Personality and ImpulseControl Disorders Chapter 20 What is




- Slides: 54
Personality and Impulse-Control Disorders Chapter 20
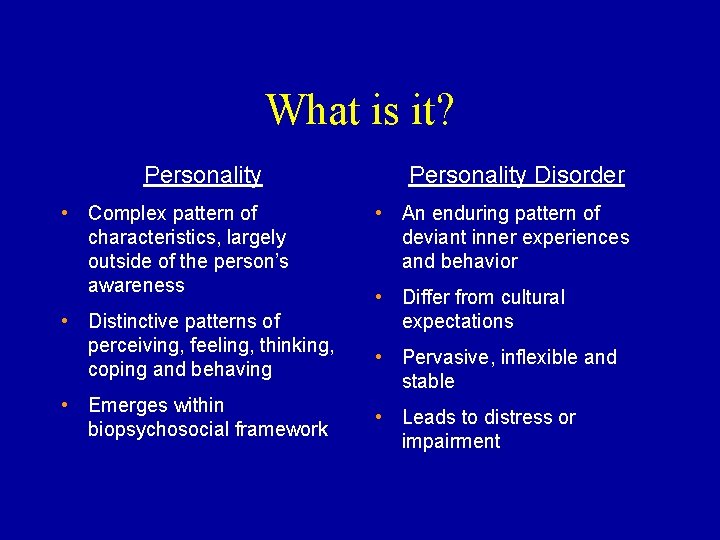
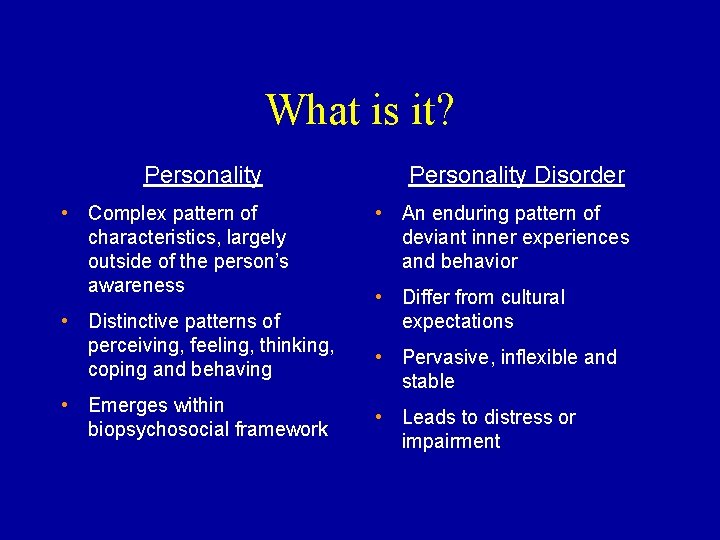
What is it? Personality • Complex pattern of characteristics, largely outside of the person’s awareness • Distinctive patterns of perceiving, feeling, thinking, coping and behaving • Emerges within biopsychosocial framework Personality Disorder • An enduring pattern of deviant inner experiences and behavior • Differ from cultural expectations • Pervasive, inflexible and stable • Leads to distress or impairment
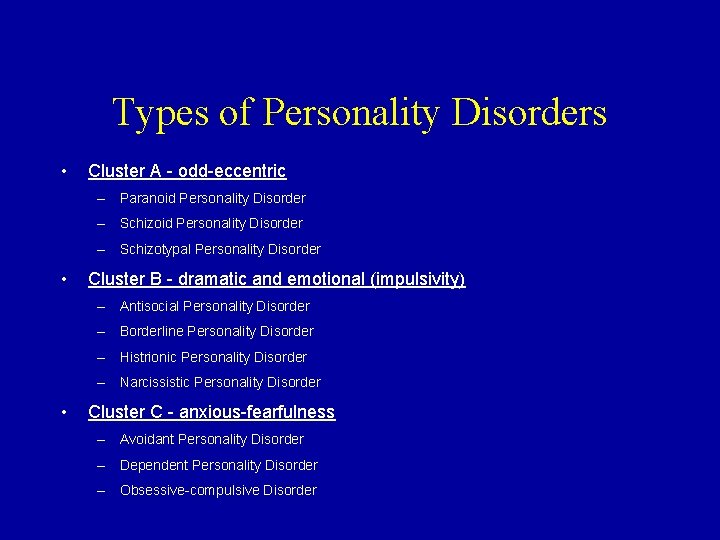
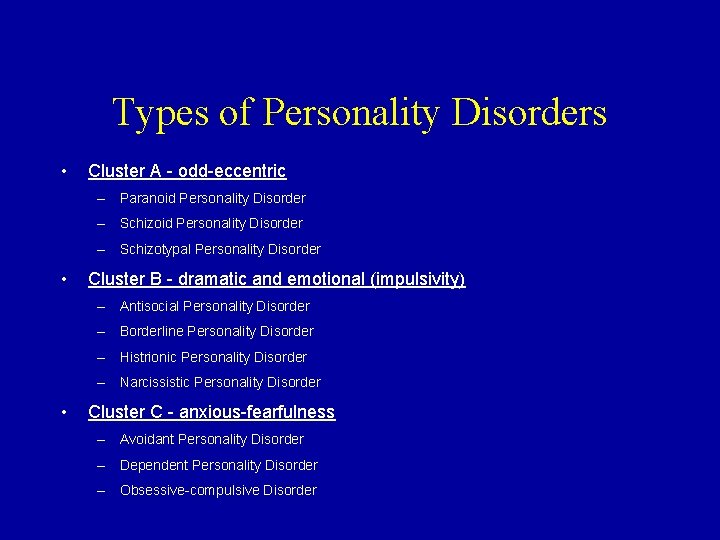
Types of Personality Disorders • Cluster A - odd-eccentric – Paranoid Personality Disorder – Schizotypal Personality Disorder • Cluster B - dramatic and emotional (impulsivity) – Antisocial Personality Disorder – Borderline Personality Disorder – Histrionic Personality Disorder – Narcissistic Personality Disorder • Cluster C - anxious-fearfulness – Avoidant Personality Disorder – Dependent Personality Disorder – Obsessive-compulsive Disorder
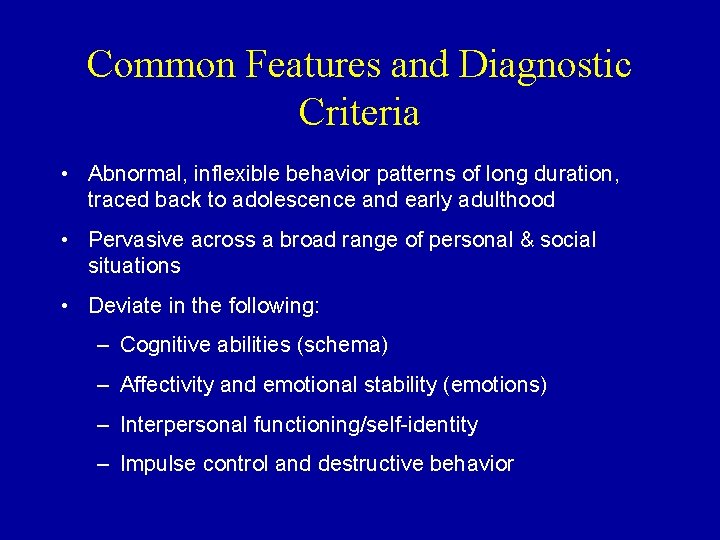
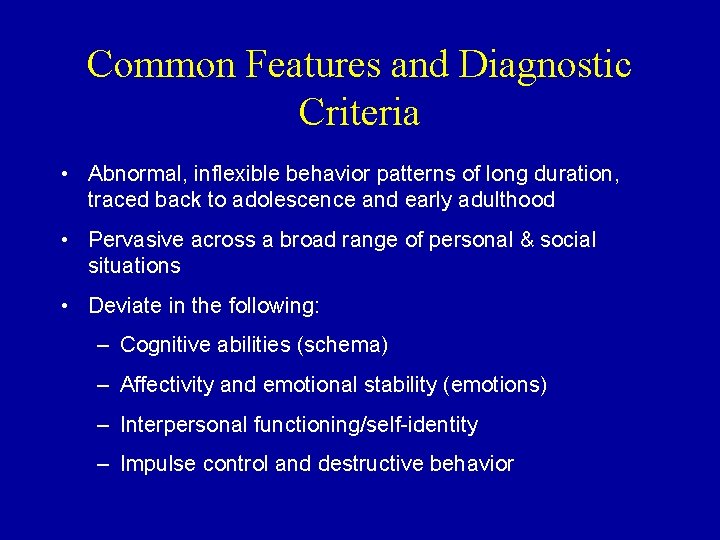
Common Features and Diagnostic Criteria • Abnormal, inflexible behavior patterns of long duration, traced back to adolescence and early adulthood • Pervasive across a broad range of personal & social situations • Deviate in the following: – Cognitive abilities (schema) – Affectivity and emotional stability (emotions) – Interpersonal functioning/self-identity – Impulse control and destructive behavior
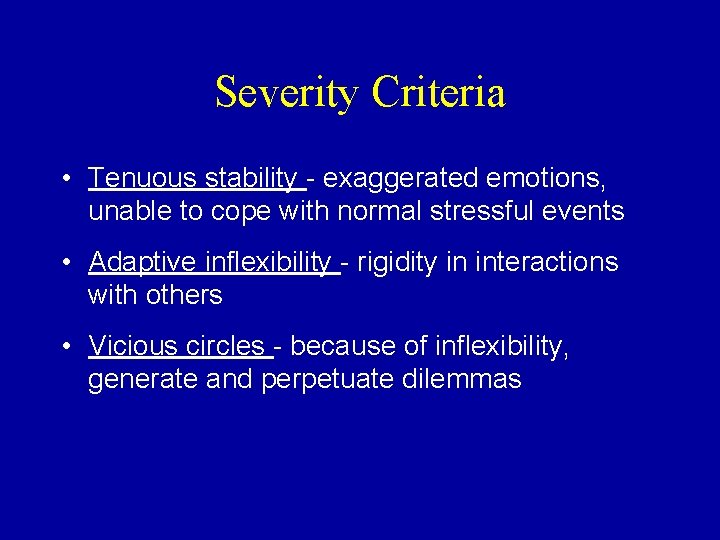
Severity Criteria • Tenuous stability - exaggerated emotions, unable to cope with normal stressful events • Adaptive inflexibility - rigidity in interactions with others • Vicious circles - because of inflexibility, generate and perpetuate dilemmas
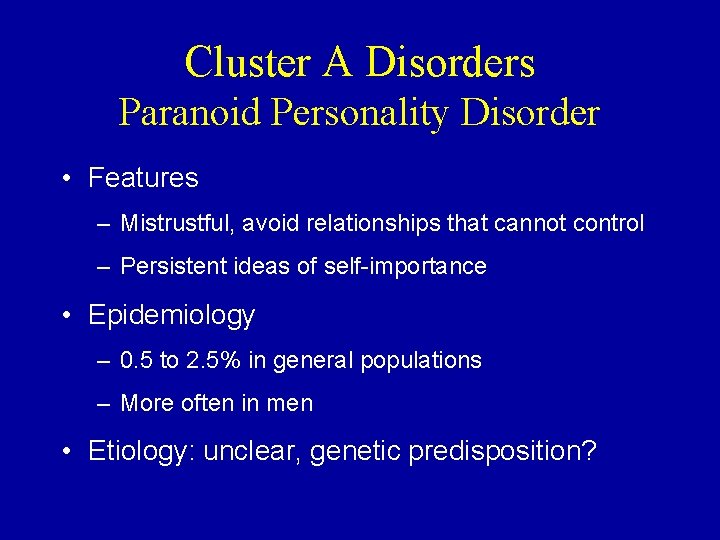
Cluster A Disorders Paranoid Personality Disorder • Features – Mistrustful, avoid relationships that cannot control – Persistent ideas of self-importance • Epidemiology – 0. 5 to 2. 5% in general populations – More often in men • Etiology: unclear, genetic predisposition?
Cluster A Disorders Paranoid Personality Disorder Nursing Management – Patients seen for other health problems – Nsg DX: Disturbed thought process, social isolation – Nursing Interventions • It can be difficult to establish nurse-patient relationship. • If trust is established, help patient identify problem areas. • Changing thought patterns takes time.
Cluster A Disorders Schizoid Personality Disorder • Features – Expressively impassive and interpersonally unengaged – Introverted and reclusive, engage in solitary activities – Communication sometimes confused – Incapable of forming social relationships – Minimum introspection, self-awareness and interpersonal experiences • Epidemiology – Rarely diagnosed in clinical settings – Avoidant personality disorder occurs in 30 to 35% of cases • Etiology: speculative
Cluster A Disorders Schizoid Personality Disorder Nursing Management • Nursing Diagnosis: Impaired social interactions and chronic low self-esteem • Goal: To enhance experience of pleasure • Interventions – Provide social skill training. – Encourage social interactions.
Cluster A Disorders Schizotypal Personality Disorder • Features – Eccentric – Pattern of social and interpersonal deficits – Void of close friends – Odd beliefs – Ideas of reference – When psychotic, symptoms mimic schizophrenia. • Epidemiology • 0. 7 to 5. 1% prevalence • Etiology: unknown • Speculation that this is a part of a continuum of schizophreniarelated disorders
