Curiculum vitae EDUCATION Master of Medicine in Pain



- Slides: 180
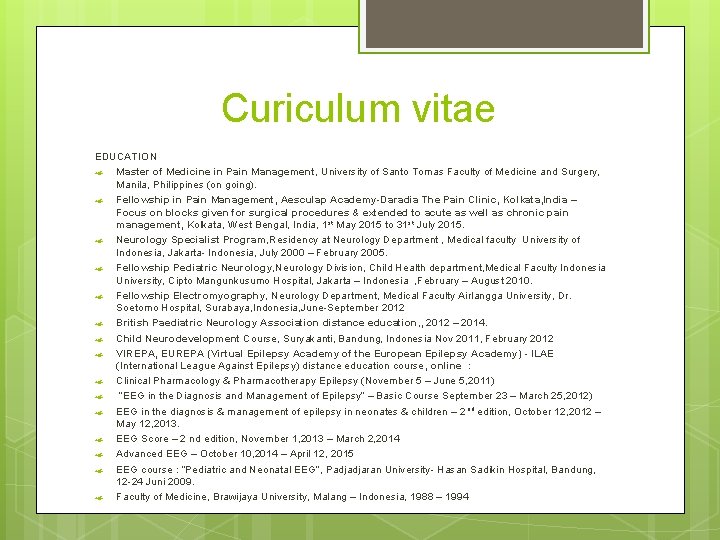
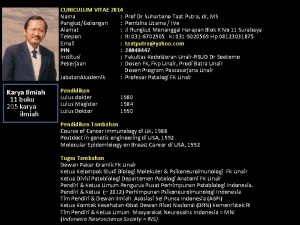
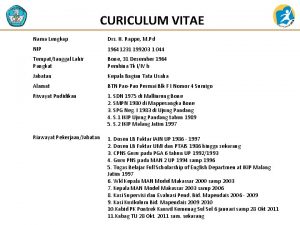
Curiculum vitae EDUCATION Master of Medicine in Pain Management, University of Santo Tomas Faculty of Medicine and Surgery, Manila, Philippines (on going). Fellowship in Pain Management, Aesculap Academy-Daradia The Pain Clinic, Kolkata, India – Focus on blocks given for surgical procedures & extended to acute as well as chronic pain management, Kolkata, West Bengal, India, 1 st May 2015 to 31 st July 2015. Neurology Specialist Program, Residency at Neurology Department , Medical faculty University of Indonesia, Jakarta- Indonesia, July 2000 – February 2005. Fellowship Pediatric Neurology, Neurology Division, Child Health department, Medical Faculty Indonesia University, Cipto Mangunkusumo Hospital, Jakarta – Indonesia , February – August 2010. Fellowship Electromyography, Neurology Department, Medical Faculty Airlangga University, Dr. Soetomo Hospital, Surabaya, Indonesia, June-September 2012 British Paediatric Neurology Association distance education, , 2012 – 2014. Child Neurodevelopment Course, Suryakanti, Bandung, Indonesia Nov 2011, February 2012 VIREPA, EUREPA (Virtual Epilepsy Academy of the European Epilepsy Academy) - ILAE (International League Against Epilepsy) distance education course , online : Clinical Pharmacology & Pharmacotherapy Epilepsy (November 5 – June 5, 2011) “EEG in the Diagnosis and Management of Epilepsy” – Basic Course September 23 – March 25, 2012) EEG in the diagnosis & management of epilepsy in neonates & children – 2 nd edition, October 12, 2012 – May 12, 2013. EEG Score – 2 nd edition, November 1, 2013 – March 2, 2014 Advanced EEG – October 10, 2014 – April 12, 2015 EEG course : “Pediatric and Neonatal EEG”, Padjadjaran University- Hasan Sadikin Hospital, Bandung, 12 -24 Juni 2009. Faculty of Medicine, Brawijaya University, Malang – Indonesia, 1988 – 1994
HEADACHE dr. Istiana Sari, Sp. S, FIPM RS Hermina Bekasi
Introduction Commonest neurological consultation Need for systematic approach 3
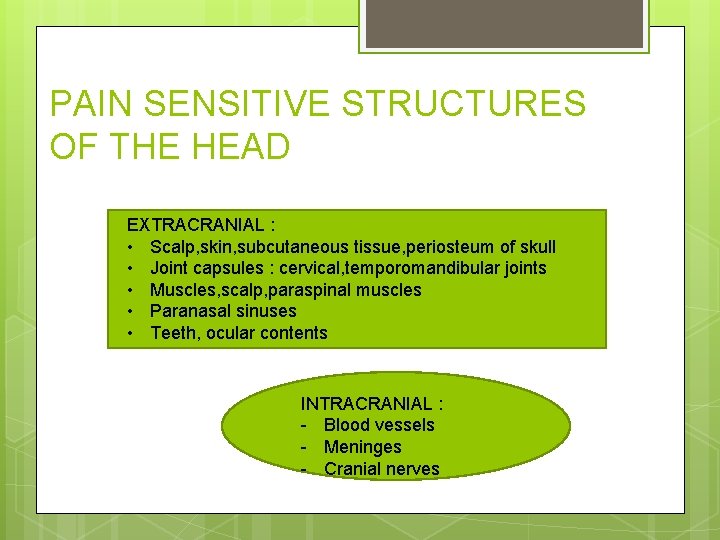
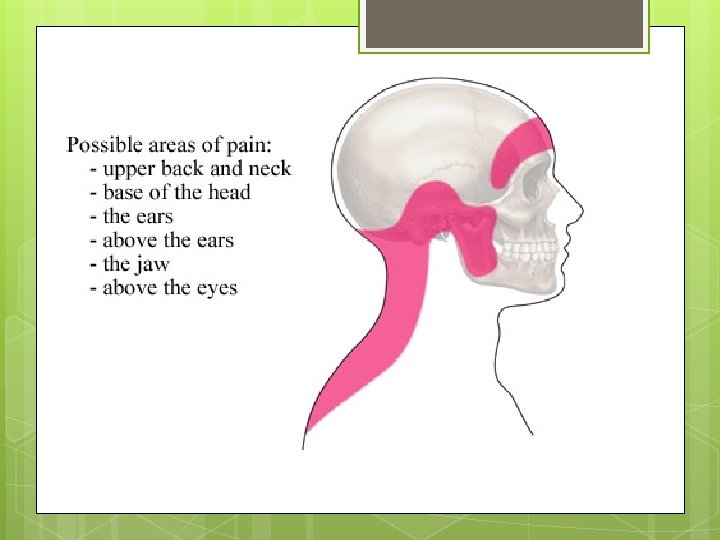
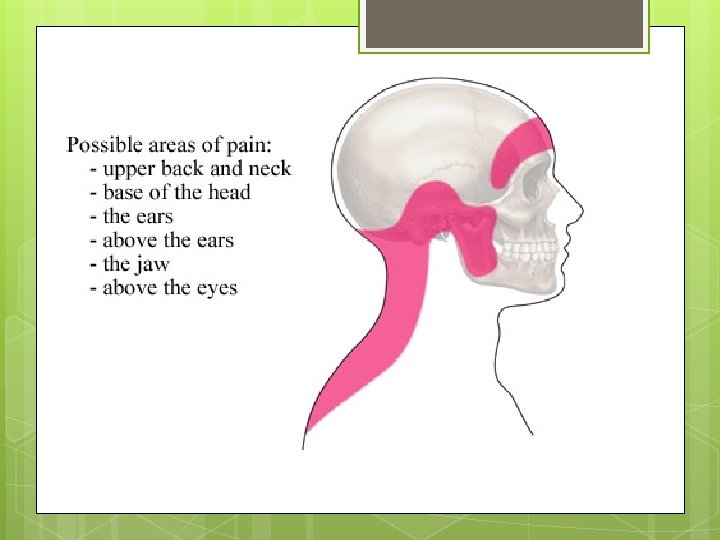
PAIN SENSITIVE STRUCTURES OF THE HEAD EXTRACRANIAL : • Scalp, skin, subcutaneous tissue, periosteum of skull • Joint capsules : cervical, temporomandibular joints • Muscles, scalp, paraspinal muscles • Paranasal sinuses • Teeth, ocular contents INTRACRANIAL : - Blood vessels - Meninges - Cranial nerves
Causes of headaches. 1. Traction or dilatation of intracranial or extracranial arteries. 2. Traction of large extracranial veins 3. Compression, traction or inflammation of cranial and spinal nerves 4. Spasm and trauma to cranial and cervical muscles. 5. Meningeal irritation and raised intracranial pressure 6. Disturbance of intracerebral serotonergic projections
Objectives 1. 2. 3. Become aware of the IHS classification Be able to diagnose and treat the common types of primary headache Be able to recognize the “red flags” of dangerous secondary headache
Classification IHS ICHD-1(1988) to ICHD-2(2004) Primary Secondary 7
INTERNATIONAL HEADACHE SOCIETY (HIS) CRITERIA HIS has developed criteria to divide headaches into primary and secondary types Ø Primary type : headaches without specific cause (migraine, tension, cluster) Ø Secondary type : headaches with underlying structural or metabolic cause Ø
IHS CLASSIFICATION THE PRIMARY HEADACHES 1. 2. Migraine 1. 1 Migraine without aura (common migraine) 1. 2 Migraine with aura (classic migraine) 1. 3 Basilar migraine 1. 4 Familial hemiplegic migraine Tension type headache 2. 1 Infrequent episodic TTH 2. 2 Frequent episodic TTH 2. 3 Chronic TTH International Classification of Headache Disorders, 2 nd ed, Cephalgia 2004; 24 (supp; -1)1 -160)
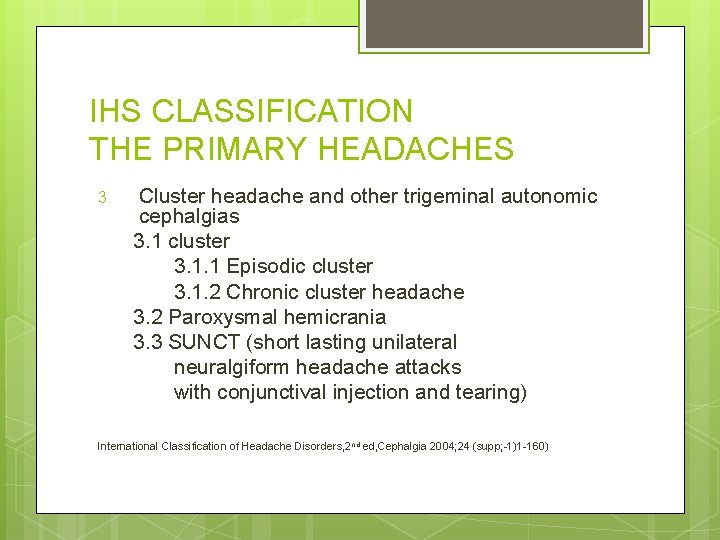
IHS CLASSIFICATION THE PRIMARY HEADACHES 3. Cluster headache and other trigeminal autonomic cephalgias 3. 1 cluster 3. 1. 1 Episodic cluster 3. 1. 2 Chronic cluster headache 3. 2 Paroxysmal hemicrania 3. 3 SUNCT (short lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing) International Classification of Headache Disorders, 2 nd ed, Cephalgia 2004; 24 (supp; -1)1 -160)
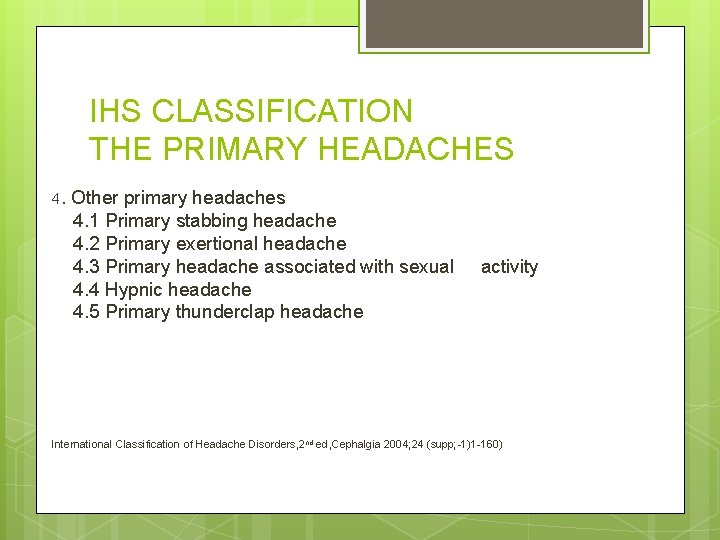
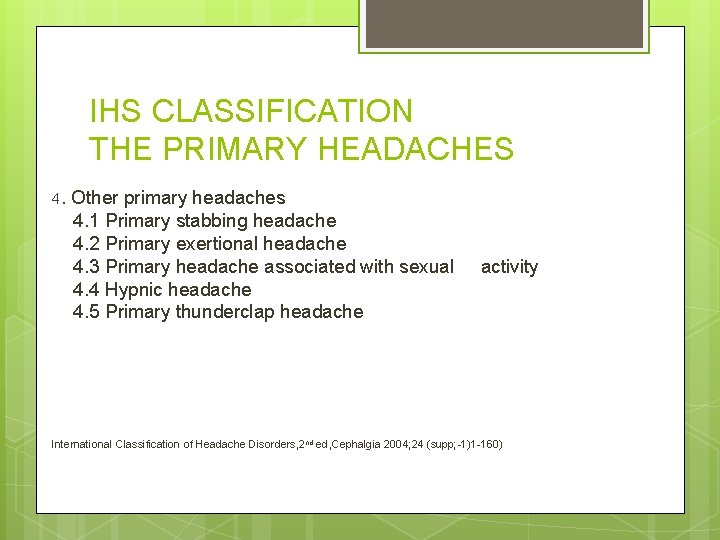
IHS CLASSIFICATION THE PRIMARY HEADACHES 4. Other primary headaches 4. 1 Primary stabbing headache 4. 2 Primary exertional headache 4. 3 Primary headache associated with sexual 4. 4 Hypnic headache 4. 5 Primary thunderclap headache activity International Classification of Headache Disorders, 2 nd ed, Cephalgia 2004; 24 (supp; -1)1 -160)
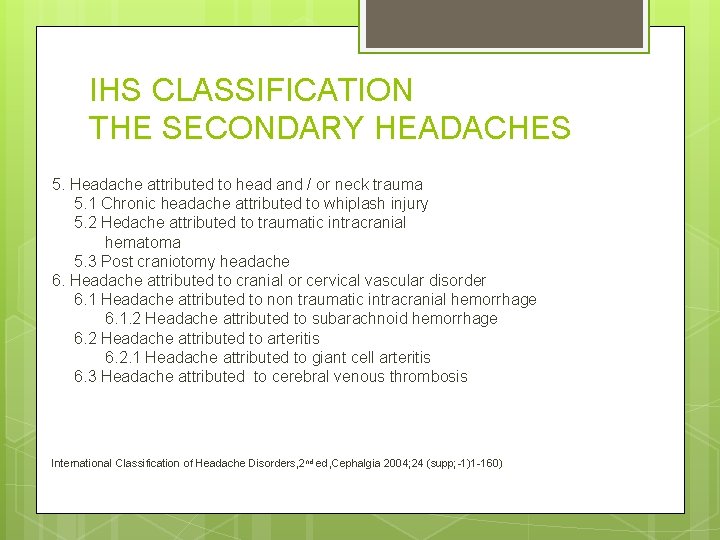
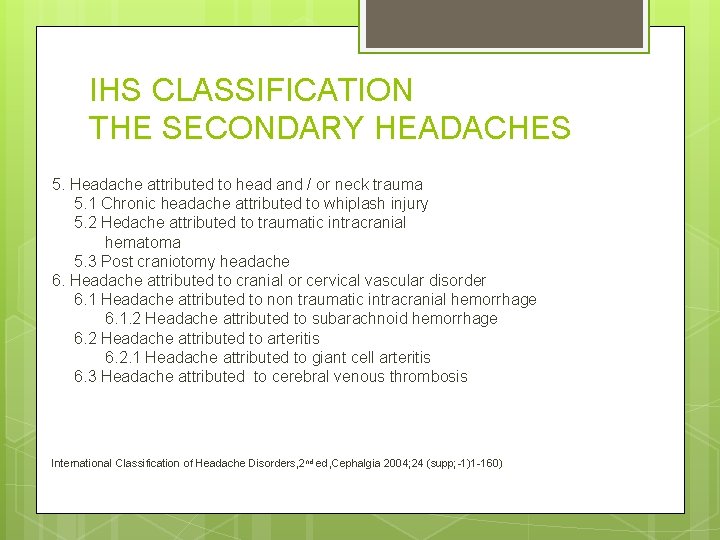
IHS CLASSIFICATION THE SECONDARY HEADACHES 5. Headache attributed to head and / or neck trauma 5. 1 Chronic headache attributed to whiplash injury 5. 2 Hedache attributed to traumatic intracranial hematoma 5. 3 Post craniotomy headache 6. Headache attributed to cranial or cervical vascular disorder 6. 1 Headache attributed to non traumatic intracranial hemorrhage 6. 1. 2 Headache attributed to subarachnoid hemorrhage 6. 2 Headache attributed to arteritis 6. 2. 1 Headache attributed to giant cell arteritis 6. 3 Headache attributed to cerebral venous thrombosis International Classification of Headache Disorders, 2 nd ed, Cephalgia 2004; 24 (supp; -1)1 -160)
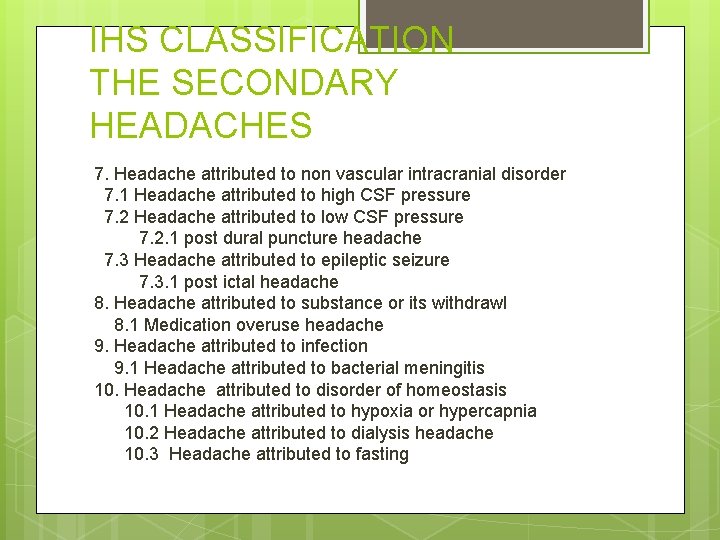
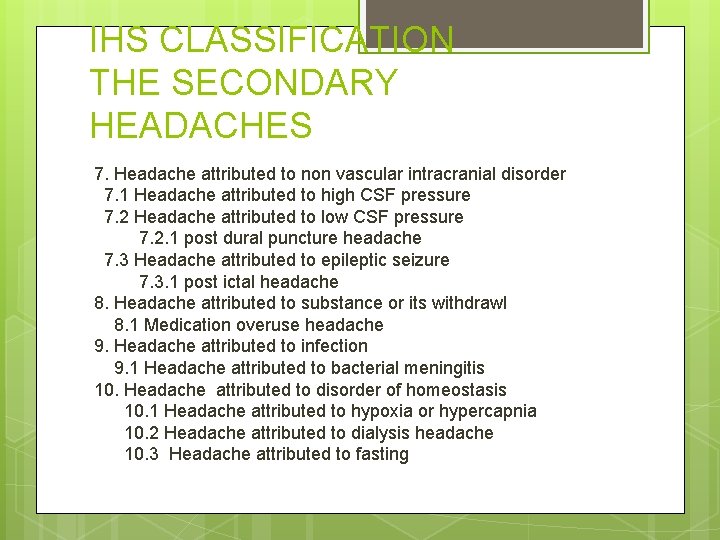
IHS CLASSIFICATION THE SECONDARY HEADACHES 7. Headache attributed to non vascular intracranial disorder 7. 1 Headache attributed to high CSF pressure 7. 2 Headache attributed to low CSF pressure 7. 2. 1 post dural puncture headache 7. 3 Headache attributed to epileptic seizure 7. 3. 1 post ictal headache 8. Headache attributed to substance or its withdrawl 8. 1 Medication overuse headache 9. Headache attributed to infection 9. 1 Headache attributed to bacterial meningitis 10. Headache attributed to disorder of homeostasis 10. 1 Headache attributed to hypoxia or hypercapnia 10. 2 Headache attributed to dialysis headache 10. 3 Headache attributed to fasting
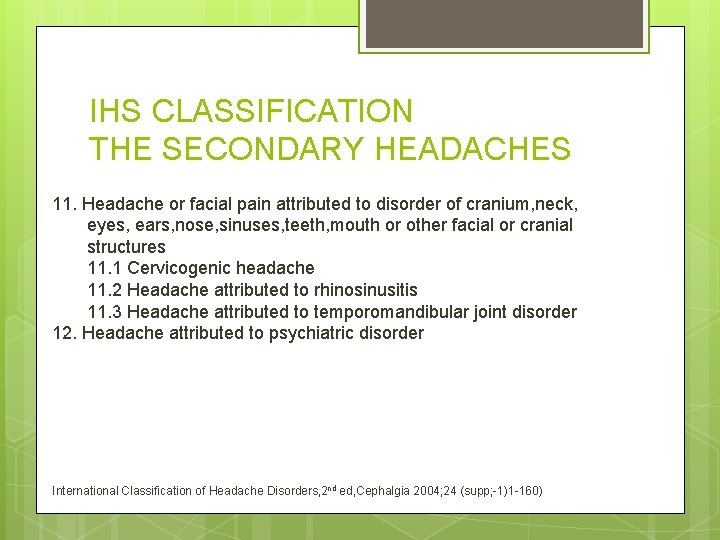
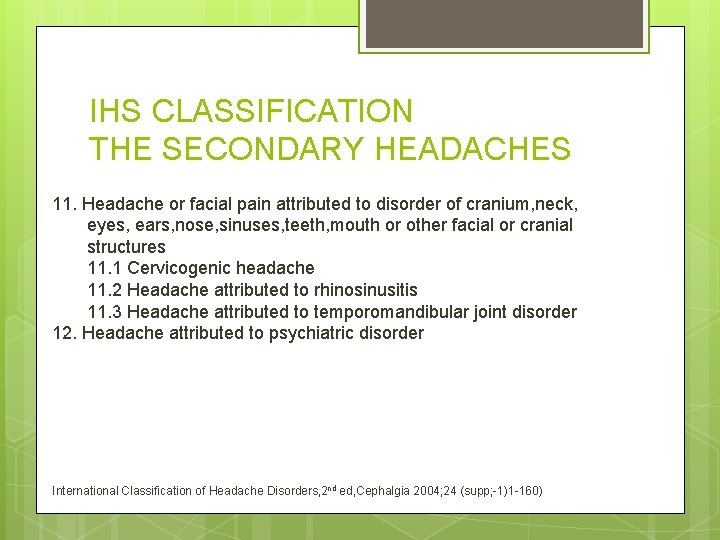
IHS CLASSIFICATION THE SECONDARY HEADACHES 11. Headache or facial pain attributed to disorder of cranium, neck, eyes, ears, nose, sinuses, teeth, mouth or other facial or cranial structures 11. 1 Cervicogenic headache 11. 2 Headache attributed to rhinosinusitis 11. 3 Headache attributed to temporomandibular joint disorder 12. Headache attributed to psychiatric disorder International Classification of Headache Disorders, 2 nd ed, Cephalgia 2004; 24 (supp; -1)1 -160)
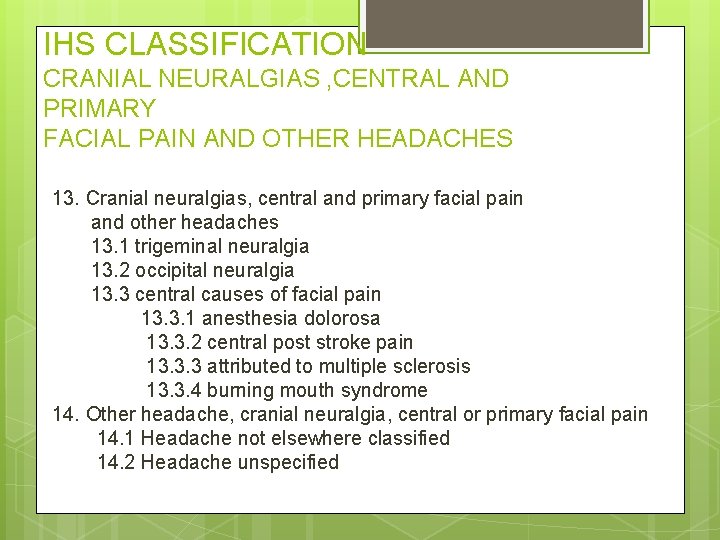
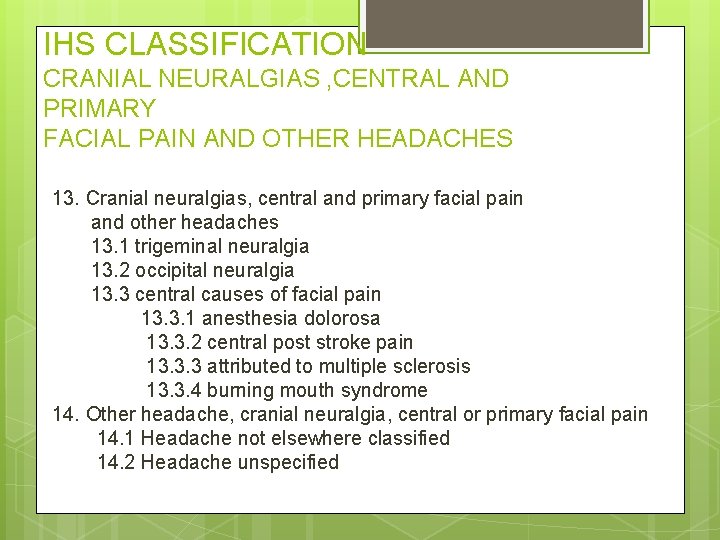
IHS CLASSIFICATION CRANIAL NEURALGIAS , CENTRAL AND PRIMARY FACIAL PAIN AND OTHER HEADACHES 13. Cranial neuralgias, central and primary facial pain and other headaches 13. 1 trigeminal neuralgia 13. 2 occipital neuralgia 13. 3 central causes of facial pain 13. 3. 1 anesthesia dolorosa 13. 3. 2 central post stroke pain 13. 3. 3 attributed to multiple sclerosis 13. 3. 4 burning mouth syndrome 14. Other headache, cranial neuralgia, central or primary facial pain 14. 1 Headache not elsewhere classified 14. 2 Headache unspecified
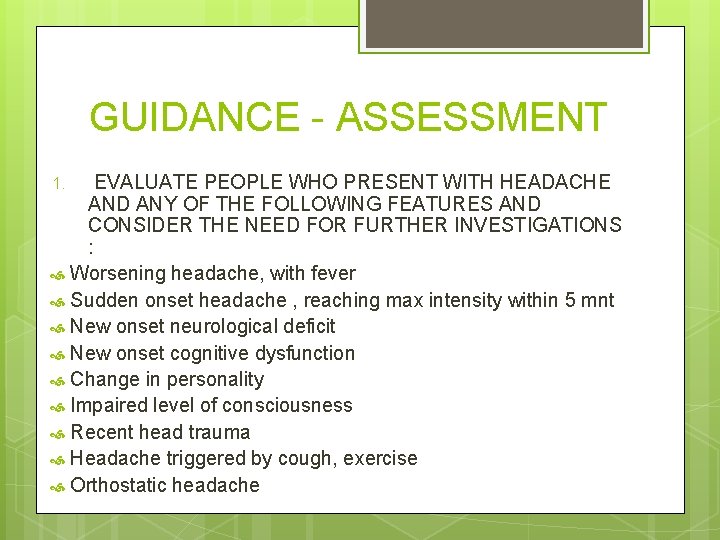
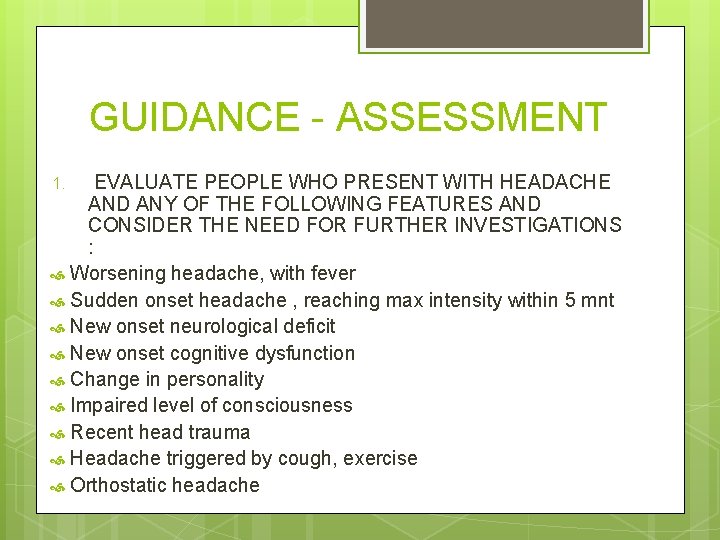
GUIDANCE - ASSESSMENT EVALUATE PEOPLE WHO PRESENT WITH HEADACHE AND ANY OF THE FOLLOWING FEATURES AND CONSIDER THE NEED FOR FURTHER INVESTIGATIONS : Worsening headache, with fever Sudden onset headache , reaching max intensity within 5 mnt New onset neurological deficit New onset cognitive dysfunction Change in personality Impaired level of consciousness Recent head trauma Headache triggered by cough, exercise Orthostatic headache 1.
