The Geriatric Giants Dr Hannah Seymour Consultant Geriatrician




























- Slides: 108
The Geriatric Giants Dr Hannah Seymour Consultant Geriatrician RPH
Aknowledge slides from • Dr Kate Ingram • Dr Mark Donaldson • Dr Chris Beer • Dr Sean Maher
GIANTS OF GERIATRICS (Isaacs 1970) • Immobility • Instability • Intellectual Impairment • Incontinence • Iatrogenesis
I’m going to talk about • Cognition – Forgetfulness vs Delirium vs Dementia • Falls – Reversible causes in the community • Immobility – How to avoid and manage it • Incontinence – Especially reversible causes • Iatrogenic Conditions – Especially Polypharmcy & Malnutrition

Cognition
Cognitive Screening Tests • Screening Detection amongst “healthy” community members of (unsuspected) disorders or risk factors • Case Finding Detection of cognitive impairment where high probability of disease in particular population or setting
Cognitive Screening Tests • Normal ageing vs MCI vs early dementia? • No perfect test for early detection • Case for detection of mild cognitive impairment unclear Risks vs benefits, costs, no effective therapies May change with new therapies • Emphasis on detection of dementia Benefit from interventions • Should always be done if memory complaints or history suggestive of dementia
Cognitive Screening Tests • Detect cognitive impairment from any cause • Don’t diagnose dementia! • Generally test orientation, recall of short and long term memory, personal information, attention and other domains eg visuospatial

Cognitive Screening Tests: MMSE • Standardised MMSE Molloy et al 1991 • Floor and ceiling effects • Western background, education, language • No test of executive function • Orientation • Registration, Recall • Attention • Calculation • Language • Visual construction
Cognitive Screening Tests: Geriatric Depression Scale (GDS) Yesavage 1983 • 30 Questions Cut off 11 Sens 84% Spec 95% Cut off 14 Sens 80% Spec 100% • 15 Question version • 4 & 10 Question versions • Yes or No responses to questions about depression symptoms • Depression an important cause of cognitive impairment
Dementia • Global cognitive impairment • Irreversible • Clear sensorium • Usually progressive

Dementia: Causes • Alzheimer’s • Lewy Body • Frontotemporal • Parkinson’s • Cushing’s, Addison’s, Thyroid, parathyroid, diabetes • Vitamin B 12, thiamine, nicotine deficiency • Huntington’s • Normal pressure hydrocephalus, Head injury, space occupying lesion, multiple sclerosis • Vascular • Syphilis, HIV, encephalitis, CJD • Other extrapyramidal syndromes Stroke Small vessel ischaemia Adapted from Eastley R. , Assessment of Dementia, in Dementia, Eds Burns, O’Brien & Ames
Dementia: Some “Reversible or partly reversible” Causes • Drugs • Liver disease • Depression • Normal pressure hydrocephalus • Metabolic causes • Subdural haematoma • Thyroid Disease • Neoplasm • Vitamin B 12 deficiency • Hypercalcaemia Adapted from Eastley R. , Assessment of Dementia, in Dementia, Eds Burns, O’Brien & Ames
Dementia: Diagnostic features • development of multiple cognitive deficits • impairment in occupational or social functioning • decline from a previously higher level of functioning • memory impairment • And at least one of: aphasia apraxia agnosia disturbance in executive functioning. Adapted from Diagnostic and Statistical Manual of mental disorders IV edition revised 2000, American Psychiatric Association
Diagnostic features: Memory • Memory impairment needed for diagnosis • early prominent symptom • new learning impaired • forgets previously learned material • loses valuables, forget food cooking, lost in unfamiliar territory, poor medication compliance • forgets personal details eg family, occupation, address, own name Adapted from Diagnostic and Statistical Manual of mental disorders IV edition revised 2000, American Psychiatric Association
Diagnostic features: Aphasia • Language difficulty • Loss of complexity • Naming people or objects • Repetition • Comprehension (verbal and written) • eventually mute Adapted from Diagnostic and Statistical Manual of mental disorders IV edition revised 2000, American Psychiatric Association

