Geriatric Psychiatry Vicki Kijewski M D vickikijewskiuiowa edu



















- Slides: 51
Geriatric Psychiatry Vicki Kijewski, M. D. vicki-kijewski@uiowa. edu June 8, 2016
Objectives • Compare and Contrast the 3 D’s – Delirium, dementia, depression • Identify 4 other common geriatric psychiatric syndromes • Describe diagnosis and management strategies
Geriatric Psychiatry Syndromes • Acute Confusion (Delirium) • Memory Loss (Dementia) • Depression • Insomnia • Anxiety • Suspiciousness and Agitation • Hypochondriasis
Acute Confusion (Delirium) • De • Lira • Ium “Away from” “Furrow in a field” Singular • “A going off the ploughed track, a madness”

Delirium • Acute onset • Decreased ability to maintain attention • Difficulty shifting attention • Disorganized thinking and speech • Memory disturbance • Altered level of consciousness • Disturbance in sleep-wake cycle • Anxiety, fear, irritability and anger • May appear apathetic and withdrawn

Why worry about delirium? • Common • Leads to prolonged hospitalizations • Leads to functional decline • Leads to institutionalization • Mortality at 2 year f/u nearly 50% • Although generally reversible, often the harbinger of future problems

Types of Delirium • Hyperactive • Hypoactive • Mixed
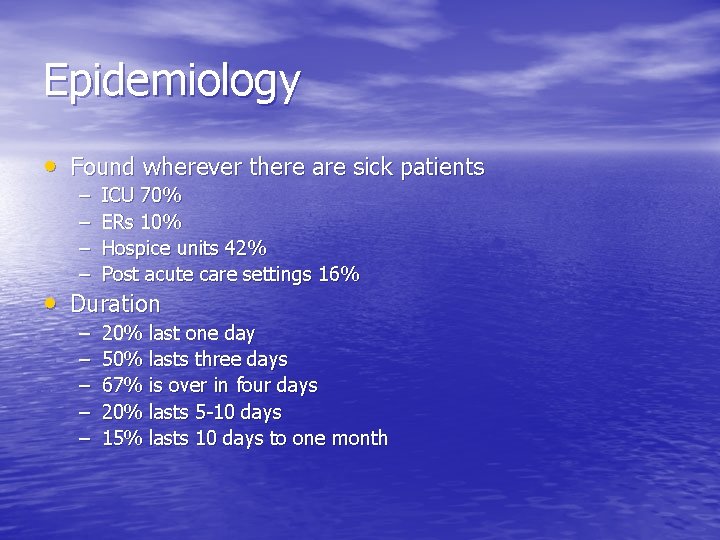
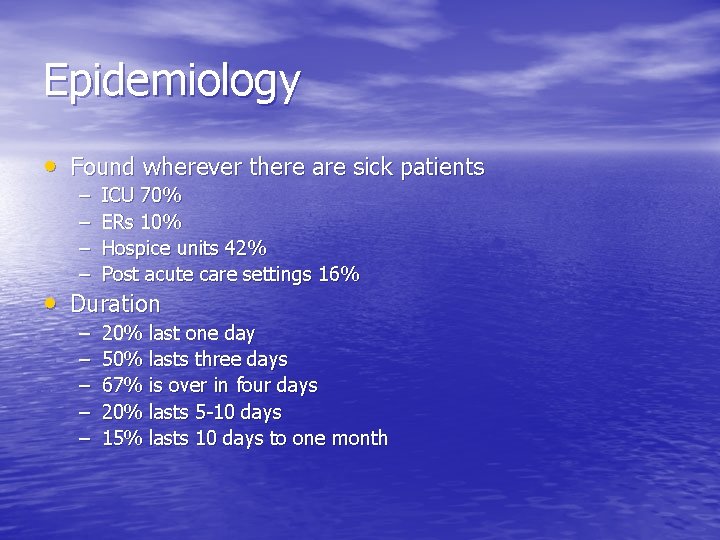
Epidemiology • Found wherever there are sick patients – – ICU 70% ERs 10% Hospice units 42% Post acute care settings 16% – – – 20% last one day 50% lasts three days 67% is over in four days 20% lasts 5 -10 days 15% lasts 10 days to one month • Duration
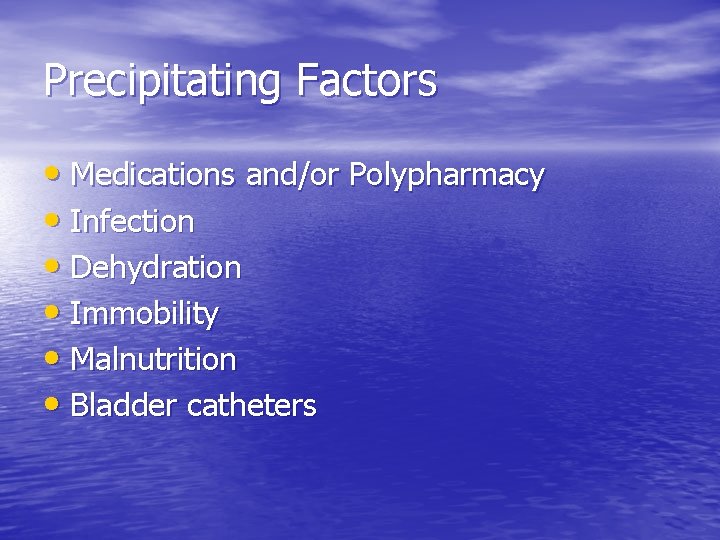
Precipitating Factors • Medications and/or Polypharmacy • Infection • Dehydration • Immobility • Malnutrition • Bladder catheters
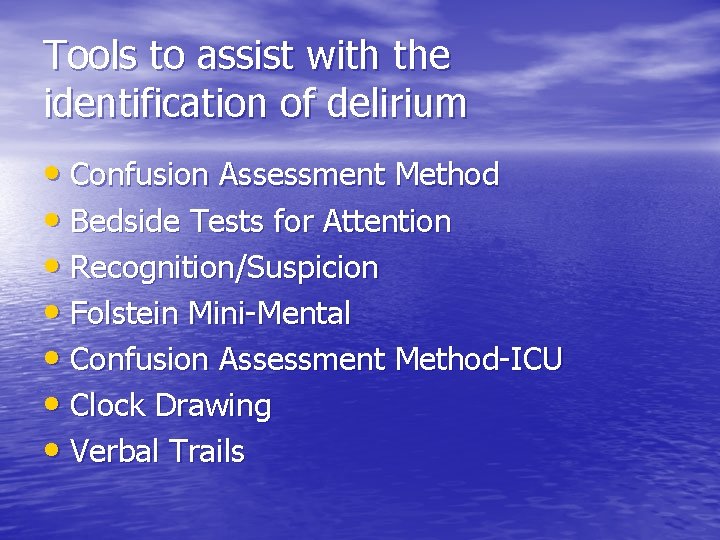
Tools to assist with the identification of delirium • Confusion Assessment Method • Bedside Tests for Attention • Recognition/Suspicion • Folstein Mini-Mental • Confusion Assessment Method-ICU • Clock Drawing • Verbal Trails

