Complications of Intravenous Therapy Principles of IV Therapy











- Slides: 61
Complications of Intravenous Therapy Principles of IV Therapy ADN 136 Fall Qr 09
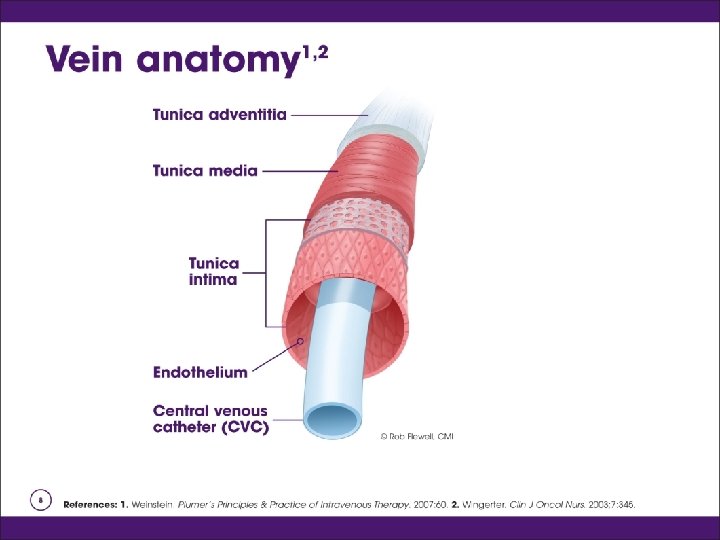
Complications of IV Therapy o o o Nursing assumed the role of intravenous therapy in the 1940’s Application of the nursing process is critical in the prevention of complications 90% of hospitalized patients receive IV fluids and medications
Complications of IV Therapy o Classified according to their location n n Local complication: at or near the insertions site or as a result of mechanical failure Systemic complications: occur within the vascular system, remote from the IV site. Can be serious and life threatening
Local complications o o Occur as adverse reactions or trauma to the surrounding venipuncture site Assessing and monitoring are the key components to early intervention Good venipuncture technique is the main factor related to the prevention of most local complications associated with IV Therapy. Local complications include: hematoma, thrombosis, phlebitis, postinfusion phlebitis, thrombophlebitis, infiltration, extravasation, local infection, and veno spasm.
Hematoma o Hematoma and ecchymosis demote formations resulting from the infiltration of blood into the tissues at the venipuncture site n n n Related to venipuncture technique Use of large bore cannula: Trauma to the vein during insertion Patients receiving anticoagulant therapy and long term steroids
Hematoma o o o Subcutaneous hematoma is the most common complication Can be a starting point for other complications: thrombophlebitis and infection Related to: n n n Nicking the vein Discontinuing the IV without apply adequate pressure Applying the tourniquet to tightly above a priviously attempted venipuncture site.