Diagnostic features: Apraxia • Difficulty performing motor task despite intact comprehension power Sensation • Trouble with everyday tasks eg cleaning teeth, washing Adapted from Diagnostic and Statistical Manual of mental disorders IV edition revised 2000, American Psychiatric Association
Diagnostic features: Agnosia • Difficulty recognising objects or people • Trouble recognising ordinary objects, family members, even themselves in photographs or mirrors Adapted from Diagnostic and Statistical Manual of mental disorders IV edition revised 2000, American Psychiatric Association
Diagnostic features: Executive Functioning • ability to think abstractly • judgement, reasoning, insight • plan, initiate, sequence, monitor, and stop complex behaviour • difficulty coping with novel tasks or complexity • poor choices • financial problems • at risk behaviour due to lack of insight Adapted from Diagnostic and Statistical Manual of mental disorders IV edition revised 2000, American Psychiatric Association
Diagnostic features: Behaviour • Delusions, especially paranoia • Social withdrawal • Hallucinations, especially visual • Neglect of personal care, home, nutrition • Irritability, aggression (verbal and physical) • Resistiveness • Agitation, wandering, getting lost • Apathy • Sleep disturbance • Mood disturbance Anxiety Depression • Demanding, attention seeking, repetitive Adapted from Hecker J. , Dementia and Alzheimer’s Disease in A Practical Guide to Geriatric Medicine. Ratnaike R
Dementia: Assessment • History – most important • Examination • Neuropsychometric testing • Laboratory tests FBP, U&E, TFT, B 12, folate, BSL, syphilis serology, ESR, Urinalysis, calcium +/- lumbar puncture, EEG • Imaging CT, MRI SPECT, PET
Dementia: Alzheimer’s Disease • Accounts for 60% of Dementia in Australia • Neuronal degeneration with plaques of beta amyloid and neurofibrillary tangles • Early onset forms due to gene mutations • Main feature is memory loss, plus other domains, gradually progressive • Treatment with cholinesterase inhibitors (donepezil, galantamine, rivastigmine) or memantine • New therapies seem promising Adapted from Hecker J. , Dementia and Alzheimer’s Disease in A Practical Guide to Geriatric Medicine. Ratnaike R
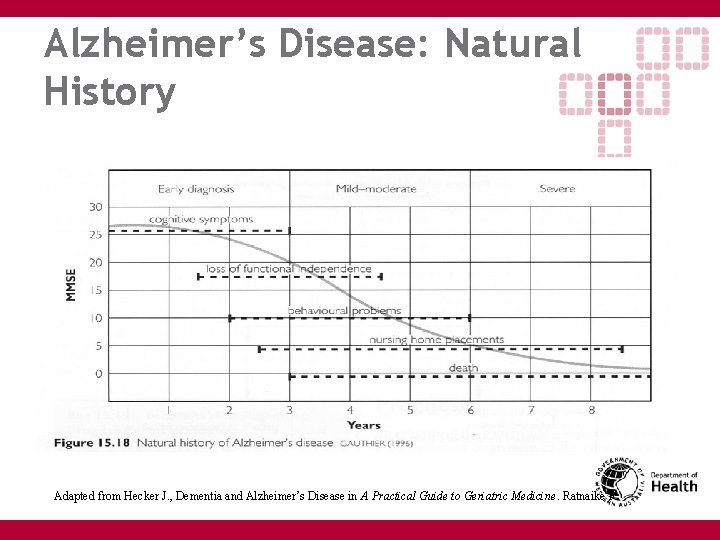
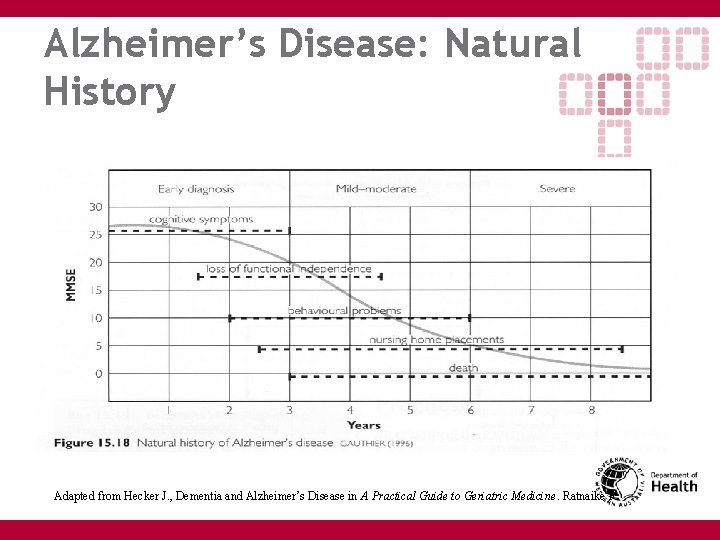
Alzheimer’s Disease: Natural History Adapted from Hecker J. , Dementia and Alzheimer’s Disease in A Practical Guide to Geriatric Medicine. Ratnaike R
Dementia: Lewy Body Disease • Lewy bodies = neuronal inclusions of neurofilament protein ubiquitin • Found in basal ganglia in PD, diffusely through cerebral cortex in DLB - spectrum of same disease? • Classic features of cognitive impairment plus Fluctuation in cognition, alertness, attention Visual hallucinations Parkinsonism • Respond to cholinesterase inhibitors • Very sensitive to antipsychotics => rigidity Adapted from Hecker J. , Dementia and Alzheimer’s Disease in A Practical Guide to Geriatric Medicine. Ratnaike R
Dementia: Vascular Dementia • Cognitive impairment due cerebrovascular disease Small vessel ischaemic changes - gradual decline Recurrent stroke - stepwise deterioration • Evidence of vascular changes on CT/MRI • Vascular risk factors - HTN, cholesterol, diabetes, smoking, existing cardiac disease • Often early onset gait disturbance (balance and/or gait dyspraxia), falls, urinary incontinence • Often frontal lobe features, emotional lability, pseudobulbar palsy with speech/swallowing problems Adapted from Hecker J. , Dementia and Alzheimer’s Disease in A Practical Guide to Geriatric Medicine. Ratnaike R
Dementia: Frontotemporal Dementia • Probably represents several diseases • Early loss of personal and social awareness • Disinhibition often prominent • Mental rigidity, inflexibility, “concrete” • Depression and anxiety prominent • Speech and language disturbance Reduced in complexity Echolalia, stereotypy • Early primitive reflexes and urinary incontinence • Late rigidity, tremor Adapted from Hecker J. , Dementia and Alzheimer’s Disease in A Practical Guide to Geriatric Medicine. Ratnaike R

Dementia: Management • Treat reversible causes! • Education • Cholinesterase inhibitors (AD, LBD) • Control of vascular risk factors • Maintain cognitive and physical activity • Treat depression
Dementia: Practical Issues • Education • Memory aids • Counselling • Home safety • Community Resources • Driving Alzheimer’s Assoc Respite in home, day centres & residential • Enduring Power of attorney • Testamentary capacity • Advanced directives Crisis Care • Continence Care packages • Residential Care • Strategies for managing behaviour Adapted from Hecker J Dementia and Alzheimer’s Disease in A Practical Guide to Geriatric Medicine. Ratnaike R

Dementia: Take home messages • Cognitive screening tools only detect cognitive impairment they don’t diagnose • History suggestive of dementia or abnormal cognitive test result should result in suggestion for further evaluation • A diagnosis of dementia requires decline in occupational and social functioning, at least one other cognitive domain impaired (aphasia, agnosia, apraxia, executive dysfunction), as well memory • Interventions usually beneficial • Carer support vital to management

Delirium in Older People
Delirium: Definition • de lira “to wander” • Clinical syndrome characterised by rapid onset of altered consciousness and cognition that fluctuates

Delirium: Epidemiology • Prevalence in elderly hospital admissions 10 - 24% • Incidence during hospital stay 6 - 56% • Post operative incidence 10 - 61%

Delirium: Aetiology • Geriatric syndrome • Multiple factors acting in concert • Patient vulnerability • Predisposing factors • Precipitating factors
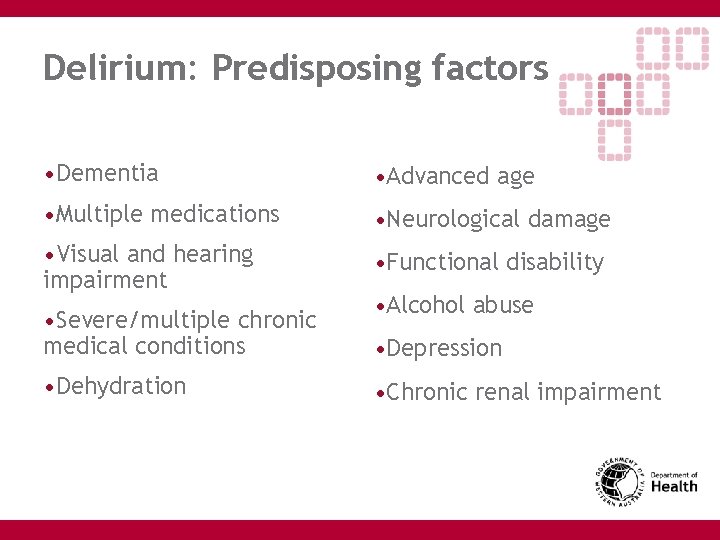
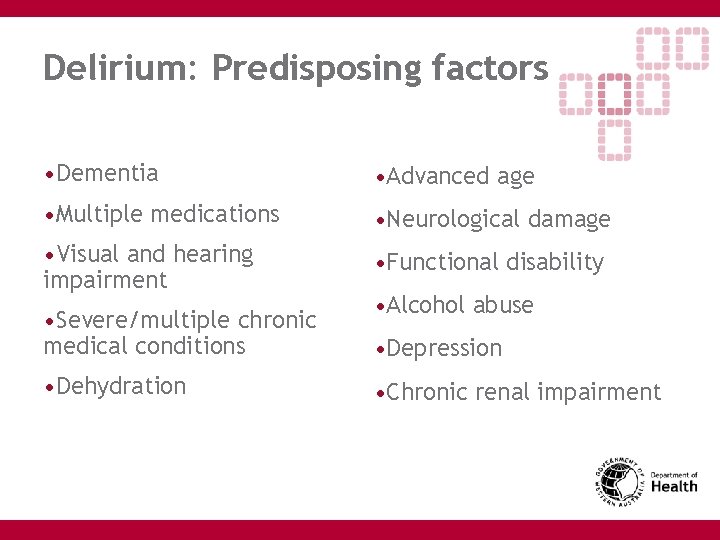
Delirium: Predisposing factors • Dementia • Advanced age • Multiple medications • Neurological damage • Visual and hearing impairment • Functional disability • Severe/multiple chronic medical conditions • Dehydration • Alcohol abuse • Depression • Chronic renal impairment
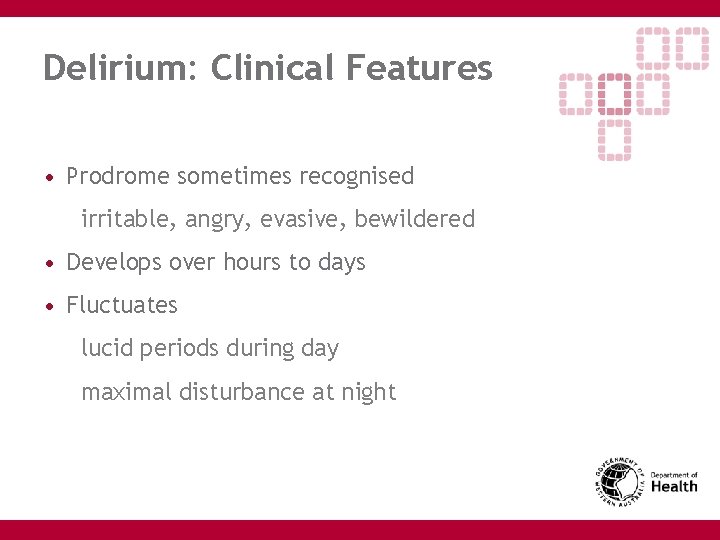
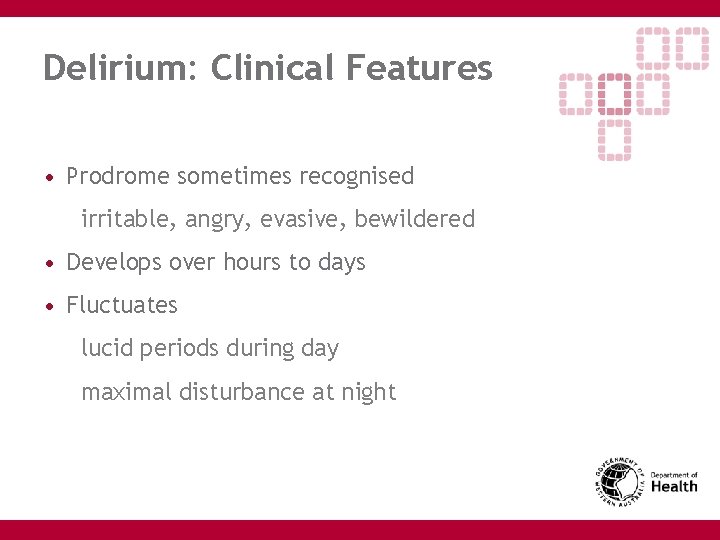
Delirium: Clinical Features • Prodrome sometimes recognised irritable, angry, evasive, bewildered • Develops over hours to days • Fluctuates lucid periods during day maximal disturbance at night

