PEDIATRIC ASSESSMENT Essentials for School Nurses Patti Lucarelli





- Slides: 108
PEDIATRIC ASSESSMENT Essentials for School Nurses Patti Lucarelli, MSN, RN, CPNP Jersey Shore University Medical Center K. Hovnanian Children’s Hospital Family Health Center Georgian Court University School of Nursing
Objectives • Understand the importance of Assessment and Triage and how they interplay in the Health Care Setting • Identify essential components of a “focused” Pediatric Assessment • Utilize the assessment information to differentiate between minor and more serious conditions (Triage) • Identify and implement nursing interventions based on the assessment and triage provided Sound Familiar?
Essential Pediatric Nursing Skills • • • Knowledge of Growth and Development of a Therapeutic Relationship Communication with children and their parents Understanding of family dynamics and parent-child relationships: IDENTIFY KEY FAMILY MEMBERS Knowledge of Health Promotion & Disease Prevention Patient Education and Anticipatory Guidance Practice of Therapeutic and Atraumatic Care Patient and Family Advocacy Caring, Supportive & Culturally Sensitive Interactions Coordination and Collaboration CRITICAL THINKING
Equipment What’s in Your setting? • Airway support equipment, Ambu-bags • Stethoscope & Sphygmomanometer • Pen Light • Pulse Ox & Cardiac Monitor • Nebulizer • Otoscope / Opthalmoscope • O 2

The single most important part of the health assessment is…… the
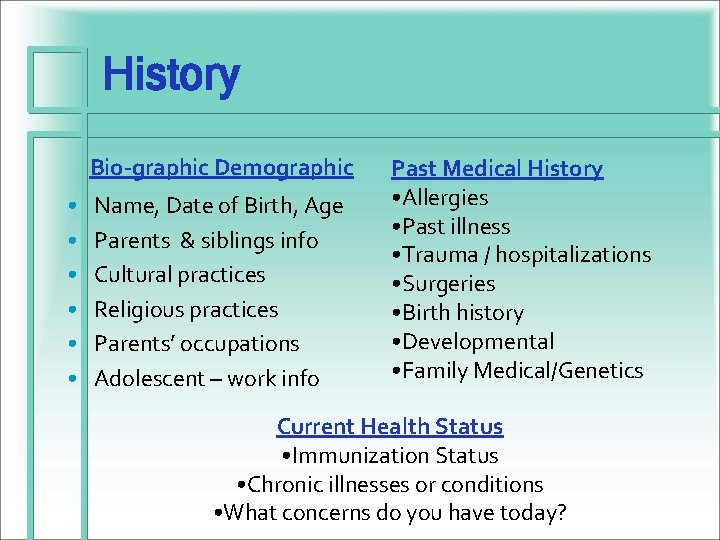
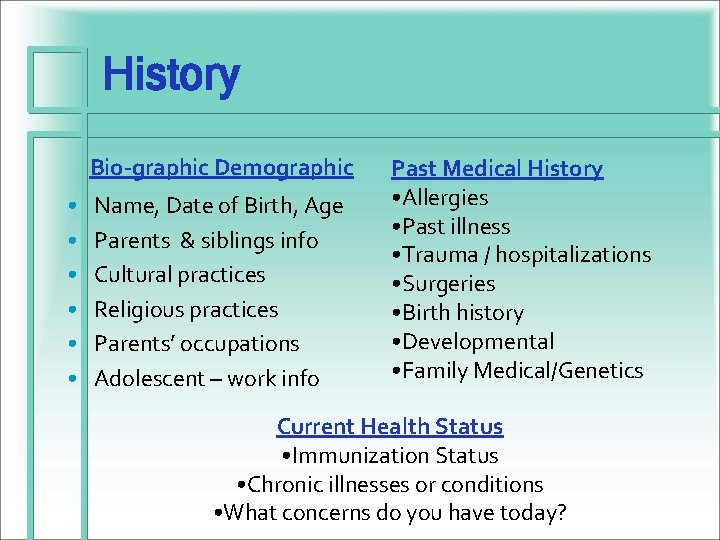
History Bio-graphic Demographic • • • Name, Date of Birth, Age Parents & siblings info Cultural practices Religious practices Parents’ occupations Adolescent – work info Past Medical History • Allergies • Past illness • Trauma / hospitalizations • Surgeries • Birth history • Developmental • Family Medical/Genetics Current Health Status • Immunization Status • Chronic illnesses or conditions • What concerns do you have today?
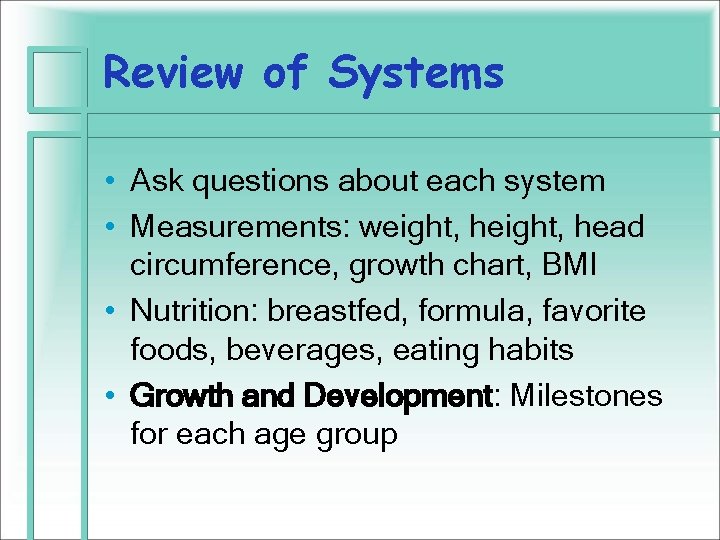
Review of Systems • Ask questions about each system • Measurements: weight, head circumference, growth chart, BMI • Nutrition: breastfed, formula, favorite foods, beverages, eating habits • Growth and Development: Milestones for each age group
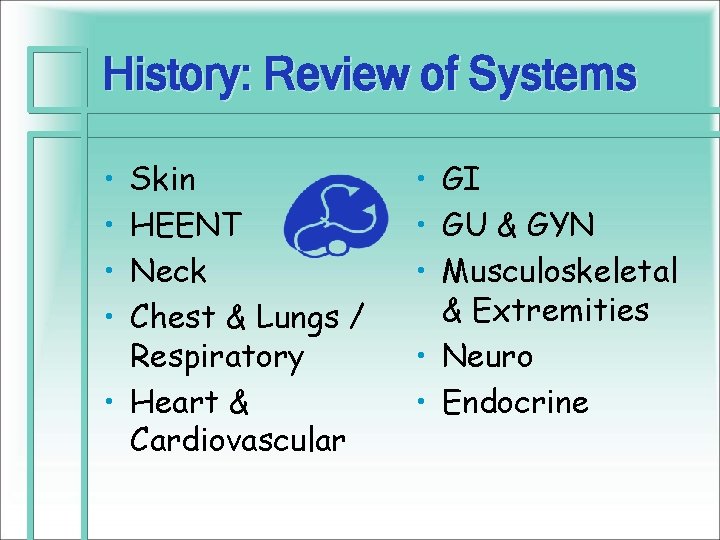
History: Review of Systems • • Skin HEENT Neck Chest & Lungs / Respiratory • Heart & Cardiovascular • GI • GU & GYN • Musculoskeletal & Extremities • Neuro • Endocrine
Patti’s Nitty Gritty Trio • Sleep & Activity • Appetite • Bowel & Bladder • In a time crunch, these three questions should give you enough insight into the child’s general functioning – • Can get more detailed if any (+) responses
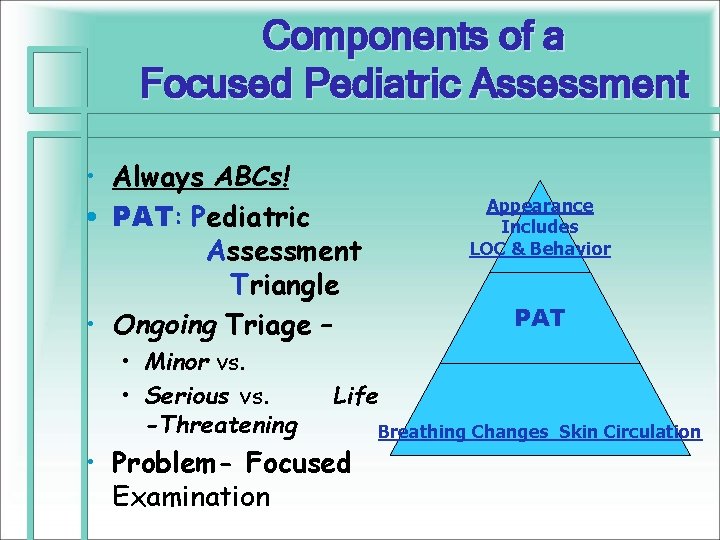
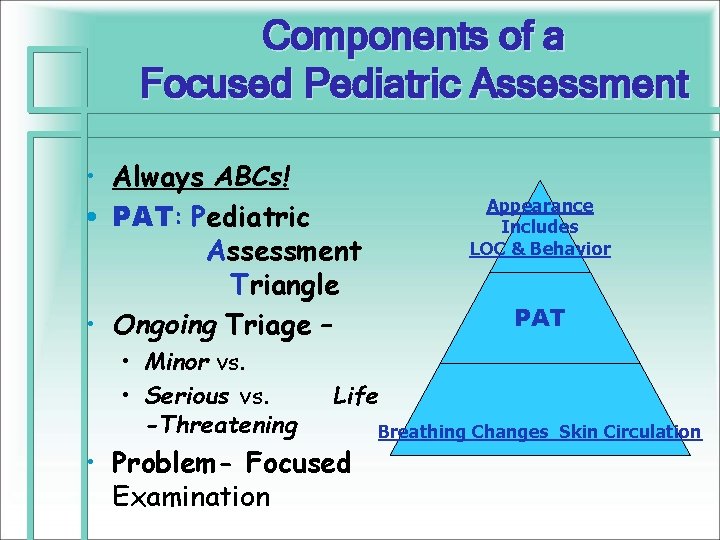
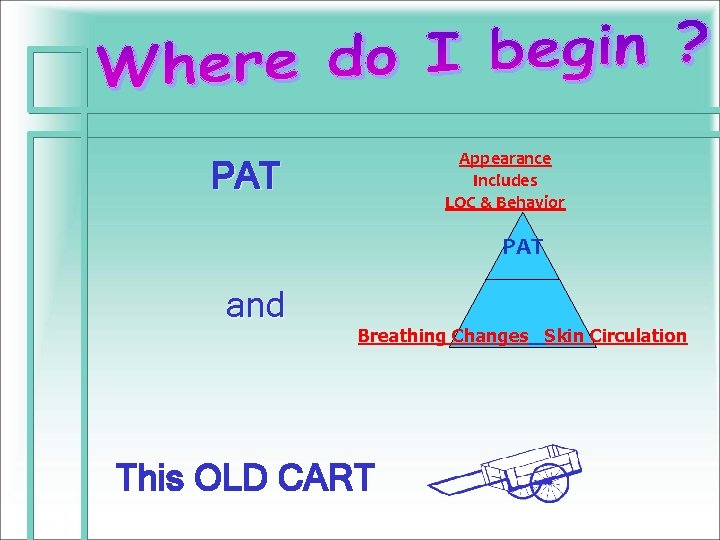
Components of a Focused Pediatric Assessment • Always ABCs! • PAT: Pediatric Assessment Triangle • Ongoing Triage – • Minor vs. • Serious vs. -Threatening Appearance Includes LOC & Behavior PAT Life • Problem- Focused Examination Breathing Changes Skin Circulation
PAT General Appearance Work of Breathing Circulation to the Skin

APPEARANCE Tone Interactiveness Consolability Look/gaze Speech/cry
Work of Breathing • Increased or Decreased Respirations • Stridor • Wheezing
Circulation to the Skin • Inadequate perfusion of vital organs • Leads to compensatory mechanisms in nonessential functions • Ex: vasoconstriction in the skin.
