North Thames Paediatric Network An overview VISION Function


- Slides: 18
North Thames Paediatric Network An overview
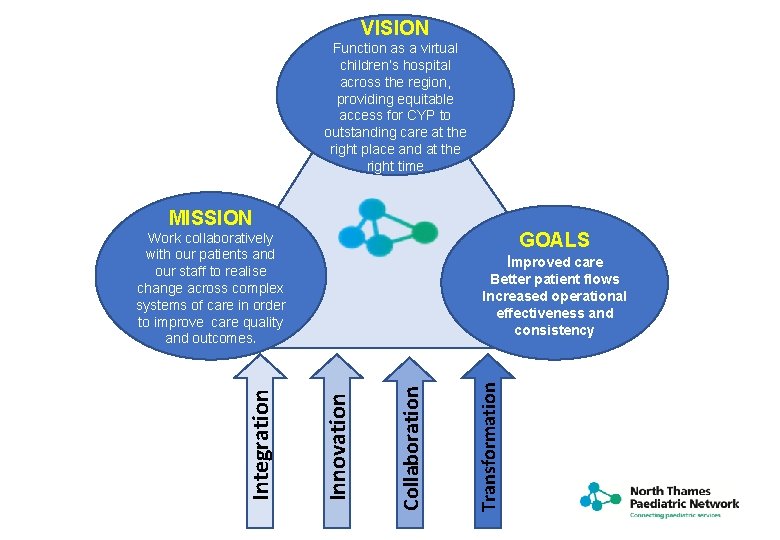
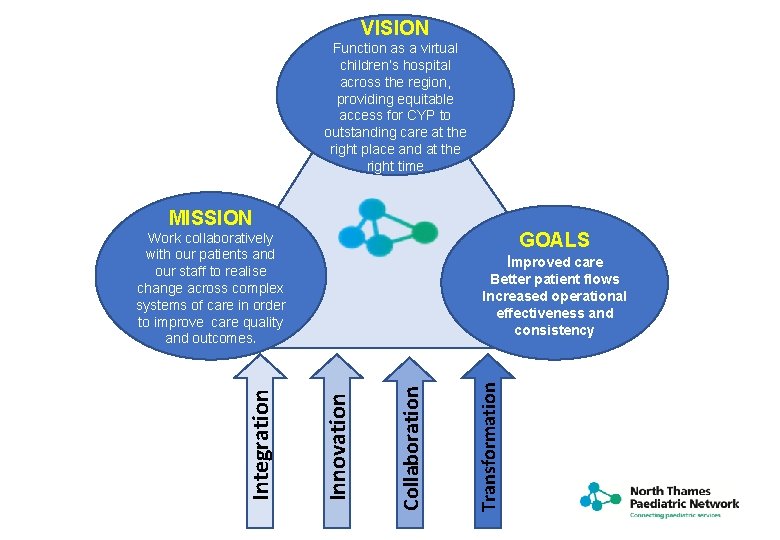
VISION Function as a virtual children’s hospital across the region, providing equitable access for CYP to outstanding care at the right place and at the right time MISSION GOALS Improved care Transformation Collaboration Better patient flows Increased operational effectiveness and consistency Innovation Integration Work collaboratively with our patients and our staff to realise change across complex systems of care in order to improve care quality and outcomes.

In five years , London will have the best healthcare for children ned g i s s de child e c i Serv nd the arou Specialist care provided in the community e obil m ble ce i x e l A f orkfor w tra Seam nsi tio less n ser to a vic es dult n o s u Foc ention v pre oke d sp n a Hub odels m job d e eas ion r c n I act f s i t sa on i t a i var s d ce vice u d Re in ser A virtual children’s hospital across the region providing equitable access for children and young people to outstanding care at the right place, right time
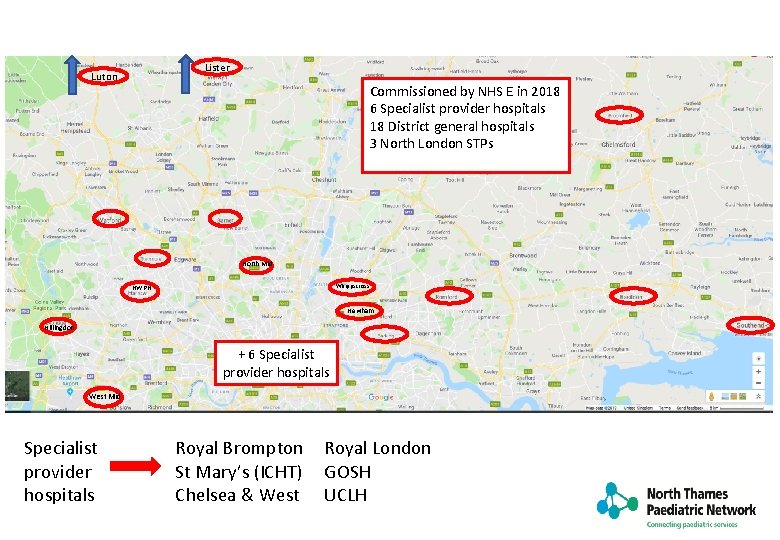
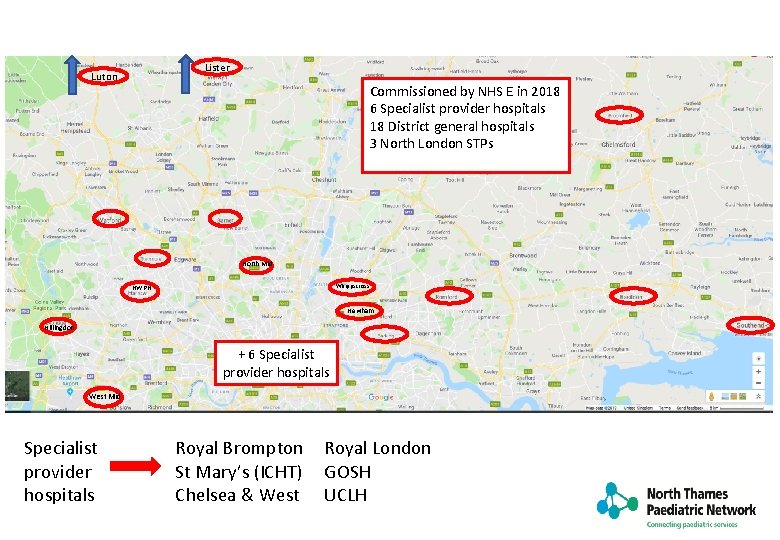
Lister Luton Commissioned by NHS E in 2018 6 Specialist provider hospitals 18 District general hospitals 3 North London STPs North Mid Whippscross NWPH Newham Hillingdon + 6 Specialist provider hospitals West Mid Specialist provider hospitals Royal Brompton St Mary’s (ICHT) Chelsea & West Royal London GOSH UCLH
