The Three Ds Depression Dementia and Delirium A








- Slides: 76

The Three D’s: Depression, Dementia, and Delirium A Learning Module for Effective Social Work Practice with Older Adults Dr. Robin P. Bonifas, MSW, Ph. D Arizona State University School of Social Work
Acknowledgements The development of this curriculum module was made possible through a Gero Innovations Grant from the CSWE Gero-Ed Center's Master's Advanced Curriculum (MAC) Project and the John A. Hartford Foundation.
Overview § Rationale for learning about older adults and the three D’s. § Overview of the three D’s: § Symptoms § Epidemiology § Assessment tools § Cultural considerations related to populations of the Southwest § Differential diagnosis of the three D’s.
Why Learn about Working with Older Adults? § The demographic imperative. § Older adults are the fastest growing segment of the population. § Among older adults, those age 85 and over are the fastest growing group. § Illness, cognitive decline, and mental health issues are not normal manifestations of aging, however, the incidence of these conditions increases with age.
Why Learn about Working with Older Adults? § Bottom Line: § The largest growing segment of the population, the oldest-old, is also most likely to experience stressful health and mental health conditions, which often bring them in contact with social work practitioners.
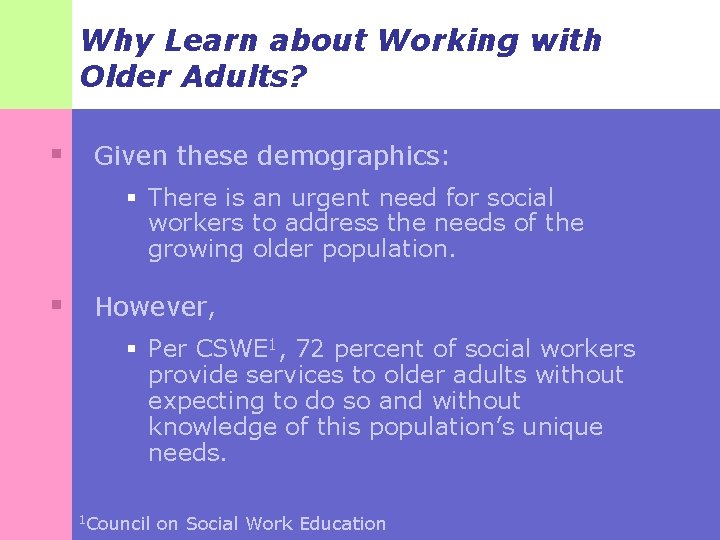
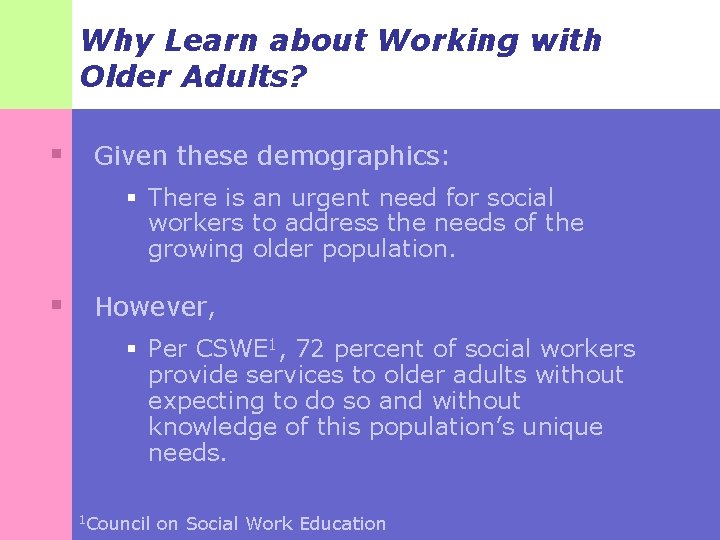
Why Learn about Working with Older Adults? § Given these demographics: § There is an urgent need for social workers to address the needs of the growing older population. § However, § Per CSWE 1, 72 percent of social workers provide services to older adults without expecting to do so and without knowledge of this population’s unique needs. 1 Council on Social Work Education
Why Learn about Working with Older Adults? § As ethical and competent practitioners, it is important to prepare ourselves for effective practice with client groups we are likely to serve. § These next slides illustrate the projected growth of the population over 65 in the U. S. and internationally…
