Primary Care Management of the Degenerative Spine Jim





- Slides: 45
Primary Care Management of the Degenerative Spine Jim Messerly D. O.
Nothing to Disclose
Low Back Pain- Where’s the Pain Coming From? ? ?
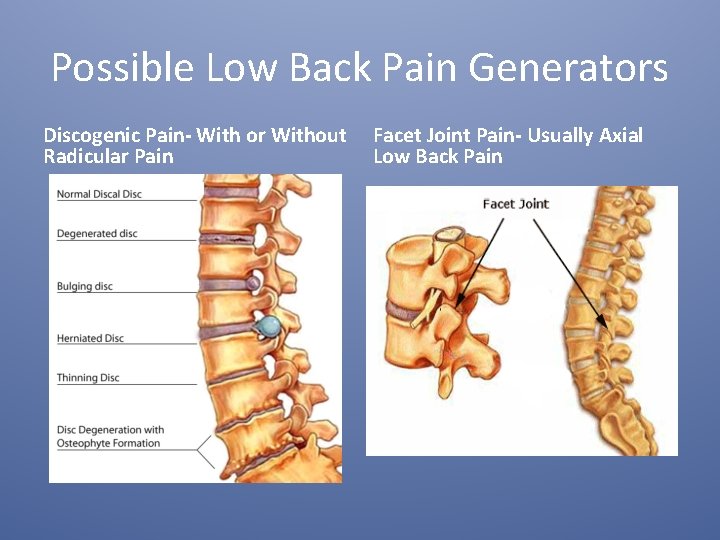
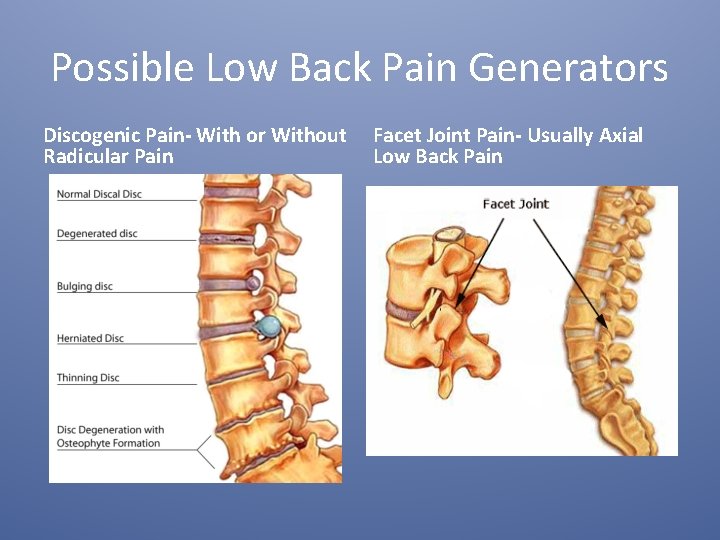
Possible Low Back Pain Generators Discogenic Pain- With or Without Radicular Pain Facet Joint Pain- Usually Axial Low Back Pain
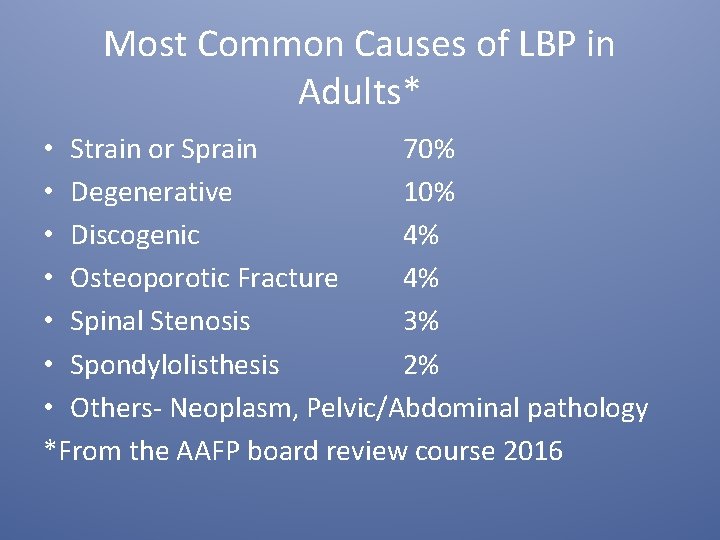
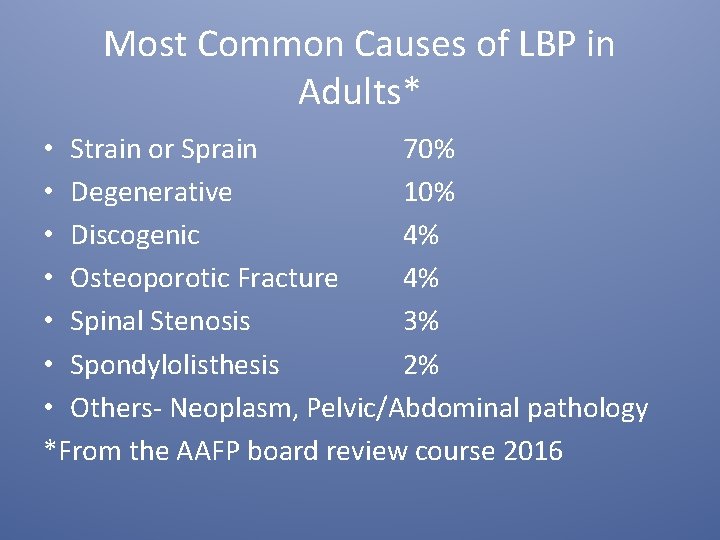
Most Common Causes of LBP in Adults* • Strain or Sprain 70% • Degenerative 10% • Discogenic 4% • Osteoporotic Fracture 4% • Spinal Stenosis 3% • Spondylolisthesis 2% • Others- Neoplasm, Pelvic/Abdominal pathology *From the AAFP board review course 2016
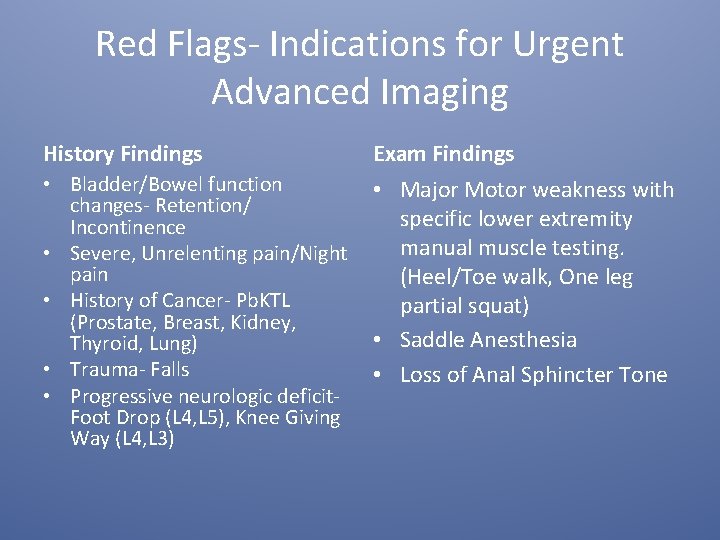
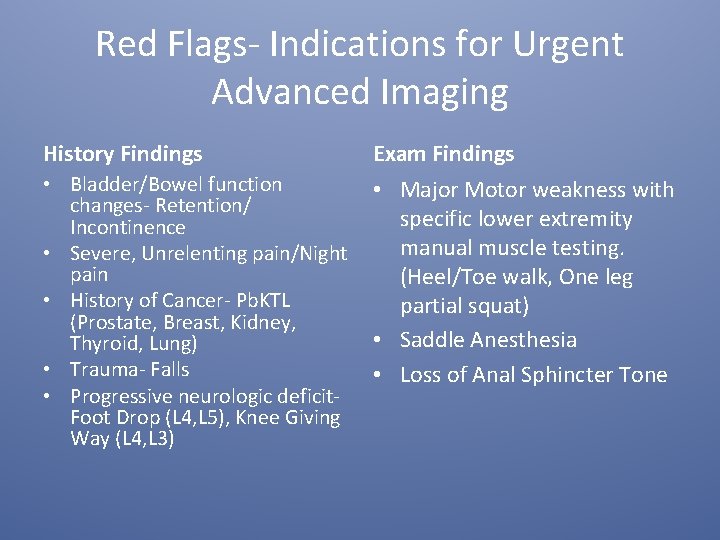
Red Flags- Indications for Urgent Advanced Imaging History Findings Exam Findings • Bladder/Bowel function changes- Retention/ Incontinence • Severe, Unrelenting pain/Night pain • History of Cancer- Pb. KTL (Prostate, Breast, Kidney, Thyroid, Lung) • Trauma- Falls • Progressive neurologic deficit. Foot Drop (L 4, L 5), Knee Giving Way (L 4, L 3) • Major Motor weakness with specific lower extremity manual muscle testing. (Heel/Toe walk, One leg partial squat) • Saddle Anesthesia • Loss of Anal Sphincter Tone
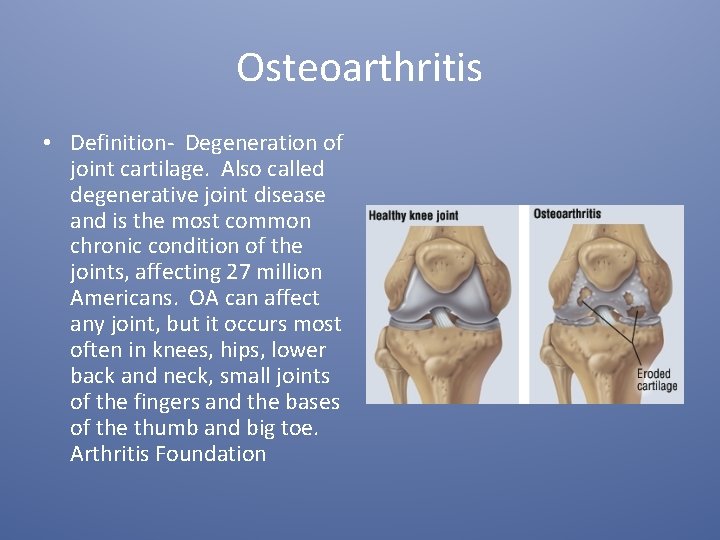
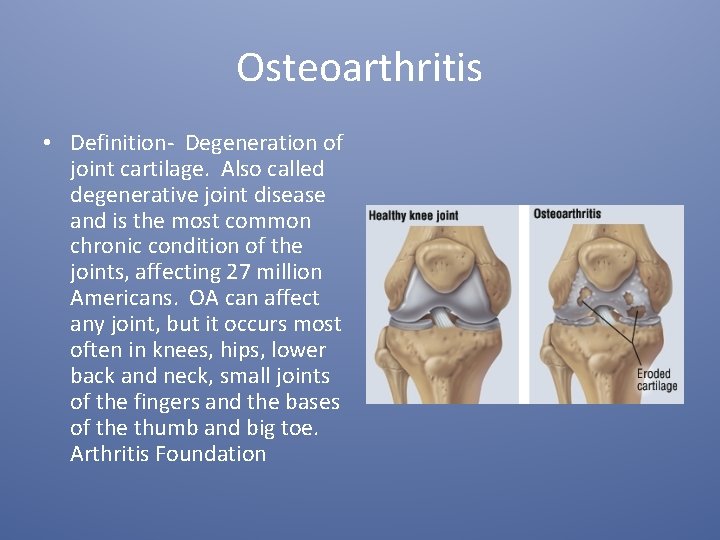
Osteoarthritis • Definition- Degeneration of joint cartilage. Also called degenerative joint disease and is the most common chronic condition of the joints, affecting 27 million Americans. OA can affect any joint, but it occurs most often in knees, hips, lower back and neck, small joints of the fingers and the bases of the thumb and big toe. Arthritis Foundation
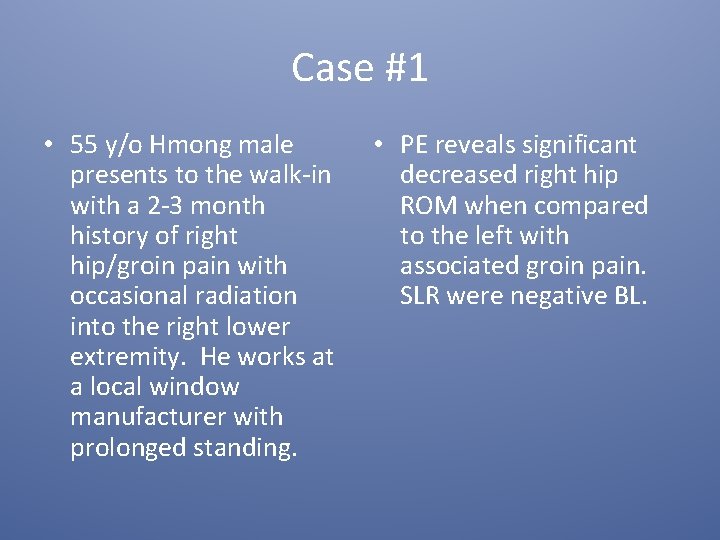
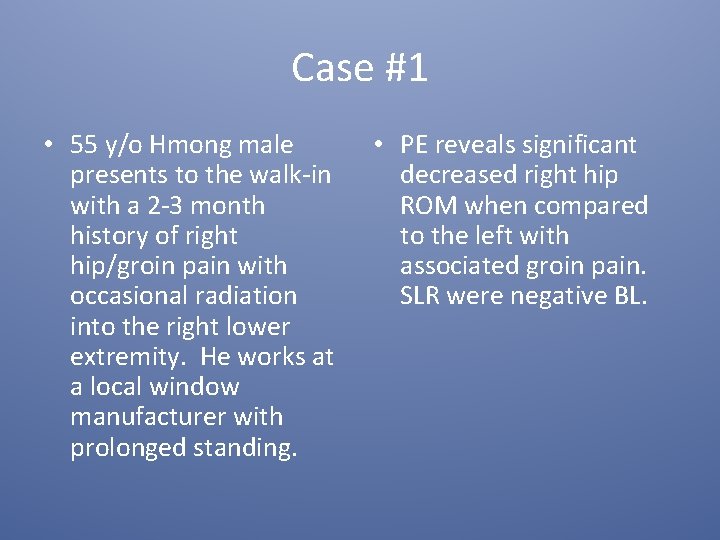
Case #1 • 55 y/o Hmong male presents to the walk-in with a 2 -3 month history of right hip/groin pain with occasional radiation into the right lower extremity. He works at a local window manufacturer with prolonged standing. • PE reveals significant decreased right hip ROM when compared to the left with associated groin pain. SLR were negative BL.

