Neurotic Disorders Neurotic Disorders Neurotic stressrelated and somatoform
- Slides: 18
Neurotic Disorders
Neurotic Disorders • Neurotic, stress-related, and somatoform disorders have common historical origin with the concept of neurosis and association of a substantial proportion of these disorders with psychological causation. • Mixtures of symptoms, especially anxiety and depressive ones are common in these disorders • About one fourth of the population in developed countries will suffer from neurotic disorders during its lifetime course. • With the exception of social phobia their frequency is higher in women than in men.
Phobic Anxiety Disorders • In agoraphobia, social and specific phobias, anxiety is evoked predominantly by certain well-defined situations or objects, which are external to the individual and are not currently dangerous. • As a result, these situations or objects are characteristically avoided or endured with dread. • Phobic anxiety fluctuates from mild uneasy to terror. The individual’s concern may focus on individual symptoms such as palpitations or feeling faint and is often associated with secondary fears of dying, losing control, or going mad. • The anxiety is not relieved by the knowledge that other people do not regard the situation in question as dangerous or threatening.
Agoraphobia • „Agoraphobia“ - the fear from marketplace. • Agoraphobia includes various phobias embracing fears of leaving home: fears of entering shops, crowds, and public places, or of traveling alone in trains, buses, underground or planes. • The lack of an immediately available exit is one of the key features of many agoraphobic situations. • The avoidance behaviour causes sometimes that the sufferer becomes completely housebound. • Most sufferers are women. Onset - early adult life. • The lifetime prevalence - between 5— 7%. • High co-morbidity with panic disorder; depressive and obsessional symptoms and social phobias may be also present.
Social Phobias • Clinical picture - fear of scrutiny by other people in comparatively small groups leading to avoidance of social situations • The fears may be • discrete - restricted to eating in public, to be introduced to other people, to public speaking, or to encounters with the opposite sex • diffuse - social situations outside the family circle. • • Direct eye-to-eye confrontation may be stressful. Low self-esteem and fear of criticism. Symptoms may progress to panic attacks. Avoidance - almost complete social isolation. Usually start in childhood or adolescence. Estimation of lifetime prevalence - between 10 -13 %. It is equally common in both sexes. Secondary alcoholism.
Specific (Isolated) Phobias 1. Fears of proximity to particular animals • • • spiders (arachnophobia) insects (entomophobia) snakes (ophidiophobia) 2. Fears of specific situations such as • • heights (acrophobia) thunder (keraunophobia) darkness (nyctophobia) closed spaces (claustrophobia) 3. Fears of diseases, injuries or medical examinations • • • http: //www. youtub e. com/watch? v=9 rl 7 Lr 6 e. DLc visiting a dentist the sight of blood (hemophobia) or injury (pain —odynophobia) the fear of exposure to venereal diseases (syphilidophobia) or AIDS-phobia. Usually arise in childhood or early adult life and can persist for decades if they remain untreated. Lifetime prevalence - between 10 -20%.
Other Anxiety Disorders • Manifestations of anxiety are also the major symptoms of these disorders, however, it is not restricted to any particular environmental situation.
Panic Disorder • The essential features are recurrent attacks of severe anxiety (panic attacks) which are not restricted to any particular situation or set of circumstances. • Typical symptoms are palpitations, chest pain, choking sensations, dizziness, and feelings of unreality (depersonalisation or derealization). • Individual attacks usually last for minutes only. The frequency of attacks varies substantially. • Frequent and predictable panic attacks produce fear of being alone or going into public places. • The afflicted persons used to think that they got a serious somatic disease. • The course of panic disorder is long-lasting and is complicated with various comorbidities, in half of the cases with agoraphobia. • The estimation of lifetime prevalence moves between 1 -3%.
General Anxiety Disorder • The essential feature is anxiety lasting more than 6 months, which is generalized and persistent but not restricted to, or even strongly predominating in, any particular environmental circumstances. • Symptoms: continuous feelings of nervousness, trembling, muscular tension, sweating, lightheadedness, palpitations, dizziness, and stomach discomfort. • Fears that the person or a relative will shortly become ill or have an accident are often expressed, together with a variety of other worries and forebodings. • The estimation of lifetime prevalence moves between 4 -6 %. • This disorder is more common in women, and often related to chronic environmental stress. • Its course uses to be fluctuating and chronic connected with symptoms of frustration, sadness and complicated with abuse of alcohol and other illicit drugs.
Obsessive-Compulsive Disorder • Obsessional thought are ideas, images or impulses that enter the individual’s mind again and again in a stereotyped form. • They are recognized as the individual’s own thoughts, even though they are involuntary and often repugnant. Common obsessions include fears of contamination, of harming other persons or sinning against God. • Compulsions are repetitive, purposeful, and intentional behaviours or mental acts performed in response to obsessions or according to certain rule that must be applied rigidly. Compulsions are meant to neutralize or reduce discomfort or to prevent a dreaded event or situation. • Autonomic anxiety symptoms are often present. • There is very frequent comorbidity with depression (about 80%) - suicidal thoughts. Obsessive-compulsory symptoms may appear in early stages of schizophrenia. • The life time prevalence: 2 - 3%. Equally common in men and women. The course is variable and more likely to be chronic. http: //www. youtube. com /watch? v=e g 14 F 72 p. Y-4
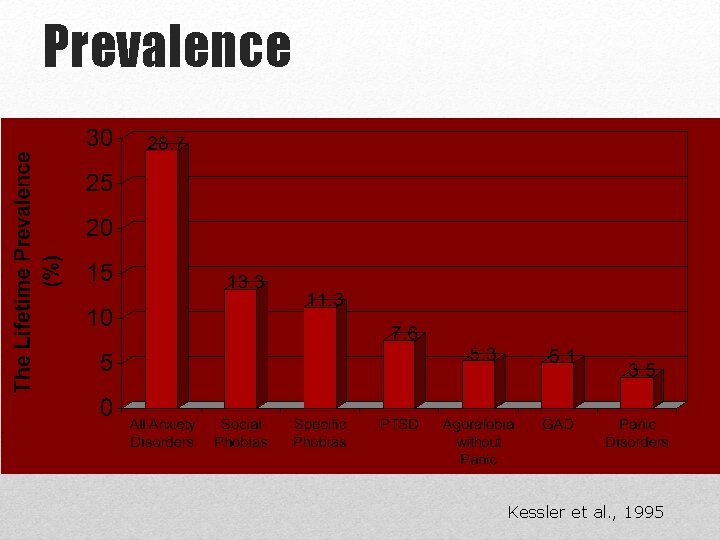
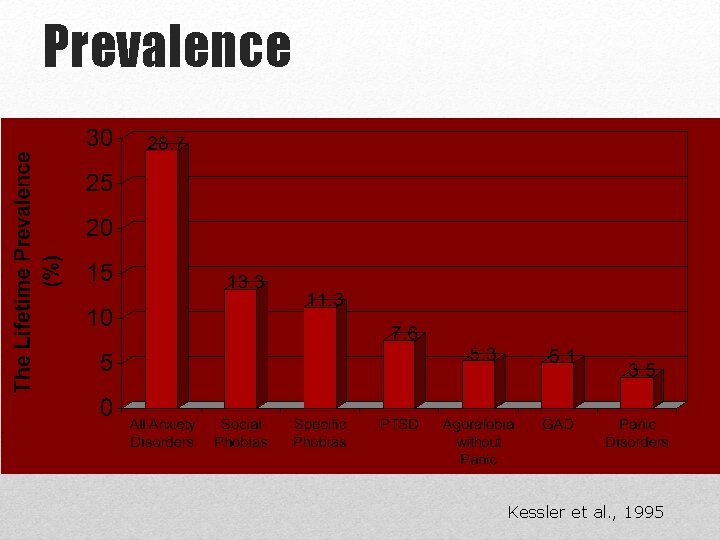
Prevalence Kessler et al. , 1995
Dissociative Amnesia • The main feature is loss of memory, usually of important recent event, which is not due to organic mental disorder and is too extensive to be explained by ordinary forgetfulness or fatigue. • The amnesia is usually centered on traumatic events, such as accidents, combat experiences, or unexpected bereavements, and used to be partial and selective. • The amnesia typically develops suddenly and can last from minutes to days. • Differential diagnosis: complicated; it is necessary to rule out all organic brain disorders as well as various intoxications. The most difficult differentiation is from conscious simulation - malingering.
Dissociative Stupor • The individual suffers from diminution or absence of voluntary movement and normal responsiveness to external stimuli such as light, noise, and touch. • The person lies or sits largely motionless for long periods of time. • Speech and spontaneous and purposeful movement are completely absent. • Muscle tone, posture, breathing, and sometimes eye-opening and coordinated eye movements are such that it is clear that the individual is neither asleep nor unconscious. • Positive evidence of psychogenic causation in the form of either recent stressful events or prominent interpersonal or social problems.
Reaction to Severe Stress, and Adjustment Disorders • This category differs from others in that it includes disorders identifiable not only on grounds of symptomatology and course but also on the basis of one or other of two • Causative influences: • an exceptionally stressful life event (e. g. natural or man-made disaster, combat, serious accident, witnessing the violent death of others, or being the victim of torture, terrorism, rape, or other crime) producing an acute stress reaction • significant life change leading to continued unpleasant circumstances that result in an adjustment disorder • Stressful event is thought to be the primary and overriding causal factor, and the disorder would not have occurred without its impact.
Acute Stress Reaction • A transient disorder of significant severity, which develops in an individual without any previous mental disorder in response to exceptional physical and/or psychological stress. • Not all people exposed to the same stressful event develop the disorder. • The symptoms: an initial state of „daze”, with some constriction of the field of consciousness and narrowing of attention, inability to comprehend stimuli, and disorientation. This state may be followed either by further withdrawal from the surrounding situation (extreme variant - dissociative stupor), or by agitation and overactivity. • Autonomic signs - tachycardia, sweating or flushing, as well as other anxiety or depressive symptoms. • The symptoms usually appear within minutes of the impact of the stressful event, and disappear within several hours, maximally 2— 3 days.
Post-traumatic Stress Disorder (PTSD) http: //www. youtube. com/watch? v=LM_nw 5 N 3 n-I • PTSD is a delayed and/or protracted response to a stressful event of an exceptionally threatening or catastrophic nature. • The three major elements of PTSD include 1) reexperiencing the trauma through dreams or recurrent and intrusive thoughts (“flashbacks”) 2) showing emotional numbing such as feeling detached from others 3) having symptoms of autonomic hyperarousal such as irritability and exaggerated startle response, insomnia • Commonly there is fear and avoidance of cues that remind the sufferer of the original trauma. Anxiety and depression are commonly associated with the above symptoms. Excessive use of alcohol and drugs may be a complicating factor. • The onset follows the trauma with a latency period, which may range from several weeks to months, but rarely more than half a year. • The lifetime prevalence is estimated at about 0. 5% in men and 1. 2% in women.
Hypochondriacal Disorder • The disorder is characterized by a persistent preoccupation and a fear of developing or having one or more serious and progressive physical disorders. • Patients persistently complain of physical problems or are persistently preoccupied with their physical appearance. • The fear is based on the misinterpretation of physical signs and sensations. • Physician physical examination does not reveal any physical disorder, but the fear and convictions persist despite the reassurance.
Persistent Somatoform Pain Disorder • The predominant symptom is a persistent severe and distressing pain that cannot be explained fully by a physiological process of physical illness. • Pain occurs in association with emotional conflicts or psychosocial problems. • The expression of chronic pain may vary with different personalities and cultures. • The patient is not malingering and the complaints about the intensity of the pain are to be believed.
 What is neurosis disorder
What is neurosis disorder Neurosis disorder
Neurosis disorder Somatic symptom disorder
Somatic symptom disorder Somatization disorder
Somatization disorder Somatization disorder
Somatization disorder Gangguan somatoform
Gangguan somatoform Hyperventilation
Hyperventilation Epidemiologi gangguan somatoform
Epidemiologi gangguan somatoform Narrow limits to life
Narrow limits to life Difference between neurotic and psychotic
Difference between neurotic and psychotic Neurotic anxiety example
Neurotic anxiety example Anxiety mnemonic
Anxiety mnemonic Free floating anxiety
Free floating anxiety Freudian slip meaning
Freudian slip meaning Neurotic anxiety example
Neurotic anxiety example Neurotic person
Neurotic person Physiological disorders unit 14
Physiological disorders unit 14 Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders