1 Pain Management Consultant Professor Dr Yekefallah Seyedeh










- Slides: 127
1
Pain Management Consultant Professor : Dr Yekefallah Seyedeh Hedyeh Banihashemi & Mahtab Salehi Master students of critical care nursing (entrance Mehr 92) Automn 1392 2
objective �Explain the pain definition & its pathophysiology �Know different pain theories especially Gate-control �Describe different types of pain �Explain pain treatment (Drug & Nondrug) �Assess patient’s pain & know different assessment tools �Determine nursing process �Know geriatric & pediatric consideration 3

Pain It is an unpleasant sensory & emotional experience associated with actual or potential tissue damage. 4
Are these sentences true or false? 1. The best judges of the existence and severity of patient’s pain are the physicians and nurses caring for the patients. False 5
2. Patients should not receive analgesic until the cause of pain is diagnosed. False 6
3. Pain makes anxiety worse. True 7
4. Patients who are knowledgable about opioid analgesics and who make regular efforts to obtain them are drug seeking (Addicted) False 8
5. Critically ill patients , especially those who appear to be unconscious or have received a neuromuscular blocking agents , do feel pain and recall painfull episodes in ICU. True 9
6. Patients with PTSD (Post Traumatic Stress Disorder) show low sensitivity to acute pain and rarely have chronic pain. False 10
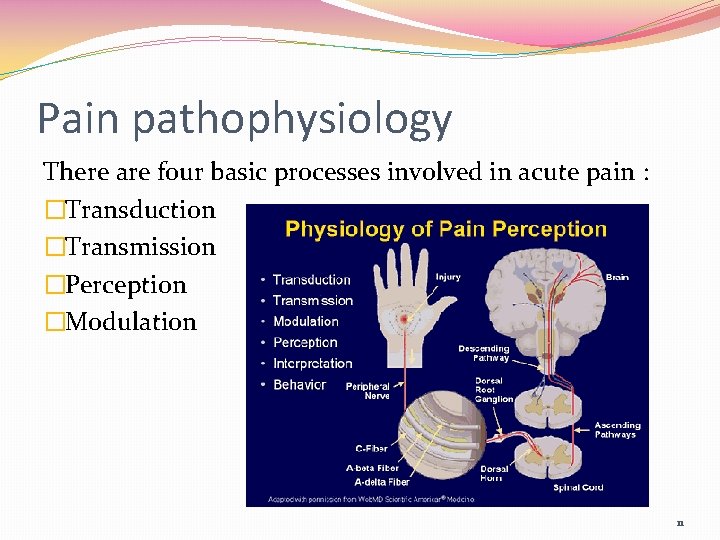
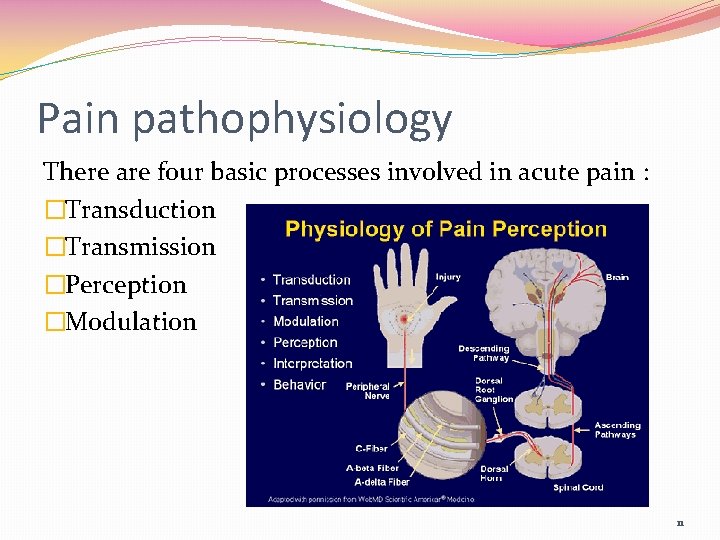
Pain pathophysiology There are four basic processes involved in acute pain : �Transduction �Transmission �Perception �Modulation 11

�C fibres Primary afferent fibres Small diameter Unmyelinated Slow conducting Pain quality Diffuse Dull Burning Aching Referred to as ‘slow’ or second’ pain �A-delta fibres Primary afferent fibres Large diameter Myelinated Fast conducting Pain quality Well-localised Sharp Stinging Pricking Referred to as ‘fast’ or ‘first’ pain 12
Transduction �Transduction begins when the free nerve endings (nociceptors) of C fibres and A-delta fibres of primary afferent neurones respond to noxious stimuli. Nociceptors are exposed to noxious stimuli when tissue damage and inflammation occurs as a result of, for example, trauma, surgery, inflammation, infection, and ischemia. 13
… transduction �The cause of stimulation may be internal, such as pressure exerted by a tumour or external, for example, a burn. This noxious stimulation causes a release of chemical mediators from the damaged cells including: prostaglandin bradykinin serotonin substance P potassium histamine 14
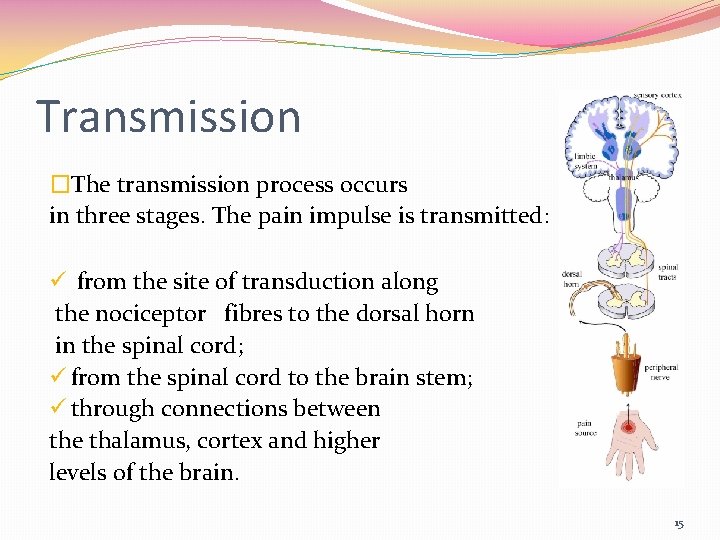
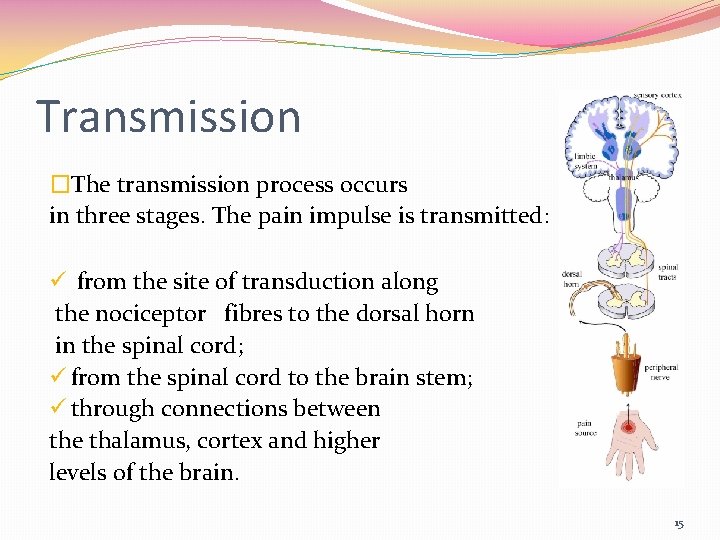
Transmission �The transmission process occurs in three stages. The pain impulse is transmitted: ü from the site of transduction along the nociceptor fibres to the dorsal horn in the spinal cord; ü from the spinal cord to the brain stem; ü through connections between the thalamus, cortex and higher levels of the brain. 15
… transmission �In order for the pain impulses to be transmitted across the synaptic cleft , excitatory neurotransmitters are released , these neurotransmitters are: Ø adenosine triphosphate; Ø glutamate; Ø calcitonin gene-related peptide; Ø bradykinin; Ø nitrous oxide; Ø substance P. 16
Perception �Perception of pain is the end result of the neuronal activity of pain transmission and where pain becomes a conscious multidimensional experience. �The multidimensional experience of pain has affective -motivational, sensory-discriminative, emotional and behavioural components. �When the painful stimuli are transmitted to the brain stem and thalamus, multiple cortical areas are activated and responses are elicited. 17
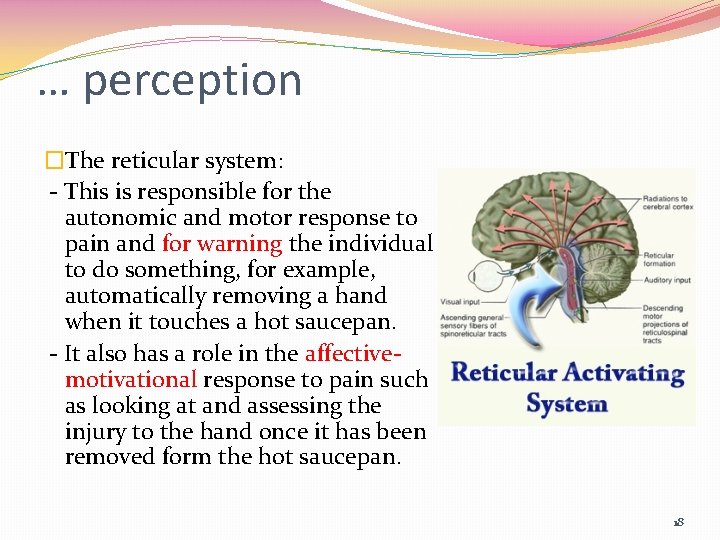
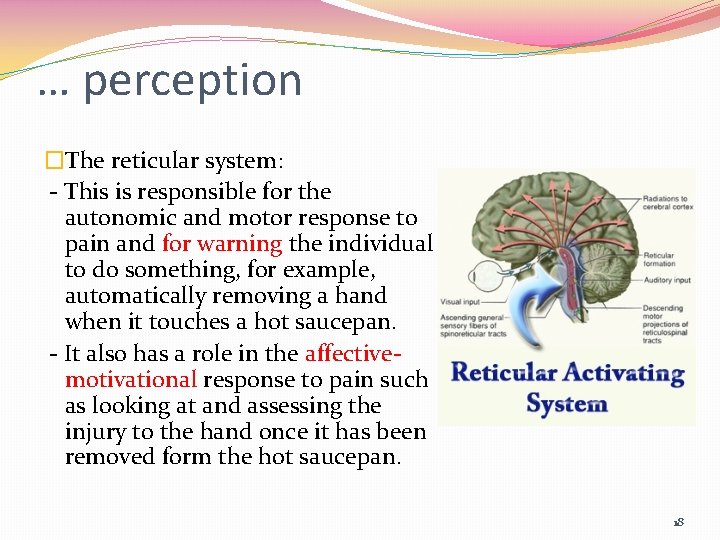
… perception �The reticular system: - This is responsible for the autonomic and motor response to pain and for warning the individual to do something, for example, automatically removing a hand when it touches a hot saucepan. - It also has a role in the affectivemotivational response to pain such as looking at and assessing the injury to the hand once it has been removed form the hot saucepan. 18
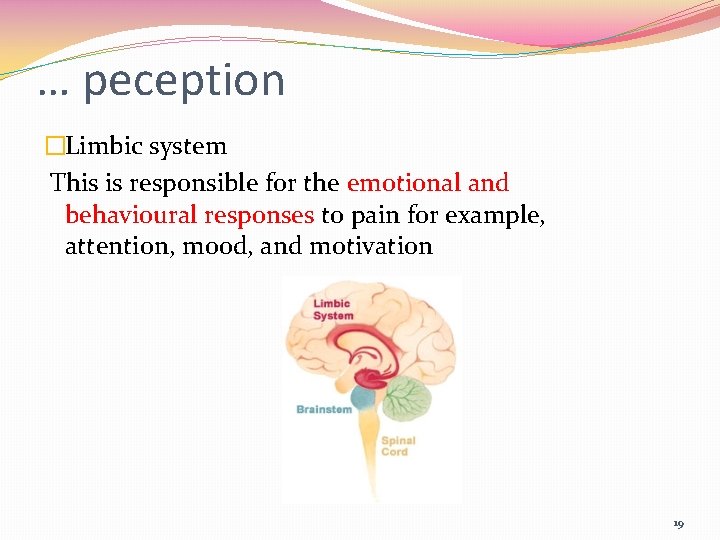
… peception �Limbic system This is responsible for the emotional and behavioural responses to pain for example, attention, mood, and motivation 19
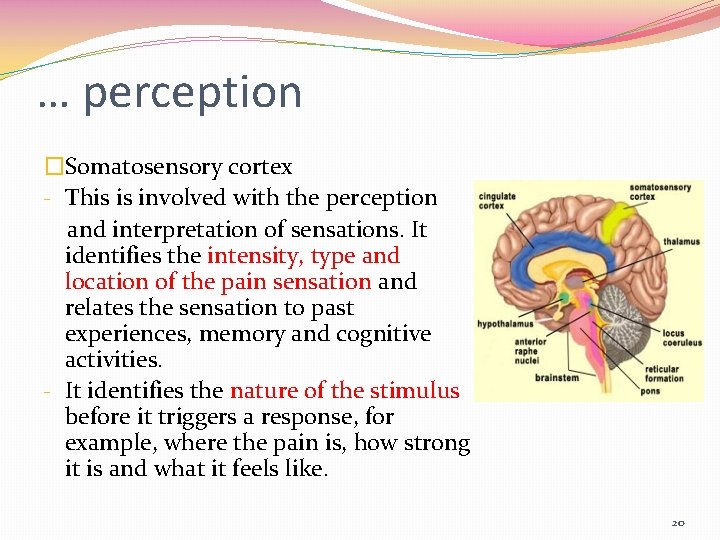
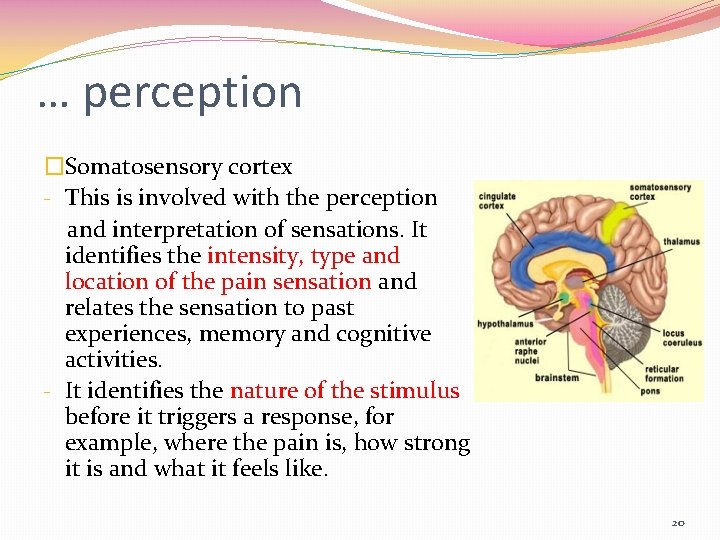
… perception �Somatosensory cortex - This is involved with the perception and interpretation of sensations. It identifies the intensity, type and location of the pain sensation and relates the sensation to past experiences, memory and cognitive activities. - It identifies the nature of the stimulus before it triggers a response, for example, where the pain is, how strong it is and what it feels like. 20