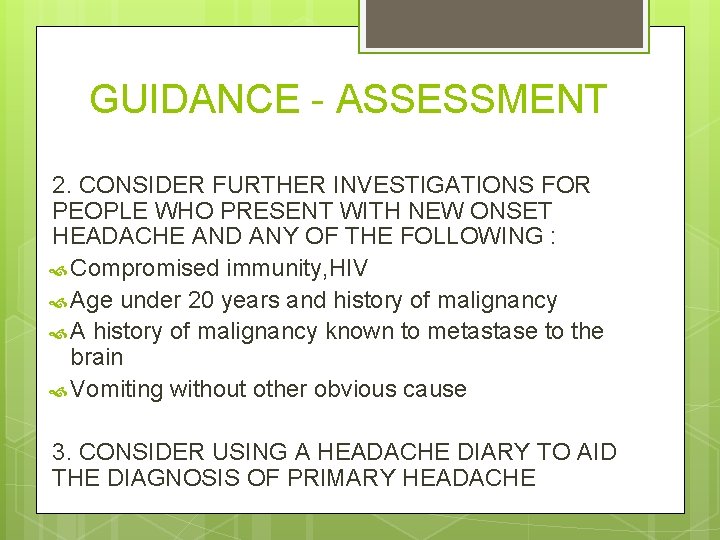
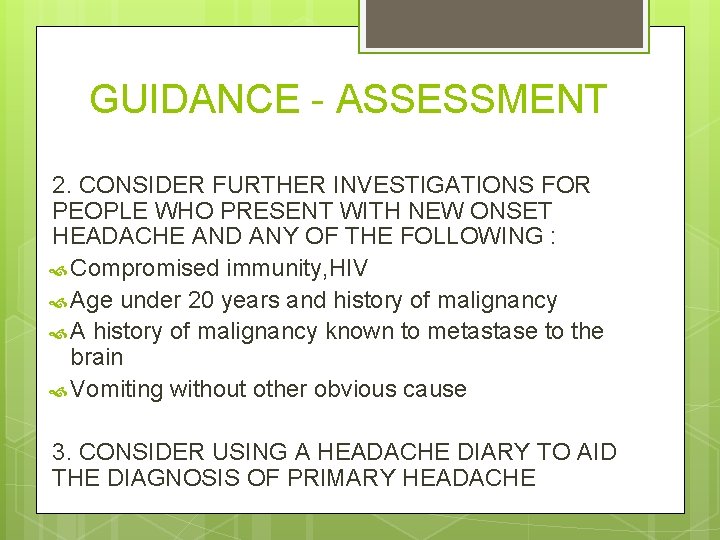
GUIDANCE - ASSESSMENT 2. CONSIDER FURTHER INVESTIGATIONS FOR PEOPLE WHO PRESENT WITH NEW ONSET HEADACHE AND ANY OF THE FOLLOWING : Compromised immunity, HIV Age under 20 years and history of malignancy A history of malignancy known to metastase to the brain Vomiting without other obvious cause 3. CONSIDER USING A HEADACHE DIARY TO AID THE DIAGNOSIS OF PRIMARY HEADACHE
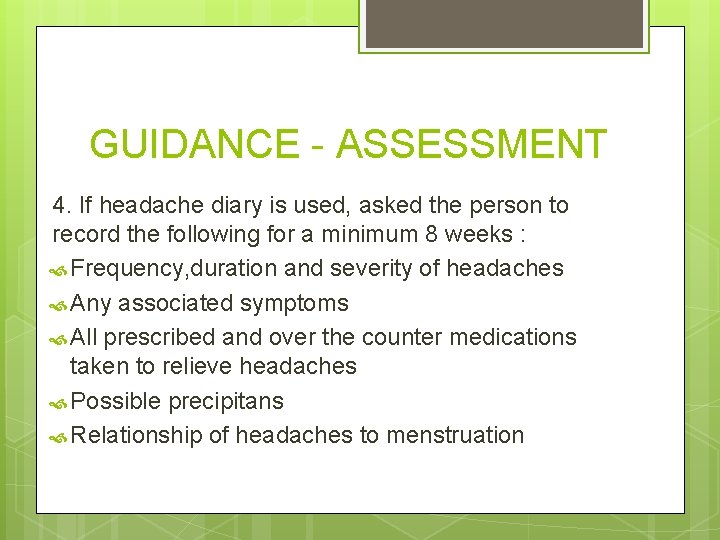
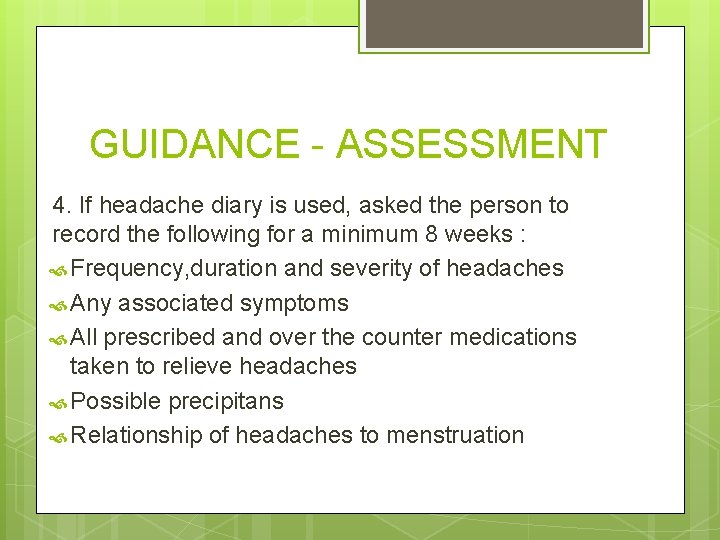
GUIDANCE - ASSESSMENT 4. If headache diary is used, asked the person to record the following for a minimum 8 weeks : Frequency, duration and severity of headaches Any associated symptoms All prescribed and over the counter medications taken to relieve headaches Possible precipitans Relationship of headaches to menstruation
Secondary headaches 19
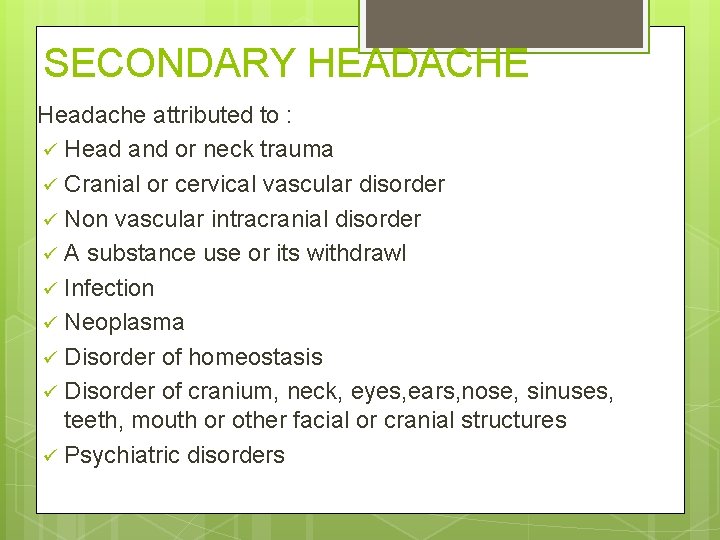
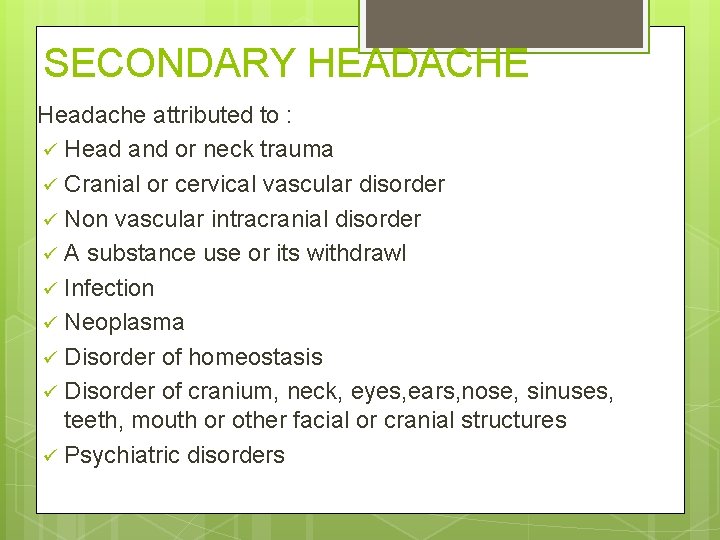
SECONDARY HEADACHE Headache attributed to : ü Head and or neck trauma ü Cranial or cervical vascular disorder ü Non vascular intracranial disorder ü A substance use or its withdrawl ü Infection ü Neoplasma ü Disorder of homeostasis ü Disorder of cranium, neck, eyes, ears, nose, sinuses, teeth, mouth or other facial or cranial structures ü Psychiatric disorders
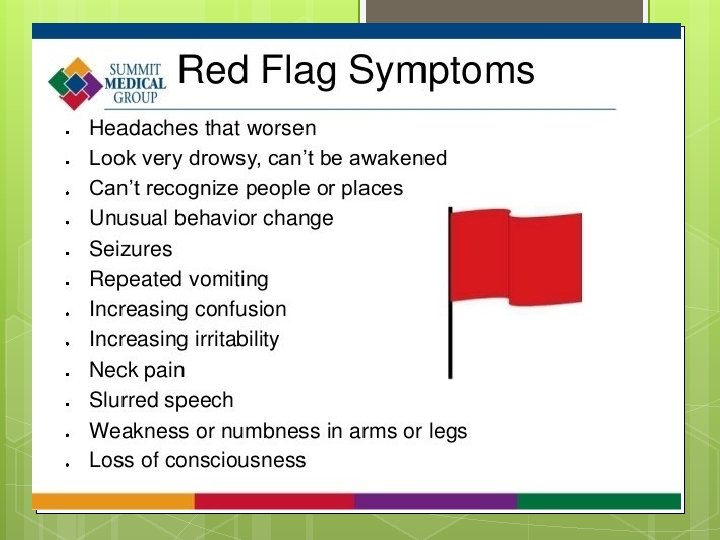
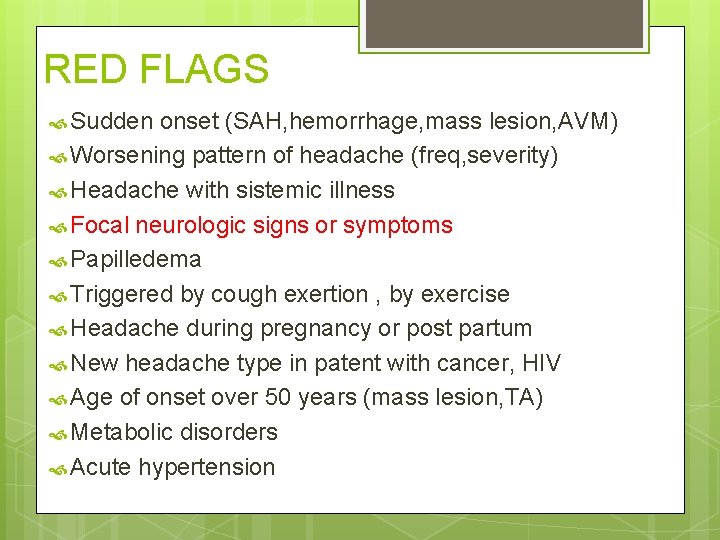
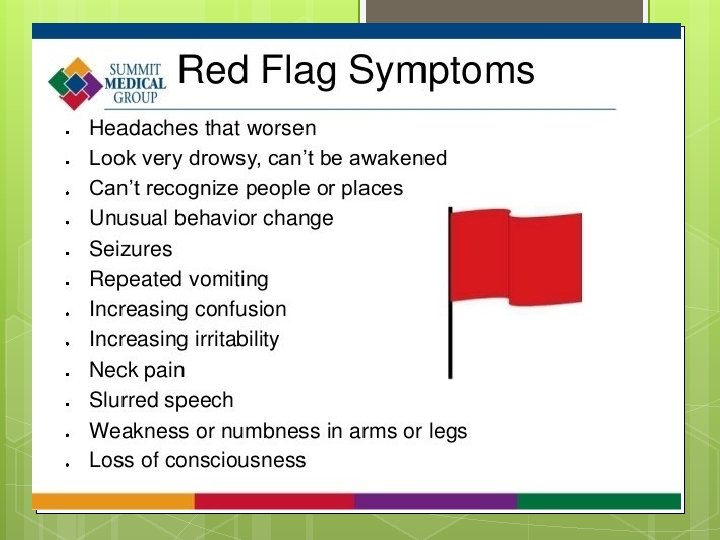
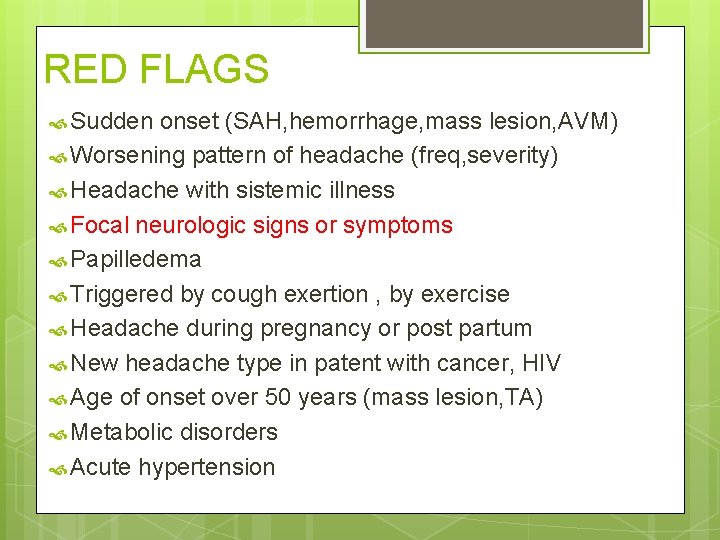
RED FLAGS Sudden onset (SAH, hemorrhage, mass lesion, AVM) Worsening pattern of headache (freq, severity) Headache with sistemic illness Focal neurologic signs or symptoms Papilledema Triggered by cough exertion , by exercise Headache during pregnancy or post partum New headache type in patent with cancer, HIV Age of onset over 50 years (mass lesion, TA) Metabolic disorders Acute hypertension
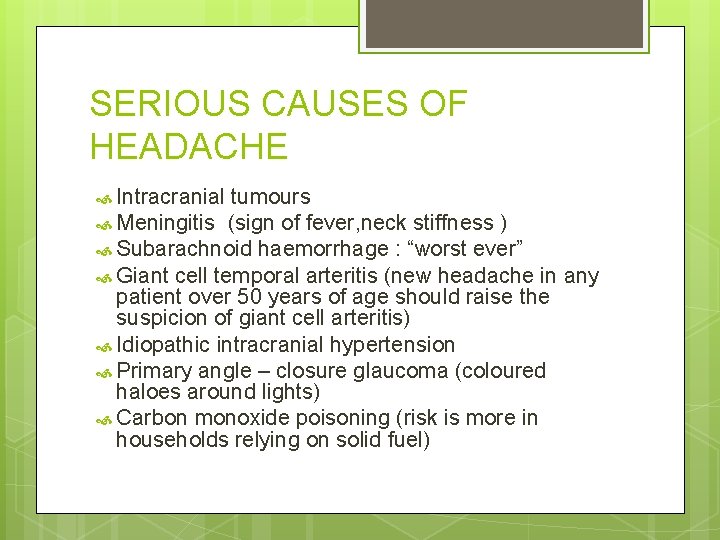
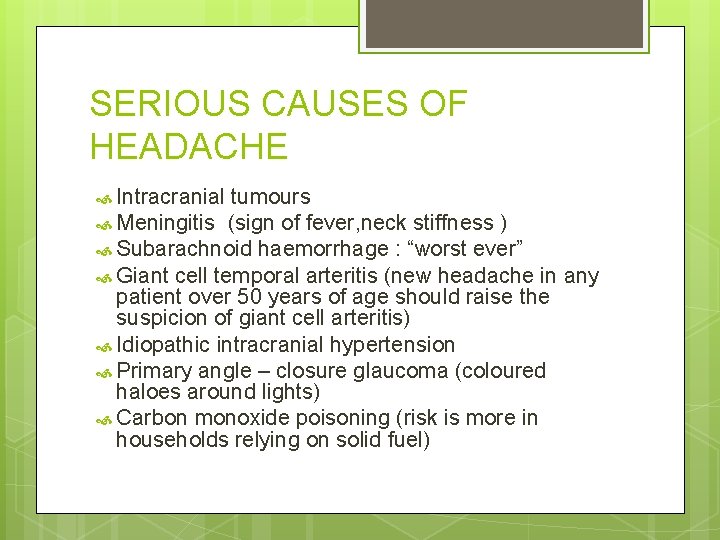
SERIOUS CAUSES OF HEADACHE Intracranial tumours Meningitis (sign of fever, neck stiffness ) Subarachnoid haemorrhage : “worst ever” Giant cell temporal arteritis (new headache in any patient over 50 years of age should raise the suspicion of giant cell arteritis) Idiopathic intracranial hypertension Primary angle – closure glaucoma (coloured haloes around lights) Carbon monoxide poisoning (risk is more in households relying on solid fuel)
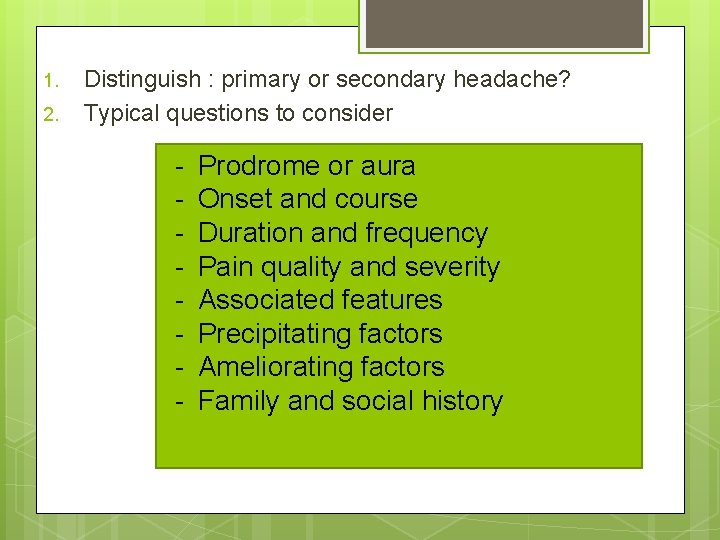
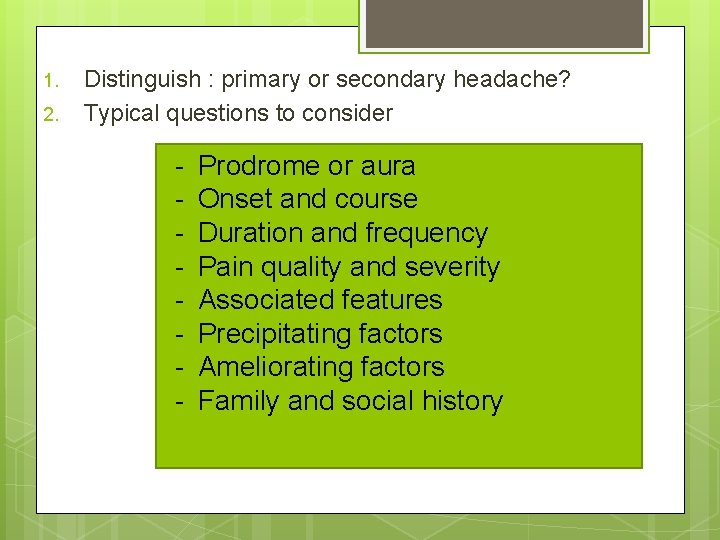
1. 2. Distinguish : primary or secondary headache? Typical questions to consider - Prodrome or aura Onset and course Duration and frequency Pain quality and severity Associated features Precipitating factors Ameliorating factors Family and social history
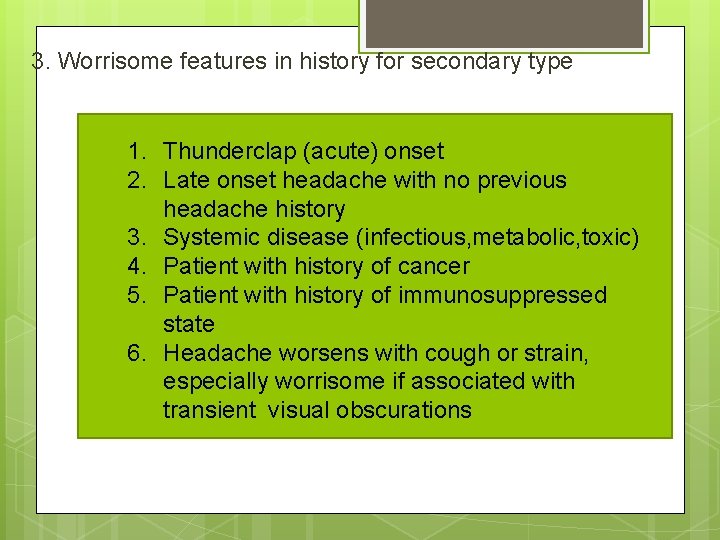
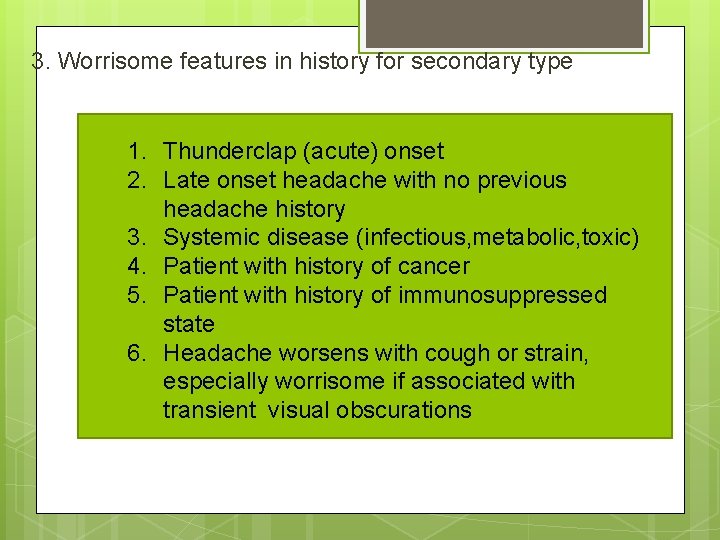
3. Worrisome features in history for secondary type 1. Thunderclap (acute) onset 2. Late onset headache with no previous headache history 3. Systemic disease (infectious, metabolic, toxic) 4. Patient with history of cancer 5. Patient with history of immunosuppressed state 6. Headache worsens with cough or strain, especially worrisome if associated with transient visual obscurations
PHYSICAL EXAMINATION
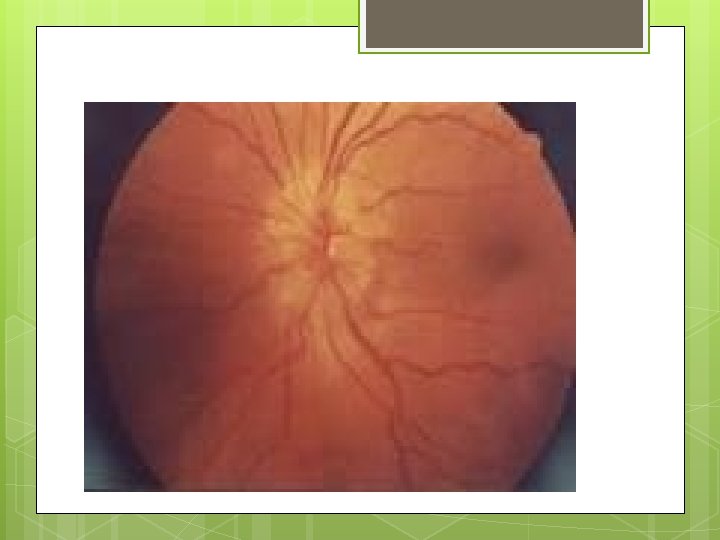
a. b. Aimed at distinguishing between primary and secondary types of headache Worrisome features in physical examination suggesting a secondary type 1. Focal neurologic deficits 2. Papilledema
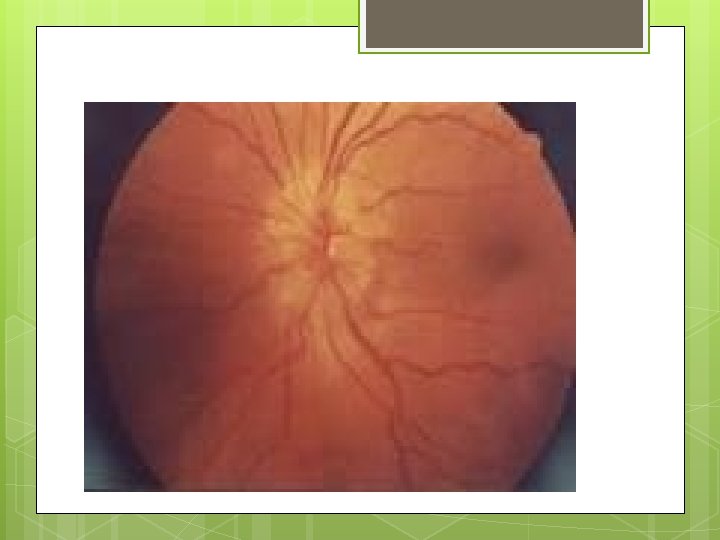
Papilledema
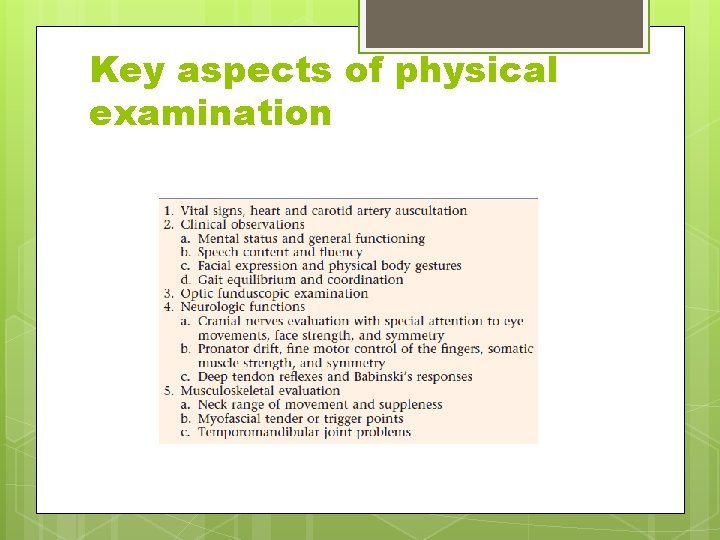
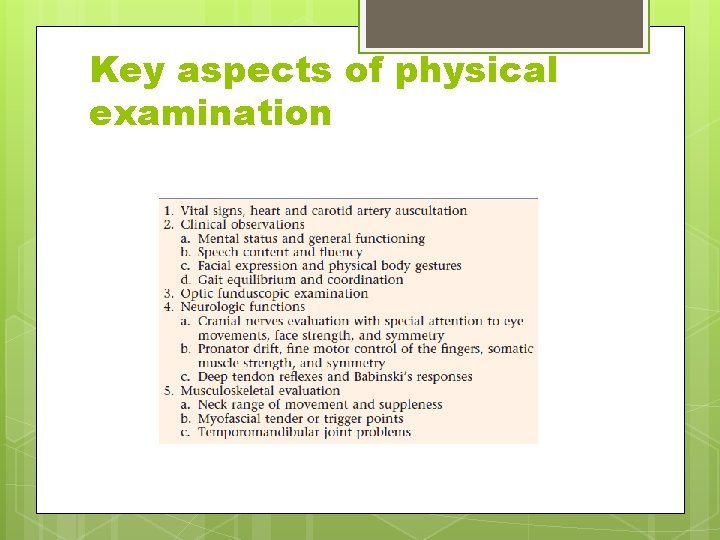
Key aspects of physical examination
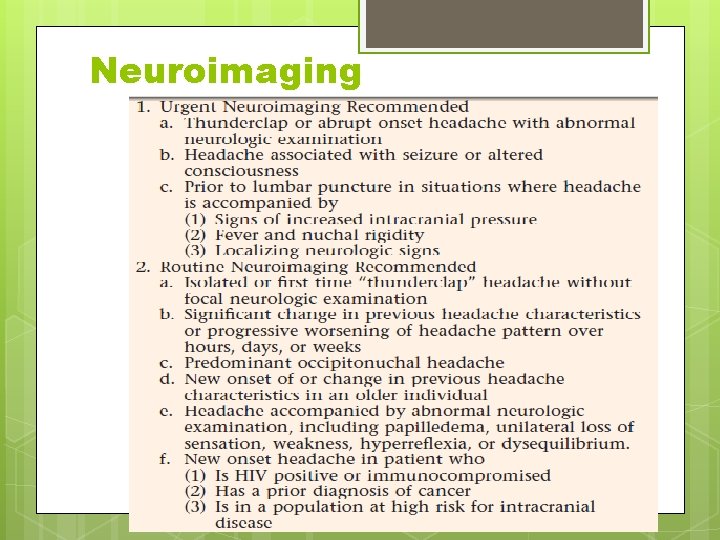
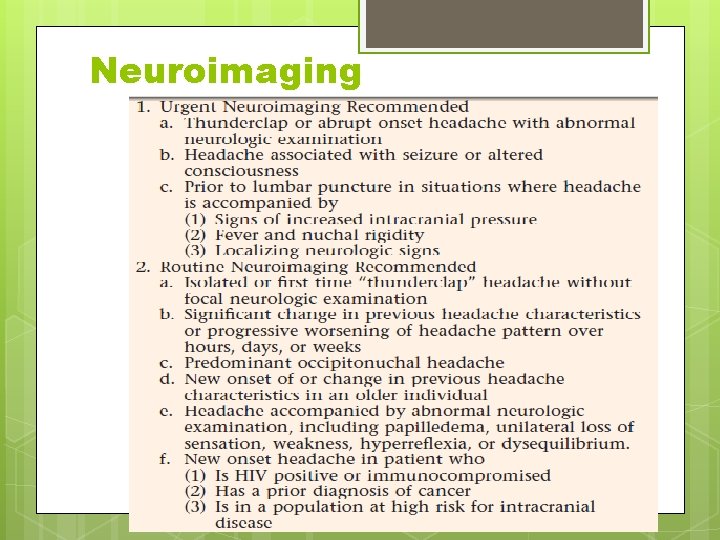
Neuroimaging
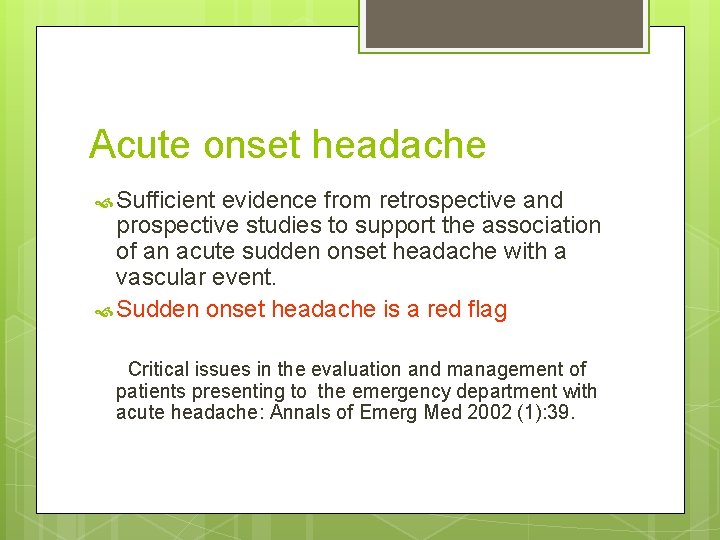
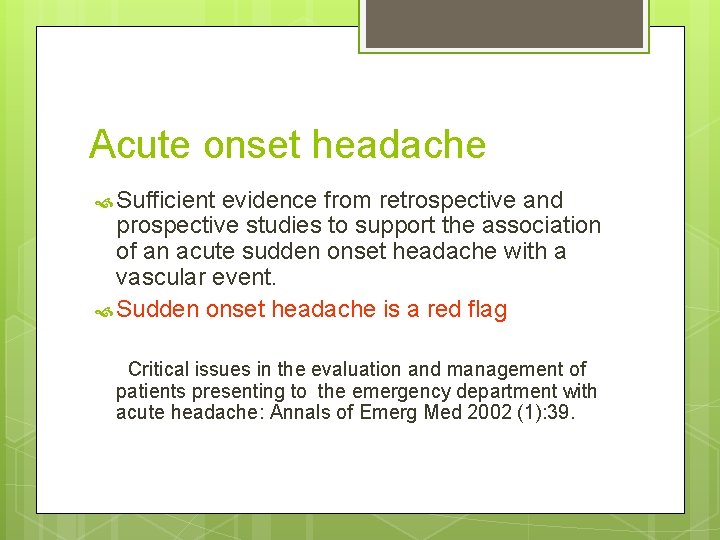
Acute onset headache Sufficient evidence from retrospective and prospective studies to support the association of an acute sudden onset headache with a vascular event. Sudden onset headache is a red flag Critical issues in the evaluation and management of patients presenting to the emergency department with acute headache: Annals of Emerg Med 2002 (1): 39.
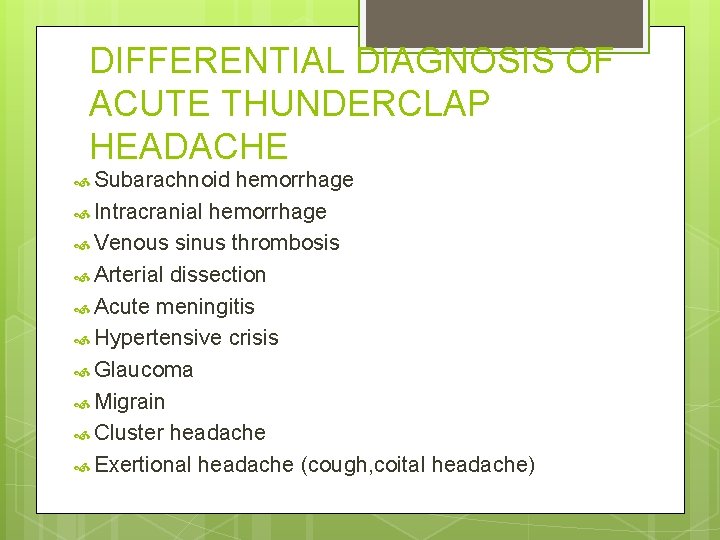
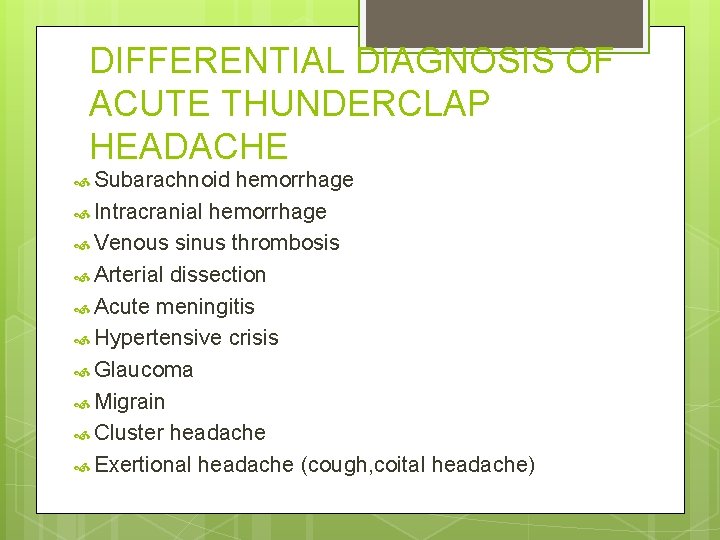
DIFFERENTIAL DIAGNOSIS OF ACUTE THUNDERCLAP HEADACHE Subarachnoid hemorrhage Intracranial hemorrhage Venous sinus thrombosis Arterial dissection Acute meningitis Hypertensive crisis Glaucoma Migrain Cluster headache Exertional headache (cough, coital headache)
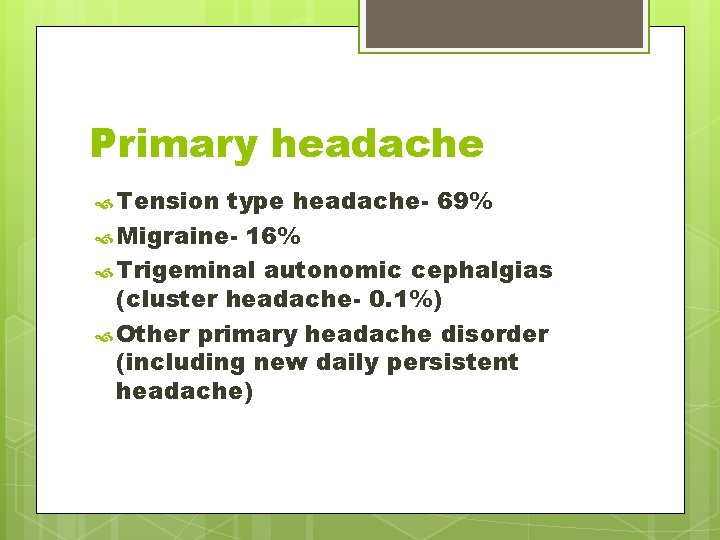
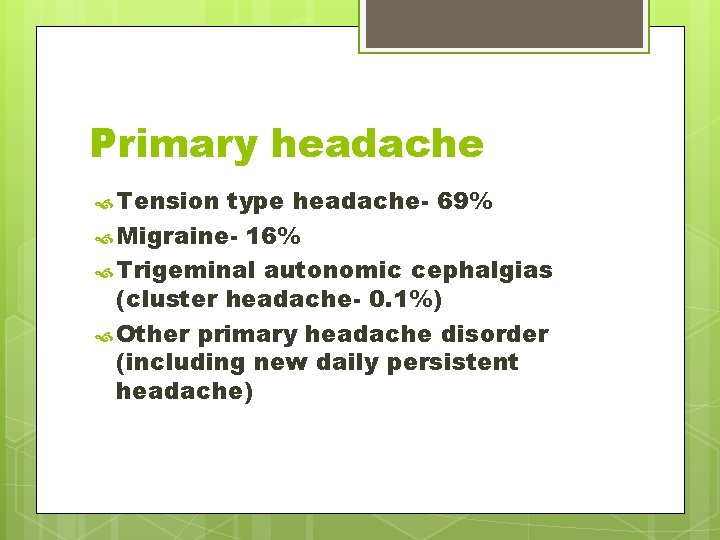
Primary headache Tension type headache- 69% Migraine- 16% Trigeminal autonomic cephalgias (cluster headache- 0. 1%) Other primary headache disorder (including new daily persistent headache)
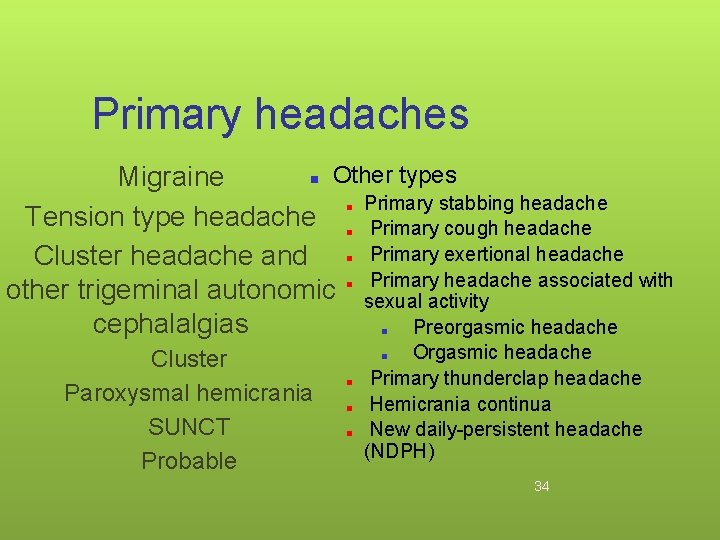
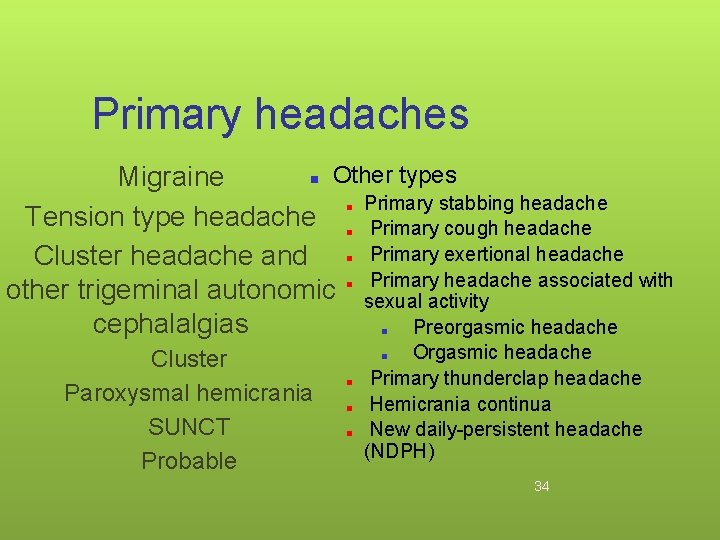
Primary headaches ■ Other types Migraine ■ Primary stabbing headache Tension type headache ■ Primary cough headache Cluster headache and ■ Primary exertional headache Primary headache associated with other trigeminal autonomic ■ sexual activity cephalalgias Preorgasmic headache ■ Cluster Paroxysmal hemicrania SUNCT Probable Orgasmic headache Primary thunderclap headache Hemicrania continua New daily-persistent headache (NDPH) ■ ■ 34
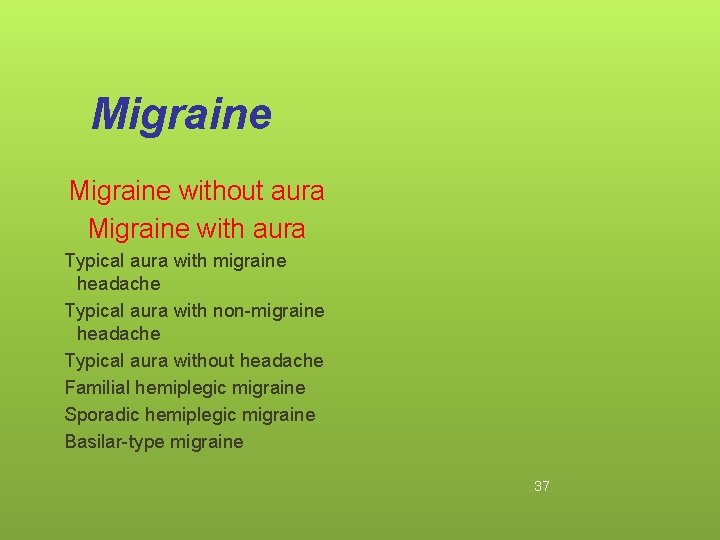
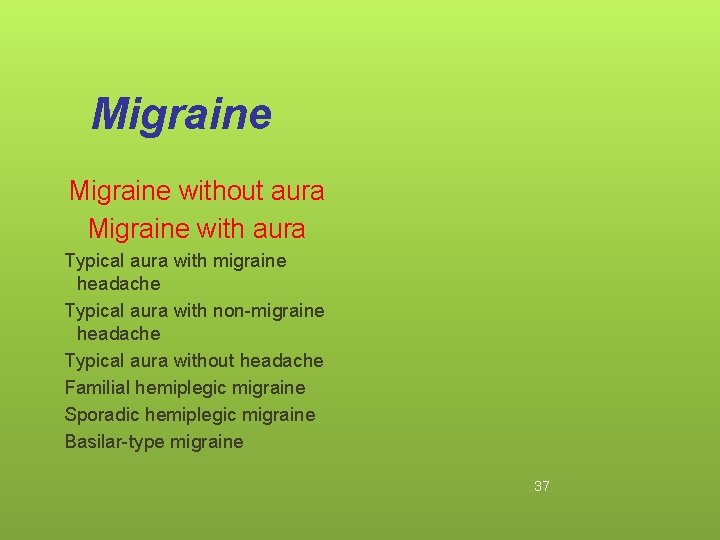
Migraine without aura Migraine with aura Typical aura with migraine headache Typical aura with non-migraine headache Typical aura without headache Familial hemiplegic migraine Sporadic hemiplegic migraine Basilar-type migraine 37
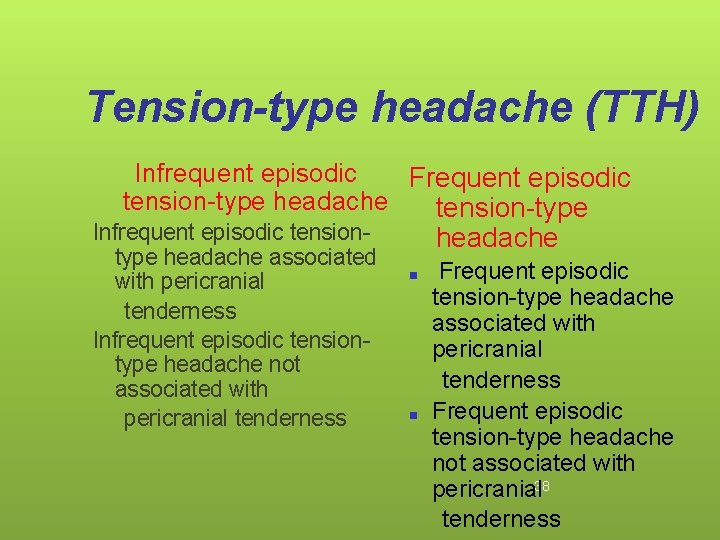
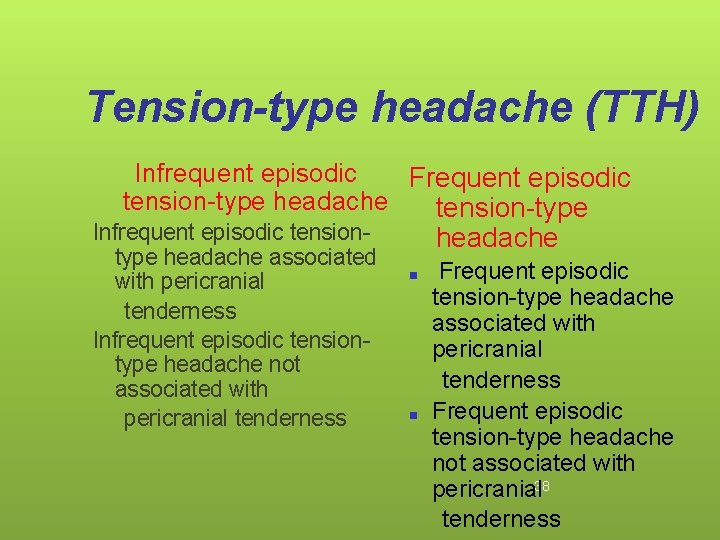
Tension-type headache (TTH) Infrequent episodic Frequent episodic tension-type headache tension-type Infrequent episodic tensiontype headache associated with pericranial tenderness Infrequent episodic tensiontype headache not associated with pericranial tenderness headache ■ ■ Frequent episodic tension-type headache associated with pericranial tenderness Frequent episodic tension-type headache not associated with pericranial 38 tenderness
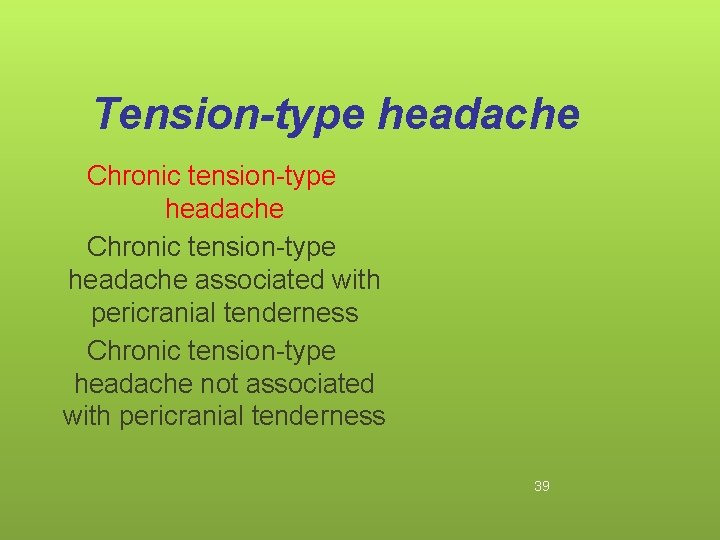
Tension-type headache Chronic tension-type headache associated with pericranial tenderness Chronic tension-type headache not associated with pericranial tenderness 39
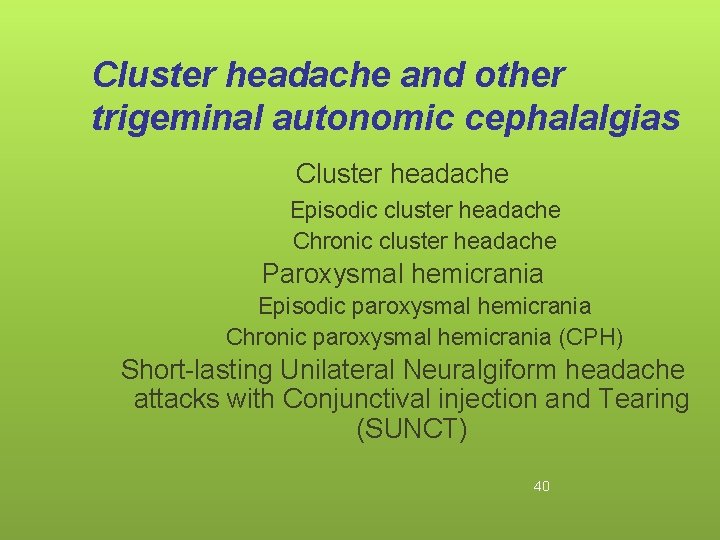
Cluster headache and other trigeminal autonomic cephalalgias Cluster headache Episodic cluster headache Chronic cluster headache Paroxysmal hemicrania Episodic paroxysmal hemicrania Chronic paroxysmal hemicrania (CPH) Short-lasting Unilateral Neuralgiform headache attacks with Conjunctival injection and Tearing (SUNCT) 40
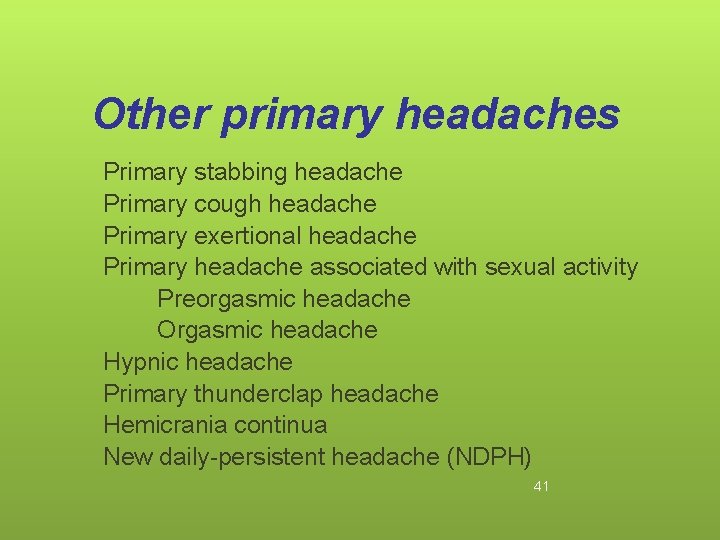
Other primary headaches Primary stabbing headache Primary cough headache Primary exertional headache Primary headache associated with sexual activity Preorgasmic headache Orgasmic headache Hypnic headache Primary thunderclap headache Hemicrania continua New daily-persistent headache (NDPH) 41
Migraine 42
Phases of Migraine • Prodrome-1 -24 hrs prior to onset • Aura-0 -60 min prior to or with pain onset. • Visual, Sensory, Speech • Headache-4 -72 hrs • Specific characteristics, Associated symp. • Postdrome- post pain symptoms which last for hrs to days 43
Triggers § Hormonal § Menstruation, ovulation, OCP, hormonal replacement § Dietary triggers § Alcohol, nitrite–laden meat, monosodium glutamate, aspartame, choclate, aged cheese, missing a meal, red wine 44
Triggers § Psychologic triggers § Stress, period after stress(weekend or vacation), anxiety, worry, depression § Sleep related triggers § Lack of or excessive sleep § Physical or environmental triggers § Glare, flashing lights, visual stimulation, fluorescent light, odours, weather changes, high altitude, change in posture, physical exertion 45
Triggers • Drugs • Nitroglycerine, histamine, reserpine, hydralazine, ranitidine, estrogen • Miscellaneous • Head trauma, physical exertion, fatigue • Trigger zones 46
Triggers Trigger factors increase the probability of a migraine attack in the short term (usually <48 hours) in a person with migraine 47
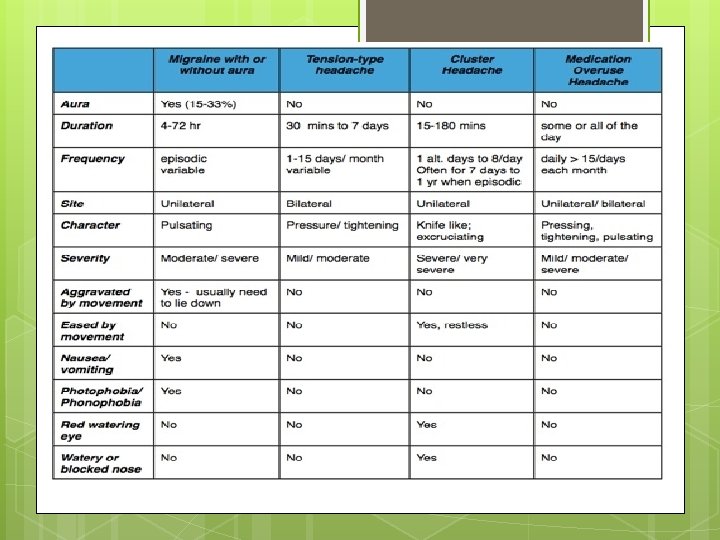
Migraine without aura § Common migraine, hemicrania simplex § Recurrent headache disorder manifesting in attacks lasting 4– 72 hours. § Typical characteristics are unilateral location(60%), pulsating quality, moderate or severe intensity, aggravation by routine physical activity and association with nausea and/or photophobia and phonophobia. § Commonest subtype, has a higher average attack frequency and is usually more disabling than Migraine with aura 48
Migraine without aura Diagnostic criteria: A. At least 5 attacks fulfilling criteria B–D B. Headache attacks lasting 4– 72 hours (untreated or unsuccessfully treated) C. Headache has at least two of the following: unilateral location pulsating quality moderate or severe pain intensity aggravation by or causing avoidance of routine physical activity (eg, walking or climbing stairs) 49
Migraine without aura D. During headache at least one of the following: 1. nausea and/or vomiting 2. photophobia and phonophobia E. Not attributed to another disorder 50
Migraine without aura • Migraine headache is usually frontotemporal. Occipital headache in children, whether unilateral or bilateral, is rare and calls for diagnostic caution; may be structural • Pulsating means throbbing or varying with the heartbeat. • In young children, photophobia and phonophobia may be inferred from their behaviour. • Migraine without aura often has a strict menstrual relationship. 51
Migraine with aura • Classic or classical migraine, ophthalmic, hemiparaesthetic, hemiplegic migrain • Recurrent disorder manifesting in attacks of reversible focal neurological symptoms that usually develop gradually over 5– 20 minutes and last for less than 60 minutes. 52
Migraine with aura • The aura is the complex of neurological symptoms that occurs just before or at the onset of migraine headache • Premonitory symptoms occur hours to a day or two before a migraine attack (with or without aura). They include various combinations of fatigue, difficulty in concentrating, neck stiffness, sensitivity to light or sound, nausea, blurred vision, yawning and pallor. 53
Migraine with aura • • • Typical aura with migraine headache Typical aura with non-migraine headache Typical aura without headache Familial hemiplegic migraine (FHM) Sporadic hemiplegic migraine Basilar-type migraine 54
Migraine with aura Diagnostic criteria: A. At least 2 attacks fulfilling criterion B B. Migraine aura fulfilling criteria B and C for one of the subforms C. Not attributed to another disorder 55
Typical aura with migraine headache Diagnostic criteria: A. At least 2 attacks fulfilling criteria B–D B. Aura consisting of at least one of the following, but no motor weakness: 1. fully reversible visual symptoms including positive features (eg, flickering lights, spots or lines) and/or negative features (loss of vision) 2. fully reversible sensory symptoms including positive features (pins and needles) and/or negative features (numbness) 3. fully reversible dysphasic speech disturbance 56
Typical aura with migraine headache C. At least two of the following: • homonymous visual symptoms and/or unilateral sensory symptoms • at least one aura symptom develops gradually over ≥ 5 minutes and/or different aura symptoms occur in succession over ≥ 5 min • each symptom lasts ≥ 5 and < 60 minutes D. Headache fulfilling criteria B–D for Migraine without aura begins during the aura or follows aura within 60 minutes E. Not attributed to another disorder 57
Typical aura with migraine headache • Additional loss or blurring of central vision may occur. • Rare secondary mimics including carotid dissection, arteriovenous malformation and seizure. • Visual aura is the most common type of aura, often presenting as a fortification spectrum, scotoma • If the aura includes motor weakness- Familial hemiplegic migraine or Sporadic hemiplegic migraine. • Symptoms usually follow one another in succession beginning with visual, then sensory symptoms and dysphasia. 58
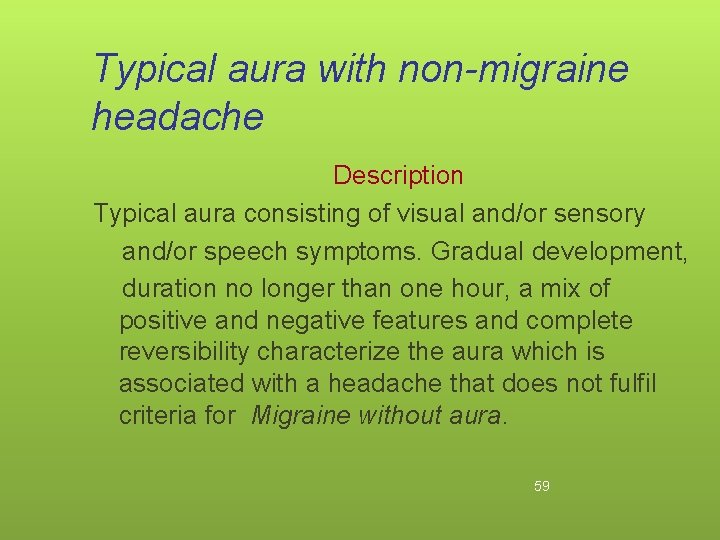
Typical aura with non-migraine headache Description Typical aura consisting of visual and/or sensory and/or speech symptoms. Gradual development, duration no longer than one hour, a mix of positive and negative features and complete reversibility characterize the aura which is associated with a headache that does not fulfil criteria for Migraine without aura. 59
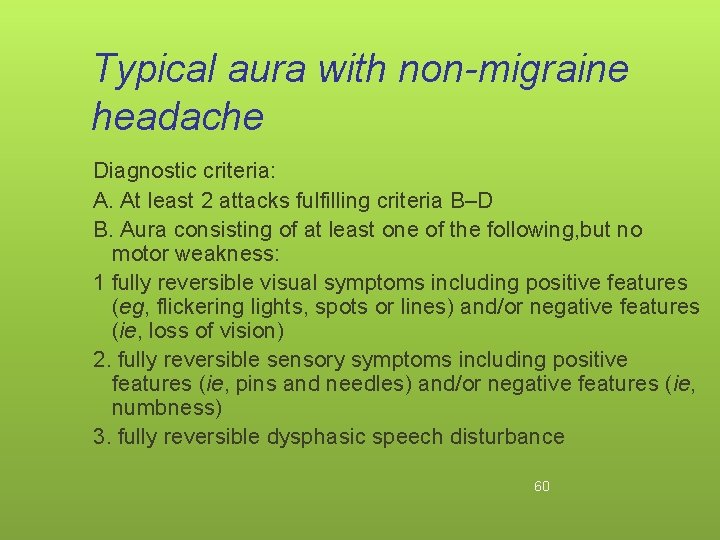
Typical aura with non-migraine headache Diagnostic criteria: A. At least 2 attacks fulfilling criteria B–D B. Aura consisting of at least one of the following, but no motor weakness: 1 fully reversible visual symptoms including positive features (eg, flickering lights, spots or lines) and/or negative features (ie, loss of vision) 2. fully reversible sensory symptoms including positive features (ie, pins and needles) and/or negative features (ie, numbness) 3. fully reversible dysphasic speech disturbance 60
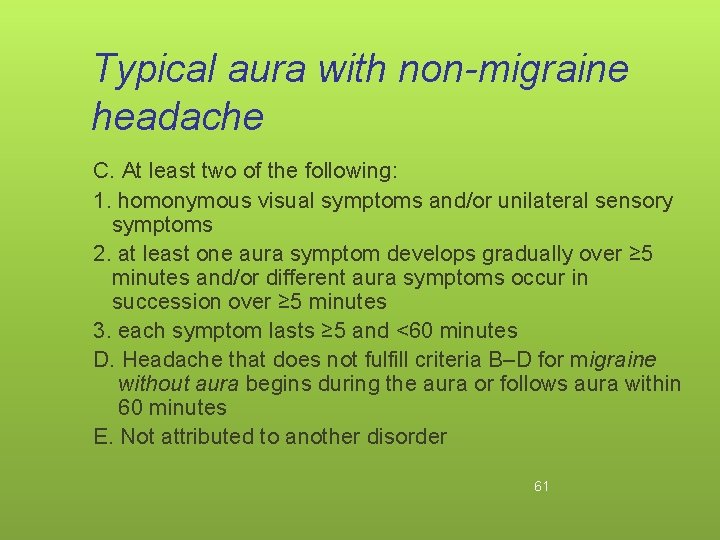
Typical aura with non-migraine headache C. At least two of the following: 1. homonymous visual symptoms and/or unilateral sensory symptoms 2. at least one aura symptom develops gradually over ≥ 5 minutes and/or different aura symptoms occur in succession over ≥ 5 minutes 3. each symptom lasts ≥ 5 and <60 minutes D. Headache that does not fulfill criteria B–D for migraine without aura begins during the aura or follows aura within 60 minutes E. Not attributed to another disorder 61
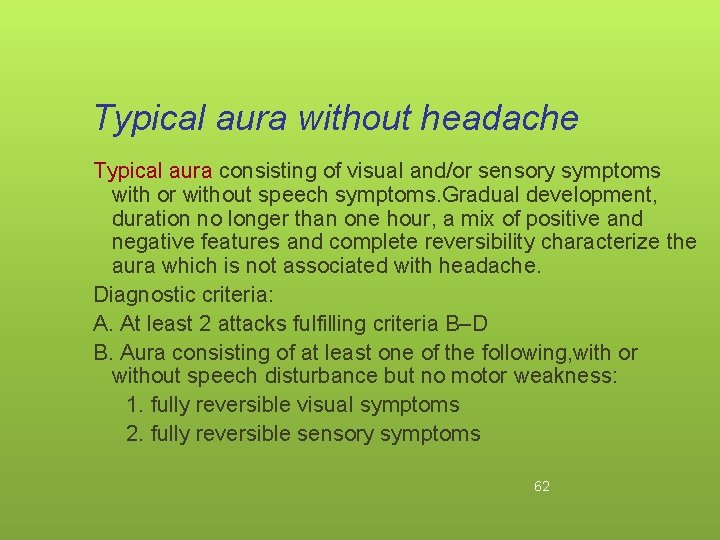
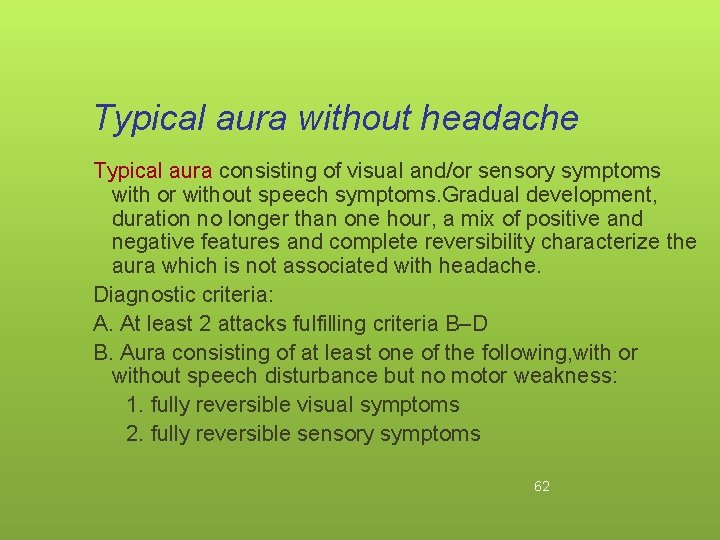
Typical aura without headache Typical aura consisting of visual and/or sensory symptoms with or without speech symptoms. Gradual development, duration no longer than one hour, a mix of positive and negative features and complete reversibility characterize the aura which is not associated with headache. Diagnostic criteria: A. At least 2 attacks fulfilling criteria B–D B. Aura consisting of at least one of the following, with or without speech disturbance but no motor weakness: 1. fully reversible visual symptoms 2. fully reversible sensory symptoms 62
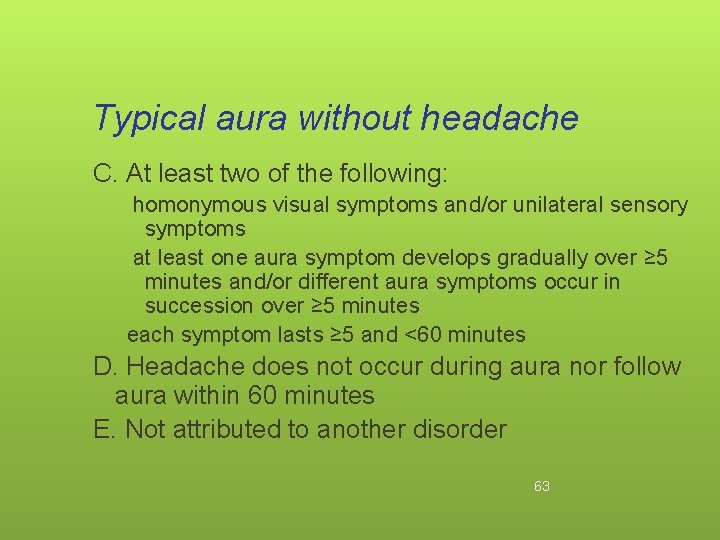
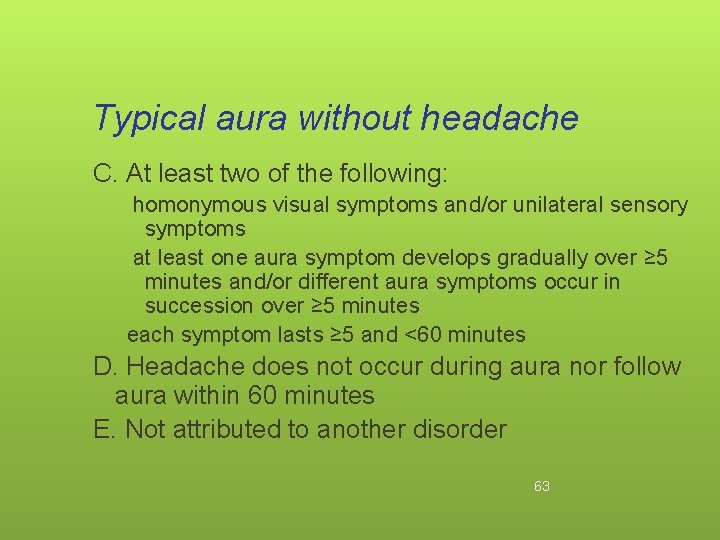
Typical aura without headache C. At least two of the following: homonymous visual symptoms and/or unilateral sensory symptoms at least one aura symptom develops gradually over ≥ 5 minutes and/or different aura symptoms occur in succession over ≥ 5 minutes each symptom lasts ≥ 5 and <60 minutes D. Headache does not occur during aura nor follow aura within 60 minutes E. Not attributed to another disorder 63
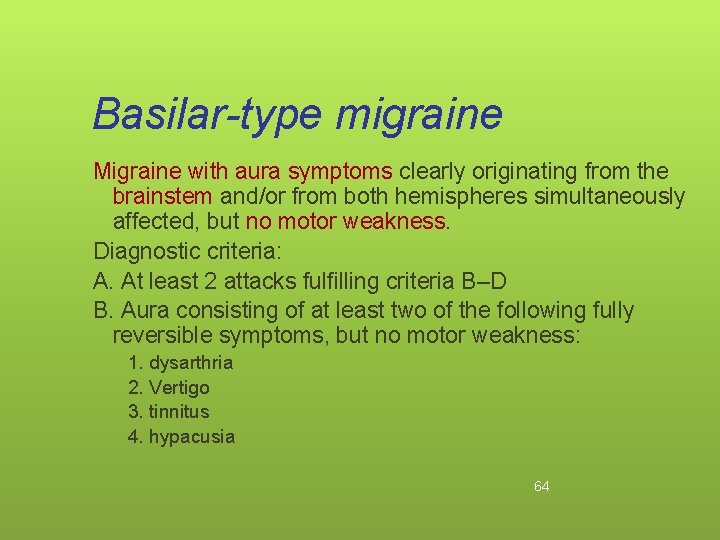
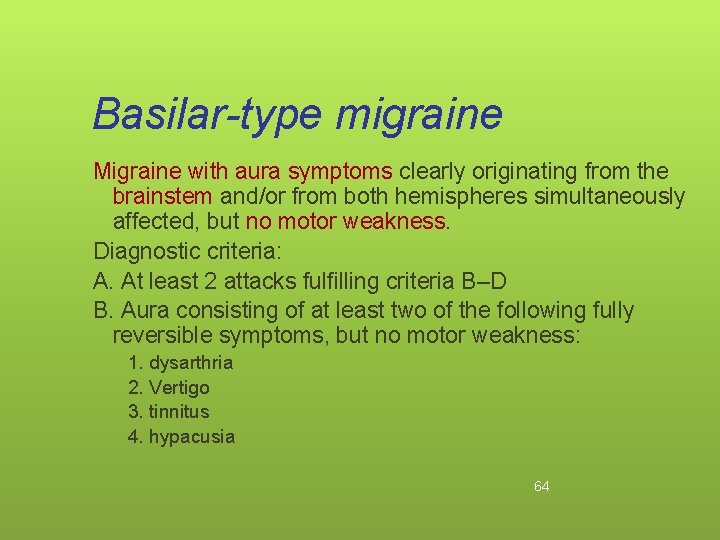
Basilar-type migraine Migraine with aura symptoms clearly originating from the brainstem and/or from both hemispheres simultaneously affected, but no motor weakness. Diagnostic criteria: A. At least 2 attacks fulfilling criteria B–D B. Aura consisting of at least two of the following fully reversible symptoms, but no motor weakness: 1. dysarthria 2. Vertigo 3. tinnitus 4. hypacusia 64
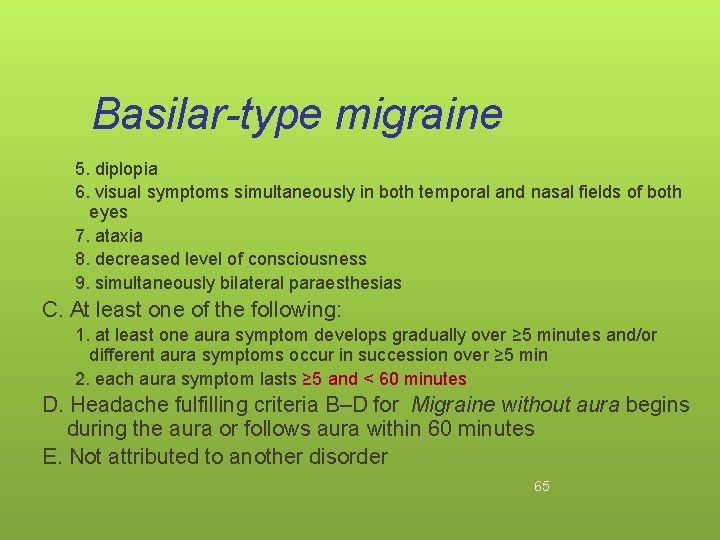
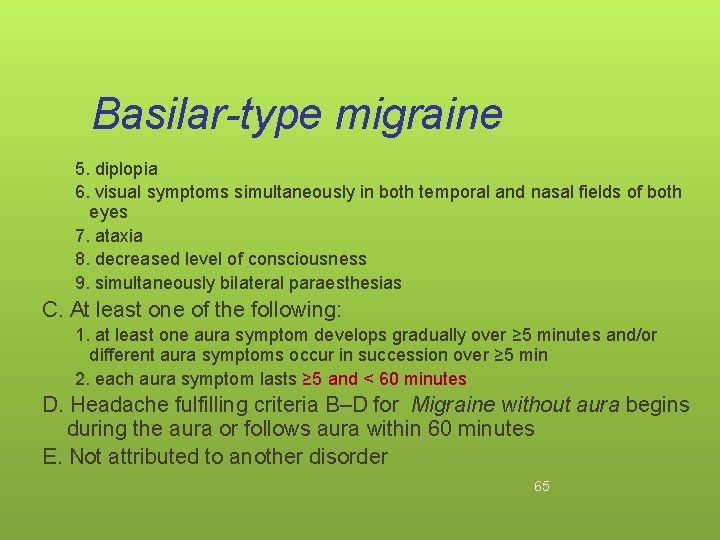
Basilar-type migraine 5. diplopia 6. visual symptoms simultaneously in both temporal and nasal fields of both eyes 7. ataxia 8. decreased level of consciousness 9. simultaneously bilateral paraesthesias C. At least one of the following: 1. at least one aura symptom develops gradually over ≥ 5 minutes and/or different aura symptoms occur in succession over ≥ 5 min 2. each aura symptom lasts ≥ 5 and < 60 minutes D. Headache fulfilling criteria B–D for Migraine without aura begins during the aura or follows aura within 60 minutes E. Not attributed to another disorder 65
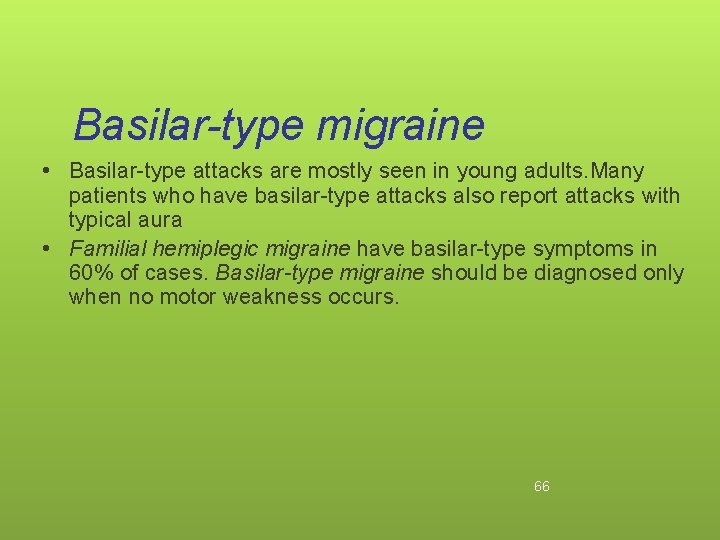
Basilar-type migraine • Basilar-type attacks are mostly seen in young adults. Many patients who have basilar-type attacks also report attacks with typical aura • Familial hemiplegic migraine have basilar-type symptoms in 60% of cases. Basilar-type migraine should be diagnosed only when no motor weakness occurs. 66
Complications of migraine • • • Chronic migraine Status migrainosus Persistent aura without infarction Migrainous infarction Migraine-triggered seizure 67
Migrainous infarction Description: One or more migrainous aura symptoms associated with an ischemic brain lesion in appropriate territory demonstrated by neuroimaging. Diagnostic criteria: A. The present attack in a patient with Migraine with aura is typical of previous attacks except that one or more aura symptoms persists for >60 minutes B. Neuroimaging demonstrates ischemic infarction in a relevant area C. Not attributed to another disorder 68
Migrainous infarction • Ischemic stroke in a migraine sufferer may be categorized as cerebral infarction of other cause coexisting with migraine, cerebral infarction of other cause presenting with symptoms resembling migraine with aura, or cerebral infarction occurring during the course of a typical migraine with aura attack. Only the last fulfils criteria for Migrainous infarction. • Increased risk for stroke in migraine patients has been demonstrated in women under age 45 in several studies. 69
Migraine-triggered seizure Description: A seizure triggered by a migraine aura. Diagnostic criteria: A. Migraine fulfilling criteria for Migraine with aura B. A seizure fulfilling diagnostic criteria for one type of epileptic attack occurs during or within 1 hour after a migraine aura Migraine and epilepsy are prototypical examples of paroxysmal brain disorders. While migraine-like headaches are quite frequently seen in the postictal period, sometimes a seizure occurs during or following a migraine attack. This phenomenon, sometimes referred to as migralepsy, has been described in patients with migraine with aura. 70
MIGRAIN WITH OR WITHOUT AURA TREATMENT ACUTE TREATMENT • Offer combination oral Triptan & NSAID, oral Triptan & paracetamol • For people who prefer to take only one drug, consider monotherapy with an oral Triptan, NSAID, aspirin (900 mg) or paracetamol • Do not offer ergots or opioids for the acute treatment of migraine • For people in whom oral preparation are not tolerated : offer a non oral preparation of metoclopramide or prochlorperazine, consider adding a non oral NSAID or triptan
MIGRAIN WITH OR WITHOUT AURA TREATMENT PROPHYLACTIC TREATMENT • Topiramate (associated with risk of fetal malformation & can impair the effectiveness of hormonal contraception) • Valproic acid • 10 session of acupuncture over 5 -8 weeks • Riboflavin (400 mg once a day) may be effective in reducing migraine frequency & intensity • Review the need for continuing migraine prophylaxis 6 monts after start
evidence ANTIDEPPRESSANTS : • Amitriptyline, venlafaxine for migrain prevention (Level B) • Divalproex sodium, sodium valproate, and topiramate are established as effective and should be offered for migrain prevention