Initial Assessment (s) • Primary • Secondary • E = Exposure • A = Airway • F = Full Set of Vitals • B = Breathing • G = Give Comfort • C = Circulation Measures including Pain Assessment & Tx. • D = Disability • H = Head –to-Toe assessment & history • I = Inspect posterior surfaces – rashes, bruising
Physical Assessment • The approach is: • Orderly • Systematic • Head-to-toe • But FLEXIBILIY is essential • And be kind and gentle • but firm, direct and honest
Physical Assessment General Appearance & Behavior • • • Facial expression Posture / movement Hygiene Behavior Developmental Status
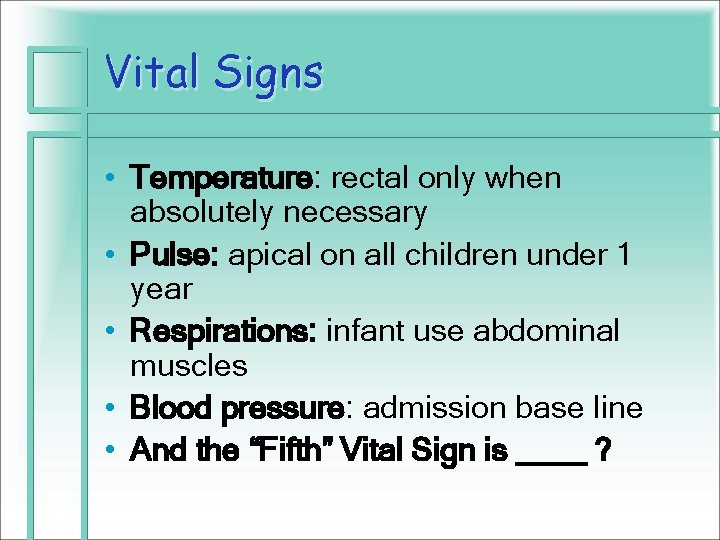
Vital Signs • Temperature: rectal only when absolutely necessary • Pulse: apical on all children under 1 year • Respirations: infant use abdominal muscles • Blood pressure: admission base line • And the “Fifth” Vital Sign is ____ ?
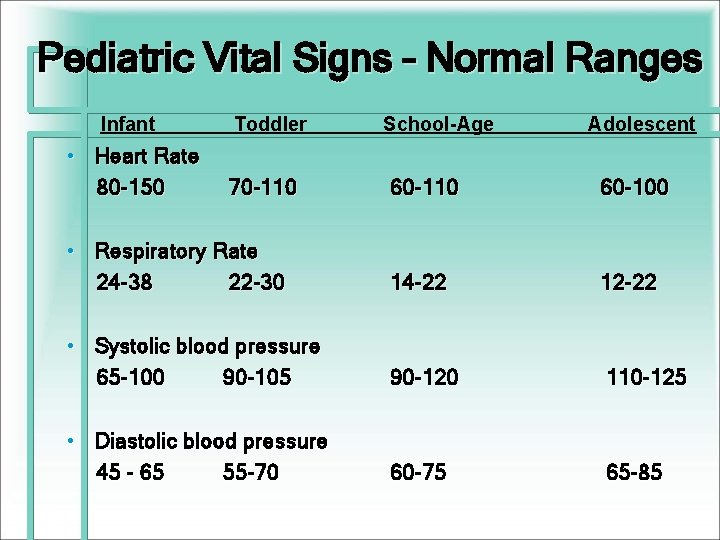
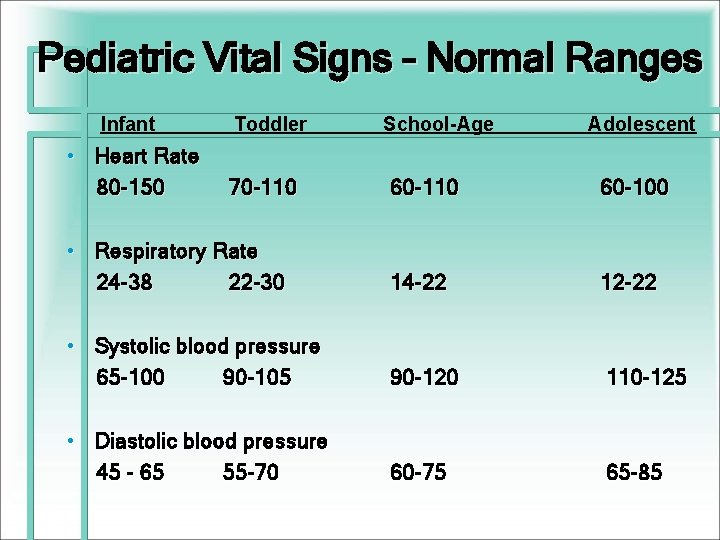
Pediatric Vital Signs – Normal Ranges Infant Toddler School-Age Adolescent • Heart Rate 80 -150 70 -110 60 -100 • Respiratory Rate 24 -38 22 -30 14 -22 12 -22 • Systolic blood pressure 65 -100 90 -105 90 -120 110 -125 • Diastolic blood pressure 45 - 65 55 -70 60 -75 65 -85
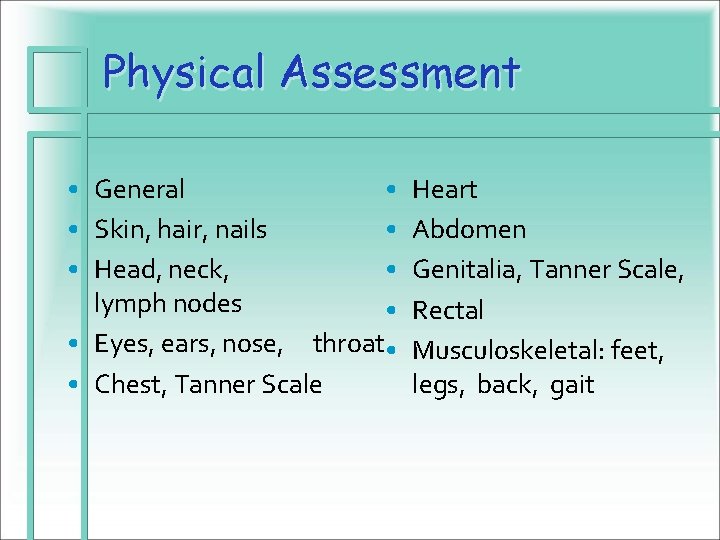
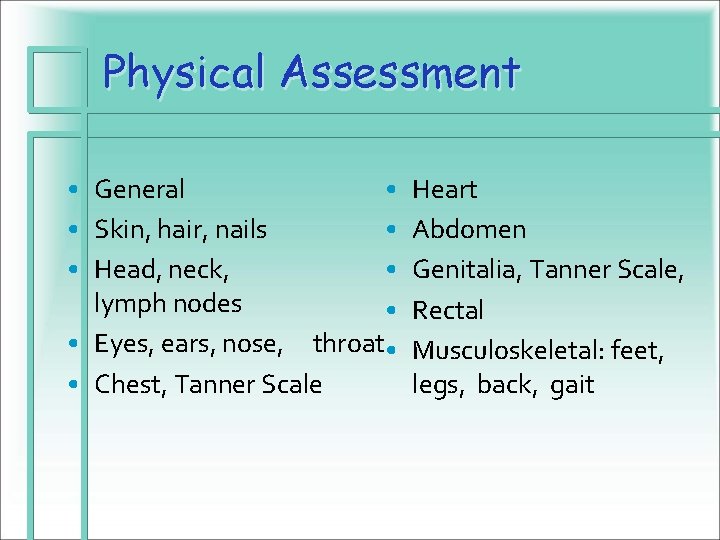
Physical Assessment • General • • Skin, hair, nails • • Head, neck, • lymph nodes • • Eyes, ears, nose, throat • • Chest, Tanner Scale Heart Abdomen Genitalia, Tanner Scale, Rectal Musculoskeletal: feet, legs, back, gait
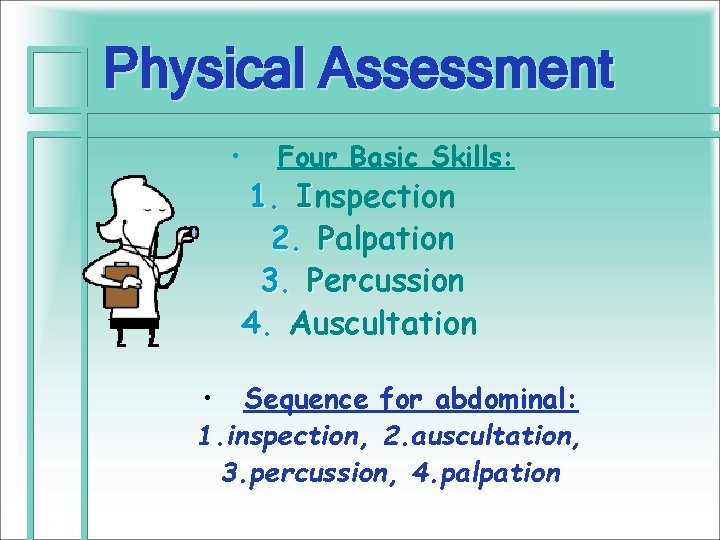
Physical Assessment • Four Basic Skills: 1. Inspection 2. Palpation 3. Percussion 4. Auscultation • Sequence for abdominal: 1. inspection, 2. auscultation, 3. percussion, 4. palpation
Inspection • Use all your senses • The essential First Step of the Physical Exam
Palpation • Use of your fingers and palms to determine: • • • Temperature Hydration Texture Shape Movement Areas of Tenderness • Warm hands and short nails • Palpate areas of tenderness / pain last • Talk with the child during palpation to help him relax • Be observant of reactions to palpation • Move firmly without hesitation
Palpation • For the ticklish child: place her hands over your hands and have the child do the pressing down.
Percussion Use of tapping to produce sounds that are characterized according to: • • Intensity Pitch Duration Quality Direct vs. Indirect
Auscultation • Listening for body sounds • Bell: low-pitched • - heart • Diaphragm: high-pitched • – lung & bowel LUNGS: Listen to all lung fields FRONT AND BACK! auscultate for breath sounds and adventitious sounds
“I P P A” • Practice, Practice • by knowing what the norm is, you’ll be able to pick up on the abnormal, even if you can’t diagnose it…. • The important thing is to be able to say “This is not right” • and refer appropriately!
