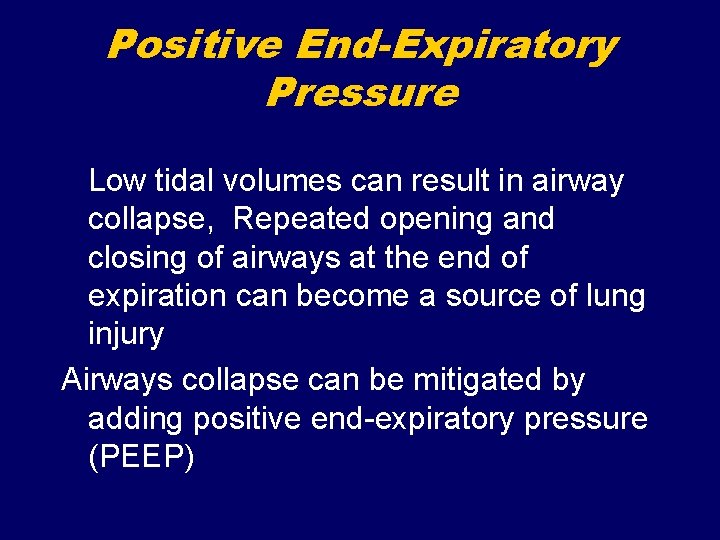
Positive End-Expiratory Pressure Low tidal volumes can result in airway collapse, Repeated opening and closing of airways at the end of expiration can become a source of lung injury Airways collapse can be mitigated by adding positive end-expiratory pressure (PEEP)
Permissive Hypercapnia Another consequence of low volume ventilation is a reduction in CO 2 elimination via the lungs, which can lead to hypercapnia and respiratory