Introducing outcome measures for palliative care in a

- Slides: 15
Introducing outcome measures for palliative care in a hospice setting Mary Denholm (CMT 1) Tabitha Thomas (Consultant) Arthur Rank House Hospice June 2015
Background • Outcome measures are a relatively new concept in palliative care • Conventional measures not applicable • Need to reflect the holistic approach of the specialty • Time frames short, quality of life of utmost importance – need to see direct relevance and benefit
Outcomes and Complexity Collaborative (OACC) Cicely Saunders Institute, King’s College London Initially SE London moving nationally “Open collaborative” Aiming for collaborative database to share experience of outcome measures • Goals include quality improvement, linking evidence and treatment, assess efficacy of interventions and “realistic and meaningful benchmarking” • •
The Outcome Measures Suite • Set of validated measures including: 1. Phase of illness (AN-SNAP modified definitions) 2. Australian Modified Karnofsky Performance Scale 3. Integrated Palliative Care Outcome Scale (IPOS) 4. Zarit Burden Interview (caregiver burden)
Aims of this QIP • PRIMARY OBJECTIVES: – To introduce step 3 (IPOS questionnaire) of the outcome measures suite to the Inpatient Unit at ARH – To audit implementation and compliance rates over a period of several months – Gather staff views on IPOS as an outcome measure • SECONDARY OBJECTIVES: – To forward this information to the OACC once complete
Integrated Palliative care Outcome Scale (IPOS) • Two versions – patient and proxy • Two questionnaires for each patient (admission and day 3 -5) • 10 questions (and subquestions) • Cover common symptoms (pain, SOB, bowel habit etc), and mood, practical/financial concerns, family worries, “being at peace”
Methods - audit • First cycle (August 2014) – Record sheet of new admissions, and whether first and second questionnaires completed • Second cycle (September – October 2014) – Process repeated following further discussion and raising of awareness with medical staff • Third assessment (May 2015) – ‘Snapshot’ assessment of current compliance rates
Methods – staff questionnaire • Simple staff questionnaire designed and distributed (November 2014) assessing: – Knowledge of IPOS – Willingness to help with IPOS implementation/completion – Views on usefulness of IPOS – Any other concerns or feedback
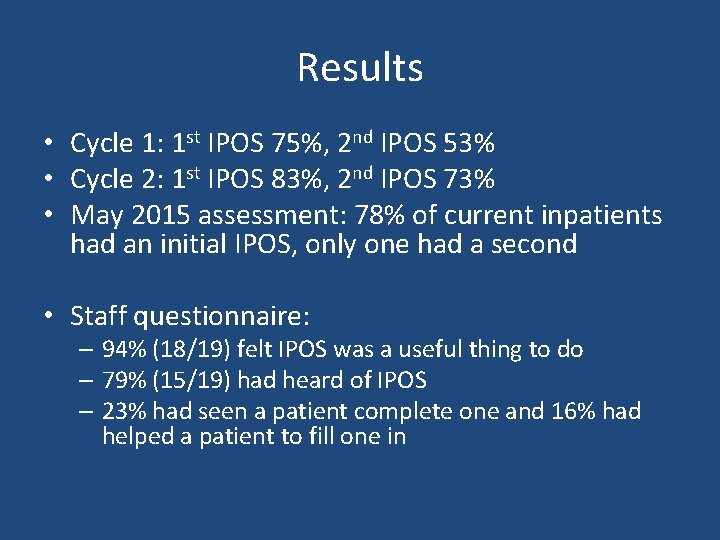
Results • Cycle 1: 1 st IPOS 75%, 2 nd IPOS 53% • Cycle 2: 1 st IPOS 83%, 2 nd IPOS 73% • May 2015 assessment: 78% of current inpatients had an initial IPOS, only one had a second • Staff questionnaire: – 94% (18/19) felt IPOS was a useful thing to do – 79% (15/19) had heard of IPOS – 23% had seen a patient complete one and 16% had helped a patient to fill one in
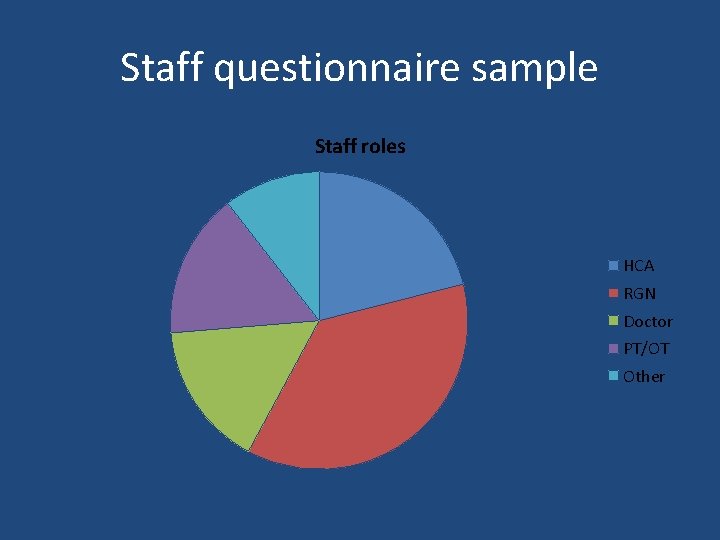
Staff questionnaire sample Staff roles HCA RGN Doctor PT/OT Other
Verbal feedback • Some patients are too poorly for this. Is this necessary for improving patient care/or symptom management? • Feel that patients are trying to cope with uncontrolled symptoms and struggling sometimes with their journey and would this be a benefit to them? • Patients’ relatives might have a contribution to symptom based questionnaires • Symptom based questionnaire would be useful if the information is the used by the MDT to address those symptoms • Self-perceived patient perspective very valuable
Educational intervention • Information sheet designed and distributed to staff • Explanation of IPOS methods and validity • Proposed value and benefits • Role within larger national initiative
Further steps and re-audit • Maintain and improve usage and compliance • Aim for process not to be user dependent – Some progress made by using ‘Getting to Know Me’ folders • Continue to widen staff participation • Further assess role of proxy questionnaire
Future directions • Provide information to national collaborative • Explore differences in patient symptom perception when completing questionnaires independently vs. with help from a relative • Continue to work as a team to tailor these outcome measures to the hospice environment and ethos

Questions?