Paediatric respiratory distress EMC SDMH 2015 Identify paediatric

- Slides: 23
Paediatric respiratory distress { EMC SDMH 2015
Identify paediatric respiratory distress Become familiar with common causes Understand management protocols and disposition Objectives
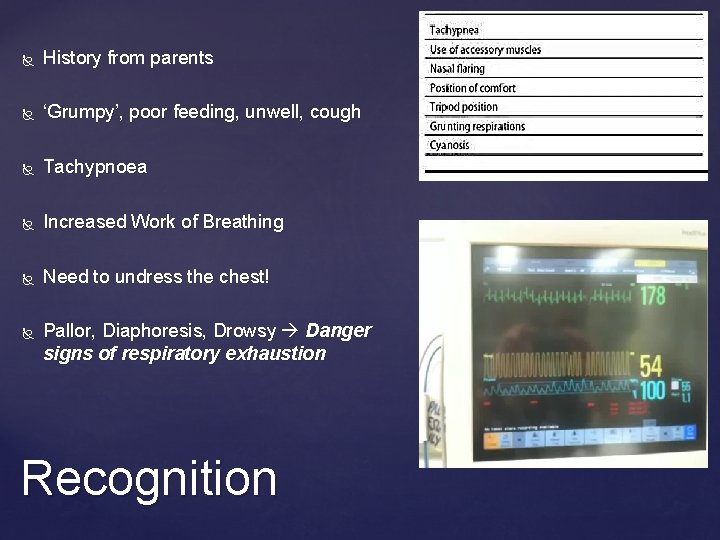
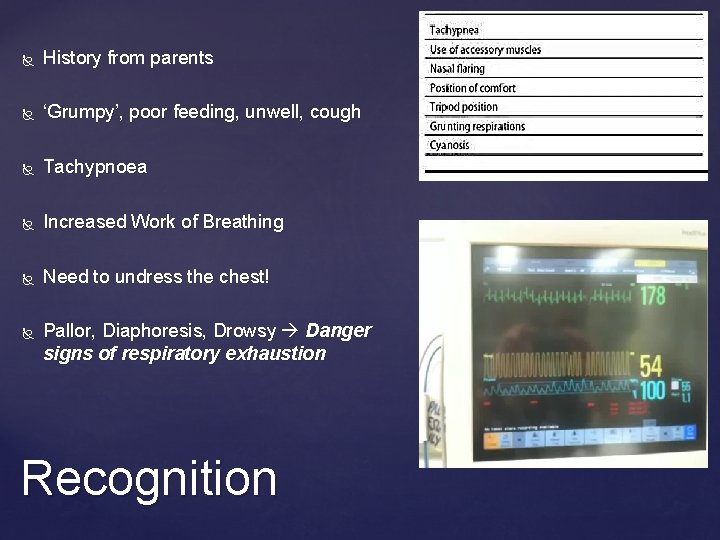
History from parents ‘Grumpy’, poor feeding, unwell, cough Tachypnoea Increased Work of Breathing Need to undress the chest! Pallor, Diaphoresis, Drowsy Danger signs of respiratory exhaustion Recognition
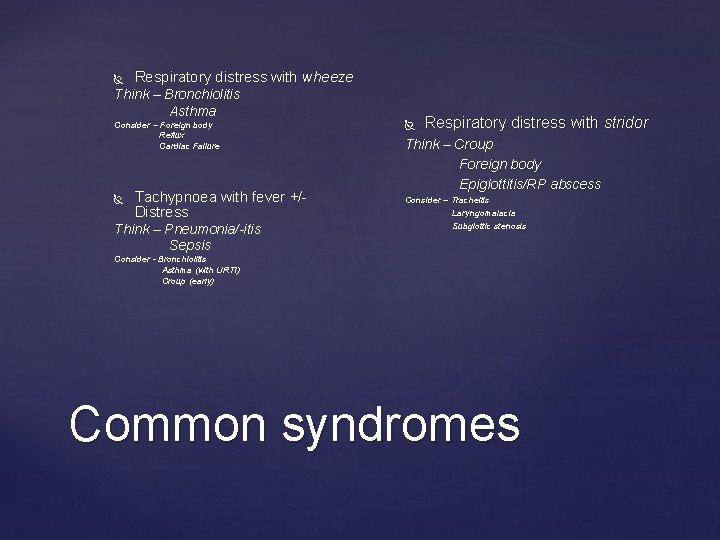
Respiratory distress with wheeze Think – Bronchiolitis Asthma Consider – Foreign body Reflux Cardiac Failure Tachypnoea with fever +/Distress Think – Pneumonia/-itis Sepsis Respiratory distress with stridor Think – Croup Foreign body Epiglottitis/RP abscess Consider – Tracheitis Laryngomalacia Subglottic stenosis Consider - Bronchiolitis Asthma (with URTI) Croup (early) Common syndromes
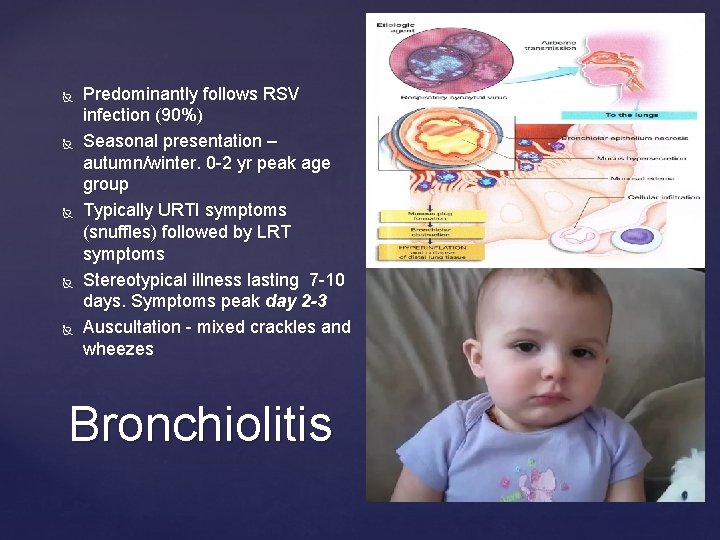
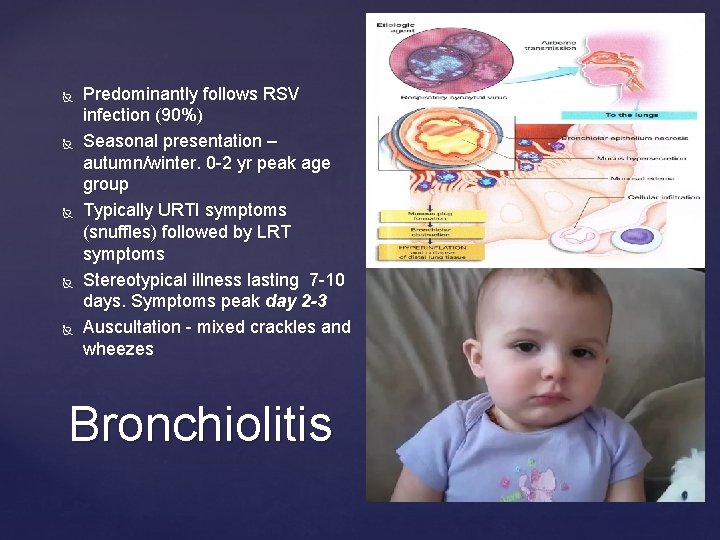
Predominantly follows RSV infection (90%) Seasonal presentation – autumn/winter. 0 -2 yr peak age group Typically URTI symptoms (snuffles) followed by LRT symptoms Stereotypical illness lasting 7 -10 days. Symptoms peak day 2 -3 Auscultation - mixed crackles and wheezes Bronchiolitis
