Chapter 166 General Approach to the Pediatric Patient






































- Slides: 107
Chapter 166. General Approach to the Pediatric Patient 2018. 3. 29 정재윤
DISTINGUISHING PRINCIPLES OF DISEASE TEMPERATURE REGULATION AIRWAY CARDIOVASCULAR MUSCULOSKELETAL IMMUNOLOGIC PHARMACOLOGIC


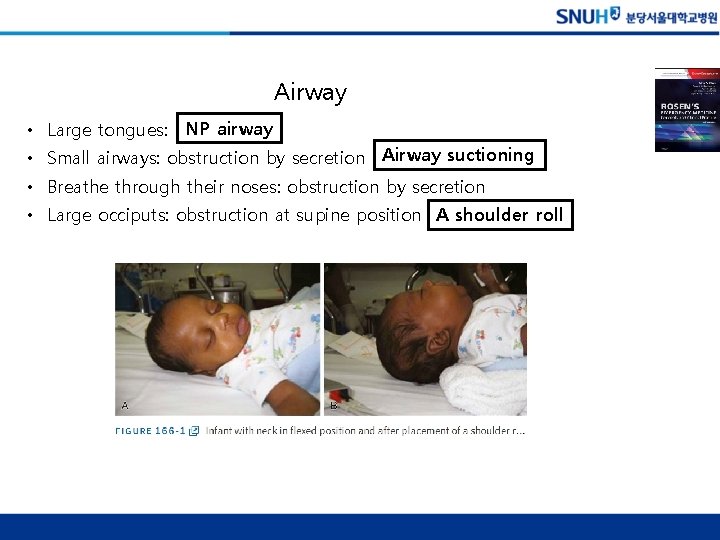
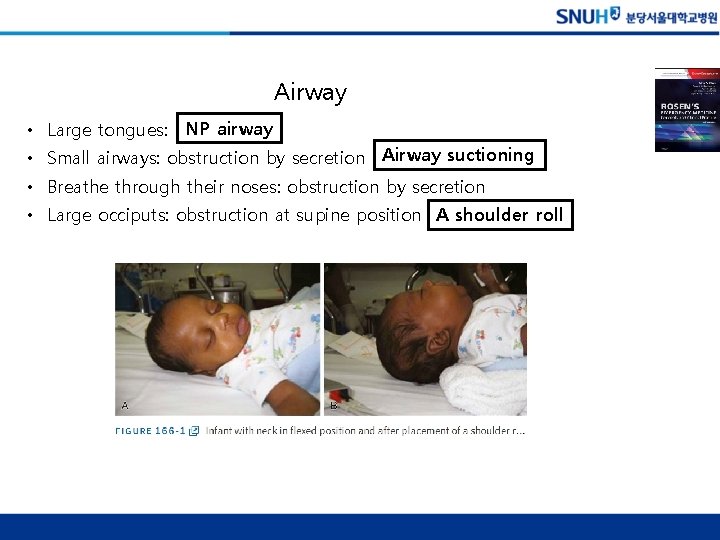
Airway • Large tongues: NP airway • Small airways: obstruction by secretion Airway suctioning • Breathe through their noses: obstruction by secretion • Large occiputs: obstruction at supine position A shoulder roll
Cardiovascular • Heart rate – Tachycardia: fever, anxiety, pain, or fear, cardiovascular compromise의 early sign – Bradycardia: cardiopulmonary failure and impending cardiac arrest. – 반복측정이 중요하다 – Pulse는 약한데 tachycardia가 있으면 shock state라고 고려해야 한다 • Blood pressure – Compensatory mechanism: increased HR, systemic vascular resistance – Hypotension은 shock의 late finding

Immunologic and pharmacologic • Immunologic – Immature immune system – Prone to infection – < 1 moth with fever: SBI risk up to 10% full sepsis w/u • Pharmacologic – Weight based dosing – Medication errors: frequent • Simple calculation mistakes • Scale mistakes: pounds vs kilograms • Medication should not young infants but frequently prescribed to adults: ceftriaxone causing bilirubin encephalopathy
DEVELOPMENTAL YOUNG INFANTS (<12 MONTHS OF AGE) TODDLERS (1 - TO 2 -YEAR-OLDS) PRESCHOOLERS (3 - TO 5 -YEAR-OLDS) SCHOOL-AGE CHILDREN ADOLESCENTS

EVALUATION HISTORY PEDIATRIC ASSESSMENT TRIANGLE APPEARANCE WORK OF BREATHING CIRCULATION LENGTH-BASED RESUSCITATION TAPE PHYSICAL EXAMINATION