History and Physical Examination • Obtain collateral information • Review medication lists • Over the counter medications • New medications or recently discontinued medications • Physical examination • Neurological examination

WHHHHIMP • Wernicke’s or withdrawal • Hypoxemia • Hypertensive encephalopathy • Hypoglycemia • Hypoperfusion • Intracranial bleeding or infection • Meningitis or Encephalitis • Poisons or medications

Prevention and Treatment • Identify those at risk for delirium • Prevent dehydration, immobility, physical • • restraints, sleep deprivation, indwelling bladder catheters Avoid factors known to cause or aggravate delirium Identify and treat underlying acute illness Provide supportive care to prevent further cognitive and physical decline Control dangerous/disruptive behaviors
Prevention strategies • Adequate CNS oxygen delivery • Pain management but titrate to lowest dose • Elimination of unnecessary medications • Regulation of bowel/bladder function • Nutrition • Early mobilization • Monitoring for complications • Assuring appropriate environmental stimuli • ? Use of medications to prevent delirium
Symptomatic Treatment • No medications are FDA approved for the • • • treatment of delirium Use of Anti-psychotics is controversial No clinical practice guidelines UK-NIHCE recommends short term, lowest dose – Distressed individuals with harmful behaviors not responsive to other environmental strategies • Benzodiazepines – Indicated only for alcohol or sedative-hypnotic withdrawal
Delirium • Multifactorial • Remains poorly understood • Prevention and early recognition are key • Identify and treat underlying medical conditions • Nonpharmacologic interventions should be attempted

Memory Loss • Major Neurocognitive Disorders • Mild Neurocognitive Disorders • More common in those > 75 • At least 10% of persons > 65 in community • Relatively indolent • Progressive

