PAEDIATRIC PALLIATIVE CARE PAEDIATRIC PALLIATIVE PAIN Dr Emma



- Slides: 63
PAEDIATRIC PALLIATIVE CARE & PAEDIATRIC PALLIATIVE PAIN Dr Emma Heckford May 2012 Registrar in Paediatric Palliative Medicine, University Hospital Wales Disclaimer: Whilst every effort has been made to ensure that the information in this presentation is accurate and referenced the author does not accept any responsibility for the use by any third parties.
Introduction to Paediatric Palliative Care Pain in Paediatric Palliative Care Case Studies
Introduction to Paediatric Palliative Care
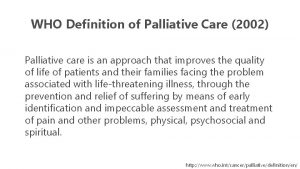
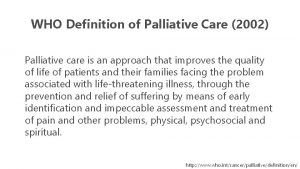
Palliative Care for Children ACT/RCPCH definition (2009): “an active and total approach to care, embracing physical, emotional, social and spiritual elements” Active (not simply stopping treatment) Total ‘Best quality of life for patient and family throughout course of a life-limiting illness’
PPC - Since when? Evolution over last 30 years Various models of care based on local needs and resources Paediatric Palliative Medicine now a recognised subspecialty Currently in UK: 10 tertiary consultants ~ 50 ‘paediatricians with a special interest’
Why PPC? At least 50% of child deaths in UK caused by LLCs ~ 20, 000 children in England living with conditions likely to require PC input But: - Symptom management suboptimal Professional anxieties Most children die in hospital, often intensive care
Making a difference Offering (and enabling) child and family choices Improving quality of life – ‘as well as possible for as long as possible’ Supporting adjustment and goal setting Improving experience of death Improving bereavement outcomes
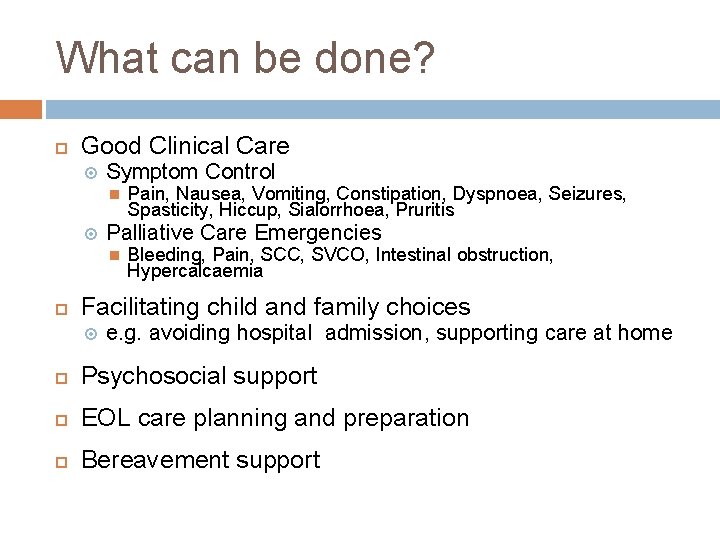
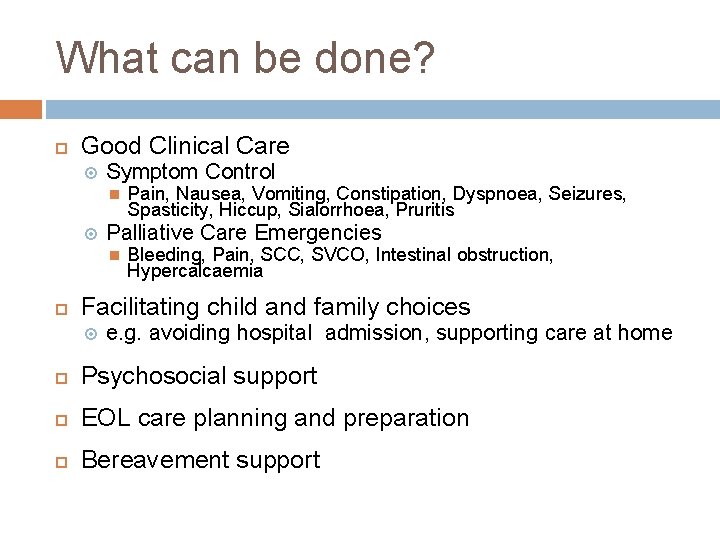
What can be done? Good Clinical Care Symptom Control Palliative Care Emergencies Pain, Nausea, Vomiting, Constipation, Dyspnoea, Seizures, Spasticity, Hiccup, Sialorrhoea, Pruritis Bleeding, Pain, SCC, SVCO, Intestinal obstruction, Hypercalcaemia Facilitating child and family choices e. g. avoiding hospital admission, supporting care at home Psychosocial support EOL care planning and preparation Bereavement support
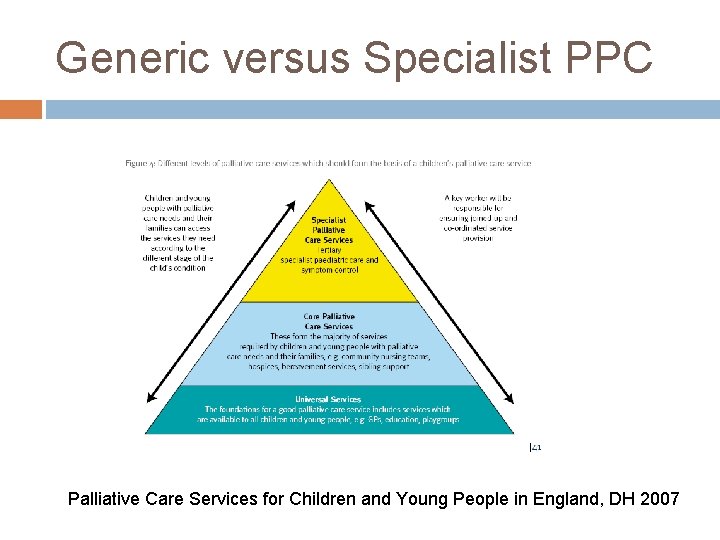
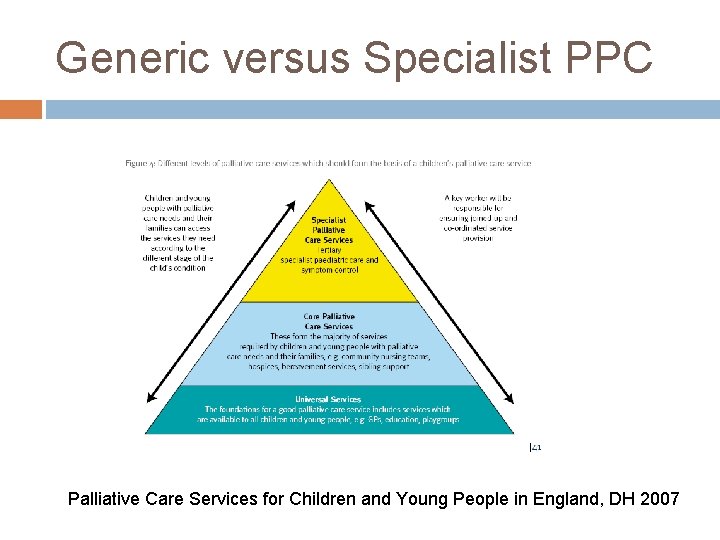
Generic versus Specialist PPC Palliative Care Services for Children and Young People in England, DH 2007
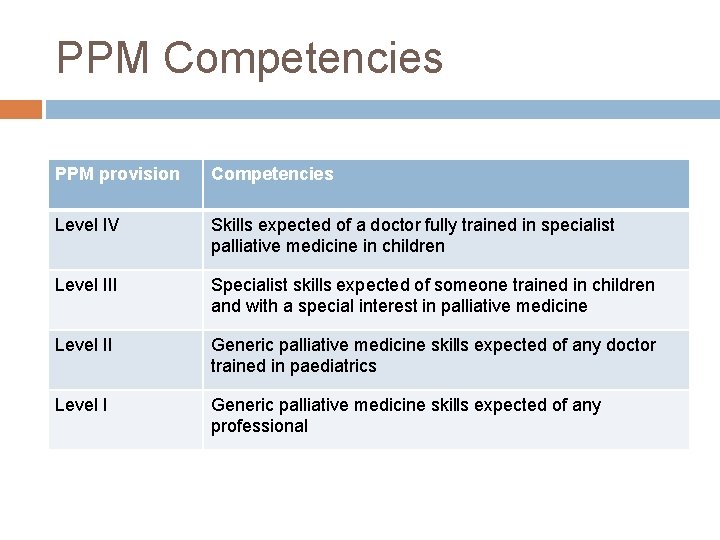
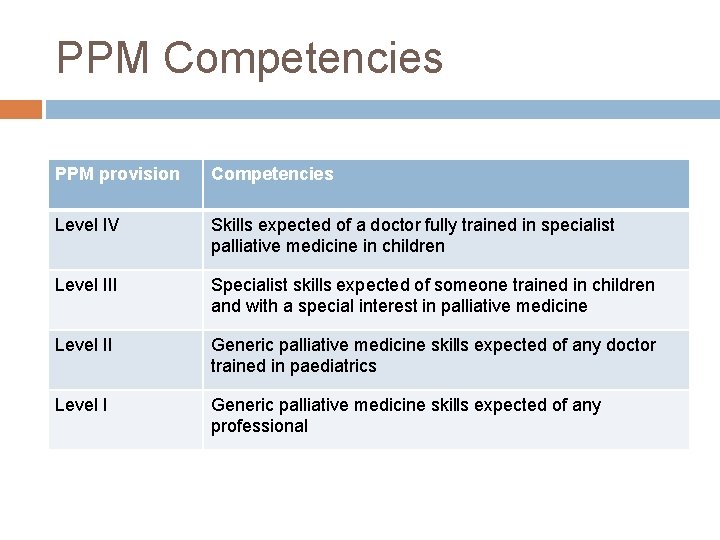
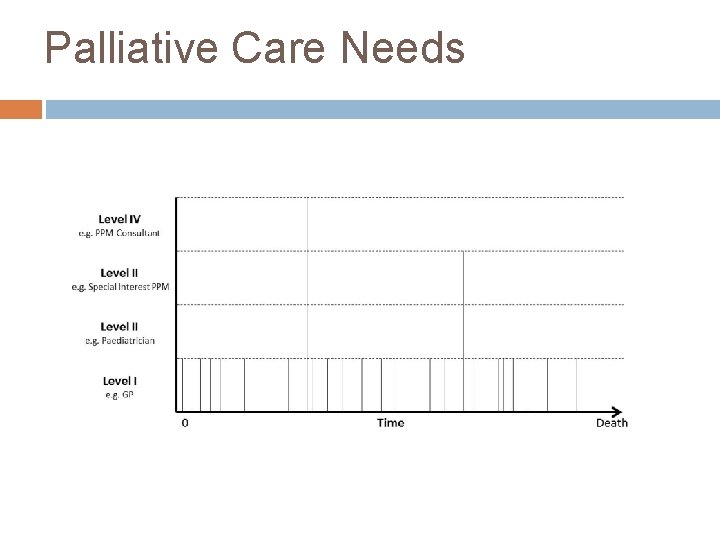
PPM Competencies PPM provision Competencies Level IV Skills expected of a doctor fully trained in specialist palliative medicine in children Level III Specialist skills expected of someone trained in children and with a special interest in palliative medicine Level II Generic palliative medicine skills expected of any doctor trained in paediatrics Level I Generic palliative medicine skills expected of any professional
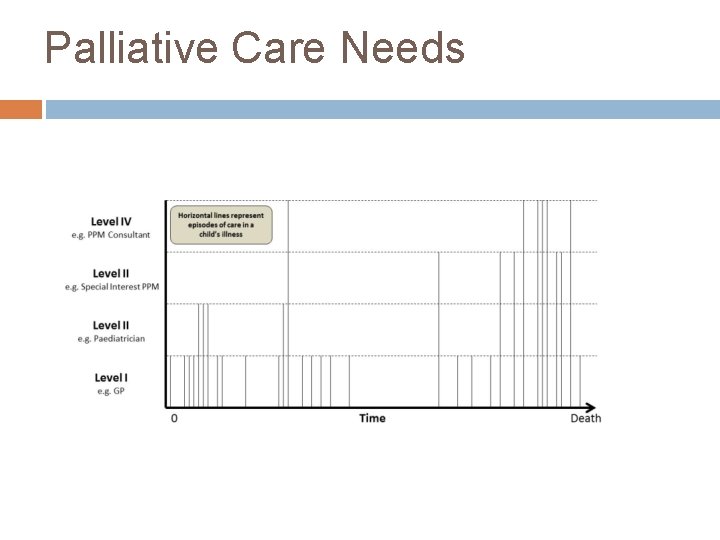
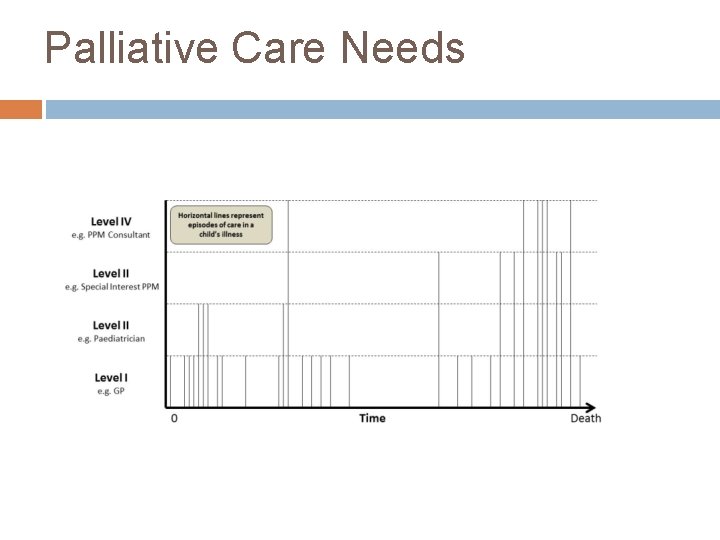
Palliative Care Needs
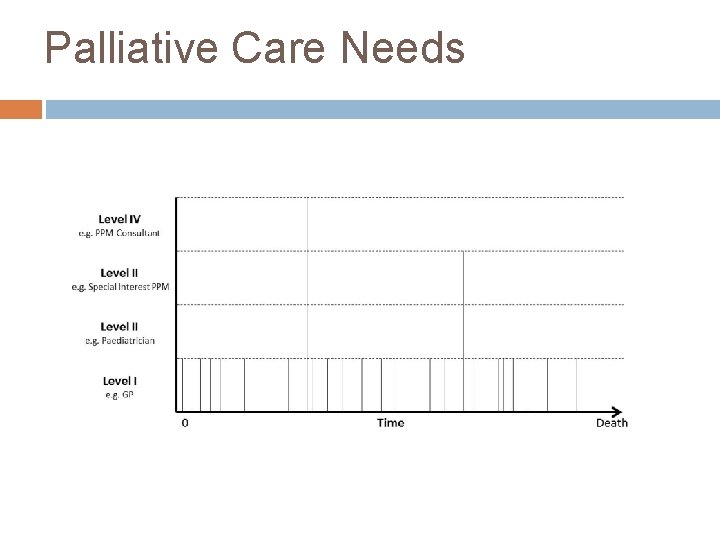
Palliative Care Needs
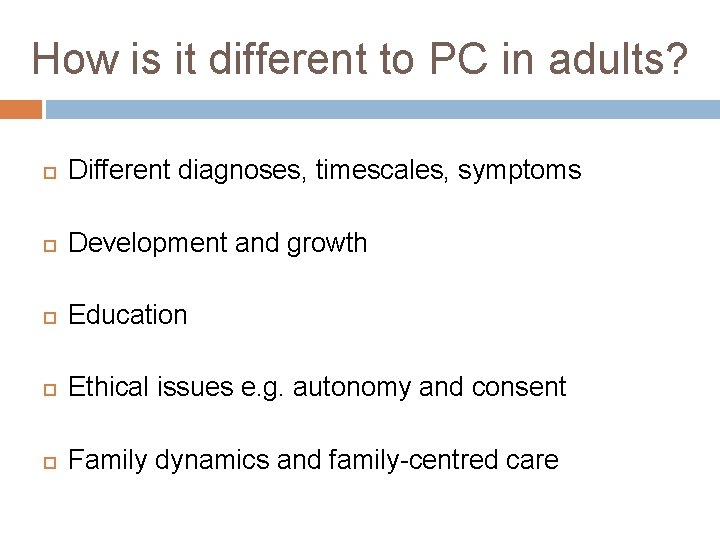
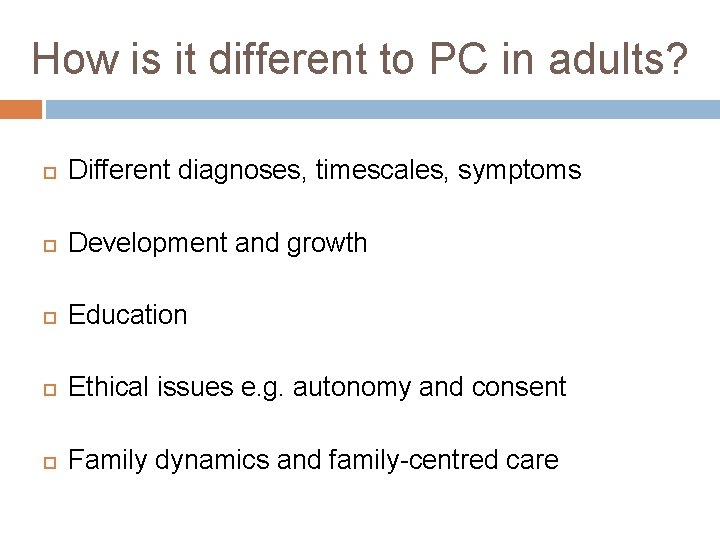
How is it different to PC in adults? Different diagnoses, timescales, symptoms Development and growth Education Ethical issues e. g. autonomy and consent Family dynamics and family-centred care
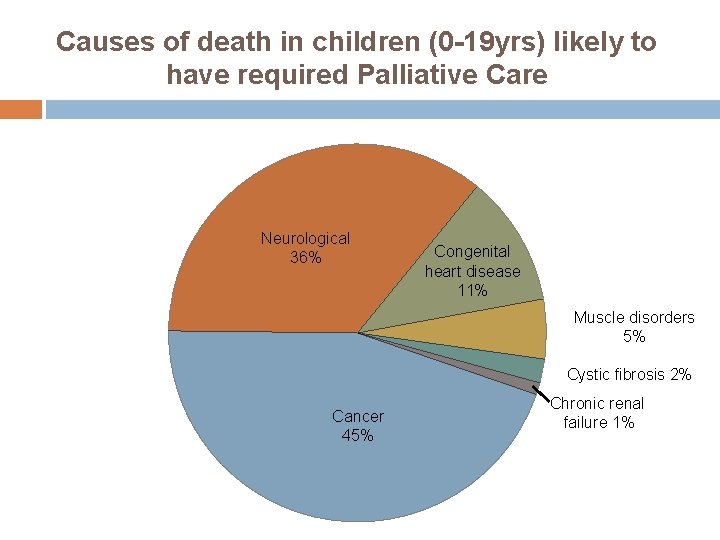
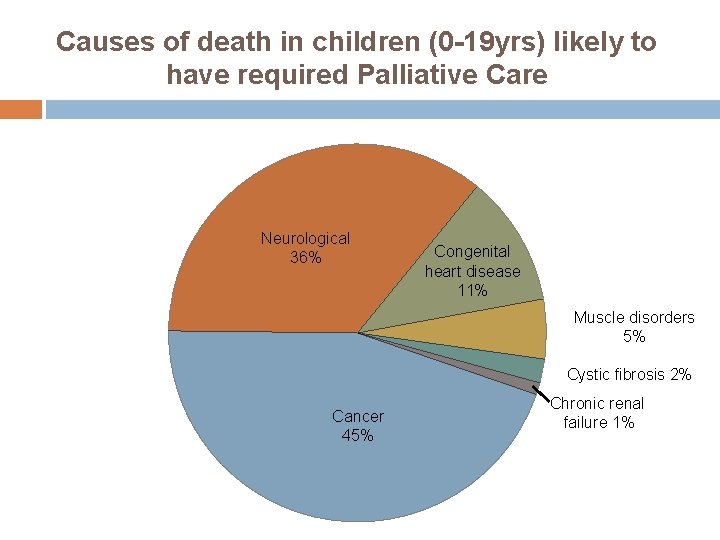
Causes of death in children (0 -19 yrs) likely to have required Palliative Care Neurological 36% Congenital heart disease 11% Muscle disorders 5% Cystic fibrosis 2% Cancer 45% Chronic renal failure 1%
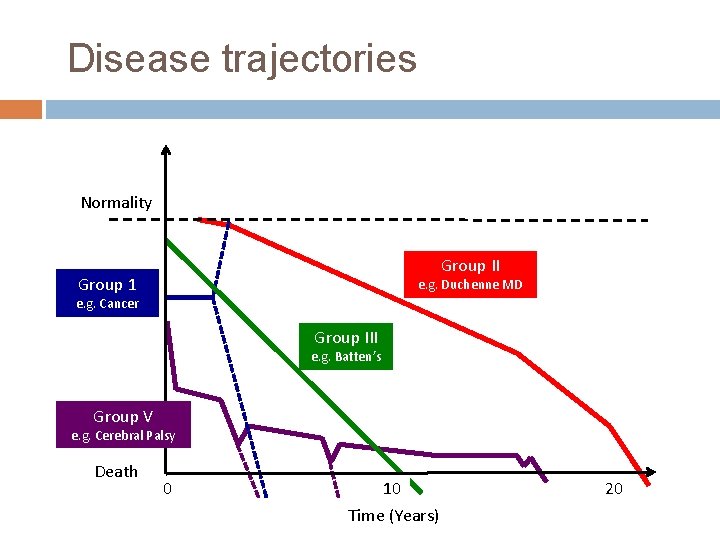
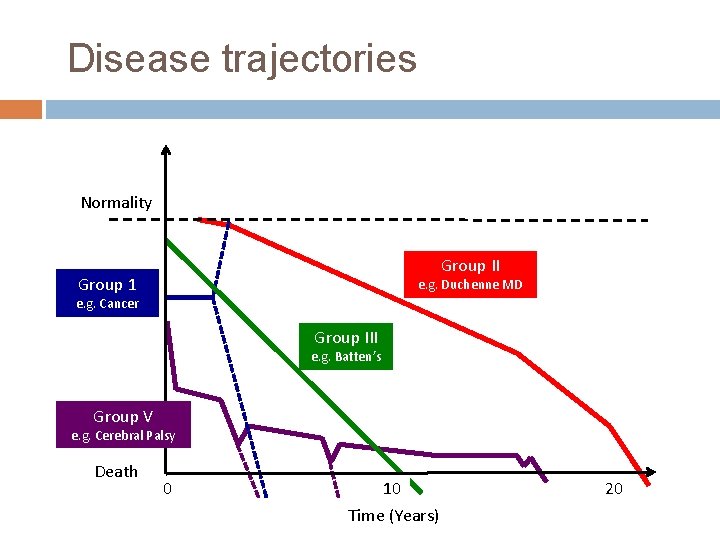
Disease trajectories Normality Group II Group 1 e. g. Duchenne MD e. g. Cancer Group III e. g. Batten’s Group V e. g. Cerebral Palsy Death 0 10 Time (Years) 20
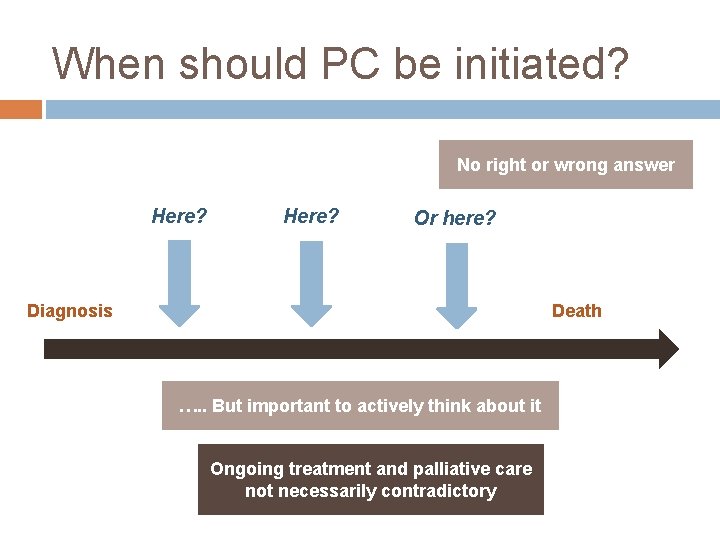
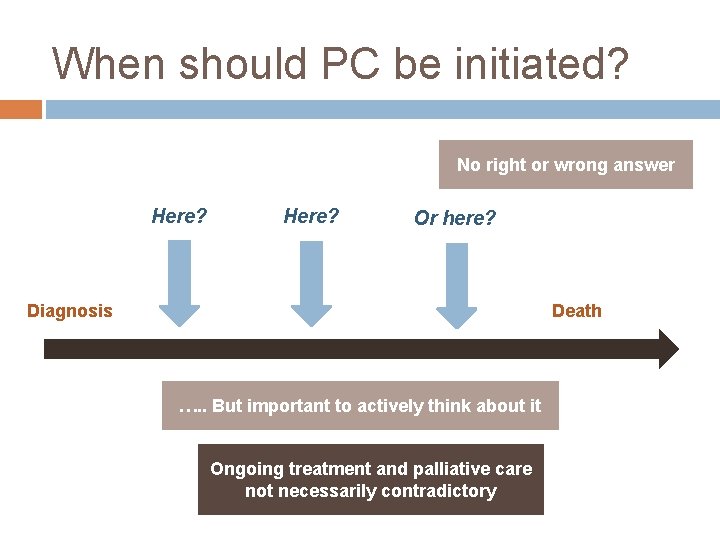
When should PC be initiated? No right or wrong answer Here? Or here? Diagnosis Death …. . But important to actively think about it Ongoing treatment and palliative care not necessarily contradictory
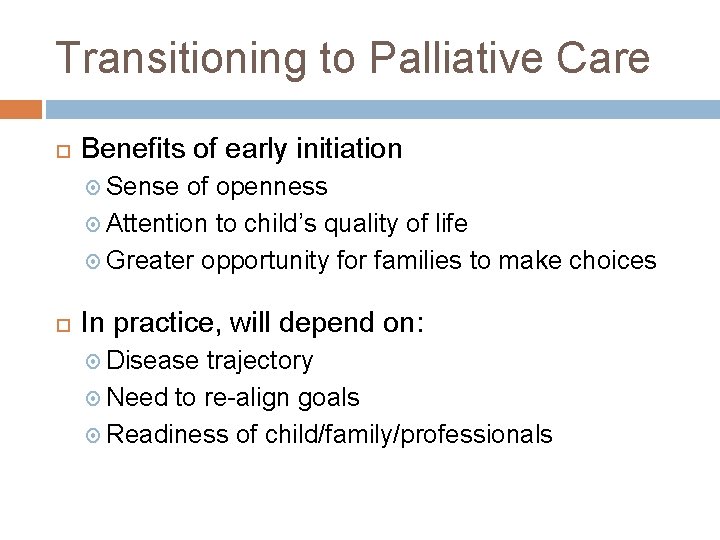
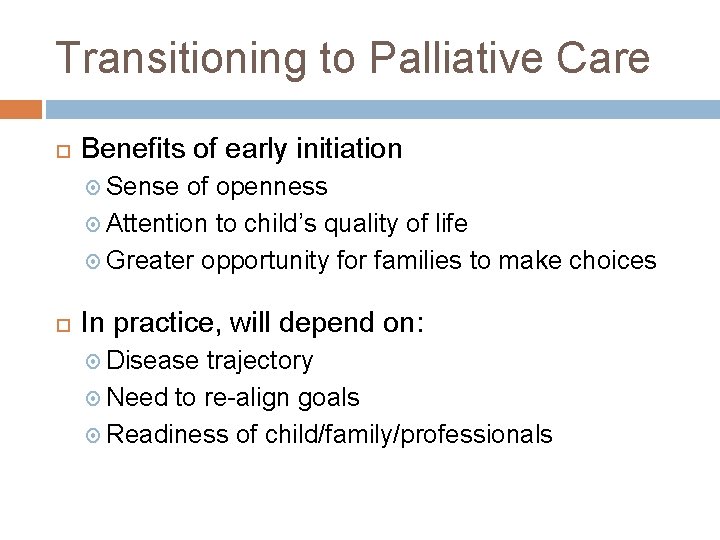
Transitioning to Palliative Care Benefits of early initiation Sense of openness Attention to child’s quality of life Greater opportunity for families to make choices In practice, will depend on: Disease trajectory Need to re-align goals Readiness of child/family/professionals
Which symptoms? Few studies Symptoms and their management poorly documented especially non-pain symptoms and especially if non-oncology diagnoses
Which symptoms? Probably pain, dyspnoea, fatigue, nausea/vomiting the most prevalent Also fatigue, agitation, seizures, spasms, secretions, constipation, sleep disturbance, anxiety……
Balance of burden and benefit A key principle Includes balancing of physical and emotional/spiritual aspects Needs careful thought – e. g. ‘prolonging life’ No such thing as interventions that are always appropriate or inappropriate Evidence-based (as far as possible)
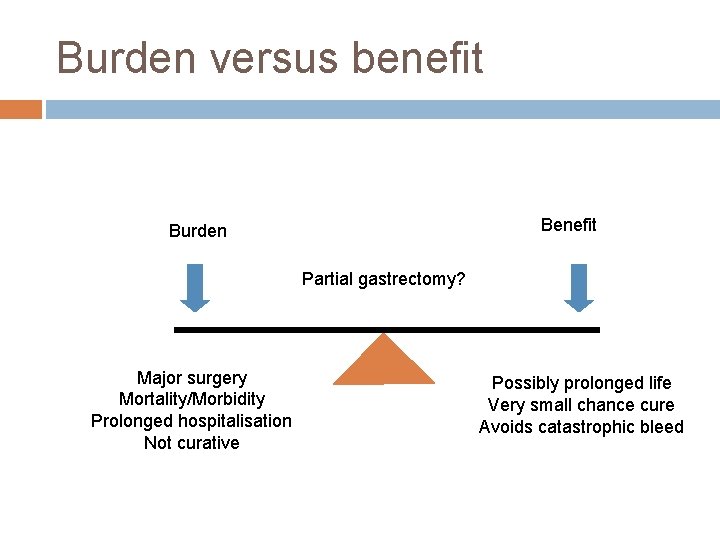
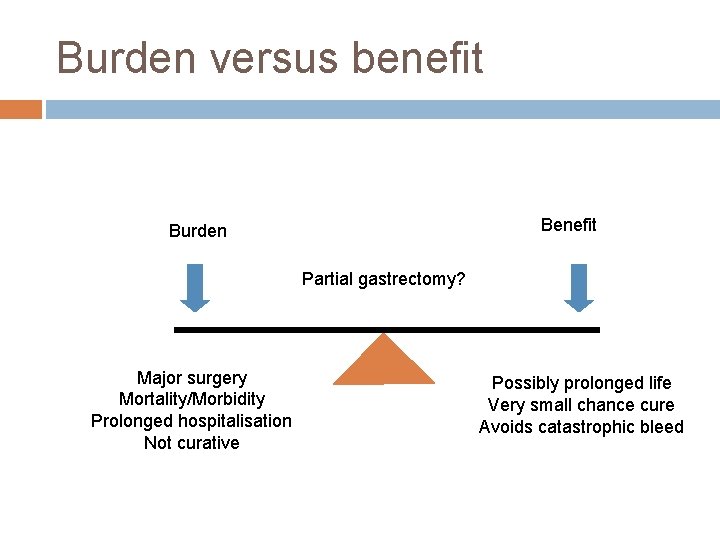
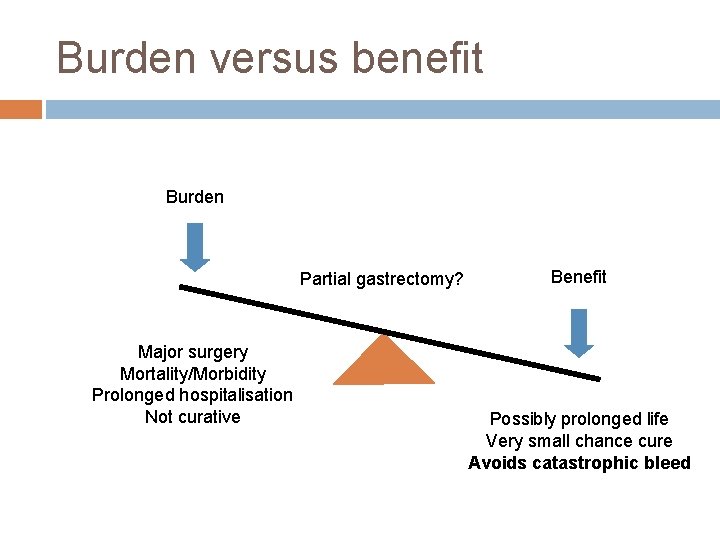
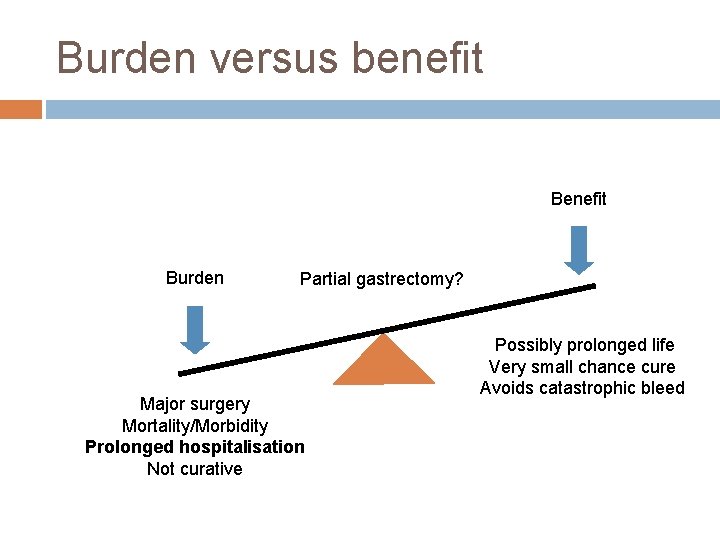
Burden versus benefit Burden Partial gastrectomy? Major surgery Mortality/Morbidity Prolonged hospitalisation Not curative Possibly prolonged life Very small chance cure Avoids catastrophic bleed
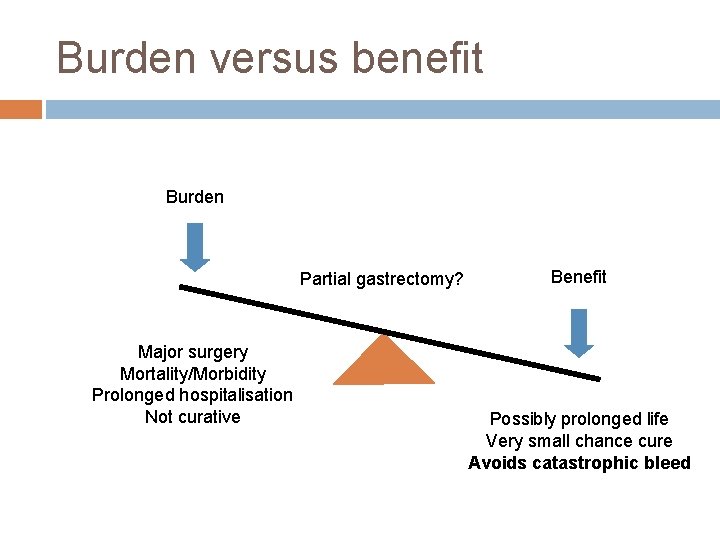
Burden versus benefit Burden Partial gastrectomy? Major surgery Mortality/Morbidity Prolonged hospitalisation Not curative Benefit Possibly prolonged life Very small chance cure Avoids catastrophic bleed
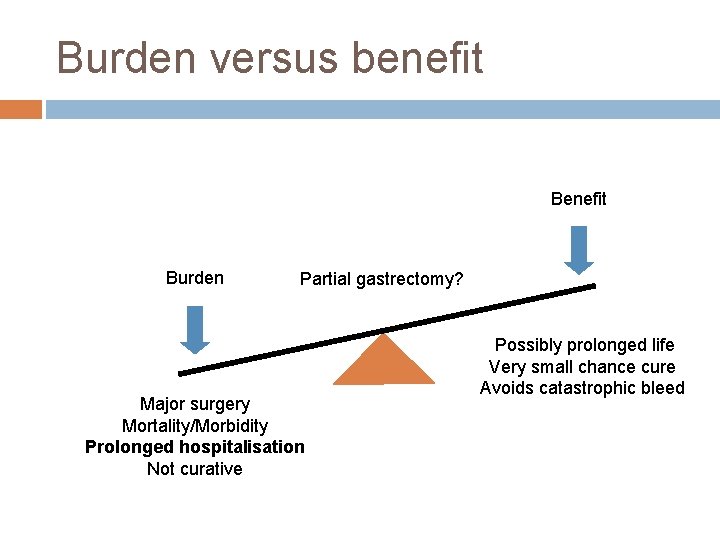
Burden versus benefit Burden Partial gastrectomy? Major surgery Mortality/Morbidity Prolonged hospitalisation Not curative Possibly prolonged life Very small chance cure Avoids catastrophic bleed
Pain in Paediatric Palliative Care
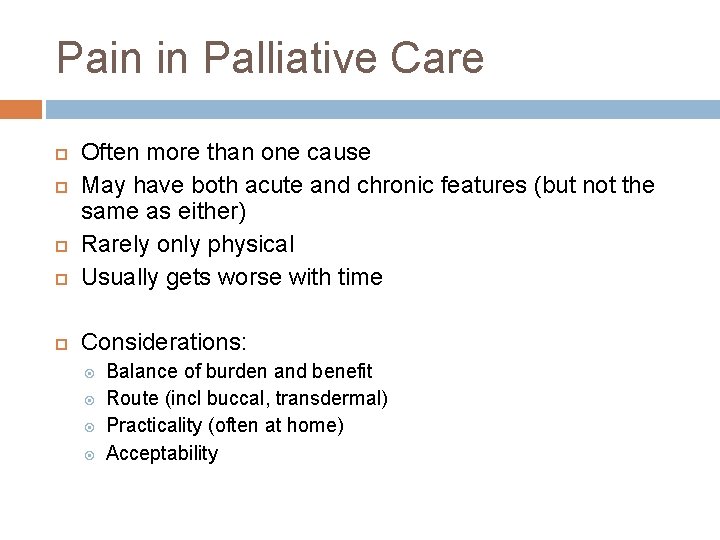
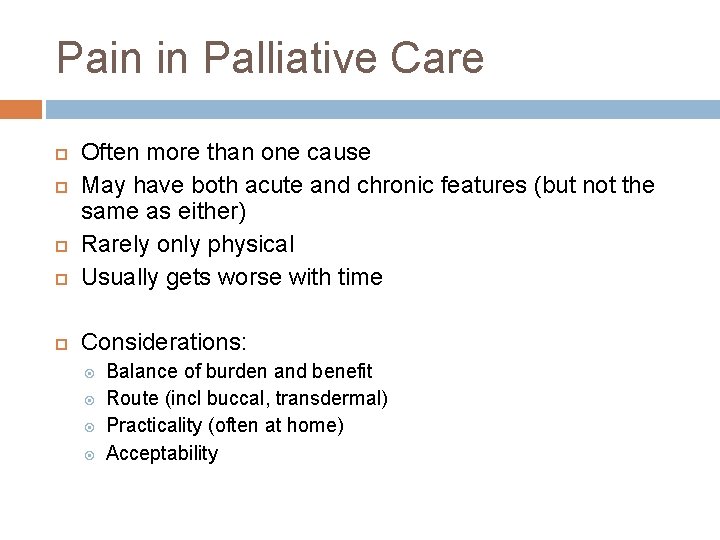
Pain in Palliative Care Often more than one cause May have both acute and chronic features (but not the same as either) Rarely only physical Usually gets worse with time Considerations: Balance of burden and benefit Route (incl buccal, transdermal) Practicality (often at home) Acceptability
Pain in Palliative Care Unpleasant sensory and emotional experience Entirely subjective – ‘what the patient says hurts’ Japanese study - 75% children with LLCs had pain in last weeks of life
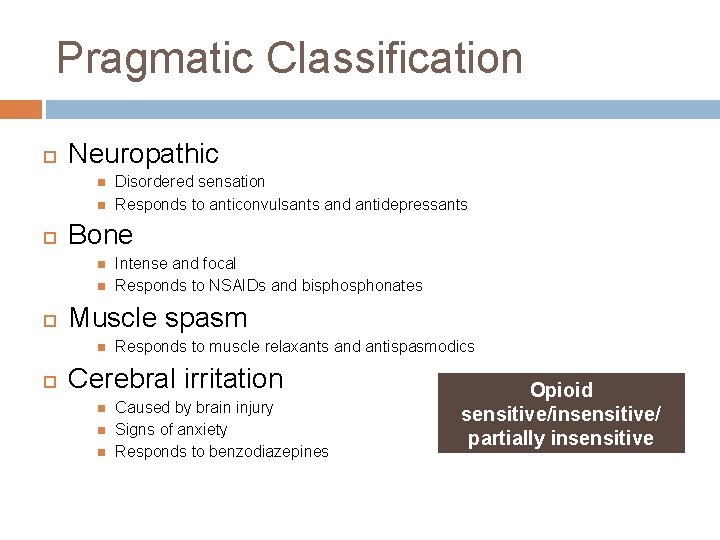
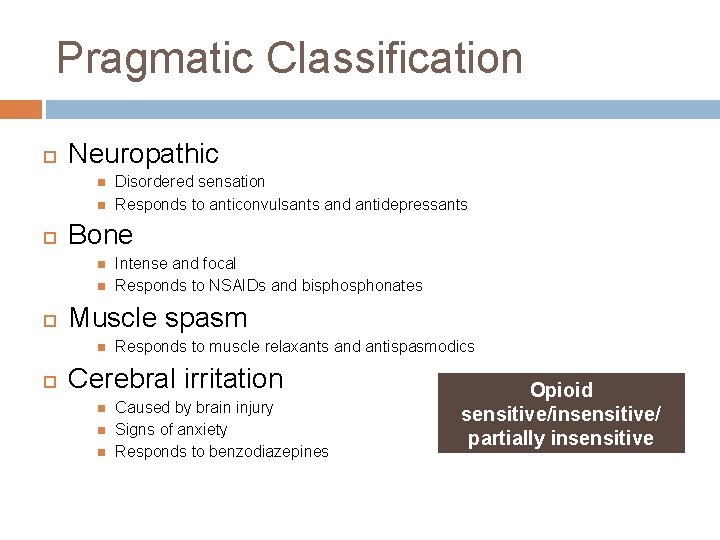
Pragmatic Classification Neuropathic Bone Intense and focal Responds to NSAIDs and bisphonates Muscle spasm Disordered sensation Responds to anticonvulsants and antidepressants Responds to muscle relaxants and antispasmodics Cerebral irritation Caused by brain injury Signs of anxiety Responds to benzodiazepines Opioid sensitive/insensitive/ partially insensitive
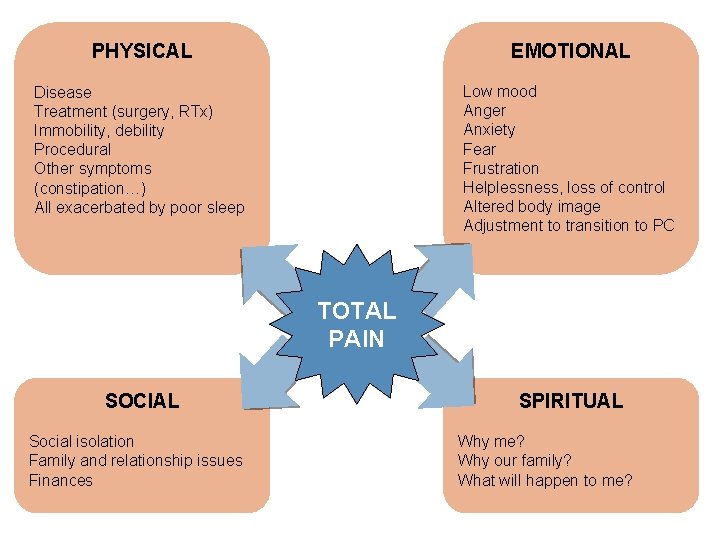
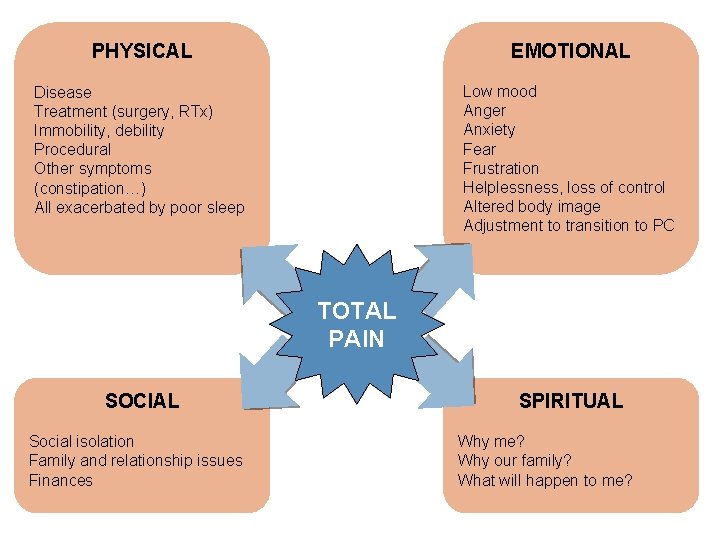
PHYSICAL EMOTIONAL Disease Treatment (surgery, RTx) Immobility, debility Procedural Other symptoms (constipation…) All exacerbated by poor sleep Low mood Anger Anxiety Fear Frustration Helplessness, loss of control Altered body image Adjustment to transition to PC TOTAL PAIN SOCIAL Social isolation Family and relationship issues Finances SPIRITUAL Why me? Why our family? What will happen to me?
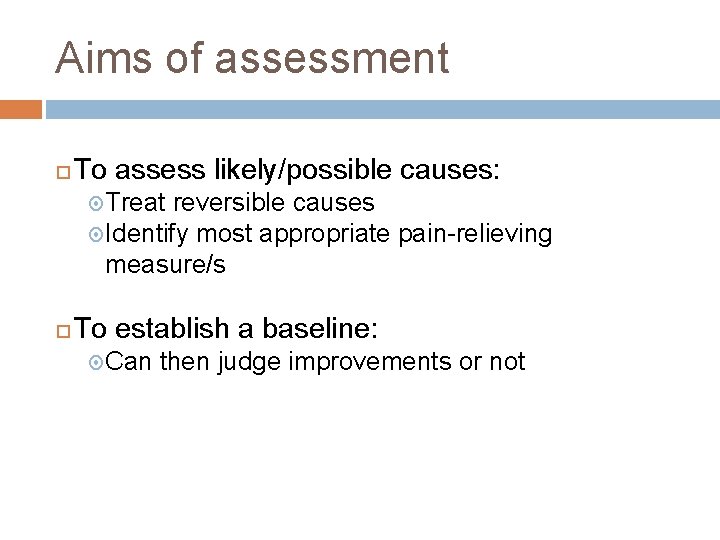
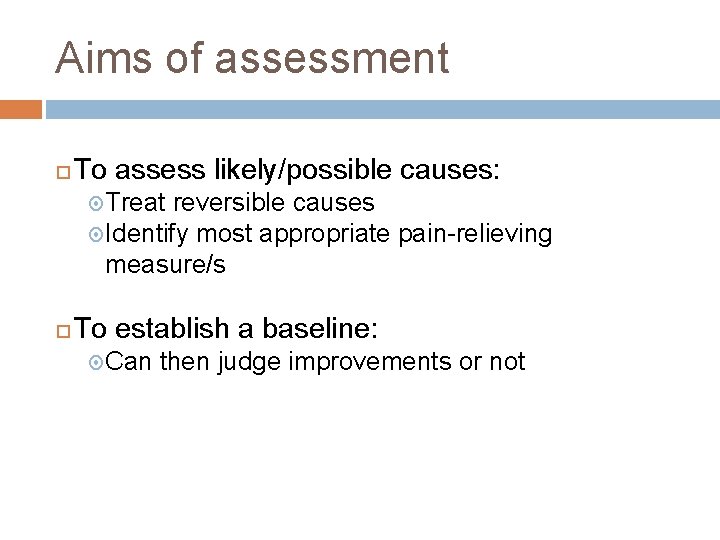
Aims of assessment To assess likely/possible causes: Treat reversible causes Identify most appropriate pain-relieving measure/s To establish a baseline: Can then judge improvements or not
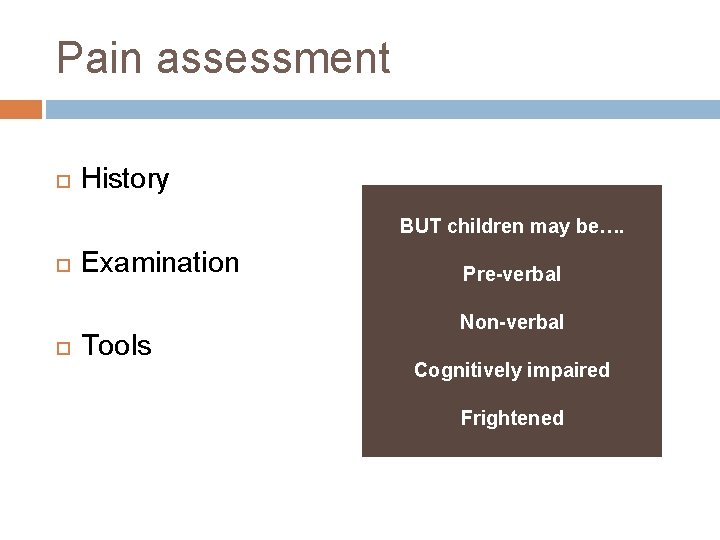
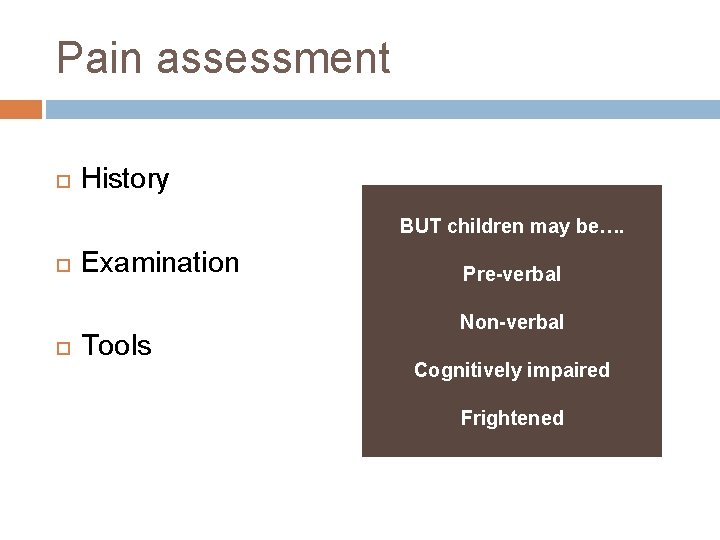
Pain assessment History BUT children may be…. Examination Tools Pre-verbal Non-verbal Cognitively impaired Frightened
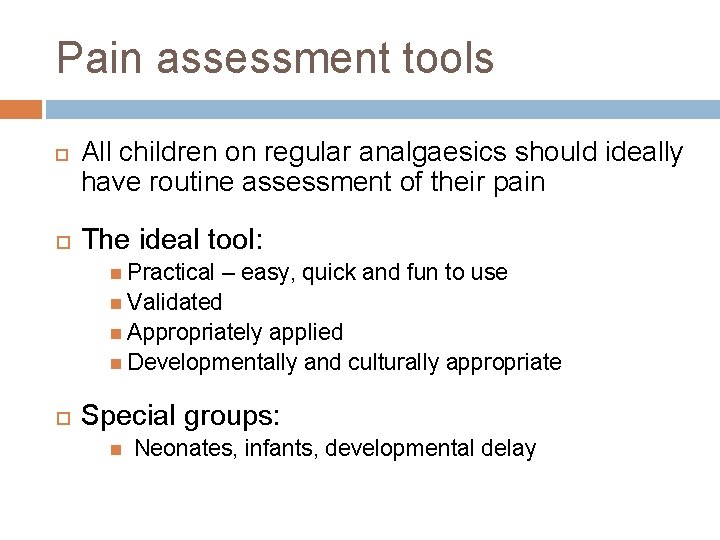
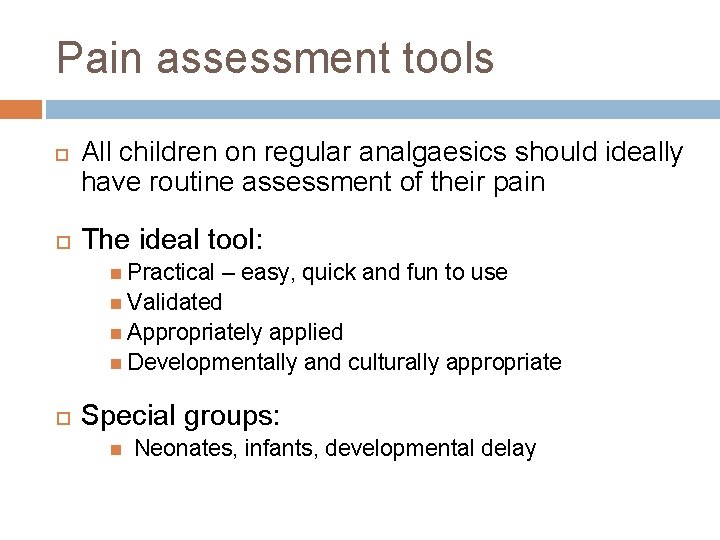
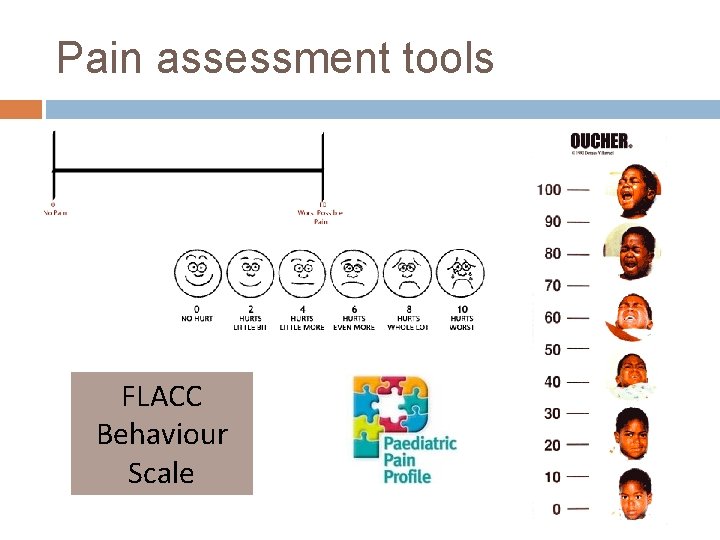
Pain assessment tools All children on regular analgaesics should ideally have routine assessment of their pain The ideal tool: Practical – easy, quick and fun to use Validated Appropriately applied Developmentally and culturally appropriate Special groups: Neonates, infants, developmental delay
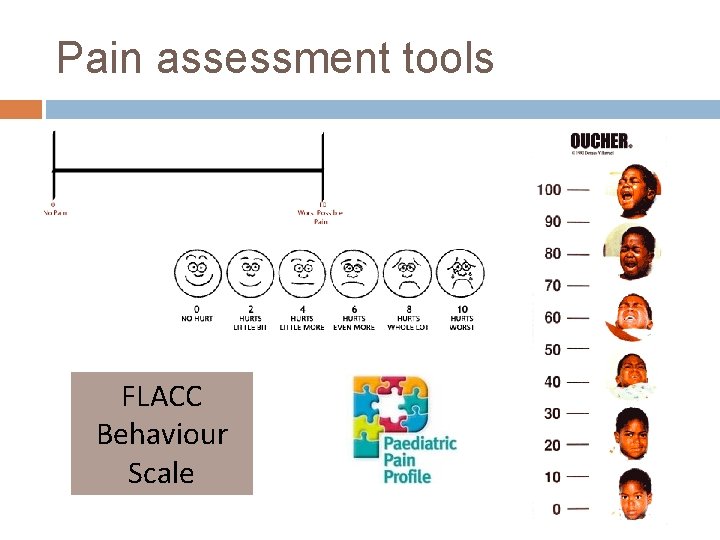
Pain assessment tools FLACC Behaviour Scale
Pain management WHO approach Current gold standard in PPM 3 tiers plus adjuvants at each stage
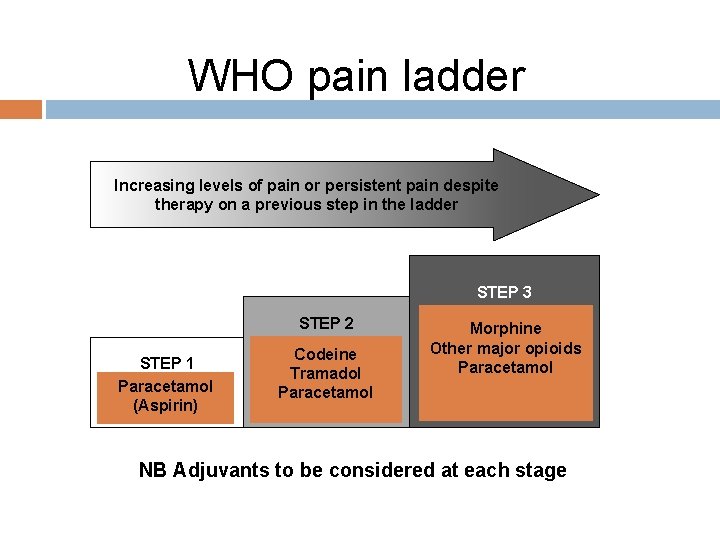
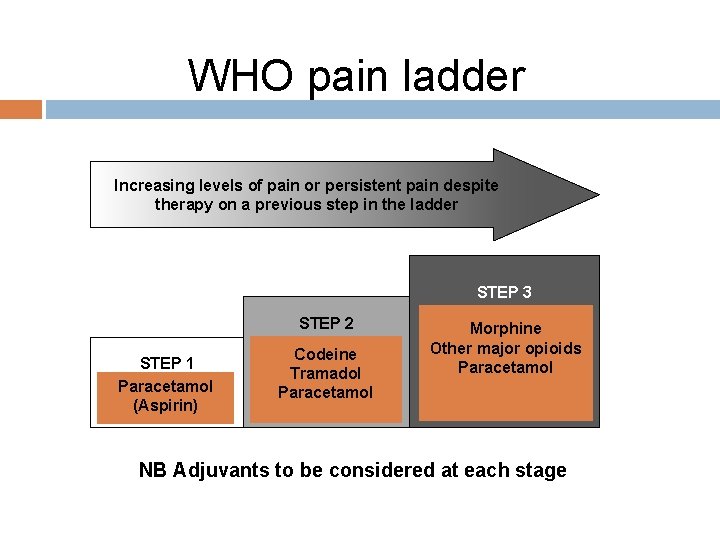
WHO pain ladder Increasing levels of pain or persistent pain despite therapy on a previous step in the ladder STEP 1 Nonopioid Paracetamol +/adjuvant (Aspirin) STEP 2 Mild opioid for Codeine moderate pain Tramadol +/- nonopioid Paracetamol +/- adjuvant STEP 3 Strong opioid for Morphine severe pain Other opioids +/-major nonopioid Paracetamol +/- adjuvant NB Adjuvants to be considered at each stage
Golden Rules By the ladder – do not rotate, move up By the clock – major opioids regular with breakthrough By the route - avoid needles if possible By the child
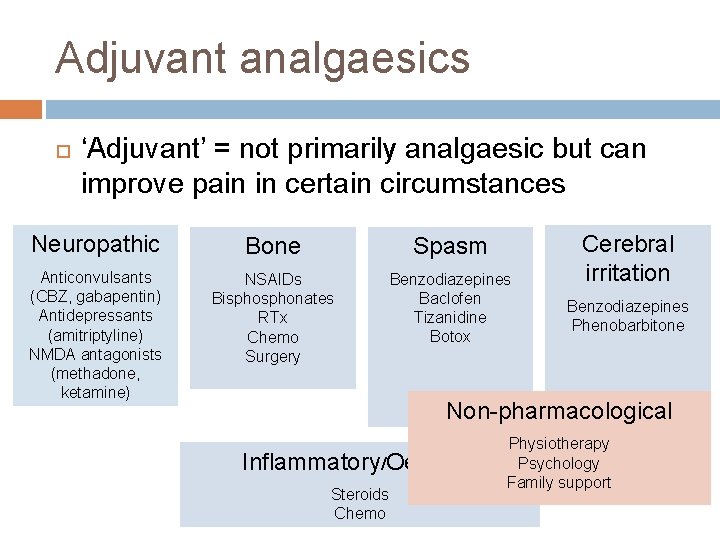
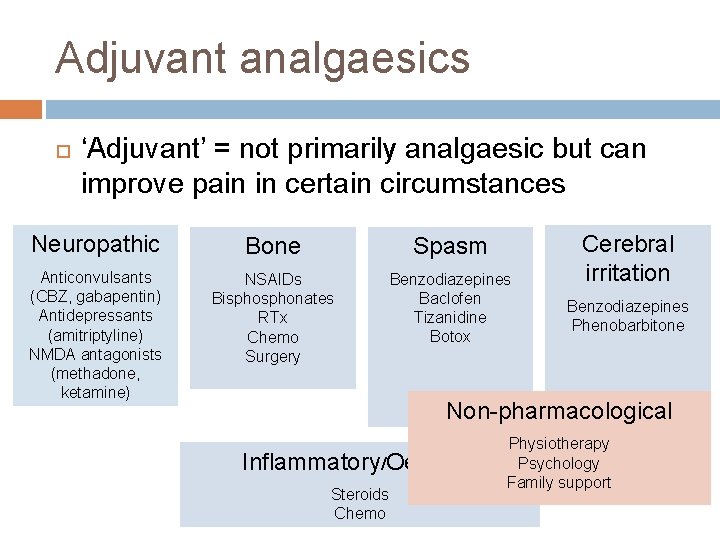
Adjuvant analgaesics ‘Adjuvant’ = not primarily analgaesic but can improve pain in certain circumstances Neuropathic Bone Spasm Anticonvulsants (CBZ, gabapentin) Antidepressants (amitriptyline) NMDA antagonists (methadone, ketamine) NSAIDs Bisphonates RTx Chemo Surgery Benzodiazepines Baclofen Tizanidine Botox Cerebral irritation Benzodiazepines Phenobarbitone Non-pharmacological Inflammatory/Oedema Steroids Chemo Physiotherapy Psychology Family support
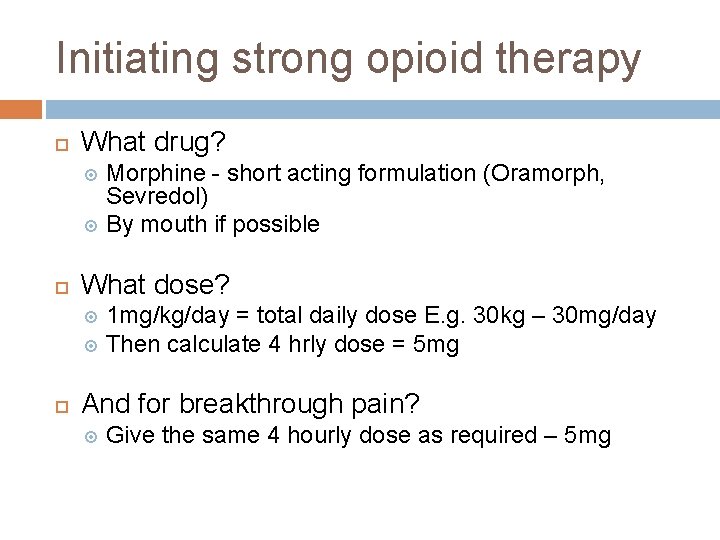
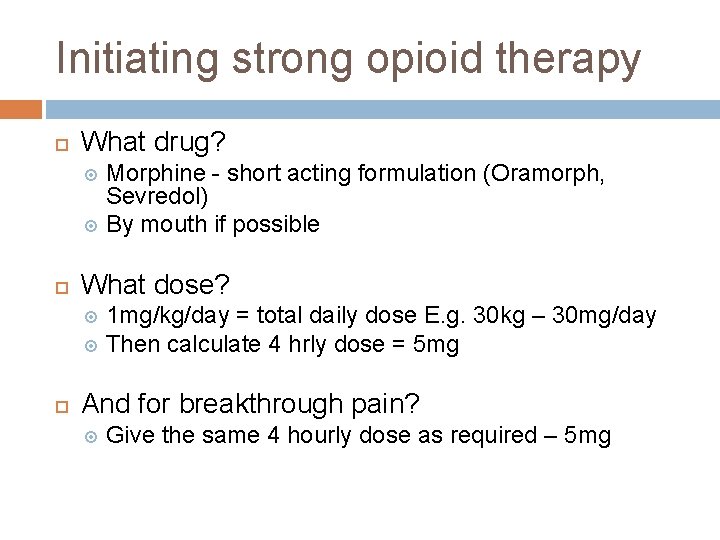
Initiating strong opioid therapy What drug? Morphine - short acting formulation (Oramorph, Sevredol) By mouth if possible What dose? 1 mg/kg/day = total daily dose E. g. 30 kg – 30 mg/day Then calculate 4 hrly dose = 5 mg And for breakthrough pain? Give the same 4 hourly dose as required – 5 mg
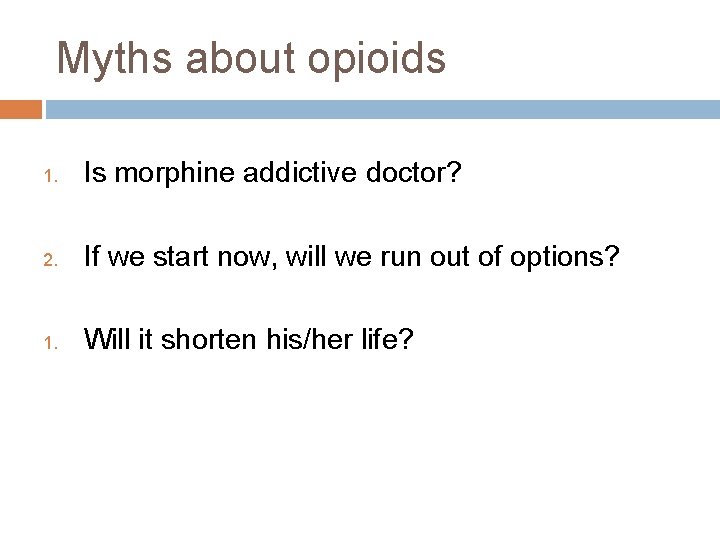
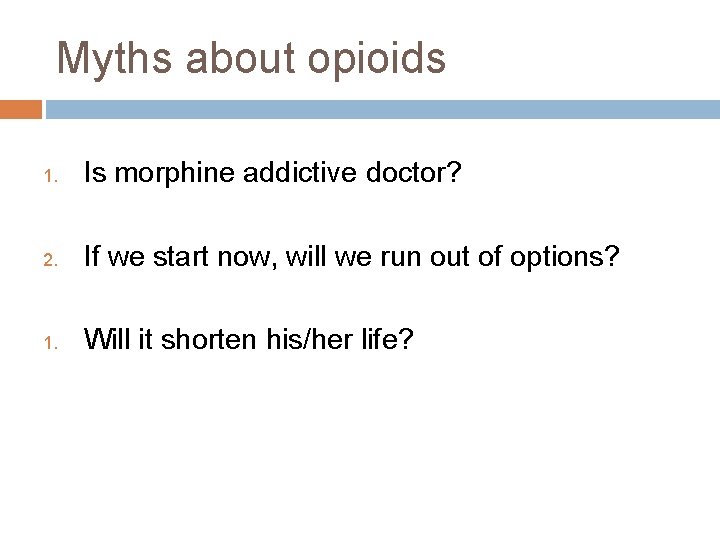
Myths about opioids 1. Is morphine addictive doctor? 2. If we start now, will we run out of options? 1. Will it shorten his/her life?
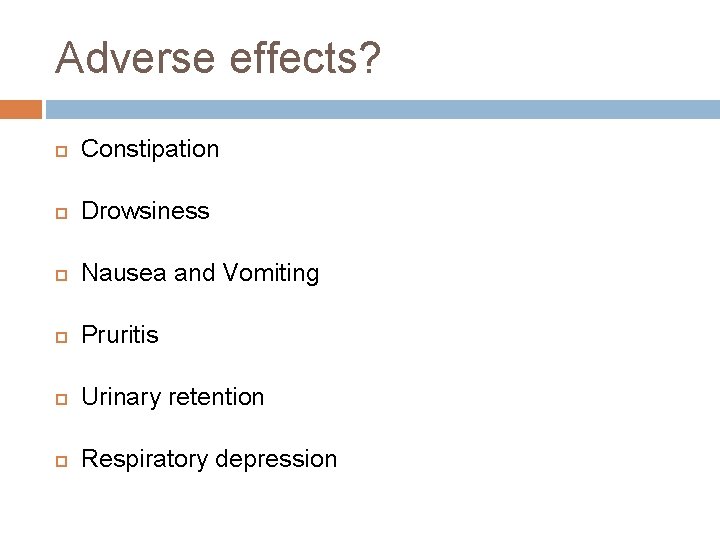
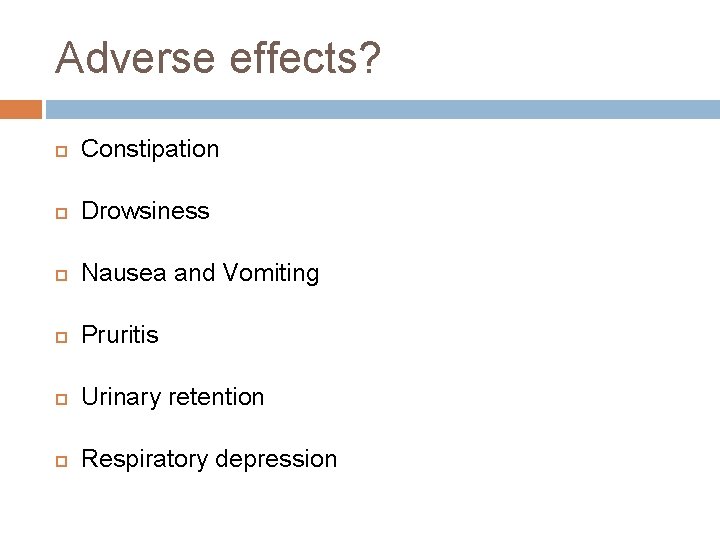
Adverse effects? Constipation Drowsiness Nausea and Vomiting Pruritis Urinary retention Respiratory depression
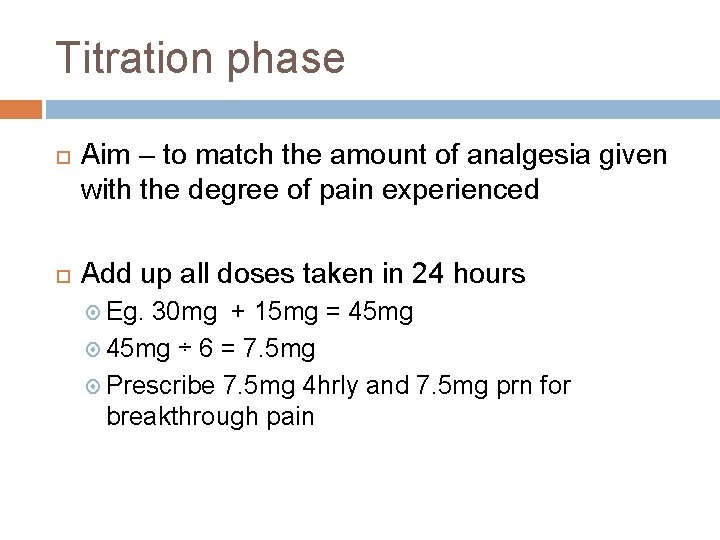
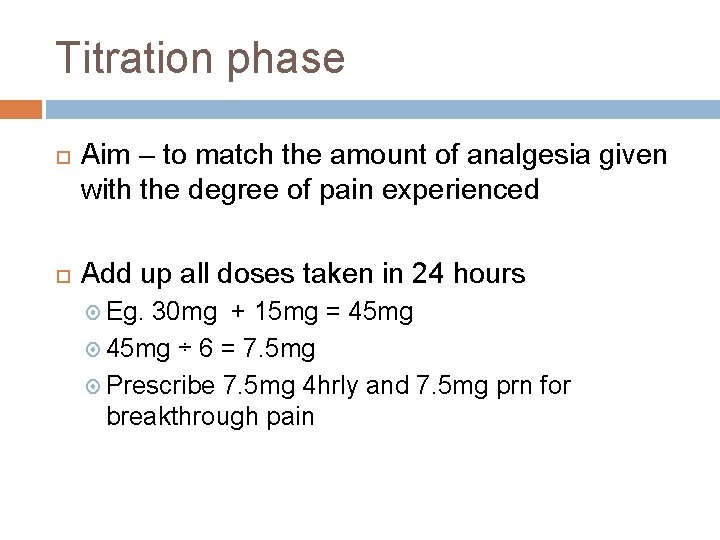
Titration phase Aim – to match the amount of analgesia given with the degree of pain experienced Add up all doses taken in 24 hours Eg. 30 mg + 15 mg = 45 mg ÷ 6 = 7. 5 mg Prescribe 7. 5 mg 4 hrly and 7. 5 mg prn for breakthrough pain

Maintenance phase More convenient opioid preparations MST E. g. If total daily Oramorph requirement: 45 mg Appropriate MST dose: 22. 5 mg bd Breakthrough still 7. 5 mg oramorph prn Other strong opioids Patches – fentanyl, buprenorphine S/C – diamorphine Also – methadone, oxycodone, hydromorphone Breakthrough usually still oramorph
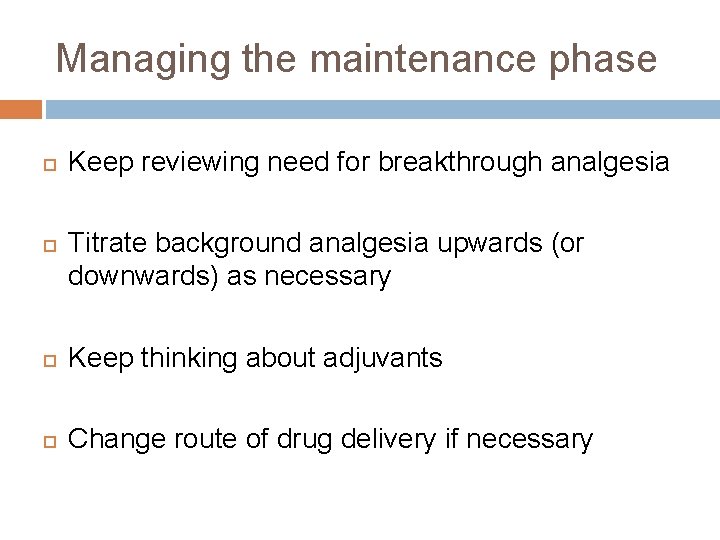
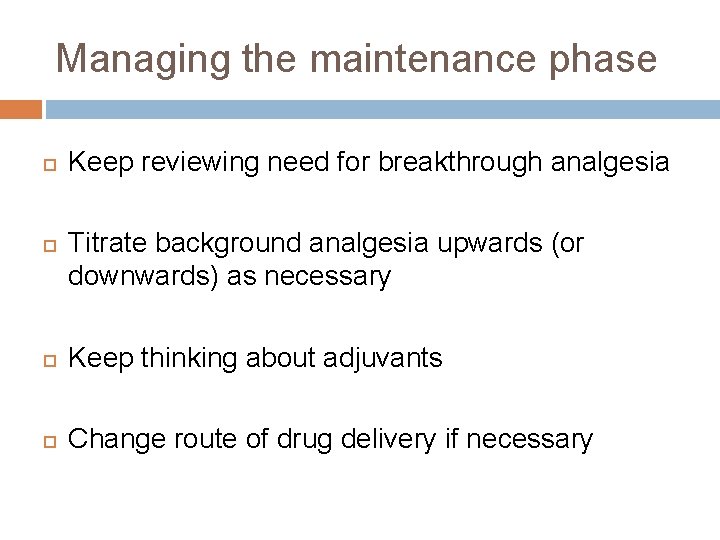
Managing the maintenance phase Keep reviewing need for breakthrough analgesia Titrate background analgesia upwards (or downwards) as necessary Keep thinking about adjuvants Change route of drug delivery if necessary
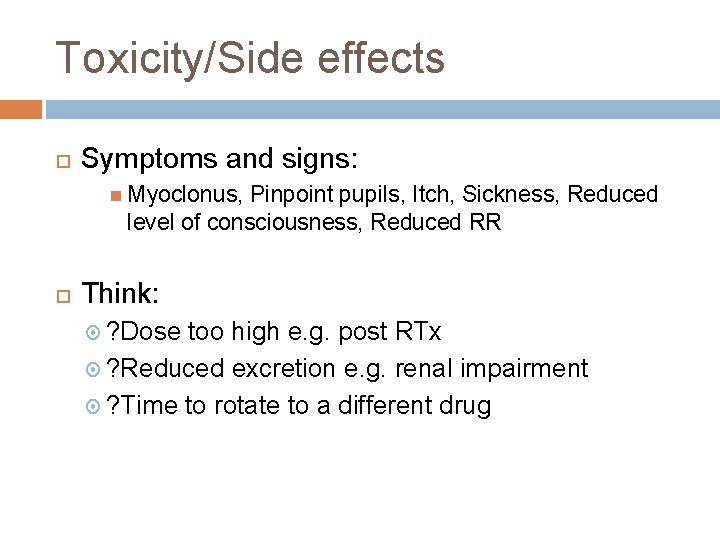
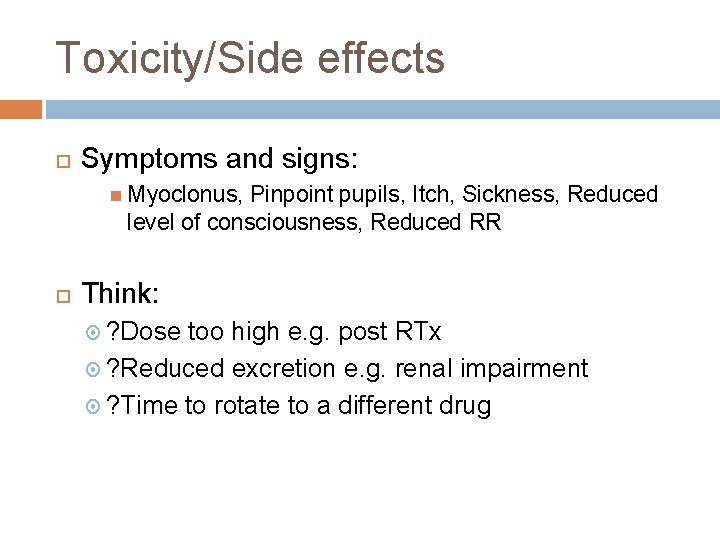
Toxicity/Side effects Symptoms and signs: Myoclonus, Pinpoint pupils, Itch, Sickness, Reduced level of consciousness, Reduced RR Think: ? Dose too high e. g. post RTx ? Reduced excretion e. g. renal impairment ? Time to rotate to a different drug
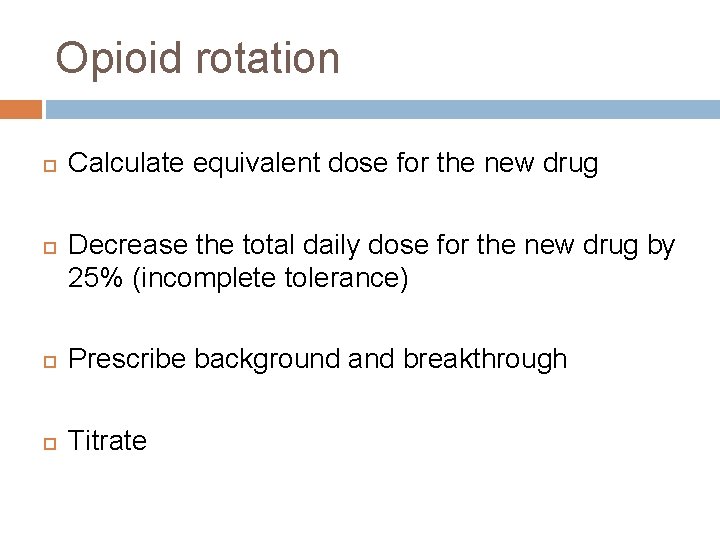
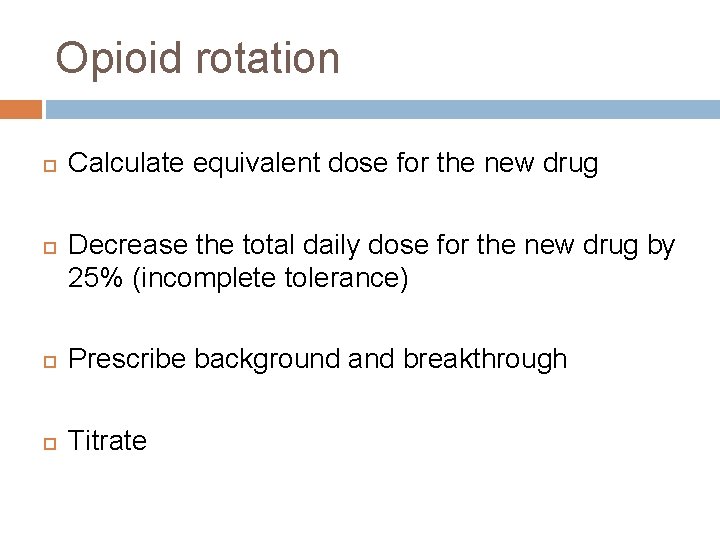
Opioid rotation Calculate equivalent dose for the new drug Decrease the total daily dose for the new drug by 25% (incomplete tolerance) Prescribe background and breakthrough Titrate
Don’t forget…. . Adjuvants Non-pharmacological interventions Managing other symptoms too Talking and listening Explanation and understanding can go a long way “the pain seemed to go by just talking”
Case Studies
Sophie Teenager with severe cerebral palsy Less well over last 6/12 – chest infections, spasms Fewer smiles, more agitated Scoliosis worse, history of hip dislocation Upset on moving and handling
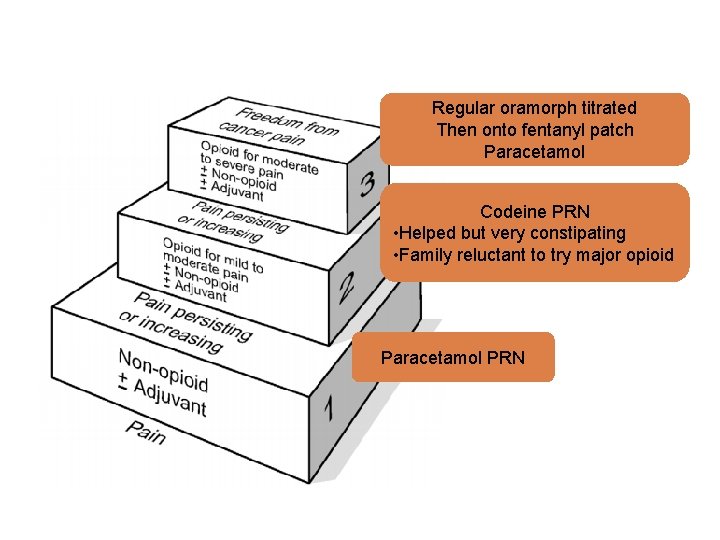
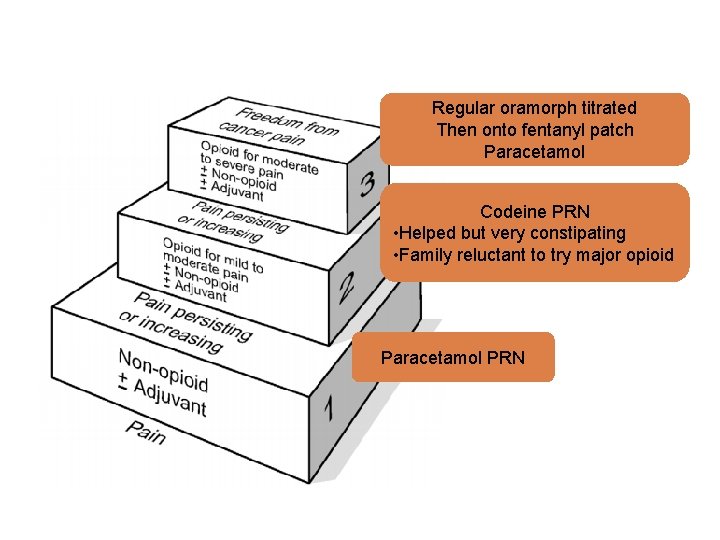
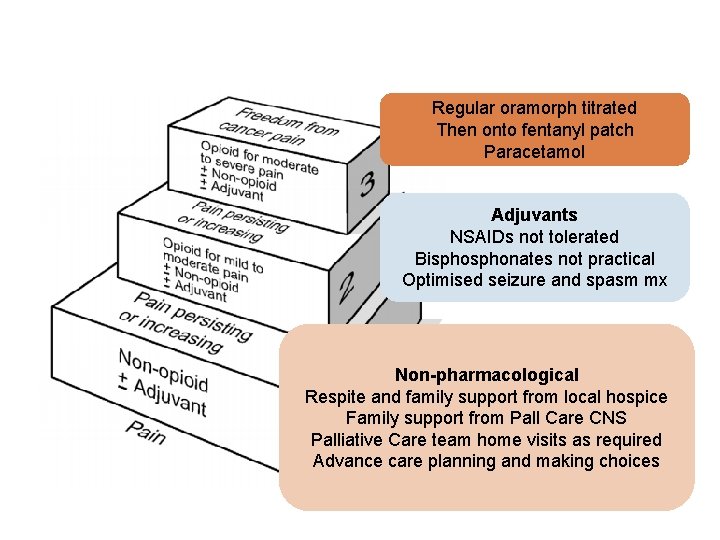
Regular oramorph titrated Then onto fentanyl patch Paracetamol Codeine PRN • Helped but very constipating • Family reluctant to try major opioid Paracetamol PRN
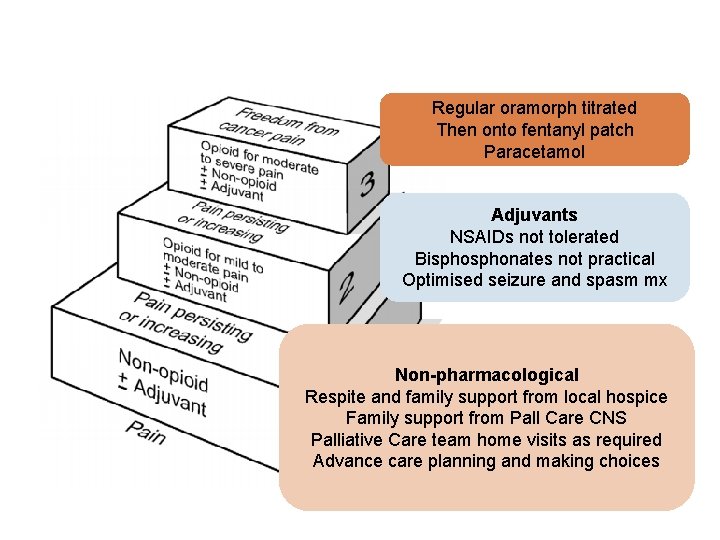
Regular oramorph titrated Then onto fentanyl patch Paracetamol Adjuvants NSAIDs not tolerated Bisphonates not practical Optimised seizure and spasm mx Non-pharmacological Respite and family support from local hospice Family support from Pall Care CNS Palliative Care team home visits as required Advance care planning and making choices
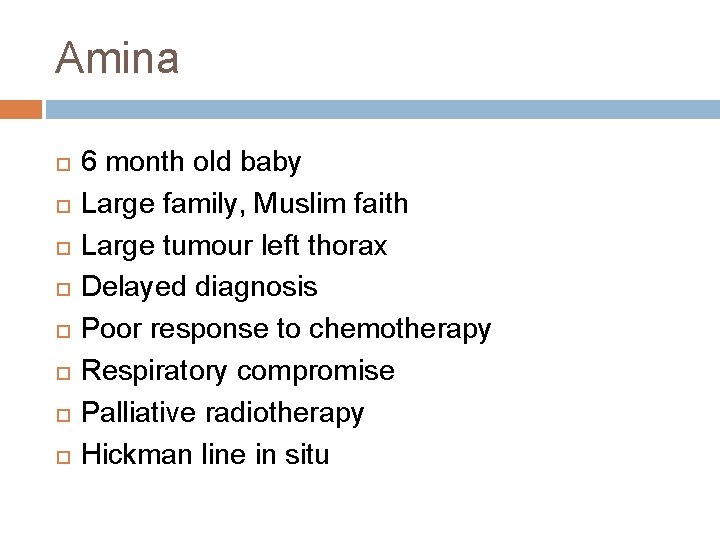
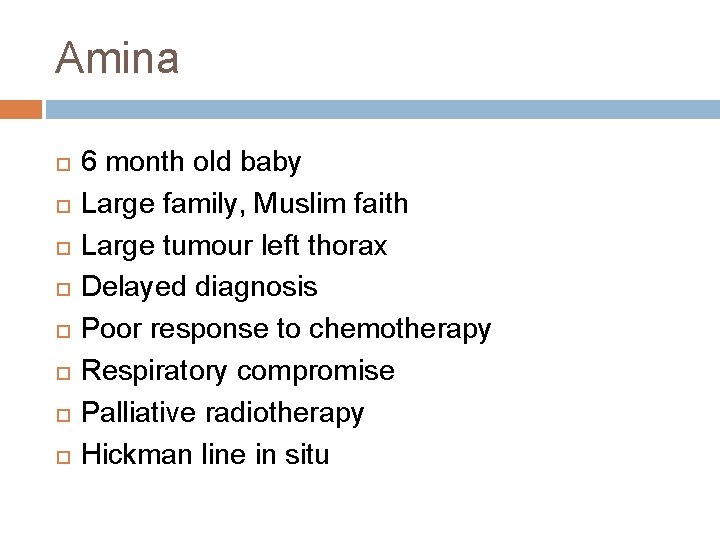
Amina 6 month old baby Large family, Muslim faith Large tumour left thorax Delayed diagnosis Poor response to chemotherapy Respiratory compromise Palliative radiotherapy Hickman line in situ
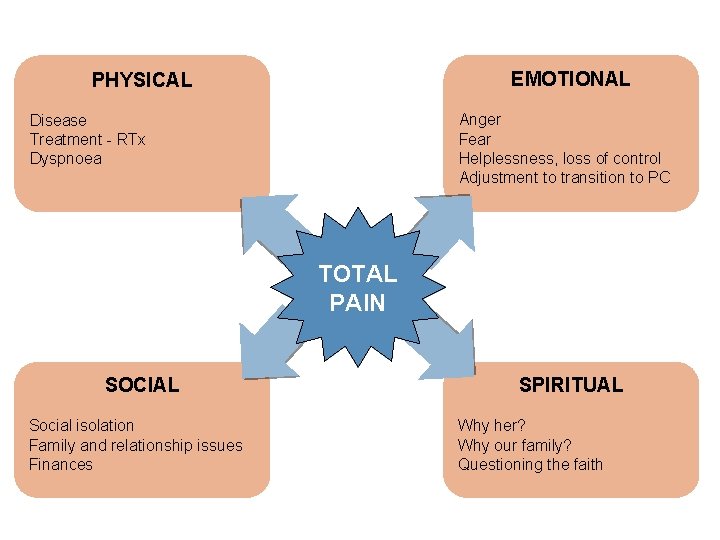
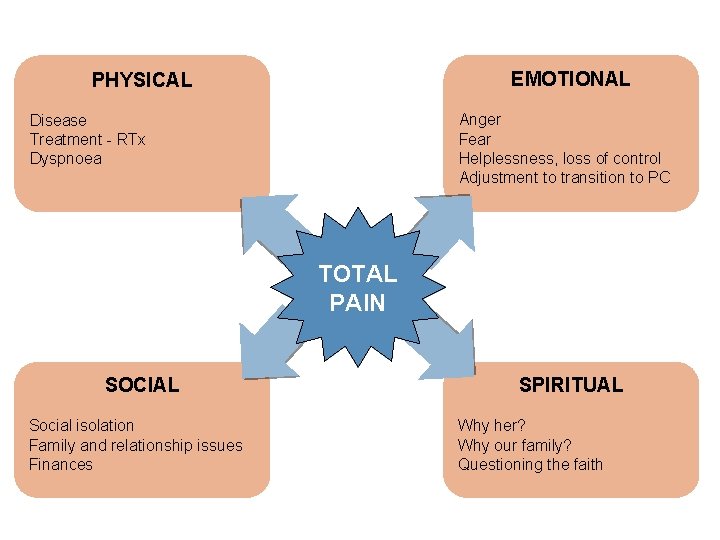
EMOTIONAL PHYSICAL Anger Fear Helplessness, loss of control Adjustment to transition to PC Disease Treatment - RTx Dyspnoea TOTAL PAIN SOCIAL Social isolation Family and relationship issues Finances SPIRITUAL Why her? Why our family? Questioning the faith
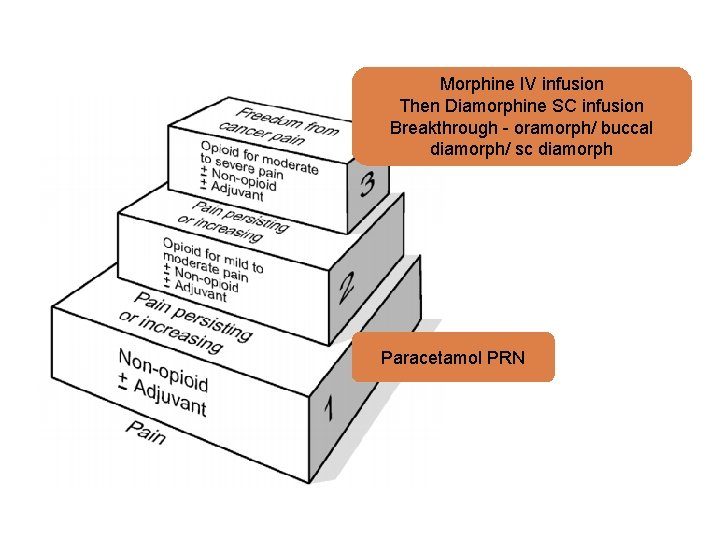
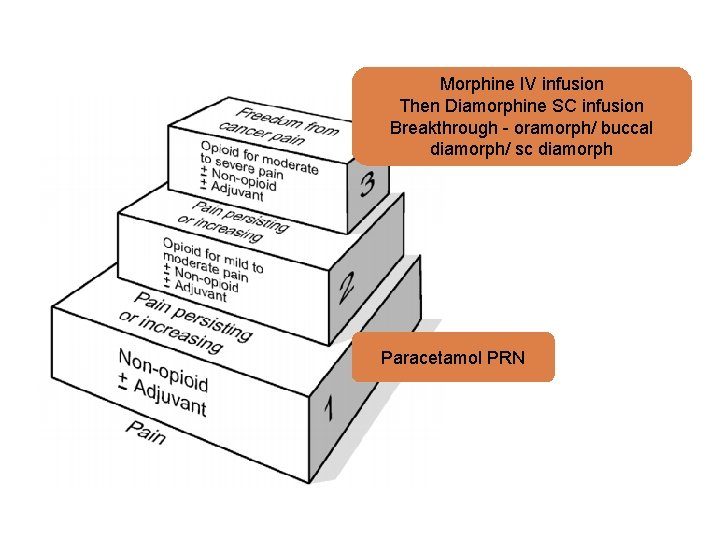
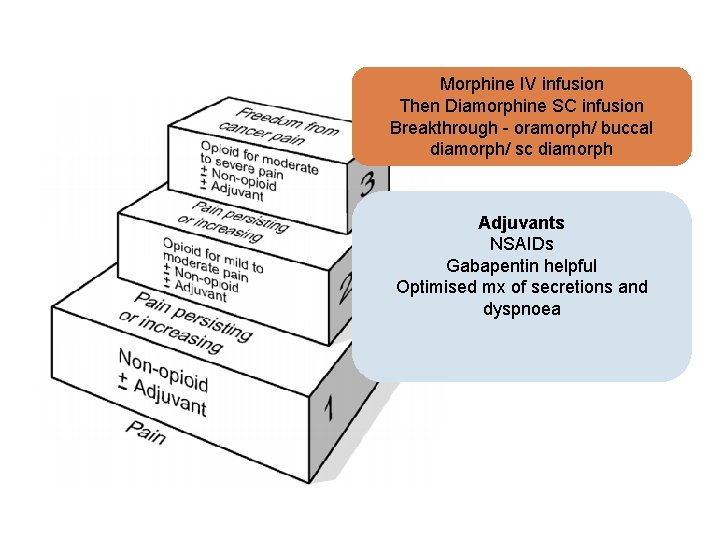
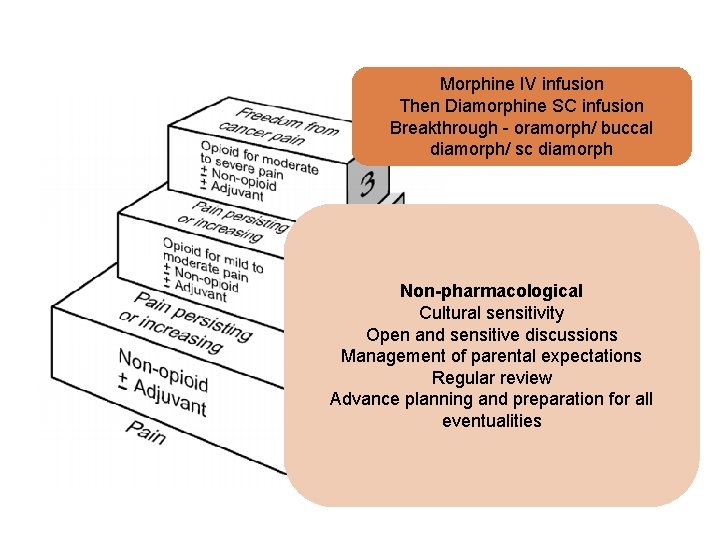
Morphine IV infusion Then Diamorphine SC infusion Breakthrough - oramorph/ buccal diamorph/ sc diamorph Paracetamol PRN
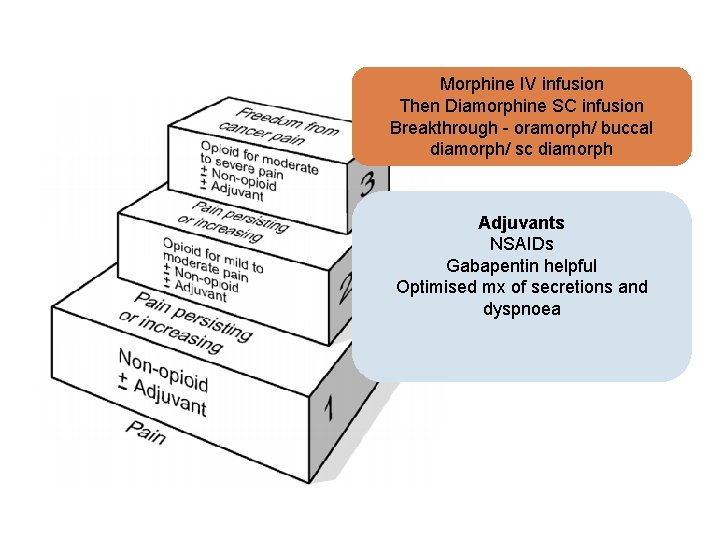
Morphine IV infusion Then Diamorphine SC infusion Breakthrough - oramorph/ buccal diamorph/ sc diamorph Adjuvants NSAIDs Gabapentin helpful Optimised mx of secretions and dyspnoea
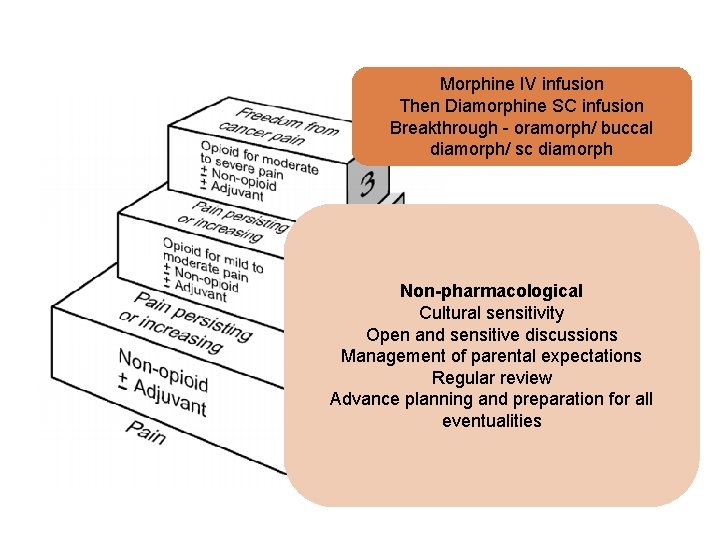
Morphine IV infusion Then Diamorphine SC infusion Breakthrough - oramorph/ buccal diamorph/ sc diamorph Non-pharmacological Cultural sensitivity Open and sensitive discussions Management of parental expectations Regular review Advance planning and preparation for all eventualities
Summary Introduction to Paediatric Palliative Care Pain in Paediatric Palliative Care Case Studies
Take home messages Burden versus benefit Total pain Holistic approach Challenging the myths and optimising care
Where to find out more (1) Textbooks:

Where to find out more (2) Together for short lives resources www. togetherforshortlives. org. uk

Where to find out more (3) Diploma in Palliative Care, Cardiff University
“How people die remains in the memory of those who live on” Dame Cicely Saunders
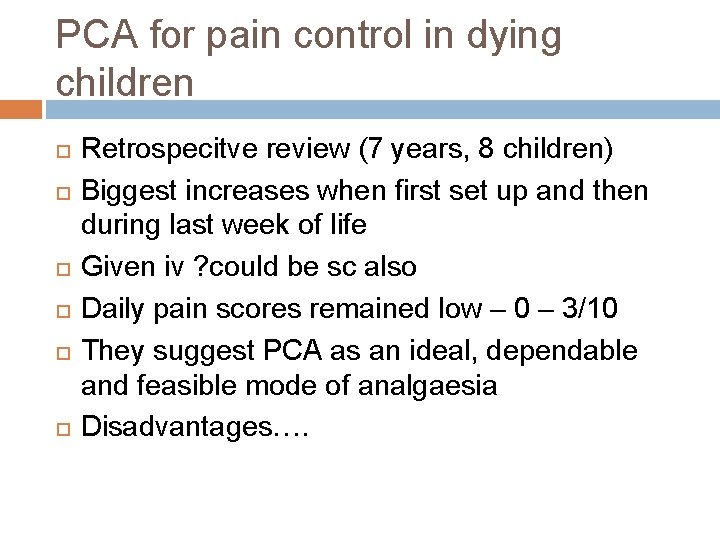
PCA for pain control in dying children Retrospecitve review (7 years, 8 children) Biggest increases when first set up and then during last week of life Given iv ? could be sc also Daily pain scores remained low – 0 – 3/10 They suggest PCA as an ideal, dependable and feasible mode of analgaesia Disadvantages….
Limitations of WHO approach High dose codeine vs low dose morphine Incident pain (as opposed to breakthrough pain)
Neonates Start at reduced dose (30 – 50%) because: Longer elimination (renal) Reduced hepatic enzyme activity (reduced clearance) ? BBB more permeable Opioid receptors not fully developed Safest to start low and titrate Ensuring free access to breakthrough
 Palliative care vs hospice care
Palliative care vs hospice care Breast tenderness before period vs early pregnancy sign
Breast tenderness before period vs early pregnancy sign Period cramps vs early pregnancy cramps
Period cramps vs early pregnancy cramps Mad pain
Mad pain Franciscan palliative care
Franciscan palliative care Akps score palliative care
Akps score palliative care Palliative care matters
Palliative care matters Just in case bag palliative care
Just in case bag palliative care European delirium association
European delirium association Palliative care assistant
Palliative care assistant Oacc palliative care
Oacc palliative care Hospice of the bluegrass frankfort ky
Hospice of the bluegrass frankfort ky Traduttore italiano inglese
Traduttore italiano inglese Dr hong-phuc tran
Dr hong-phuc tran Hospice satisfaction survey
Hospice satisfaction survey What is amber care
What is amber care Ethical issues in palliative care
Ethical issues in palliative care Anergia definition
Anergia definition European certificate in essential palliative care
European certificate in essential palliative care Calvary palliative care kogarah
Calvary palliative care kogarah Palliative care quality collaborative
Palliative care quality collaborative Sas assessment tool
Sas assessment tool Goc palliative care
Goc palliative care Principles of palliative care
Principles of palliative care Goscote palliative care centre
Goscote palliative care centre Parallel planning palliative care
Parallel planning palliative care Palliative care programme
Palliative care programme Anorexia, nausea and vomiting
Anorexia, nausea and vomiting Seamus hesney
Seamus hesney Npcrc
Npcrc Palliative care in nepal
Palliative care in nepal Textbook of palliative care communication
Textbook of palliative care communication Palliative care at home barry
Palliative care at home barry Tertiary level of care
Tertiary level of care Nursing diagnosis for angina
Nursing diagnosis for angina How to calculate drip rate
How to calculate drip rate Paediatric et tube size formula
Paediatric et tube size formula Paediatric nursing meaning
Paediatric nursing meaning Introduction modern concept of child care
Introduction modern concept of child care Paediatric respiratory history
Paediatric respiratory history Supracondylar fracture rch
Supracondylar fracture rch Head tilt chin lift
Head tilt chin lift Paediatric bls
Paediatric bls North thames paediatric network
North thames paediatric network Infant epiglottis anatomy
Infant epiglottis anatomy South thames paediatric network
South thames paediatric network Mallampati grad
Mallampati grad Kenya paediatric research consortium
Kenya paediatric research consortium Pc hpc pmh dh
Pc hpc pmh dh Modern concept of child care wikipedia
Modern concept of child care wikipedia List of suspending agents
List of suspending agents Pediatric assessment triangle
Pediatric assessment triangle Paediatric et tube size formula
Paediatric et tube size formula Physical environment for a sick child
Physical environment for a sick child Paediatric vital signs
Paediatric vital signs Paediatric fluid chart
Paediatric fluid chart Suspension definition pharmacy
Suspension definition pharmacy Provocative/palliative
Provocative/palliative Adjuvant neoadjuvant palliative
Adjuvant neoadjuvant palliative Palliative fase
Palliative fase Pps scale
Pps scale Log80 ausl romagna
Log80 ausl romagna Fiberpharm
Fiberpharm Palliative prognostic index
Palliative prognostic index