Personality Disorders Contents What is a Personality Disorder
![Crisis Management Plan (2) When I feel [EMOTION] and feel like [BEHAVIOUR], I will Crisis Management Plan (2) When I feel [EMOTION] and feel like [BEHAVIOUR], I will](https://slidetodoc.com/presentation_image/d23e65976041bc1ab68d47b31dcf29a7/image-33.jpg)
- Slides: 34
Personality Disorders
Contents � What is a Personality Disorder? � Management � There’s & Containment no “I” in “Team”
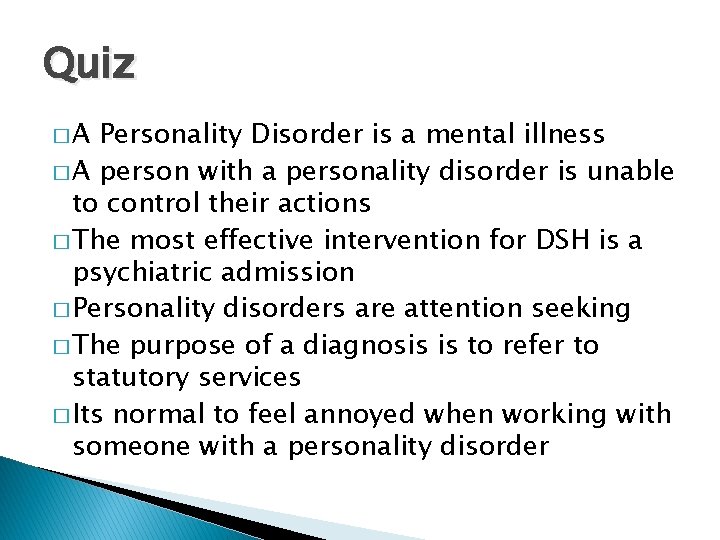
Quiz �A Personality Disorder is a mental illness � A person with a personality disorder is unable to control their actions � The most effective intervention for DSH is a psychiatric admission � Personality disorders are attention seeking � The purpose of a diagnosis is to refer to statutory services � Its normal to feel annoyed when working with someone with a personality disorder
Personality � ‘personality’ refers to the collection of characteristics/traits developed � By our late teens we have developed our own personality (thinking, feeling and behaving). � These stay pretty much the same for the rest of our life. Usually, our personality allows us to get on reasonably well with other people.
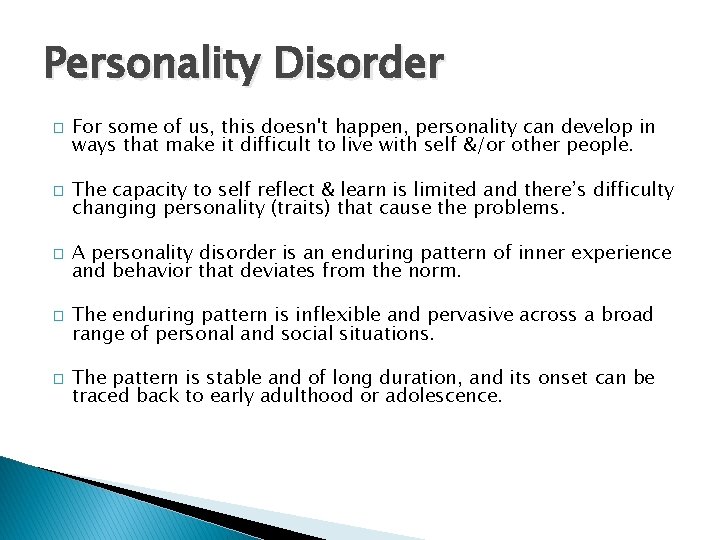
Personality Disorder � � � For some of us, this doesn't happen, personality can develop in ways that make it difficult to live with self &/or other people. The capacity to self reflect & learn is limited and there’s difficulty changing personality (traits) that cause the problems. A personality disorder is an enduring pattern of inner experience and behavior that deviates from the norm. The enduring pattern is inflexible and pervasive across a broad range of personal and social situations. The pattern is stable and of long duration, and its onset can be traced back to early adulthood or adolescence.
What causes Personality Disorders � � � Most experts agree that there is no single cause of personality disorder It is likely to be caused by a combination of factors. genetics – genes inherited may make people more vulnerable, given certain environmental factors (see below) neurotransmitters –neurotransmitters can have a significant effect on mood and behaviour neurobiology – environmental factors – events that happened in a person’s past, i. e. relationship with your family, abuse, lack of validation,
Can Personality Disorders be treated? � � � People with a diagnosis of personality disorder have not, in the past, had enough help from mental health services. These services have been more focussed on mental illnesses like schizophrenia, bipolar disorder. There have been arguments about whether mental health services can offer anything useful to people with personality disorders. Some Personality Disorders are more receptive to treatment. Harm minimisation approach
Do Personality Disorders Change over time? � Yes. � There is evidence that they tend to improve slowly with age. � Antisocial behaviour and impulsiveness, in particular, seem to reduce in your 30 s and 40 s � Why?
Traits or Disorder � Research suggests that personality disorders tend to fall into three groups. � As you read through the descriptions of each type, you may well recognise some aspects of your own personality. � Traits Disorder
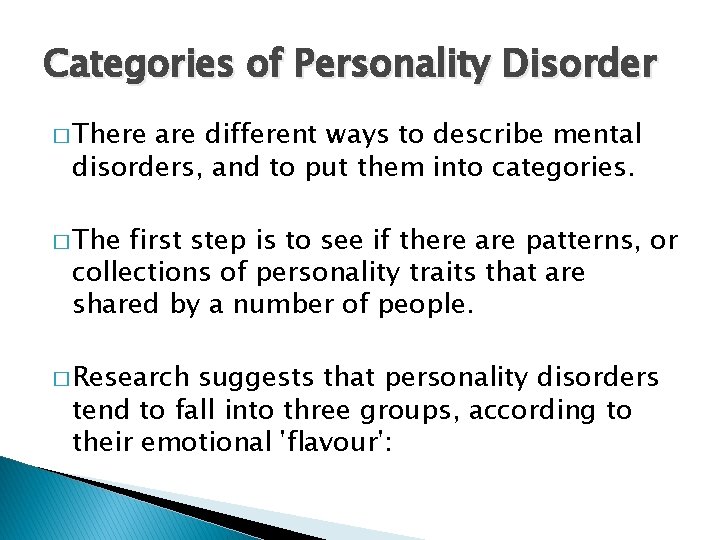
Categories of Personality Disorder � There are different ways to describe mental disorders, and to put them into categories. � The first step is to see if there are patterns, or collections of personality traits that are shared by a number of people. � Research suggests that personality disorders tend to fall into three groups, according to their emotional 'flavour':
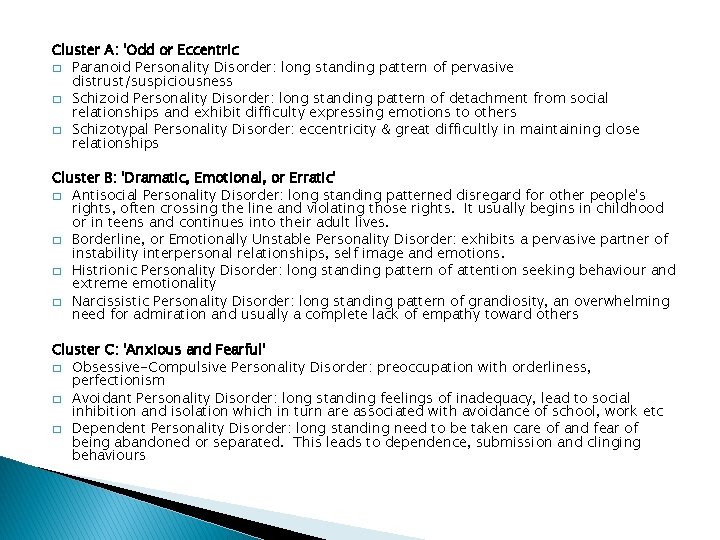
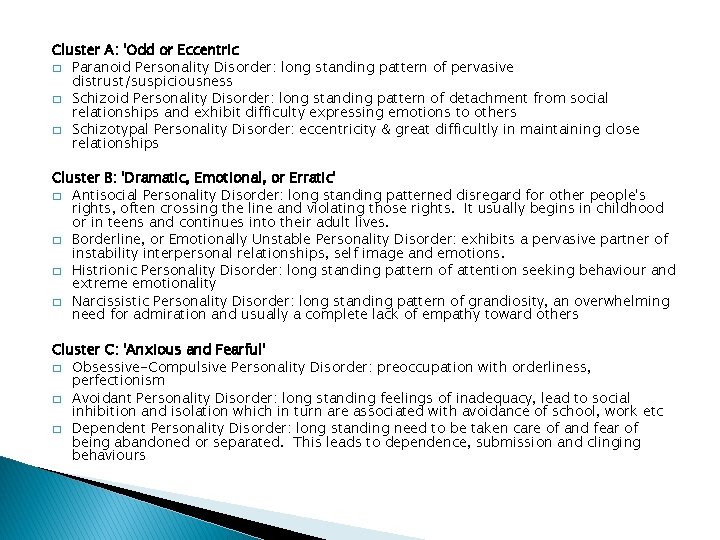
Cluster A: 'Odd or Eccentric � Paranoid Personality Disorder: long standing pattern of pervasive distrust/suspiciousness � Schizoid Personality Disorder: long standing pattern of detachment from social relationships and exhibit difficulty expressing emotions to others � Schizotypal Personality Disorder: eccentricity & great difficultly in maintaining close relationships Cluster B: 'Dramatic, Emotional, or Erratic' � Antisocial Personality Disorder: long standing patterned disregard for other people's rights, often crossing the line and violating those rights. It usually begins in childhood or in teens and continues into their adult lives. � Borderline, or Emotionally Unstable Personality Disorder: exhibits a pervasive partner of instability interpersonal relationships, self image and emotions. � Histrionic Personality Disorder: long standing pattern of attention seeking behaviour and extreme emotionality � Narcissistic Personality Disorder: long standing pattern of grandiosity, an overwhelming need for admiration and usually a complete lack of empathy toward others Cluster C: 'Anxious and Fearful' � Obsessive-Compulsive Personality Disorder: preoccupation with orderliness, perfectionism � Avoidant Personality Disorder: long standing feelings of inadequacy, lead to social inhibition and isolation which in turn are associated with avoidance of school, work etc � Dependent Personality Disorder: long standing need to be taken care of and fear of being abandoned or separated. This leads to dependence, submission and clinging behaviours
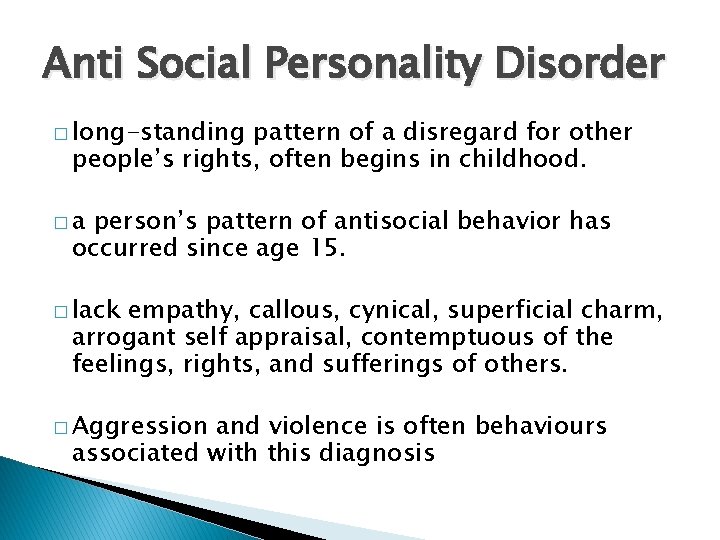
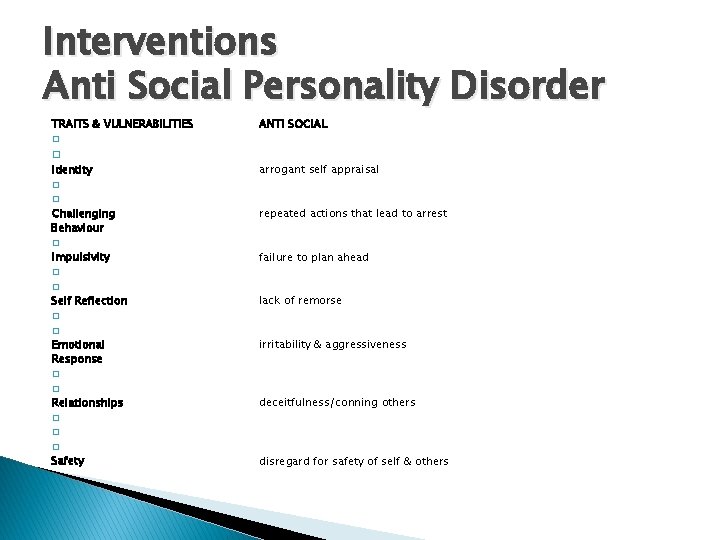
Anti Social Personality Disorder � long-standing pattern of a disregard for other people’s rights, often begins in childhood. �a person’s pattern of antisocial behavior has occurred since age 15. � lack empathy, callous, cynical, superficial charm, arrogant self appraisal, contemptuous of the feelings, rights, and sufferings of others. � Aggression and violence is often behaviours associated with this diagnosis
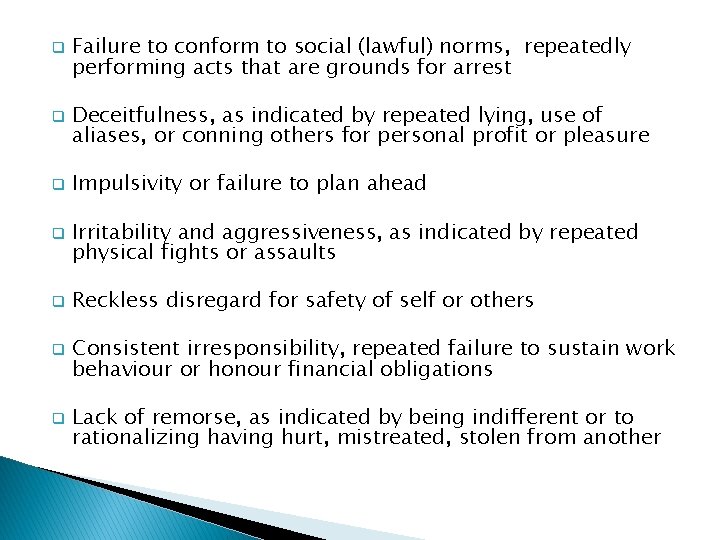
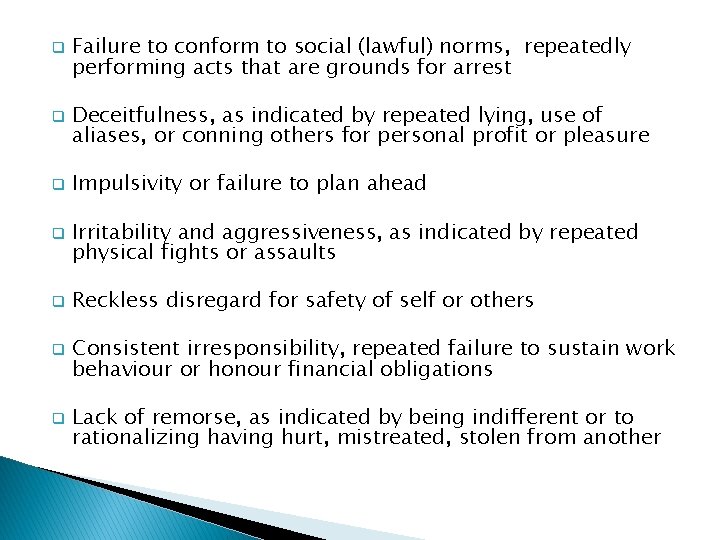
q q q q Failure to conform to social (lawful) norms, repeatedly performing acts that are grounds for arrest Deceitfulness, as indicated by repeated lying, use of aliases, or conning others for personal profit or pleasure Impulsivity or failure to plan ahead Irritability and aggressiveness, as indicated by repeated physical fights or assaults Reckless disregard for safety of self or others Consistent irresponsibility, repeated failure to sustain work behaviour or honour financial obligations Lack of remorse, as indicated by being indifferent or to rationalizing having hurt, mistreated, stolen from another
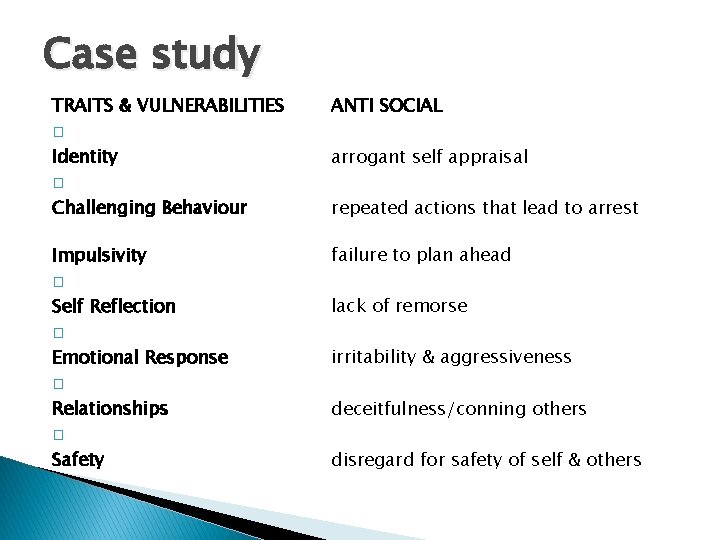
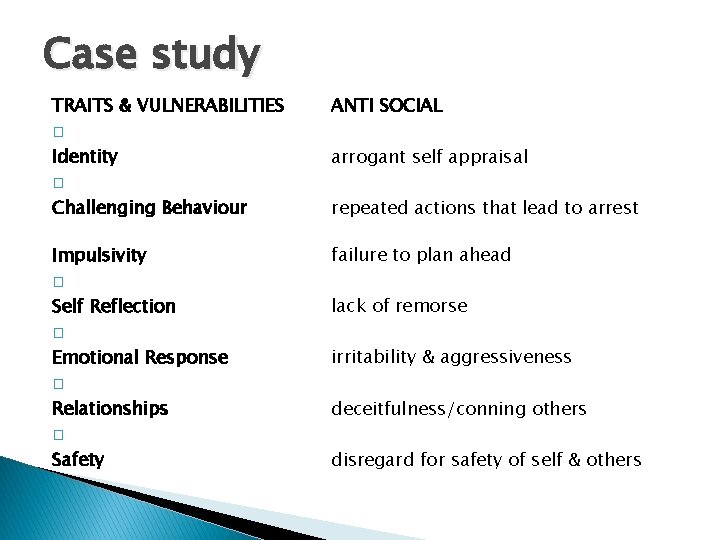
Case study TRAITS & VULNERABILITIES � Identity � Challenging Behaviour ANTI SOCIAL Impulsivity � Self Reflection � Emotional Response � Relationships failure to plan ahead arrogant self appraisal repeated actions that lead to arrest lack of remorse irritability & aggressiveness deceitfulness/conning others � Safety disregard for safety of self & others
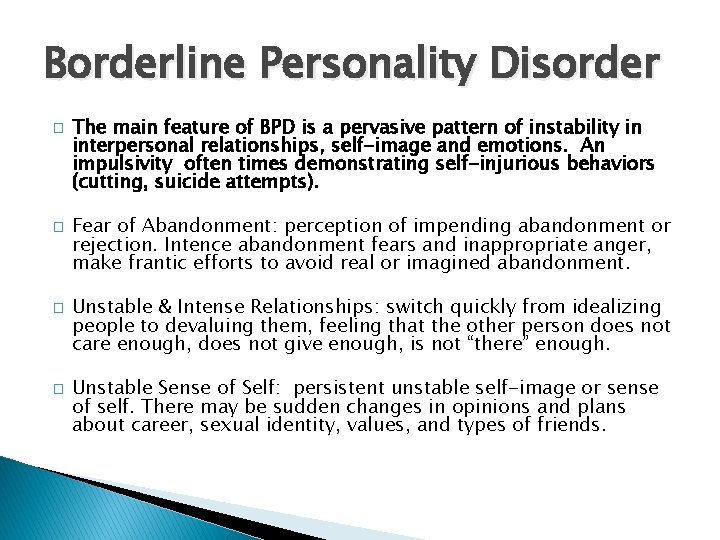
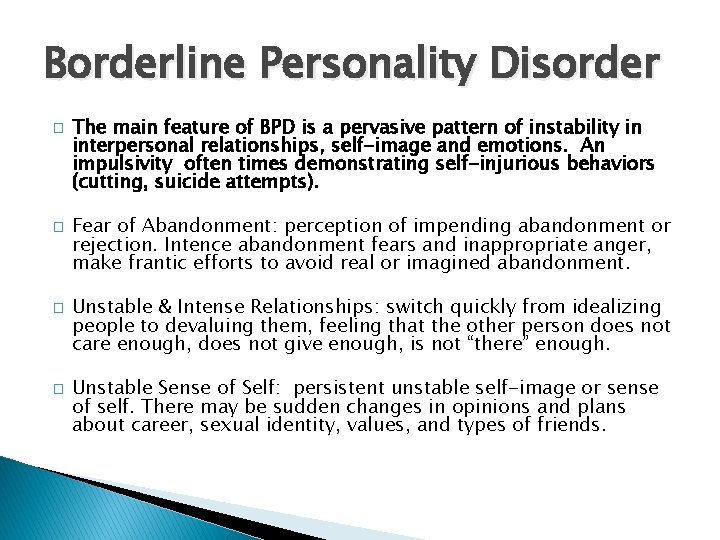
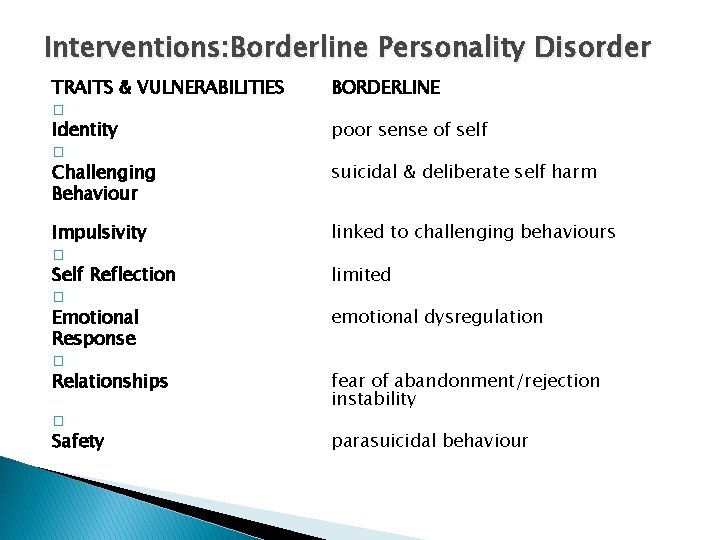
Borderline Personality Disorder � � The main feature of BPD is a pervasive pattern of instability in interpersonal relationships, self-image and emotions. An impulsivity often times demonstrating self-injurious behaviors (cutting, suicide attempts). Fear of Abandonment: perception of impending abandonment or rejection. Intence abandonment fears and inappropriate anger, make frantic efforts to avoid real or imagined abandonment. Unstable & Intense Relationships: switch quickly from idealizing people to devaluing them, feeling that the other person does not care enough, does not give enough, is not “there” enough. Unstable Sense of Self: persistent unstable self-image or sense of self. There may be sudden changes in opinions and plans about career, sexual identity, values, and types of friends.
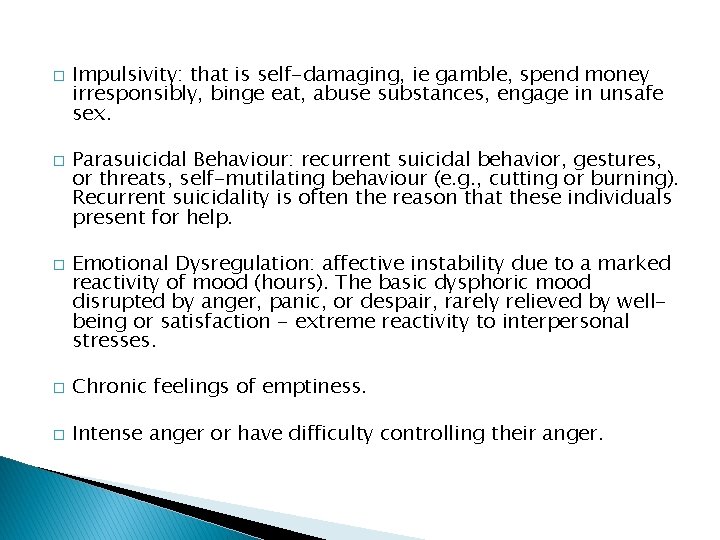
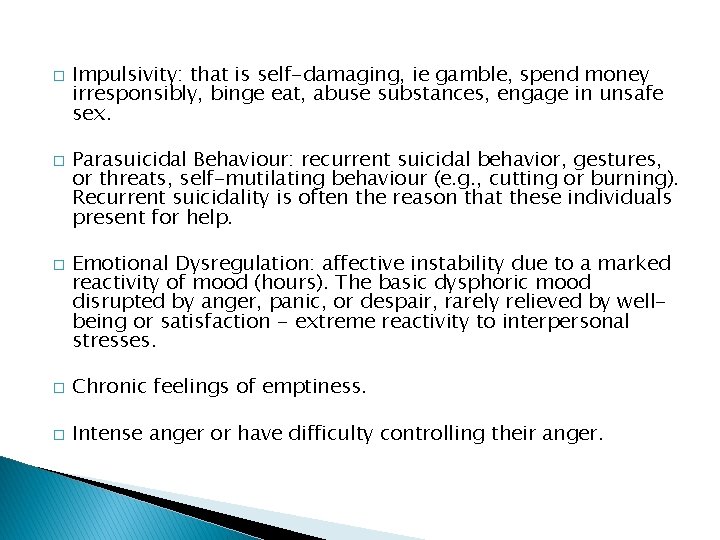
� � � Impulsivity: that is self-damaging, ie gamble, spend money irresponsibly, binge eat, abuse substances, engage in unsafe sex. Parasuicidal Behaviour: recurrent suicidal behavior, gestures, or threats, self-mutilating behaviour (e. g. , cutting or burning). Recurrent suicidality is often the reason that these individuals present for help. Emotional Dysregulation: affective instability due to a marked reactivity of mood (hours). The basic dysphoric mood disrupted by anger, panic, or despair, rarely relieved by wellbeing or satisfaction - extreme reactivity to interpersonal stresses. � Chronic feelings of emptiness. � Intense anger or have difficulty controlling their anger.
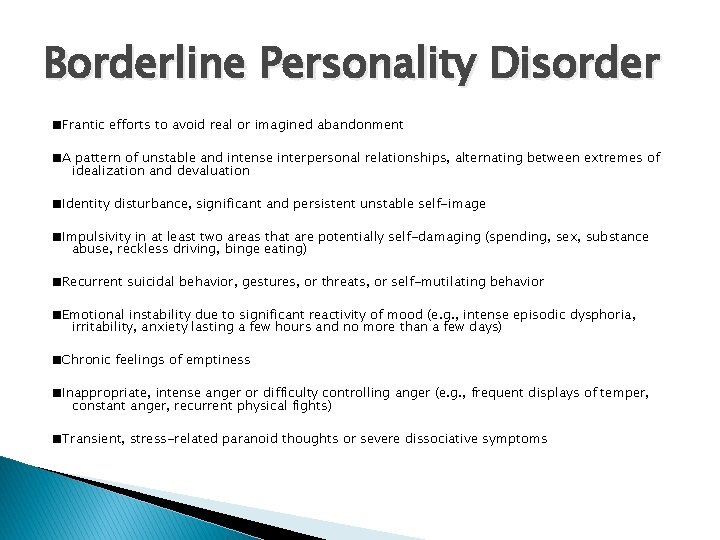
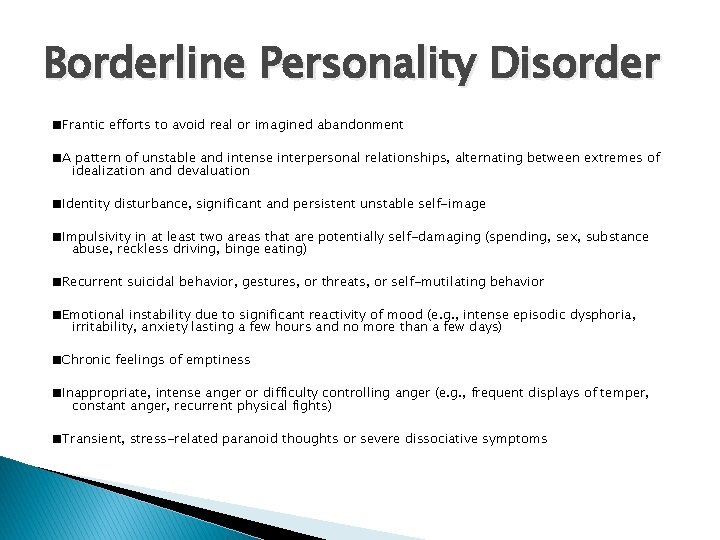
Borderline Personality Disorder ■Frantic efforts to avoid real or imagined abandonment ■A pattern of unstable and intense interpersonal relationships, alternating between extremes of idealization and devaluation ■Identity disturbance, significant and persistent unstable self-image ■Impulsivity in at least two areas that are potentially self-damaging (spending, sex, substance abuse, reckless driving, binge eating) ■Recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior ■Emotional instability due to significant reactivity of mood (e. g. , intense episodic dysphoria, irritability, anxiety lasting a few hours and no more than a few days) ■Chronic feelings of emptiness ■Inappropriate, intense anger or difficulty controlling anger (e. g. , frequent displays of temper, constant anger, recurrent physical fights) ■Transient, stress-related paranoid thoughts or severe dissociative symptoms
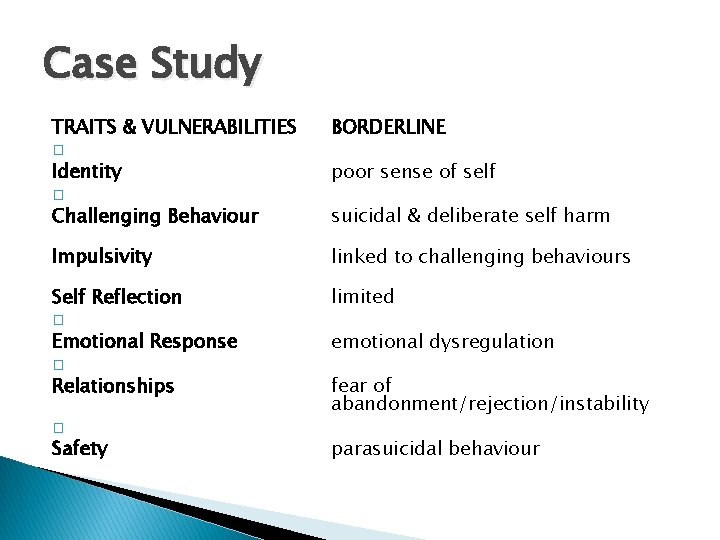
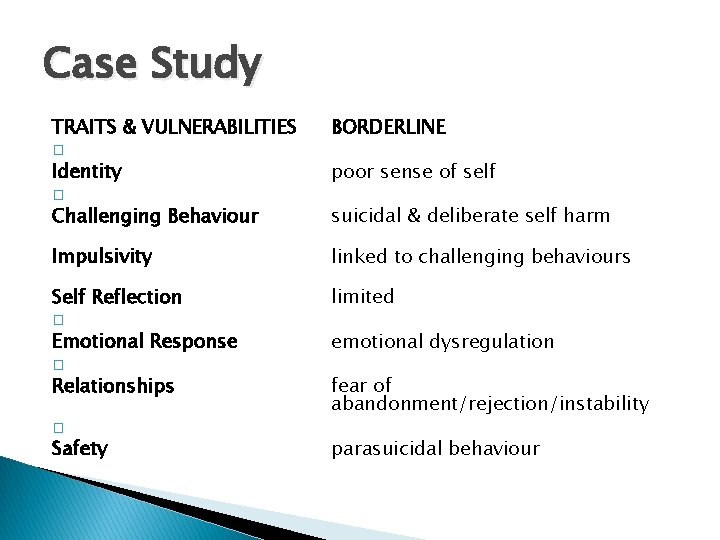
Case Study TRAITS & VULNERABILITIES � Identity � Challenging Behaviour BORDERLINE Impulsivity Self Reflection � Emotional Response � Relationships linked to challenging behaviours Safety � poor sense of self suicidal & deliberate self harm limited emotional dysregulation fear of abandonment/rejection/instability parasuicidal behaviour
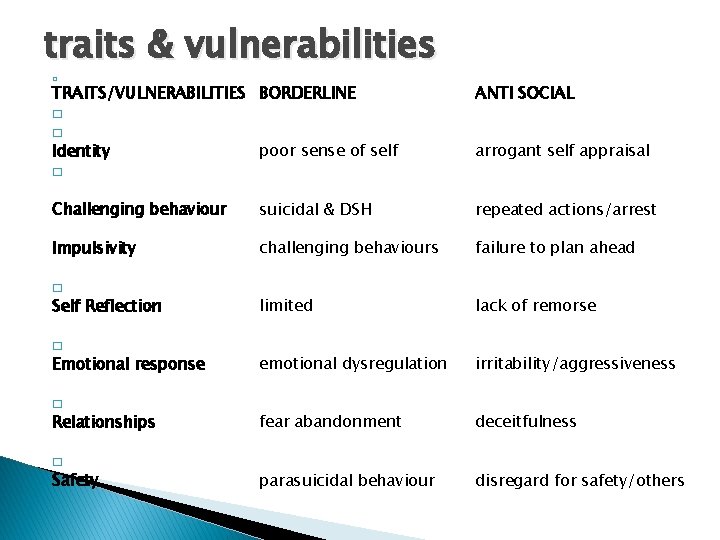
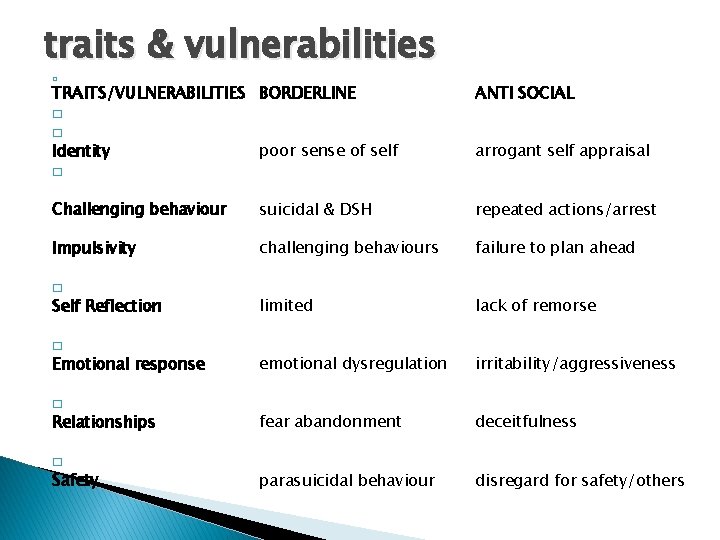
traits & vulnerabilities � TRAITS/VULNERABILITIES BORDERLINE � � Identity poor sense of self � ANTI SOCIAL Challenging behaviour suicidal & DSH repeated actions/arrest Impulsivity challenging behaviours failure to plan ahead Self Reflection limited lack of remorse Emotional response emotional dysregulation irritability/aggressiveness Relationships fear abandonment deceitfulness parasuicidal behaviour disregard for safety/others arrogant self appraisal � � Safety
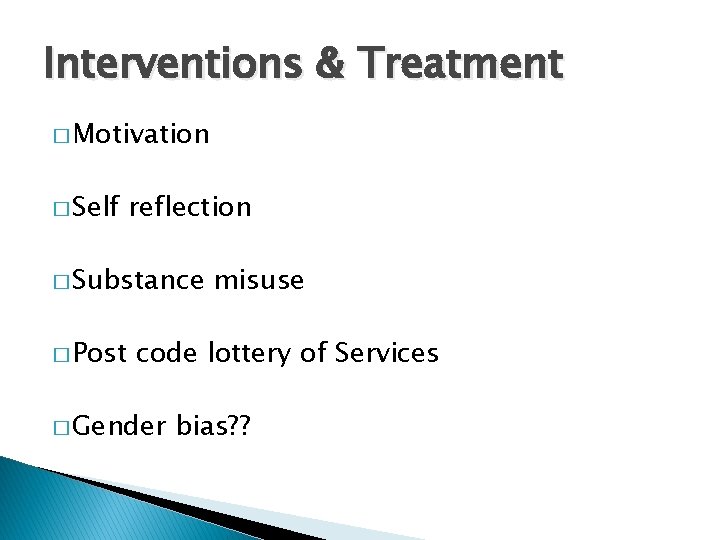
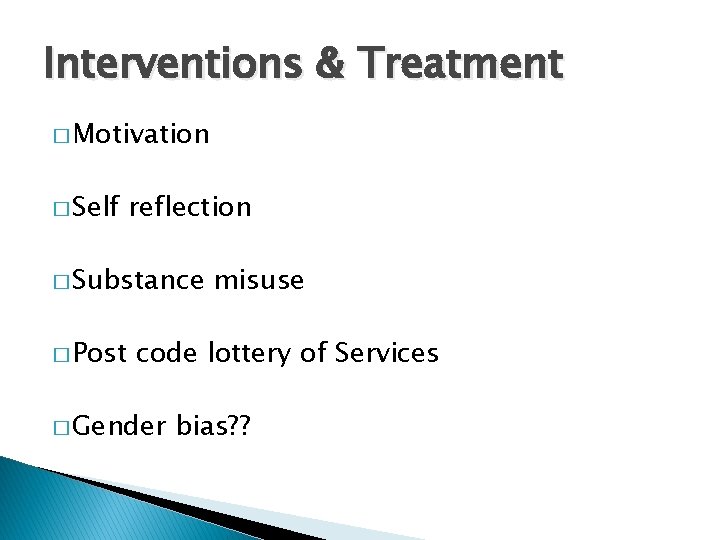
Interventions & Treatment � Motivation � Self reflection � Substance � Post misuse code lottery of Services � Gender bias? ?
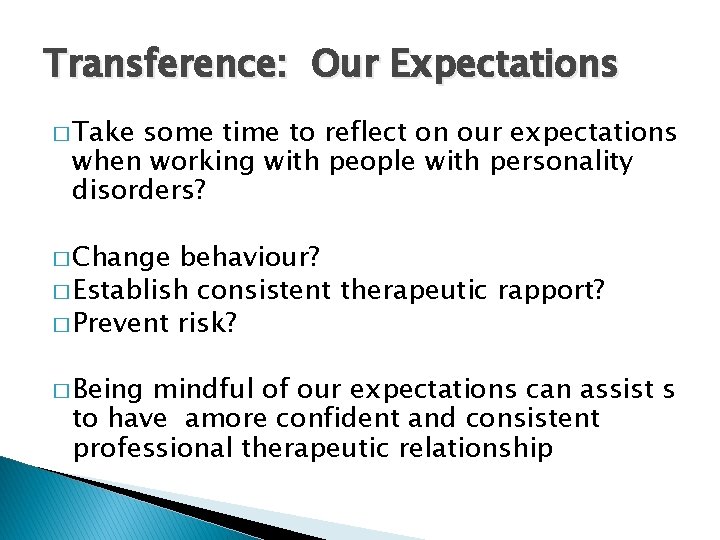
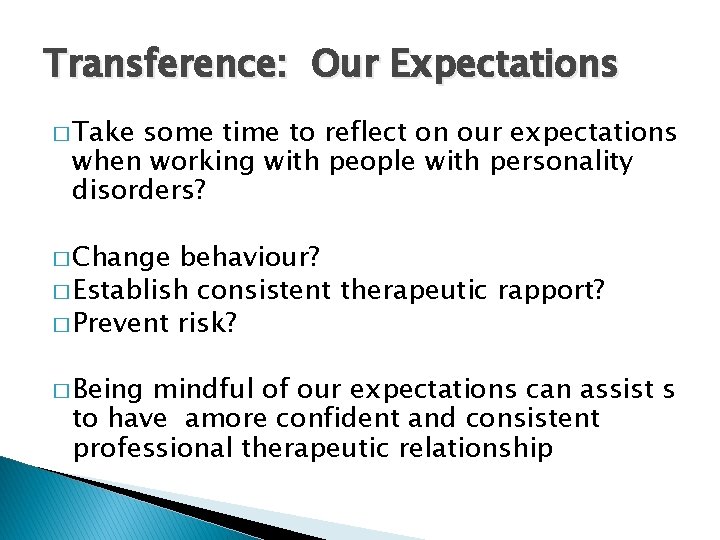
Transference: Our Expectations � Take some time to reflect on our expectations when working with people with personality disorders? � Change behaviour? � Establish consistent therapeutic rapport? � Prevent risk? � Being mindful of our expectations can assist s to have amore confident and consistent professional therapeutic relationship
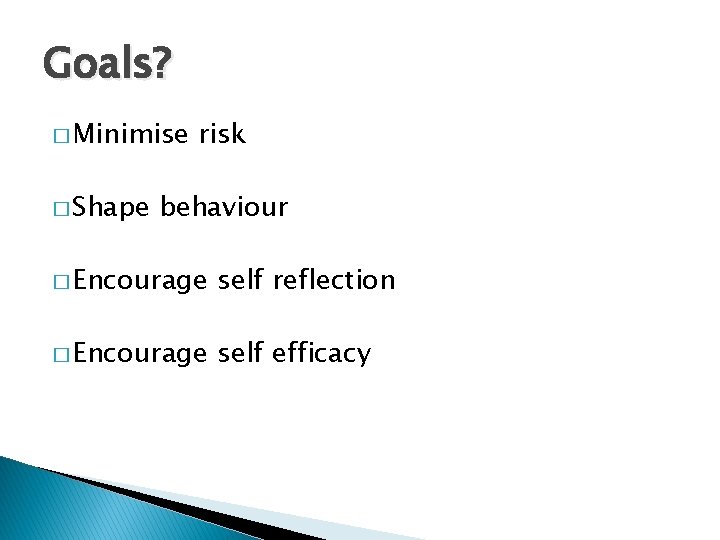
Goals? � Minimise � Shape risk behaviour � Encourage self reflection � Encourage self efficacy
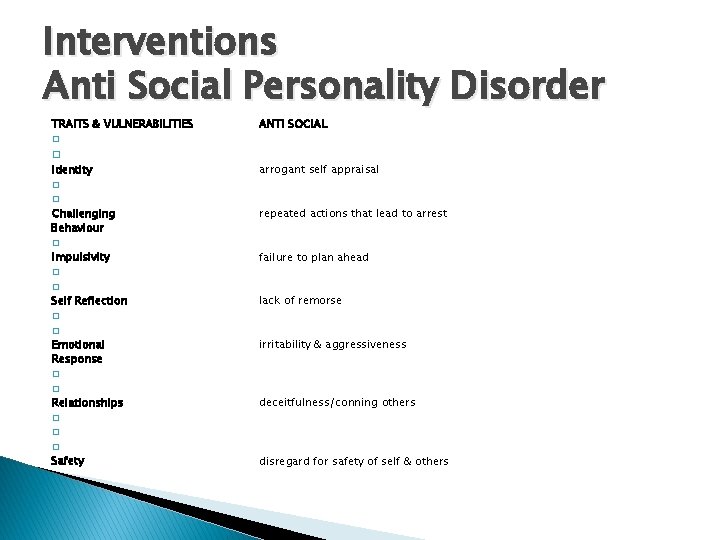
Interventions Anti Social Personality Disorder TRAITS & VULNERABILITIES � � Identity � � Challenging Behaviour � Impulsivity � � Self Reflection � � Emotional Response � � Relationships ANTI SOCIAL arrogant self appraisal repeated actions that lead to arrest failure to plan ahead lack of remorse irritability & aggressiveness deceitfulness/conning others � � Safety � disregard for safety of self & others
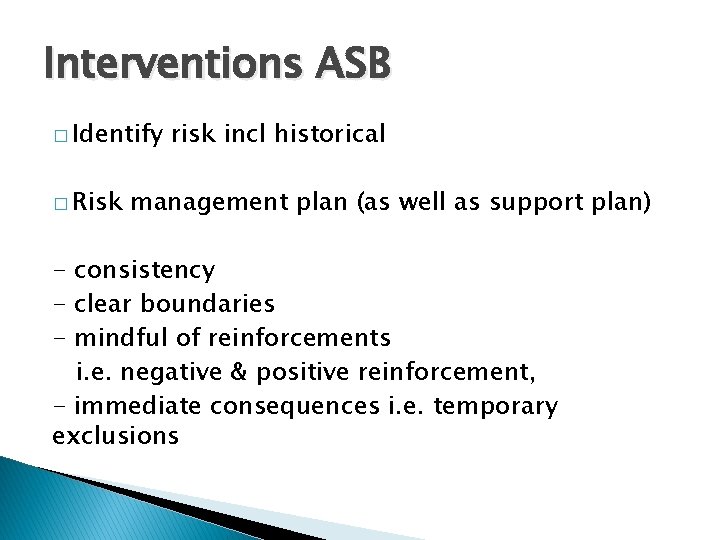
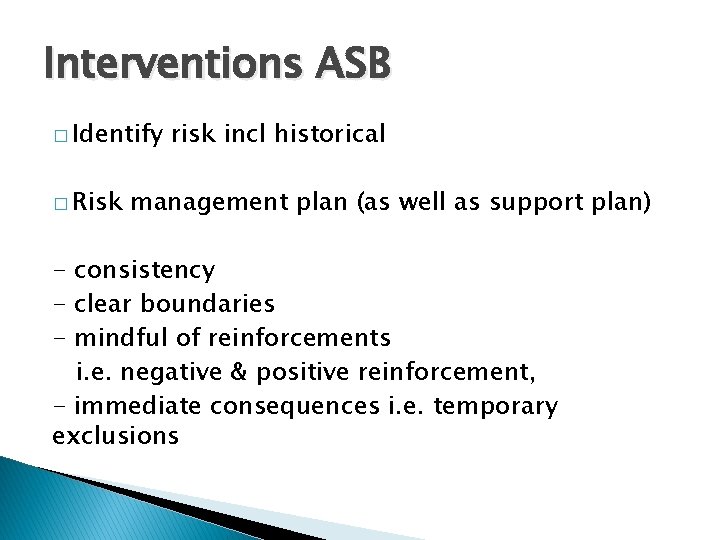
Interventions ASB � Identify � Risk risk incl historical management plan (as well as support plan) - consistency - clear boundaries - mindful of reinforcements i. e. negative & positive reinforcement, - immediate consequences i. e. temporary exclusions
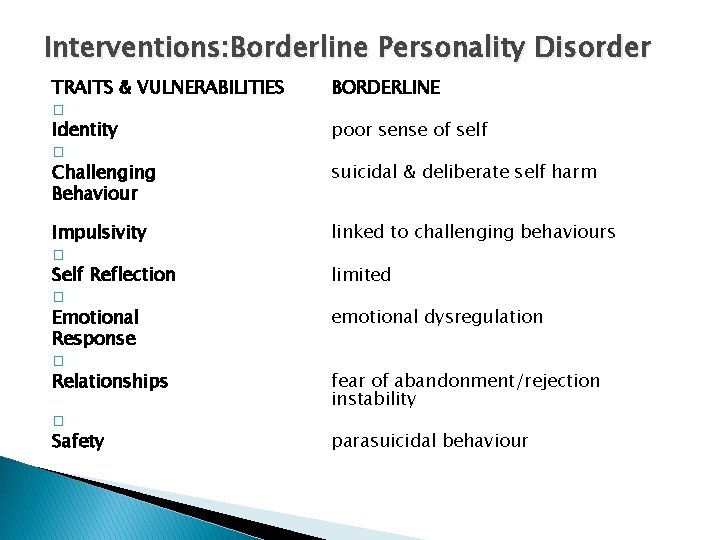
Interventions: Borderline Personality Disorder TRAITS & VULNERABILITIES � Identity � Challenging Behaviour Impulsivity � Self Reflection � Emotional Response � Relationships Safety � BORDERLINE poor sense of self suicidal & deliberate self harm linked to challenging behaviours limited emotional dysregulation fear of abandonment/rejection instability parasuicidal behaviour
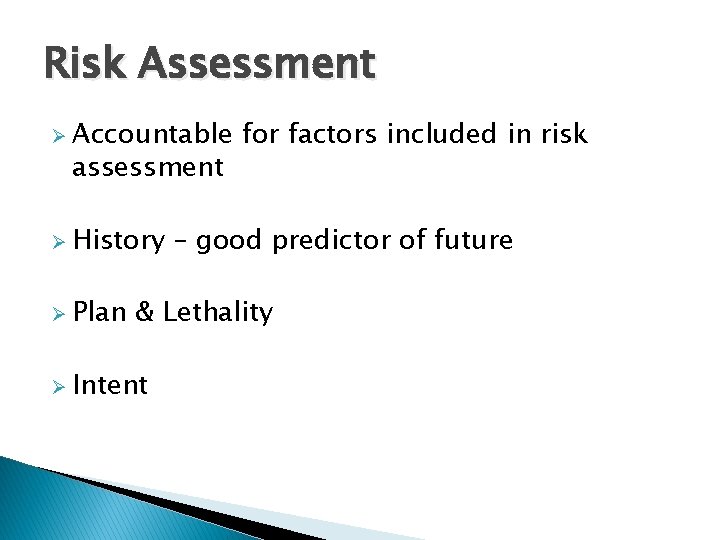
Risk Assessment Ø Accountable assessment Ø History Ø Plan for factors included in risk – good predictor of future & Lethality Ø Intent
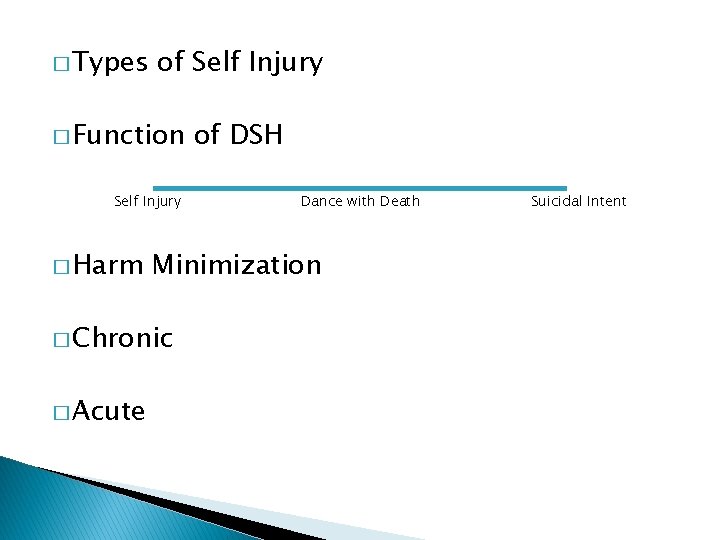
� Types of Self Injury � Function Self Injury � Harm Dance with Death Minimization � Chronic � Acute of DSH Suicidal Intent
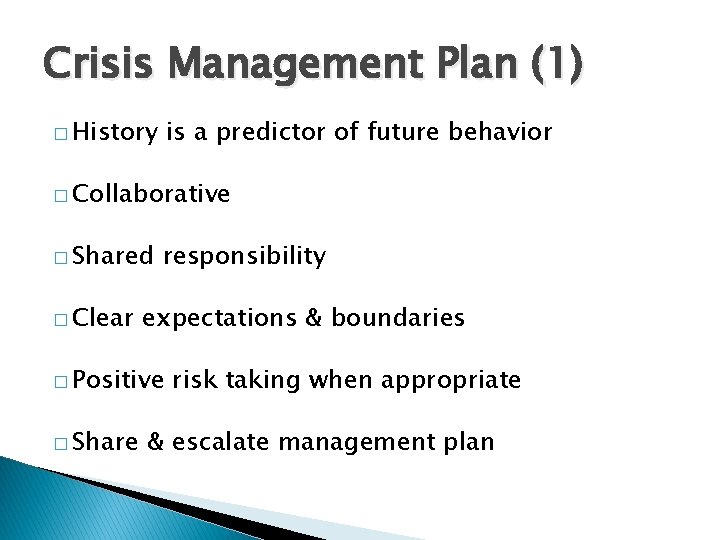
Crisis Management Plan (1) � History is a predictor of future behavior � Collaborative � Shared � Clear responsibility expectations & boundaries � Positive � Share risk taking when appropriate & escalate management plan
Emotional Dysregulation “I cant control myself” “I just react”
Habitual Maladaptive Behaviours � i. e. substance misuse, DSH � Linked � Work � Often to impulsivity in the short term – reinforcement formed at early age – survival � Continue required � No into adult hood when no longer other tools in tool box
communication � Therapeutic relationship � Transference and counter transference issues & most importantly lashings of � Validation & Empathy
interventions DEAL WITH DISTRESS FIRST - Remove from situation - Strategies to reduce distress i. e. distractions ONCE DISTRESS REDUCES THEN DISCUSS ISSUE REFLECTIVE PRAXIS ABC
![Crisis Management Plan 2 When I feel EMOTION and feel like BEHAVIOUR I will Crisis Management Plan (2) When I feel [EMOTION] and feel like [BEHAVIOUR], I will](https://slidetodoc.com/presentation_image/d23e65976041bc1ab68d47b31dcf29a7/image-33.jpg)
Crisis Management Plan (2) When I feel [EMOTION] and feel like [BEHAVIOUR], I will try [INTENSE SENSATIONS] & [DISTRACTIONS] & then I will talk with a staff member. If I still feel very unsafe I will call [EMERGENCY #]
Systemic Change � Consistency � Risk sharing � Reflective practice & supervision
 Conversion disorder
Conversion disorder Cluster b
Cluster b Cluster c
Cluster c Avoidant personality disorder
Avoidant personality disorder Personality disorder types
Personality disorder types Personality disorder
Personality disorder Cluster b personality disorder traits
Cluster b personality disorder traits Borderline personality disorder mnemonic
Borderline personality disorder mnemonic Dsm v personality disorders
Dsm v personality disorders Paranoia disorder
Paranoia disorder Psychology chapter 15
Psychology chapter 15 Cluster b personality disorders
Cluster b personality disorders Group c personality disorders
Group c personality disorders Karla homulka
Karla homulka Cluster b personality disorder
Cluster b personality disorder Weird wild wacky personality disorders
Weird wild wacky personality disorders What causes narcissistic personality disorder
What causes narcissistic personality disorder Emotionally unstable personality disorder
Emotionally unstable personality disorder Traits of avoidant personality disorder
Traits of avoidant personality disorder Type b personality disorder
Type b personality disorder Histrionic vs borderline
Histrionic vs borderline Ineffective impulse control
Ineffective impulse control Schizoid personality disorder
Schizoid personality disorder Histrionic personality disorder
Histrionic personality disorder Sarah skett
Sarah skett Neurotic definition
Neurotic definition Dependent personality disorder
Dependent personality disorder Dsm 5 axis chart
Dsm 5 axis chart Cluster b personlighedsforstyrrelser
Cluster b personlighedsforstyrrelser Parking lot of the personality disordered
Parking lot of the personality disordered Psychological disorders
Psychological disorders Borderline personality disorder test
Borderline personality disorder test Hirarki diagnosis gangguan jiwa
Hirarki diagnosis gangguan jiwa Comorbid adhd and bpd
Comorbid adhd and bpd Obsessive-compulsive personality disorder test
Obsessive-compulsive personality disorder test