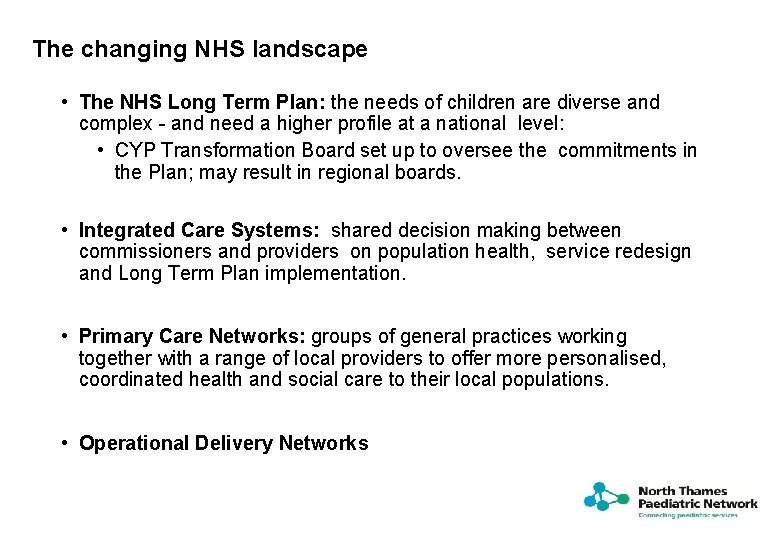
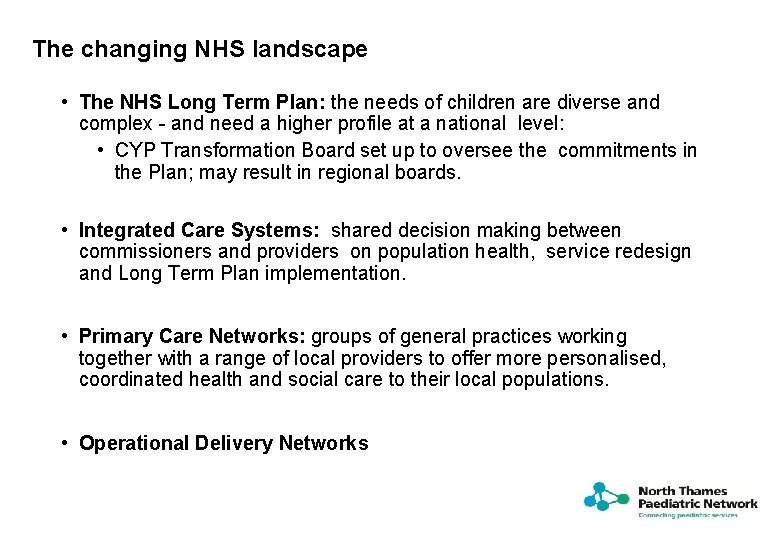
The changing NHS landscape • The NHS Long Term Plan: the needs of children are diverse and complex - and need a higher profile at a national level: • CYP Transformation Board set up to oversee the commitments in the Plan; may result in regional boards. • Integrated Care Systems: shared decision making between commissioners and providers on population health, service redesign and Long Term Plan implementation. • Primary Care Networks: groups of general practices working together with a range of local providers to offer more personalised, coordinated health and social care to their local populations. • Operational Delivery Networks
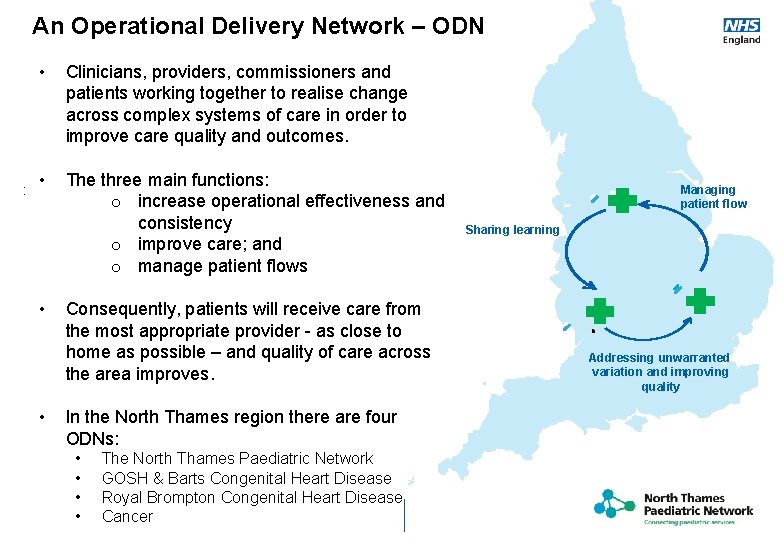
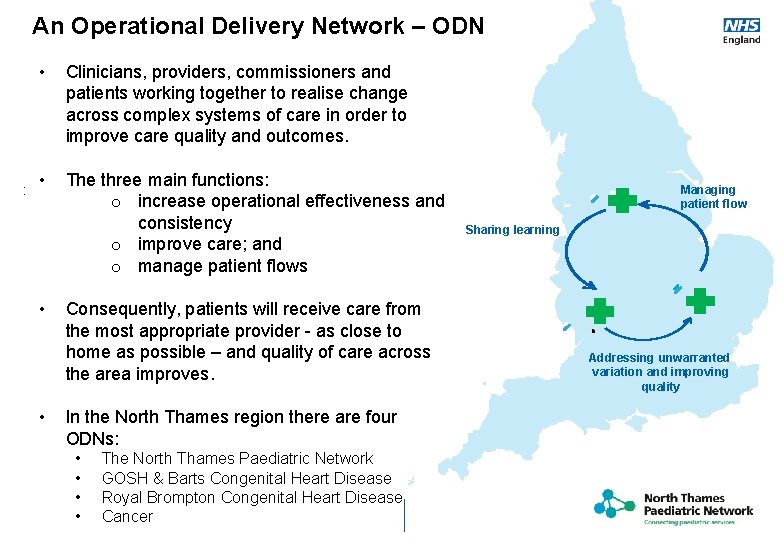
An Operational Delivery Network – ODN : • Clinicians, providers, commissioners and patients working together to realise change across complex systems of care in order to improve care quality and outcomes. • The three main functions: o increase operational effectiveness and consistency o improve care; and o manage patient flows • • Consequently, patients will receive care from the most appropriate provider - as close to home as possible – and quality of care across the area improves. In the North Thames region there are four ODNs: • • • Introduction • The North Thames Paediatric Network GOSH & Barts Congenital Heart Disease Royal Brompton Congenital Heart Disease Cancer Managing patient flow Sharing learning Addressing unwarranted variation and improving quality
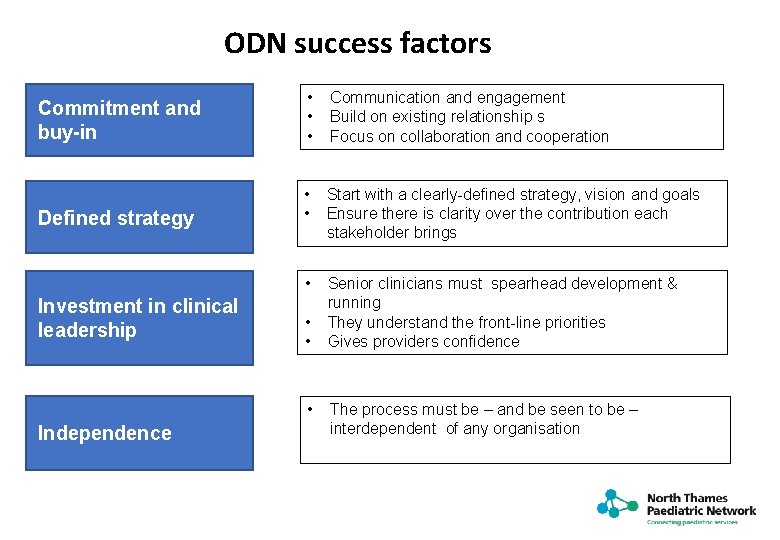
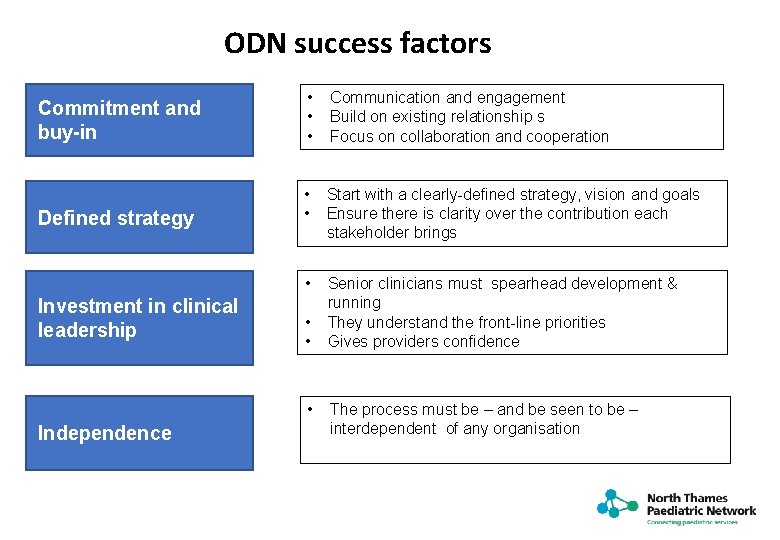
ODN success factors Commitment and buy-in • • • Communication and engagement Build on existing relationship s Focus on collaboration and cooperation Defined strategy • • Start with a clearly-defined strategy, vision and goals Ensure there is clarity over the contribution each stakeholder brings • Senior clinicians must spearhead development & running They understand the front-line priorities Gives providers confidence Investment in clinical leadership • • • Independence The process must be – and be seen to be – interdependent of any organisation
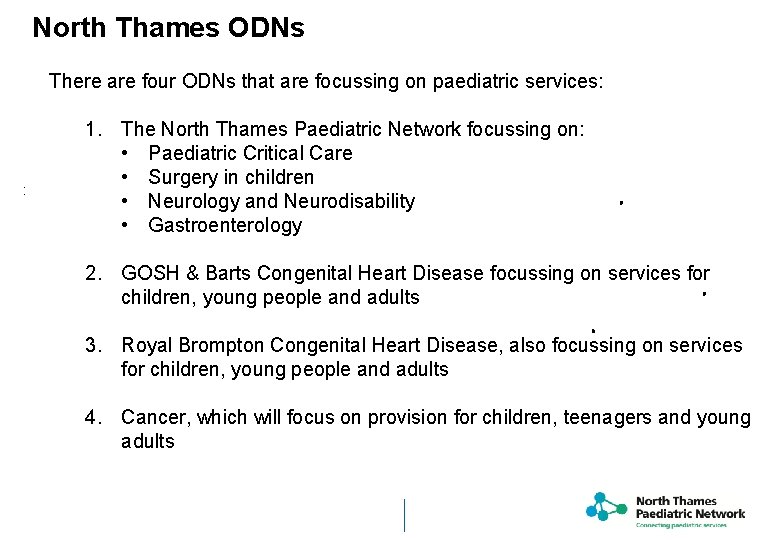
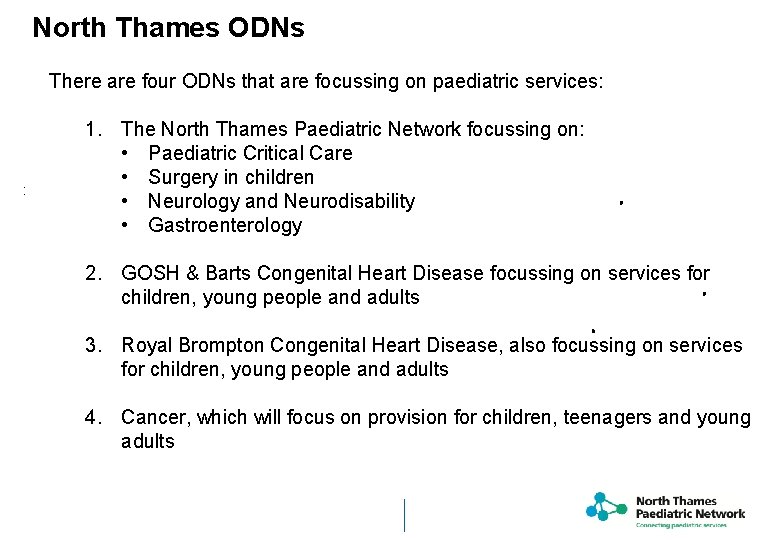
North Thames ODNs There are four ODNs that are focussing on paediatric services: 1. The North Thames Paediatric Network focussing on: • Paediatric Critical Care • Surgery in children • Neurology and Neurodisability • Gastroenterology : 2. GOSH & Barts Congenital Heart Disease focussing on services for children, young people and adults 3. Royal Brompton Congenital Heart Disease, also focussing on services for children, young people and adults 4. Cancer, which will focus on provision for children, teenagers and young adults Introduction
