Pediatric Shock Pathophysiology Classification Evaluation and Management Presented

- Slides: 41
Pediatric Shock: Pathophysiology, Classification, Evaluation and Management Presented by: Jan Elliott MSN, APRN, FNP-C
Background Most frequent causes of shock: Hypovolemia from gastroenteritis most common worldwide Trauma is still significant cause of death in children Severe Sepsis is frequently seen in children world wide Low birthweight infants Infants younger than one month of age Immunosuppressed patients Chronically ill children
Definition Pathophysiologic state that results in decreased tissue perfusion Initially reversible Prolonged tissue hypoxia: Generalized cellular hypoxia Derangement of critical biochemical processes
Reference: Pomerantz, W. J. & Roback, M. G. (2018). Pathophysiology and classification of shock in children. Retrieved from: https: //www. uptodate. com/contents/pathophysiology-and-classification-of-shock-in-children/print? topic. Ref=6397&source=see_link Waltzman, M. (2018). Initial evaluation of shock in children. Retrieved from: https: //www. uptodate. com/contents/initial-evaluation-ofshock-inchildren? search=initial%20 evaluation%20 of%20 shock%20 in%20 children&source=search_result&selected. Title=1~150&usage_type=default &display_rank=1 Waltzman, M. (2018). Initial Management of shock in children. Retrieved from: https: //www. uptodate. com/contents/initialmanagement-of-shock-in-children? source=history_widget Weiss, S. L. & Pomerantz, W. J. (2018). Septic shock