SOMATOFORM DISORDERS Types of Somatoform Disorders As per





- Slides: 31
SOMATOFORM DISORDERS
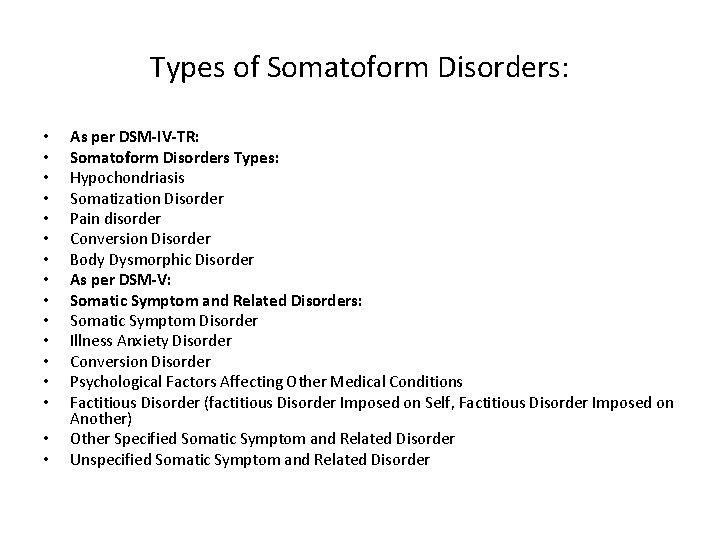
Types of Somatoform Disorders: • • • • As per DSM-IV-TR: Somatoform Disorders Types: Hypochondriasis Somatization Disorder Pain disorder Conversion Disorder Body Dysmorphic Disorder As per DSM-V: Somatic Symptom and Related Disorders: Somatic Symptom Disorder Illness Anxiety Disorder Conversion Disorder Psychological Factors Affecting Other Medical Conditions Factitious Disorder (factitious Disorder Imposed on Self, Factitious Disorder Imposed on Another) Other Specified Somatic Symptom and Related Disorder Unspecified Somatic Symptom and Related Disorder

Types of Somatoform Disorders: • As per ICD-10, Somatoform Disorders are categorised as follows: • Somatisation Disorder • Hypochondriasis/Hypochondriacal Disorder • Somatoform Autonomic Dysfunction • Other Somatoform Disorders
Features of Somatoform Disorders: • • Somatoform disorders (‘soma’ means body) are a group of conditions that involve physical symptoms and complaints suggesting the presence of a medical condition but without any evidence of physical pathology to account for them (APA, 2000). Though there is no adequate physical basis, the disorder is characterised by a persistent request by the patient for investigations and treatment despite repeated assurances by the treating doctors. The clinical manifestations of somatoform disorders range from blindness to paralysis to stomach pains to a sign of cancer, etc. Affected individuals are typically preoccupied with their state of health and with their various presumed disorders or diseases of bodily organs. Equally important is the fact that the affected persons have no control over their symptoms. They are also not intentionally faking symptoms or attempting to deceive others. They genuinely and sometimes passionately believe that something is terribly wrong with their bodies. The prevalence of the disorder appear to vary considerably among different cultures.
Features of Hypochondriasis: • • • It is also referred to as the Somatic Symptom Disorder, as per DSM-V. It is characterised by six or more months of a general and non-delusional preoccupation with fears of having, or the idea that one has, a serious disease based on the person’s misinterpretation of bodily symptoms. This preoccupation causes significant distress and impairment in one’s life. It is not accounted for by another psychiatric or medical disorder. A subset of individuals with these symptoms has poor insight about the presence of this disorder. It is the most commonly seen somatoform disorder. It occurs about equally in men and women. It can start at any age, although early adulthood is the most common age of onset. Once hypochondriasis develops, it tends to be a chronic disorder if left untreated, although the severity may wax and wane over time. Individuals with hypochondriasis also suffer from mood disorders, panic disorder and/or other somatoform disorders ( especially somatization disorder; Creed and Barsky, 2004).
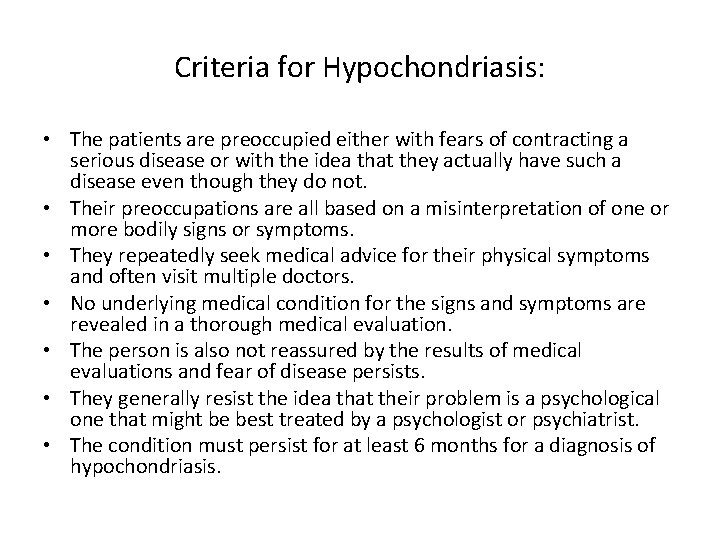
Criteria for Hypochondriasis: • The patients are preoccupied either with fears of contracting a serious disease or with the idea that they actually have such a disease even though they do not. • Their preoccupations are all based on a misinterpretation of one or more bodily signs or symptoms. • They repeatedly seek medical advice for their physical symptoms and often visit multiple doctors. • No underlying medical condition for the signs and symptoms are revealed in a thorough medical evaluation. • The person is also not reassured by the results of medical evaluations and fear of disease persists. • They generally resist the idea that their problem is a psychological one that might be best treated by a psychologist or psychiatrist. • The condition must persist for at least 6 months for a diagnosis of hypochondriasis.
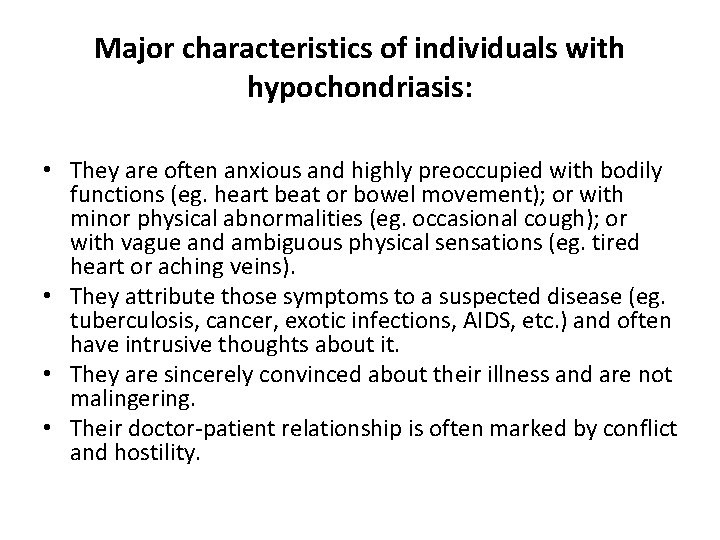
Major characteristics of individuals with hypochondriasis: • They are often anxious and highly preoccupied with bodily functions (eg. heart beat or bowel movement); or with minor physical abnormalities (eg. occasional cough); or with vague and ambiguous physical sensations (eg. tired heart or aching veins). • They attribute those symptoms to a suspected disease (eg. tuberculosis, cancer, exotic infections, AIDS, etc. ) and often have intrusive thoughts about it. • They are sincerely convinced about their illness and are not malingering. • Their doctor-patient relationship is often marked by conflict and hostility.
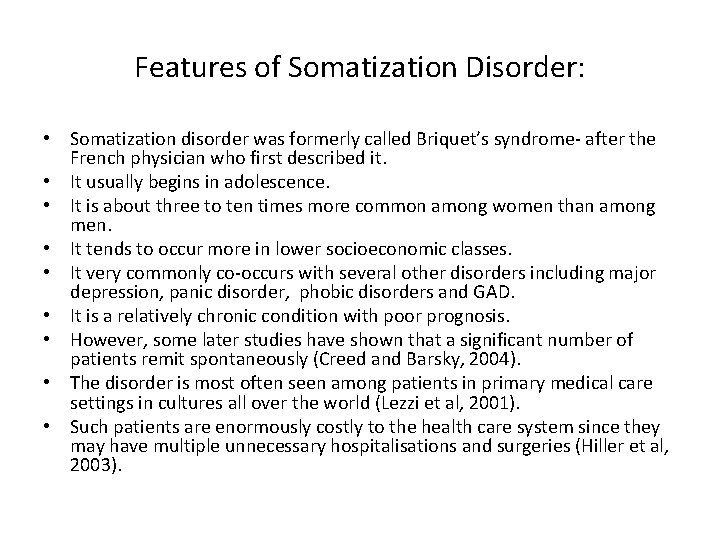
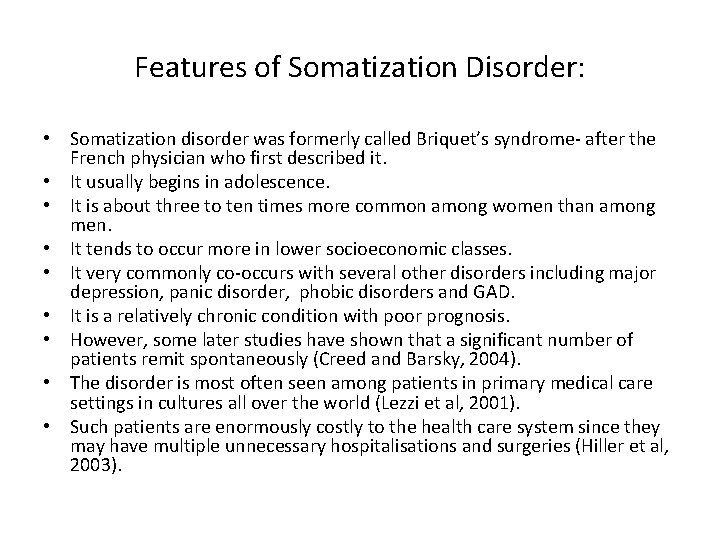
Features of Somatization Disorder: • Somatization disorder was formerly called Briquet’s syndrome- after the French physician who first described it. • It usually begins in adolescence. • It is about three to ten times more common among women than among men. • It tends to occur more in lower socioeconomic classes. • It very commonly co-occurs with several other disorders including major depression, panic disorder, phobic disorders and GAD. • It is a relatively chronic condition with poor prognosis. • However, some later studies have shown that a significant number of patients remit spontaneously (Creed and Barsky, 2004). • The disorder is most often seen among patients in primary medical care settings in cultures all over the world (Lezzi et al, 2001). • Such patients are enormously costly to the health care system since they may have multiple unnecessary hospitalisations and surgeries (Hiller et al, 2003).
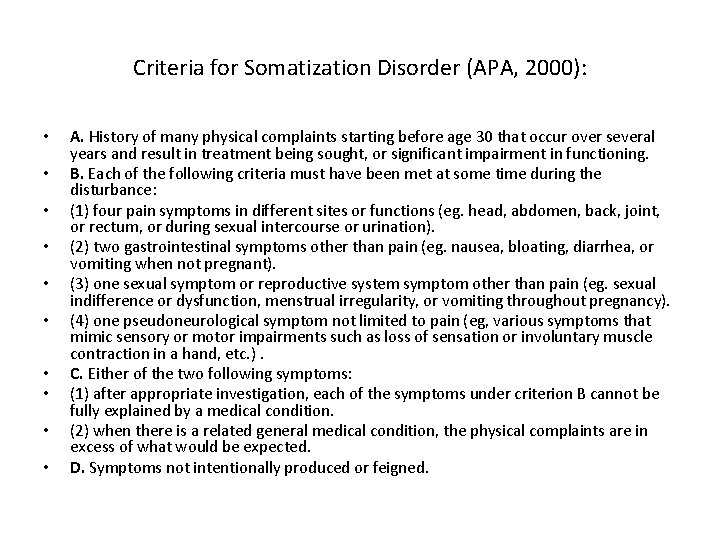
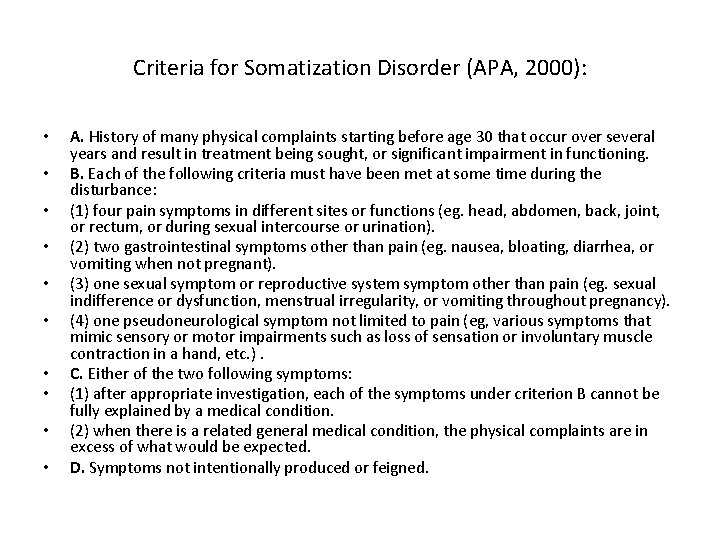
Criteria for Somatization Disorder (APA, 2000): • • • A. History of many physical complaints starting before age 30 that occur over several years and result in treatment being sought, or significant impairment in functioning. B. Each of the following criteria must have been met at some time during the disturbance: (1) four pain symptoms in different sites or functions (eg. head, abdomen, back, joint, or rectum, or during sexual intercourse or urination). (2) two gastrointestinal symptoms other than pain (eg. nausea, bloating, diarrhea, or vomiting when not pregnant). (3) one sexual symptom or reproductive system symptom other than pain (eg. sexual indifference or dysfunction, menstrual irregularity, or vomiting throughout pregnancy). (4) one pseudoneurological symptom not limited to pain (eg, various symptoms that mimic sensory or motor impairments such as loss of sensation or involuntary muscle contraction in a hand, etc. ). C. Either of the two following symptoms: (1) after appropriate investigation, each of the symptoms under criterion B cannot be fully explained by a medical condition. (2) when there is a related general medical condition, the physical complaints are in excess of what would be expected. D. Symptoms not intentionally produced or feigned.

Comparison between somatization disorder and hypochondriasis: • Both the disorders often co-occur. • Both are characterised by preoccupation with physical symptoms. • Only people with hypochondriasis tend to be convinced that they have an organic disease. • With hypochondriasis the person usually has only one or a few primary symptoms; while in somatization disorder, there are multiple symptoms.
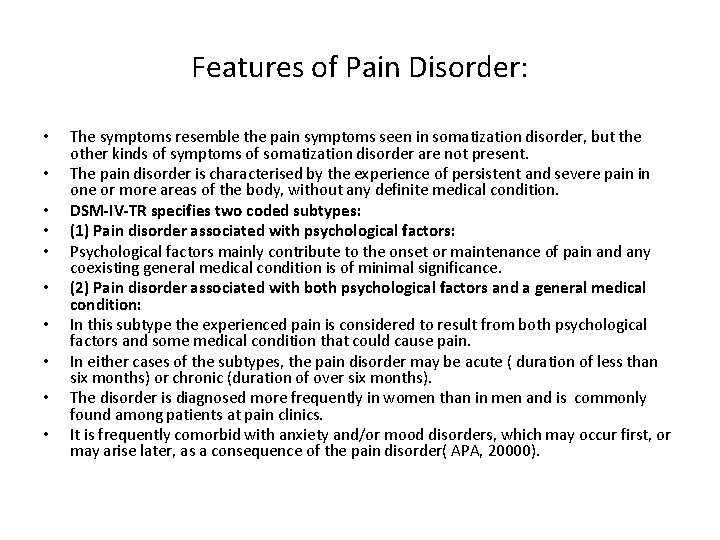
Features of Pain Disorder: • • • The symptoms resemble the pain symptoms seen in somatization disorder, but the other kinds of symptoms of somatization disorder are not present. The pain disorder is characterised by the experience of persistent and severe pain in one or more areas of the body, without any definite medical condition. DSM-IV-TR specifies two coded subtypes: (1) Pain disorder associated with psychological factors: Psychological factors mainly contribute to the onset or maintenance of pain and any coexisting general medical condition is of minimal significance. (2) Pain disorder associated with both psychological factors and a general medical condition: In this subtype the experienced pain is considered to result from both psychological factors and some medical condition that could cause pain. In either cases of the subtypes, the pain disorder may be acute ( duration of less than six months) or chronic (duration of over six months). The disorder is diagnosed more frequently in women than in men and is commonly found among patients at pain clinics. It is frequently comorbid with anxiety and/or mood disorders, which may occur first, or may arise later, as a consequence of the pain disorder( APA, 20000).
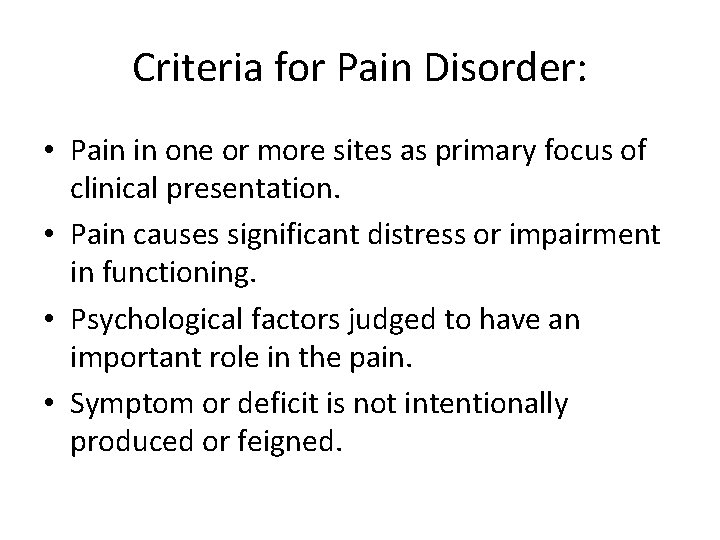
Criteria for Pain Disorder: • Pain in one or more sites as primary focus of clinical presentation. • Pain causes significant distress or impairment in functioning. • Psychological factors judged to have an important role in the pain. • Symptom or deficit is not intentionally produced or feigned.
Characteristics of Patients with Pain Disorder: • They are often unable to work or to perform the usual daily chores. • They sometimes declare themselves under disability. • Their resulting inactivity (including an avoidance of physical activity) and social isolation may lead to depression and to a loss of physical strength and endurance. • This fatigue and loss of strength can then exacerbate the pain in a kind of vicious cycle (Bouman et al, 1999). • The behavioural component of pain increases when it is reinforced by attention, sympathy, or avoidance of unwanted activities. • Such individuals also repeatedly seek new doctors in the hope of getting medical confirmation of their pain or to obtain medication to relieve their suffering.
Body Dysmorphic Disorder: • • • Criteria: Preoccupation with some perceived or imagined defect or defects in appearance. If slight physical anomaly is present, person’s concern is markedly excessive. Preoccupation is so intense as to cause clinically significant distress and/or impairment in social or occupational functioning. Features: Although not necessary for diagnosis, BDD patients often have compulsive checking behaviours (eg. checking their appearances in the mirror excessively or hiding or repairing a perceived flaw). Another common symptom is avoidance of usual activities because of fear that other people will see the imaginary defect and be repulsed. People with BDD may focus on any one or more than one body parts; their skin having blemishes, breasts too small, face too thin (or too fat) or disfigured by visible blood vessels that others find repulsive, etc. The more common locations for perceived defects include the skin, hair, nose, eyes, legs, chin, breasts/chest, stomach, lips, body build and face size /shape (Phillips, 2005). Their concerns about their body parts are extreme, often leading to complete preoccupation and significant emotional pain. About half of BDD patients have concerns about their appearance that are of delusional intensity (Allen and Hollander, 2004).
Body Dysmorphic Disorder: • • • In severe cases, they may become so isolated that they lock themselves up in their house and never go out even to work, with the average employment rate at about 50% (Neziroglu et al, 2004). The other people do not even see the defects, or see a very minor flaw within the normal range. The BDD patients seek constant reassurance from friends and family about their defects , but they provide them with only temporary relief. Some may seek reassurance by checking mirrors countless times in a day, while others may avoid mirrors completely. They frequently engage in excessive grooming behaviour, often trying to camouflage their perceived defects through hairstyles, clothing, or makeup (Sarwer et al, 2004). The age of onset is usually adolescence, with prevalence approximately equal in men and women. Suicide attempts, or successful suicide cases, along with a depressive diagnosis are often found. Rates of comorbid social phobia and OCD are also quite substantial. Sufferers often seek cosmetic medical treatments, but is usually not satisfied with the treatment outcome. They do not visit a psychiatrist or psychologist usually.

Illness Anxiety Disorder: • Characterised by a preoccupation with being sick or with developing a disease of some kind. • It is a variant of somatic symptom disorder or hypochondriasis. • In this disorder, there a few, or no somatic symptoms and the patients are primarily concerned with the idea, that they are ill. • The diagnosis may also be applicable for those with a medical illness, but whose anxiety is out of proportion to their diagnosis and who assume the worst possible outcome imaginable.
Psychological Factors Affecting Other Medical Conditions: • • • This category covers physical disorders caused by, or adversely affected by, emotional or psychological factors. Examples include gastrointestinal disturbances, like peptic ulcer, cardiovascular or respiratory system disorders, etc. A medical condition must always be present for a diagnosis to be made. Its diagnostic criteria exclude the following: (1) Classic mental disorders that have physical symptoms as part of the disorder(eg. conversion disorder, in which a physical symptom is produced by psychological conflict). (2) Somatization disorder, in which the physical symptoms are not based on organic pathology. (3) Hypochondriasis, in which patients have an exaggerated concern with their health. (4) Physical complaints that are frequently associated with mental disorders. (5) Physical complaints associated with substance-related disorders (eg. coughing due to nicotine dependency)
Factitious Disorder: • • • Factitious Disorder: Such patients simulate, induce, or aggravate illness to receive medical attention, regardless of whether or not they are ill. They may inflict painful, deforming, or life-threatening injury on themselves, their children, or other dependents. The person intentionally produces psychological or physical symptoms (or both), even undergoing repeated hospitalisations, but there are no external incentives. The patients often surreptitiously alter their physiology (eg. by taking drugs) in order to simulate various real illnesses. They may be at risk for serious injury or death and may even need to be committed to an institution for their own protection. Criteria for Factitious Disorder: Intentional production or feigning of physical or psychological signs and symptoms. Motivation for the behaviour is to assume a sick role. There are no external incentives for the behaviour; like economic gain or avoiding legal responsibilities, as seen in Malingering.
Other Specified or Unspecified Somatic Symptom Disorder: • • This DSM-V category is used to describe conditions characterised by one or more unexplained physical symptoms of at least 6 months’ duration, which are below the threshold for a diagnosis of somatic symptom disorder. The symptoms are not caused, or fully explained, by another medical, psychiatric, or substance abuse disorder, and they cause clinically significant distress or impairment. Two types of symptom patterns may be seen in patients with other specified or unspecified somatic symptom disorder; those involving the ANS and those involving sensations of fatigue or weakness. In what is sometimes referred to as the autonomic arousal disorder, some patients are affected with symptoms that are limited to bodily functions innervated by the ANS. Such patients have complaints involving the cardiovascular, respiratory, gastrointestinal, urogenital. and dermatological systems. Other patients complain of mental and physical fatigue, physical weakness and exhaustion, and inability to perform many everyday activities because of their symptoms. A few examples are neurasthenia, pseudocyesis, etc.
Conversion Disorder: • • Conversion disorder, or functional neurological symptom disorder(as per DSM-V) is an illness of symptoms or deficits that affect voluntary motor or sensory functions, which suggest another medical or neurological condition, but that is judged to be caused by psychological factors because the illness is preceded by conflicts or other stressors. The symptoms or deficits are not intentionally produced and are not caused by substance use, are not limited to pain or sexual symptoms. The gain is primarily psychological and not social, monetary, or legal. The symptoms usually start or are exacerbated by preceding emotional or interpersonal conflicts , or stressors. The term conversion was introduced by Sigmund Freud, who, based on his work with Anna O, hypothesized that the symptoms of conversion disorder reflect unconscious conflicts, stemming from repressed sexual energy (eg. feelings of guilt about the desire to masturbate may be solved by developing a paralyzed hand). This syndrome was originally combined with somatization disorder and was referred to as hysteria, conversion reaction, or dissociative reaction. Paul Briquet and Jean-Martin Charcot contributed to the development of the concept of conversion disorder by noting the influence of heredity on the symptom and the common association with a traumatic event.
Criteria for Conversion Disorder: • • • One or more symptoms affecting voluntary motor or sensory function that suggest a neurological or other medical condition. Psychological factors judged to be associated with the symptoms because they were preceded by conflicts or other stressors. Symptom or deficit cannot be fully explained by a general medical condition. Symptom or deficit causes distress or impairment in functioning. Finally, the person must not intentionally produce or fake the symptoms. A few typical examples of symptoms include: partial paralysis blindness deafness pseudoseizures. Distinguishing Malingering from Conversion Disorder: In malingering, unlike conversion disorder, the person is intentionally producing or grossly exaggerating physical symptoms and is motivated by external incentives like avoiding work or military service, obtaining financial compensation, or evading criminal prosecution.
Clinical Picture of Conversion Disorder: • Paralysis, blindness and mutism are the most common symptoms. • The disorder may be most commonly associated with passiveaggressive, dependent, antisocial and histrionic personality disorders. • The range of symptoms is as diverse as the physically based ailments. There are four categories of symptoms: • (1) Sensory Symptoms or Deficits: • Anaesthesia and paresthesia are common, especially of the extremities. • All sensory modalities can be involved, and the distribution of the disturbance is usually inconsistent with either central or peripheral neurological disease. • The symptoms may involve the organs of special sense.
Clinical Picture of Conversion Disorder: • The sensory deficits in the different systems are: • Visual: blindness and tunnel vision (though blind, the person is often able to navigate successfully across a room). • Auditory: deafness (the person orients oneself upon hearing one’s name) • Tactile: sensitivity to feeling, or anaesthesia, where a person loses feeling in a part of the body ( eg. stocking-and-glove anaesthesia), with the loss of sensation having no anatomical sense. • The symptoms can be unilateral or bilateral, but neurological evaluation reveals intact sensory pathways. • In conversion disorder blindness, for example, the patient walks around without collision or self-injury, their pupils react to light, and their corticalevoked potentials are normal. • Various case studies reveal that in conversion disorder, the sensory input is registered but that is somehow screened from explicit conscious recognition.
Clinical Picture of Conversion Disorder: • • • (2)Motor Symptoms or Deficits: It includes abnormal movements, gait disturbance, weakness and paralysis. Gross rhythmical tremors, choreiform movements, tics and jerks may be present. The movements generally worsen when attention is called to them. One gait disturbance is astasia-abasia, which is widely ataxic, staggering gait, accompanied by gross, irregular, jerky truncal movements and thrashing and waving arm movements. Patients with the symptom rarely fall and even if they do, they are generally not injured. Other common motor disturbances are paralysis and paresis involving one, two, or all four limbs, although distribution of the involved muscles does not conform to the neural pathways. Reflexes remain normal, the EMG findings are normal. The patients have no fasciculations or muscle atrophy, except after long-standing conversion paralysis. Conversion paralysis is usually confined to a single limb such as an arm or a leg. The loss of function is usually selective (eg. the person is unable to write, but is able to use the same muscle for scratching, or able to walk only in an emergency situation, etc).

Clinical Picture of Conversion Disorder: • • Aphonia: one of the most common speech-related conversion disturbances, when a person is able to talk only in a whisper, although he/she can cough in a normal manner. Another common motor symptom is difficulty swallowing or the sensation of a lump in the throat. (3)Seizures: Tongue biting, urinary incontinence, and injuries after falling can occur, although those symptoms are generally not present in conversion seizures or pseudoseizures. They resemble epileptic seizures to some extent, but such patients do not show any EEG abnormalities, or any confusion or loss of memory afterward, unlike the latter. Moreover, such patients often show excessive thrashing about and writhing not seen with true seizures, and they rarely injure themselves in falls or lose control over their bowels and bladder, unlike patients with true seizures. However, about one third of patients with pseudoseizures also have a coexisting epileptic disorder. Pupillary and gag reflexes are retained after pseudoseizure and patients have no postseizure increase in prolactin concentration.
Clinical Picture of Conversion Disorder: • • • (4)Mixed presentation from the first three categories: The various symptoms from the previous three categories are present in combination. Other Associated Features: Several psychological symptoms have also been associated with conversion disorder. Freud’s astute clinical observations about primary and secondary gains are still incorporated into contemporary views of conversion disorder. • • • Primary Gain: this refers to continued escape or avoidance of a stressful situation The symptoms have a symbolic value; they represent an unconscious psychological conflict. The physical manifestation of symptoms provide a plausible excuse, enabling an individual to escape or avoid an intolerably stressful situation without having to take responsibility for doing so. Patients achieve primary gain by keeping internal conflicts outside their awareness, or by neutralizing intrapsychic conflict. • • • Secondary Gain: patients gain tangible advantages and benefits as a result of being sick ; like being excused from obligations and difficult life situations, receiving support and assistance that might not otherwise be forthcoming, and controlling other person’s behaviour. It enables patients to gain attention from loved ones or financial compensation, that tends to reinforce the maintenance of disability.

Clinical Picture of Conversion Disorder: • La Belle Indifference: it refers to a patient’s attitude of inappropriate lack of concern toward serious symptoms; the patient seems unconcerned about what appears to be a major impairment. • The presence or absence of this symptom is not pathognomonic of conversion disorder, but is often associated with the condition. • Identification: patients may unconsciously model their symptoms on those of someone important to them. • For example a parent or a person who has recently died may serve as a model for conversion disorder. • During pathological grief reactions bereaved persons commonly have symptoms of the disease.
Important Issues in Diagnosis: • • • Since the symptoms of conversion disorder can simulate a variety of medical conditions, accurate diagnosis is often difficult. It is crucial for the suffering person to receive a thorough medical and neurological examination. During World Wars, conversion disorder was one of the most frequently diagnosed psychiatric syndromes among soldiers, when it occurred under highly stressful combat conditions in men, who would ordinarily be considered stable. At present, it is more prevalent among the rural and low socioeconomic background population who are medically unsophisticated. The disorder is more prevalent among women compared to men. It most commonly occurs in early adolescence or early adulthood. It generally has a rapid onset after a significant stressor and often resolves within two weeks if the stressor is removed, although it commonly recurs. In many cases, it has a more chronic course. It frequently occurs along with other disorders like major depression, anxiety, somatization and dissociative disorders. Neurological disorders (eg. dementia and other degenerative diseases), brain tumors and basal ganglia disease must be considered in differential diagnosis.
Aetiology of Conversion Disorder: • Psychoanalytic Theory: • It suggests that conversion disorder is caused by repression of unconscious, intrapsychic conflict and conversion of anxiety into a physical symptom. • The conflict is between an instinctual impulse (eg. aggression or sexuality) and the prohibitions against its expression. • The symptoms allow partial expression of the forbidden wish or urge, but disguise it, so that patients can avoid consciously confronting their unacceptable impulses. • Hence, the symptom has a symbolic relation to the unconscious conflict (eg. vaginismus protects the patient from expressing unacceptable sexual wishes). • The symptoms also allow patients to communicate that they need special consideration and special treatment. Such symptoms may function as a nonverbal means of controlling or manipulating others.
Aetiology of Conversion Disorder: • • Learning Theory: In terms of conditioned learning theory, a conversion symptom can be seen as a piece of classically conditioned learned behaviour. The symptoms of illness learned in childhood, are called forth as a means of coping with an otherwise impossible situation. Biological Factors: Increasing data implicate biological and neuropsychological factors in the development of conversion disorder symptoms. Preliminary brain-imaging studies have found hypometabolism of the dominant hemisphere and hypermetabolism of the nondominant hemisphere and have implicated impaired hemispheric communication in the cause of the disorder. The symptoms may be caused by an excessive cortical arousal that sets off negative feedback loops between the cerebral cortex and the brainstem reticular formation, which in turn inhibit the patient’s awareness of bodily sensation, which may explain the observed sensory deficits in them. Neuropsychological tests sometimes reveal subtle cerebral impairments in verbal communication, memory, vigilance, affective incongruity and attention in such patients.
Treatment of Conversion Disorder: • Resolution of the symptoms are often spontaneous, although it is facilitated by insight-oriented supportive or behaviour therapy. • The most important feature of therapy is a relationship with a caring and confident therapist. • With resistant patients, physicians may suggest stress and coping focused psychotherapy. • Hypnosis, anxiolytics and behavioural relaxation exercises are effective in some cases. • Psychodynamic approaches include psychoanalysis and insight-oriented psychotherapy, in which patients explore intrapsychic conflicts and the symbolism of the conversion disorder symptoms. • Brief and direct forms of short-term psychotherapy have also been used to treat conversion disorder. • The longer the duration of these patients’ sick role and the more they have regressed, the more difficult is the treatment.
 Nursing care plan for somatoform disorder
Nursing care plan for somatoform disorder What is neurosis disorder
What is neurosis disorder Somatoform disorders
Somatoform disorders Neurosis
Neurosis Somatoform disorder
Somatoform disorder Gangguan somatoform
Gangguan somatoform Hyperventilation treatment
Hyperventilation treatment Epidemiologi gangguan somatoform
Epidemiologi gangguan somatoform Types of sensory disorders
Types of sensory disorders Anticholinergic rhyme
Anticholinergic rhyme Types of dissociative disorders
Types of dissociative disorders Dissociative amnesia
Dissociative amnesia Moltiplicazioni con numeri periodici
Moltiplicazioni con numeri periodici Coop per me e per te
Coop per me e per te Mio diletto
Mio diletto Pats joja kojos uz ausu
Pats joja kojos uz ausu 27 miles per gallon into kilometers per liter
27 miles per gallon into kilometers per liter Why is a minute 60 seconds
Why is a minute 60 seconds 1.800 dam/jam = hm/menit
1.800 dam/jam = hm/menit Per stirpes v per capita
Per stirpes v per capita Multas per gentes et multa per aequora vectus
Multas per gentes et multa per aequora vectus Longum iter est
Longum iter est Per capita vs per stirpes
Per capita vs per stirpes Multās per gentēs et multa per aequora vectus
Multās per gentēs et multa per aequora vectus What are physiological disorders health and social care
What are physiological disorders health and social care Unit 14 business level 3
Unit 14 business level 3 Neurocognitive disorders
Neurocognitive disorders Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders The flinders model
The flinders model Assistive technology for behavior
Assistive technology for behavior Ego dystonic
Ego dystonic