Delirium: Clinical Features • Inattention • Disorientation • Short term memory impairment • Thinking is disordered • Speech rambling and incoherent • Delusions, misperceptions and visual hallucinations • Distress
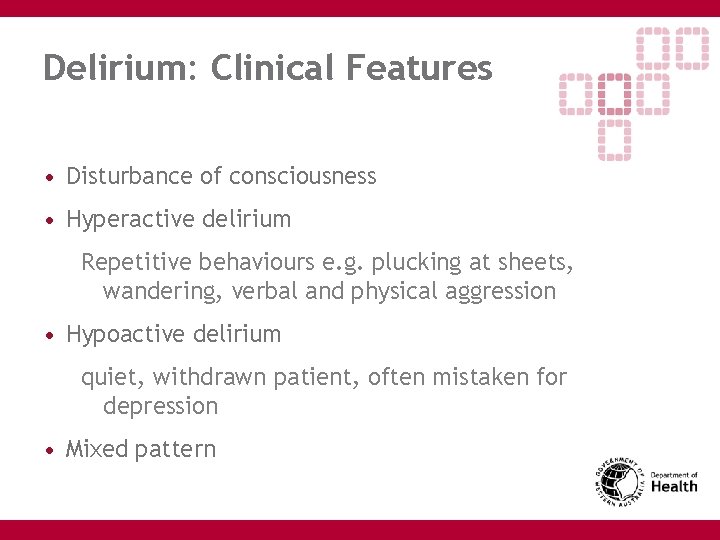
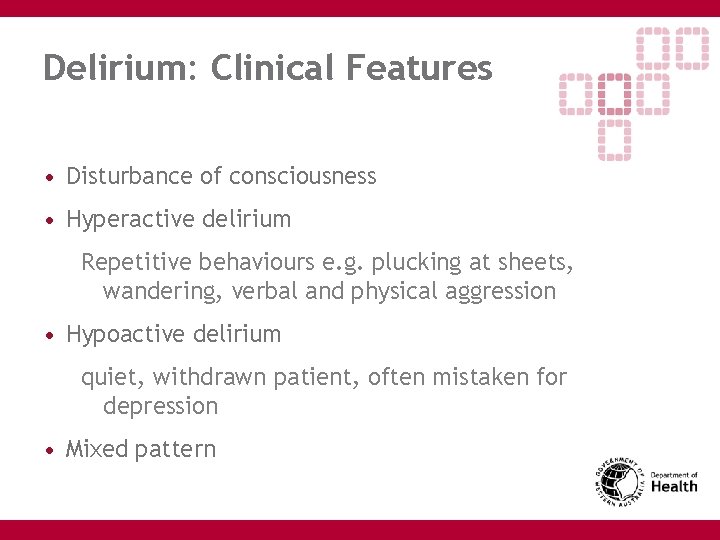
Delirium: Clinical Features • Disturbance of consciousness • Hyperactive delirium Repetitive behaviours e. g. plucking at sheets, wandering, verbal and physical aggression • Hypoactive delirium quiet, withdrawn patient, often mistaken for depression • Mixed pattern
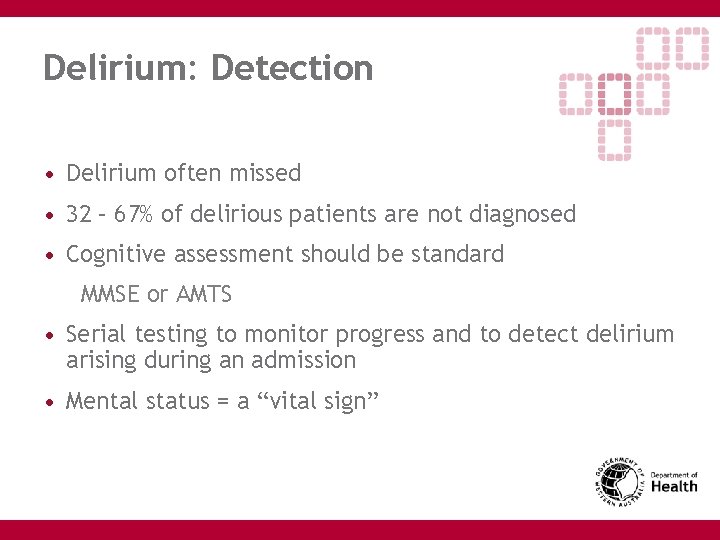
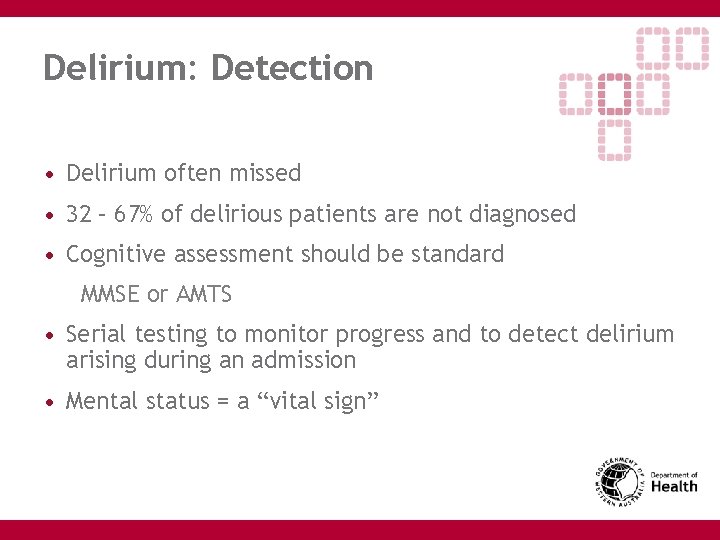
Delirium: Detection • Delirium often missed • 32 – 67% of delirious patients are not diagnosed • Cognitive assessment should be standard MMSE or AMTS • Serial testing to monitor progress and to detect delirium arising during an admission • Mental status = a “vital sign”
Delirium: Detection Confusion Assessment Method (Inouye et al Ann Int Med 1990; 113: 234 -42) 1 Acute onset and fluctuation of cognition AND 2 Inattention with EITHER 3 Disorganised thinking OR 4 Altered level of consciousness
Delirium: Management • Treat underlying causes • Correct dehydration • Review medications • Non Pharmacological • Monitor progress
Delirium: Outcomes Duration • More persistent than previously realised • up to one week in 60% • two weeks in 20% • four weeks in 15% • more than four weeks in 5% • Others report delirium still present at 6 months O'Keeffe S The prognostic significance of delirium in older hospital patients J of the Am Geriatr Soc 1997; 45(2): 174 -8
Delirium: Outcomes Cognitive decline • Early cognitive impairment unmasked by acute illness • May be acute and permanent deficits due to ischaemia, hypoxia or mediated by glucocorticoids or cytokines Francis J Prognosis after hospital discharge of older medical patients with delirium. J Am Geriatr Soc 1992; 40(6): 601 -6

Delirium: Take Home Messages • Common • Distressing • Often Missed • Cognitive testing should be routine • Complex Geriatric Syndrome • Preventable • Predicts adverse outcomes
Falls -Prevention and Management
Definition • “A fall occurs when environmental hazards or demands exceed an individual’s ability to maintain postural stability” Mary Tinetti ASGM ASM 2001
Enormity of the Problem • 33% over 65 yrs fall annually • 50% of these have repeat falls • In nursing homes 50 -65% fall annually • 10 -15% of falls result in serious injury • 1% hip fracture rate
Breakdown of Discussion • Falls in community dwelling elderly • Compliance problems • Unanswered questions
Modifiable Risk Factors for Falls in the Community • Psychotropic drugs – especially benzodiazepines • Multiple drugs • Postural Hypotension • Environmental hazards • Vision • Poor balance or gait • Poor functioning with ADLs • Footwear

Preventing Falls in the Community • Independence model of care • Screening of home environment by OT / health worker • Psychotropic medication withdrawal • Medication review/ minimization • Appropriate vision aids & footwear • Balance and exercise program • Avoiding Injury - Treating Osteoporosis

Falls Clinic Process Multidisciplinary- everyone assessed by the following: • Geriatrician- full history, examination, investigation, including osteoporosis workup • Nurse-lying and standing BP, vision, continence, community supports • Physiotherapist- administers Fallscreen, ? need for walking aid, teaches patient to get up off floor, strength and balance exercise program, sets home program, general footwear advice • OT- ADL assessment, 50% get home visit, group education sessions +/- social work assessment for package of care, hostel/ N/H +/- clinical psychologist to address fear of falling or podiatry
Falls Clinic Process Contd. • All new patients discussed at a multidisciplinary meeting at the end of the clinic, and management plan formulated • Length of time attending the clinic approx 6 -10 weeks. • On discharge, given home exercise program • Followed up 4 months following discharge
What about in the Kimberley • No research in remote or Indigenous settings • Moving to single multiskilled professional in metro areas • Can do great functional assessments and improve reversible risk factors • Independence model of care very important
Who Should Have a Comprehensive Falls Assessment? • All older persons to be asked once a year about falls • If 1 fall -GP assessment, and observe the ‘Get up and go” test • Triggers for further assessment >1 fall in last year A fall resulting in injuries Abnormalities in gait or balance Symptoms of dizziness Evidence of a fear of falling

Hip Protectors • Reduce hip fracture rate (by 50%) for those in nursing homes with a high risk of falling • Compliance is problematic- 38 – 57% in various studies
Vitamin D Deficiency and Falls • Causes muscle weakness and probably falls • Leads to osteoporosis and increased risk of fracture • Very common in elderly, community dwelling population (? Indigenous) • Almost universal in residential care • Replacement with calcium reduces fractures in residential care and in those who are deficient in the community
Patient Compliance with Fall Initiatives • Survey in Aust (Whitehead, 2003) 72% reluctant to do exercises 57% reluctant to stop sleeping tablets 43% reluctant to have a home assessment • Campbell, JAGS, 1999 Study demonstrated reduced falls with psychotropic withdrawal program and home based exercises 47% had restarted their psychotropics within 1 mth

Patient Compliance with Fall Initiatives • Simpson UK study investigated barriers to a falls program The elderly patients involved had reduced understanding of the benefits of exercise Home visits were considered intrusive, and felt that there was inadequate negotiation about the necessary changes resulting in resentment
Summary • Falls are a hallmark of the frail elderly • Falls are usually multifactorial in origin • DON’T be pessimistic- multidisciplinary treatment can prevent up to 60% of falls • The elderly have the most to gain by treating their osteoporosis

Immobility
How to avoid it? • Encourage functional mobility • Educate family and carers • Early rehabilitation • Appropriate use and maintenance of mobility aids • Physiotherapy if possible
Management of the Immobile Patient • Ensure no reversible causes can be identified • Encourage Independence within limits of mobility
Avoiding Pressure Ulcers • Regular assessment of bony prominences • Regular turning to relieve pressure – ideally 2 hourly • Use pillows if no air mattresses available • Avoid friction and shearing forces (safe manual handling) • Skin Hygeine and Moisture • Leave blisters intact • Get help early – for example Donna Angel at RPH will advise
Urinary Incontinence in the Elderly
Incontinence in the Elderly • Prevalence in community dwelling elderly -women 30% -men 15% • 60% of nursing home residents • Risks -parity (association is weak in women over 65 yrs) -hysterectomy -obesity