Pelvis X-ray

Lateral L-Spine
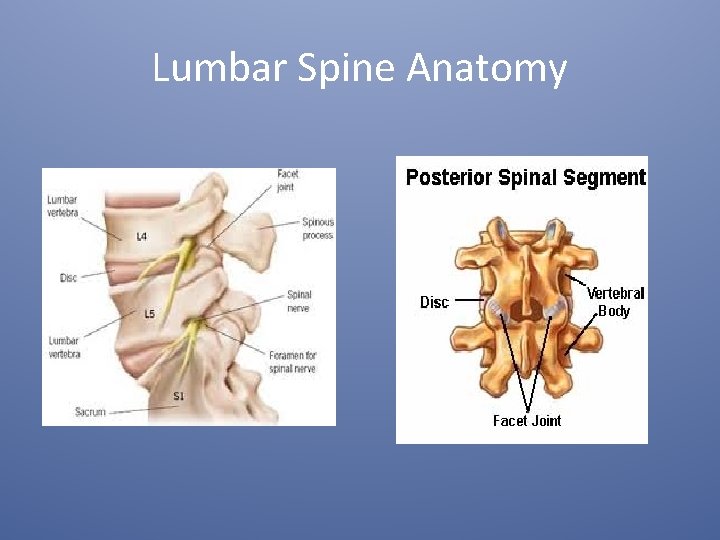
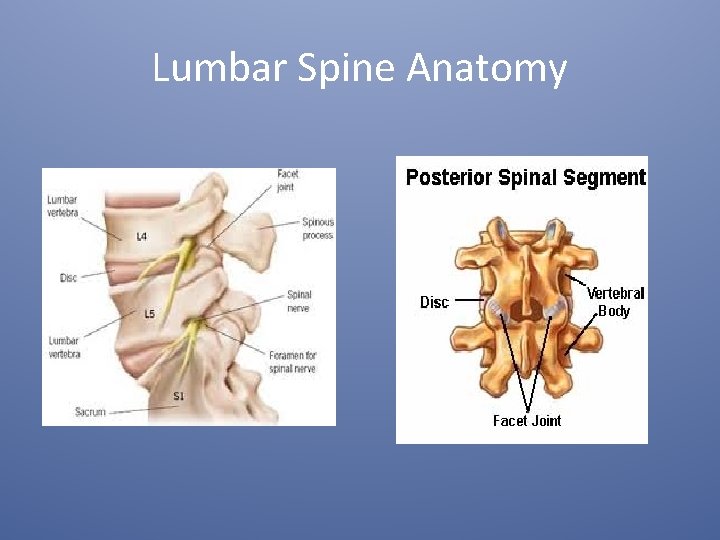
Lumbar Spine Anatomy
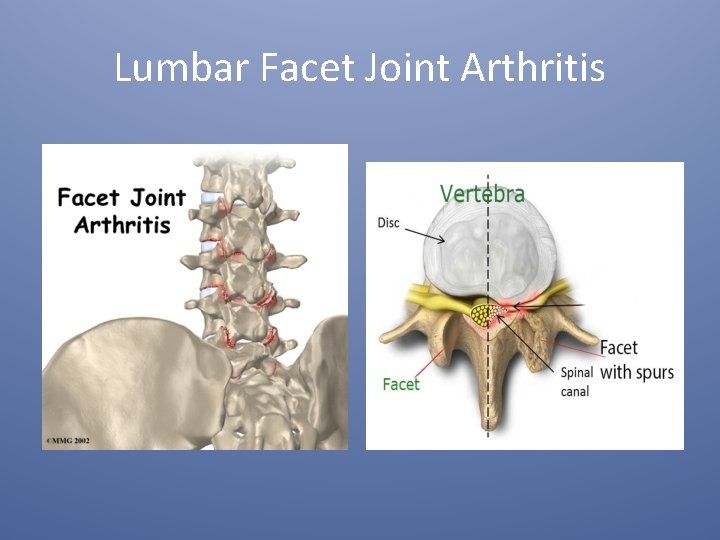
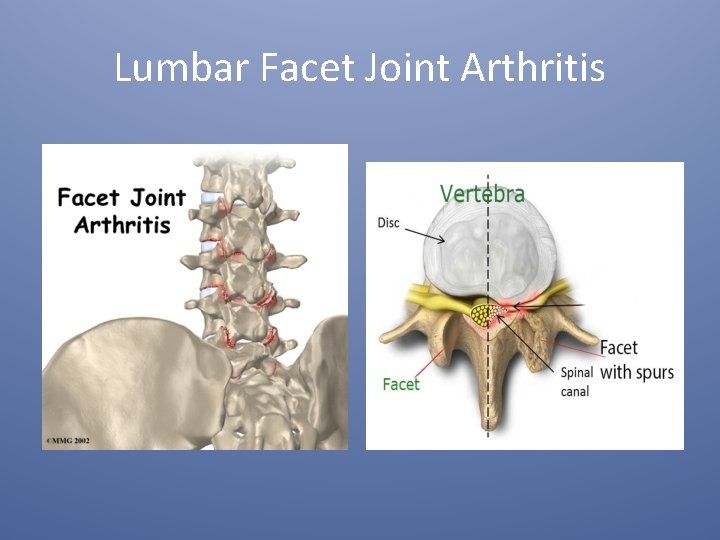
Lumbar Facet Joint Arthritis
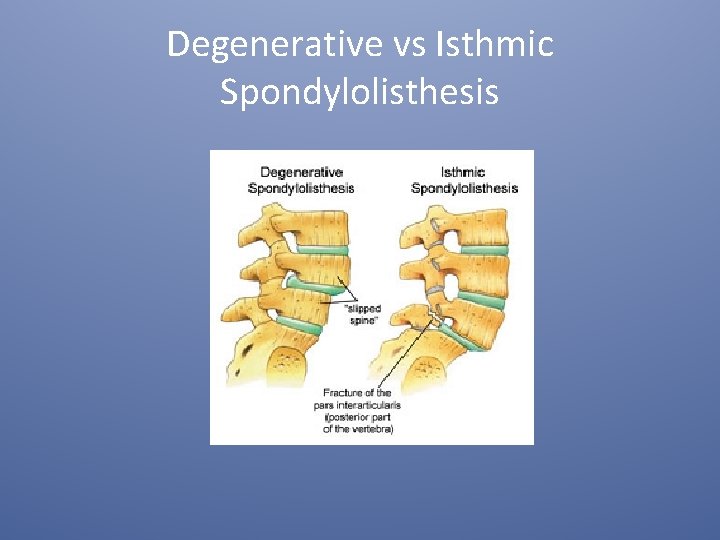
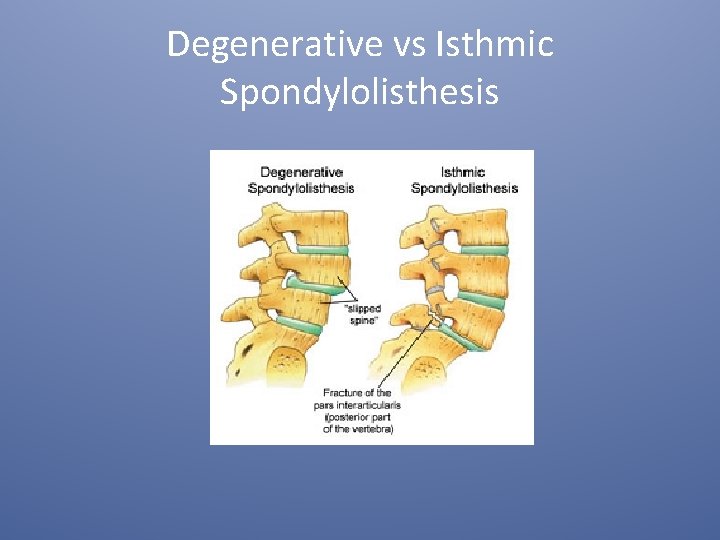
Degenerative vs Isthmic Spondylolisthesis
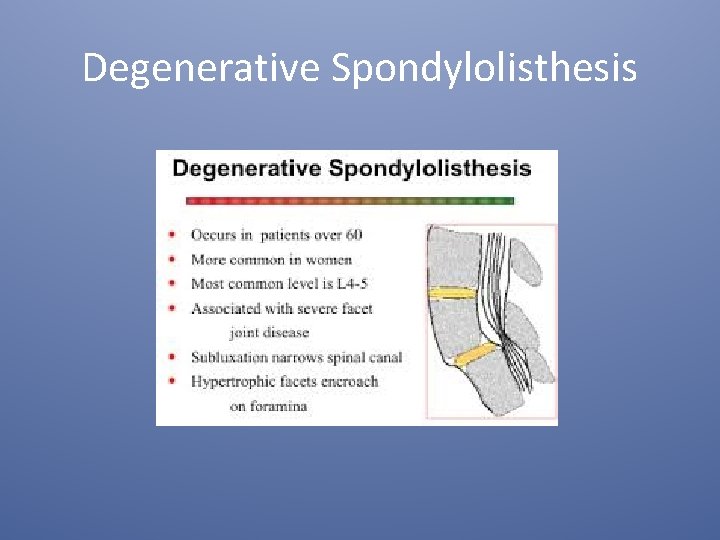
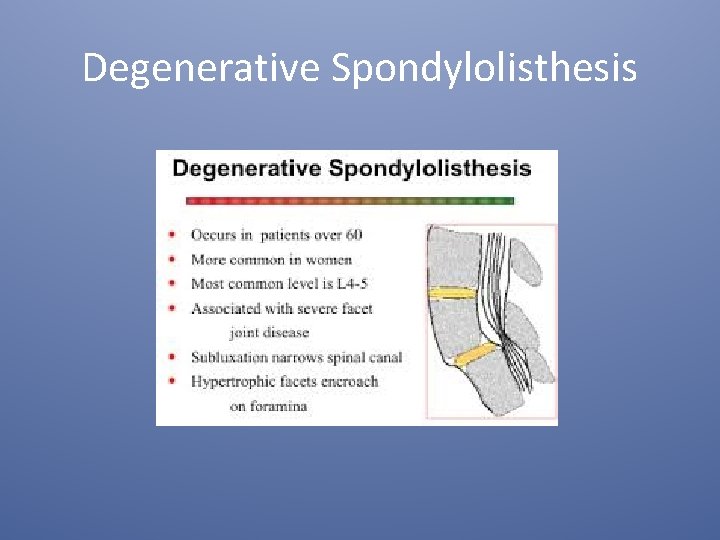
Degenerative Spondylolisthesis
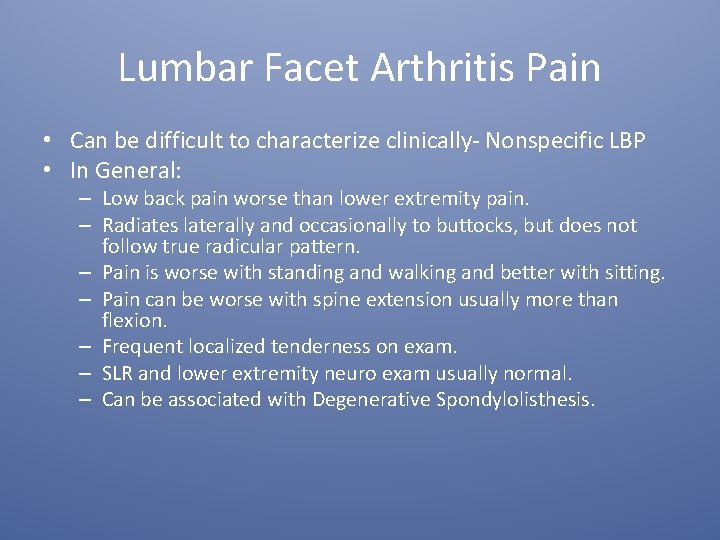
Lumbar Facet Arthritis Pain • Can be difficult to characterize clinically- Nonspecific LBP • In General: – Low back pain worse than lower extremity pain. – Radiates laterally and occasionally to buttocks, but does not follow true radicular pattern. – Pain is worse with standing and walking and better with sitting. – Pain can be worse with spine extension usually more than flexion. – Frequent localized tenderness on exam. – SLR and lower extremity neuro exam usually normal. – Can be associated with Degenerative Spondylolisthesis.
