HEALTH OF OLDER PEOPLE TEAM HOP TEAM Palmerston


- Slides: 15

HEALTH OF OLDER PEOPLE TEAM (HOP TEAM) Palmerston North Health of Older People (HOP Team) Palmerston North
Why a HOP Team? • To meet the goals of the National Health Strategy - ‘wrap around’ service for older people • Deliver healthcare that is centred on the needs of older people • Work closely with and collaboratively with GPTs, IFHC and community based providers • Minimise inappropriate presentations/admissions to hospital • Keep older adults independent in their own homes for as long as possible • To help GPTs diagnose frailty. • Working alongside Kauri Healthcare enhancing support for the increasing frail elderly
And Why Kauri Health Care? • It has been a 12 month pilot funded by the DHB • Kauri Health Care has 18, 000+ patients and 19 GPs • KHC has merged Vivian Street, Albert Street, Grey Street, Amesbury Street practices and all associated administration under one roof. • It is an Integrated Family Health Centre with a population base that will test and refine the existing HOP Team model.
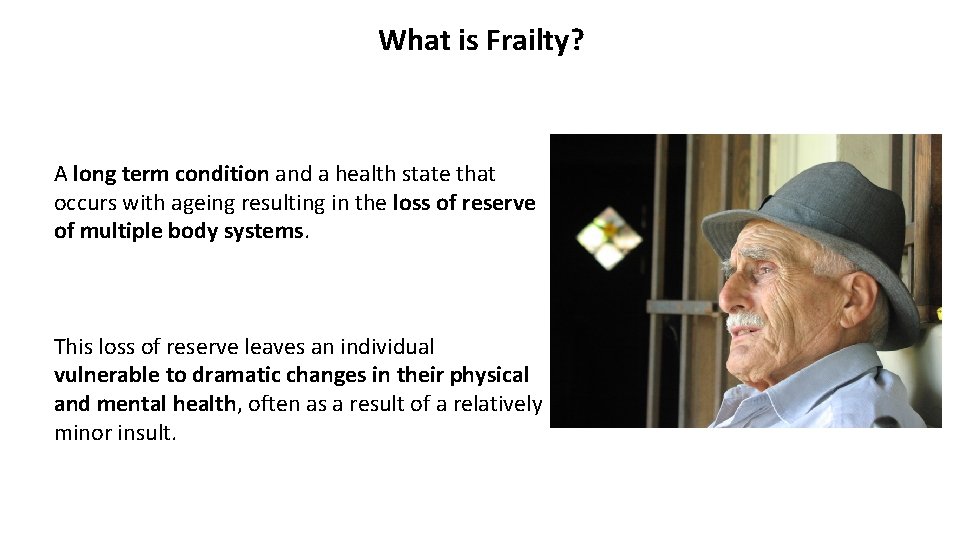
What is Frailty? A long term condition and a health state that occurs with ageing resulting in the loss of reserve of multiple body systems. This loss of reserve leaves an individual vulnerable to dramatic changes in their physical and mental health, often as a result of a relatively minor insult.
Who are the frail elderly? They have moderate to complex age related needs which include: - • Frailty impacting on dependence • Functional decline impacting on dependence • Those who health is unstable (but not acute) who are at risk and present frequently to GPT or ED • They have multiple interacting pathologies • They have polypharmacy issues • And cognitive decline that is impacting on function and behaviour
What helps in the management of frailty? • Person centred care • A Comprehensive Geriatric Assessment and plan • Anticipatory care, EPOA, Advance Care Plan • Integrated health and social care systems • Joint working with GP teams, ambulance, EH, OAMH • Support for carers • Alternatives to hospital
Who sits at the table? • Anne Stapleton • Syed Zaman • Esther Willis • Donna Steven • Jen Haddon • Kate Mc. Kenzie • Fiona Fouhy • Dianne Eade • Alistair Whyte • Fiona Roberts-Wall Clinical Nurse Specialist CNS Consultant Geriatrician GP with special interest (Kauri Healthcare) Clinical Nurse leader (Kauri Healthcare) Occupational Therapist Social Worker Physiotherapist Supportlinks Pharmacist Administration
Key Worker- on this occasion – CNS • Initial assessment • Referral on to other team members as indicated by the patients need. • Ongoing phone discussions. Geriatrician • Medical Assessment – pain issues and medication adjustments – liaison with GP in respect of these. Occupational Therapist • Provided chair raiser • Problem solved alternate ways of doing household tasks • Provided threshholdramps to access Miss Green Social Worker • Assisted with Disability Allowance for medications, heating and lawns/gardens. • Mobility Parking Card • End of Life Planning – completed Advance Directive • Assisted locating historical EPOA and the lawyer who held this • Discussion held round end of life concerns. Physiotherapist Had discussions with Miss Green re management of pain and mobility through access to hydrotherapy. Encourage proper of walking frame.