Tension-type headache (TTH) • most common type of primary headache: • its lifetime prevalence in the general population ranges from 30 to 78% • Previously considered to be primarily psychogenic but now neurobiologic basis. Peripheral pain mechanisms are most likely to play a role in Infrequent & Frequent episodic tension type headache whereas central pain mechanisms play a more important role in Chronic tension-type headache. 74
Tension-type headache (TTH) Frequent episodic Infrequent episodic tension-type headache Infrequent episodic tensiontype headache associated with pericranial tenderness Infrequent episodic tensiontype headache not associated with pericranial tenderness ■ ■ Frequent episodic tension-type headache associated with pericranial tenderness Frequent episodic tension-type headache not associated with pericranial 75 tenderness
Tension-type headache Chronic tension-type headache associated with pericranial tenderness Chronic tension-type headache not associated with pericranial tenderness 76
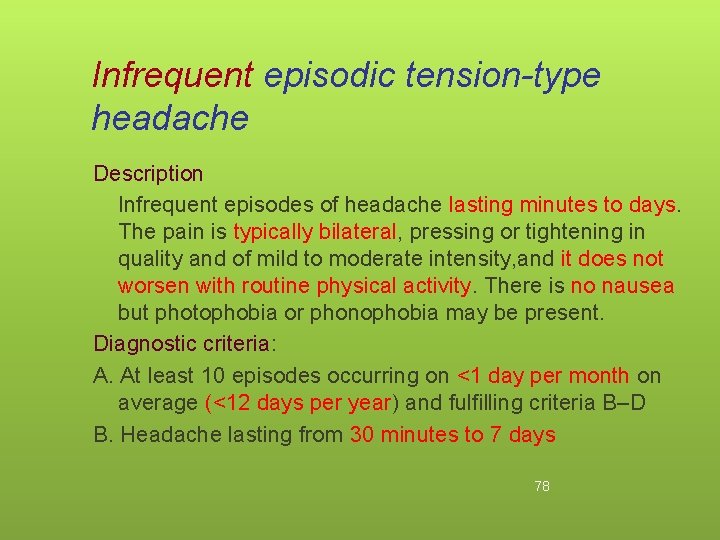
Infrequent episodic tension-type headache Description Infrequent episodes of headache lasting minutes to days. The pain is typically bilateral, pressing or tightening in quality and of mild to moderate intensity, and it does not worsen with routine physical activity. There is no nausea but photophobia or phonophobia may be present. Diagnostic criteria: A. At least 10 episodes occurring on <1 day per month on average (<12 days per year) and fulfilling criteria B–D B. Headache lasting from 30 minutes to 7 days 78
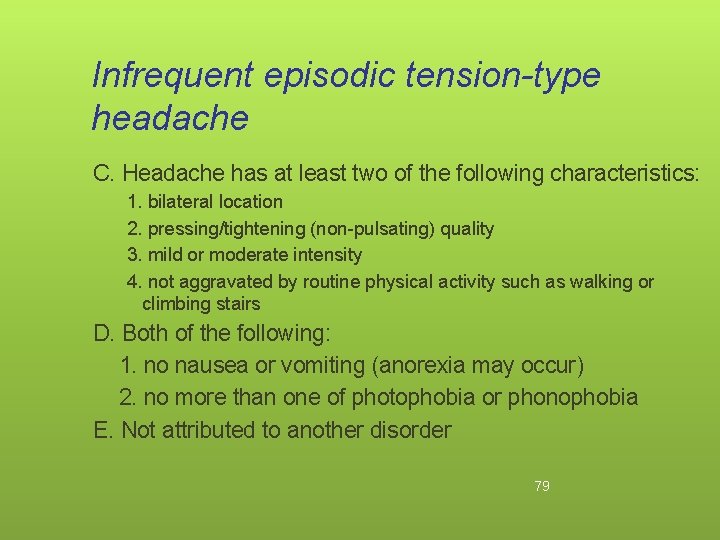
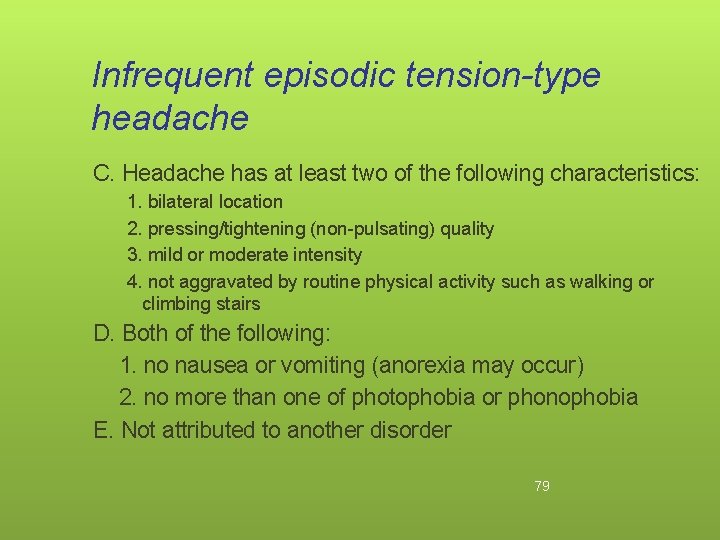
Infrequent episodic tension-type headache C. Headache has at least two of the following characteristics: 1. bilateral location 2. pressing/tightening (non-pulsating) quality 3. mild or moderate intensity 4. not aggravated by routine physical activity such as walking or climbing stairs D. Both of the following: 1. no nausea or vomiting (anorexia may occur) 2. no more than one of photophobia or phonophobia E. Not attributed to another disorder 79
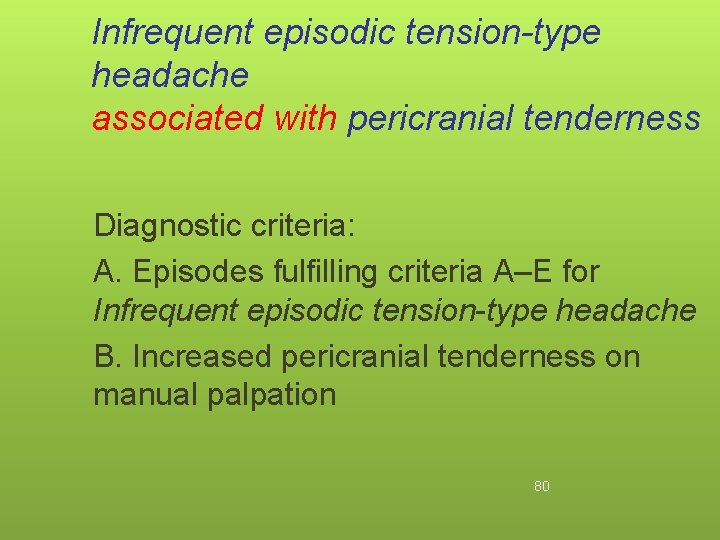
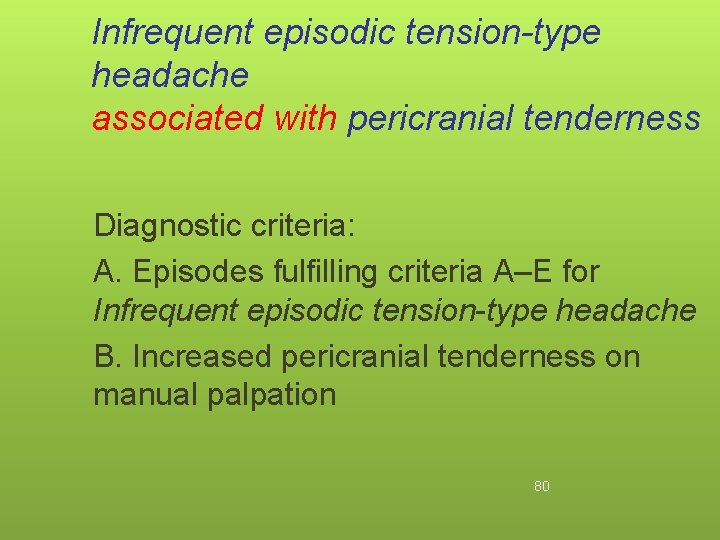
Infrequent episodic tension-type headache associated with pericranial tenderness Diagnostic criteria: A. Episodes fulfilling criteria A–E for Infrequent episodic tension-type headache B. Increased pericranial tenderness on manual palpation 80
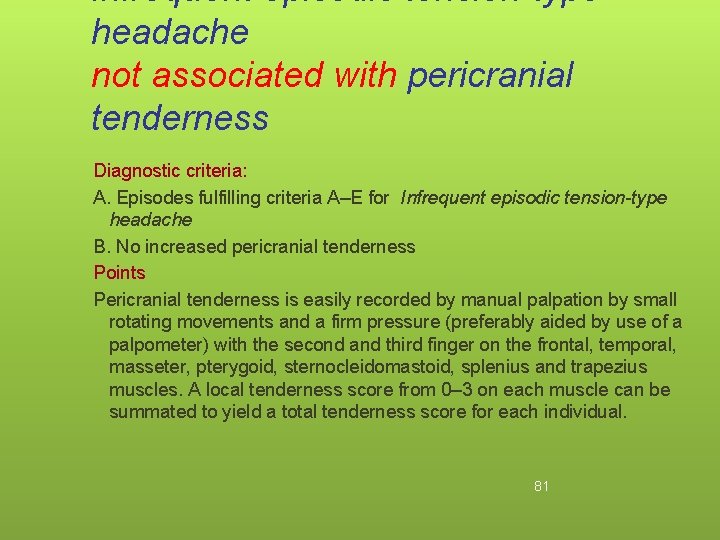
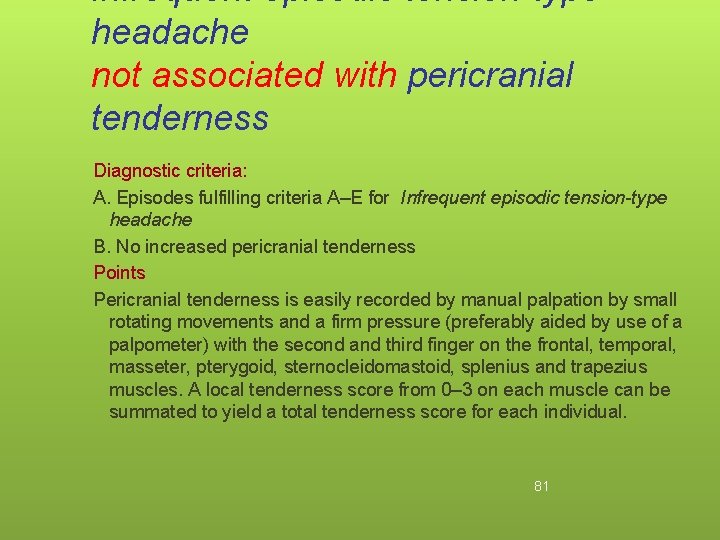
Infrequent episodic tension-type headache not associated with pericranial tenderness Diagnostic criteria: A. Episodes fulfilling criteria A–E for Infrequent episodic tension-type headache B. No increased pericranial tenderness Points Pericranial tenderness is easily recorded by manual palpation by small rotating movements and a firm pressure (preferably aided by use of a palpometer) with the second and third finger on the frontal, temporal, masseter, pterygoid, sternocleidomastoid, splenius and trapezius muscles. A local tenderness score from 0– 3 on each muscle can be summated to yield a total tenderness score for each individual. 81
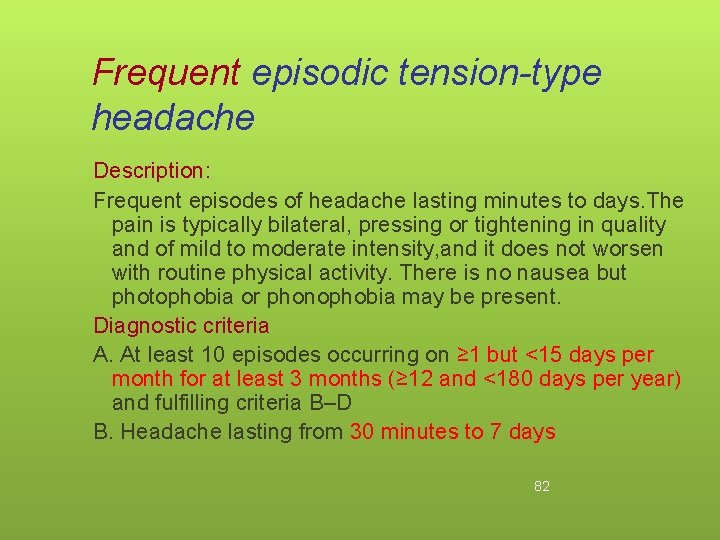
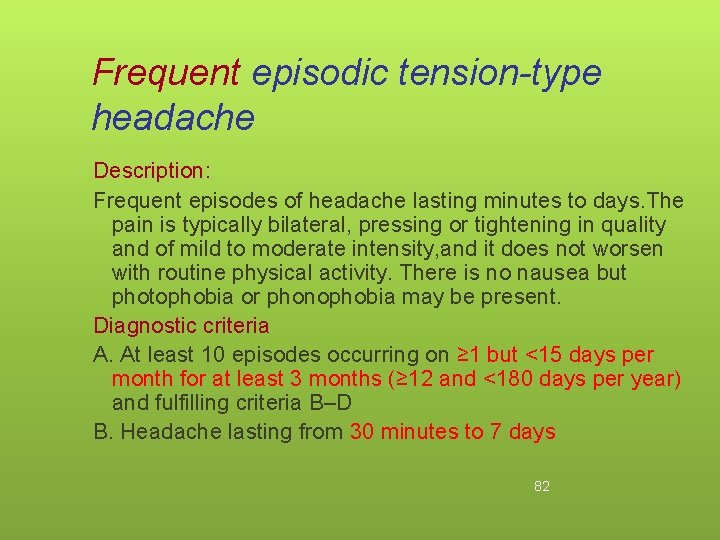
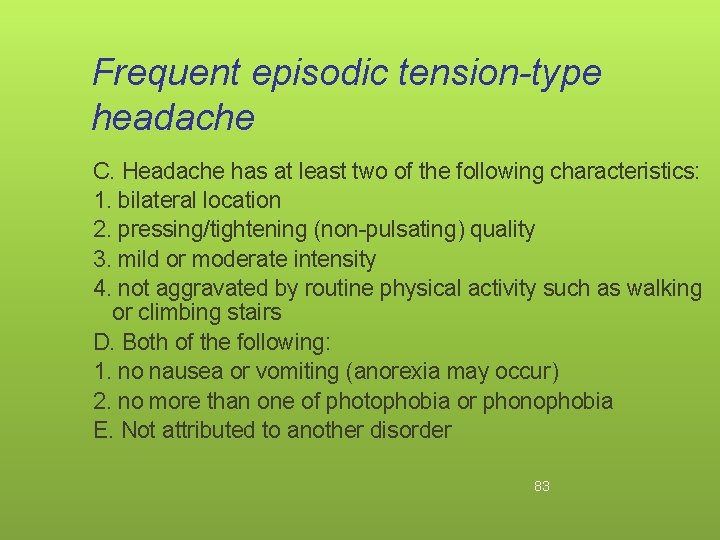
Frequent episodic tension-type headache Description: Frequent episodes of headache lasting minutes to days. The pain is typically bilateral, pressing or tightening in quality and of mild to moderate intensity, and it does not worsen with routine physical activity. There is no nausea but photophobia or phonophobia may be present. Diagnostic criteria A. At least 10 episodes occurring on ≥ 1 but <15 days per month for at least 3 months (≥ 12 and <180 days per year) and fulfilling criteria B–D B. Headache lasting from 30 minutes to 7 days 82
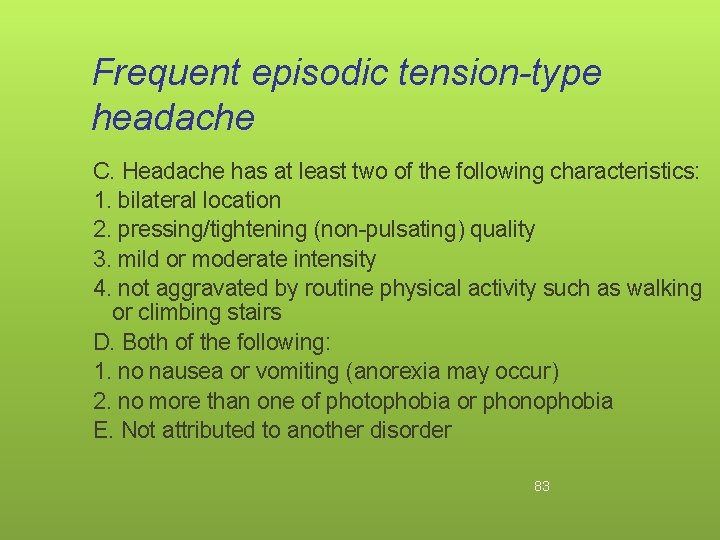
Frequent episodic tension-type headache C. Headache has at least two of the following characteristics: 1. bilateral location 2. pressing/tightening (non-pulsating) quality 3. mild or moderate intensity 4. not aggravated by routine physical activity such as walking or climbing stairs D. Both of the following: 1. no nausea or vomiting (anorexia may occur) 2. no more than one of photophobia or phonophobia E. Not attributed to another disorder 83
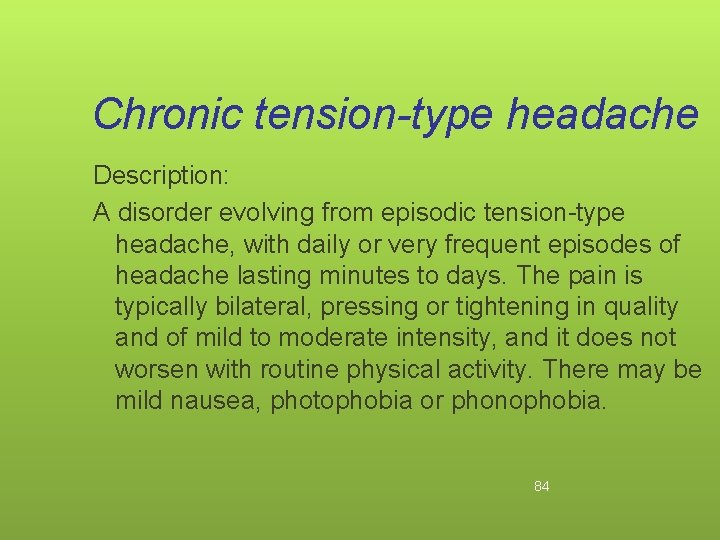
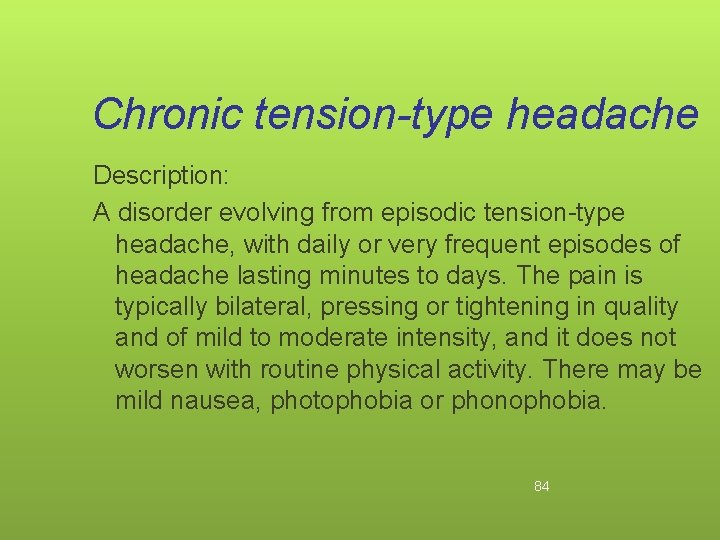
Chronic tension-type headache Description: A disorder evolving from episodic tension-type headache, with daily or very frequent episodes of headache lasting minutes to days. The pain is typically bilateral, pressing or tightening in quality and of mild to moderate intensity, and it does not worsen with routine physical activity. There may be mild nausea, photophobia or phonophobia. 84
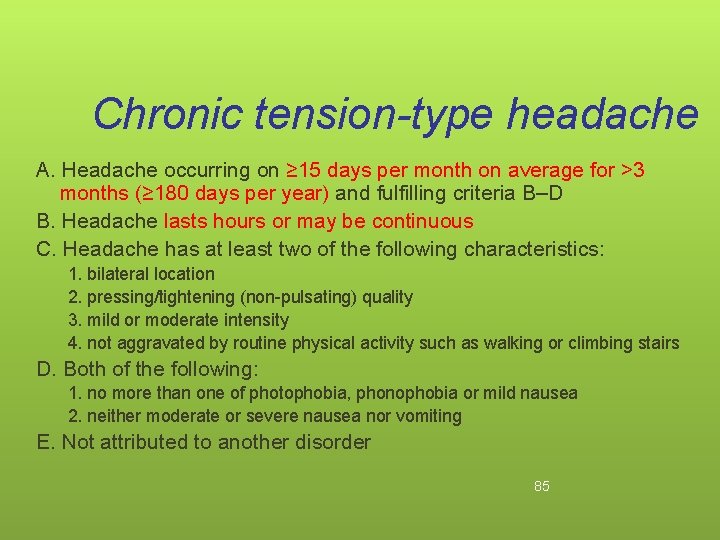
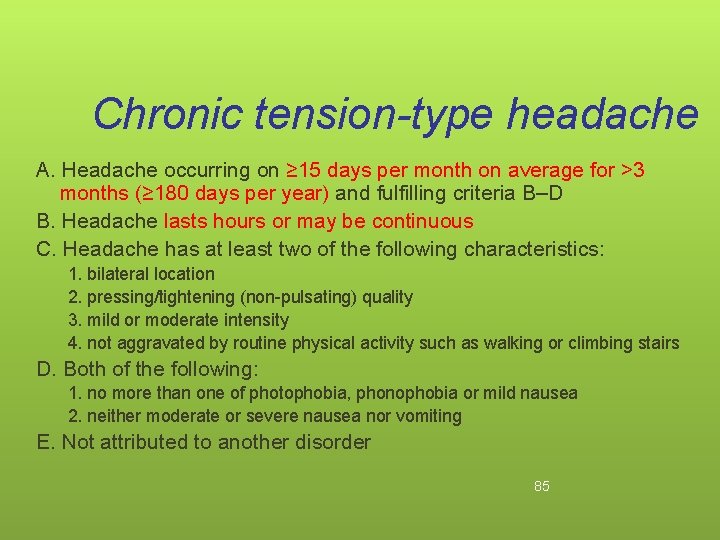
Chronic tension-type headache A. Headache occurring on ≥ 15 days per month on average for >3 months (≥ 180 days per year) and fulfilling criteria B–D B. Headache lasts hours or may be continuous C. Headache has at least two of the following characteristics: 1. bilateral location 2. pressing/tightening (non-pulsating) quality 3. mild or moderate intensity 4. not aggravated by routine physical activity such as walking or climbing stairs D. Both of the following: 1. no more than one of photophobia, phonophobia or mild nausea 2. neither moderate or severe nausea nor vomiting E. Not attributed to another disorder 85

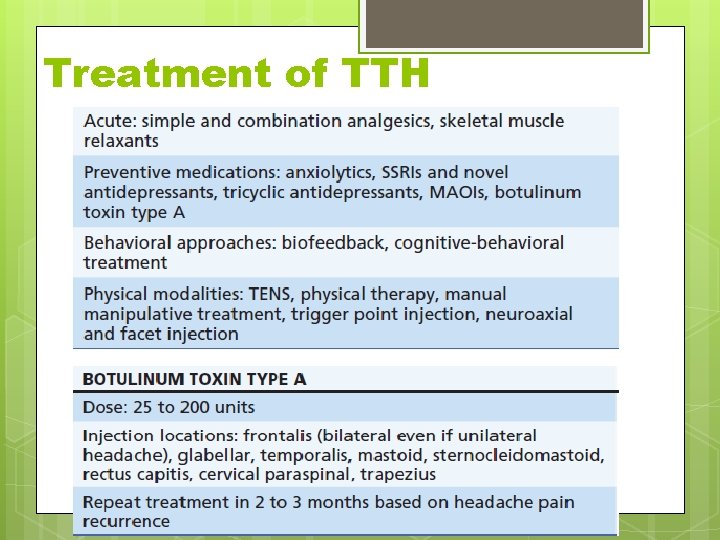
TENSION TYPE HEADACHE TREATMENT ACUTE TREATMENT • Aspirin, Paracetamol, NSAID Taking into account the person’s preference, comorbidities and risk of adverse events • Do not offer opioids for the acute treatment of Tension Type Headache PROPHYLACTIC TREATMENT • Consider a course of up to 10 sessions of accupuncture over 5 -8 weeks for the prophylactic treatment of chronic tension type headache
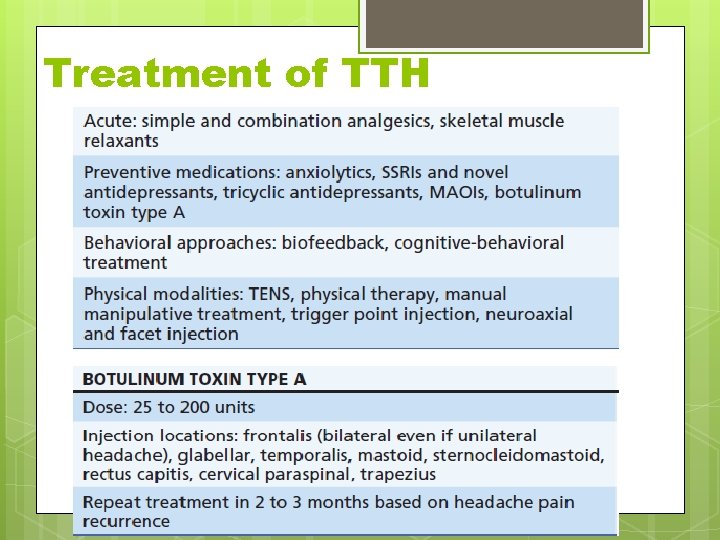
Treatment of TTH
Cluster headache and other trigeminal autonomic cephalalgias Cluster headache Episodic cluster headache Chronic cluster headache Paroxysmal hemicrania Episodic paroxysmal hemicrania Chronic paroxysmal hemicrania (CPH) Short-lasting Unilateral Neuralgiform headache attacks with Conjunctival injection and Tearing (SUNCT) 88
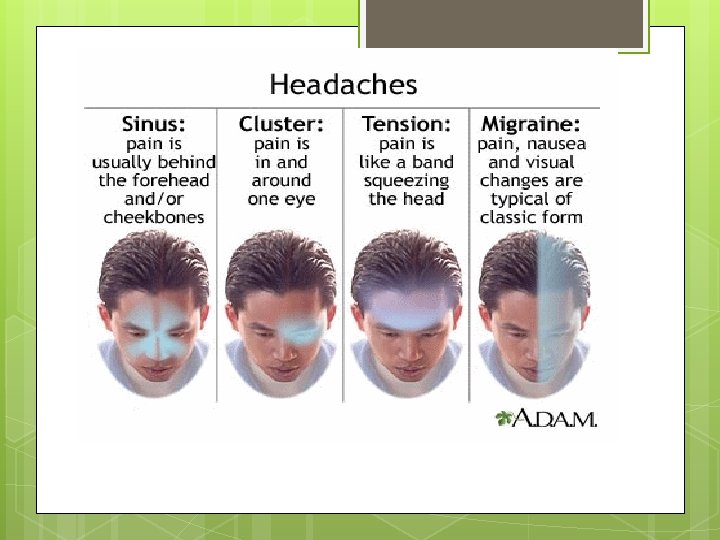
Cluster headache Attacks of severe, strictly unilateral pain which is orbital, supraorbital, temporal or in any combination of these sites, lasting 15– 180 minutes and occurring from once every other day to 8 times a day. The attacks are associated with one or more of the following, all of which are ipsilateral: conjunctival injection, lacrimation, nasal congestion, rhinorrhoea, forehead and facial sweating, miosis, ptosis, eyelid oedema. Most patients are restless or agitated during an attack. Diagnostic criteria: A. At least 5 attacks fulfilling criteria B–D B. Severe or very severe unilateral orbital, supraorbital and/or temporal pain lasting 15– 180 minutes if untreated 89
Cluster headache C. Headache is accompanied by at least one of the following: 1. ipsilateral conjunctival injection and/or lacrimation 2. ipsilateral nasal congestion and/or rhinorrhoea 3. ipsilateral eyelid oedema 4. ipsilateral forehead and facial sweating 5. ipsilateral miosis and/or ptosis 6. a sense of restlessness or agitation D. Attacks have a frequency from one every other day to 8 per day E. Not attributed to another disorder 90
Cluster headache Attacks usually occur in series (cluster periods) lasting for weeks or months separated by remission periods usually lasting months or years. However, about 10– 15% of patients have chronic symptoms without remissions During a cluster period, and in the chronic subtype, attacks occur regularly and may be provoked by alcohol, histamine or nitroglycerine. Pain almost invariably recurs on the same side during an individual cluster period. 91
Cluster headache • During the worst attacks, the intensity of pain is excruciating. Patients are usually unable to lie down and characteristically pace the floor. • Age at onset is usually 20– 40 years. Prevalence is 3– 4 times higher in men than in women. • Cluster headache with coexistent trigeminal neuralgia (cluster-tic syndrome). Some patients have been described who have both Cluster headache and Trigeminal neuralgia. They should receive both diagnoses 92

Episodic cluster headache Cluster headache attacks occurring in periods lasting 7 days to 1 year separated by pain-free periods lasting 1 month or longer. Diagnostic criteria: Attacks fulfilling criteria A–E for Cluster headache At least two cluster periods lasting 7– 365 days and separated by pain-free remission periods of ≥ 1 month Note: Cluster periods usually last between 2 wks - 3 months. 93
Chronic cluster headache Cluster headache attacks occurring for more than 1 year without remission or with remissions lasting less than 1 month. Diagnostic criteria: Attacks fulfilling criteria A–E for Cluster headache Attacks recur over >1 year without remission periods or with remission periods lasting <1 month Primary and secondary 94
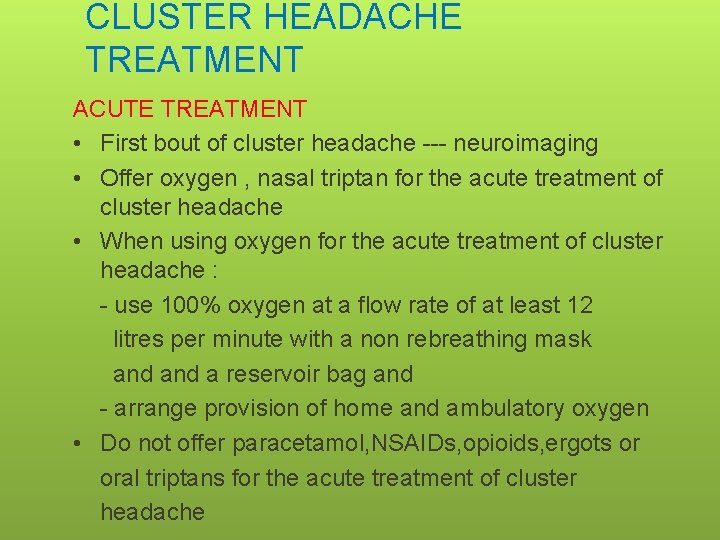
CLUSTER HEADACHE TREATMENT ACUTE TREATMENT • First bout of cluster headache --- neuroimaging • Offer oxygen , nasal triptan for the acute treatment of cluster headache • When using oxygen for the acute treatment of cluster headache : - use 100% oxygen at a flow rate of at least 12 litres per minute with a non rebreathing mask and a reservoir bag and - arrange provision of home and ambulatory oxygen • Do not offer paracetamol, NSAIDs, opioids, ergots or oral triptans for the acute treatment of cluster headache
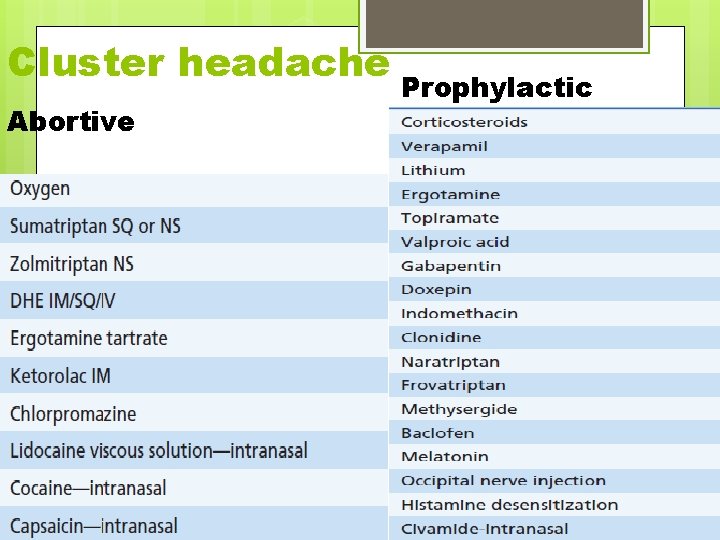
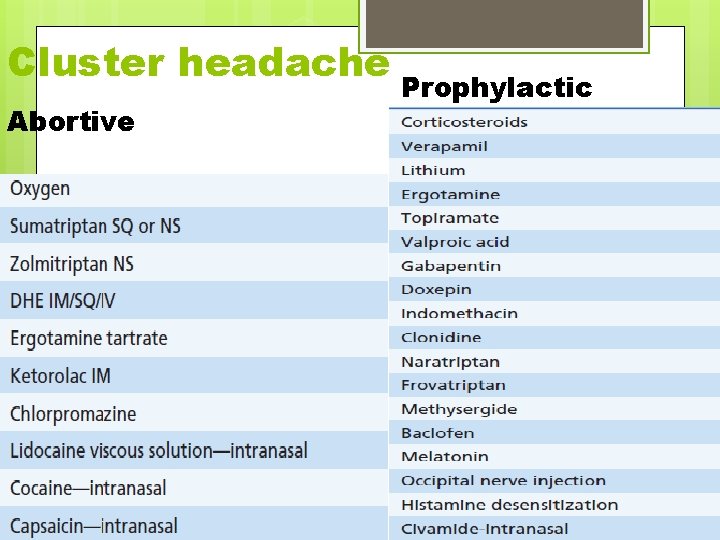
Cluster headache Abortive Prophylactic
