MECHANICAL VENTILATION Indications Relieve respiratory distress Rest respiratory



















- Slides: 51

MECHANICAL VENTILATION

Indications Relieve respiratory distress Rest respiratory muscles Decrease work of breathing Improve oxygenation Prevent or reverse atelectasis Improve ventilation Decrease O 2 consumption Permit sedation Stabilize chest wall Prevent complications
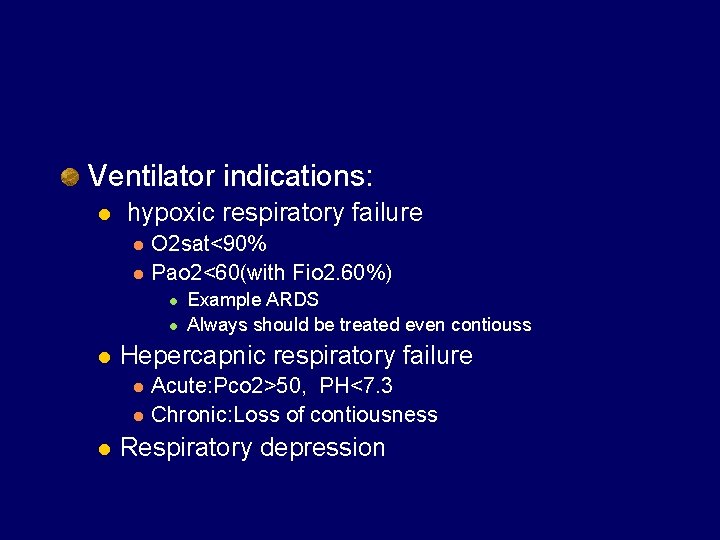
Ventilator indications: l hypoxic respiratory failure l l O 2 sat<90% Pao 2<60(with Fio 2. 60%) l l l Hepercapnic respiratory failure l l l Example ARDS Always should be treated even contiouss Acute: Pco 2>50, PH<7. 3 Chronic: Loss of contiousness Respiratory depression
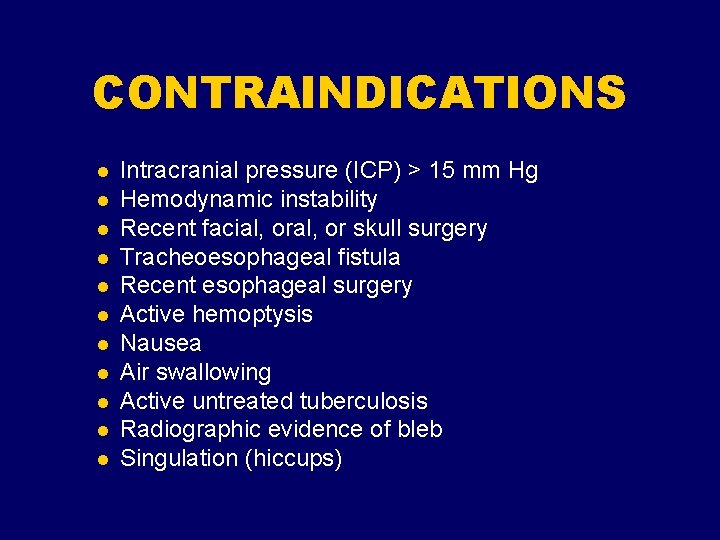
CONTRAINDICATIONS l l l Intracranial pressure (ICP) > 15 mm Hg Hemodynamic instability Recent facial, or skull surgery Tracheoesophageal fistula Recent esophageal surgery Active hemoptysis Nausea Air swallowing Active untreated tuberculosis Radiographic evidence of bleb Singulation (hiccups)

Mechanical Ventilation Abbreviations: VT: Tidal volume (ml) RR: Respiratory Rate (bpm) MV: Minute Volume = VT x RR (l/m)) Fi. O 2: Fraction of inspired Oxygen PEEP: Positive end expiratory pressure (cm. H 20) (I: E) Ratio : Ratio of inspiratory to expiratory time. Ti: Inspiratory time Flowrate: Speed of gas flow in liters per minute.

Ventilator settings 1. 2. 3. 4. 5. 6. 7. 8. Ventilator mode Respiratory rate Tidal volume or pressure settings Inspiratory flow I: E ratio PEEP Fi. O 2 Inspiratory trigger

Mode FIO 2 20% -100% Rate 4 -30 Tidal volume 4 -9 cc/kg Flow 20 -100 Lit/min PEEP/CPAP 0 -22 mm. H 2 O Pressure 5 -20 mm. H 2 O Just for PSV Mode P ins 5 -40 mm H 2 o Just for CMV Mode Trigger 1 cc/sec (flow trigger) -1 Cm H 2 O(pressure trigger) Always on minimum I/E ratio 1/4 1/3 1/2 1/1 2
Respiratory Rate
Tidal Volume or Pressure setting Maximum volume/pressure to achieve good ventilation and oxygenation without producing alveolar overdistention Max cc/kg = 10 cc/kg Some clinical exceptions
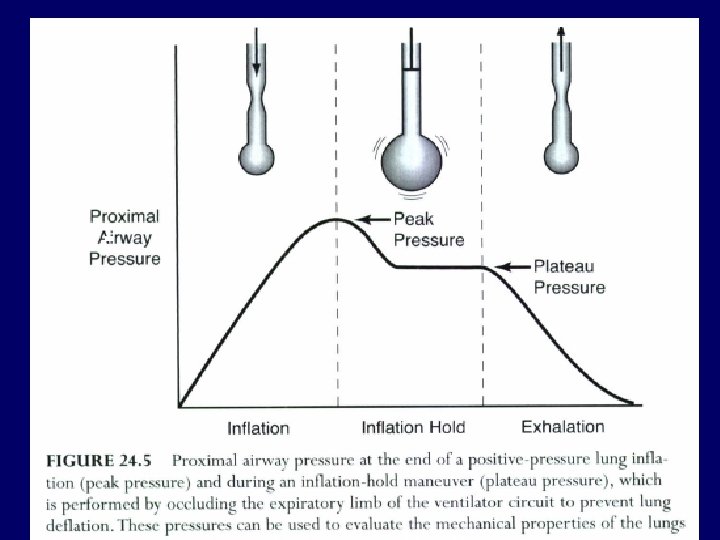
Tidal Volume Vt > TLC can result in over-distended lung and lung injury TLC reduced in lung disease TLC plateau pressure = 30 – 35 cm. H 2 O
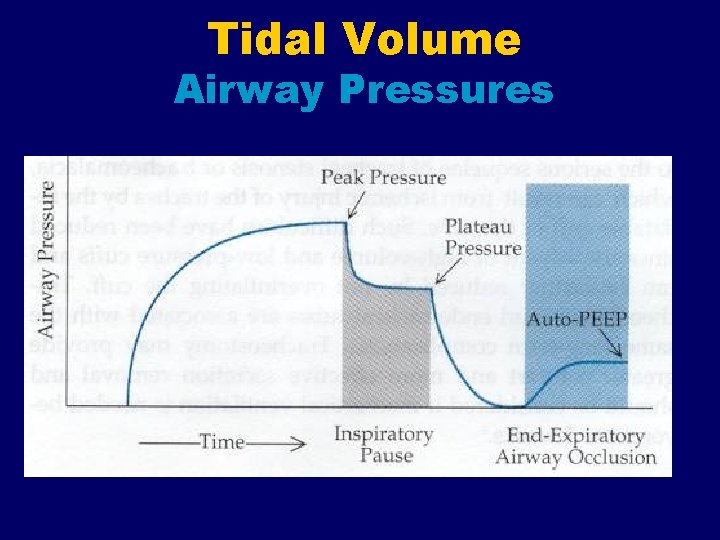
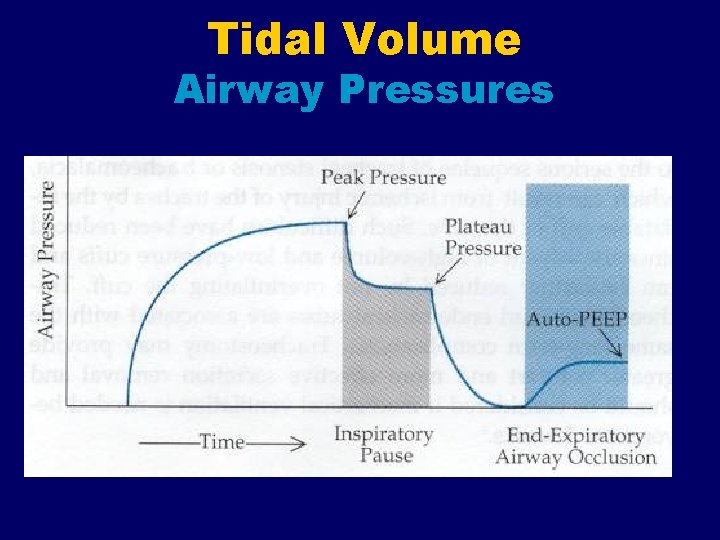
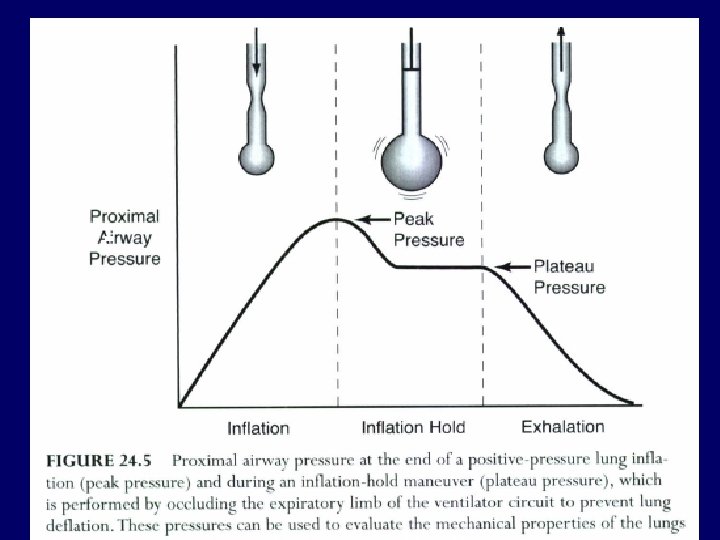
Tidal Volume Airway Pressures
Tidal Volume What Vt should be used? Traditionally 10 -12 ml/kg l “Kg” based on ideal body weight l l PBW (male) = 50 + 2. 3 [(Ht in inches) – 60] PBW (female) = 45. 5 + 2. 3[(Ht in inches) – 60] l Theoretically prevents atelectasis l Most appropriate if normal lungs l Anesthesia, drug overdose