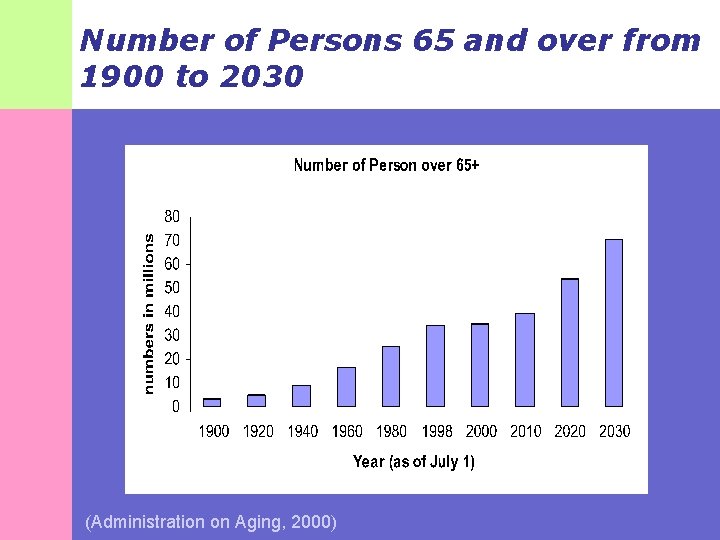
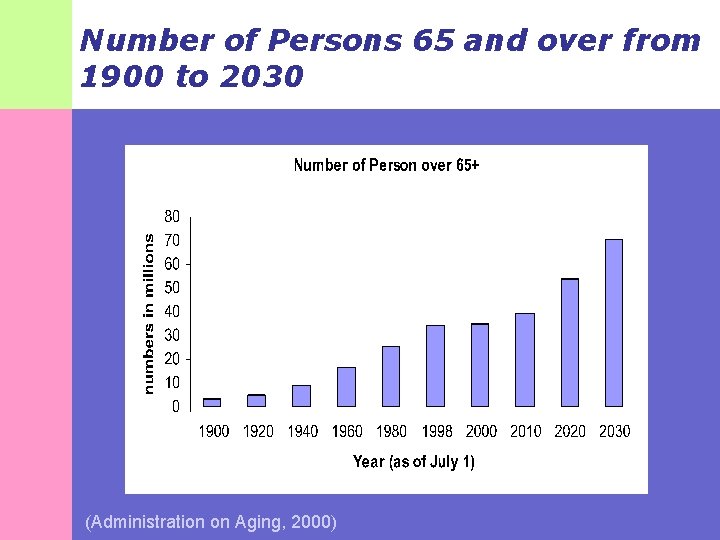
Number of Persons 65 and over from 1900 to 2030 (Administration on Aging, 2000)

Number of Persons 85 and Over 1900 to 2050 (U. S. Census Bureau, 1996)
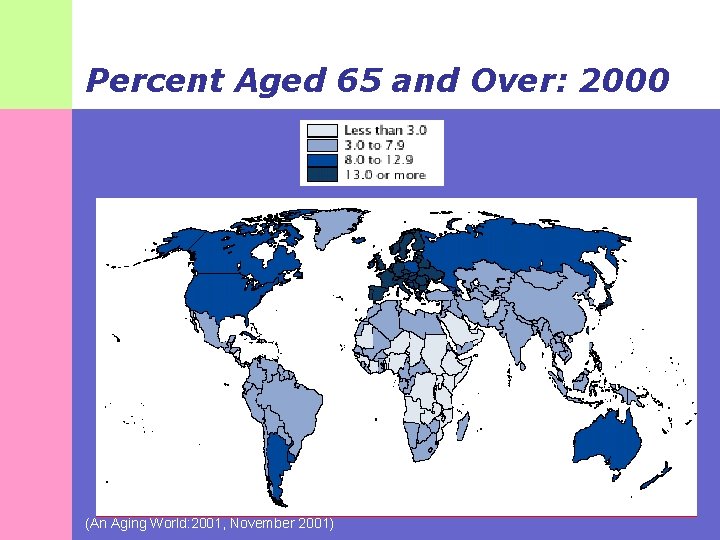
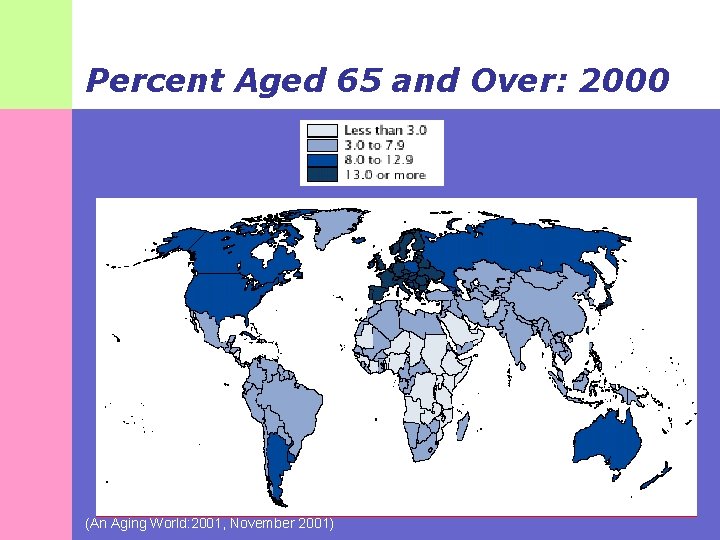
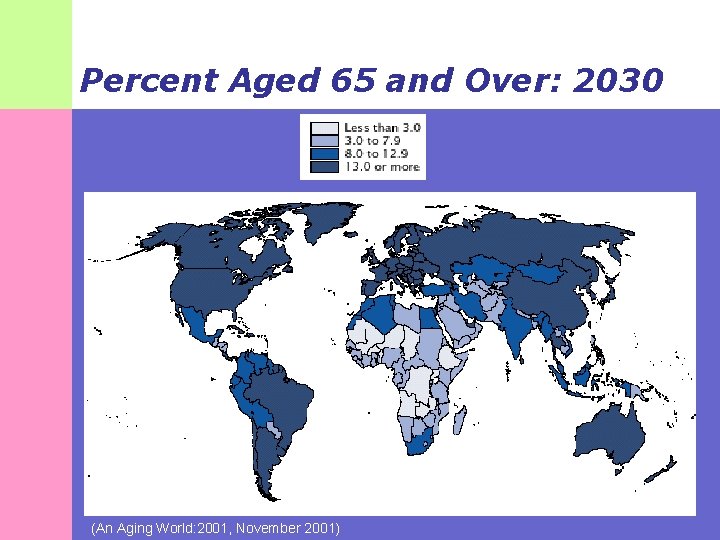
Percent Aged 65 and Over: 2000 (An Aging World: 2001, November 2001)
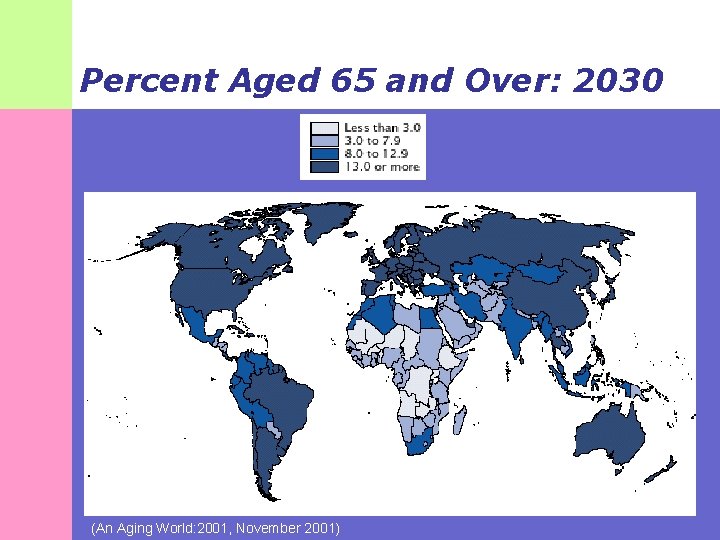
Percent Aged 65 and Over: 2030 (An Aging World: 2001, November 2001)
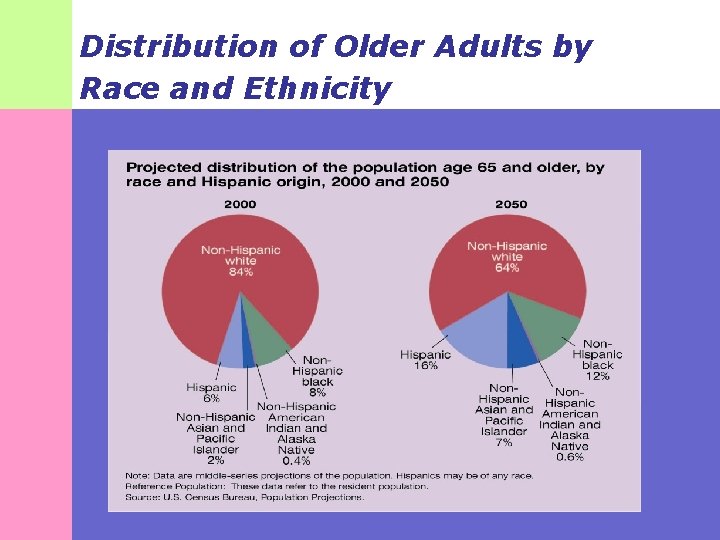
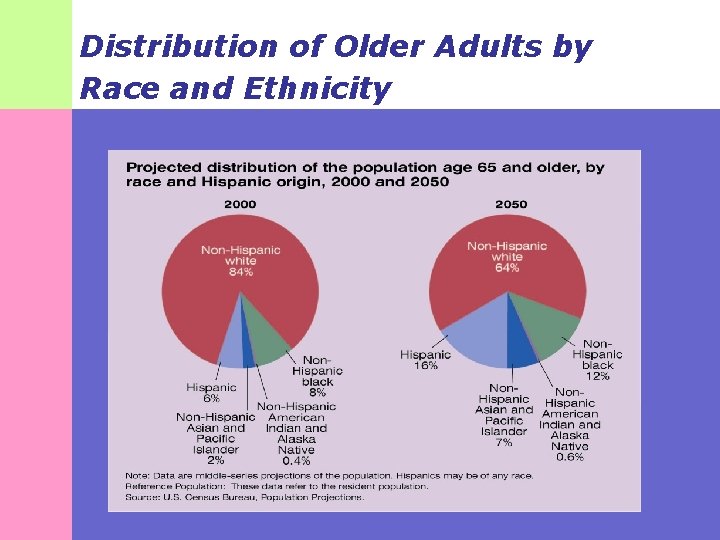
Distribution of Older Adults by Race and Ethnicity
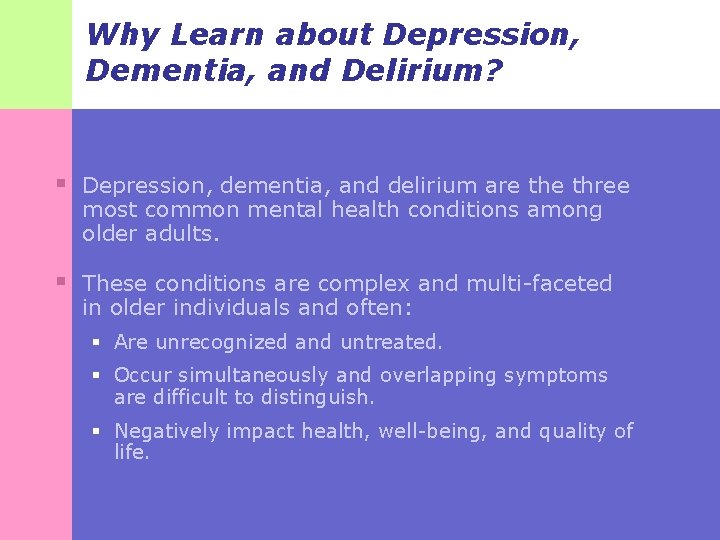
Why Learn about Depression, Dementia, and Delirium? § Depression, dementia, and delirium are three most common mental health conditions among older adults. § These conditions are complex and multi-faceted in older individuals and often: § Are unrecognized and untreated. § Occur simultaneously and overlapping symptoms are difficult to distinguish. § Negatively impact health, well-being, and quality of life.
The Three D’s §Symptoms §Epidemiology §Assessment Tools §Cultural Considerations

Depression in Older Adults
Depression: Symptoms § You are probably fairly familiar this point with the symptoms of depression … § However, depression manifests differently in older adults than it does in younger populations. § This section reviews the symptoms of depression, highlighting common differences specific to older adults.
Depression: Symptoms § Three types of symptoms: § Mood § Physical § Cognitive
Depression: Mood Symptoms § Sadness § In older adults, sadness may be denied -many complain of bodily aches and pains, rather than admitting to their true feelings of sadness. § Loss of interest and pleasure in usual activities. § Irritability § This is especially common in older adults.
Depression: Physical Symptoms § Abnormal appetite with weight loss or weight gain. § Abnormal sleep § Difficulty falling asleep, frequent awakenings during the night or very early morning awakening. § Fatigue or loss of energy. § Psychomotor retardation or agitation.