Modulation �The modulation of pain involves changing or inhibiting transmission of pain impulses in the spinal cord. �The multiple, complex pathways involved in the modulation of pain are referred to as the descending modulatory pain pathways (DMPP) and these can lead to either an increase in the transmission of pain impulses (excitatory) or a decrease in transmission (inhibition). �Inhibitory neurotransmitters include: v endogenous opioids (enkephalins and endorphins); v serotonin (5 -HT); v norepinephirine (noradrenalin); v gamma-aminobutyric acid (GABA); v neurotensin; v acetylcholine; v oxytocin. 21
Pain theories �Specificity theory �Pattern theory �Intensity theory �Gate control theory 22
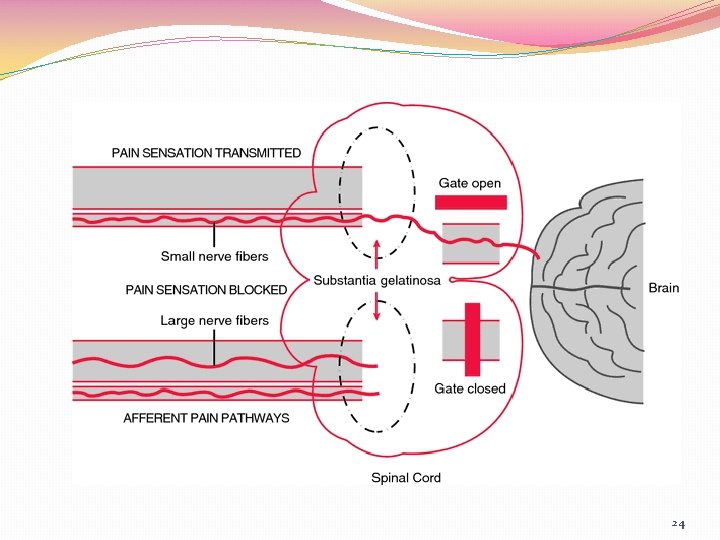
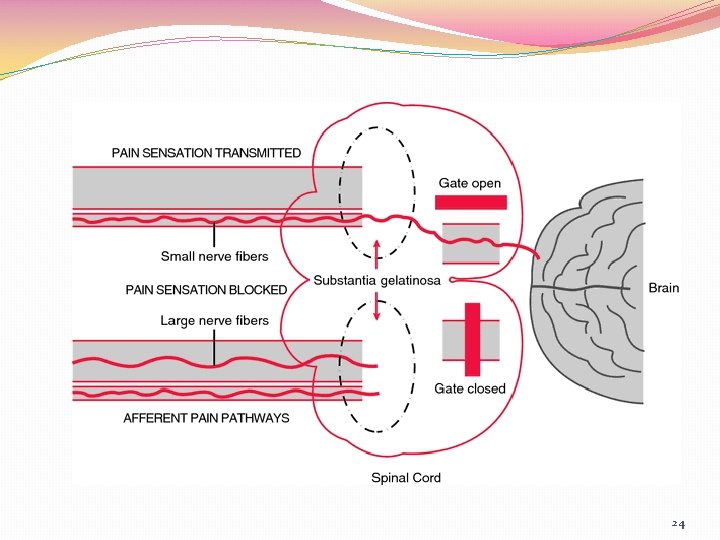
Gate control theory �Proposed by Ronald Melzack and Patrick Wall during the early 1960 s �Gate control theory suggests that the spinal cord contains a neurological "gate" that either blocks pain signals or allows them to continue on to the brain �Pain signals traveling via small nerve fibers are allowed to pass through, while signals sent by large nerve fibers are blocked. �Gate control theory is often used to explain phantom or chronic pain. 23
24
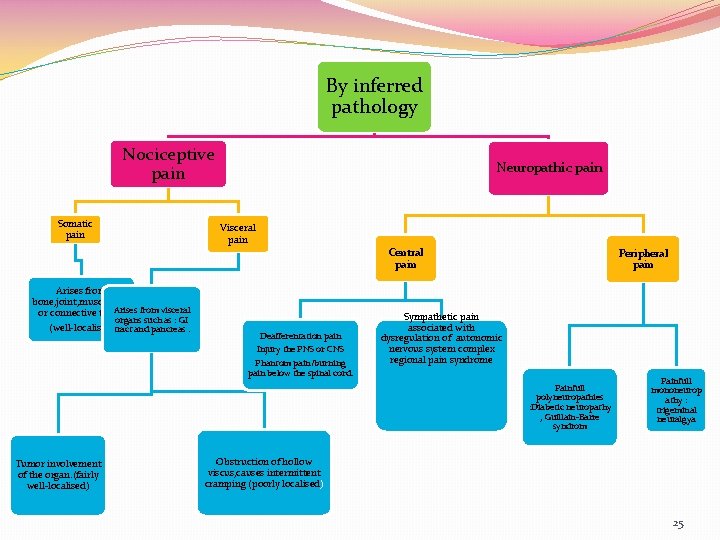
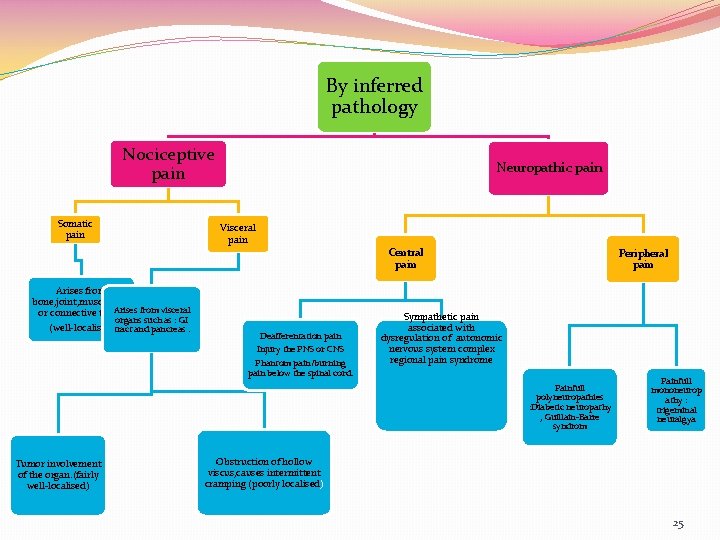
By inferred pathology Nociceptive pain Somatic pain Neuropathic pain Visceral pain Central pain Arises from bone, joint, muscle, skin Arises from visceral or connective tissue organs such as : GI (well-localised)tract and pancreas. Deafferentation pain Injury the PNS or CNS Phantom pain/burning pain below the spinal cord. Peripheral pain Sympathetic pain associated with dysregulation of autonomic nervous system complex regional pain syndrome Painfull polyneuropathies : Diabetic neuropathy , Guillain-Barre syndrom Tumor involvement of the organ. (fairly well-localised) Painfull mononeurop athy : trigeminal neuralgya Obstruction of hollow viscus, causes intermittent cramping (poorly localised) 25

Phantom pain 26
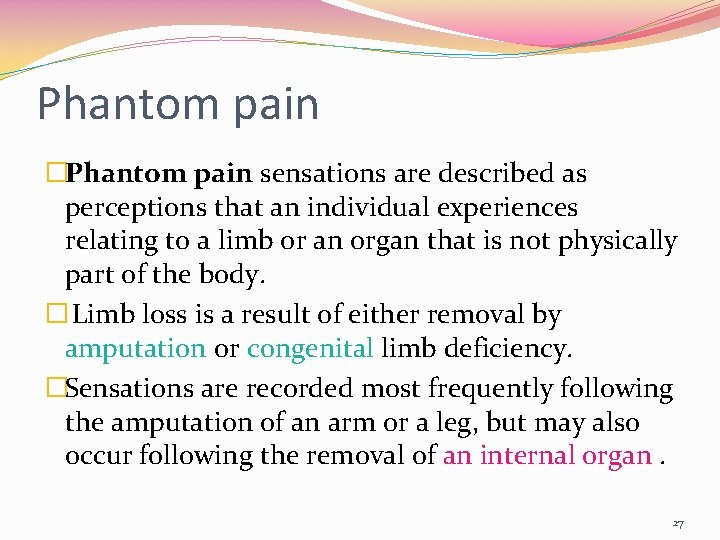
Phantom pain �Phantom pain sensations are described as perceptions that an individual experiences relating to a limb or an organ that is not physically part of the body. � Limb loss is a result of either removal by amputation or congenital limb deficiency. �Sensations are recorded most frequently following the amputation of an arm or a leg, but may also occur following the removal of an internal organ. 27
… phantom pain There are various types of sensations that may be felt: v Sensations related to the phantom limb's posture, length and volume e. g. feeling that the phantom limb is behaving just like a normal limb like sitting with the knee bent or feeling that the phantom limb is as heavy as the other limb. v Sensations of movement (e. g. feeling that the phantom foot is moving). v Sensations of touch, temperature, pressure and itchiness. Many amputees report of feeling heat, tingling, itchiness, and pain. 28
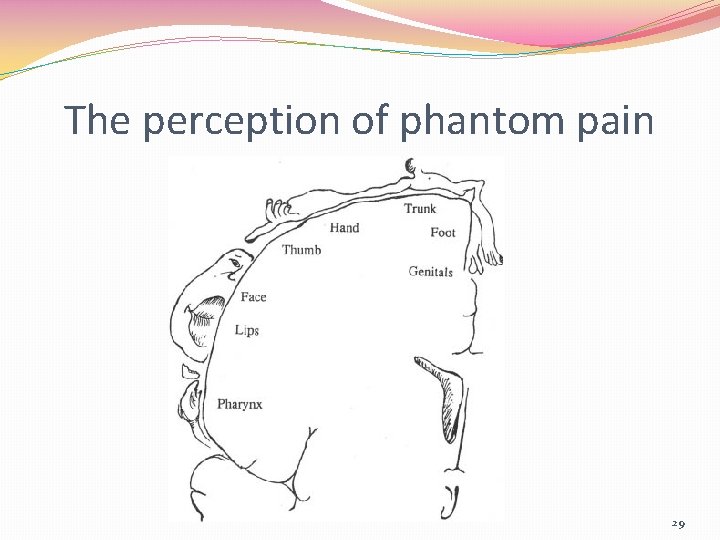
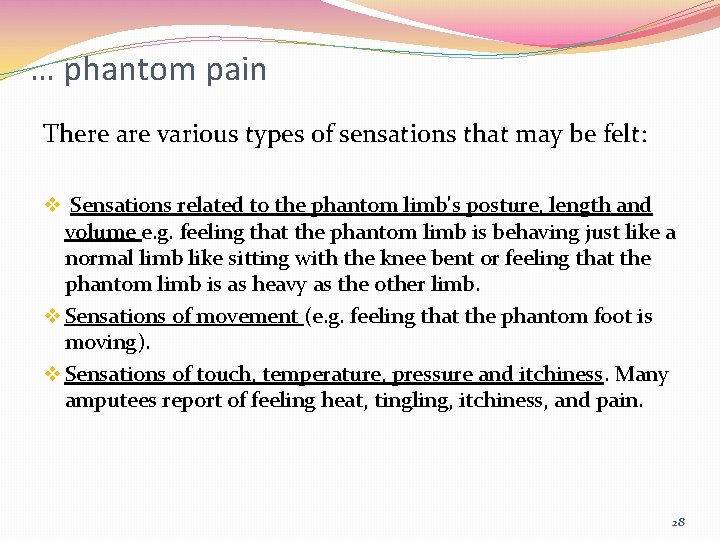
The perception of phantom pain 29
30
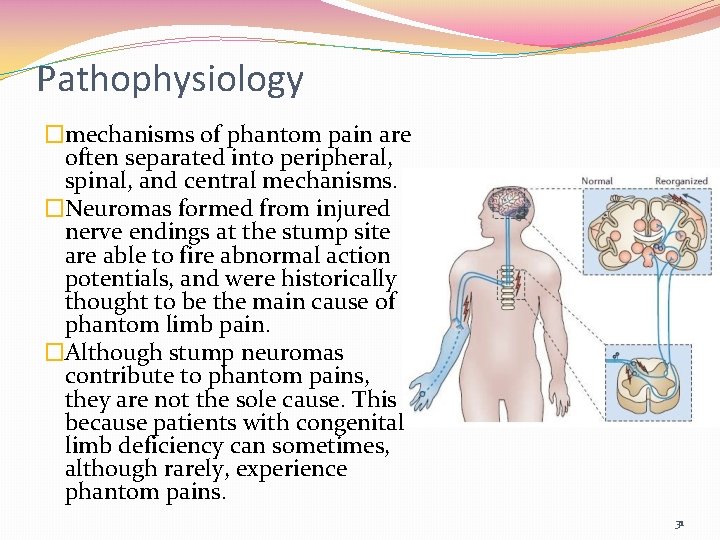
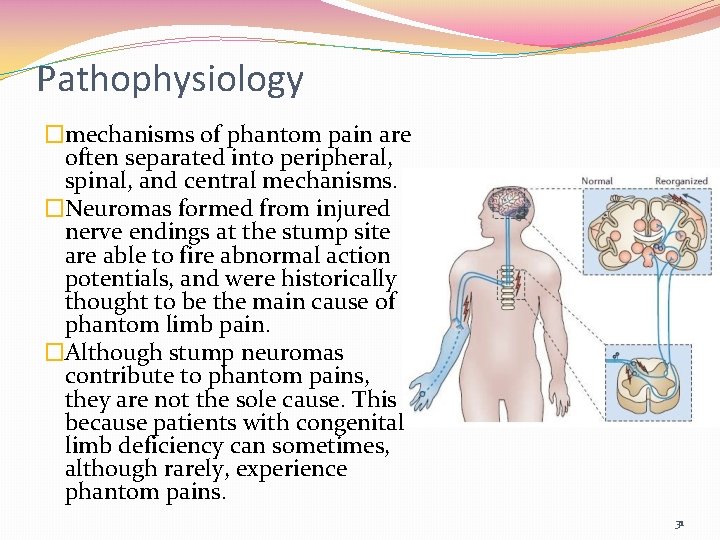
Pathophysiology �mechanisms of phantom pain are often separated into peripheral, spinal, and central mechanisms. �Neuromas formed from injured nerve endings at the stump site are able to fire abnormal action potentials, and were historically thought to be the main cause of phantom limb pain. �Although stump neuromas contribute to phantom pains, they are not the sole cause. This is because patients with congenital limb deficiency can sometimes, although rarely, experience phantom pains. 31
Stump pain �Stump pain that occurs immediately after amputation is acute nociceptive pain and usually resolves after a few weeks as the wound heals. � Infection or wound dehiscence may prolong postoperative pain in some cases. � Stump pain can persist for much longer than the initial period of wound healing, lasting months or years, and occurs in 13 -71%of cases. 32
Phantom pain �The precise incidence of phantom pain is not known. recent evidence suggests rates of approximately 50 -78%. �Phantom pain normally occurs within the first week after amputation. �Phantom pain has been described in various terms (e. g. shooting, burning, cramping and aching) and is characteristically localized in the distal area of the phantom limb. 33

Phantom pain treatment It includes : ü Pharmacological therapy ü Noninvasive therapy ü Minimally invasive therapy ü Surgery 34
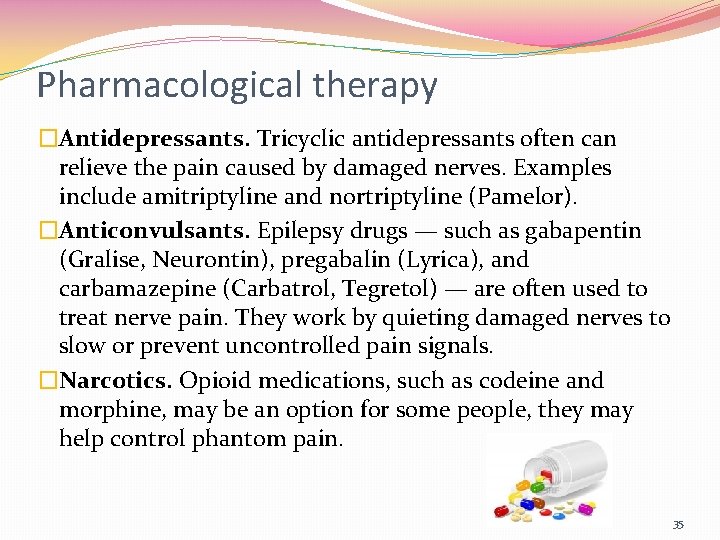
Pharmacological therapy �Antidepressants. Tricyclic antidepressants often can relieve the pain caused by damaged nerves. Examples include amitriptyline and nortriptyline (Pamelor). �Anticonvulsants. Epilepsy drugs — such as gabapentin (Gralise, Neurontin), pregabalin (Lyrica), and carbamazepine (Carbatrol, Tegretol) — are often used to treat nerve pain. They work by quieting damaged nerves to slow or prevent uncontrolled pain signals. �Narcotics. Opioid medications, such as codeine and morphine, may be an option for some people, they may help control phantom pain. 35
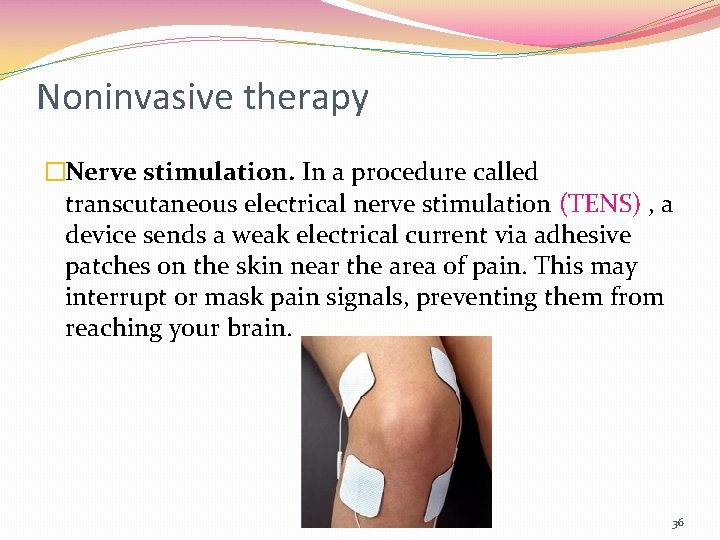
Noninvasive therapy �Nerve stimulation. In a procedure called transcutaneous electrical nerve stimulation (TENS) , a device sends a weak electrical current via adhesive patches on the skin near the area of pain. This may interrupt or mask pain signals, preventing them from reaching your brain. 36
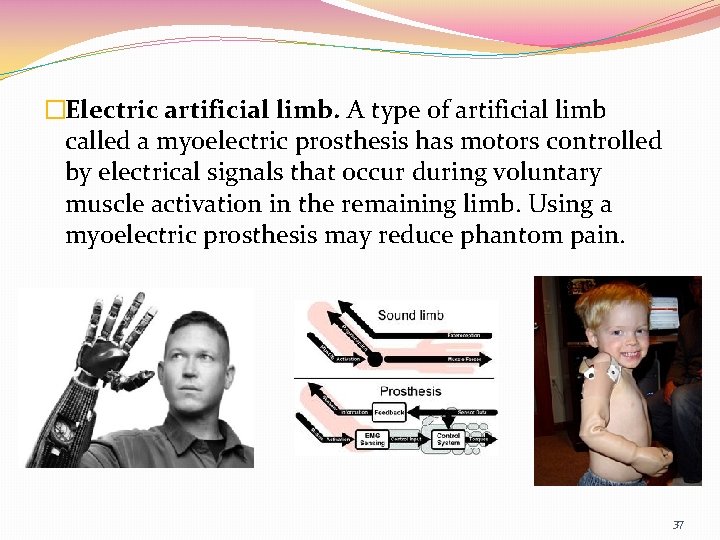
�Electric artificial limb. A type of artificial limb called a myoelectric prosthesis has motors controlled by electrical signals that occur during voluntary muscle activation in the remaining limb. Using a myoelectric prosthesis may reduce phantom pain. 37
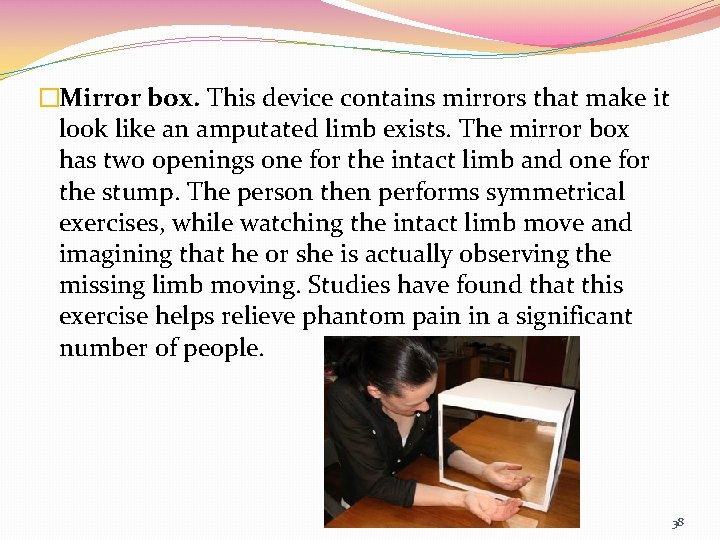
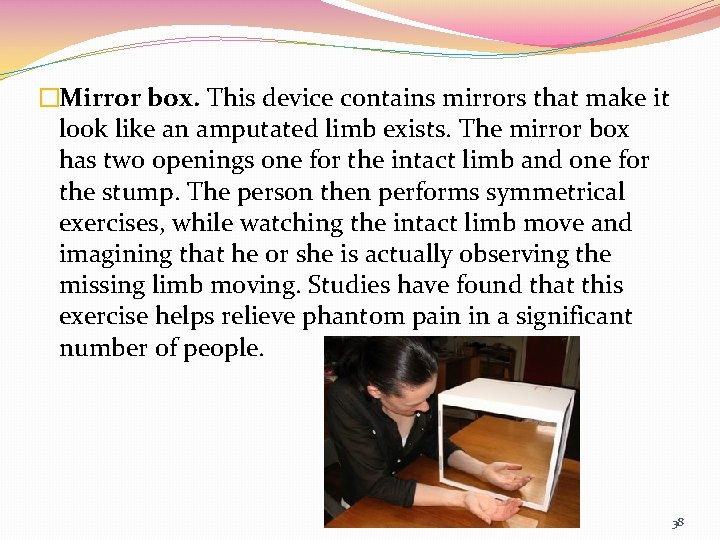
�Mirror box. This device contains mirrors that make it look like an amputated limb exists. The mirror box has two openings one for the intact limb and one for the stump. The person then performs symmetrical exercises, while watching the intact limb move and imagining that he or she is actually observing the missing limb moving. Studies have found that this exercise helps relieve phantom pain in a significant number of people. 38
�Acupuncture. It's thought that acupuncture stimulates your central nervous system to release the body's natural pain-relieving endorphins. Acupuncture is generally considered safe when performed correctly. 39
Minimally invasive therapy �Injection. Sometimes injecting pain-killing medications local anesthetics, steroids or both into the stump can provide relief of phantom limb pain. �Spinal cord stimulation. Your doctor inserts tiny electrodes along your spinal cord. A small electrical current delivered to the spinal cord can sometimes relieve pain. �Intrathecal delivery system. This procedure allows medication to be delivered directly into the spinal fluid. 40
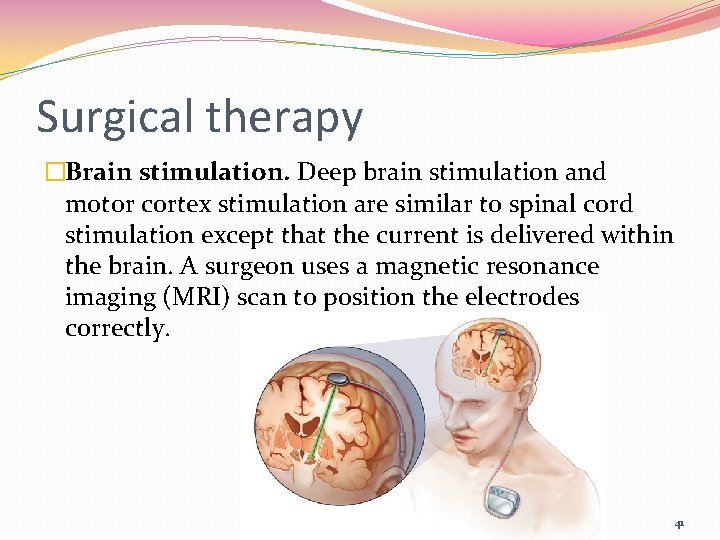
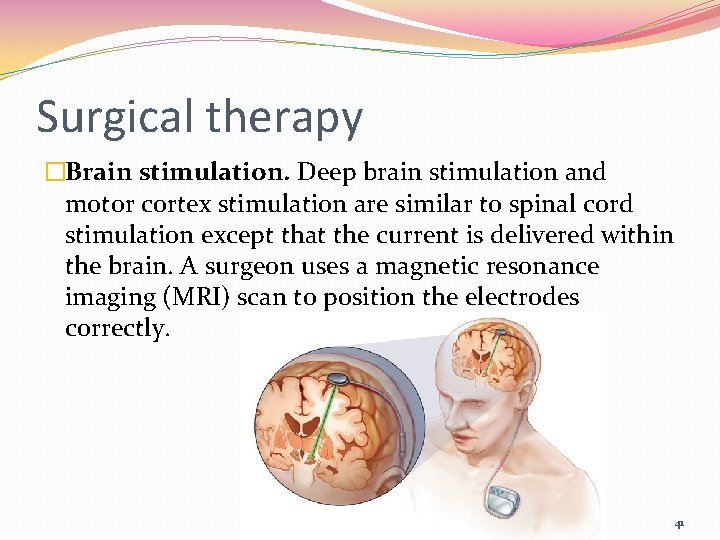
Surgical therapy �Brain stimulation. Deep brain stimulation and motor cortex stimulation are similar to spinal cord stimulation except that the current is delivered within the brain. A surgeon uses a magnetic resonance imaging (MRI) scan to position the electrodes correctly. 41
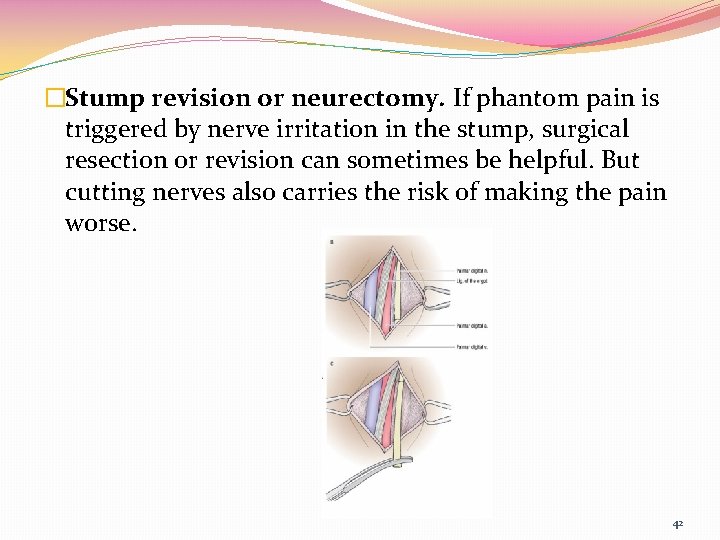
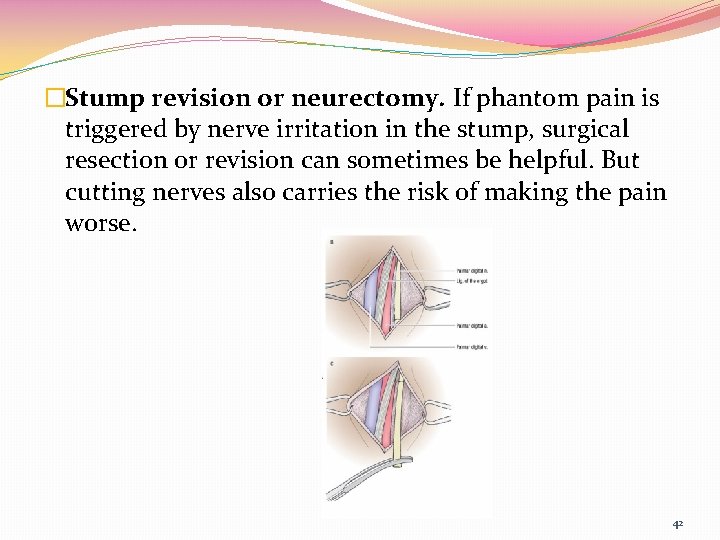
�Stump revision or neurectomy. If phantom pain is triggered by nerve irritation in the stump, surgical resection or revision can sometimes be helpful. But cutting nerves also carries the risk of making the pain worse. 42
Newer approaches to relieve phantom pain �Virtual reality goggles The computer program for the goggles mirrors the person's intact limb, so it looks like there's been no amputation. The person then moves his or her virtual limb around to accomplish various tasks, such as batting away a ball hanging in midair. Although this technique has been tested on only a few people, it appears to help relieve phantom pain 43
�Researchers at University of California, San Diego, reported results of a new study that found amputees find relief from phantom limb pain by simply watching someone else rub their hands together. �The researchers believe the act of watching another person rub their hands together activates the amputee’s brains cells, essentially fooling the brain into thinking the amputee’s missing hand is being massaged. 44
45
THE EFFECT OF ACUPRESSURE ON PHANTOM PAIN IN CLIENT WITH EXTREMITIES AMPUTATION �Z. Pouresmail *, A. Saberi Shaheed Beheshti University of Medical Sciences, Tehran, Iran �Analyzing statistical tests, indicates that acupressure treatment can decrease intensity of phantom pain (p < 0. 0001) and decrease amount of medications (p < 0. 005) and both of hypothesis were accepted. 46
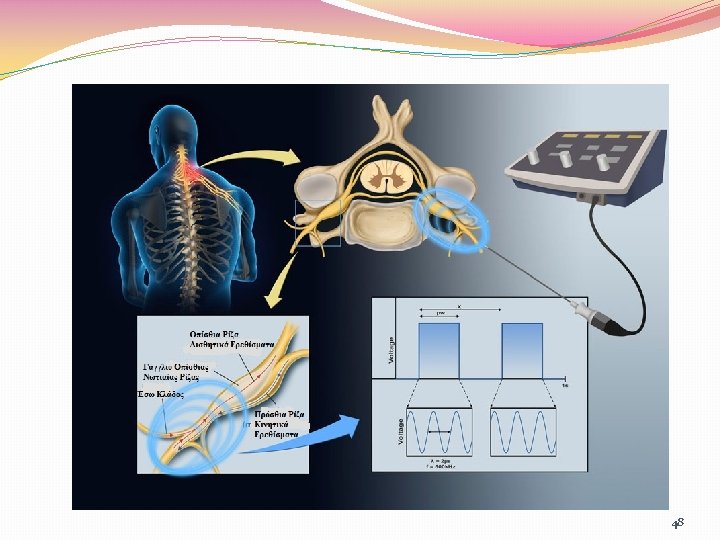
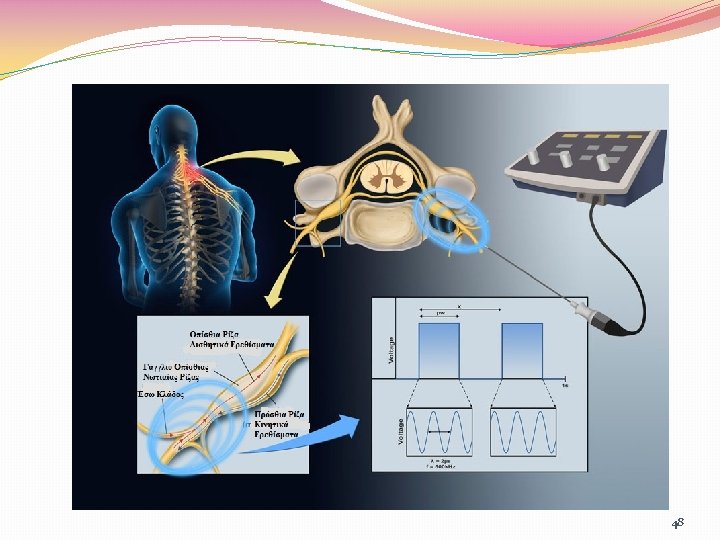
Pulsed Radiofrequency of Lumbar Dorsal Root Ganglion for Chronic Postamputation Phantom Pain �Farnad Imani 1*, Helen Gharaei 1, Mehran Rezvani 1 �Global clinical improvement was good in one patient, with a 40% decrease in pain on the visual analogue scale (VAS) in 6 months, and moderate in the second patient, with a 30% decrease in pain scores in 4 months. � PRF of the dorsal root ganglia at the L 4 and L 5 nerve roots may be an effective therapeutic option for patients with refractory phantom pain. 47
48
Phantom limb pain after amputation in diabetic patients does not differ from that after amputation in nondiabetic patients �There is a commonly held belief that diabetic amputees experience less phantom limb pain than nondiabetic amputees because of the effects of diabetic peripheral neuropathy �Participants with diabetes were further divided into those with long-duration diabetes (>10 years) and those with short-duration diabetes. �Our findings suggest that there is no large difference in the prevalence, characteristics, or intensity of PLP when comparing diabetic and nondiabetic amputees. �prevalence in DM group (82. 0%) and the ND group (89. 4%) (P = 0. 391) 49
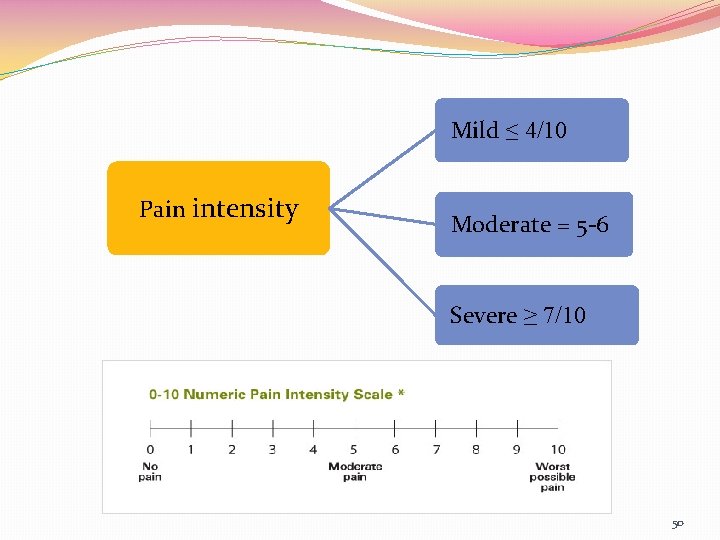
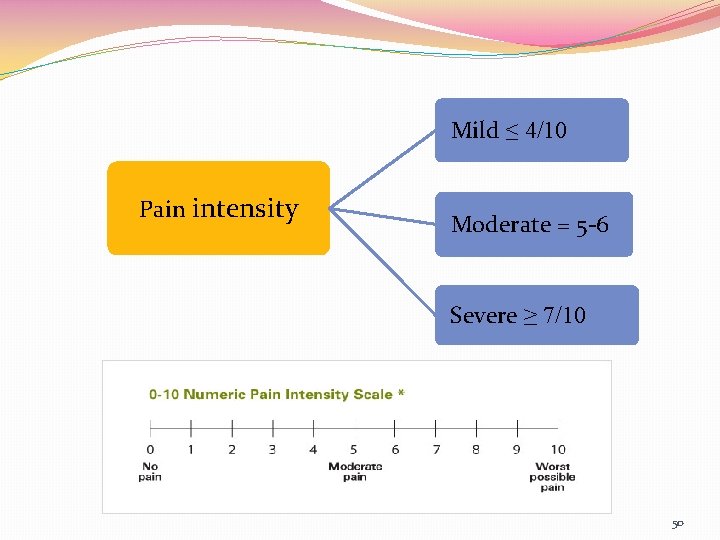
Mild ≤ 4/10 Pain intensity Moderate = 5 -6 Severe ≥ 7/10 50

Timing Acute Chronic ≤ 3 -6 month ≥ 3 -6 month 51
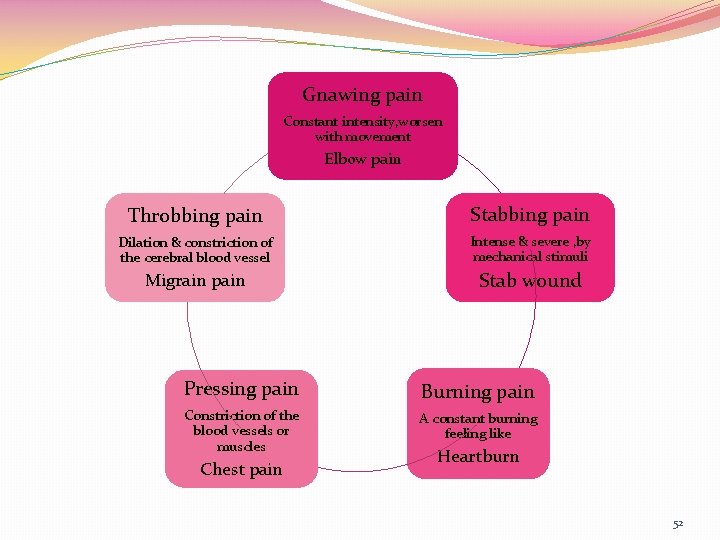
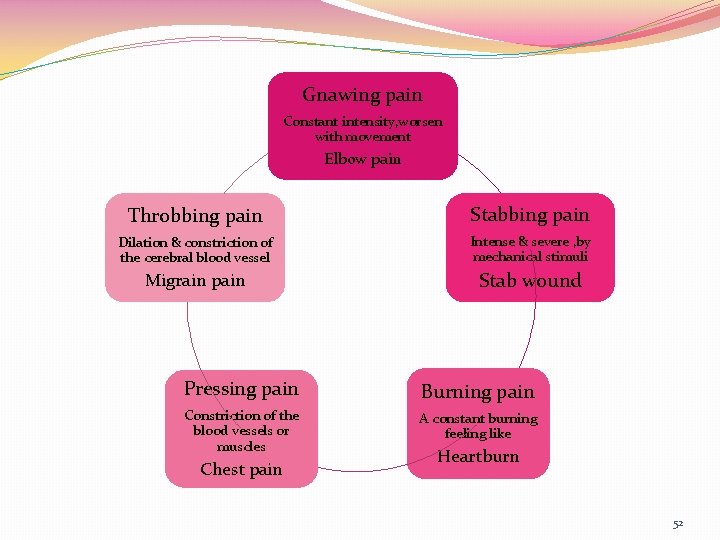
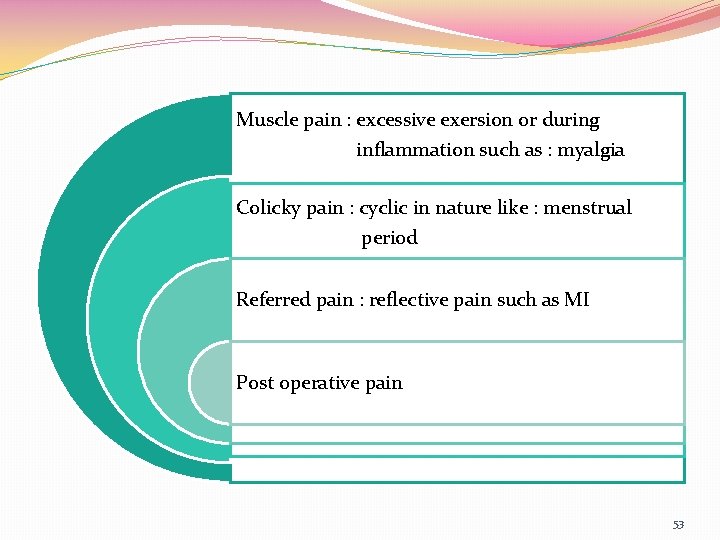
Gnawing pain Constant intensity, worsen with movement Elbow pain Throbbing pain Stabbing pain Dilation & constriction of the cerebral blood vessel Intense & severe , by mechanical stimuli Migrain pain Stab wound Pressing pain Burning pain Constriction of the blood vessels or muscles A constant burning feeling like Chest pain Heartburn 52
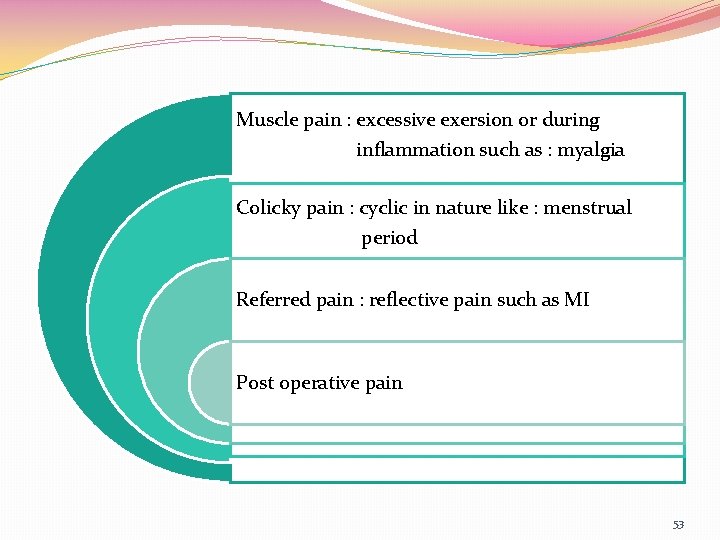
Muscle pain : excessive exersion or during inflammation such as : myalgia Colicky pain : cyclic in nature like : menstrual period Referred pain : reflective pain such as MI Post operative pain 53

Pain Assessment 54
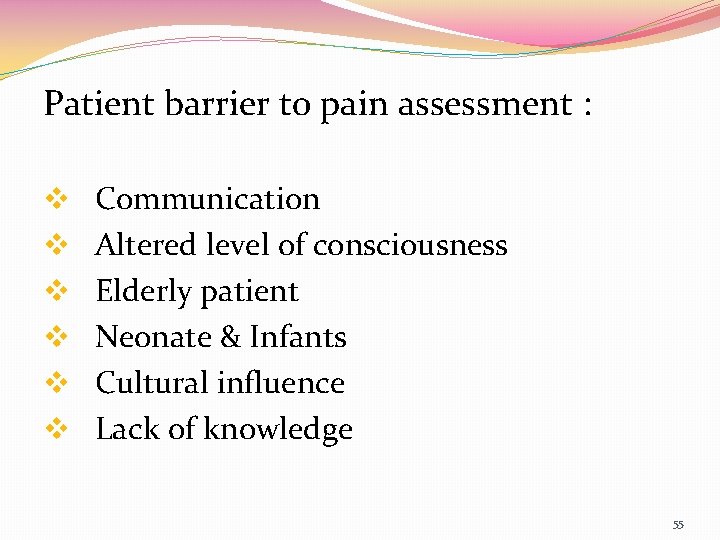
Patient barrier to pain assessment : v Communication v Altered level of consciousness v Elderly patient v Neonate & Infants v Cultural influence v Lack of knowledge 55
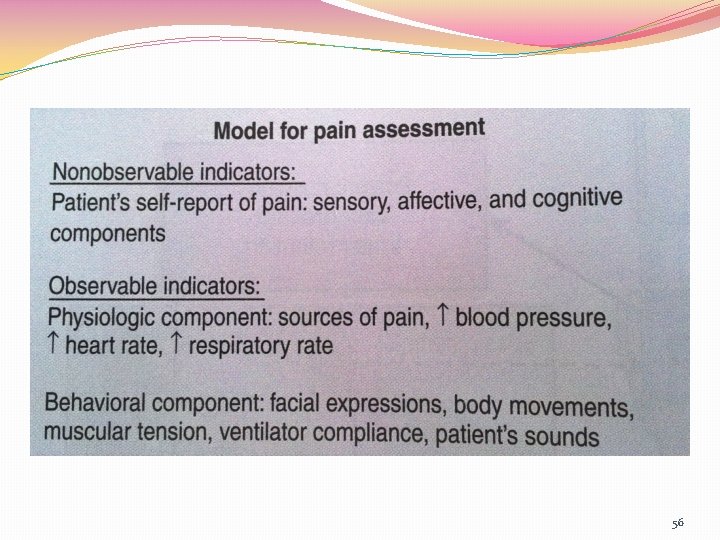
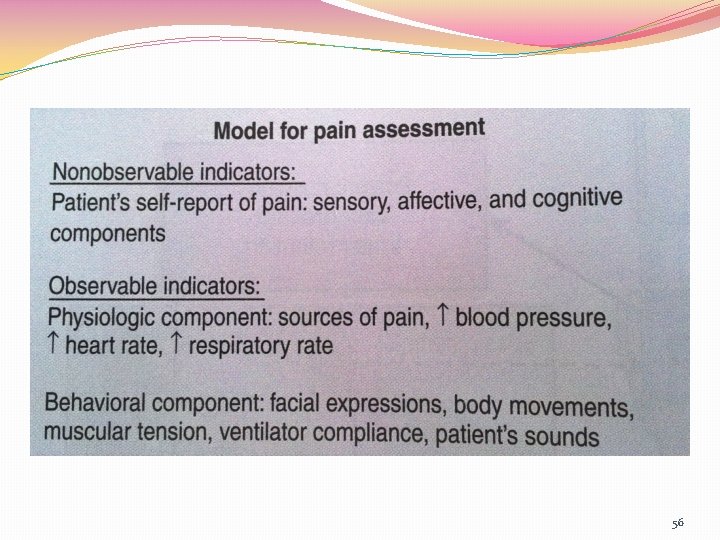
56
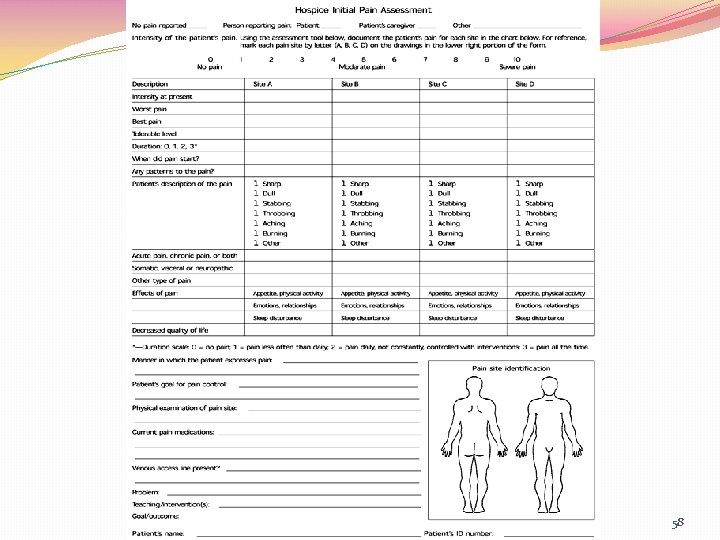
Assessment Tools: 1. Initial pain assessment tool 57
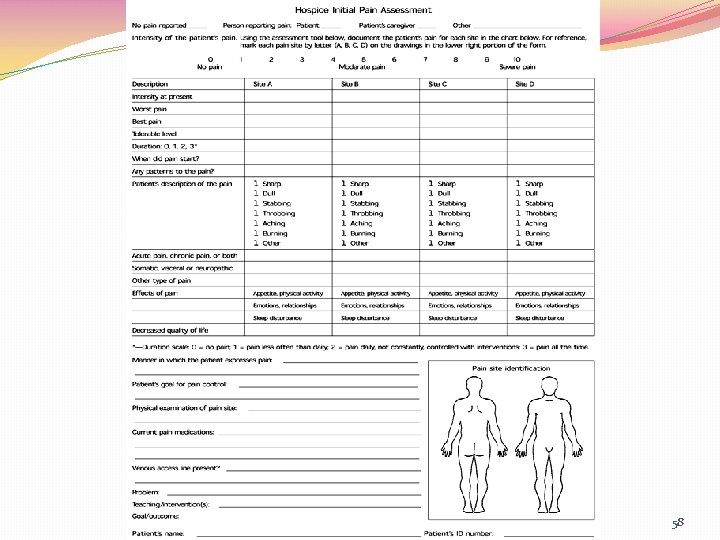
58
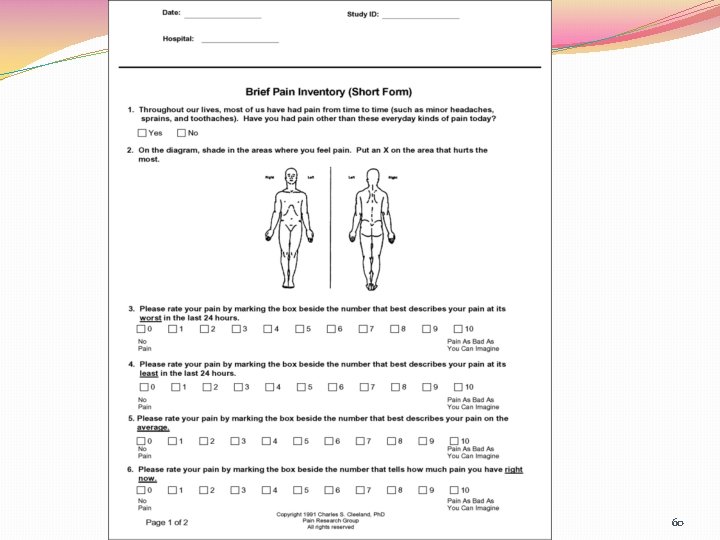
2. Brief pain inventory 59
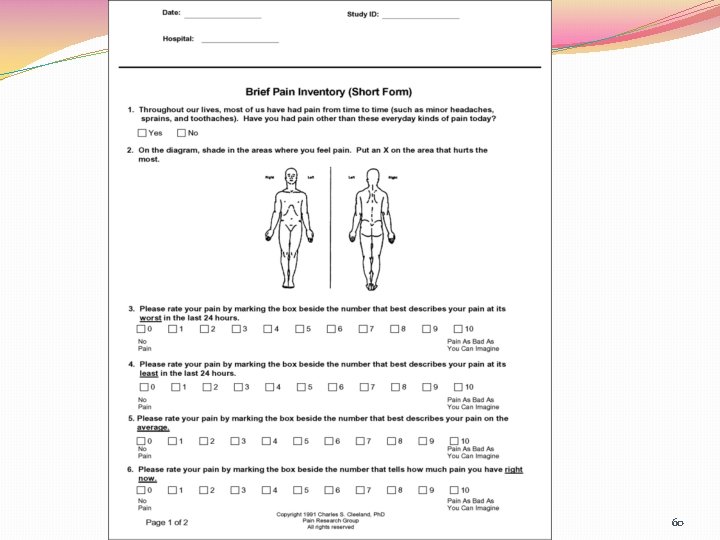
60
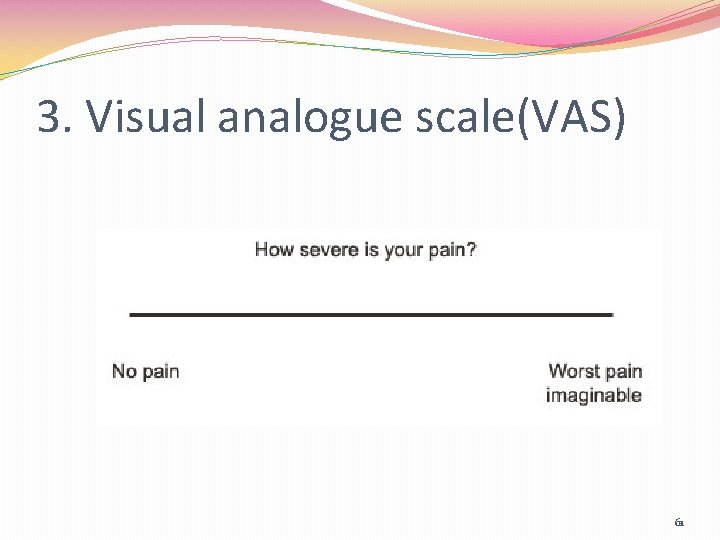
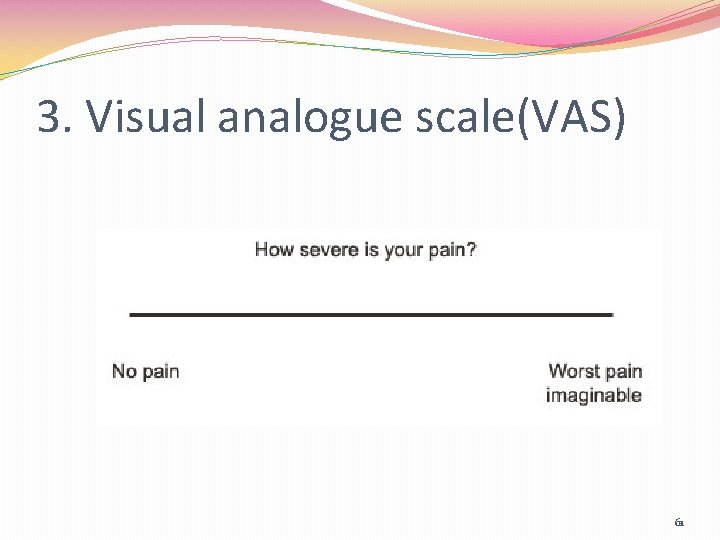
3. Visual analogue scale(VAS) 61
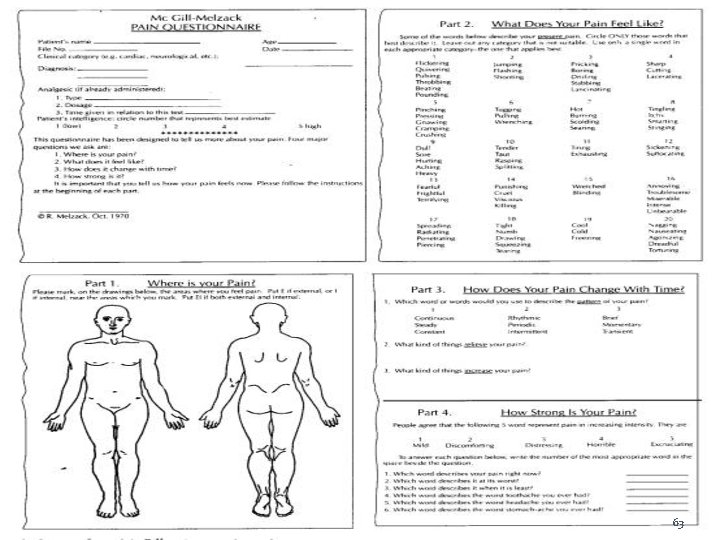
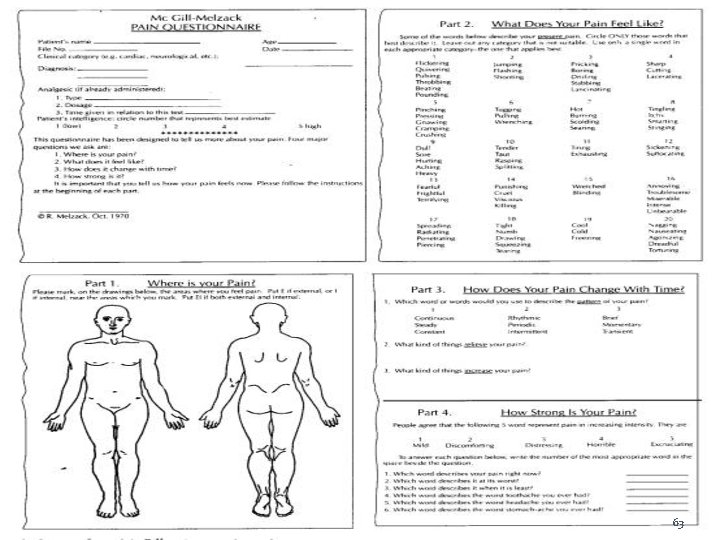
4. Mcgill pain questionnaire �Where is your pain? �What Does Your Pain Feel Like? �How Does Your Pain Change with Time? �How Strong is Your Pain? 62
63
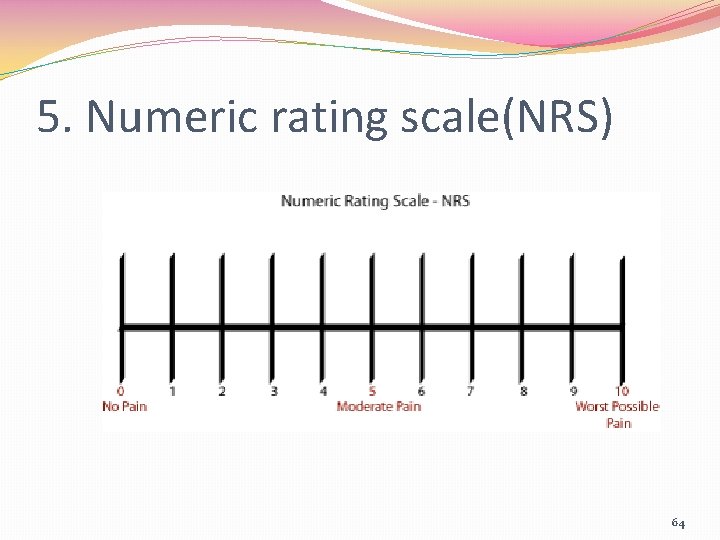
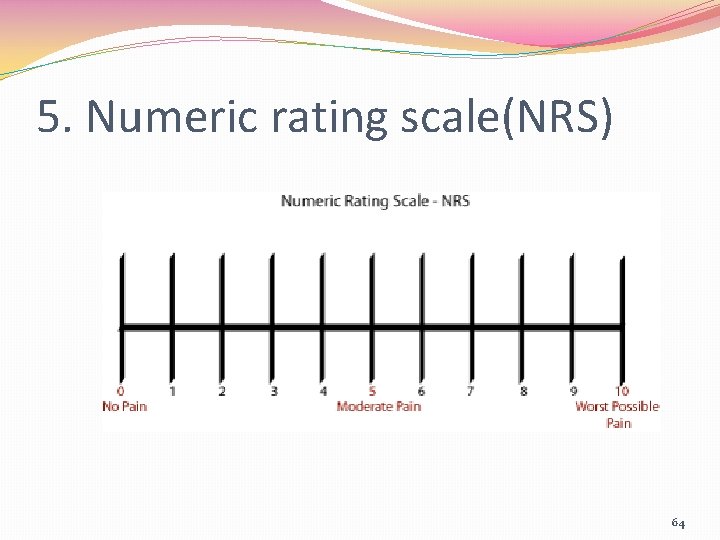
5. Numeric rating scale(NRS) 64
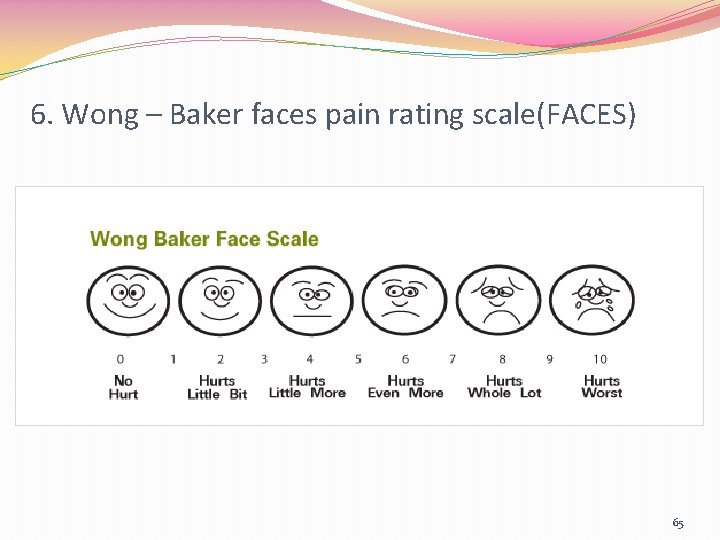
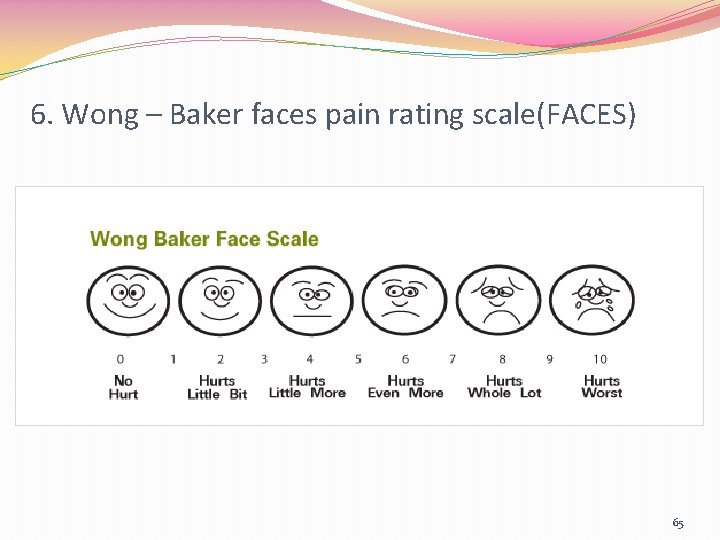
6. Wong – Baker faces pain rating scale(FACES) 65
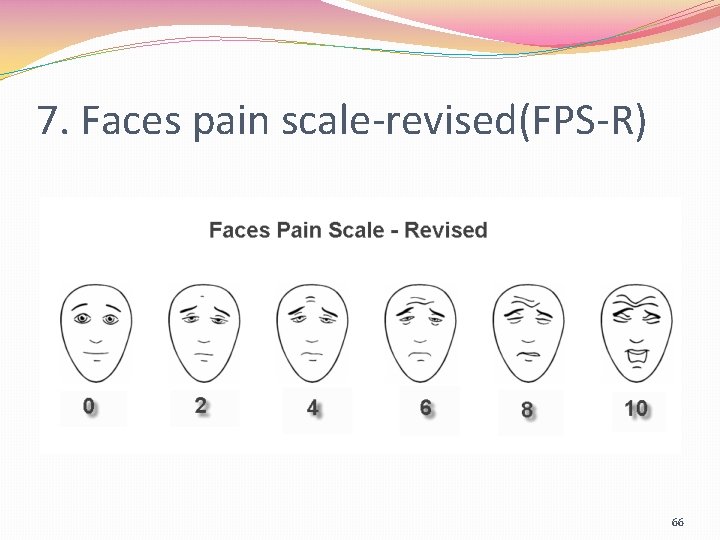
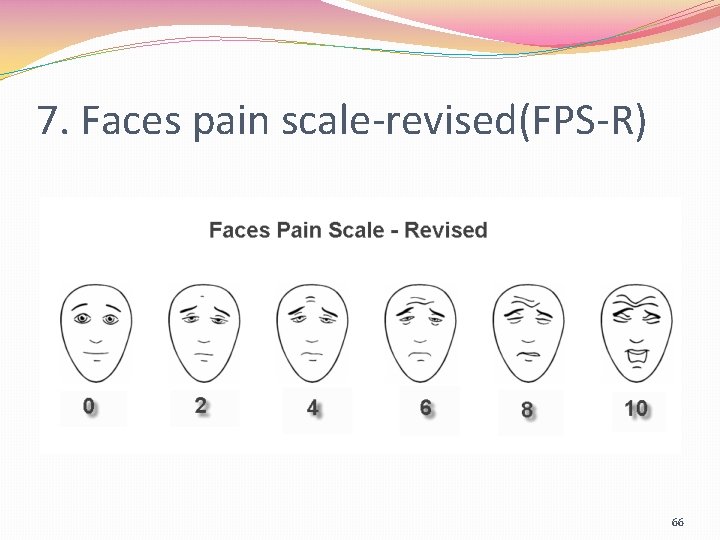
7. Faces pain scale-revised(FPS-R) 66
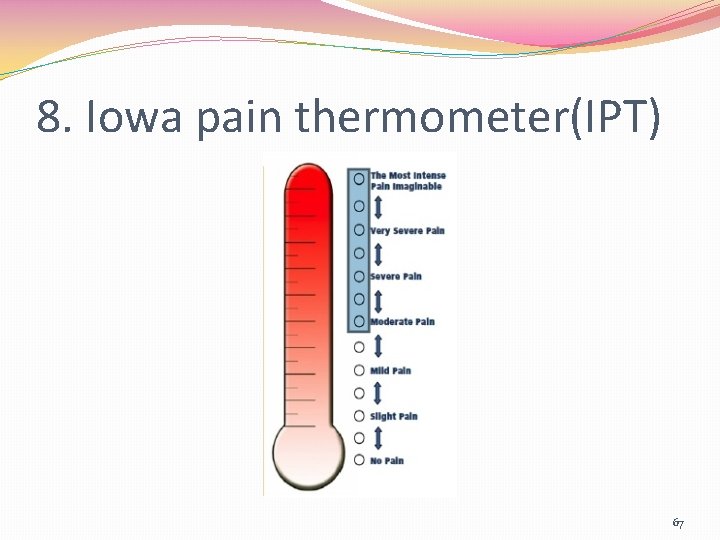
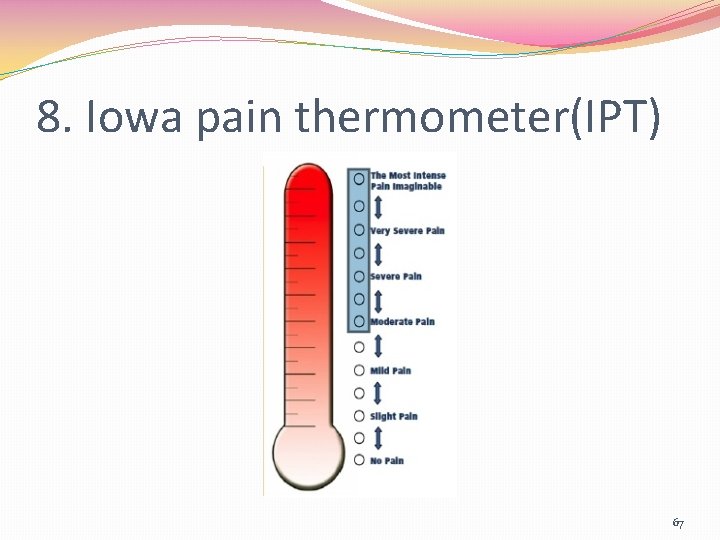
8. Iowa pain thermometer(IPT) 67
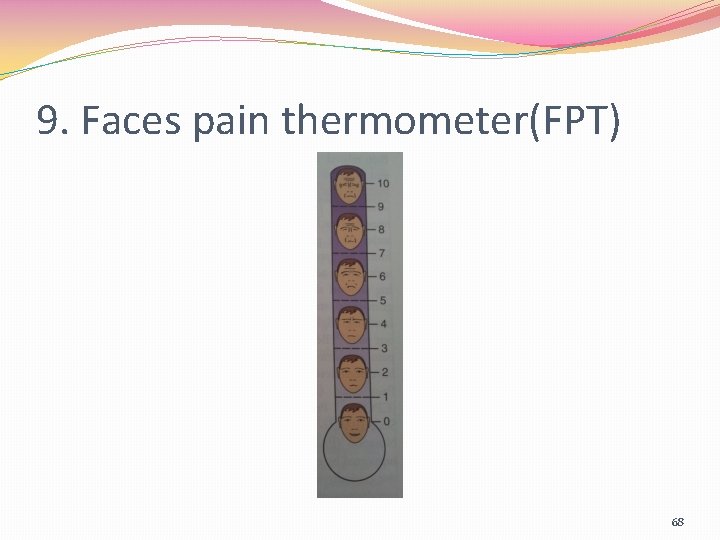
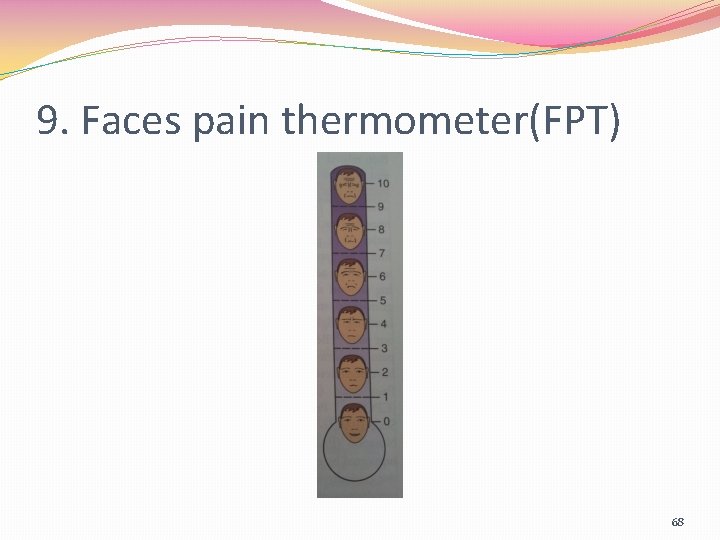
9. Faces pain thermometer(FPT) 68
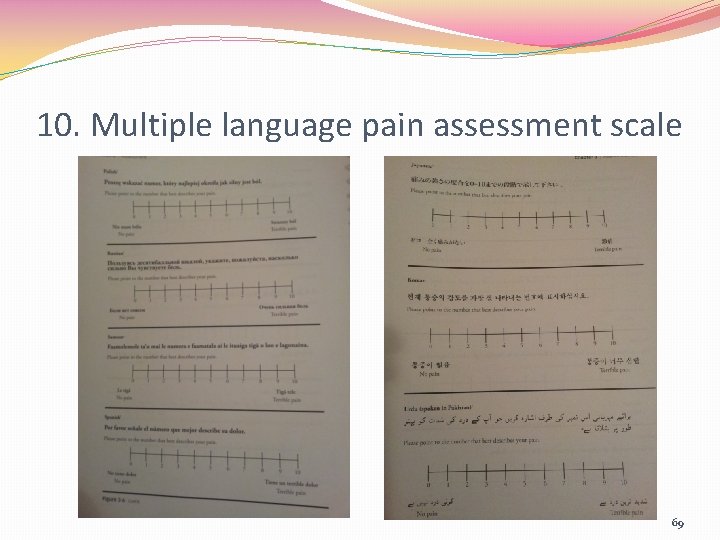
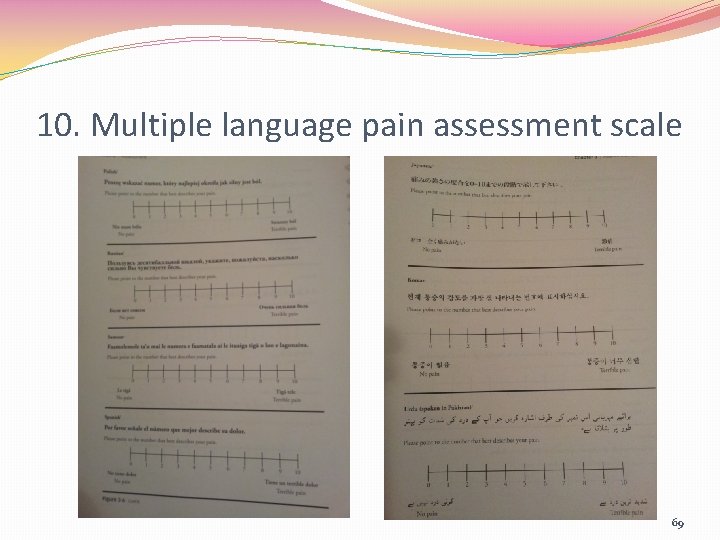
10. Multiple language pain assessment scale 69
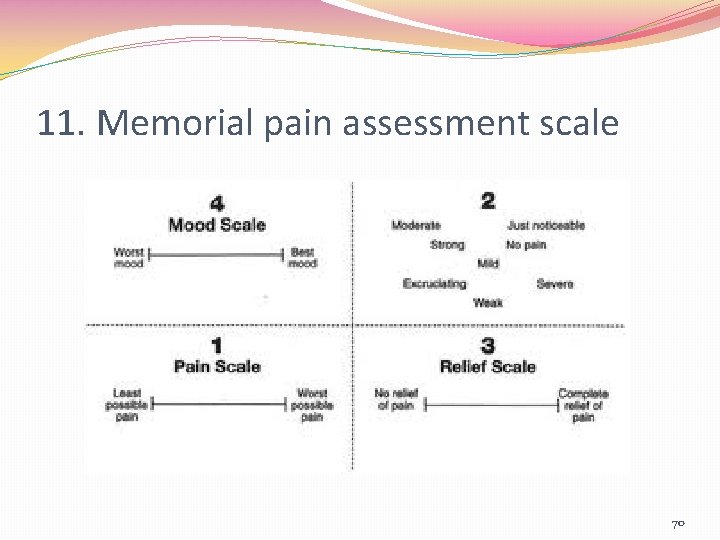
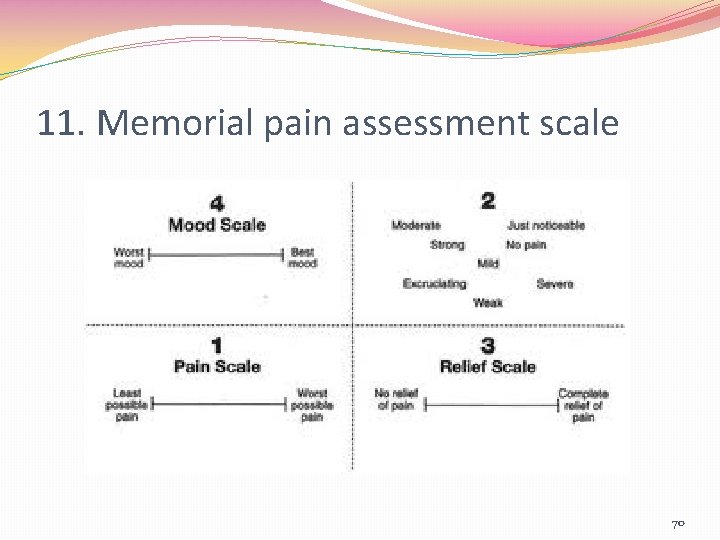
11. Memorial pain assessment scale 70
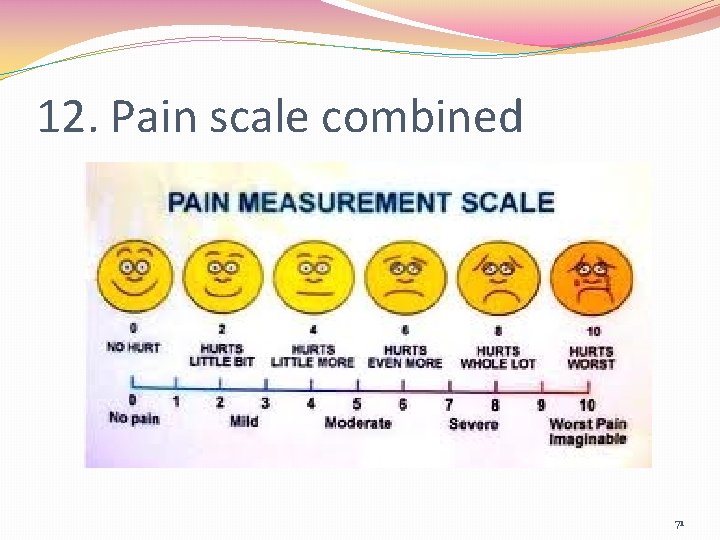
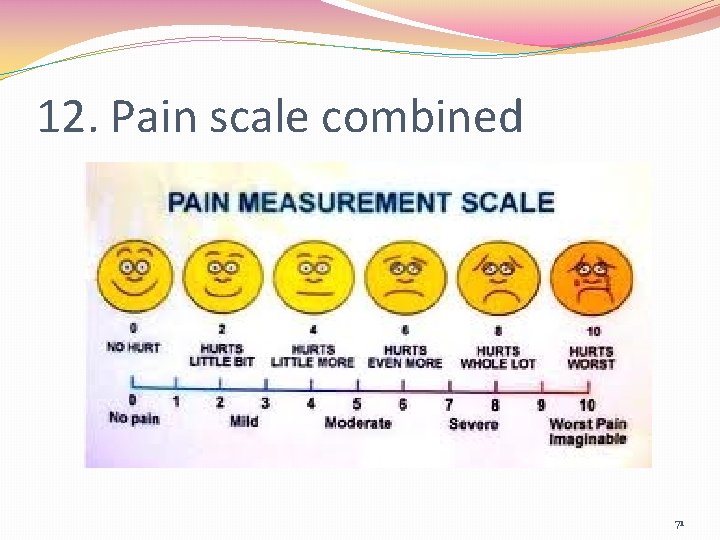
12. Pain scale combined 71
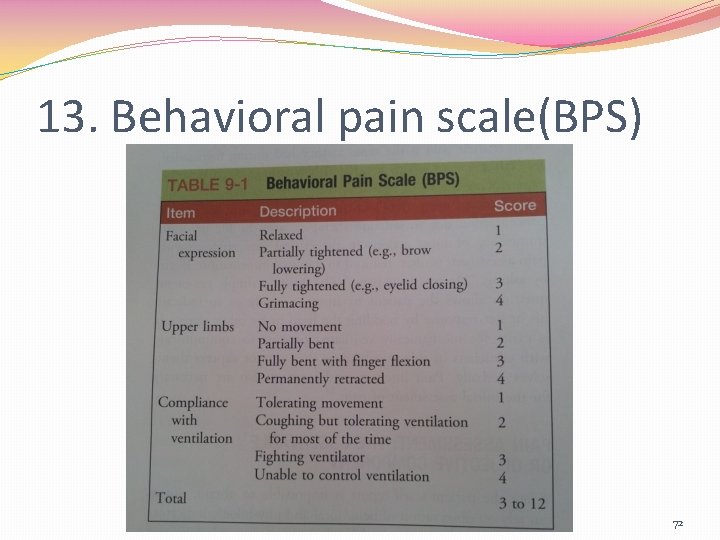
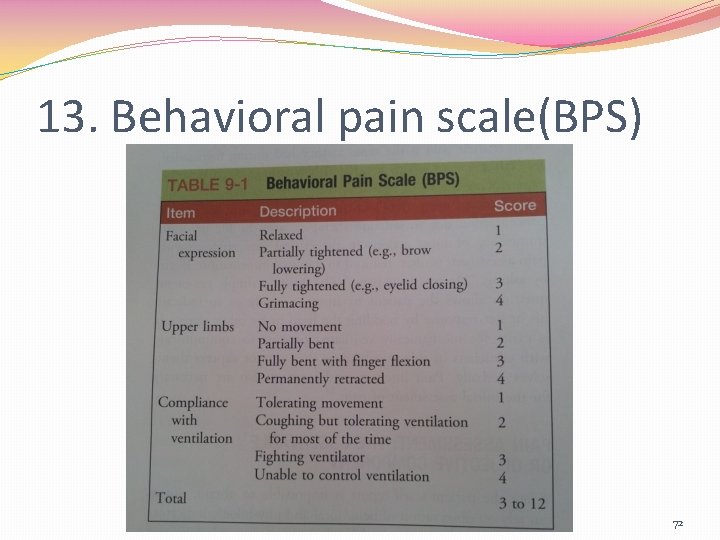
13. Behavioral pain scale(BPS) 72
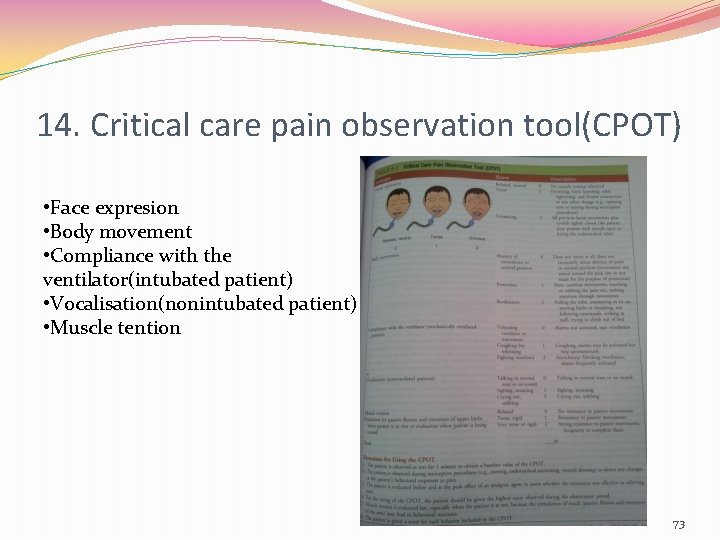
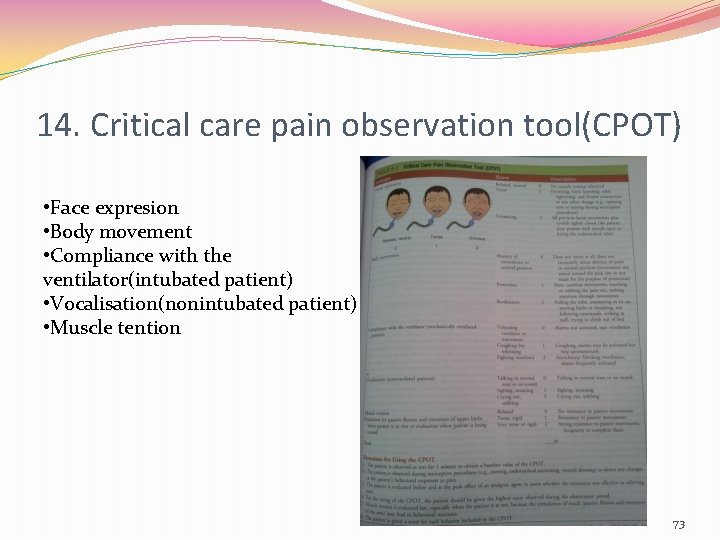
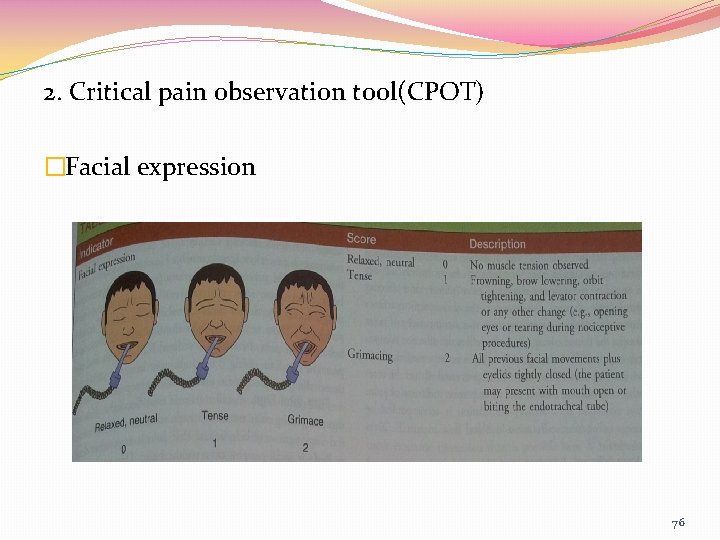
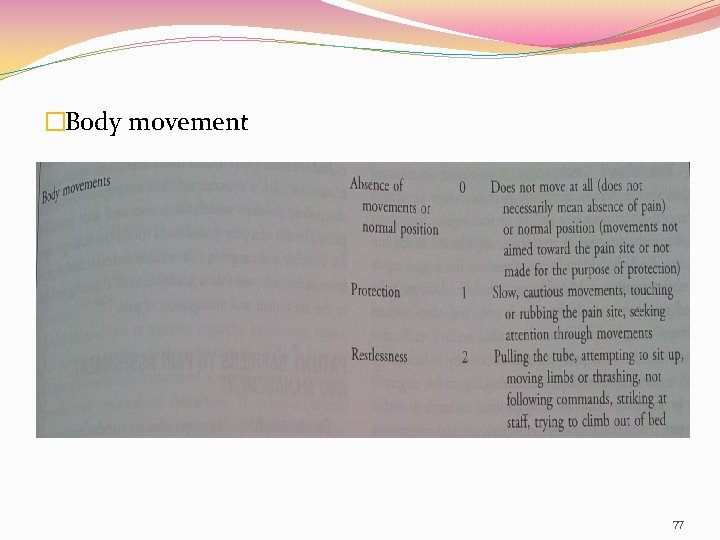
14. Critical care pain observation tool(CPOT) • Face expresion • Body movement • Compliance with the ventilator(intubated patient) • Vocalisation(nonintubated patient) • Muscle tention 73
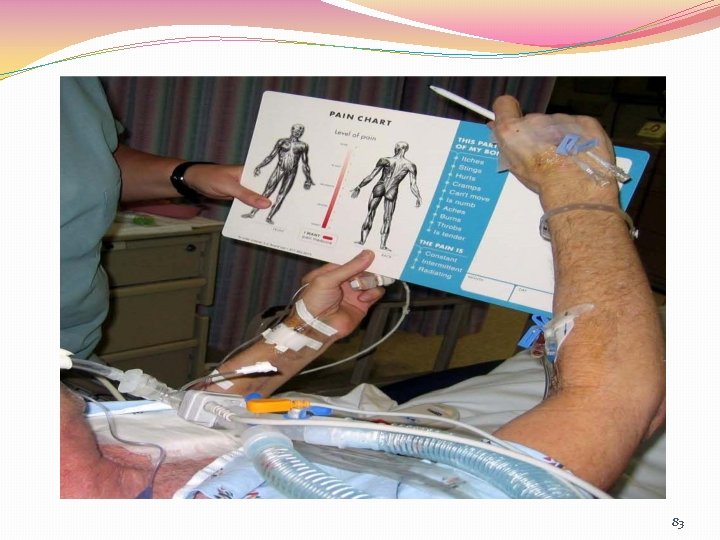
The patient self-report is possible PQRSTU Questionaire : P: Provocative and Palliative or aggravating factors Q: Quality(pain sensation) R: Region or location , Radiation S: Severity and other Symptoms T: Timing(onset, duration, frequency) U: Understanding: patient’s perception of the problem or cognitive experience of pain 74
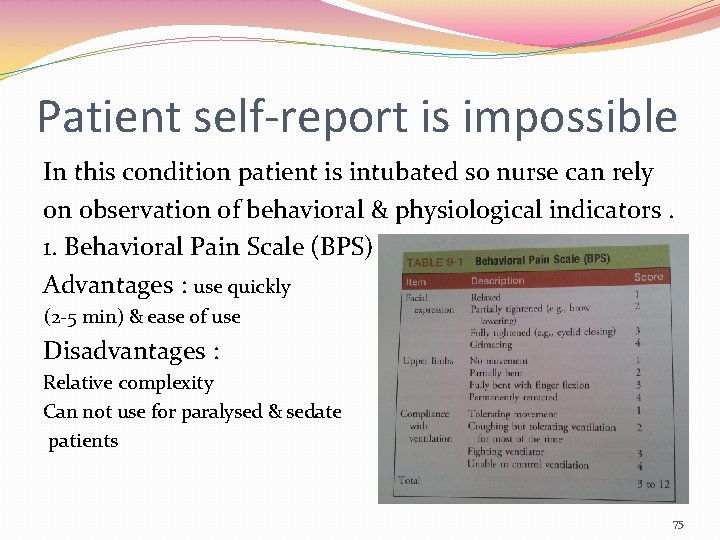
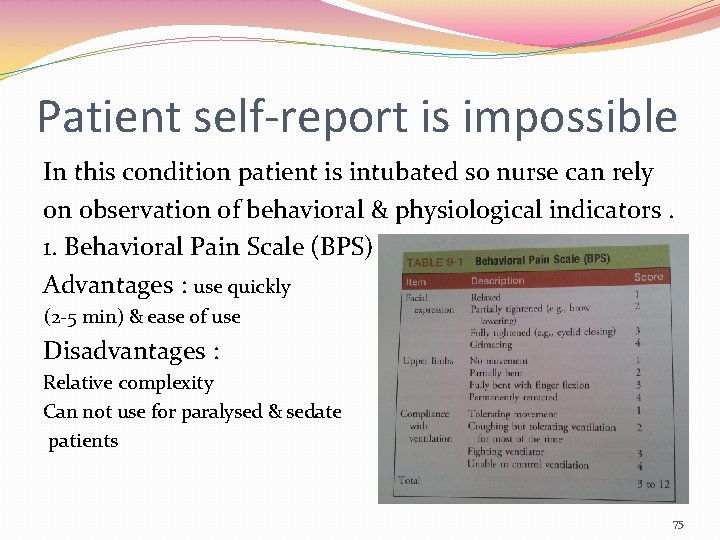
Patient self-report is impossible In this condition patient is intubated so nurse can rely on observation of behavioral & physiological indicators. 1. Behavioral Pain Scale (BPS) Advantages : use quickly (2 -5 min) & ease of use Disadvantages : Relative complexity Can not use for paralysed & sedate patients 75
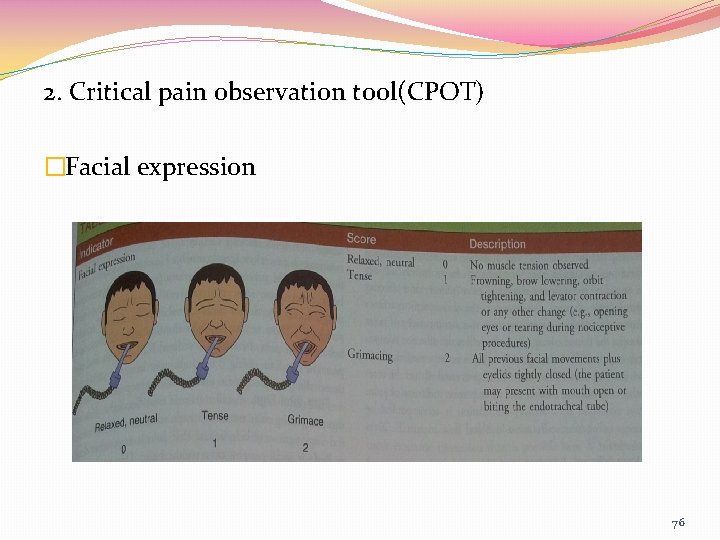
2. Critical pain observation tool(CPOT) �Facial expression 76
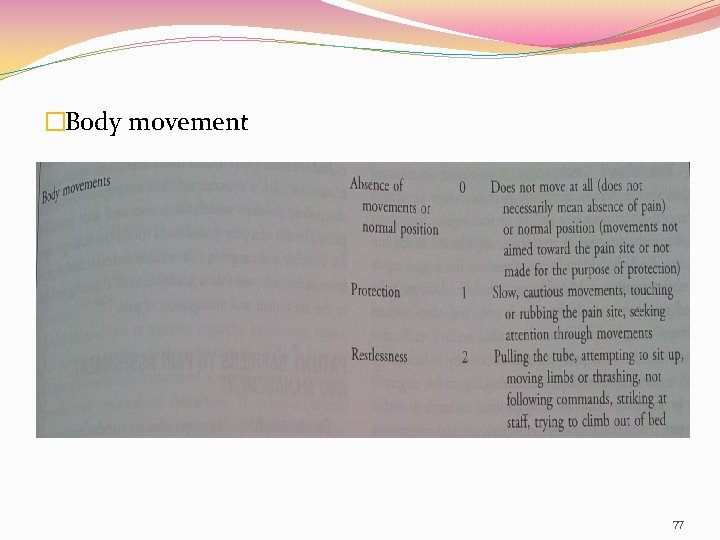
�Body movement 77
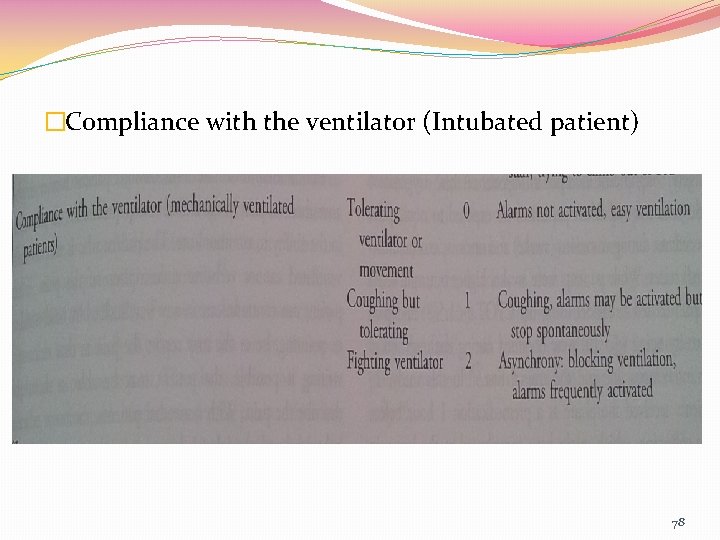
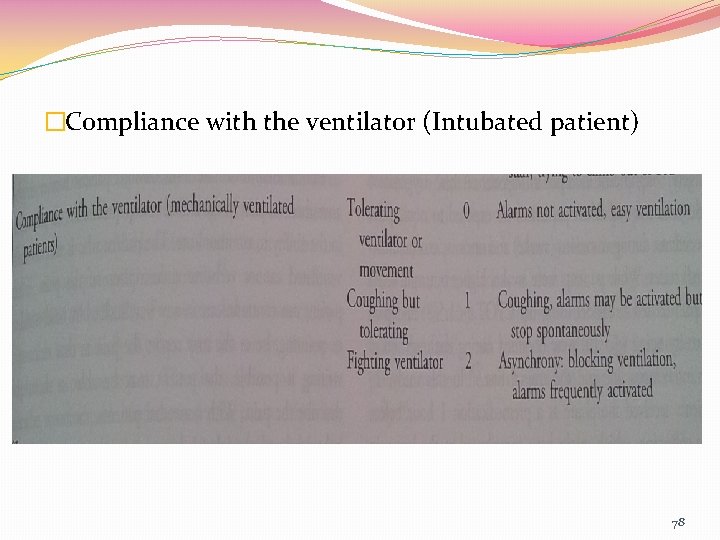
�Compliance with the ventilator (Intubated patient) 78
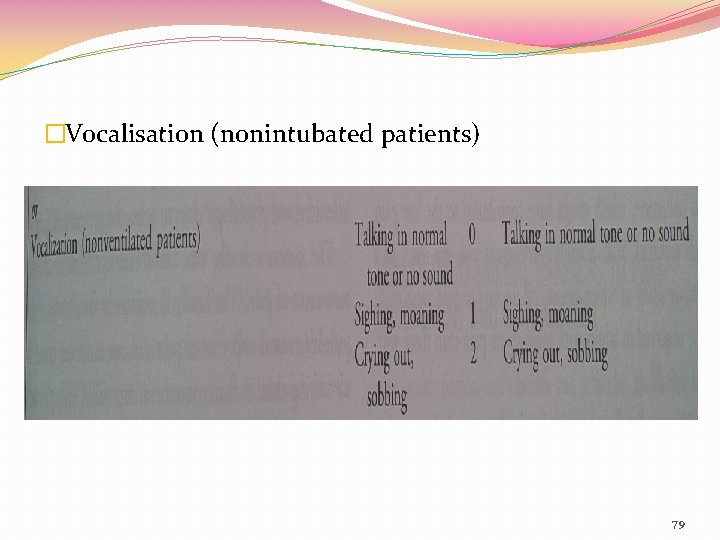
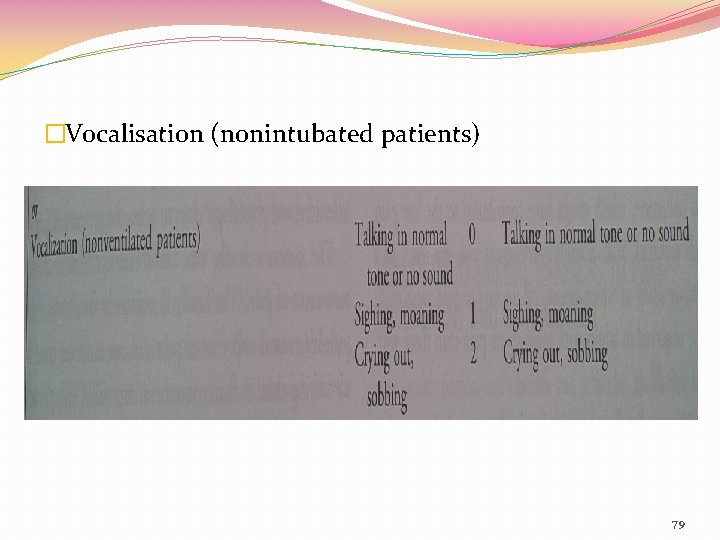
�Vocalisation (nonintubated patients) 79
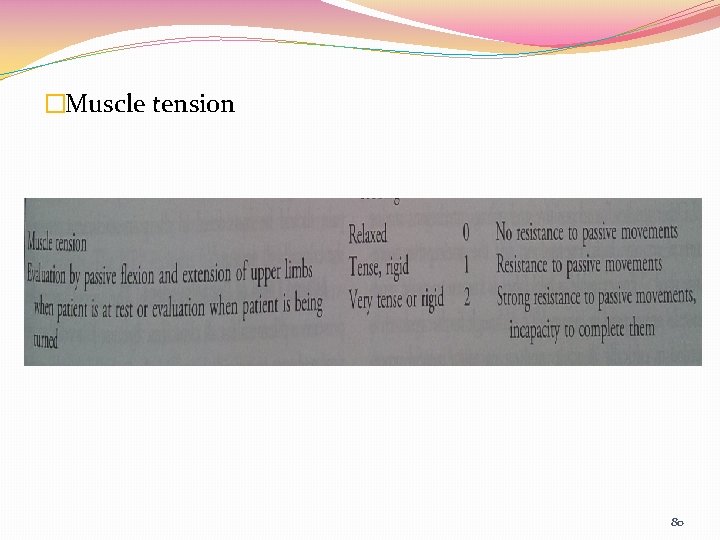
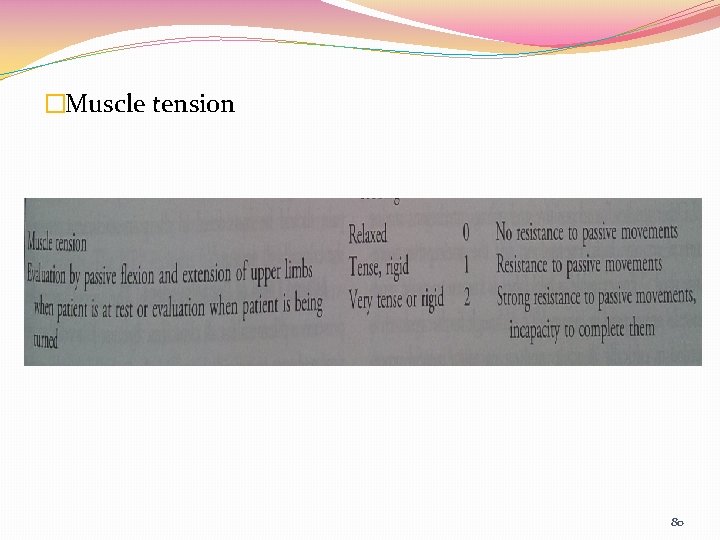
�Muscle tension 80
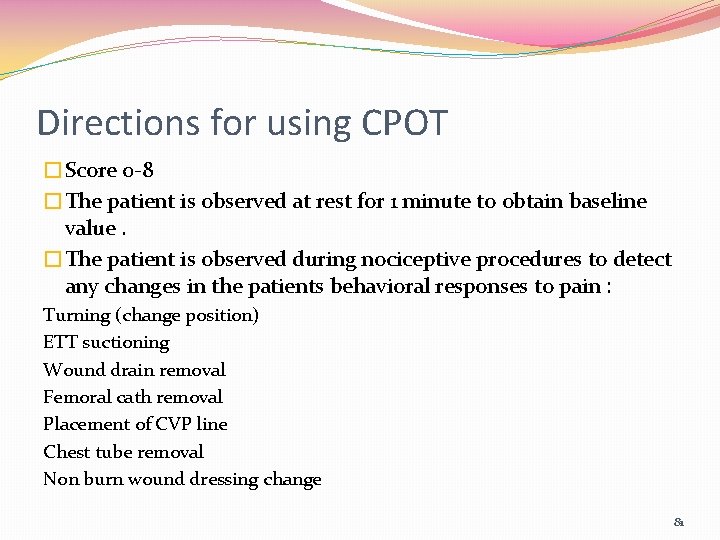
Directions for using CPOT �Score 0 -8 �The patient is observed at rest for 1 minute to obtain baseline value. �The patient is observed during nociceptive procedures to detect any changes in the patients behavioral responses to pain : Turning (change position) ETT suctioning Wound drain removal Femoral cath removal Placement of CVP line Chest tube removal Non burn wound dressing change 81
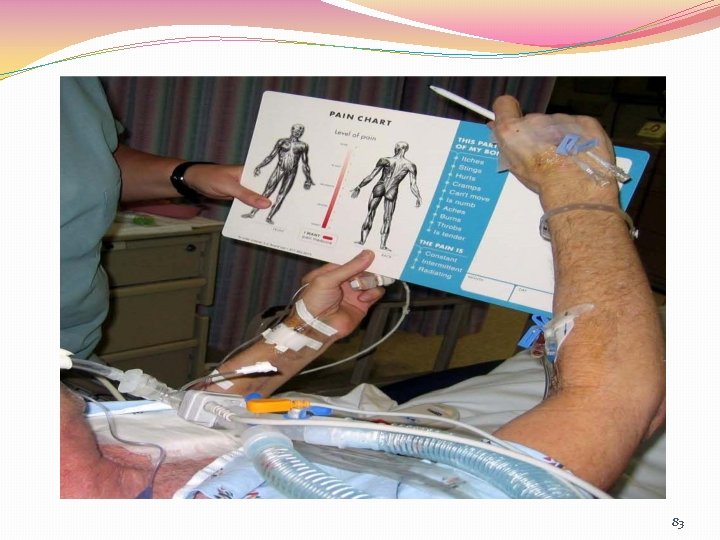
Continued… �The patient is evaluated before and at the peak effect of an analgesic agents. �Muscle tension is evaluated last when patient is at rest �The validity of this scale is recommended by experts �Advantages : ü Quick enough to be used in ICU ü Simple to understand ü Easy to complete ü Helpful for nursing practice 82