Continence requires: • Adequate mobility • Mentation • Motivation • Manual dexterity • Intact lower urinary tract function
Medical Complications • Rashes • Pressure ulcers • UTI • Falls • Fractures
Psychosocial complications • Embarrassment • Stigmatisation • Isolation • Depression • Institutionalisation risk

A Normal Bladder • First urge to void occurs when bladder volume is 150 – 300 mls • Normal bladder volume 300 – 600 mls • Bladder capacity declines with age and post void bladder volumes increases (up to 50 – 100 mls) • Involuntary bladder contractions also increase with age • Lose the ability to concentrate urine at night (ADH secretion) with nocturia 1 – 2 x)

Causes of Transient Incontinence • Delirium • Infection (symptomatic UTI) • Atrophic vaginitis/ urethritis • Pharmaceuticals • Psychological • Excessive urine output • Restricted mobility • Stool impaction
Drugs Affecting Continence • Diuretics • Anticholinergics • Psychotropics • ACE inhibitors (cough) • Narcotics • Alpha blockers (urethral relaxation) • B agonists (retention) • Calcium channel blockers (retention)
Persistent Incontinence -Stress • Involuntary loss of urine (usually small amounts) with increases in intra- abdominal pressure (coughing, sneezing, laughing, exercising) • In women, causes include lack of oestrogen, obesity, previous vaginal deliveries, previous surgery • In men (rare) causes include radiotherapy and prostatectomy.
Persistent Incontinence -Urge • Leakage of urine (larger volumes) due to inability to delay voiding after sensation of bladder fullness is felt • Associated symptoms include nocturia, urinary frequency • Causes Ideopathic (Detrusor overactivity) Local pathology- tumour, stone, diverticuli, outflow obstruction CNS disorders- stroke
Detrusor hyperactivity with Impaired Contractility (DHIC) • A subset of patients will have this, emptying less than 1/3 of bladder volume • Are predisposed to urinary retention
Persistent Incontinence -Overflow • Leakage of urine (small amounts) resulting from mechanical forces on an overdistended bladder • Causes Anatomical obstruction by prostate, stricture, cystocoele Acontractile bladder associated with diabetes or spinal cord injury Medication related
Assessment • History Characteristics of incontinence Medical problems, medications, bothersomeness • Bladder chart • Examination General- esp CCF, venous insufficiency Abdominal PR lumbosacral innervation In women- inspect for prolapse, cough test, atrophic vaginitis Assessment of mental state and mobility
Assessment • Urinalysis the relationship of asymptomatic bactiuria with incontinence is controversial. No benefit from treating the nursing home population ? Eradicate bactiuria once and assess it effect on incontinence • Post Void Residual Volume – Important to rule out significant retention <100 mls normal >200 mls abnormal
Assessment- selected patients • Urine culture, cytology • Blood glucose, calcium, renal function • Abdominal ultrasound • Urodynamics Recent data suggest that it has little clinical utility in urge incontinence
Management • Supportive measures • Education • Environmental changes eg toilet light on • Use of toilet substitutes eg bottle, commode • Modification of fluid intake patterns • Alcohol, caffeine avoidance • Management of constipation • Smoking cessation, treatment of cough
Management- Behavoural • Pelvic floor exercises- useful for urge and stress incontinence • Bladder Retraining Urge incontinence Progressive lengthening of intervoiding interval
Management- Behavoural Institutionalised patients • Scheduled toiletting- 2 hrly during day, 4 hrly at night • Habit training- variable schedule depending on patients voiding patterns • Prompted toiletting- prompted to toilet 2 hrly, only toiletted on request, positive reinforcement (25 40% of nursing home residents respond)
Management Urge Incontinence- Drugs • Anticholinergics eg. Oxybutinin 2. 5 - 5 mg tds have 60 – 70% reduction in frequency of incontinence episodes Probably work via afferent pathways S/Es: dry mouth, constipation, confusion, urinary retention • Oestrogen vaginal cream 0. 5 -1 g nightly for 1 month, then 2 -3 x/ week (NB oral oestrogens worsened incontinence in the WHI study)

Management Stress Incontinence- Drugs Little role for medications Imipramine 25 -50 mg tds (anticholinergic as well, so there is an argument for using it for mixed urge/ stress incontinence) Efficacy date is lacking, though and has side effects ++ in elderly Duloxitene- serotonin and noradrenaline reuptake inhibitor (results in 50 -54% reduction in frequency of incontinence). Causes initial nausea
Management of Overflow Incontinence Catheter if significant retention then: Refer to urology who may advise medication and or surgery Drugs - Prazosin, Tamsulosin, Terazosin

Management- other strategies • Surgery - TURP - Bladder neck elevation, peri-urethral collagen injections • Catheters- IMCs, IDCs • Botulinum toxin injection into detrusor muscle or bladder neck • Continence pessaries- for women with large prolapses when surgery is contraindicated • Desmopressin for large volume nocturia
Iatrogenic Problems