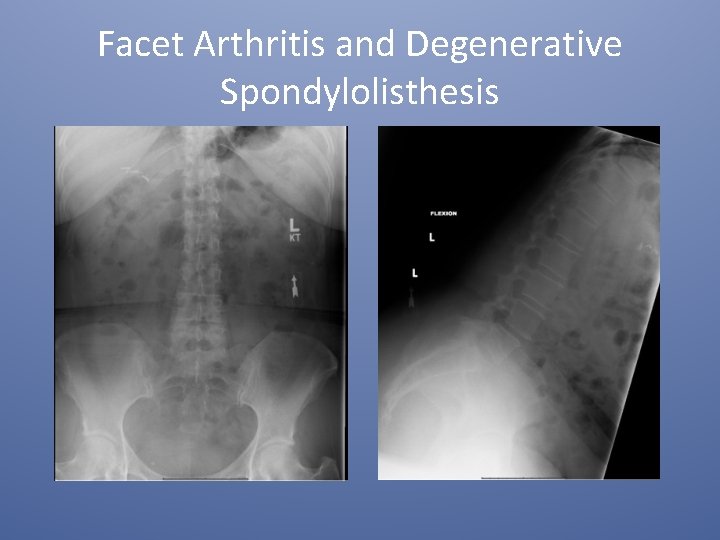
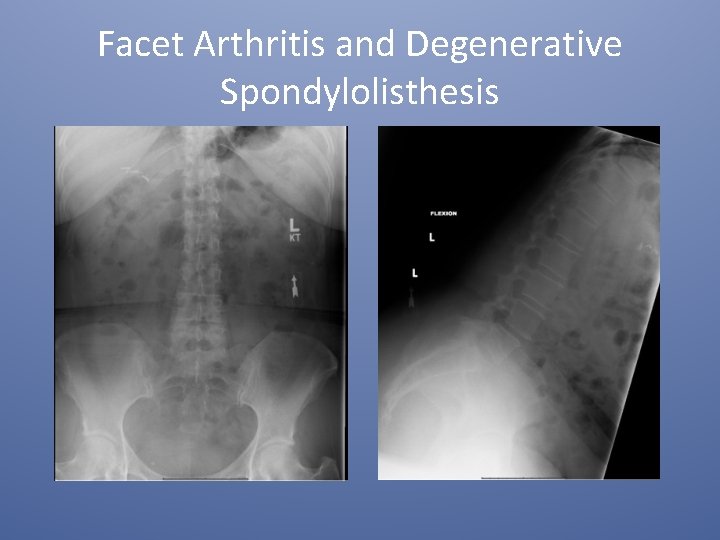
Facet Arthritis and Degenerative Spondylolisthesis
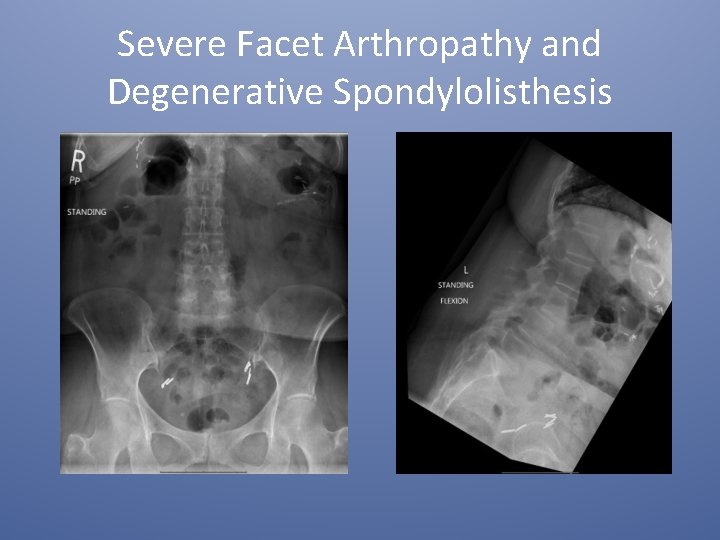
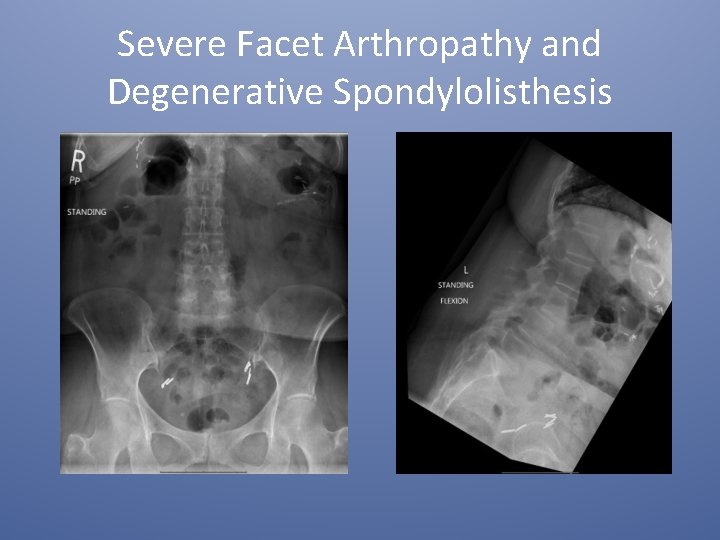
Severe Facet Arthropathy and Degenerative Spondylolisthesis
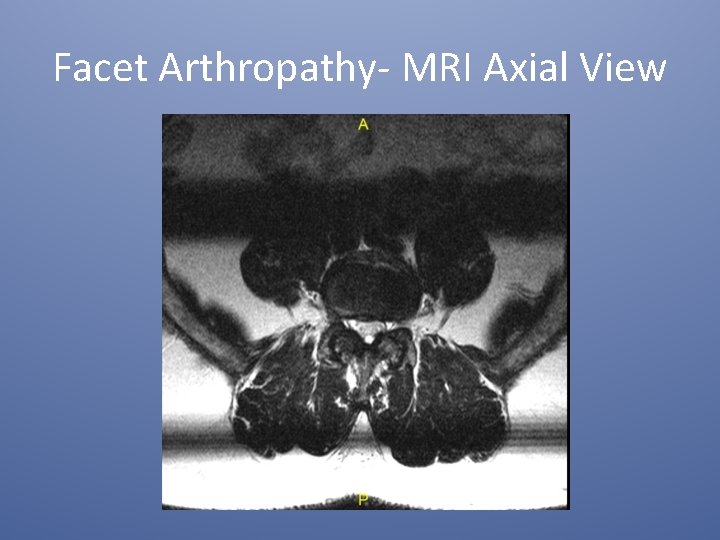
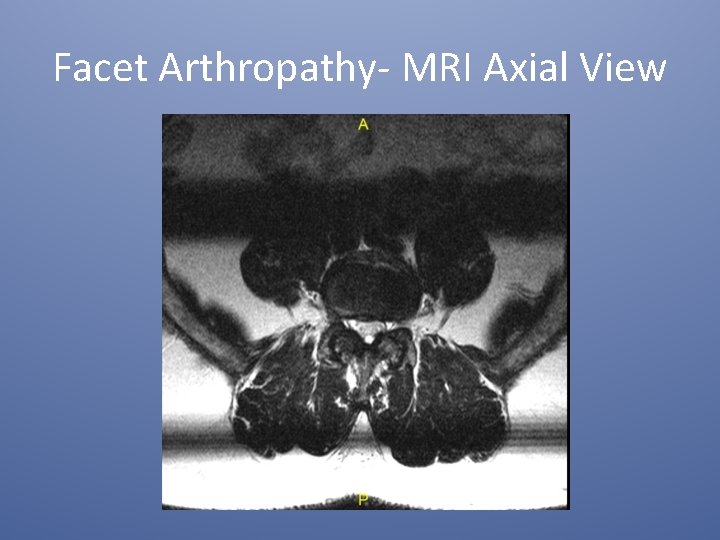
Facet Arthropathy- MRI Axial View

Facet Arthropathy/Degenerative Spondylolisthesis- Sagittal MRI
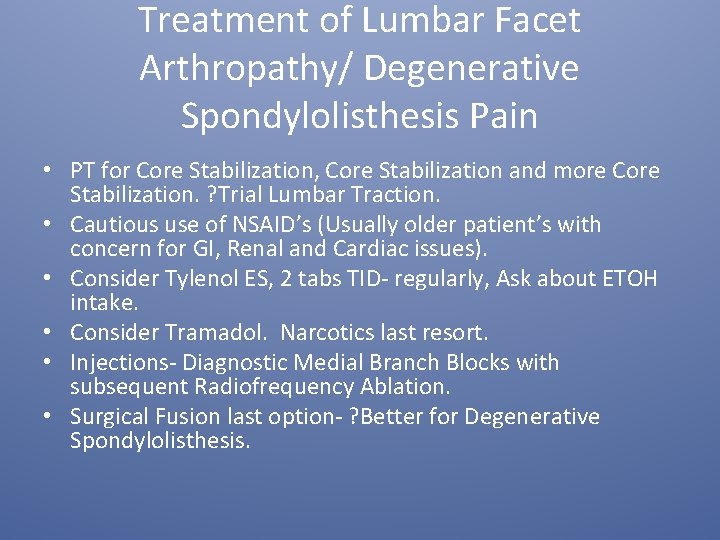
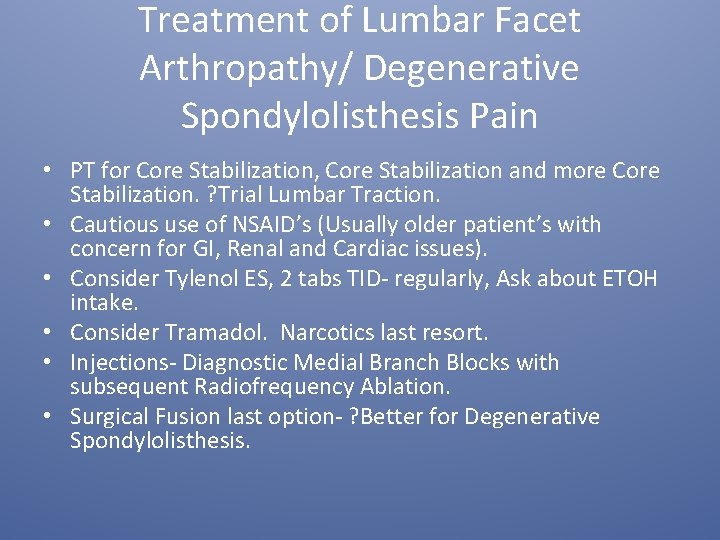
Treatment of Lumbar Facet Arthropathy/ Degenerative Spondylolisthesis Pain • PT for Core Stabilization, Core Stabilization and more Core Stabilization. ? Trial Lumbar Traction. • Cautious use of NSAID’s (Usually older patient’s with concern for GI, Renal and Cardiac issues). • Consider Tylenol ES, 2 tabs TID- regularly, Ask about ETOH intake. • Consider Tramadol. Narcotics last resort. • Injections- Diagnostic Medial Branch Blocks with subsequent Radiofrequency Ablation. • Surgical Fusion last option- ? Better for Degenerative Spondylolisthesis.