Memory Loss (Dementia) • Alzheimer’s dementia 60% • Vascular dementia • Dementia with Lewy bodies • Mixed type • Mild cognitive impairment
Clinical Characteristics • Memory impairment • Language disturbance • Difficulty carrying out motor activities • Failure to recognize objects • Difficulty with calculations • Focal neurological signs (Va. D) • Disturbances in executive function
Screening/Diagnosis • Folstein MMSE • Montreal Cognitive Assessment – www. mocatest. org • Neuropsychological Assessment • TSH, B 12, Metabolic Profile • Hearing, vision, alcohol use, drug use • HIV, syphilis • Imaging

Memory Loss • Prevention? – Using a computer – Moderate physical exercise • Not helpful – Gingko biloba – Fish oil – Antioxidants – Vitamins – NSAIDS
Treatments • Increasing patient safety • Increasing functionality • Improving quality of life • Reduce patient harm • Reduce caregiver stress • Educate patient and caregiver – www. alz. org or 1 -800 -272 -3900

Treatments • Initiation of environmental safety measures • Formal driving evaluation • Home safety evaluation • Regular exercise • Social supports • Consistent environment • Problem solving therapy

Capacity Evaluations End of Life Planning • Capacity assessment – Specific ability to make a decision at a given point in time – Conversation • Communicate • Understanding of intervention • Risks/benefits/alternatives • Express a choice • Rationale for decision
Medications • FDA approved medications for moderate dementia – Donepezil (cholinesterase inhibitor) – Rivastigmine (cholinesterase inhibitor) – Galantamine (cholinesterase inhibitor) – Memantine (NMDA receptor antagonist) • When should they be stopped?

Medications • Consider an SSRI if mood disorder • In general avoid benzodiazepines • What about antipsychotics? – Controversial – 10% of hospitalizations in the setting of dementia are related to behavioral issues
Dementia associated behaviors • Physical aggression • Verbal aggression • Wandering • Hoarding • Disinhibition • Calling out
Treatment of behaviors • Non-pharmacologic interventions • Determine cause of behavior – Hunger, boredom, pain, toileting needs, isolation, infection, …. • Familiar surroundings/caregivers • Transitional object • Simple task

Use of Antipsychotics in Dementia • Controversial • 2005 Black Box Warning • Consider if history of psychosis, mania, hallucinations or overt psychosis • Most studies ≤ 35% reduction in behavior • Efficacy similar for typical and atypical Aps • Obesity, DM, falls, TD, AMI, EPS, death

Consequences of Dementia • Failure to Thrive – Anorexia, weight loss • Frailty – Unintentional weight loss – Slow movement – Fatigue – Weakness – Low physical activity
Depression • Frequent • Often do not complain of depressed mood spontaneously • Weight loss • Insomnia • Anhedonia • Complain of difficulties with concentration and memory loss
Depression • > 10% of older adults seen by PCP suffer from depressive disorders • Rates increase in both sexes after 65 • Vague, nonspecific symptoms • Somatic complaints – Pain, change in weight, constipation, irritability, agitation, fatigue, headache, insomnia, hypersomnia, weakness
Diagnosis of Depression • Geriatric Depression Scale • PHQ-9 • Cornell Scale for Depression in Dementia • Up to 50% of caregivers of older adults may have depressive symptoms as well

Treatment of Depression • Medication – SSRIs, SNRIs, other agents • Start low, go slow but GO • Therapy – CBT, IPT, Psychodynamic • Electroconvulsive Therapy • 30% of older adults are undertreated

Suicide Risk • 5 -10% of older adults suicidal ideation • 30% of those with MDD • ↑ Lower SES, ↑ Cerebral microbleeds • Most likely to be reported to PCP • Ask directly • 40% of older adults who completed suicide had communicated wish to die to provider in last 12 months
Insomnia • 28% report difficulty falling asleep • 46% report difficulty staying asleep • Normal changes with aging – ↓ total sleep time – ↓ sleep efficiency – ↓ slow wave and REM – ↑ incidence of napping/falling asleep during day – Less tolerance for jet lag/shift work
Sleep disturbances leading to insomnia • Primary insomnia • Sleep-disorder breathing (OSA) • Periodic leg movements or noc myoclonus • Anxiety and mood disorders • Dementia • Medications • Physical Illness (CHF, COPD, Nocturia, …)