Cluster A Disorders Schizotypal Personality Disorder Nursing Management • Similar to that with schizophrenia • Increase self-worth. • Provide social skills training. • Reinforce socially appropriate dress and behavior. • Focus on enhancing cognitive skills.
Borderline Personality Disorders Clinical Course • Pervasive patterns of instability of interpersonal relationships, self-image and affects, as well as marked impulsivity that begins by early adulthood and is present in a variety of contexts • Problem areas – Regulating moods – Developing a sense of self – Maintaining interpersonal relationships – Maintaining reality-based cognitive processes – Impulsive or destructive behavior • Appear more competent than they are • Live from crisis to crisis
Borderline Personality Disorder • Affective instability - shifts in moods • Identity disturbance (identify diffusion) – Role absorption - narrow definition of self – Painful incoherence - internal disharmony – Inconsistency in thoughts, feelings and actions – Lack of commitment • Unstable interpersonal relationships – Fear of abandonment – Unstable, insecure attachments – Over idealize/intense relationships
Borderline Personality Disorder • Cognitive Dysfunctions – Dichotomous thinking – Dissociation • Dysfunctional Behaviors – Impaired problem-solving – Impulsivity – Self-injurious behaviors (parasuicidal behavior) • Compulsive • Episodic • Repetitive
Borderline Personality Disorder in Special Populations • Many children and adolescents show symptoms similar to those with BPD. • Symptoms begin in adolescents.
Epidemiology • 0. 4 to 2. 0% prevalence in general populations • In clinical populations, BPD is the most frequently diagnosed personality disorder. • Mostly women (77%) • Mean age of diagnosis is mid-20 s. • Coexistence of personality disorders with Axis I disorders (mood, substance abuse eating, dissociative and anxiety disorders)
Risk Factors • Physical and sexual abuse • Parental loss or separation
Etiology • Biologic – Abnormalities associated with affective instability, transient psychotic episodes, and impulsive, aggressive and suicidal behavior • Psychological – Psychoanalytic theory (separation-individuation; projective identification) – Maladaptive cognitive processes
Etiology: Biosocial Theories • Millon – Distinct disorder that develops as a result of both biologic and psychological factors. – Personality is shaped by a) active-passive behavior, b) pleasure-pain and c) sensitivity to self or others. • Linehan – Emotional vulnerability, self-invalidation, unrelenting crises, inhibited grieving, active passivity and apparent competence (Text Box 20. 1)
Risk Factors • Physical and sexual abuse • Separation or loss of parent at an early age (same sex for men)

Interdisciplinary Treatment • Requires the whole mental health care team • Requires a variety of medications including mood stabilizers, antidepressants and, at times, anxiolytics • Psychotherapy
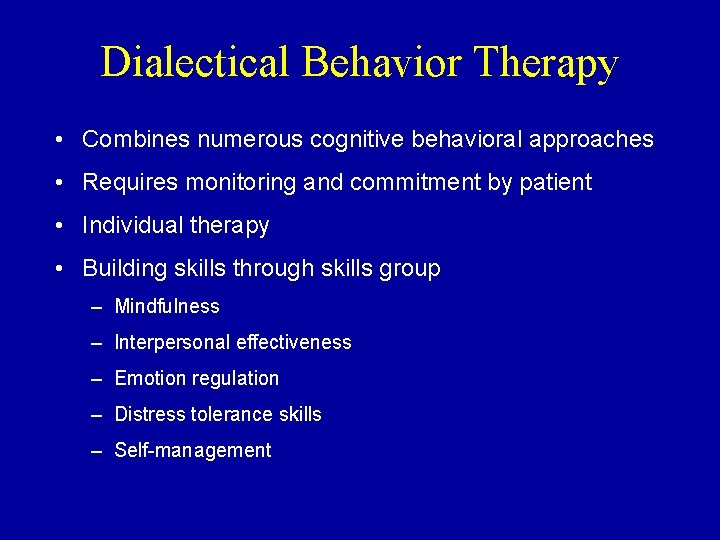
Dialectical Behavior Therapy • Combines numerous cognitive behavioral approaches • Requires monitoring and commitment by patient • Individual therapy • Building skills through skills group – Mindfulness – Interpersonal effectiveness – Emotion regulation – Distress tolerance skills – Self-management
Priority Care Safety!!!
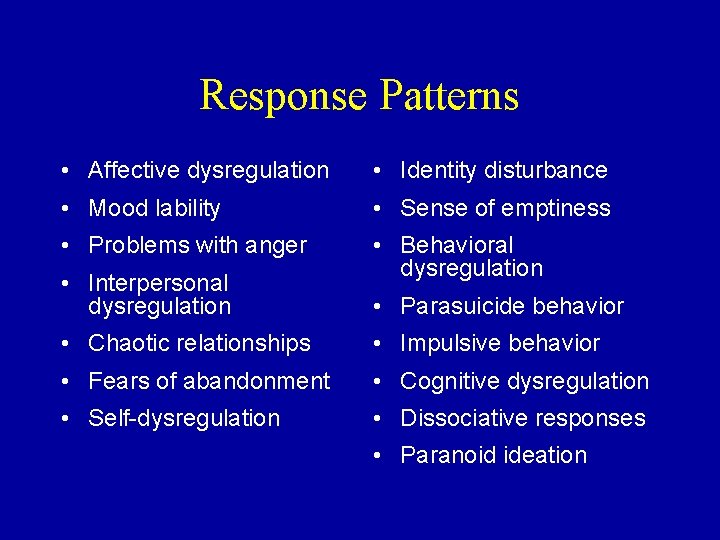
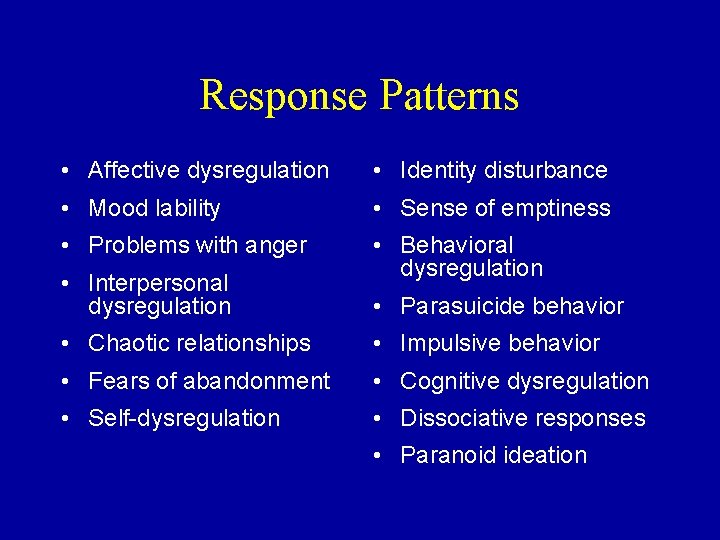
Response Patterns • Affective dysregulation • Identity disturbance • Mood lability • Sense of emptiness • Problems with anger • Behavioral dysregulation • Interpersonal dysregulation • Parasuicide behavior • Chaotic relationships • Impulsive behavior • Fears of abandonment • Cognitive dysregulation • Self-dysregulation • Dissociative responses • Paranoid ideation
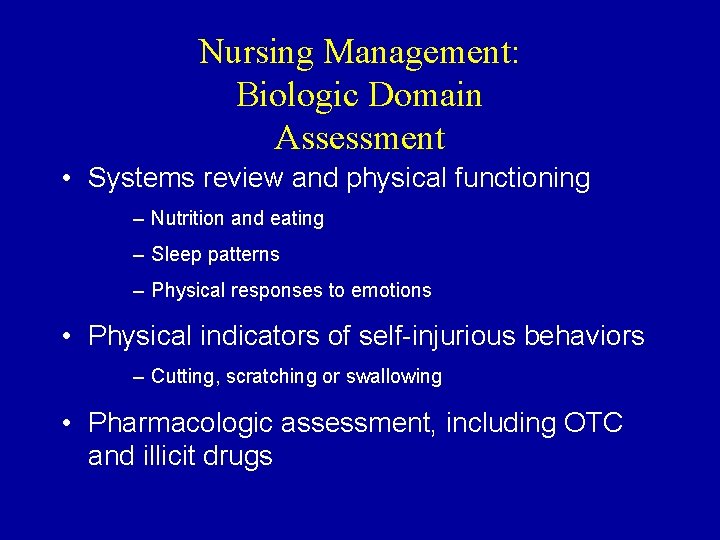
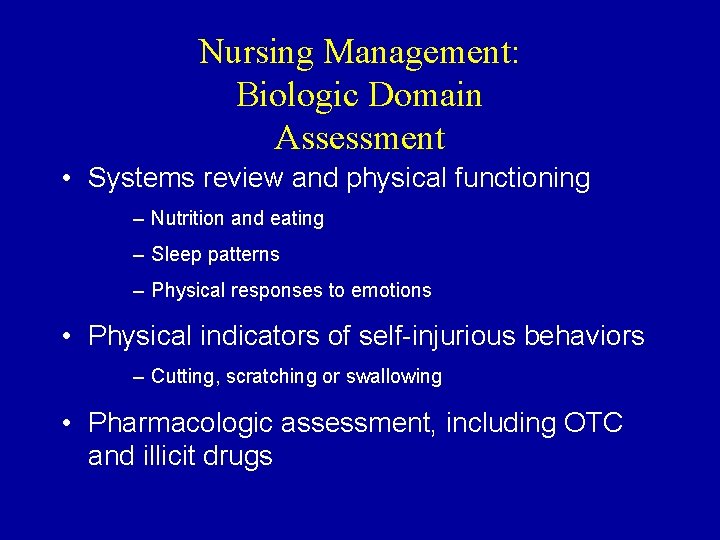
Nursing Management: Biologic Domain Assessment • Systems review and physical functioning – Nutrition and eating – Sleep patterns – Physical responses to emotions • Physical indicators of self-injurious behaviors – Cutting, scratching or swallowing • Pharmacologic assessment, including OTC and illicit drugs
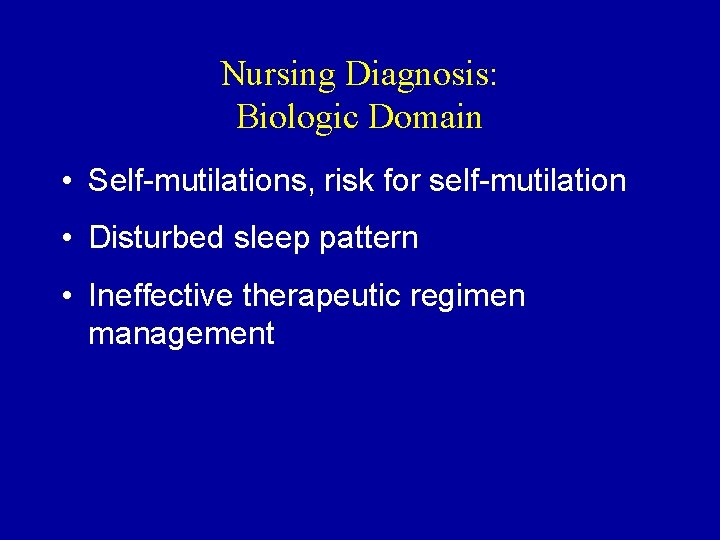
Nursing Diagnosis: Biologic Domain • Self-mutilations, risk for self-mutilation • Disturbed sleep pattern • Ineffective therapeutic regimen management
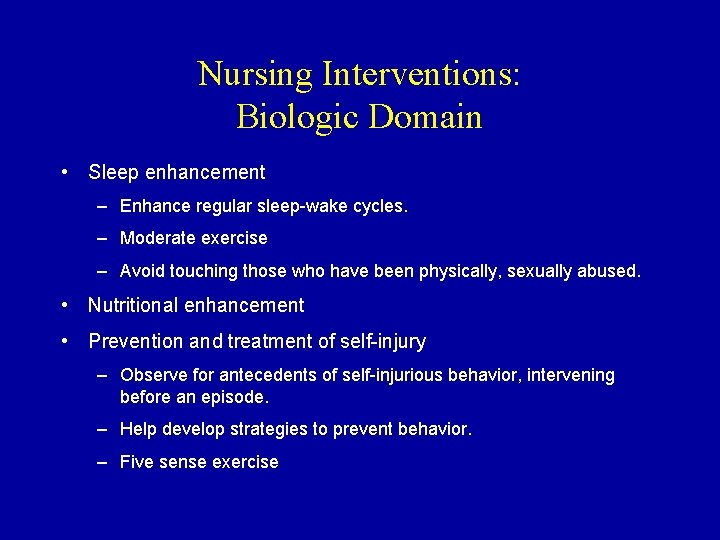
Nursing Interventions: Biologic Domain • Sleep enhancement – Enhance regular sleep-wake cycles. – Moderate exercise – Avoid touching those who have been physically, sexually abused. • Nutritional enhancement • Prevention and treatment of self-injury – Observe for antecedents of self-injurious behavior, intervening before an episode. – Help develop strategies to prevent behavior. – Five sense exercise
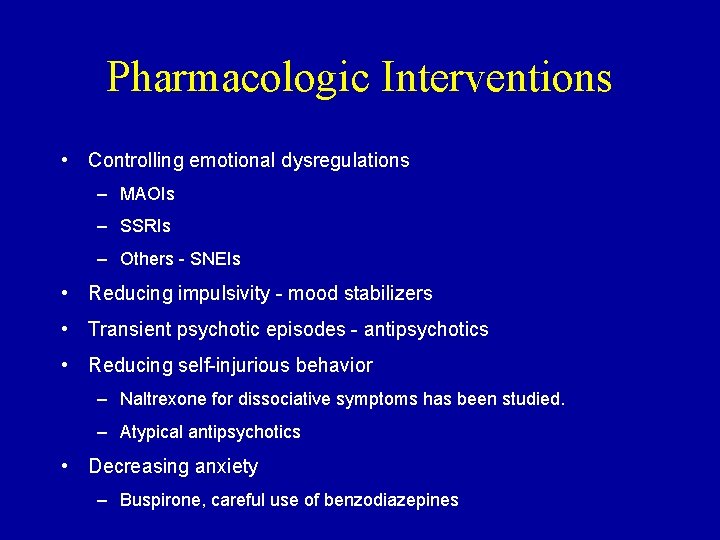
Pharmacologic Interventions • Controlling emotional dysregulations – MAOIs – SSRIs – Others - SNEIs • Reducing impulsivity - mood stabilizers • Transient psychotic episodes - antipsychotics • Reducing self-injurious behavior – Naltrexone for dissociative symptoms has been studied. – Atypical antipsychotics • Decreasing anxiety – Buspirone, careful use of benzodiazepines
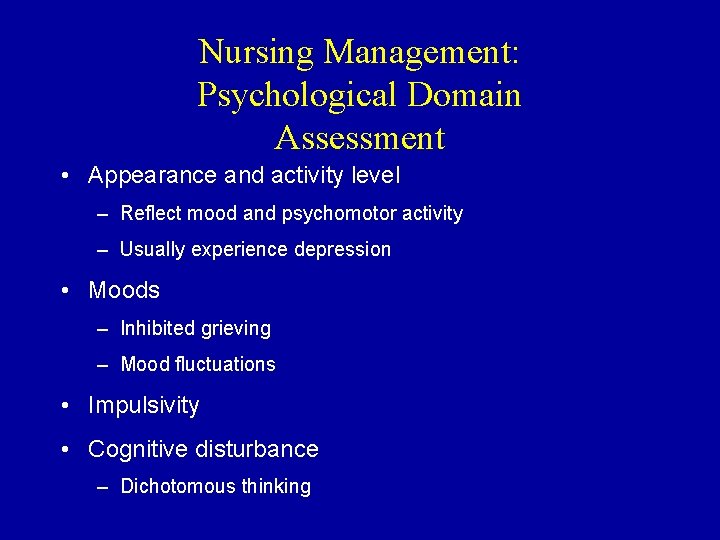
Nursing Management: Psychological Domain Assessment • Appearance and activity level – Reflect mood and psychomotor activity – Usually experience depression • Moods – Inhibited grieving – Mood fluctuations • Impulsivity • Cognitive disturbance – Dichotomous thinking
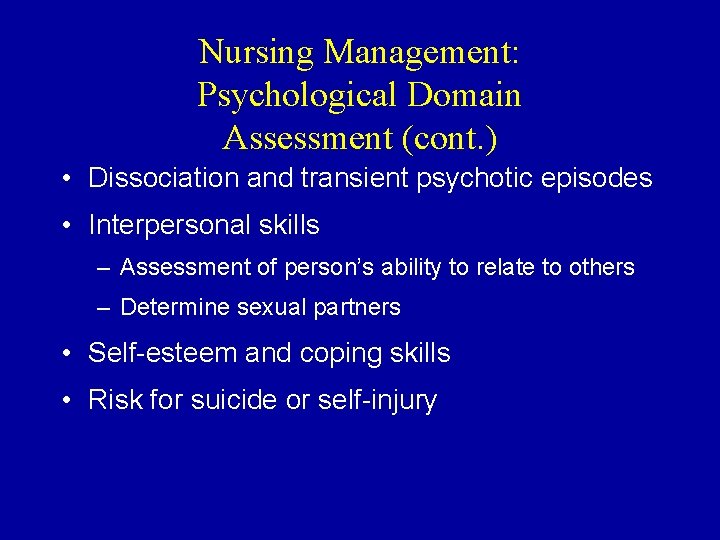
Nursing Management: Psychological Domain Assessment (cont. ) • Dissociation and transient psychotic episodes • Interpersonal skills – Assessment of person’s ability to relate to others – Determine sexual partners • Self-esteem and coping skills • Risk for suicide or self-injury
Nursing Diagnosis Psychological Domain • Risk for self-mutilation • Disturbed thought process • Ineffective coping
Pharmacologic Interventions • Monitoring and administration of medications – Easy to monitor in inpatient – Outpatients may have high rate of noncompliance. • Side effect monitoring and management – Patients appear to be more sensitive to side effects. • Drug-drug interaction – Patients tend to be prone to drug interactions. • Teaching points
Nursing Interventions: Psychological Domain • Nurse-patient relationship – Establish trust. – Recognize conflicting fears of abandonment and intimacy. – Establish personal boundaries and limitations. • Abandonment and intimacy fears – Recognize conflict. – Any termination needs to be planned carefully. • Establish personal boundaries and limitations. • Management of dissociative states – Determine triggers.
Nursing Interventions: Psychological Domain (cont. ) • Behavioral interventions – Goal is to replace dysfunctional behaviors with positive ones. – Validate positives; avoid confrontation if possible. • Cognitive interventions – Emotional regulation – Communication triad – Distraction or thought triad – Challenging dysfunctional thinking • Management of transient psychotic episodes • Patient episodes

Nursing Management: Social Domain Assessment • Functional status – Current job – Community activities • Social support systems • Family assessment

Nursing Interventions: Social Domain • Milieu management • Group interventions • Family and social support
Nursing Management Psychological Assessment • Appearance and activity level • Moods - inhibited grieving • Impulsivity • Suicide and/or self-injurious behavior – Dichotomous thinking – Dissociation and psychotic episodes • Self-esteem and coping skills
Nursing Management Social Assessment • Family • Interpersonal skills • Social support systems
Nursing Diagnosis • Risk for self-mutilation • Altered thought processes • Ineffective coping • Personal identity disturbance • Anxiety • Grief • Low self-esteem • Powerlessness • Social isolation • Spiritual distress
Biologic Interventions • Sleep management • Nutrition • Management of psychotic episodes • Prevention of self-injury • Pharmacologic management
Psychological Interventions: Cognitive • Communication triad – An “I” statement to identify and express their feelings – A nonjudgmental statement of the emotional trigger – What could be done differently or what would restore comfort to the situation • Thought stopping • Challenging dysfunctional thinking (Text Box 22 -4) • Education

Social Interventions • Milieu management • Group interventions • Family and social support
Antisocial Personality Disorder • Pervasive pattern of disregard for, and violation of, the rights of others that begins in childhood or early adolescence • Behaviorally impulsive • Interpersonally irresponsible • Fail to adapt to the ethical and social standards of community • Interpersonally engaging, but in reality lack empathy • Easily irritated, often aggressive
Epidemiology and Risk Factors • 0. 2 to 3% of the population • Age of onset - exhibit antisocial behavior before 15 • Men more often diagnosed (See Text Box 226. ) • Present in all cultures • Comorbid with alcohol and drug abuse
Etiology • Biologic – Genetic component – Five times more common in firstdegree relatives – Biochemical - not well understood • Psychological – Insecure attachments – Difficult temperament • Social – Chaotic families – Abuse
Nursing Management Assessment • Difficult to establish a relationship • Determine quality of relationships • Impulsivity • Aggression • Ability to assume responsibility for their actions • Amount of blaming others
Nursing Diagnosis • Altered role performance • Ineffective individual coping • Impaired communication • Impaired social interactions • Defensive self-esteem • Risk for violence
Nursing Management • Biologic - physical effects of chronic use of addictive substances • Psychological – Self-responsibility facilitation – Self-awareness enhancement – Anger management – Patient education • Social – Group – Milieu
Family Interventions • Help families establish boundaries. • Help families recognize patient’s responsibility for his or her actions.
Histrionic Personality Disorder • Attention seeking, life of the party, uncomfortable with single relationship • Women - dress seductively • Men - dress - “macho” • Become depressed when not center of attention
Histrionic Personality Disorder • 2 to 3% of population • Highly alert individuals • Parent modeling - “like mom” • Nursing intervention – Develop a sense of self without validation of others
Narcissistic Personality Disorder • Grandiose • Inexhaustible need for attention • Fantasies about power, unlimited success • 1% of population • Etiology - unknown • Rarely encounter them
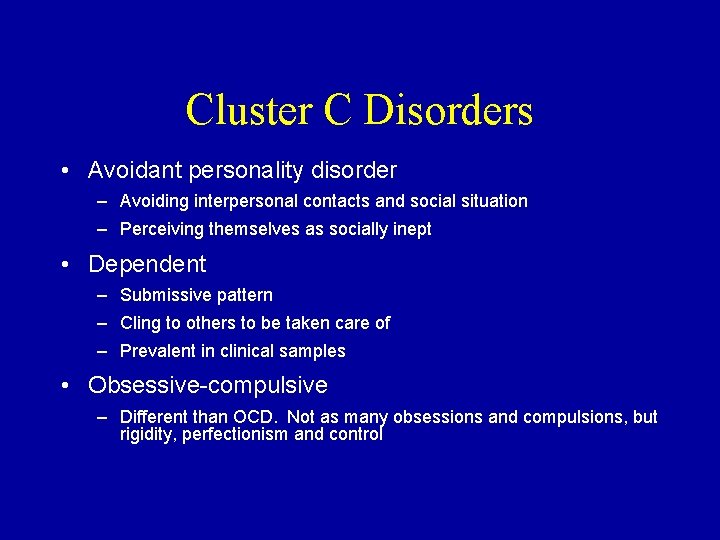
Cluster C Disorders • Avoidant personality disorder – Avoiding interpersonal contacts and social situation – Perceiving themselves as socially inept • Dependent – Submissive pattern – Cling to others to be taken care of – Prevalent in clinical samples • Obsessive-compulsive – Different than OCD. Not as many obsessions and compulsions, but rigidity, perfectionism and control
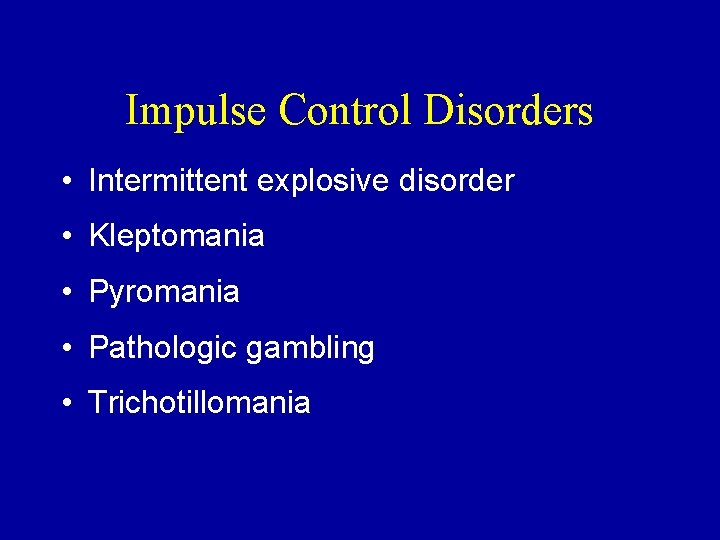
Impulse Control Disorders • Intermittent explosive disorder • Kleptomania • Pyromania • Pathologic gambling • Trichotillomania