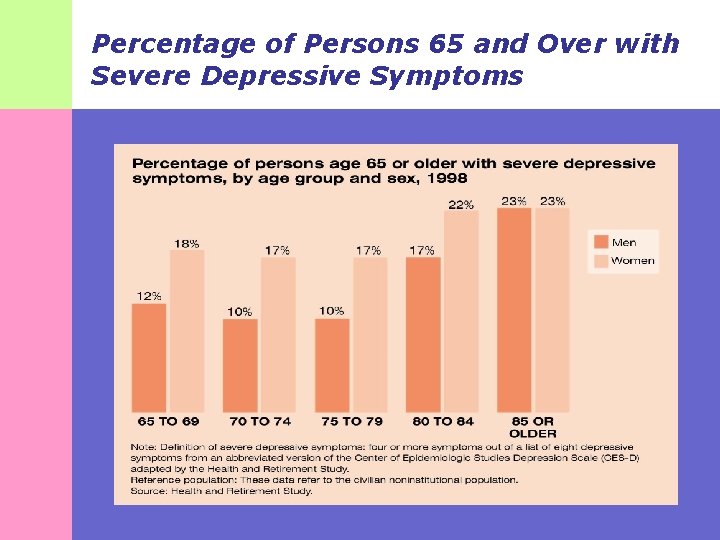
Depression: Cognitive Symptoms § Abnormal self-reproach or inappropriate guilt. § Abnormal poor concentration or indecisiveness. § The term “abnormal” here and on the previous slide means different from the individual’s usual functioning. In other words, “abnormal for him or her. ” § Morbid thoughts of death (not just fear of dying or thoughts about death) or suicide. § The next slide exhibits the incidence of depression by gender and age group …
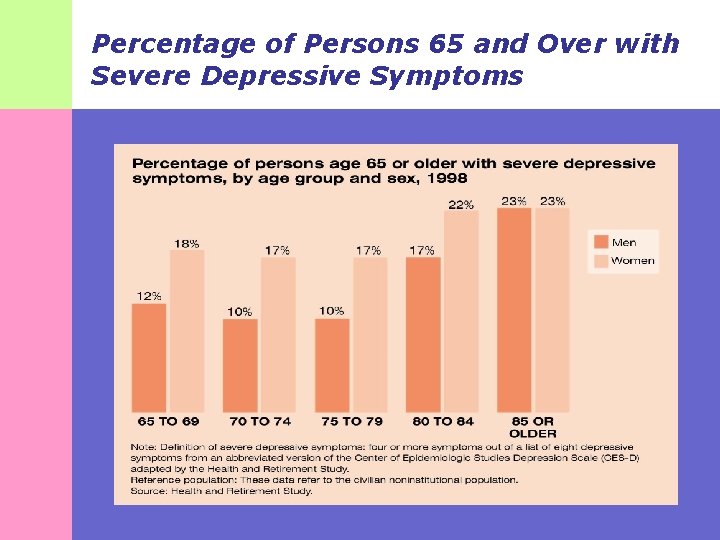
Percentage of Persons 65 and Over with Severe Depressive Symptoms
Depression: Epidemiology § Of particular concern to social workers … § … the incidence of depression is higher among older adults in clinical settings. § For example, depressive symptoms occur in: § 15 to 20 percent of community-based elders. § 37 percent of elders in primary care settings. § 50 percent of elders in long-term care settings.
Depression: Epidemiology § Among older adults: § Depression is associated with increased mortality and morbidity rates. § The incidence of depression increases in conjunction with medical conditions (Conwell, 1994). § Depression can lead to increased mortality from other diseases such as heart disease, myocardial infarction, and cancer (U. S. Dept. of Health and Human Services, 1997).

Depression: Epidemiology § Among older adults untreated depression may also result in: § Increased substance abuse. § Slowed recovery from medical illness or surgery. § Malnutrition. § Social isolation (Katz, 1996).
Depression: Epidemiology § One of the most troubling outcomes of depression is elder suicide. § Older adults have the highest risk of suicide of any age group. § The suicide rate for individuals aged 85 and older is the highest at about 21 suicides per 100, 000 people. § Studies reveal that single, white, elderly males have the highest rate of suicide and are more likely to succeed than their female counterparts.
Cultural Considerations: Native Americans § Among Native Americans: § Depression rates may be four to six times higher than the general population (Manson, Shore, & Bloom, 1985). § Higher rates of depression are also noted compared to other racial/ethnic groups (Grant & Hasin, 2005). § Native Americans typically do not seek treatment for depression, although symptoms may be present. § Depression is the most frequently diagnosed problem among those who do seek treatment from mental health clinics (Manson et al).
Cultural Considerations: Native Americans § Diagnosis complicated by co-occurrence with: § Substance abuse § Physical illness § Prolonged grief § Historical trauma § Acculturation stress § Death of friends and loved ones § Cultural differences in social interaction styles § Indigenous forms of illness (Manson et al, 1985).
Cultural Considerations: Native Americans § Diagnosis must consider this population’s world view in order to facilitate effective mental health care. § Symptoms are likely to be expressed as cultural metaphors such as: § “Heavy heart” § Self esteem problems § Lack of balance or harmony § Physical complaints § Just a “normal part of life”
Cultural Considerations: Native Americans § An association exists between depression and cognitive deficits in this population (Verney et al, 2008). § Auditory hallucinations may be present, but are often a cultural phenomenon rather than evidence of pathology. § Example: Hearing voices of deceased family members is common. § High comorbidity with alcoholism, especially among men. § Chronic symptoms of depression are common as evidenced by two or more years of ongoing symptoms (Manson et al, 1985).
Cultural Considerations: Native Americans § DSM-IV diagnostic criteria for depression may not be applicable due to: § Vast differences in tribal beliefs about mental illness. § Cultural labeling of emotions. § Conceptual language differences 1985). (Manson et al. ,
Cultural Considerations: Native Americans § Modifications to DSM-IV diagnostic criteria that may be necessary for this population: § Shorten threshold for duration of sad mood to one week from two weeks. § Assess potential presence of both chronic and major depression. § Clarify date of onset if associated with alcoholism to determine which condition is the precursor. § Assess the content and impact of auditory hallucinations before labeling them as pathological.
Cultural Considerations: Latinos/Hispanics § Latinos/Hispanics have higher rates of depression than Caucasians; this is especially true for women (Markides et al, 1999). § Factors associated with higher levels of depression in this population: § Chronic disease § Dissatisfaction with social support § Living alone § Lower income and education § Lower acculturation (Swenson, Baxter, Shetterly, 2000).
Cultural Considerations: Latinos/Hispanics § Diagnosis must consider this population’s world view in order to facilitate effective mental health care: § Illness is a matter of chance and is not amenable to change. § Espiritismo or spiritual forces are involved, thus remedies must not come from medical or mental health professionals, but from folk healers or prayer. § Mental health difficulties are “God’s will” and need to be endured (Solis-Longoria, 2007).
Cultural Considerations: Latinos/Hispanics § Common mental health related terms and conditions specific to Mexican culture: § Mal de ojo (evil eye) § Son nérvios (being nervous) § Está sufreyendo (suffering) § Susto (being scared) § Un ataque de nérvios (uncontrollable crying, screaming, verbal or physical aggression or suicidal gestures) (Yee, 1997)
Depression: Assessment Tools § Geriatric Depression Scale (GDS) § Cornell Depression Scale for Depression in Dementia § This is appropriate for clients with cognitive deficits (MMSE scores 12 or below) since the GDS requires the ability to respond accurately to yes/no questions. § Center for Epidemiological Studies Depression Scale (CES-D) § Suicide risk assessment
Depression: Assessment Tools § Native Americans § Indian Depression Schedule (IDS) § Center for Epidemiological Studies Depression Scale (CES-D) § Latinos/Hispanics § Geriatric Depression Scale (Various Spanish translations) § Center for Epidemiological Studies Depression Scale (CES-D)
Dementia and Older Adults
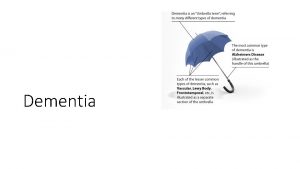
Dementia: Definition § A chronic and progressive loss of intellectual functions severe enough to interfere with everyday life.
Dementia: Symptoms § Include disturbances of multiple higher functions of the brain including: § Memory § Thinking § Orientation § Comprehension § Calculation § Learning capacity § Language and judgment. § Symptoms frequently cause changes in mood, behavior, and personality.
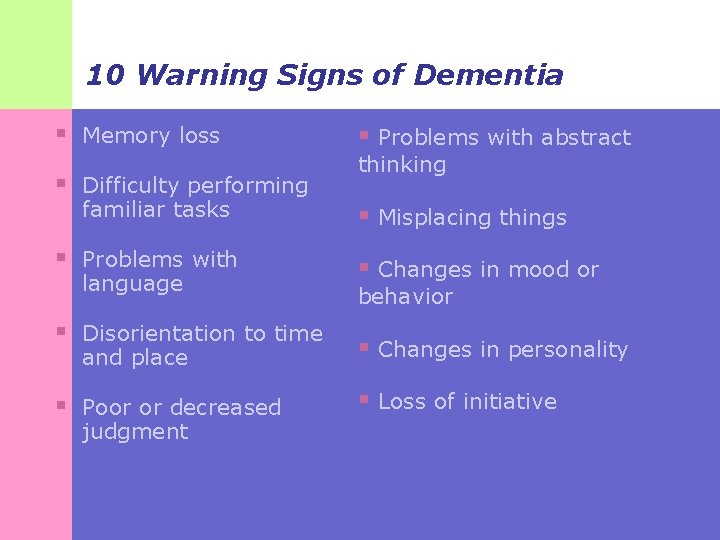
10 Warning Signs of Dementia § Memory loss § Difficulty performing familiar tasks § Problems with language § Disorientation to time and place § Poor or decreased judgment § Problems with abstract thinking § Misplacing things § Changes in mood or behavior § Changes in personality § Loss of initiative
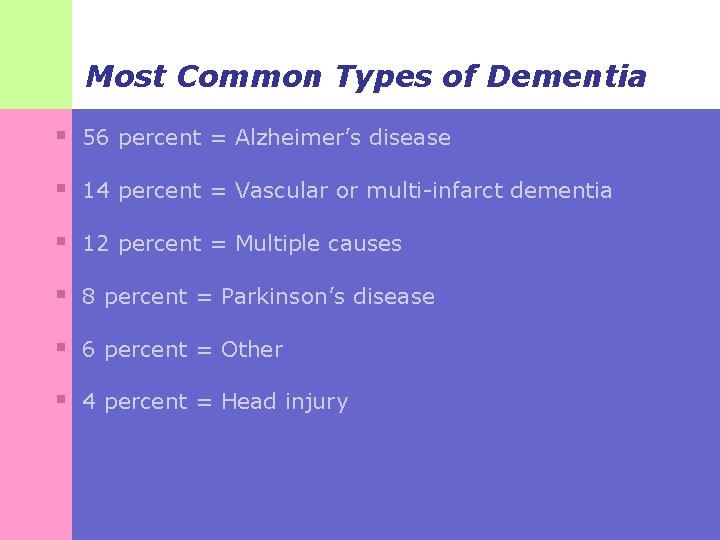
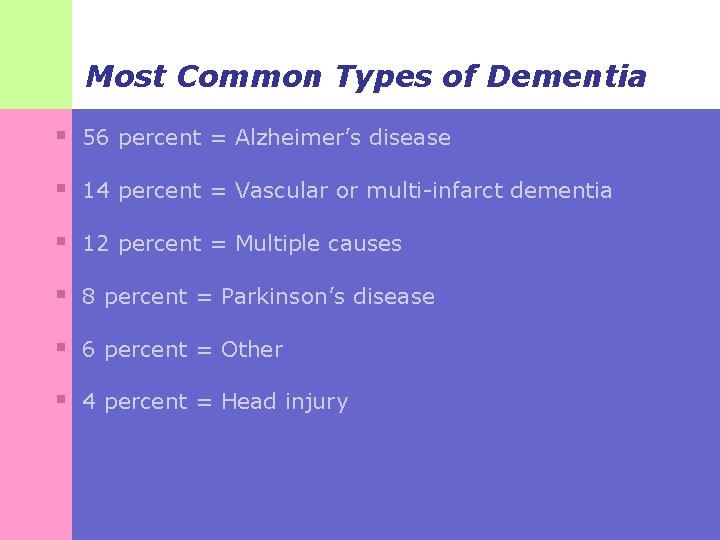
Most Common Types of Dementia § 56 percent = Alzheimer’s disease § 14 percent = Vascular or multi-infarct dementia § 12 percent = Multiple causes § 8 percent = Parkinson’s disease § 6 percent = Other § 4 percent = Head injury
Since Alzheimer’s Disease is the most common type of dementia We’ll focus specifically on it…
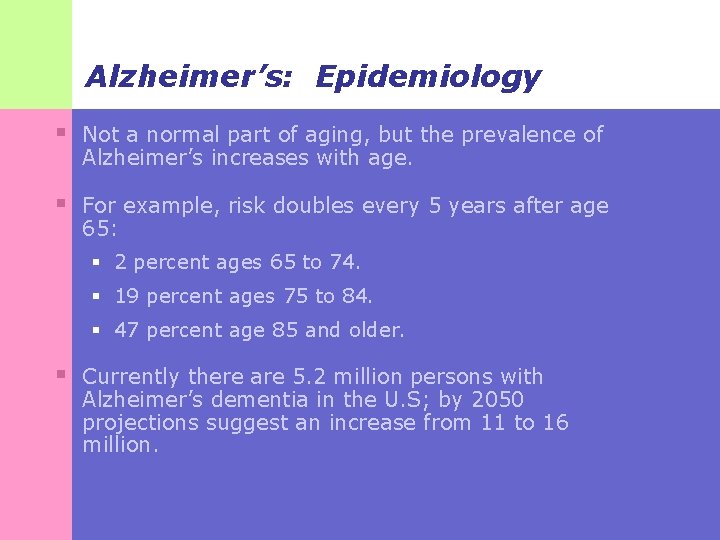
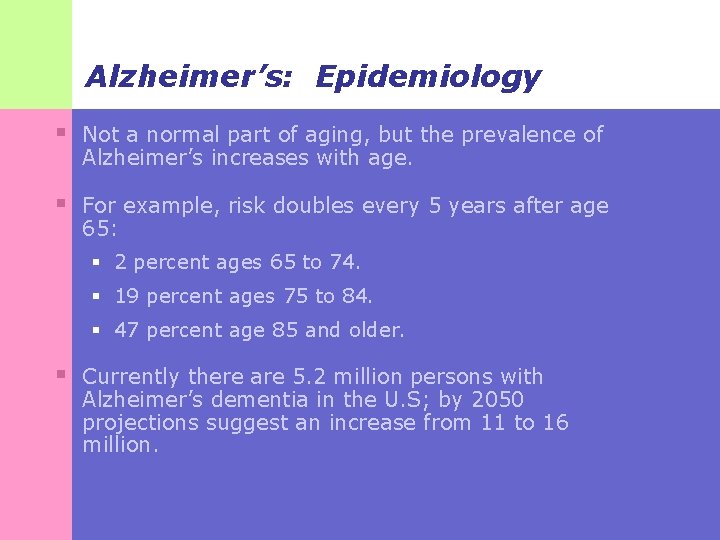
Alzheimer’s: Epidemiology § Not a normal part of aging, but the prevalence of Alzheimer’s increases with age. § For example, risk doubles every 5 years after age 65: § 2 percent ages 65 to 74. § 19 percent ages 75 to 84. § 47 percent age 85 and older. § Currently there are 5. 2 million persons with Alzheimer’s dementia in the U. S; by 2050 projections suggest an increase from 11 to 16 million.
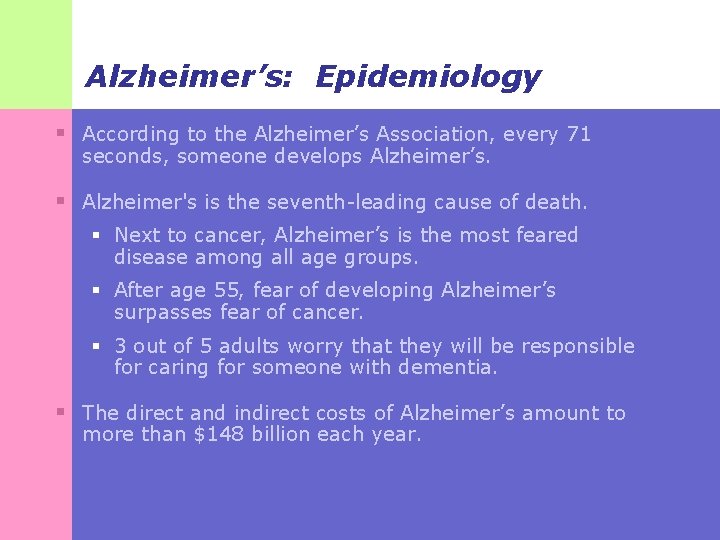
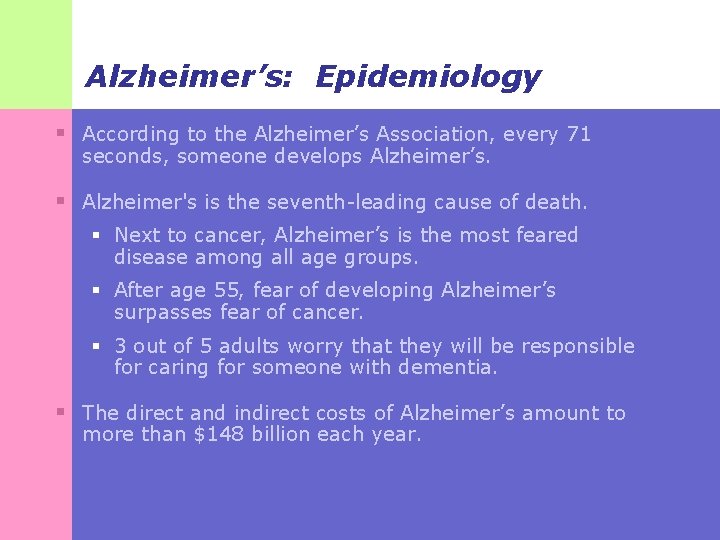
Alzheimer’s: Epidemiology § According to the Alzheimer’s Association, every 71 seconds, someone develops Alzheimer’s. § Alzheimer's is the seventh-leading cause of death. § Next to cancer, Alzheimer’s is the most feared disease among all age groups. § After age 55, fear of developing Alzheimer’s surpasses fear of cancer. § 3 out of 5 adults worry that they will be responsible for caring for someone with dementia. § The direct and indirect costs of Alzheimer’s amount to more than $148 billion each year.
