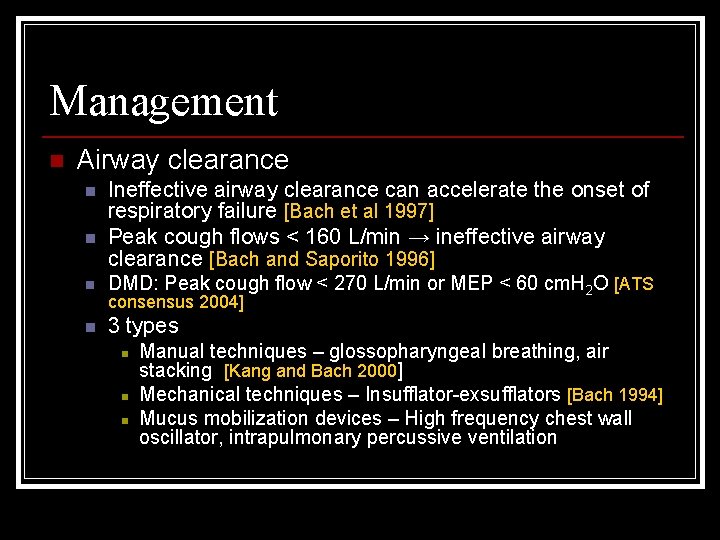
Management n Airway clearance n n Ineffective airway


- Slides: 9
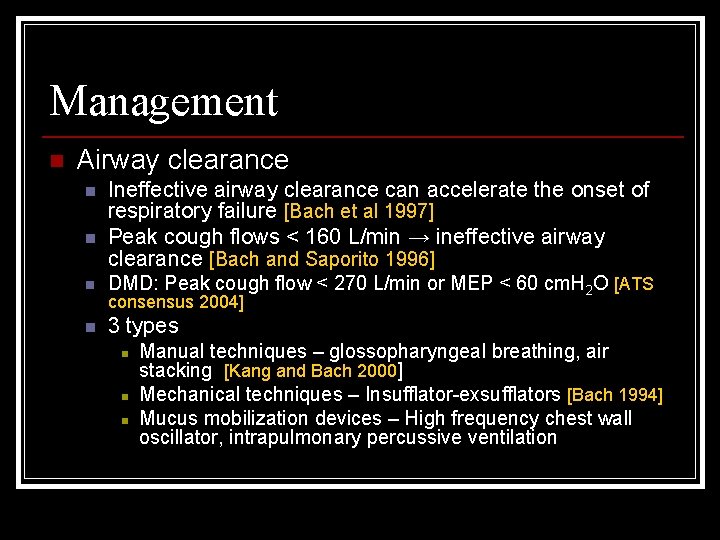
Management n Airway clearance n n Ineffective airway clearance can accelerate the onset of respiratory failure [Bach et al 1997] Peak cough flows < 160 L/min → ineffective airway clearance [Bach and Saporito 1996] n DMD: Peak cough flow < 270 L/min or MEP < 60 cm. H 2 O [ATS n 3 types consensus 2004] n n n Manual techniques – glossopharyngeal breathing, air stacking [Kang and Bach 2000] Mechanical techniques – Insufflator-exsufflators [Bach 1994] Mucus mobilization devices – High frequency chest wall oscillator, intrapulmonary percussive ventilation
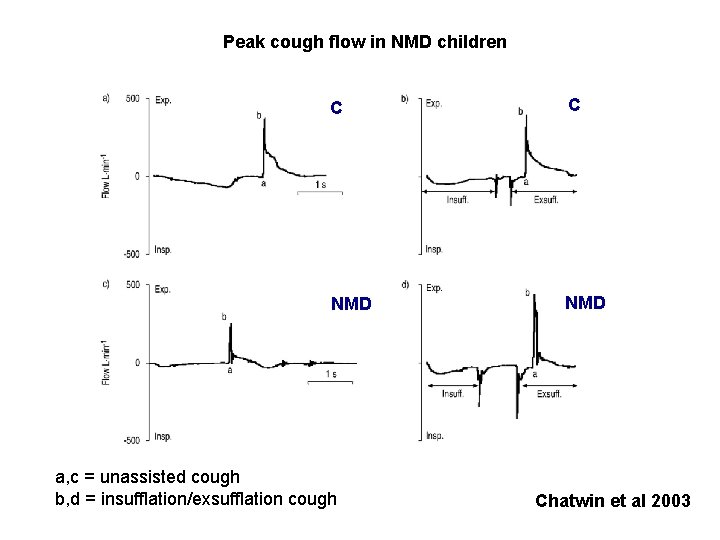
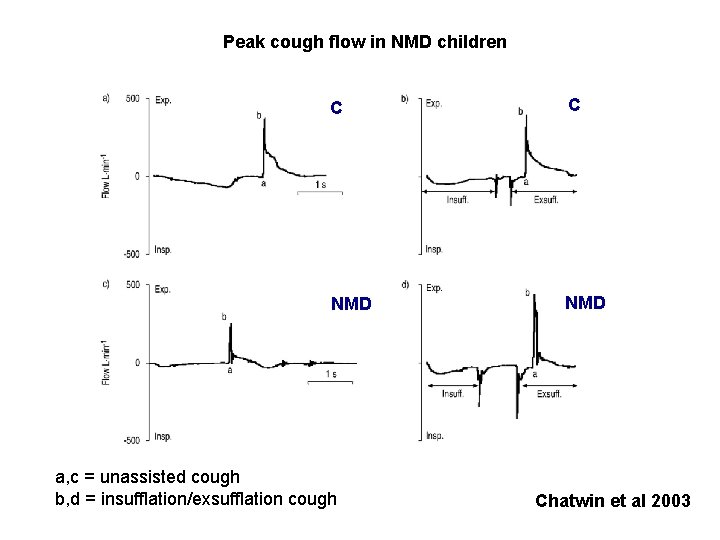
Peak cough flow in NMD children C C NMD a, c = unassisted cough b, d = insufflation/exsufflation cough Chatwin et al 2003
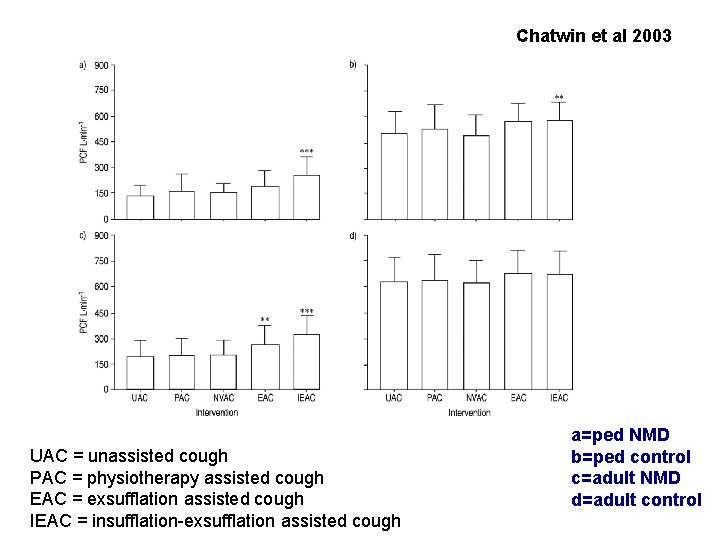
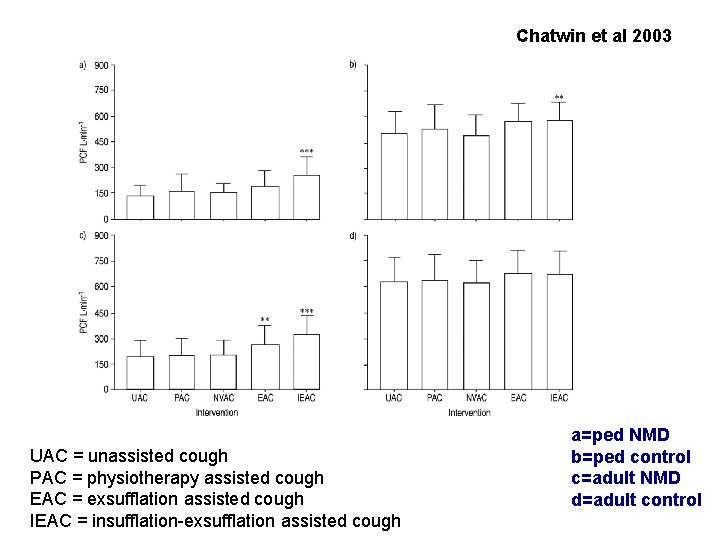
Chatwin et al 2003 UAC = unassisted cough PAC = physiotherapy assisted cough EAC = exsufflation assisted cough IEAC = insufflation-exsufflation assisted cough a=ped NMD b=ped control c=adult NMD d=adult control

Patient with SMA using the MI-E via a mouthpiece Miske, L. J. et al. Chest 2004; 125: 1406 -1412

Left, A: chest radiograph of 22 -month-old girl with SMA type I and right upper lobe density Miske, L. J. et al. Chest 2004; 125: 1406 -1412
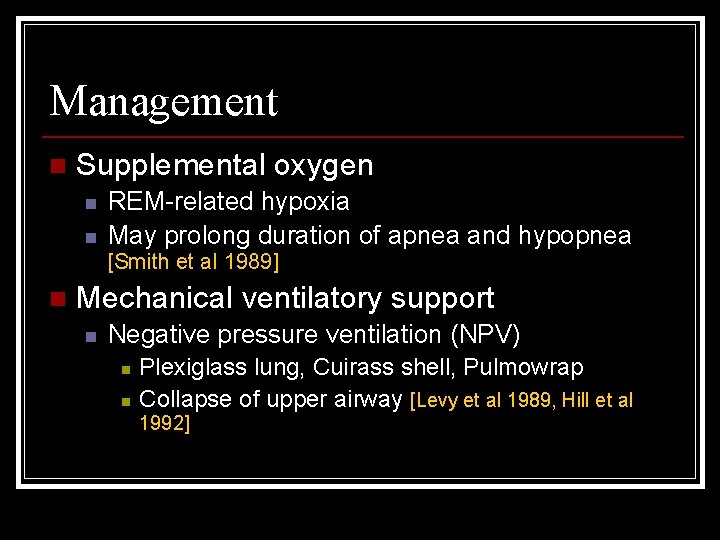
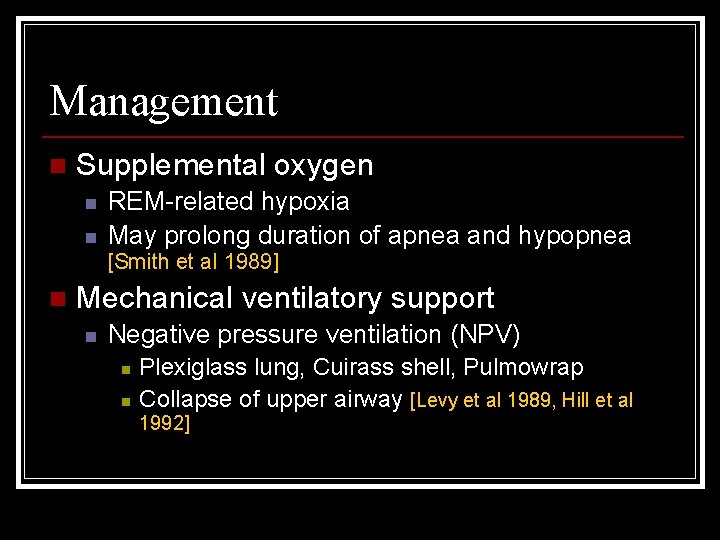
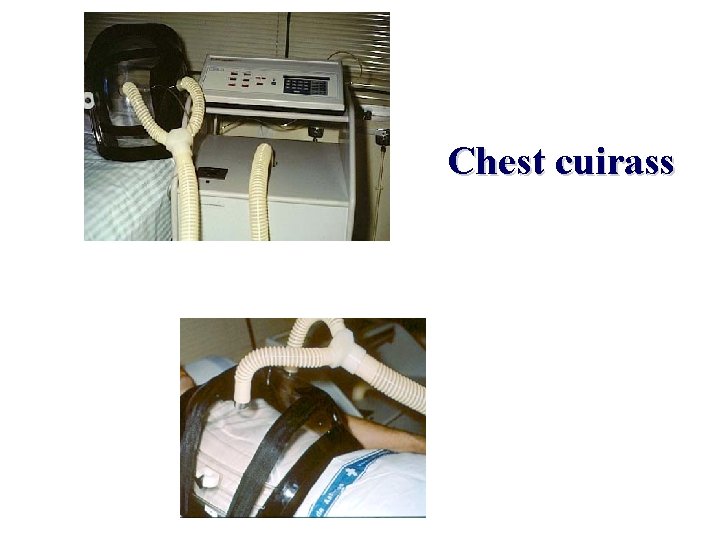
Management n Supplemental oxygen n n REM-related hypoxia May prolong duration of apnea and hypopnea [Smith et al 1989] n Mechanical ventilatory support n Negative pressure ventilation (NPV) n n Plexiglass lung, Cuirass shell, Pulmowrap Collapse of upper airway [Levy et al 1989, Hill et al 1992]
Chest cuirass
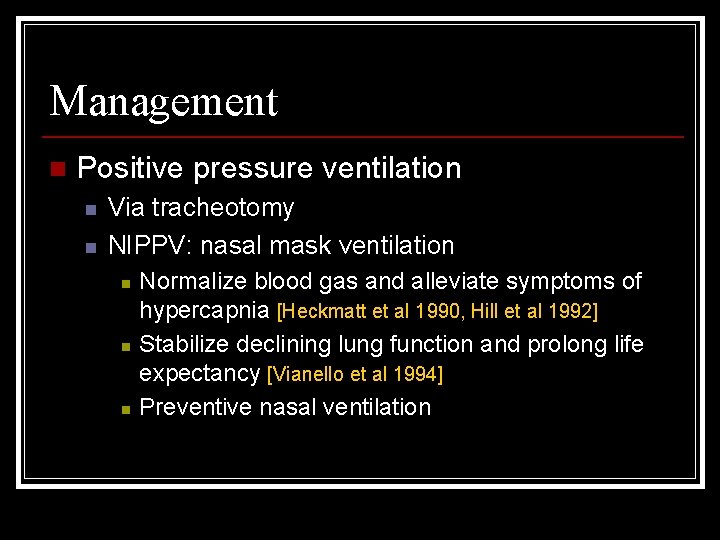
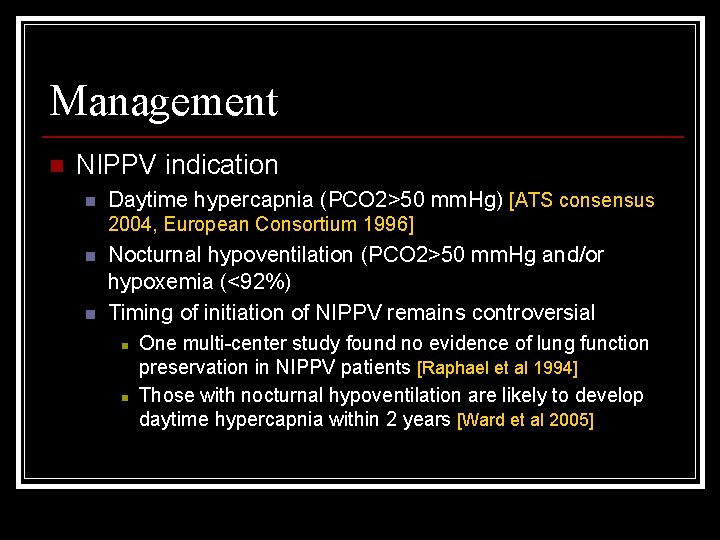
Management n Positive pressure ventilation n n Via tracheotomy NIPPV: nasal mask ventilation n Normalize blood gas and alleviate symptoms of hypercapnia [Heckmatt et al 1990, Hill et al 1992] Stabilize declining lung function and prolong life expectancy [Vianello et al 1994] Preventive nasal ventilation
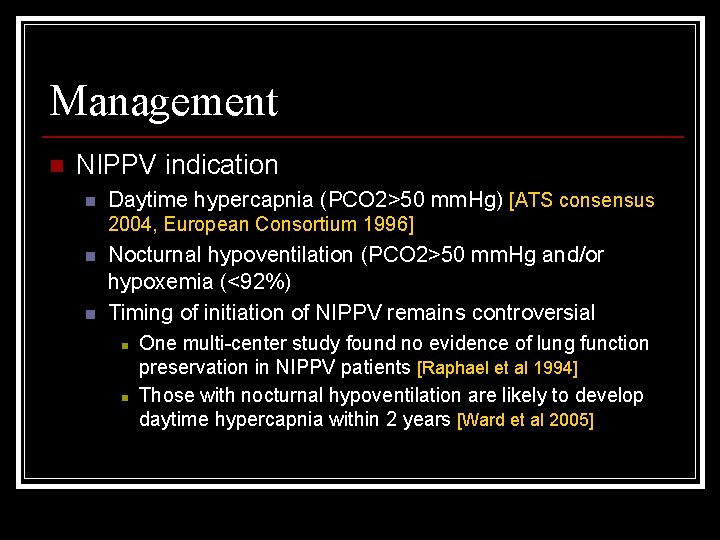
Management n NIPPV indication n Daytime hypercapnia (PCO 2>50 mm. Hg) [ATS consensus 2004, European Consortium 1996] n n Nocturnal hypoventilation (PCO 2>50 mm. Hg and/or hypoxemia (<92%) Timing of initiation of NIPPV remains controversial n n One multi-center study found no evidence of lung function preservation in NIPPV patients [Raphael et al 1994] Those with nocturnal hypoventilation are likely to develop daytime hypercapnia within 2 years [Ward et al 2005]
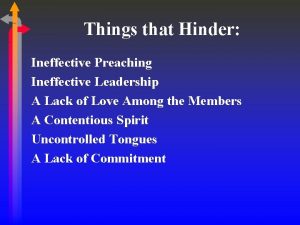
 Nursing diagnosis of lung cancer
Nursing diagnosis of lung cancer Upper airway and lower airway
Upper airway and lower airway Powerlessness related to
Powerlessness related to Ineffective performance
Ineffective performance Ineffective praise
Ineffective praise Poor listening skills
Poor listening skills Types of ineffective listening
Types of ineffective listening Differentiate effective therbligs and ineffective therbligs
Differentiate effective therbligs and ineffective therbligs Antisocial personality disorder nursing interventions
Antisocial personality disorder nursing interventions Nursing interventions for ineffective coping
Nursing interventions for ineffective coping