83

84

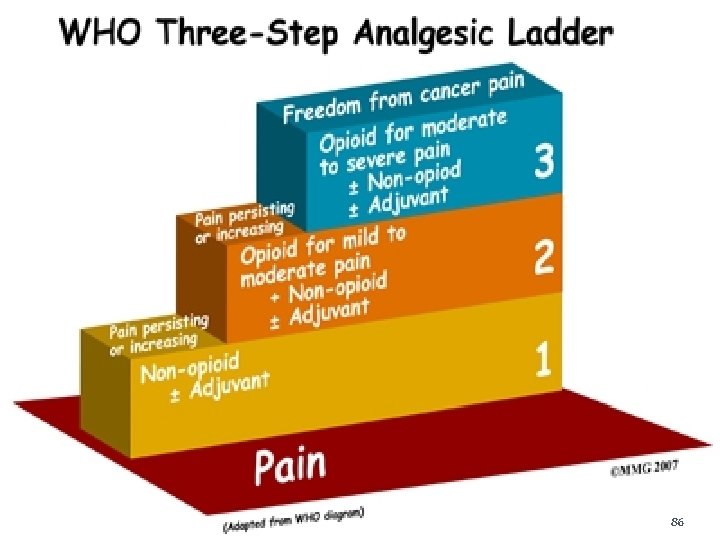
Pharmacologic control �Opioid analgesic Morphin, Fentanyl, Meperidin, Codein, Coffein, Methadon (potent opioid)Remifentanyl & Sufentanyl �Nonopioid analgesic Acetaminophen, NSAID, (adjuvant)Anticonvulsant, Ketamin, Lidocain 85
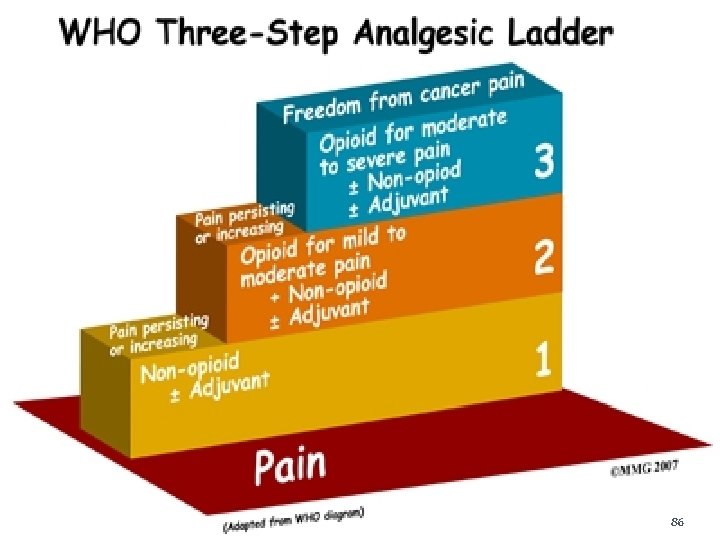
86
Placebo �A placebo is defined as any medication or procedure that produces an effect in patients resulting from its implicit or explicit intent and not from its specific physical or chemical properties (Bok, 1974). �Placebos often take the form of sugar pills, saline injections, miniscule doses of drugs, or sham procedures designed to be void of any known therapeutic value. 87
… placebo �It's well known among doctors that people can get pain relief from a placebo. Now, they're closer to understanding the phenomenon called the placebo effect. �Positive placebo effects may include symptom reduction or improvements in physiological parameters (e. g. , blood pressure) and are believed to be due to mind-body or interpersonal (e. g. , attitude and intent of caregiver) factors (Arnstein, 2003). �Negative placebo effects, ranging from minor discomforts to life-threatening complications. 88
… placebo �When the placebo was used, the response of the brain's pain-sensing regions was ratcheted down. �These studies showed "placebo effect patterns" in the prefrontal cortex. The prefrontal cortex is the brain region that becomes activated in anticipation of pain relief which triggers a reduction of activity in painsensing areas of the brain. �This interplay within the prefrontal cortex may trigger a release of pain-relieving opioids in the midbrain. 89
Surgical control �Rhizotomy It is a term chiefly referring to a neurosurgical procedure that selectively destroys problematic nerve roots in the spinal cord, most often to relieve the symptoms of neuromuscular conditions such as spastic cerebral palsy. rhizotomy precisely targets and destroys the damaged nerves that don’t receive gamma amino butyric acid, which is the core problem for people with this desease. 90
�Cordotomy It is a surgical procedure that disables selected painconducting tracts in the spinal cord, in order to achieve loss of pain and temperature perception. For patients experiencing severe pain due to cancer or other diseases for which there is currently no cure Cordotomy is usually done percutaneously with fluoroscopic guidance while the patient is under loca anesthesia. 91
�Intercostal nerve block An intercostal nerve block is an injection of a steroid or other medication around the intercostal nerves that are located under each rib. It reduces pain, and other symptoms caused by inflammation or irritation of the intercostal nerve and surrounding structures. Herpes zoster or shingles pain in the chest Pain around a chest scar after a chest surgery 92
Delivery Methods �PCA(Patient-Controlled Analgesia) 93
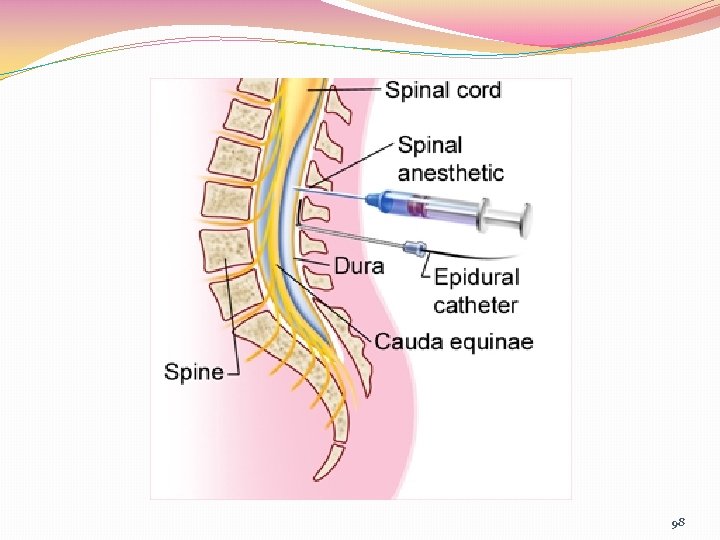
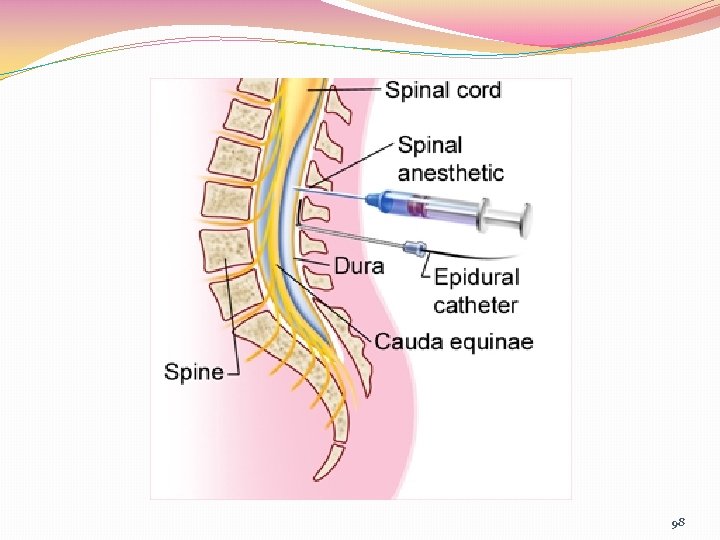
Spinal Analgesia(Subarachnoid, Intrathecal) v Injection of analgesic in to the cerebral spinal fluid with a fine needle. v As a means of reducing pain for chronic medical condition or lower back injury. v Injection below the abdomen wide awareness v Injection higher spinal affect the respiratory muscle(paralyze) no consciousness v Complication immediate (operation room) late(ward, PACU) 94
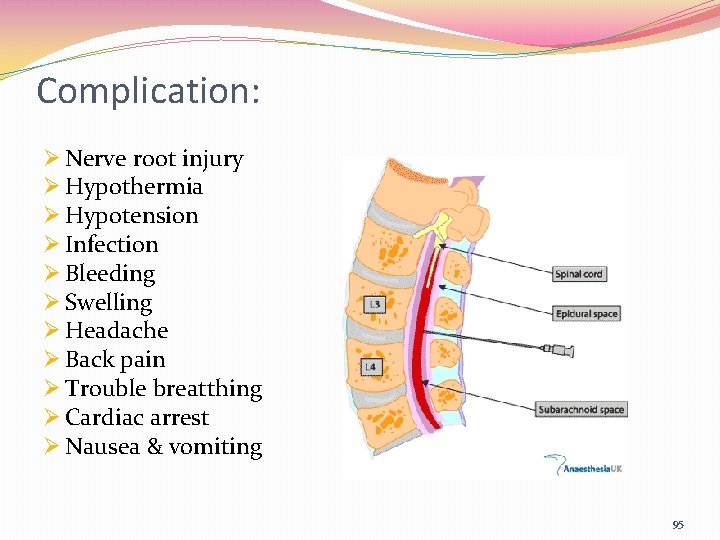
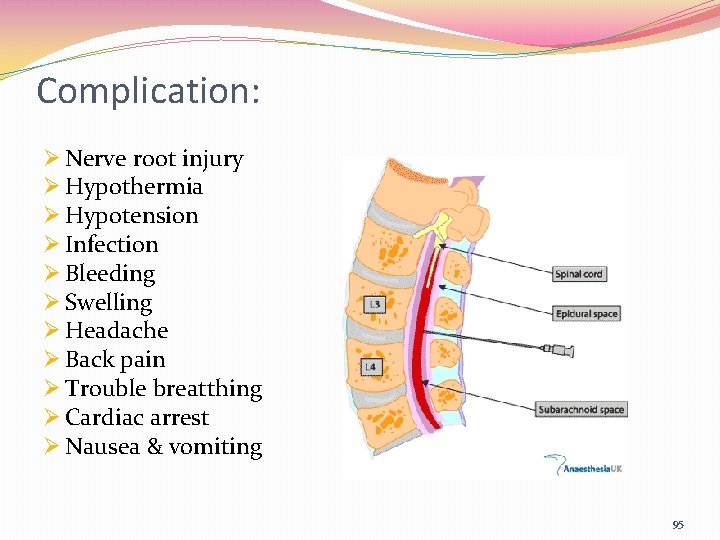
Complication: Ø Nerve root injury Ø Hypothermia Ø Hypotension Ø Infection Ø Bleeding Ø Swelling Ø Headache Ø Back pain Ø Trouble breatthing Ø Cardiac arrest Ø Nausea & vomiting 95
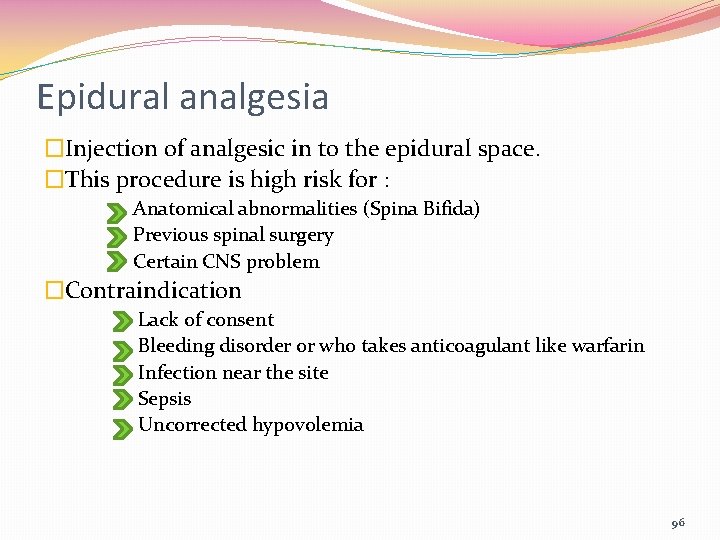
Epidural analgesia �Injection of analgesic in to the epidural space. �This procedure is high risk for : Anatomical abnormalities (Spina Bifida) Previous spinal surgery Certain CNS problem �Contraindication Lack of consent Bleeding disorder or who takes anticoagulant like warfarin Infection near the site Sepsis Uncorrected hypovolemia 96
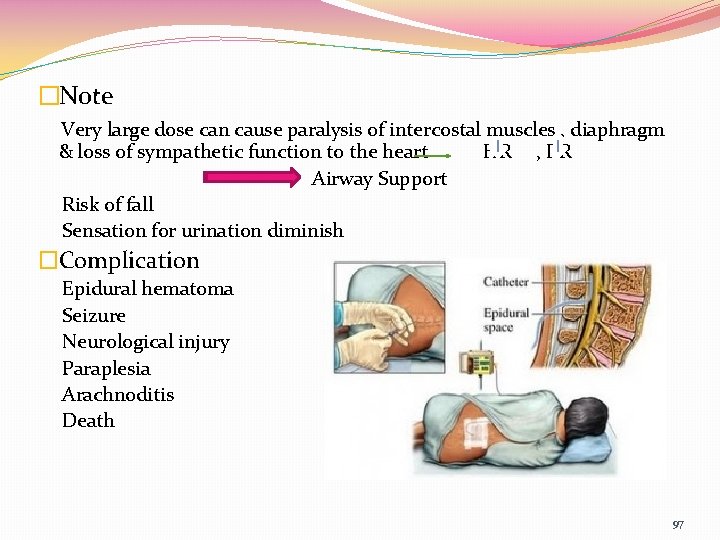
�Note Very large dose can cause paralysis of intercostal muscles , diaphragm & loss of sympathetic function to the heart HR , RR Airway Support Risk of fall Sensation for urination diminish �Complication Epidural hematoma Seizure Neurological injury Paraplesia Arachnoditis Death 97
98
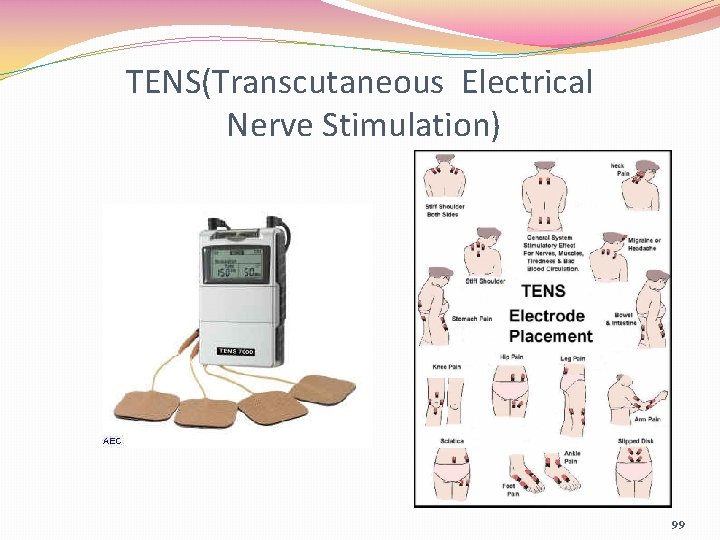
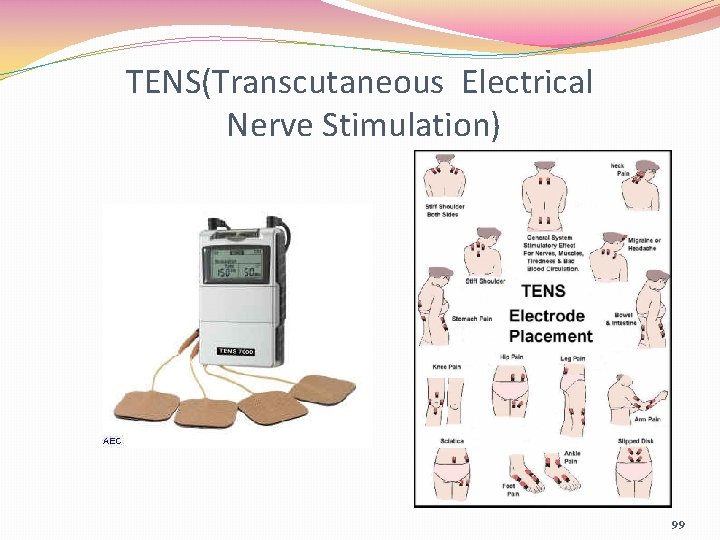
TENS(Transcutaneous Electrical Nerve Stimulation) 99
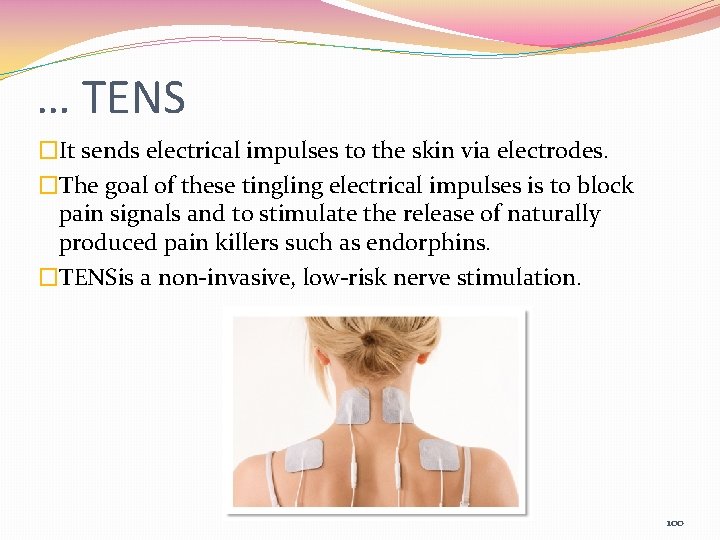
… TENS �It sends electrical impulses to the skin via electrodes. �The goal of these tingling electrical impulses is to block pain signals and to stimulate the release of naturally produced pain killers such as endorphins. �TENSis a non-invasive, low-risk nerve stimulation. 100
… TENS �Control of acute or chronic pain �Management of postsurgical pain �Reduction of post-traumatic acute pain 101
Nonpharmacologic Control 102
Guidelines for Individualizing Pain Relief �Establish a relationship of mutual trust �Use different types of pain-relief measures �Provide pain-relief measures before pain becomes severe. �Consider the client’s ability or willingness to participate in pain-relief measures. �Choose pain-relief measures on the basis of the client’s behavior reflecting the severity of pain. �Use measures that the client believes are effective. 103
… guideline �If therapy is ineffective at first, encourage the client to try it again before abandoning it. �Keep an open mind about what might relieve pain �Keep trying �Protect the client �Educate the client about pain 104
Educational approaches �Recognize and reduce stigma attached with chronic pain �Recognize and reduce stigma attached with use of pain medications �Assist client to explore personality traits and impact upon pain �Recognize the impact upon pain of catastrophizing and fear of pain �Help client develop an acceptance of pain and to move from a passive to an active orientation in addressing their pain 105
… educational approach �Address sleep hygiene and the utilization of diaphragmatic breathing and self-hypnosis skills �Recognize and reduce client isolation �Encourage and foster interpersonal support systems �Emphasize importance of physical conditioning and general good health habits 106

107
Geriatric Consideration � They accept pain as a normal & unavoidable with aging. � They may not demonstrate objective signs & symptoms because of years of adaptation & increased pain tolerance. � The effect of opioid analgesic are prolonged because of decreased metabolism & clearance of drug. � Take multiple drugs side effects drugs be started at a lower dosage � Monitoring drugs interaction is necessary. � Taking drugs with toxic metabolism that excrete renally shoild be avoided esp in those who are at risk for renal insufficiency. 108
Pediatric Considerations �Studies have shown that, when adults and children undergo the same surgery, children are under medicated. In one study, 52% of the children received no analgesic postoperatively, whereas the remaining 48% received aspirin or acetaminophen. �Maturational and chronologic age, cause of pain, coping style, parental response, culture, past pain experiences, and whether pain is acute or chronic influence the child’s response to pain. 109
… pediatric considerations Infant �Associates environment with painful experience �Cries loudly and makes verbal protests long after the stimulus is withdrawn Toddler �Fears body intrusion �Does not understand rationale for pain or have ability to conceptualize the duration of the experience, even if told �Seeks out parental figures as a source of comfort 110
… pediatric considerations Pre-schooler �Engages in magical thinking or fantasies (e. g. , believes something they thought or did caused the pain) �Uses increased verbal skills to communicate pain �Has limited understanding of time �After pain passes, talks to toys or other children about the pain experience �Denies pain, especially if he or she associates it with adverse consequences (e. g. , injection, ridicule if not brave) 111
… pediatric considerations School-Aged �Fears body injury �Can describe the cause, type, quality, and severity of pain �Can rate the severity of pain �Attempts to relate the pain experience to previous events and gain control over actions �Denies pain, especially if he or she associates it with adverse consequences �May be influenced by presence of parents in expressing pain 112
… pediatric considerations Adolescent �Considers body image as very important �May use overconfidence to compensate for fear �May use more “socially acceptable” behavioral responses to pain than do younger children, but fear and anxiety are not decreased �May be influenced by presence of parents in expressing pain 113
Nursing diagnosis �Decreased pain tolerance related to : disbelief from others and uncertainty of prognosis fatigue fear(exp of addiction , loss of control) monotony financial & social stressors lack of knowledge 114
Disbelief from others � Stablish a supportive accepting relationship acknowledge the pain listen attentively to the client’s discussion of pain � Assess the family for any misconception about pain or its treatment explain the concept of pain as an individual experience discuss factors related to increased pain & options to manage encourage family members to share their concerns privately 115
Lack of knowledge / uncertainty �Explain the cause of the pain , if known �Explain the severity of the pain & how long it will last �Explain the diagnostic tests & procedures in detail 116
Fear �Provide accurate information to reduce fear of addiction �Assist in reducing fear of losing control Include the client in setting a realistic pain goal Provide privacy for the client’s pain experience Attempt to limit the number of health care providers who provide care allow the client to share intensity of pain Involve the social worker or case manager if social or financial concerns exist 117
Fatigue �Determine the cause of fatigue (sedatives , analgesics , sleep deprivation) �Explain that pain contributes to stress which increases the fatigue �Assess present sleep pattern & the influence of pain on sleep �Provide opportunities to rest during the day & with period of uninterrupted sleep at night �Consult with physician for an increases dose of pain medication at bedtime 118
Monotony �Discuss with the client and family to use distraction method for relief (watching TV , listening to music…) �Vary the environment if possible 119
Some desired outcome �The client will experience diminished pain as evidenced by : Verbalization of decrease in or absence of pain Relaxed facial expression and body positioning Increased participation in activities Stable vital signs 120
Other diagnosis �Anxiety, fear, crisis reaction, stress �Impact on spirituality and meaningfulness; hope and hopelessness �Psychological effect of unrelieved pain on perceptions of control and self-efficacy �Depression, wish to die, suicidal risks, grief �Impact of persistent pain on habits, roles, occupational performance, and future quality of life �Personality and gender influences on pain experience 121
… other diagnosis �Loss of activity: vocational, recreational, related to family �Loss of identity: reassessing self image, grieving lost abilities, reassessing relationships and roles 122
123
Case report �Brief patient history Ms Nikjoo is a 63 y/o woman with type 2 DM & peripheral arterial occlusive disease with neuropathy. She is disabled because of limited mobility & chronic pain associated with lower extremity claudication & neuropathic pain. Her pain has been managed with gabapentin 600 mg TDS & 3 mg morphine PRN. �Clinical assessment She is admitted to the ICU after an 8 hr surgical revascularization of the right lower extremity. She is awake , alert & oriented. she complains of right lower extremity & bilateral foot pain. Her skin is warm and dry & the sensation to touch is intact and she is able to move her toes on command however she is complaining of severe burning on both feet. 124
�Diagnostic procedure She reports that her pain is a 10 on the Baker-Wong Faces Scale. �Medical diagnosis The diagnosis is acute postoperative incisional pain superimposed on chronic neuropathic pain involving both lower extremities. Neuropathic pain is likely worsened because of missed doses of gabapentin. 125
References � Carpenito/Nursing diagnosis to clinical practice /forth edition/Lippincott Williams & Wilkins/2013 � Bates’ nursing guide physical examination & history taking /Lippincott Williams & Wilkins/2012 � Linda D Urden – kathleen M Stacy – Mary E Lough /Critical Care Nursing (Diagnosis & Management)/sixth edition/mosby elsevier 2010 � Ulrich , Canale/Nursing care planning guide /sixth edition/2005 / ﺍﻋﻀﺎی ﻫیﺌﺖ ﻋﻠﻤی ﺩﺍﻧﺸکﺪﻩ پﺮﺳﺘﺎﺭی ﺷﻬیﺪ ﺑﻬﺸﺘی / � ﺍﺻﻮﻝ ﻣﺮﺍﻗﺒﺖ ﺍﺯ ﺑیﻤﺎﺭ ﺩﻭگﺎﺱ 1382/ ﺟﻠﺪ ﺩﻭﻡ 126

Thanks for your attention 127
 Promotion from assistant to associate professor
Promotion from assistant to associate professor David lewis mad pain and martian pain
David lewis mad pain and martian pain Pms vs pregnancy
Pms vs pregnancy Pms vs pregnancy symptoms
Pms vs pregnancy symptoms Knowledge management consultant
Knowledge management consultant Dr ian smith injury management consultant
Dr ian smith injury management consultant Green world group abu dhabi
Green world group abu dhabi Network management consultant
Network management consultant Colin merrin
Colin merrin Modern data architecture consultant
Modern data architecture consultant Consultant mediu
Consultant mediu A department store decides to use secret shoppers
A department store decides to use secret shoppers Judith james educational consultant
Judith james educational consultant Behavioral genetics consultant
Behavioral genetics consultant Rcem consultant sign off
Rcem consultant sign off Open source consultant
Open source consultant Verizon sip trunk
Verizon sip trunk United states lactation consultant association
United states lactation consultant association Consultant radiographer
Consultant radiographer Recruitment sales calls
Recruitment sales calls Stuart minty planning consultant
Stuart minty planning consultant Philips talent acquisition
Philips talent acquisition Nous hospital consultant
Nous hospital consultant Test consultant capgemini
Test consultant capgemini Fdot procurement office
Fdot procurement office Epicor product configurator
Epicor product configurator Nutraceutical consultant
Nutraceutical consultant Temple and family history consultant
Temple and family history consultant Scan based trading data
Scan based trading data Rodan and fields tax write offs
Rodan and fields tax write offs Expert in consultant liaison psychiatrist
Expert in consultant liaison psychiatrist Sample legal nurse consultant contract
Sample legal nurse consultant contract Internet consultant job description
Internet consultant job description Multiple consultant report
Multiple consultant report Mis consultant
Mis consultant Ayurvedic lifestyle consultant
Ayurvedic lifestyle consultant Stuart minty camden planning consultant
Stuart minty camden planning consultant Court security consultant
Court security consultant Partner technical consultant
Partner technical consultant Palo alto networks certified network security consultant
Palo alto networks certified network security consultant Dr forbes neurology
Dr forbes neurology Reza dorrani
Reza dorrani Engineers pi is 3
Engineers pi is 3 Sujata gupta consultant gynaecologist
Sujata gupta consultant gynaecologist Mrs rajlaxmi is working as the human resource consultant
Mrs rajlaxmi is working as the human resource consultant Associate consultant in capgemini
Associate consultant in capgemini Associate consultant in capgemini
Associate consultant in capgemini Consultant contract 2003
Consultant contract 2003 Threat modelling consultant
Threat modelling consultant Nous hospital consultant
Nous hospital consultant New consultant training
New consultant training Dr dan rogers
Dr dan rogers Module engineering consultant
Module engineering consultant Ph consultant
Ph consultant Sustainable tourism consultant jobs
Sustainable tourism consultant jobs Sanjeev sawai
Sanjeev sawai Wireless communication consultant
Wireless communication consultant Petrophysics consultant
Petrophysics consultant Ellucian2
Ellucian2 Principal consultant significato
Principal consultant significato Pgmdt
Pgmdt Consultant forensic psychiatrist
Consultant forensic psychiatrist Chinchilla business consultant
Chinchilla business consultant Soonercare pain management doctors
Soonercare pain management doctors Pico question example
Pico question example Stony brook pain management
Stony brook pain management Iu pain management
Iu pain management Chapter 7 nursing management of pain during labor and birth
Chapter 7 nursing management of pain during labor and birth Dr ruben gonzalez-vallina
Dr ruben gonzalez-vallina Nonpharmacologic pain management nursing
Nonpharmacologic pain management nursing Npass pain scale
Npass pain scale Pain management specialist
Pain management specialist Fundamentals of nursing pain management
Fundamentals of nursing pain management Dr danko pain management
Dr danko pain management Pain paragraphs
Pain paragraphs Dr. mehdi pain management
Dr. mehdi pain management Pain management ehr
Pain management ehr Chronic pain management irwin
Chronic pain management irwin Pain res manage
Pain res manage Dr lascarides pain management
Dr lascarides pain management Pain management synonym
Pain management synonym Top management middle management first line management
Top management middle management first line management Top management middle management first line management
Top management middle management first line management Middle level management
Middle level management Um balão de oxigênio contendo 3 x 1026
Um balão de oxigênio contendo 3 x 1026 How to send a proper email to a teacher
How to send a proper email to a teacher Sincerely yours capitalized
Sincerely yours capitalized Ppgea ufrrj
Ppgea ufrrj Rbzjttdo9f4 -site:youtube.com
Rbzjttdo9f4 -site:youtube.com Ruth guthrie rate my professor
Ruth guthrie rate my professor The professor's beloved equation
The professor's beloved equation Professor mso afskaffes
Professor mso afskaffes Mattie is a new sociology professor
Mattie is a new sociology professor Paraphrase
Paraphrase Professor edley
Professor edley Professor edley
Professor edley Brian scott peskin
Brian scott peskin Professor olaf wendler
Professor olaf wendler Um bom professor é aquele que
Um bom professor é aquele que Deutopia
Deutopia Lawrence chung rate my professor
Lawrence chung rate my professor Lei das proporções múltiplas
Lei das proporções múltiplas Professor ajit diwan
Professor ajit diwan The telephone rang inside startlingly
The telephone rang inside startlingly Flights of fancy how to read literature
Flights of fancy how to read literature How to read literature like a professor chapter titles
How to read literature like a professor chapter titles Good morning classe
Good morning classe Good day class
Good day class Inventor do telefone
Inventor do telefone Cuhk assistant professor salary
Cuhk assistant professor salary Email etiquette dos and donts
Email etiquette dos and donts Dragica vasileska rate my professor
Dragica vasileska rate my professor Professor ashley dennison
Professor ashley dennison Dear mr professor
Dear mr professor Certificado professor nota dez
Certificado professor nota dez Is president capitalized
Is president capitalized Rapd relative afferent pupillary defect
Rapd relative afferent pupillary defect Signalkarten selbstinstruktion
Signalkarten selbstinstruktion Professor dr. h a m nazmul ahsan
Professor dr. h a m nazmul ahsan F95 the professor
F95 the professor Professor michael bagshaw
Professor michael bagshaw Professor adrian smith
Professor adrian smith Professor gaia com
Professor gaia com Professor john forsythe
Professor john forsythe Professor mick waters
Professor mick waters Professor marcello govoni
Professor marcello govoni Jacob p wallenberg
Jacob p wallenberg Tspci
Tspci