Treatment of Insomnia • Nonpharmacologic Interventions – Sleep education – Sleep hygiene – Cognitive behavioral therapy – Bright light therapy
Pharmacotherapy of Insomnia • Melatonin/Ramelteon – May be helpful • OTC sleep aids (diphenhydramine) – Drug interactions, confusion, falls – Habit forming – Do not normalize sleep cycle • Sedative/Hypnotics – Increased risk of falls, confusion
Anxiety • 5% of older adults • Medical causes – Hyperthyroidism – Cardiac arrhythmia – Pulmonary emboli – Hypoglycemia – Medications such as caffeine, OTC sympathomimetic drugs, anticholinergic
Causes of Anxiety • Confusion • Depression • Fear of falling, getting lost, being attacked • Dementing disorders

Treatment • Nonpharmacologic interventions • Medications
Suspiciousness and Agitation • More common in those with cognitive impairment • Persecutory delusions • Somatic delusions
Treatment • Ensure a safe environment • Initiate a therapeutic alliance • Consider pharmacologic treatment • Anticipate acute behavioral crises.
Illness Anxiety Disorder (Hypochondriasis) • Belief of suffering from one or more serious illnesses • Exaggerated interpretation of physical signs • Abdominal/GU symptoms • Concerns not alleviated by reassurance from physician or medical evaluation • Side effects from medications

Contributing Factors • Shift anxiety from psychological conflicts to concrete problems with body functioning • Social factors • Isolation
Diagnostic Evaluation • History • Routine physical examination • Routine laboratory evaluation if indicated
Treatment • Best managed by PCP • Relatively brief but regularly scheduled visits
Managing Illness Anxiety Disorder (Hypochondriasis) • Control excessive use of healthcare services. Prescribe meds with caution. • Decrease concern and anxiety in patient • Provide assurance of professional commitment to management • Decrease family stress • Decrease anxiety, anger and frustration of health care professional
Conclusions • Acute confusion in hospitalized elders is common. Careful screening is indicated. • Important to work with family of patient with memory loss. • Good sleep hygiene is more important than pharmacological treatment • Anxiety is often comorbid with other conditions
Conclusions • Suspiciousness and agitation are the most disruptive symptoms of dementing disorders • Uncomplicated depression in late life is responsive to treatment. • Use a structured approach to the patient with hypochondriasis.
 Vicki kijewski
Vicki kijewski Community geriatric psychiatry
Community geriatric psychiatry Geriatric psychiatry definition
Geriatric psychiatry definition Neurosis vs psychosis
Neurosis vs psychosis Psychiatry in ethiopia
Psychiatry in ethiopia National network of child psychiatry access programs
National network of child psychiatry access programs Mse speech
Mse speech Gipsofia
Gipsofia Jamaica hospital psychiatry residency
Jamaica hospital psychiatry residency Radical psychiatry sociology
Radical psychiatry sociology National network of child psychiatry access programs
National network of child psychiatry access programs Core psychiatry
Core psychiatry Nbme shelf exam percentiles 2021
Nbme shelf exam percentiles 2021 Meaning of criminal psychology
Meaning of criminal psychology Mse psychiatry
Mse psychiatry Asclepiades father of psychiatry
Asclepiades father of psychiatry European psychiatry
European psychiatry Addiction expert witnesses
Addiction expert witnesses Who is this
Who is this Vicki fleming
Vicki fleming Vicki freeman
Vicki freeman Robert shell juvenile center
Robert shell juvenile center Vicki nixon
Vicki nixon Vicki carolin
Vicki carolin Vicki bernard
Vicki bernard Vicki lambert payroll
Vicki lambert payroll Vicki rundle
Vicki rundle Vicki amon-higa
Vicki amon-higa Vicki farnsworth
Vicki farnsworth Math learning center wvu
Math learning center wvu Vicki freeman
Vicki freeman Vicki turetsky
Vicki turetsky Vicki bosanko
Vicki bosanko Vicki evans
Vicki evans Sarc f
Sarc f Va geriatric scholars program
Va geriatric scholars program Geriatric case presentation
Geriatric case presentation Chapter 10 geriatric care
Chapter 10 geriatric care Geriatric syndrome 14i
Geriatric syndrome 14i Dr hannah seymour
Dr hannah seymour Gems diamond geriatric
Gems diamond geriatric Dr rose dinda martini
Dr rose dinda martini Geriatric nutrition
Geriatric nutrition Gems geriatric diamond
Gems geriatric diamond Frailty syndrome
Frailty syndrome Geriatric syndrome
Geriatric syndrome Centrum geriatric
Centrum geriatric Geriatric giants mnemonic
Geriatric giants mnemonic Geriatric competency assessment
Geriatric competency assessment Palmerston north geriatric
Palmerston north geriatric Gems diamond geriatric assessment
Gems diamond geriatric assessment Objectives of elderly care
Objectives of elderly care