Tidal Volume What Vt should be used? Lung disease present l 8 – 10 ml/kg Regardless of Vt l Pplateau < 30 – 35 cm. H 2 O
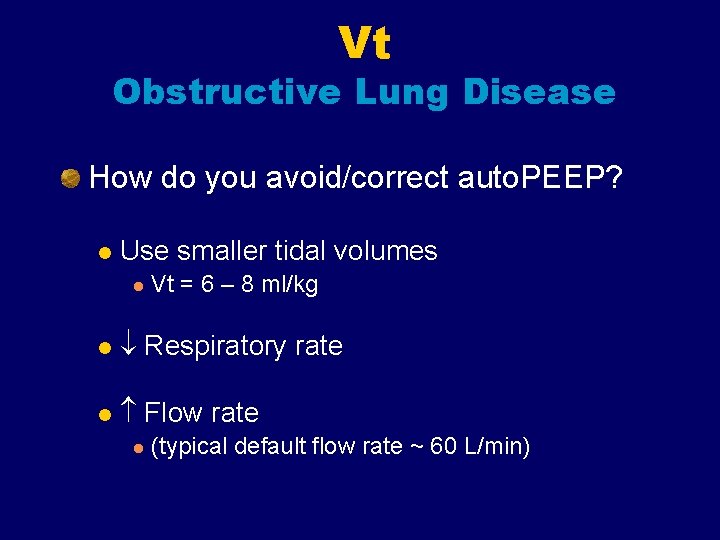
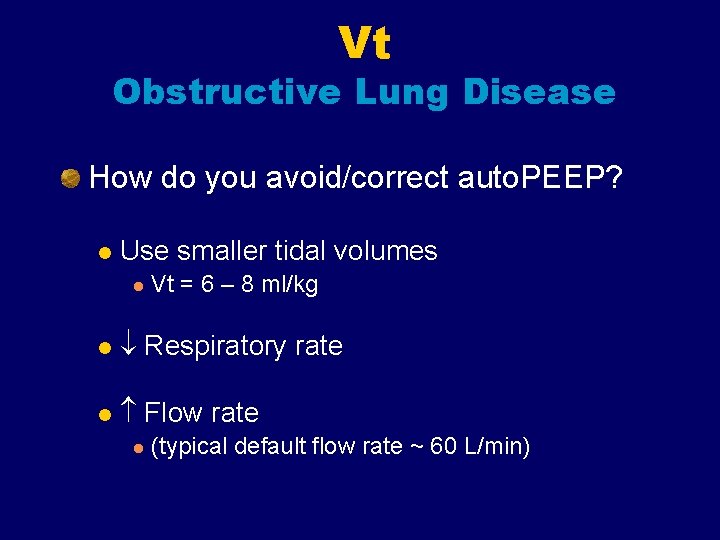
Vt Obstructive Lung Disease How do you avoid/correct auto. PEEP? l Use smaller tidal volumes l Vt = 6 – 8 ml/kg l Respiratory rate l Flow rate l (typical default flow rate ~ 60 L/min)
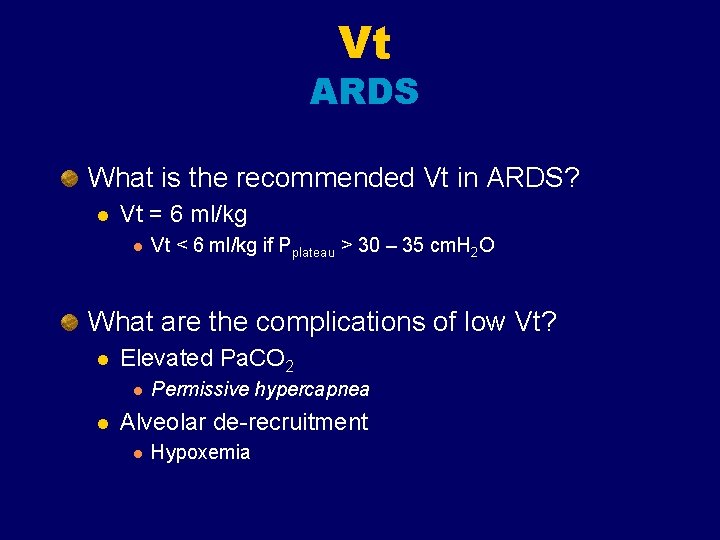
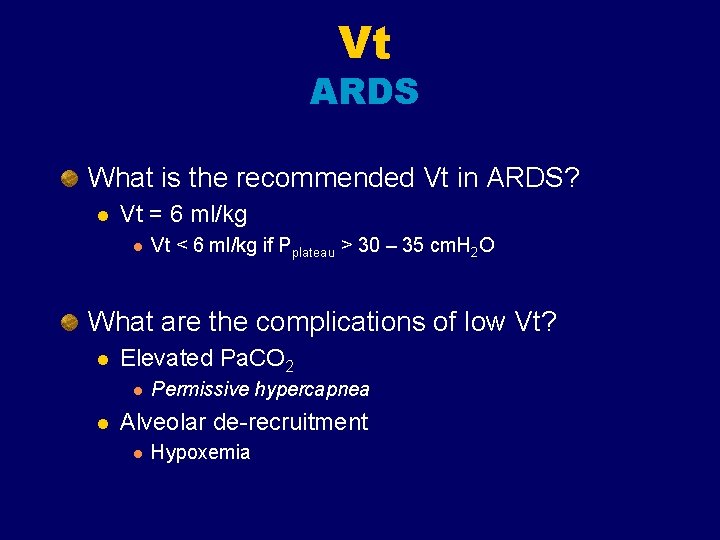
Vt ARDS What is the recommended Vt in ARDS? l Vt = 6 ml/kg l Vt < 6 ml/kg if Pplateau > 30 – 35 cm. H 2 O What are the complications of low Vt? l Elevated Pa. CO 2 l l Permissive hypercapnea Alveolar de-recruitment l Hypoxemia
Sighs Because a spontaneously breathing individual typically sighs 6 -8 times per hour to avoid microatelectasis, giving periodic machine breaths of 1. 5 -2 times the preset tidal volume 6 -8 times per hour was once recommended. Often, the peak pressure needed to deliver such a volume would predispose the patient to barotrauma. Today, sighs are usually not used if the patient is receiving tidal volumes of 10 -12 m. L/kg or requires the use of positive end-expiratory pressure (PEEP).
I: E Ratio 1: 2 Prolonged at 1: 3, 1: 4, … Inverse ratio
FIO 2 The usual goal is to use the minimum Fio 2 required to have a Pa. O 2 > 60 mmhg or a sat >90% Start at 100% Oxygen toxicity normally with Fio 2 >60%

Inspiratory flow Varies with the Vt, I: E and RR Normally about 40 -60 l/min Can be majored to 100 - 120 l/min




Positive end-expiratory pressure PEEP is a mode of therapy used in conjunction with mechanical ventilation. At the end of exhalation (either mechanical or spontaneous), patient airway pressure is maintained above atmospheric pressure by exerting a pressure that opposes complete passive emptying of the lung. This pressure is typically achieved by maintaining a positive pressure flow at the end of exhalation.
Positive end-expiratory pressure PEEP therapy can be effective when used in patients with a diffuse lung disease that results in an acute decrease in functional residual capacity (FRC). In many pulmonary diseases, FRC is reduced because of the collapse of the unstable alveoli. This reduction in lung volume decreases the surface area available for gas exchange and results in intrapulmonary shunting. If the FRC is not restored, a high concentration of inspired oxygen may be required to maintain the arterial oxygen content of the blood at an acceptable range.

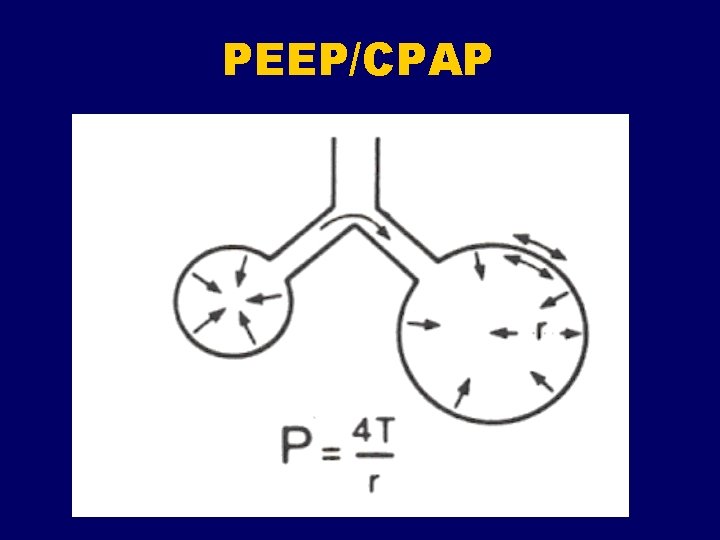
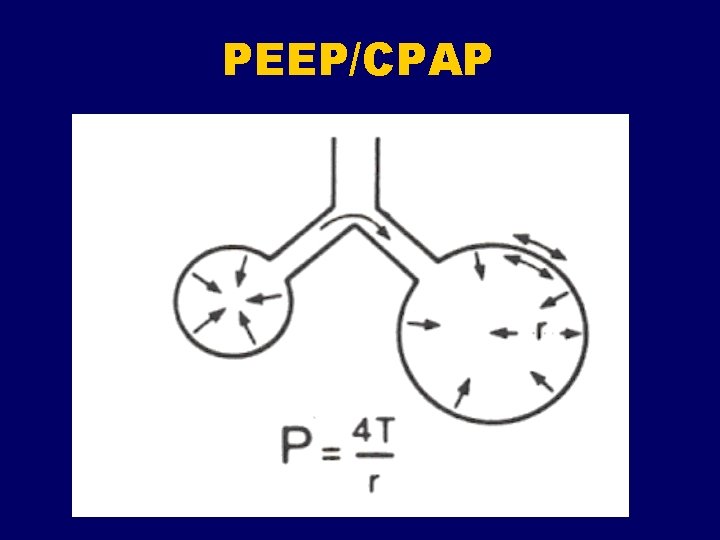
Positive end-expiratory pressure Applying continuous positive pressure at the end of exhalation (eg, PEEP, continuous positive airway pressure [CPAP]) causes an increase in alveolar pressure and an increase in alveolar volume. This increase in lung volume increases the surface area by reopening or stabilizing collapsed or unstable alveoli. This “splinting” or “propping open” of the alveoli with positive pressure may provide a better matching of ventilation to perfusion, thereby reducing the shunt effect.
Positive end-expiratory pressure Once a true shunt is changed to a ventilation/perfusion mismatch, lower concentrations of oxygen can be used to maintain an adequate Pa. O 2. PEEP therapy has also been effective for improving lung compliance. When the FRC and lung compliance are decreased, more energy and volume are needed to inflate the lung. By applying PEEP, the lung volume at the end of exhalation is increased, which decreases the work of breathing because the lung is already partially inflated; therefore, less volume and energy are needed to inflate the lung.
Positive end-expiratory pressure In summary, when used to treat patients with a diffuse lung disease, PEEP should improve compliance, decrease dead space, and decrease the intrapulmonary shunt effect. The most significant benefit of PEEP is that the patient can maintain an adequate Pa. O 2 at a lower and safer concentration of oxygen (<60%), thereby reducing the risk of oxygen toxicity.
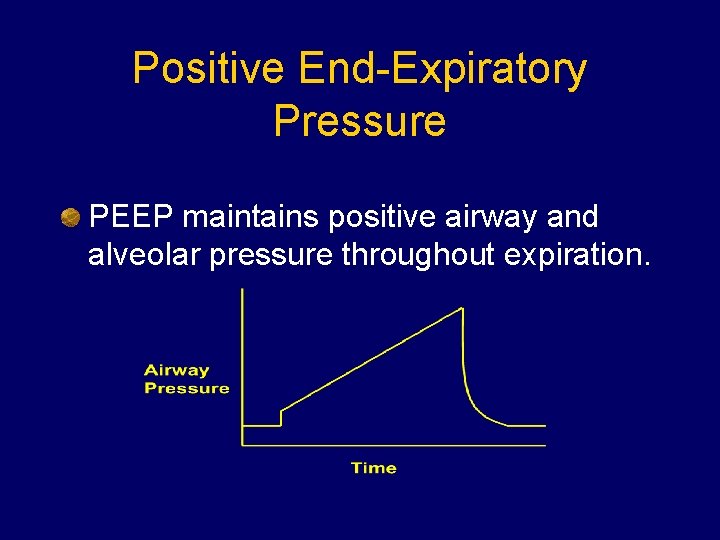
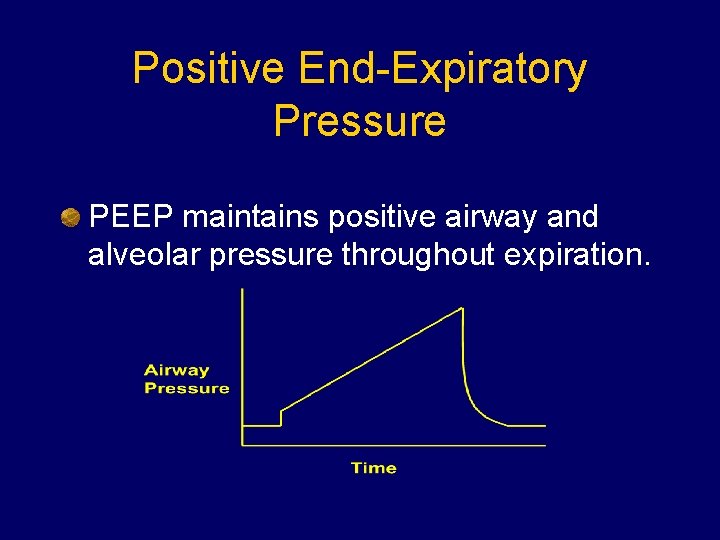
Positive End-Expiratory Pressure PEEP maintains positive airway and alveolar pressure throughout expiration.