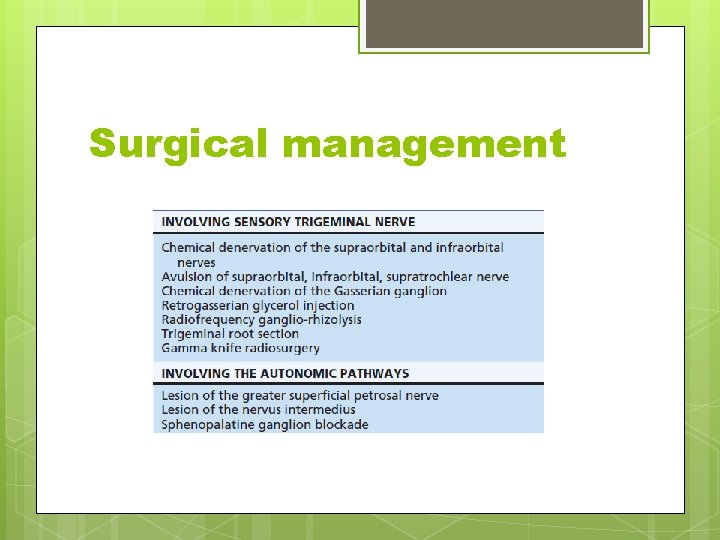
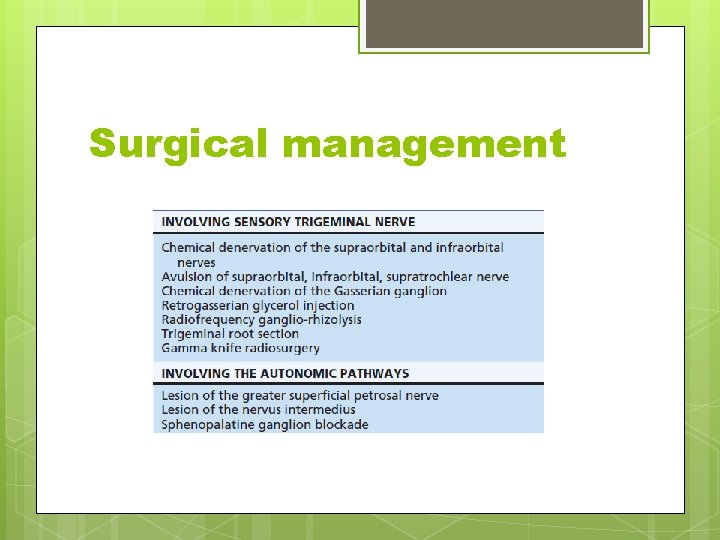
Surgical management
Secondary headaches 98
Headache attributed to head and/or neck trauma § § § Acute post-traumatic headache attributed to moderate or severe head injury Acute post-traumatic headache attributed to mild head injury Chronic post-traumatic headache attributed to moderate or severe head injury Chronic post-traumatic headache attributed to mild head injury 99
Headache attributed to head and/or neck trauma § § § Acute headache attributed to whiplash injury Chronic headache attributed to whiplash injury Headache attributed to traumatic intracranial haematoma - Headache attributed to epidural haematoma - Headache attributed to subdural haematoma 100
Headache attributed to head and/or neck trauma § Headache attributed to other head and/or neck trauma Acute headache attributed to other head and/or neck tr Chronic headache attributed to other head and/or neck tr § Post-craniotomy headache Acute post-craniotomy headache Chronic post-craniotomy headache 101
Headache attributed to cranial or cervical vascular disorder § Headache attributed to ischaemic stroke or transientischaemic attack Headache attributed to ischaemic stroke Headache attributed to transient ischaemic attack § Headache attributed to non-traumatic intracranial haemorrhage Headache attributed to intracerebral haemorrhage Headache attributed to subarachnoid haemorrhage 102
Headache attributed to cranial or cervical vascular disorder § Headache attributed to unruptured vascular malformation Headache attributed to saccular aneurysm Headache attributed to arteriovenous malformation Headache attributed to dural arteriovenous fistula Headache attributed to cavernous angioma Headache attributed to encephalotrigeminal or leptomeningeal angiomatosis (Sturge Weber Syndrome) 103
Headache attributed to cranial or cervical vascular disorder § Headache attributed to arteritis Headache attributed to giant cell arteritis Headache attributed to primary (CNS) angiitis Headache attributed to secondary (CNS) angiitis § Carotid or vertebral artery pain Headache or facial or neck pain attributed to arterial dissection Post-endarterectomy headache Carotid angioplasty headache Headache attributed to intracranial endovascular procedures Angiography headache 104
Headache attributed to cranial or cervical vascular disorder § Headache attributed to cerebral venous thrombosis § Headache attributed to other intracranial vascular disorder Headache attributed to benign angiopathy of the CNS Headache attributed to pituitary apoplexy 105
Headache attributed to nonvascular intracranial disorder § Headache attributed to high cerebrospinal fluid pressure Headache attributed to idiopathic intracranial hypertension Headache attributed to intracranial hypertension secondary to metabolic, toxic or hormonal causes Headache attributed to intracranial hypertension secondary to hydrocephalus 106
Headache attributed to nonvascular intracranial disorder § Headache attributed to low cerebrospinal fluid pressure - Post-dural puncture headache - CSF fistula headache - Headache attributed to spontaneous/idiopathic low CSF pressure 107
Headache attributed to nonvascular intracranial disorder § Headache attributed to non-infectious inflammatory disease Headache attributed to neurosarcoidosis Headache attributed to aseptic (non-infectious) meningitis Headache attributed to other non-infectious inflammatory disease Headache attributed to lymphocytic hypophysitis 108
Headache attributed to nonvascular intracranial disorder § Headache attributed to intracranial neoplasm Headache attributed to increased intracranial pressure or hydrocephalus caused by neoplasm Headache attributed directly to neoplasm Headache attributed to carcinomatous meningitis Headache attributed to hypothalamic or pituitary hyper or hyposecretion § Headache attributed to intrathecal injection 109
Headache attributed to nonvascular intracranial disorder § Headache attributed to epileptic seizure- to specify seizure type Hemicrania epileptica Post-seizure headache § § Headache attributed to Chiari malformation type I Headache attributed to other non-vascular intracranial disorder 110
Headache attributed to a substance use or its withdrawal § Headache induced by acute substance use or exposure Nitric oxide (NO) donor-induced headache Immediate NO donor-induced headache Delayed NO donor-headache Phosphodiesterase (PDE) inhibitor-induced headache Carbon monoxide-induced headache Alcohol-induced headache Immediate alcohol-induced headache Delayed alcohol-induced headache 111
Headache attributed to a substance use or its withdrawal Headache induced by food components and additives Monosodium glutamate-induced headache Cocaine-induced headache Cannabis-induced headache Histamine-induced headache Immediate histamine-induced headache Delayed histamine-induced headache 112
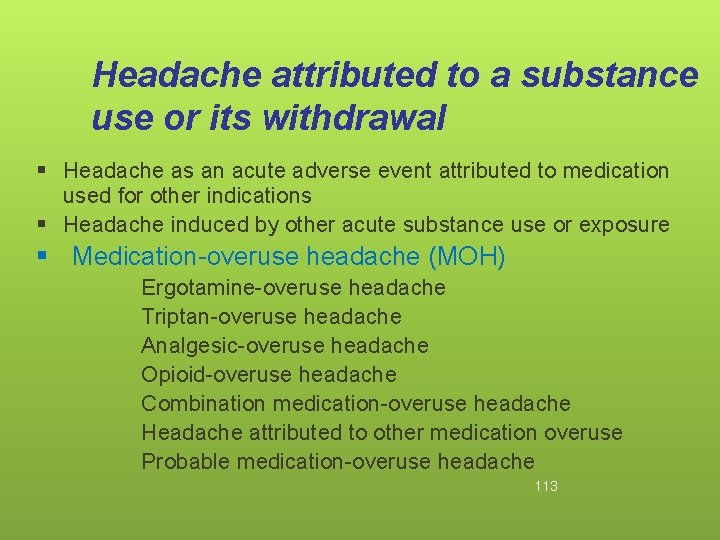
Headache attributed to a substance use or its withdrawal § Headache as an acute adverse event attributed to medication used for other indications § Headache induced by other acute substance use or exposure § Medication-overuse headache (MOH) Ergotamine-overuse headache Triptan-overuse headache Analgesic-overuse headache Opioid-overuse headache Combination medication-overuse headache Headache attributed to other medication overuse Probable medication-overuse headache 113
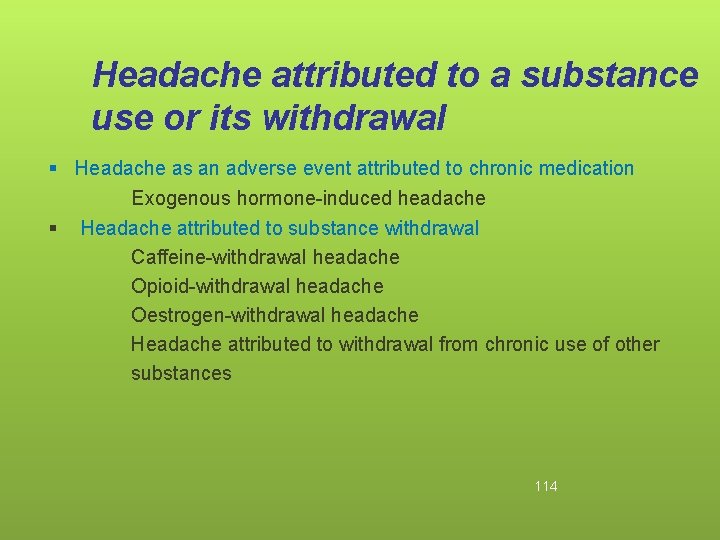
Headache attributed to a substance use or its withdrawal § Headache as an adverse event attributed to chronic medication Exogenous hormone-induced headache § Headache attributed to substance withdrawal Caffeine-withdrawal headache Opioid-withdrawal headache Oestrogen-withdrawal headache Headache attributed to withdrawal from chronic use of other substances 114
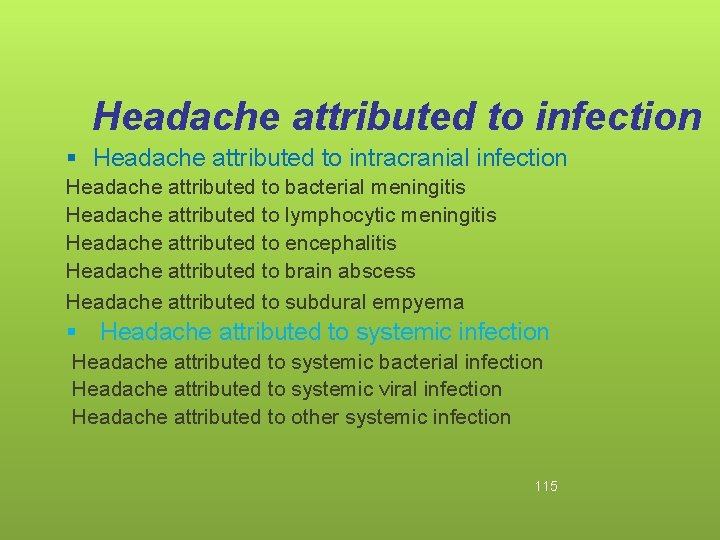
Headache attributed to infection § Headache attributed to intracranial infection Headache attributed to bacterial meningitis Headache attributed to lymphocytic meningitis Headache attributed to encephalitis Headache attributed to brain abscess Headache attributed to subdural empyema § Headache attributed to systemic infection Headache attributed to systemic bacterial infection Headache attributed to systemic viral infection Headache attributed to other systemic infection 115
Headache attributed to infection § Headache attributed to HIV/AIDS § Chronic post-infection headache § Chronic post-bacterial meningitis headache 116
Headache attributed to disorder of homoeostasis § Headache attributed to hypoxia and/or hypercapnia High-altitude headache Diving headache Sleep apnoea headache § § § Dialysis headache Headache attributed to hypothyroidism Headache attributed to fasting Cardiac cephalalgia Headache attributed to other disorder of homoeostasis 117
Headache attributed to disorder of homoeostasis Headache attributed to arterial hypertension Headache attributed to phaeochromocytoma Headache attributed to hypertensive crisis without hypertensive encephalopathy Headache attributed to pre-eclampsia Headache attributed to acute pressor response to an exogenous agent 118
Headache or facial pain attributed to disorder of cranium, neck, eyes, ears, nose, sinuses, teeth, mouth or other facial or cranial structures § Headache attributed to disorder of cranial bone § Headache attributed to disorder of neck Cervicogenic headache Headache attributed to retropharyngeal tendonitis Headache attributed to craniocervical dystonia § Headache attributed to disorder of eyes Headache attributed to acute glaucoma Headache attributed to refractive errors Headache attributed to heterophoria or heterotropia Headache attributed to ocular inflammatory disorder 119
Headache or facial pain attributed to disorder of cranium, neck, eyes, ears, nose, sinuses, teeth, mouth or other facial or cranial structures • • • Headache attributed to disorder of ears Headache attributed to rhinosinusitis Headache attributed to disorder of teeth, jaws or related structures Headache or facial pain attributed to temporomandibular joint disorder Headache attributed to other disorder of cranium, neck, eyes, ears, nose, sinuses, teeth, mouth or other facial or cervical structures 120
Headache attributed to psychiatric disorder § Headache attributed to somatisation disorder § Headache attributed to psychotic disorder 121
Cranial neuralgias and central causes of facial pain § Trigeminal neuralgia Classical trigeminal neuralgia Symptomatic trigeminal neuralgia § Glossopharyngeal neuralgia Classical glossopharyngeal neuralgia Symptomatic glossopharyngeal neuralgia § § Nervus intermedius neuralgia Superior laryngeal neuralgia Nasociliary neuralgia Supraorbital neuralgia 122
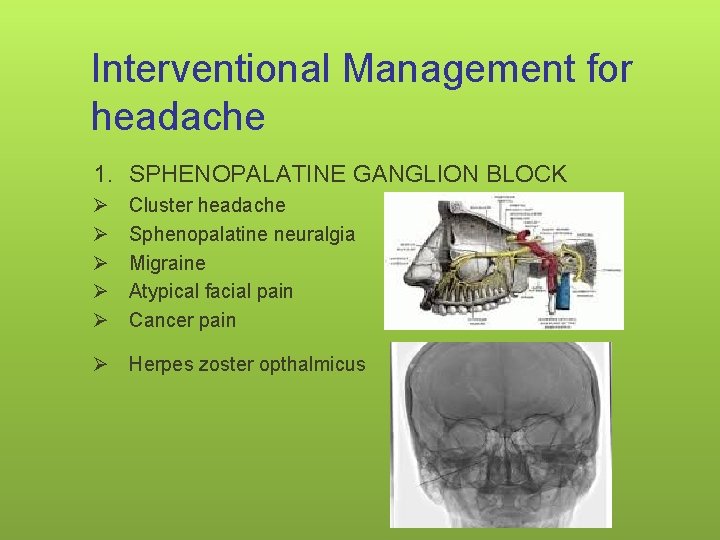
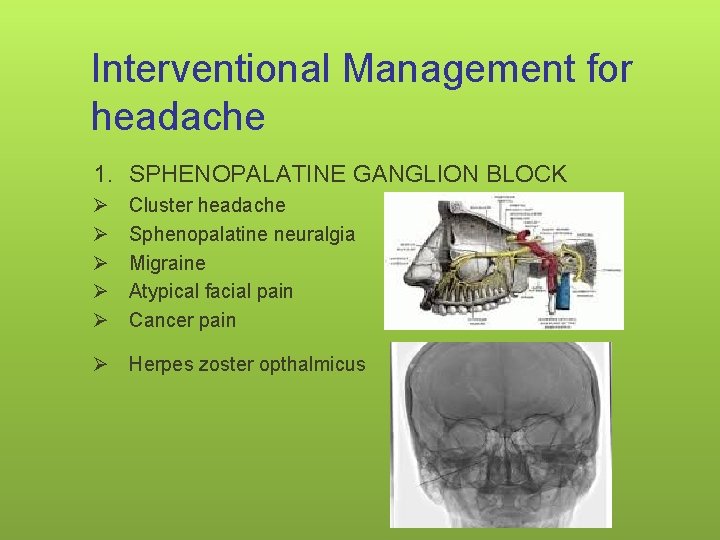
Interventional Management for headache 1. SPHENOPALATINE GANGLION BLOCK Ø Ø Ø Cluster headache Sphenopalatine neuralgia Migraine Atypical facial pain Cancer pain Ø Herpes zoster opthalmicus 123
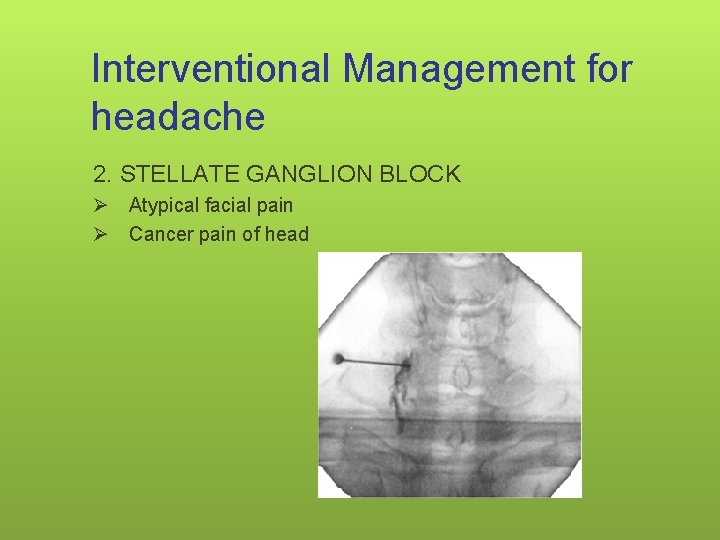
Interventional Management for headache 2. STELLATE GANGLION BLOCK Ø Atypical facial pain Ø Cancer pain of head 124
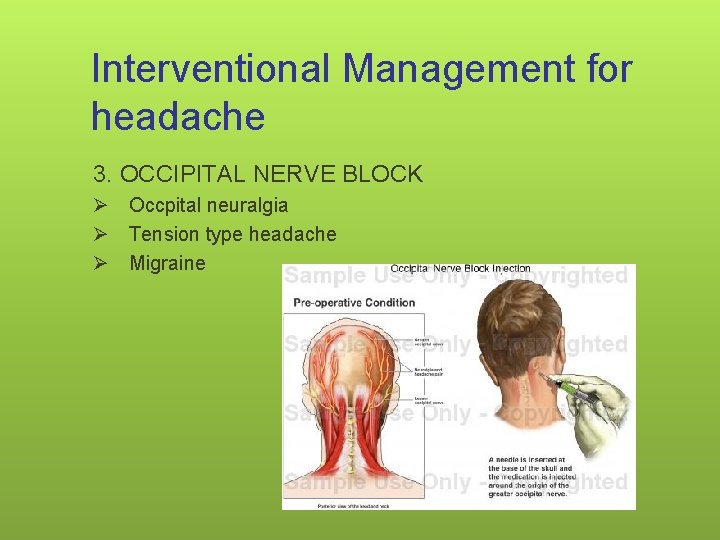
Interventional Management for headache 3. OCCIPITAL NERVE BLOCK Ø Occpital neuralgia Ø Tension type headache Ø Migraine 125
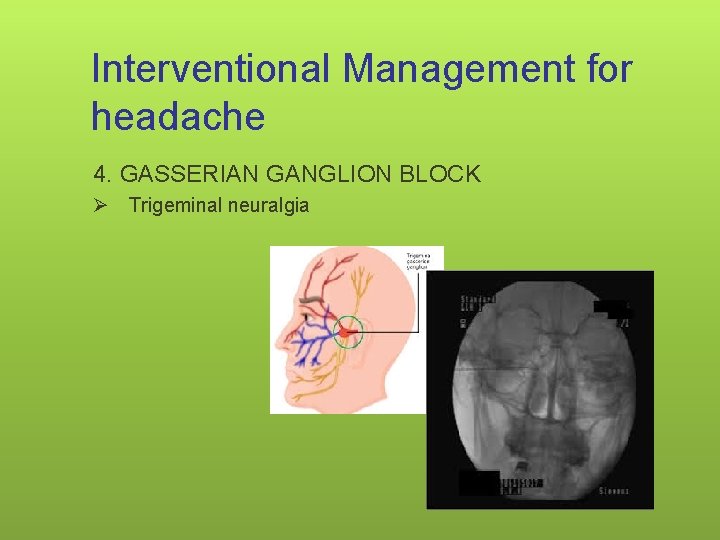
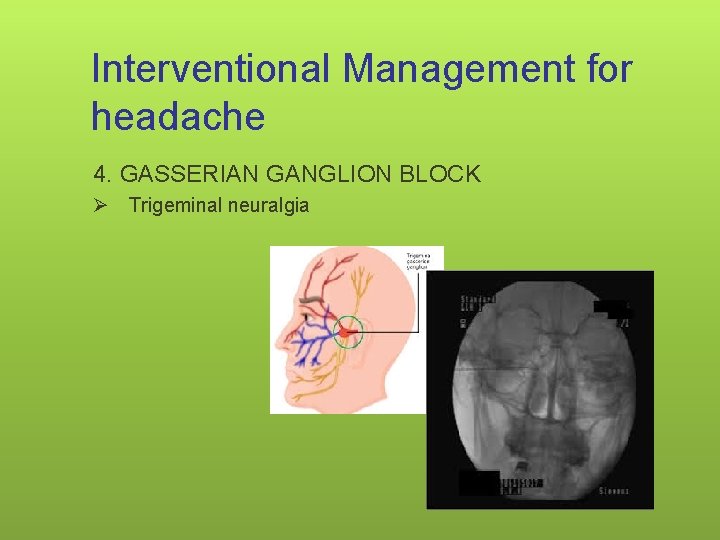
Interventional Management for headache 4. GASSERIAN GANGLION BLOCK Ø Trigeminal neuralgia 126
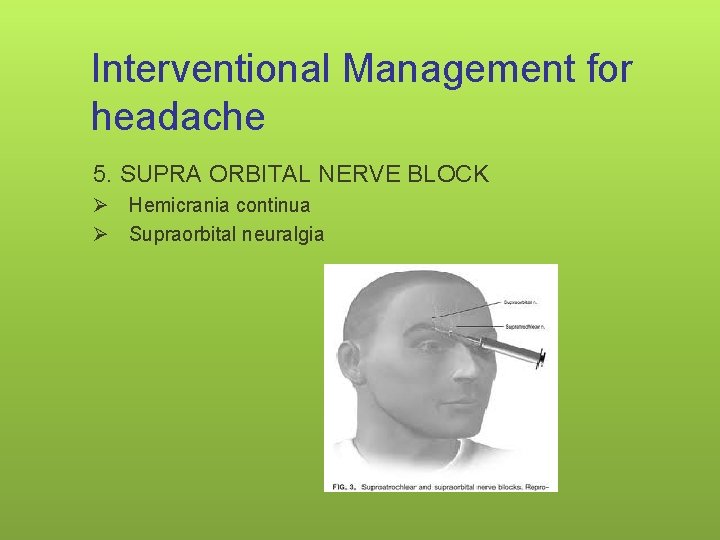
Interventional Management for headache 5. SUPRA ORBITAL NERVE BLOCK Ø Hemicrania continua Ø Supraorbital neuralgia 127
