PAEDIATRIC DELIRIUM A Paediatric Consultationliaison Psychiatry Presentation Rene



- Slides: 30

PAEDIATRIC DELIRIUM A Paediatric Consultation-liaison Psychiatry Presentation Rene Nassen Dr Sean Hatherill
“A non specific neuropsychiatric disorder that indicates global encephalopathic dysfunction in seriously ill patients” p Frequently seen in ill geriatrics and adults p Clinical picture well known in adults p Associated prognostic implications p Children - occurs commonly - often missed - seriousness underestimated p
Problems § Confusing Terminology – variety of terms used by different disciplines - ‘delirium’ , ‘acute confusional state’ , ‘acute organic brain syndrome’, ‘encephalopathy’ , ‘ICU psychosis’ , ‘cerebral insufficiency’ § Vague and longwinded psychiatric definitions – using terms like ‘clouding of consciousness’ , ‘reduced clarity of awareness of the environment’ § § Unhelpful lay and medical stereotypes Diagnostic difficulty- Underrecognised and undertreated Commonly misdiagnosed Fluctuating by nature
Yet More Problems § Relatively extensive adult delirium literature…. . but § Precious little child psych. / paediatric literature § Inherent risks of extrapolating from adult literature especially regarding treatment
This presentation Clinical picture-cases p Diagnostic features p Assessment p Management p Aetiology p Final thoughts p
The many faces of delirium p The ? Depression Referral p The ? PTSD Referral p The “Psychotic Child” Referral p The HIV+ Child