Why it works…. . • We each hold a piece of the jigsaw • Engage with each other at weekly meetings • Up to 12 disciplines available to work together • Give informal advice to GPT reducing referrals • Less gaps for clients to fall through • Share patients’ history with different disciplines • Learning for everyone • Every patient has a ‘key worker’ – the most appropriate discipline
Referral Criteria • Enrolled with KHC • 75 yrs+ or 65+ for Maori and Pacific Island • Patient/Carer consent • Moderate to complex age related needs, including but not limited to: v. Change in function – mobility and/or ADLs v. Complex social issues v. Suspected diagnosis of dementia v. Falls v. Frailty
Exclusions: • Non Kauri Health Care IFHC patient • Primary need is for Older Adult Mental health input e. g. behavioural and psychological symptoms of dementia • A need for urgent assessment • End of Life Care – patient is under Palliative Care
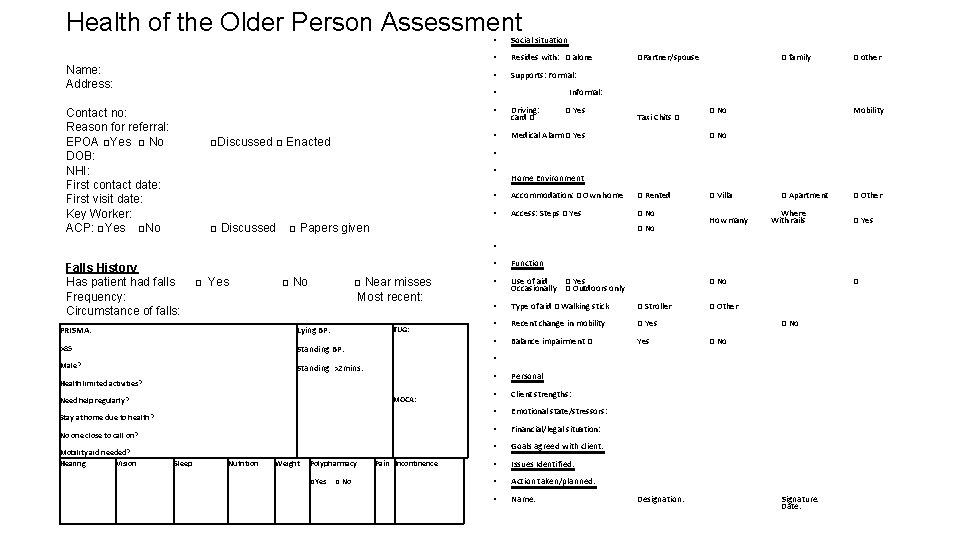
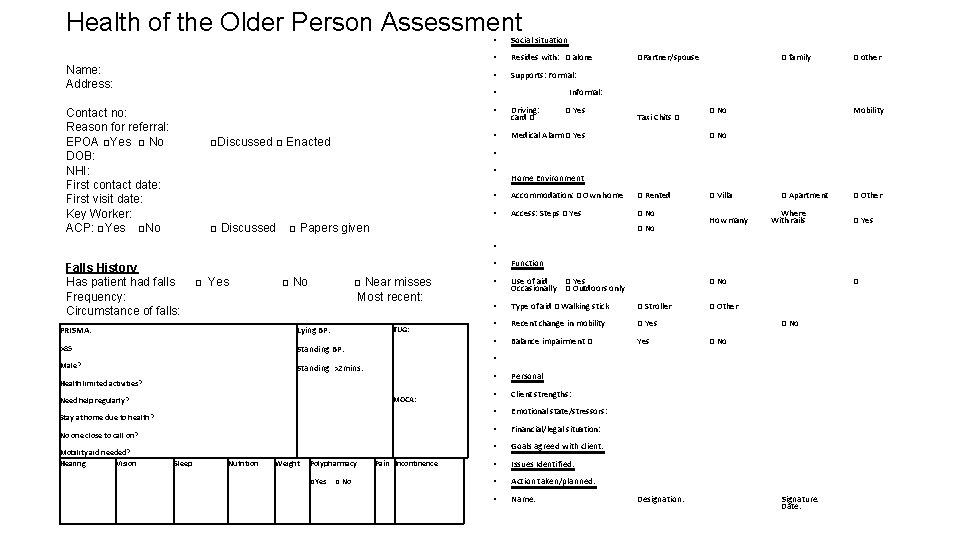
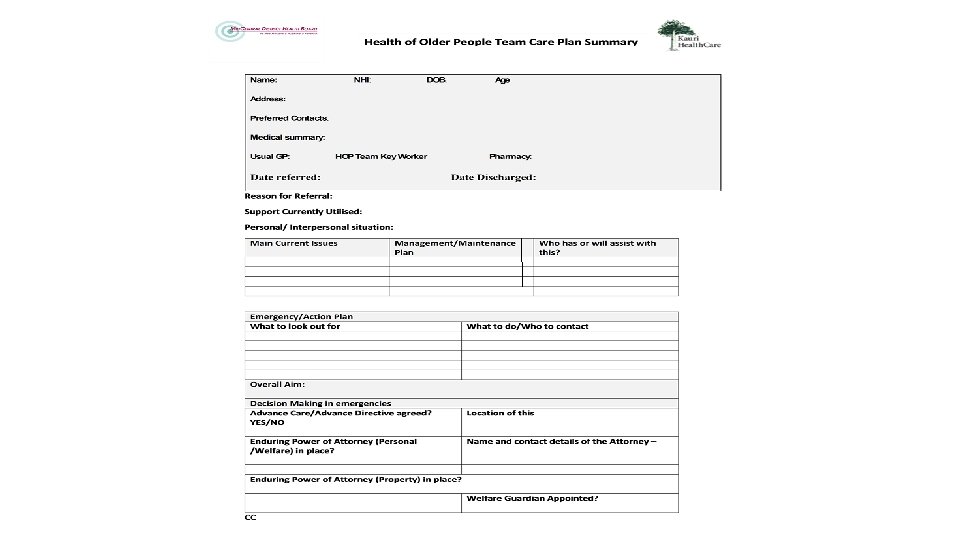
Health of the Older Person Assessment Name: Address: Social situation • Resides with: □ alone • Supports: Formal: • Contact no: Reason for referral: EPOA □Yes □ No DOB: NHI: First contact date: First visit date: Key Worker: ACP: □Yes □No □Discussed □ Enacted □ Discussed □ Yes Driving: card □ • Medical Alarm □ Yes • □ Near misses Most recent: Lying BP: TUG: >85 Standing BP: Male? Standing >2 mins: Health limited activities? Need help regularly? MOCA: Stay at home due to health? No one close to call on? Nutrition Weight Polypharmacy Taxi Chits □ Pain Incontinence □Yes □ No □ family □ other □ No Mobility □ No Home Environment • Accommodation: □ Own home □ Rented □ Villa • Access: Steps □ Yes □ No Where How many With rails □ Yes □ No □ □ No PRISMA: Sleep □ Yes □ Papers given □ No □Partner/spouse Informal: • • Falls History Has patient had falls Frequency: Circumstance of falls: Mobility aid needed? Hearing Vision • • • Function • Use of aid □ Yes Occasionally □ Outdoors only • Type of aid □ Walking stick □ Stroller • Recent change in mobility □ Yes • Balance impairment □ Yes • • Personal • Client strengths: • Emotional state/stressors: • Financial/legal situation: • Goals agreed with client: • Issues Identified: • Action taken/planned: • Name: □ Apartment □ Other □ No Designation: Signature: Date: □ Other
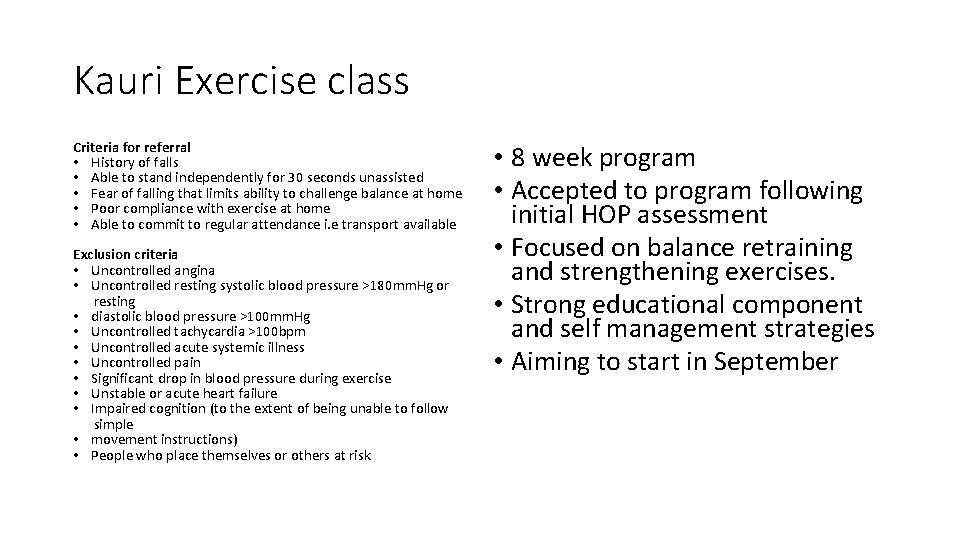
Kauri Exercise class Criteria for referral • History of falls • Able to stand independently for 30 seconds unassisted • Fear of falling that limits ability to challenge balance at home • Poor compliance with exercise at home • Able to commit to regular attendance i. e transport available Exclusion criteria • Uncontrolled angina • Uncontrolled resting systolic blood pressure >180 mm. Hg or resting • diastolic blood pressure >100 mm. Hg • Uncontrolled tachycardia >100 bpm • Uncontrolled acute systemic illness • Uncontrolled pain • Significant drop in blood pressure during exercise • Unstable or acute heart failure • Impaired cognition (to the extent of being unable to follow simple • movement instructions) • People who place themselves or others at risk • 8 week program • Accepted to program following initial HOP assessment • Focused on balance retraining and strengthening exercises. • Strong educational component and self management strategies • Aiming to start in September

Questions?