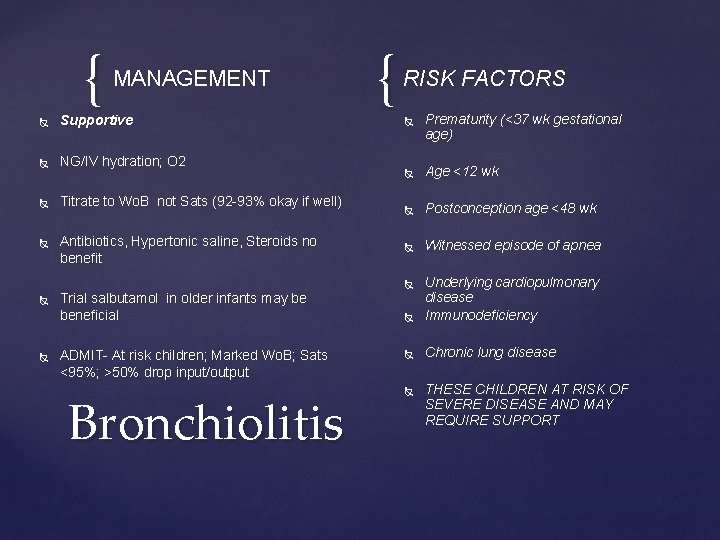
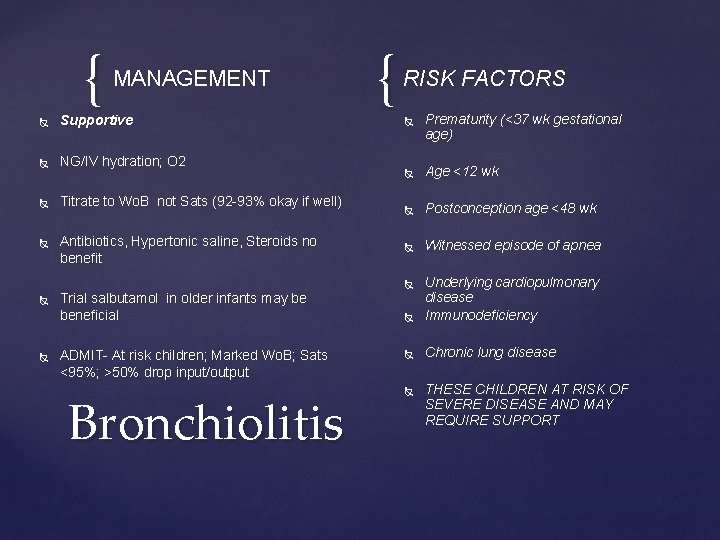
{ MANAGEMENT Supportive NG/IV hydration; O 2 Titrate to Wo. B not Sats (92 -93% okay if well) Antibiotics, Hypertonic saline, Steroids no benefit { RISK FACTORS Age <12 wk Postconception age <48 wk Witnessed episode of apnea Underlying cardiopulmonary disease Immunodeficiency Chronic lung disease Trial salbutamol in older infants may be beneficial ADMIT- At risk children; Marked Wo. B; Sats <95%; >50% drop input/output Bronchiolitis Prematurity (<37 wk gestational age) THESE CHILDREN AT RISK OF SEVERE DISEASE AND MAY REQUIRE SUPPORT
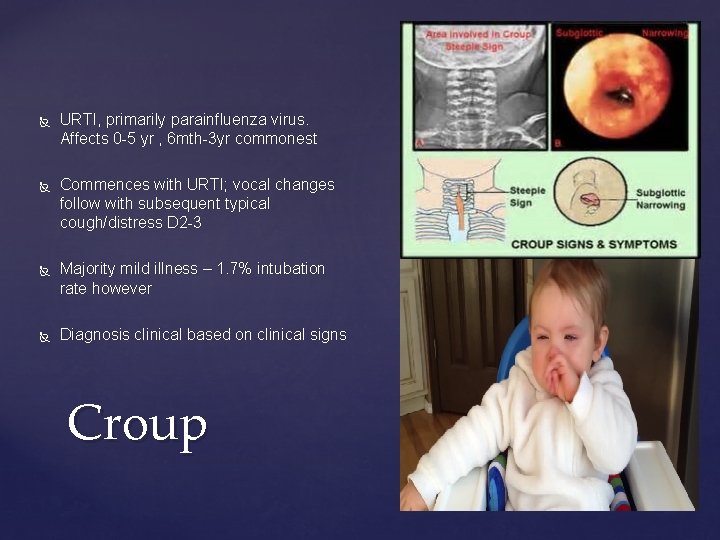
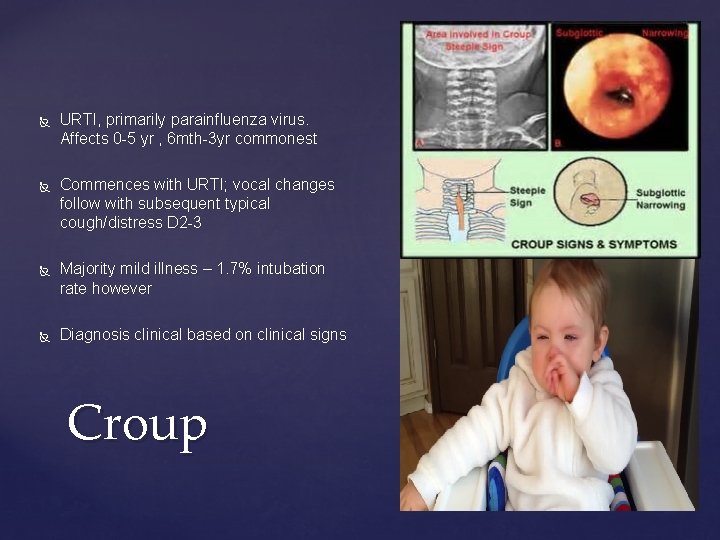
URTI, primarily parainfluenza virus. Affects 0 -5 yr , 6 mth-3 yr commonest Commences with URTI; vocal changes follow with subsequent typical cough/distress D 2 -3 Majority mild illness – 1. 7% intubation rate however Diagnosis clinical based on clinical signs Croup
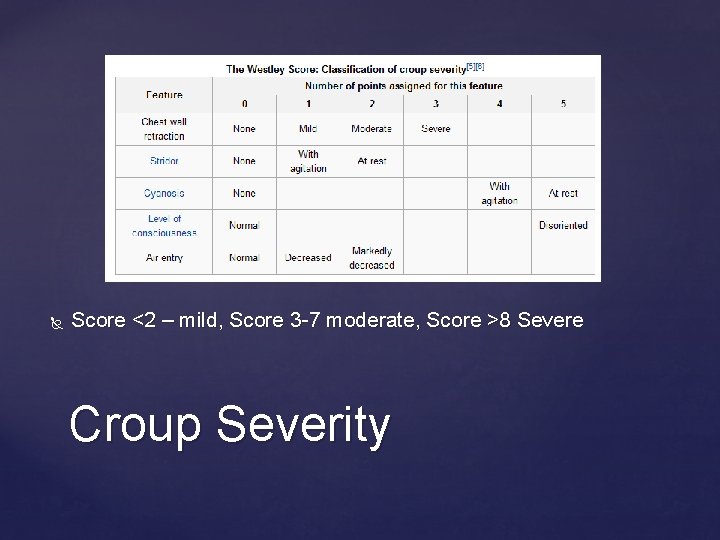
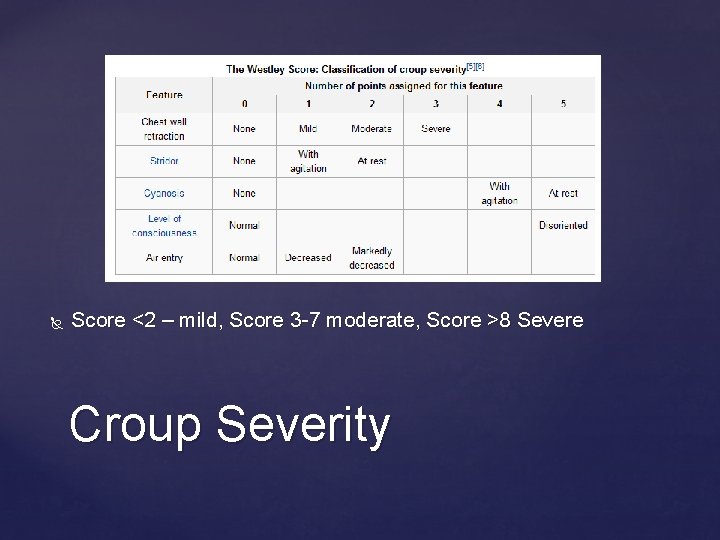
Score <2 – mild, Score 3 -7 moderate, Score >8 Severe Croup Severity
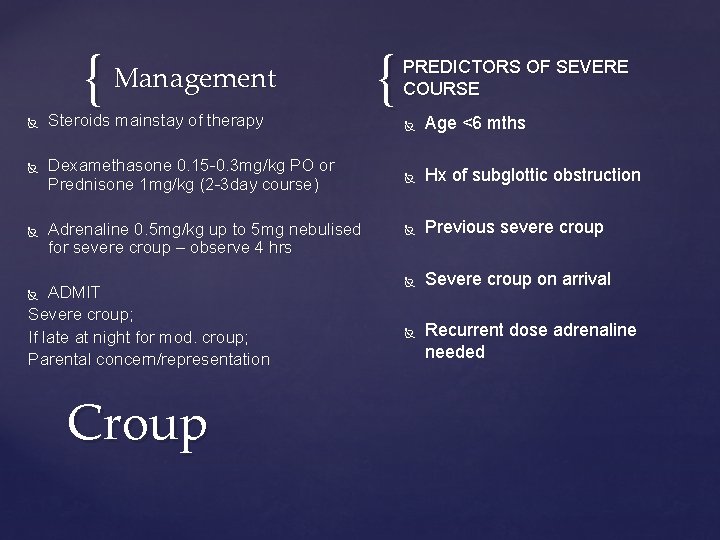
{ Management Steroids mainstay of therapy Dexamethasone 0. 15 -0. 3 mg/kg PO or Prednisone 1 mg/kg (2 -3 day course) Adrenaline 0. 5 mg/kg up to 5 mg nebulised for severe croup – observe 4 hrs ADMIT Severe croup; If late at night for mod. croup; Parental concern/representation { PREDICTORS OF SEVERE COURSE Age <6 mths Hx of subglottic obstruction Previous severe croup Severe croup on arrival Croup Recurrent dose adrenaline needed
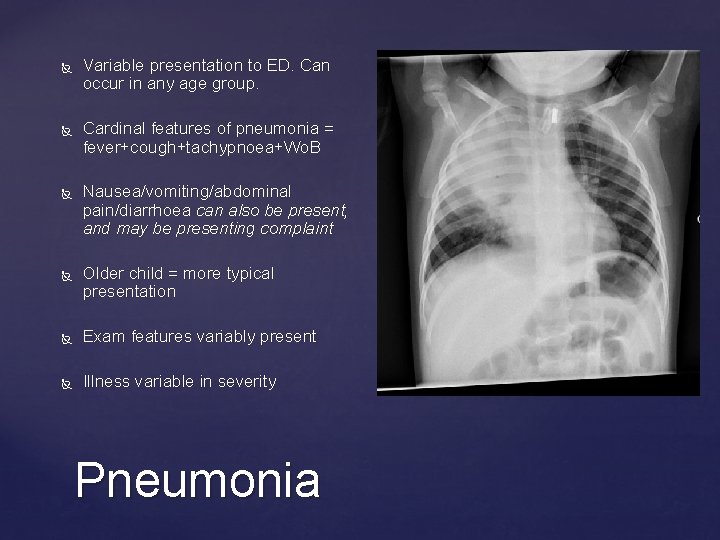
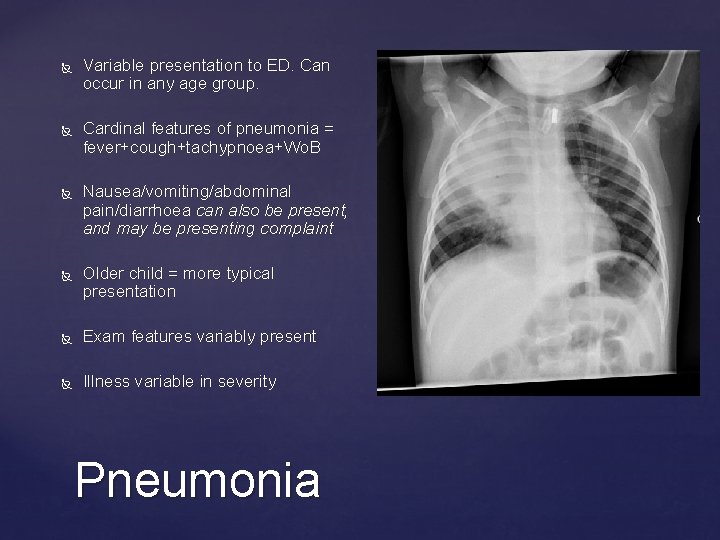
Variable presentation to ED. Can occur in any age group. Cardinal features of pneumonia = fever+cough+tachypnoea+Wo. B Nausea/vomiting/abdominal pain/diarrhoea can also be present, and may be presenting complaint Older child = more typical presentation Exam features variably present Illness variable in severity Pneumonia
State Guideline suggests use of SPOC for severity assessment Age <3 mths, Marked dehydration, Toxic appearance should guide management toward admission Pneumonia – Severity assessment
CXR – not always indicated! Consider if diagnosis unclear or pneumonia classed as moderate/severe or pleural effusion suspected or unresponsive to first line treatment Pathology – likewise limited utility in mild disease. Reserve for Mod-severe Blood culture - 10 -20% yield rate in mod-severe. Unlikely to change management, but may assist if Staph. Pneumonia Sputum culture – Younger children highly unlikely to have productive cough; however, older children may co-operate, but require good quality specimen NPA/Swabs – viral studies. May be some use in limiting therapy if positive for viral infection Pneumonia - Investigations
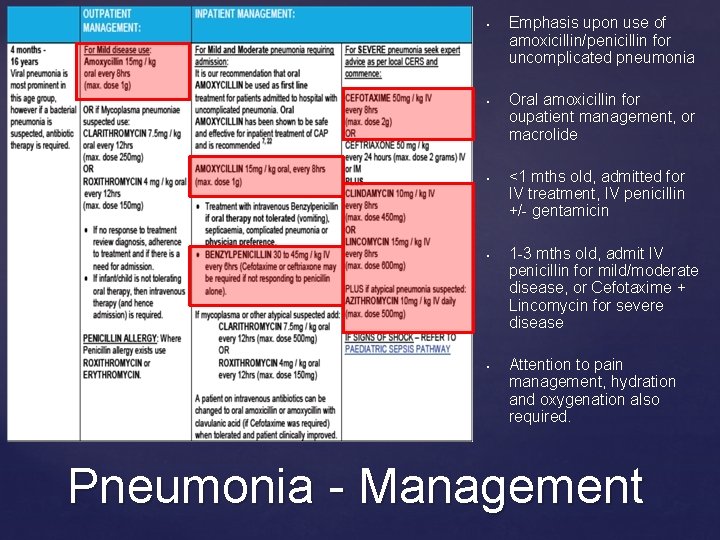
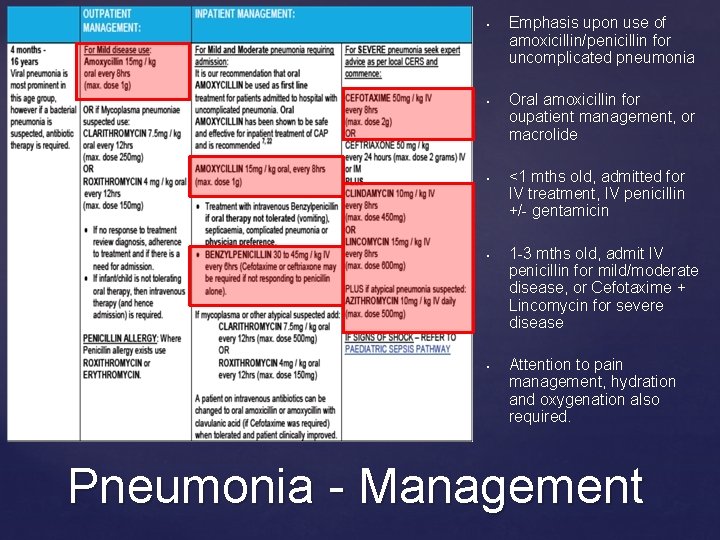
• • { • • • Emphasis upon use of amoxicillin/penicillin for uncomplicated pneumonia Oral amoxicillin for oupatient management, or macrolide <1 mths old, admitted for IV treatment, IV penicillin +/- gentamicin 1 -3 mths old, admit IV penicillin for mild/moderate disease, or Cefotaxime + Lincomycin for severe disease Attention to pain management, hydration and oxygenation also required. Pneumonia - Management
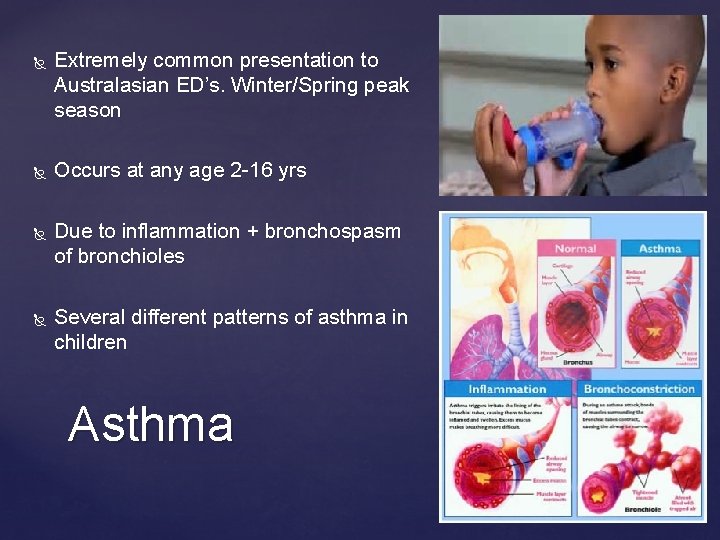
Extremely common presentation to Australasian ED’s. Winter/Spring peak season Occurs at any age 2 -16 yrs Due to inflammation + bronchospasm of bronchioles Several different patterns of asthma in children Asthma
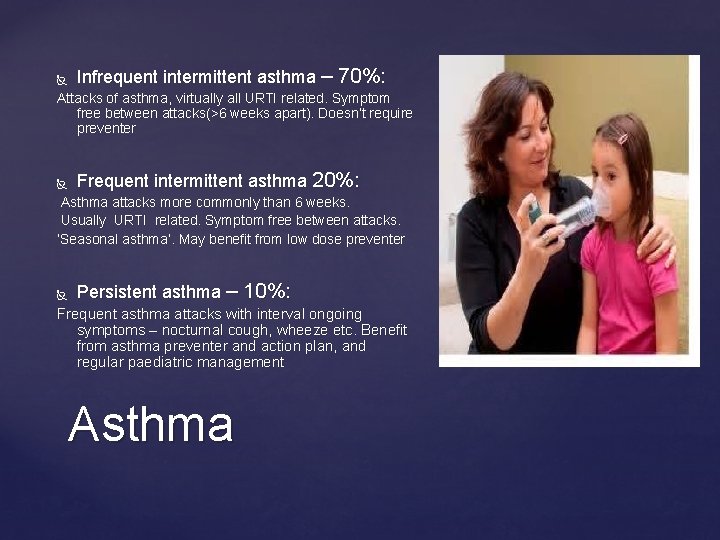
Infrequent intermittent asthma – 70%: Attacks of asthma, virtually all URTI related. Symptom free between attacks(>6 weeks apart). Doesn’t require preventer Frequent intermittent asthma 20%: Asthma attacks more commonly than 6 weeks. Usually URTI related. Symptom free between attacks. ‘Seasonal asthma’. May benefit from low dose preventer Persistent asthma – 10%: Frequent asthma attacks with interval ongoing symptoms – nocturnal cough, wheeze etc. Benefit from asthma preventer and action plan, and regular paediatric management Asthma
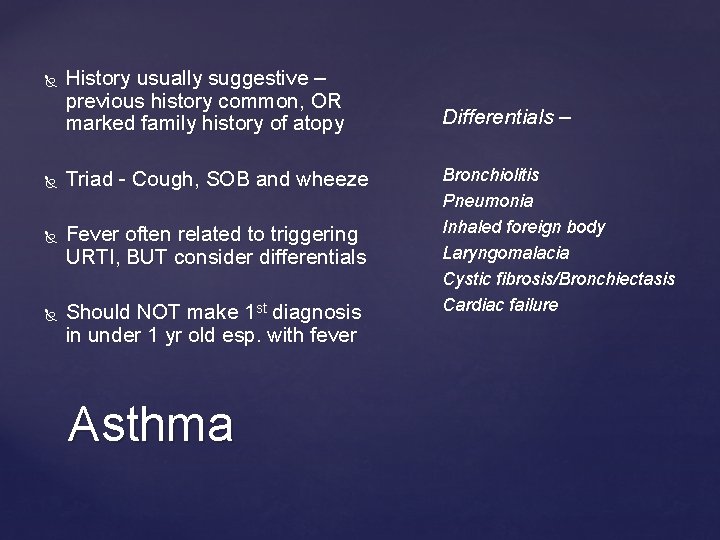
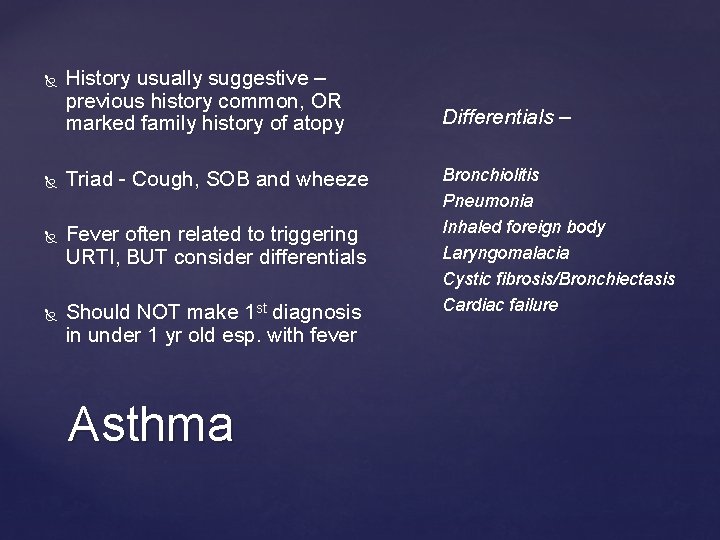
History usually suggestive – previous history common, OR marked family history of atopy Triad - Cough, SOB and wheeze Fever often related to triggering URTI, BUT consider differentials Should NOT make 1 st diagnosis in under 1 yr old esp. with fever Asthma Differentials – Bronchiolitis Pneumonia Inhaled foreign body Laryngomalacia Cystic fibrosis/Bronchiectasis Cardiac failure
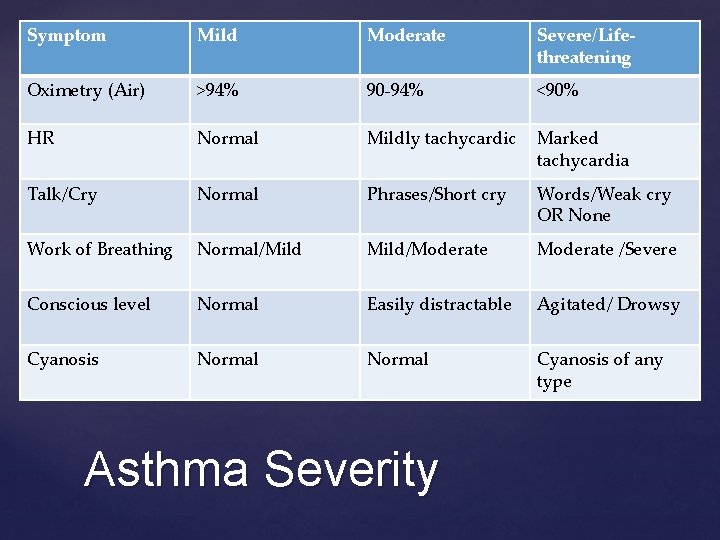
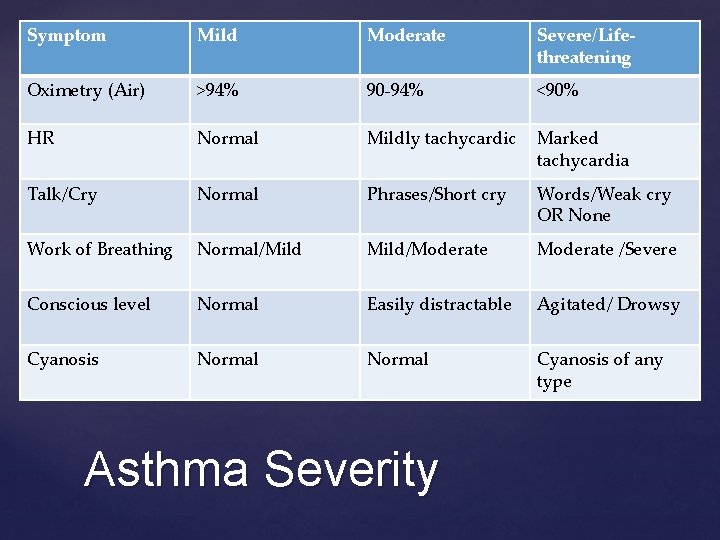
Symptom Mild Moderate Severe/Lifethreatening Oximetry (Air) >94% 90 -94% <90% HR Normal Mildly tachycardic Marked tachycardia Talk/Cry Normal Phrases/Short cry Words/Weak cry OR None Work of Breathing Normal/Mild/Moderate /Severe Conscious level Normal Easily distractable Agitated/ Drowsy Cyanosis Normal Cyanosis of any type Asthma Severity
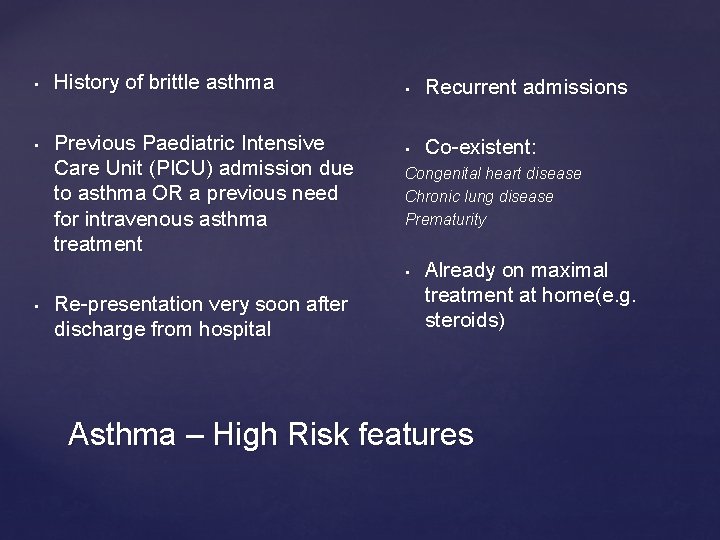
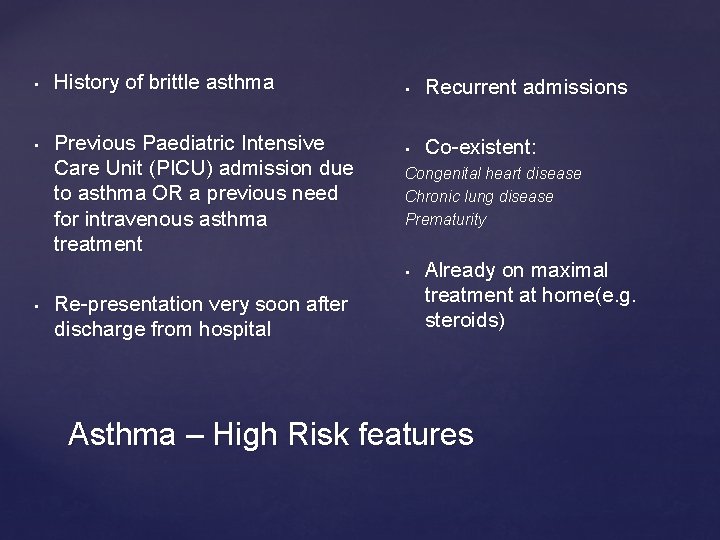
• • History of brittle asthma Previous Paediatric Intensive Care Unit (PICU) admission due to asthma OR a previous need for intravenous asthma treatment • Recurrent admissions • Co-existent: Congenital heart disease Chronic lung disease Prematurity • • Re-presentation very soon after discharge from hospital Already on maximal treatment at home(e. g. steroids) Asthma – High Risk features
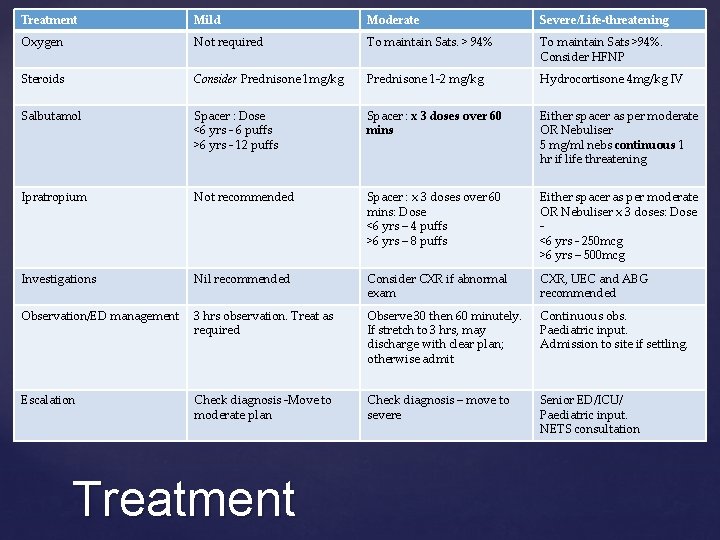
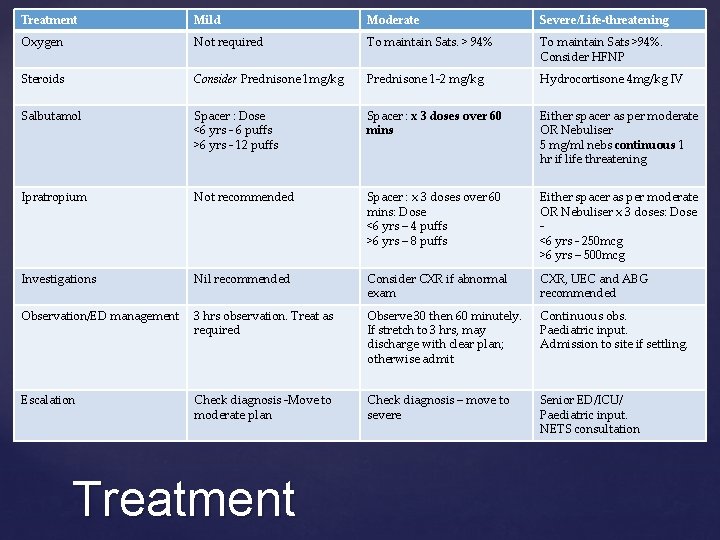
Treatment Mild Moderate Severe/Life-threatening Oxygen Not required To maintain Sats. > 94% To maintain Sats >94%. Consider HFNP Steroids Consider Prednisone 1 mg/kg Prednisone 1 -2 mg/kg Hydrocortisone 4 mg/kg IV Salbutamol Spacer : Dose <6 yrs - 6 puffs >6 yrs - 12 puffs Spacer : x 3 doses over 60 mins Either spacer as per moderate OR Nebuliser 5 mg/ml nebs continuous 1 hr if life threatening Ipratropium Not recommended Spacer : x 3 doses over 60 mins: Dose <6 yrs – 4 puffs >6 yrs – 8 puffs Either spacer as per moderate OR Nebuliser x 3 doses: Dose <6 yrs - 250 mcg >6 yrs – 500 mcg Investigations Nil recommended Consider CXR if abnormal exam CXR, UEC and ABG recommended Observation/ED management 3 hrs observation. Treat as required Observe 30 then 60 minutely. If stretch to 3 hrs, may discharge with clear plan; otherwise admit Continuous obs. Paediatric input. Admission to site if settling. Escalation Check diagnosis -Move to moderate plan Check diagnosis – move to severe Senior ED/ICU/ Paediatric input. NETS consultation Treatment
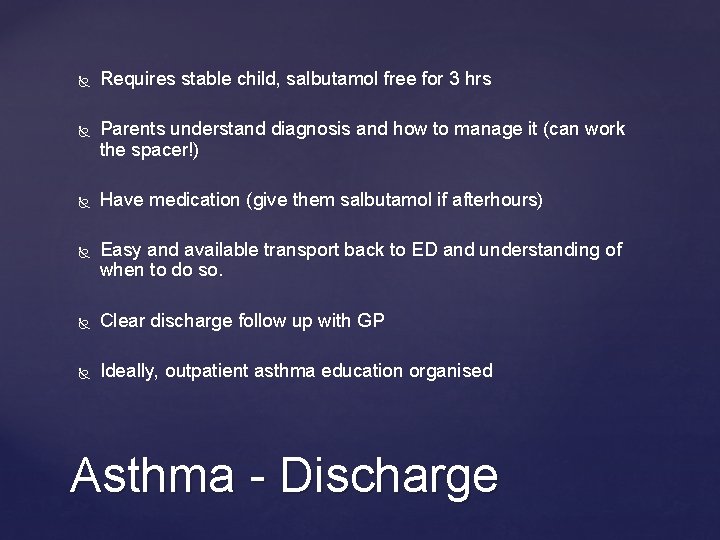
Requires stable child, salbutamol free for 3 hrs Parents understand diagnosis and how to manage it (can work the spacer!) Have medication (give them salbutamol if afterhours) Easy and available transport back to ED and understanding of when to do so. Clear discharge follow up with GP Ideally, outpatient asthma education organised Asthma - Discharge

Questions?
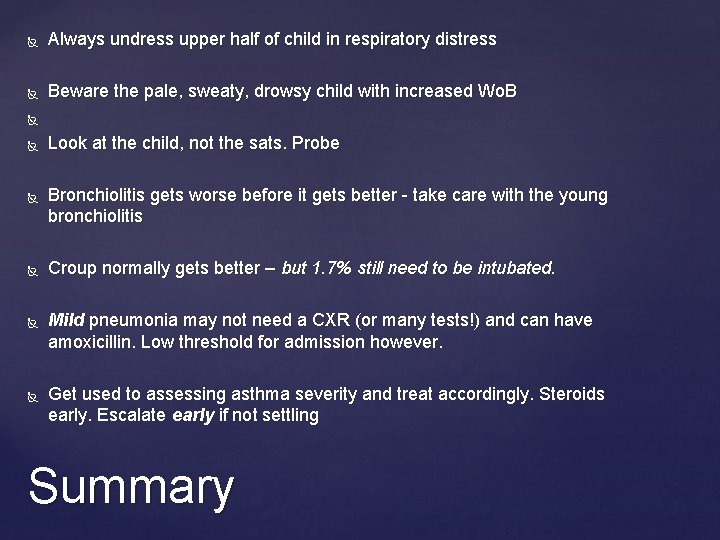
Always undress upper half of child in respiratory distress Beware the pale, sweaty, drowsy child with increased Wo. B Look at the child, not the sats. Probe Bronchiolitis gets worse before it gets better - take care with the young bronchiolitis Croup normally gets better – but 1. 7% still need to be intubated. Mild pneumonia may not need a CXR (or many tests!) and can have amoxicillin. Low threshold for admission however. Get used to assessing asthma severity and treat accordingly. Steroids early. Escalate early if not settling Summary
Thank you.
 Respiratory distress nasal flaring
Respiratory distress nasal flaring Respiratory distress
Respiratory distress Respiratory distress
Respiratory distress Paediatric respiratory history
Paediatric respiratory history Respiratory zone vs conducting zone
Respiratory zone vs conducting zone Suds scale thermometer
Suds scale thermometer Rapunzel damsel in distress
Rapunzel damsel in distress Message relay sample
Message relay sample Distress tolerance thermometer
Distress tolerance thermometer Seelonce mayday meaning
Seelonce mayday meaning Contoh distress
Contoh distress Pearlin theory
Pearlin theory Youtube.com
Youtube.com Financial distress costs
Financial distress costs Damsel in distress archetype examples
Damsel in distress archetype examples Half smile dbt
Half smile dbt Fetal distress definition
Fetal distress definition Distress signal x1
Distress signal x1 Moral distress and burnout
Moral distress and burnout Leonard pearlin's theory of psychological distress
Leonard pearlin's theory of psychological distress Sejarah psikologi klinis
Sejarah psikologi klinis Psychology, mental health and distress
Psychology, mental health and distress Eustress
Eustress Verbalisasi distress adalah
Verbalisasi distress adalah