acidosis. Allowing hypercapnia to persist in favor of maintaining low volume ventilation is known as permissive hypercapnia
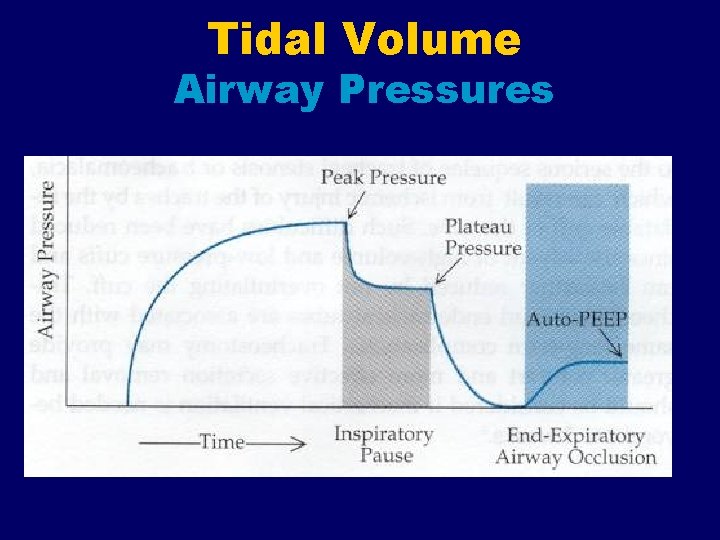
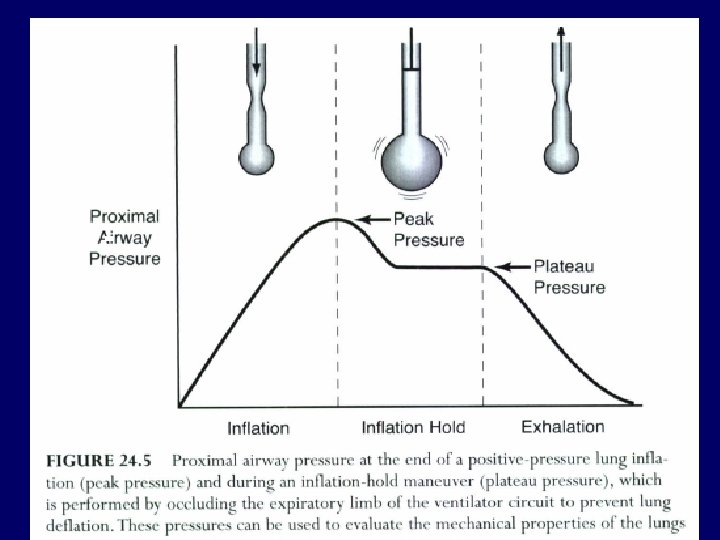
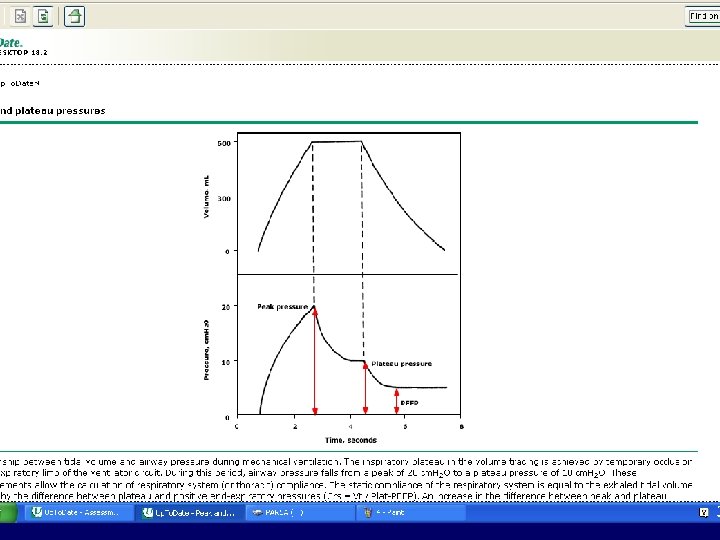
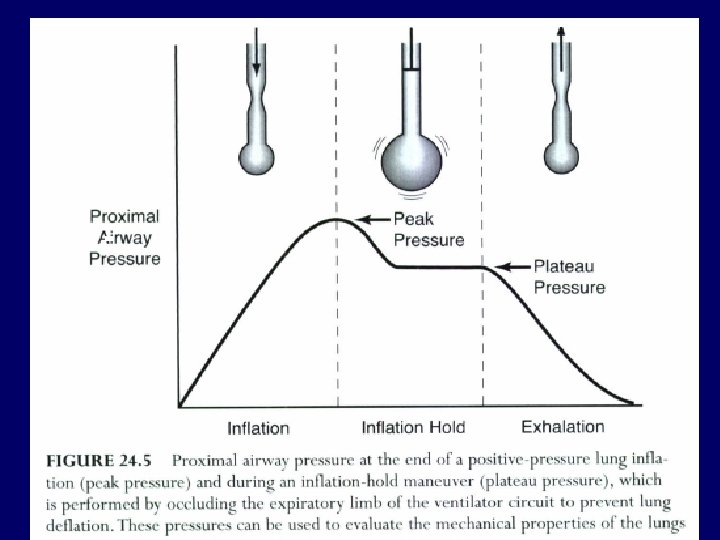
MONITORING LUNG MECHANICS Proximal Airway Pressures Positive-pressure mechanical ventilators have a pressure gauge that monitors the proximal airway pressure during each respiratory cycle.
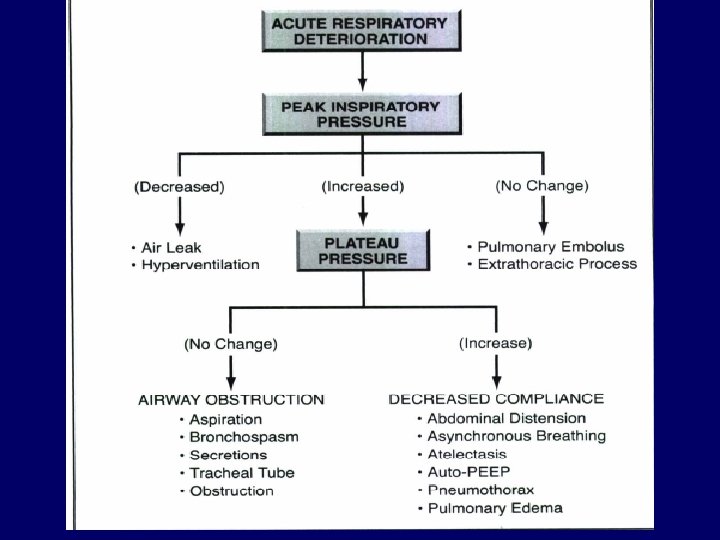
End-Inspiratory Peak Pressure The peak pressure at the end of inspiration (P peak)is a function of the inflation volume, the flow resistance in the airways, and the elastic recoil force of the lungs and chest wall P peak= (Resistance + Elastance) when the inflation volume is constant, an increase in peak inspiratory pressure indicates an increase in airway resistance or an increase in the elastic recoil force of the lungs (or both).
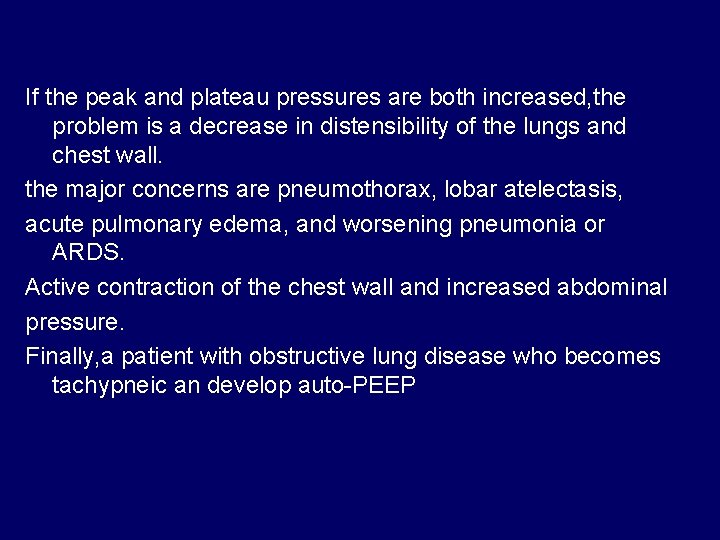
'End-Inspiratory Plateau Pressure When the inflation volume is held in the lungs, the proximal airway pressure decreases initially and then reaches a steady level, which is called the end-inspiratory plateau pressure. the Plateau Pressure is directly related to the elastic recoil force (elastance) of the lungs and chest wall. Pp. Iateau=: Elastance the difference between end-inspiratory peak and plateau pressures is proportional to the flow resistance in the airways. (P k - P I t) =: Airways Resistance
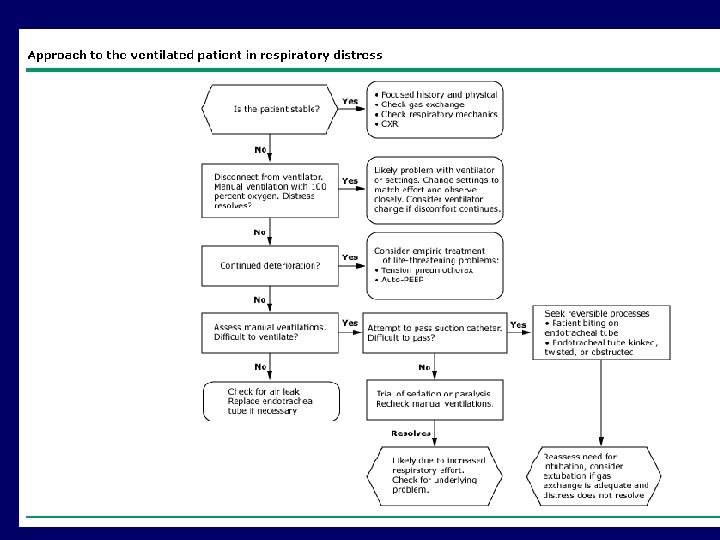
Practical Applications A common scenario in any ICU is a ventilator-dependent patient who develops a sudden deterioration in cardiopulmonary status (this could include hypotension, hypoxemia, or respiratory distress).