Hematoma o Signs and symptoms: n n Discoloration of the skin Site swelling and discomfort Inability to advance the cannula all the way into the vein during insertion Resistance to positive pressure during the lock flushing procedure
Hematoma Prevention o o o Use of an indirect method Apply tourniquet just before venipuncture Use a small need in the elderly and patients on steriods, or patients with thin skin. Use blood pressure cuff to apply pressure Be gentle
Hematoma Treatment o Apply direct, light pressure for 2 -3 minutes after needle removed Have patient elevate extremity Apply Ice o Document o o
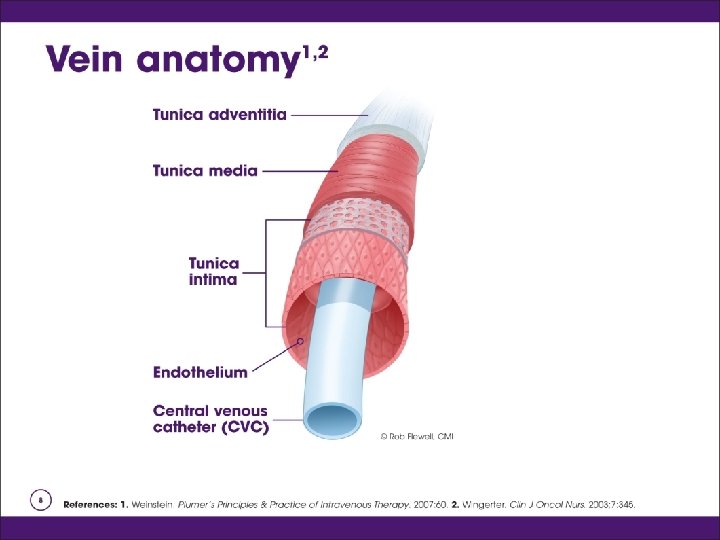
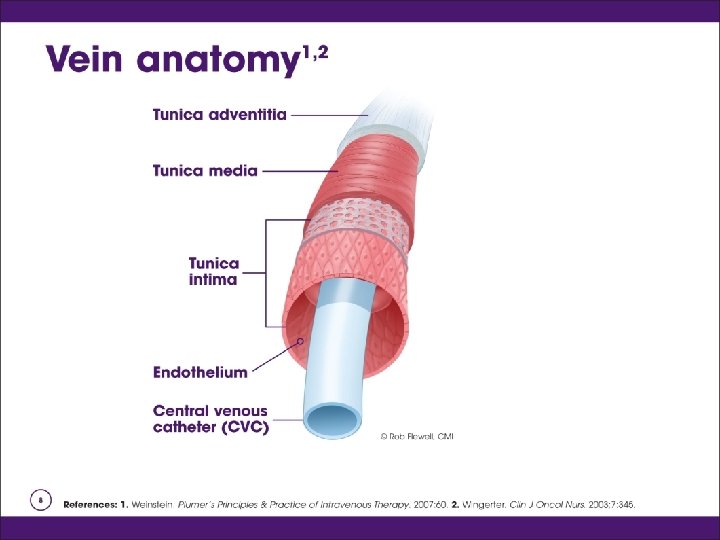
Thrombosis o o Catheter-related obsturctions can be mechanical or non-thrombotic Trauma to the endothelial cells of the venous wall causes red blood cells to adhere to the vein wall, forms a clot or Thrombosis Drip rate slows, line does not flush easily, resistance is felt Never forcible flush a catheter
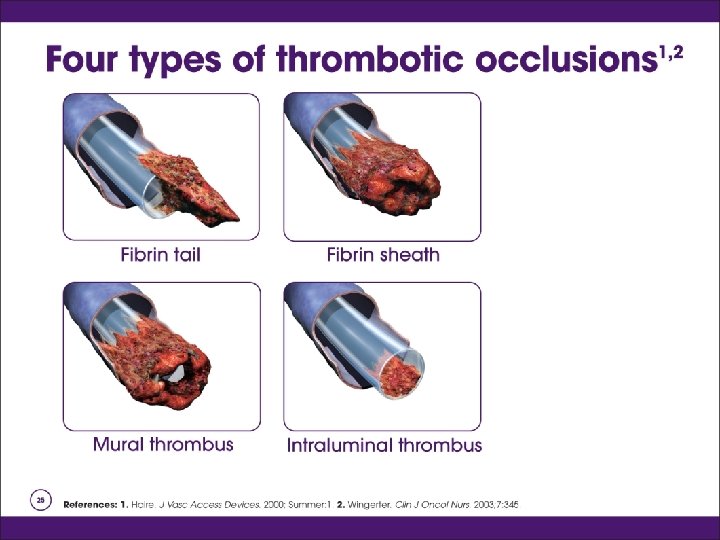
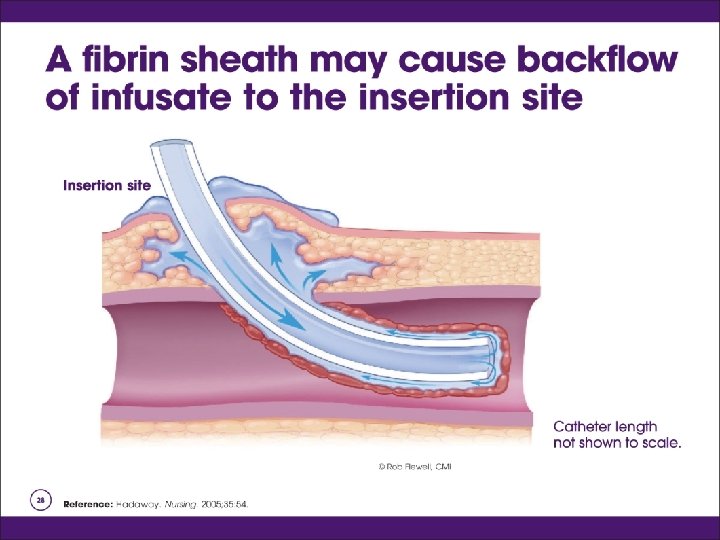
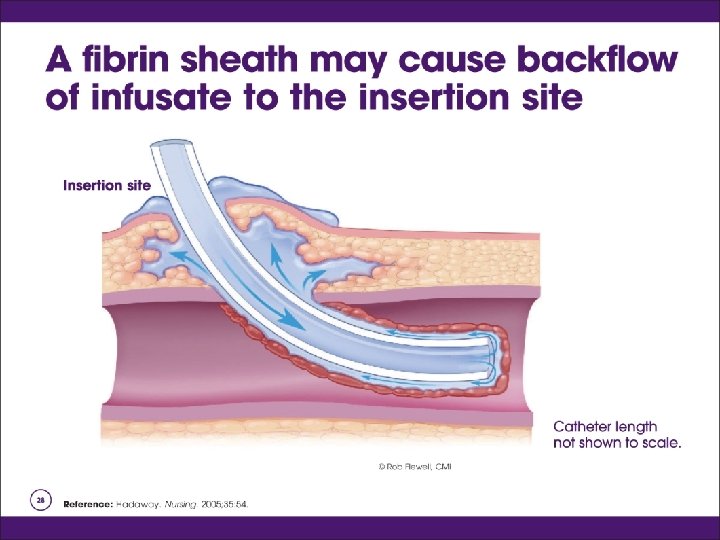
Thrombosis Types of Thrombus or occlusion o o o Persistent withdrawal occlusion Partial occlusion Complete occlusion Fibrin tail Fibrin sheath Mural thrombosis
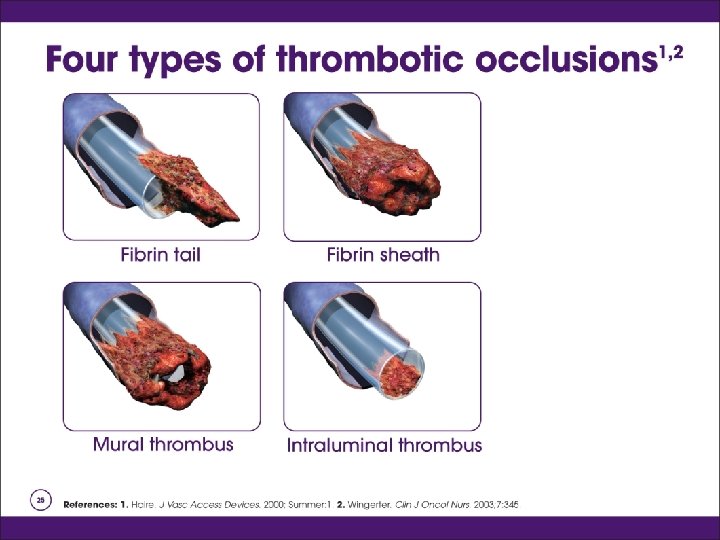
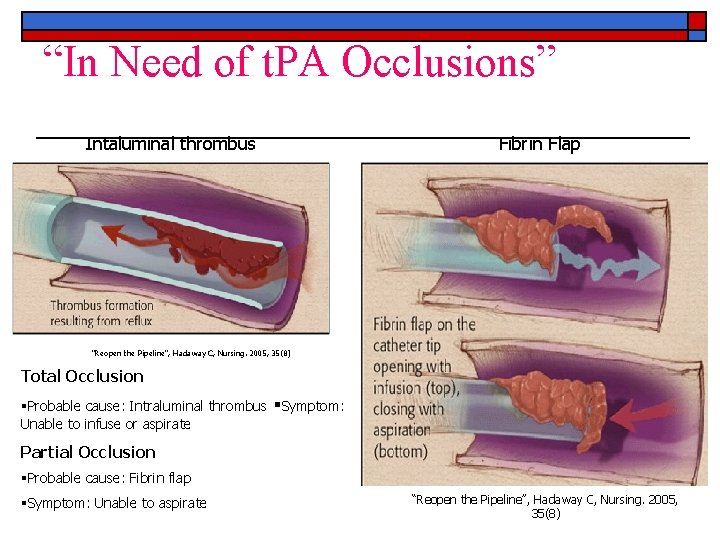
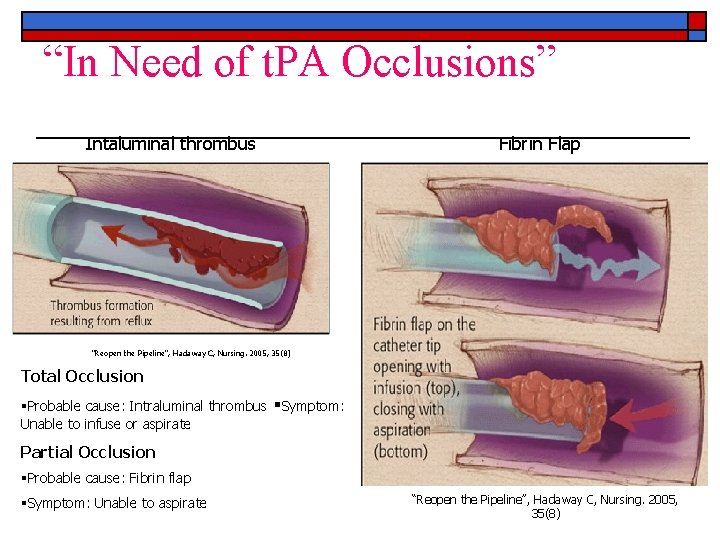
“In Need of t. PA Occlusions” Intaluminal thrombus Fibrin Flap “Reopen the Pipeline”, Hadaway C, Nursing. 2005, 35(8) Total Occlusion Probable cause: Intraluminal thrombus Unable to infuse or aspirate Symptom: Partial Occlusion Probable cause: Fibrin flap Symptom: Unable to aspirate “Reopen the Pipeline”, Hadaway C, Nursing. 2005, 35(8)
Thrombosis Types of Thrombus or occlusion o Thrombosis related to: n n n Hypertensive pt; blood backing up Low flow rate Location of the IV cannula Compression of the IV line for an extended period of time Trauma to the wall of the vein