? Depression Referral 14 yr old girl on PD awaiting renal Tx, temporarily living at St Josephs p Very unhappy with St Josephs placement p Clear history of low mood , anhedonia, ideas of hopelessness and passive suicidality p Seemingly leading to non-compliance with treatment p Admitted in status epilepticus to ICU p On return to ward – withdrawn , apathetic , uncommunicative , ? depressed On MSE p Mood difficult to assess and clinical picture dominated by cognitive deficits p Distractable , difficulty attending to questions, disorientated for time , recent memory recall problems , difficulty focusing and shifting attention and problems with mental flexibility tasks p
? Depression Referral cont. p Diagnosis of Delirium On basis of further investigations and a previous history of autoimmune thyroiditis a further diagnosis of Hashimoto’s Encephalopathy made Good response to steroids Now requires the possibility of pre-delirium underlying depression explored. p TAKE HOME… p A DIAGNOSIS OF DELIRIUM IS ONLY THE START OF THE DIAGNOSTIC PROCESS p DELIRIUM CAN BOTH MIMIC AND COMPLICATE DEPRESSION p ANTIDEPRESSANTS CAN WORSEN DELIRIUM p p p
The ? PTSD Referral A 10 yr old girl Day 10 post MVA pedestrian with multiple injuries including significant head injury and # femur , now in traction § Nursing staff at wits end § Pulling off traction , trying to get off the bed § “won’t listen” , clingy , and difficult to console (even by mother) § Repeatedly shouting “I’m going home on Monday!” On MSE § Clearly distressed , agitated , not responding to repeated explanation and reassurance § Completely amnestic for injury itself. Vaguely fearful § No repeated nightmares , intrusive trauma imagery or flashbacks § Understands questions and can give reasonable replies § Lucid intervals interrupted by periods of great distress and inconsolability § Quite subtle deficits on bedside cognitive testing §
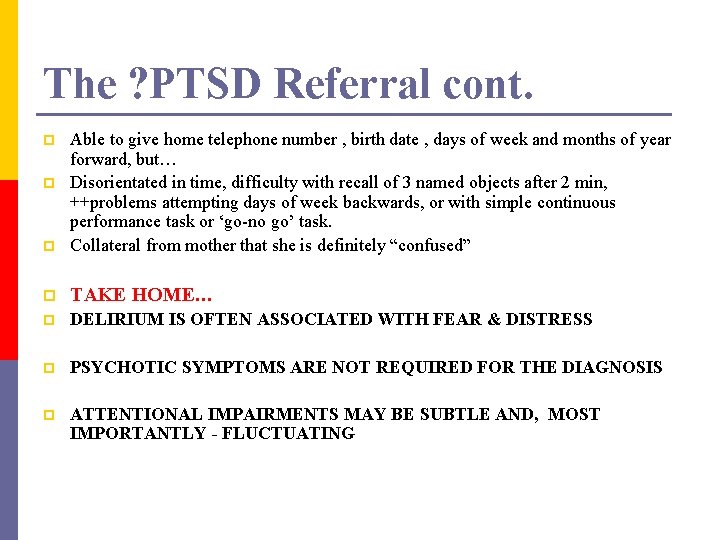
The ? PTSD Referral cont. p Able to give home telephone number , birth date , days of week and months of year forward, but… Disorientated in time, difficulty with recall of 3 named objects after 2 min, ++problems attempting days of week backwards, or with simple continuous performance task or ‘go-no go’ task. Collateral from mother that she is definitely “confused” p TAKE HOME… p DELIRIUM IS OFTEN ASSOCIATED WITH FEAR & DISTRESS p PSYCHOTIC SYMPTOMS ARE NOT REQUIRED FOR THE DIAGNOSIS p ATTENTIONAL IMPAIRMENTS MAY BE SUBTLE AND, MOST IMPORTANTLY - FLUCTUATING p p
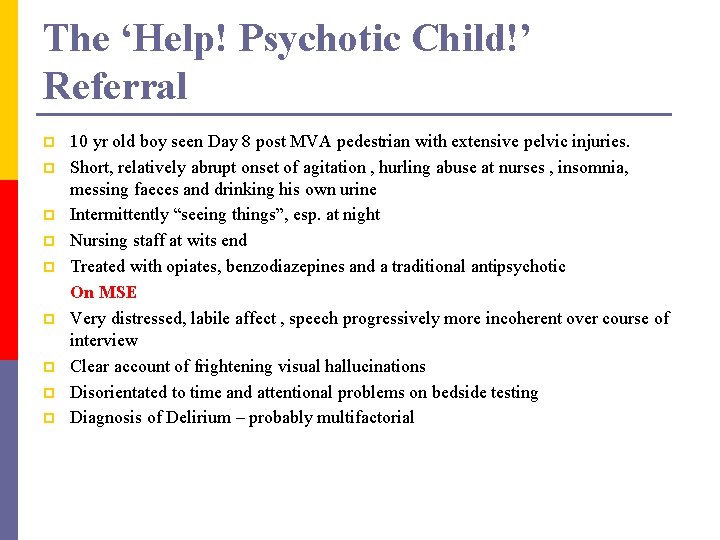
The ‘Help! Psychotic Child!’ Referral p p p p p 10 yr old boy seen Day 8 post MVA pedestrian with extensive pelvic injuries. Short, relatively abrupt onset of agitation , hurling abuse at nurses , insomnia, messing faeces and drinking his own urine Intermittently “seeing things”, esp. at night Nursing staff at wits end Treated with opiates, benzodiazepines and a traditional antipsychotic On MSE Very distressed, labile affect , speech progressively more incoherent over course of interview Clear account of frightening visual hallucinations Disorientated to time and attentional problems on bedside testing Diagnosis of Delirium – probably multifactorial
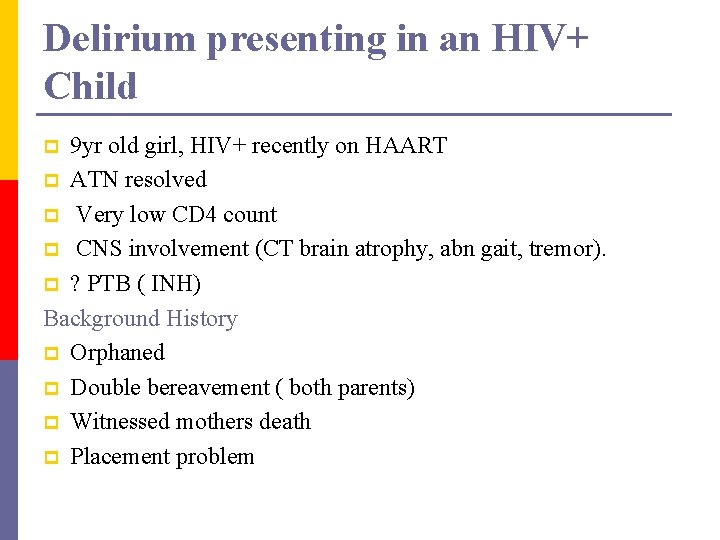
Delirium presenting in an HIV+ Child 9 yr old girl, HIV+ recently on HAART p ATN resolved p Very low CD 4 count p CNS involvement (CT brain atrophy, abn gait, tremor). p ? PTB ( INH) Background History p Orphaned p Double bereavement ( both parents) p Witnessed mothers death p Placement problem p
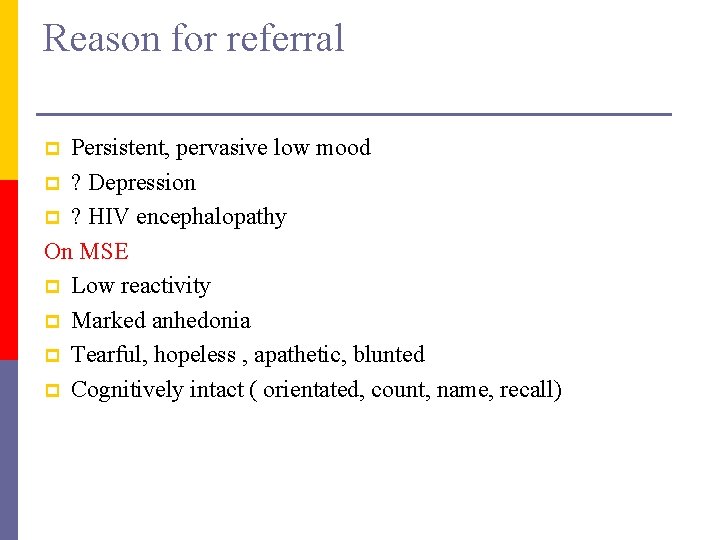
Reason for referral Persistent, pervasive low mood p ? Depression p ? HIV encephalopathy On MSE p Low reactivity p Marked anhedonia p Tearful, hopeless , apathetic, blunted p Cognitively intact ( orientated, count, name, recall) p
Diagnostically Major depressive episode p Complicated bereavement p ? ? ? PTSD p ? ? HIV encephalopathy Management p Fluoxetine 5 mg daily p EEG p 2 x weekly counselling, collateral school, liaise with social worker p
Clinical course Fluoxetine stopped, imipramine started. p Deterioration- labile mood, agitated - Hallucinations - Thought disordered p Fluctuating picture ( worse at night) On MSE: p Agitated, tearful, actively hallucinating, speech incoherent p Cognitively impaired (orientation, attention, memory, calculation) p
p Assessment: Delirium p ? Cause- Fluoxetine vs Imipramine - INH psychosis - initial presentation hypoactive delirium? - ? ? ? Immune reconstitution syndrome? p Management: low dose haloperidol * Settled after 10 days Placed at St Josephs Home
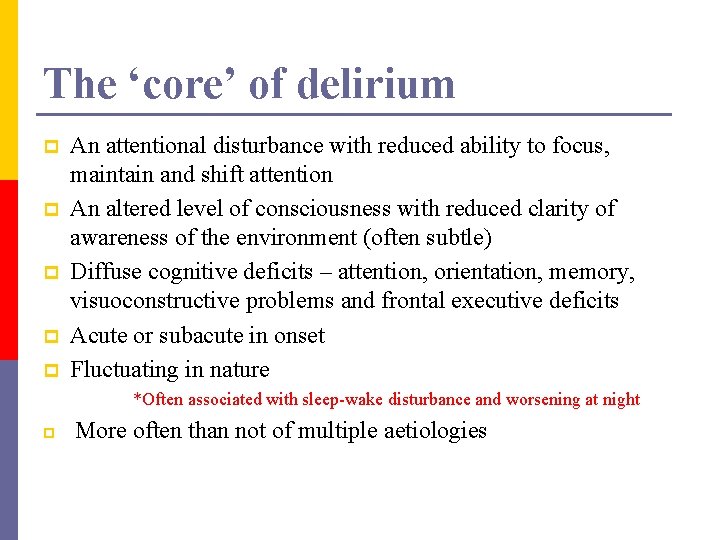
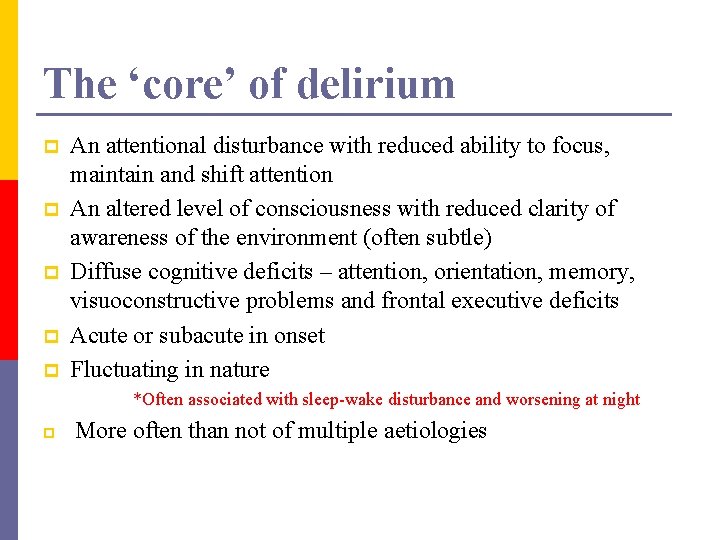
The ‘core’ of delirium p p p An attentional disturbance with reduced ability to focus, maintain and shift attention An altered level of consciousness with reduced clarity of awareness of the environment (often subtle) Diffuse cognitive deficits – attention, orientation, memory, visuoconstructive problems and frontal executive deficits Acute or subacute in onset Fluctuating in nature *Often associated with sleep-wake disturbance and worsening at night p More often than not of multiple aetiologies
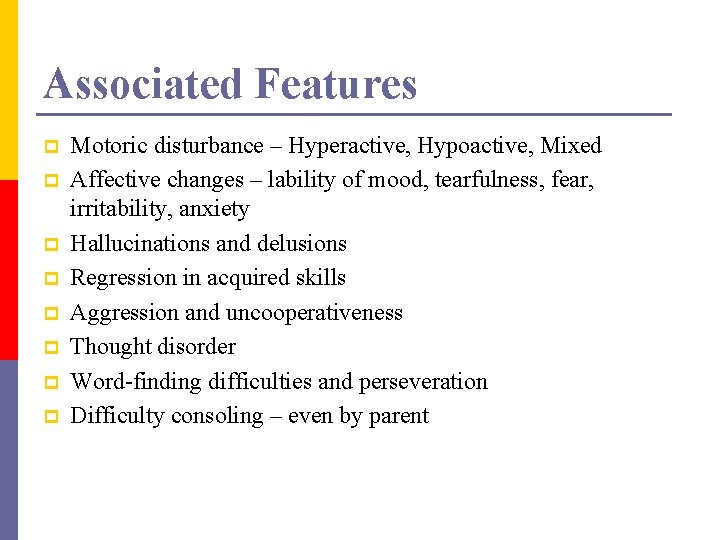
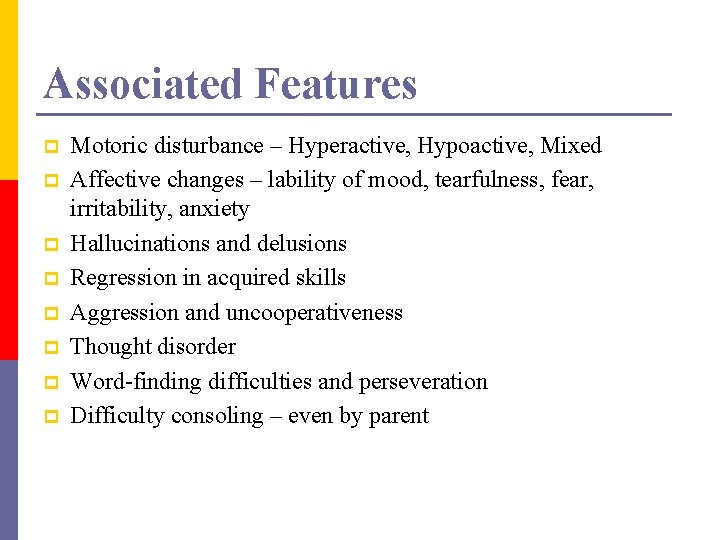
Associated Features p p p p Motoric disturbance – Hyperactive, Hypoactive, Mixed Affective changes – lability of mood, tearfulness, fear, irritability, anxiety Hallucinations and delusions Regression in acquired skills Aggression and uncooperativeness Thought disorder Word-finding difficulties and perseveration Difficulty consoling – even by parent
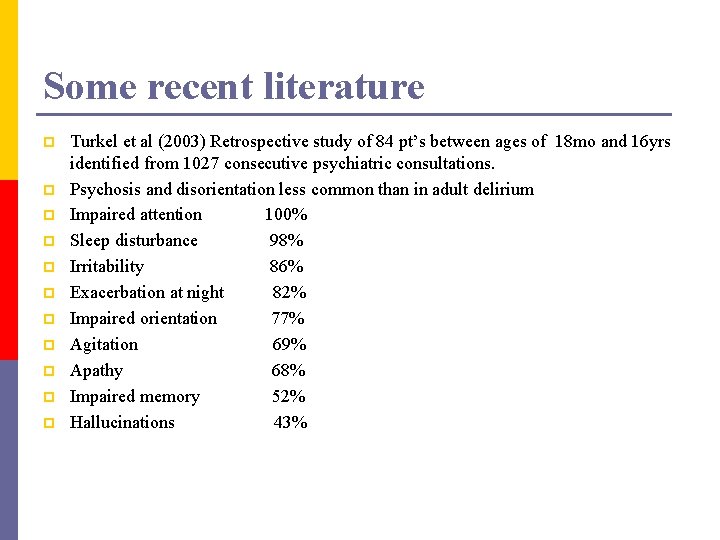
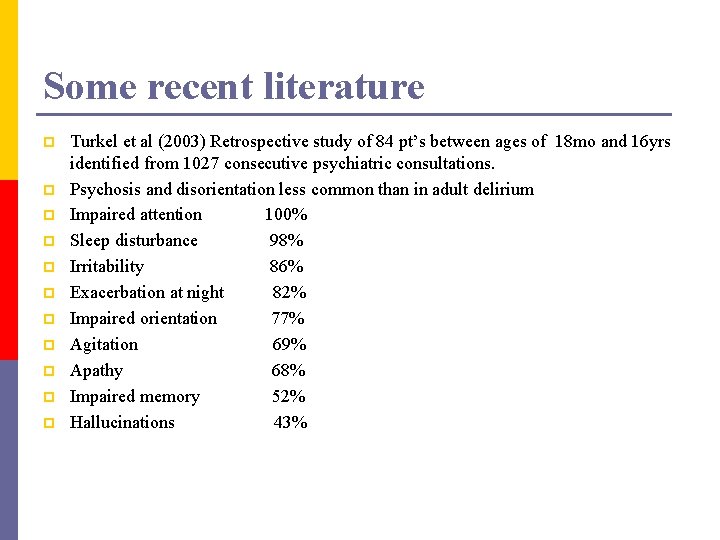
Some recent literature p p p Turkel et al (2003) Retrospective study of 84 pt’s between ages of 18 mo and 16 yrs identified from 1027 consecutive psychiatric consultations. Psychosis and disorientation less common than in adult delirium Impaired attention 100% Sleep disturbance 98% Irritability 86% Exacerbation at night 82% Impaired orientation 77% Agitation 69% Apathy 68% Impaired memory 52% Hallucinations 43%
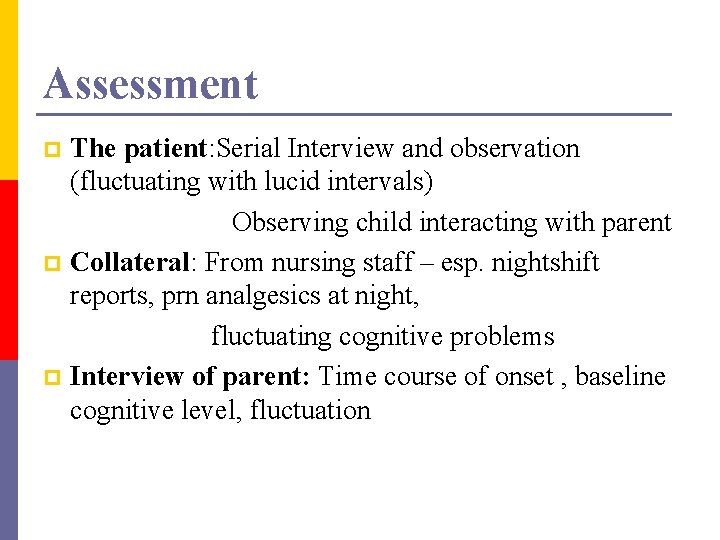
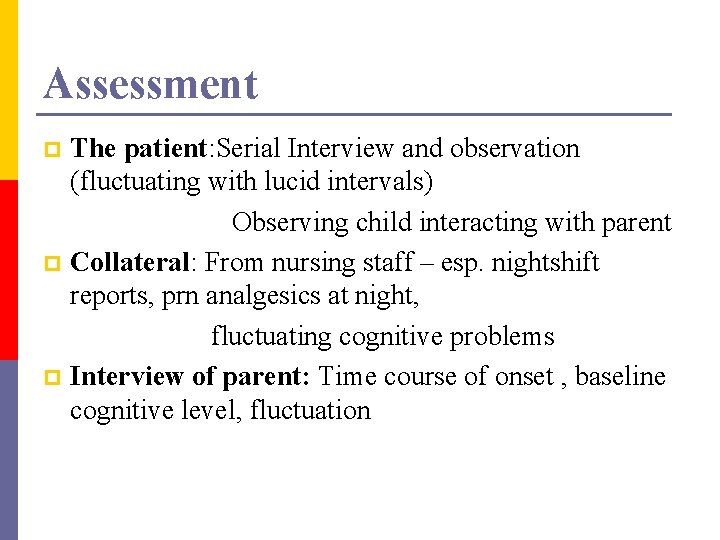
Assessment The patient: Serial Interview and observation (fluctuating with lucid intervals) Observing child interacting with parent p Collateral: From nursing staff – esp. nightshift reports, prn analgesics at night, fluctuating cognitive problems p Interview of parent: Time course of onset , baseline cognitive level, fluctuation p
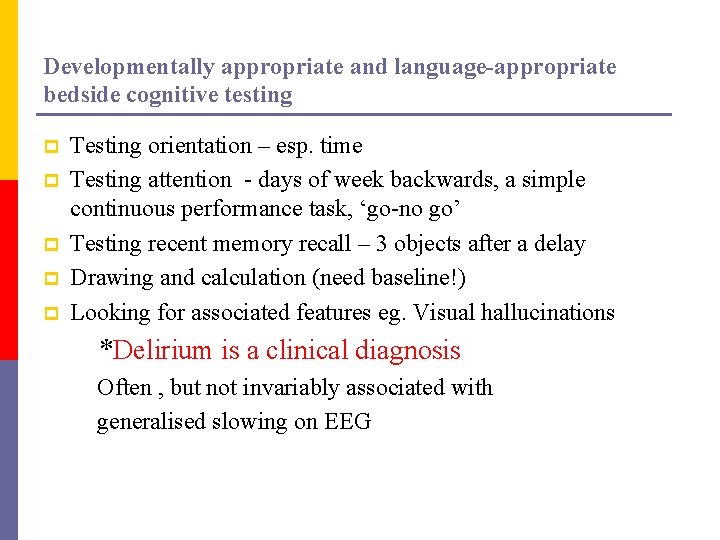
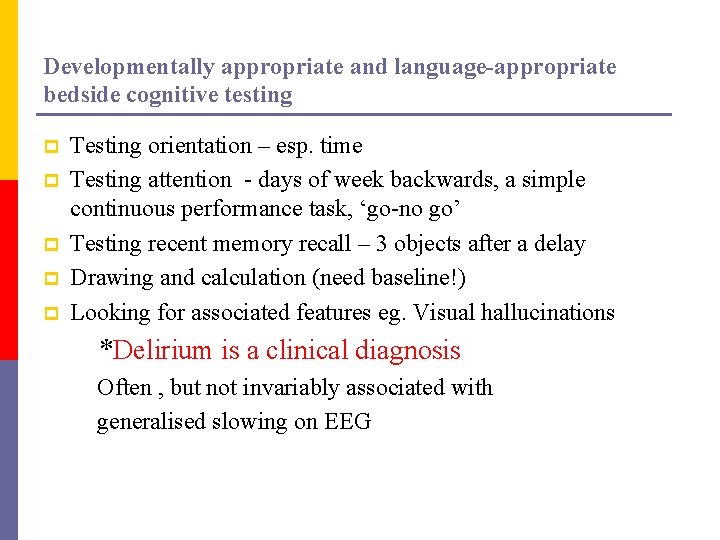
Developmentally appropriate and language-appropriate bedside cognitive testing p p p Testing orientation – esp. time Testing attention - days of week backwards, a simple continuous performance task, ‘go-no go’ Testing recent memory recall – 3 objects after a delay Drawing and calculation (need baseline!) Looking for associated features eg. Visual hallucinations *Delirium is a clinical diagnosis Often , but not invariably associated with generalised slowing on EEG
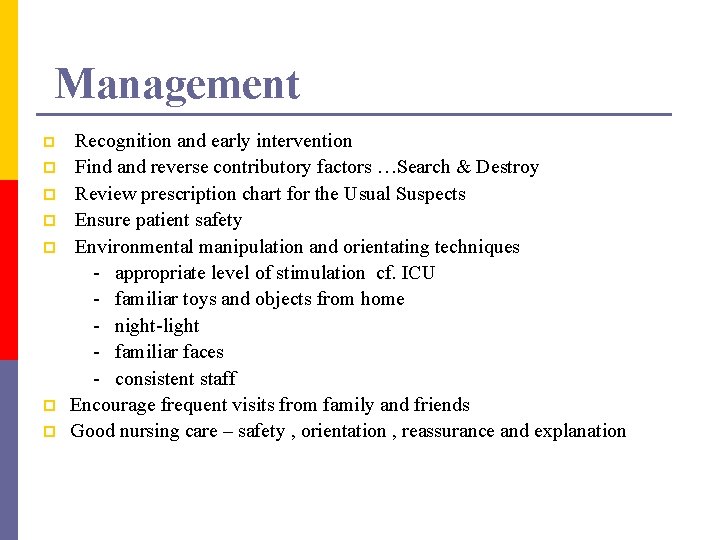
Management p p p p Recognition and early intervention Find and reverse contributory factors …Search & Destroy Review prescription chart for the Usual Suspects Ensure patient safety Environmental manipulation and orientating techniques - appropriate level of stimulation cf. ICU - familiar toys and objects from home - night-light - familiar faces - consistent staff Encourage frequent visits from family and friends Good nursing care – safety , orientation , reassurance and explanation

Assessment and Management (cont. ) p p p Monitor hydration (esp. in hypoactive delirium) Control fever Pain control USE AS FEW MEDICATIONS AS POSSIBLE PSYCHOTROPIC MEDICATION - No placebo-controlled trial data available - No FDA-approved medication specifically for delirium - Limited data to a great extent extrapolated from adults - May themselves worsen or cause delirium - Significant risks and side-effects - Cautious individualised risk – benefit analysis
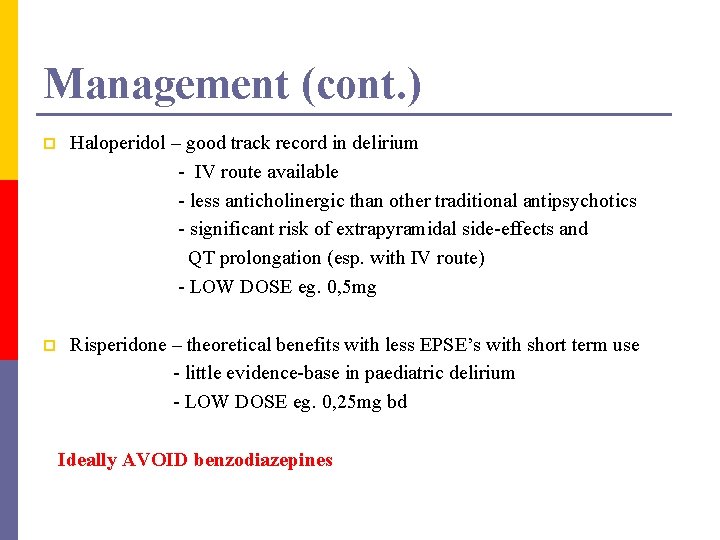
Management (cont. ) p Haloperidol – good track record in delirium - IV route available - less anticholinergic than other traditional antipsychotics - significant risk of extrapyramidal side-effects and QT prolongation (esp. with IV route) - LOW DOSE eg. 0, 5 mg p Risperidone – theoretical benefits with less EPSE’s with short term use - little evidence-base in paediatric delirium - LOW DOSE eg. 0, 25 mg bd Ideally AVOID benzodiazepines
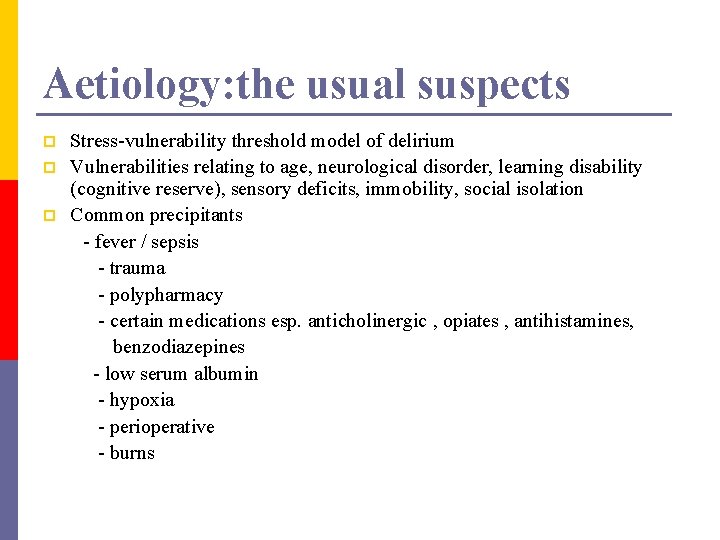
Aetiology: the usual suspects p p p Stress-vulnerability threshold model of delirium Vulnerabilities relating to age, neurological disorder, learning disability (cognitive reserve), sensory deficits, immobility, social isolation Common precipitants - fever / sepsis - trauma - polypharmacy - certain medications esp. anticholinergic , opiates , antihistamines, benzodiazepines - low serum albumin - hypoxia - perioperative - burns

I WATCH DEATH p p p I nfection W ithdrawal A cute metabolic T rauma & burns C NS pathology H ypoxia D eficiency eg. Thiamine E ndocrine A cute vascular T oxins and drugs H eavy metals
Unusual suspects p Tune et al , American J of Psychiatry 149 , 1393 – 1394, 1992 Measures of anticholinergic activity in ‘atropine-equivalents’ Digoxin Cimetedine Codeine Nifedipine (And obviously the tricyclic antidepressants)
Final take home Delirium contributes to significantly increased morbidity p The literature suggests we are missing it a lot of the time p Our prescribing practice can have a significant impact p Delirium comes in many shades and forms p Delirium can mimic most psychiatric diagnoses p It’s main mode of treatment is reversal of cause p Multiple aetiology is most common p
References p p p Schieveld et al , (2005) Delirium in Severely Ill Children in the Pediatric Intensive Care Unit. J. Am. Acad. Child Adolesc. Psychiatry , 44: 4, April 2005 Turkel et al , (2003) Delirium in Children and Adolescents , J. Neuropsychiatry Clin. Neuroscience 15: 4, 2003 Turkel et al , (2003) The Delirium Rating Scale in Children and Adolescents. Psychosomatics 44: 2 2003 Martini RD, (2005) The Diagnosis of Delirium in Pediatric Patients. J. Am. Acad. Child Adolesc. Psychiatry 44: 4 2005 Tune et al (1992) Am. J. Psychiatry 149, 1393 - 1394
Thank you
 Delirium case presentation
Delirium case presentation Acute confusion related to
Acute confusion related to Lucie big delirium
Lucie big delirium Flocculation delirium
Flocculation delirium Terminalt delirium
Terminalt delirium Delirium definition
Delirium definition Difference between dementia and delirium
Difference between dementia and delirium Francisco fernandez md
Francisco fernandez md Escala cam delirium
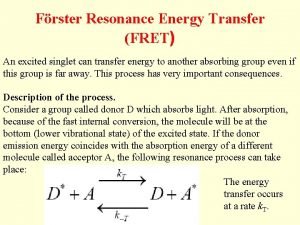
Escala cam delirium Energy transfer theory
Energy transfer theory Dr rose dinda martini
Dr rose dinda martini Types of amnesia
Types of amnesia Tingkat kesadaran gcs
Tingkat kesadaran gcs Delirium care pathways
Delirium care pathways Escala rass
Escala rass Nash delirium
Nash delirium European delirium association
European delirium association Core psychiatry
Core psychiatry Addiction expert witnesses
Addiction expert witnesses Forensic psychiatry vs forensic psychology
Forensic psychiatry vs forensic psychology Global initiative on psychiatry
Global initiative on psychiatry Psychiatry in ethiopia
Psychiatry in ethiopia Radical psychiatry sociology
Radical psychiatry sociology National network of child psychiatry access programs
National network of child psychiatry access programs National network of child psychiatry access programs
National network of child psychiatry access programs Mse speech
Mse speech Jamaica hospital psychiatry residency
Jamaica hospital psychiatry residency Mood mse
Mood mse Community geriatric psychiatry
Community geriatric psychiatry Asclepiades father of psychiatry
Asclepiades father of psychiatry Neurology shelf exam percentiles 2021
Neurology shelf exam percentiles 2021