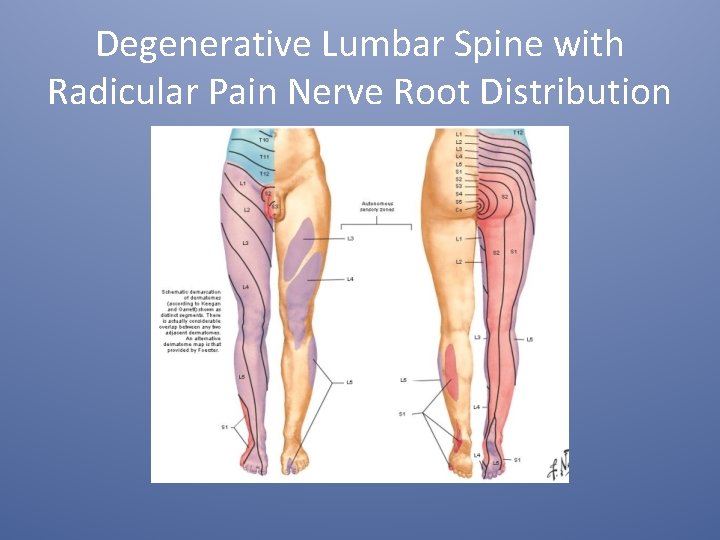
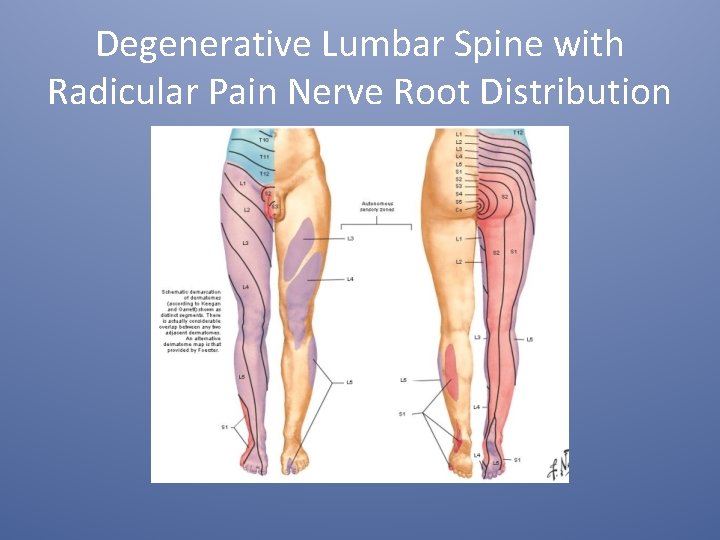
Degenerative Lumbar Spine with Radicular Pain Nerve Root Distribution
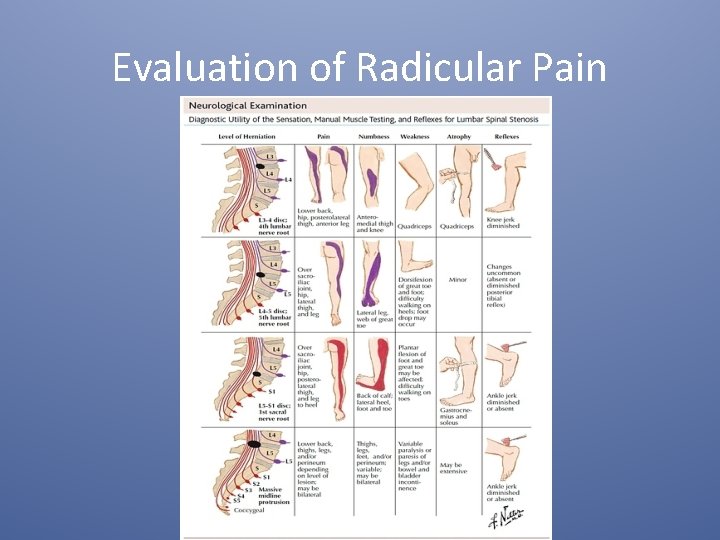
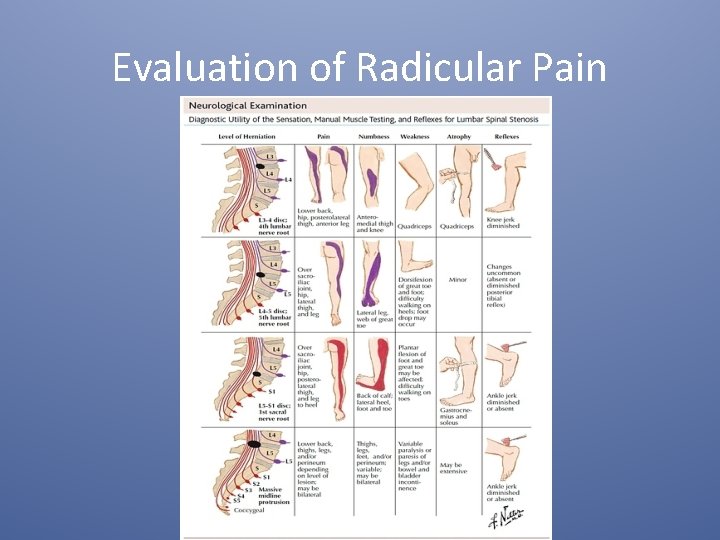
Evaluation of Radicular Pain
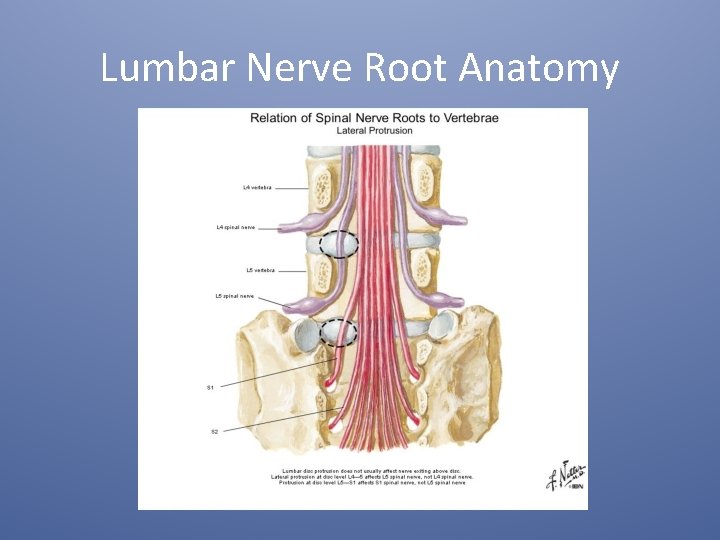
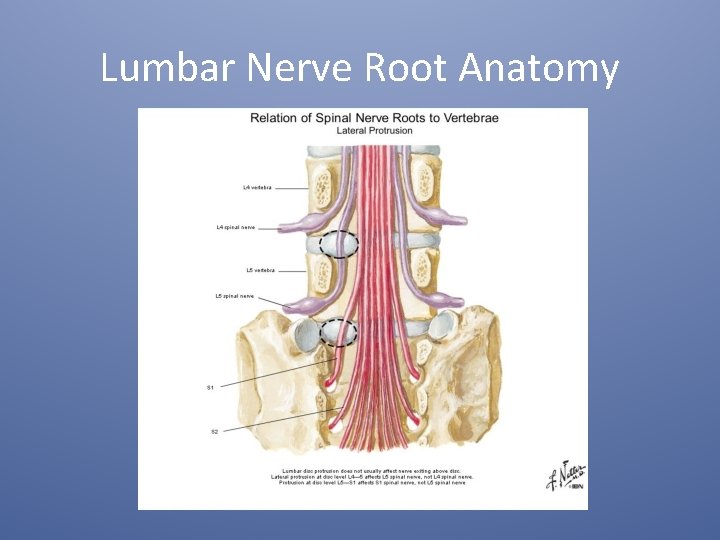
Lumbar Nerve Root Anatomy
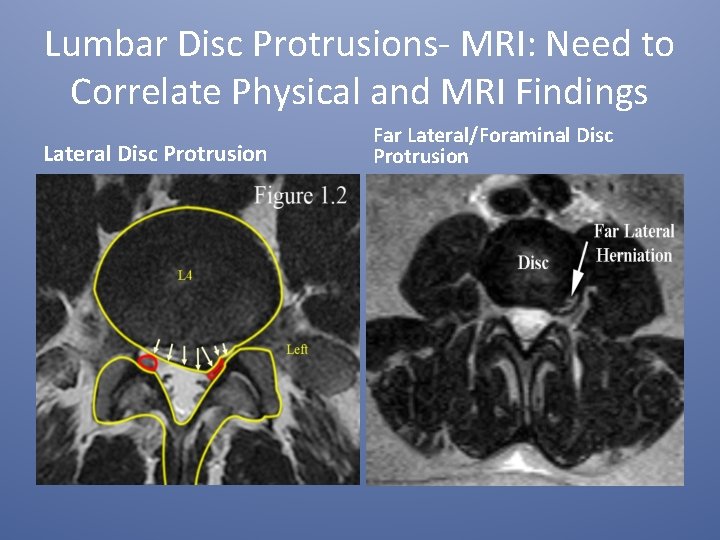
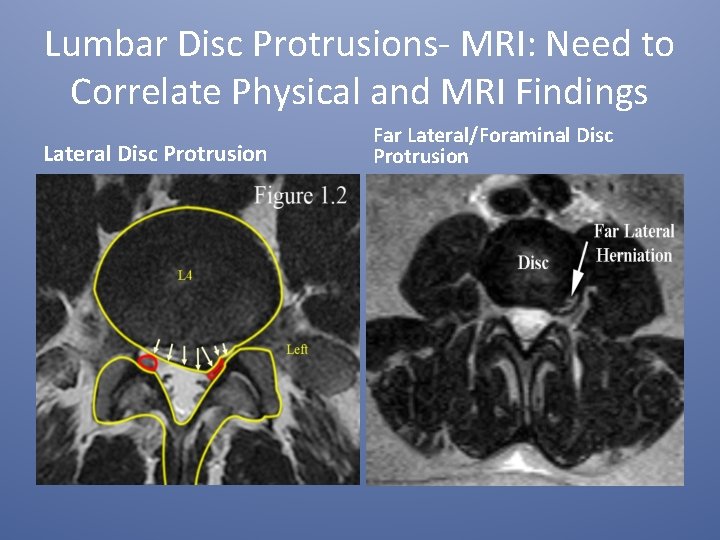
Lumbar Disc Protrusions- MRI: Need to Correlate Physical and MRI Findings Lateral Disc Protrusion Far Lateral/Foraminal Disc Protrusion
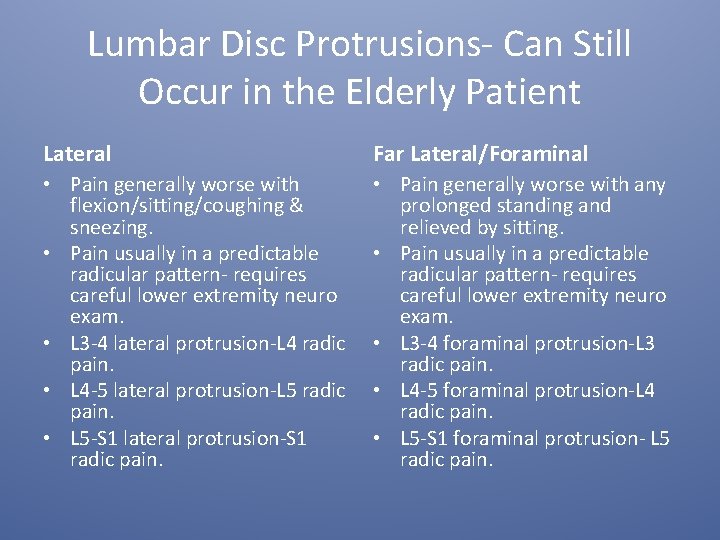
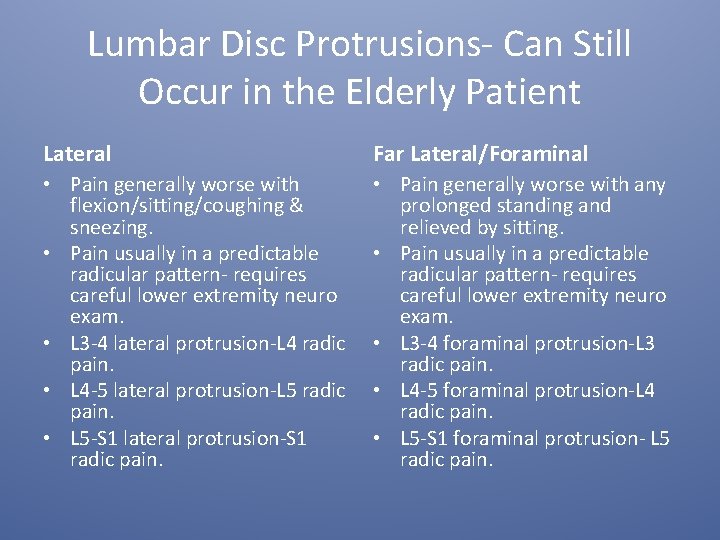
Lumbar Disc Protrusions- Can Still Occur in the Elderly Patient Lateral Far Lateral/Foraminal • Pain generally worse with flexion/sitting/coughing & sneezing. • Pain usually in a predictable radicular pattern- requires careful lower extremity neuro exam. • L 3 -4 lateral protrusion-L 4 radic pain. • L 4 -5 lateral protrusion-L 5 radic pain. • L 5 -S 1 lateral protrusion-S 1 radic pain. • Pain generally worse with any prolonged standing and relieved by sitting. • Pain usually in a predictable radicular pattern- requires careful lower extremity neuro exam. • L 3 -4 foraminal protrusion-L 3 radic pain. • L 4 -5 foraminal protrusion-L 4 radic pain. • L 5 -S 1 foraminal protrusion- L 5 radic pain.
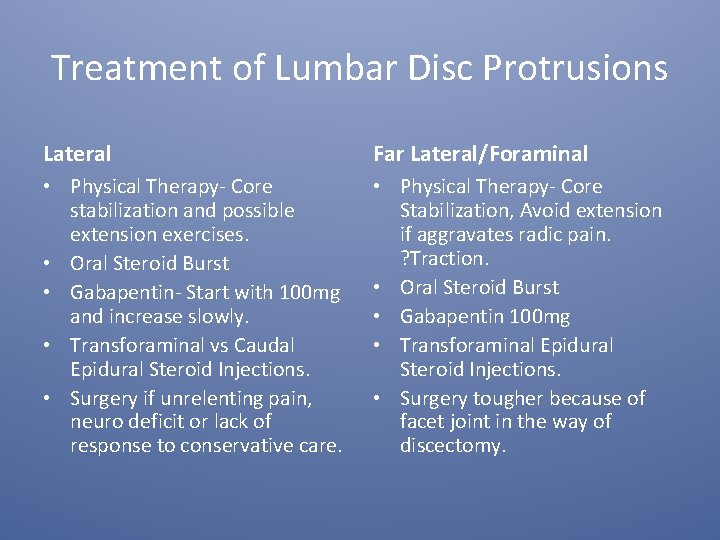
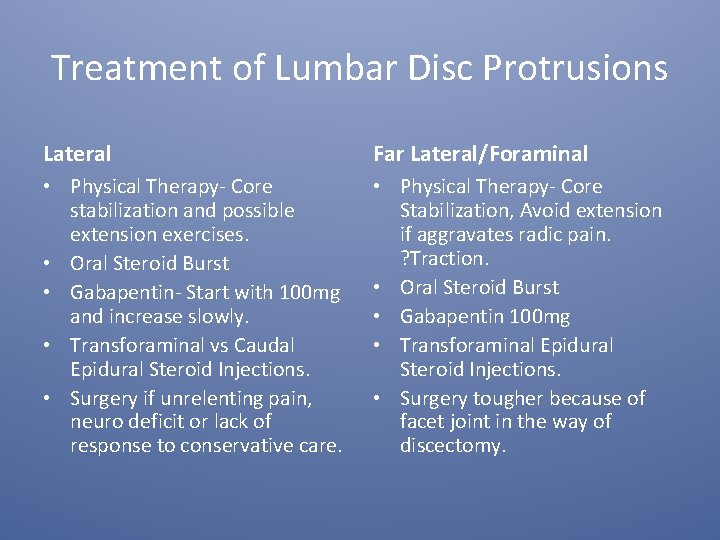
Treatment of Lumbar Disc Protrusions Lateral Far Lateral/Foraminal • Physical Therapy- Core stabilization and possible extension exercises. • Oral Steroid Burst • Gabapentin- Start with 100 mg and increase slowly. • Transforaminal vs Caudal Epidural Steroid Injections. • Surgery if unrelenting pain, neuro deficit or lack of response to conservative care. • Physical Therapy- Core Stabilization, Avoid extension if aggravates radic pain. ? Traction. • Oral Steroid Burst • Gabapentin 100 mg • Transforaminal Epidural Steroid Injections. • Surgery tougher because of facet joint in the way of discectomy.
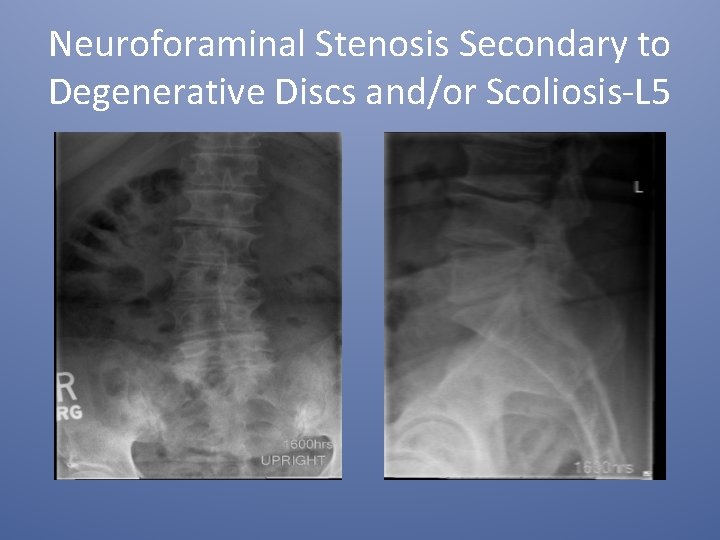
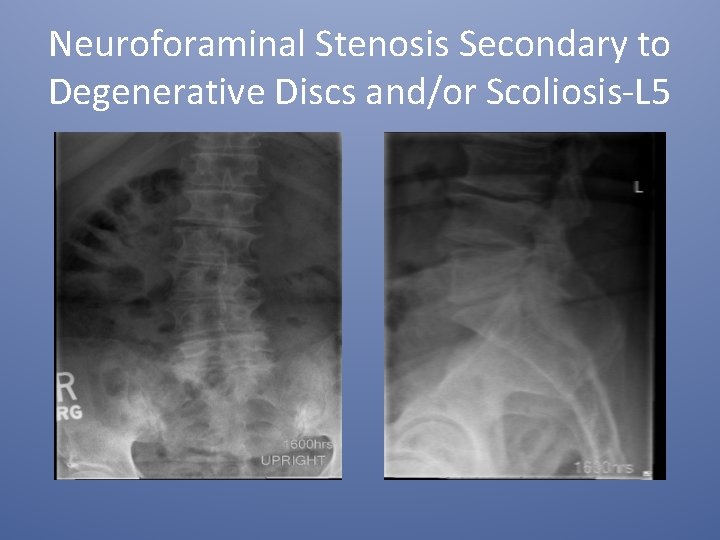
Neuroforaminal Stenosis Secondary to Degenerative Discs and/or Scoliosis-L 5

Neuroforaminal Stenosis Secondary to Degenerative Scoliosis- L 5 Radic
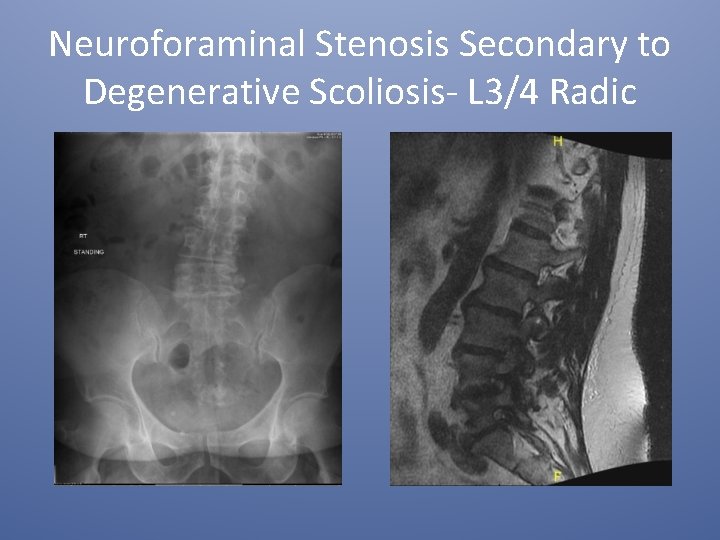
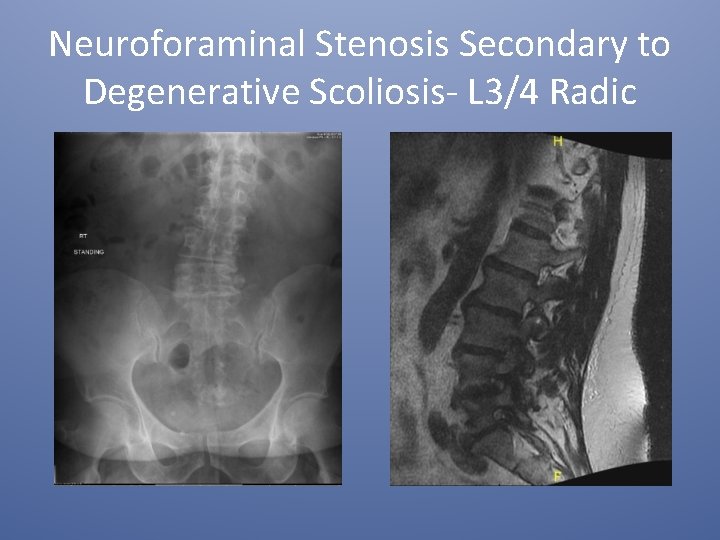
Neuroforaminal Stenosis Secondary to Degenerative Scoliosis- L 3/4 Radic
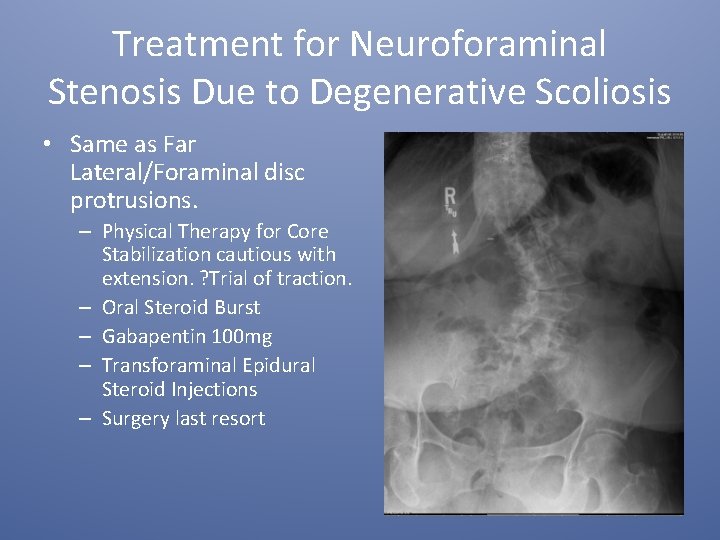
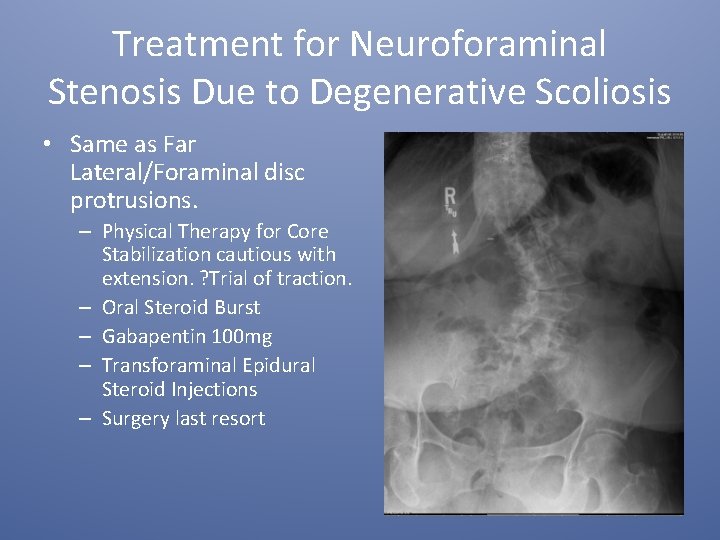
Treatment for Neuroforaminal Stenosis Due to Degenerative Scoliosis • Same as Far Lateral/Foraminal disc protrusions. – Physical Therapy for Core Stabilization cautious with extension. ? Trial of traction. – Oral Steroid Burst – Gabapentin 100 mg – Transforaminal Epidural Steroid Injections – Surgery last resort
Spinal Stenosis With and Without Neurogenic Claudication (ICD-10) • Low back pain with or without radicular pain/numbness/weakness in one or both legs that is worse with prolonged standing or walking (with lower extremity pain and cramping relieved by sitting- Neurogenic Claudication). Pain frequently better when leaning forward on shopping cart.
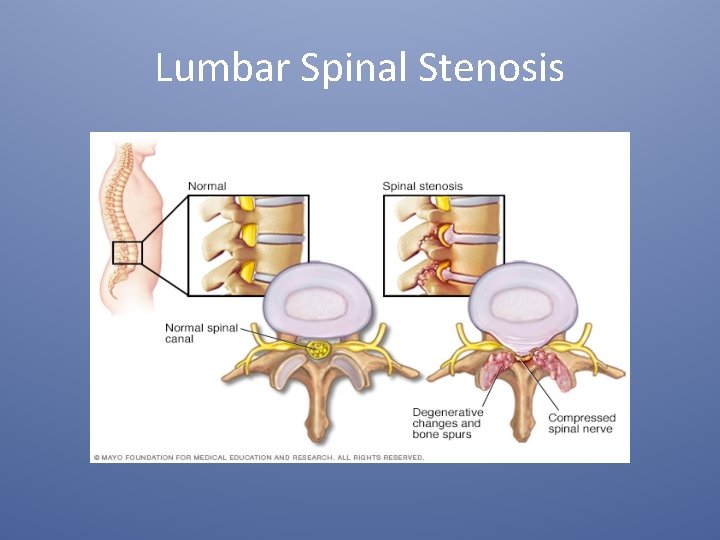
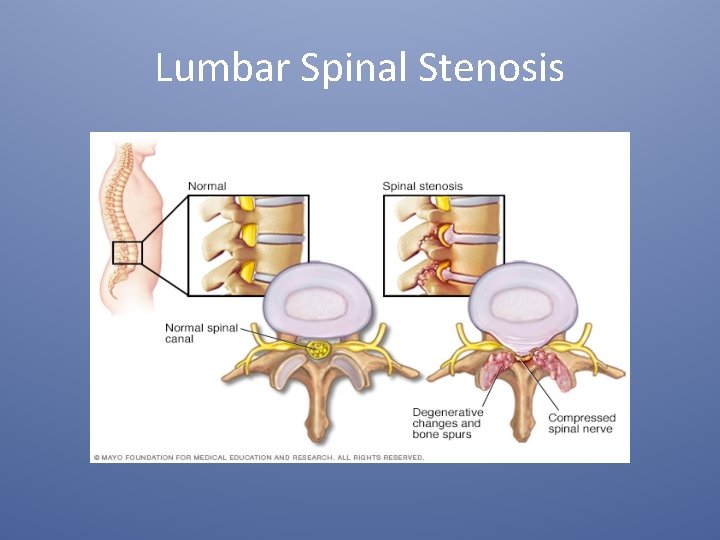
Lumbar Spinal Stenosis
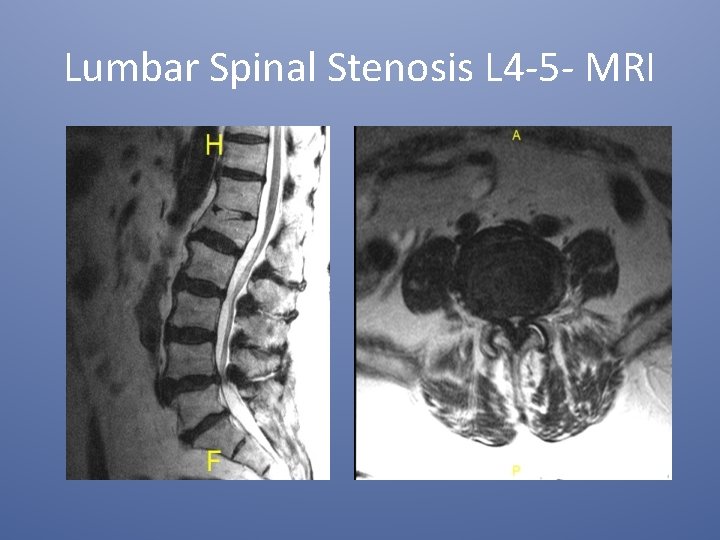
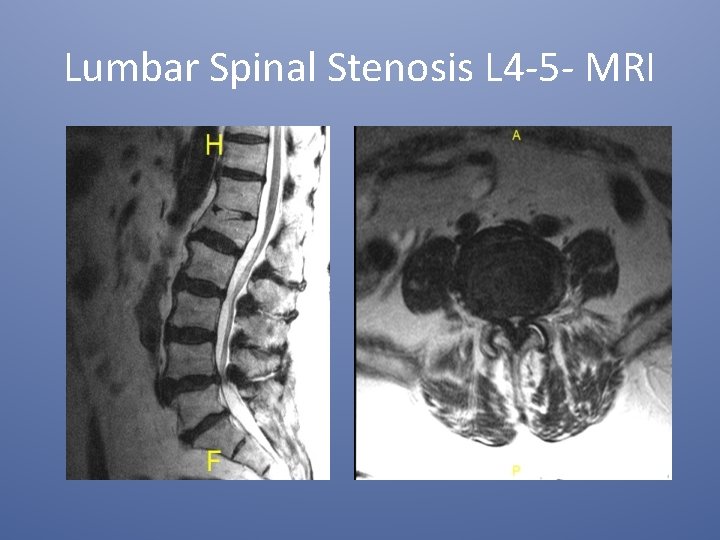
Lumbar Spinal Stenosis L 4 -5 - MRI
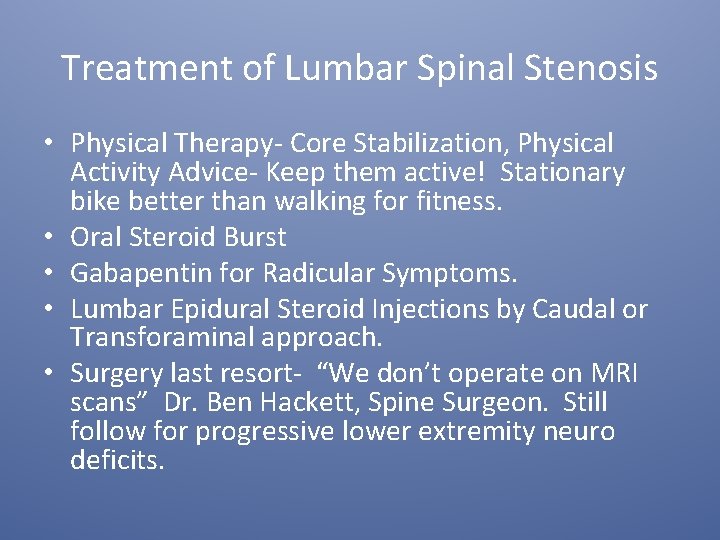
Treatment of Lumbar Spinal Stenosis • Physical Therapy- Core Stabilization, Physical Activity Advice- Keep them active! Stationary bike better than walking for fitness. • Oral Steroid Burst • Gabapentin for Radicular Symptoms. • Lumbar Epidural Steroid Injections by Caudal or Transforaminal approach. • Surgery last resort- “We don’t operate on MRI scans” Dr. Ben Hackett, Spine Surgeon. Still follow for progressive lower extremity neuro deficits.
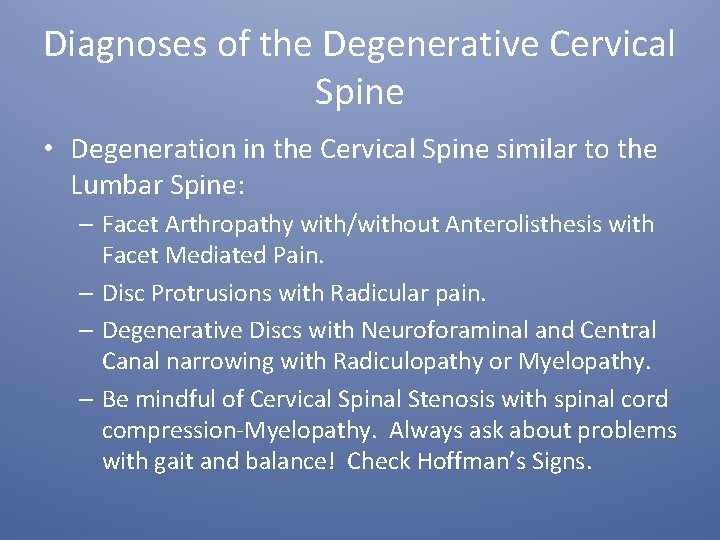
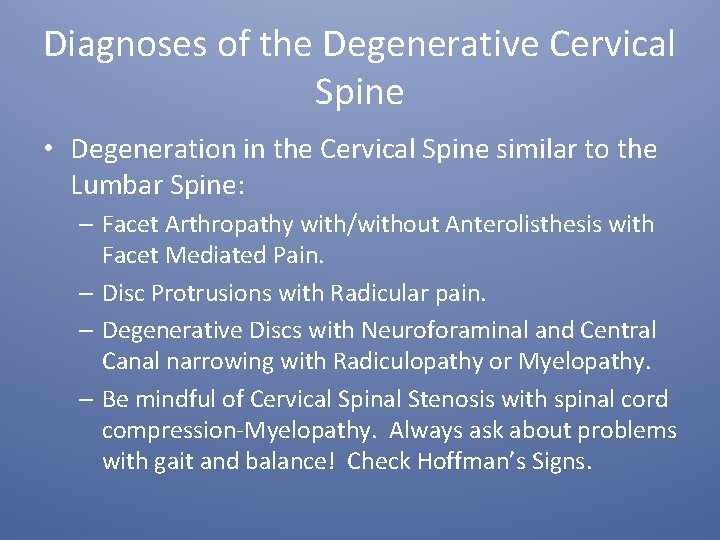
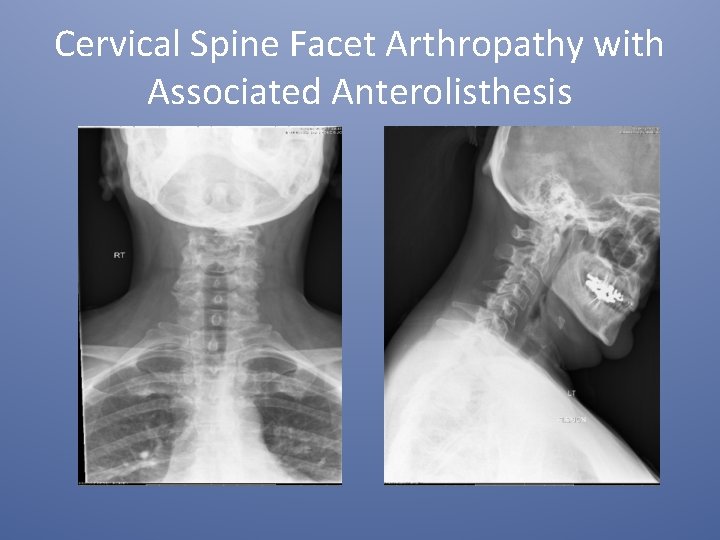
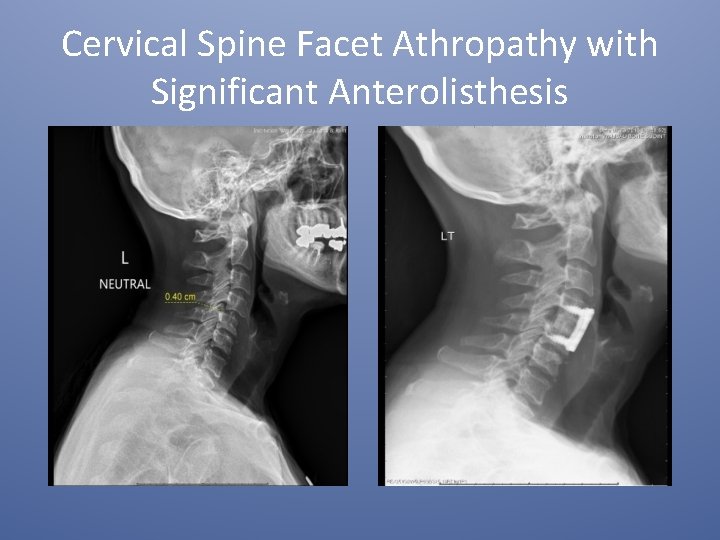
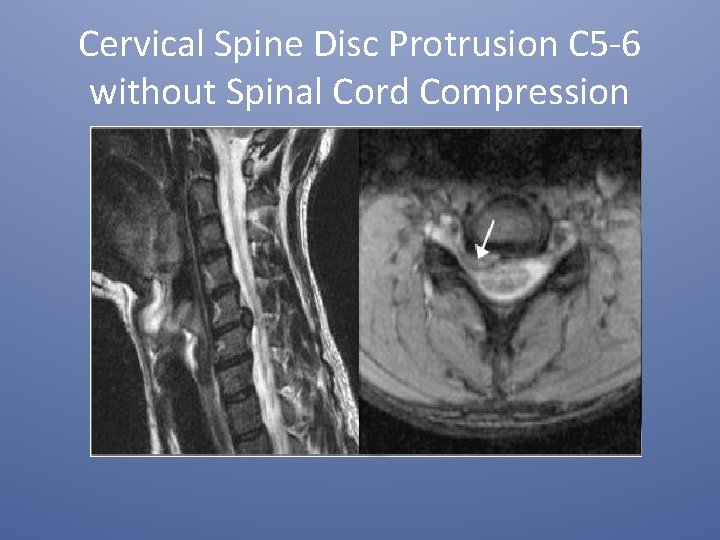
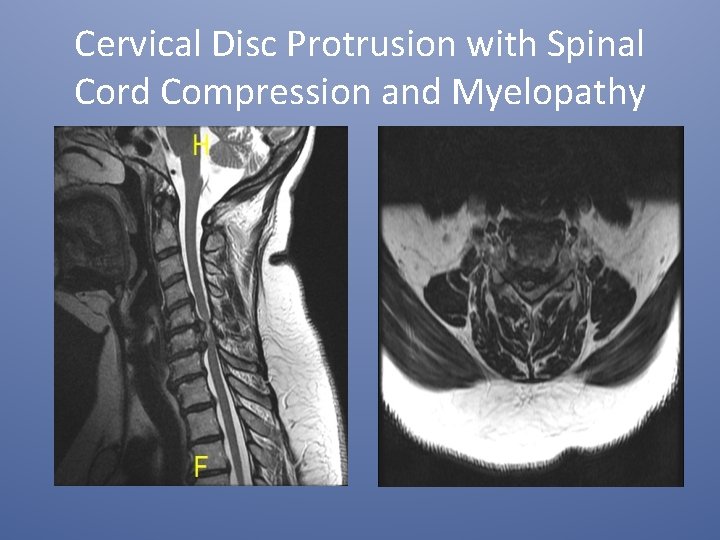
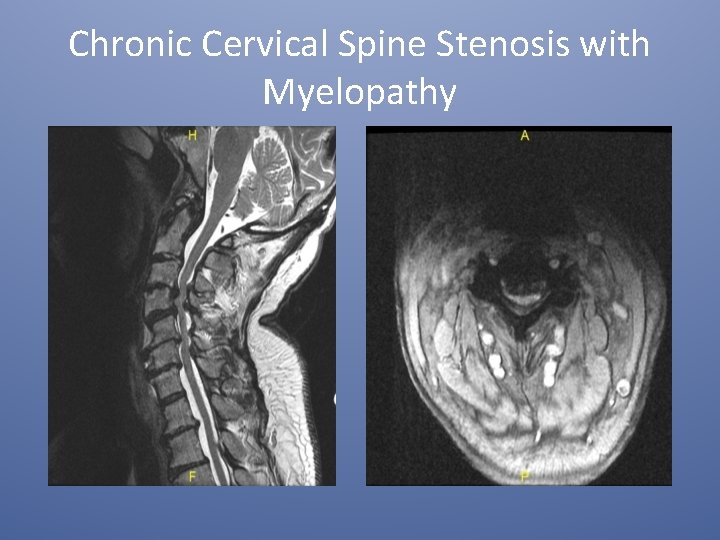
Diagnoses of the Degenerative Cervical Spine • Degeneration in the Cervical Spine similar to the Lumbar Spine: – Facet Arthropathy with/without Anterolisthesis with Facet Mediated Pain. – Disc Protrusions with Radicular pain. – Degenerative Discs with Neuroforaminal and Central Canal narrowing with Radiculopathy or Myelopathy. – Be mindful of Cervical Spinal Stenosis with spinal cord compression-Myelopathy. Always ask about problems with gait and balance! Check Hoffman’s Signs.
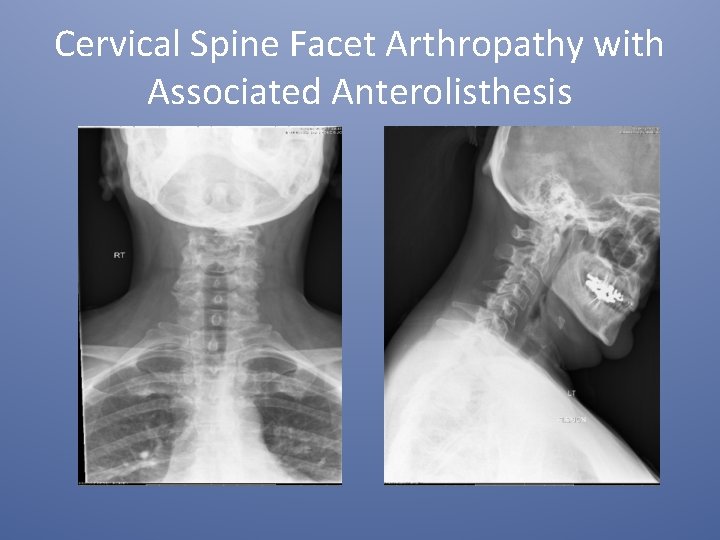
Cervical Spine Facet Arthropathy with Associated Anterolisthesis
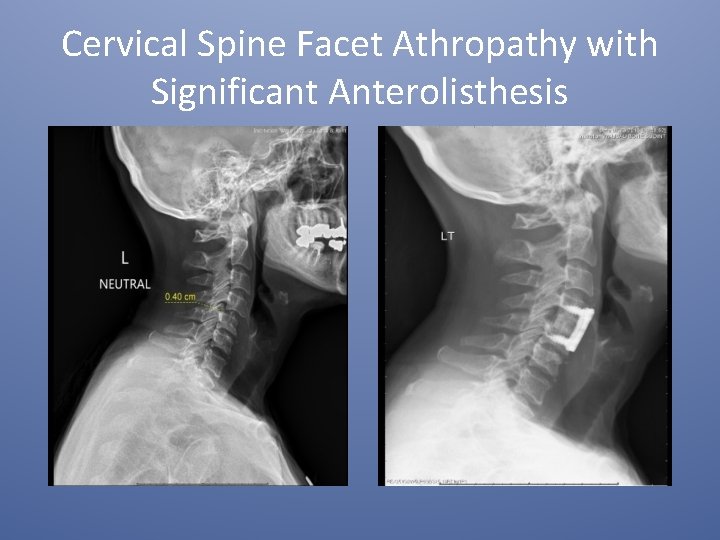
Cervical Spine Facet Athropathy with Significant Anterolisthesis
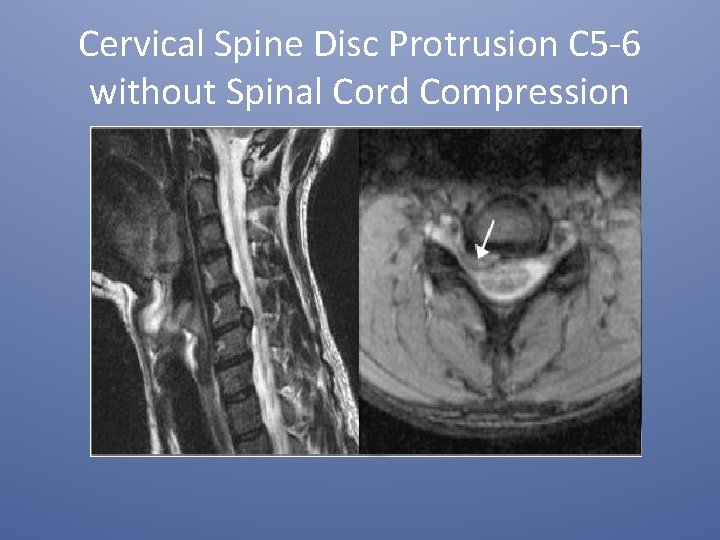
Cervical Spine Disc Protrusion C 5 -6 without Spinal Cord Compression
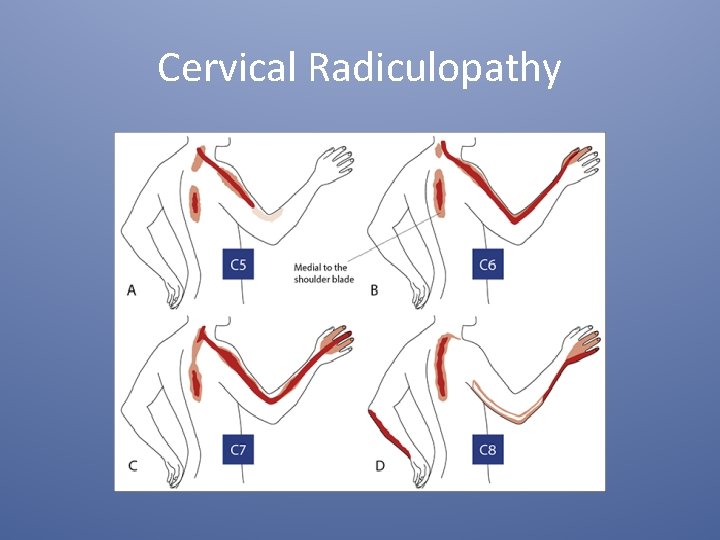
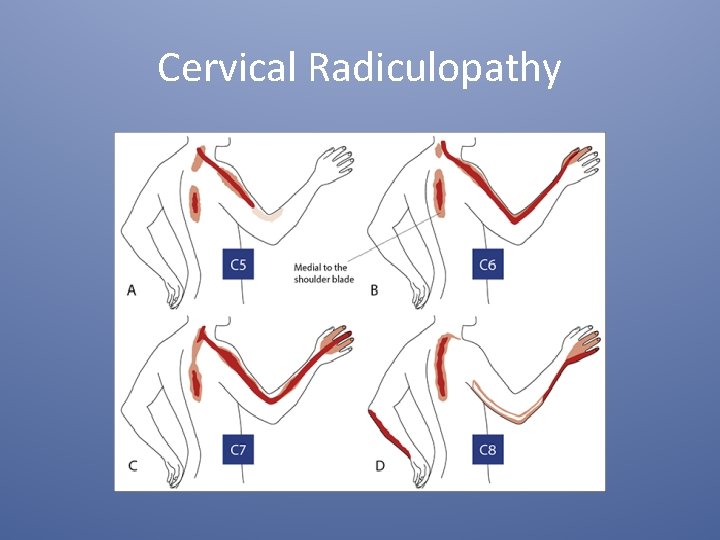
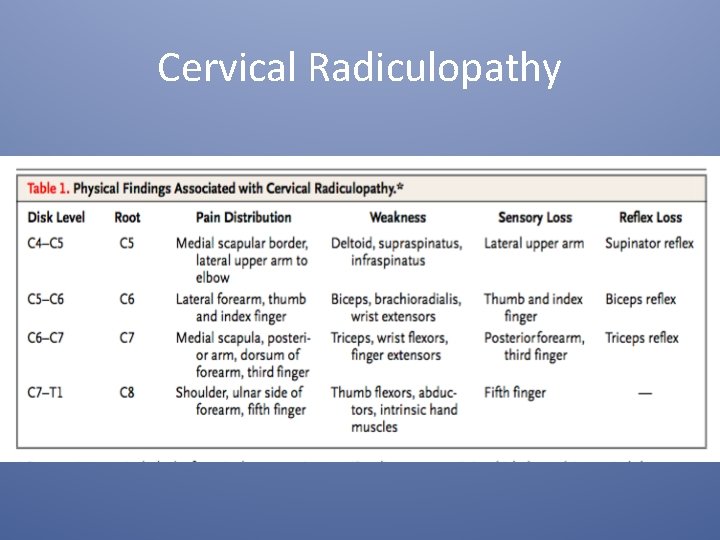
Cervical Radiculopathy
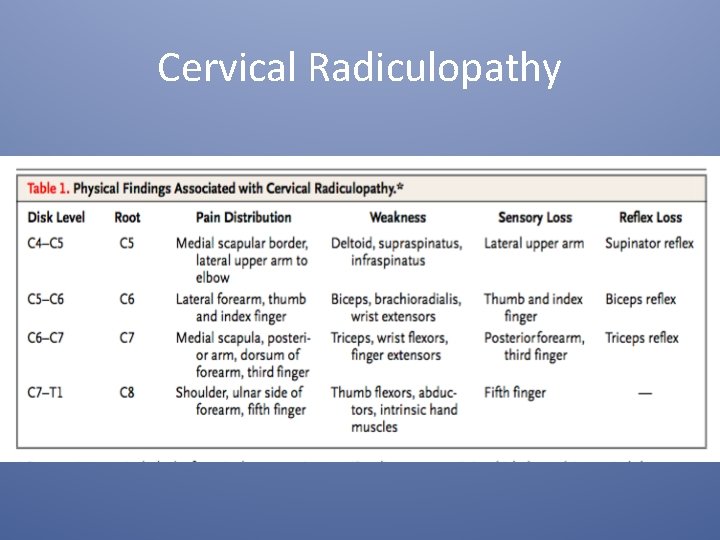
Cervical Radiculopathy
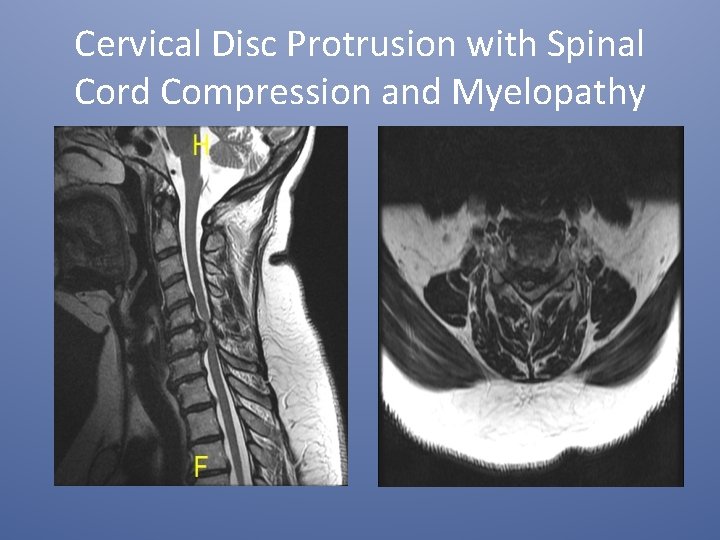
Cervical Disc Protrusion with Spinal Cord Compression and Myelopathy
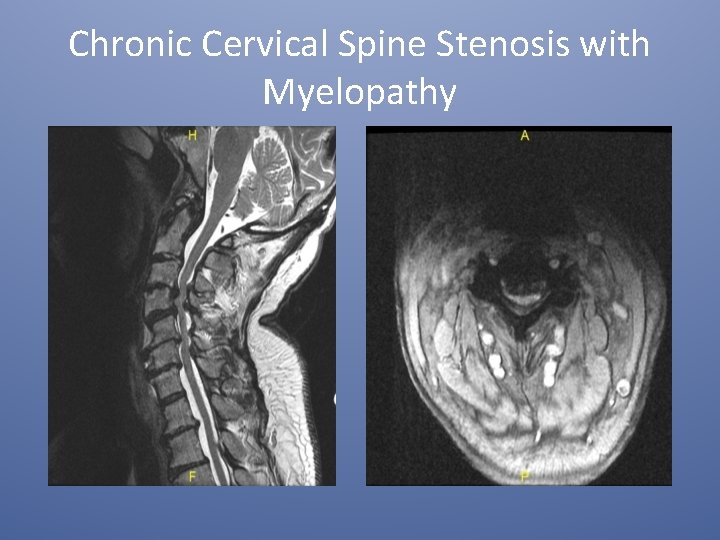
Chronic Cervical Spine Stenosis with Myelopathy
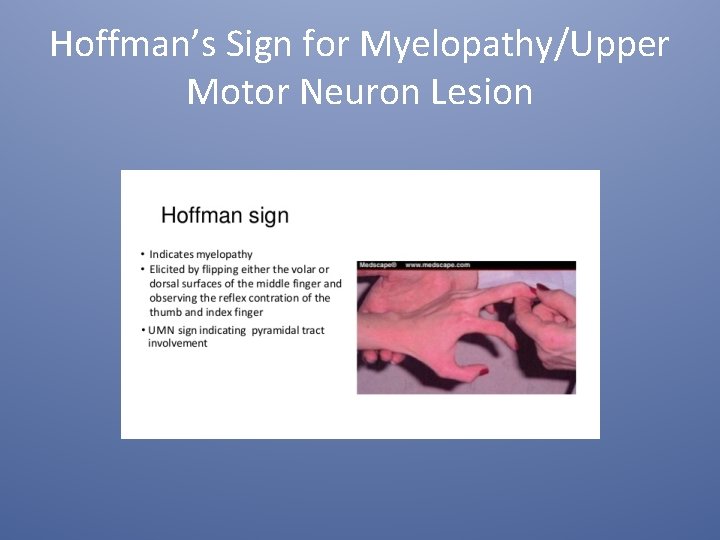
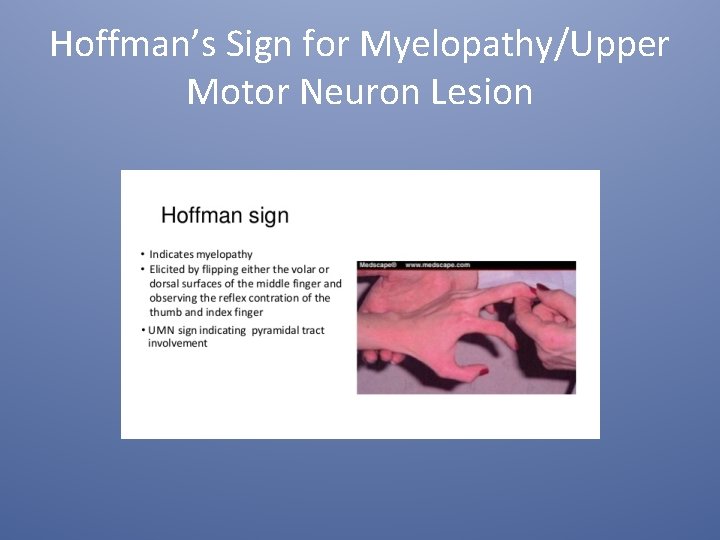
Hoffman’s Sign for Myelopathy/Upper Motor Neuron Lesion
Other Signs of Myelopathy/Upper Motor Neuron Lesion • • Hyperreflexia Sustained Clonus Babinski Sign Romberg’s Testing Heel/Toe Walk Tandem Gait Lhermitte’s Sign

That’s All Folks
 Level of care primary secondary tertiary
Level of care primary secondary tertiary Degenerative myelopathy wayne
Degenerative myelopathy wayne Fascetaria
Fascetaria Spinal cord spasticity
Spinal cord spasticity Genu recurvatum
Genu recurvatum Dorsolumbar
Dorsolumbar Shilla procedure
Shilla procedure Rib vertebral angle
Rib vertebral angle Nerve fibers
Nerve fibers Genial tubercle
Genial tubercle The story spine
The story spine The story spine
The story spine Interalveolar septa mandible
Interalveolar septa mandible Spine technologies india pvt ltd
Spine technologies india pvt ltd Ankle range of motion goniometer
Ankle range of motion goniometer Schober test adalah
Schober test adalah Posterior inferior iliac spine
Posterior inferior iliac spine Bid rent theory model
Bid rent theory model 1/2 inch binder spine template
1/2 inch binder spine template Sulcus lacrimalis
Sulcus lacrimalis Short spine board
Short spine board Quartiere spine bianche matera
Quartiere spine bianche matera Spine vs thorn
Spine vs thorn Fabric connect extreme
Fabric connect extreme Spine precautions
Spine precautions Intervertebral disc prolapse
Intervertebral disc prolapse Chapter 5 the skeletal system vertebral column
Chapter 5 the skeletal system vertebral column A short backboard or vest-style immobilization
A short backboard or vest-style immobilization Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Chapter 20 worksheet the spine
Chapter 20 worksheet the spine Anterior superior iliac spine
Anterior superior iliac spine Tata letak layout toko
Tata letak layout toko Ganglion on spine
Ganglion on spine Spine layout store
Spine layout store Diarrhea reflexology
Diarrhea reflexology Gerdy's tubercle
Gerdy's tubercle Facet joint anatomy
Facet joint anatomy Functions of cerebellum
Functions of cerebellum Spine arthrokinematics
Spine arthrokinematics Thoracic vertebrae superior view
Thoracic vertebrae superior view Spine blood spatter definition
Spine blood spatter definition Milwaukee brace
Milwaukee brace Glenoid fossa
Glenoid fossa Rattle spine nms
Rattle spine nms Spine pathology
Spine pathology Decussation of pyramids
Decussation of pyramids