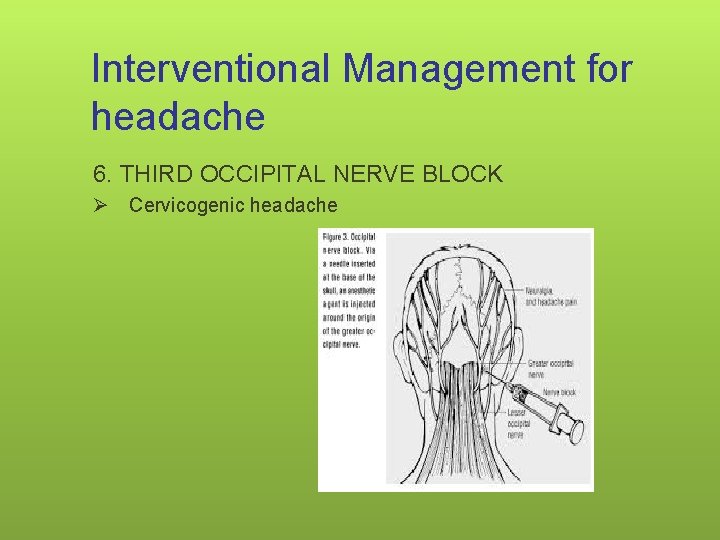
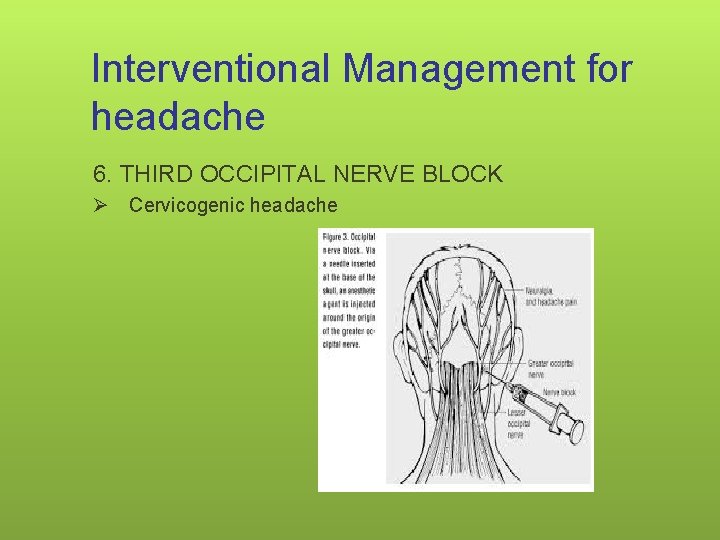
Interventional Management for headache 6. THIRD OCCIPITAL NERVE BLOCK Ø Cervicogenic headache 128
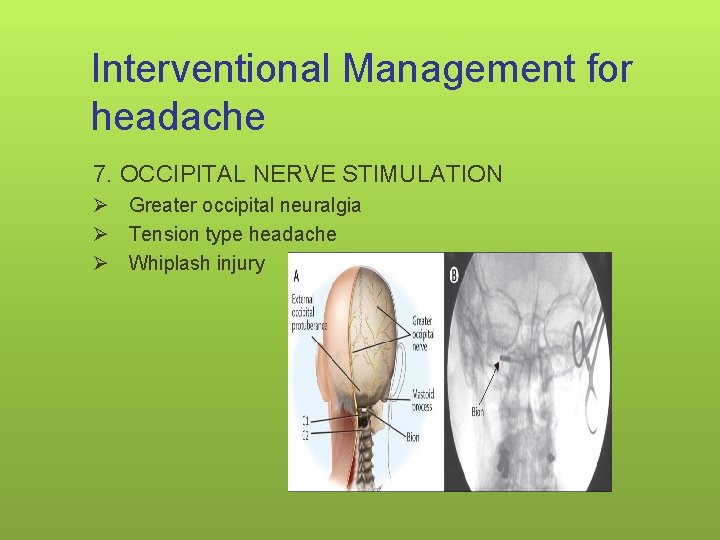
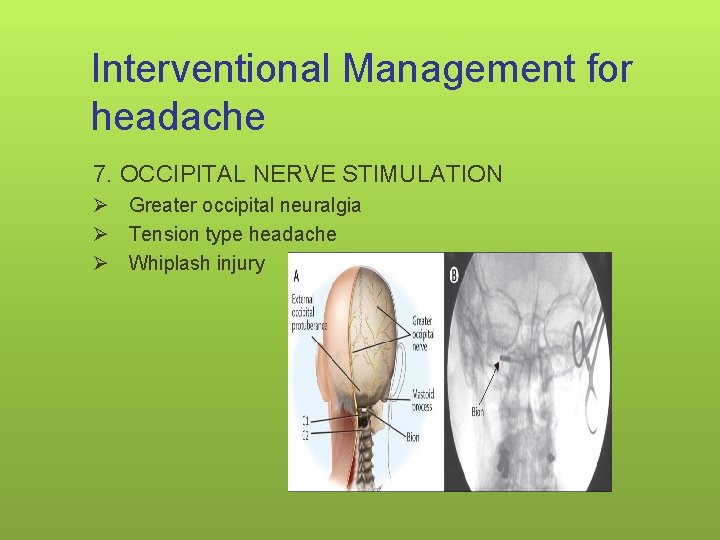
Interventional Management for headache 7. OCCIPITAL NERVE STIMULATION Ø Greater occipital neuralgia Ø Tension type headache Ø Whiplash injury 129

THANK YOU
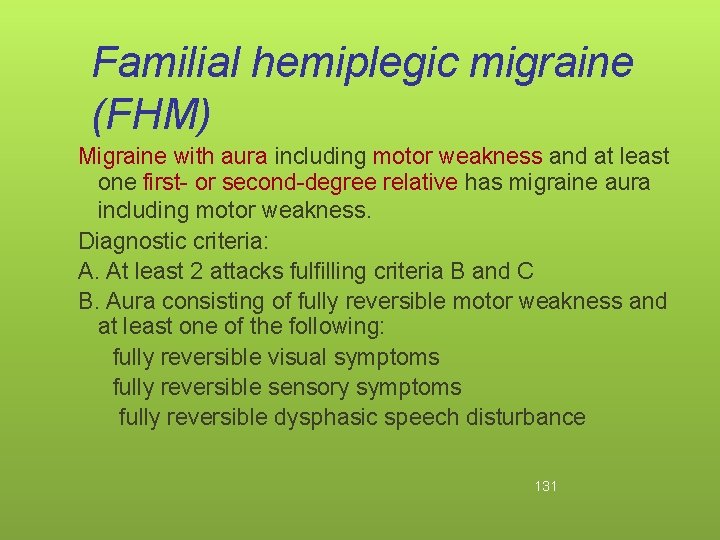
Familial hemiplegic migraine (FHM) Migraine with aura including motor weakness and at least one first- or second-degree relative has migraine aura including motor weakness. Diagnostic criteria: A. At least 2 attacks fulfilling criteria B and C B. Aura consisting of fully reversible motor weakness and at least one of the following: fully reversible visual symptoms fully reversible sensory symptoms fully reversible dysphasic speech disturbance 131
Familial hemiplegic migraine (FHM) C. At least two of the following: at least one aura symptom develops gradually over ≥ 5 minutes and/or different aura symptoms occur in succession over ≥ 5 minutes each aura symptom lasts ≥ 5 minutes and <24 hours headache fulfilling criteria B–D for Migraine without aura begins during the aura or follows onset of aura within 60 minutes D. At least one first- or second-degree relative has had attacks fulfilling these criteria A–E E. Not attributed to another disorder 132
Sporadic hemiplegic migraine Migraine with aura including motor weakness but no first- or second-degree relative has aura including motor weakness. Diagnostic criteria: A. At least 2 attacks fulfilling criteria B and C B. Aura consisting of fully reversible motor weakness and at least one of the following: 1. fully reversible visual symptoms 2. fully reversible sensory symptoms 3. fully reversible dysphasic speech disturbance 133
Sporadic hemiplegic migraine C. At least two of the following: 1. at least one aura symptom develops gradually over ≥ 5 minutes and/or different aura symptoms occur in succession over ≥ 5 minutes 2. each aura symptom lasts ≥ 5 minutes and <24 hours 3. headache fulfilling criteria B–D for Migraine without aura begins during the aura or follows onset of aura within 60 minutes D. No first- or second-degree relative has attacks fulfilling these criteria A–E E. Not attributed to another disorder 134
Sporadic hemiplegic migraine • Sporadic cases occur with approximately the same prevalence as familial cases. • More prevalent in males and often associated with transient hemiparesis and aphasia. • Sporadic cases always require neuroimaging and other tests to rule out other cause. A lumbar puncture is also necessary to rule out pseudomigraine with temporary neurological symptoms and lymphocytic pleocytosis. 135
Childhood periodic syndromes that are commonly precursors of migraine • • • Cyclical vomiting Abdominal migraine Benign paroxysmal vertigo of childhood 136
Cyclical vomiting Description: Recurrent episodic attacks, usually stereotypical in the individual patient, of vomiting and intense nausea. Attacks are associated with pallor and lethargy. There is complete resolution of symptoms between attacks. Diagnostic criteria: A. At least 5 attacks fulfilling criteria B and C B. Episodic attacks, stereotypical in the individual patient, of intense nausea and vomiting lasting from 1 hour to 5 days C. Vomiting during attacks occurs at least 4 times/hour for at least 1 hour 137
Cyclical vomiting D. Symptom-free between attacks E. Not attributed to another disorder Note: In particular, history and physical examination do not show signs of gastrointestinal disease. Cyclical vomiting is a self-limiting episodic condition of childhood, with periods of complete normality between episodes. No pain 138
Abdominal migraine Description: An idiopathic recurrent disorder seen mainly in children and characterized by episodic midline abdominal pain manifesting in attacks lasting 1– 72 hours with normality between episodes. The pain is of moderate to severe intensity and associated with vasomotor symptoms, nausea and vomiting. Diagnostic criteria: A. At least 5 attacks fulfilling criteria B–D B. Attacks of abdominal pain lasting 1– 72 hours (untreated or unsuccessfully treated) 139
Abdominal migraine C. Abdominal pain has all of the following characteristics: midline location, periumbilical or poorly localised dull or ‘just sore’ quality moderate or severe intensity D. During abdominal pain at least 2 of the following: anorexia nausea vomiting pallor E. Not attributed to another disorder 140
Abdominal migraine • In particular, history and physical examination do not show signs of gastrointestinal or renal disease or such disease has been ruled out by appropriate investigations. • Pain is severe enough to interfere with normal daily activities. • Children may find it difficult to distinguish anorexia from nausea. The pallor is often accompanied by dark shadows under the eyes. In a few patients flushing is the predominant vasomotor phenomenon. • Most children with abdominal migraine will develop migraine headache later in life. 141
Benign paroxysmal vertigo of childhood Description: This probably heterogeneous disorder is characterized by recurrent brief episodic attacks of vertigo occurring without warning and resolving spontaneously in otherwise healthy children. Diagnostic criteria: A. At least 5 attacks fulfilling criterion B B. Multiple episodes of severe vertigo, occurring without warning and resolving spontaneously after minutes to hours C. Normal neurological examination and audiometric and vestibular functions between attacks D. Normal electroencephalogram 142
Benign paroxysmal vertigo of childhood Note: Often associated with nystagmus or vomiting; Unilateral throbbing headache may occur in some attacks. 143
Retinal migraine Description: Repeated attacks of monocular visual disturbance, including scintillations, scotomata or blindness, associated with migraine headache. Diagnostic criteria: A. At least 2 attacks fulfilling criteria B and C B. Fully reversible monocular positive and/or negative visual phenomena (eg, scintillations, scotomata or blindness) confirmed by examination during an attack or (after proper instruction) by the patient’s drawing of a monocular field defect during an attack C. Headache fulfilling criteria B–D for Migraine without aura begins during the visual symptoms or follows them within 60 minutes D. Normal ophthalmological examination between attacks E. Not attributed to another disorder 144
Retinal migraine • Appropriate investigations exclude other causes of transient monocular blindness. • Some patients who complain of monocular visual disturbance in fact have hemianopia. Some cases without headache have been reported, but their migrainous nature cannot be ascertained. • Other causes of transient monocular blindness (amaurosis fugax), such as optic neuropathy or carotid dissection, must be excluded. 145
Paroxysmal hemicrania Attacks with similar characteristics of pain and associated symptoms and signs to those of cluster headache, but they are shorter-lasting, more frequent, occur more commonly in females and respond absolutely to indomethacin. Diagnostic criteria: A. At least 20 attacks fulfilling criteria B–D B. Attacks of severe unilateral orbital, supraorbital or temporal pain lasting 2– 30 minutes 146
Paroxysmal hemicrania C. Headache is accompanied by at least one of the following: 1. ipsilateral conjunctival injection and/or lacrimation 2. ipsilateral nasal congestion and/or rhinorrhoea 3. ipsilateral eyelid oedema 4. ipsilateral forehead and facial sweating 5. ipsilateral miosis and/or ptosis D. Attacks have a frequency above 5 per day for more than half of the time, although periods with lower frequency may occur 147
Paroxysmal hemicrania E. Attacks are prevented completely by therapeutic doses of indomethacin F. Not attributed to another disorder In order to rule out incomplete response, indomethacin should be used in a dose of ≥ 150 mg daily orally or rectally, or ≥ 100 mg by injection, but for maintenance smaller doses are often sufficient. There is no male predominance. Onset is usually in adulthood, although childhood cases are reported. Paroxysmal hemicrania with trigeminal neuralgia (CPH-tic syndrome) 148
Episodic paroxysmal hemicrania Attacks of paroxysmal hemicrania occurring in periods lasting 7 days to 1 year separated by painfree periods lasting 1 month or longer. Diagnostic criteria: A. Attacks fulfilling criteria A–F for 3. 2 Paroxysmal hemicrania B. At least two attack periods lasting 7– 365 days , separated by pain-free remission periods of ≥ 1 month 149
Chronic paroxysmal hemicrania Attacks of paroxysmal hemicrania occurring for more than 1 year without remission or with remissions lasting less than 1 month. Diagnostic criteria: A. Attacks fulfilling criteria A–F for Paroxysmal hemicrania B. Attacks recur over >1 year without remission periods or with remission periods lasting <1 month 150
Short-lasting Unilateral Neuralgiform headache attacks with Conjunctival injection and Tearing (SUNCT) This syndrome is characterised by short-lasting attacks of unilateral pain that are much briefer than those seen in any other TAC and very often accompanied by prominent lacrimation and redness of the ipsilateral eye. Diagnostic criteria: A. At least 20 attacks fulfilling criteria B–D B. Attacks of unilateral orbital, supraorbital or temporal stabbing or pulsating pain lasting 5– 240 seconds C. Pain is accompanied by ipsilateral conjunctival injection and lacrimation D. Attacks occur with a frequency from 3 to 200 per day E. Not attributed to another disorder 151