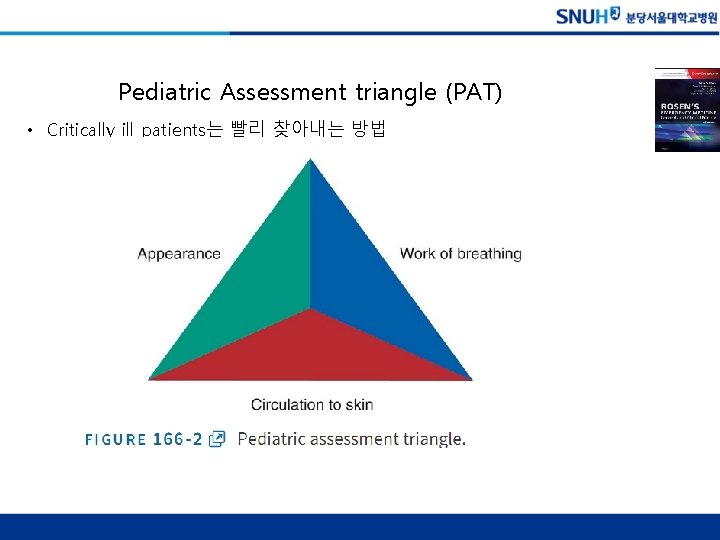
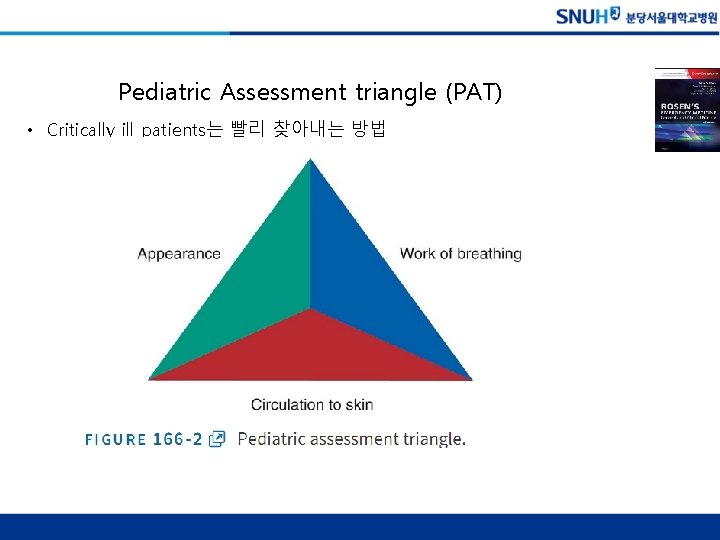
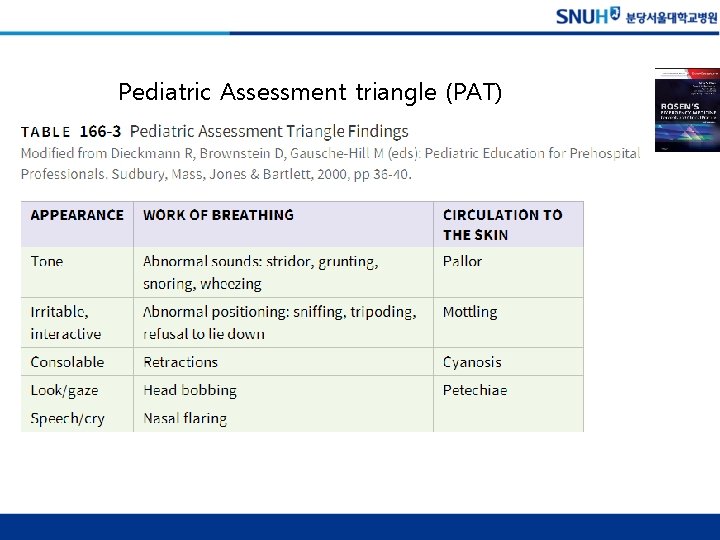
Pediatric Assessment triangle (PAT) • Critically ill patients는 빨리 찾아내는 방법
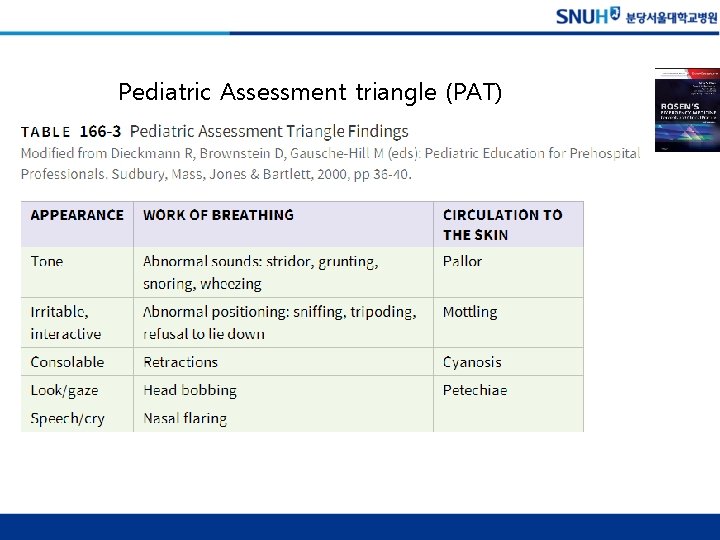
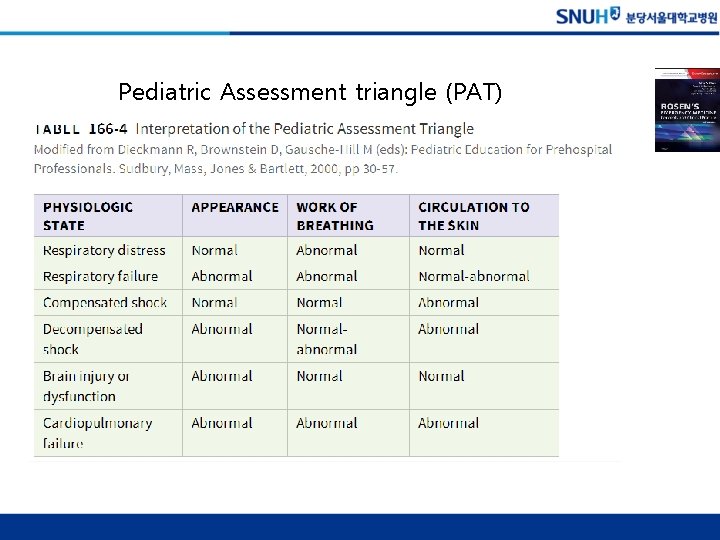
Pediatric Assessment triangle (PAT)
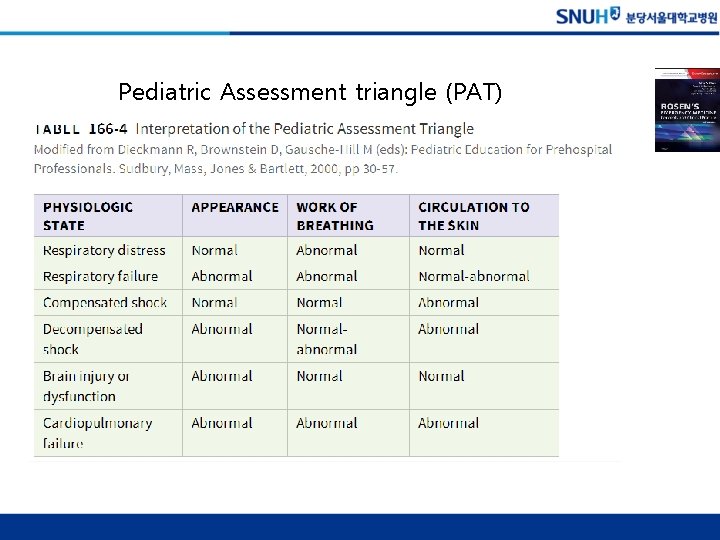
Pediatric Assessment triangle (PAT)
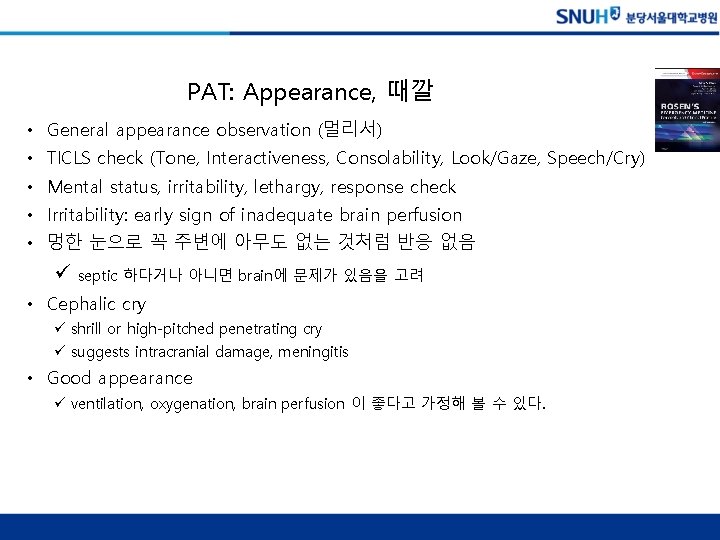
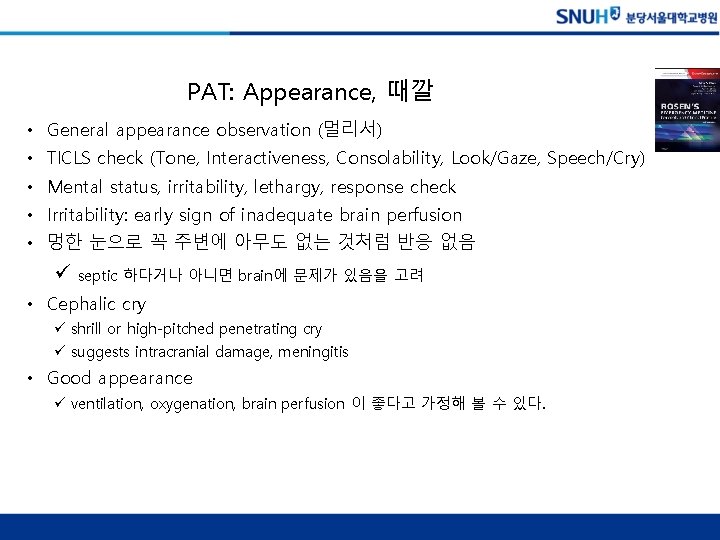
PAT: Appearance, 때깔 • General appearance observation (멀리서) • TICLS check (Tone, Interactiveness, Consolability, Look/Gaze, Speech/Cry) • Mental status, irritability, lethargy, response check • Irritability: early sign of inadequate brain perfusion • 멍한 눈으로 꼭 주변에 아무도 없는 것처럼 반응 없음 ü septic 하다거나 아니면 brain에 문제가 있음을 고려 • Cephalic cry ü shrill or high-pitched penetrating cry ü suggests intracranial damage, meningitis • Good appearance ü ventilation, oxygenation, brain perfusion 이 좋다고 가정해 볼 수 있다.
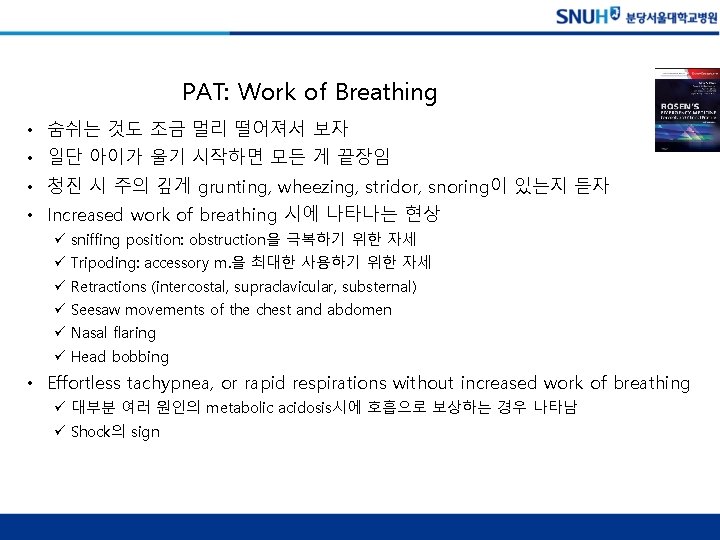
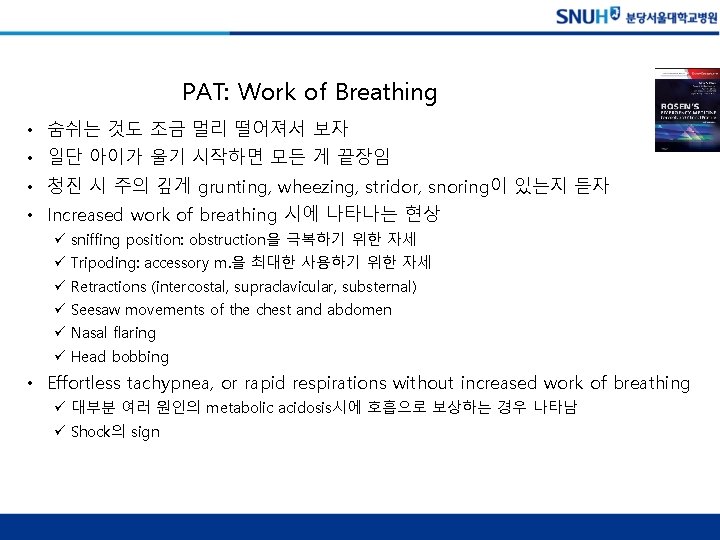
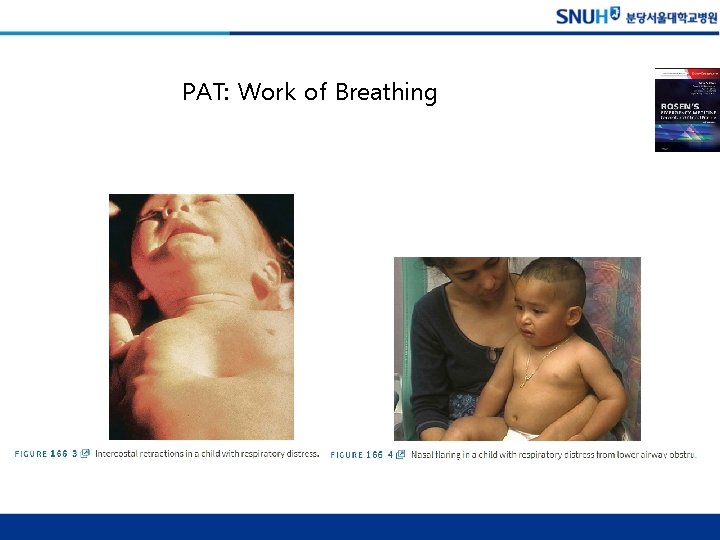
PAT: Work of Breathing • 숨쉬는 것도 조금 멀리 떨어져서 보자 • 일단 아이가 울기 시작하면 모든 게 끝장임 • 청진 시 주의 깊게 grunting, wheezing, stridor, snoring이 있는지 듣자 • Increased work of breathing 시에 나타나는 현상 ü sniffing position: obstruction을 극복하기 위한 자세 ü Tripoding: accessory m. 을 최대한 사용하기 위한 자세 ü Retractions (intercostal, supraclavicular, substernal) ü Seesaw movements of the chest and abdomen ü Nasal flaring ü Head bobbing • Effortless tachypnea, or rapid respirations without increased work of breathing ü 대부분 여러 원인의 metabolic acidosis시에 호흡으로 보상하는 경우 나타남 ü Shock의 sign
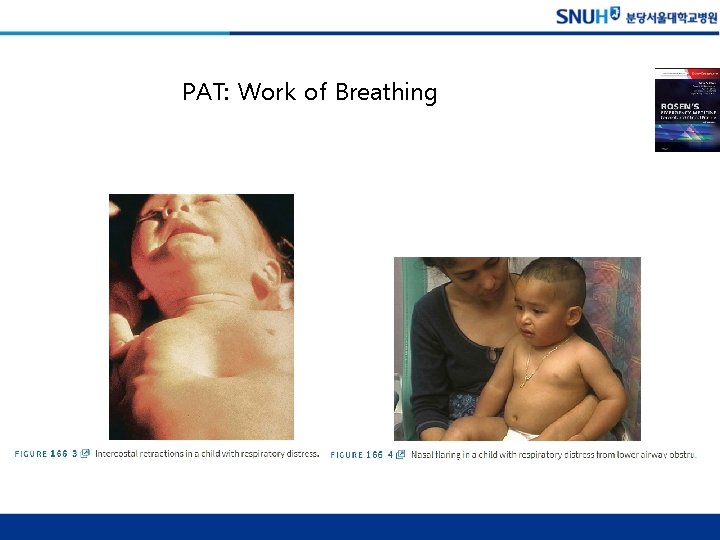
PAT: Work of Breathing

Length-Based Resuscitation Tape and physical exam • Length-Based Resuscitation Tape (Broselow tape) • Physical examination – Mental status 평가: GCS, AVPU – Order of examination (자극적이지 않은 것 부터) • 청진 귀, 입안 검사 – Tympanic membrane 검사 – Vaginal examination • 엄마 무릎 위, frog leg
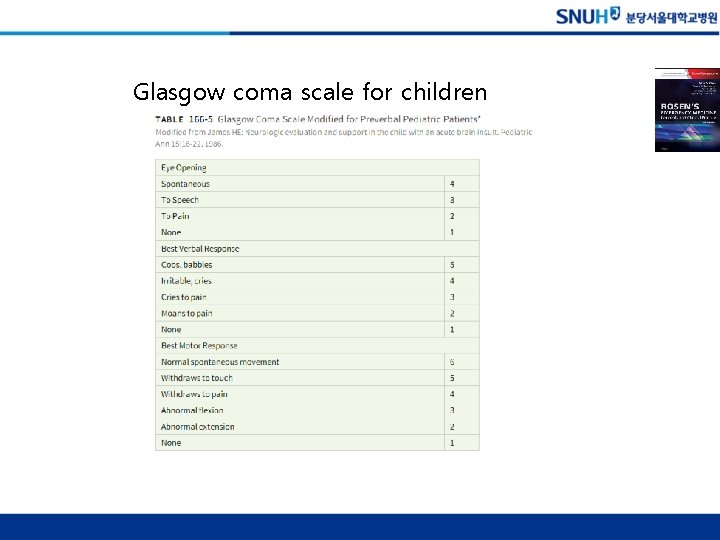
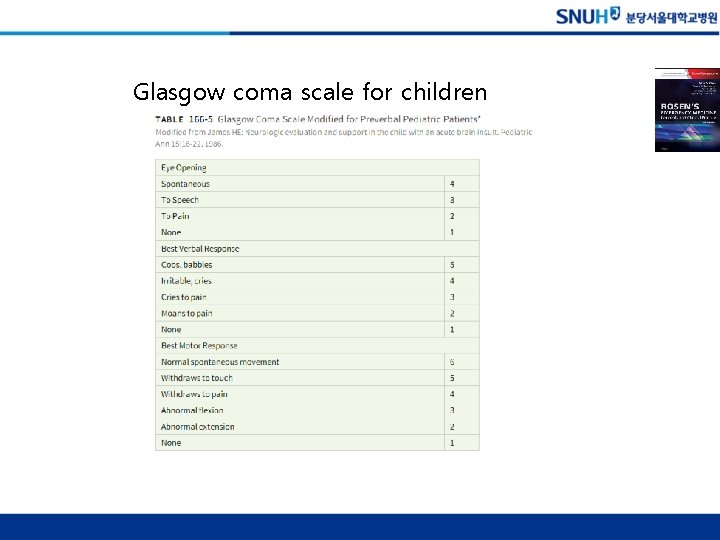
Glasgow coma scale for children
SPECIFIC DISORDERS CHILDREN WITH SPECIAL HEALTH CARE NEEDS NEONATAL INTENSIVE CARE UNIT GRADUATE ALTERED MENTAL STATUS SEIZURES TRAUMA CHILD ABUSE
NICU graduate • Premature baby: gestational age를 기준으로 발달력을 확인 • Increased respiratory infection compared with term infants • Chronic lung disease due to severe prematurity • History시 반드시 check 해야 함
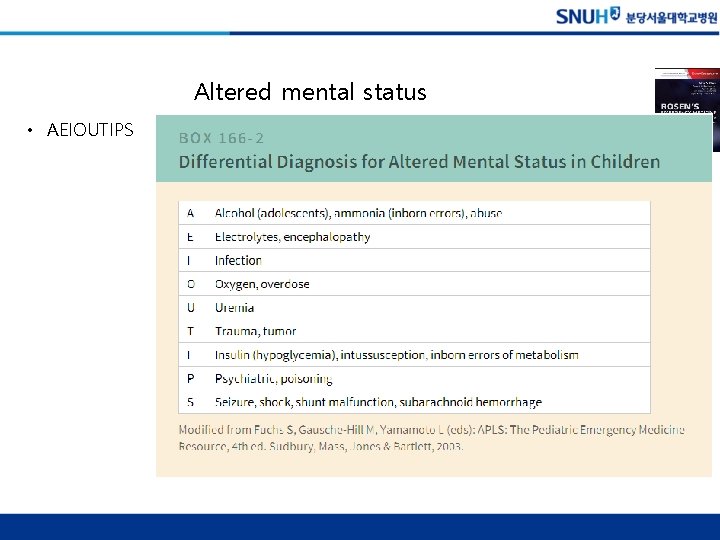
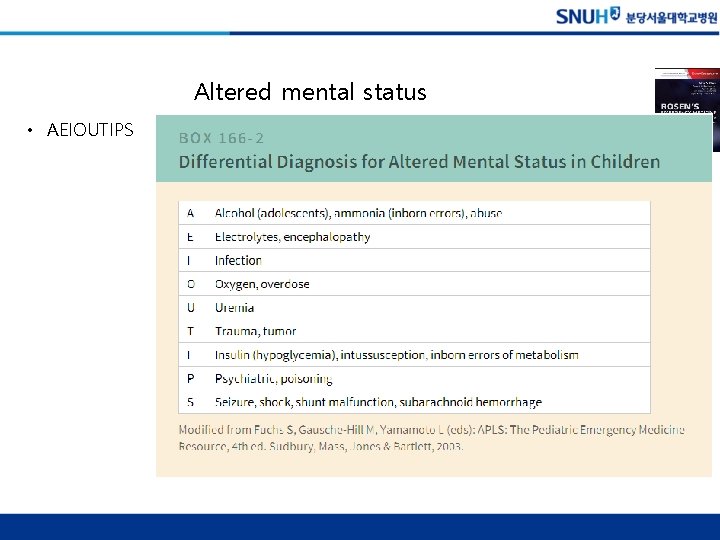
Altered mental status • AEIOUTIPS


Child abuse • 영아 진료 시 반드시 한번은 생각해야 보아야 할 문제 – Mechanism inconsistent with the injury – History inconsistent with the developmental level of the child (Box 166 -3). – Physical examination clues • Bruises in young infants • Bruises on certain areas of the body, such as the ear and trunk 24 (Box 166 -4). – Fractures in children younger than 18 months without a significant witnessed trauma mechanism
Chapter 106. Emergency Care of Children

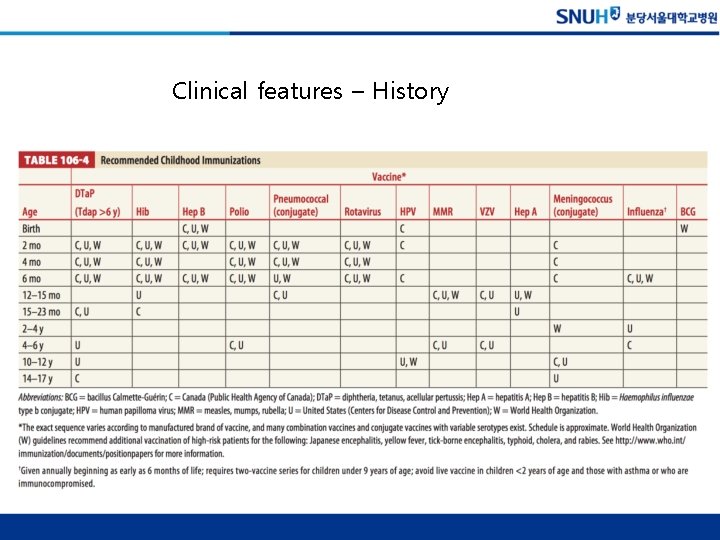
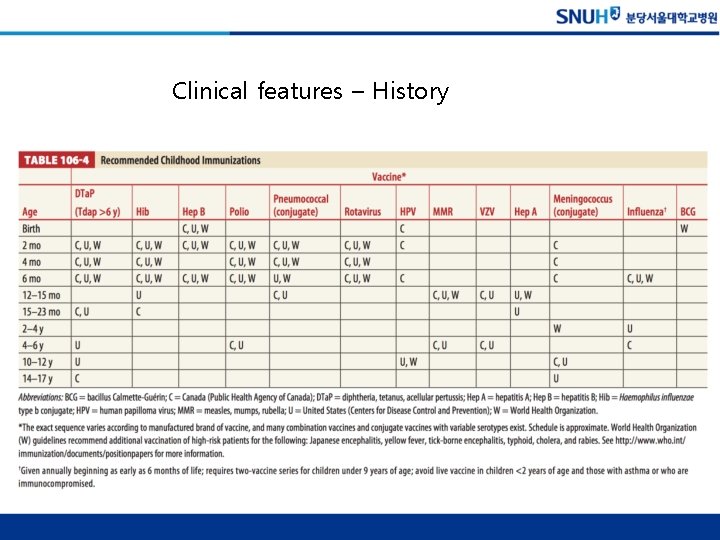
Clinical features – History
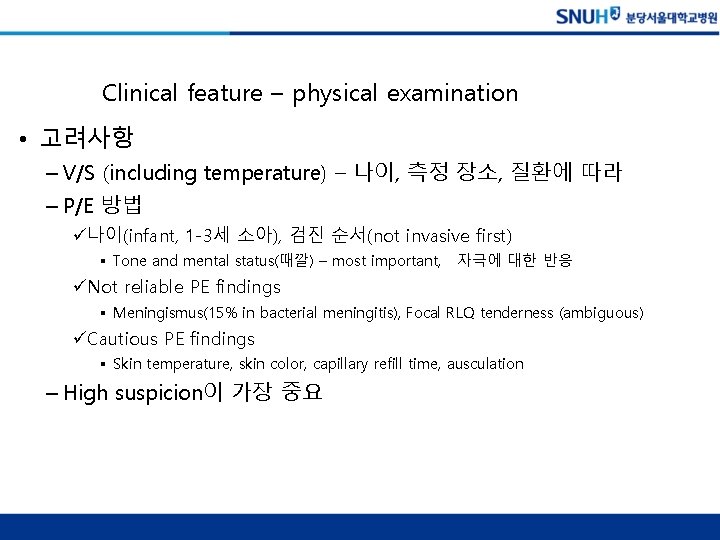
Clinical feature – physical examination • 고려사항 – V/S (including temperature) – 나이, 측정 장소, 질환에 따라 – P/E 방법 ü나이(infant, 1 -3세 소아), 검진 순서(not invasive first) § Tone and mental status(때깔) – most important, 자극에 대한 반응 üNot reliable PE findings § Meningismus(15% in bacterial meningitis), Focal RLQ tenderness (ambiguous) üCautious PE findings § Skin temperature, skin color, capillary refill time, ausculation – High suspicion이 가장 중요

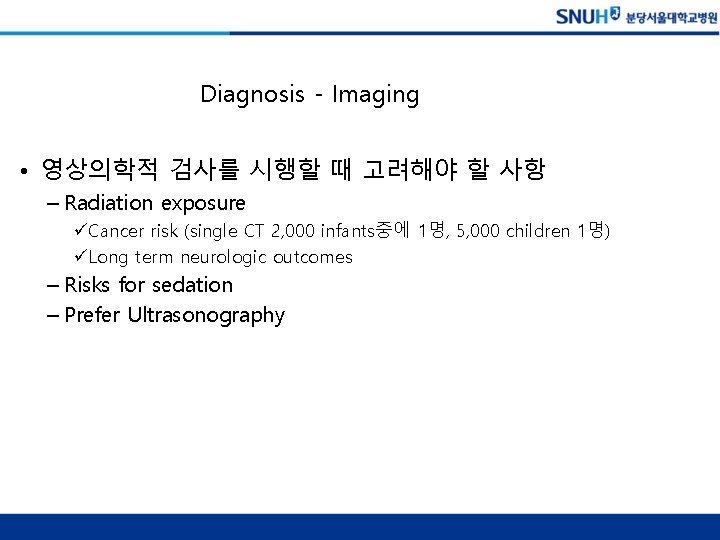
Diagnosis - Imaging • 영상의학적 검사를 시행할 때 고려해야 할 사항 – Radiation exposure üCancer risk (single CT 2, 000 infants중에 1명, 5, 000 children 1명) üLong term neurologic outcomes – Risks for sedation – Prefer Ultrasonography
Treatment • Special considerations – 나이 (신생아, 영아, 소아) – Hypotension (late phase에 나타남) – Respiratory arrest가 많다 – 약물 투여 (dosae for kilogram)

CHAPTER 112. INTRAVENOUS AND INTRAOSSEOUS ACCESS IN INFANTS AND CHILDREN


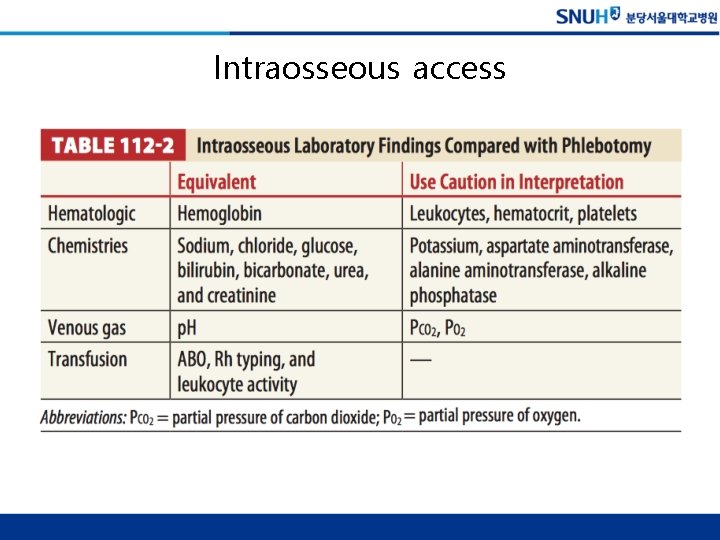
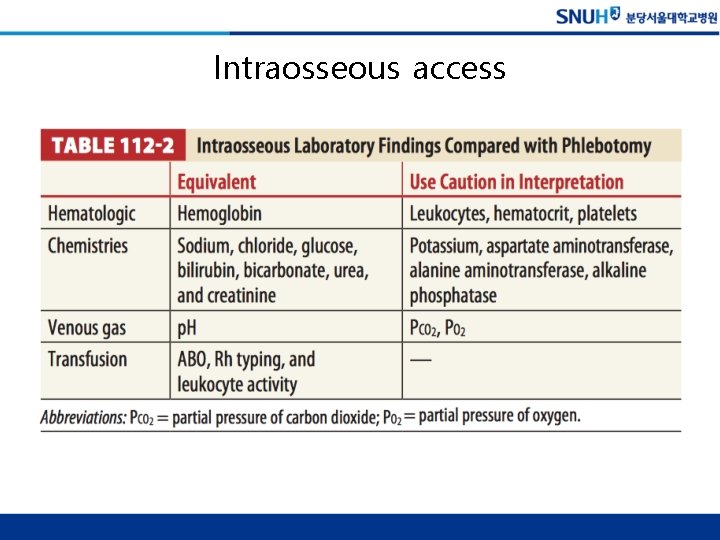
Intraosseous access
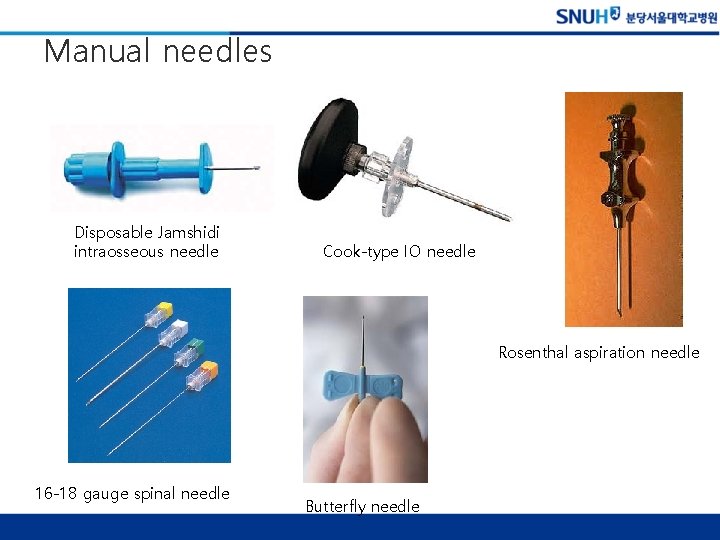
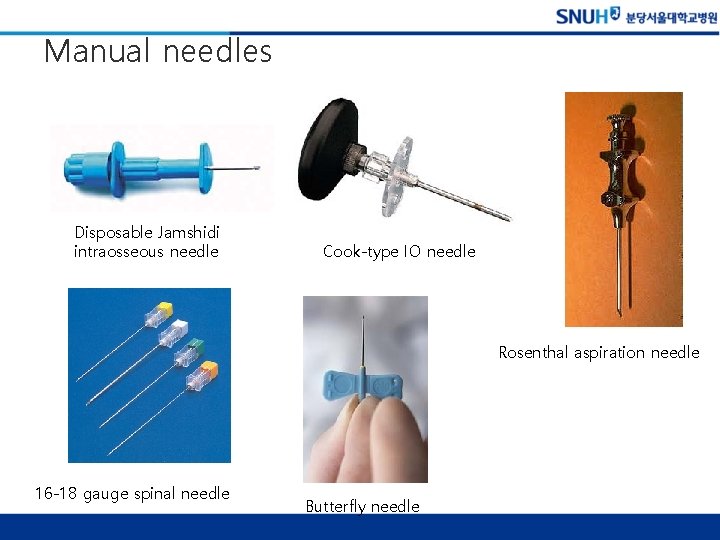
Manual needles Disposable Jamshidi intraosseous needle Cook-type IO needle Rosenthal aspiration needle 16 -18 gauge spinal needle Butterfly needle
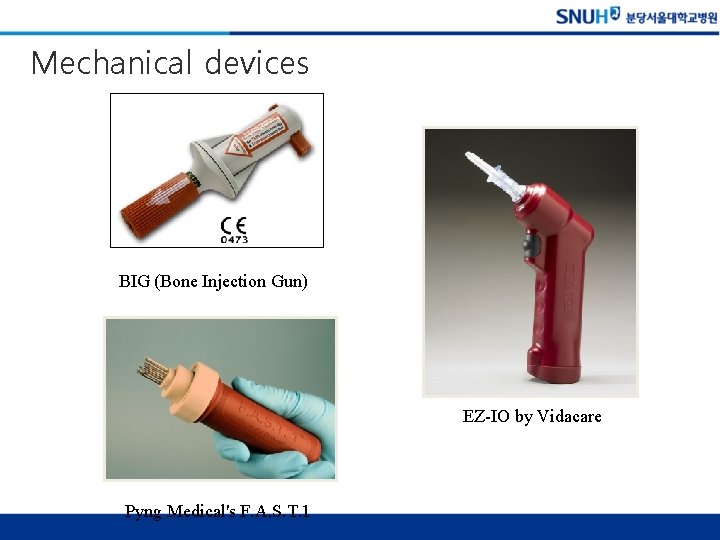
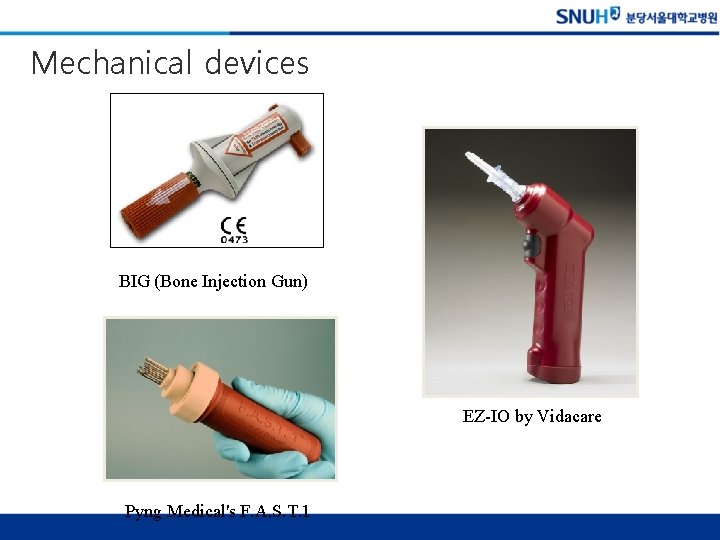
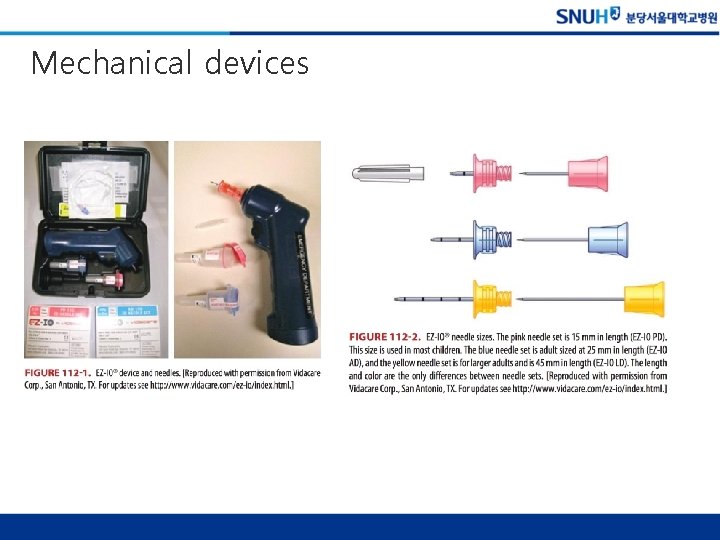
Mechanical devices BIG (Bone Injection Gun) EZ-IO by Vidacare Pyng Medical's F. A. S. T. 1
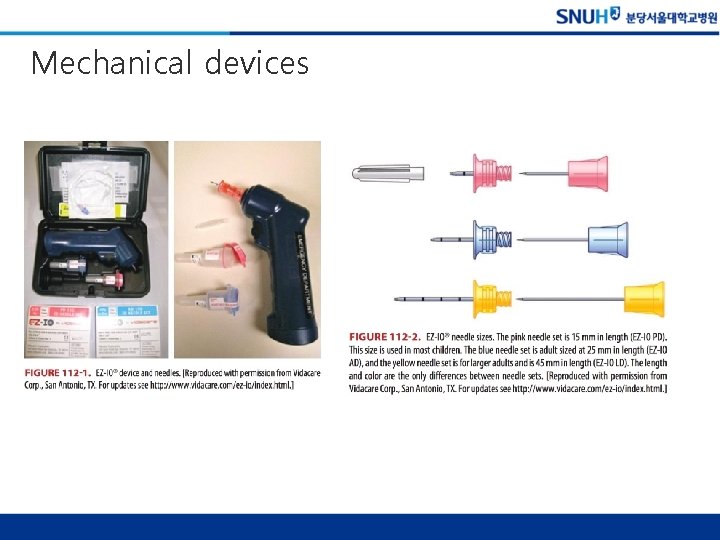
Mechanical devices
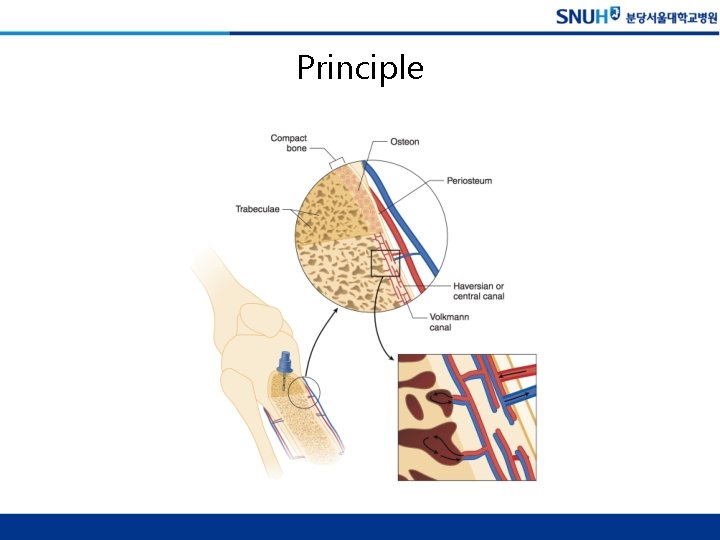
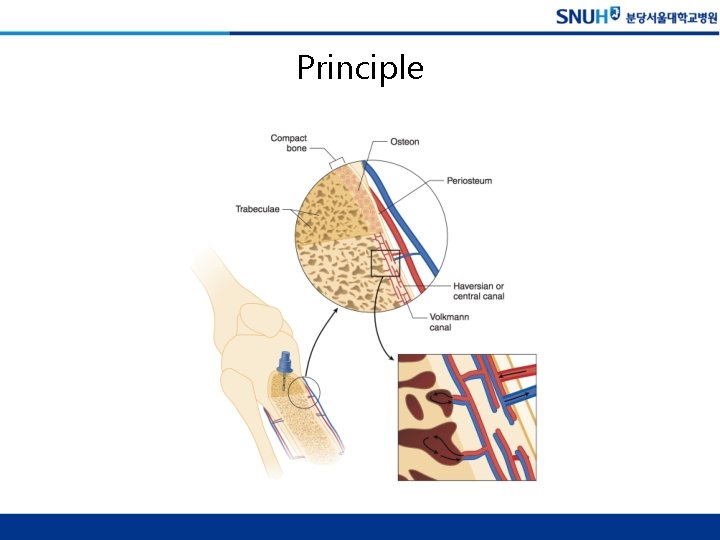
Principle
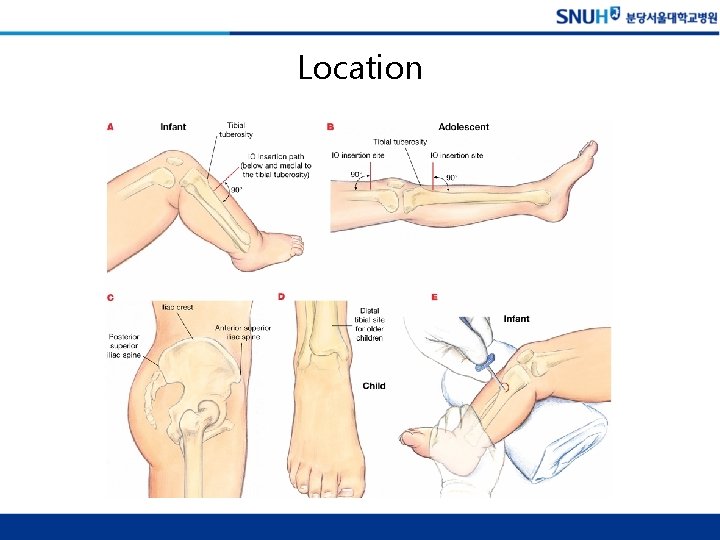
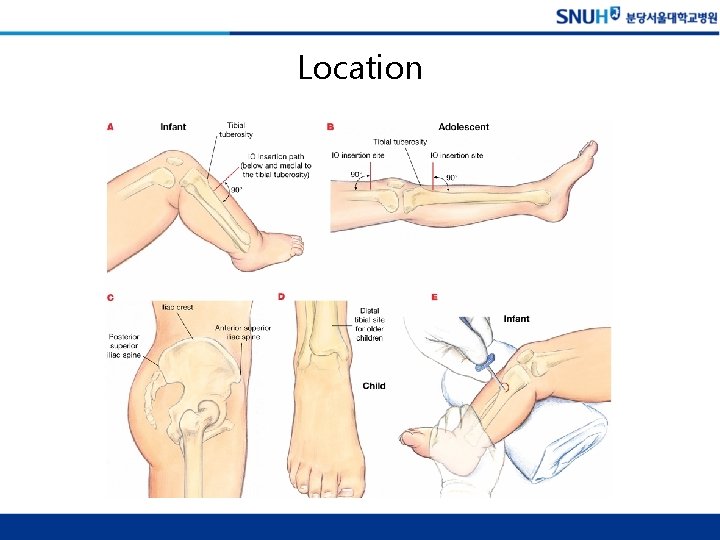
Location
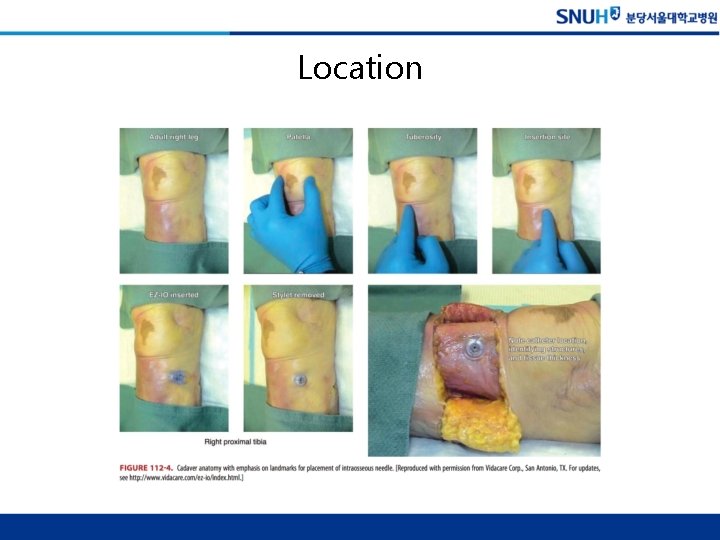
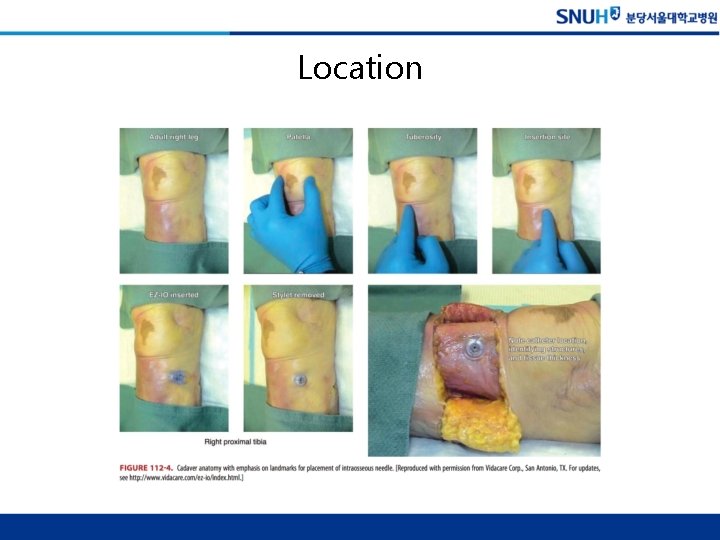
Location
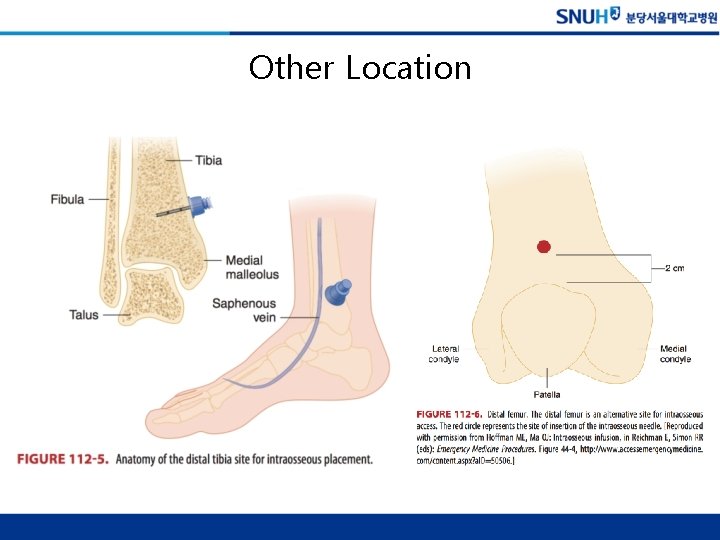
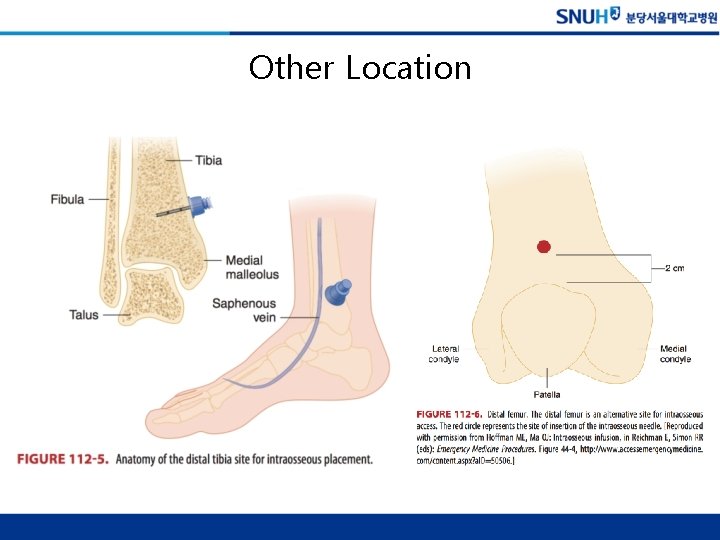
Other Location
New IO devices – BIG
New IO devices – EZ-IO

New IO devices – FAST 1
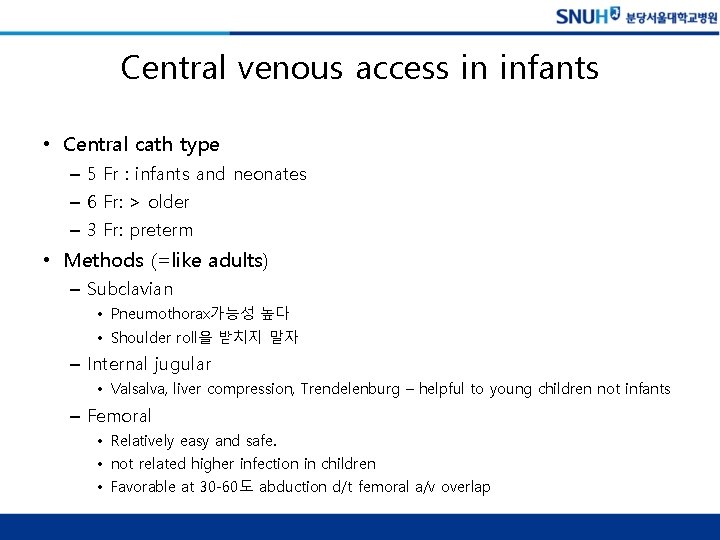
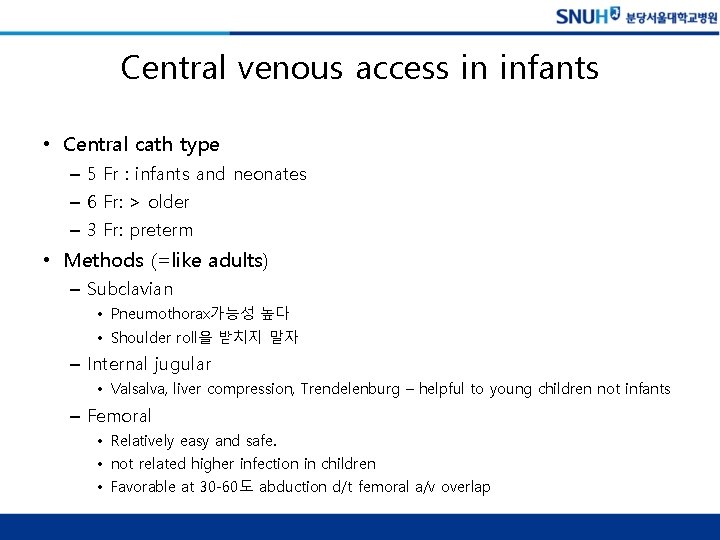
Central venous access in infants • Central cath type – 5 Fr : infants and neonates – 6 Fr: > older – 3 Fr: preterm • Methods (=like adults) – Subclavian • Pneumothorax가능성 높다 • Shoulder roll을 받치지 말자 – Internal jugular • Valsalva, liver compression, Trendelenburg – helpful to young children not infants – Femoral • Relatively easy and safe. • not related higher infection in children • Favorable at 30 -60도 abduction d/t femoral a/v overlap
Chapter 115. Sudden Infant Death Syndrome and Apparent Life-Threatening Event
SUDDEN INFANT DEATH SYNDROME


Pathophysiology • 아직 잘 모름 (현재까지 70개 이상의 이론이 있음) • 여러 가지 theories (mechanism에 대한 다양한 연구가 이루어지고 있다) ü 보호자에게 눌려 질식 ü Milk allergy ü Thymic enlargement ü Cardiac dysfunction including dysarrythmia ü medullary serotonergic pathology ü environmental stressors ü poverty, or prenatal exposure to cigarettes, alcohol, and illicit drugs ü genetic factors, male gender ü Sleep habit (supine prone)


APPARENT LIFE-THREATENING EVENT
Apparent Life-Threatening Event (ALTE) • 정의 – 보호자를 놀라게 하는 다음과 같은 event üApnea üColor change(cyanosis, pallor, or plethora) üChange in muscle tone (limp or stiff) üChoking or gagging • Incidence – Peak: 1주에서 2개월 사이 – 대부분 10주 이내에 발생 • Risk factors – RSV infection, prematurity, recent anesthesia – known gastroesophageal reflux or airway/maxillofacial anomalies

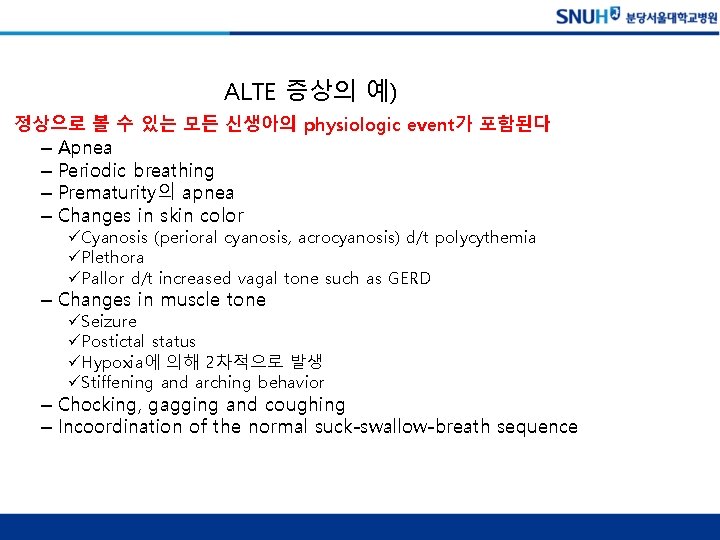
ALTE 증상의 예) 정상으로 볼 수 있는 모든 신생아의 physiologic event가 포함된다 – – Apnea Periodic breathing Prematurity의 apnea Changes in skin color üCyanosis (perioral cyanosis, acrocyanosis) d/t polycythemia üPlethora üPallor d/t increased vagal tone such as GERD – Changes in muscle tone üSeizure üPostictal status üHypoxia에 의해 2차적으로 발생 üStiffening and arching behavior – Chocking, gagging and coughing – Incoordination of the normal suck-swallow-breath sequence
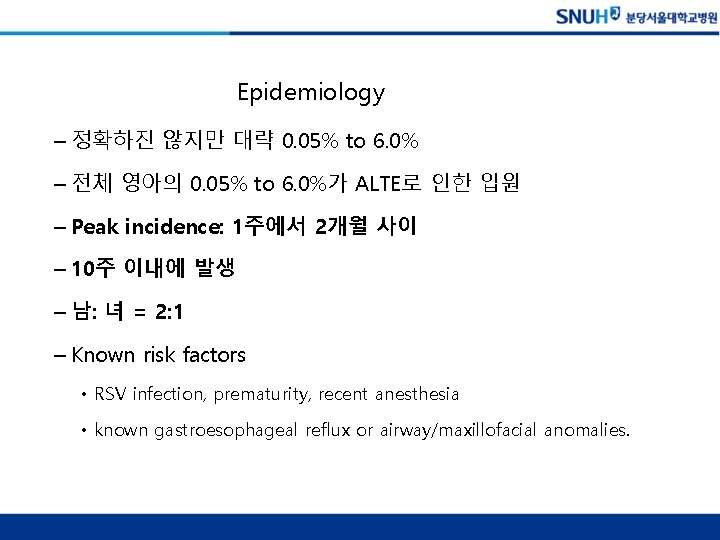
Epidemiology – 정확하진 않지만 대략 0. 05% to 6. 0% – 전체 영아의 0. 05% to 6. 0%가 ALTE로 인한 입원 – Peak incidence: 1주에서 2개월 사이 – 10주 이내에 발생 – 남: 녀 = 2: 1 – Known risk factors • RSV infection, prematurity, recent anesthesia • known gastroesophageal reflux or airway/maxillofacial anomalies.
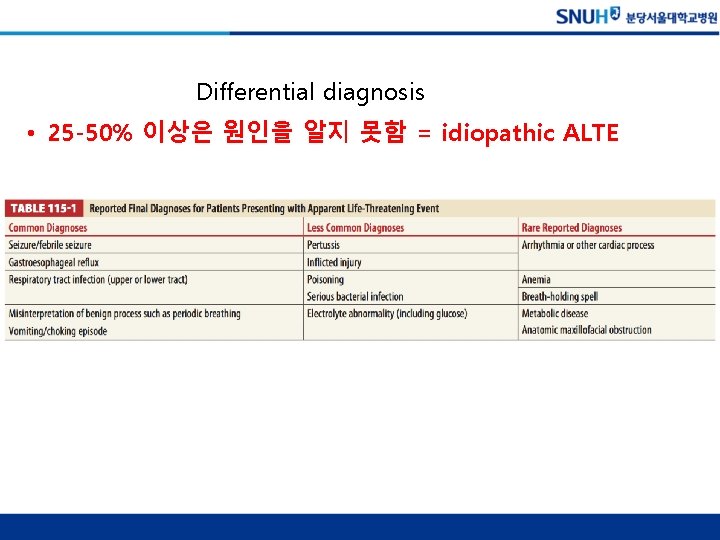
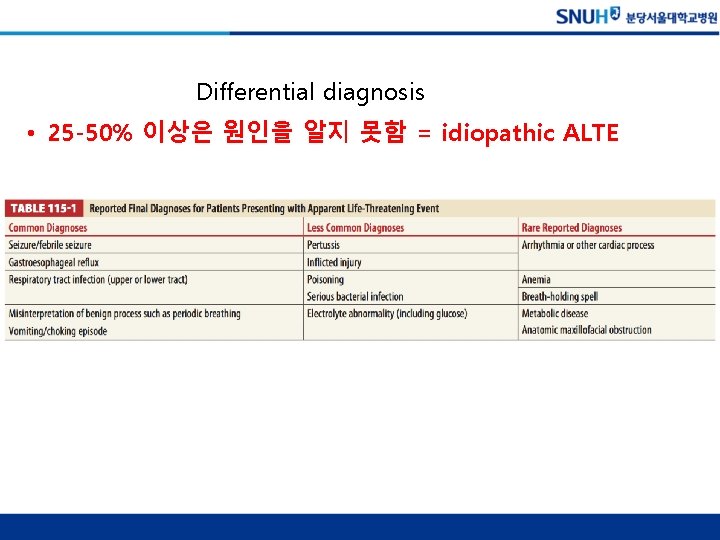
Differential diagnosis • 25 -50% 이상은 원인을 알지 못함 = idiopathic ALTE
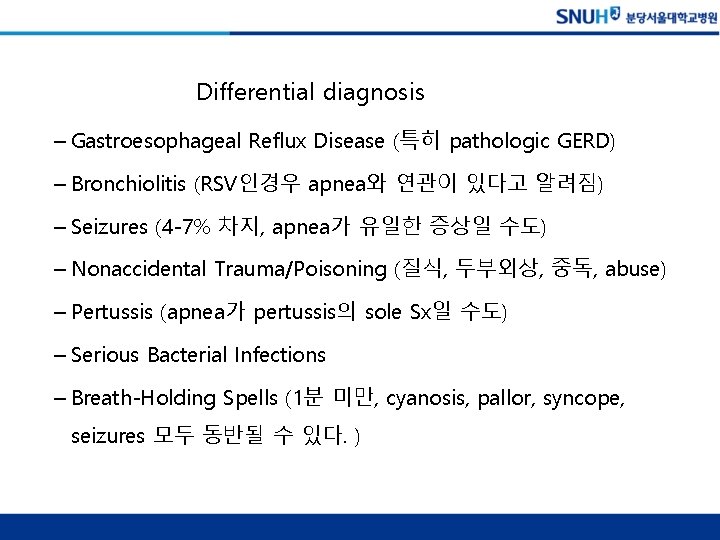
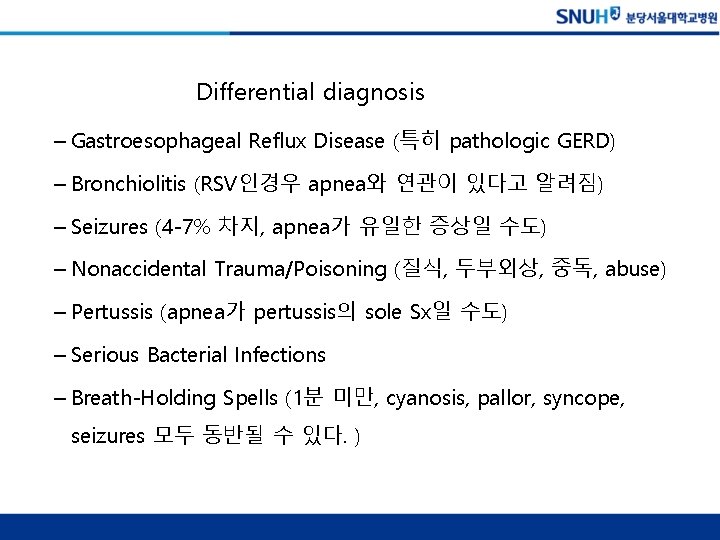
Differential diagnosis – Gastroesophageal Reflux Disease (특히 pathologic GERD) – Bronchiolitis (RSV인경우 apnea와 연관이 있다고 알려짐) – Seizures (4 -7% 차지, apnea가 유일한 증상일 수도) – Nonaccidental Trauma/Poisoning (질식, 두부외상, 중독, abuse) – Pertussis (apnea가 pertussis의 sole Sx일 수도) – Serious Bacterial Infections – Breath-Holding Spells (1분 미만, cyanosis, pallor, syncope, seizures 모두 동반될 수 있다. )

CHAPTER 111. NEONATAL EMERGENCIES AND COMMON NEONATAL PROBLEMS

NORMAL VEGETATIVE FUNCTIONS AND COMMON CONCERNS OF CAREGIVERS OF NORMAL INFANTS
Normal Vegetative Functions and Common Concerns of Caregivers of Normal Infants • 모든 신생아가 똑같을 순 없다. • Normal variants로 인해 부모들이 ER 방문이 많다 • 먹는 pattern, 체중 증가, 변, 피부, 호흡 등등








CONSIDERATIONS IN THE CRITICALLY ILL NEONATE
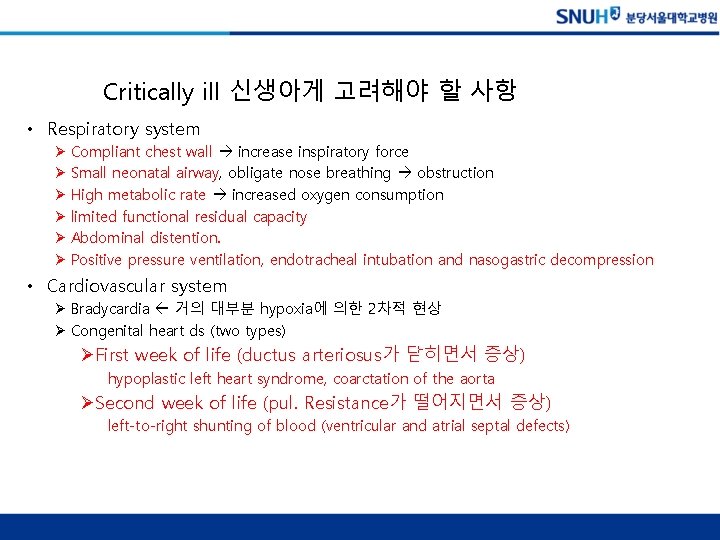
Critically ill 신생아게 고려해야 할 사항 • Respiratory system Ø Compliant chest wall increase inspiratory force Ø Small neonatal airway, obligate nose breathing obstruction Ø High metabolic rate increased oxygen consumption Ø limited functional residual capacity Ø Abdominal distention. Ø Positive pressure ventilation, endotracheal intubation and nasogastric decompression • Cardiovascular system Ø Bradycardia 거의 대부분 hypoxia에 의한 2차적 현상 Ø Congenital heart ds (two types) ØFirst week of life (ductus arteriosus가 닫히면서 증상) hypoplastic left heart syndrome, coarctation of the aorta ØSecond week of life (pul. Resistance가 떨어지면서 증상) left-to-right shunting of blood (ventricular and atrial septal defects)
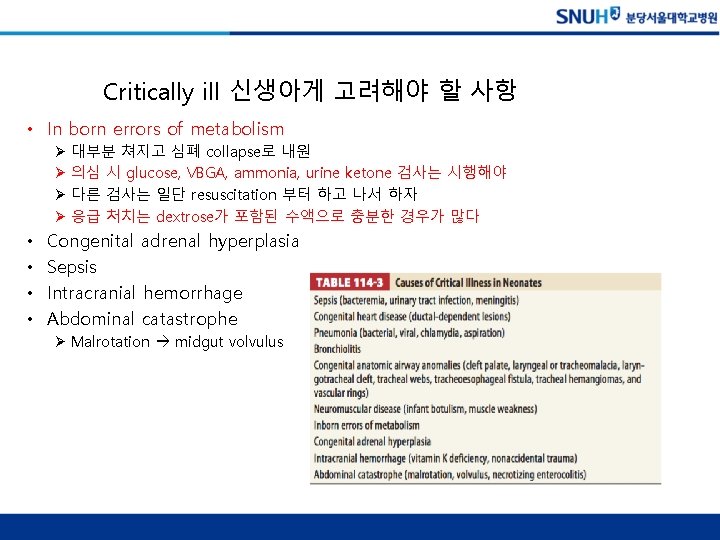
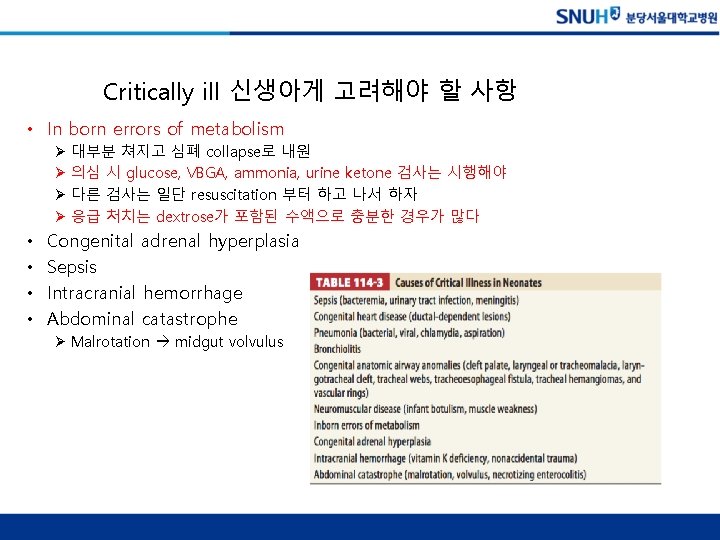
Critically ill 신생아게 고려해야 할 사항 • In born errors of metabolism Ø 대부분 쳐지고 심폐 collapse로 내원 Ø 의심 시 glucose, VBGA, ammonia, urine ketone 검사는 시행해야 Ø 다른 검사는 일단 resuscitation 부터 하고 나서 하자 Ø 응급 처치는 dextrose가 포함된 수액으로 충분한 경우가 많다 • • Congenital adrenal hyperplasia Sepsis Intracranial hemorrhage Abdominal catastrophe Ø Malrotation midgut volvulus
SYMPTOM-BASED NEONATAL PROBLEMS AND EMERGENCIES
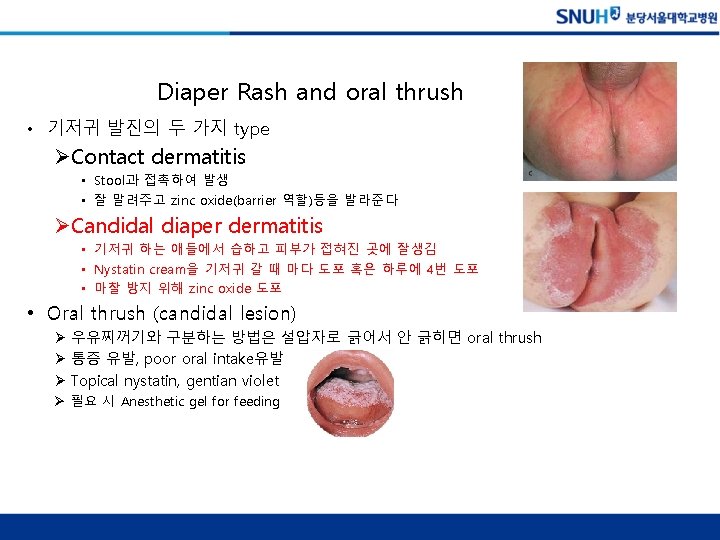
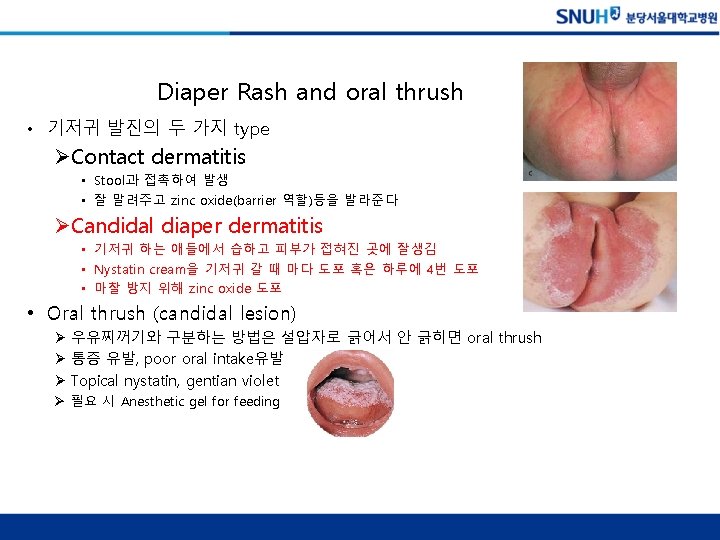
Diaper Rash and oral thrush • 기저귀 발진의 두 가지 type ØContact dermatitis • Stool과 접촉하여 발생 • 잘 말려주고 zinc oxide(barrier 역할)등을 발라준다 ØCandidal diaper dermatitis • 기저귀 하는 애들에서 습하고 피부가 접혀진 곳에 잘생김 • Nystatin cream을 기저귀 갈 때 마다 도포 혹은 하루에 4번 도포 • 마찰 방지 위해 zinc oxide 도포 • Oral thrush (candidal lesion) Ø 우유찌꺼기와 구분하는 방법은 설압자로 긁어서 안 긁히면 oral thrush Ø 통증 유발, poor oral intake유발 Ø Topical nystatin, gentian violet Ø 필요 시 Anesthetic gel for feeding
CARDIORESPIRATORY SYMPTOMS

Noisy Breathing and Stridor • Stertor Ø 흡기시 코고는 소리 양상 Ø 일반적으로 benign Ø choanal stenosis도 고려해 봐야 (NG tube 넣어서 통과 안되면. . ) • Stridor Ø Laryngomalacia Ø Congenital anomaly of trachea, bronchus Ø Worsening with cry or increased activity: laryngomalacia, tracheomalacia, or subglottic hemangioma Ø Worsening by feeding: vascular ring, laryngeal cleft, or TEF Ø Tracheal stenosis Ø With hoarseness or weak cry: vocal cord paralysis Ø Subglottic stenosis: post intubated neonate Ø Infection(croup, epiglottitis, and abscess): rare



Vomiting • Metabolic and Endocrinologic Disorders – 응급실에 내원한 신생아가 의식의 변화가 있고 혈당이 낮으면 바로 의심해야 함 – Inborn errors of metabolism – Congenital adrenal hyperplasia – Lab results ü hypoglycemia, metabolic acidosis ü hyperammonemia, or electrolyte disturbances – Emergency treatment ü 즉각적인 수액 공급, Dextrose가 포함된 수액(일단 시간을 벌자) ü 저혈당, 전해질 이상 교정 ü Steroids 투여 고려 (hydrocortisone, 12. 5 to 25. 0 milligrams IM, IV, or IO)
Necrotizing Enterocolitis • 글쎄 원인 아직 잘 모름 (다양한 원인이 섞여 있지 않을까…) • 미숙아에게 많다 하지만 정상 신생아에서도 있을 수 있다. • Symptoms ü 잘 안 먹으려하고 복부팽만, 복벽에 color change, 무호흡, shock ü 다양한 presentation을 할 수 있다. • X-ray finding ü pneumatosis intestinalis (intramural air) 과 hepatic portal air ü X-ray는 Lt lateral decubitus로 찍어야 free air가 잘 보임 • Management ü Bowel rest + broad spectrum antibiotics(ampicillin, cefotaxime, and clindamycin)
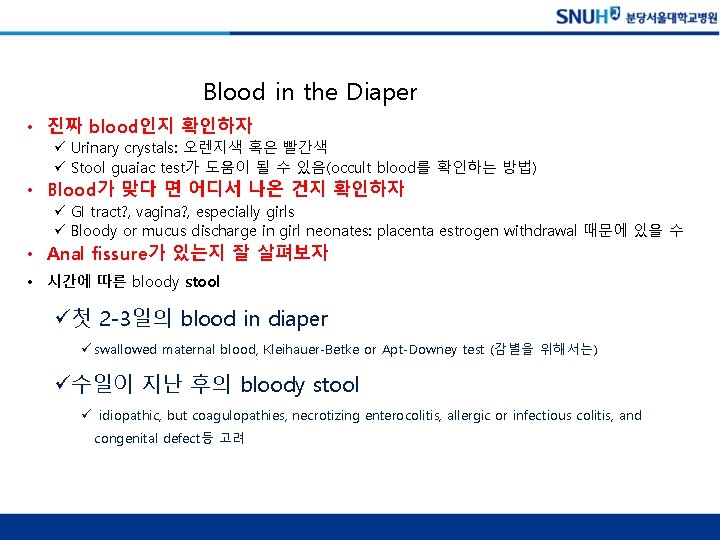
Blood in the Diaper • 진짜 blood인지 확인하자 ü Urinary crystals: 오렌지색 혹은 빨간색 ü Stool guaiac test가 도움이 될 수 있음(occult blood를 확인하는 방법) • Blood가 맞다 면 어디서 나온 건지 확인하자 ü GI tract? , vagina? , especially girls ü Bloody or mucus discharge in girl neonates: placenta estrogen withdrawal 때문에 있을 수 • Anal fissure가 있는지 잘 살펴보자 • 시간에 따른 bloody stool ü첫 2 -3일의 blood in diaper ü swallowed maternal blood, Kleihauer-Betke or Apt-Downey test (감별을 위해서는) ü수일이 지난 후의 bloody stool ü idiopathic, but coagulopathies, necrotizing enterocolitis, allergic or infectious colitis, and congenital defect등 고려


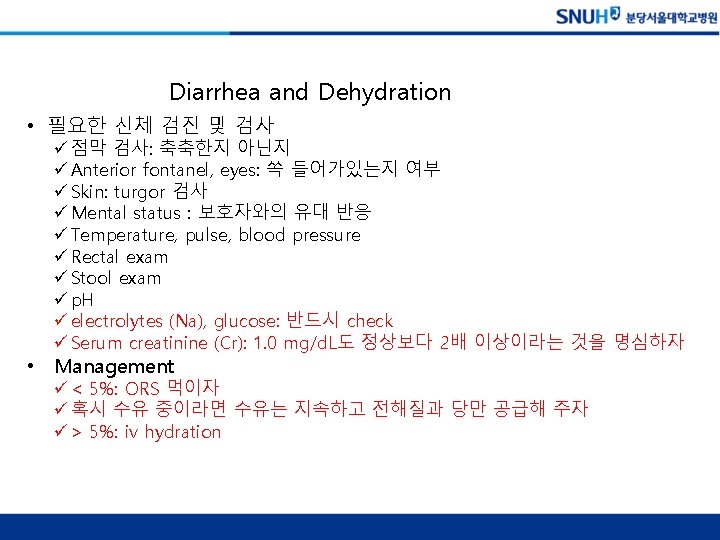
Diarrhea and Dehydration • 필요한 신체 검진 및 검사 ü 점막 검사: 축축한지 아닌지 ü Anterior fontanel, eyes: 쏙 들어가있는지 여부 ü Skin: turgor 검사 ü Mental status : 보호자와의 유대 반응 ü Temperature, pulse, blood pressure ü Rectal exam ü Stool exam ü p. H ü electrolytes (Na), glucose: 반드시 check ü Serum creatinine (Cr): 1. 0 mg/d. L도 정상보다 2배 이상이라는 것을 명심하자 • Management ü < 5%: ORS 먹이자 ü 혹시 수유 중이라면 수유는 지속하고 전해질과 당만 공급해 주자 ü > 5%: iv hydration


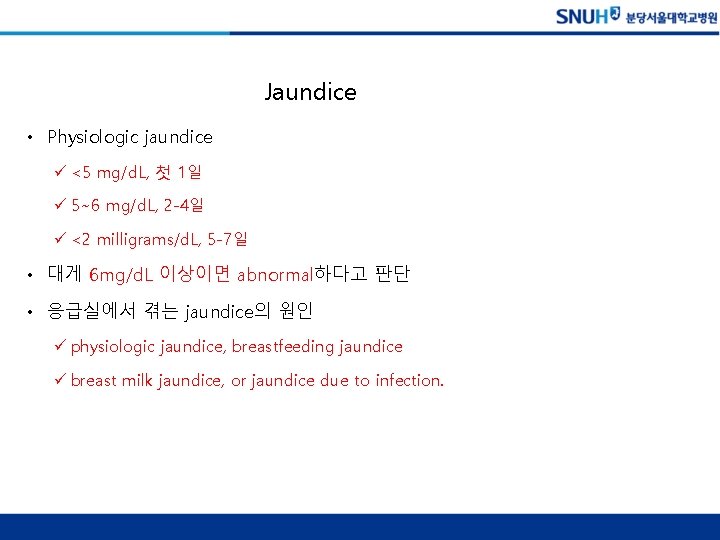
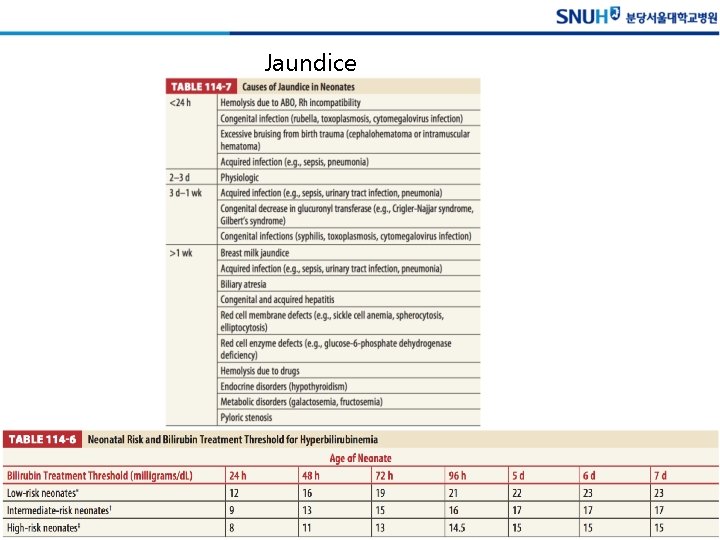
Jaundice • Physiologic jaundice ü <5 mg/d. L, 첫 1일 ü 5~6 mg/d. L, 2 -4일 ü <2 milligrams/d. L, 5 -7일 • 대게 6 mg/d. L 이상이면 abnormal하다고 판단 • 응급실에서 겪는 jaundice의 원인 ü physiologic jaundice, breastfeeding jaundice ü breast milk jaundice, or jaundice due to infection.
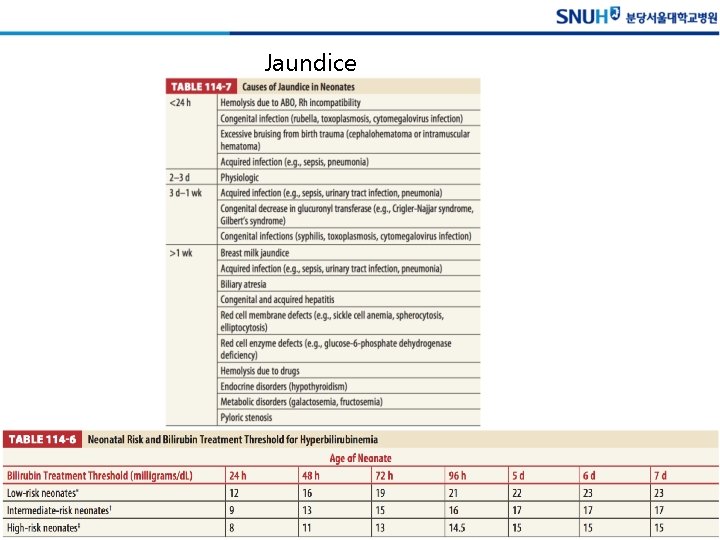
Jaundice
EYE COMPLAINTS
• Watery Eyes ü 정상적으로 눈곱이 끼고 discharge가 있을 수 있다. ü 실제 아이의 눈물샘관은 좁아져 있어서 이런 현상이 나타남 ü 12개월 넘어서까지 증상이 지속되면 안과 consult필요 • Red Eye and Irritation ü 주로 corneal abrasion d/t 본인의 손 안과 검진 ü Acute glaucoma 드물다, 바로 안과 치료 필요 ü Eye Discharge and Redness • Eye Discharge and Redness – Conjunctivitis üChlamydia trachomatis, Neisseria gonorrhoeae 항생제 üViral cause conservative üHerpes simplex conjunctivitis + vesicle full sepsis w/u , acyclovir – Gonococcal infection cefotaxime – Chlamydia conjunctivitis macrolide
NEONATAL SEPSIS

• 주 원인 균 üβ-hemolytic streptococci : ampicillin üenteric organisms (E. coli, Klebsiella species, H. influenza) : aminoglycoside (gentamicin, if meningitis, cefotaxime, ceftazidime) üListeria monocytogenes: ampicillin üEnteroviruses (coxsackievirus and echovirus) üHerpes: acyclovir • Full sepsis w/u including spinal tapping
NEUROLOGIC COMPLAINTS
Abnormal Movements and Seizures • Seizure movement와 감별해야 할 movement ü benign sleep myoclonus ü rhythmic myoclonic jerks, 잠잘 때 정상적으로 나타나는 ü 건드리거나 깨우면 없어짐 • Tetany ü Associated hypocalcemia ü Di. George syndrome • Sz인지 아닌지 감별하는 게 중요함 • 아주 미묘한 움직임도 Sz일 수 있음 ü eye deviation, tongue thrusting, eyelid fluttering, apnea, pedaling movements, or arching
CHAPTER 145. DIABETES IN CHILDREN
Pediatric DKA • Definition – p. H<7. 30 – HCO 3 < 15 m. Eg/L – Hyperglycemia > 200 mg/d. L – Ketonemia or ketouria • Sx – Due to dehydration and metabolic acidosis – Depressed consciousness (cerebral edema? ) – Abdominal pain and vomiting • DDX – Vomiting + Ketoacidosis + normal glucose toxic 감별 (ethylene glycol, alcohol, salicylates)
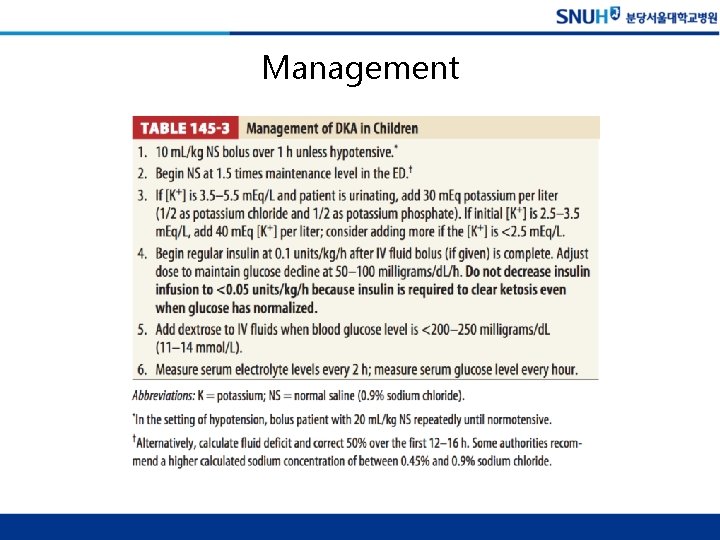
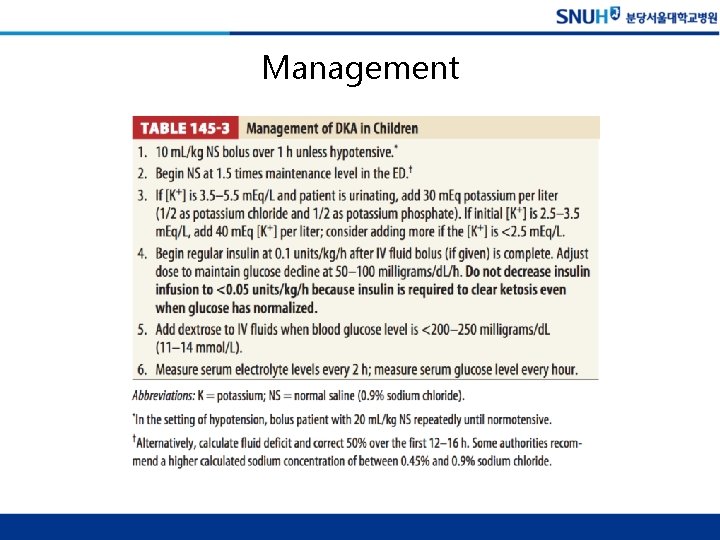
Management