PEI Palliative Care Conference Uncontrolled Pain in Palliative






















- Slides: 100

PEI Palliative Care Conference: Uncontrolled Pain in Palliative Care – An approach for when nothing seems to work ! Dr Edward J. Fitzgibbon Palliative Care Physician The Ottawa Hospital June 11 th 2015
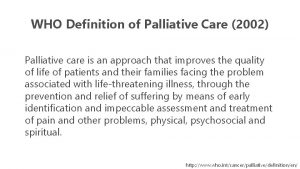
Cecily Saunders • “Palliative Care begins from the understanding that every patient has his or her own story, relationships and culture, and is worthy of respect as a unique individual. This respect includes giving the best available medical care and making the advances of recent decades available so that all have the best chance of using their time well”. Davies, E, Higginson, I. J. Palliative Care: the solid fact. WHO http: //www. euro. who. int/document/E 82931. pdf(2004)

Ready…. .

Outline • • Pain in Palliative Care. Pathophysiology Assessment An Approach to Management Non-Opioids Co-Analgesics Opioids Cases and discussion
Pain • Pain is defined “as an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage” (IASP 1979) • Pain is always subjective and each individual learns the meaning of pain through their experiences of injury or disease during early life. • Pain is a very personal experience and is what the patient says it is !

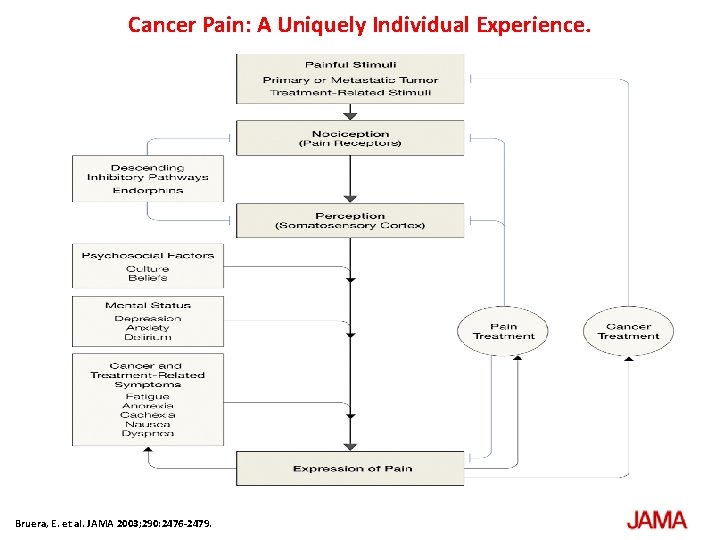
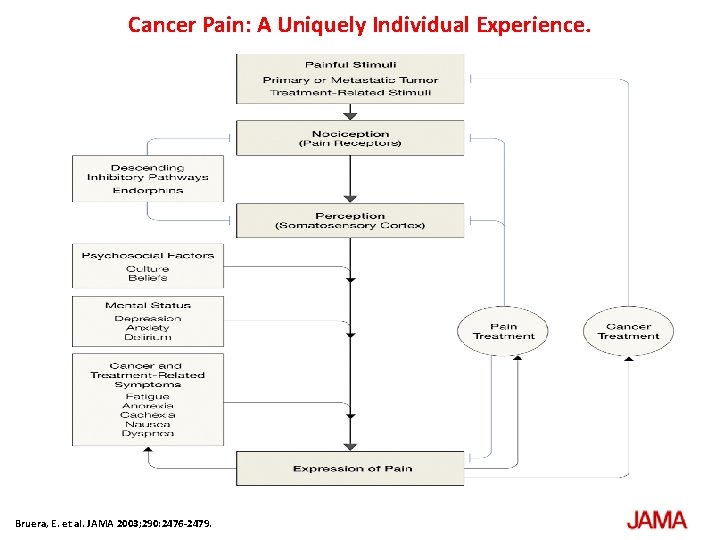
Cancer Pain: A Uniquely Individual Experience. Bruera, E. et al. JAMA 2003; 290: 2476 -2479.
Barriers to Pain Management • In-hospital patients with pain from non-surgical conditions are less likely to have their pain taken seriously enough to be treated. • Patient/ family reluctance to report pain and/or take opioids • Physician reluctance to prescribe opioids. • There is a large gap between what is known and what is practiced in the treatment of all kinds of pain
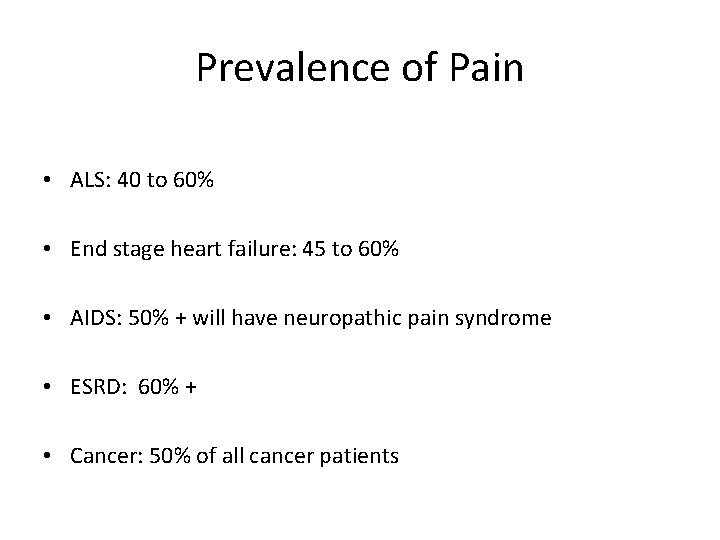
Prevalence of Pain • ALS: 40 to 60% • End stage heart failure: 45 to 60% • AIDS: 50% + will have neuropathic pain syndrome • ESRD: 60% + • Cancer: 50% of all cancer patients
Cancer Pain : Defining the Challenge • “Cancer Pain is a mixture of acute pain, chronic pain, tumor specific pain and treatment related pain, all compounded by ongoing psychological responses of distress and suffering. ” ( Fitzgibbon D. R, Loeser J. D, : Cancer Pain (2010) Lippincott Williams)
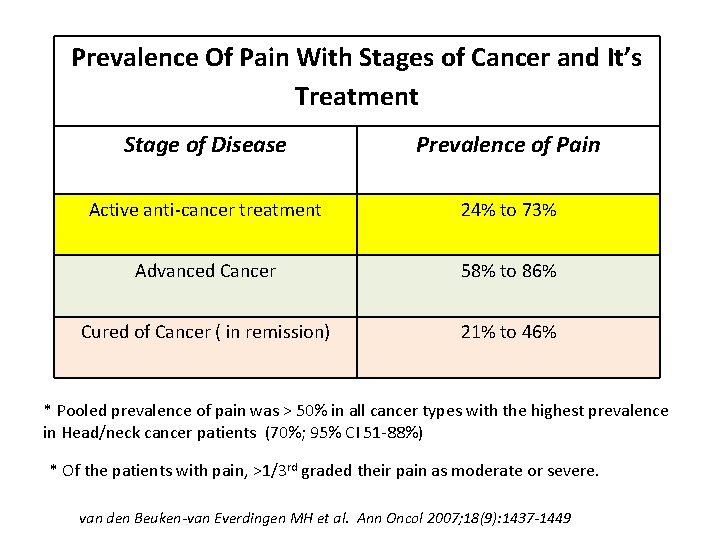
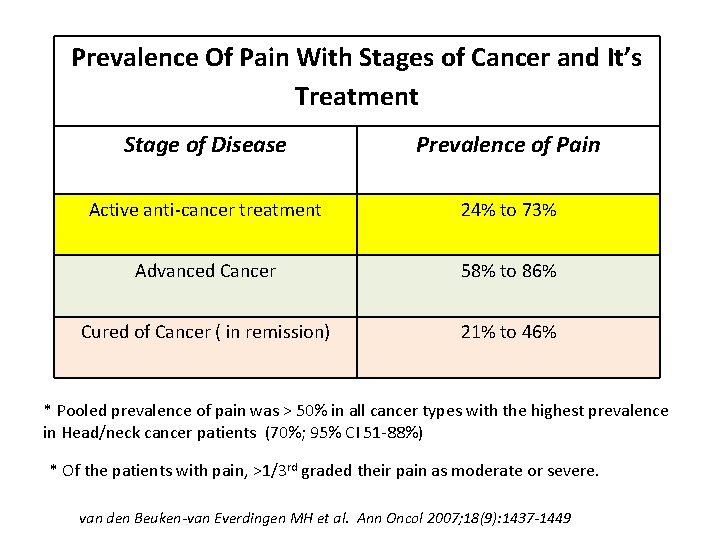
Prevalence Of Pain With Stages of Cancer and It’s Treatment Stage of Disease Prevalence of Pain Active anti-cancer treatment 24% to 73% Advanced Cancer 58% to 86% Cured of Cancer ( in remission) 21% to 46% * Pooled prevalence of pain was > 50% in all cancer types with the highest prevalence in Head/neck cancer patients (70%; 95% CI 51 -88%) * Of the patients with pain, >1/3 rd graded their pain as moderate or severe. van den Beuken-van Everdingen MH et al. Ann Oncol 2007; 18(9): 1437 -1449
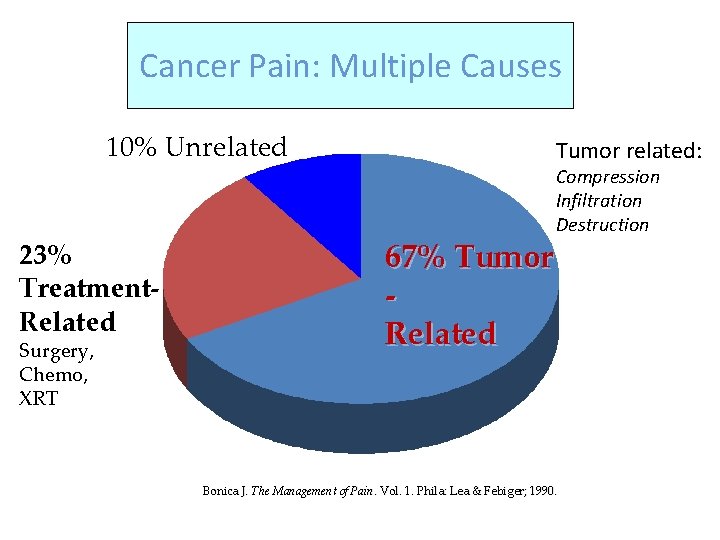
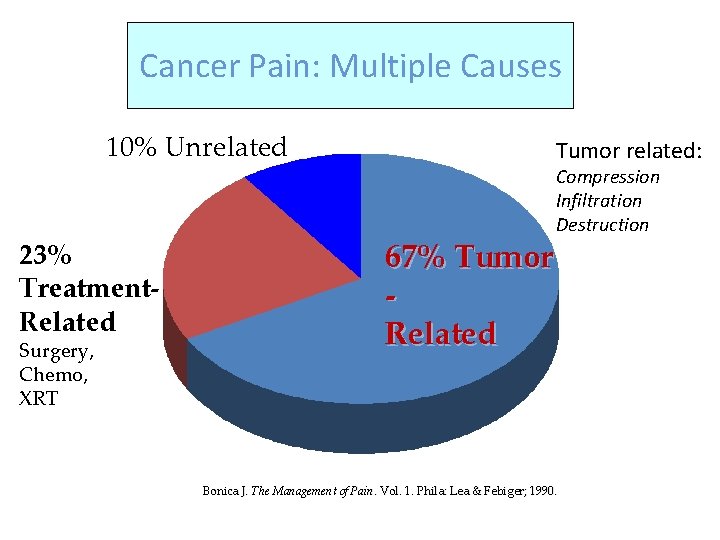
Cancer Pain: Multiple Causes 10% Unrelated 23% Treatment. Related Surgery, Chemo, XRT Tumor related: 67% Tumor Related Compression Infiltration Destruction Bonica J. The Management of Pain. Vol. 1. Phila: Lea & Febiger; 1990.
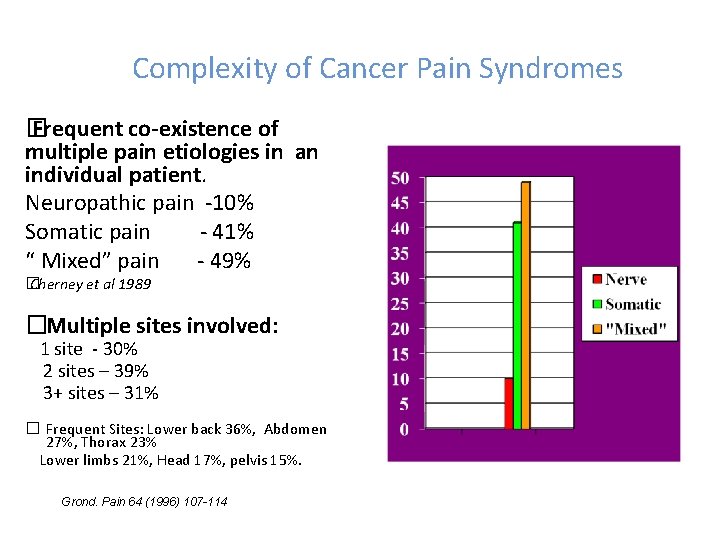
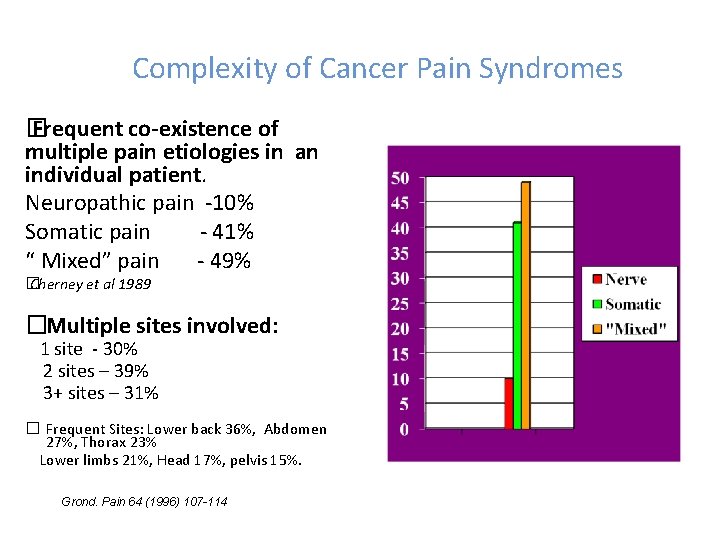
Complexity of Cancer Pain Syndromes � Frequent co-existence of multiple pain etiologies in an individual patient. Neuropathic pain -10% Somatic pain - 41% “ Mixed” pain - 49% � Cherney et al 1989 �Multiple sites involved: 1 site - 30% 2 sites – 39% 3+ sites – 31% � Frequent Sites: Lower back 36%, Abdomen 27%, Thorax 23% Lower limbs 21%, Head 17%, pelvis 15%. Grond. Pain 64 (1996) 107 -114

Cancer Pain Higher Pain Scores are associated with: • • • Presence of Breakthrough Pain Neuropathic pain Lower Performance status ( KPS <70%) Younger patient ( <60 yrs) More advanced disease. Cognitive impairment Caraceni. Pain 82 (1999) 263 -274

Cancer Pain: ‘Hard to treat’ • Opioid responsiveness and optimal pain control is inversely related to the presence of: • • Neuropathic pain. Breakthrough pain. Previous opioid exposure. Cognitive impairment and Psychological distress. Bruera. JPSM. 1989
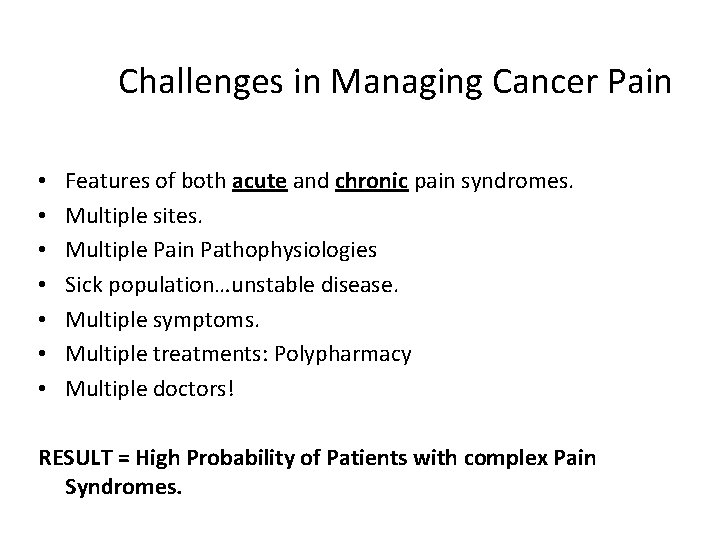
Challenges in Managing Cancer Pain • • Features of both acute and chronic pain syndromes. Multiple sites. Multiple Pain Pathophysiologies Sick population…unstable disease. Multiple symptoms. Multiple treatments: Polypharmacy Multiple doctors! RESULT = High Probability of Patients with complex Pain Syndromes.
Assessment

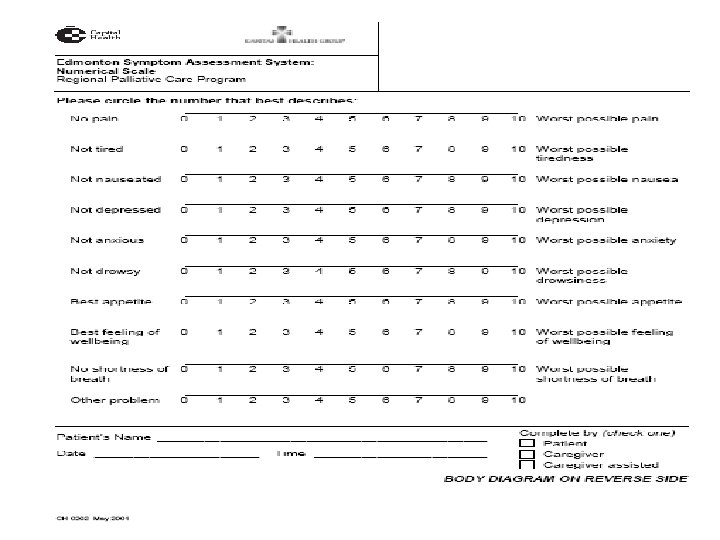
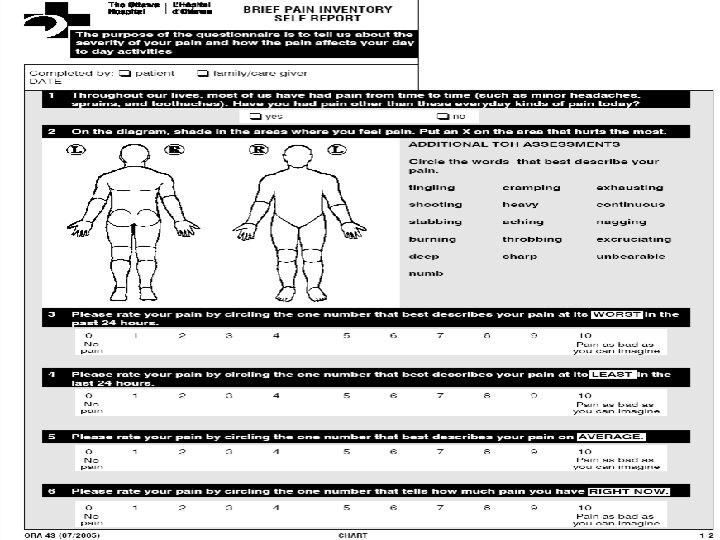
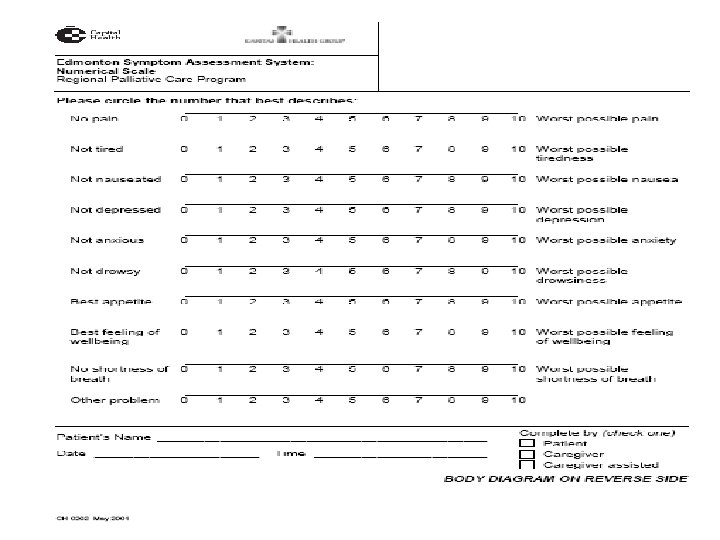
An Approach to Managing Cancer Pain. 1. 2. 3. 4. History of Cancer + History of Pain. Standard assessment tools (ESAS, BPI) Document pain syndromes involved. …
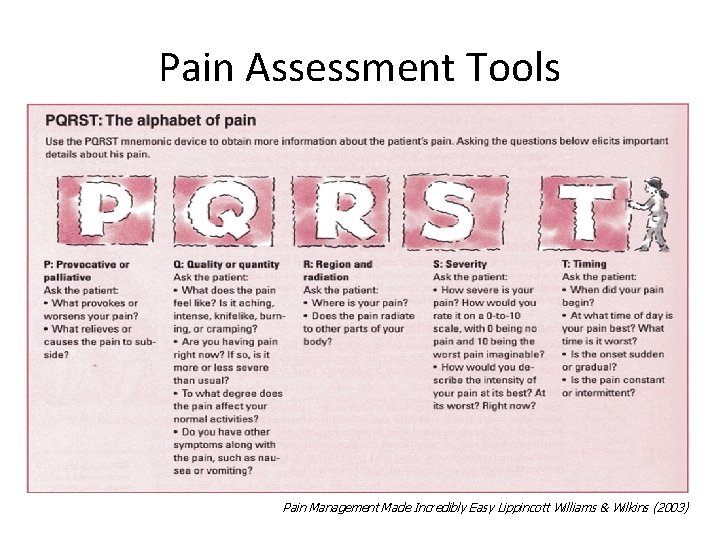
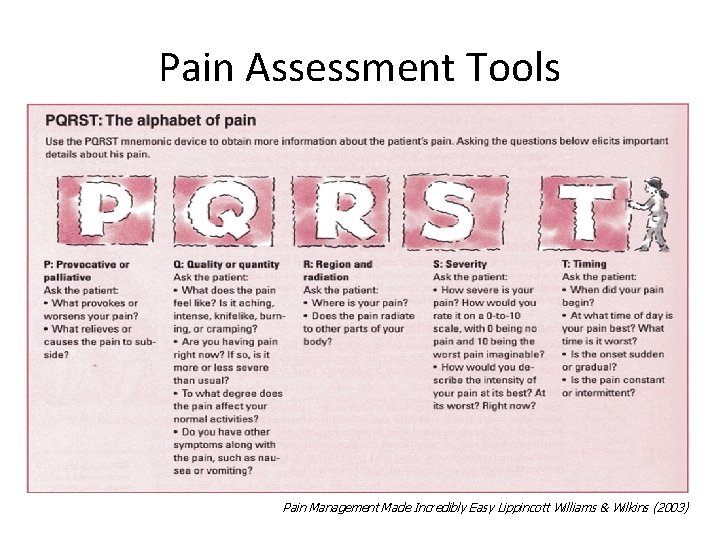
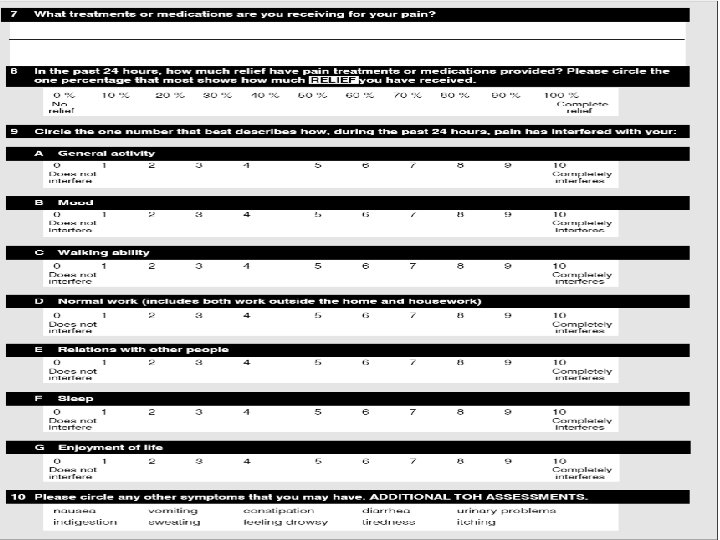
Pain Assessment Tools Pain Management Made Incredibly Easy Lippincott Williams & Wilkins (2003)
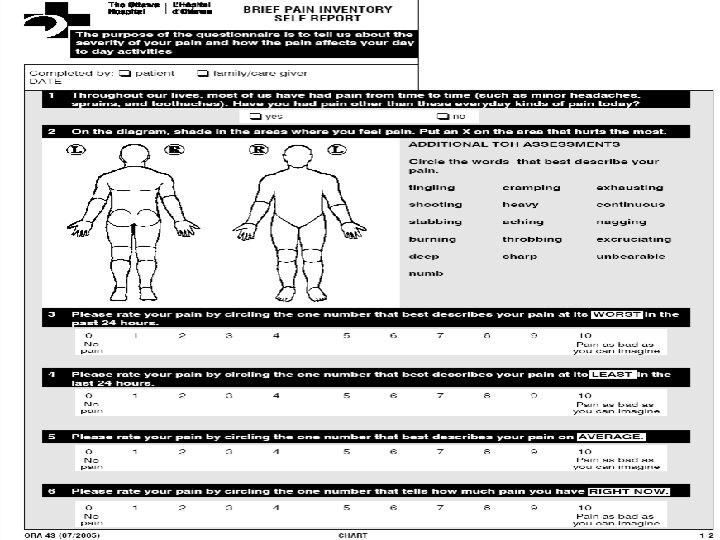
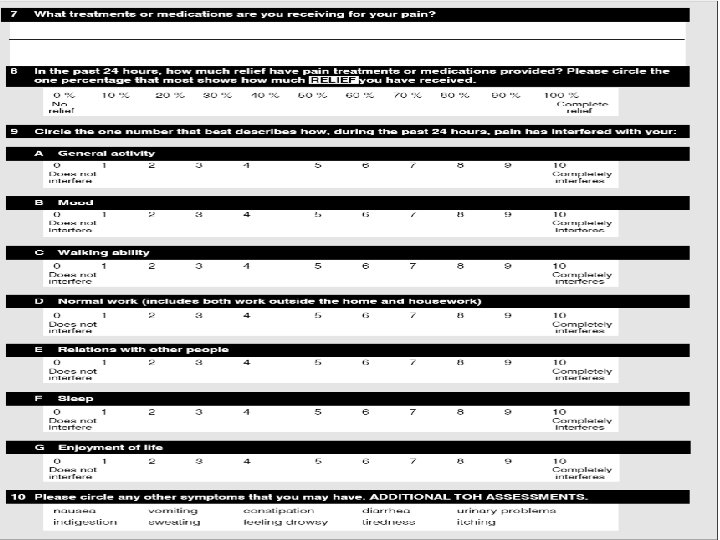
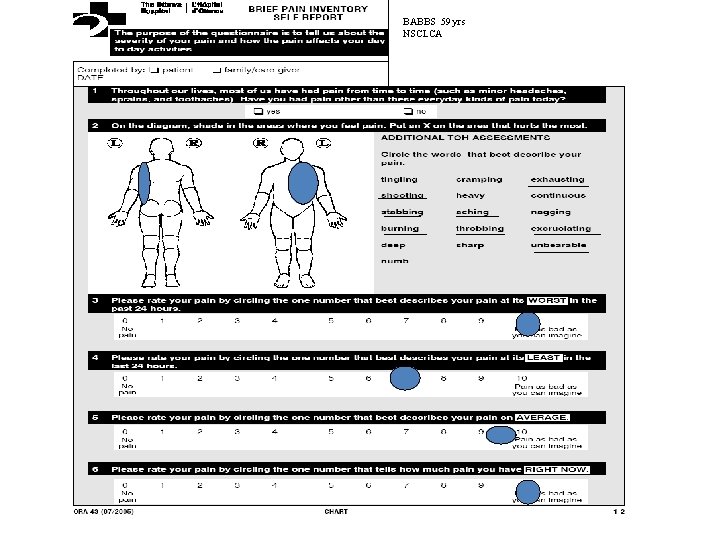
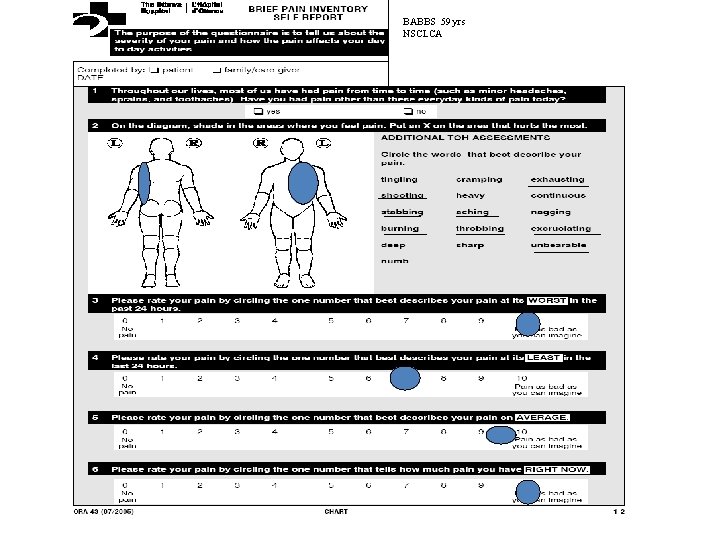
BABBS 59 yrs NSCLCA

HDMContin 6 mgs q 12. Dil 2 mgs q 2 h prn; TCA 60 mgs; Laxatives; Chx ; Stemetil Previously: Oxy. Contin 20 mgs TID & Oxy. IR q 4 h PRN Pt was taking 40 mg q 4 h straight = 500 -600 mgs morph/24 hrs
Managing Cancer Pain. 1. 2. 3. 4. 5. 6. History of Cancer + History of Pain. Standard assessment tools (ESAS, BPI) Document pain syndromes involved. Is cause known? – appropriate investigations. Formulate Treatment plan - ‘realistic goals’. Target Treatment @ Pain and Cause of Pain.

The Cause: Tumor Related Pain

After Chemo/XRT

Managing Cancer Pain. 1. 2. 3. 4. 5. 6. 7. History of Cancer + History of Pain. Standard assessment tools (ESAS, BPI) Document pain syndromes involved. Is cause known? – appropriate investigations. Formulate Treatment plan - ‘realistic goals’. Target Treatment @ Pain and Cause of Pain. WHO analgesic ladder.

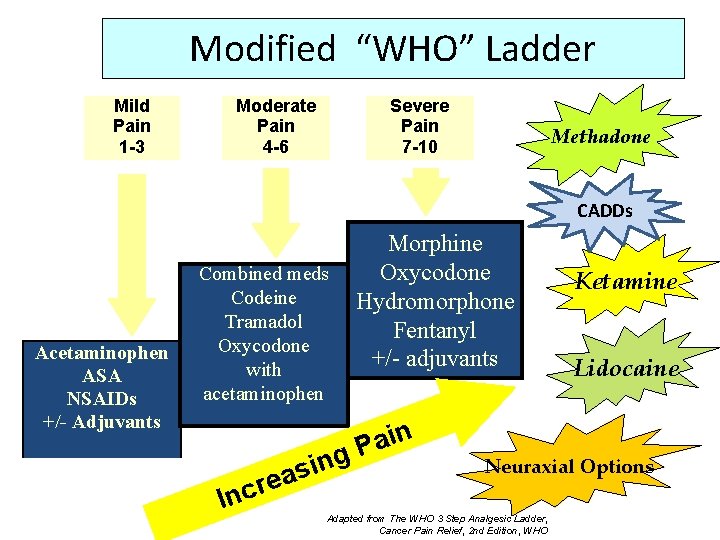
The WHO Analgesic Ladder “This three-step approach of administering the right drug in the right dose at the right time is inexpensive and 80 -90% effective. ” WHO advisory panel 2008 If Rx following the WHO ladder’ patients rated their pain relief : Good 76% Satisfactory 12% Inadequate 12% Zech DF, Grond s et al, Pain 1995; 63: 65 -76
WHO Analgesic ladder : Principles of use • By the mouth. Oral meds whenever possible • By the clock. Continuous pain should be treated with regularly scheduled meds + breakthrough meds as needed. • By the ladder. Choose step appropriate for patient’s pain. No ceiling for pure opioids as long as patient gets benefit and can tolerate side effects. • For the individual. The “right dose” is the dose of the right drug that adequately relieves the patients' pain with minimum side effects • With attention to detail. Successful implementation requires meticulous follow up once a new prescription is issued. Ascertain compliance, drug efficacy and side effects. Cancer pain relief , Geneva , Switzerland, WHO 1996.
WHO Ladder: Step 1: Non-Opioids • Acetaminophen. • NSAIDs • Early use of Co. Analgesics
Acetaminophen • • • Ø Ø Ø N-Acetyl-Para-Amino-Phenol (APAP). Potent antipyretic, weak anti-inflammatory Mild to Moderate Analgesic actions. . . HOW? Probable Central Cox 2 inhibitor Serotonergic agent, acts via desc inhibitory pathways* Blocks metabolism Cannabinoids. Ø Ø Oral bioavailabitlity: 70 -100%. tmax: 0. 5 to 1 hr, t 1/2: 1. 5 -2 hrs CYP metabolism : 4% to toxic metabolite NAPQI. Caution: drug interactions, (Coumadin, and Et. OH. ) Max daily dose 4 gm/day. Graham G G, et al. Mechanism of action of Paracetamol. Am J Ther 2005; 12: 46 -55
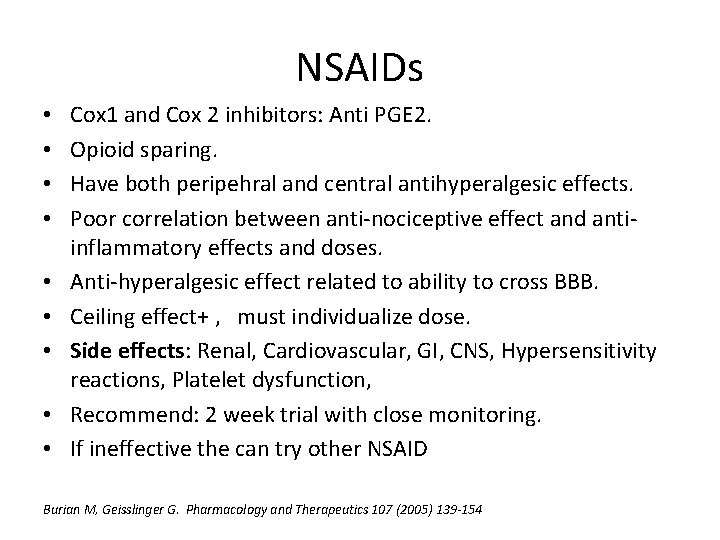
NSAIDs • • • Cox 1 and Cox 2 inhibitors: Anti PGE 2. Opioid sparing. Have both peripehral and central antihyperalgesic effects. Poor correlation between anti-nociceptive effect and antiinflammatory effects and doses. Anti-hyperalgesic effect related to ability to cross BBB. Ceiling effect+ , must individualize dose. Side effects: Renal, Cardiovascular, GI, CNS, Hypersensitivity reactions, Platelet dysfunction, Recommend: 2 week trial with close monitoring. If ineffective the can try other NSAID Burian M, Geisslinger G. Pharmacology and Therapeutics 107 (2005) 139 -154
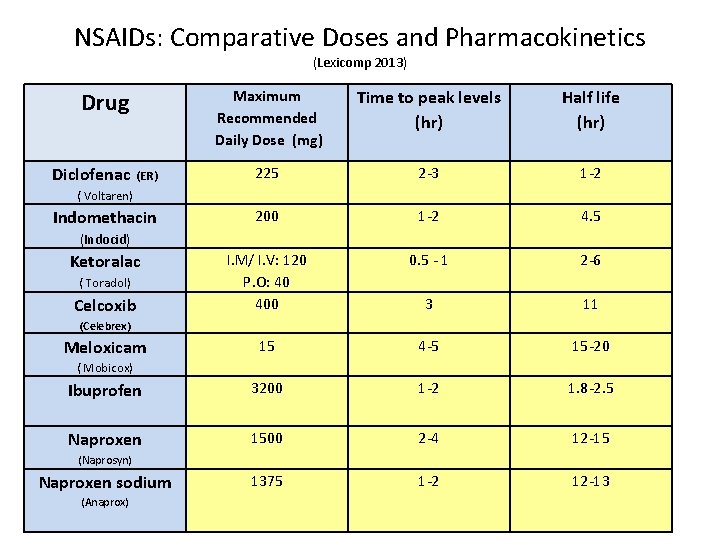
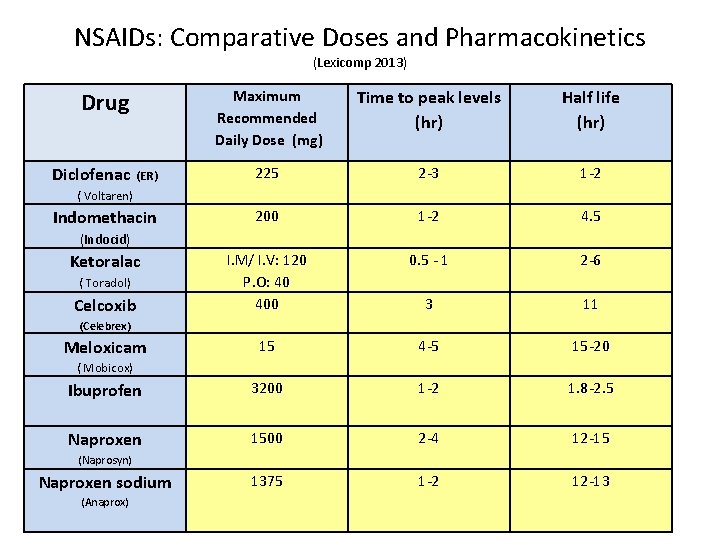
NSAIDs: Comparative Doses and Pharmacokinetics (Lexicomp 2013) Maximum Recommended Daily Dose (mg) Time to peak levels (hr) Half life (hr) (ER) 225 2 -3 1 -2 Indomethacin 200 1 -2 4. 5 I. M/ I. V: 120 P. O: 40 400 0. 5 - 1 2 -6 3 11 15 4 -5 15 -20 Ibuprofen 3200 1 -2 1. 8 -2. 5 Naproxen 1500 2 -4 12 -15 1375 1 -2 12 -13 Drug Diclofenac ( Voltaren) (Indocid) Ketoralac ( Toradol) Celcoxib (Celebrex) Meloxicam ( Mobicox) (Naprosyn) Naproxen sodium (Anaprox)
WHO Ladder: Step 2 ‘Weak’ Opioids • Codeine • Tramadol • Tapentadol • Early use of appropriate Co analgesic
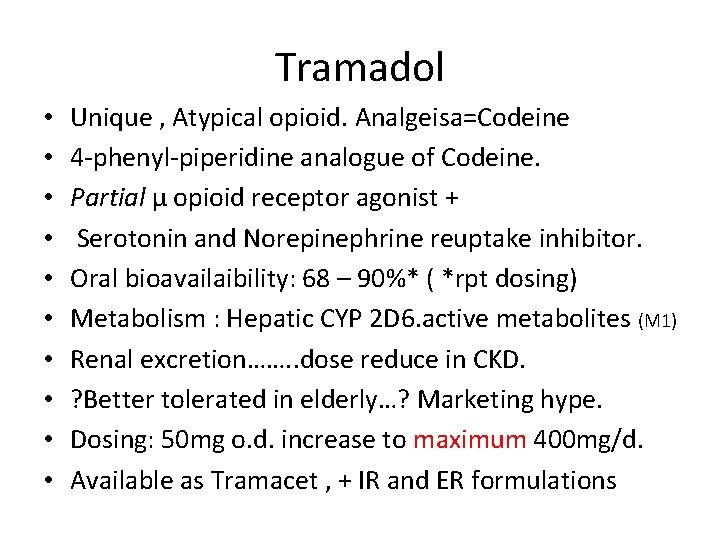
Tramadol • • • Unique , Atypical opioid. Analgeisa=Codeine 4 -phenyl-piperidine analogue of Codeine. Partial μ opioid receptor agonist + Serotonin and Norepinephrine reuptake inhibitor. Oral bioavailaibility: 68 – 90%* ( *rpt dosing) Metabolism : Hepatic CYP 2 D 6. active metabolites (M 1) Renal excretion……. . dose reduce in CKD. ? Better tolerated in elderly…? Marketing hype. Dosing: 50 mg o. d. increase to maximum 400 mg/d. Available as Tramacet , + IR and ER formulations
WHO Ladder: Step 3 ‘Stronger’ Opioids • • Morphine Hydromorphone Fentanyl Oxycodone • Early use of appropriate Co analgesic
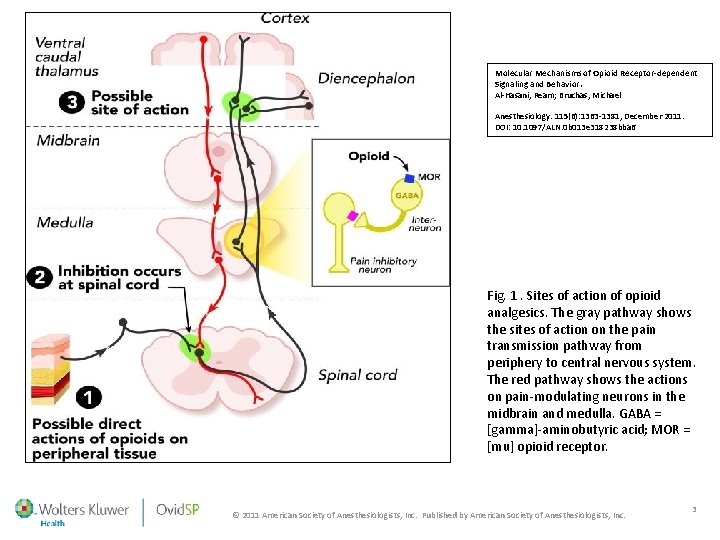
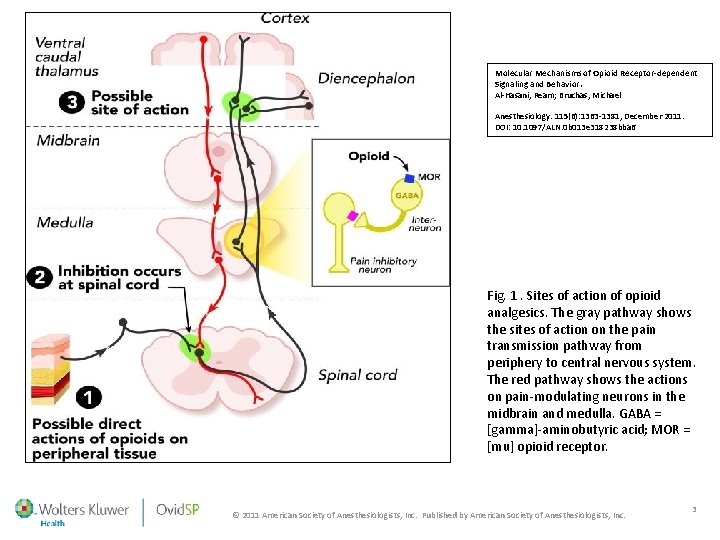
Molecular Mechanisms of Opioid Receptor-dependent Signaling and Behavior. Al-Hasani, Ream; Bruchas, Michael Anesthesiology. 115(6): 1363 -1381, December 2011. DOI: 10. 1097/ALN. 0 b 013 e 318238 bba 6 Fig. 1. Sites of action of opioid analgesics. The gray pathway shows the sites of action on the pain transmission pathway from periphery to central nervous system. The red pathway shows the actions on pain-modulating neurons in the midbrain and medulla. GABA = [gamma]-aminobutyric acid; MOR = [mu] opioid receptor. © 2011 American Society of Anesthesiologists, Inc. Published by American Society of Anesthesiologists, Inc. 3
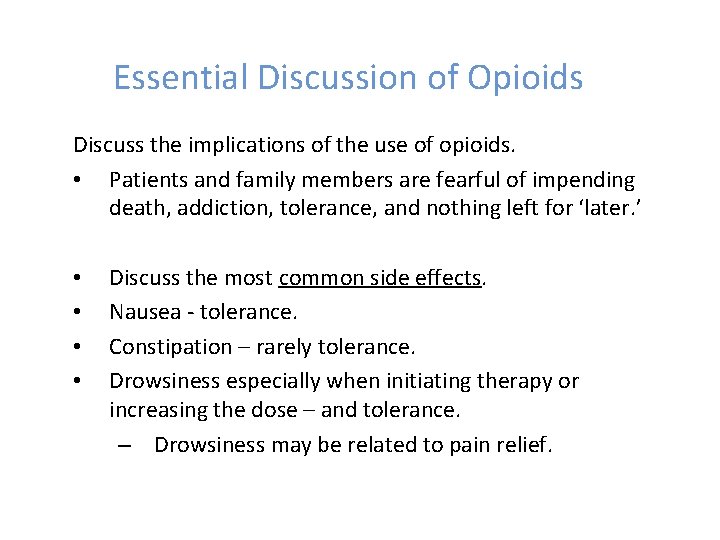
Essential Discussion of Opioids Discuss the implications of the use of opioids. • Patients and family members are fearful of impending death, addiction, tolerance, and nothing left for ‘later. ’ • • Discuss the most common side effects. Nausea - tolerance. Constipation – rarely tolerance. Drowsiness especially when initiating therapy or increasing the dose – and tolerance. – Drowsiness may be related to pain relief.

Organ System Effects of Morphine and it`s Surrogates Central Nervous System ↑ Analgesia ↑ Euphoria* ↑ Sedation ↓ Respiratory rate ↓Cough reflex ↑ Miosis ↑ Truncal rigidity ** ↑ Nausea and vomiting Behavioural restlessness. *addiction potential ** esp Fentanyl/ Sufentanyl Peripheral Gastrointestinal system: ↑Constipation ↓Gastric motility ↓Digestion in small intestine ↓Peristaltic waves in the colon ↑Constriction of biliary sphincter ↑Esophageal reflux Other Smooth Muscle: ↑Depression of Renal function ↓Uterine tone ↑Urinary retention Skin: ↑Itching and sweating ↑Flushing of face/neck. Cardiovascular System: ↓Blood Pressure + heart rate Immune System: ↓Lymphocyte function ↓Cytotoxic activity of natural killer cells Al-Hasani, Ream et al. Anesthesiology. 115(6): 1363 -1381, Dec 2011. Molecular Mechanisms of Opioid receptor-dependant signaling and behaviour.

Factors Associated with Successful Opioid Therapy Age and weight (pharmacokinetic/pharmacodynamic differences) Severity and Pathophysiology of pain Severity, nature, extent of disease. Allergies or drug intolerances Psychological factors + History of addiction (CAGE) Response to previous opioid therapy ( patient’s preference) Co existing disease ( cardiovascular, Pulmonary, GI etc) Renal and Liver function Drug Route: PO / IV/ SQ/ TD / IT etc. Pharmacodynamic Factors and Pharmacologic Interactions Fitzgibbon D, et al. Lippincott, Cancer Pain, 2010
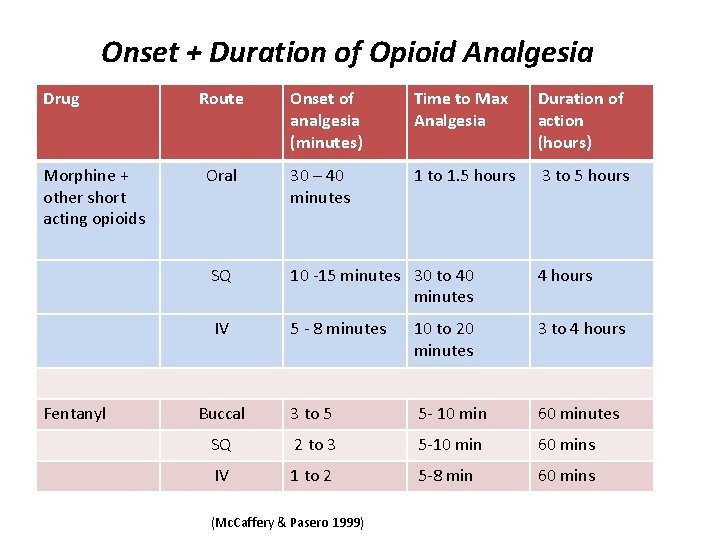
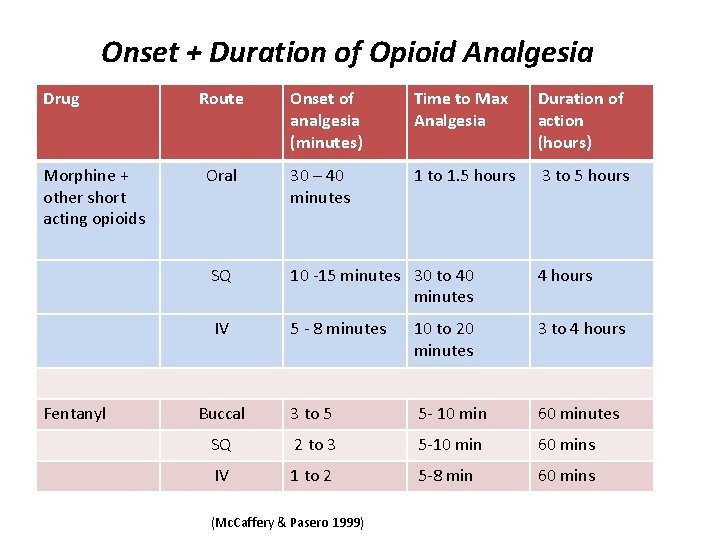
Onset + Duration of Opioid Analgesia Drug Morphine + other short acting opioids Fentanyl Route Onset of analgesia (minutes) Time to Max Analgesia Duration of action (hours) Oral 30 – 40 minutes 1 to 1. 5 hours 3 to 5 hours SQ 10 -15 minutes 30 to 40 minutes 4 hours IV 5 - 8 minutes 10 to 20 minutes 3 to 4 hours Buccal 3 to 5 5 - 10 min 60 minutes SQ 2 to 3 5 -10 min 60 mins IV 1 to 2 5 -8 min 60 mins (Mc. Caffery & Pasero 1999)
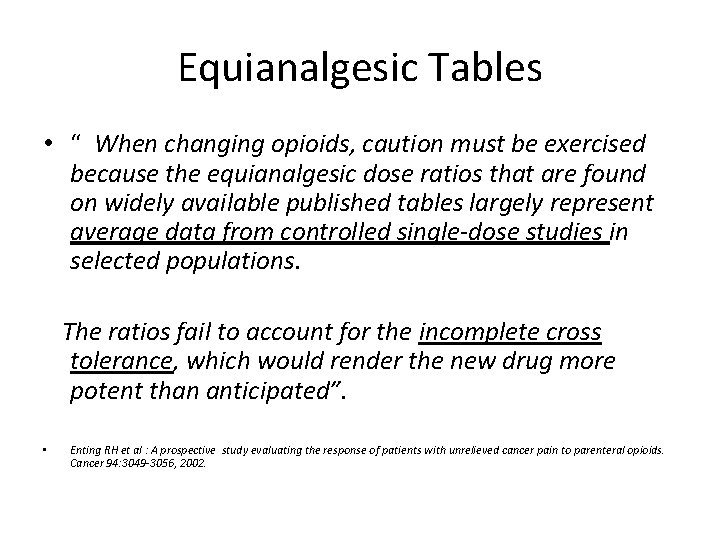
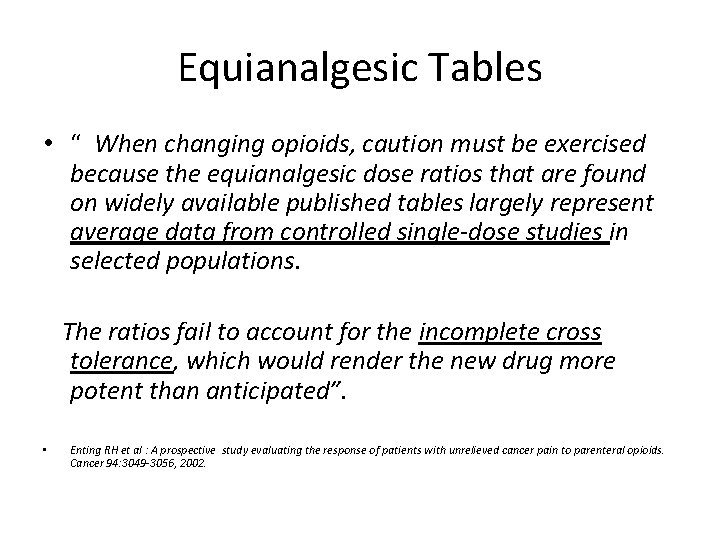
Equianalgesic Tables • “ When changing opioids, caution must be exercised because the equianalgesic dose ratios that are found on widely available published tables largely represent average data from controlled single-dose studies in selected populations. The ratios fail to account for the incomplete cross tolerance, which would render the new drug more potent than anticipated”. • Enting RH et al : A prospective study evaluating the response of patients with unrelieved cancer pain to parenteral opioids. Cancer 94: 3049 -3056, 2002.
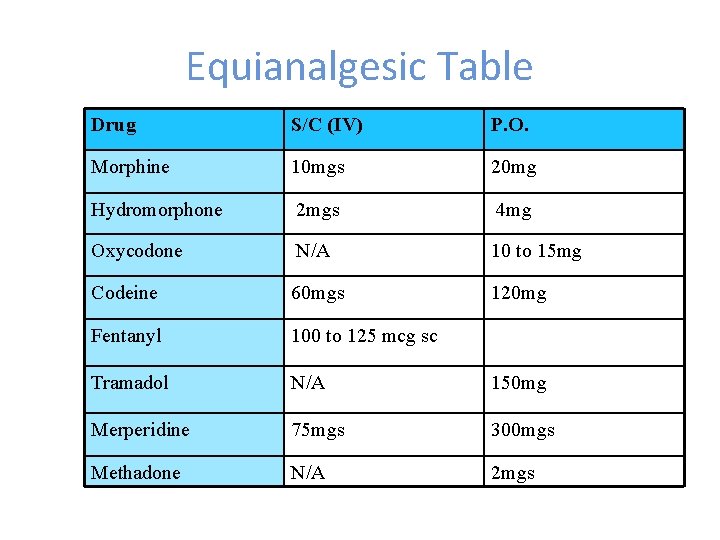
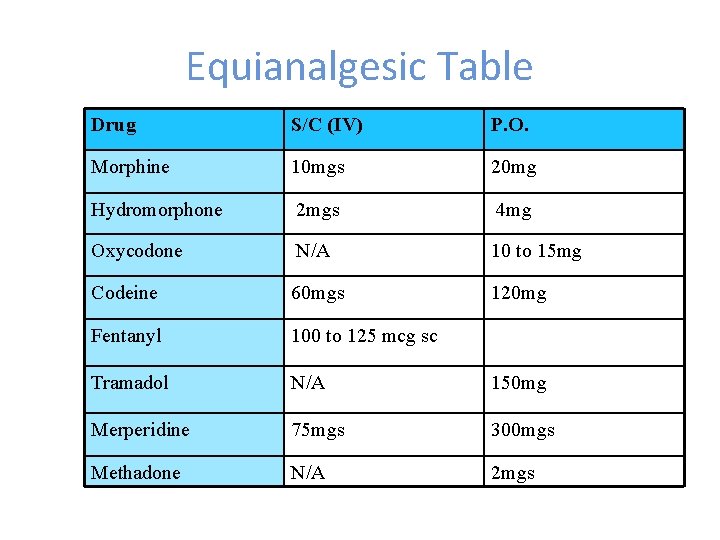
Equianalgesic Table Drug S/C (IV) P. O. Morphine 10 mgs 20 mg Hydromorphone 2 mgs 4 mg Oxycodone N/A 10 to 15 mg Codeine 60 mgs 120 mg Fentanyl 100 to 125 mcg sc Tramadol N/A 150 mg Merperidine 75 mgs 300 mgs Methadone N/A 2 mgs
What Opioid do I choose?
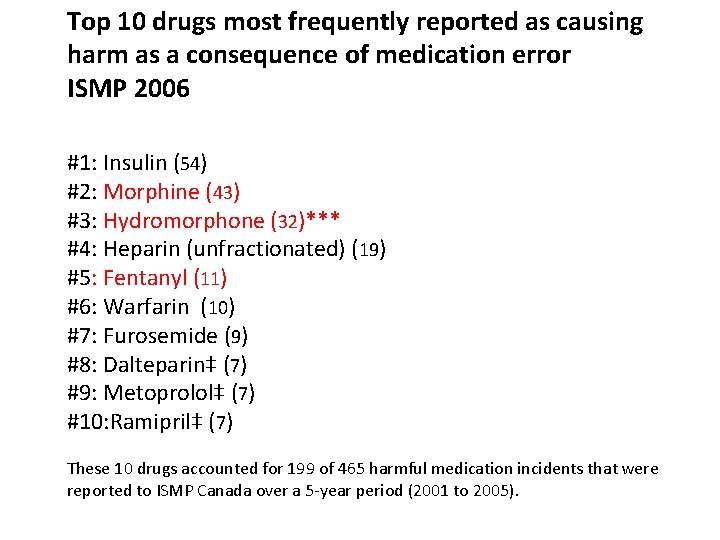
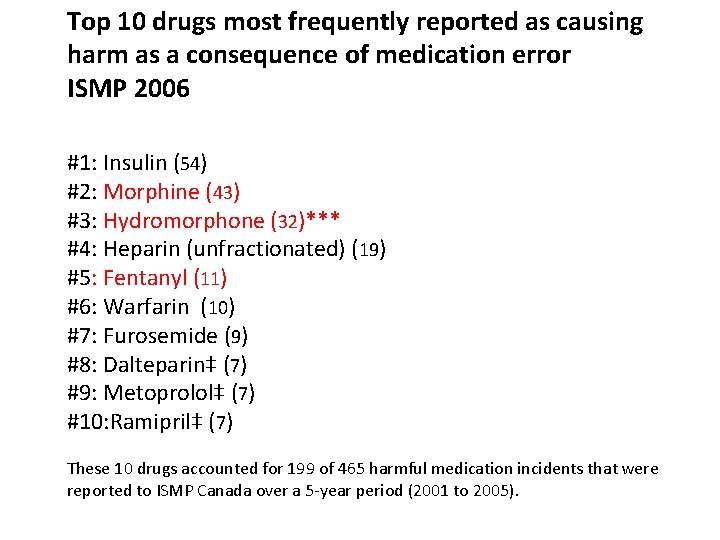
Top 10 drugs most frequently reported as causing harm as a consequence of medication error ISMP 2006 #1: Insulin (54) #2: Morphine (43) #3: Hydromorphone (32)*** #4: Heparin (unfractionated) (19) #5: Fentanyl (11) #6: Warfarin (10) #7: Furosemide (9) #8: Dalteparin‡ (7) #9: Metoprolol‡ (7) #10: Ramipril‡ (7) These 10 drugs accounted for 199 of 465 harmful medication incidents that were reported to ISMP Canada over a 5 -year period (2001 to 2005).

5 mg
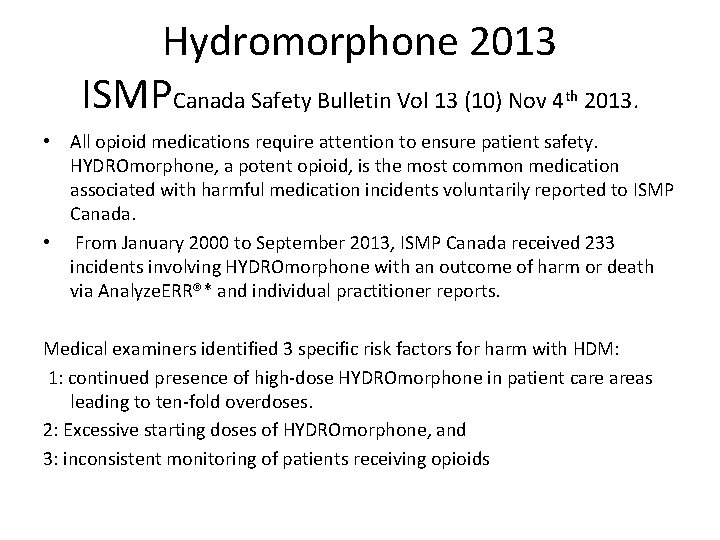
Hydromorphone 2013 ISMPCanada Safety Bulletin Vol 13 (10) Nov 4 th 2013. • All opioid medications require attention to ensure patient safety. HYDROmorphone, a potent opioid, is the most common medication associated with harmful medication incidents voluntarily reported to ISMP Canada. • From January 2000 to September 2013, ISMP Canada received 233 incidents involving HYDROmorphone with an outcome of harm or death via Analyze. ERR®* and individual practitioner reports. Medical examiners identified 3 specific risk factors for harm with HDM: 1: continued presence of high-dose HYDROmorphone in patient care areas leading to ten-fold overdoses. 2: Excessive starting doses of HYDROmorphone, and 3: inconsistent monitoring of patients receiving opioids
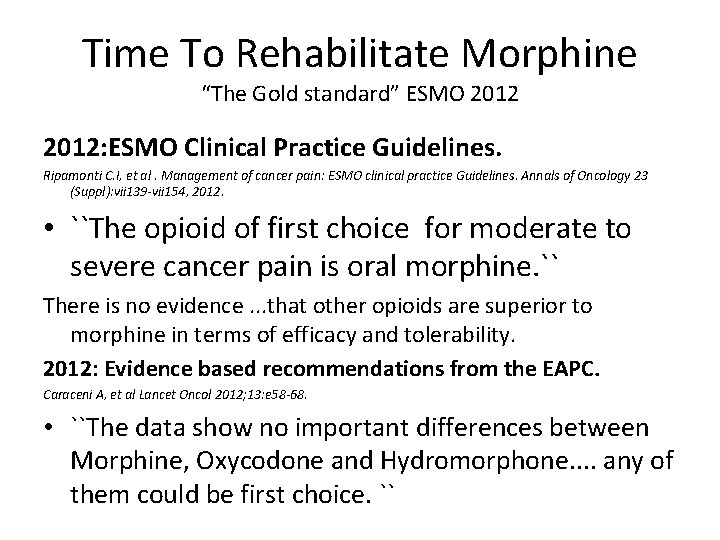
Time To Rehabilitate Morphine “The Gold standard” ESMO 2012: ESMO Clinical Practice Guidelines. Ripamonti C. I, et al. Management of cancer pain: ESMO clinical practice Guidelines. Annals of Oncology 23 (Suppl): vii 139 -vii 154, 2012. • ``The opioid of first choice for moderate to severe cancer pain is oral morphine. `` There is no evidence. . . that other opioids are superior to morphine in terms of efficacy and tolerability. 2012: Evidence based recommendations from the EAPC. Caraceni A, et al Lancet Oncol 2012; 13: e 58 -68. • ``The data show no important differences between Morphine, Oxycodone and Hydromorphone. . any of them could be first choice. ``
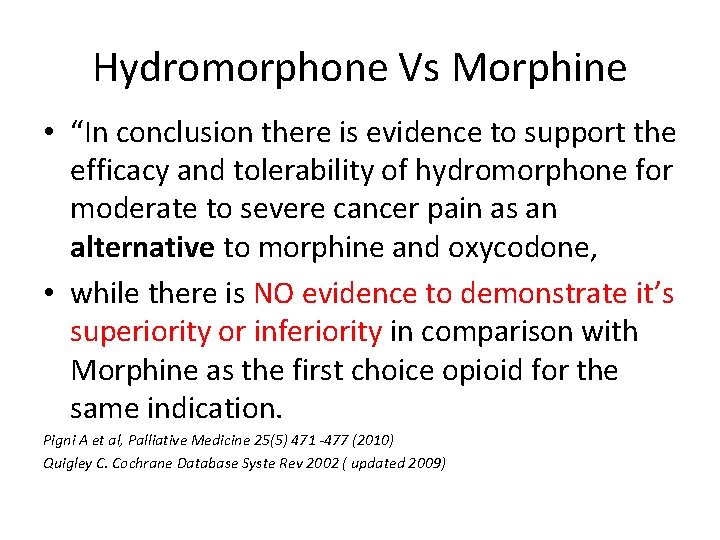
Hydromorphone Vs Morphine • “In conclusion there is evidence to support the efficacy and tolerability of hydromorphone for moderate to severe cancer pain as an alternative to morphine and oxycodone, • while there is NO evidence to demonstrate it’s superiority or inferiority in comparison with Morphine as the first choice opioid for the same indication. Pigni A et al, Palliative Medicine 25(5) 471 -477 (2010) Quigley C. Cochrane Database Syste Rev 2002 ( updated 2009)
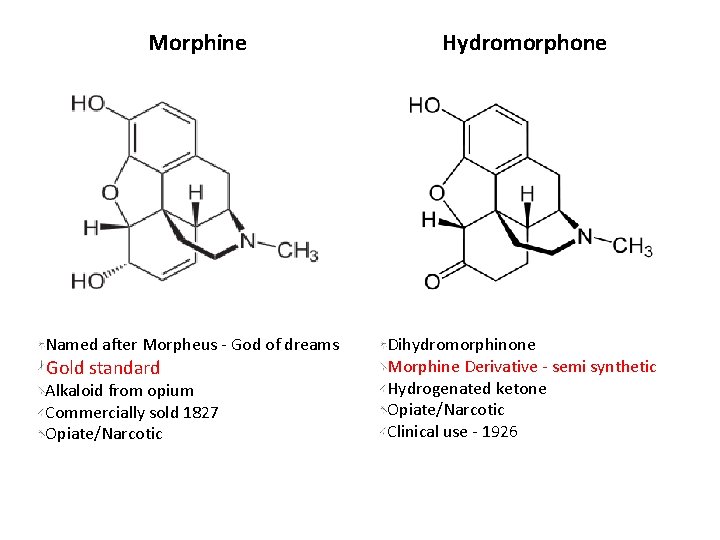
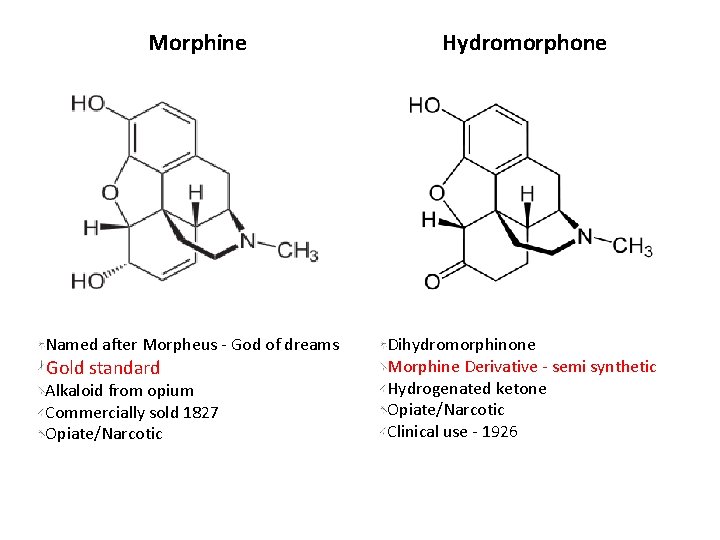
Morphine Named after Morpheus - God of dreams Gold standard Alkaloid from opium Commercially sold 1827 Opiate/Narcotic Hydromorphone Dihydromorphinone Morphine Derivative - semi synthetic Hydrogenated ketone Opiate/Narcotic Clinical use - 1926
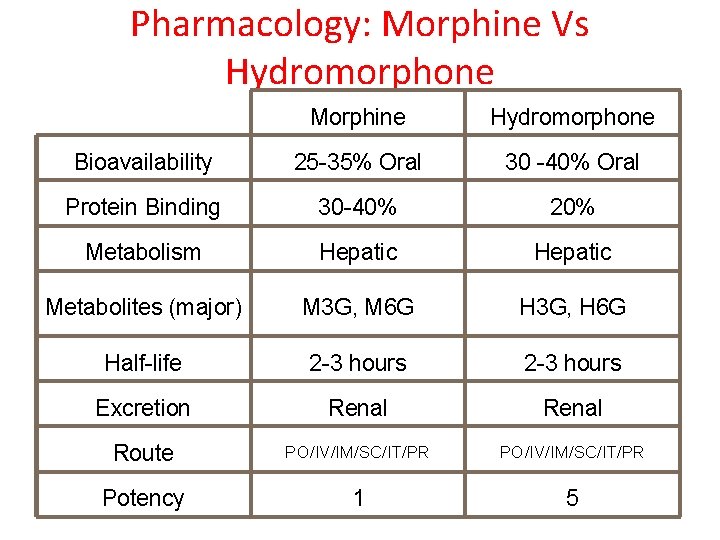
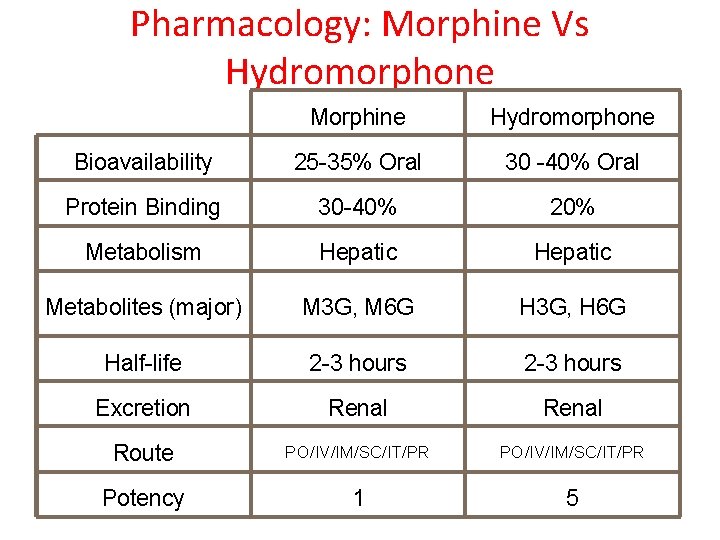
Pharmacology: Morphine Vs Hydromorphone Morphine Hydromorphone Bioavailability 25 -35% Oral 30 -40% Oral Protein Binding 30 -40% 20% Metabolism Hepatic Metabolites (major) M 3 G, M 6 G H 3 G, H 6 G Half-life 2 -3 hours Excretion Renal Route PO/IV/IM/SC/IT/PR Potency 1 5

Major Opioid Metabolites The Metabolism of Opioid Agents and the Clinical Impact of Their Active Metabolites. Smith, Howard Clinical Journal of Pain. 27(9): 824 -838, November/December 2011. 2

Pharmacologic properties attributable to M 3 G, M 6 G, and H 3 G (Care beyond cure p 52, 4 2010) th • • • M 3 G ( + H 3 G) Central agitation Hallucinations Myoclonus Convulsions Coma Hyperalgesia • • • M 6 G ( + H 6 G) Sedation Nausea Respiratory depression Coma Analgesic effect Factors that may increase accumulation of Morphine/HDM metabolites Age > 70 yrs. Renal failure ( factors that may ppt RF : urinary obstruction, Meds e. g. NSAIDs, ACE etc, cancers: MM, Lymphoma] Dehydration Rapid + substantial increases in opioid doses Long term use.
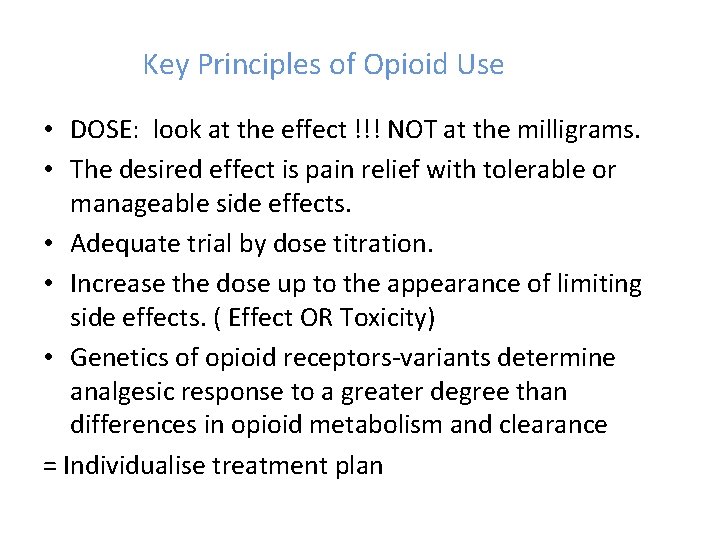
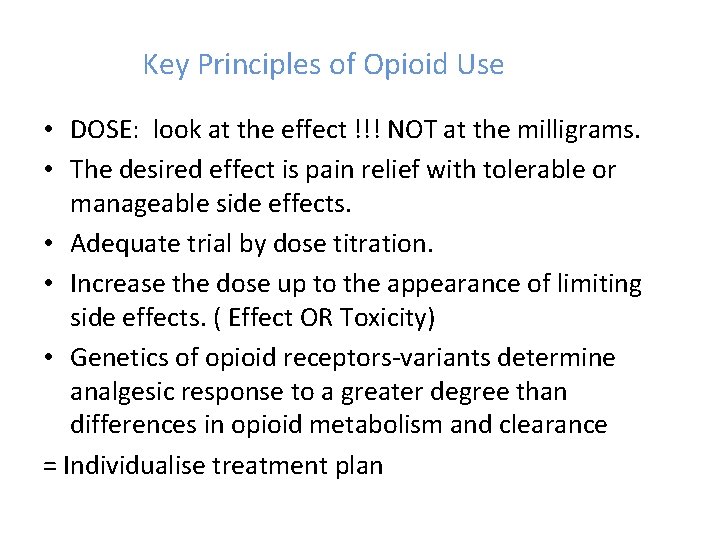
Key Principles of Opioid Use • DOSE: look at the effect !!! NOT at the milligrams. • The desired effect is pain relief with tolerable or manageable side effects. • Adequate trial by dose titration. • Increase the dose up to the appearance of limiting side effects. ( Effect OR Toxicity) • Genetics of opioid receptors-variants determine analgesic response to a greater degree than differences in opioid metabolism and clearance = Individualise treatment plan
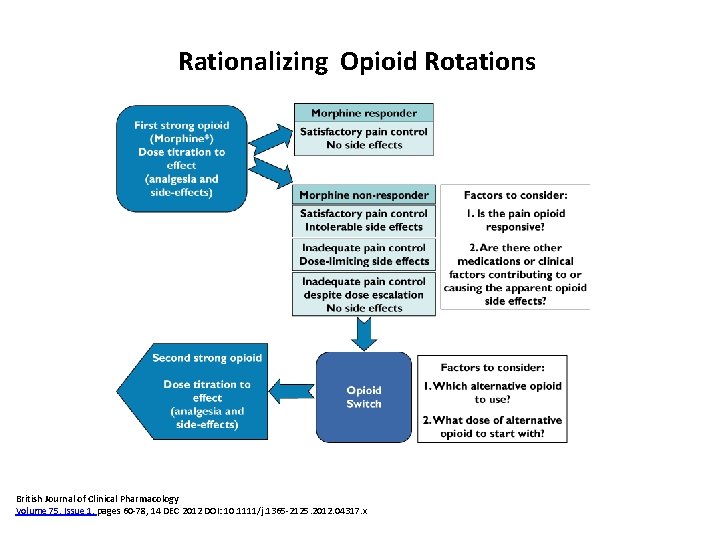
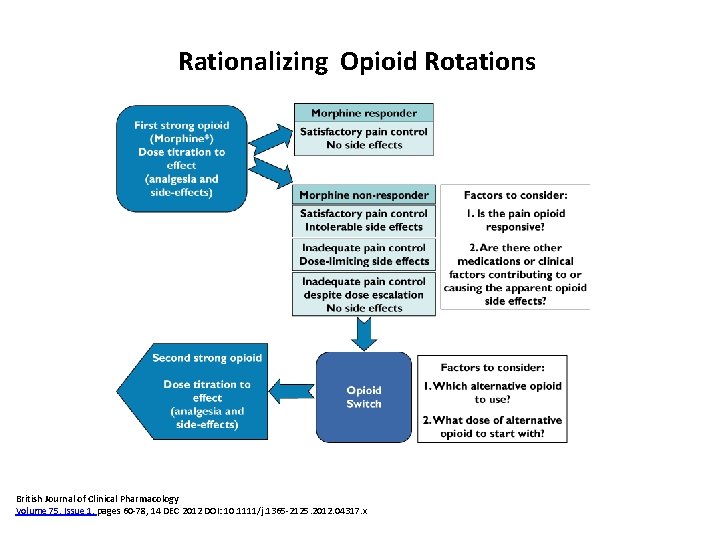
Rationalizing Opioid Rotations British Journal of Clinical Pharmacology Volume 75, Issue 1, pages 60 -78, 14 DEC 2012 DOI: 10. 1111/j. 1365 -2125. 2012. 04317. x
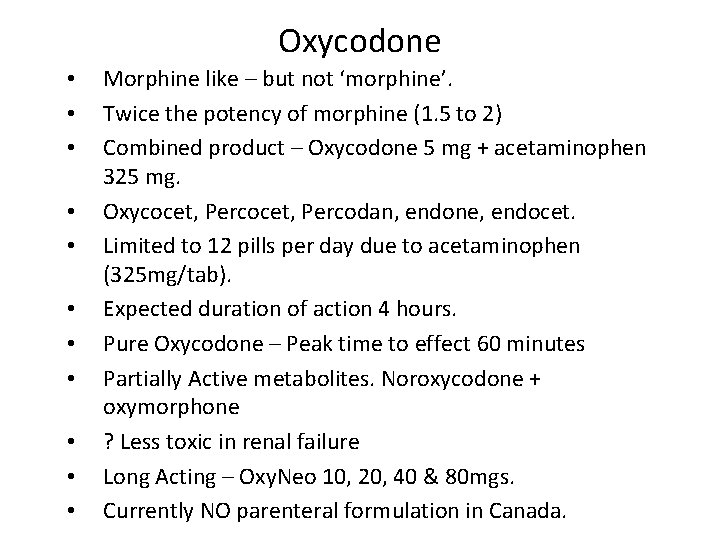
Oxycodone • • • Morphine like – but not ‘morphine’. Twice the potency of morphine (1. 5 to 2) Combined product – Oxycodone 5 mg + acetaminophen 325 mg. Oxycocet, Percodan, endone, endocet. Limited to 12 pills per day due to acetaminophen (325 mg/tab). Expected duration of action 4 hours. Pure Oxycodone – Peak time to effect 60 minutes Partially Active metabolites. Noroxycodone + oxymorphone ? Less toxic in renal failure Long Acting – Oxy. Neo 10, 20, 40 & 80 mgs. Currently NO parenteral formulation in Canada.
• • • Fentanyl NOT morphine like. Inactive when swallowed. Hepatic metabolism- metabolites are inactive + non-toxic Renal excretion; < 10% of unchanged drug excreted in urine. ? Safer in hepatic + renal failure. Absorbed buccally, sublingually, subcutaneously, intravenously. 75 times more potent than morphine. VERY short acting. SC dose peak time to effect 15 -20 mins. SC dose duration of action 40 -60 mins.
Long Acting Preparations • • • Establish the dose. Calculate the appropriate breakthrough dose. Be aware of the slow rise in serum values. Peak time to effect is about 8 hours. However, provides constant opioid release. Improved compliance and Qo. L. • Not Indicated as First Option in Acute Pain !
Transdermal Fentanyl • • • Fentanyl TD duration of action ~72 hours. Slow onset of action when initiated. Cachectic patients may require patch changes q 48 hours. Apply above the waist. Apply to an area that is well perfused. Do not apply over a hairy area. Do not shave - but clip if necessary. Ensure good adhesion. Dose dependent on surface area. Rotate patch sites.
Managing Cancer Pain. 1. 2. 3. 4. 5. 6. 7. 8. History of Cancer + History of Pain. Standard assessment tools (ESAS, BPI) Document pain syndromes involved. Is cause known? – appropriate investigations. Formulate Treatment plan - ‘realistic goals’. Target Treatment @ Pain and Cause of Pain. WHO analgesic ladder. Early use of Co-Analgesics: Multi-Modal Analgesia
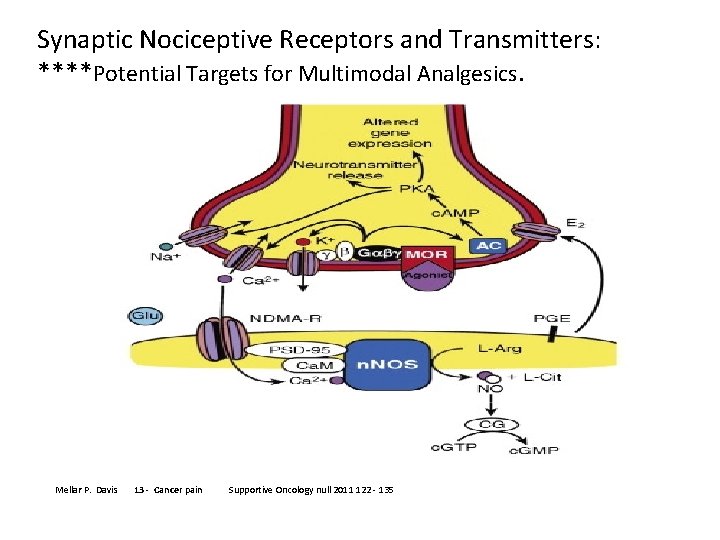
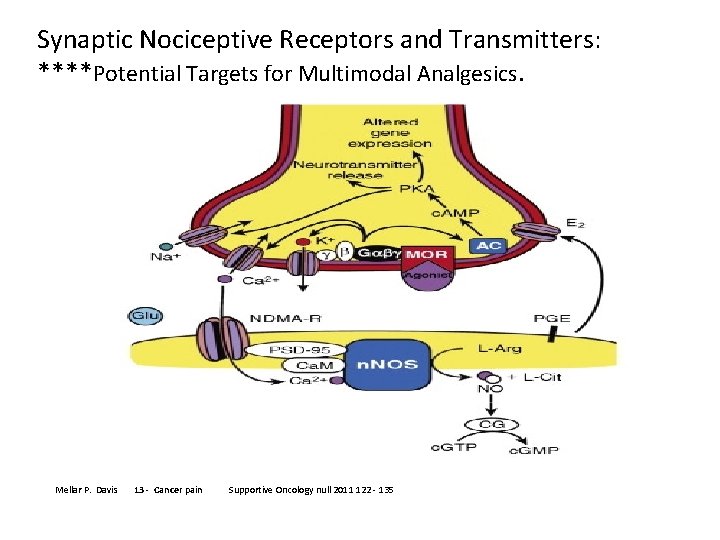
Synaptic Nociceptive Receptors and Transmitters: ****Potential Targets for Multimodal Analgesics. Mellar P. Davis 13 - Cancer pain Supportive Oncology null 2011 122 - 135
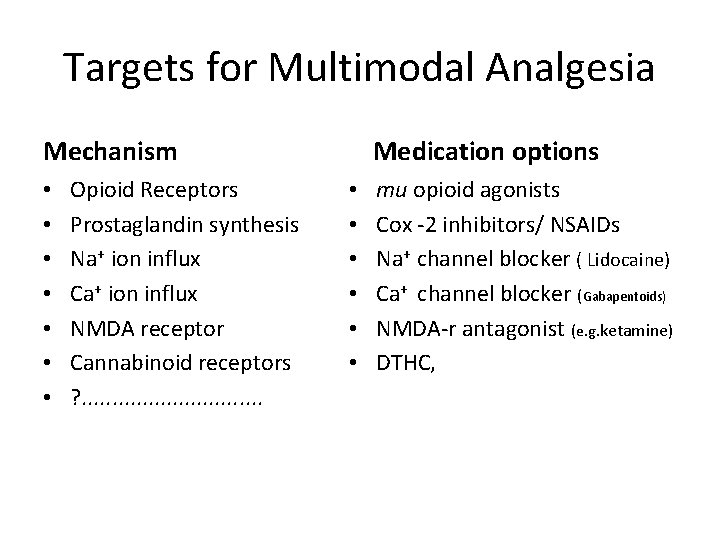
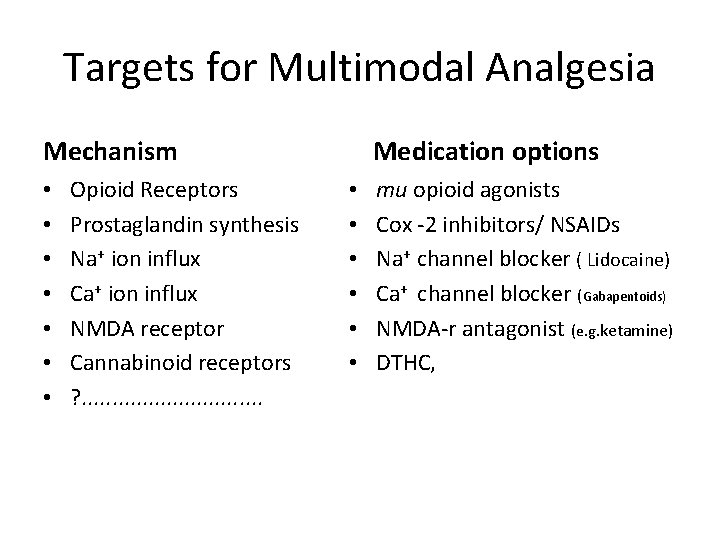
Targets for Multimodal Analgesia Mechanism • • Opioid Receptors Prostaglandin synthesis Na+ ion influx Ca+ ion influx NMDA receptor Cannabinoid receptors ? . . . . Medication options • • • mu opioid agonists Cox -2 inhibitors/ NSAIDs Na+ channel blocker ( Lidocaine) Ca+ channel blocker (Gabapentoids) NMDA-r antagonist (e. g. ketamine) DTHC,
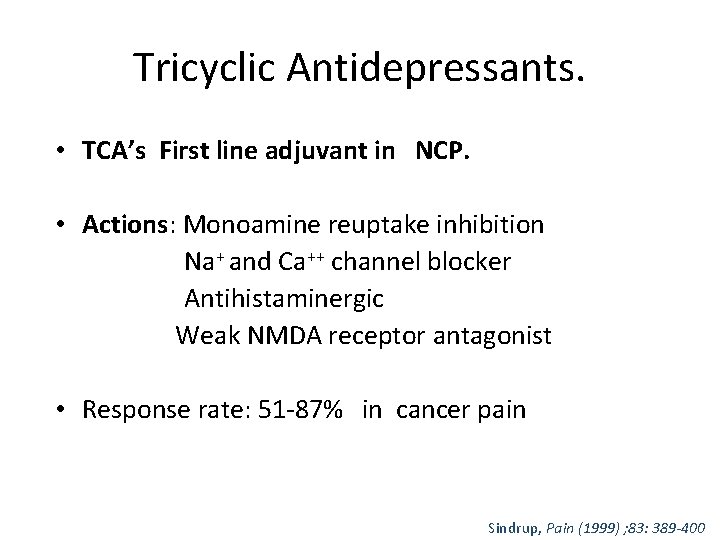
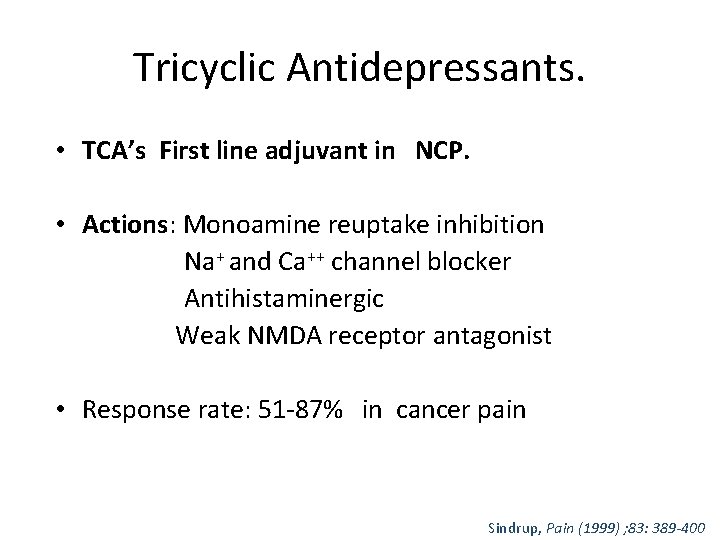
Tricyclic Antidepressants. • TCA’s First line adjuvant in NCP. • Actions: Monoamine reuptake inhibition Na+ and Ca++ channel blocker Antihistaminergic Weak NMDA receptor antagonist • Response rate: 51 -87% in cancer pain Sindrup, Pain (1999) ; 83: 389 -400
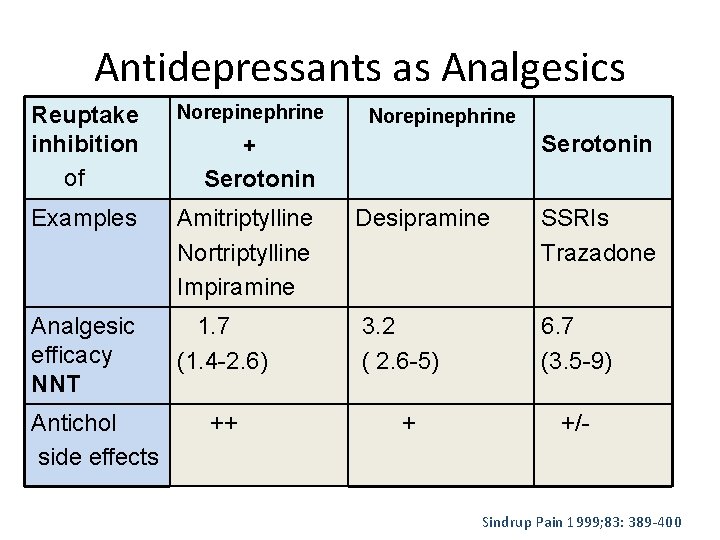
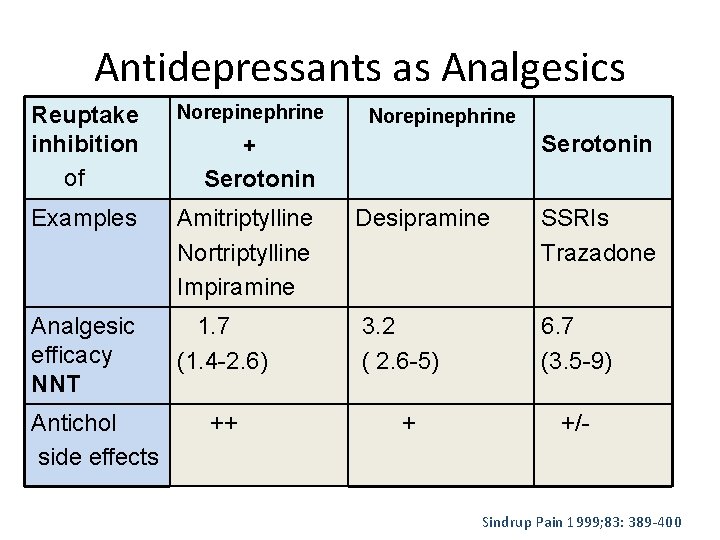
Antidepressants as Analgesics Reuptake inhibition • of Norepinephrine Examples Amitriptylline Nortriptylline Impiramine Desipramine SSRIs Trazadone Analgesic efficacy NNT 1. 7 (1. 4 -2. 6) 3. 2 ( 2. 6 -5) 6. 7 (3. 5 -9) Antichol side effects Norepinephrine Serotonin + Serotonin ++ + +/- Sindrup Pain 1999; 83: 389 -400
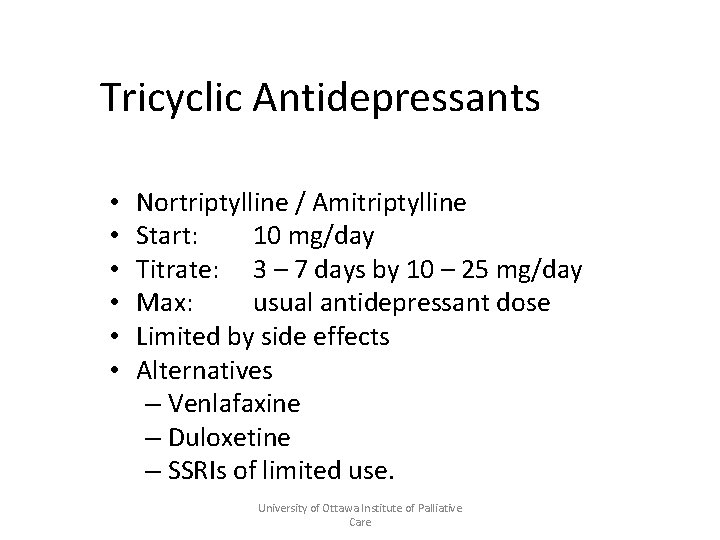
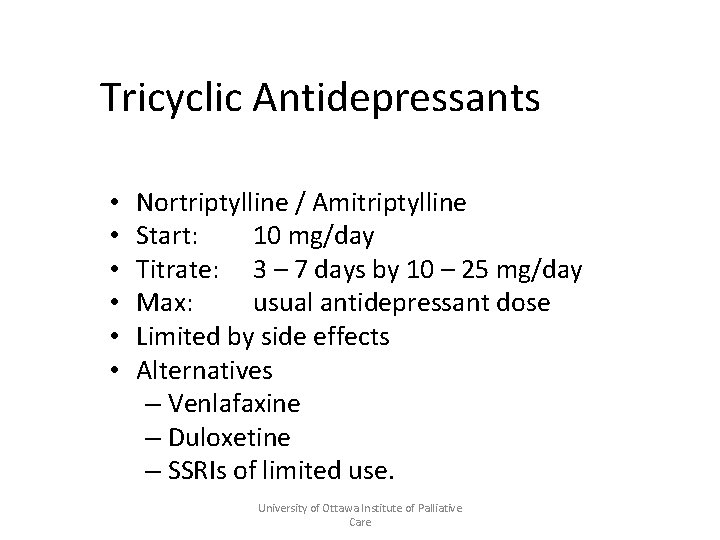
Tricyclic Antidepressants • • • Nortriptylline / Amitriptylline Start: 10 mg/day Titrate: 3 – 7 days by 10 – 25 mg/day Max: usual antidepressant dose Limited by side effects Alternatives – Venlafaxine – Duloxetine – SSRIs of limited use. University of Ottawa Institute of Palliative Care
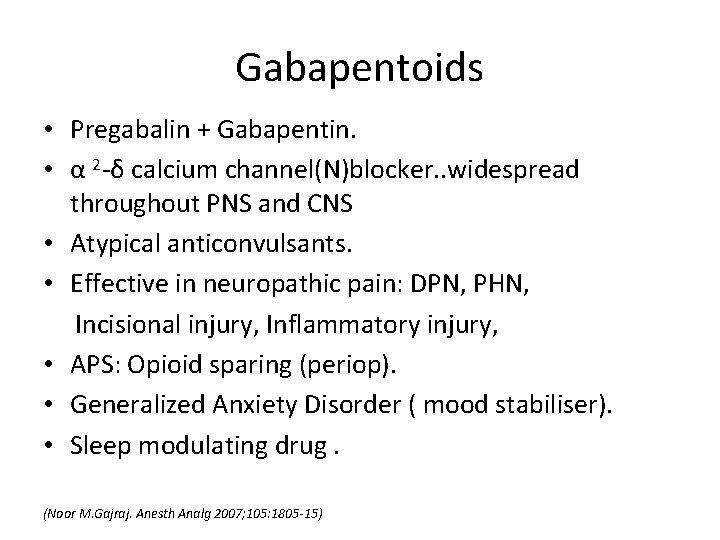
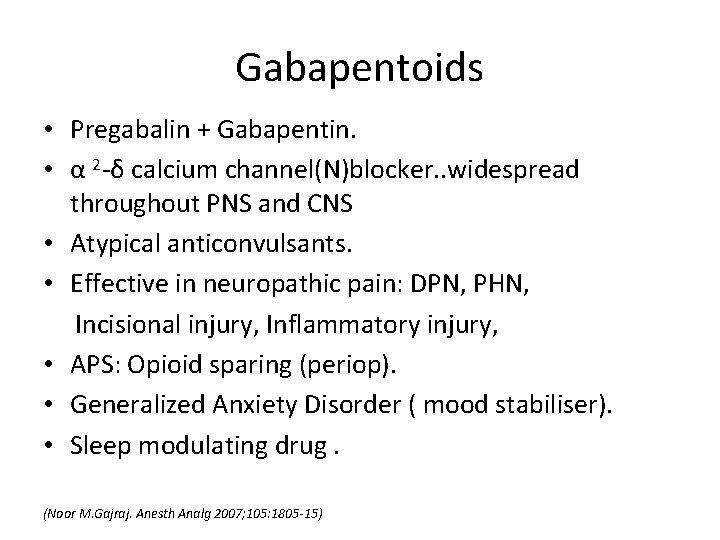
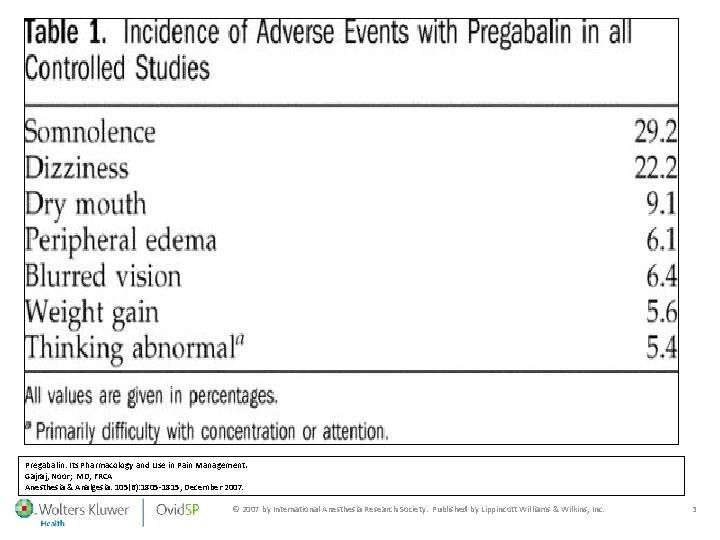
Gabapentoids • Pregabalin + Gabapentin. • α 2 -δ calcium channel(N)blocker. . widespread throughout PNS and CNS • Atypical anticonvulsants. • Effective in neuropathic pain: DPN, PHN, Incisional injury, Inflammatory injury, • APS: Opioid sparing (periop). • Generalized Anxiety Disorder ( mood stabiliser). • Sleep modulating drug. (Noor M. Gajraj. Anesth Analg 2007; 105: 1805 -15)
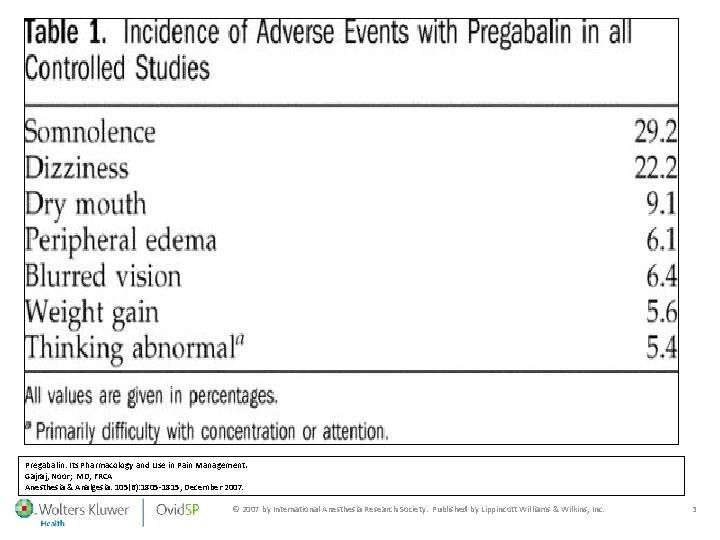
. Pregabalin: Its Pharmacology and Use in Pain Management. Gajraj, Noor; MD, FRCA Anesthesia & Analgesia. 105(6): 1805 -1815, December 2007. © 2007 by International Anesthesia Research Society. Published by Lippincott Williams & Wilkins, Inc. 3

. Comparison of Gabapentin and Pregabalin: Its Pharmacology and Use in Pain Management. Gajraj, Noor; MD, FRCA. Anesthesia & Analgesia. 105(6): 1805 -1815, December 2007. . 4
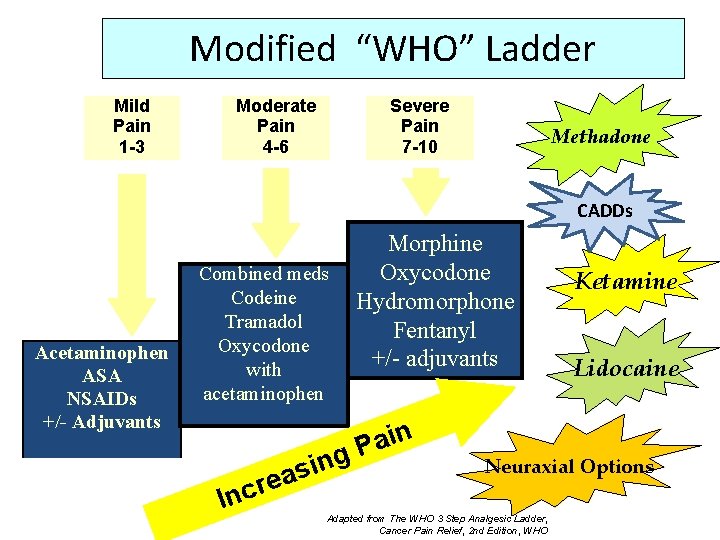
Modified “WHO” Ladder Mild Pain 1 -3 Moderate Pain 4 -6 Severe Pain 7 -10 Methadone CADDs Acetaminophen ASA NSAIDs +/- Adjuvants Combined meds Codeine Tramadol Oxycodone with acetaminophen n i a P g n i s a re Inc Morphine Oxycodone Hydromorphone Fentanyl +/- adjuvants Ketamine Lidocaine Neuraxial Options Adapted from The WHO 3 Step Analgesic Ladder, Cancer Pain Relief, 2 nd Edition, WHO

Managing Cancer Pain. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. History of Cancer + History of Pain. Standard assessment tools (ESAS, BPI) Document pain syndromes involved. Is cause known? – appropriate investigations. Formulate Treatment plan - ‘realistic goals’. Target Treatment @ Pain and Cause of Pain. WHO analgesic ladder. Early use of Co-Analgesics: Multi-Modal Analgesia Balance treatment efficacy/side effects /cost. Set dose and time limits for review.
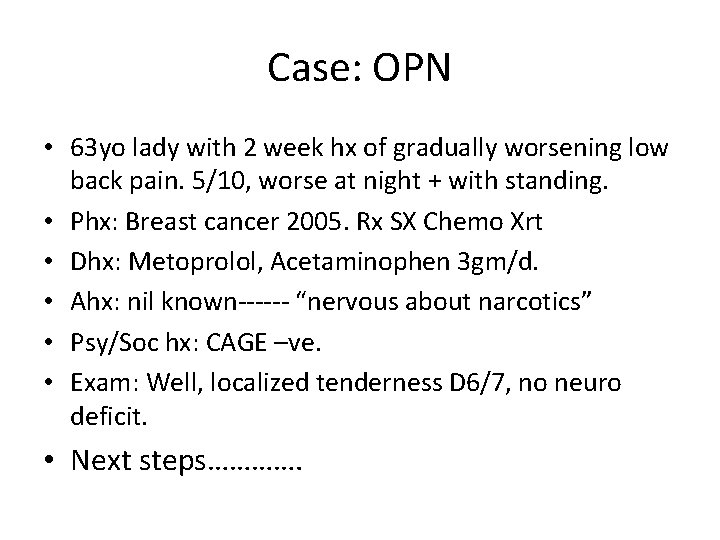
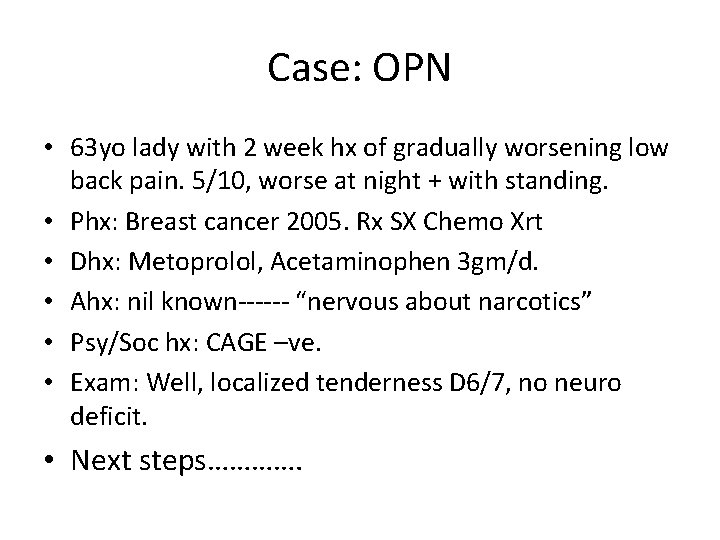
Case: OPN • 63 yo lady with 2 week hx of gradually worsening low back pain. 5/10, worse at night + with standing. • Phx: Breast cancer 2005. Rx SX Chemo Xrt • Dhx: Metoprolol, Acetaminophen 3 gm/d. • Ahx: nil known------ “nervous about narcotics” • Psy/Soc hx: CAGE –ve. • Exam: Well, localized tenderness D 6/7, no neuro deficit. • Next steps………….
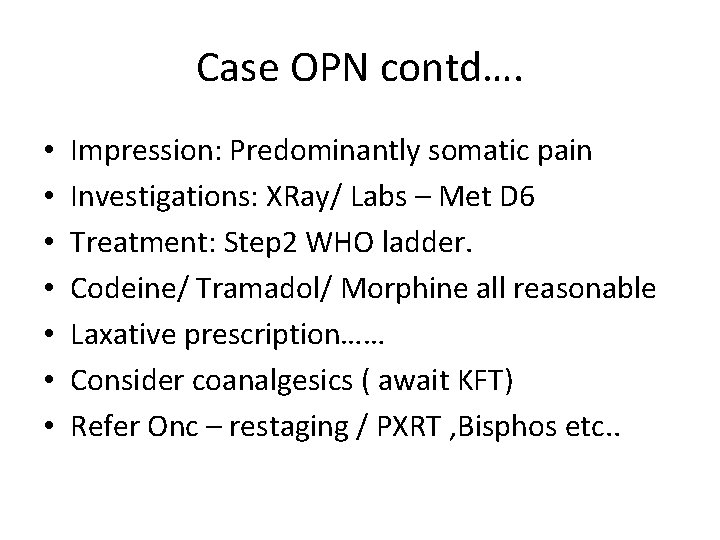
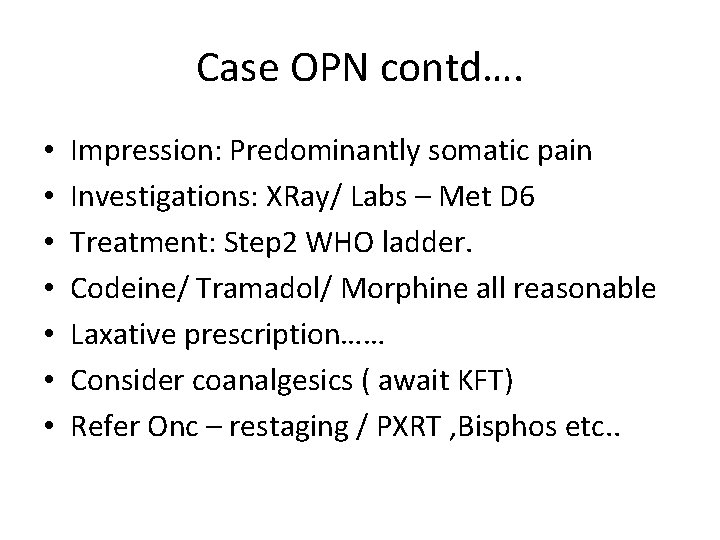
Case OPN contd…. • • Impression: Predominantly somatic pain Investigations: XRay/ Labs – Met D 6 Treatment: Step 2 WHO ladder. Codeine/ Tramadol/ Morphine all reasonable Laxative prescription…… Consider coanalgesics ( await KFT) Refer Onc – restaging / PXRT , Bisphos etc. .
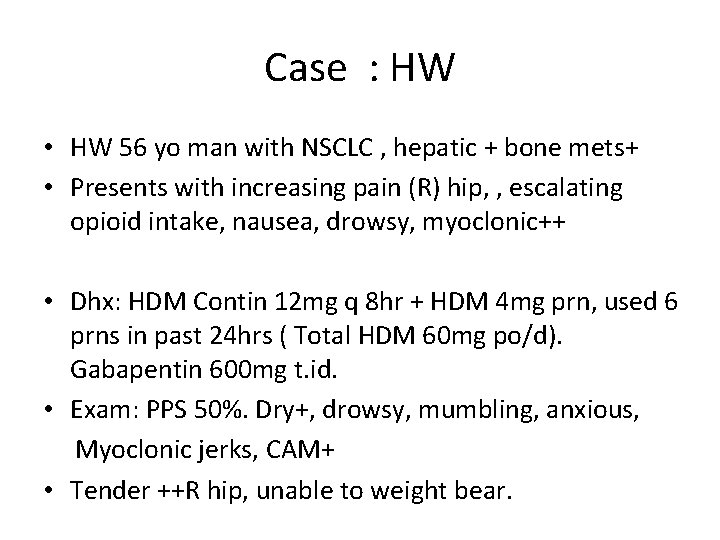
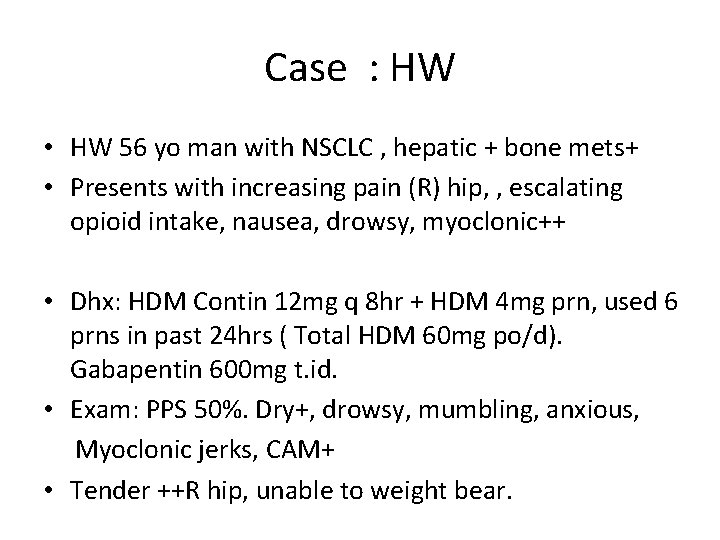
Case : HW • HW 56 yo man with NSCLC , hepatic + bone mets+ • Presents with increasing pain (R) hip, , escalating opioid intake, nausea, drowsy, myoclonic++ • Dhx: HDM Contin 12 mg q 8 hr + HDM 4 mg prn, used 6 prns in past 24 hrs ( Total HDM 60 mg po/d). Gabapentin 600 mg t. id. • Exam: PPS 50%. Dry+, drowsy, mumbling, anxious, Myoclonic jerks, CAM+ • Tender ++R hip, unable to weight bear.
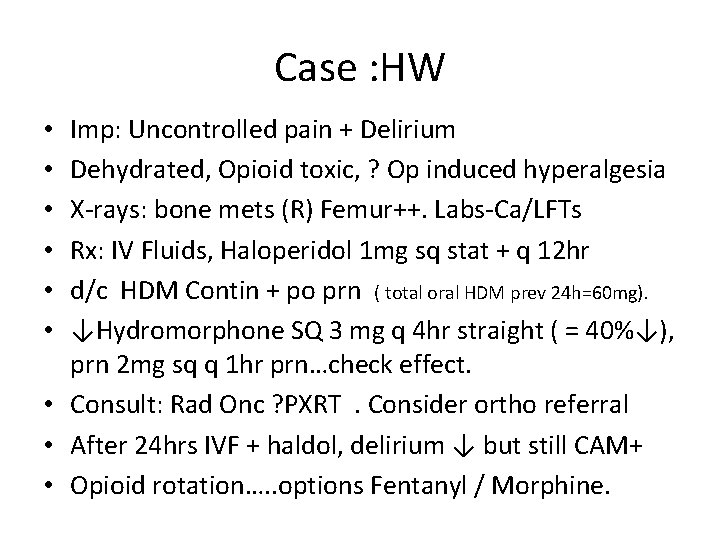
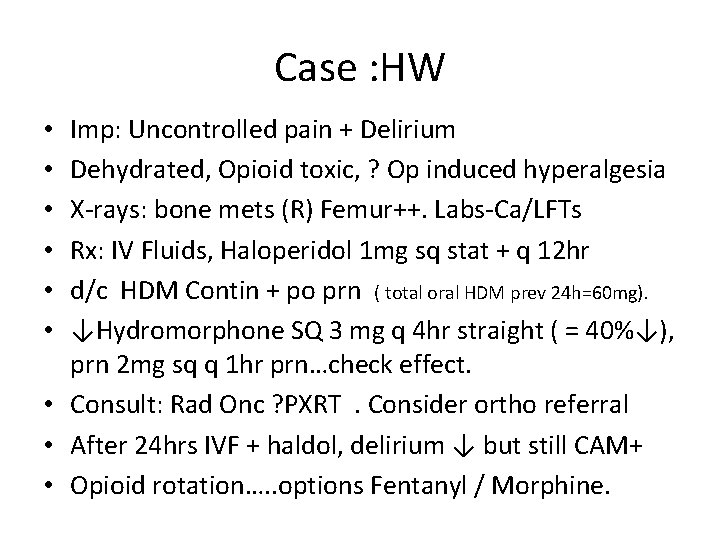
Case : HW Imp: Uncontrolled pain + Delirium Dehydrated, Opioid toxic, ? Op induced hyperalgesia X-rays: bone mets (R) Femur++. Labs-Ca/LFTs Rx: IV Fluids, Haloperidol 1 mg sq stat + q 12 hr d/c HDM Contin + po prn ( total oral HDM prev 24 h=60 mg). ↓Hydromorphone SQ 3 mg q 4 hr straight ( = 40%↓), prn 2 mg sq q 1 hr prn…check effect. • Consult: Rad Onc ? PXRT. Consider ortho referral • After 24 hrs IVF + haldol, delirium ↓ but still CAM+ • Opioid rotation…. . options Fentanyl / Morphine. • • •
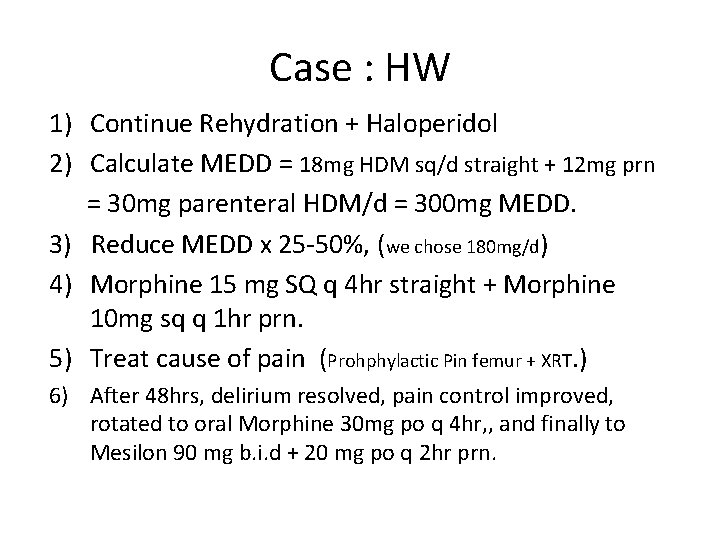
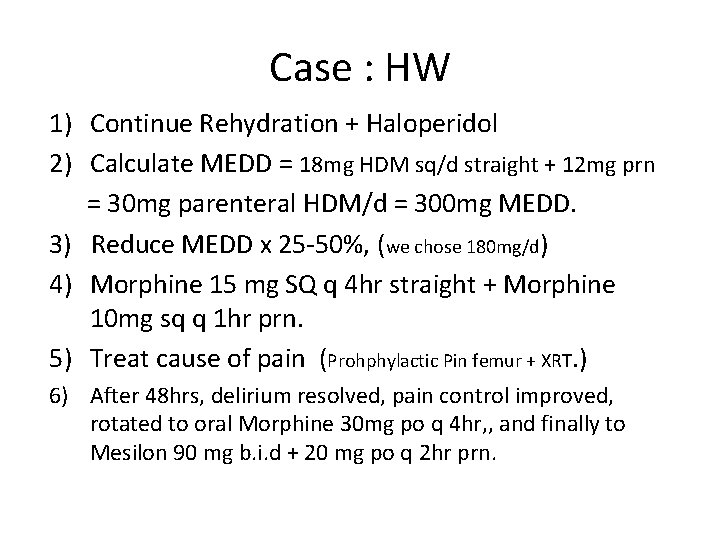
Case : HW 1) Continue Rehydration + Haloperidol 2) Calculate MEDD = 18 mg HDM sq/d straight + 12 mg prn = 30 mg parenteral HDM/d = 300 mg MEDD. 3) Reduce MEDD x 25 -50%, (we chose 180 mg/d) 4) Morphine 15 mg SQ q 4 hr straight + Morphine 10 mg sq q 1 hr prn. 5) Treat cause of pain (Prohphylactic Pin femur + XRT. ) 6) After 48 hrs, delirium resolved, pain control improved, rotated to oral Morphine 30 mg po q 4 hr, , and finally to Mesilon 90 mg b. i. d + 20 mg po q 2 hr prn.
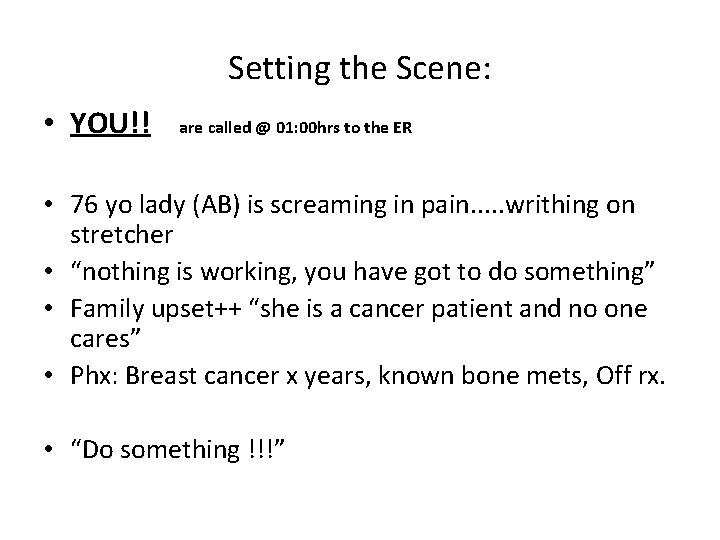
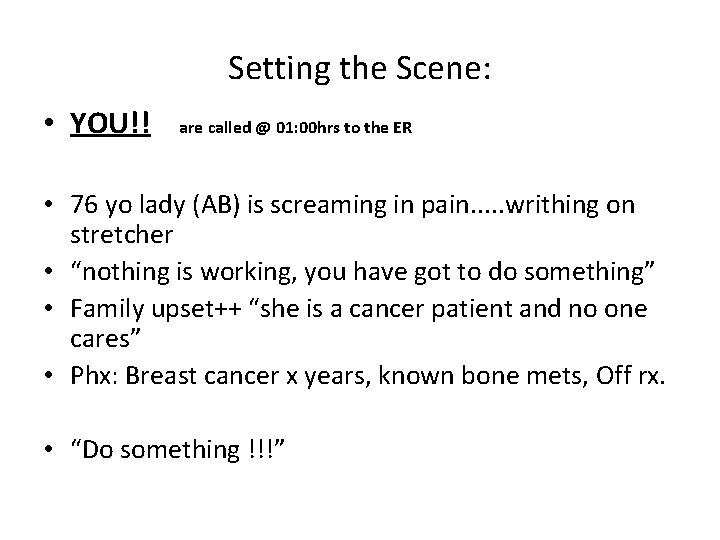
Setting the Scene: • YOU!! are called @ 01: 00 hrs to the ER • 76 yo lady (AB) is screaming in pain. . . writhing on stretcher • “nothing is working, you have got to do something” • Family upset++ “she is a cancer patient and no one cares” • Phx: Breast cancer x years, known bone mets, Off rx. • “Do something !!!”
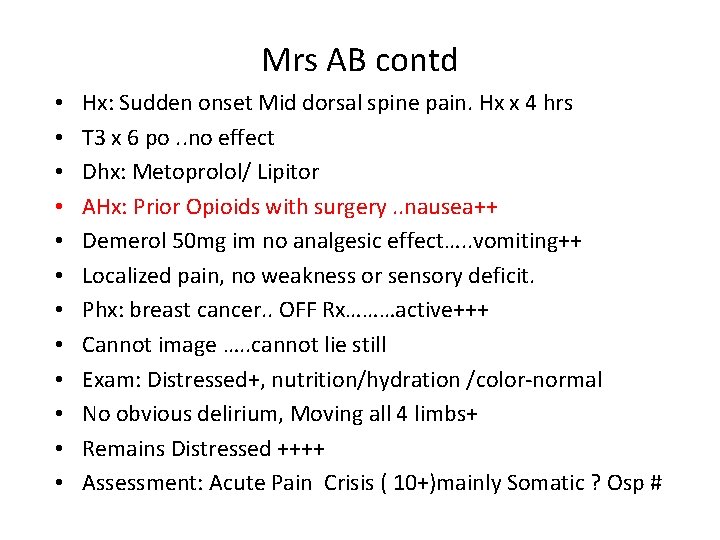
Mrs AB contd • • • Hx: Sudden onset Mid dorsal spine pain. Hx x 4 hrs T 3 x 6 po. . no effect Dhx: Metoprolol/ Lipitor AHx: Prior Opioids with surgery. . nausea++ Demerol 50 mg im no analgesic effect…. . vomiting++ Localized pain, no weakness or sensory deficit. Phx: breast cancer. . OFF Rx………active+++ Cannot image …. . cannot lie still Exam: Distressed+, nutrition/hydration /color-normal No obvious delirium, Moving all 4 limbs+ Remains Distressed ++++ Assessment: Acute Pain Crisis ( 10+)mainly Somatic ? Osp #
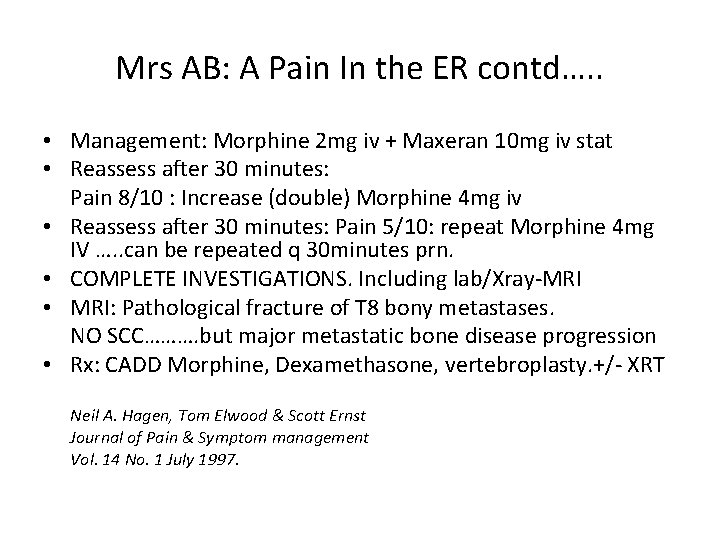
Mrs AB: A Pain In the ER contd…. . • Management: Morphine 2 mg iv + Maxeran 10 mg iv stat • Reassess after 30 minutes: Pain 8/10 : Increase (double) Morphine 4 mg iv • Reassess after 30 minutes: Pain 5/10: repeat Morphine 4 mg IV …. . can be repeated q 30 minutes prn. • COMPLETE INVESTIGATIONS. Including lab/Xray-MRI • MRI: Pathological fracture of T 8 bony metastases. NO SCC………. but major metastatic bone disease progression • Rx: CADD Morphine, Dexamethasone, vertebroplasty. +/- XRT Neil A. Hagen, Tom Elwood & Scott Ernst Journal of Pain & Symptom management Vol. 14 No. 1 July 1997.
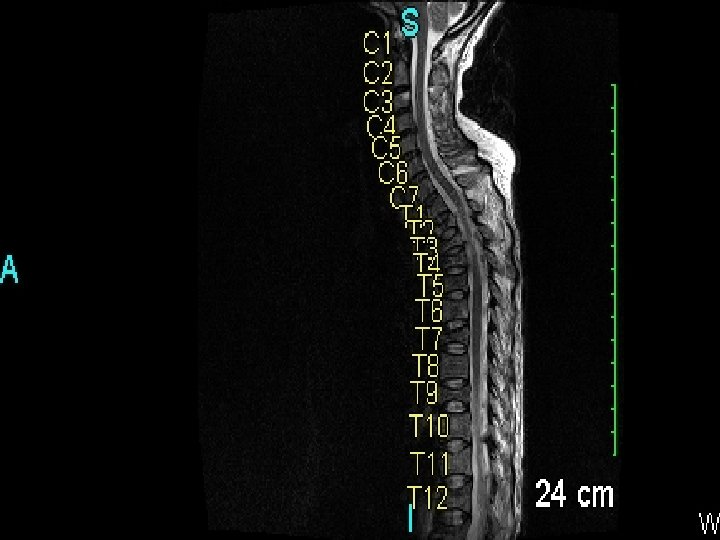
DMD: • 46 yo F, with 3/12 hx escalating back pain, now using walker……. . pain 10/10+ ( + = “don’t ask anymore!) • Exam: pale frail “small” lady…. distress++, • Multiple tender points on spine, ribs + pelvis. • PPS 50%. • Pain: somatic with ++++ incident pain, minor NP • Labs; Hgb 70 g/l, Creatinine 250 umol/l • Meds: Dex 8 mg/d, HDM Contin 12 mg b. i. d+ 4 mg q 2 hr, TCA • Intolerant opioids…nauseating, drowsy, hallucinations+ • CADD Fentanyl 60 ucg/hr…. . . . helps but cannot move due to pain!. . . increasing dose …. drowsy+ hallucinations. • Dx: Multiple myeloma/ renal failure/ low opioid threshold………………. MRI --
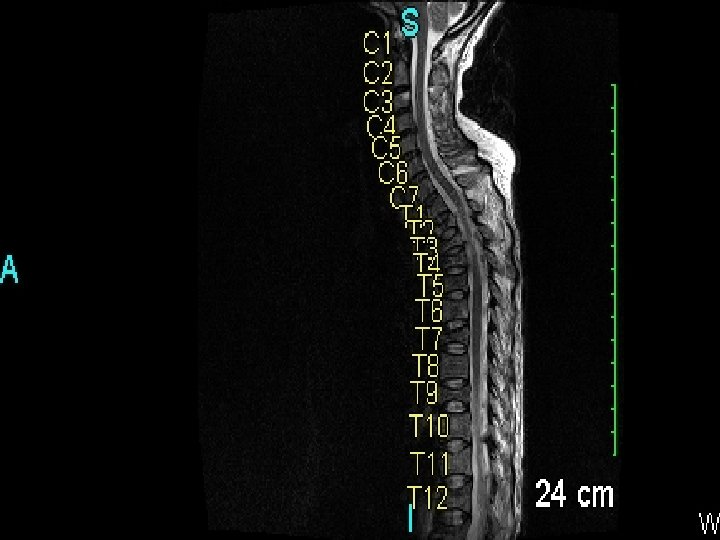
Xena “ Warrior Princess” • • PCA Ketamine 2 mg /hr …no bolus Day 3. . Combined Fentanyl (40) + Ketamine (2) per ml Rate 1. 5 mls /hr , 1 ml q 20 mins prn. Pain controlled at rest -- Start chemo + physio + TLSO brace. • • • Day 80: PCA a nuisance. …. . cant go to rehab with it. Feeling better………. mobilising well……how about the PCA? Start Methadone 2. 5 mg q 8 hr……titrate PCA Day 8. . stop PCA, Methadone 10 mg q 8 hr + 5 mg q 3 hrs prn HOME.
Successful Treatment of Pain Depends On ………… • • • Determining that pain is present! Focused History and Physical Exam Identifying + Charting Pain mechanisms involved WHO analgesic ladder. Clear Treatment plan Predominance of neuropathic or incident pain Presence or absence of Delirium Patient’s + family’s expectations and beliefs Goals of Care clear. Attitudes + Knowledge of Health Care Professionals Leave your egos at the door!
Questions? ?

Dilemma in Palliative Care I really think you should sue your doctor for malpractice! Two years ago he only gave you six months to live!

Another Case • • • Mr. B is a 74 year old man with extensive small cell cancer of the lung. (PPS 40%) Multiple hepatic and bone metastases. Hepatic and renal function normal. Initially treated with chemotherapy and radiation to the lung and the spine. Presented to the clinic with complaints of increasing ‘excruciating’ back pain (10+/10).
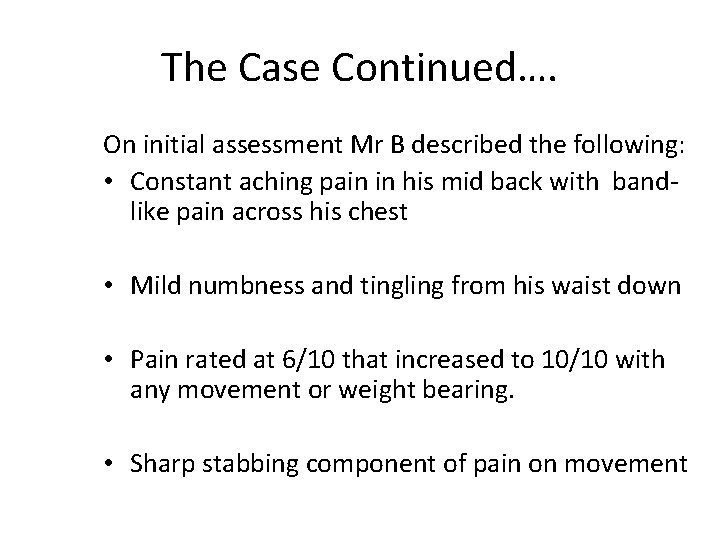
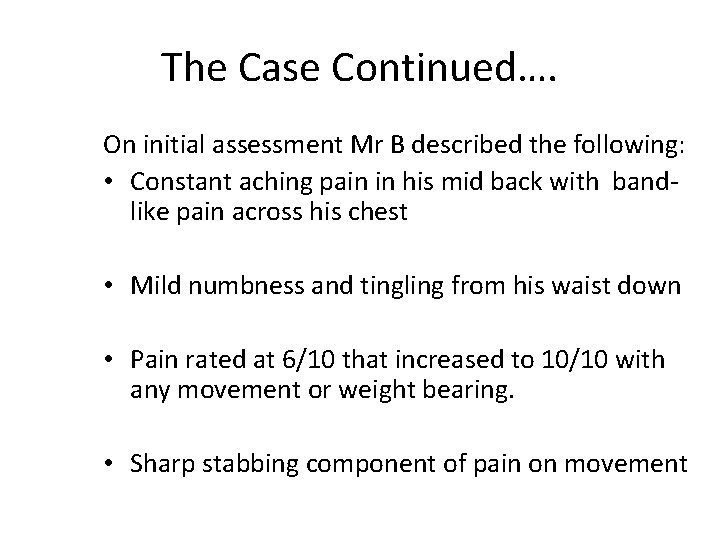
The Case Continued…. On initial assessment Mr B described the following: • Constant aching pain in his mid back with bandlike pain across his chest • Mild numbness and tingling from his waist down • Pain rated at 6/10 that increased to 10/10 with any movement or weight bearing. • Sharp stabbing component of pain on movement
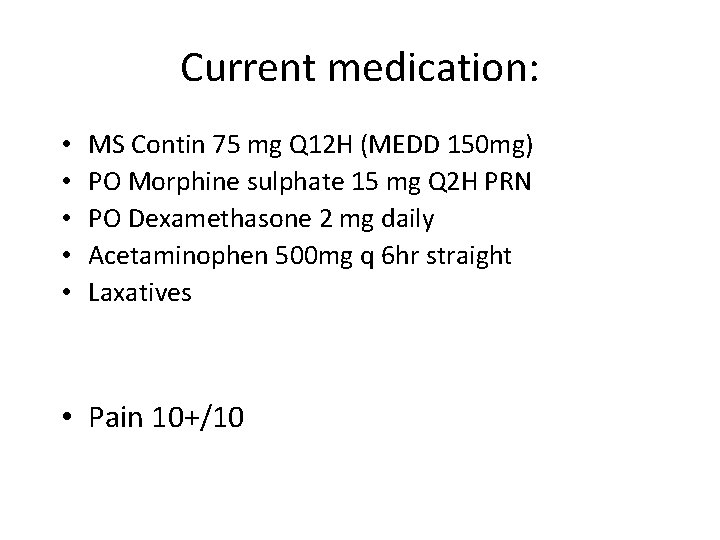
Current medication: • • • MS Contin 75 mg Q 12 H (MEDD 150 mg) PO Morphine sulphate 15 mg Q 2 H PRN PO Dexamethasone 2 mg daily Acetaminophen 500 mg q 6 hr straight Laxatives • Pain 10+/10
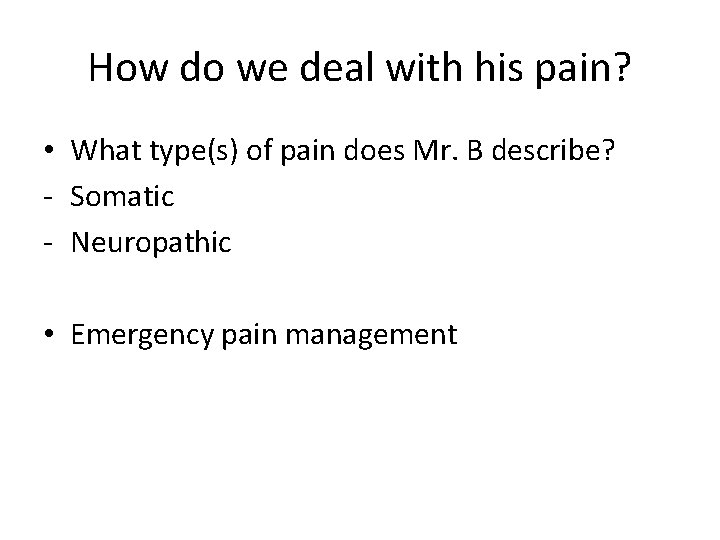
How do we deal with his pain? • What type(s) of pain does Mr. B describe? - Somatic - Neuropathic • Emergency pain management
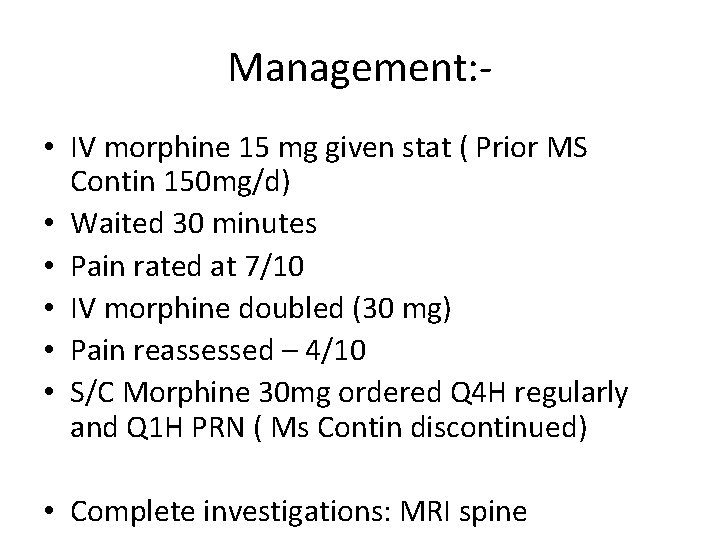
Management: • IV morphine 15 mg given stat ( Prior MS Contin 150 mg/d) • Waited 30 minutes • Pain rated at 7/10 • IV morphine doubled (30 mg) • Pain reassessed – 4/10 • S/C Morphine 30 mg ordered Q 4 H regularly and Q 1 H PRN ( Ms Contin discontinued) • Complete investigations: MRI spine
Causes of Mr. B’s Pain • MRI spine: Progression of bone mets in thoracic and lumbar spine with possible compression fractures but no SCC • CT scan also shows extensive progression of lung and liver metastases
Additional Management • Dexamethasone 16 mg/d • Pregabalin 25 mg po stat + t. i. d. • Titrated to 50 mg t. i. d after 48 hrs. • Urgent PXRT
Continuation • Mr. B’s baseline pain improved however incidental pain remained challenging. He required frequent breakthrough pain medication but developed some confusion and myoclonus, drowsiness +. Dry+ • Morphine changed to dilaudid SC infusion via CADD (5 X stronger than morphine) • IV hydration.
Continuation • Mr. B was discharged home on Dec 23 rd to spend Christmas with his family @ home. • Mr. B died on Dec 30 th peacefully at home surrounded by his family.
Vision for Palliative Care Every person, when faced with an incurable disease, has the opportunity to live life fully, to receive timely and appropriate symptom management, to be supported along with his/her family with dignity and respect throughout the course of their illness, and in the face of incurable disease, to have the opportunity to die in a setting of his/her choice. CCO Signature Event: Toronto March 2006
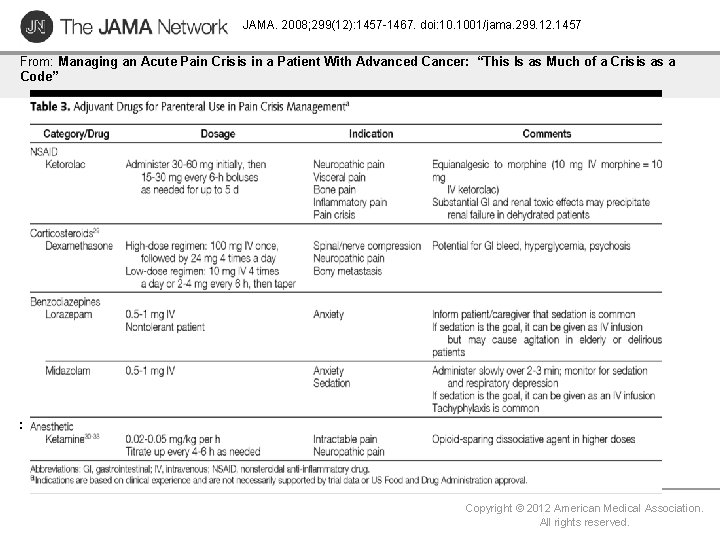
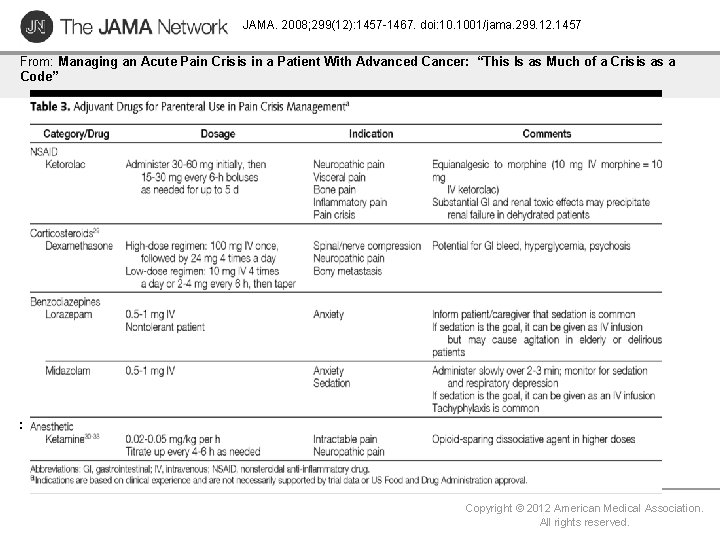
JAMA. 2008; 299(12): 1457 -1467. doi: 10. 1001/jama. 299. 12. 1457 From: Managing an Acute Pain Crisis in a Patient With Advanced Cancer: “This Is as Much of a Crisis as a Code” : Copyright © 2012 American Medical Association. All rights reserved.
Opioid Responsiveness A patient in pain should not be declared “unresponsive to opioids” until he/she has failed a titrated, sequential trial of all of the different opioid analgesics.
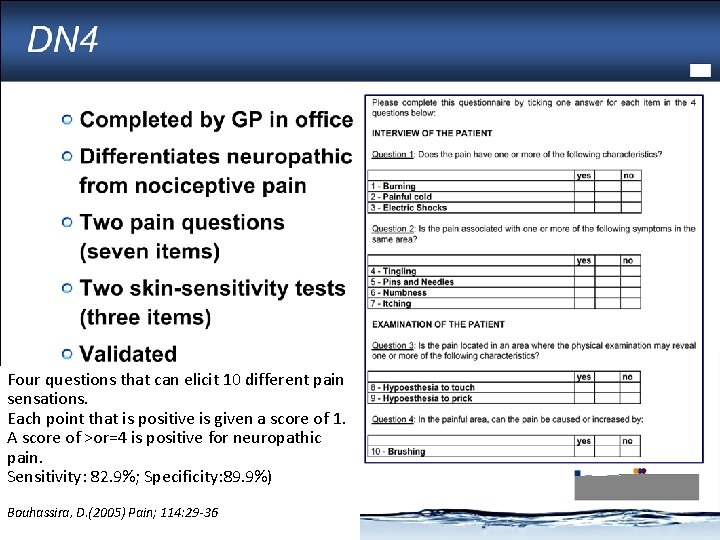
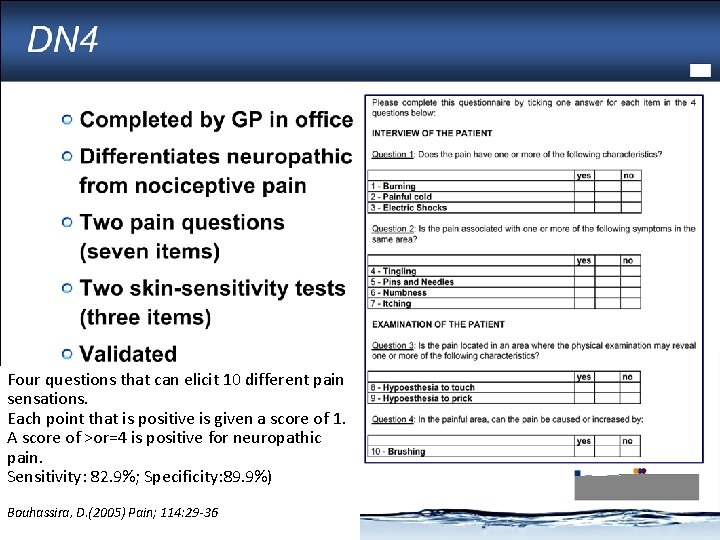
DN 4 Four questions that can elicit 10 different pain sensations. Each point that is positive is given a score of 1. A score of >or=4 is positive for neuropathic pain. Sensitivity: 82. 9%; Specificity: 89. 9%) Bouhassira, D. (2005) Pain; 114: 29 -36

Ketoralac: parenteral NSAID analgesic NSAID: non-selective reversible Cox 1 +2 inhibitor. 30 mg IV equianalgesic with 10 -12 mg Moprhine. Oral bioavailability= 100% Onset analgesia IV/IM = 30 mins, Peak 2 hrs, duration 8 hrs. Dosing: IV/IM 30 mg q hr prn ( max 120 mg/d) Oral: 20 mg stat, 10 mg po q 4 hr prn (max 40 mg /d) Max duration of use ( ≤ 5 days). • Metabolism: 68 -92% excreted unchanged in urine. • Toxicity: Renal: increase risk ATN, ARF , esp if dehydrated. CVS: increased risk thrombotic events (MI /CVA) GI: increased peptic ulceration/perforation *All side effects increased with prolonged use ≥ 5 days * • • •
 Palliative care versus hospice care
Palliative care versus hospice care Mad pain
Mad pain Period symptoms
Period symptoms Period cramps vs early pregnancy cramps
Period cramps vs early pregnancy cramps Esas-r
Esas-r Rug-adl score
Rug-adl score Hospice satisfaction survey
Hospice satisfaction survey Principles of palliative care
Principles of palliative care Palliative care in nepal
Palliative care in nepal Palliative care assistant
Palliative care assistant European certificate in palliative care
European certificate in palliative care Parallel planning palliative care
Parallel planning palliative care Franciscan palliative care
Franciscan palliative care Integrated palliative care outcome scale
Integrated palliative care outcome scale Problem severity score
Problem severity score Palliative care quality collaborative
Palliative care quality collaborative Antiemetic pediatric dose
Antiemetic pediatric dose Just in case bag palliative care
Just in case bag palliative care What is amber care
What is amber care Goscote palliative care centre
Goscote palliative care centre Palliative care at home barry
Palliative care at home barry Bluegrass hospice care
Bluegrass hospice care Calvary palliative care kogarah
Calvary palliative care kogarah Anorexia, nausea and vomiting
Anorexia, nausea and vomiting Palliative care matters
Palliative care matters Dr hong-phuc tran
Dr hong-phuc tran Goc palliative care
Goc palliative care National palliative care research center
National palliative care research center European delirium association
European delirium association Epeco
Epeco Textbook of palliative care communication
Textbook of palliative care communication Oacc palliative care
Oacc palliative care Ethical issues in palliative care
Ethical issues in palliative care Primary care secondary care tertiary care
Primary care secondary care tertiary care Angina care plan
Angina care plan Controlled and uncontrolled observation
Controlled and uncontrolled observation The sign for an uncontrolled railroad crossing is a
The sign for an uncontrolled railroad crossing is a Chapter 7 negotiating intersections
Chapter 7 negotiating intersections Chapter 7 negotiating intersections
Chapter 7 negotiating intersections Single phase half wave uncontrolled rectifier with rl load
Single phase half wave uncontrolled rectifier with rl load Uncontrolled copy 意味
Uncontrolled copy 意味 Vocab level d unit 3
Vocab level d unit 3 Kellogg drawing stages
Kellogg drawing stages Uncontrolled clonal proliferation
Uncontrolled clonal proliferation Uncontrolled foreign fishing
Uncontrolled foreign fishing Controlled uncontrolled and blind intersections
Controlled uncontrolled and blind intersections Uncontrolled aerodrome procedures
Uncontrolled aerodrome procedures Uncontrolled cell division
Uncontrolled cell division An uncontrollable outburst of emotion
An uncontrollable outburst of emotion Bi state primary care conference
Bi state primary care conference Missionary care conference
Missionary care conference Viabilidad institucional de un proyecto
Viabilidad institucional de un proyecto Cc pei
Cc pei Dimension convivencial
Dimension convivencial Pei progetto di vita
Pei progetto di vita Esempio verifica pei
Esempio verifica pei Ng pei tong
Ng pei tong Im pei pronunciation
Im pei pronunciation Metas del pei
Metas del pei Plano de ação de nivelamento pei
Plano de ação de nivelamento pei Easter seals pei
Easter seals pei Sang xing tang
Sang xing tang Obiettivi pei per aree
Obiettivi pei per aree Ejemplos de resultados de un proyecto
Ejemplos de resultados de un proyecto Usr mantova
Usr mantova Importancia de pei
Importancia de pei Obiettivi pei per aree
Obiettivi pei per aree Profilo dinamico funzionale
Profilo dinamico funzionale Obiettivi pei per aree
Obiettivi pei per aree Acn cable
Acn cable Factors affecting soil erosion
Factors affecting soil erosion Pei
Pei Animadoras infantiles xxx
Animadoras infantiles xxx Pei escuela de lenguaje
Pei escuela de lenguaje La pei zrenjanin
La pei zrenjanin Ritopei
Ritopei Pei tong primary school psle result
Pei tong primary school psle result Kei+pei=kef+pef calculator
Kei+pei=kef+pef calculator Pei tong primary school uniform
Pei tong primary school uniform Kaf vav kuf
Kaf vav kuf I've been everywhere in canada my home
I've been everywhere in canada my home Phyllis pei
Phyllis pei Chou pei suan ching
Chou pei suan ching Phyllis pei
Phyllis pei Pei internet
Pei internet Barriere e facilitatori a scuola
Barriere e facilitatori a scuola Esempio verifica pei
Esempio verifica pei Barriere e facilitatori esempi pei
Barriere e facilitatori esempi pei Jacqueline pei
Jacqueline pei Griglia di osservazione su base icf
Griglia di osservazione su base icf Punti di forza e debolezza insegnante
Punti di forza e debolezza insegnante Ieoh ming pei philosophy
Ieoh ming pei philosophy Luna
Luna Pei punti di forza e debolezza esempi
Pei punti di forza e debolezza esempi Cos'è il pei
Cos'è il pei Griglie di osservazione erickson
Griglie di osservazione erickson Enfoques de la gestión escolar
Enfoques de la gestión escolar Kei+pei=kef+pef calculator
Kei+pei=kef+pef calculator Www.myblueprint/tcdsb
Www.myblueprint/tcdsb Commissioner of oaths pei
Commissioner of oaths pei Pei javeriana
Pei javeriana