in children: rapid recognition and initial resuscitation (first hour). Retrieved from: https: //www. uptodate. com/contents/septic-shock-in-children-rapid-recognition-and-initial-resuscitation-firsthour? search=initial%20 evaluation%20 of%20 shock%20 in%20 children&source=search_result&selected. Title=6~150&usage_type=default&di splay_rank=6
Derangement of Critical Biochemical Processes Cell membrane ion pump dysfunction Intracellular edema Leakage of intracellular contents into extracellular space Inadequate regulation of intracellular p. H
Dynamic Process Decompensation begins with derangement of biochemical processes Rapid progression to irreversible shock Mortality less in children Incidents of shock increasing in children Pre-hypotensive shock recognition lowers mortality
� Shotgun Approach
E. R. S. L Early Recognition Saves Lives
Early Recognition Tachycardia (not conclusive alone) Central & Peripheral pulses quality Skin color, temp & moisture Capillary refill Mental Status Hypotension: late sign, decompensation has occurred
Approach & Timeline 1 st Hour Airway, oxygenation, ventilation Circulation Threshold heart rate (not too high or too low) to ensure adequate CO
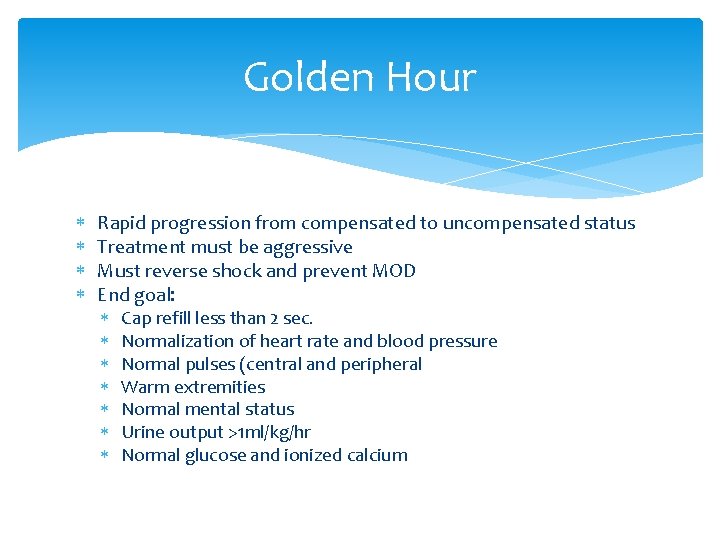
Golden Hour Rapid progression from compensated to uncompensated status Treatment must be aggressive Must reverse shock and prevent MOD End goal: Cap refill less than 2 sec. Normalization of heart rate and blood pressure Normal pulses (central and peripheral Warm extremities Normal mental status Urine output >1 ml/kg/hr Normal glucose and ionized calcium
Within that Golden Hour Prompt identification and treatment of the site or sites of infection Broad spectrum IV antibiotics within one hour of presentation Effective delivery requires two IV sites: 1 st devoted to fluid resus and 2 nd for antibiotics If possible cultures should be obtained prior to antibiotics
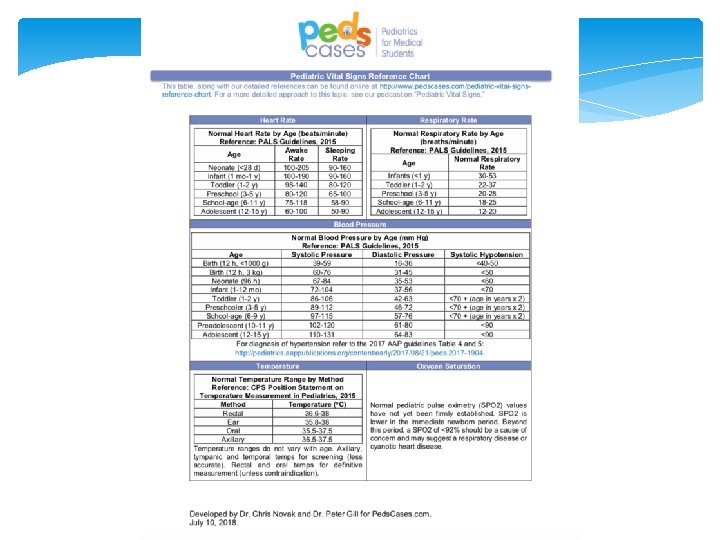
Stages of Shock in Children Compensated: B/P normal Hypotensive: compensatory mechanisms overwhelmed Irreversible: tachycardia changes to bradycardia
Mechanisms of Shock Hypovolemic GI losses, hemorrhage insensible losses (burns), 3 rd spacing Distributive Sepsis, anaphylaxis, neurological injury (↑T 6) Cardiogenic Myocardial injury, dysrhythmias, CHD, poisonings, sepsis Obstructive Hypoplastic left heart, tamponade, PE, pneumothorax
Obstructive Shock Must be identified and treated: Cardiac tamponade Pulmonary embolus Pneumothorax Ductal dependent congenital heart defect (prostaglandin E 1)
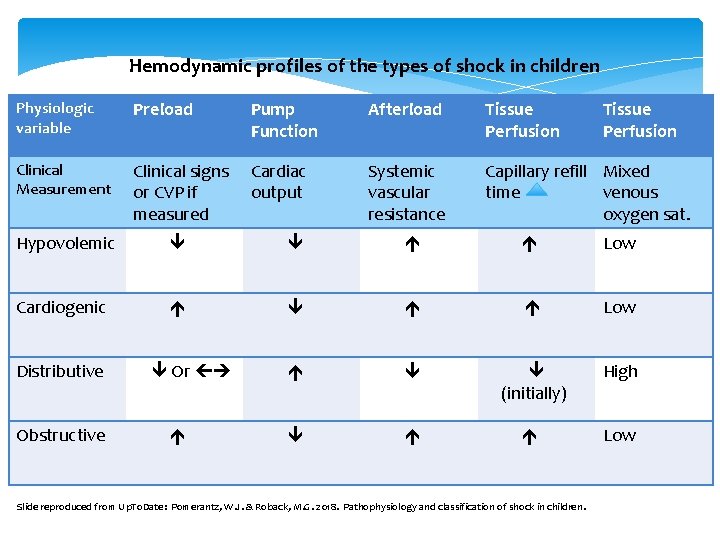
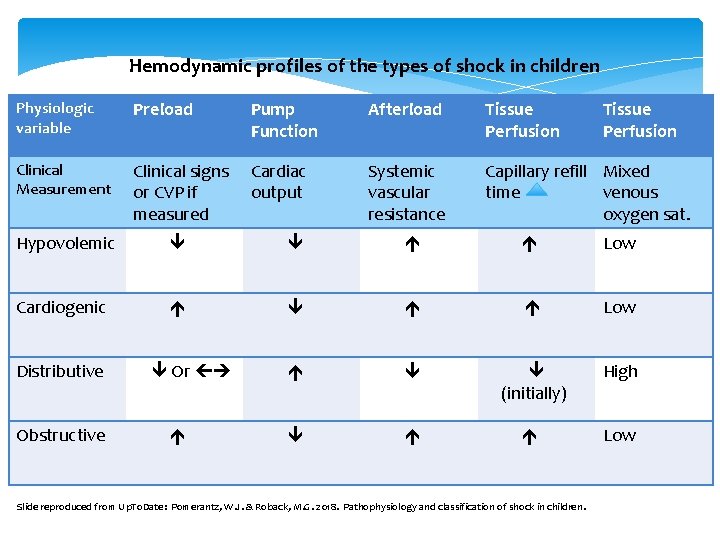
Hemodynamic profiles of the types of shock in children Physiologic variable Preload Pump Function Afterload Tissue Perfusion Clinical Measurement Clinical signs or CVP if measured Cardiac output Systemic vascular resistance Capillary refill Mixed time venous oxygen sat. Hypovolemic Low Cardiogenic Low (initially) High Low Distributive Obstructive Or Slide reproduced from Up. To. Date: Pomerantz, W. J. & Roback, M. G. 2018. Pathophysiology and classification of shock in children.
Goals of Management Systolic B/P at least 5 th percentile for age Quality of central and peripheral pulses (strong distal pulses equal to central) Skin perfusion (warm, with cap refill < 2 seconds Mental status (normal) Urine output (≥ 1 ml/kg/hour once volume is restored) Serum Lactate (2. 0 -2. 5)

Priorities of Management CABC as in PALS, ENPC Identify etiology Treatment of causative mechanism of shock Monitoring of progress
Fluids? How Much? How fast? Hypovolemic shock 20 ml/kg bolus isotonic crystalloid Infuse over 5 -10 minutes Repeat up to four times in patients w/o improvement and NO signs of fluid overload Consider Blood Replacement if hemorrhage Consider Vasoactive drug therapy and corticosteroid administration in sepsis
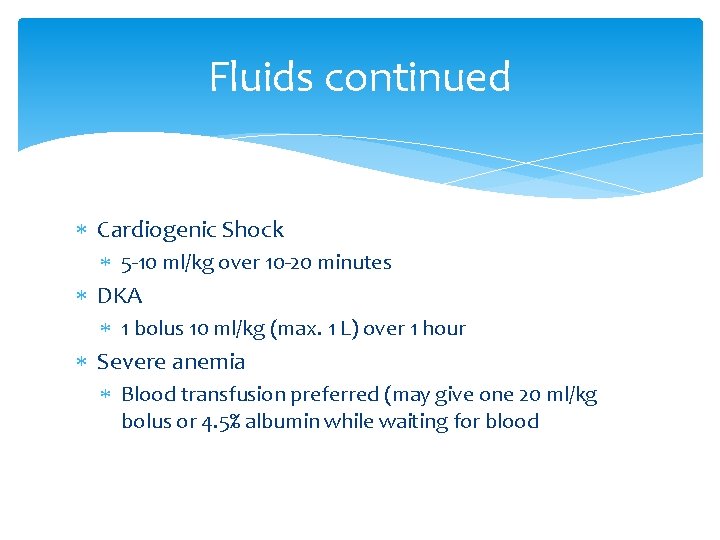
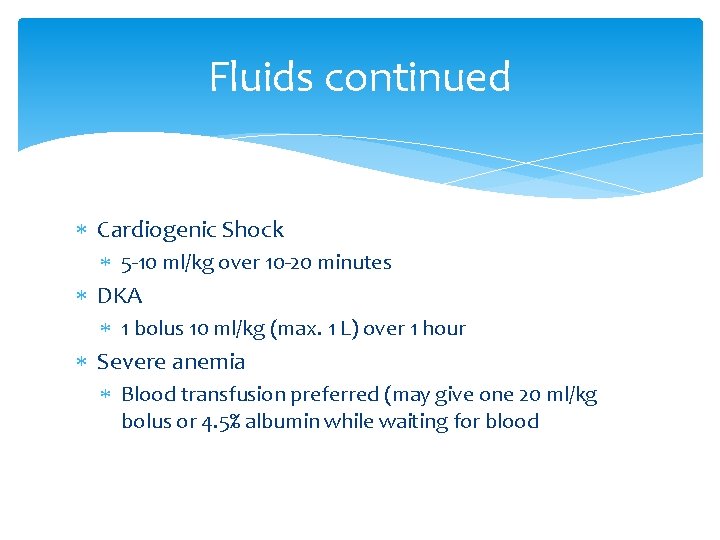
Fluids continued Cardiogenic Shock 5 -10 ml/kg over 10 -20 minutes DKA 1 bolus 10 ml/kg (max. 1 L) over 1 hour Severe anemia Blood transfusion preferred (may give one 20 ml/kg bolus or 4. 5% albumin while waiting for blood
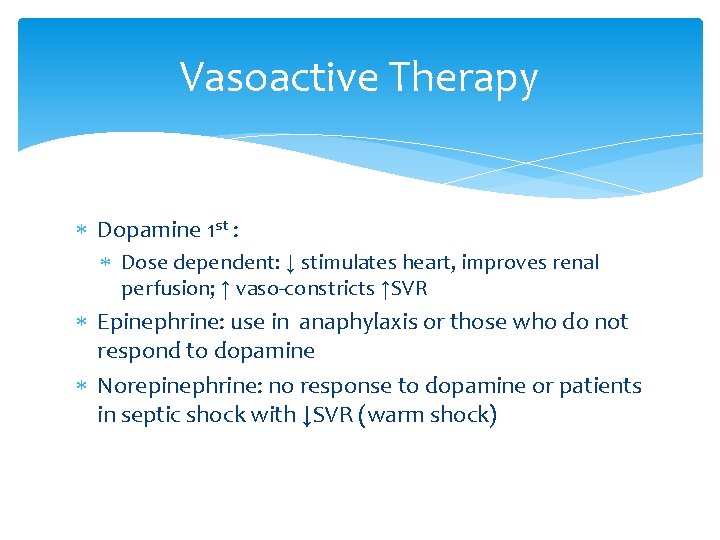
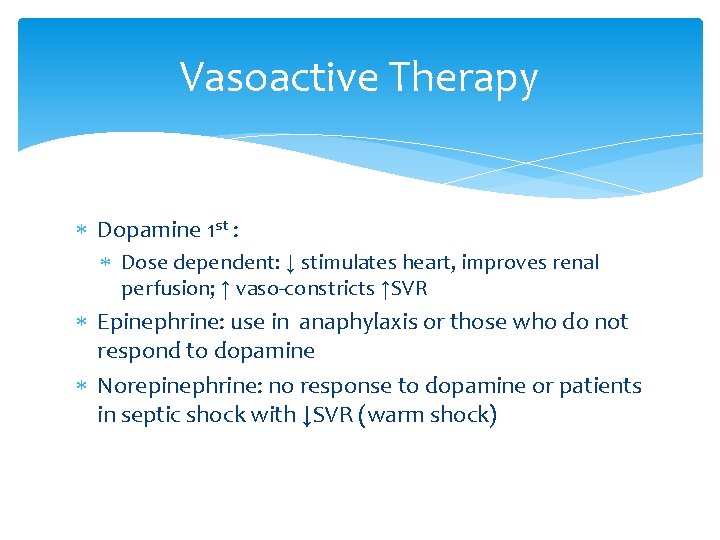
Vasoactive Therapy Dopamine 1 st : Dose dependent: ↓ stimulates heart, improves renal perfusion; ↑ vaso-constricts ↑SVR Epinephrine: use in anaphylaxis or those who do not respond to dopamine Norepinephrine: no response to dopamine or patients in septic shock with ↓SVR (warm shock)
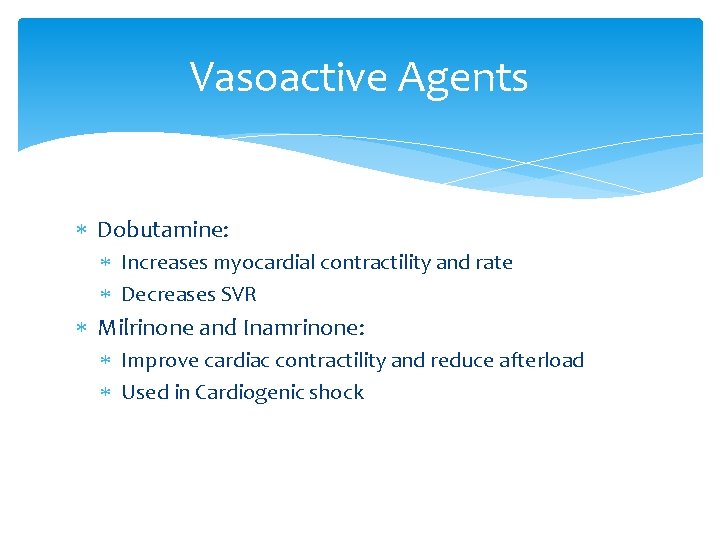
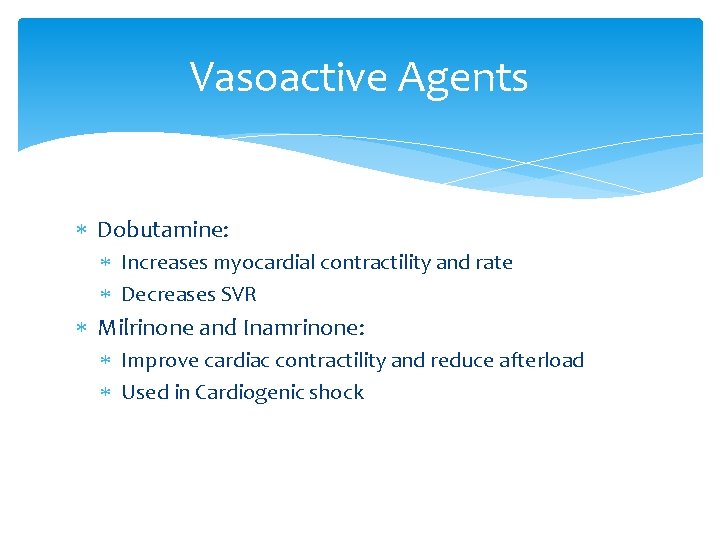
Vasoactive Agents Dobutamine: Increases myocardial contractility and rate Decreases SVR Milrinone and Inamrinone: Improve cardiac contractility and reduce afterload Used in Cardiogenic shock
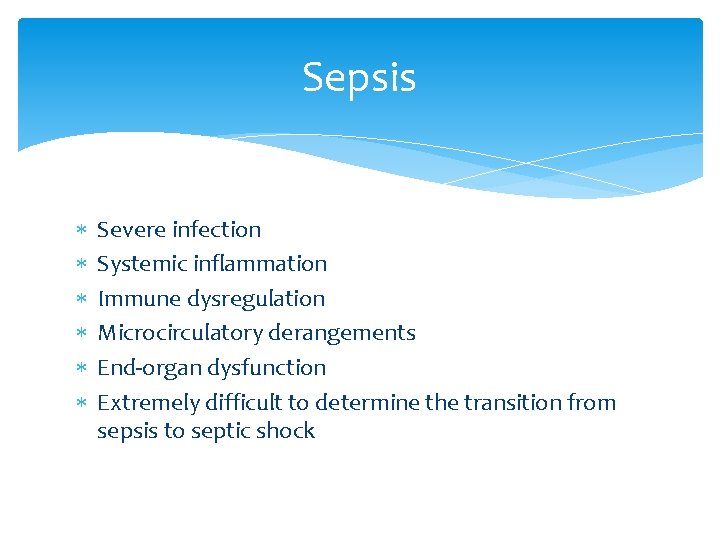
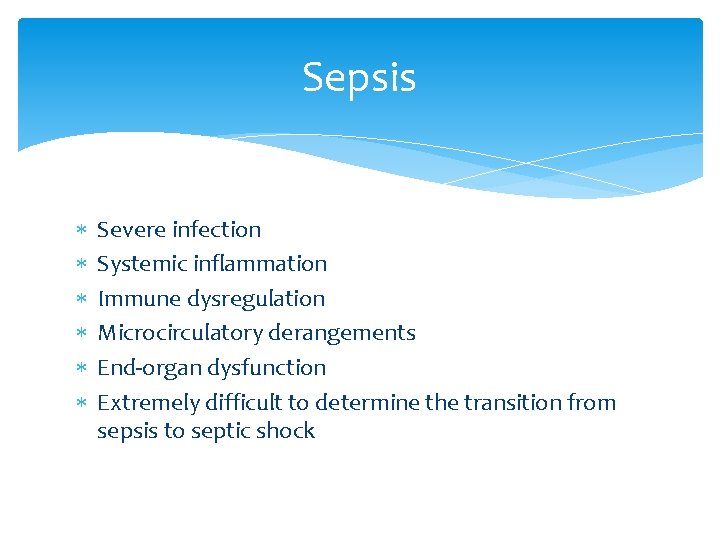
Sepsis Severe infection Systemic inflammation Immune dysregulation Microcirculatory derangements End-organ dysfunction Extremely difficult to determine the transition from sepsis to septic shock
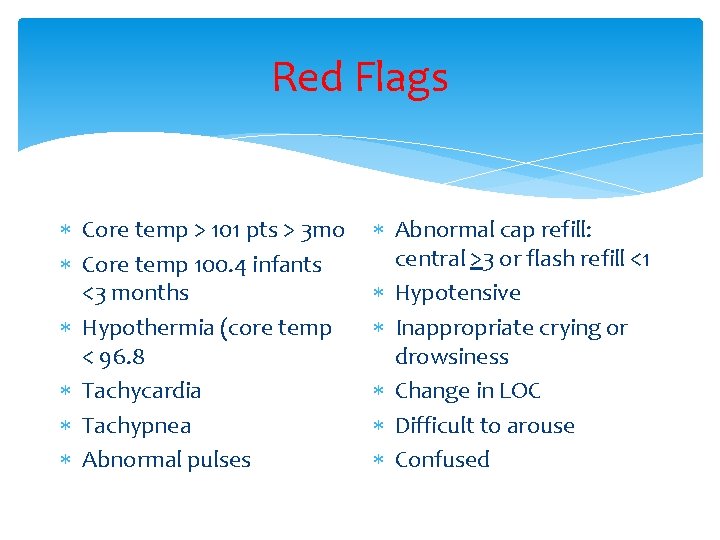
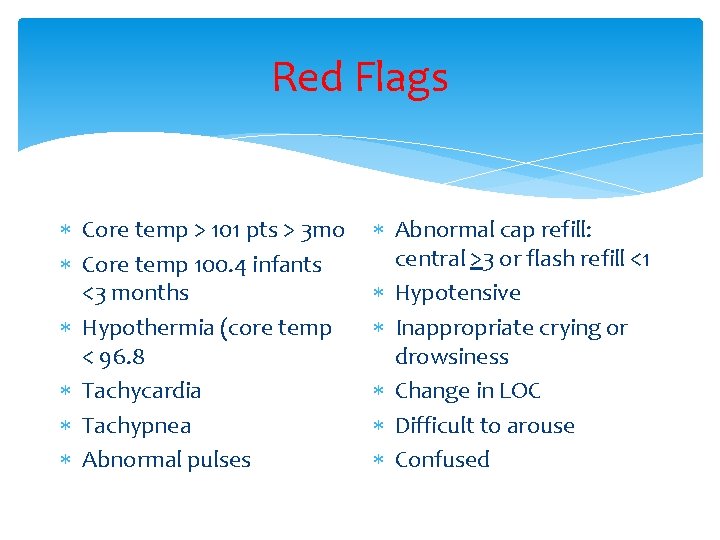
Red Flags Core temp > 101 pts > 3 mo Core temp 100. 4 infants <3 months Hypothermia (core temp < 96. 8 Tachycardia Tachypnea Abnormal pulses Abnormal cap refill: central >3 or flash refill <1 Hypotensive Inappropriate crying or drowsiness Change in LOC Difficult to arouse Confused
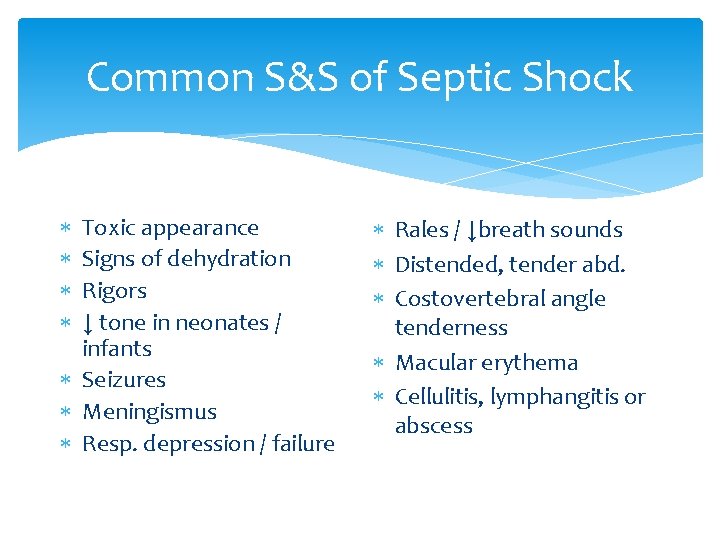
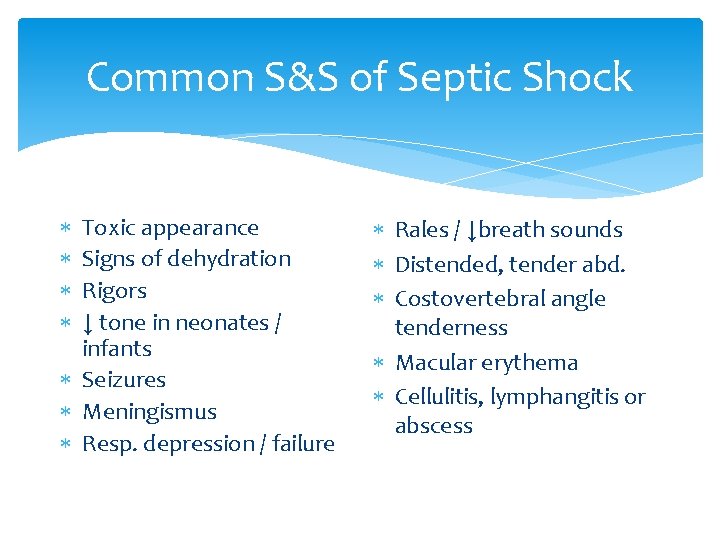
Common S&S of Septic Shock Toxic appearance Signs of dehydration Rigors ↓ tone in neonates / infants Seizures Meningismus Resp. depression / failure Rales / ↓breath sounds Distended, tender abd. Costovertebral angle tenderness Macular erythema Cellulitis, lymphangitis or abscess
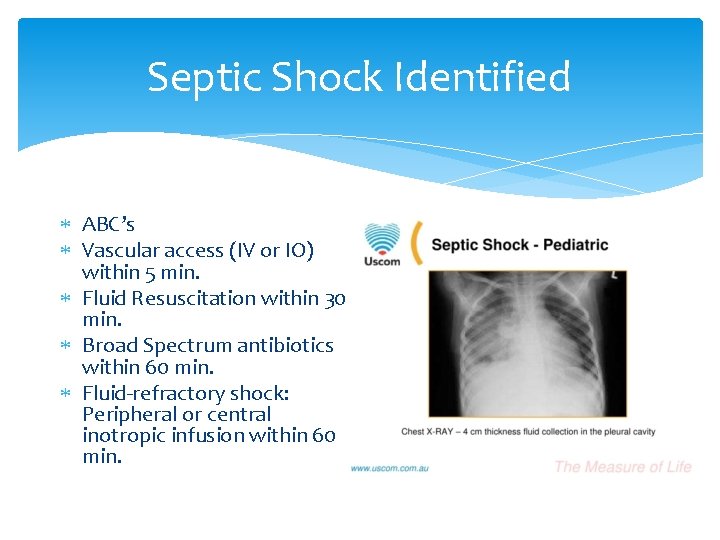
Septic Shock Identified ABC’s Vascular access (IV or IO) within 5 min. Fluid Resuscitation within 30 min. Broad Spectrum antibiotics within 60 min. Fluid-refractory shock: Peripheral or central inotropic infusion within 60 min.
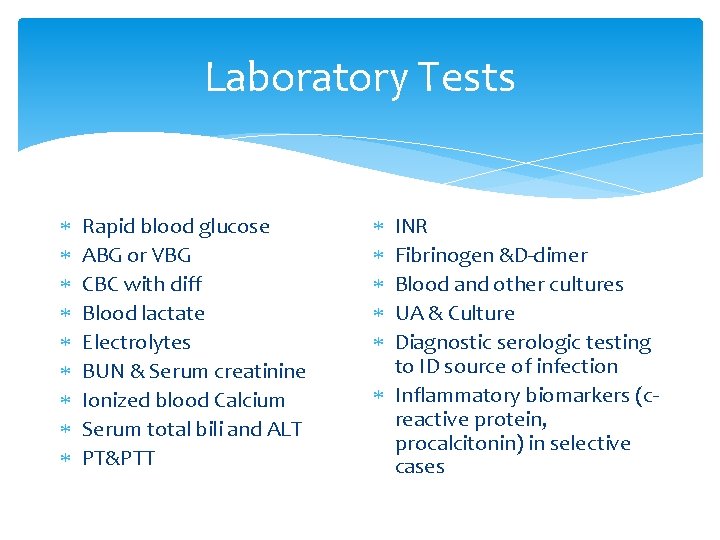
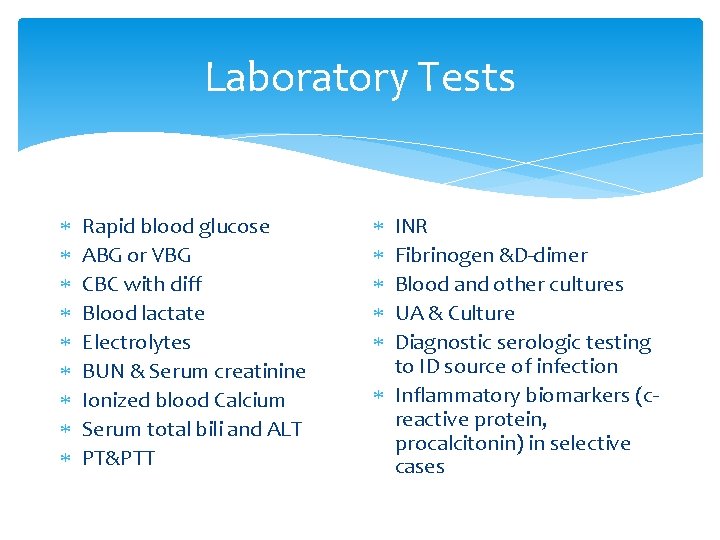
Laboratory Tests Rapid blood glucose ABG or VBG CBC with diff Blood lactate Electrolytes BUN & Serum creatinine Ionized blood Calcium Serum total bili and ALT PT&PTT INR Fibrinogen &D-dimer Blood and other cultures UA & Culture Diagnostic serologic testing to ID source of infection Inflammatory biomarkers (creactive protein, procalcitonin) in selective cases
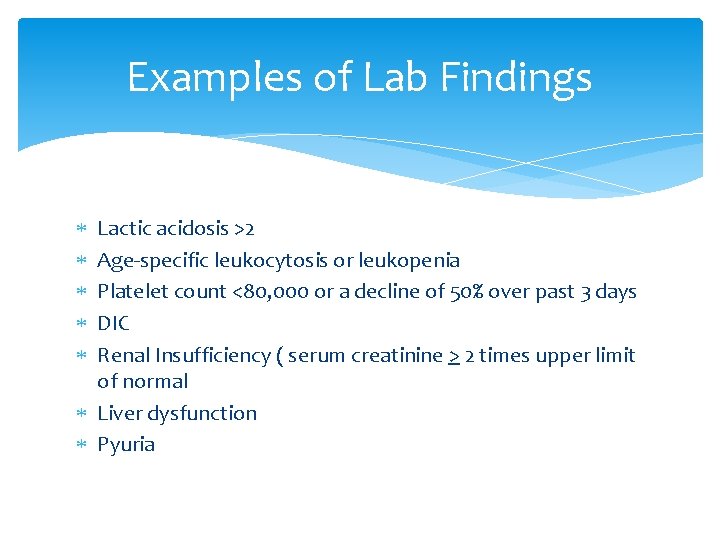
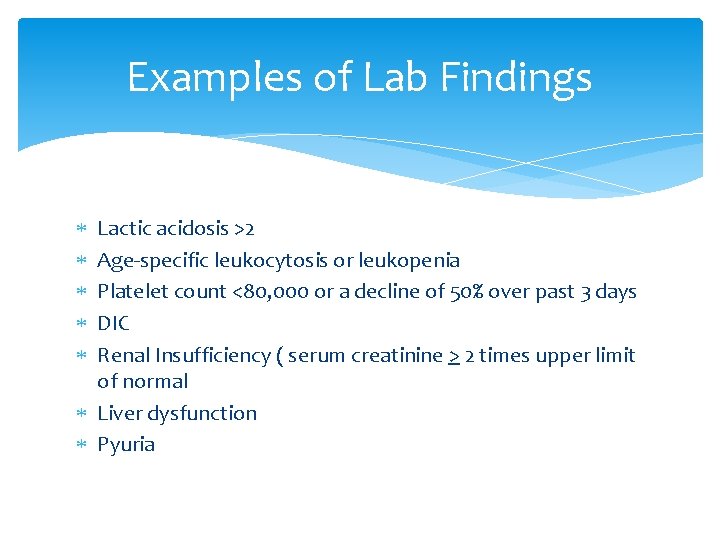
Examples of Lab Findings Lactic acidosis >2 Age-specific leukocytosis or leukopenia Platelet count <80, 000 or a decline of 50% over past 3 days DIC Renal Insufficiency ( serum creatinine > 2 times upper limit of normal Liver dysfunction Pyuria
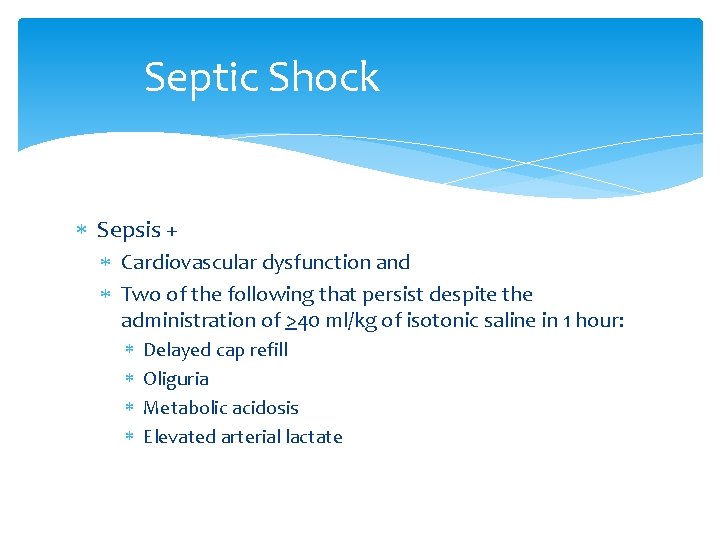
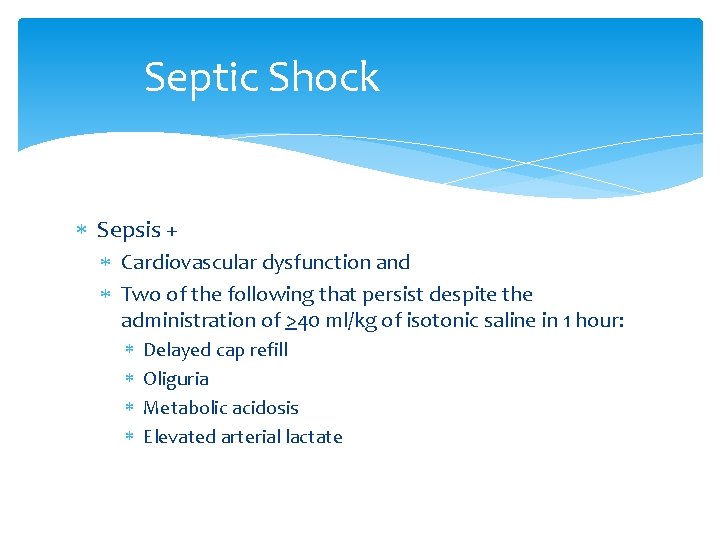
Septic Shock Sepsis + Cardiovascular dysfunction and Two of the following that persist despite the administration of >40 ml/kg of isotonic saline in 1 hour: Delayed cap refill Oliguria Metabolic acidosis Elevated arterial lactate
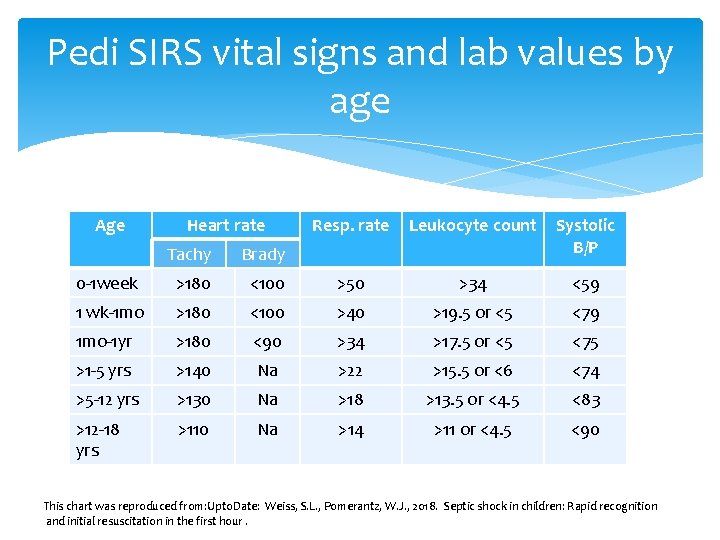
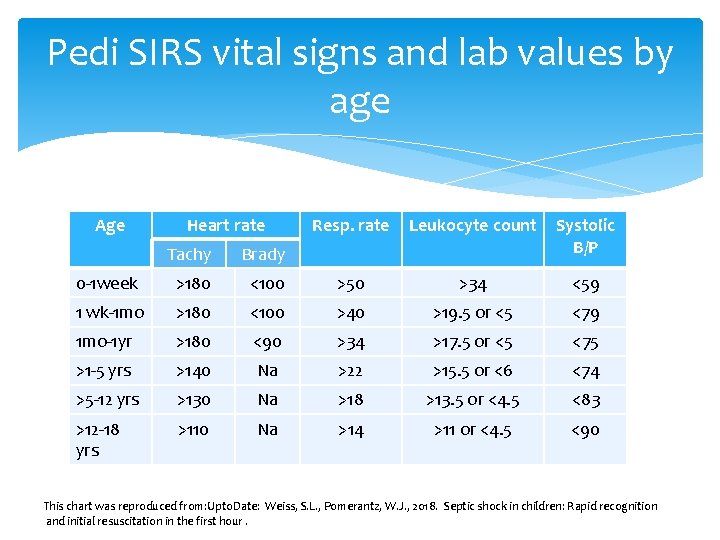
Pedi SIRS vital signs and lab values by age Age Heart rate Resp. rate Leukocyte count Systolic B/P Tachy Brady 0 -1 week >180 <100 >50 >34 <59 1 wk-1 mo >180 <100 >40 >19. 5 or <5 <79 1 mo-1 yr >180 <90 >34 >17. 5 or <5 <75 >1 -5 yrs >140 Na >22 >15. 5 or <6 <74 >5 -12 yrs >130 Na >18 >13. 5 or <4. 5 <83 >12 -18 yrs >110 Na >14 >11 or <4. 5 <90 This chart was reproduced from: Upto. Date: Weiss, S. L. , Pomerantz, W. J. , 2018. Septic shock in children: Rapid recognition and initial resuscitation in the first hour.
Cold versus Warm Shock
Warm Shock Hyperdynamic (vasodilation) Usually the initial presentation of adults Not necessarily the presentation in children Fever Flushed warm skin Tachypnea Flash capillary refill Bounding pulses No mottling of skin or if present, only feet and ankles
Sepsis: Cold Shock Frequent initial presentation in children Hypotension Tachycardia (narrow pulse pressure) Cold extremities Rapid shallow respirations Oliguria Altered LOC Cyanosis
Antibiotic Considerations Child’s age, history, co-morbidities, clinical syndrome, Gram stain data, and local resistance patterns Consultation with Pediatric Infectious Disease specialist
Antibiotic Recommendation Children >28 days (normal hosts) Vancomycin: (15 mg/kg, max. 1 -2 G, initial dose) Plus Cefotaxime (100 mg/kg, max 2 G for initial dose) Or Ceftriaxone (75 mg/kg, max 2 G for initial dose) Consider adding aminoglycoside (gentamycin) for GU Consider piperacillin with tazobactam, clindamycin or metronidazole for GI Consider combination therapy (to cover resistant organisms)
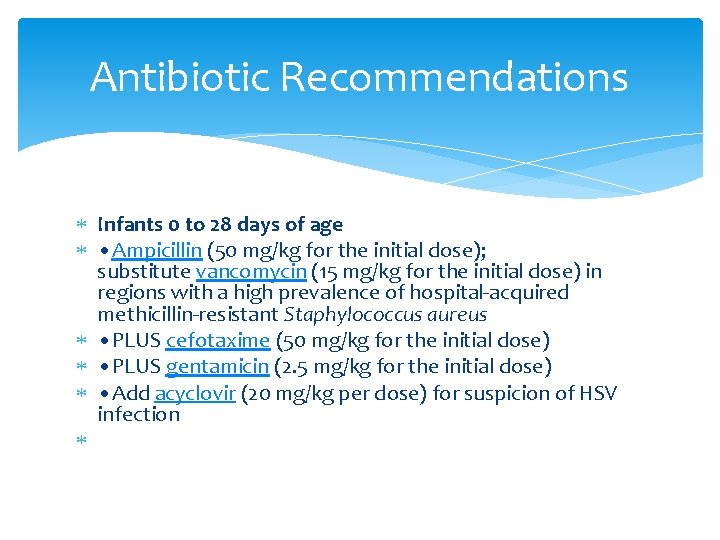
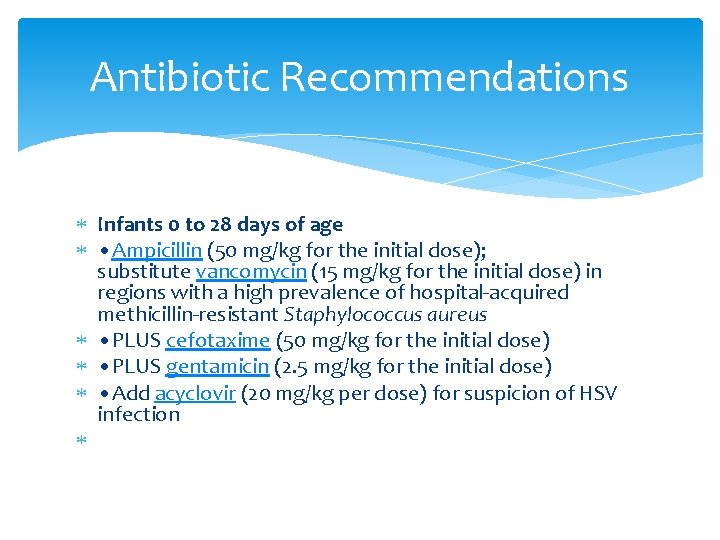
Antibiotic Recommendations Infants 0 to 28 days of age • Ampicillin (50 mg/kg for the initial dose); substitute vancomycin (15 mg/kg for the initial dose) in regions with a high prevalence of hospital-acquired methicillin-resistant Staphylococcus aureus • PLUS cefotaxime (50 mg/kg for the initial dose) • PLUS gentamicin (2. 5 mg/kg for the initial dose) • Add acyclovir (20 mg/kg per dose) for suspicion of HSV infection
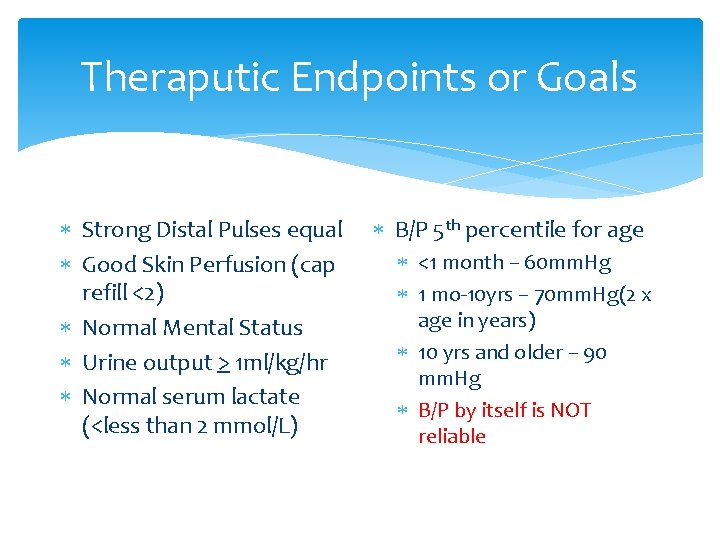
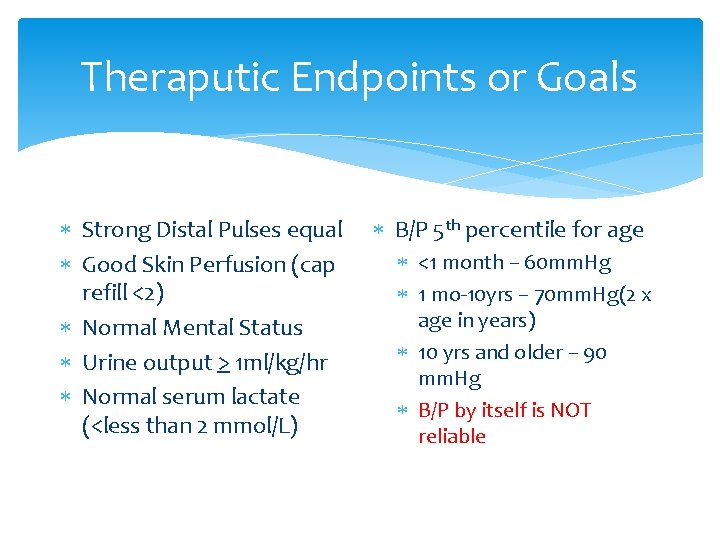
Theraputic Endpoints or Goals Strong Distal Pulses equal Good Skin Perfusion (cap refill <2) Normal Mental Status Urine output > 1 ml/kg/hr Normal serum lactate (<less than 2 mmol/L) B/P 5 th percentile for age <1 month – 60 mm. Hg 1 mo-10 yrs – 70 mm. Hg(2 x age in years) 10 yrs and older – 90 mm. Hg B/P by itself is NOT reliable
Summary E. R. S. L. Identify the type or types of shock Manage accordingly Continuous monitoring and re-evaluation Remember: May be presenting with multiple problems
Questions