H E E N T Head Eyes Ears Nose Neck Throat
HEENT: Head & Neck, Eyes, Ears, Nose, Face, Mouth & Throat • Head: Symmetry of skull and face • Neck: Structure, movement, trachea, thyroid, vessels and lymph nodes • Eyes: Vision, placement, external and internal fundoscopic exam • Ears: Hearing, external, ear canal and otoscopic exam of tympanic membrane • Nose: Structure, exudate, sinuses • Mouth: Structures of mouth, teeth and pharynx
Head • Shape: “Normo. Cephalic – ATraumatic” AT • Lesions • ? Edema
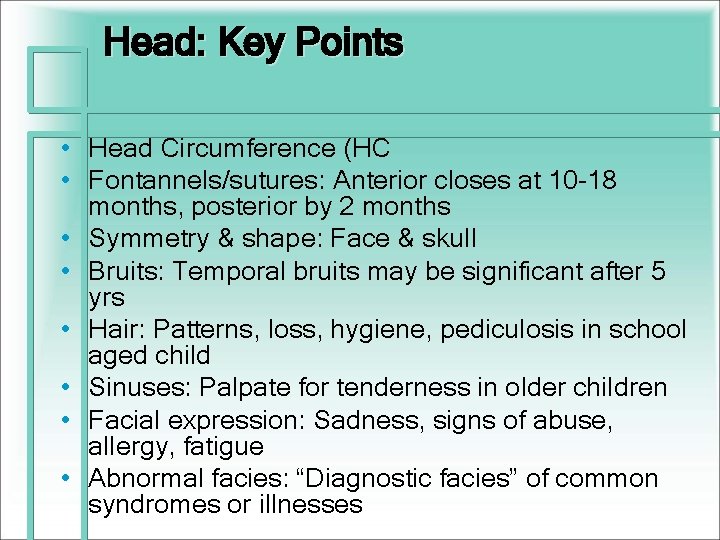
Head: Key Points • Head Circumference (HC • Fontannels/sutures: Anterior closes at 10 -18 months, posterior by 2 months • Symmetry & shape: Face & skull • Bruits: Temporal bruits may be significant after 5 yrs • Hair: Patterns, loss, hygiene, pediculosis in school aged child • Sinuses: Palpate for tenderness in older children • Facial expression: Sadness, signs of abuse, allergy, fatigue • Abnormal facies: “Diagnostic facies” of common syndromes or illnesses
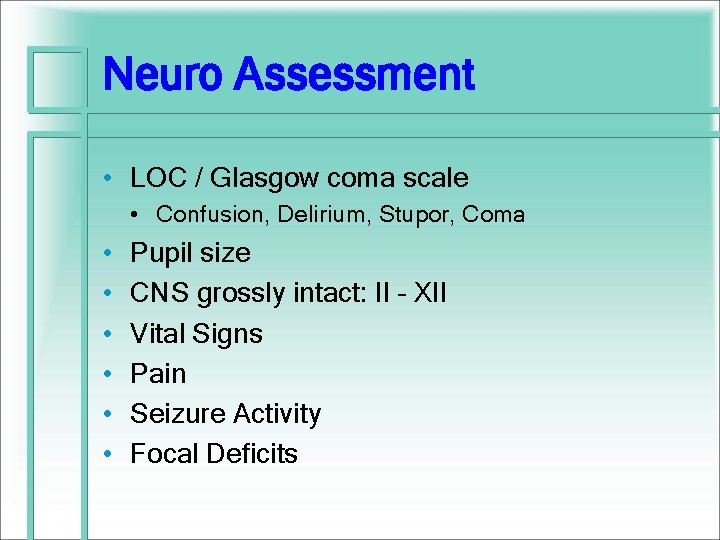
Neuro Assessment • LOC / Glasgow coma scale • Confusion, Delirium, Stupor, Coma • • • Pupil size CNS grossly intact: II – XII Vital Signs Pain Seizure Activity Focal Deficits
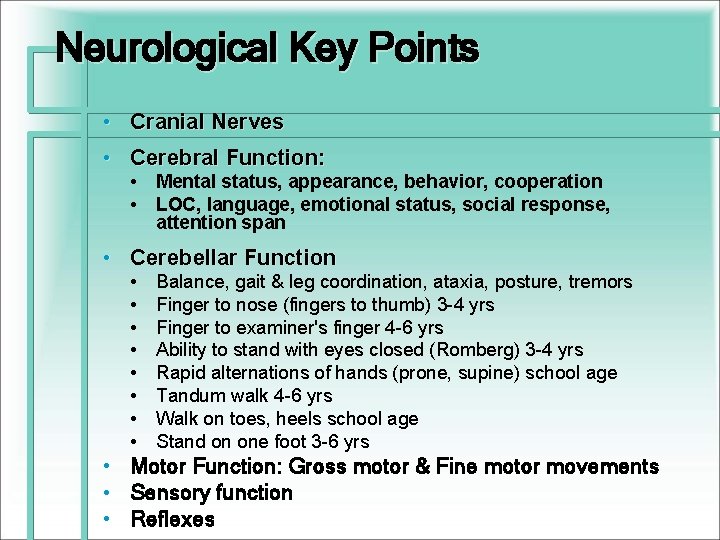
Neurological Key Points • Cranial Nerves • Cerebral Function: • Mental status, appearance, behavior, cooperation • LOC, language, emotional status, social response, attention span • Cerebellar Function • • • Balance, gait & leg coordination, ataxia, posture, tremors Finger to nose (fingers to thumb) 3 -4 yrs Finger to examiner's finger 4 -6 yrs Ability to stand with eyes closed (Romberg) 3 -4 yrs Rapid alternations of hands (prone, supine) school age Tandum walk 4 -6 yrs Walk on toes, heels school age Stand on one foot 3 -6 yrs Motor Function: Gross motor & Fine motor movements Sensory function Reflexes
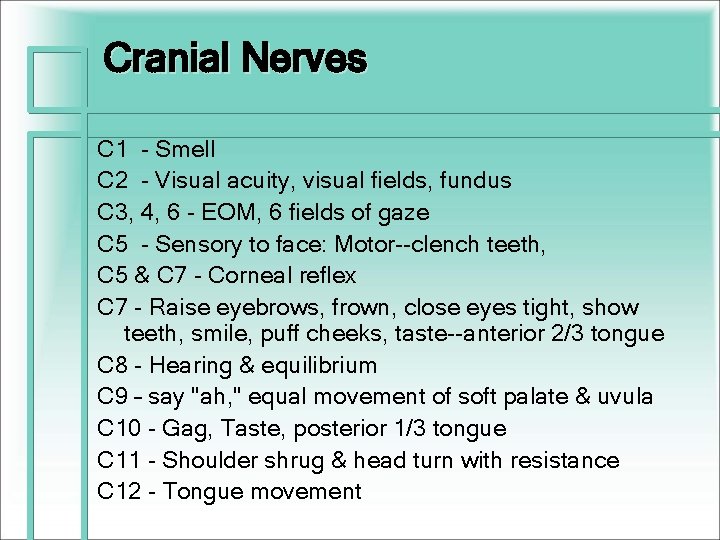
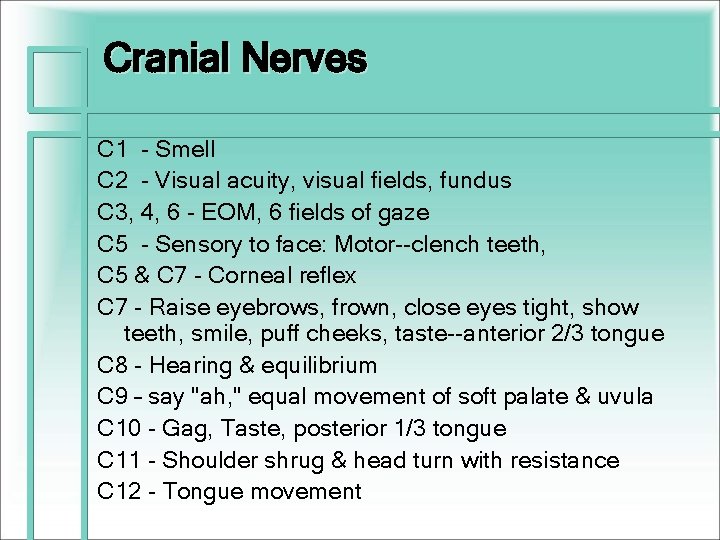
Cranial Nerves C 1 - Smell C 2 - Visual acuity, visual fields, fundus C 3, 4, 6 - EOM, 6 fields of gaze C 5 - Sensory to face: Motor--clench teeth, C 5 & C 7 - Corneal reflex C 7 - Raise eyebrows, frown, close eyes tight, show teeth, smile, puff cheeks, taste--anterior 2/3 tongue C 8 - Hearing & equilibrium C 9 – say "ah, " equal movement of soft palate & uvula C 10 - Gag, Taste, posterior 1/3 tongue C 11 - Shoulder shrug & head turn with resistance C 12 - Tongue movement
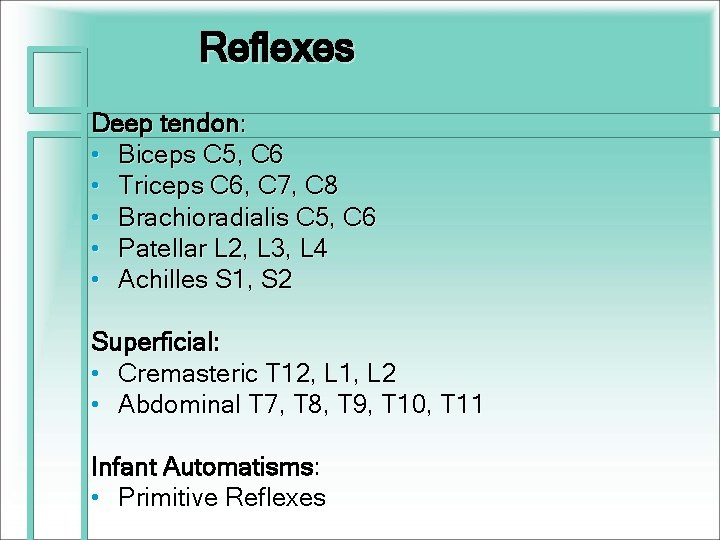
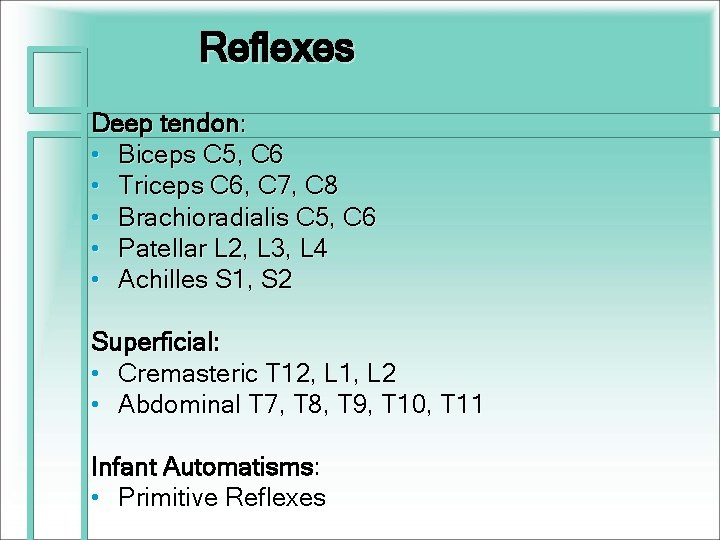
Reflexes Deep tendon: • Biceps C 5, C 6 • Triceps C 6, C 7, C 8 • Brachioradialis C 5, C 6 • Patellar L 2, L 3, L 4 • Achilles S 1, S 2 Superficial: • Cremasteric T 12, L 1, L 2 • Abdominal T 7, T 8, T 9, T 10, T 11 Infant Automatisms: • Primitive Reflexes
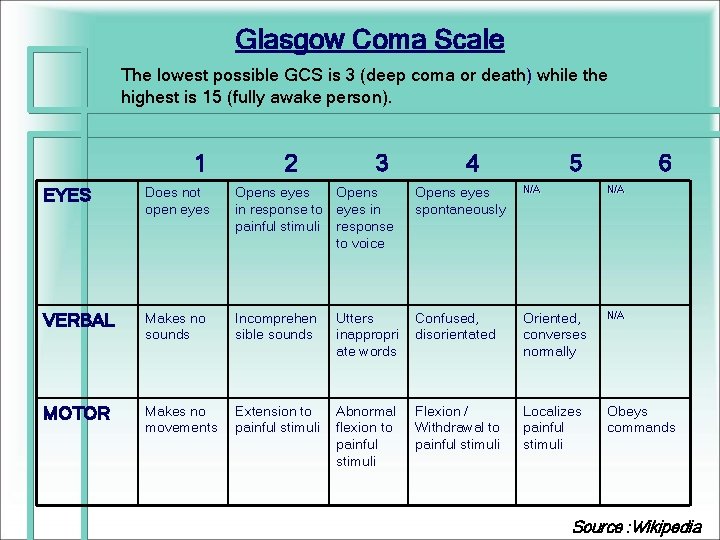
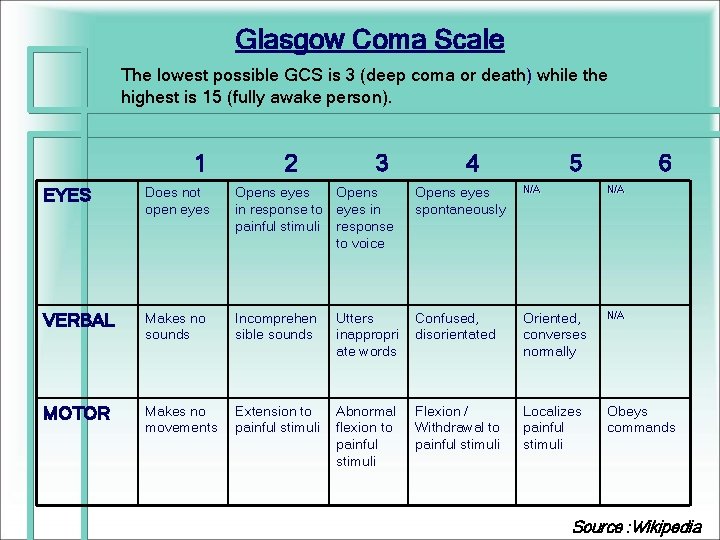
Glasgow Coma Scale The lowest possible GCS is 3 (deep coma or death) while the highest is 15 (fully awake person). 1 2 3 4 5 6 EYES Does not open eyes Opens in response to eyes in painful stimuli response to voice Opens eyes spontaneously N/A VERBAL Makes no sounds Incomprehen sible sounds Utters inappropri ate words Confused, disorientated Oriented, converses normally N/A MOTOR Makes no movements Extension to painful stimuli Abnormal flexion to painful stimuli Flexion / Withdrawal to painful stimuli Localizes painful stimuli Obeys commands Source : Wikipedia
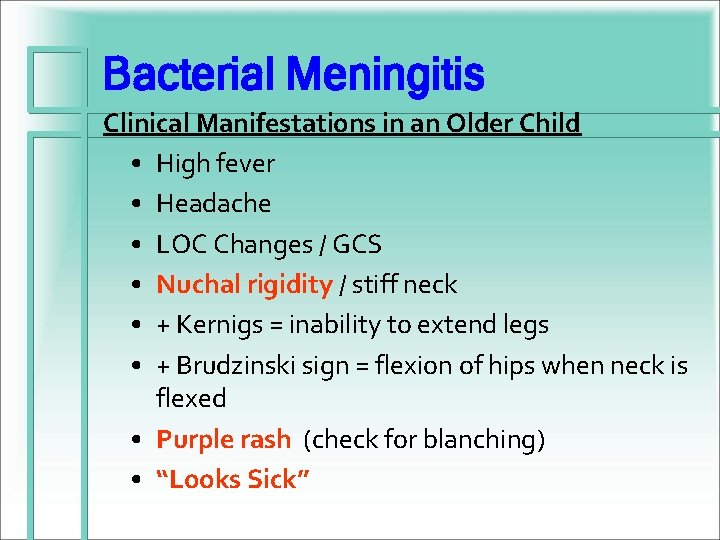
