Somatoform Disorders Dr Okine Somatoform Disorders n n






- Slides: 33

Somatoform Disorders Dr. Okine
Somatoform Disorders n n Have you ever used or faked Sx to get out of having to perform important activities (exams, classes, work, social functions)? Have you ever used tactics to gain attention and sympathy?
Characteristics of the Somatoform Disorders n n Somatization: the expression of psychological pain through physical sx or concerns Unexplained physical symptoms or bodily preoccupations n n n Somatization Disorder, Conversion Disorder, Pain Disorder, Undifferentiated Somatoform Disorder: experiencing pain with no apparent medical basis Hypochondriasis: preoccupation with having a serious medical condition or disease Body Dysmorphic Disorder: preoccupation with a perceived serious defect in appearance
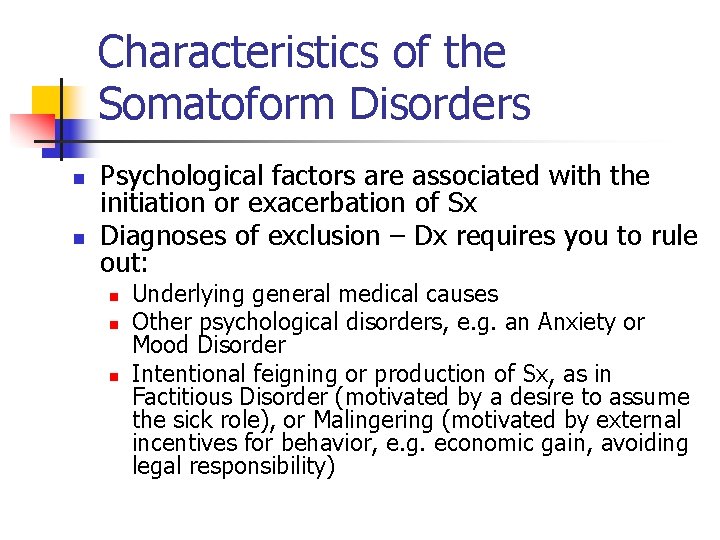
Characteristics of the Somatoform Disorders n n Psychological factors are associated with the initiation or exacerbation of Sx Diagnoses of exclusion – Dx requires you to rule out: n n n Underlying general medical causes Other psychological disorders, e. g. an Anxiety or Mood Disorder Intentional feigning or production of Sx, as in Factitious Disorder (motivated by a desire to assume the sick role), or Malingering (motivated by external incentives for behavior, e. g. economic gain, avoiding legal responsibility)
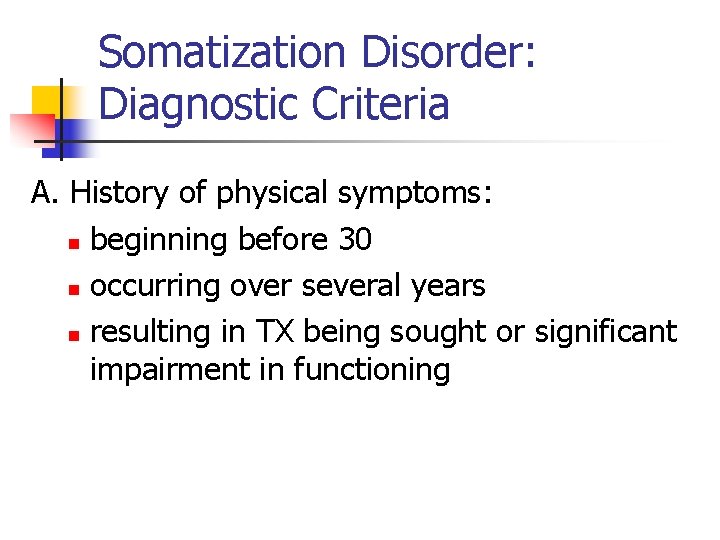
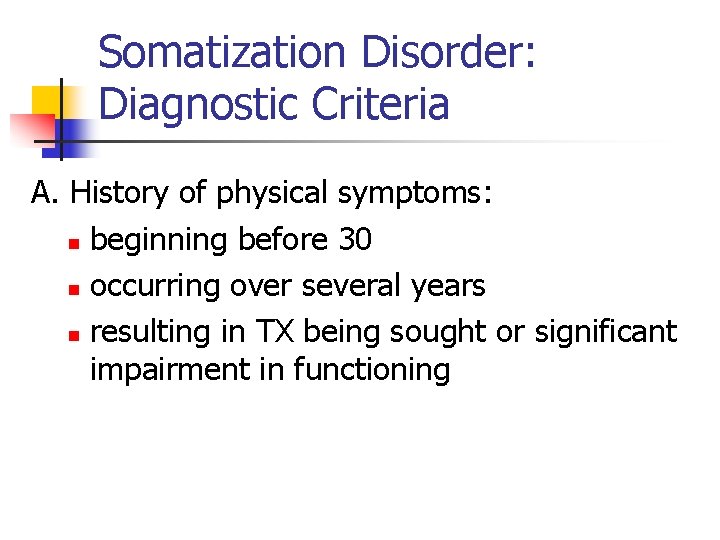
Somatization Disorder: Diagnostic Criteria A. History of physical symptoms: n beginning before 30 n occurring over several years n resulting in TX being sought or significant impairment in functioning
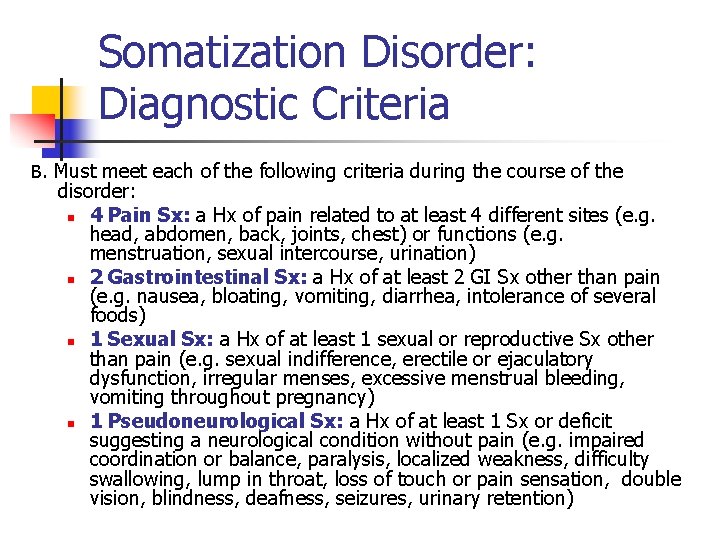
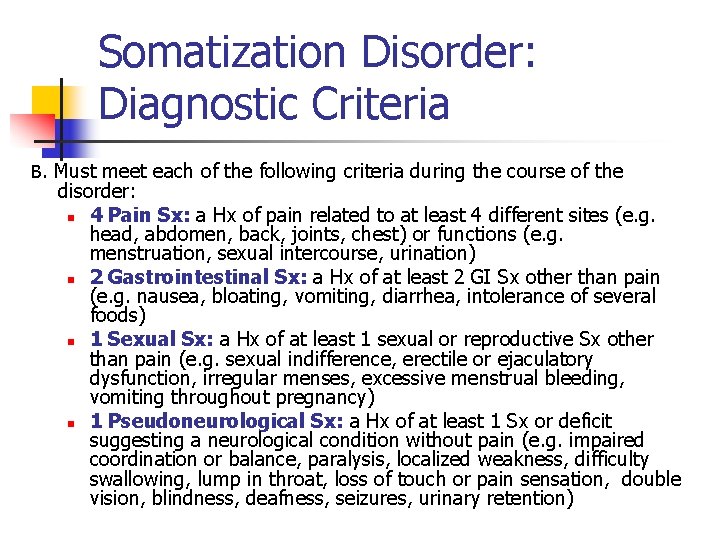
Somatization Disorder: Diagnostic Criteria B. Must meet each of the following criteria during the course of the disorder: n 4 Pain Sx: a Hx of pain related to at least 4 different sites (e. g. head, abdomen, back, joints, chest) or functions (e. g. menstruation, sexual intercourse, urination) n 2 Gastrointestinal Sx: a Hx of at least 2 GI Sx other than pain (e. g. nausea, bloating, vomiting, diarrhea, intolerance of several foods) n 1 Sexual Sx: a Hx of at least 1 sexual or reproductive Sx other than pain (e. g. sexual indifference, erectile or ejaculatory dysfunction, irregular menses, excessive menstrual bleeding, vomiting throughout pregnancy) n 1 Pseudoneurological Sx: a Hx of at least 1 Sx or deficit suggesting a neurological condition without pain (e. g. impaired coordination or balance, paralysis, localized weakness, difficulty swallowing, lump in throat, loss of touch or pain sensation, double vision, blindness, deafness, seizures, urinary retention)

Somatization Disorder: Diagnostic Criteria C. Either (1) or (2): (1) Symptoms not fully accounted for by a general medical condition or the effects of a substance (2) When there is a related medical condition, the complaints and resulting social or occupational impairment exceed what would be expected D. Symptoms are not intentionally feigned or produced, as in Factitious Disorder or Malingering

Somatization Disorder: General Characteristics n n a complex medical history inconsistencies between subjective complaints and objective findings colorful, dramatic quality to complaints – exaggerating and elaborating on physical and psychiatric Sx respond to psychological/social problems with physical symptoms
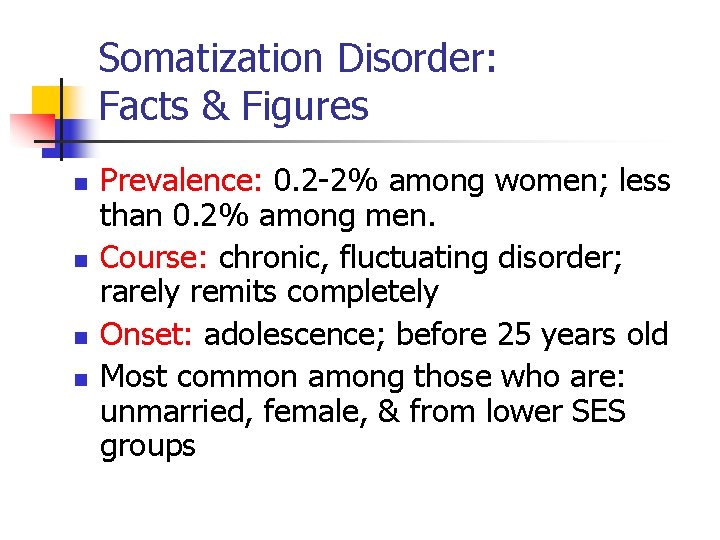
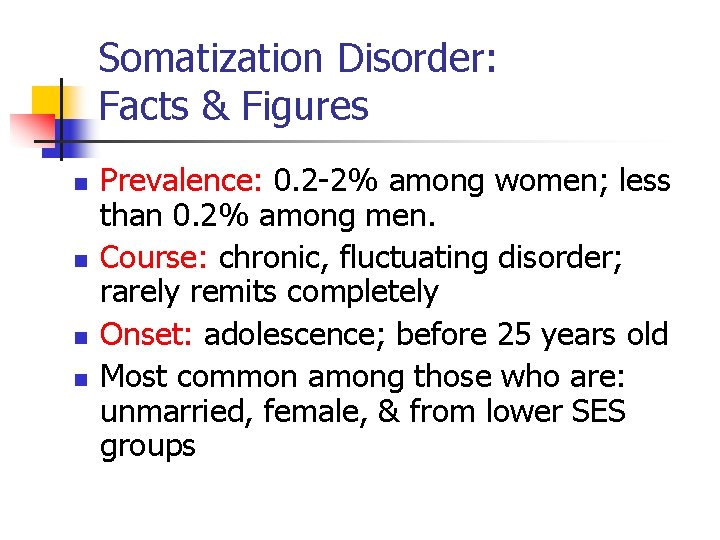
Somatization Disorder: Facts & Figures n n Prevalence: 0. 2 -2% among women; less than 0. 2% among men. Course: chronic, fluctuating disorder; rarely remits completely Onset: adolescence; before 25 years old Most common among those who are: unmarried, female, & from lower SES groups
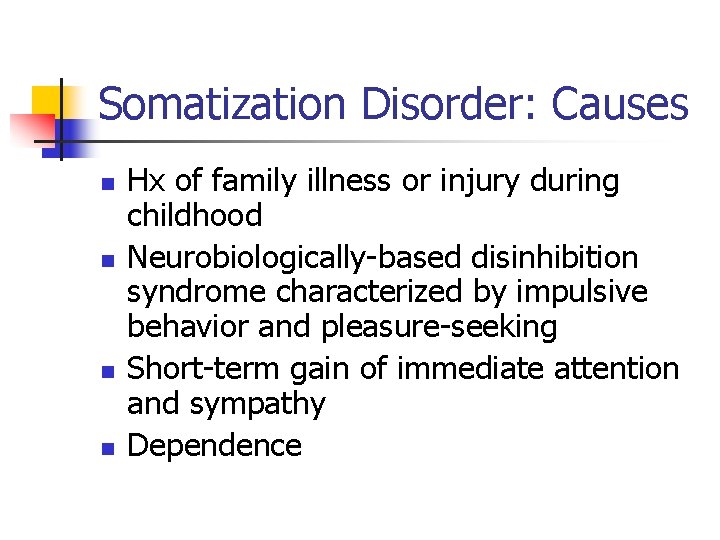
Somatization Disorder: Causes n n Hx of family illness or injury during childhood Neurobiologically-based disinhibition syndrome characterized by impulsive behavior and pleasure-seeking Short-term gain of immediate attention and sympathy Dependence
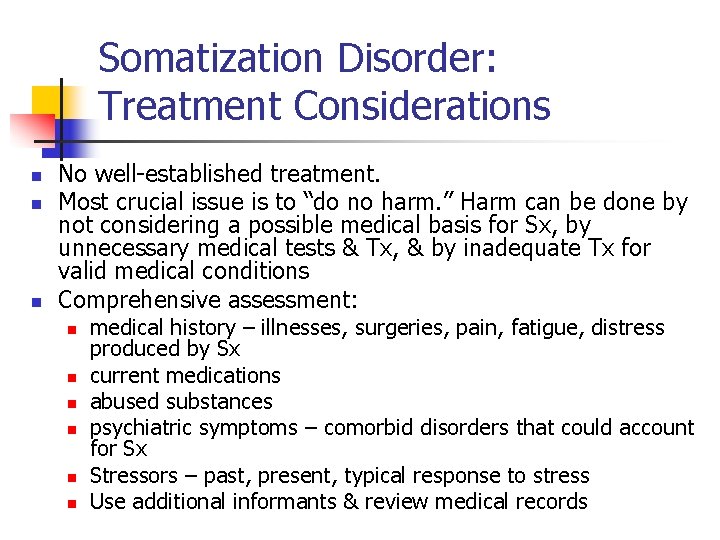
Somatization Disorder: Treatment Considerations n n n No well-established treatment. Most crucial issue is to “do no harm. ” Harm can be done by not considering a possible medical basis for Sx, by unnecessary medical tests & Tx, & by inadequate Tx for valid medical conditions Comprehensive assessment: n n n medical history – illnesses, surgeries, pain, fatigue, distress produced by Sx current medications abused substances psychiatric symptoms – comorbid disorders that could account for Sx Stressors – past, present, typical response to stress Use additional informants & review medical records
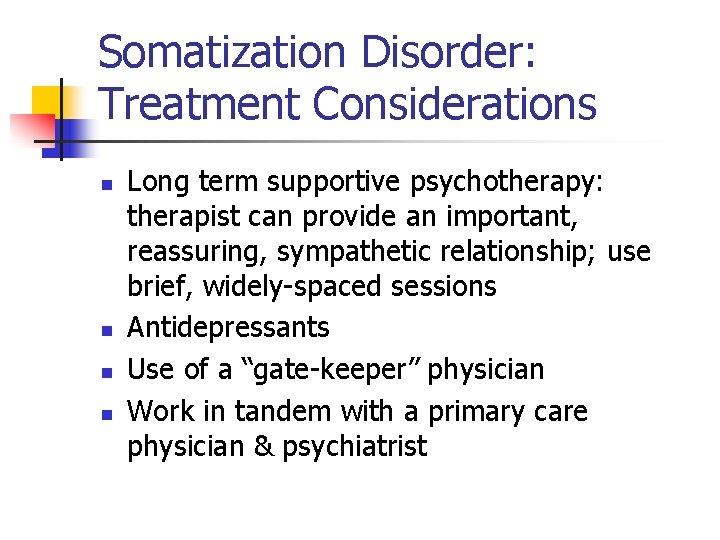
Somatization Disorder: Treatment Considerations n n Long term supportive psychotherapy: therapist can provide an important, reassuring, sympathetic relationship; use brief, widely-spaced sessions Antidepressants Use of a “gate-keeper” physician Work in tandem with a primary care physician & psychiatrist
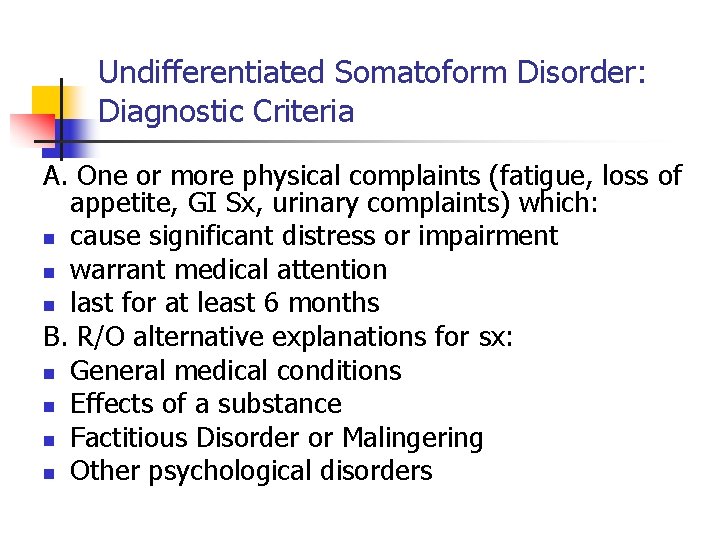
Undifferentiated Somatoform Disorder: Diagnostic Criteria A. One or more physical complaints (fatigue, loss of appetite, GI Sx, urinary complaints) which: n cause significant distress or impairment n warrant medical attention n last for at least 6 months B. R/O alternative explanations for sx: n General medical conditions n Effects of a substance n Factitious Disorder or Malingering n Other psychological disorders
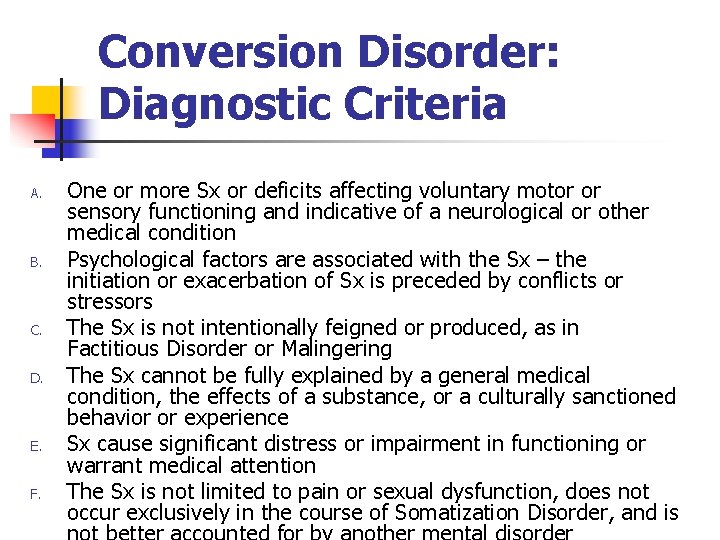
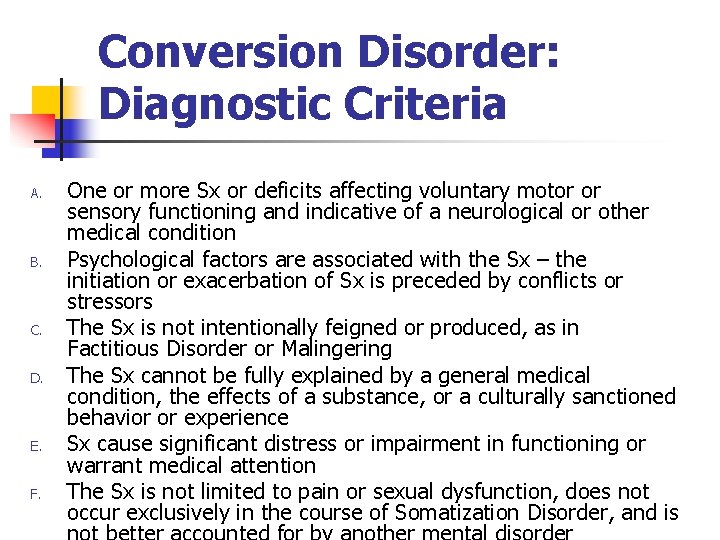
Conversion Disorder: Diagnostic Criteria A. B. C. D. E. F. One or more Sx or deficits affecting voluntary motor or sensory functioning and indicative of a neurological or other medical condition Psychological factors are associated with the Sx – the initiation or exacerbation of Sx is preceded by conflicts or stressors The Sx is not intentionally feigned or produced, as in Factitious Disorder or Malingering The Sx cannot be fully explained by a general medical condition, the effects of a substance, or a culturally sanctioned behavior or experience Sx cause significant distress or impairment in functioning or warrant medical attention The Sx is not limited to pain or sexual dysfunction, does not occur exclusively in the course of Somatization Disorder, and is

Conversion Disorder: Specifiers n Specifiers: n n With Motor Sx or Deficits – e. g. impaired coordination or balance, paralysis, localized weakness, difficulty swallowing, lump in throat, urinary retention With Sensory Sx or Deficits – loss of touch or pain sensation, double vision, blindness, deafness, hallucinations With Seizures or Convulsions With Mixed Presentation
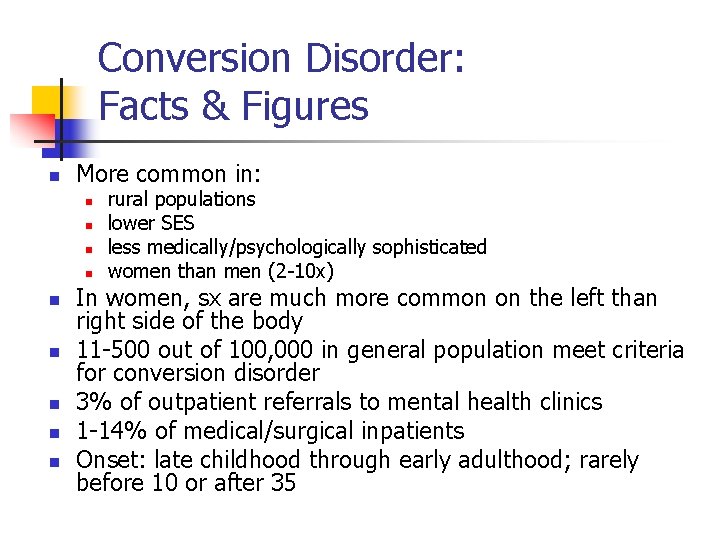
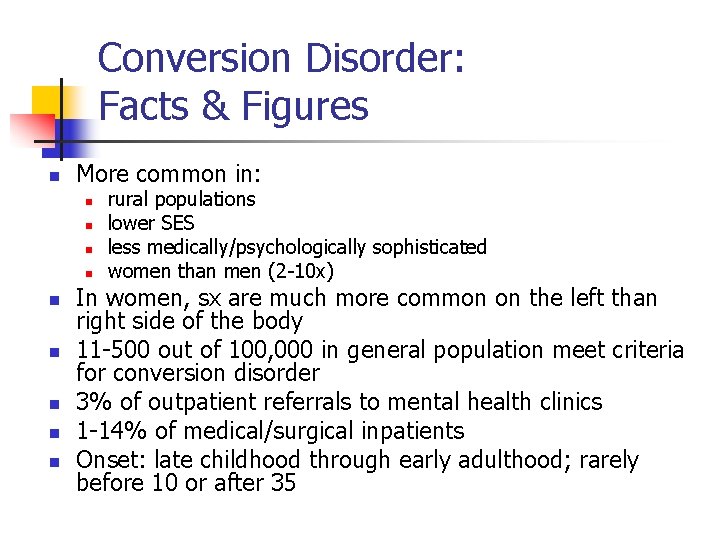
Conversion Disorder: Facts & Figures n More common in: n n n n n rural populations lower SES less medically/psychologically sophisticated women than men (2 -10 x) In women, sx are much more common on the left than right side of the body 11 -500 out of 100, 000 in general population meet criteria for conversion disorder 3% of outpatient referrals to mental health clinics 1 -14% of medical/surgical inpatients Onset: late childhood through early adulthood; rarely before 10 or after 35
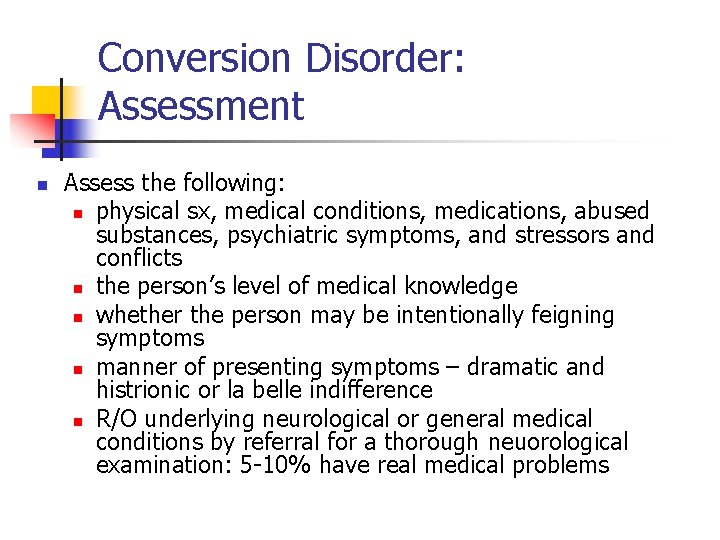
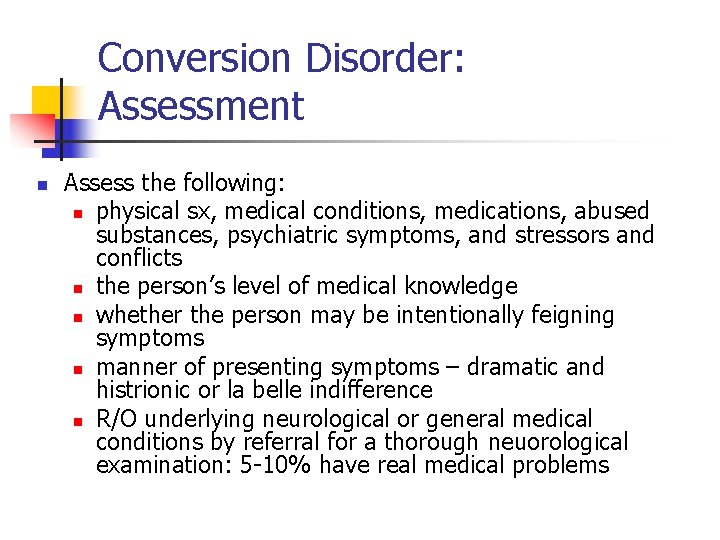
Conversion Disorder: Assessment n Assess the following: n physical sx, medical conditions, medications, abused substances, psychiatric symptoms, and stressors and conflicts n the person’s level of medical knowledge n whether the person may be intentionally feigning symptoms n manner of presenting symptoms – dramatic and histrionic or la belle indifference n R/O underlying neurological or general medical conditions by referral for a thorough neuorological examination: 5 -10% have real medical problems
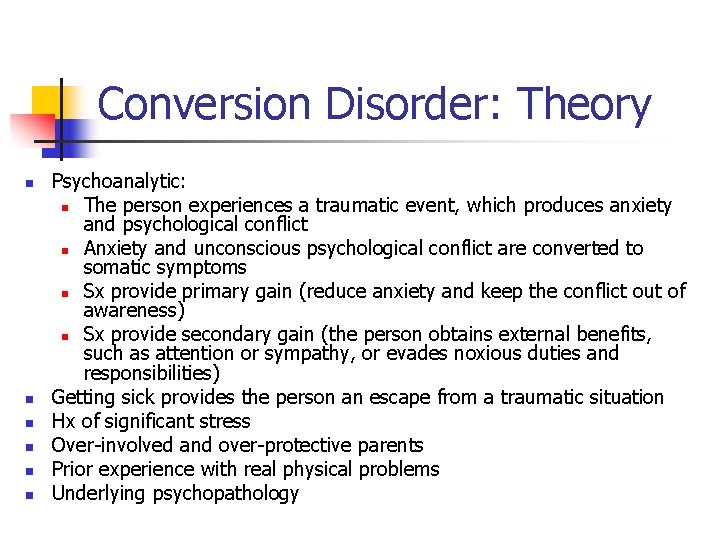
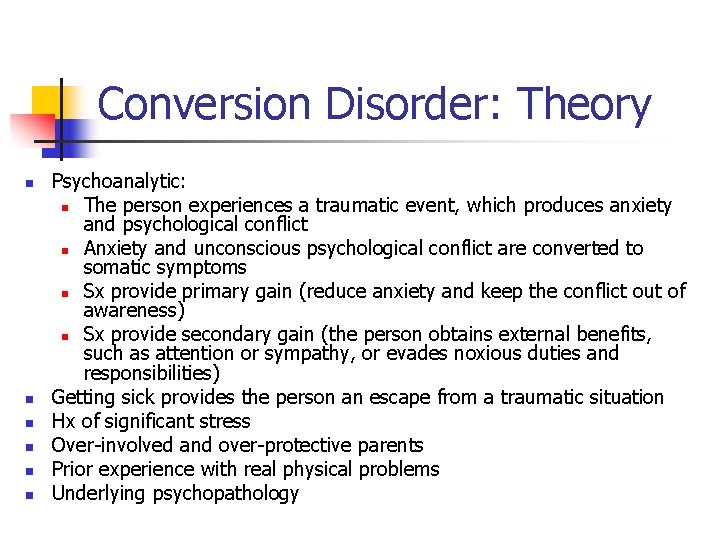
Conversion Disorder: Theory n n n Psychoanalytic: n The person experiences a traumatic event, which produces anxiety and psychological conflict n Anxiety and unconscious psychological conflict are converted to somatic symptoms n Sx provide primary gain (reduce anxiety and keep the conflict out of awareness) n Sx provide secondary gain (the person obtains external benefits, such as attention or sympathy, or evades noxious duties and responsibilities) Getting sick provides the person an escape from a traumatic situation Hx of significant stress Over-involved and over-protective parents Prior experience with real physical problems Underlying psychopathology
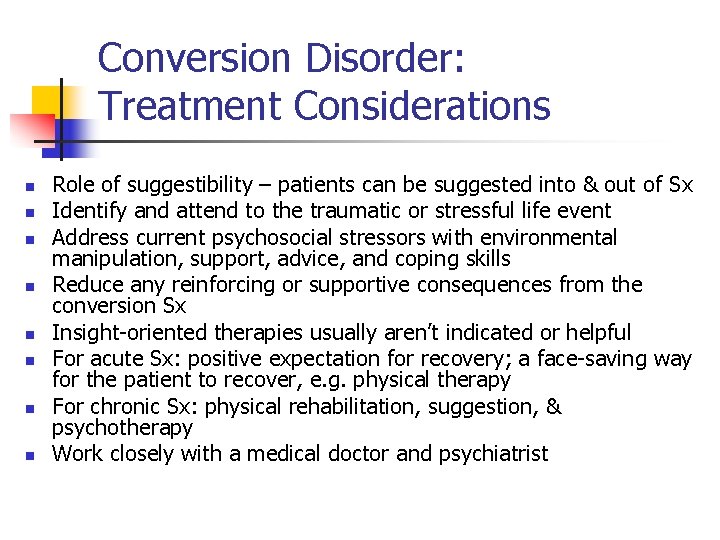
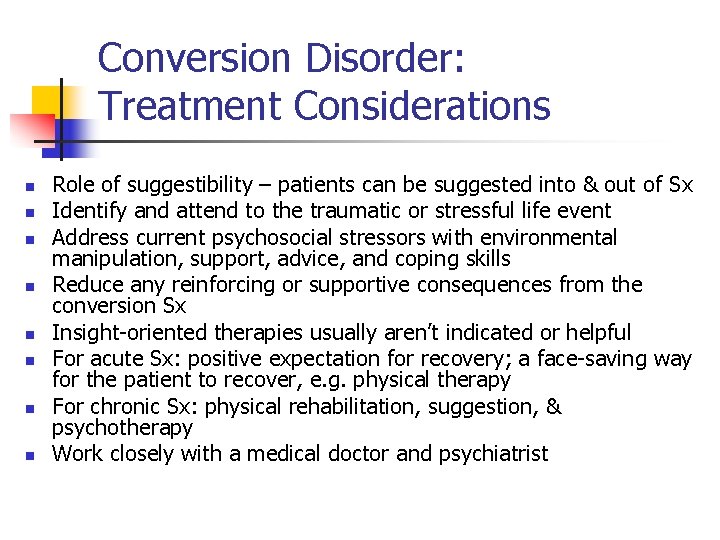
Conversion Disorder: Treatment Considerations n n n n Role of suggestibility – patients can be suggested into & out of Sx Identify and attend to the traumatic or stressful life event Address current psychosocial stressors with environmental manipulation, support, advice, and coping skills Reduce any reinforcing or supportive consequences from the conversion Sx Insight-oriented therapies usually aren’t indicated or helpful For acute Sx: positive expectation for recovery; a face-saving way for the patient to recover, e. g. physical therapy For chronic Sx: physical rehabilitation, suggestion, & psychotherapy Work closely with a medical doctor and psychiatrist
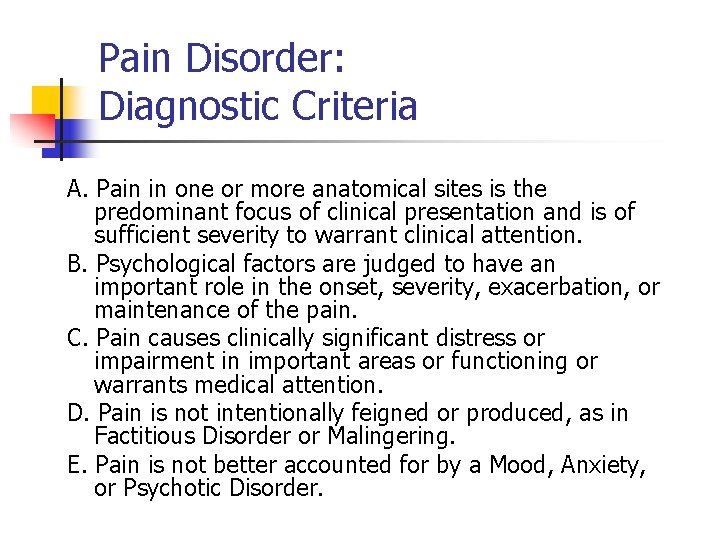
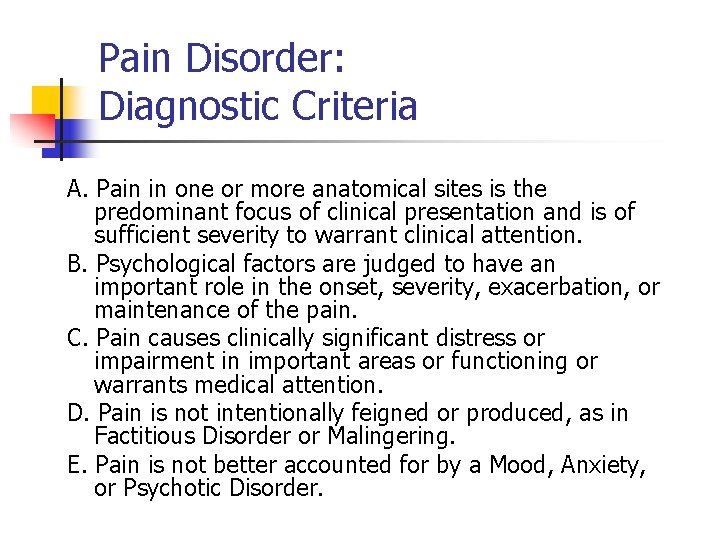
Pain Disorder: Diagnostic Criteria A. Pain in one or more anatomical sites is the predominant focus of clinical presentation and is of sufficient severity to warrant clinical attention. B. Psychological factors are judged to have an important role in the onset, severity, exacerbation, or maintenance of the pain. C. Pain causes clinically significant distress or impairment in important areas or functioning or warrants medical attention. D. Pain is not intentionally feigned or produced, as in Factitious Disorder or Malingering. E. Pain is not better accounted for by a Mood, Anxiety, or Psychotic Disorder.
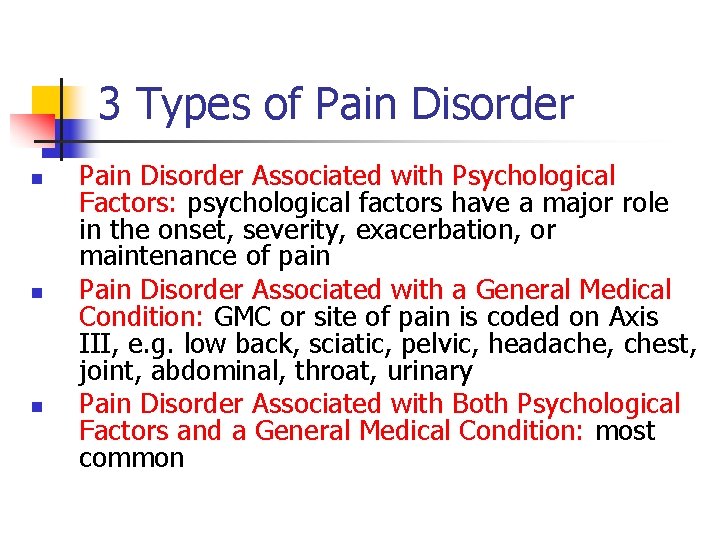
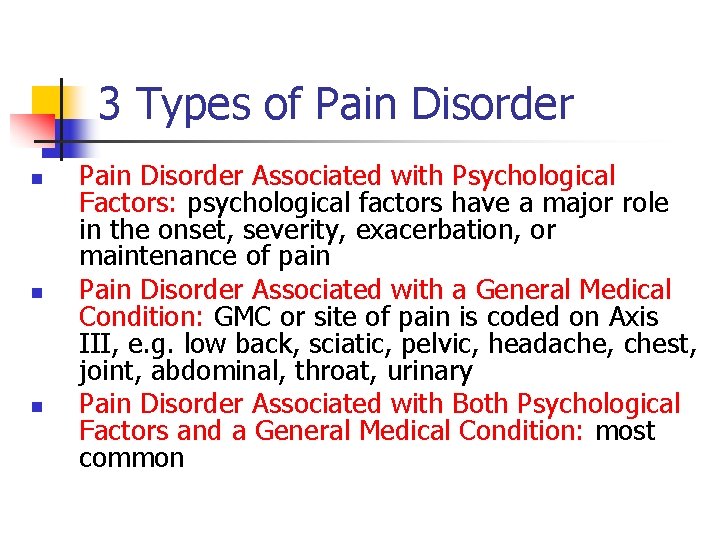
3 Types of Pain Disorder n n n Pain Disorder Associated with Psychological Factors: psychological factors have a major role in the onset, severity, exacerbation, or maintenance of pain Pain Disorder Associated with a General Medical Condition: GMC or site of pain is coded on Axis III, e. g. low back, sciatic, pelvic, headache, chest, joint, abdominal, throat, urinary Pain Disorder Associated with Both Psychological Factors and a General Medical Condition: most common
Pain Disorder: Specifiers n Acute: duration less than 6 months n Chronic: duration 6 months or longer
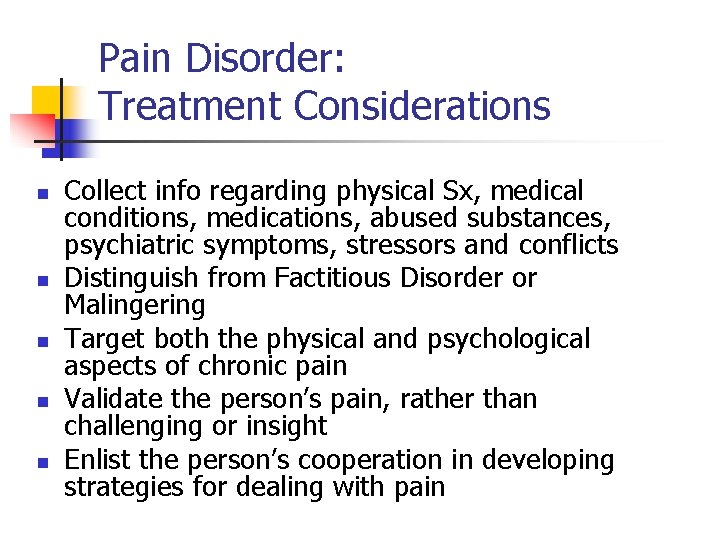
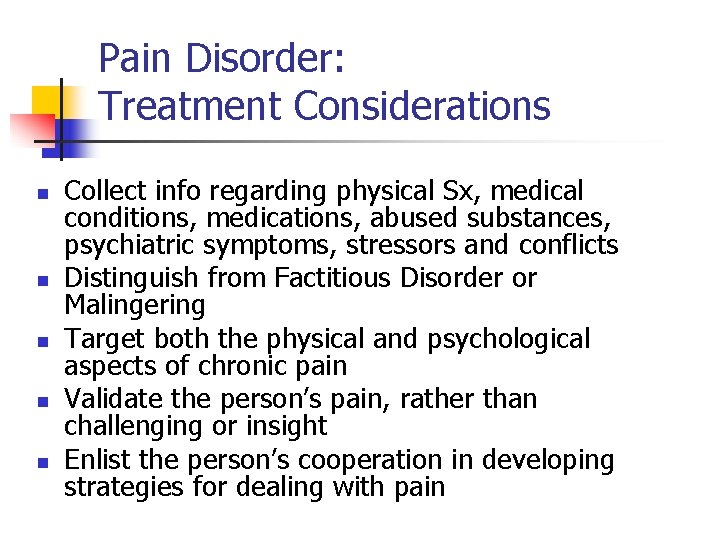
Pain Disorder: Treatment Considerations n n n Collect info regarding physical Sx, medical conditions, medications, abused substances, psychiatric symptoms, stressors and conflicts Distinguish from Factitious Disorder or Malingering Target both the physical and psychological aspects of chronic pain Validate the person’s pain, rather than challenging or insight Enlist the person’s cooperation in developing strategies for dealing with pain
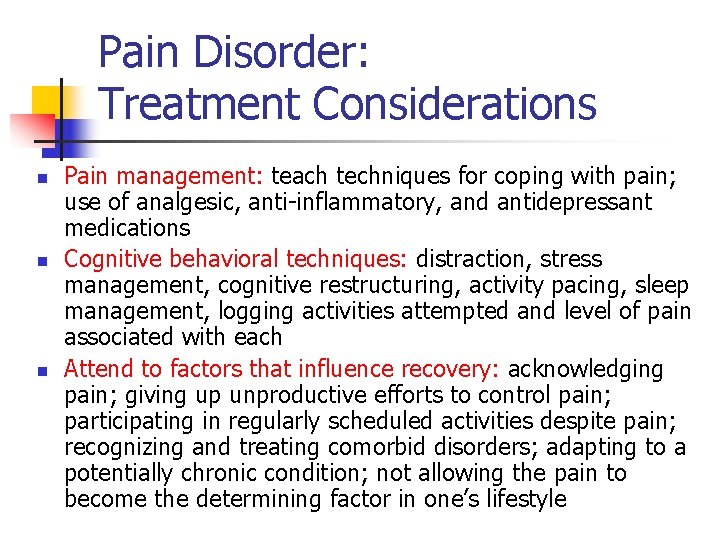
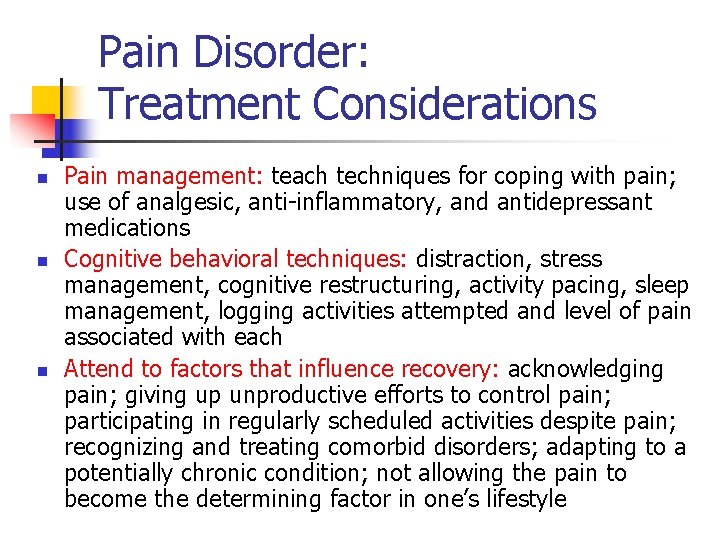
Pain Disorder: Treatment Considerations n n n Pain management: teach techniques for coping with pain; use of analgesic, anti-inflammatory, and antidepressant medications Cognitive behavioral techniques: distraction, stress management, cognitive restructuring, activity pacing, sleep management, logging activities attempted and level of pain associated with each Attend to factors that influence recovery: acknowledging pain; giving up unproductive efforts to control pain; participating in regularly scheduled activities despite pain; recognizing and treating comorbid disorders; adapting to a potentially chronic condition; not allowing the pain to become the determining factor in one’s lifestyle
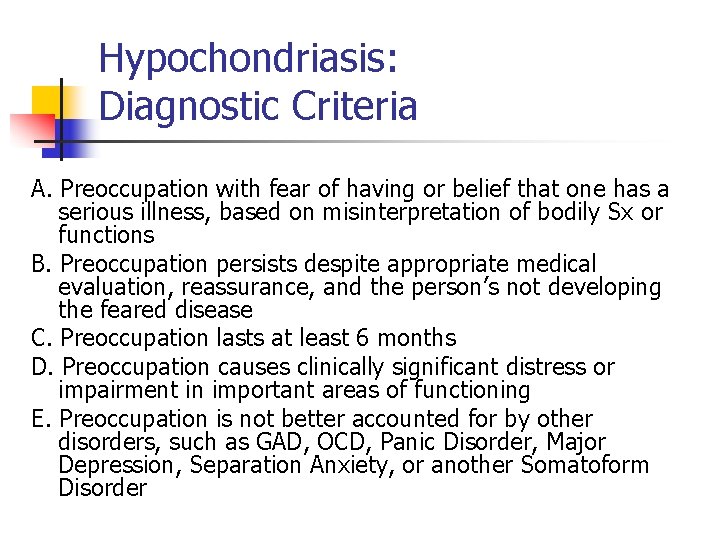
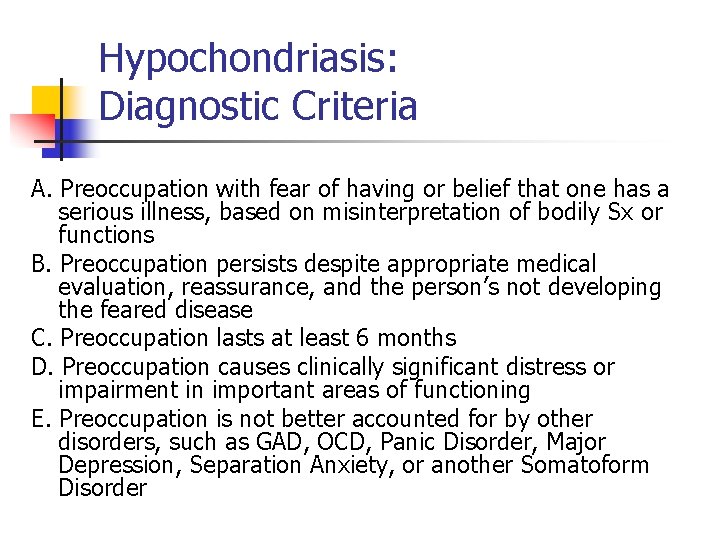
Hypochondriasis: Diagnostic Criteria A. Preoccupation with fear of having or belief that one has a serious illness, based on misinterpretation of bodily Sx or functions B. Preoccupation persists despite appropriate medical evaluation, reassurance, and the person’s not developing the feared disease C. Preoccupation lasts at least 6 months D. Preoccupation causes clinically significant distress or impairment in important areas of functioning E. Preoccupation is not better accounted for by other disorders, such as GAD, OCD, Panic Disorder, Major Depression, Separation Anxiety, or another Somatoform Disorder
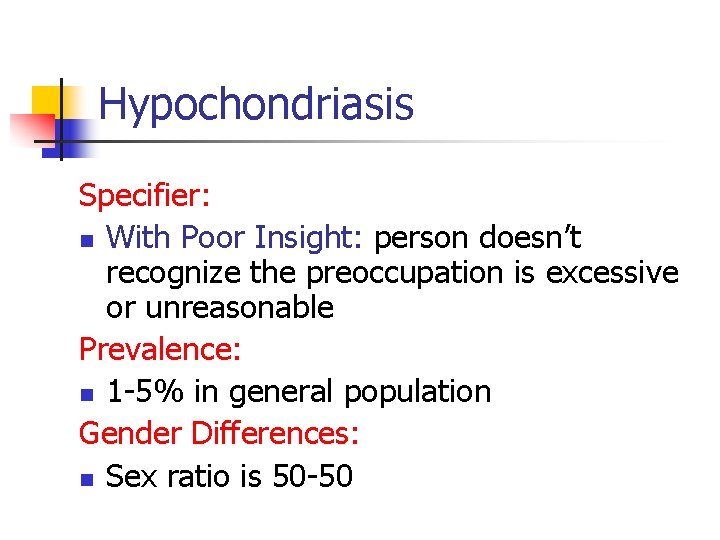
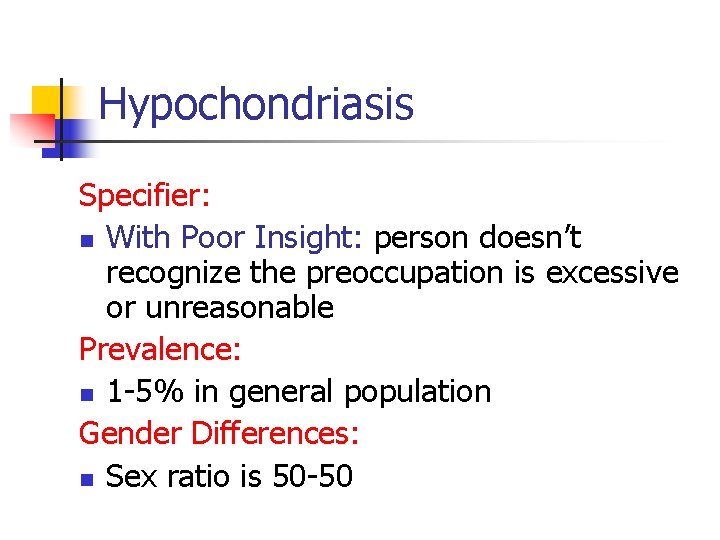
Hypochondriasis Specifier: n With Poor Insight: person doesn’t recognize the preoccupation is excessive or unreasonable Prevalence: n 1 -5% in general population Gender Differences: n Sex ratio is 50 -50
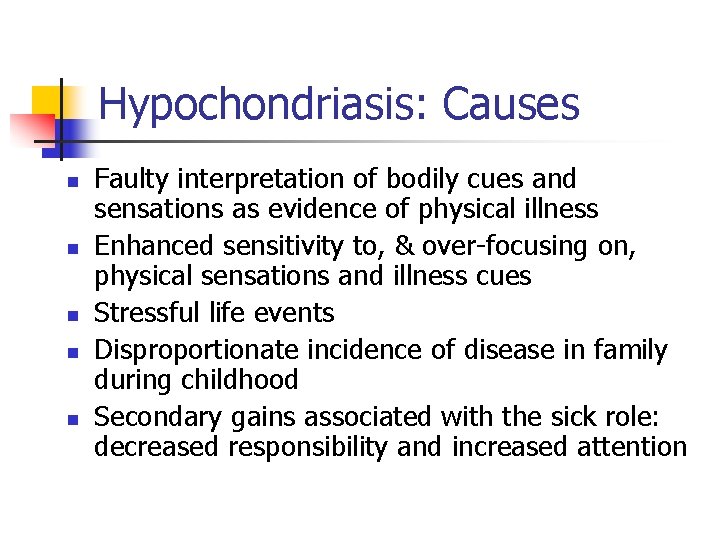
Hypochondriasis: Causes n n n Faulty interpretation of bodily cues and sensations as evidence of physical illness Enhanced sensitivity to, & over-focusing on, physical sensations and illness cues Stressful life events Disproportionate incidence of disease in family during childhood Secondary gains associated with the sick role: decreased responsibility and increased attention

Hypochondriasis: Treatments n n n Cognitive behavioral treatment: identifying & challenging illness-related misinterpretations of bodily sensations; showing patients how to create Sx by focusing attention on certain body areas Stress management Explanatory therapy: reassurance & education regarding the source and origins of Sx
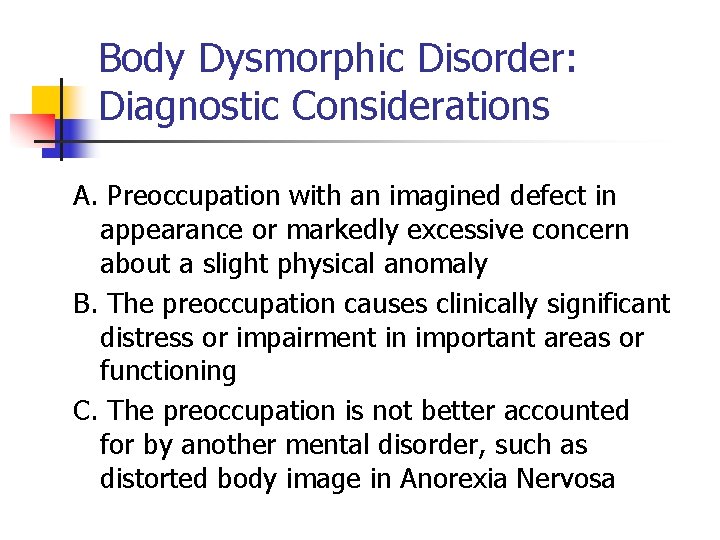
Body Dysmorphic Disorder: Diagnostic Considerations A. Preoccupation with an imagined defect in appearance or markedly excessive concern about a slight physical anomaly B. The preoccupation causes clinically significant distress or impairment in important areas or functioning C. The preoccupation is not better accounted for by another mental disorder, such as distorted body image in Anorexia Nervosa
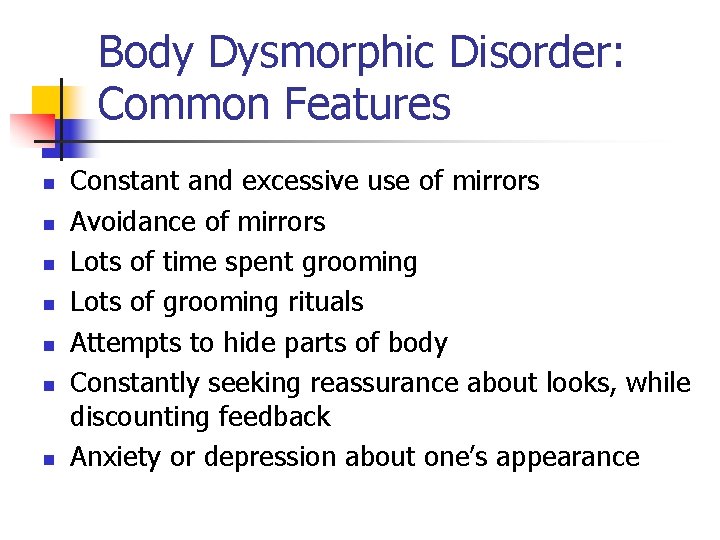
Body Dysmorphic Disorder: Common Features n n n n Constant and excessive use of mirrors Avoidance of mirrors Lots of time spent grooming Lots of grooming rituals Attempts to hide parts of body Constantly seeking reassurance about looks, while discounting feedback Anxiety or depression about one’s appearance

Body Dysmorphic Disorder: Facts & Figures n n People with BDD often seek help from dermatologists and plastic surgeons (rates of BDD in these settings is 6 -15%) BDD is under-recognized & under-diagnosed in nonpsychiatric settings BDD is infrequent in mental health settings Onset: adolescence and young adulthood
Body Dysmorphic Disorder: Causes n n Defense mechanism of displacement: displacing underlying psychological conflict and anxiety onto a body part Variant of OCD
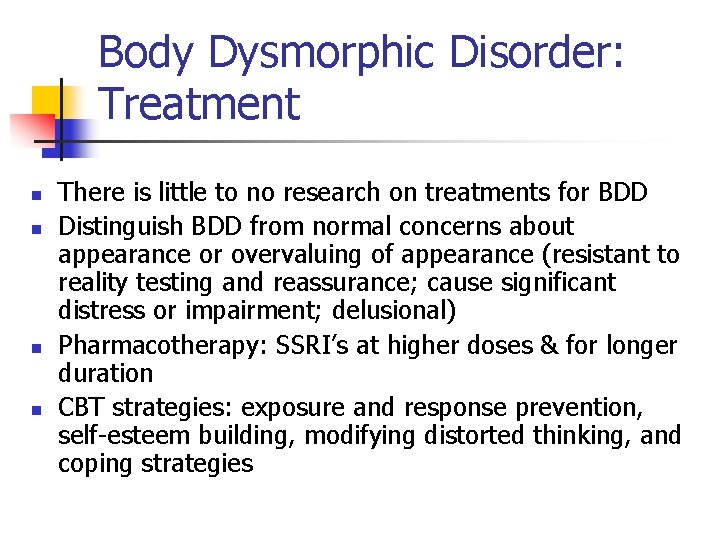
Body Dysmorphic Disorder: Treatment n n There is little to no research on treatments for BDD Distinguish BDD from normal concerns about appearance or overvaluing of appearance (resistant to reality testing and reassurance; cause significant distress or impairment; delusional) Pharmacotherapy: SSRI’s at higher doses & for longer duration CBT strategies: exposure and response prevention, self-esteem building, modifying distorted thinking, and coping strategies
 Neurotic stress-related and somatoform disorders
Neurotic stress-related and somatoform disorders Somatization disorder
Somatization disorder Neurosis disorder
Neurosis disorder Nursing diagnosis for somatoform disorder
Nursing diagnosis for somatoform disorder Gangguan somatoform
Gangguan somatoform Ahmad
Ahmad Epidemiologi gangguan somatoform
Epidemiologi gangguan somatoform Somatization disorder
Somatization disorder Paraphilic disorders
Paraphilic disorders Phenylketonuria mcq
Phenylketonuria mcq Causes of paraphilic disorders
Causes of paraphilic disorders Anxiety disorders def
Anxiety disorders def Btec level 3 health and social care unit 14 coursework
Btec level 3 health and social care unit 14 coursework Icd 10 skin infection
Icd 10 skin infection Autism authorization online program
Autism authorization online program Sleep disorders
Sleep disorders Chapter 47 urinary and reproductive disorders
Chapter 47 urinary and reproductive disorders Major neurocognitive disorder criteria
Major neurocognitive disorder criteria Anorexia psychodynamic explanation
Anorexia psychodynamic explanation Immunoproliferative disorders examples
Immunoproliferative disorders examples Difference between mendelian and chromosomal disorders
Difference between mendelian and chromosomal disorders Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Schizoid personality disorder
Schizoid personality disorder Unit 14 physiological disorders
Unit 14 physiological disorders Mental health disorders
Mental health disorders Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chromosomal mutation
Chromosomal mutation Paranoid personality disorder
Paranoid personality disorder Bernard soulier syndrome
Bernard soulier syndrome What is detachment disorder
What is detachment disorder Bipolar and other related disorders
Bipolar and other related disorders Chapter 14 psychological disorders
Chapter 14 psychological disorders Protraction disorders
Protraction disorders Paraphilia disorders
Paraphilia disorders