PEEP/CPAP Indications Refractory hypoxemia Pa. O 2/FIO 2 < 150 l Prototypic disease = ARDS l COPD with air-trapping “Physiologic” PEEP
PEEP/CPAP Where do you start? l PEEP = 5 – 7 cm. H 2 O l Increase in increments of 2 -3 cm. H 2 O Where do you stop? l Goals: Adequate oxygenation l FIO 2 reduced to acceptable level l l No upper limit exists

Positive End-Expiratory Pressure Physiologic Effects Increases end-expiratory volume l Prevents alveolar collapse Reduces shunt fraction l Improves Pa. O 2 l l May over-distend alveoli l Ventilator-induced lung injury
Positive End-Expiratory Pressure Physiologic Effects Increases pleural (intra-thoracic) pressure l Reduces venous return l Reduces cardiac output and DO 2
PEEP What are the secondary effects of PEEP? Barotrauma l Diminish cardiac output l Regional hypoperfusion l Na. Cl retention l Augmentation of ICP? l Paradoxal hypoxemia l
PEEP Relative Contraindications: Barotrauma l Airway trauma l Unilateral lung disease l Hemodynamic instability l Hypovolemia l ICP? l Bronchopleural fistula l

PEEP/CPAP Why might PEEP worsen hypoxemia in unilateral lung disease? l Effects of PEEP go to normal alveoli and not diseased alveoli
PEEP/CPAP
PEEP/CPAP Complications What is the most feared complication? l Barotrauma What is the most common? l Reductions in cardiac output Loss of venous return to right atrium l Paradoxical movement of intraventricular septum l Pulmonary vessel compression l
Ventilator Settings Changing Initial Settings Base changes in FIO 2 on: ABG’s l Pulse oximetry l Base changes in Vt and/or RR on: Normalizing p. H, NOT Pa. CO 2 or HCO 3 l Avoid “routine” ABG’s l
Oxygenation decisions With the target Pa. O 2 identified, the FIO 2 can be adjusted using the following formula: New FIO 2 = (old FIO 2 X desired Pa. O 2)/measured Pa. O 2
Ventilation Decisions New rate = (old rate X measured PCO 2)/desired PCO 2