Thrombosis o Signs and Symptoms n n n o Fever and Malaise Slowed or stopped infusion rate Inability to flush Prevention n n Use pumps and controllers to manage flow rate Microdrip tubing for rate below 50 m. L/hr Avoid areas of flexion Use filters Avoid lower extremeties
Thrombosis o Treatment n n n o Never flush a cannula to remove an occlusion Discontunue the cannula Notify the physician and assess the site for circulatory impairment Document
Phlebitis o Inflammation of the vein in which the endothelial cells of the venous wall become irritated and cells roughen, allowing platelets to adhere and predispose the vein to inflamation-induced phlebitis n Tender to touch and can be very painful
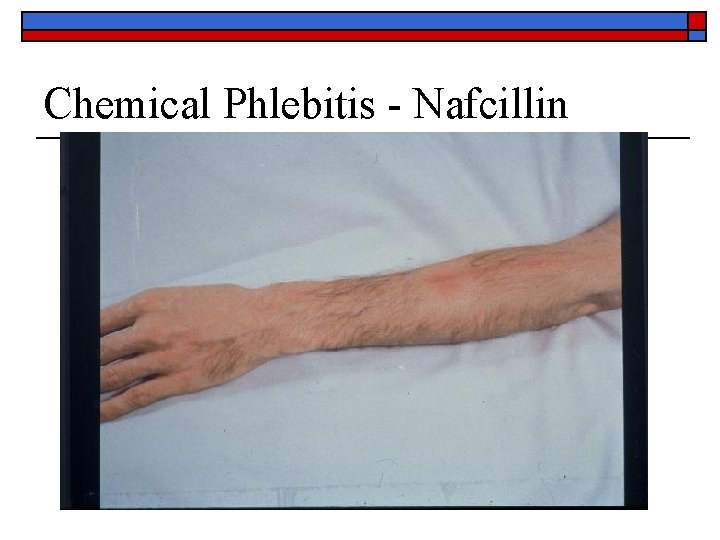
Phlebitis o Mechanical: n n o To large a catheter for the size of the vein Manipulation of the catheter: improper stabilization Chemical: vein becomes inflamed by irritating or vessicant solutions or medication n n Irritation medication or solution Improperly mixed or diluted Too-rapid infusion Presence of particulate matter
Phlebitis o Chemical (cont): n n The more acidic the IV solution the greater the risk Additives: Potassium Type of material Length of dwell: o n 30% by day 2, 39 -40% by day 3 (Macki and Ringer) The slower the rate of infusion the less irritation
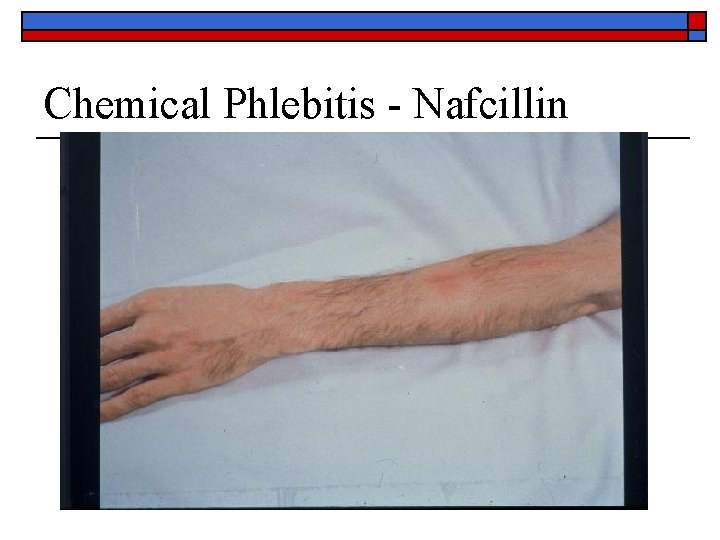
Chemical Phlebitis - Nafcillin
Phlebitis Bacterial o o o Also called Septic phlebitis: least common Inflammation of the intima of the vein Contributing factors n n n n Poor aseptic technique Failure to detect breaks in the integrity of the equipment Poor insertion technique Inadequate stabilization Failure to perform site assessment Aseptic preparation of solutions Hand washing and preparing the skin
Phlebitis Postinfusion o o Inflamation of the vein 48 -96 hr after discontinued Factors that contribute: n n n n Insertion technique Condition of the vein used Type, compatibility, p. H of solution used Gauge, size, length, and material Dwell time Infrequent dressing change Host factors: age, gender, age and presence of disease
Phlebitis o o Immune system causes leukocytes to gather at the inflamed site Pyrogens stimulate the hypothalamus to raise body temperature Pyrogens stimulate bone marrow to release more leukocytes Redness and tenderness increase
Phlebitis o Signs and Symptoms n n n o Redness at the site Site warm to touch Local swelling Palpable cord along the vein Sluggish infusion rate Increase in basal temperature of 1 degree C or more Prevention n n Use larger veins for hypertonic solutions Central lines for Infusions lasting longer than 5 days
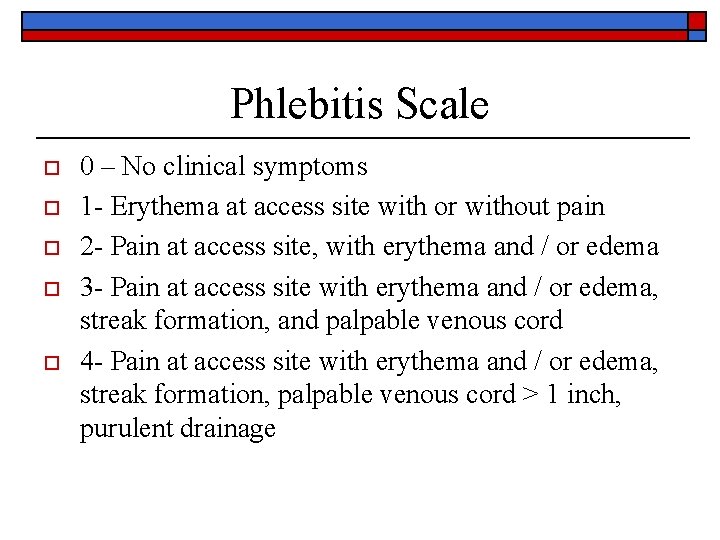
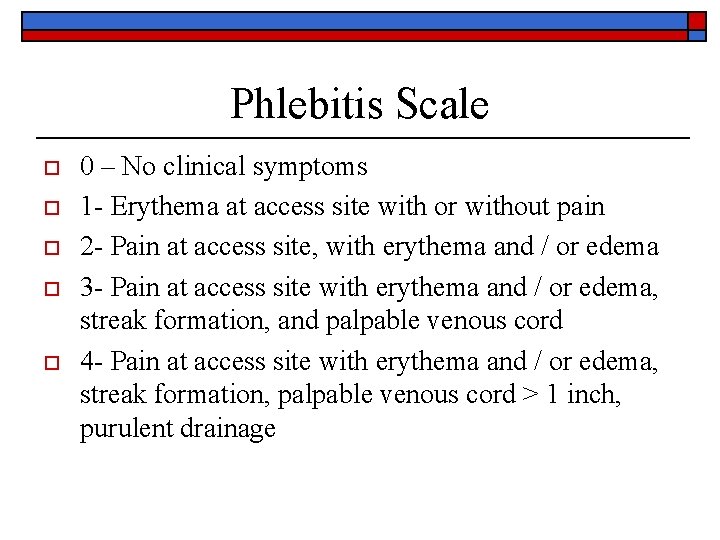
Phlebitis Scale o o o 0 – No clinical symptoms 1 - Erythema at access site with or without pain 2 - Pain at access site, with erythema and / or edema 3 - Pain at access site with erythema and / or edema, streak formation, and palpable venous cord 4 - Pain at access site with erythema and / or edema, streak formation, palpable venous cord > 1 inch, purulent drainage


Thrombophlebitis o o Thrombophlebitis denotes a twofold injury: thrombosis and inflammation Related to: n n n Use of veins in the lower extremity Use of hypertonic or highly acidic infusion solutions Causes similar to those leading to phlebitis
Thrombophlebitis o Signs and Symptoms n n n n Sluggish flow rate Edema in the limbs Tender and cord like vein Site warm to the touch Visible red line above venipuncture site Diminished arterial pulses Mottling and cyanosis of the extremities
Thrombophlebitis o Prevention n n n Use veins in the forearm rather than the hands Do not use veins in a joint Assess site q 4 hr in adults, q 2 hr in children Catheter securment Infuse at rate prescribed Use the smallest size catheter to do the job Proper dilution
Thrombophlebitis o Septic thrombophlebits can be prevented: n n n Appropriate skin preparation Aseptic technique in the maintance of infusion Proper hand hygiene o o o 60% from patients skin 35% from the line itself 5% from hands
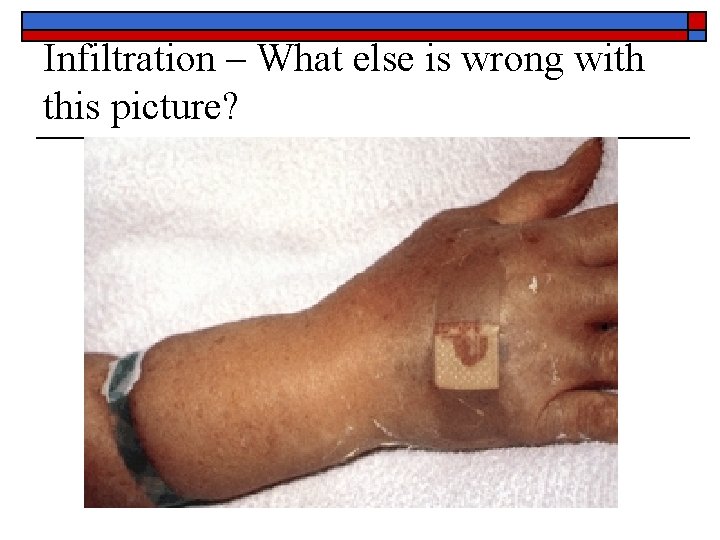
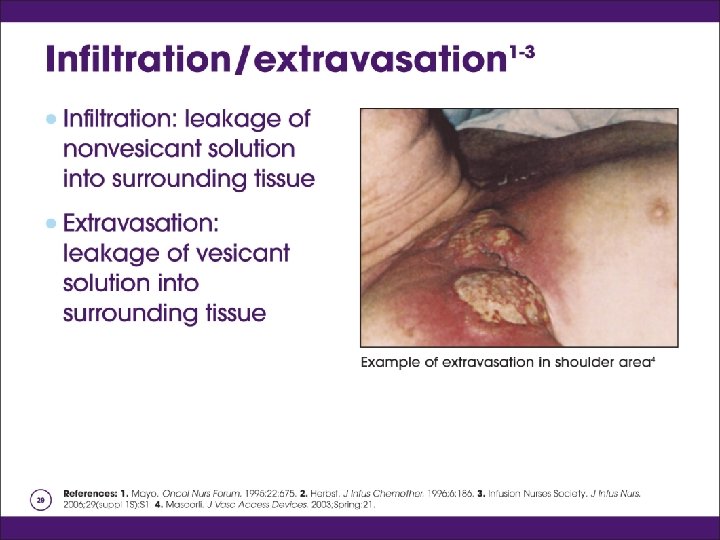
Infiltration o o o The inadvertent administration of a nonvesicant solution into surrounding tissue Dislodgment of the catheter from the vein Second to phlebitis as a cuase of IV therapy morbidity
Infiltration o Related to: n n n Puncture of the distal vein wall during access Puncture of the vein wall by mechanical friction Dislodgement of the catheter from the intima of the vien Poor securment High delivery rate Overmanipulation
Infiltration o Signs and Symptoms n n n Coolness of the skin around site Taut skin Dependent edema Absence of blood return “Pinkish” blood return Infusion rate slows

Infiltration o Complications fall into 3 catagories n n n Ulceration and possible tissue necrosis Compartment syndrome Reflex sympathetic dystrophy syndrome
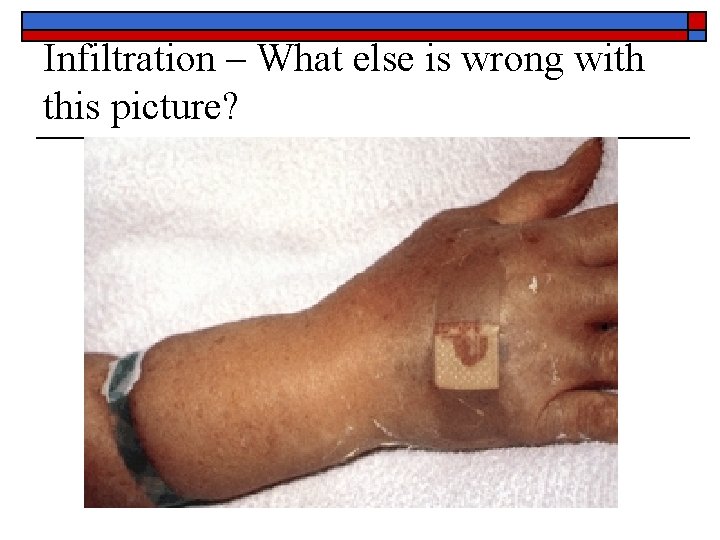
Infiltration – What else is wrong with this picture?
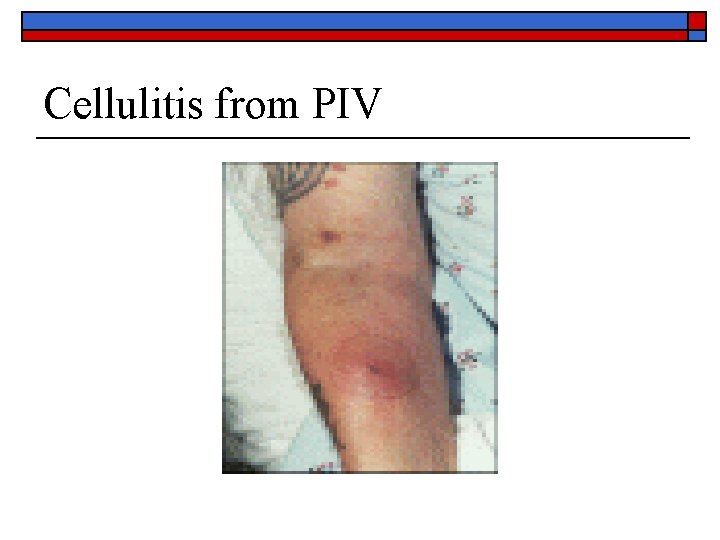
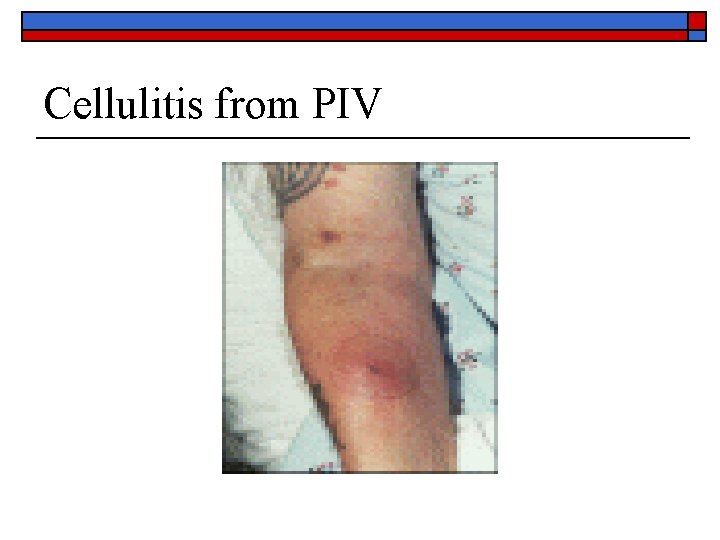
Cellulitis from PIV
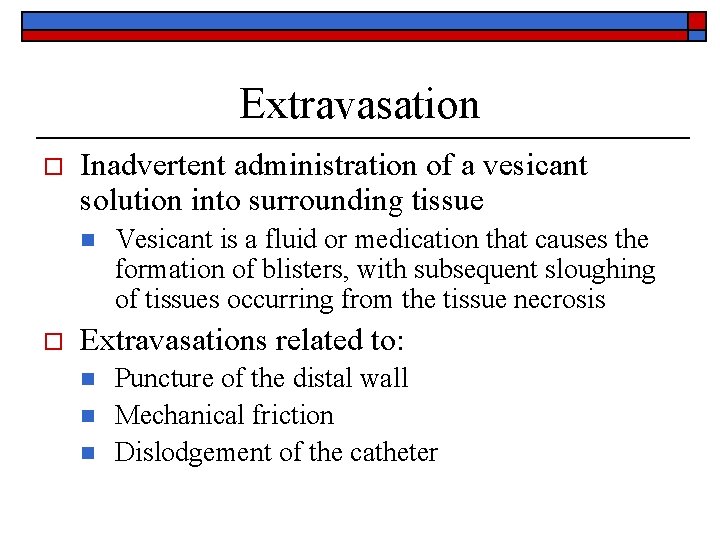
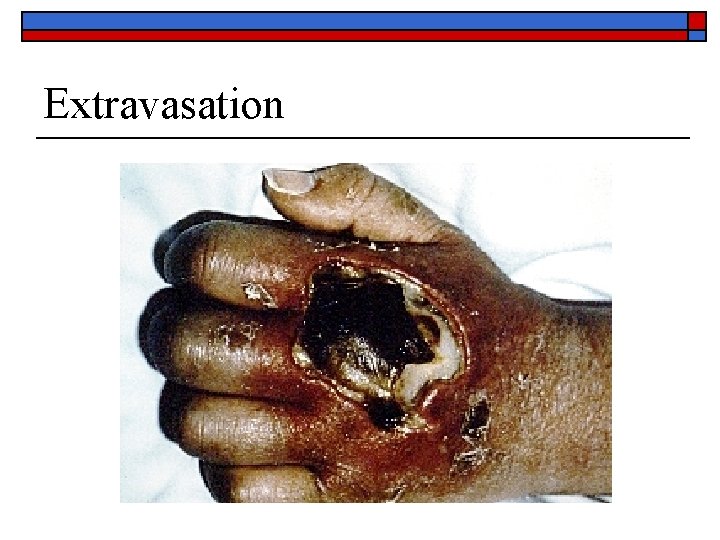
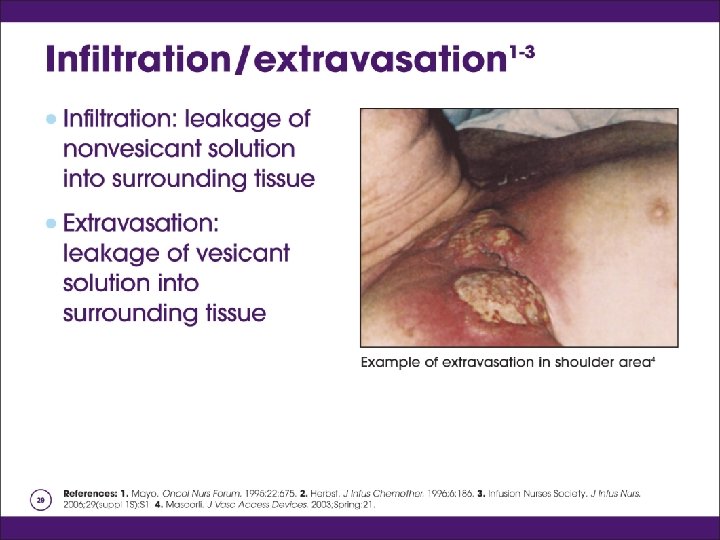
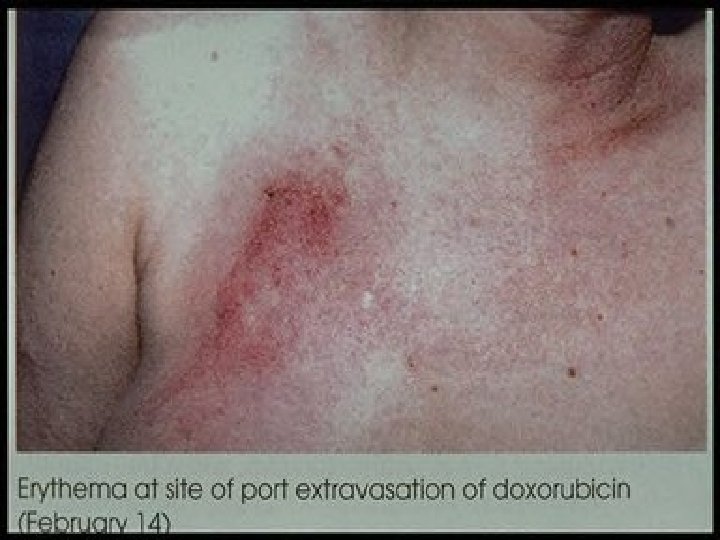
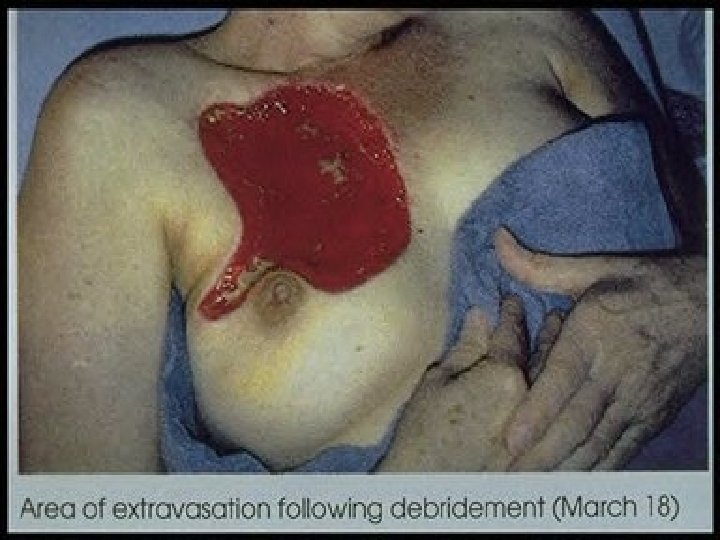
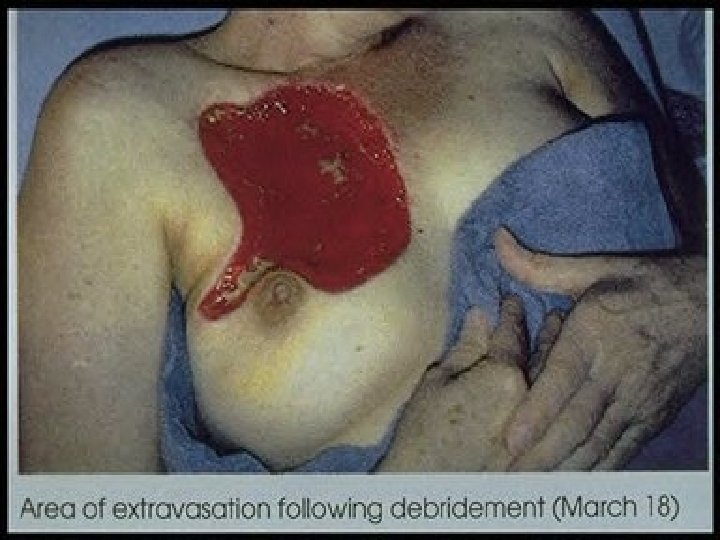
Extravasation o Inadvertent administration of a vesicant solution into surrounding tissue n o Vesicant is a fluid or medication that causes the formation of blisters, with subsequent sloughing of tissues occurring from the tissue necrosis Extravasations related to: n n n Puncture of the distal wall Mechanical friction Dislodgement of the catheter
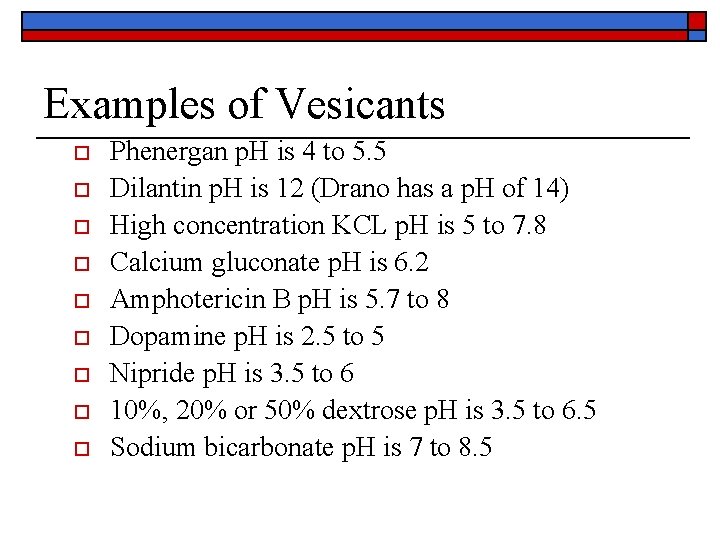
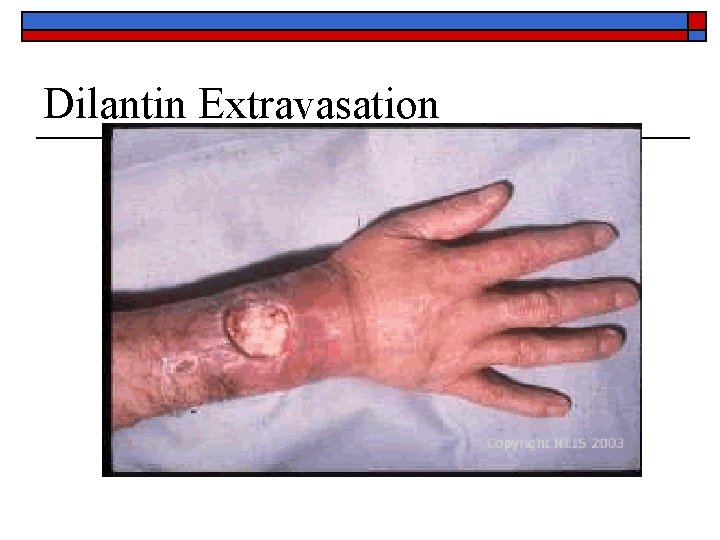
Examples of Vesicants o o o o o Phenergan p. H is 4 to 5. 5 Dilantin p. H is 12 (Drano has a p. H of 14) High concentration KCL p. H is 5 to 7. 8 Calcium gluconate p. H is 6. 2 Amphotericin B p. H is 5. 7 to 8 Dopamine p. H is 2. 5 to 5 Nipride p. H is 3. 5 to 6 10%, 20% or 50% dextrose p. H is 3. 5 to 6. 5 Sodium bicarbonate p. H is 7 to 8. 5
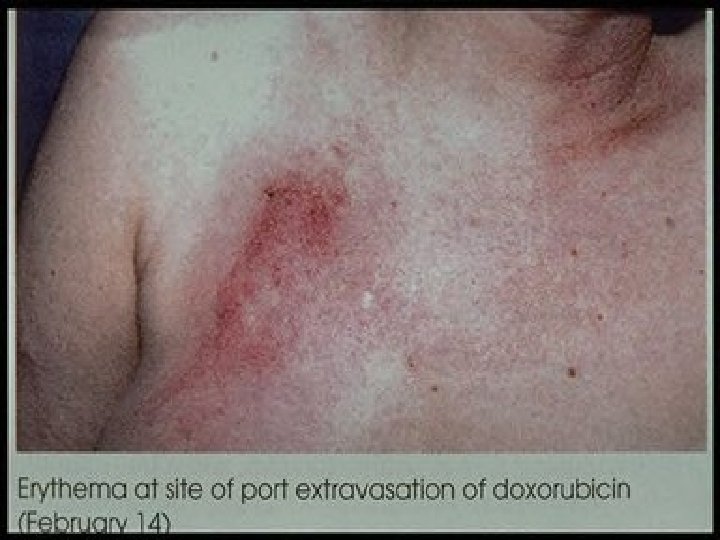
Extravasations o Signs and Symptoms n n n n Complaints of pain or burning Swelling proximal to or distal to the IV site Puffiness of the dependent part of the limb Skin tightness at the veinpuncture site Blanching and coolness of the skin Slow or stopped infusion Damp or wet dressing
Extravasations o Prevention: n n Use of skilled practitioners Knowledge of vesicants Condition of the patients veins Drug administration technique o o o If continuous give in CVAD Only with brisk blood return of 3 -5 cc Use of a free flow IV Do not use a pump on vesicants given peripherally Assess for blood return frequently
Extravasations (cont) o Prevention (cont) n n Site of venous access Condition of the patient o o o n Vomiting, coughing, retchin Sedated Unable to communicate Treatment
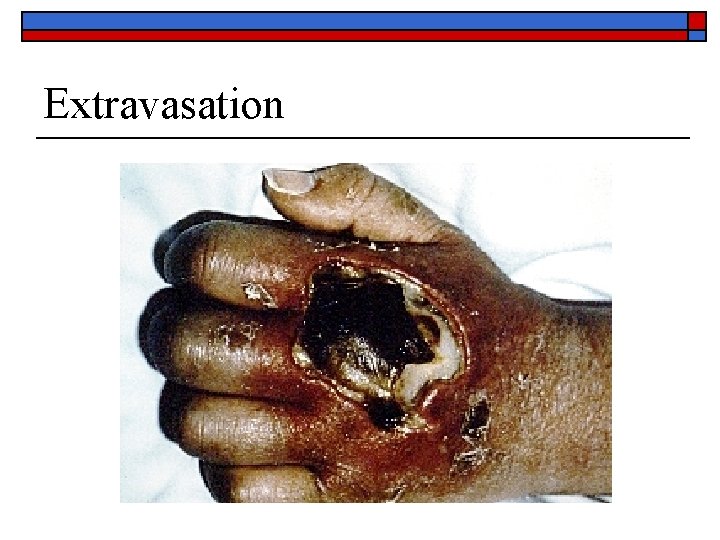
Extravasation
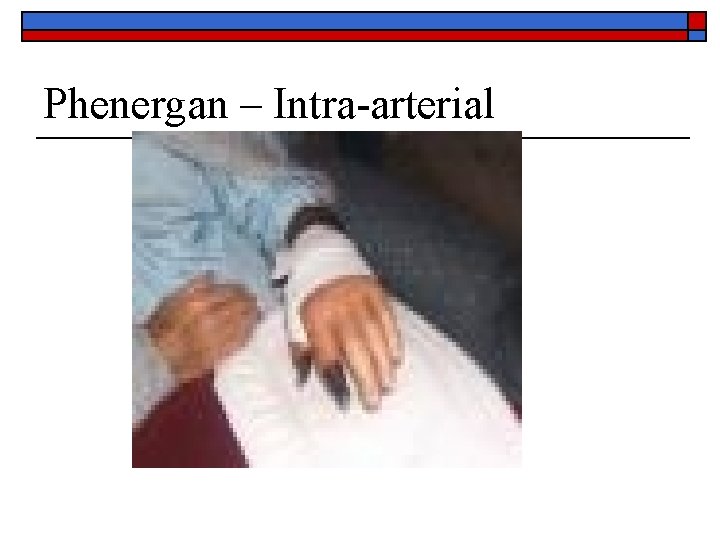
Phenergan – Intra-arterial

Phenergan Intra-arterial
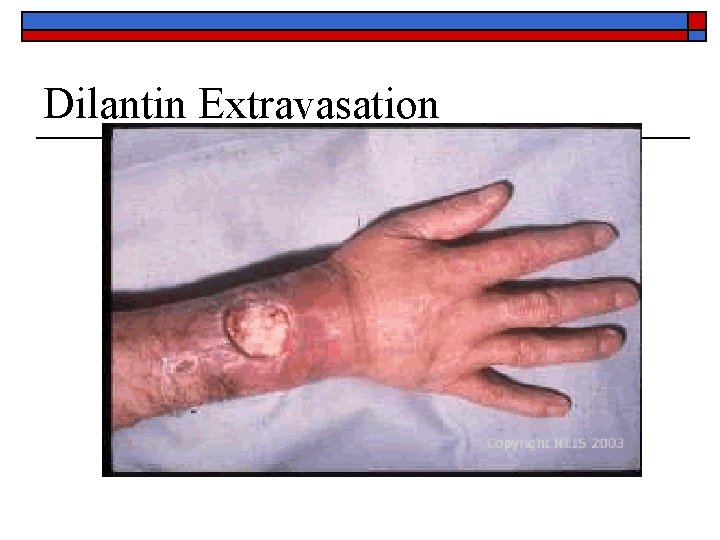
Dilantin Extravasation







Other Complications o Local infection: n n o Microbial contamination of the cannula or the infusate Thrombus becomes infected Venous Spasm: a sudden involuntary contraction of a vein or an artery resulting in temporary cessation of blood flow through a vessel
Systemic Complications o We will cover when we talk about Central Venous Access Devices
 Infiltrated iv pictures
Infiltrated iv pictures Iv removal documentation example
Iv removal documentation example Site:slidetodoc.com
Site:slidetodoc.com Simplifying nonperfect roots quizlet
Simplifying nonperfect roots quizlet Iv cannula labelling
Iv cannula labelling Intravenous medication administration pretest
Intravenous medication administration pretest Line & catheter label - intravenous burette
Line & catheter label - intravenous burette Medication administration 4 pretest
Medication administration 4 pretest User applied labelling
User applied labelling Humanistic therapies aim to boost
Humanistic therapies aim to boost Psychodynamic and humanistic therapies have in common
Psychodynamic and humanistic therapies have in common Bioness integrated therapy system occupational therapy
Bioness integrated therapy system occupational therapy Massive blood transfusion complications
Massive blood transfusion complications Complications of gestational diabetes
Complications of gestational diabetes Methimazole dosing guidelines
Methimazole dosing guidelines Phlegmasia cerulea dolens definition
Phlegmasia cerulea dolens definition Local complications
Local complications Post dated pregnancy complications
Post dated pregnancy complications Complications of shigellosis
Complications of shigellosis Septic arthritis complications
Septic arthritis complications Iv site complications
Iv site complications C section complications
C section complications Blood transfusion requirements
Blood transfusion requirements Adhesive arachnoiditis
Adhesive arachnoiditis Heart failure complications
Heart failure complications Rapamune
Rapamune Complications of schizophrenia
Complications of schizophrenia Gastrostomie complications
Gastrostomie complications Thoracentesis complications
Thoracentesis complications Complications of hydrocephalus
Complications of hydrocephalus Dd of meningitis
Dd of meningitis Asma rp
Asma rp Molecular cell biology of diabetic complications
Molecular cell biology of diabetic complications C section layers
C section layers Dr neil stone
Dr neil stone Why does liver disease cause splenomegaly
Why does liver disease cause splenomegaly Indication of blood transfusion
Indication of blood transfusion Complications of respiratory failure
Complications of respiratory failure Postpartum thyroiditis
Postpartum thyroiditis The events and complications begin to resolve themselves
The events and complications begin to resolve themselves Layer of episiotomy
Layer of episiotomy Glomerulonephritis complications
Glomerulonephritis complications Trach disconnect wedge
Trach disconnect wedge Hyperlipidemia complications
Hyperlipidemia complications Insulin resistance symptoms
Insulin resistance symptoms Low thyroid function symptoms
Low thyroid function symptoms Early and late complications of blood transfusion
Early and late complications of blood transfusion Varicella zoster complications
Varicella zoster complications Deviated septum
Deviated septum Fiksasi internal dan eksternal adalah
Fiksasi internal dan eksternal adalah Septic arthritis complications
Septic arthritis complications Eclampsia definicion
Eclampsia definicion Stroke precautions nursing
Stroke precautions nursing What is a short story
What is a short story Most common complication of central venous catheter
Most common complication of central venous catheter Complications of blood transfusion
Complications of blood transfusion Lecture title
Lecture title Eswl complications
Eswl complications Abdominal insufflation complications
Abdominal insufflation complications Otitis media complications
Otitis media complications Gestational diabetes ppt
Gestational diabetes ppt Cast slab splint
Cast slab splint