Polypharmacy
Objectives • Understand why Polypharmacy is common in older people • Identify the problems caused by polypharmacy in older people • Monitor and manage Polypharmacy • Understand inappropriate versus appropriate Polypharmacy
The Challenge of Geriatric Clinical Pharmacology ‘to balance an incomplete evidence base for efficacy in frail, older people against the problems related to adverse drug reactions without denying older people potentially valuable pharmacotherapeutic interventions’ Le Couter et al
Polypharmacy • 5 or more drugs • 20 -40% of older people
Causes of Polypharmacy • Comorbidities • Age • Prescriber (what influences prescribers? ) • Reluctance to cease another prescriber’s prescription • ‘Rational Polypharmacy’
Risks of Polypharmacy • Adverse drug reactions common cause of hospital admission morbidity and mortality • Falling, delirium and the other geriatric syndromes may be drug-related • Medication errors polypharmacy, per se, appears to be a risk factor for adverse outcomes
What are the goals of care? • Often different in frail person • Risks of polypharmacy higher in frail person with limited homeostatic reserve Eg antihypertensives

Weigh risks and benefits • Efficacy • Risk of ADR • Pt wishes
Common difficult areas • Include Benzodiazepine and psychotropic polypharmacy • Antihypertensives Medication Withdrawal Can be Achieved

Is Discontinuation Safe? • Psychotropic withdrawal reactions • Anti anginals • Anticonvulsant medications
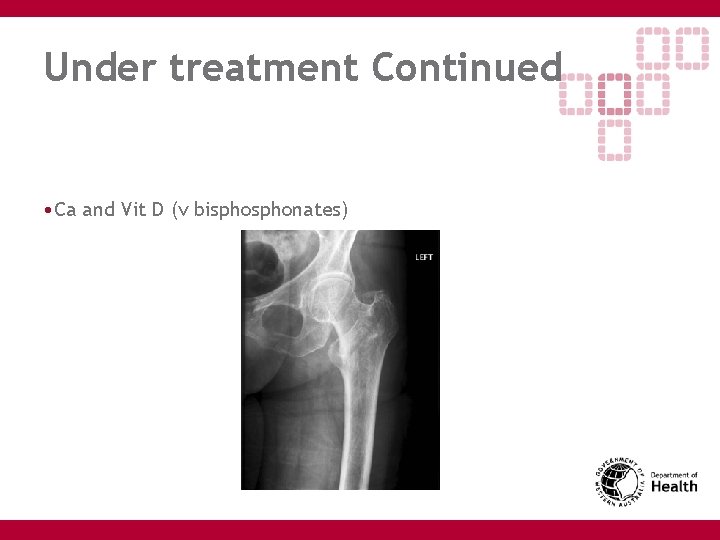
Other Difficult Areas - Under treatment • Analgesics • Osteoporosis therapy (Anticoagulants) (ACE-inhibitors and B-blockers)
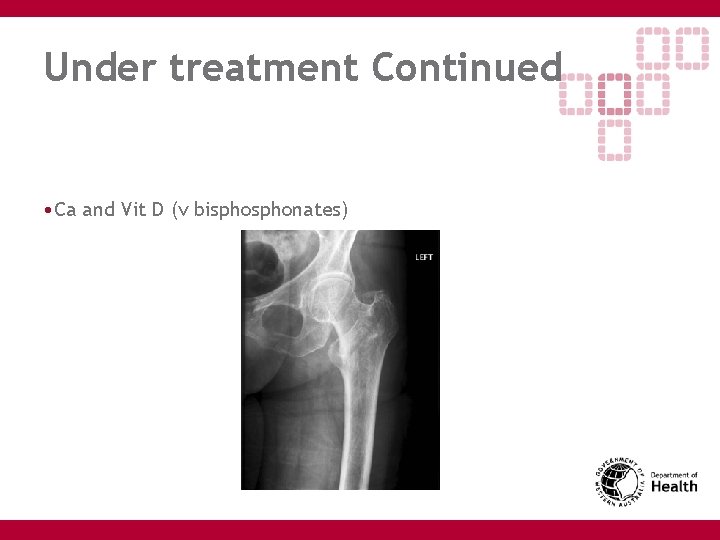
Under treatment Continued • Ca and Vit D (v bisphonates)
Reviewing Medications • View and Record all medications, including OTC’s, herbs, dietary supplements • Ask about other prescribers • Cautious medication withdrawal where indicated
Use aids • Simplify regimens • Medication cards • Dosette Boxes • ‘Webster Pack’ • Supervised medications • Involving caregivers
Conclusions • Avoid polypharmacy • Weigh risks and benefits • Scrutinise all medication prescriptions critically • Monitor therapy carefully in elderly patients

Malnutrition
Prevalence • Increases with frailty and physical dependance • Estimated 4. 8% recipients of domiciliary aged care clients • 27. 7% Sub-acute crae
Consequences • More GP consultations • More prescriptions • Higher hospital admission rate • Increased risk of: Falls Prolonged hospitalisation Institutionalisation Infections Pressure Ulcers Death

Nutritional Frailty • Disability due to unintentional loss of body weight and sarcopenia • Search for medical causes • Low Socioeconomic status significant risk factor • As are poor health, polypharmacy, low mood, low cognition.
Non Physiological Causes • Social Factors – Poverty, Inability to shop, cook or feed • Psychological Factors – Alcohol, Depression, Dementia • Medical Factors – Cancer, Chronic Disease • Medications – Side Effects common

Screening • Two Question Rapid Screen Positive if : Body Mass Index <22 kg/m 2 Weight loss > 7. 5% over 3 months