(SUNCT) Patients may be seen with only one of conjunctival injection or tearing, or other cranial autonomic symptoms such as nasal congestion, rhinorrhoea or eyelid oedema may be seen. The literature suggests that the most common mimics of SUNCT are lesions in the posterior fossa or involving the pituitary gland. SUNCT with coexistent trigeminal neuralgia SUNCT with autonomic symptoms-SUNA 152
• Probable trigeminal autonomic cephalalgia • Headache attacks that are believed to be a subtype of trigeminal autonomic cephalalgia but which do not quite meet the diagnostic criteria for any of the subtypes described above. • Probable cluster headache • Probable paroxysmal hemi crania • Probable SUNCT 153
Other primary headaches Primary stabbing headache Primary cough headache Primary exertional headache Primary headache associated with sexual activity Preorgasmic headache Orgasmic headache Hypnic headache Primary thunderclap headache Hemicrania continua New daily-persistent headache (NDPH) 154
Contd-Includes headaches that are clinically heterogeneous. The pathogenesis of these types of headache is still poorly understood, and their treatment is suggested on the basis of anecdotal reports or uncontrolled trials Several headache disorders included in this chapter can be symptomatic and need careful evaluation by imaging and/or other appropriate tests. 155
Primary stabbing headache Previously used terms: Ice-pick pains, jabs and jolts, ophthalmodynia periodica Description: Transient and localised stabs of pain in the head that occur spontaneously in the absence of organic disease of underlying structures or of the cranial nerves. 156
Primary stabbing headache Diagnostic criteria: A. Head pain occurring as a single stab or a series of stabs and fulfilling criteria B–D B. Exclusively or predominantly felt in the distribution of the first division of the trigeminal nerve (orbit, temple and parietal area) C. Stabs last for up to a few seconds and recur with irregular frequency ranging from one to many per day D. No accompanying symptoms E. Not attributed to another disorder 157
Primary stabbing headache Stabbing pains are more commonly experienced by people subject to migraine (about 40%) or cluster headache (about 30%), in which cases they are felt in the site habitually affected by these headaches. A positive response to indomethacin has been reported in some uncontrolled studies, whilst others have observed partial or no responses. 158
Primary cough headache Benign cough headache, Valsalva-maneuver headache Description: Headache precipitated by coughing or straining in the absence of any intracranial disorder. Diagnostic criteria: A. Headache fulfilling criteria B and C B. Sudden onset, lasting from one second to 30 minutes C. Brought on by and occurring only in association with coughing, straining and/or Valsalva maneuver D. Not attributed to another disorder 159
Primary cough headache is usually bilateral and predominantly affects patients older than 40 years of age. Whilst indomethacin is usually effective in the treatment of primary cough headache, a positive response to this medication has also been reported in some symptomatic cases. 160
Primary cough headache Cough headache is symptomatic in about 40% of cases and the large majority of these present with Arnold-Chiari malformation type I. Other reported causes of symptomatic cough headache include carotid or vertebrobasilar diseases and cerebral aneurysms. Diagnostic neuroimaging plays an important role in differentiating secondary cough headache from Primary cough headache 161
Primary exertional headache Benign exertional headache Headache precipitated by any form of exercise. Subforms such as ‘weight-lifters’ headache’ are recognised. Diagnostic criteria: A. Pulsating headache fulfilling criteria B and C B. Lasting from 5 minutes to 48 hours C. Brought on by and occurring only during or after physical exertion D. Not attributed to another disorder 162
On first occurrence of this headache type it is mandatory to exclude subarachnoid haemorrhage and arterial dissection. Primary exertional headache occurs particularly in hot weather or at high altitude. There are reports of prevention in some patients by the ingestion of ergotamine tartrate. Indomethacin has been found effective in the majority of the cases. Headache described in weight-lifters has been considered a subform of Primary exertional headache; because of its sudden onset and presumed mechanism it may have more similarities to Primary cough headache. 163
Primary headache associated with sexual activity • Benign sex headache, coital cephalalgia, benign vascular sexual headache, sexual headache • Headache precipitated by sexual activity, usually starting as a dull bilateral ache as sexual excitement increases and suddenly becoming intense at orgasm, in the absence of any intracranial disorder. 164
Preorgasmic headache Diagnostic criteria: A. Dull ache in the head and neck associated with awareness of neck and/or jaw muscle contraction and fulfilling criterion B B. Occurs during sexual activity and increases with sexual excitement C. Not attributed to another disorder 165
Orgasmic headache Postural headache resembling that of low CSF pressure has been reported to develop after coitus. Such headache should be coded as Headache attributed to spontaneous (or idiopathic) low CSF pressure because it is due to CSF leakage. Diagnostic criteria: A. Sudden severe (‘explosive’) headache fulfilling criterion B B. Occurs at orgasm C. Not attributed to another disorder 166
Orgasmic headache On first onset of orgasmic headache it is mandatory to exclude conditions such as subarachnoid haemorrhage and arterial dissection. Two subtypes (dull type and explosive type headache) were included in the first edition of The International Classification of Headache Disorders. Now excluded No firm data are available on the duration of primary headache associated with sexual activity, but it is usually considered to last from 1 min-3 hr 167
Hypnic headache syndrome, ‘alarm clock’ headache Attacks of dull headache that always awaken the patient from asleep. Diagnostic criteria: A. Dull headache fulfilling criteria B–D B. Develops only during sleep, and awakens patient 168
C. At least two of the following characteristics: 1. occurs >15 times per month 2. lasts ≥ 15 minutes after waking 3. first occurs after age of 50 years D. No autonomic symptoms and no more than one of nausea, photophobia or phonophobia E. Not attributed to another disorder 169
• • • Intracranial disorders must be excluded. Distinction from one of the trigeminal autonomic cephalalgias is necessary for effective management. The pain of hypnic headache is usually mild to moderate, but severe pain is reported by approximately 20% of patients. Pain is bilateral in about two-thirds of cases. The attack usually lasts from 15 to 180 minutes, but longer durations have been described. Caffeine and lithium have been effective treatments in several reported cases. 170
Primary thunderclap headache Primary cough headache, Primary exertional headache and Primary headache associated with sexual activity can all present as thunderclap headache but should be diagnosed as those headache types not as Primary thunderclap headache. Description: High-intensity headache of abrupt onset mimicking that of ruptured cerebral aneurysm. 171
Diagnostic criteria: A. Severe head pain fulfilling criteria B and C B. Both of the following characteristics: 1. sudden onset, reaching maximum intensity in <1 min 2. lasting from 1 hour to 10 days C. Does not recur regularly over subsequent weeks or months D. Not attributed to another disorder 1. Headache may recur within the first week after onset. 2. Normal CSF and normal brain imaging are required. 172
• Evidence that thunderclap headache exists as a primary condition is poor: the search for an underlying cause should be exhaustive. • Thunderclap headache is frequently associated with serious vascular intracranial disorders, particularly subarachnoid haemorrhage. 173
• • Other conditions including intracerebral haemorrhage, cerebral venous thrombosis, unruptured vascular malformation (mostly aneurysm), arterial dissection (intra and extracranial), CNS angiitis, reversible benign CNS angiopathy and pituitary apoplexy. Other organic causes of thunderclap headache are colloid cyst of the third ventricle, CSF hypotension and acute sinusitis (particularly with barotrauma). Primary thunderclap headache should be the diagnosis only when all organic causes have been excluded. 174
Hemicrania continua Persistent strictly unilateral headache responsive to indomethacin. Diagnostic criteria: A. Headache for >3 months fulfilling criteria B–D B. All of the following characteristics: 1. unilateral pain without side-shift 2. daily and continuous, without pain-free periods 3. moderate intensity, but with exacerbations of severe pain 175
C. At least one of the following autonomic features occurs during exacerbations and ipsilateral to the side of pain: 1. conjunctival injection and/or lacrimation 2. nasal congestion and/or rhinorrhoea 3. ptosis and/or miosis D. Complete response to therapeutic doses of indomethacin E. Not attributed to another disorder 176
• Hemicrania continua is usually unremitting, but rare cases of remission are reported. Whether this headache type can be subdivided according to length of history and persistence is yet to be determined 177
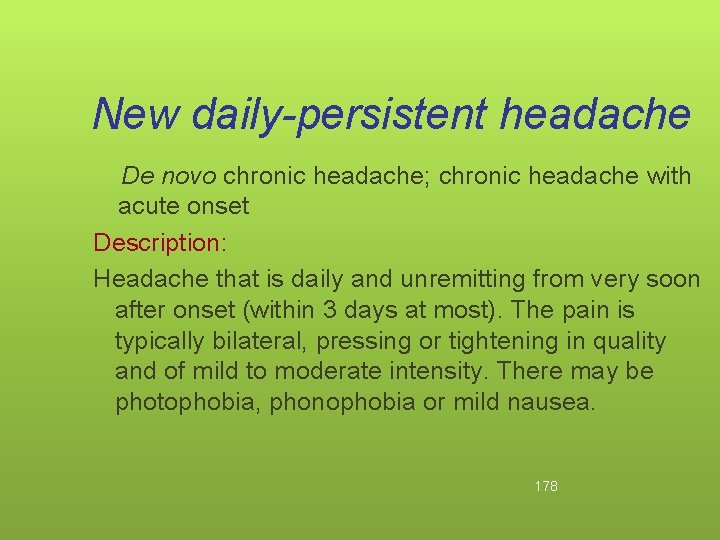