Assist-control, volume Ingento EP & Drazen J: Mechanical Ventilators, in Hall JB, Scmidt GA, & Wood LDH(eds. ): Principles of Critical Care
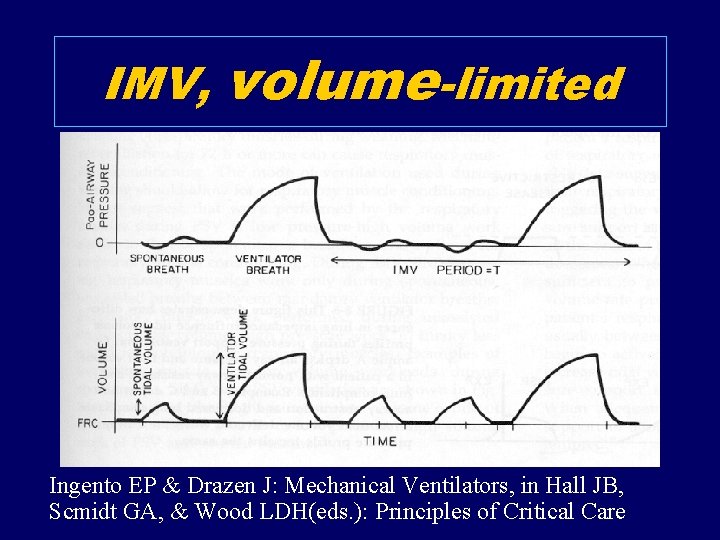
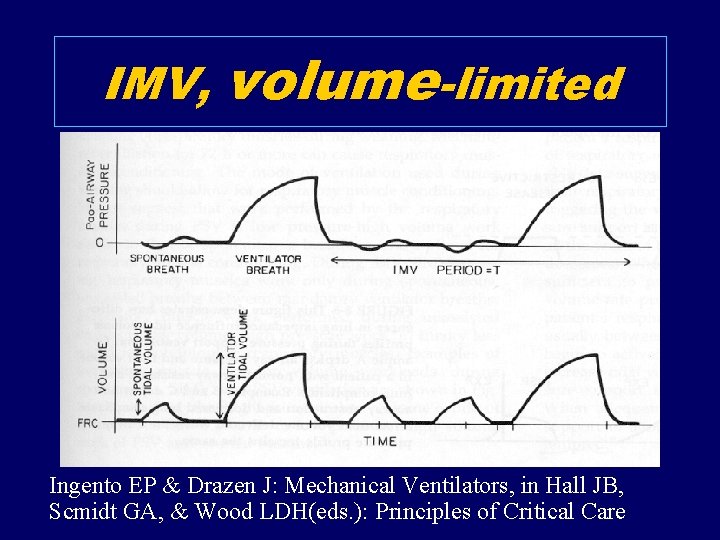
IMV, volume-limited Ingento EP & Drazen J: Mechanical Ventilators, in Hall JB, Scmidt GA, & Wood LDH(eds. ): Principles of Critical Care
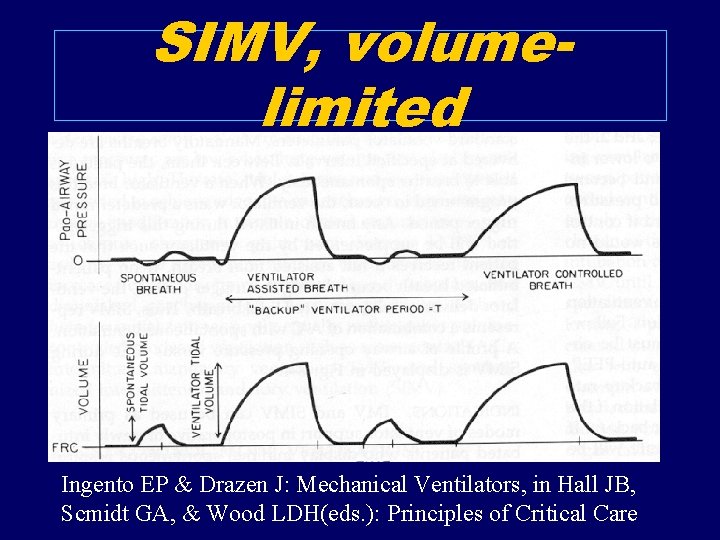
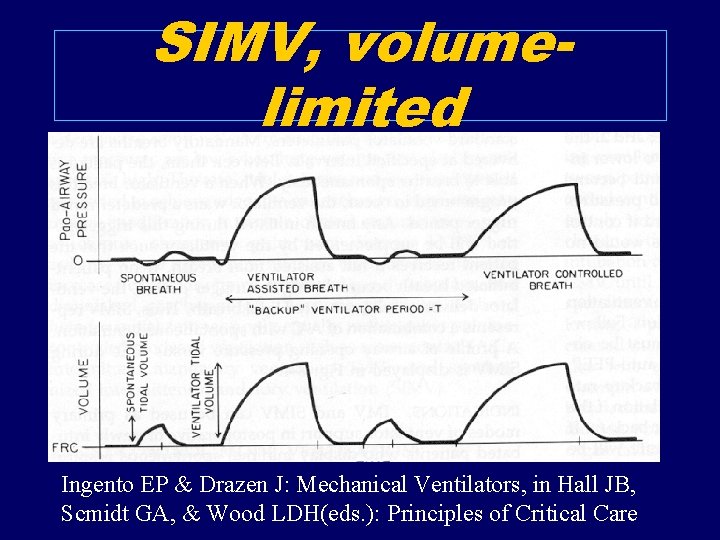
SIMV, volumelimited Ingento EP & Drazen J: Mechanical Ventilators, in Hall JB, Scmidt GA, & Wood LDH(eds. ): Principles of Critical Care
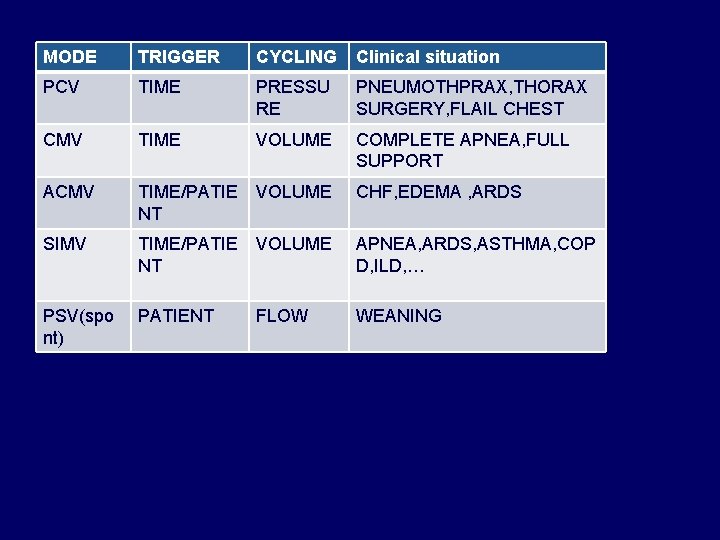
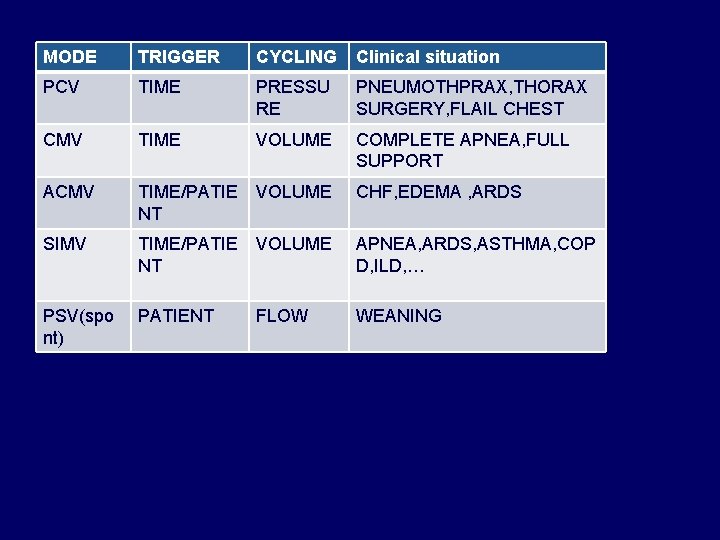
MODE TRIGGER CYCLING Clinical situation PCV TIME PRESSU RE PNEUMOTHPRAX, THORAX SURGERY, FLAIL CHEST CMV TIME VOLUME COMPLETE APNEA, FULL SUPPORT ACMV TIME/PATIE NT VOLUME CHF, EDEMA , ARDS SIMV TIME/PATIE NT VOLUME APNEA, ARDS, ASTHMA, COP D, ILD, … PSV(spo nt) PATIENT FLOW WEANING
PCV: pressure controled Ventilation CMV: controled mode ventilation ACMV: Assist controled mode ventilation SIMV: spontanous intermittent mandatory ventilation PSV: pressure support ventilation ASV: asssist spontanous ventilation



 Mechanical ventilation modes
Mechanical ventilation modes Pressure support ventilation
Pressure support ventilation Indication for mechanical ventilation
Indication for mechanical ventilation Malampti
Malampti Respiratory distress
Respiratory distress Respiratory distress
Respiratory distress Respiratory distress nasal flaring
Respiratory distress nasal flaring Types of ventilation fire fighting
Types of ventilation fire fighting Mechanical ventilation definition
Mechanical ventilation definition Dope in mechanical ventilation
Dope in mechanical ventilation Transpulmonary pressure formula
Transpulmonary pressure formula Mechanical ventilation 101
Mechanical ventilation 101 Iron lung
Iron lung Ventilation learning package
Ventilation learning package Rest and rest seats
Rest and rest seats Hamlet in purgatory
Hamlet in purgatory Occlusal rest seat
Occlusal rest seat Object at rest stays at rest
Object at rest stays at rest Rest seat
Rest seat Conducting zone respiratory
Conducting zone respiratory Actual mechanical advantage vs ideal mechanical advantage
Actual mechanical advantage vs ideal mechanical advantage Direct costs of financial distress
Direct costs of financial distress What is an archetype?
What is an archetype? What is stress
What is stress Distress tolerance thermometer
Distress tolerance thermometer Leonard pearlin theory of psychological distress
Leonard pearlin theory of psychological distress Message relay sample
Message relay sample Emotional thermometer
Emotional thermometer Psychology, mental health and distress
Psychology, mental health and distress Distress signal x1
Distress signal x1 Contoh distress
Contoh distress Distress example
Distress example Meconium grade 1 2 3
Meconium grade 1 2 3 Tipp skill dbt
Tipp skill dbt Nursing management of fetal distress
Nursing management of fetal distress Fetal distress definition
Fetal distress definition Paragraph about stress
Paragraph about stress Moral distress and burnout
Moral distress and burnout Static theory of capital structure
Static theory of capital structure Pengertian psikologi klinis makro
Pengertian psikologi klinis makro Damsel in distress archetype examples
Damsel in distress archetype examples Eustress and distress drawing
Eustress and distress drawing Distress words survival
Distress words survival Verbalisasi distress adalah
Verbalisasi distress adalah Leonard pearlin's theory of psychological distress
Leonard pearlin's theory of psychological distress Featal distress
Featal distress Estructuras del relieve
Estructuras del relieve Estructura aclinal
Estructura aclinal Fauna zona austral
Fauna zona austral Principales unidades de relieve del mundo
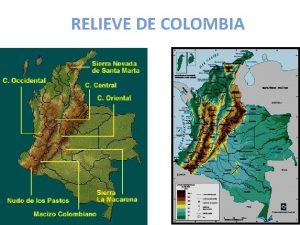
Principales unidades de relieve del mundo Relieve interno
Relieve interno El modelado del relieve
El modelado del relieve