Airway Management in Pediatric Patients PAT THORPE MSN

- Slides: 30
Airway Management in Pediatric Patients PAT THORPE, MSN, CPN CLINICAL CO COORDINATOR GARFIELD WATSON RT PEDIATRIC INTENSIVE CARE UNIT NICKLAUS CHILDREN HOSPITAL SEPTEMBER 26, 2017
Facts �Appropriate airway management is the key to success in pediatric patients. �Most pediatric cardiac arrests begin with respiratory arrest. �Anatomy and physiology of pediatric airway varies from those of adults. �Effective airway management includes anticipating and planning for problems. �Impaired breathing affects the gas exchange in the lungs, thereby causing low oxygen level and high carbon dioxide level un the blood.
Overview �Discuss the differences between pediatric and adult airways �Discuss the various oxygen delivery system �Discuss various airway modes �Identify conditions of respiratory comprise in children �Management of Respiratory failure �Bag –Mask Ventilation
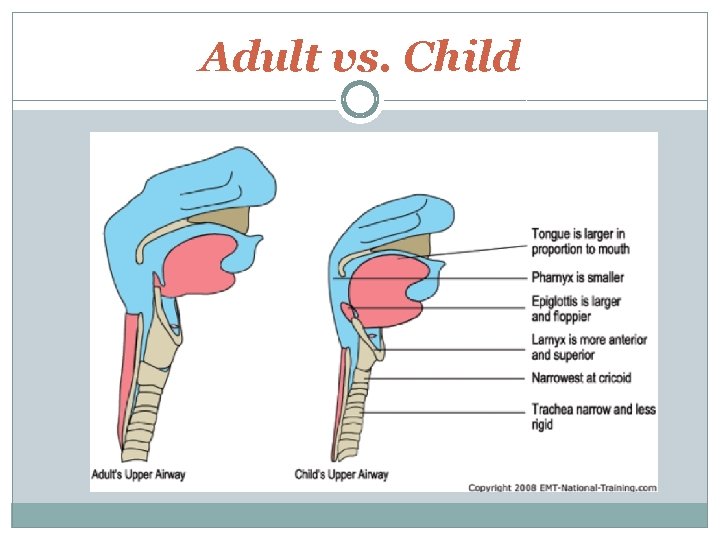
Features of Pediatric Airway � Narrower airway hence easily obstructed �Foreign body, edema, secretions blood � Larger tongue which is posteriorly displaced � Longer and floppy epiglottis � Higher anterior larynx � Narrower vocal cord, making intubation more difficult � Shorter trachea � Larger head.
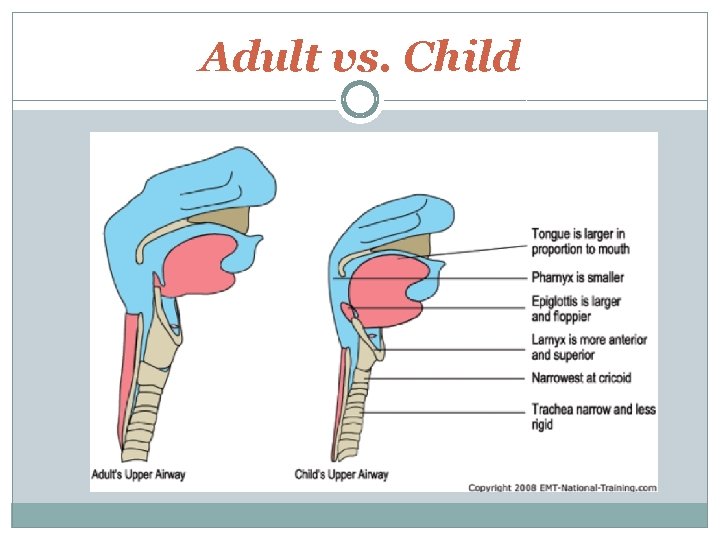
Adult vs. Child
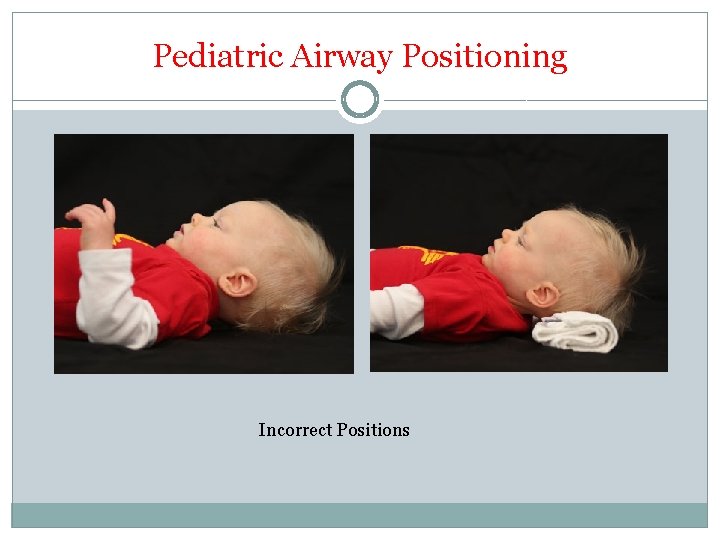
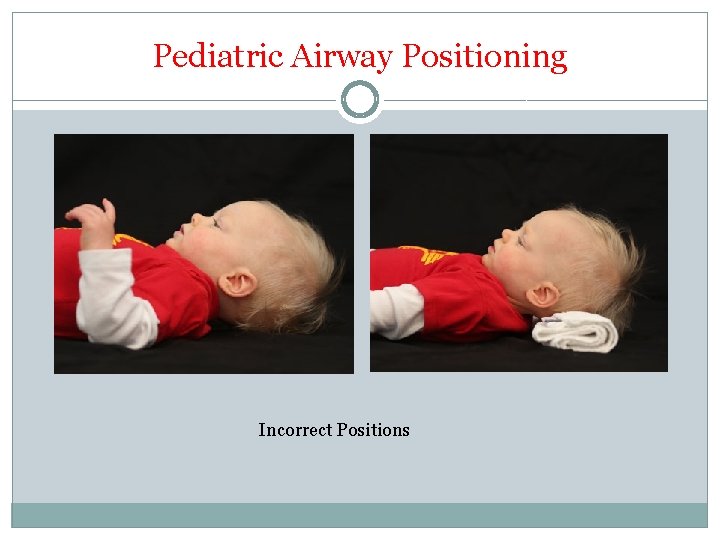
Pediatric Airway Positioning Incorrect Positions
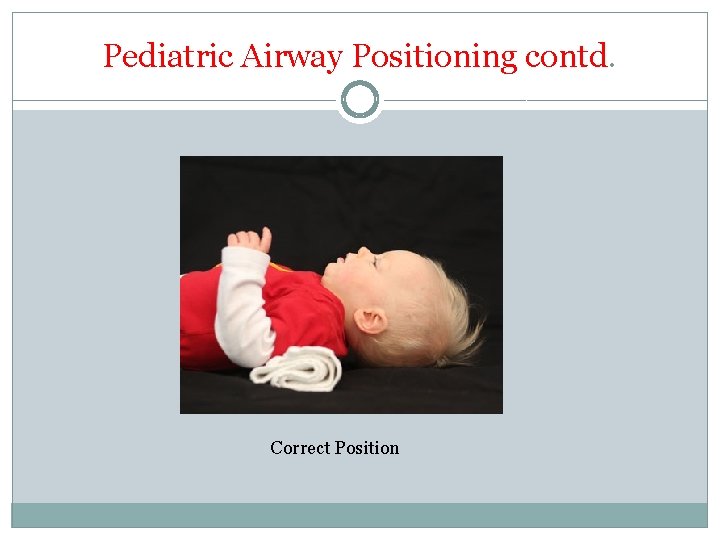
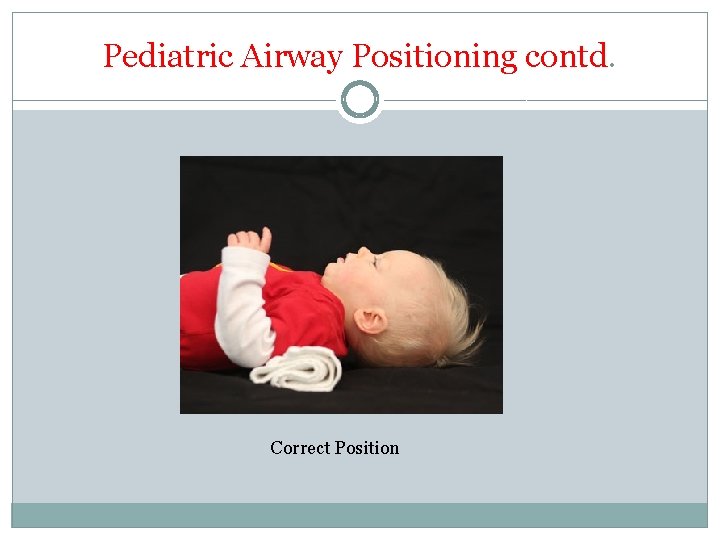
Pediatric Airway Positioning contd. Correct Position
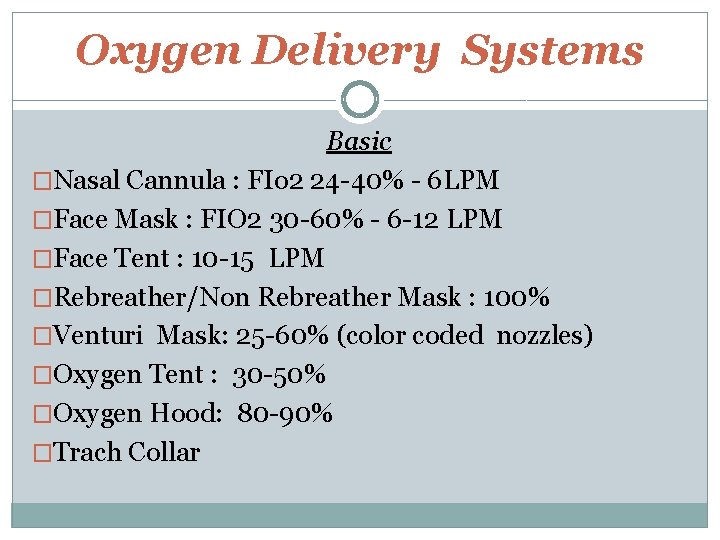
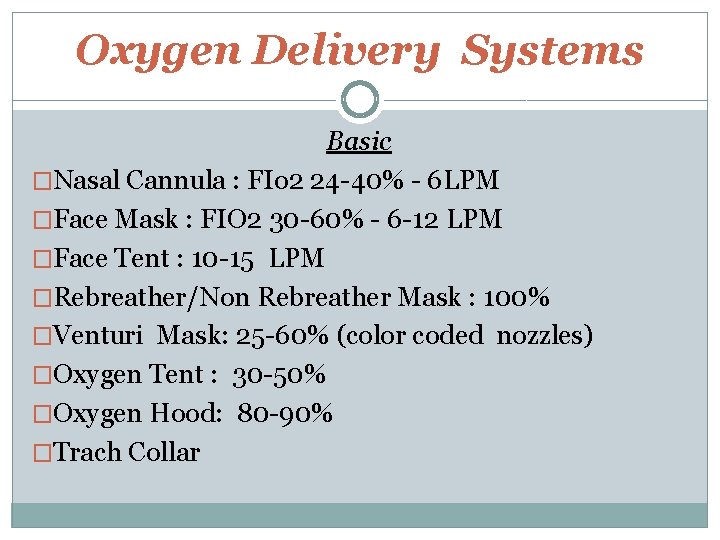
Oxygen Delivery Systems Basic �Nasal Cannula : FIo 2 24 -40% - 6 LPM �Face Mask : FIO 2 30 -60% - 6 -12 LPM �Face Tent : 10 -15 LPM �Rebreather/Non Rebreather Mask : 100% �Venturi Mask: 25 -60% (color coded nozzles) �Oxygen Tent : 30 -50% �Oxygen Hood: 80 -90% �Trach Collar
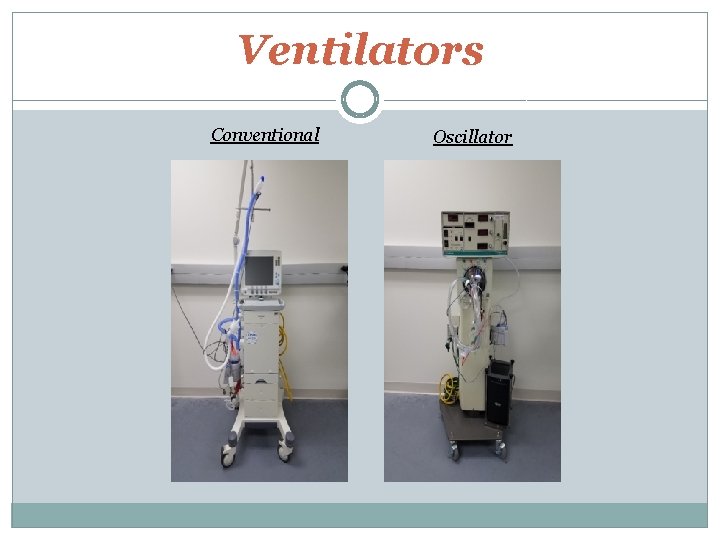
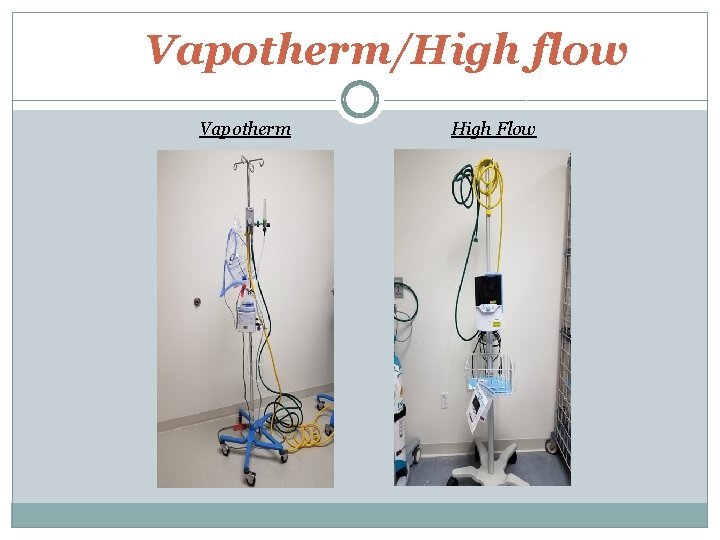
Oxygen Delivery System contd Advanced �Vapotherm �CPAP (Continuous positive airway pressure) �Bi-PAP (Bi-level positive airway pressure) �Ventilator �Oscillator (HFOV)
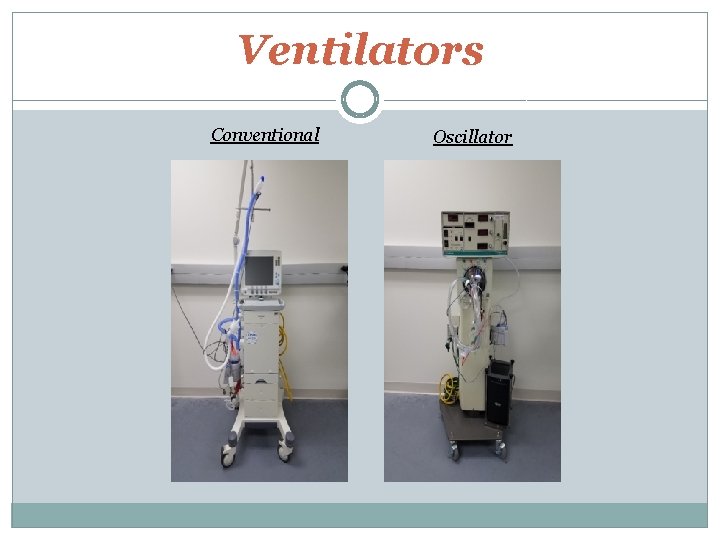
Ventilators Conventional Oscillator
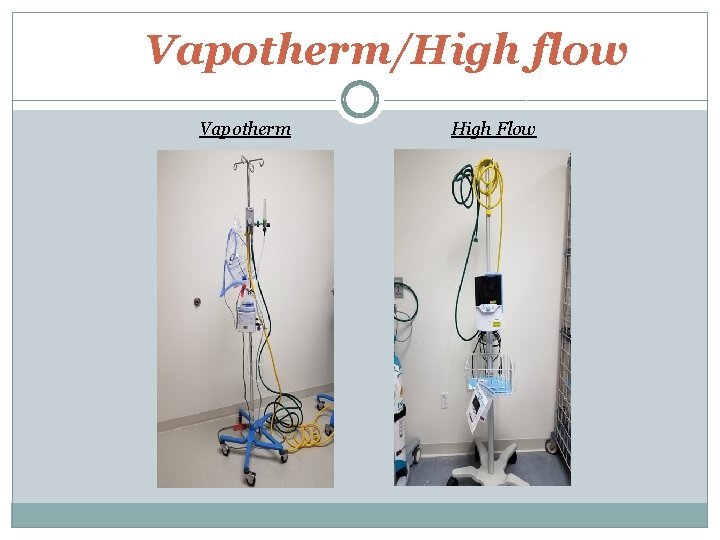
Vapotherm/High flow Vapotherm High Flow

Bipap
Artificial Airway Modes Artificial airways are used to establish patent airway and facilitate respiration �Oropharyngeal ( Oral airway) �Nasopharyngeal (Nasal Trumpet) �Laryngeal Mask Airway (LMA) �Endotracheal/Nasotracheal Tube (ETT) �Tracheostomy Tubes
Oropharyngeal/ Oral Airways �Not usually used in conscious children - vomiting risk �Prevents the tongue from falling back and occluding pharynx �Facilitates in secretion removal �Short term use only �May be used to prevent biting of orotracheal tube
Nasopharyngeal Airways � May be used in conscious and unconscious patients in maintaining airway patency �Soft rubber or plastic tubes �Provide opening from nares to posterior pharyngeal wall � Provide access to pharyngeal suctioning �Often become compressed or obstructed �Could require frequent suctioning to maintain patency
Laryngeal Mask Airway �Used in unconscious patients without intact gag/ cough reflexes �A tube with a balloon mask at the end to seal the hypopharynx �Alternate to endotracheal intubation �Able to use with mechanical ventilation �Does not protect against aspiration �Selection is based on patient size: eg. Size 1 (infant) to size 5 (adults)
Endotracheal Tubes �Oral or nasal �Inserted for respiratory failure requiring mechanical ventilation �May have “cuffs” at the distal end to seal the trachea, preventing air leaks around the tube �Smallest size: 2. 0 uncuffed �Largest size: 10. 5 cuffed �Sizing Equation: (age in years/4) +4 = ETT size Equal to the child’s pinky or nares width May also use Broselow Resuscitation Tape, based on child’s length.
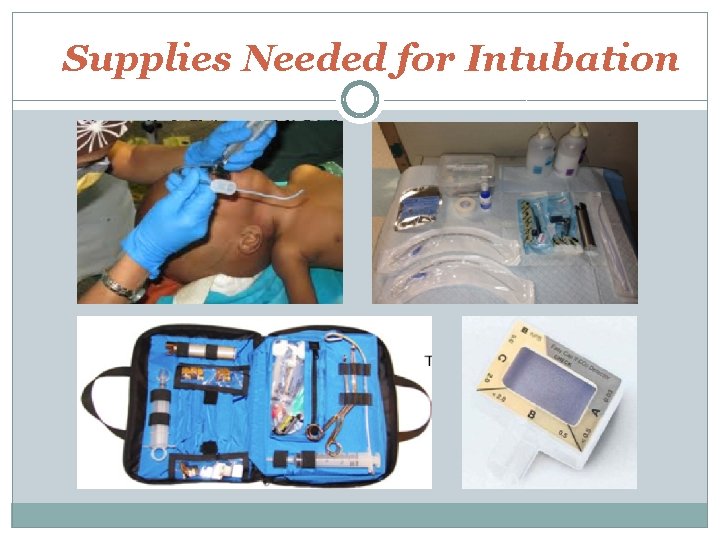
Endotracheal tubes contd Insertion �Using laryngoscope with Mac (curved-children and adults) or Miller (straight-infants), the epiglottis is lifted, and the ETT is passed between the vocal cords into the trachea �Patient is sedated and paralyzed � When intubated the depth of tube should be 3 x ETT size. �Position is confirmed by Pedi-cap/ETCO 2 dectector, 0 xygen saturation, breath sounds, chest expansion, chest x-ray and water vapor inside the tube.
Supplies Needed for Intubation
Tracheostomy Tubes �Surgical opening in the trachea �Emergent or Elective placement �Sizing depends on size of the child; based on physical measurement �Cuffed or Uncuffed �Common types: Shiley, Bivona Flex tend (for the chubby-necked).
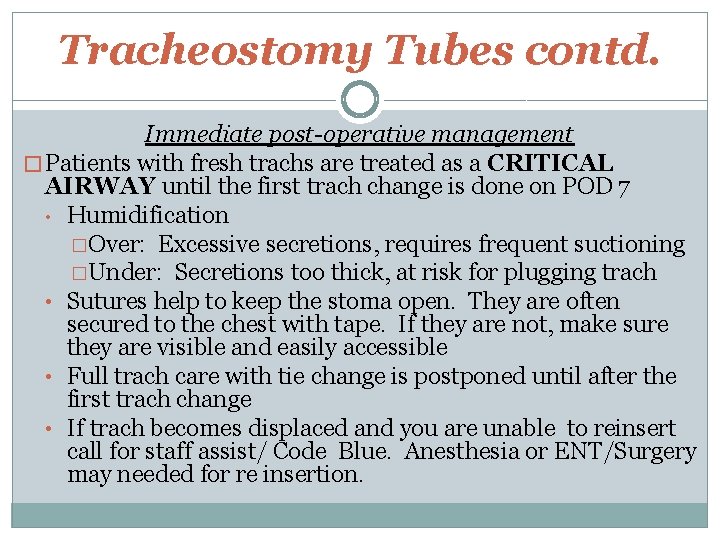
Tracheostomy Tubes contd. Immediate post-operative management � Patients with fresh trachs are treated as a CRITICAL AIRWAY until the first trach change is done on POD 7 • Humidification �Over: Excessive secretions, requires frequent suctioning �Under: Secretions too thick, at risk for plugging trach • Sutures help to keep the stoma open. They are often secured to the chest with tape. If they are not, make sure they are visible and easily accessible • Full trach care with tie change is postponed until after the first trach change • If trach becomes displaced and you are unable to reinsert call for staff assist/ Code Blue. Anesthesia or ENT/Surgery may needed for re insertion.
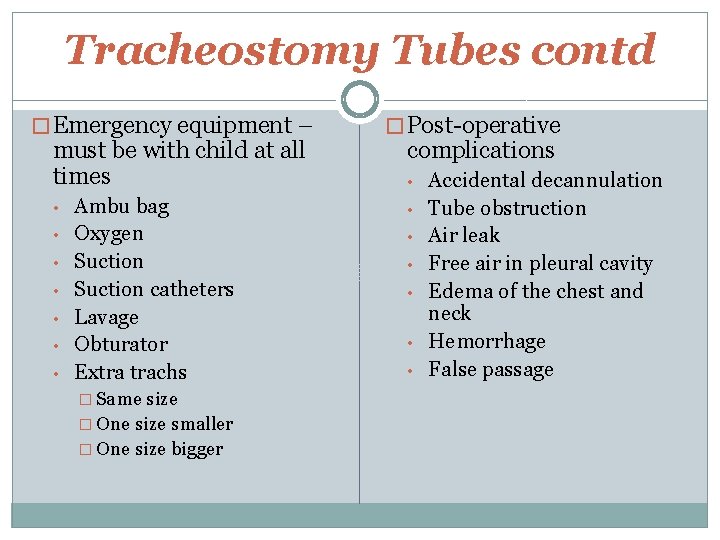
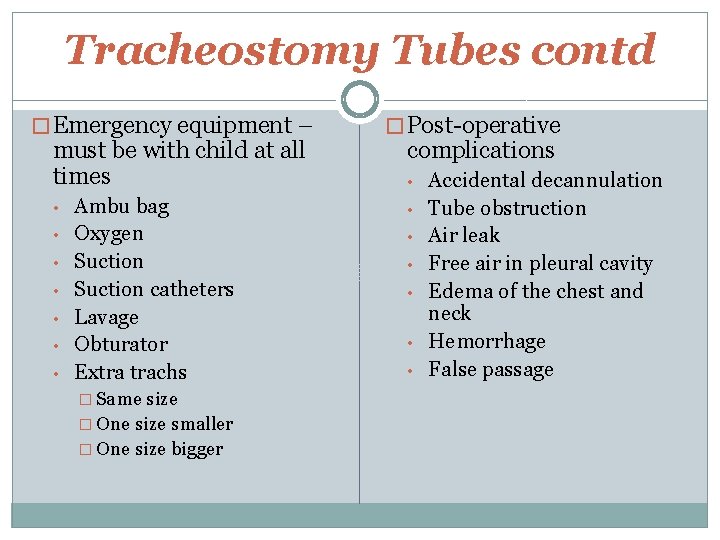
Tracheostomy Tubes contd � Emergency equipment – must be with child at all times • • Ambu bag Oxygen Suction catheters Lavage Obturator Extra trachs � Same size � One size smaller � One size bigger � Post-operative complications • • Accidental decannulation Tube obstruction Air leak Free air in pleural cavity Edema of the chest and neck Hemorrhage False passage
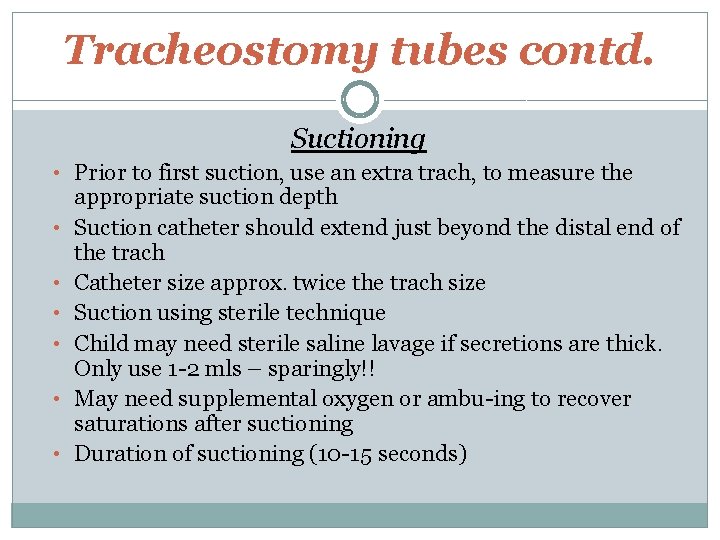
Tracheostomy tubes contd. Suctioning • Prior to first suction, use an extra trach, to measure the • • • appropriate suction depth Suction catheter should extend just beyond the distal end of the trach Catheter size approx. twice the trach size Suction using sterile technique Child may need sterile saline lavage if secretions are thick. Only use 1 -2 mls – sparingly!! May need supplemental oxygen or ambu-ing to recover saturations after suctioning Duration of suctioning (10 -15 seconds)
Respiratory Distress • • • Signs and Symptoms Tachypnea, Tachycardia, Agitation, Grunting, Flaring, Retractions Wheezing, Stridor, Inability to lie down Use of Accessory muscles, Sweating Head bobbing, Cyanosis, Apnea
Respiratory Failure • • Signs & Symptoms Increased WOB Decreased lung volumes/alveolar collapse Upper airway obstruction- stridor and retraction Lower airway obstruction- wheezing Decreased air entry Compromised perfusion Altered LOC
Respiratory Failure Management • Prevention* • Non-invasive monitoring –pulse ox • Invasive monitoring – blood gases • Supplemental O 2 • Mechanical ventilation
BAG-MASK VENTILATION �Used to support patients with inadequate respiratory effort �Positioning is key in performing adequate BMV � 3 key points • • • Maintain open airway Establish seal between mask and face Deliver optimal breath volume and respiratory rate
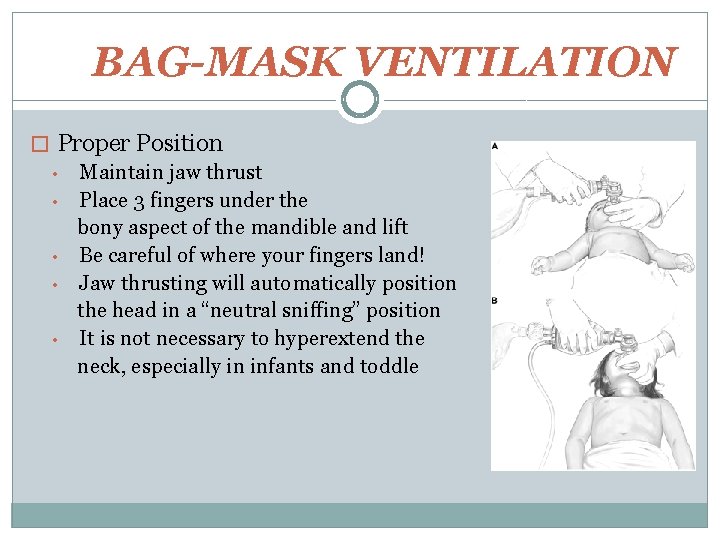
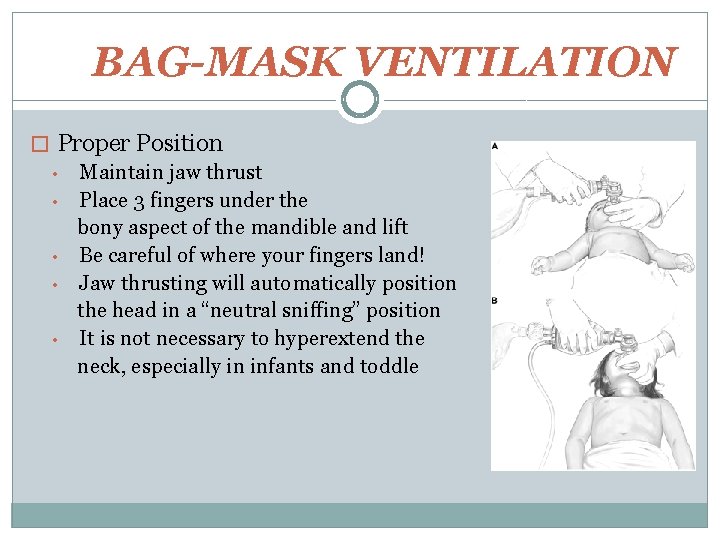
BAG-MASK VENTILATION � Proper Position • Maintain jaw thrust • Place 3 fingers under the bony aspect of the mandible and lift • Be careful of where your fingers land! • Jaw thrusting will automatically position the head in a “neutral sniffing” position • It is not necessary to hyperextend the neck, especially in infants and toddle
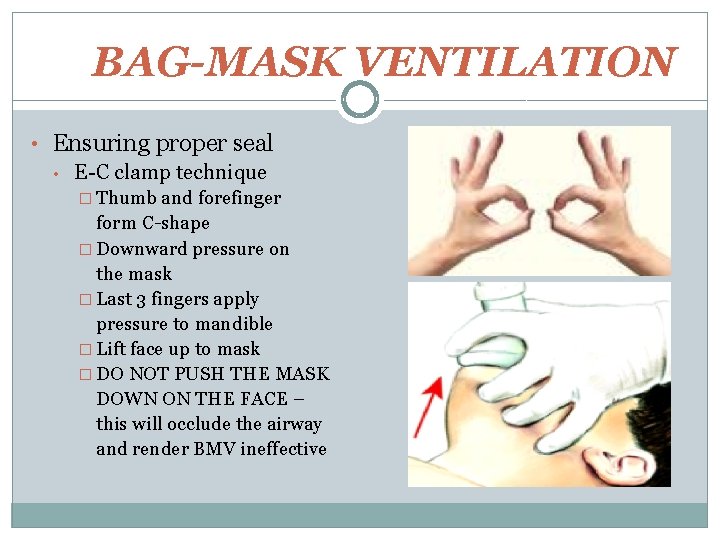
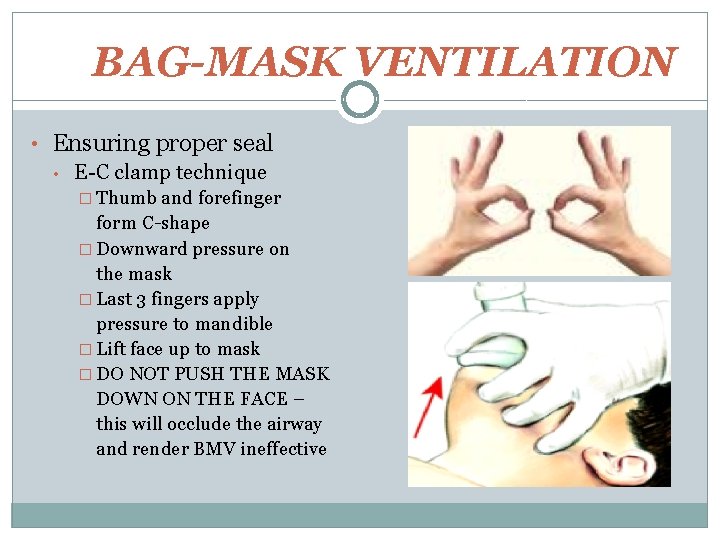
BAG-MASK VENTILATION • Ensuring proper seal • E-C clamp technique � Thumb and forefinger form C-shape � Downward pressure on the mask � Last 3 fingers apply pressure to mandible � Lift face up to mask � DO NOT PUSH THE MASK DOWN ON THE FACE – this will occlude the airway and render BMV ineffective
BAG-MASK VENTILATION �Assessing adequate Bag-Mask Ventilation • • • Look for chest rise Listen for bilateral breath sounds Note vital signs Assess patient’s color and perfusion Monitor oxygen saturation
 Epiglottic
Epiglottic Pat pat seguimiento
Pat pat seguimiento Pat pediatric assessment
Pat pediatric assessment Normal values of vital signs
Normal values of vital signs Pediatric assessment triangle
Pediatric assessment triangle Paediatric assessment triangle
Paediatric assessment triangle Savannah thorpe
Savannah thorpe Gina thorpe
Gina thorpe Karla thorpe
Karla thorpe Thorpe park competitors
Thorpe park competitors Space art lesson
Space art lesson Thorpe bay yacht club
Thorpe bay yacht club Rfi group
Rfi group Thermodynamic control
Thermodynamic control Sale and leaseback ifrs 16
Sale and leaseback ifrs 16 Airway management acls
Airway management acls Tracheostomy stoma
Tracheostomy stoma Airway ladder
Airway ladder Npa measurement
Npa measurement Airway abcde
Airway abcde Sandwich manuver adalah
Sandwich manuver adalah Stepwise airway management
Stepwise airway management Instant messenger msn
Instant messenger msn Msn
Msn Chamberlain fnp reviews
Chamberlain fnp reviews Msn msft
Msn msft Msn wetter jakutsk
Msn wetter jakutsk Msn dating
Msn dating Msn messenger chat rooms
Msn messenger chat rooms Messenger
Messenger Legal nurse consultant websites
Legal nurse consultant websites