What is Alzheimer’s Disease? § Like all dementias, it is a disease of the brain causing progressive declines in memory. § Results in the loss of intellectual functions severe enough to interfere with everyday life specifically related to: § Thinking § Remembering § Reasoning
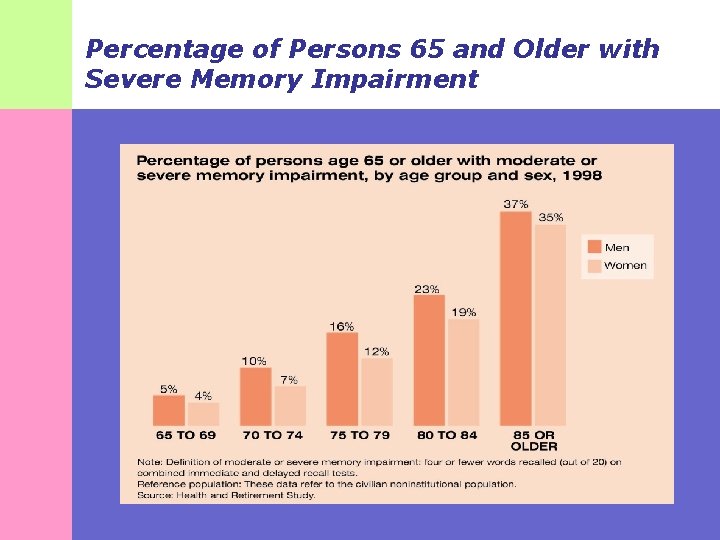
What is Alzheimer’s Disease? § Hallmarks: Begins gradually with individual variation in the rate of progression. § Symptoms: § Forget recent events § Have difficulty performing familiar tasks § Confusion § Personality and behavioral changes § Impaired judgment § Communication difficulties § In late stages, the individual is totally unable to care for him or herself. § The next slide depicts the extent of severe memory impairment by age group…
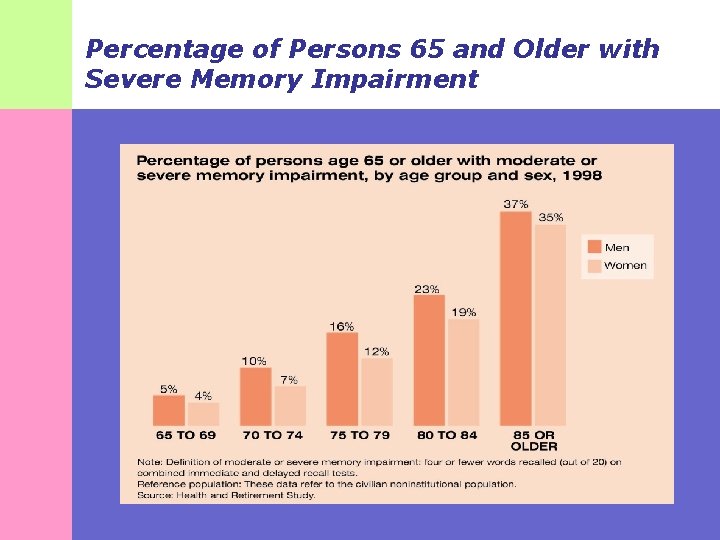
Percentage of Persons 65 and Older with Severe Memory Impairment

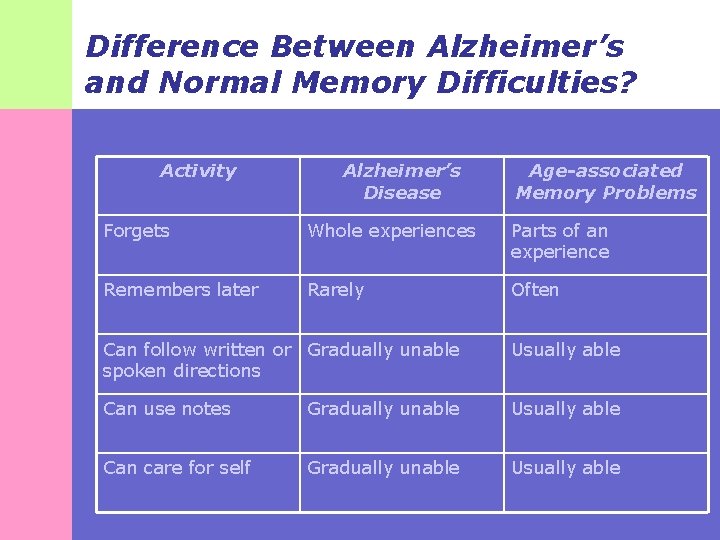
Difference Between Alzheimer’s and Normal Memory Difficulties? § Many older adults fear that minor memory problems they experience may signify Alzheimer’s dementia. § The following slide contrasts the memory problems related to Alzheimer’s dementia with the minor memory problems sometimes associated with aging …
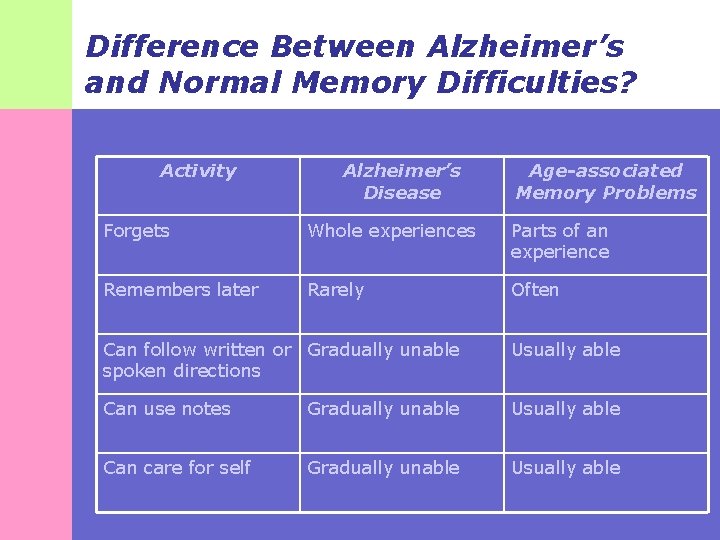
Difference Between Alzheimer’s and Normal Memory Difficulties? Activity Alzheimer’s Disease Age-associated Memory Problems Forgets Whole experiences Parts of an experience Remembers later Rarely Often Can follow written or Gradually unable spoken directions Usually able Can use notes Gradually unable Usually able Can care for self Gradually unable Usually able
Difference Between Alzheimer’s and Normal Memory Difficulties? § An example of forgetting part of an experience with normal memory challenges: You forget where you put your car keys. § How this would present with Alzheimer’s Dementia: You forget what your car keys are for.
Stages of Alzheimer’s disease has recognizable stages: 1. No cognitive impairment 2. Very mild decline 3. Mild cognitive decline 4. Moderate cognitive decline 5. Moderately severe cognitive decline 6. Severe cognitive decline 7. Very severe cognitive decline
Cultural Considerations § Latino/Hispanic Elders § Show symptoms of dementia 5 years earlier than Caucasians and are two times more likely to develop Alzheimer's by age 90. § This earlier presentation may be related to: § Fewer years of formal education. § Higher levels of diabetes, hypertension, and stroke. § Factors associated with dementia § Presence of depressive symptoms § Age 80 and above § History of stroke § Illiteracy (Black & Markides, 1998)
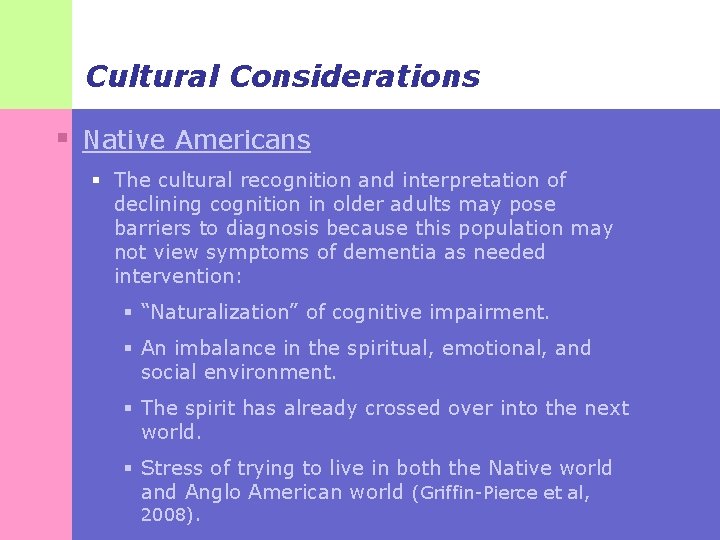
Cultural Considerations § Native Americans § There is limited research on Native populations and dementia, but it is considered to be relatively rare. § Risk levels for developing dementia are mixed: § Decreased due to early mortality… § … but increased due to high rates of stroke, diabetes, and alcohol abuse. § There is currently an absence of culturally appropriate cognitive measures.