New daily-persistent headache De novo chronic headache; chronic headache with acute onset Description: Headache that is daily and unremitting from very soon after onset (within 3 days at most). The pain is typically bilateral, pressing or tightening in quality and of mild to moderate intensity. There may be photophobia, phonophobia or mild nausea. 178
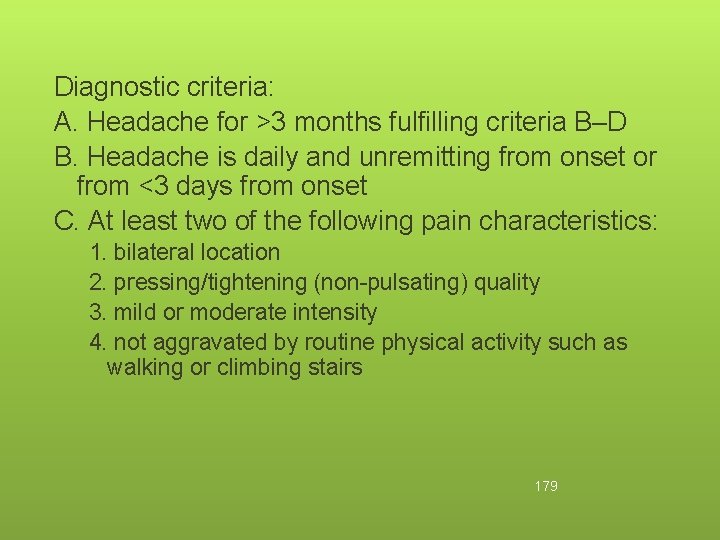
Diagnostic criteria: A. Headache for >3 months fulfilling criteria B–D B. Headache is daily and unremitting from onset or from <3 days from onset C. At least two of the following pain characteristics: 1. bilateral location 2. pressing/tightening (non-pulsating) quality 3. mild or moderate intensity 4. not aggravated by routine physical activity such as walking or climbing stairs 179
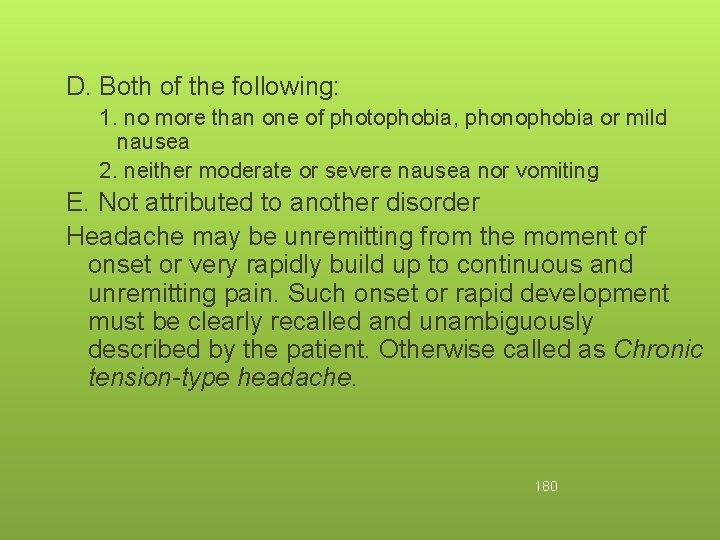
D. Both of the following: 1. no more than one of photophobia, phonophobia or mild nausea 2. neither moderate or severe nausea nor vomiting E. Not attributed to another disorder Headache may be unremitting from the moment of onset or very rapidly build up to continuous and unremitting pain. Such onset or rapid development must be clearly recalled and unambiguously described by the patient. Otherwise called as Chronic tension-type headache. 180
 Primer za cv
Primer za cv Curiculum vital
Curiculum vital Curiculum vite
Curiculum vite Mad pain
Mad pain Menstruation during pregnancy symptoms
Menstruation during pregnancy symptoms Signs of period vs pregnancy
Signs of period vs pregnancy Lignum vitae bearings
Lignum vitae bearings Características internas y externas del mapa conceptual
Características internas y externas del mapa conceptual Non scholae sed vitae discimus
Non scholae sed vitae discimus Curriculum vitae de jesus de nazaret
Curriculum vitae de jesus de nazaret Job application communication skills
Job application communication skills British curriculum vitae
British curriculum vitae Contents of curriculum vitae
Contents of curriculum vitae Label the cranial dura septa and associated sinuses.
Label the cranial dura septa and associated sinuses. Integer vitae scelerisque purus
Integer vitae scelerisque purus Arbor vitae
Arbor vitae Caracteristicas externas de oficio
Caracteristicas externas de oficio Objective for cv
Objective for cv Finis vitae sed non amoris
Finis vitae sed non amoris Arbor vitae uteri
Arbor vitae uteri Sheep brain superior view
Sheep brain superior view Curriculum vitae caracteristicas externas
Curriculum vitae caracteristicas externas Curricuum vitae
Curricuum vitae Anamnesis vitae example
Anamnesis vitae example Eco vitae
Eco vitae Sommaire de cv
Sommaire de cv Evangelium vitae 33
Evangelium vitae 33 Curriculum vitae importancia
Curriculum vitae importancia What iscurriculum vitae
What iscurriculum vitae Regula vitae
Regula vitae Minuta de acuerdos
Minuta de acuerdos Arnagon
Arnagon Curriculum vitae esquema
Curriculum vitae esquema Curriculum vitae unico
Curriculum vitae unico Curriculum vitae výslovnost
Curriculum vitae výslovnost Cornu of uterus
Cornu of uterus Encv
Encv Components of a curriculum vitae
Components of a curriculum vitae Cual es la sexta regla del manual de mooney
Cual es la sexta regla del manual de mooney Zivotois
Zivotois Curriculum vitae forma
Curriculum vitae forma Bank niemowlaka rydygiera
Bank niemowlaka rydygiera Curriculum vitae de carlos slim
Curriculum vitae de carlos slim Cv på latin
Cv på latin Struktur curriculum vitae
Struktur curriculum vitae Is als a non formal education
Is als a non formal education Differences between health education and health promotion
Differences between health education and health promotion Backbone of extension education
Backbone of extension education Basilic vein location
Basilic vein location Presenting complaint
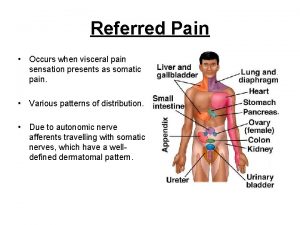
Presenting complaint Referred pain definition
Referred pain definition Le pain que tu nous donnes
Le pain que tu nous donnes Societal impact of pain
Societal impact of pain Moshe schein
Moshe schein Pisa pain
Pisa pain Pain management okc soonercare
Pain management okc soonercare Probably armed possibly not analysis
Probably armed possibly not analysis Remains by simon armitage annotated
Remains by simon armitage annotated Prostate referred pain
Prostate referred pain Diagramme fast exemple
Diagramme fast exemple Cpot pain scale
Cpot pain scale Pico format question example
Pico format question example Chest pain in pediatrics
Chest pain in pediatrics Pqrst pain assessment
Pqrst pain assessment Unpleasant sensory and emotional experience
Unpleasant sensory and emotional experience Internal medicine jeopardy questions and answers
Internal medicine jeopardy questions and answers What is pain
What is pain Pain management stony brook
Pain management stony brook Colderra definition
Colderra definition Painad
Painad Grading scale of pain
Grading scale of pain Pain score chart kkm
Pain score chart kkm Ms pain points
Ms pain points Npass tool
Npass tool Coat hanger pain
Coat hanger pain Larry leeman
Larry leeman Pain de vie corps ressuscité
Pain de vie corps ressuscité Digestion chimique
Digestion chimique Nccpc pain scale
Nccpc pain scale Iv site complications
Iv site complications Iu health pain management
Iu health pain management Typical vs atypical chest pain
Typical vs atypical chest pain Lumbar referral patterns
Lumbar referral patterns Pain school international
Pain school international Pqrstu pain assessment
Pqrstu pain assessment Npass pain scale
Npass pain scale Mechanical vs inflammatory pain
Mechanical vs inflammatory pain Acute abdomen
Acute abdomen Pancreazin
Pancreazin Nociceptive pain
Nociceptive pain Abdominal pain history taking sample
Abdominal pain history taking sample Headache pain chart
Headache pain chart Typical chest pain
Typical chest pain Du pain et des roses chanson
Du pain et des roses chanson Oesteoma
Oesteoma Seigneur nous venons tous t'offrir le pain
Seigneur nous venons tous t'offrir le pain Streak formation iv
Streak formation iv Au bon catering
Au bon catering Cries pain scale
Cries pain scale Chest pain in pediatrics
Chest pain in pediatrics Chapter 7 nursing management of pain during labor and birth
Chapter 7 nursing management of pain during labor and birth Chapter 31 comfort rest and sleep
Chapter 31 comfort rest and sleep Ceo pain
Ceo pain Dr vallina gastroenterology
Dr vallina gastroenterology Canadian c spine rules
Canadian c spine rules Pain intensity scales
Pain intensity scales Non verbal pain scale pdf
Non verbal pain scale pdf Lodcraft history taking
Lodcraft history taking Lodcraft
Lodcraft Midline abdominal pain
Midline abdominal pain Referred pain from appendicitis
Referred pain from appendicitis Cbgabg
Cbgabg Epigastric pain
Epigastric pain Ulq pain
Ulq pain Ruq pain
Ruq pain Little league shoulder pain location
Little league shoulder pain location Pqrstu pain
Pqrstu pain Total pain
Total pain Vision gives pain a purpose
Vision gives pain a purpose What is true labor
What is true labor Translational research institute on pain in later life
Translational research institute on pain in later life Rrhexis medical term
Rrhexis medical term Symbole du pain dans la bible
Symbole du pain dans la bible True labour pains
True labour pains True labour pain
True labour pain Scala dolore nrs
Scala dolore nrs Neuroforaminal stenosis
Neuroforaminal stenosis Epigastric pain differential diagnosis
Epigastric pain differential diagnosis Pain perdu histoire
Pain perdu histoire Parietal pain
Parietal pain Total pain
Total pain Pain attenuation definition
Pain attenuation definition Pain ladder who
Pain ladder who Twisting vibration
Twisting vibration Quad screen results chart
Quad screen results chart Nccpc pain scale
Nccpc pain scale Acute abdomen treatment
Acute abdomen treatment Fetal head
Fetal head Nurses responsibility of oxytocin
Nurses responsibility of oxytocin Chest pain triage
Chest pain triage Nsaids examples
Nsaids examples Chronic pain definition
Chronic pain definition Loratadine bone pain
Loratadine bone pain True labour pain definition
True labour pain definition True labour pain definition
True labour pain definition Petmac chest pain
Petmac chest pain 50 shades of chest pain
50 shades of chest pain Nprs scale
Nprs scale Pelvic pain meaning
Pelvic pain meaning Retrosternal chest pain
Retrosternal chest pain Plissit model
Plissit model Chronic pain comorbidities
Chronic pain comorbidities Ac pain
Ac pain Description of pain
Description of pain Their pain your voice
Their pain your voice Amennorrhoea
Amennorrhoea Expérience de l'eau iodée
Expérience de l'eau iodée Swellingo
Swellingo Jumbo shrimp figurative language
Jumbo shrimp figurative language Rachel beaty
Rachel beaty Anterior vs posterior abdominal wall
Anterior vs posterior abdominal wall Sympathetic parasympathetic
Sympathetic parasympathetic Pain management specialist
Pain management specialist Fundamentals of nursing pain management
Fundamentals of nursing pain management Pain pathway spinal cord
Pain pathway spinal cord Total pain
Total pain Dr danko pain management
Dr danko pain management Major pain point
Major pain point Sclerotogenous pain patterns
Sclerotogenous pain patterns Le pain de ta vie
Le pain de ta vie Formule de calcul boulangerie
Formule de calcul boulangerie Searing pain definition
Searing pain definition Total pain
Total pain God understands our pain
God understands our pain Le grillardin menu
Le grillardin menu Anterior knee pain differential diagnosis
Anterior knee pain differential diagnosis Poker chip pain scale
Poker chip pain scale Beyer oucher pain scale
Beyer oucher pain scale Brief pain inventory
Brief pain inventory Bury integrated pain service
Bury integrated pain service Capa pain assessment tool
Capa pain assessment tool