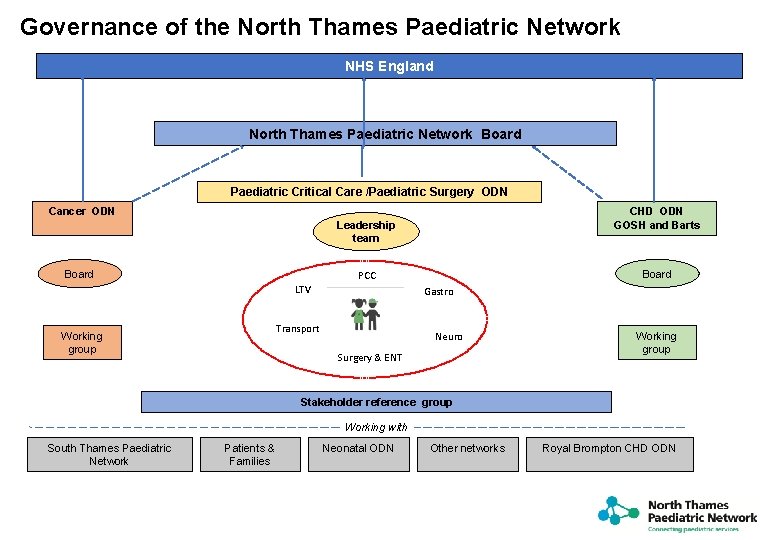
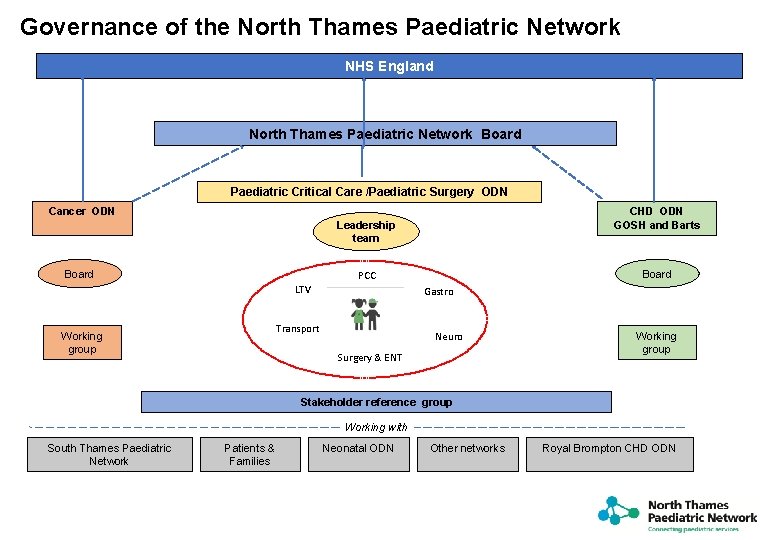
Governance of the North Thames Paediatric Network NHS England North Thames Paediatric Network Board Paediatric Critical Care /Paediatric Surgery ODN Cancer ODN CHD ODN GOSH and Barts Leadership team Board Working group Board PCC LTV Gastro Transport Neuro Surgery & ENT Working group Stakeholder reference group Working with South Thames Paediatric Network Patients & Families Neonatal ODN Other networks Royal Brompton CHD ODN
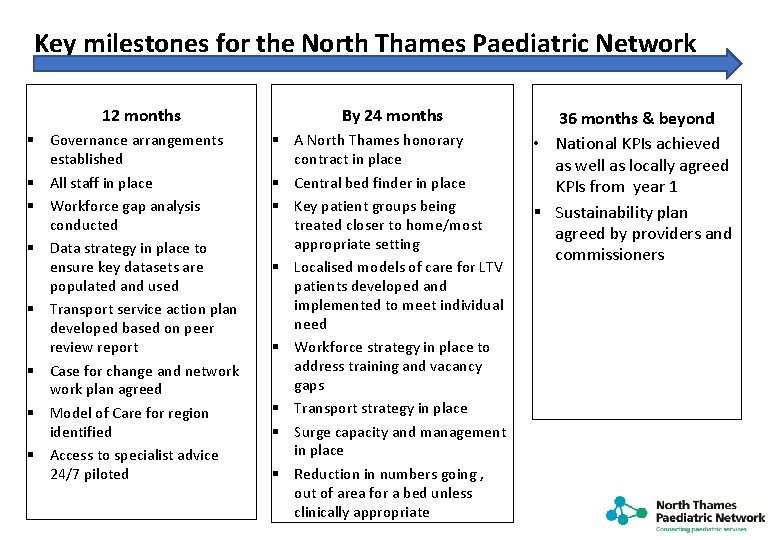
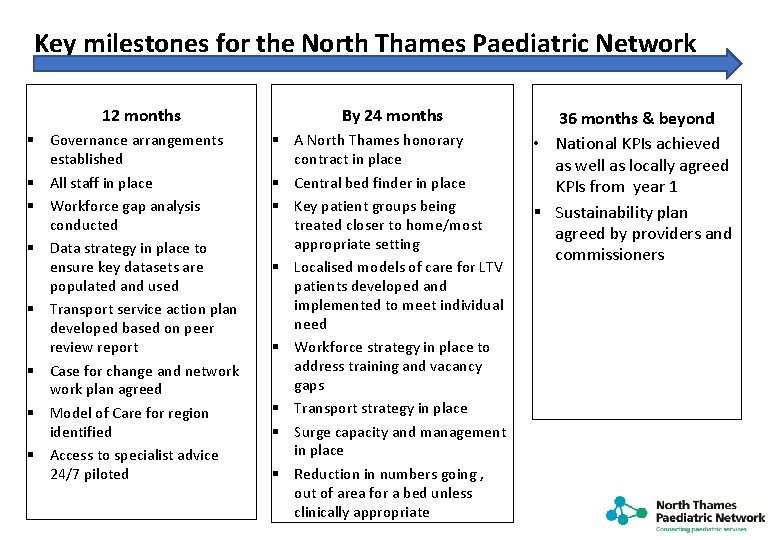
Key milestones for the North Thames Paediatric Network 12 months § Governance arrangements established § All staff in place § Workforce gap analysis conducted § Data strategy in place to ensure key datasets are populated and used § Transport service action plan developed based on peer review report § Case for change and network plan agreed § Model of Care for region identified § Access to specialist advice 24/7 piloted By 24 months § A North Thames honorary contract in place § Central bed finder in place § Key patient groups being treated closer to home/most appropriate setting § Localised models of care for LTV patients developed and implemented to meet individual need § Workforce strategy in place to address training and vacancy gaps § Transport strategy in place § Surge capacity and management in place § Reduction in numbers going , out of area for a bed unless clinically appropriate 36 months & beyond • National KPIs achieved as well as locally agreed KPIs from year 1 § Sustainability plan agreed by providers and commissioners
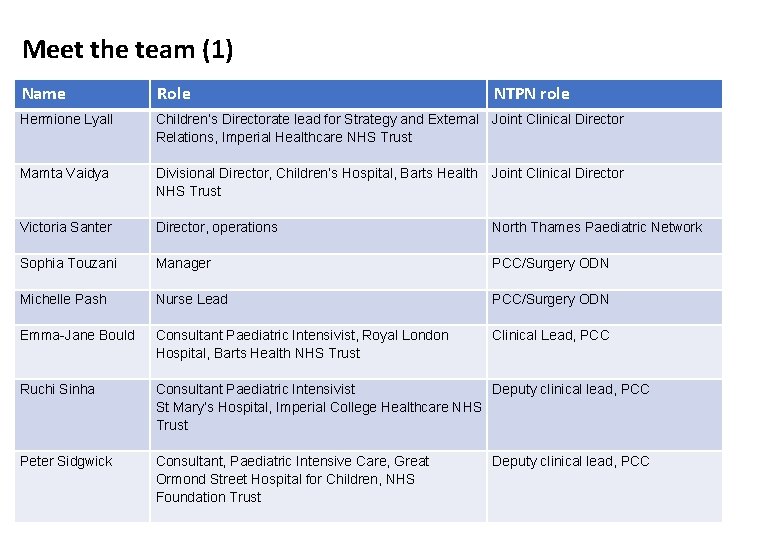
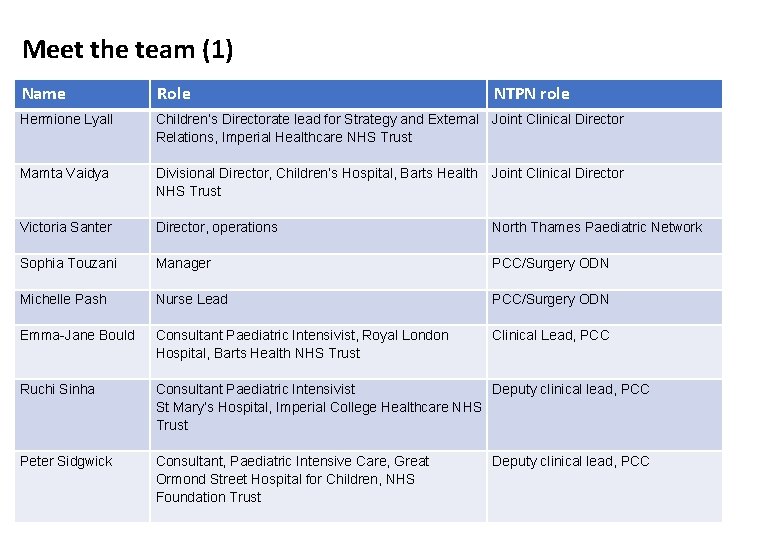
Meet the team (1) Name Role Hermione Lyall Children’s Directorate lead for Strategy and External Joint Clinical Director Relations, Imperial Healthcare NHS Trust Mamta Vaidya Divisional Director, Children’s Hospital, Barts Health Joint Clinical Director NHS Trust Victoria Santer Director, operations Manager Nurse Lead Consultant Paediatric Intensivist, Royal London Hospital, Barts Health NHS Trust Consultant Paediatric Intensivist St Mary’s Hospital, Imperial College Healthcare NHS Trust Consultant, Paediatric Intensive Care, Great Ormond Street Hospital for Children, NHS Foundation Trust Sophia Touzani Michelle Pash Emma-Jane Bould Ruchi Sinha Peter Sidgwick NTPN role North Thames Paediatric Network PCC/Surgery ODN Clinical Lead, PCC Deputy clinical lead, PCC
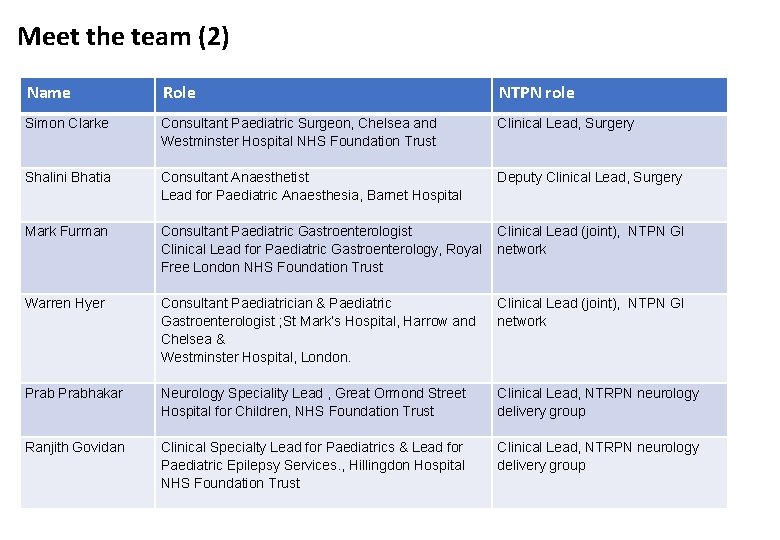
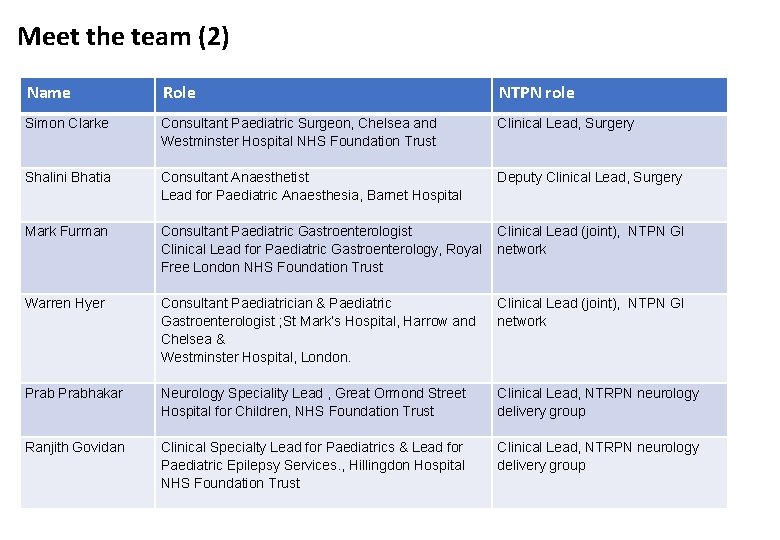
Meet the team (2) Name Role NTPN role Simon Clarke Consultant Paediatric Surgeon, Chelsea and Westminster Hospital NHS Foundation Trust Consultant Anaesthetist Lead for Paediatric Anaesthesia, Barnet Hospital Consultant Paediatric Gastroenterologist Clinical Lead for Paediatric Gastroenterology, Royal Free London NHS Foundation Trust Consultant Paediatrician & Paediatric Gastroenterologist ; St Mark’s Hospital, Harrow and Chelsea & Westminster Hospital, London. Neurology Speciality Lead , Great Ormond Street Hospital for Children, NHS Foundation Trust Clinical Specialty Lead for Paediatrics & Lead for Paediatric Epilepsy Services. , Hillingdon Hospital NHS Foundation Trust Clinical Lead, Surgery Shalini Bhatia Mark Furman Warren Hyer Prabhakar Ranjith Govidan Deputy Clinical Lead, Surgery Clinical Lead (joint), NTPN GI network Clinical Lead, NTRPN neurology delivery group
North Thames Paediatric Network Initial plans of work
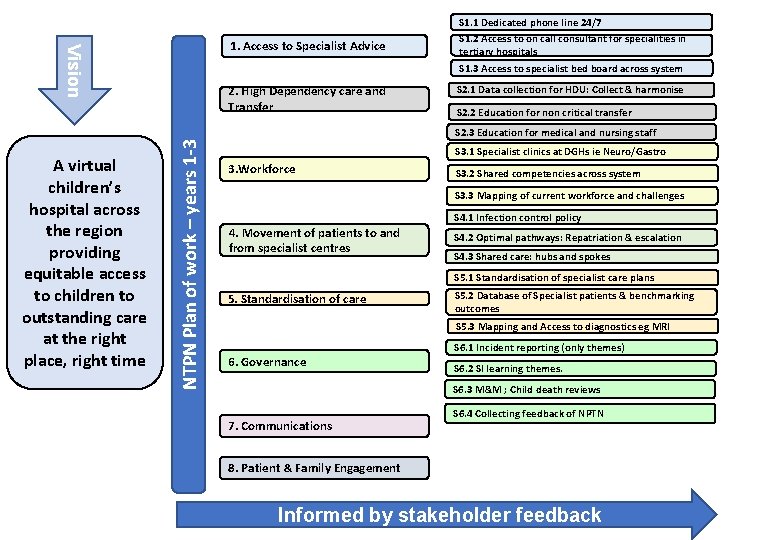
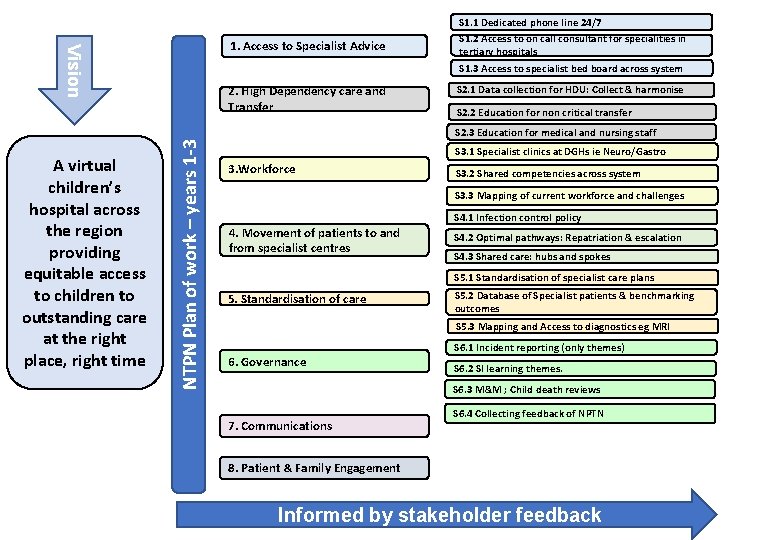
Vision 1. Access to Specialist Advice 2. High Dependency care and Transfer S 1. 1 Dedicated phone line 24/7 S 1. 2 Access to on call consultant for specialities in tertiary hospitals S 1. 3 Access to specialist bed board across system S 2. 1 Data collection for HDU: Collect & harmonise S 2. 2 Education for non critical transfer A virtual children’s hospital across the region providing equitable access to children to outstanding care at the right place, right time NTPN Plan of work – years 1 -3 S 2. 3 Education for medical and nursing staff S 3. 1 Specialist clinics at DGHs ie Neuro/Gastro 3. Workforce S 3. 2 Shared competencies across system S 3. 3 Mapping of current workforce and challenges S 4. 1 Infection control policy 4. Movement of patients to and from specialist centres S 4. 2 Optimal pathways: Repatriation & escalation S 4. 3 Shared care: hubs and spokes S 5. 1 Standardisation of specialist care plans 5. Standardisation of care S 5. 2 Database of Specialist patients & benchmarking outcomes S 5. 3 Mapping and Access to diagnostics eg MRI 6. Governance S 6. 1 Incident reporting (only themes) S 6. 2 SI learning themes. S 6. 3 M&M ; Child death reviews 7. Communications S 6. 4 Collecting feedback of NPTN 8. Patient & Family Engagement Informed by stakeholder feedback
• Paediatric Critical Care - areas of focus: • • • Beds; reducing occupancy to 90% by Year 2 HDU Level 2 provision Helping to DGHs to develop competencies Delayed discharge and step down processes Non-urgent transport strategy Learning from child deaths reviews – and SIs Ethical framework for LTV patients – and CYP with complex, long-term conditions. To include transition to adult services End of life pathways GIRFT review 2019/20 Surgery and CYP - areas of focus to be determined but to include: • • Mapping demand across the region and current pathways of care Using GIRFT data to baseline capacity across the region Mapping of current provision across the region Working with DGH colleagues to identify current challenges ; eg surgical, anaesthesia or ENT
Neurology – areas of focus: • • A shared, on-call rota to enable access to specialist advice 24/7 Access to Rapid Assessment Neurology Unit (RANU) Protocols for investigations prior to specialist referrals Outreach clinics Stroke pathways Guidelines re care of children with developmental delay CNS cover in DGHs & Community for epilepsy Transition to adult services • Gastroenterology - areas of focus: • • Referral pathways Data capture re workforce and waiting times Mapping referral pathways to quaternary services IBD; grading severity with timescales GI bleeding rota Primary Care support in regards to common GHI disorder Standardise TPN Transition to adult services
Workforce • • • Mapping of current resources to understand the pressures Mapping education offers across the region so all can benefit Regional agreement on honorary contracts and passports Developing the medical workforce Improving access to therapies; especially SLT New roles: ANP; nursing associates; physicians associates Increased role for Pharmacy Recruitment and retention strategy Links with Capital Nurse, HEE and Royal Colleges Business Intelligence and Data • Pathways of care to be mapped to determine current patient flows • Baseline of demand capacity at both tertiary and acute providers across relevant services being established. • Exploring Day of Care survey to provide a snapshot in time regarding delays within a system. • Mapping of diagnostic capacity and capability; eg scanning under sedation and GA • Building relationships with AHSCs – encouraging a research focussed approach to care.

Contact us at: england. ntpn@nhs. net