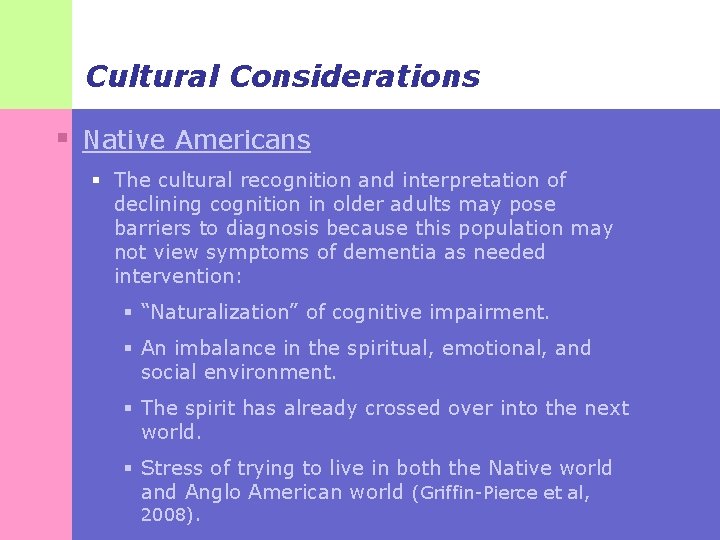
Cultural Considerations § Native Americans § The cultural recognition and interpretation of declining cognition in older adults may pose barriers to diagnosis because this population may not view symptoms of dementia as needed intervention: § “Naturalization” of cognitive impairment. § An imbalance in the spiritual, emotional, and social environment. § The spirit has already crossed over into the next world. § Stress of trying to live in both the Native world and Anglo American world (Griffin-Pierce et al, 2008).
Alzheimer’s: Assessment § There is no absolute method for diagnosing Alzheimer’s dementia other than autopsy. § The clinical diagnosis of this condition is accomplished by ruling out other potential causes of cognitive decline.
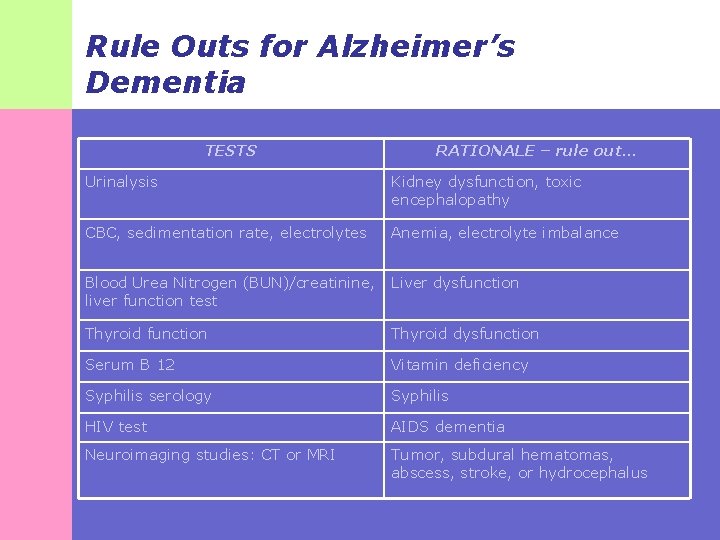
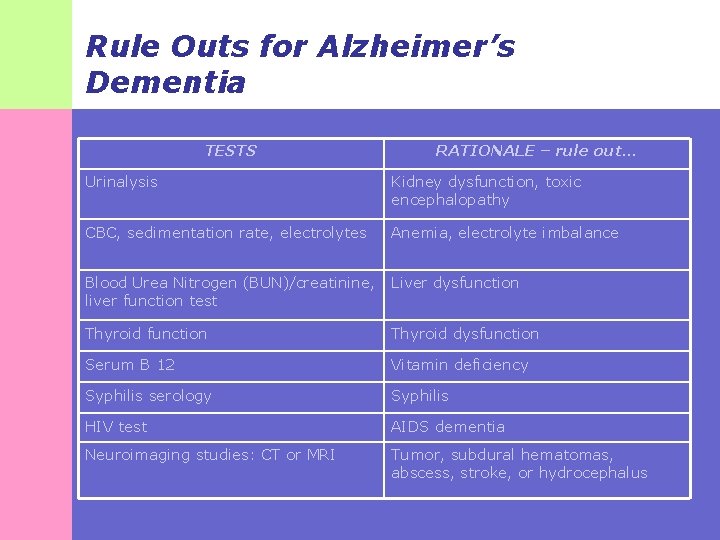
Rule Outs for Alzheimer’s Dementia TESTS RATIONALE – rule out… Urinalysis Kidney dysfunction, toxic encephalopathy CBC, sedimentation rate, electrolytes Anemia, electrolyte imbalance Blood Urea Nitrogen (BUN)/creatinine, liver function test Liver dysfunction Thyroid dysfunction Serum B 12 Vitamin deficiency Syphilis serology Syphilis HIV test AIDS dementia Neuroimaging studies: CT or MRI Tumor, subdural hematomas, abscess, stroke, or hydrocephalus
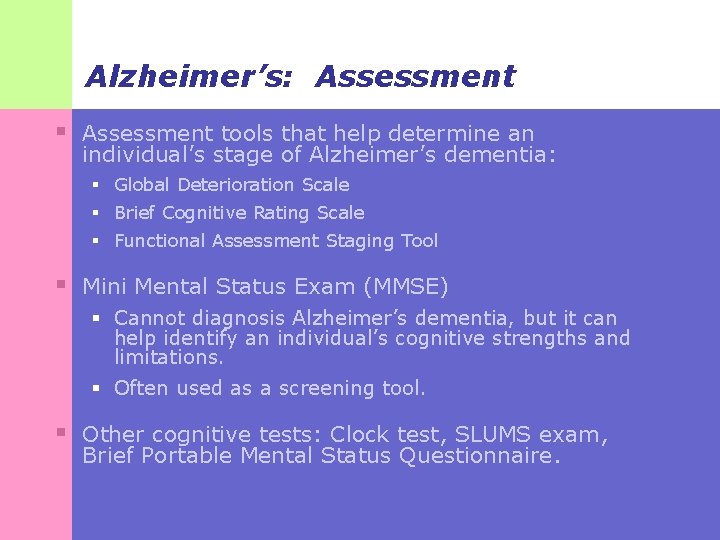
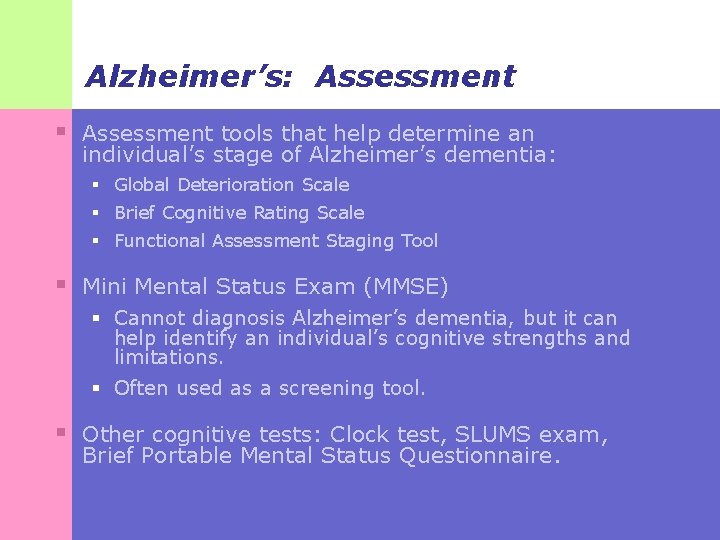
Alzheimer’s: Assessment § Assessment tools that help determine an individual’s stage of Alzheimer’s dementia: § Global Deterioration Scale § Brief Cognitive Rating Scale § Functional Assessment Staging Tool § Mini Mental Status Exam (MMSE) § Cannot diagnosis Alzheimer’s dementia, but it can help identify an individual’s cognitive strengths and limitations. § Often used as a screening tool. § Other cognitive tests: Clock test, SLUMS exam, Brief Portable Mental Status Questionnaire.
Alzheimer’s Assessment: Cultural Considerations § Results of cognitive assessment are influenced by: § Education § Socioeconomic status § Ethnicity § Literacy § Acculturation § Hispanic/Latino elders and Native American elders may have false positive scores for cognitive decline due to cultural bias inherent in common cognitive assessment tools. § This may be more pronounced in Native Americans due to language styles and language interpretive systems, for example oral traditions as memory aids rather than mnemonics used in dominant society (Griffin-Pierce et al, 2008).
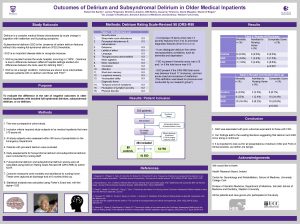
Delirium in Older Adults
Delirium: Definition § A mental disturbance characterized by sudden changes in mental functioning or acute confusion and fluctuating levels of consciousness. § Delirium is the most acute condition of the three D’s and is a true medical emergency.

Delirium: Symptoms § Disorganized thinking § Disorientation to time and place § Reduced level of attention (drowsiness) § Client may fall asleep during an interview. § Increased or decreased psychomotor activity § Or apathy, which is sometimes mistaken for depression § Increased agitation § Disturbances in sleep cycle
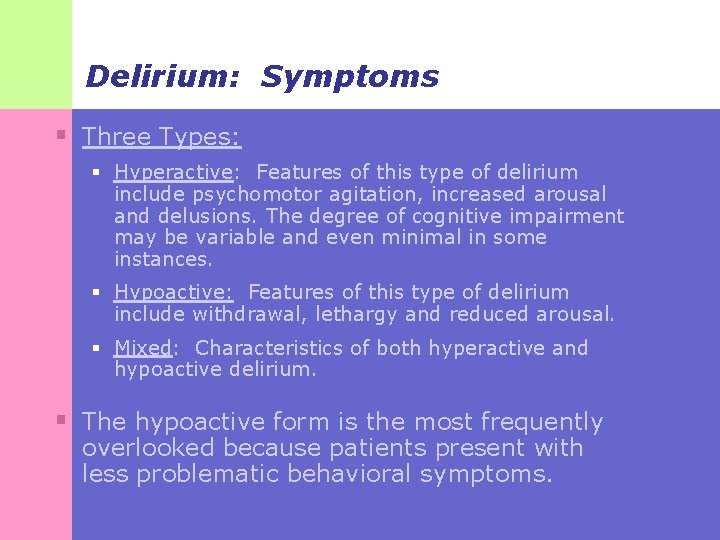
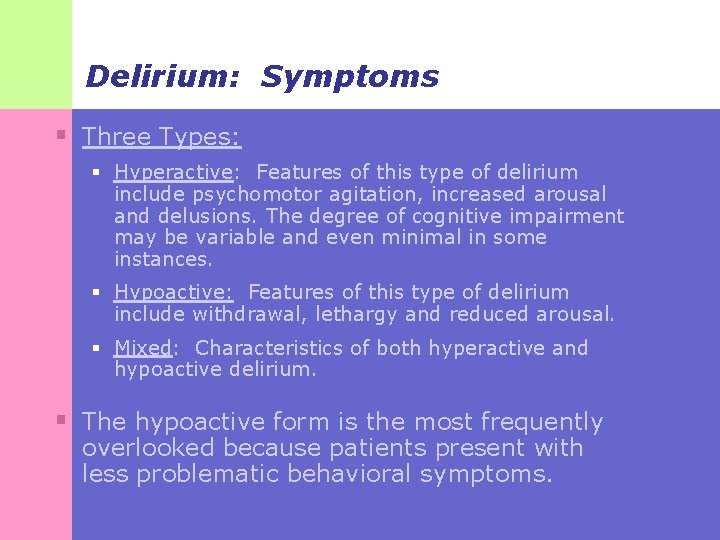
Delirium: Symptoms § Three Types: § Hyperactive: Features of this type of delirium include psychomotor agitation, increased arousal and delusions. The degree of cognitive impairment may be variable and even minimal in some instances. § Hypoactive: Features of this type of delirium include withdrawal, lethargy and reduced arousal. § Mixed: Characteristics of both hyperactive and hypoactive delirium. § The hypoactive form is the most frequently overlooked because patients present with less problematic behavioral symptoms.
Delirium: Symptoms § Four criteria are assessed in diagnosing delirium: § Acute onset and fluctuating course § Inattention § Disorganized thinking § Altered level of consciousness § The diagnosis of delirium requires the presence of criteria 1 and 2 and either 3 or 4.
Delirium: Epidemiology § Present in 10 -15 percent of older adult hospital admissions. § Occurs in: § 10 -30% 0 f hospitalized older adults. § More than 50% of post-operative hospitalized patients. § 70 -80% in the ICU. § Up to 60% of nursing home residents over age 75 may have delirium at any time! § 1 year mortality rate is 35 -40 percent.
What Causes Delirium? § The primary causes are underlying medical conditions, medications, or drug withdrawal: § Urinary tract infections § Reaction to prescribed medications or illicit drugs § Low blood pressure § Head injuries or falls § Dehydration § Alcohol withdrawal § Sensory deprivation (often experienced by hospitalized seniors, those having hearing impairments, or other sensory input limitations).
Delirium: Assessment § Because delirium is an emergency medical condition, medical (rather than social work) assessment and intervention is warranted. § However, given that delirium is one of the most under-recognized conditions in older adults, social work awareness of how to identify it is critical to enhancing quality of care. § Similarly, familiarity with standards of care for the treatment of delirium will help social workers serve as informed advocates for their older clients.

Cultural Considerations § Native Americans and Hispanic/Latinos are at greater risk for health disparities and less than optimal health/mental health care. § Individuals from these population groups require even greater diligence from health care providers to detect delirium. § Social work involvement can assist the care team to ensure these individuals do not fall through the cracks.

Now that you have an understanding of the differences among the three D’s … … Things get more complicated.
It is common for older adults to experience more than one of the three D’s at the same time! § So how do you tell the difference among the three of them? § Next we’ll look at differential diagnosis of the three D’s …
Depression and Dementia § 20 -40 percent incidence rate; equal across men and women. § In the nursing home setting, rates may be as high as 50 to 75 percent.
Depression in Dementia: Difficult to Diagnose § Some symptoms of dementia mimic those of depression (see handout): § Apathy § Loss of interest § Social withdrawal § Cognitive deficits hinder verbalization of sadness, hopelessness, guilt and other feelings associated with depression.
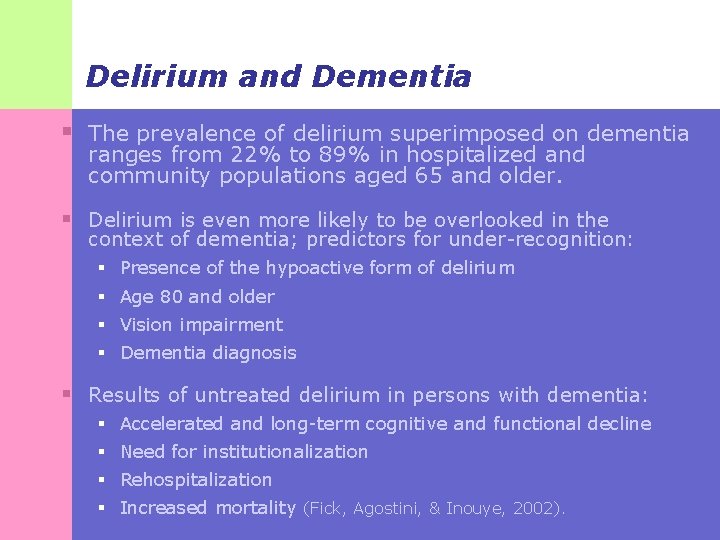
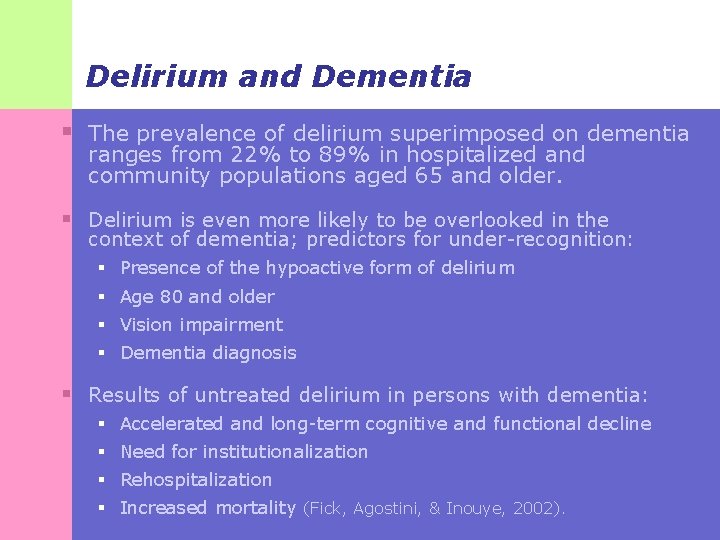
Delirium and Dementia § The prevalence of delirium superimposed on dementia ranges from 22% to 89% in hospitalized and community populations aged 65 and older. § Delirium is even more likely to be overlooked in the context of dementia; predictors for under-recognition: § Presence of the hypoactive form of delirium § Age 80 and older § Vision impairment § Dementia diagnosis § Results of untreated delirium in persons with dementia: § Accelerated and long-term cognitive and functional decline § Need for institutionalization § Rehospitalization § Increased mortality (Fick, Agostini, & Inouye, 2002).
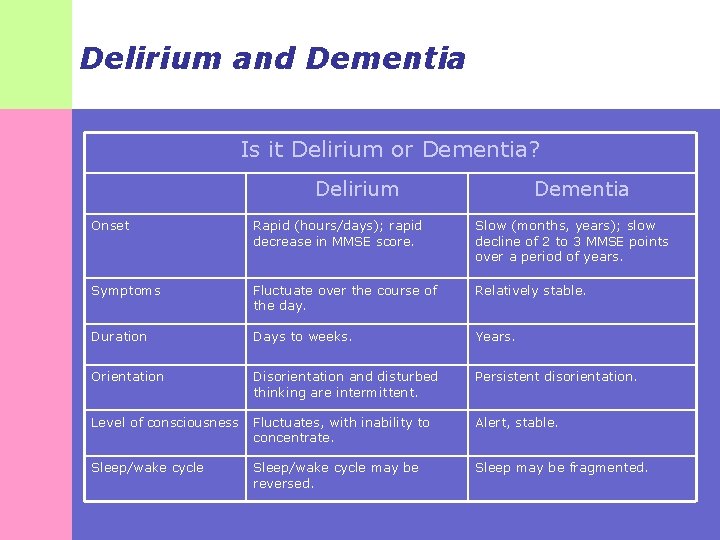
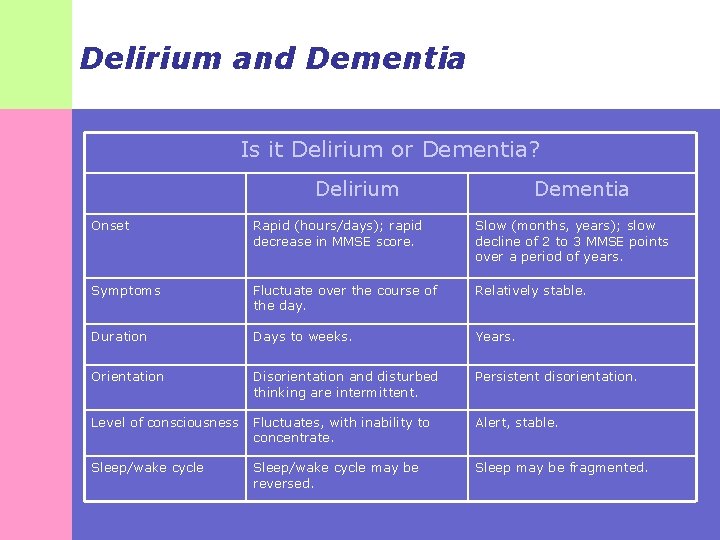
Delirium and Dementia Is it Delirium or Dementia? Delirium Dementia Onset Rapid (hours/days); rapid decrease in MMSE score. Slow (months, years); slow decline of 2 to 3 MMSE points over a period of years. Symptoms Fluctuate over the course of the day. Relatively stable. Duration Days to weeks. Years. Orientation Disorientation and disturbed thinking are intermittent. Persistent disorientation. Level of consciousness Fluctuates, with inability to concentrate. Alert, stable. Sleep/wake cycle may be reversed. Sleep may be fragmented.
Resources for Obtaining Assessment Tools § Geriatric Depression Scale: http: //www. stanford. edu/~yesavage/GDS. html § Indian Depression Schedule: Manson, S. M. , Shore, J. H. , & Bloom, J. D. (1985). The depressive experience in American Indian communities: A challenge for psychiatric theory and diagnosis. In A. Kleinman and B. Good (Eds. ) Culture and depression: Studies in the anthropology and cross-cultural psychiatry of affect and disorder, pp. 331 -368. Berkeley, CA: University of California Press. § Cornell Scale for Depression in Dementia: http: //img. medscape. com/pi/emed/ckb/psychiatry/285 911 -1335300 -1356106 -1392041. pdf § CES-D: http: //patienteducation. stanford. edu/research/cesd. pdf
Resources for Obtaining Assessment Tools § Suicide risk assessment: http: //www. valueoptions. com/providers/Network/NCSC _Government/Suicide_Risk_assessment_Form. pdf § MMSE: http: //www. minimental. com/ § SLUMS: http: //medschool. slu. edu/agingsuccessfully/pdfsurveys /slumsexam_05. pdf § Clock Drawing Test: http: //alzheimers. about. com/od/diagnosisissues/a/cloc k_test. htm § Short portable mental status questionnaire: http: //www. npcrc. org/usr_doc/adhoc/psychosocial/SP MSQ. pdf
Resources for Obtaining Assessment Tools § Brief Cognitive Rating Scale: http: //www. zarcrom. com/users/alzheimers/4 cp 8 a. html § Global Deterioration Scale: http: //web. missouri. edu/~proste/tool/cog/Glo bal-Deterioration-Scale. pdf § Functional Assessment Staging (FAST): http: //www. bigtreemurphy. com/Reisberg%20 FAST. htm
 Difference between dementia and delirium
Difference between dementia and delirium Francisco fernandez md
Francisco fernandez md Amnesia
Amnesia Lucie big delirium
Lucie big delirium Sindrom delirium akut
Sindrom delirium akut Nash delirium
Nash delirium Terminalt delirium
Terminalt delirium Cam icu escala
Cam icu escala Delirium care pathways
Delirium care pathways Acute confusion related to
Acute confusion related to Delirium definition
Delirium definition Frster
Frster R
R Delirium case presentation
Delirium case presentation Flocculation delirium
Flocculation delirium Gcs normal
Gcs normal European delirium association
European delirium association 3 zones of human awareness
3 zones of human awareness Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease Chapter 49 confusion and dementia
Chapter 49 confusion and dementia Confusion dementia and alzheimer disease chapter 19
Confusion dementia and alzheimer disease chapter 19 Confusion dementia and alzheimer's disease
Confusion dementia and alzheimer's disease Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease Wendylett sheets 1 carer
Wendylett sheets 1 carer Dementia treatments and interventions near patterson
Dementia treatments and interventions near patterson Bookcase analogy dementia
Bookcase analogy dementia Dementia pugilistica
Dementia pugilistica Enriched model of care social psychology
Enriched model of care social psychology Glycogen storage disease mnemonic
Glycogen storage disease mnemonic Dementia 2015
Dementia 2015 Tom kitwood enriched model of dementia care
Tom kitwood enriched model of dementia care Reversible dementia
Reversible dementia Epilepsy
Epilepsy Barbara's story dementia
Barbara's story dementia Fast scale for dementia
Fast scale for dementia Risk factor dementia
Risk factor dementia Hospice lcd dementia
Hospice lcd dementia Life story work dementia
Life story work dementia Trasodone
Trasodone Dementia friendly nevada
Dementia friendly nevada Promoting excellence in dementia care
Promoting excellence in dementia care Rarly signs of dementia
Rarly signs of dementia Dementia capable care
Dementia capable care Crescare
Crescare Pal checklist
Pal checklist Symptoms of dementia
Symptoms of dementia Positive risk-taking dementia
Positive risk-taking dementia Alzheimer's dementia
Alzheimer's dementia Dementia
Dementia Alzheimers society contented dementia
Alzheimers society contented dementia Frontotemporal dementia
Frontotemporal dementia Unit 40 health and social care
Unit 40 health and social care Enriched model of dementia care
Enriched model of dementia care Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Dementia
Dementia Lewry body dementia
Lewry body dementia Living well with dementia scotland
Living well with dementia scotland Dementia
Dementia Dementia pictures
Dementia pictures Dcm methode
Dcm methode 850 000 steps for dementia
850 000 steps for dementia Dementia is a condition characterized by
Dementia is a condition characterized by Dementia care in bath
Dementia care in bath Compare and contrast president hoover and roosevelt
Compare and contrast president hoover and roosevelt Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worm breton
Tư thế worm breton Chúa sống lại
Chúa sống lại Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân