Personality disorder in later life Waseem Jerjes Personality
- Slides: 35
Personality disorder in later life Waseem Jerjes
Personality disorder in later life • 81 -year-old refereed from general adult service in 2012 following a deterioration of her mental state. Detained under MHA on older adult mental health ward. • Patient had taken multiple overdoses and has a psychiatric background of anxiety and depression. • During that time she was found wandering partially dressed and barefoot on a traffic island, reported to have written notes that she wanted to join her husband in his grave • Self-neglect, non-compliance, overdose and periods of extreme distress
Personality disorder in later life • Many stressors: sister and husband passed away. She lost her home, dog died. Relationship with 2 of her 3 sons had broken down. • • Experienced feelings of loneliness and rejection Mood instability and poor self-image Bouts of anger - take her anger out on herself Suicidal threats Quick to be angry when her expectations are not met Pervasive psychological dependence on other people. Has difficulty making everyday decisions without an excessive amount of advice and reassurance from others.
Personality disorder in later life • Multiple phone calls every day to CMHT • Secretaries and reception staff • Very personal, inappropriate and rude • Restriction of telephone contact with NHS premises to a maximum of three a day
Psychiatric history • Has been in contact with mental health services for many years • 60 X referrals to mental health services and had 28 X MHA assessments • Formally admitted under MHA 6 times (2012 -2014) • Multiple episodes of intentional overdoses in the past - Paracetamol, Co-Codamol, Diazepam, Zopiclone, Metformin - Most recently at her husband’s grave
Social/personal/family history • Retired, widowed lady, living in supported housing for the last 2 -3 years. • Has 3 sons, only in contact with one of them • Was happily married for 50 years, very close and supportive relationship. Became carer for her husband for 5 years after being diagnosed with vascular dementia. The husband was later transferred to a care home in 2012 and passed away in 2013. • Sister died from terminal cancer recently. • Dog had to be put down recently. • Transferred to sheltered accommodation afterwards.
Personal/family history • Difficult childhood, mother had TB, patient had to look after her, also spent some time in children's homes with her two sisters. Spent some time with her grandmother and other relatives. • More recently has declined residential places as they trigger negative childhood memories
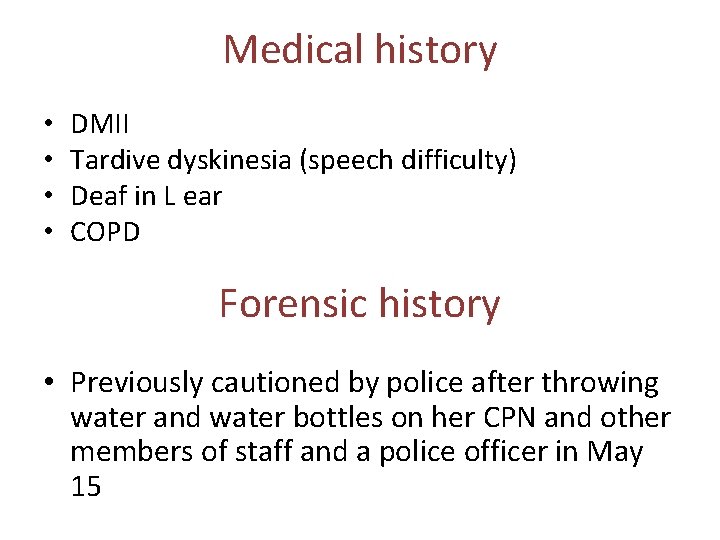
Medical history • • DMII Tardive dyskinesia (speech difficulty) Deaf in L ear COPD Forensic history • Previously cautioned by police after throwing water and water bottles on her CPN and other members of staff and a police officer in May 15
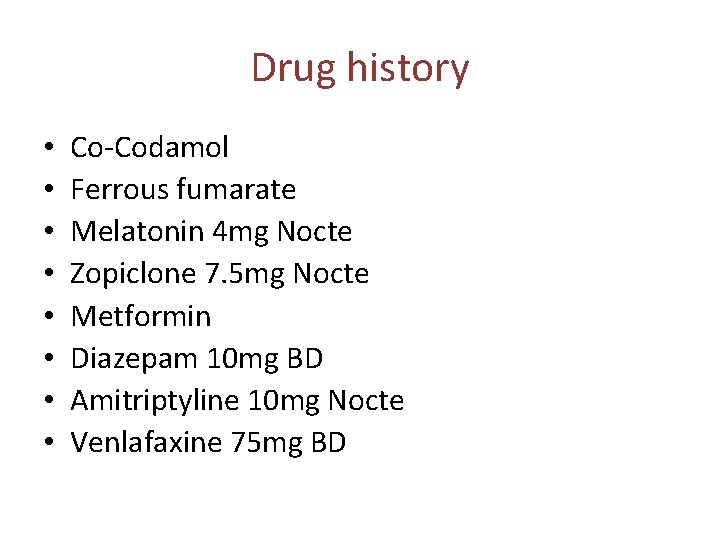
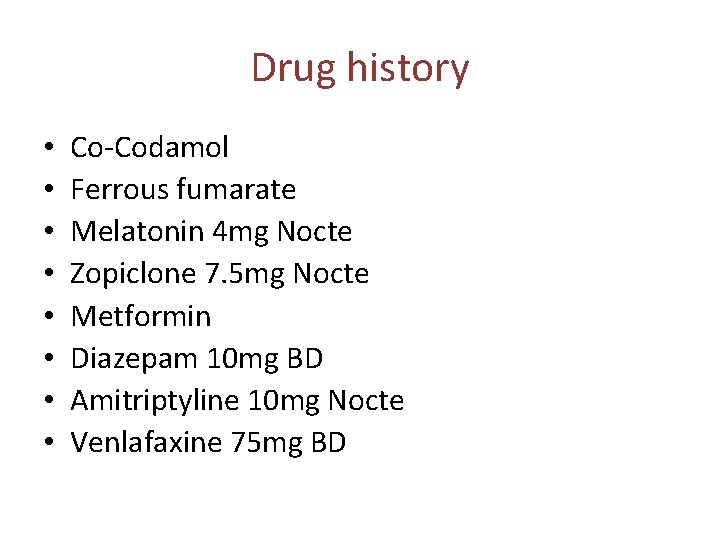
Drug history • • Co-Codamol Ferrous fumarate Melatonin 4 mg Nocte Zopiclone 7. 5 mg Nocte Metformin Diazepam 10 mg BD Amitriptyline 10 mg Nocte Venlafaxine 75 mg BD
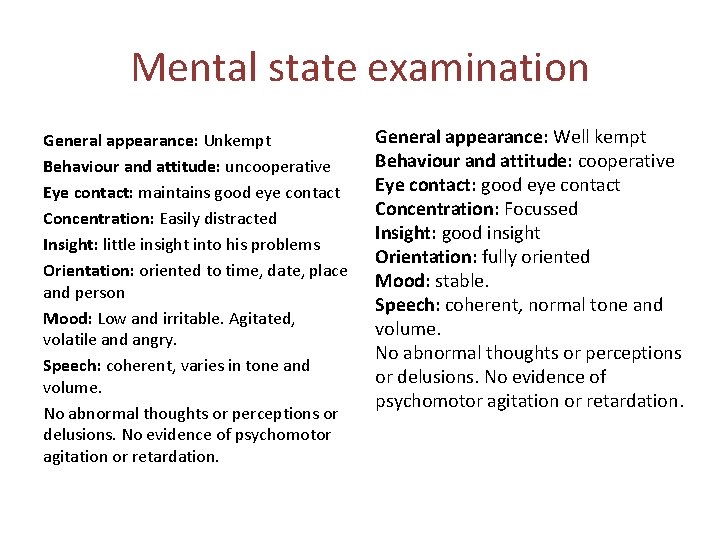
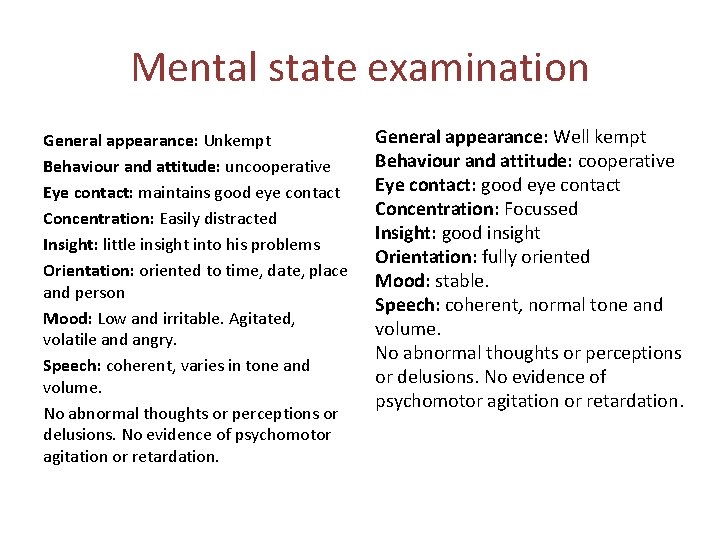
Mental state examination General appearance: Unkempt Behaviour and attitude: uncooperative Eye contact: maintains good eye contact Concentration: Easily distracted Insight: little insight into his problems Orientation: oriented to time, date, place and person Mood: Low and irritable. Agitated, volatile and angry. Speech: coherent, varies in tone and volume. No abnormal thoughts or perceptions or delusions. No evidence of psychomotor agitation or retardation. General appearance: Well kempt Behaviour and attitude: cooperative Eye contact: good eye contact Concentration: Focussed Insight: good insight Orientation: fully oriented Mood: stable. Speech: coherent, normal tone and volume. No abnormal thoughts or perceptions or delusions. No evidence of psychomotor agitation or retardation.
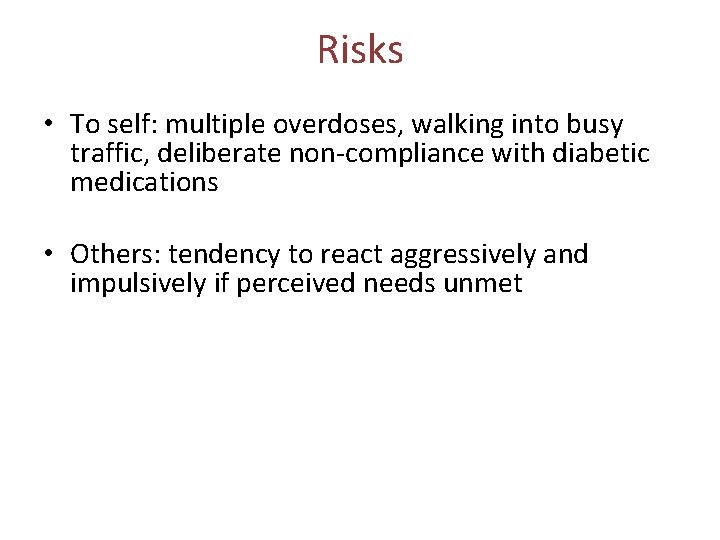
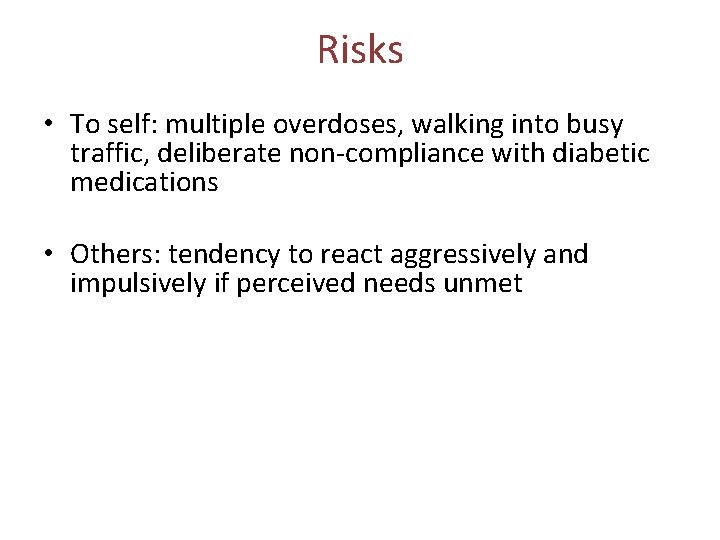
Risks • To self: multiple overdoses, walking into busy traffic, deliberate non-compliance with diabetic medications • Others: tendency to react aggressively and impulsively if perceived needs unmet
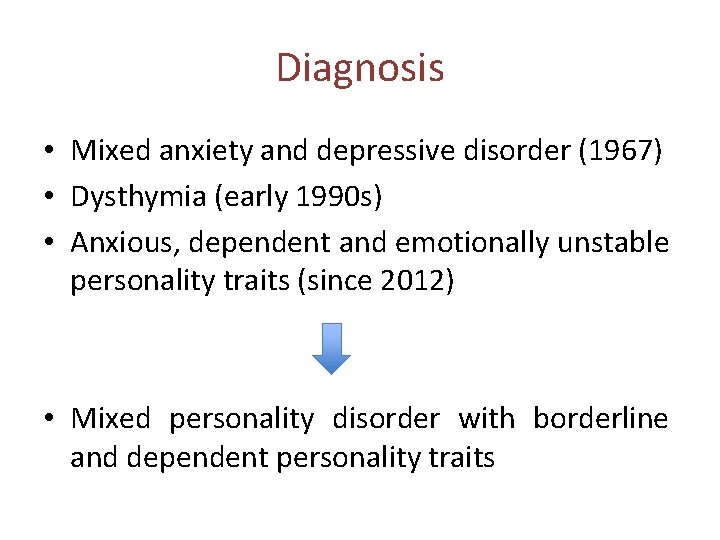
Diagnosis • Mixed anxiety and depressive disorder (1967) • Dysthymia (early 1990 s) • Anxious, dependent and emotionally unstable personality traits (since 2012) • Mixed personality disorder with borderline and dependent personality traits
Diagnosis and management • Current care plan - Has a CPN who she sees once a fortnight for an hour - Planned telephone call every 2 weeks from her CPN - Permitted 3 telephone calls a day to the CMHT (previously numerous calls per day blocking access to others) - OPC appointment with Consultant every 3 months
Personality · Personality is a unique and long-term pattern of inner experience and outward behavior · Tends to be consistent and is often described in terms of “traits” · Also flexible, allowing us to learn and adapt to new environments …. for those with personality disorders
Personality disorder • An enduring, rigid pattern of inner experience and outward behavior that impairs sense of self, emotional experience, goals, and capacity for empathy and/or intimacy • The rigid traits of people with personality disorders often lead to psychological pain for the individual or others
Recognizable personality disorders · Typically becomes recognizable in adolescence or early adulthood and symptoms last for years · Among the most difficult psychological disorders to treat · Many sufferers are not even aware of it · High comorbidity: complicates a person’s chances for a successful recovery from other psychological problems
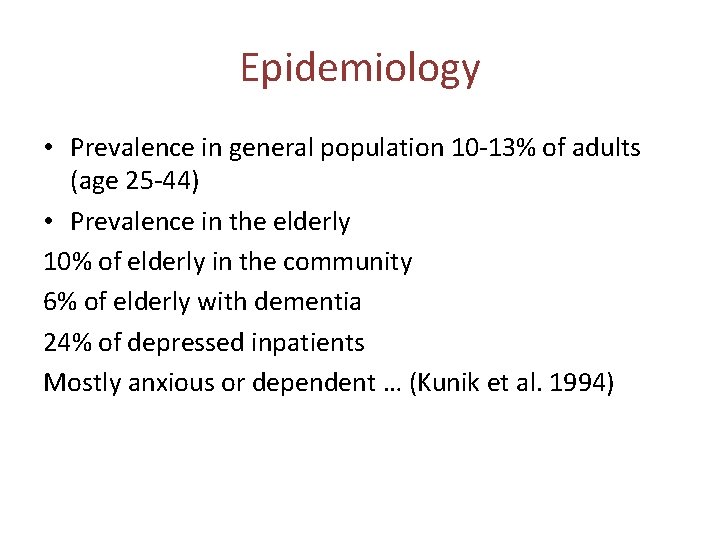
Epidemiology • Prevalence in general population 10 -13% of adults (age 25 -44) • Prevalence in the elderly 10% of elderly in the community 6% of elderly with dementia 24% of depressed inpatients Mostly anxious or dependent … (Kunik et al. 1994)
Modes of presentation in elderly • • Social withdrawal Behavioural problems Poor compliance Self-neglect … (Rosenthal et al. 1999) • • Harm to self or others Anxiety/depression Somatisation Substance misuse … (Speer and Bates 1992)
Classifying personality disorder · The DSM-5 identifies ten personality disorders and separates these into three groups or “clusters”: · Odd or eccentric behavior · Paranoid, schizoid, and schizotypal · Dramatic, emotional, or erratic behavior · Antisocial, borderline, histrionic, and narcissistic · Anxious or fearful behavior · Avoidant, dependent, and obsessive-compulsive
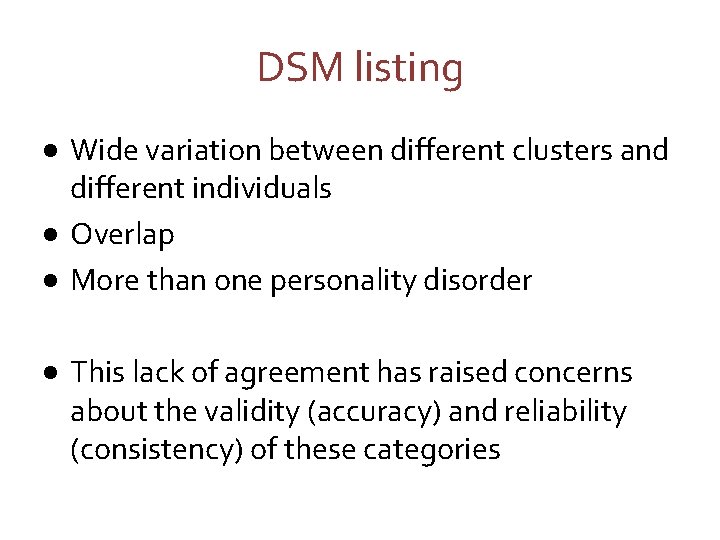
DSM listing · Wide variation between different clusters and different individuals · Overlap · More than one personality disorder · This lack of agreement has raised concerns about the validity (accuracy) and reliability (consistency) of these categories
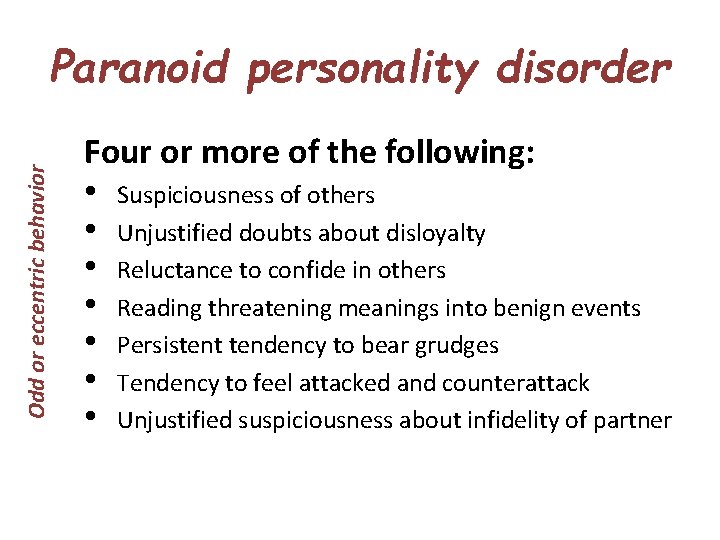
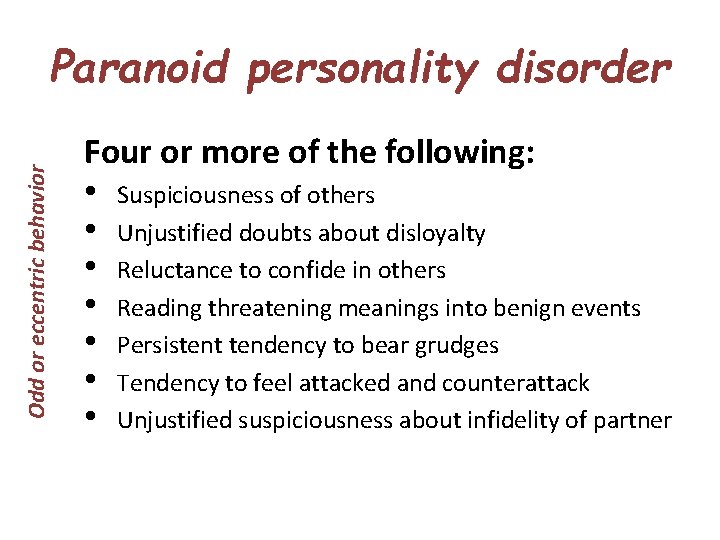
Odd or eccentric behavior Paranoid personality disorder Four or more of the following: • Suspiciousness of others • Unjustified doubts about disloyalty • Reluctance to confide in others • Reading threatening meanings into benign events • Persistent tendency to bear grudges • Tendency to feel attacked and counterattack • Unjustified suspiciousness about infidelity of partner
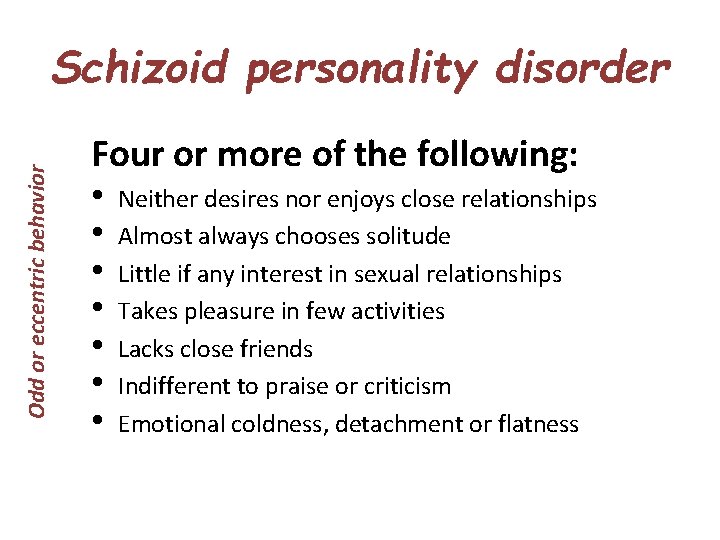
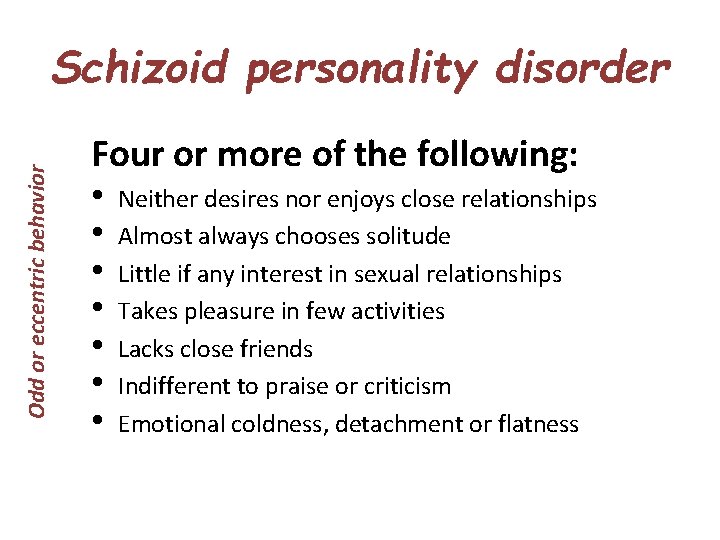
Odd or eccentric behavior Schizoid personality disorder Four or more of the following: • • Neither desires nor enjoys close relationships Almost always chooses solitude Little if any interest in sexual relationships Takes pleasure in few activities Lacks close friends Indifferent to praise or criticism Emotional coldness, detachment or flatness
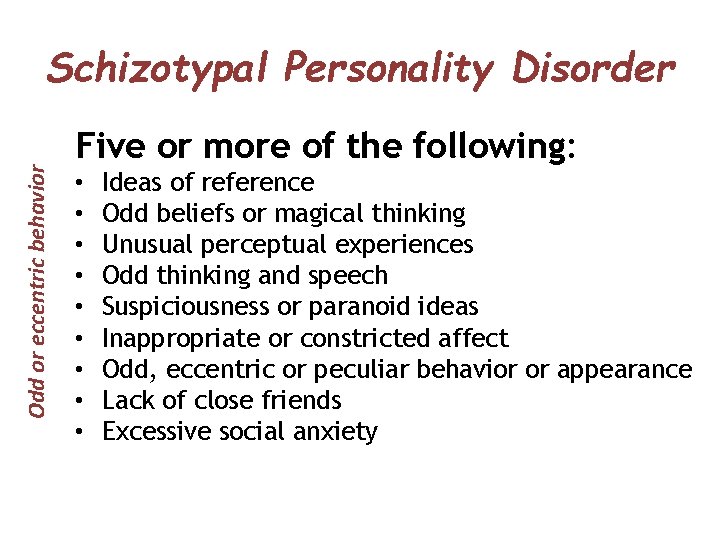
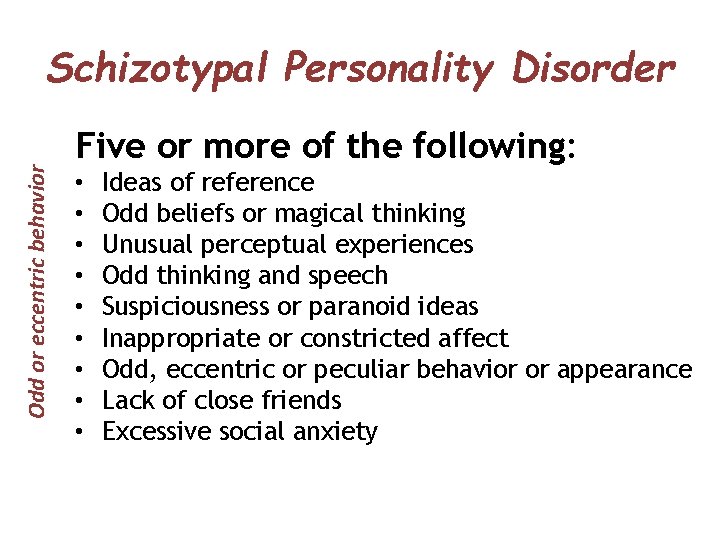
Odd or eccentric behavior Schizotypal Personality Disorder Five or more of the following: • • • Ideas of reference Odd beliefs or magical thinking Unusual perceptual experiences Odd thinking and speech Suspiciousness or paranoid ideas Inappropriate or constricted affect Odd, eccentric or peculiar behavior or appearance Lack of close friends Excessive social anxiety
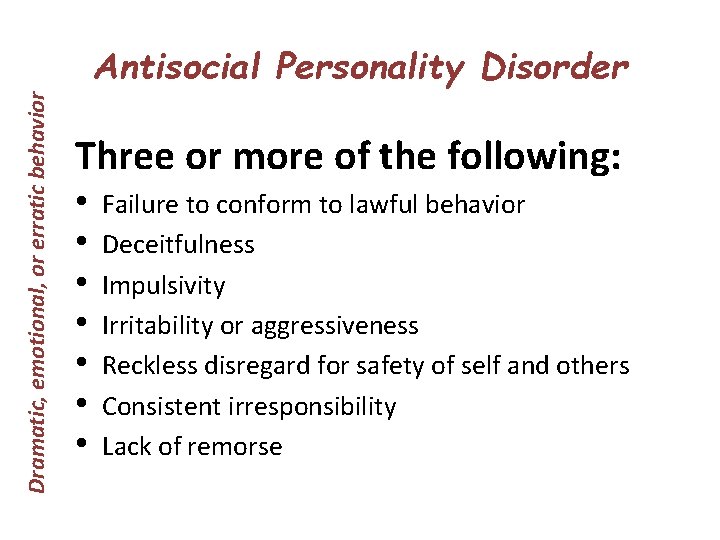
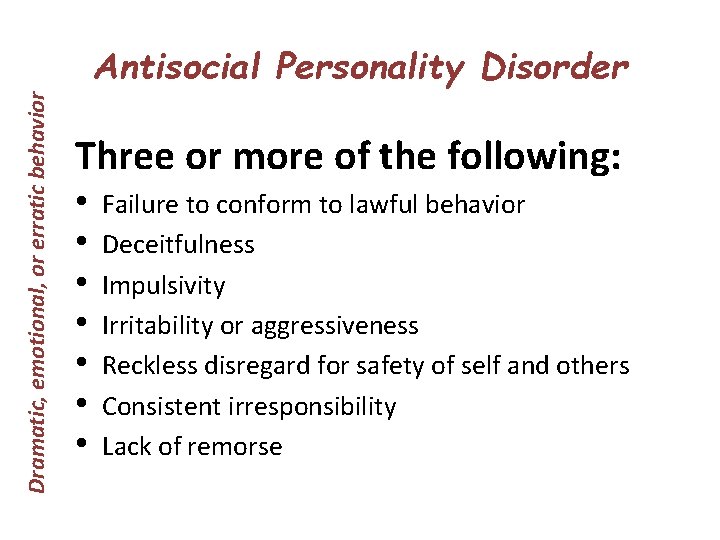
Dramatic, emotional, or erratic behavior Antisocial Personality Disorder Three or more of the following: • • Failure to conform to lawful behavior Deceitfulness Impulsivity Irritability or aggressiveness Reckless disregard for safety of self and others Consistent irresponsibility Lack of remorse
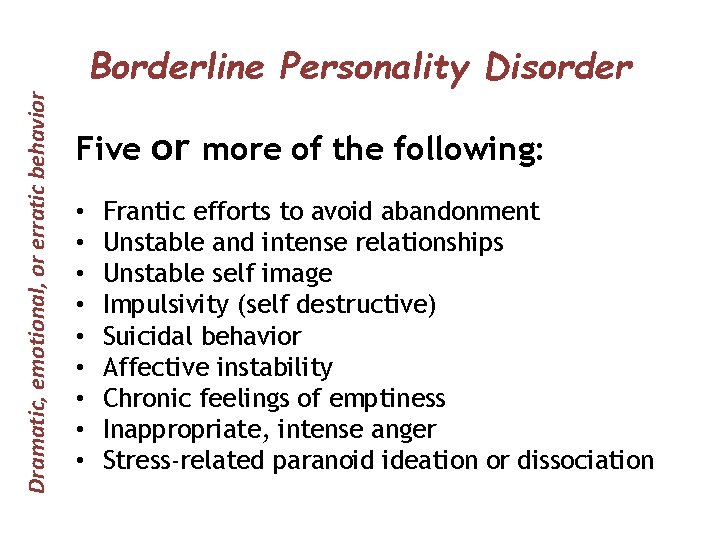
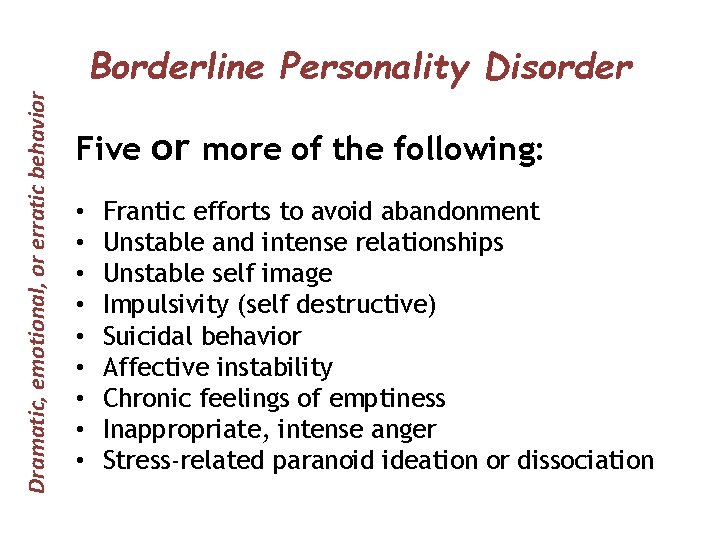
Dramatic, emotional, or erratic behavior Borderline Personality Disorder Five or more of the following: • • • Frantic efforts to avoid abandonment Unstable and intense relationships Unstable self image Impulsivity (self destructive) Suicidal behavior Affective instability Chronic feelings of emptiness Inappropriate, intense anger Stress-related paranoid ideation or dissociation
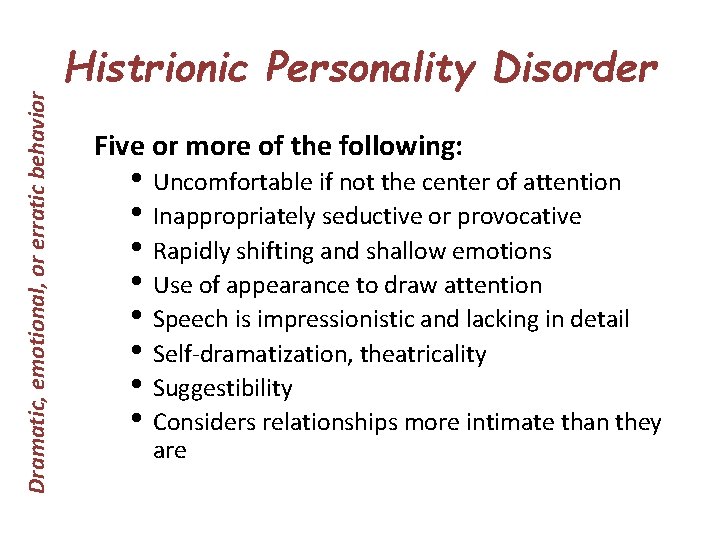
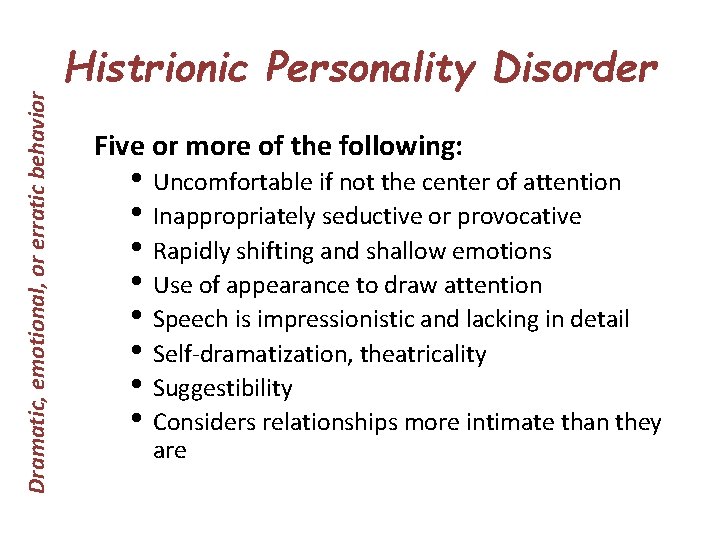
Dramatic, emotional, or erratic behavior Histrionic Personality Disorder Five or more of the following: • Uncomfortable if not the center of attention • Inappropriately seductive or provocative • Rapidly shifting and shallow emotions • Use of appearance to draw attention • Speech is impressionistic and lacking in detail • Self-dramatization, theatricality • Suggestibility • Considers relationships more intimate than they are
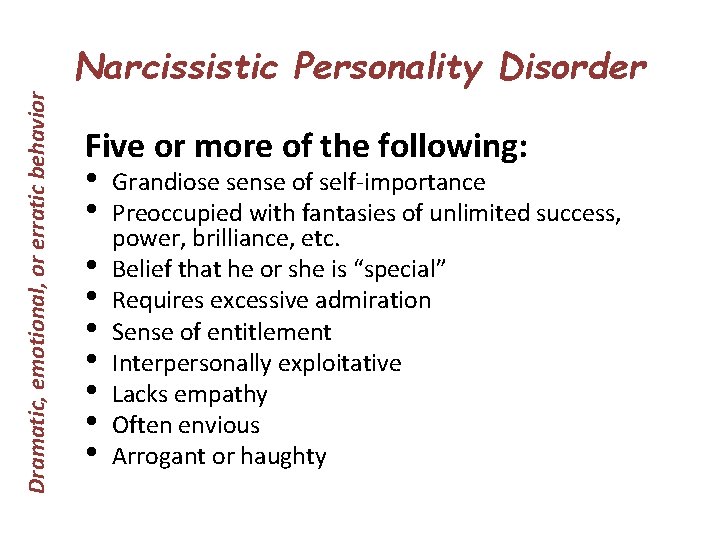
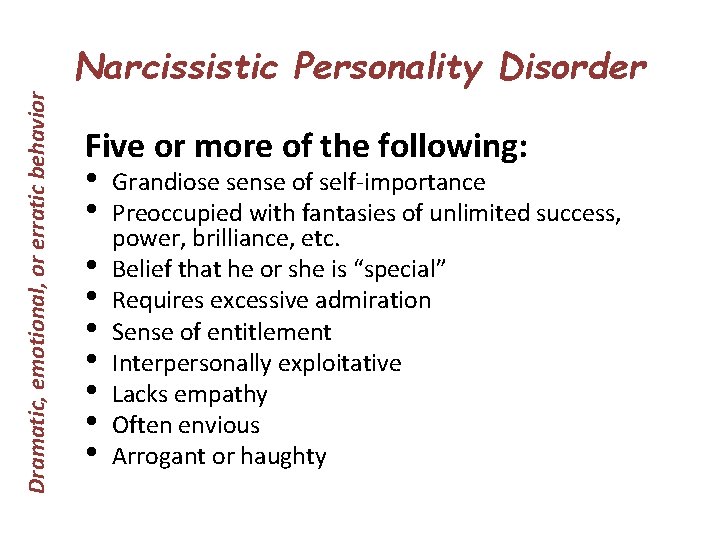
Dramatic, emotional, or erratic behavior Narcissistic Personality Disorder Five or more of the following: • Grandiose sense of self-importance • Preoccupied with fantasies of unlimited success, • • power, brilliance, etc. Belief that he or she is “special” Requires excessive admiration Sense of entitlement Interpersonally exploitative Lacks empathy Often envious Arrogant or haughty
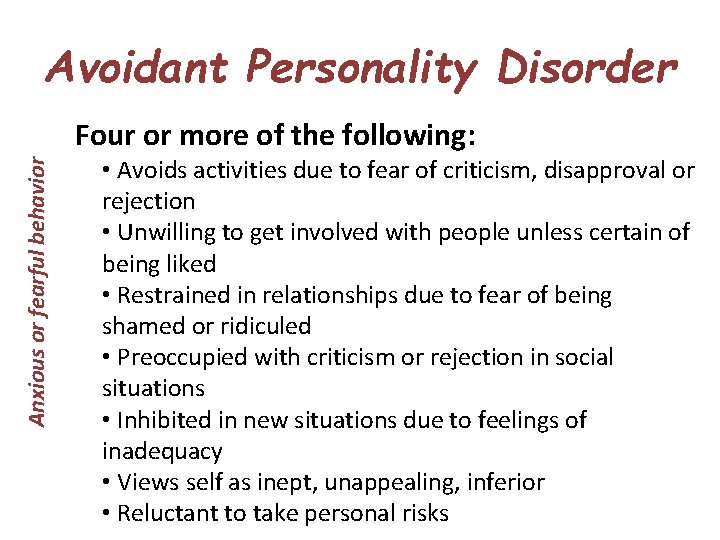
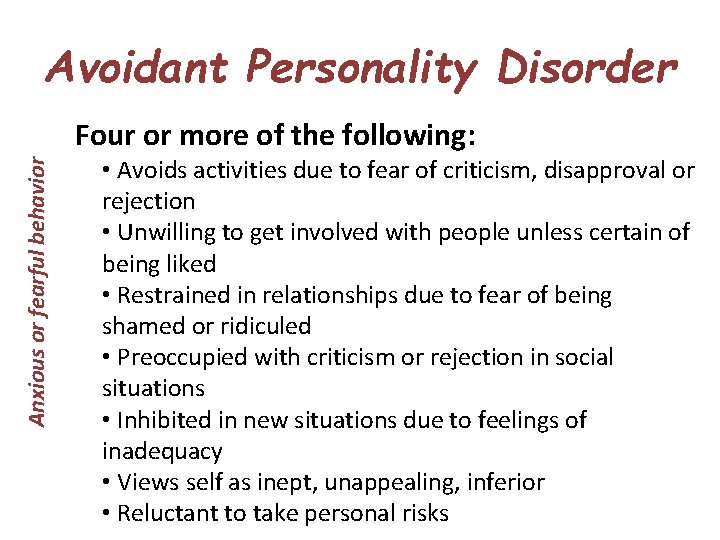
Avoidant Personality Disorder Anxious or fearful behavior Four or more of the following: • Avoids activities due to fear of criticism, disapproval or rejection • Unwilling to get involved with people unless certain of being liked • Restrained in relationships due to fear of being shamed or ridiculed • Preoccupied with criticism or rejection in social situations • Inhibited in new situations due to feelings of inadequacy • Views self as inept, unappealing, inferior • Reluctant to take personal risks
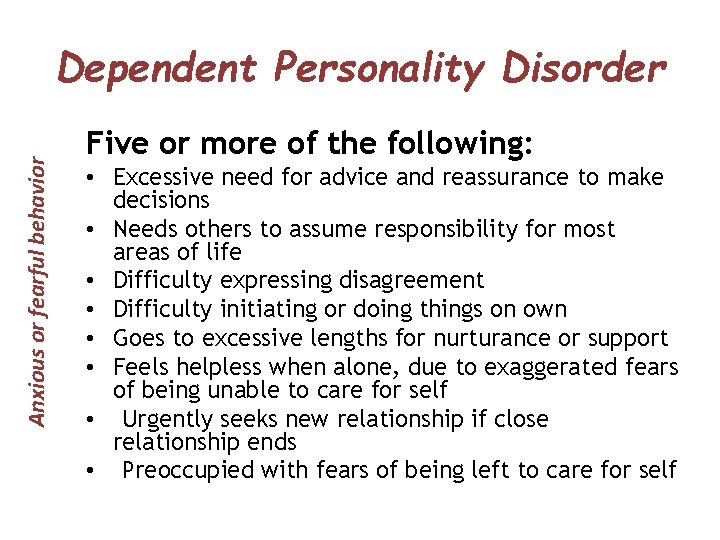
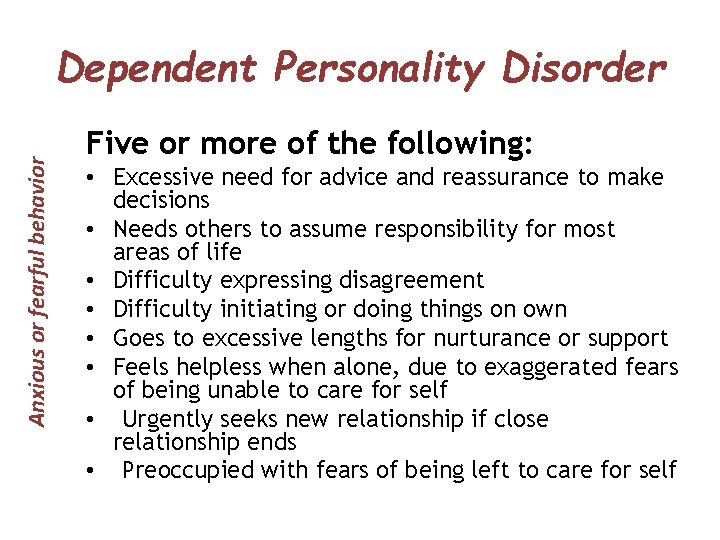
Anxious or fearful behavior Dependent Personality Disorder Five or more of the following: • Excessive need for advice and reassurance to make decisions • Needs others to assume responsibility for most areas of life • Difficulty expressing disagreement • Difficulty initiating or doing things on own • Goes to excessive lengths for nurturance or support • Feels helpless when alone, due to exaggerated fears of being unable to care for self • Urgently seeks new relationship if close relationship ends • Preoccupied with fears of being left to care for self
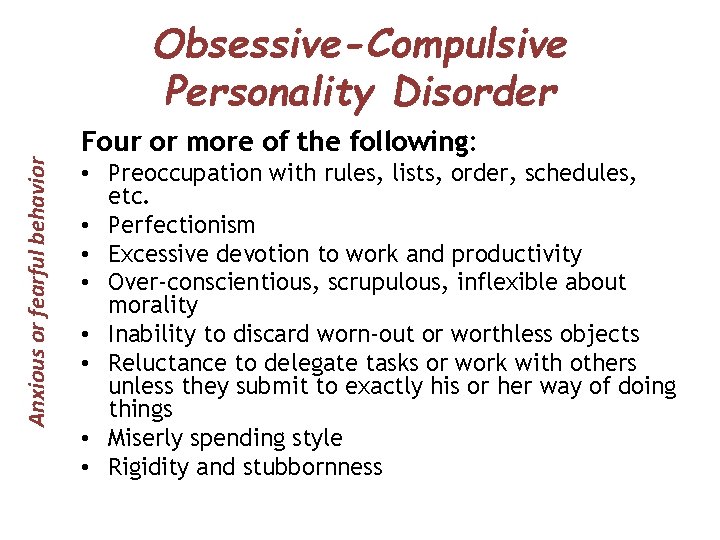
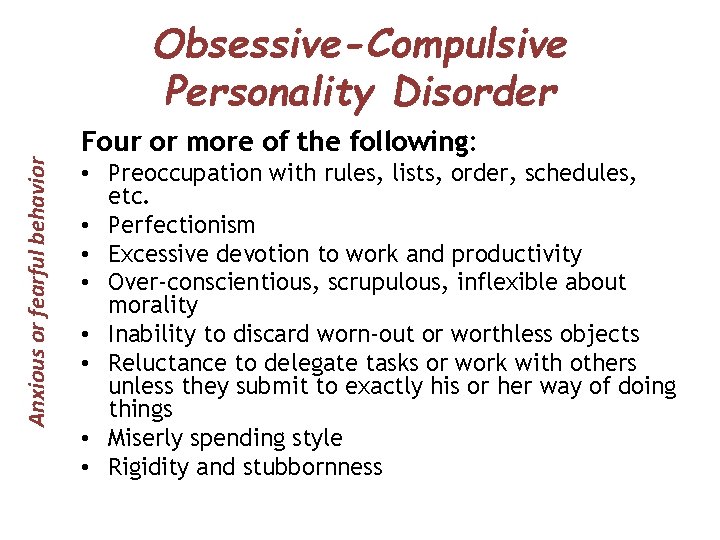
Anxious or fearful behavior Obsessive-Compulsive Personality Disorder Four or more of the following: • Preoccupation with rules, lists, order, schedules, etc. • Perfectionism • Excessive devotion to work and productivity • Over-conscientious, scrupulous, inflexible about morality • Inability to discard worn-out or worthless objects • Reluctance to delegate tasks or work with others unless they submit to exactly his or her way of doing things • Miserly spending style • Rigidity and stubbornness
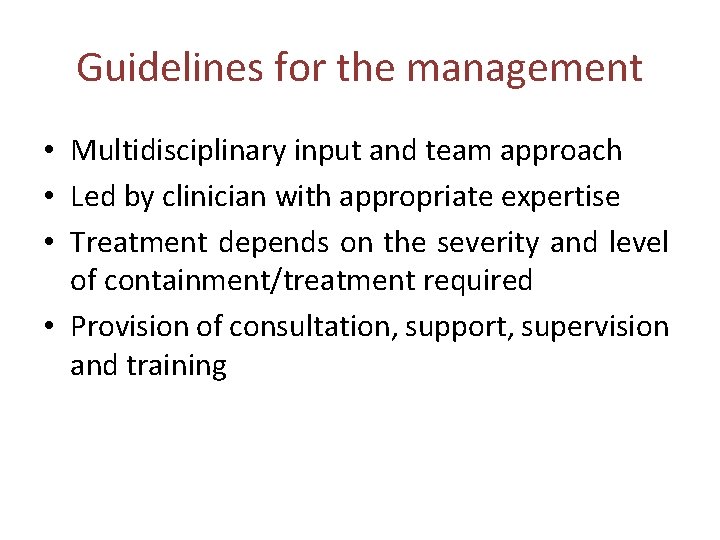
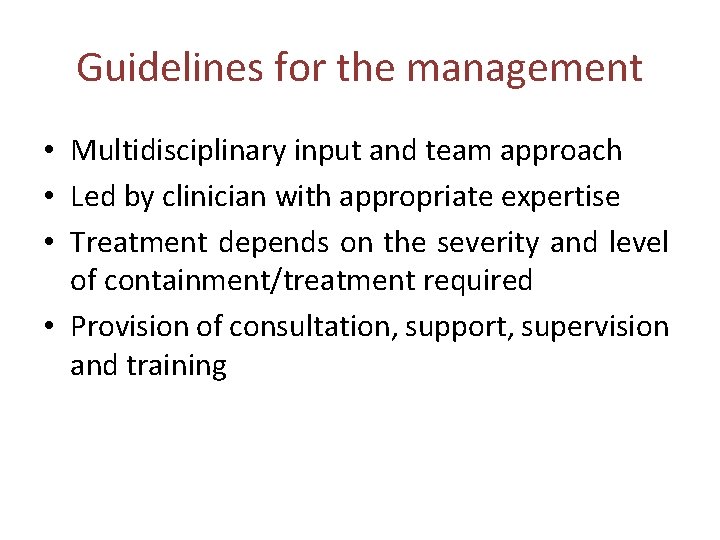
Guidelines for the management • Multidisciplinary input and team approach • Led by clinician with appropriate expertise • Treatment depends on the severity and level of containment/treatment required • Provision of consultation, support, supervision and training
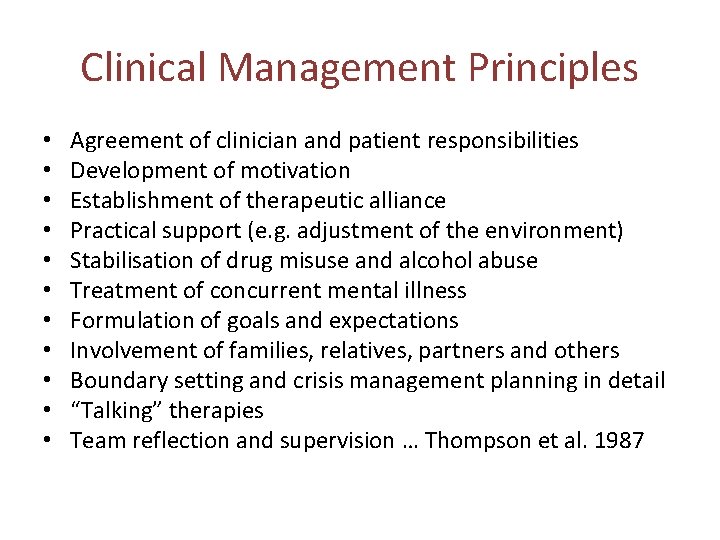
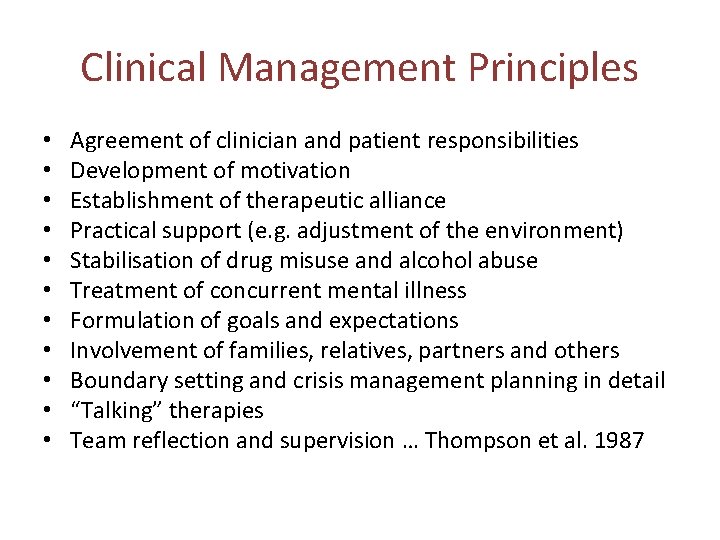
Clinical Management Principles • • • Agreement of clinician and patient responsibilities Development of motivation Establishment of therapeutic alliance Practical support (e. g. adjustment of the environment) Stabilisation of drug misuse and alcohol abuse Treatment of concurrent mental illness Formulation of goals and expectations Involvement of families, relatives, partners and others Boundary setting and crisis management planning in detail “Talking” therapies Team reflection and supervision … Thompson et al. 1987
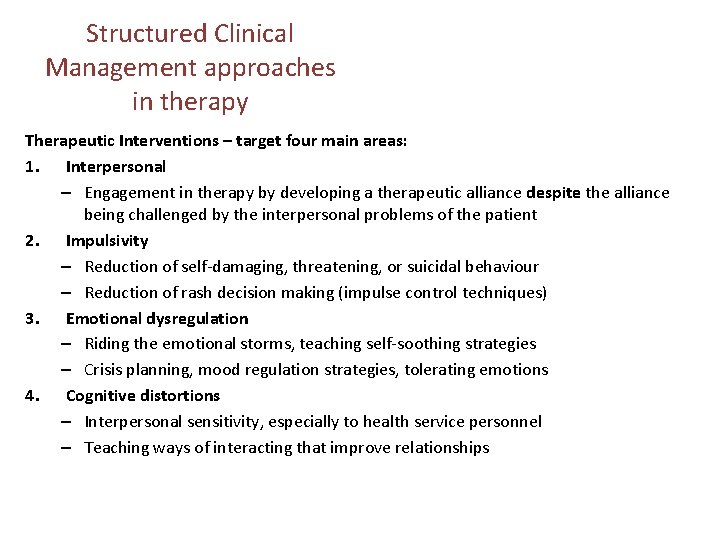
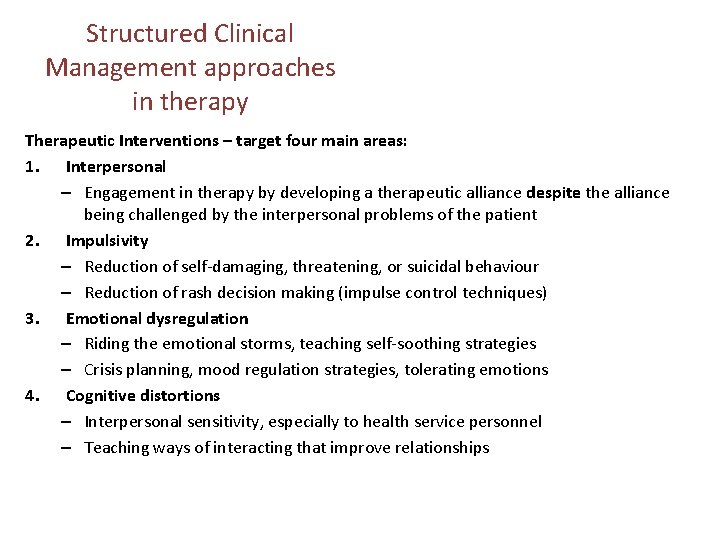
Structured Clinical Management approaches in therapy Therapeutic Interventions – target four main areas: 1. Interpersonal – Engagement in therapy by developing a therapeutic alliance despite the alliance being challenged by the interpersonal problems of the patient 2. Impulsivity – Reduction of self-damaging, threatening, or suicidal behaviour – Reduction of rash decision making (impulse control techniques) 3. Emotional dysregulation – Riding the emotional storms, teaching self-soothing strategies – Crisis planning, mood regulation strategies, tolerating emotions 4. Cognitive distortions – Interpersonal sensitivity, especially to health service personnel – Teaching ways of interacting that improve relationships
Conclusion • • Approach is working Very few A&E attendances Last MHA admission 2014 More appropriate phone calls
Thank you • Questions?
 Schizotypal personality
Schizotypal personality Somatization disorder dsm 5
Somatization disorder dsm 5 Waseem ahmad khan
Waseem ahmad khan Waseem ikram
Waseem ikram Waseem ikram
Waseem ikram Waseem ikram
Waseem ikram Primary control vs secondary control
Primary control vs secondary control Campaign to end loneliness measurement tool
Campaign to end loneliness measurement tool Bipolar disorder meaning
Bipolar disorder meaning Personality disorder types
Personality disorder types Emotionally unstable personality disorder
Emotionally unstable personality disorder Cluster b personality disorder
Cluster b personality disorder Psychopath vs sociopath
Psychopath vs sociopath Cluster c
Cluster c Nos personality disorder
Nos personality disorder Personality trait disorder
Personality trait disorder Cluster b personality traits
Cluster b personality traits Anankastic personality disorder
Anankastic personality disorder Site:slidetodoc.com
Site:slidetodoc.com Enduring pattern meaning
Enduring pattern meaning Neurotic personality disorder
Neurotic personality disorder Narcissistic behavior
Narcissistic behavior The neurotic need for affection and approval
The neurotic need for affection and approval Adhd or bpd
Adhd or bpd Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Cluster c
Cluster c Borderline personality disorder mnemonic
Borderline personality disorder mnemonic Types of borderline personality disorder dsm-5
Types of borderline personality disorder dsm-5 Obsessive compulsive personality disorder symptoms
Obsessive compulsive personality disorder symptoms Ap psychology abnormal behavior
Ap psychology abnormal behavior Type b personality disorder
Type b personality disorder Skizoid personlighedsforstyrrelse
Skizoid personlighedsforstyrrelse Color code personality test white
Color code personality test white Squidward personality disorder
Squidward personality disorder Avoidant personality disorder
Avoidant personality disorder Sarah skett
Sarah skett