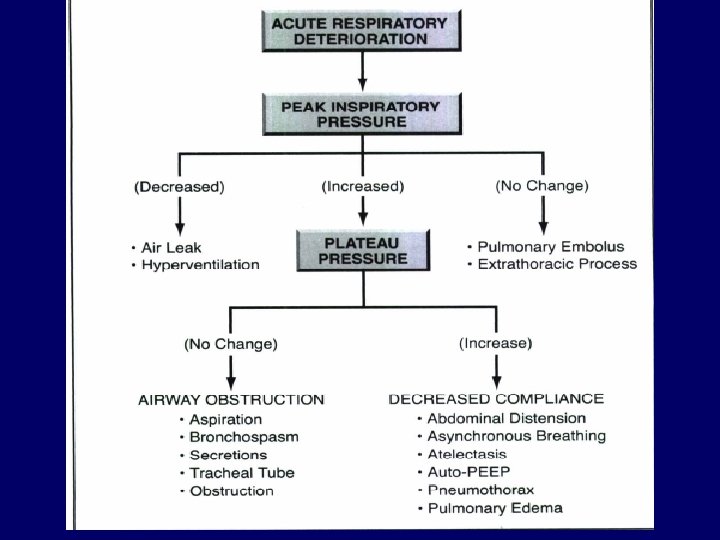
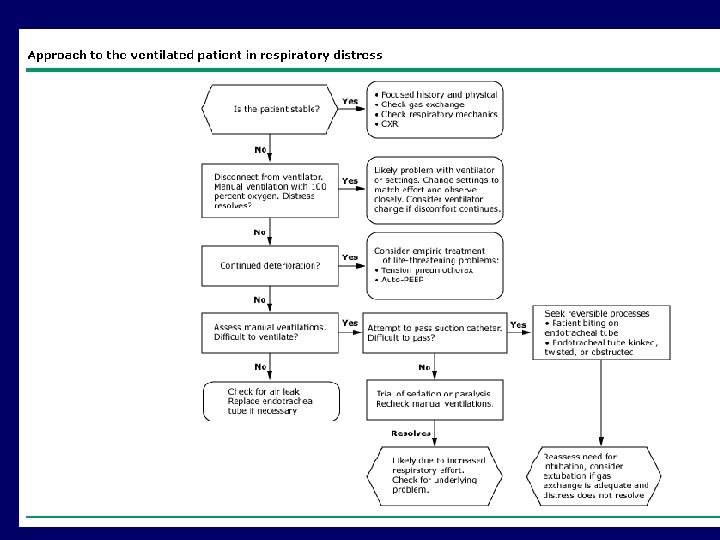
If the peak pressure is increased but the plateau pressure is unchanged, the problem is an increase in airways resistance. In this situation, the major concerns are obstruction of the tracheal tube, airway obstruction from secretions, and acute bronchospasm. Therefore, airways suctioning is indicated to clear secretions, followed by an aerosolized bronchodilator treatment if necessary.
If the peak and plateau pressures are both increased, the problem is a decrease in distensibility of the lungs and chest wall. the major concerns are pneumothorax, lobar atelectasis, acute pulmonary edema, and worsening pneumonia or ARDS. Active contraction of the chest wall and increased abdominal pressure. Finally, a patient with obstructive lung disease who becomes tachypneic an develop auto-PEEP