Management • Treat/Manage reversible causes • Educate individual and family – www. nhmrc. gov. au/publications/synopses/n 23 syn. htm • Oral supplements with macronutrients • Lack of evidence for most vitamin supplements • Ref : Malnutrition in older people - Australian Family Physician Vol 33, No 10 October 2004
 Geriatric giants
Geriatric giants Geriatric giants
Geriatric giants Geriatric giants mnemonic
Geriatric giants mnemonic Dr rose dinda martini
Dr rose dinda martini Dr john ward geriatrician newcastle
Dr john ward geriatrician newcastle Elementary data organization in data structure
Elementary data organization in data structure Donna seymour
Donna seymour Pass and seymour arc fault receptacle
Pass and seymour arc fault receptacle Kelly hoppen facts
Kelly hoppen facts Under the bleachers by seymour butz
Under the bleachers by seymour butz Seymour house dundee
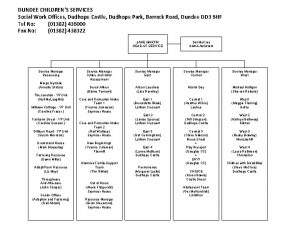
Seymour house dundee William seymour miracles
William seymour miracles Mike seymour manchester
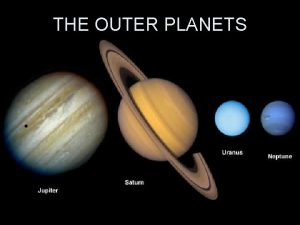
Mike seymour manchester Neptune's atmosphere
Neptune's atmosphere Hundred handed giants greek mythology
Hundred handed giants greek mythology Hundred handed giants greek mythology
Hundred handed giants greek mythology Brokk hammer skin
Brokk hammer skin They might be giants math
They might be giants math They might be giants cells
They might be giants cells Hydrostatic equilibrium
Hydrostatic equilibrium Geriatic giants
Geriatic giants They might be giants periodic table
They might be giants periodic table On the hr diagram red supergiants like betelgeuse lie
On the hr diagram red supergiants like betelgeuse lie Anunnaki planet
Anunnaki planet Standing on the shoulders of giants
Standing on the shoulders of giants Outer planets
Outer planets Giants by lydia pender
Giants by lydia pender Galileo: on the shoulders of giants
Galileo: on the shoulders of giants Palmerston north geriatric
Palmerston north geriatric Geriatric syndrome
Geriatric syndrome Geriatric psychiatry definition
Geriatric psychiatry definition Geriatric hat trick
Geriatric hat trick Geriatric nutrition
Geriatric nutrition Gems diamond geriatric assessment
Gems diamond geriatric assessment Sarc-f
Sarc-f Objectives of elderly care
Objectives of elderly care Dr rose dinda martini
Dr rose dinda martini Community geriatric psychiatry
Community geriatric psychiatry Geriatric competency assessment
Geriatric competency assessment 10:5 meeting the needs of the elderly
10:5 meeting the needs of the elderly Gems diamond geriatric
Gems diamond geriatric What is geriatric syndromes
What is geriatric syndromes Geriatric case presentation
Geriatric case presentation Gems diamond geriatric
Gems diamond geriatric Va geriatric scholars program
Va geriatric scholars program Centrum geriatric
Centrum geriatric Frailty syndrome
Frailty syndrome Palo alto networks certified network security consultant
Palo alto networks certified network security consultant Expert in consultant liaison psychiatrist
Expert in consultant liaison psychiatrist Ellucian2
Ellucian2 Stuart minty planning consultant
Stuart minty planning consultant Test consultant capgemini
Test consultant capgemini Dan rogers it consultant
Dan rogers it consultant Rcem consultant sign off
Rcem consultant sign off Dr gupta stepping hill hospital
Dr gupta stepping hill hospital Mis consultant
Mis consultant Dartos tissue
Dartos tissue Family history consultant training
Family history consultant training Assertivel
Assertivel United states lactation consultant association
United states lactation consultant association Sanjeev sawai
Sanjeev sawai Claudia norman a marketing consultant
Claudia norman a marketing consultant Associate consultant in capgemini
Associate consultant in capgemini Nous hospital consultant
Nous hospital consultant Raeburn forbes
Raeburn forbes Sample legal nurse consultant contract
Sample legal nurse consultant contract Fdot selection results
Fdot selection results Ivan calimani
Ivan calimani Module engineering consultant
Module engineering consultant Open source consultant
Open source consultant Green world international training center
Green world international training center Court security consultant
Court security consultant Ayurvedic lifestyle consultant
Ayurvedic lifestyle consultant Scan based trading consultant
Scan based trading consultant What is a consultant radiographer
What is a consultant radiographer Talent acquisition consultant philips
Talent acquisition consultant philips Wireless communication consultant
Wireless communication consultant Judith james educational consultant
Judith james educational consultant Consultant contract 2003
Consultant contract 2003 Scot rife
Scot rife Reza dorrani
Reza dorrani Internet consultant job description
Internet consultant job description Epicor configurator
Epicor configurator New consultant in casualty
New consultant in casualty Mcts mcitp
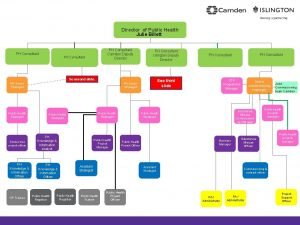
Mcts mcitp Julie billett public health
Julie billett public health Knowledge management consultants
Knowledge management consultants A.s environs ltd is dealing in environment
A.s environs ltd is dealing in environment Modern data architecture consultants
Modern data architecture consultants Partner technical consultant
Partner technical consultant New consultant training
New consultant training Petrophysics consultant
Petrophysics consultant Script for recruiter cold call
Script for recruiter cold call Nous hospital consultant
Nous hospital consultant New consultant training
New consultant training Behavioral genetics consultant
Behavioral genetics consultant Chloe ashford
Chloe ashford Engineers pi is 3
Engineers pi is 3 Acat imt
Acat imt Stuart minty camden planning consultant
Stuart minty camden planning consultant Nutra metrix
Nutra metrix Psychiatrist leicester
Psychiatrist leicester Sustainable tourism consultant jobs
Sustainable tourism consultant jobs Verizon ip centrex
Verizon ip centrex Consultant mediu
Consultant mediu Associate consultant in capgemini
Associate consultant in capgemini độ dài liên kết
độ dài liên kết Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào