Delirium Vicki Kijewski M D vickikijewskiuiowa edu Delirium

- Slides: 36
Delirium Vicki Kijewski, M. D. vicki-kijewski@uiowa. edu
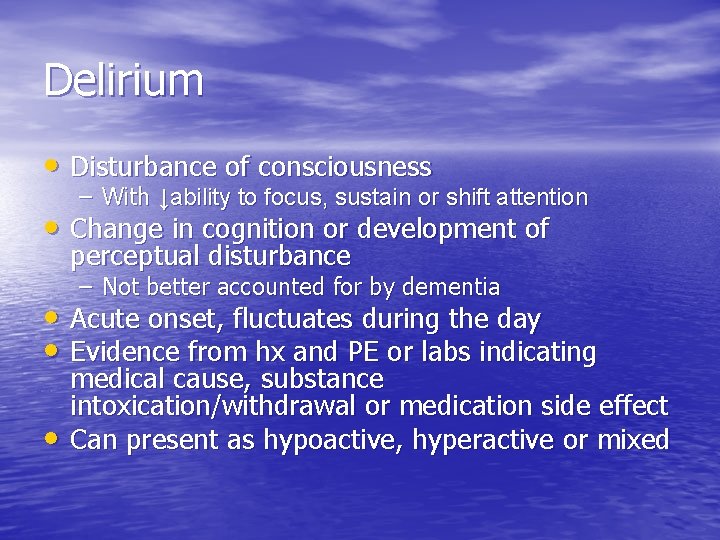
Delirium • Disturbance of consciousness – With ↓ability to focus, sustain or shift attention • Change in cognition or development of perceptual disturbance – Not better accounted for by dementia • Acute onset, fluctuates during the day • Evidence from hx and PE or labs indicating • medical cause, substance intoxication/withdrawal or medication side effect Can present as hypoactive, hyperactive or mixed
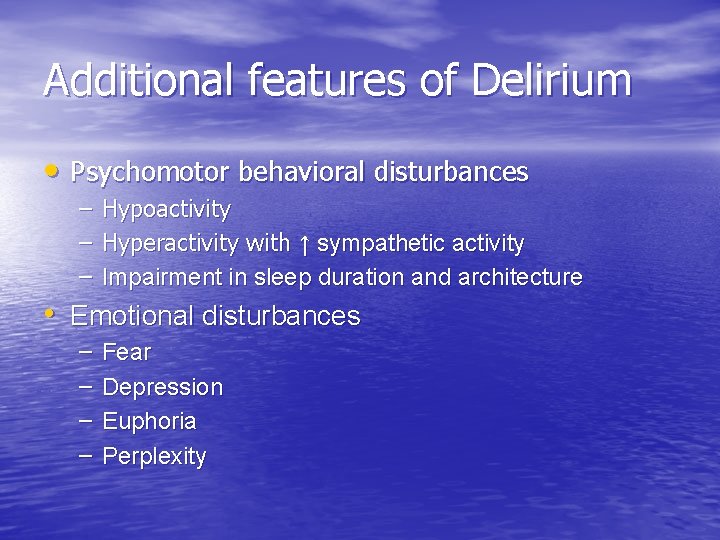
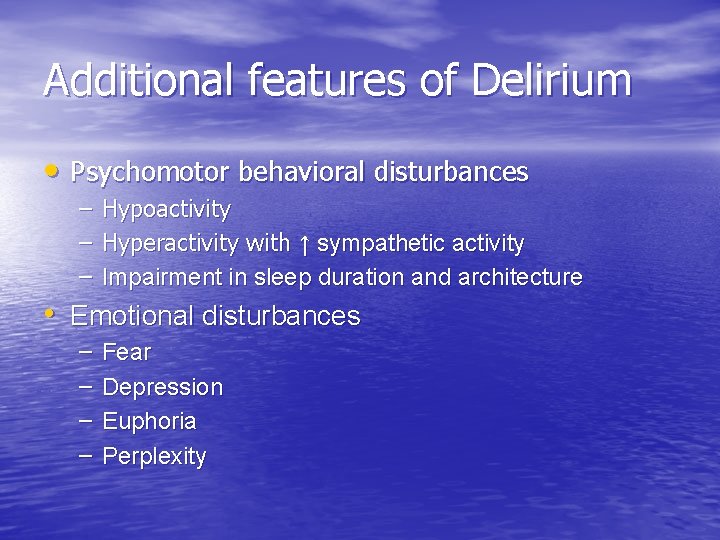
Additional features of Delirium • Psychomotor behavioral disturbances – Hypoactivity – Hyperactivity with ↑ sympathetic activity – Impairment in sleep duration and architecture • Emotional disturbances – – Fear Depression Euphoria Perplexity
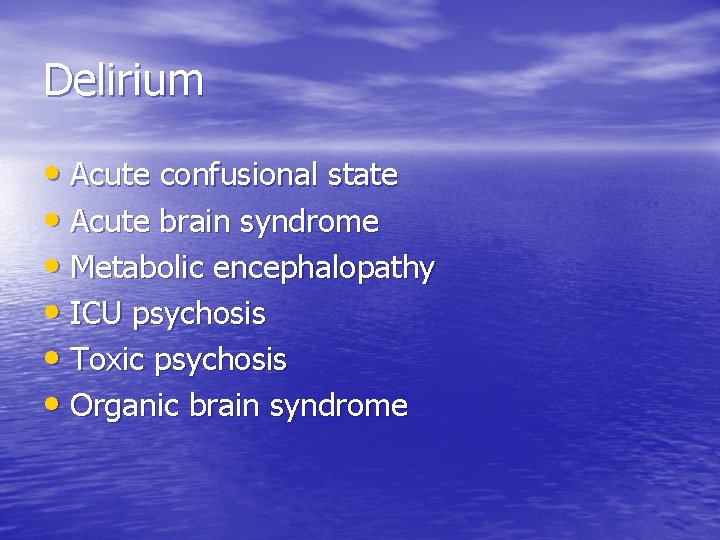
Delirium • Acute confusional state • Acute brain syndrome • Metabolic encephalopathy • ICU psychosis • Toxic psychosis • Organic brain syndrome
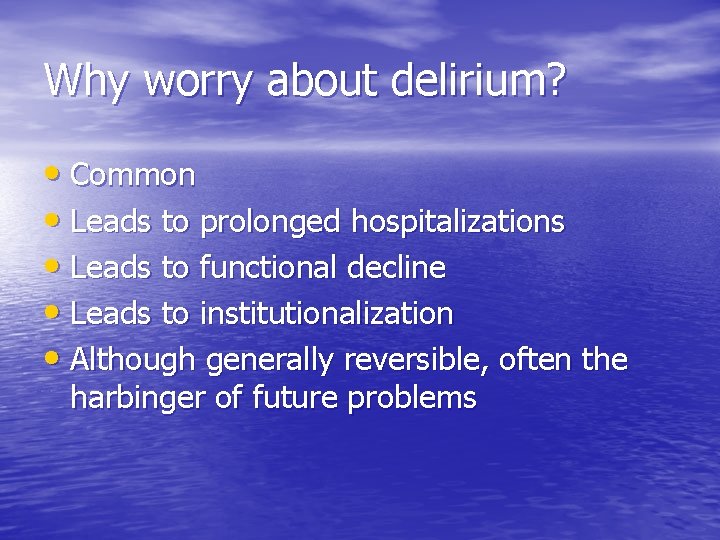
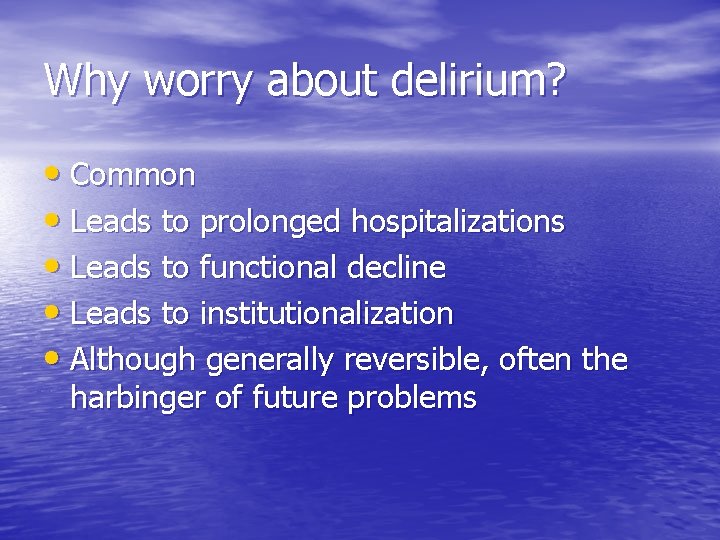
Why worry about delirium? • Common • Leads to prolonged hospitalizations • Leads to functional decline • Leads to institutionalization • Although generally reversible, often the harbinger of future problems
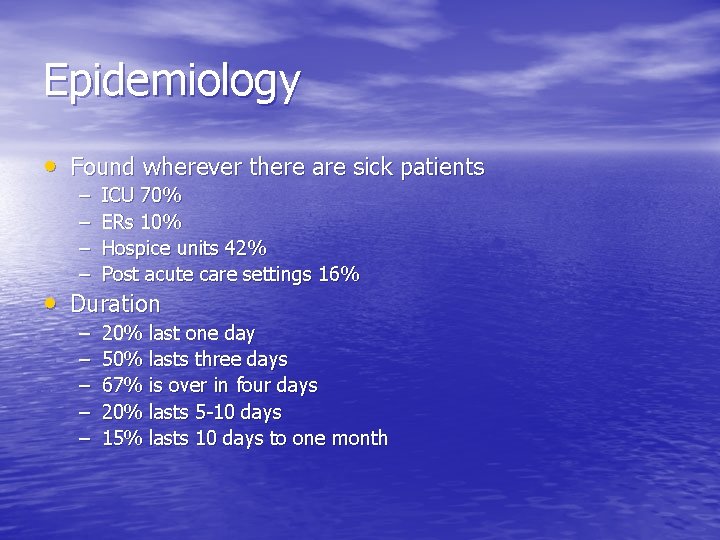
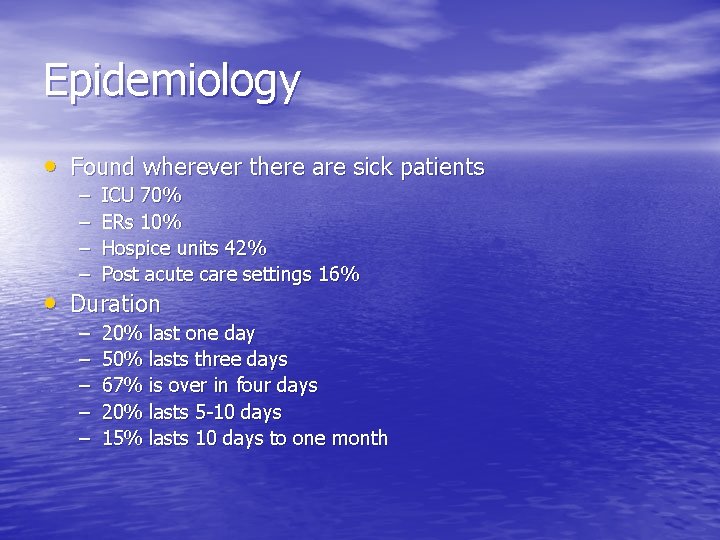
Epidemiology • Found wherever there are sick patients – – ICU 70% ERs 10% Hospice units 42% Post acute care settings 16% – – – 20% last one day 50% lasts three days 67% is over in four days 20% lasts 5 -10 days 15% lasts 10 days to one month • Duration
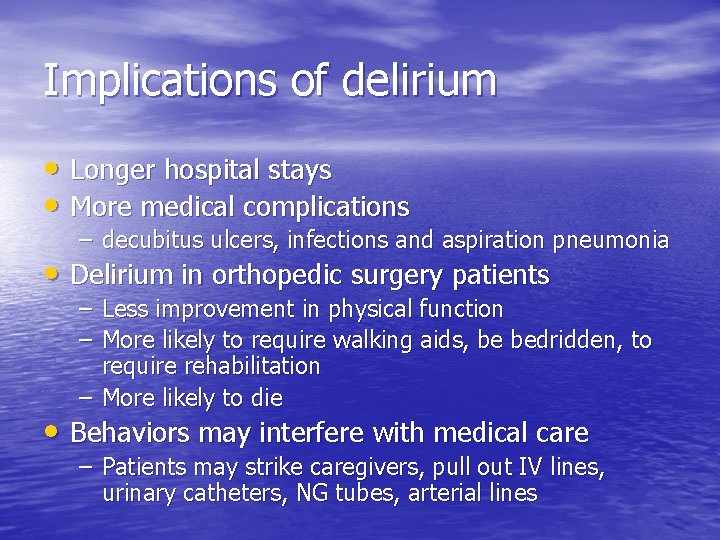
Implications of delirium • Longer hospital stays • More medical complications – decubitus ulcers, infections and aspiration pneumonia • Delirium in orthopedic surgery patients – Less improvement in physical function – More likely to require walking aids, be bedridden, to require rehabilitation – More likely to die • Behaviors may interfere with medical care – Patients may strike caregivers, pull out IV lines, urinary catheters, NG tubes, arterial lines
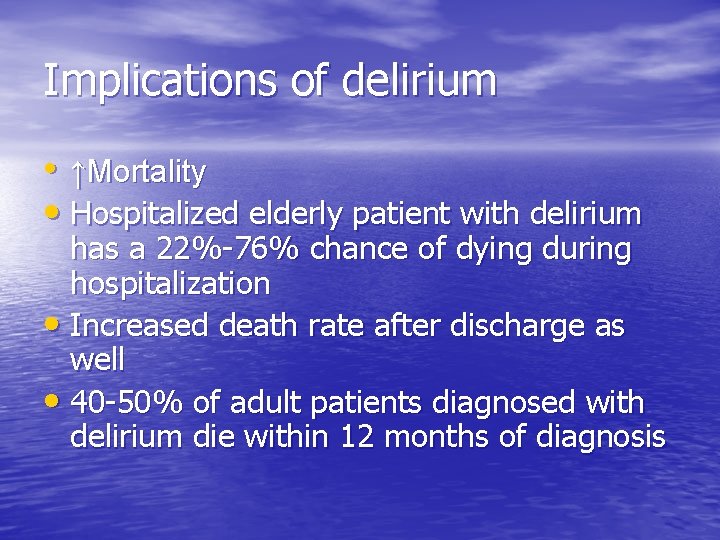
Implications of delirium • ↑Mortality • Hospitalized elderly patient with delirium has a 22%-76% chance of dying during hospitalization • Increased death rate after discharge as well • 40 -50% of adult patients diagnosed with delirium die within 12 months of diagnosis
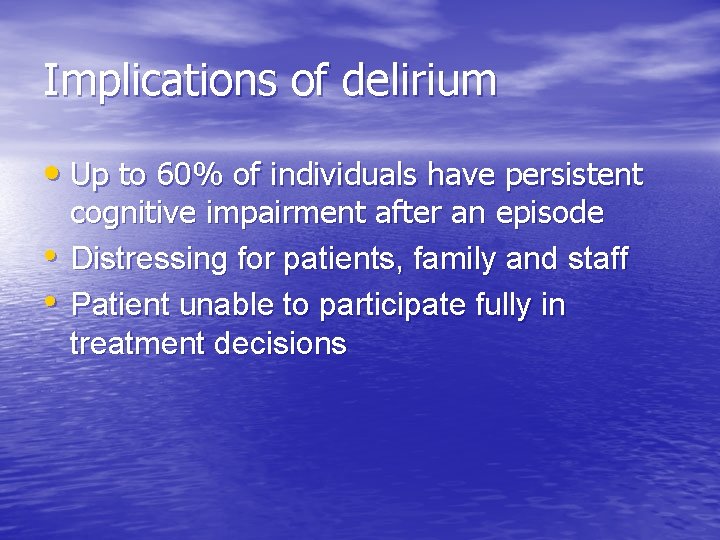
Implications of delirium • Up to 60% of individuals have persistent • • cognitive impairment after an episode Distressing for patients, family and staff Patient unable to participate fully in treatment decisions
Pathogenesis • Poorly understood • Underlying medical conditions • Medications • Drug/Alcohol Withdrawal • Substance Intoxication
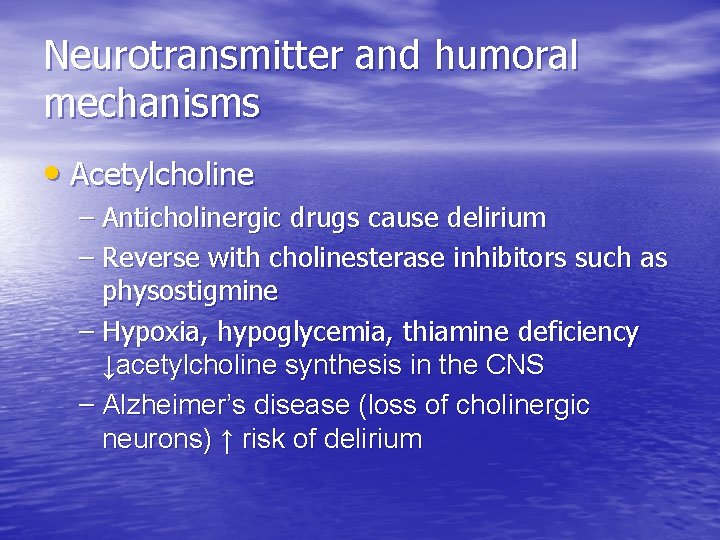
Neurotransmitter and humoral mechanisms • Acetylcholine – Anticholinergic drugs cause delirium – Reverse with cholinesterase inhibitors such as physostigmine – Hypoxia, hypoglycemia, thiamine deficiency ↓acetylcholine synthesis in the CNS – Alzheimer’s disease (loss of cholinergic neurons) ↑ risk of delirium
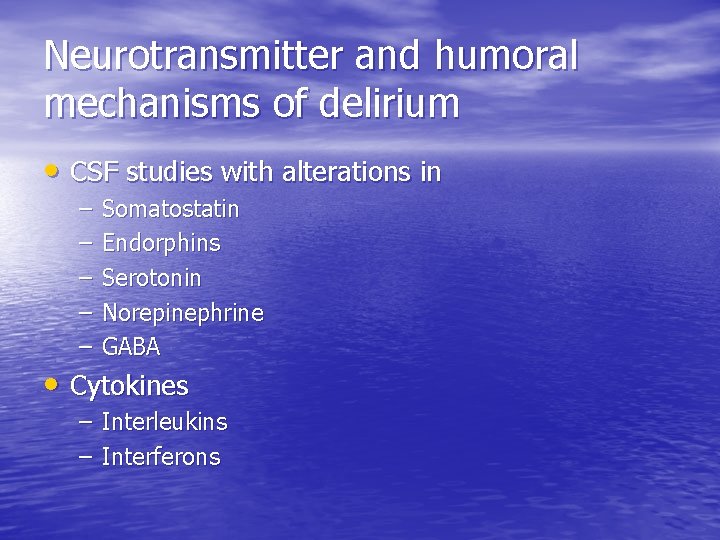
Neurotransmitter and humoral mechanisms of delirium • CSF studies with alterations in – – – Somatostatin Endorphins Serotonin Norepinephrine GABA • Cytokines – Interleukins – Interferons
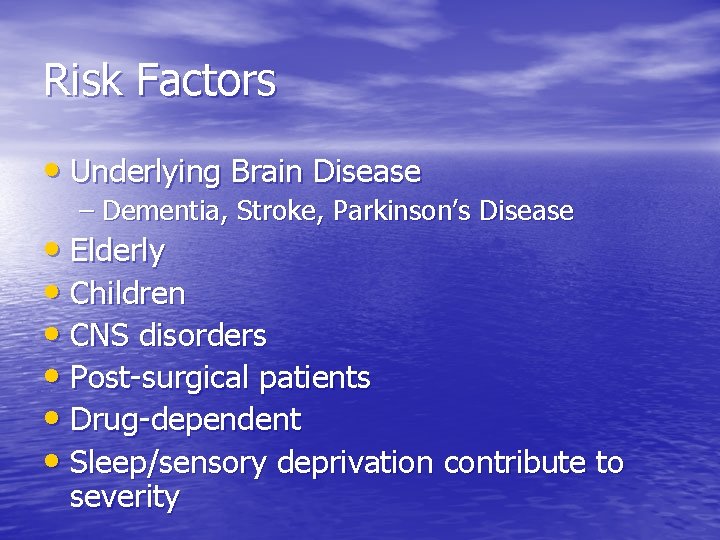
Risk Factors • Underlying Brain Disease – Dementia, Stroke, Parkinson’s Disease • Elderly • Children • CNS disorders • Post-surgical patients • Drug-dependent • Sleep/sensory deprivation contribute to severity
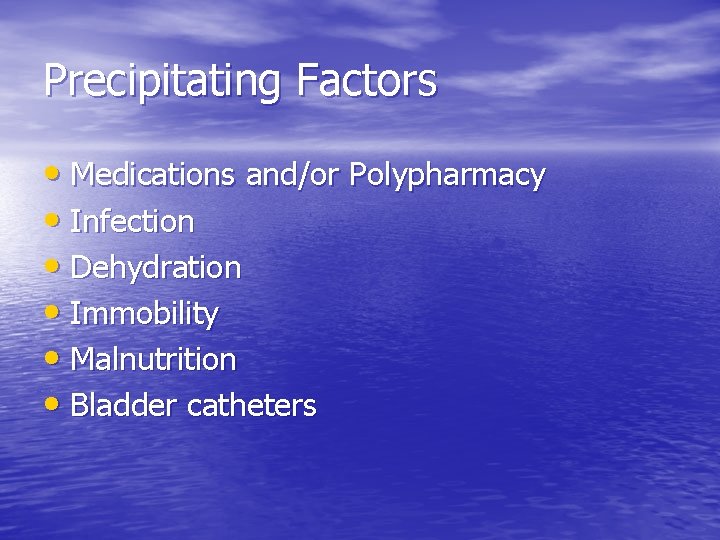
Precipitating Factors • Medications and/or Polypharmacy • Infection • Dehydration • Immobility • Malnutrition • Bladder catheters
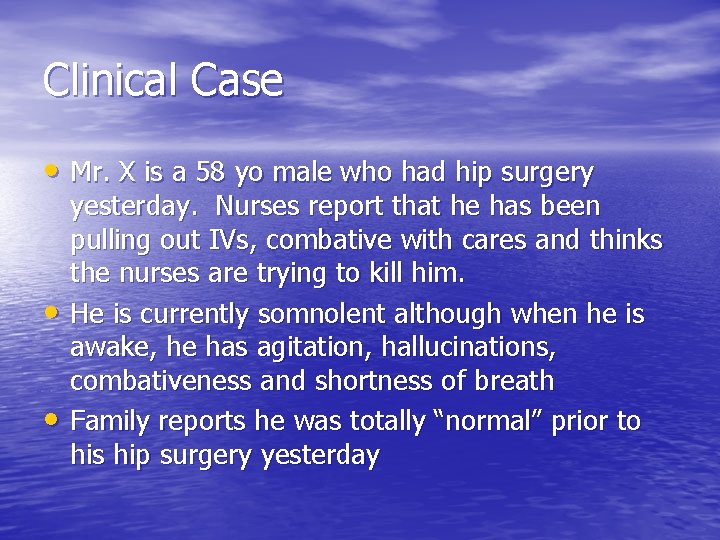
Clinical Case • Mr. X is a 58 yo male who had hip surgery • • yesterday. Nurses report that he has been pulling out IVs, combative with cares and thinks the nurses are trying to kill him. He is currently somnolent although when he is awake, he has agitation, hallucinations, combativeness and shortness of breath Family reports he was totally “normal” prior to his hip surgery yesterday
Psych consult is requested • What labs, tests, history or collateral information would you like?
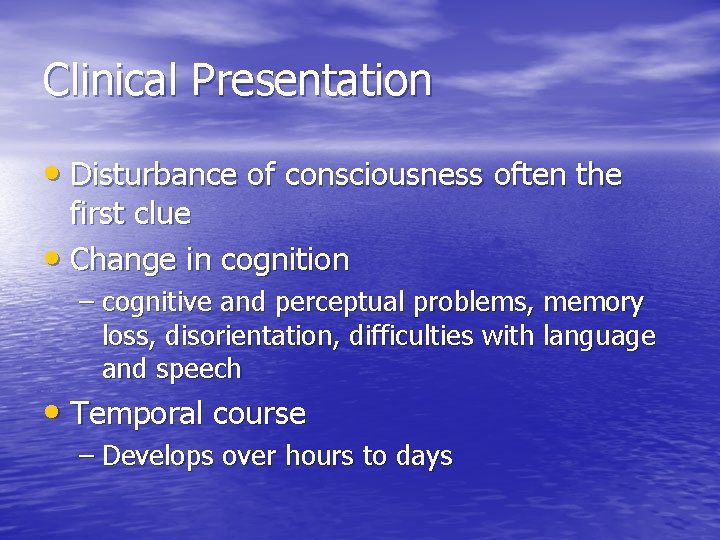
Clinical Presentation • Disturbance of consciousness often the first clue • Change in cognition – cognitive and perceptual problems, memory loss, disorientation, difficulties with language and speech • Temporal course – Develops over hours to days
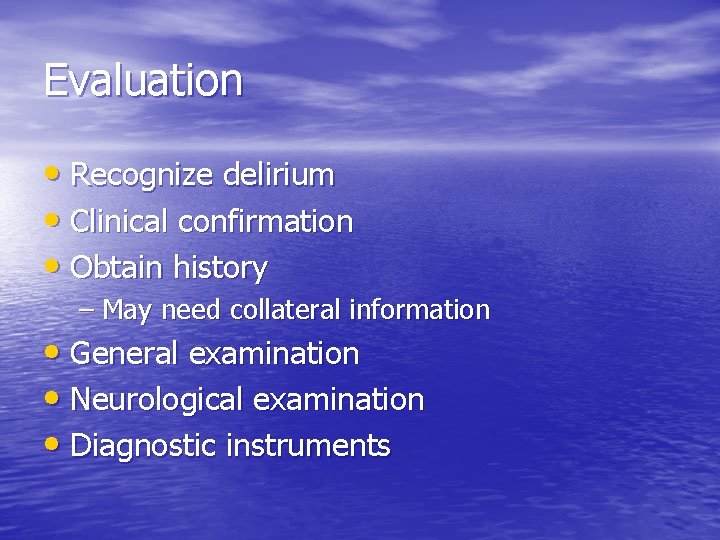
Evaluation • Recognize delirium • Clinical confirmation • Obtain history – May need collateral information • General examination • Neurological examination • Diagnostic instruments
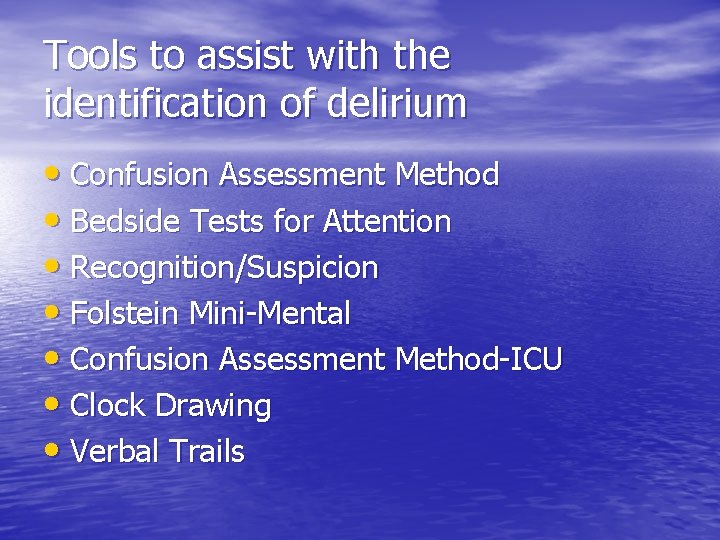
Tools to assist with the identification of delirium • Confusion Assessment Method • Bedside Tests for Attention • Recognition/Suspicion • Folstein Mini-Mental • Confusion Assessment Method-ICU • Clock Drawing • Verbal Trails
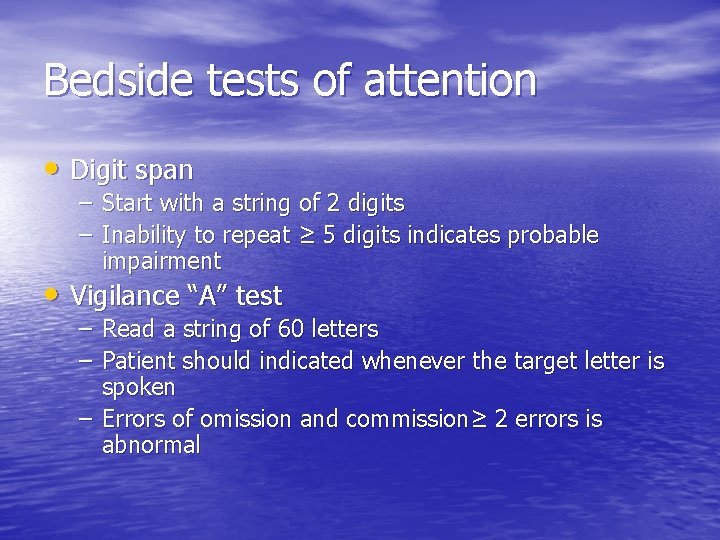
Bedside tests of attention • Digit span – Start with a string of 2 digits – Inability to repeat ≥ 5 digits indicates probable impairment • Vigilance “A” test – Read a string of 60 letters – Patient should indicated whenever the target letter is spoken – Errors of omission and commission≥ 2 errors is abnormal
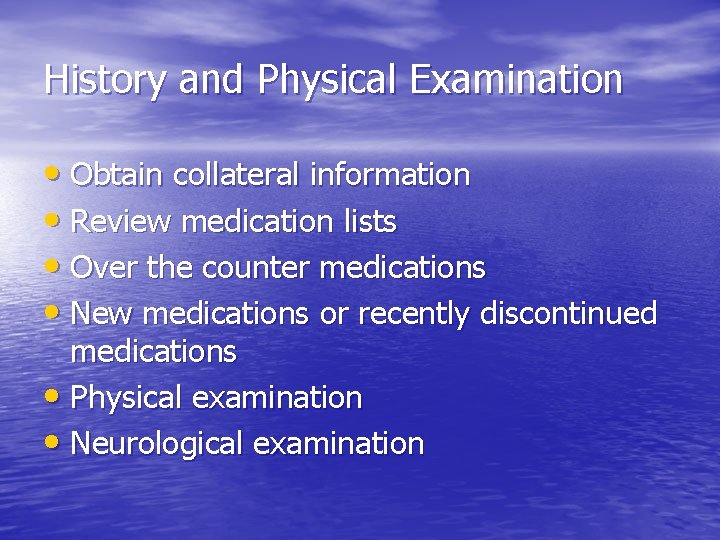
History and Physical Examination • Obtain collateral information • Review medication lists • Over the counter medications • New medications or recently discontinued medications • Physical examination • Neurological examination
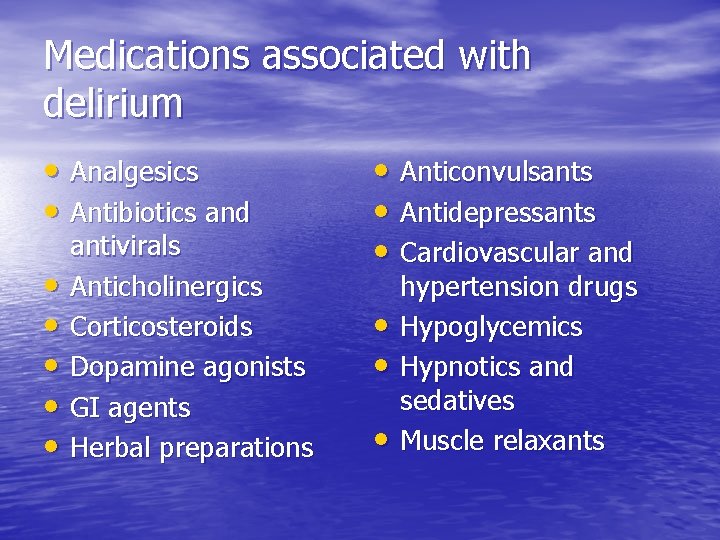
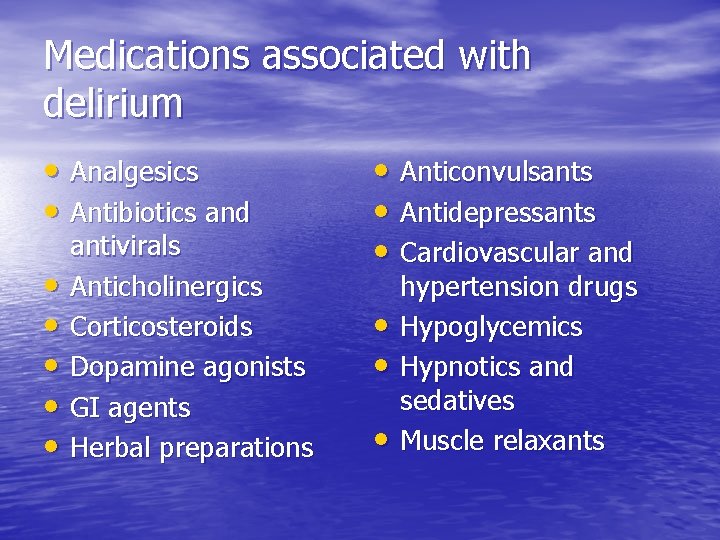
Medications associated with delirium • Analgesics • Antibiotics and • • • antivirals Anticholinergics Corticosteroids Dopamine agonists GI agents Herbal preparations • Anticonvulsants • Antidepressants • Cardiovascular and • • • hypertension drugs Hypoglycemics Hypnotics and sedatives Muscle relaxants
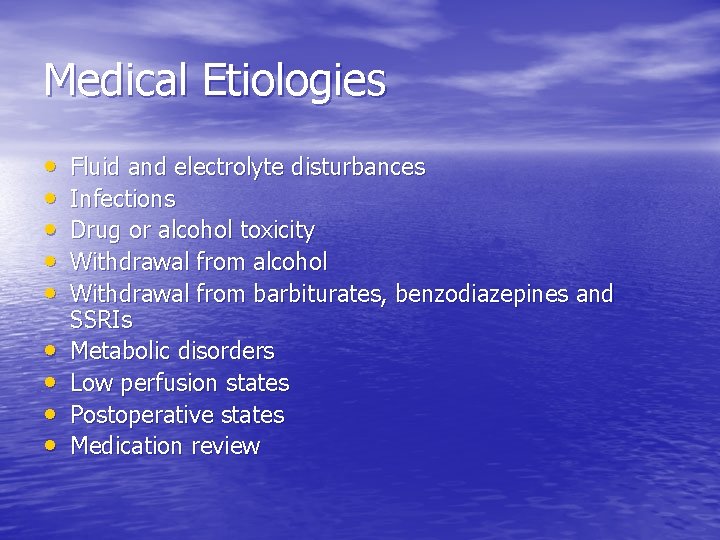
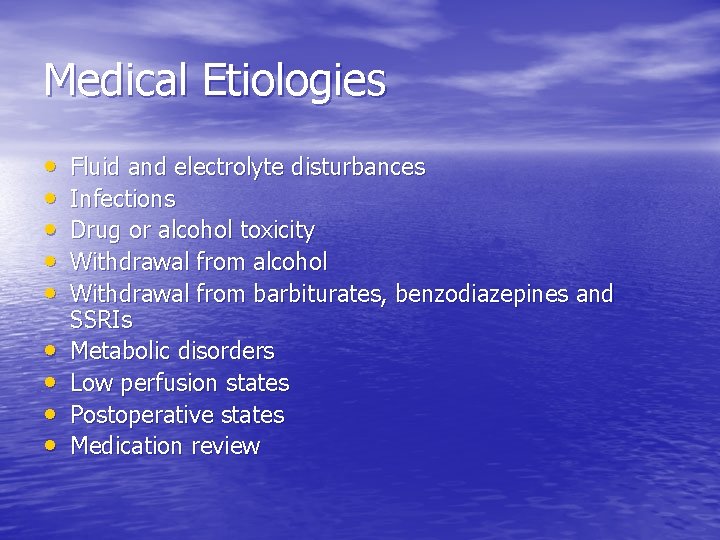
Medical Etiologies • • • Fluid and electrolyte disturbances Infections Drug or alcohol toxicity Withdrawal from alcohol Withdrawal from barbiturates, benzodiazepines and SSRIs Metabolic disorders Low perfusion states Postoperative states Medication review
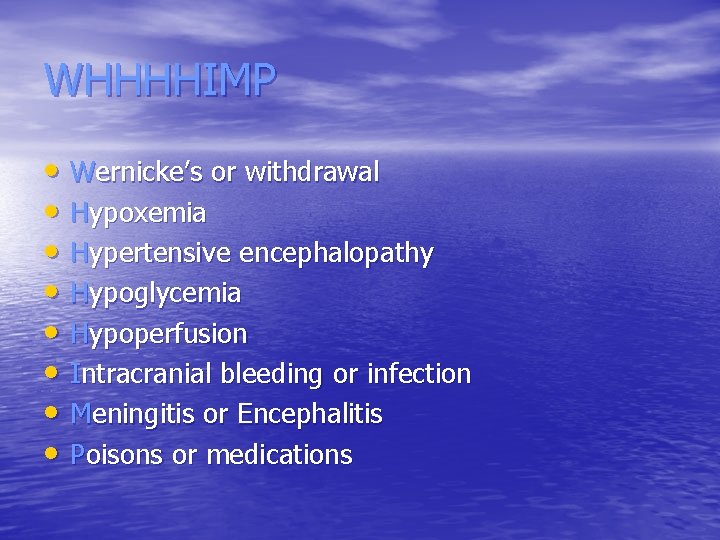
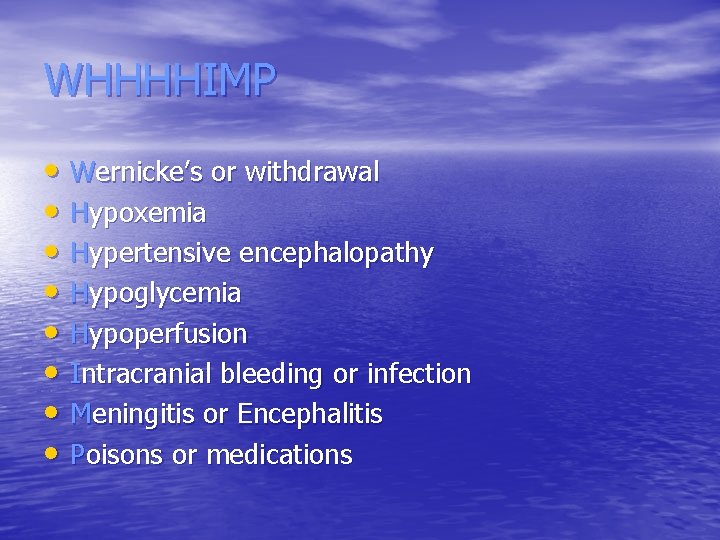
WHHHHIMP • Wernicke’s or withdrawal • Hypoxemia • Hypertensive encephalopathy • Hypoglycemia • Hypoperfusion • Intracranial bleeding or infection • Meningitis or Encephalitis • Poisons or medications

I WATCH DEATH • Infection • Withdrawal • Acute Metabolic • Trauma • CNS Pathology • Hypoxia • Deficiencies • Endocrinopathies • Acute vascular • Toxins or drugs • Heavy Metals
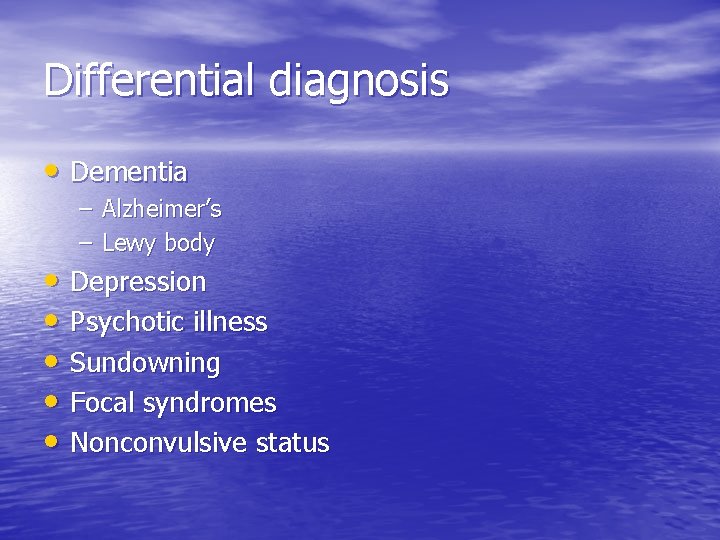
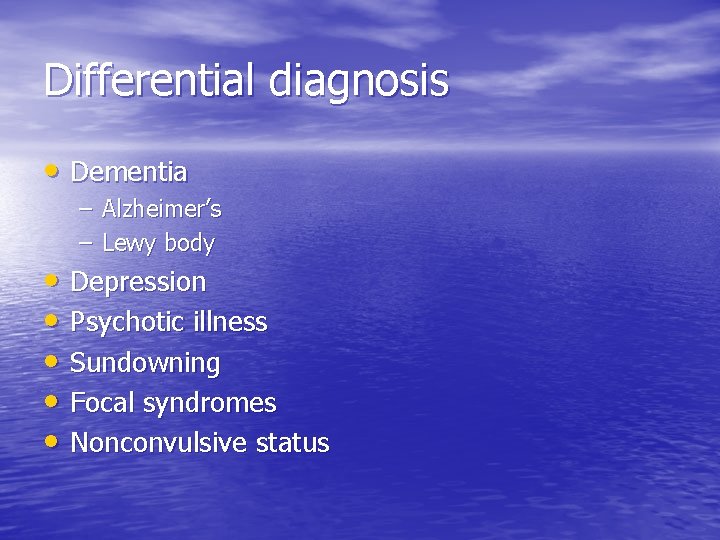
Differential diagnosis • Dementia – Alzheimer’s – Lewy body • Depression • Psychotic illness • Sundowning • Focal syndromes • Nonconvulsive status
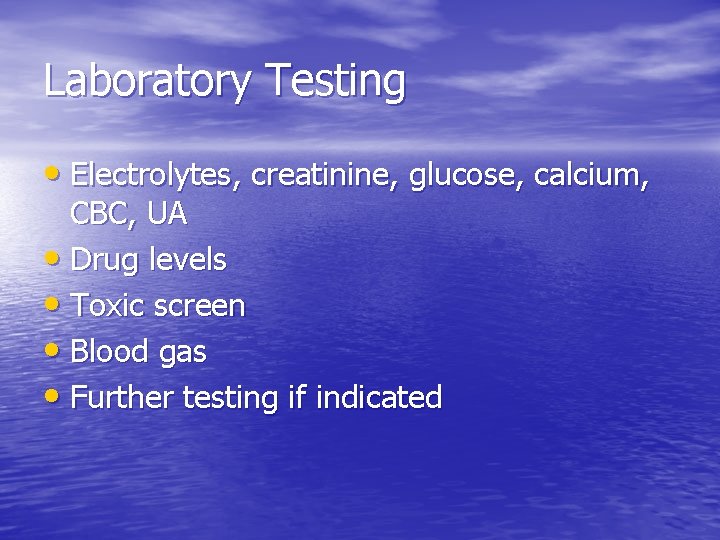
Laboratory Testing • Electrolytes, creatinine, glucose, calcium, CBC, UA • Drug levels • Toxic screen • Blood gas • Further testing if indicated
Neurological testing • Neuroimaging – CT – MRI • Lumbar puncture • EEG
Prevention and Treatment • Identify those at risk for delirium • Prevent dehydration, immobility, physical • • restraints, sleep deprivation, indwelling bladder catheters Avoid factors known to cause or aggravate delirium Identify and treat underlying acute illness Provide supportive care to prevent further cognitive and physical decline Control dangerous/disruptive behaviors
Prevention strategies • Adequate CNS oxygen delivery • Pain management but titrate to lowest dose • Elimination of unnecessary medications • Regulation of bowel/bladder function • Nutrition • Early mobilization • Monitoring for complications • Assuring appropriate environmental stimuli • ? Use of medications to prevent delirium
Medication based trials for preventing delirium • Mixed results • Haloperidol prior to hip surgery • Donepezil to prevent postoperative delirium • Rivastigmine to prevent delirium in elderly hospitalized patients • Haloperidol or ziprasidone in mechanically ventilated patients
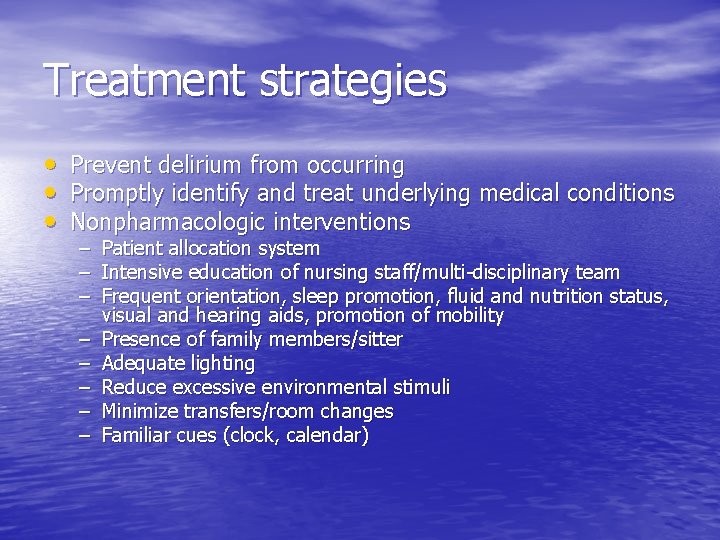
Treatment strategies • Prevent delirium from occurring • Promptly identify and treat underlying medical conditions • Nonpharmacologic interventions – Patient allocation system – Intensive education of nursing staff/multi-disciplinary team – Frequent orientation, sleep promotion, fluid and nutrition status, visual and hearing aids, promotion of mobility – Presence of family members/sitter – Adequate lighting – Reduce excessive environmental stimuli – Minimize transfers/room changes – Familiar cues (clock, calendar)
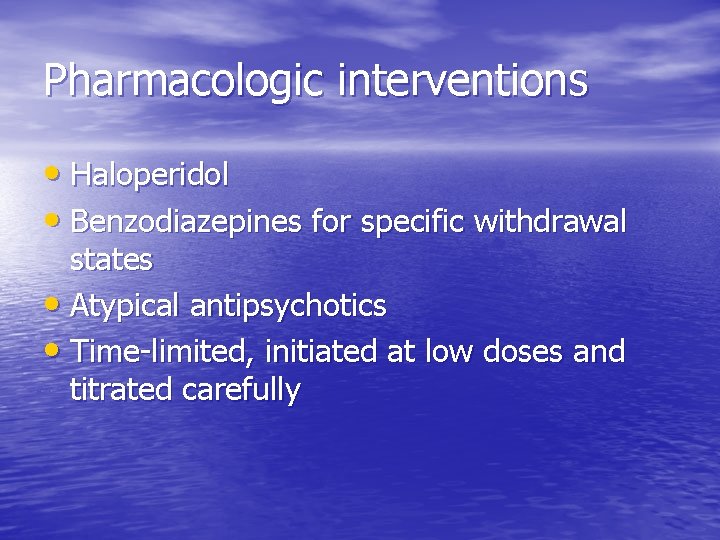
Pharmacologic interventions • Haloperidol • Benzodiazepines for specific withdrawal states • Atypical antipsychotics • Time-limited, initiated at low doses and titrated carefully
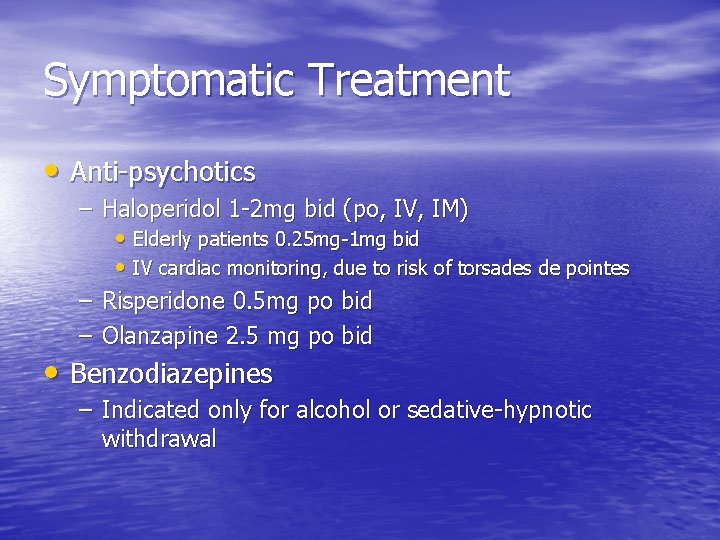
Symptomatic Treatment • Anti-psychotics – Haloperidol 1 -2 mg bid (po, IV, IM) • Elderly patients 0. 25 mg-1 mg bid • IV cardiac monitoring, due to risk of torsades de pointes – Risperidone 0. 5 mg po bid – Olanzapine 2. 5 mg po bid • Benzodiazepines – Indicated only for alcohol or sedative-hypnotic withdrawal
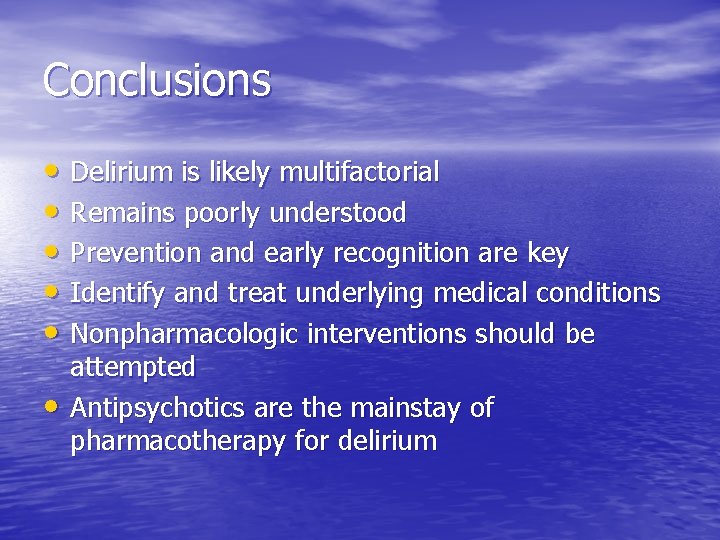
Conclusions • Delirium is likely multifactorial • Remains poorly understood • Prevention and early recognition are key • Identify and treat underlying medical conditions • Nonpharmacologic interventions should be • attempted Antipsychotics are the mainstay of pharmacotherapy for delirium
Summary • Common • Often underrecognized • Potentially life-threatening • Treatment can save lives and shorten hospital stays • Bizarre behavior often necessitates psychiatric consultation
 Vicki kijewski
Vicki kijewski Vicki bernard
Vicki bernard Mlambert customer service
Mlambert customer service Vicki rundle
Vicki rundle Vicki amon-higa
Vicki amon-higa Vicki turetsky
Vicki turetsky Math learning center wvu
Math learning center wvu Vicki freeman
Vicki freeman Vicki bosanko
Vicki bosanko Vicki fleming
Vicki fleming Vicki evans
Vicki evans Vicki freeman
Vicki freeman Robert shell juvenile center
Robert shell juvenile center Vicki farnsworth
Vicki farnsworth Vicki carolin
Vicki carolin Vicki nixon
Vicki nixon Nash delirium
Nash delirium Delirium definition
Delirium definition Lucie big delirium
Lucie big delirium Gcs somnolen
Gcs somnolen Delirium case presentation
Delirium case presentation Terminalt delirium
Terminalt delirium Delirium definition
Delirium definition Difference between dementia and delirium
Difference between dementia and delirium Types of amnesia
Types of amnesia Flocculation delirium
Flocculation delirium Escala rass
Escala rass Excited delirium перевод
Excited delirium перевод Sindrom delirium akut
Sindrom delirium akut Driver diagram palliative care
Driver diagram palliative care Difference between delirium and dementia ppt
Difference between delirium and dementia ppt Delirium care pathways
Delirium care pathways Delirium refractario
Delirium refractario Edu.sharif.edu
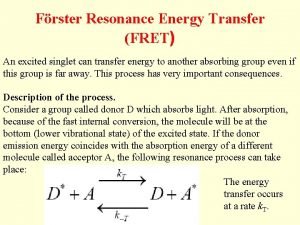
Edu.sharif.edu Ysu bursar office
Ysu bursar office Latrobe.edu.au library
Latrobe.edu.au library Portali studentor notat
Portali studentor notat