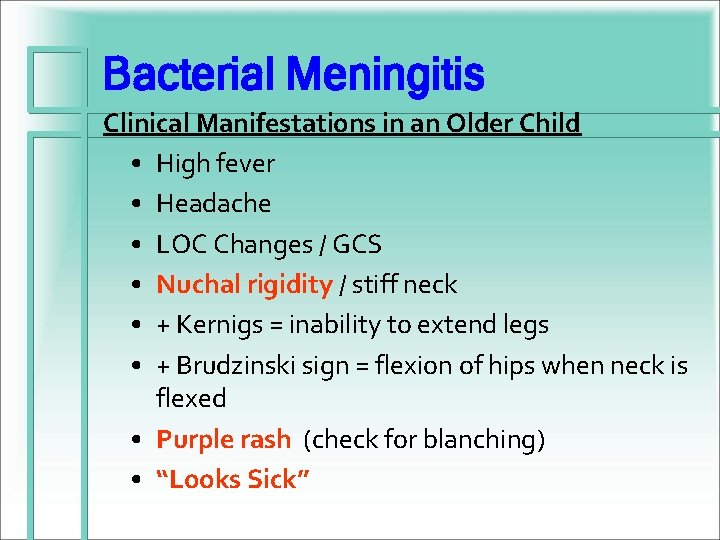
Bacterial Meningitis Clinical Manifestations in an Older Child • High fever • Headache • LOC Changes / GCS • Nuchal rigidity / stiff neck • + Kernigs = inability to extend legs • + Brudzinski sign = flexion of hips when neck is flexed • Purple rash (check for blanching) • “Looks Sick”
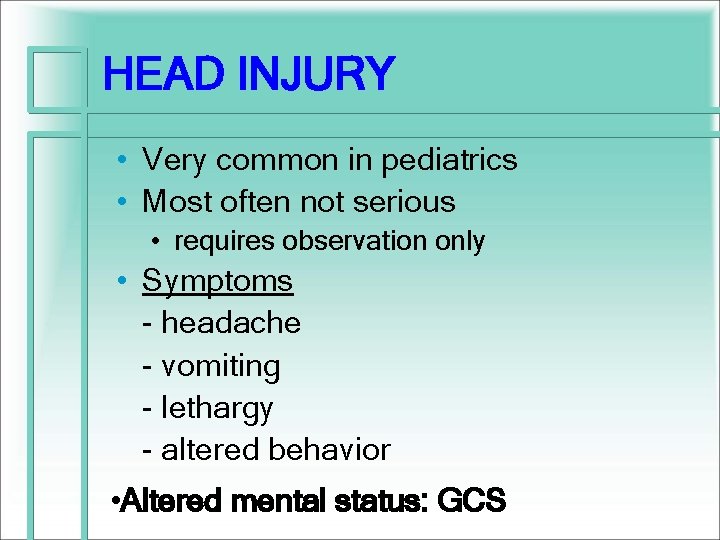
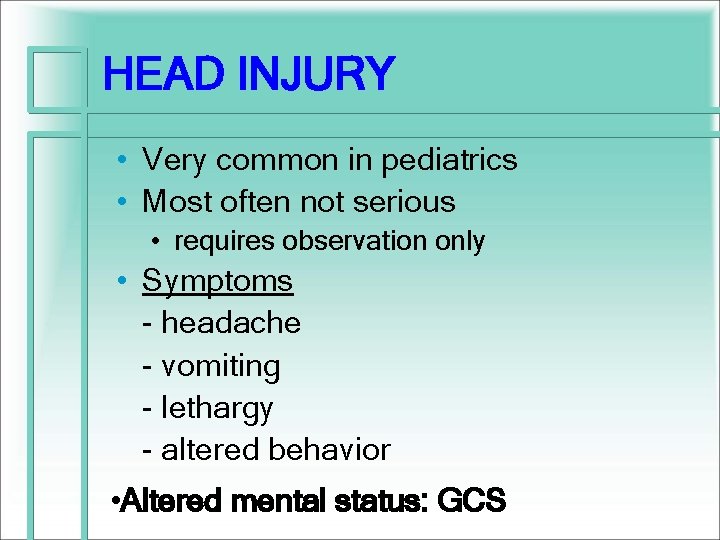
HEAD INJURY • Very common in pediatrics • Most often not serious • requires observation only • Symptoms - headache - vomiting - lethargy - altered behavior • Altered mental status: GCS
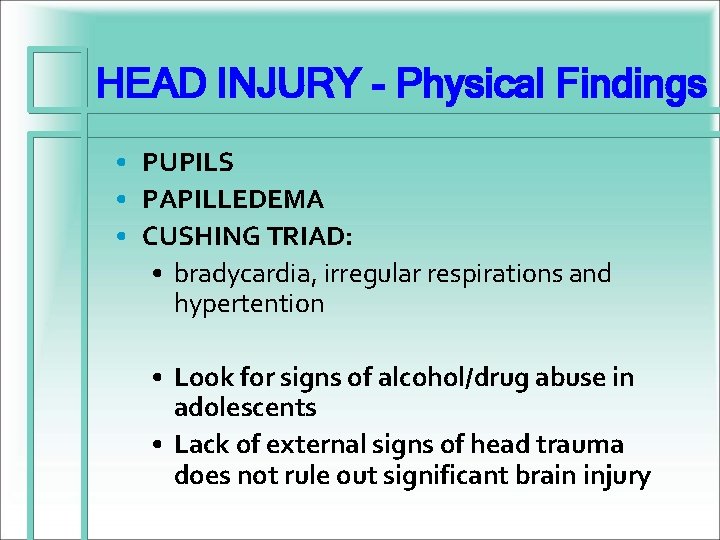
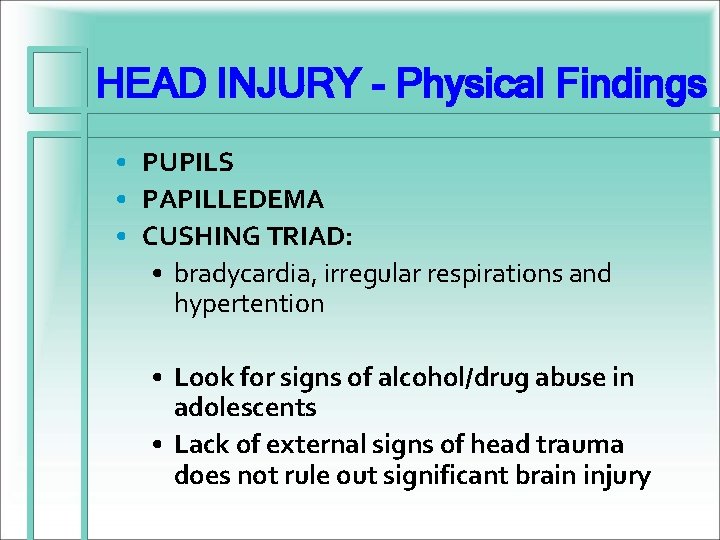
HEAD INJURY - Physical Findings • PUPILS • PAPILLEDEMA • CUSHING TRIAD: • bradycardia, irregular respirations and hypertention • Look for signs of alcohol/drug abuse in adolescents • Lack of external signs of head trauma does not rule out significant brain injury
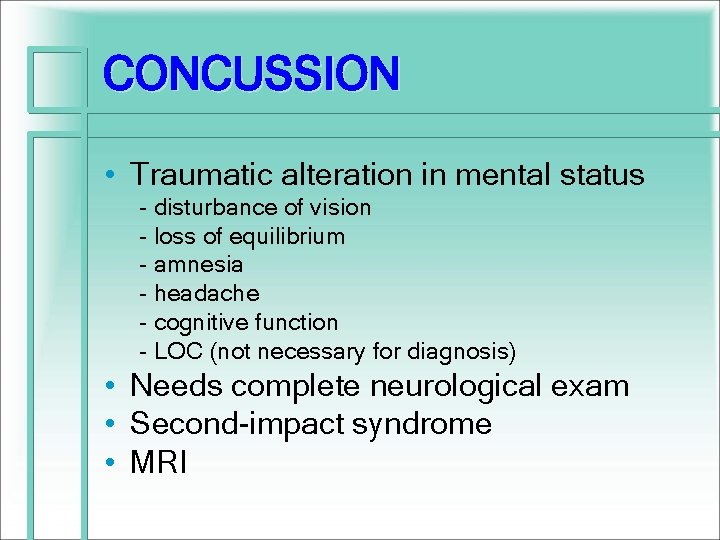
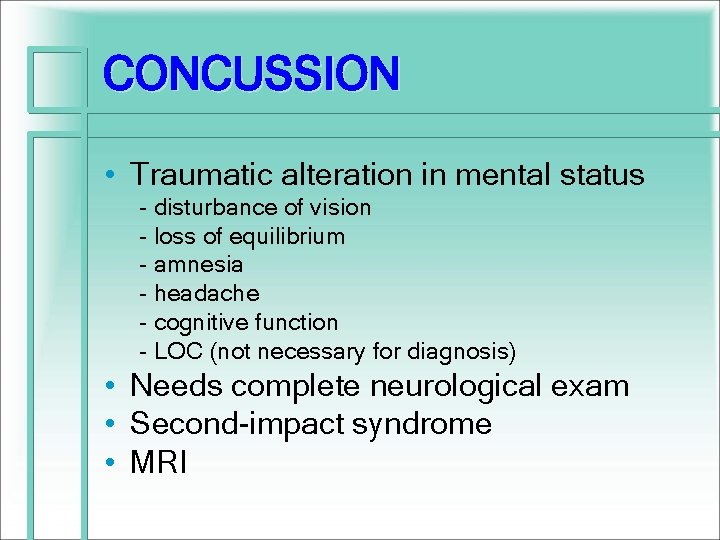
CONCUSSION • Traumatic alteration in mental status - disturbance of vision - loss of equilibrium - amnesia - headache - cognitive function - LOC (not necessary for diagnosis) • Needs complete neurological exam • Second-impact syndrome • MRI
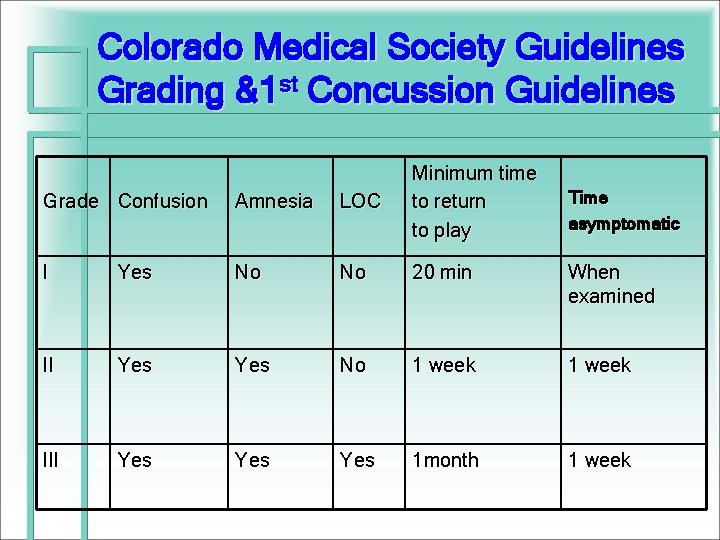
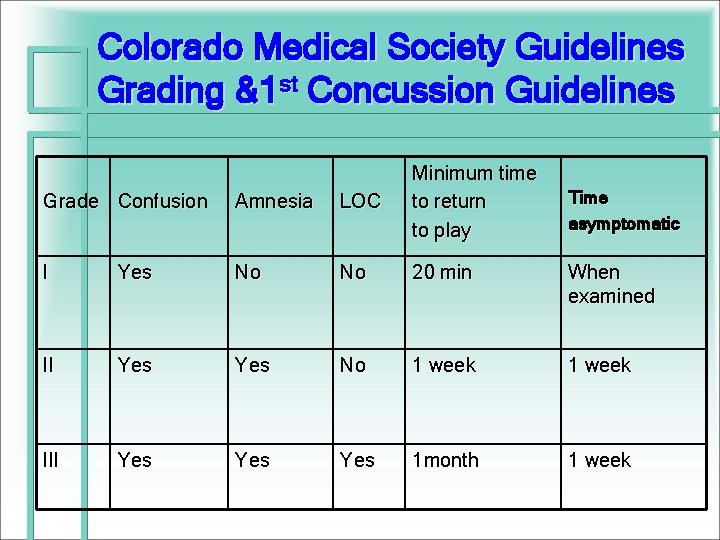
Colorado Medical Society Guidelines Grading &1 st Concussion Guidelines Grade Confusion Amnesia LOC Minimum time to return to play I Yes No No 20 min When examined II Yes No 1 week III Yes Yes 1 month 1 week Time asymptomatic
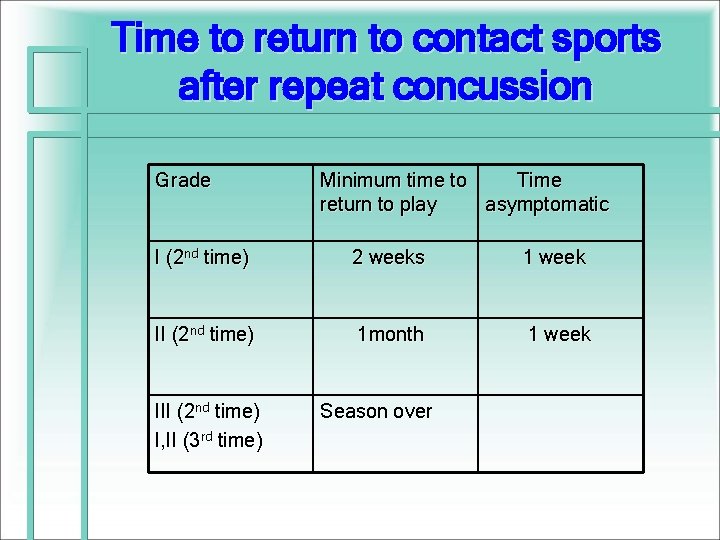
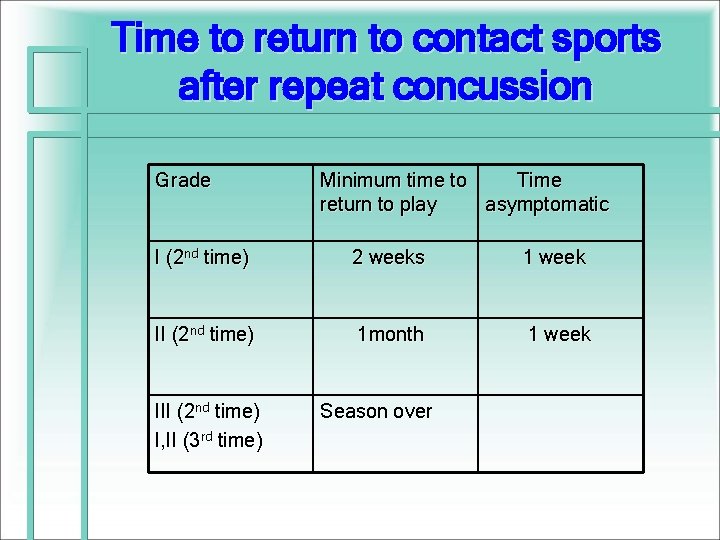
Time to return to contact sports after repeat concussion Grade Minimum time to Time return to play asymptomatic I (2 nd time) 2 weeks 1 week II (2 nd time) 1 month 1 week III (2 nd time) I, II (3 rd time) Season over
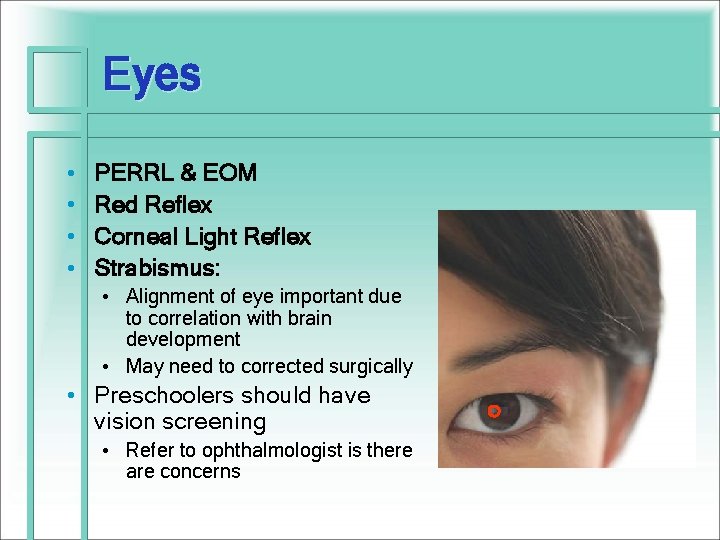
Eyes • • PERRL & EOM Red Reflex Corneal Light Reflex Strabismus: • Alignment of eye important due to correlation with brain development • May need to corrected surgically • Preschoolers should have vision screening • Refer to ophthalmologist is there are concerns o
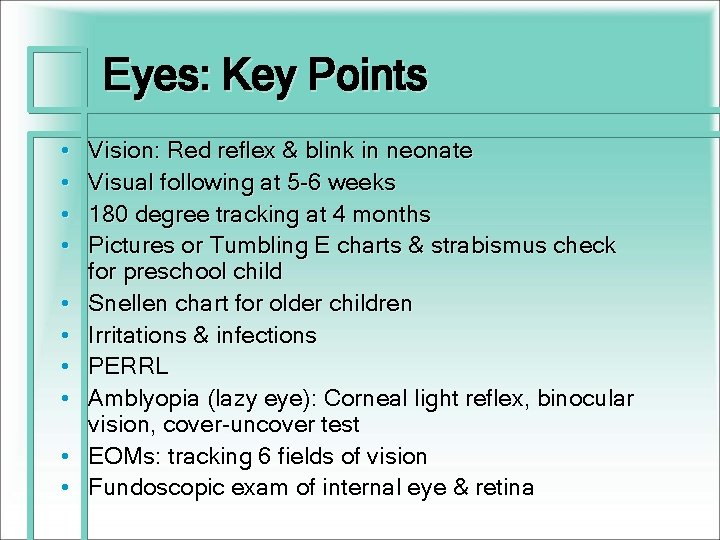
Eyes: Key Points • • • Vision: Red reflex & blink in neonate Visual following at 5 -6 weeks 180 degree tracking at 4 months Pictures or Tumbling E charts & strabismus check for preschool child Snellen chart for older children Irritations & infections PERRL Amblyopia (lazy eye): Corneal light reflex, binocular vision, cover-uncover test EOMs: tracking 6 fields of vision Fundoscopic exam of internal eye & retina
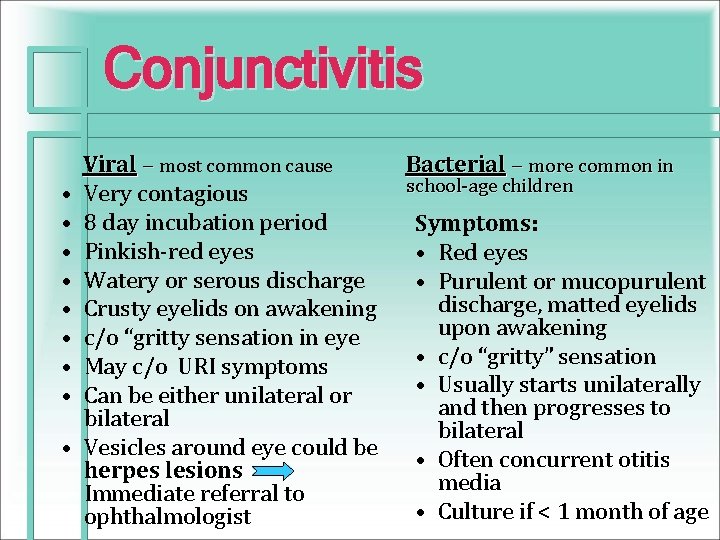
Conjunctivitis Viral – most common cause • Very contagious • 8 day incubation period • Pinkish-red eyes • Watery or serous discharge • Crusty eyelids on awakening • c/o “gritty sensation in eye • May c/o URI symptoms • Can be either unilateral or bilateral • Vesicles around eye could be herpes lesions Immediate referral to ophthalmologist Bacterial – more common in school-age children Symptoms: • Red eyes • Purulent or mucopurulent discharge, matted eyelids upon awakening • c/o “gritty” sensation • Usually starts unilaterally and then progresses to bilateral • Often concurrent otitis media • Culture if < 1 month of age
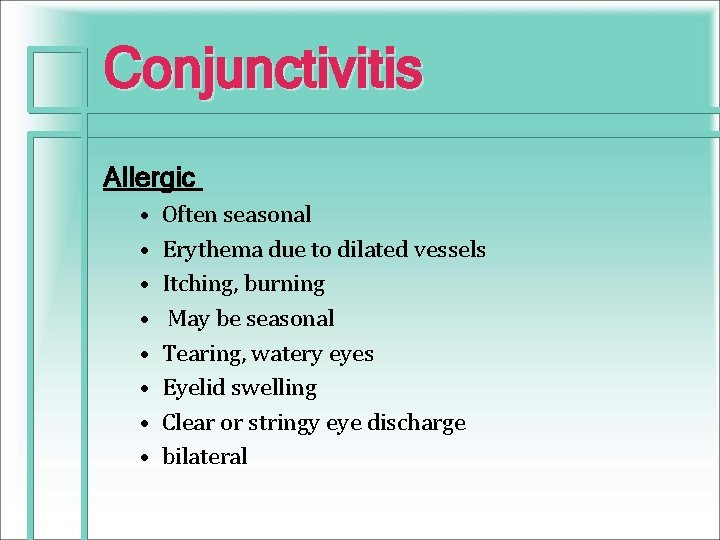
Conjunctivitis Allergic • • Often seasonal Erythema due to dilated vessels Itching, burning May be seasonal Tearing, watery eyes Eyelid swelling Clear or stringy eye discharge bilateral
Ears: Key Points • Ask about hearing concerns • Inquire about infant’s response to • Observe an older infant’s/toddlers speech pattern • • Inspect the ears • Assess the shape of the ears Determine if both ears are well formed • Assess
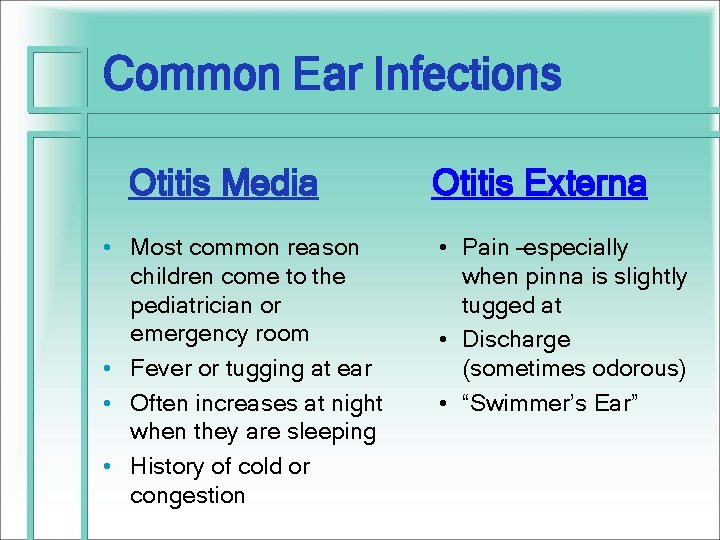
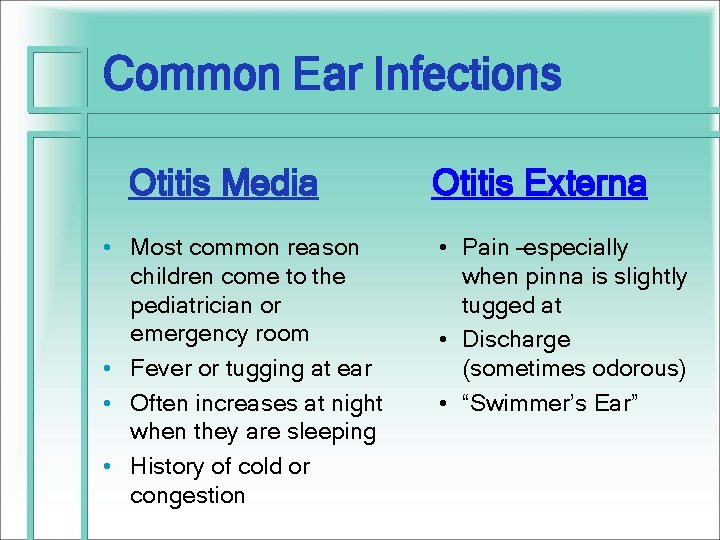
Common Ear Infections Otitis Media • Most common reason children come to the pediatrician or emergency room • Fever or tugging at ear • Often increases at night when they are sleeping • History of cold or congestion Otitis Externa • Pain –especially when pinna is slightly tugged at • Discharge (sometimes odorous) • “Swimmer’s Ear”
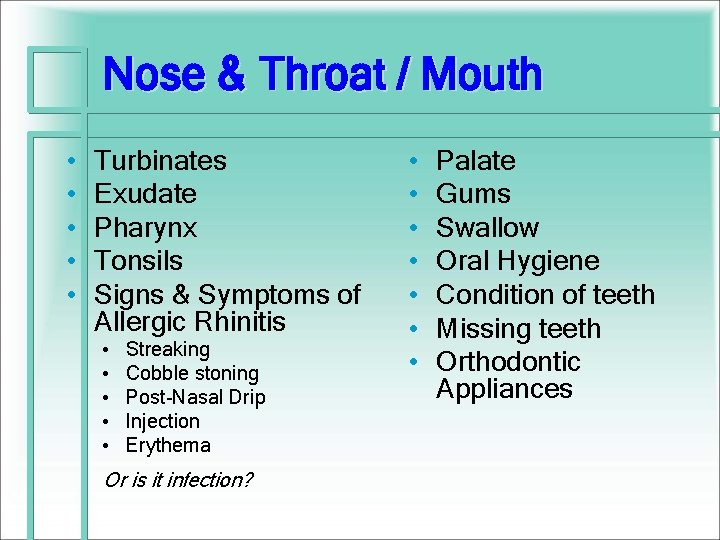
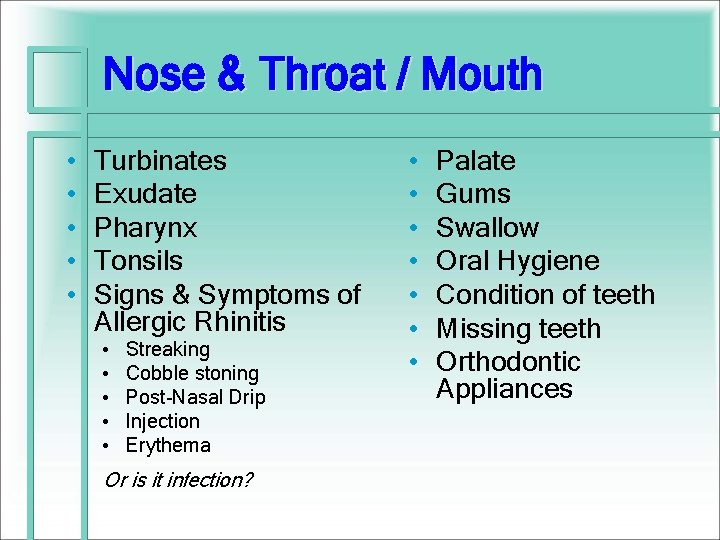
Nose & Throat / Mouth • • • Turbinates Exudate Pharynx Tonsils Signs & Symptoms of Allergic Rhinitis • • • Streaking Cobble stoning Post-Nasal Drip Injection Erythema Or is it infection? • • Palate Gums Swallow Oral Hygiene Condition of teeth Missing teeth Orthodontic Appliances
Nose: Key Points • • • Exam nose & mouth after ears Observe shape & structural deviations Nares: (check patency, mucous membranes, discharge, turbinates, bleeding) Septum: (check for deviation) Infants are obligate nose breathers Nasal flaring is associated with respiratory distress
Nose: Variations • Allergy: “allergic salute” - line across nose. • Infection • Foreign body: • Foul odor or unilateral discharge • Structure variations • Bell’s palsy
Nose and Throat Sinusitis: • • • Fever Purulent rhinorrhea Facial Pain – cheeks, forehead Breath odor Chronic cough – could be day and night (+) Post-nasal drip
Mouth & Pharynx: Key Points • Lips: color, symmetry, moisture, swelling, sores, fissures • Buccal mucosa, gingivae, tongue & palate for moisture, color, intactness, bleeding, lesions. • Tongue & frenulum - movement, size & texture • Teeth - caries, malocclusion and loose teeth. • Uvula: symmetrical movement or bifid uvula • Voice quality, Speech • Breath - halitosis
Ears, Nose and Throat Sore Throats Is it strept or is it viral or could it be mono? Lymph nodes & ROM
Neck: Key Points • √ position, lymph nodes, masses, fistulas, clefts • Suppleness & Range of Motion (ROM) • Check clavicle in newborn • Head control in infant • Trachea & thyroid in midline • Carotid arteries (bruits) • Torticollis • Webbing • Meningeal irritation
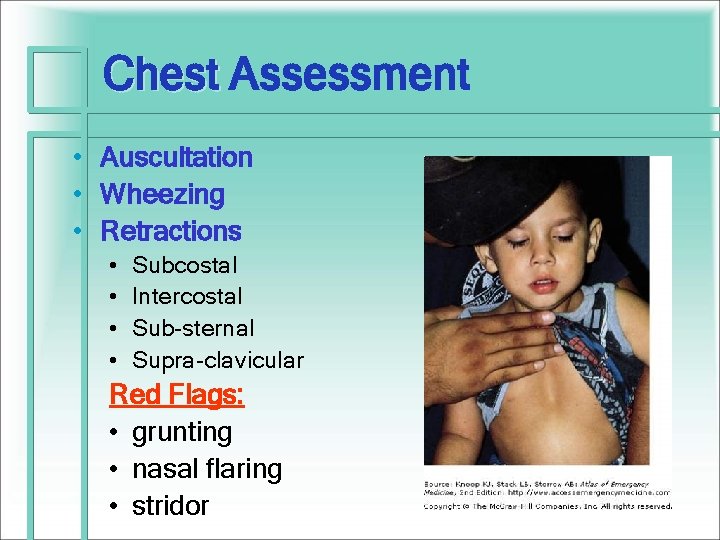
Chest Assessment • How does the child look? • Color • Work of Breathing: Effort used to breathe Auscultation • • All 4 quadrants Front and back Take the time to listen Be sure about “lungs CTAB” (clear to auscultation bilaterally)
Lungs & Respiratory: Key Points • Quality of Respirations: • Symmetry, Expansion, Effort, Dyspnea • S & S Respiratory Distress: • Color: cyanosis, pallor, circumoral cyanosis, mottling • Tachypnea • Retractions • Nasal flaring • Grunting (expiratory) • Stridor - inspiratory: croup • Adventitious sounds: • Crackles / Rales • Rhonchi - course breath sounds • Wheeze – inspiratory vs. expiratory
Lungs & Respiratory: Key Points • Clubbing • Snoring (expiratory): upper airway obstruction, allergy, • Fremitus: • Increased in pneumonia, atelectasis, mass • Decreased in asthma, pneumothorax or FB • Dullness to percussion: fluid or mass
Work of Breathing • Increased or Decreased Respirations • Stridor • Wheezing
Chest Assessment Chest • Auscultation • Wheezing • Retractions • • Subcostal Intercostal Sub-sternal Supra-clavicular Red Flags: • grunting • nasal flaring • stridor
All that Wheezes isn’t always Asthma… Think: • Infection • Foreign body aspiration • Anaphylaxis • Insect bites/stings, medications, food allergies
And all Asthma doesn’t always Wheeze! • Cough • Fatigue • Reduced exercise tolerance
Coughs • Allergies • Asthma • Infections – pneumonia, bronchitis, bronchiolitis • Sinusitis – Post-nasal drip • GERD • Cigarette smoking • Exposure to secondhand smoke, • Other pollutants
Cough - Characteristics • • • Dry, non-productive Mucousy – productive Croupy Acute – less than 2 -3 weeks Chronic – more than 2 -3 weeks Associating Symptoms
Chest Pain • Call 911 if severe, acute, unremitting – needs immediate attention - very rare • Non-cardiac – most common • Musculoskeletal: costochondritis • Pulmonary • Gastrointestinal e. g. GERD • Psychogenic • Often no significant physical findings • Must rule out Cardiac origin – refer to PCP or pedi cardiologist
Circulatory • Auscultating Heart Sounds The Auscultation Assistant – Heart Murmurs, Heart Sounds, and Breath Sounds. http: //www. wilkes. med. ucla. edu/inex. htm Pillitter • Perfusion – capillary refill • “Warm to touch”
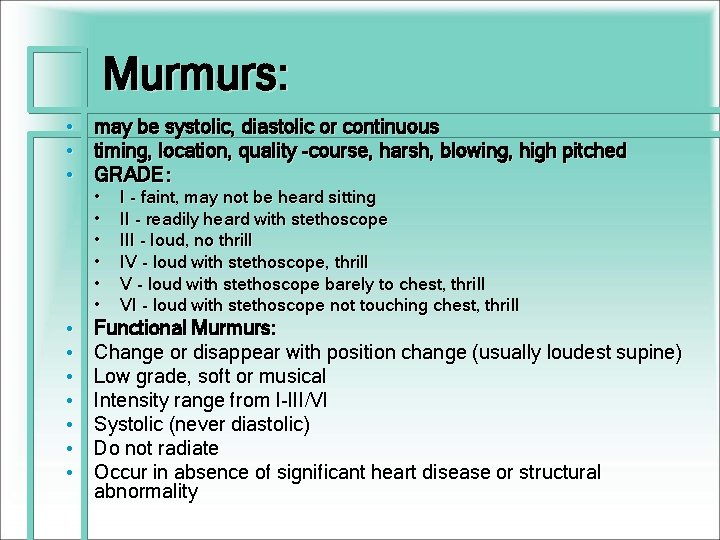
Murmurs: • may be systolic, diastolic or continuous • timing, location, quality -course, harsh, blowing, high pitched • GRADE: • • • • I - faint, may not be heard sitting II - readily heard with stethoscope III - loud, no thrill IV - loud with stethoscope, thrill V - loud with stethoscope barely to chest, thrill VI - loud with stethoscope not touching chest, thrill Functional Murmurs: Change or disappear with position change (usually loudest supine) Low grade, soft or musical Intensity range from I-III/VI Systolic (never diastolic) Do not radiate Occur in absence of significant heart disease or structural abnormality
Gastro-Intestinal Abdominal Assessment Pillitteri
Abdomen: Key Points • • Contour Bowel Sounds & Peristalsis Skin: color, veins Umbilicus Assess for Tenderness, Ridigity, Tympany, Dullness Hernias: umbilical, inguinal, femoral Masses - size, shape, dullness, position, mobility Liver, Spleen, Kidneys, Bladder
Bowel Sounds • Normal: every 10 to 30 seconds. • Listen in each quadrant long enough to hear at least one bowel sound. • • Absent Hypoactive Normoactive Hyperactive
Stomachaches and Abdominal Pain • • • Excessive gas Chronic constipation Lactose intolerance Viral gastroenteritis Irritable bowel syndrome • Heartburn or indigestion • GERD • Food allergy • Parasite infections (Giardia) What are we most concerned about?
Stomachaches and Abdominal Pain • Appendicitis • Bowel obstruction -Cholecystitis with or without gallstones • Food poisoning (salmonella, shigella) • Inflammatory Bowel Disease – • Crohn's disease • Ulcerative colitis • • Hernia Intussusception Kidney stones Pancreatitis Sickle cell crisis Ulcers Urinary tract infections
Signs and Symptoms • • Appearance –color, facial, ROM, gait, position Pain – get your pain scales out Nausea Vomiting Diarrhea Bloating Vomiting Inability to pass gas or stool
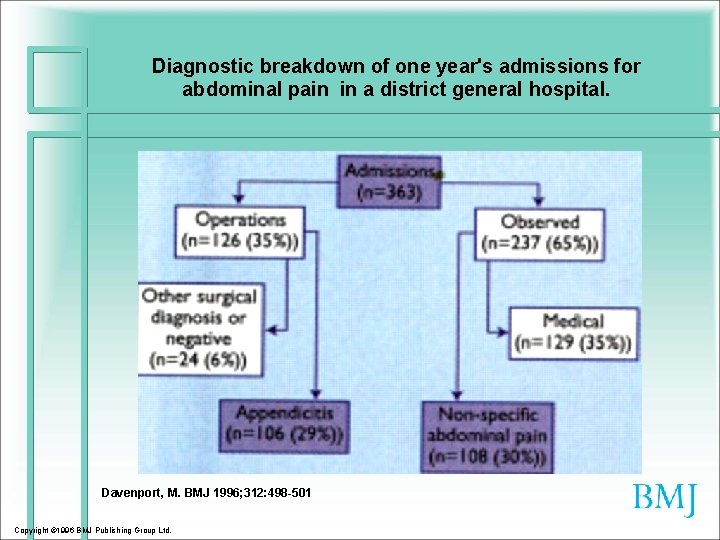
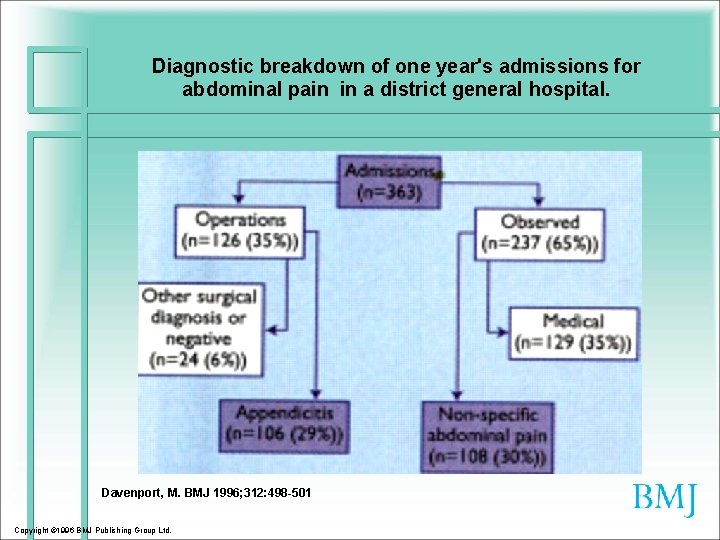
Diagnostic breakdown of one year's admissions for abdominal pain in a district general hospital. Davenport, M. BMJ 1996; 312: 498 -501 Copyright © 1996 BMJ Publishing Group Ltd.
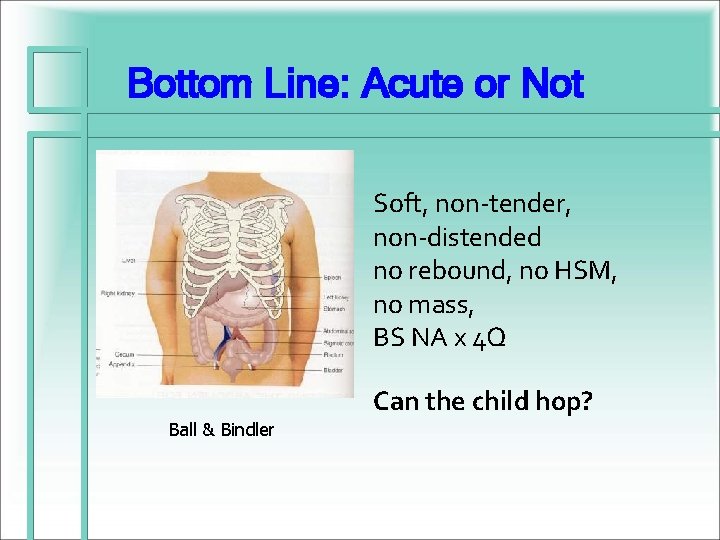
Bottom Line: Acute or Not Soft, non-tender, non-distended no rebound, no HSM, no mass, BS NA x 4 Q Can the child hop? Ball & Bindler
Musculo-Skeletal • FROM, MAE - neck, shoulder, elbow, wrist, hip, knee, ankle, foot, digits • Alignment, contour, strength, weakness & symmetry • Limb, joint mobility: stiffness, contractures • Gait – observe child walking without shoes • Spinal alignment - Scoliosis • Muscle Strength & Tone • Hips – O & B • Reflexes • Pre-Participation Sports P. E. – • NJ’s new guidelines: http: //www. state. nj. us/education/districts/ppeq. doc
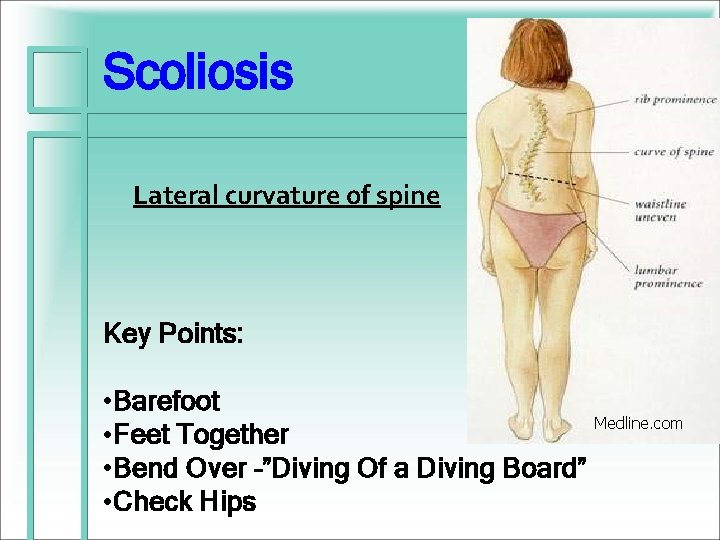
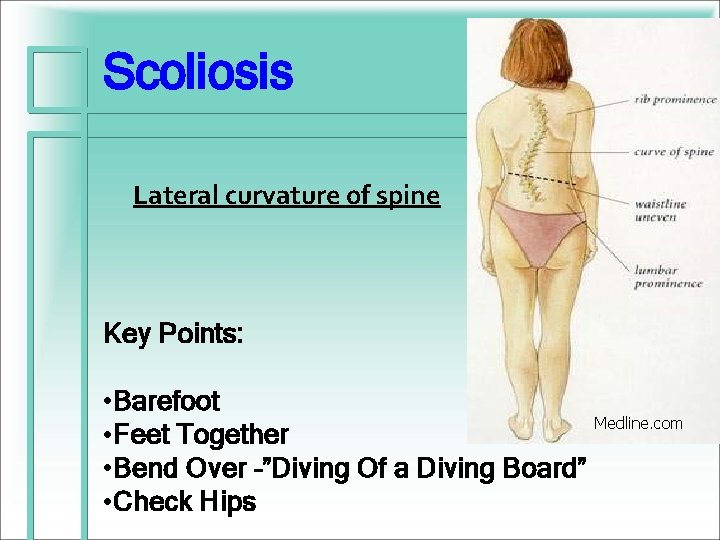
Scoliosis Lateral curvature of spine Key Points: • Barefoot • Feet Together • Bend Over –”Diving Of a Diving Board” • Check Hips Medline. com
Assessment • The Five P’s: • • • Pain Paresthesia Passive stretch Pressure Pulse-less-ness

Skin, Nails & Hair • • Rashes Lesions Lacerations Lumps Bruises Bites Infections
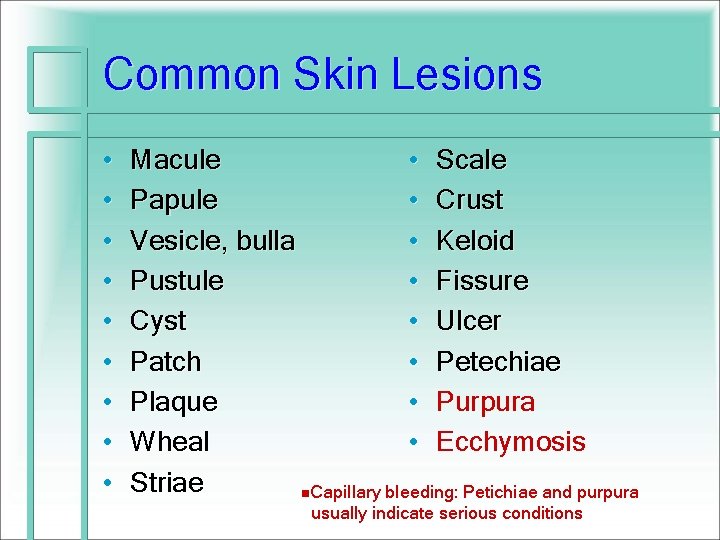
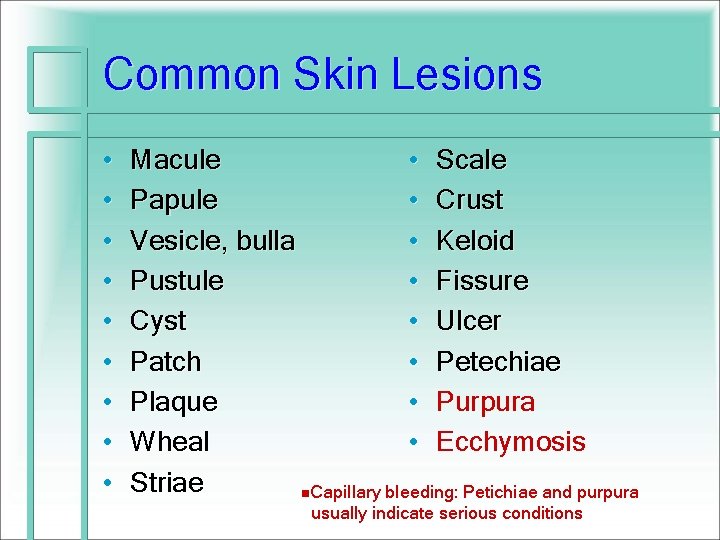
Common Skin Lesions • • • Macule • Scale Papule • Crust Vesicle, bulla • Keloid Pustule • Fissure Cyst • Ulcer Patch • Petechiae Plaque • Purpura Wheal • Ecchymosis Striae n. Capillary bleeding: Petichiae and purpura usually indicate serious conditions

Skin Infections • • • Bacterial infections Abscess formation Severity varies with skin integrity, immune and cellular defenses • Examples: • impetigo • cellulitis
Viral Skin Infections • Most communicable diseases of childhood have characteristic rash • Examples: verruca, herpes simplex types I and II, varicella zoster, molluscum contagiosum
Fungal Skin Infections • Superficial infections that live on the skin • Also known as dermatophytoses, tinea • Transmission from person to person or from infected animal to human • Examples: tinea capitis, tinea corporis, tinea pedis, candidiasis
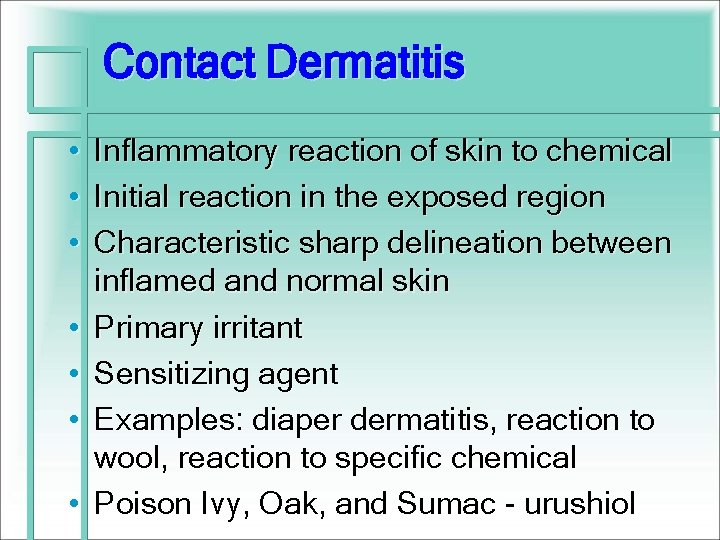
Contact Dermatitis • • Inflammatory reaction of skin to chemical Initial reaction in the exposed region Characteristic sharp delineation between inflamed and normal skin Primary irritant Sensitizing agent Examples: diaper dermatitis, reaction to wool, reaction to specific chemical Poison Ivy, Oak, and Sumac - urushiol

Miscellaneous Skin Disorders • • • Urticaria Psoriasis Alopecia Intertrigo Stevens-Johnson syndrome Neurofibromatosis
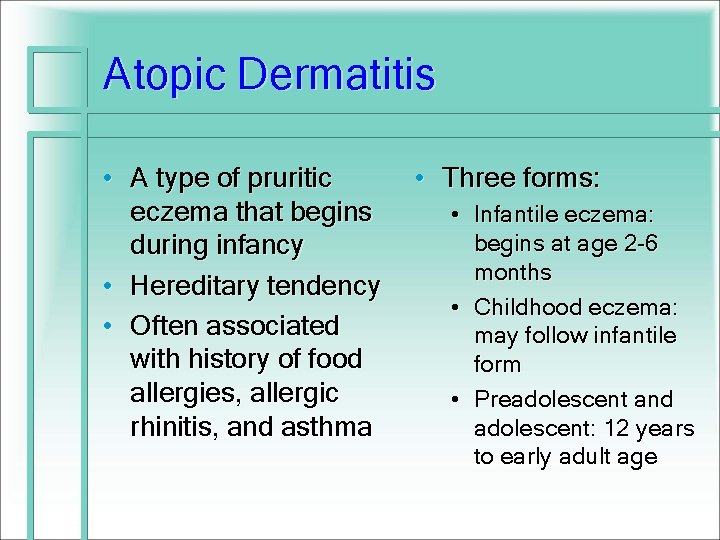
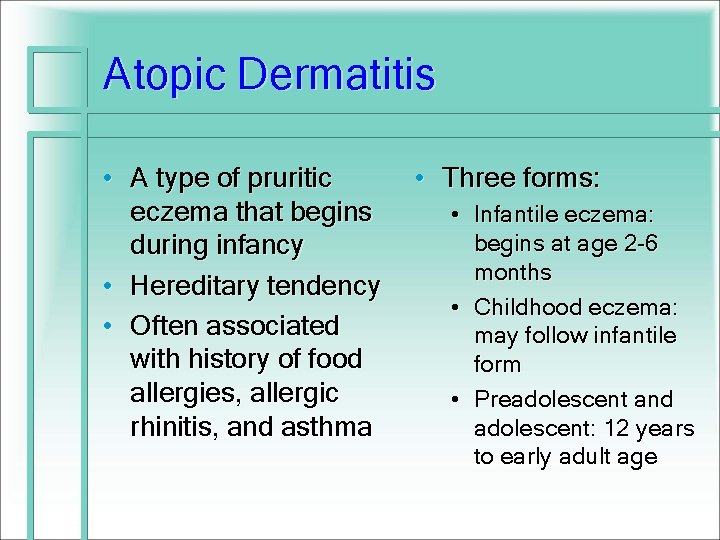
Atopic Dermatitis • A type of pruritic eczema that begins during infancy • Hereditary tendency • Often associated with history of food allergies, allergic rhinitis, and asthma • Three forms: • Infantile eczema: begins at age 2 -6 months • Childhood eczema: may follow infantile form • Preadolescent and adolescent: 12 years to early adult age
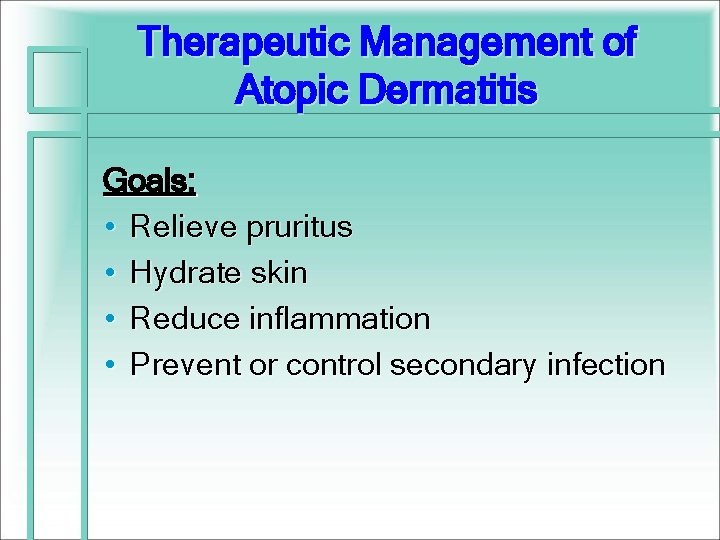
Therapeutic Management of Atopic Dermatitis Goals: • Relieve pruritus • Hydrate skin • Reduce inflammation • Prevent or control secondary infection
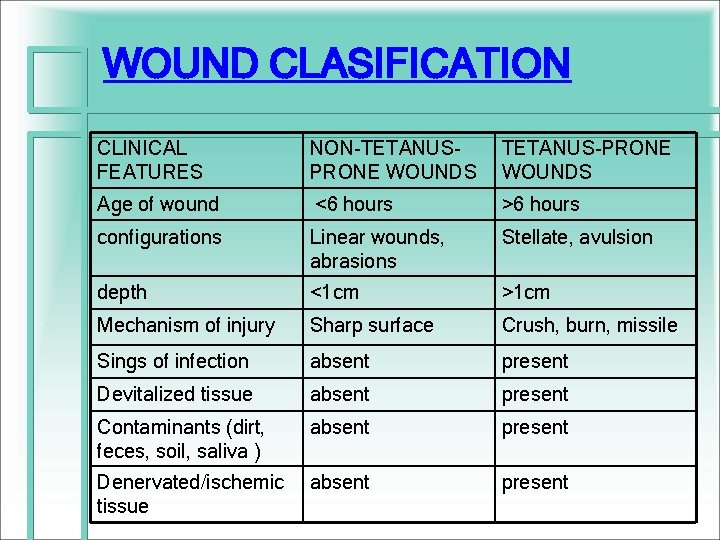
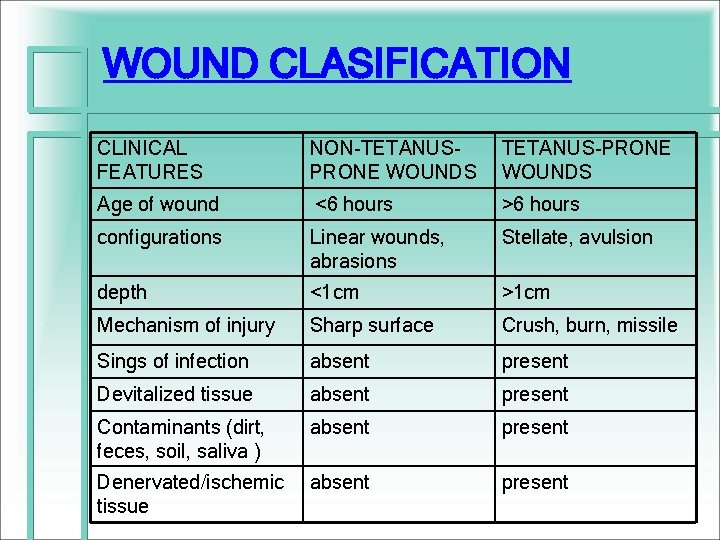
WOUND CLASIFICATION CLINICAL FEATURES NON-TETANUSPRONE WOUNDS TETANUS-PRONE WOUNDS Age of wound <6 hours >6 hours configurations Linear wounds, abrasions Stellate, avulsion depth <1 cm >1 cm Mechanism of injury Sharp surface Crush, burn, missile Sings of infection absent present Devitalized tissue absent present Contaminants (dirt, feces, soil, saliva ) absent present Denervated/ischemic tissue absent present
The School-Age Child • Privacy and modesty. • Explain procedures and equipment. • Interact with child during exam.
Adolescent • Privacy issues – first consideration • HEADS: home life, education, alcohol, drugs, sexual activity / suicide • GAPS Guidelines for Adolescent Preventive Services • Bright Futures
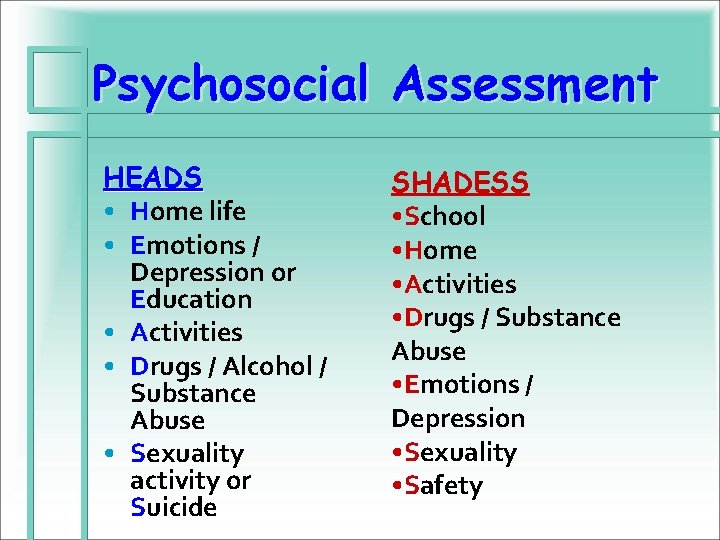
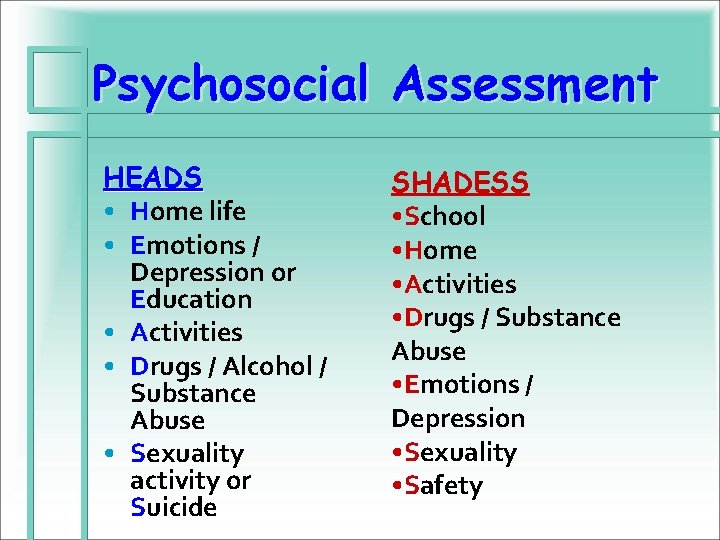
Psychosocial Assessment HEADS • Home life • Emotions / Depression or Education • Activities • Drugs / Alcohol / Substance Abuse • Sexuality activity or Suicide SHADESS • School • Home • Activities • Drugs / Substance Abuse • Emotions / Depression • Sexuality • Safety
Common School Health Focused Assessments • The “I don’t feel good” – where do I begin? • Behavioral / Mental Health Concerns • Chronic Conditions & Special Needs • What Else?
The “I don’t feel good”
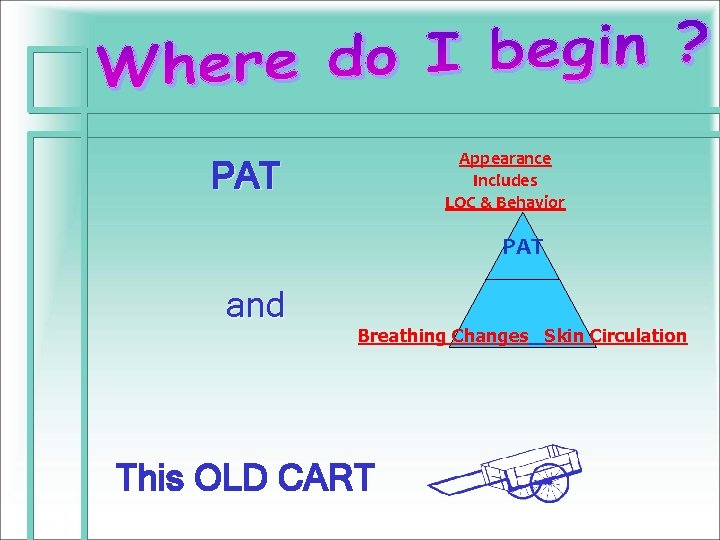
Appearance Includes LOC & Behavior PAT and Breathing Changes Skin Circulation This OLD CART
Common School Health Focused Assessments • Emergencies & Trauma – Allergic Reactions, Asthma, Head, Abdomen, Limb, Other • Skin – Rashes, Lacerations, Lumps, Bumps & Bruises • The Frequent Fliers – Headaches, Stomachaches, Chest Pain, Coughs & Fevers • Other HEENT
Emergencies & Trauma • Allergic Reactions • Asthma • Head • Abdomen • Limb • Other
The Frequent Fliers • • • Headaches Stomachaches Nosebleeds Chest Pain Coughs & Fevers
Frequent Fliers If only you could cash in on those miles!
Behavioral / Mental Health Concerns • • • Developmental Delays Depression Aggressive Behaviors Suicide Risks Other Mental Health Issues
Chronic Conditions & Special Needs • Asthma • Diabetes • Neuro – seizures • Sickle Cell Anemia • Cerebral Palsy • ADHD
Additional “To – Do’s” • Documentation • –SOAP Notes • Quality Improvement – - chart reviews • Confidentiality – seriously!
Resources and References
• Jan Chandler RN, MSN, CNS, PNP Pediatric Nursing: Nursing Care of Children and Young Adults: Pediatric Physical Assessment • Colyar, M. Well Child Assessment for Primary Care Providers. Philadelphia, PA: F. A. Davis Company. • Duderstadt, K. Pediatric Physical Examination. St. Louis, MO: Mosby, Inc. • Engel, J. Pediatric Assessment 5 th. Ed. St. Louis, MO: Mosby, Inc. • Wong’s Essentials of Pediatric Nursing 8 th ed. • AAP Preparticipation Physical Evaluation. Available @ www. aap. org • Resource Manual for the Nurse in the School Setting http: //www. emsc. org/school/frameschool. htm • American Medical Association Guidelines for Adolescent Preventive Services (GAPS) http: //www. ama-assn. org/ama/pub/category/2280. html • American School Health Association http: //www. ashaweb. org • The Auscultation Assistant @ http: //www. wilkes. med. ucla. edu/intro. html • BMI Calculator: http: //www. cdc. gov/nccdphp/dnpa/bmi / • 2007 Asthma Guidelines: http: //www. nhlbi. nih. gov/guidelines/asthma/index. htm
We Know It’s a Jungle Out There!
The Power of Nursing Never doubt how vitally important you are; never doubt how important your work is – and never expect anyone to acknowledge it before you do. Every moment, in everything you do, you are making a difference. In fact, you are in the business of making a difference in other people’s lives. In that difference lies their healing and your power. Never forget it. Leah L. Curtin, RN, MS, MA, DSC, FAAN