Practical pointers on delirium and psychiatric challenges at














- Slides: 56
Practical pointers on delirium and psychiatric challenges at the end of life Oregon Hospice & Palliative Care Professional Practices Exchange Sunriver, OR Monday, September 26, 2016
Maureen Nash, MD, MS, FAPA, FACP Fellow, American College of Physicians Fellow, American Psychiatric Association Board Certified in Internal Medicine Board Certified in Psychiatry Copyright 2016 Nash
Disclosures Maureen Nash, MD, MS, FAPA Nothing to Disclose regarding Financial Conflicts of Interest Off-label use of medications will be discussed *Off-label does NOT mean illegal, ill-advised, or non-evidence based EMAIL: docmcnash@gmail. com Copyright 2016 Nash
Objectives • At the end of this presentation, you will be able to list 3 ways to decrease the risk of delirium • At the end of this presentation you will be able to list 3 ways to treat delirium • Understand which psychiatric symptoms are amenable to pharmacological treatment and which are amenable to behavioral/environmental interventions Copyright 2016 Nash

Confusion in the Older Adult • Delirium – Disturbance of consciousness and a change in cognition developing over a short period of time – Usually rapid onset • Dementia-Major Neurocognitive Disorder) – Deficits in at least two areas of brain functioning, usually including memory – Usually gradually progressive Copyright 2016 Nash
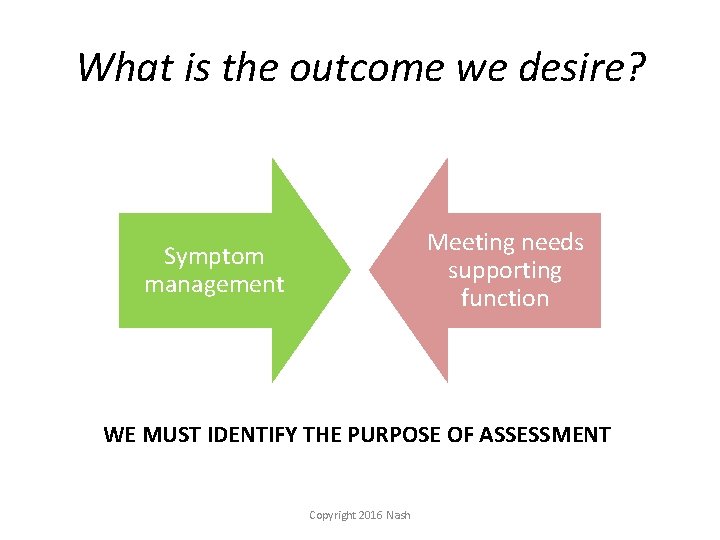
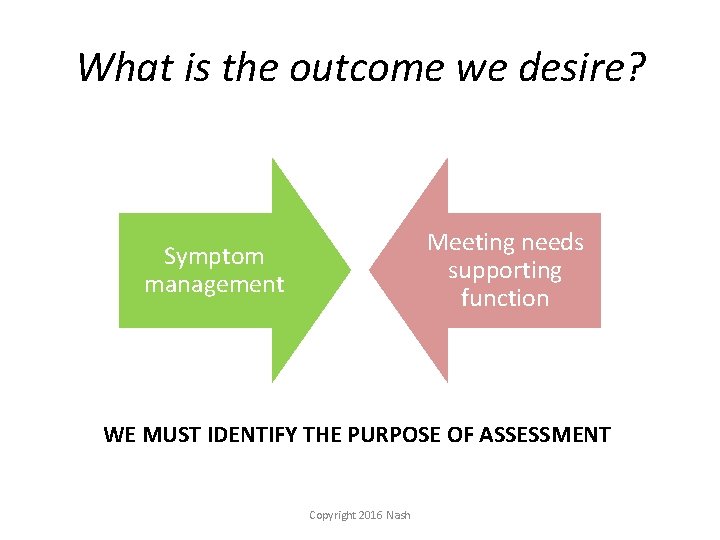
What is the outcome we desire? Meeting needs supporting function Symptom management WE MUST IDENTIFY THE PURPOSE OF ASSESSMENT Copyright 2016 Nash
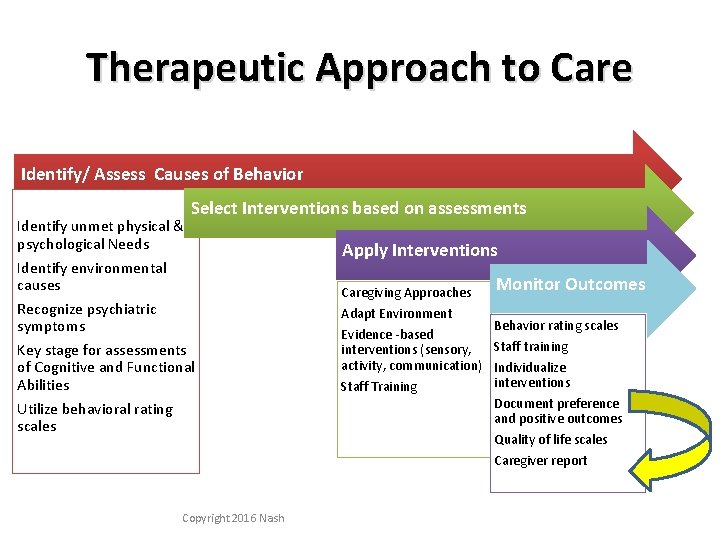
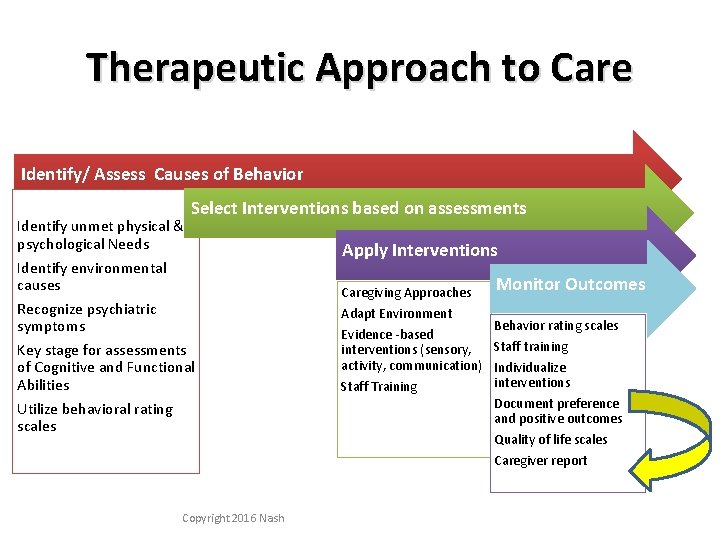
Therapeutic Approach to Care Identify/ Assess Causes of Behavior Identify unmet physical & psychological Needs Select Interventions based on assessments Identify environmental causes Recognize psychiatric symptoms Apply Interventions Caregiving Approaches Adapt Environment Key stage for assessments of Cognitive and Functional Abilities Utilize behavioral rating scales Copyright 2016 Nash Monitor Outcomes Behavior rating scales Evidence ‐based Staff training interventions (sensory, activity, communication) Individualize interventions Staff Training Document preference and positive outcomes Quality of life scales Caregiver report
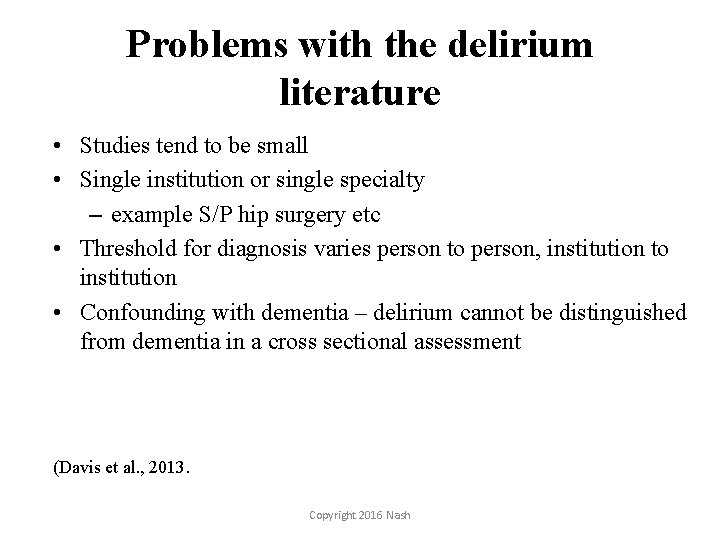
Problems with the delirium literature • Studies tend to be small • Single institution or single specialty – example S/P hip surgery etc • Threshold for diagnosis varies person to person, institution to institution • Confounding with dementia – delirium cannot be distinguished from dementia in a cross sectional assessment (Davis et al. , 2013. Copyright 2016 Nash

Clinical Pearl • Differentiating delirium from dementia with behavior disturbance is not straightforward • Time course is important BUT there is great overlap due to “sub-acute” Delirium and also Dementia with Behavior Disturbance • Who is most likely to be delirious? Those with dementia or other organic brain damage are most likely Copyright 2016 Nash
What is delirium and what causes it?
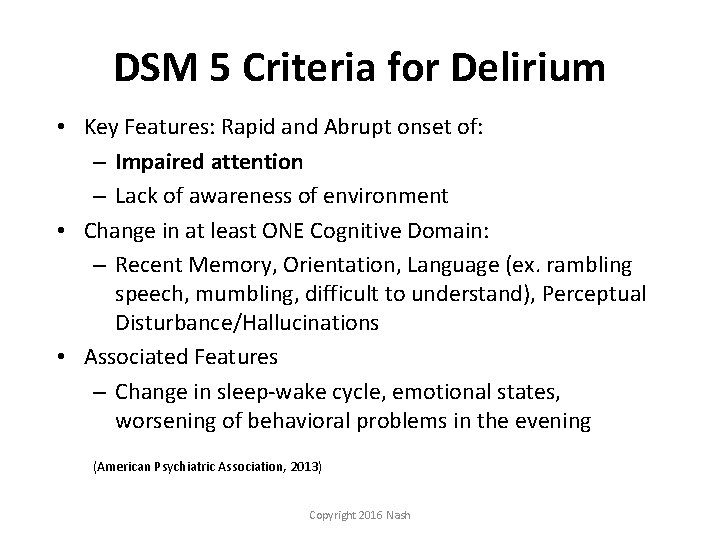
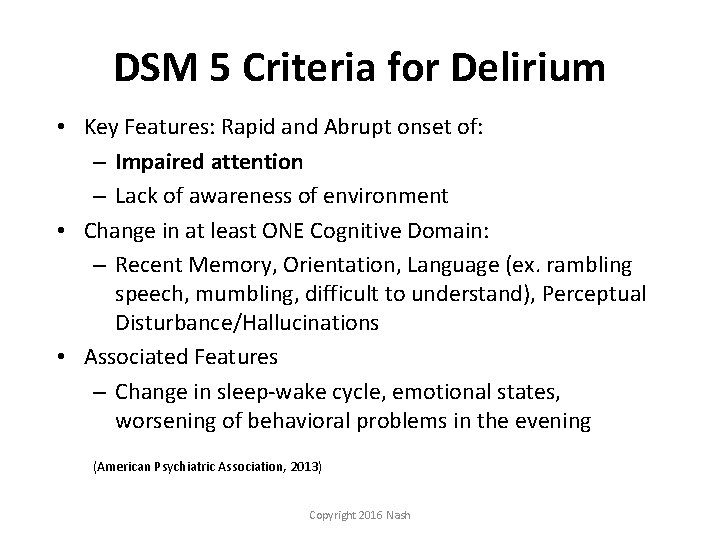
DSM 5 Criteria for Delirium • Key Features: Rapid and Abrupt onset of: – Impaired attention – Lack of awareness of environment • Change in at least ONE Cognitive Domain: – Recent Memory, Orientation, Language (ex. rambling speech, mumbling, difficult to understand), Perceptual Disturbance/Hallucinations • Associated Features – Change in sleep‐wake cycle, emotional states, worsening of behavioral problems in the evening (American Psychiatric Association, 2013) Copyright 2016 Nash
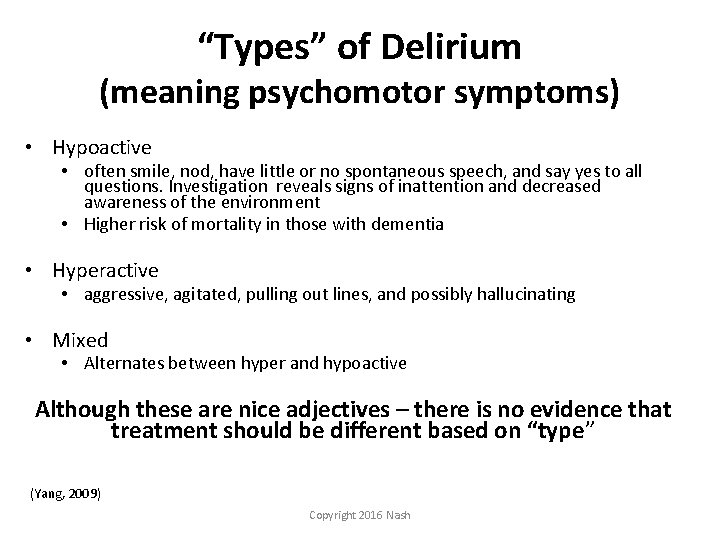
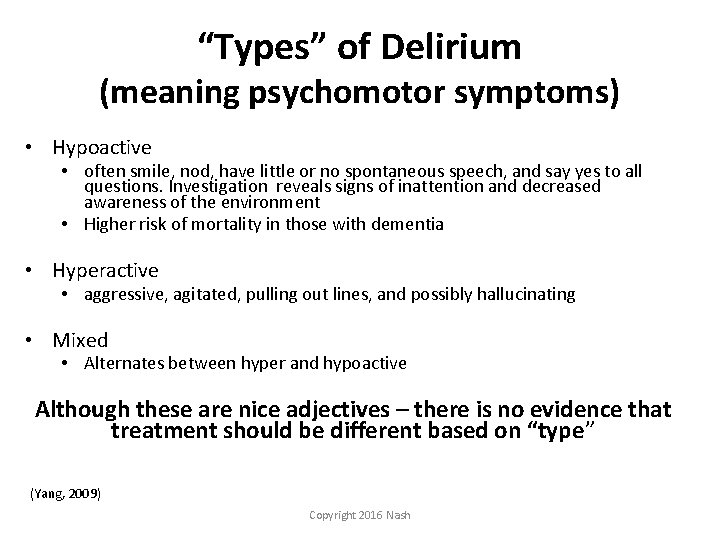
“Types” of Delirium (meaning psychomotor symptoms) • Hypoactive • often smile, nod, have little or no spontaneous speech, and say yes to all questions. Investigation reveals signs of inattention and decreased awareness of the environment • Higher risk of mortality in those with dementia • Hyperactive • aggressive, agitated, pulling out lines, and possibly hallucinating • Mixed • Alternates between hyper and hypoactive Although these are nice adjectives – there is no evidence that treatment should be different based on “type” (Yang, 2009) Copyright 2016 Nash
Usual or at least Common Course • Onset may be abrupt • More typically, delirium begins with restlessness, irritability, anxiety or sleep disturbance • Full syndrome within 1‐ 3 days • May progress to stupor, coma, seizures, or death, particularly if etiology unknown Copyright 2016 Nash
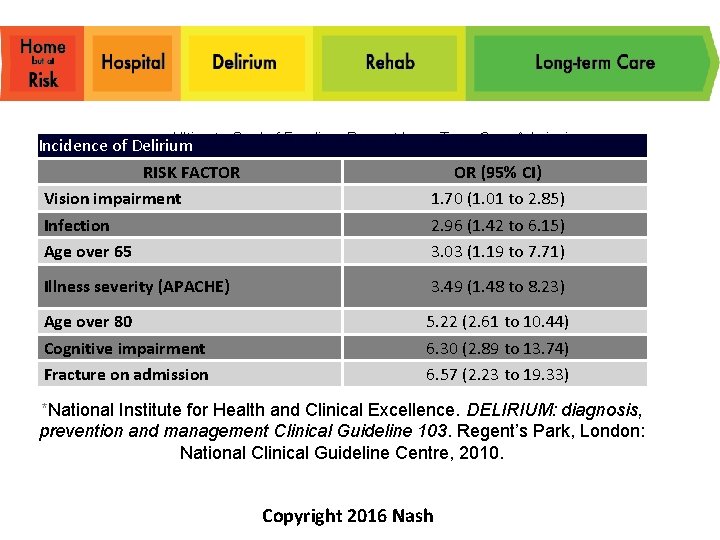
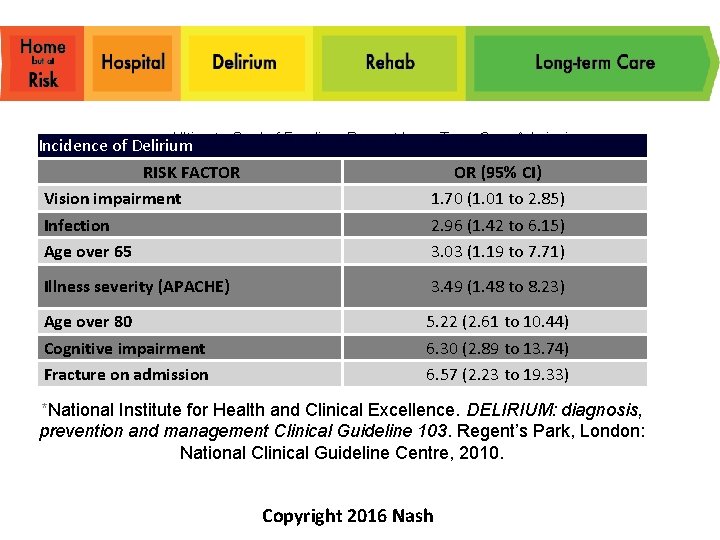
Ultimate Goal of Funding: Prevent Long Term Care Admissions Incidence of Delirium RISK FACTOR OR (95% CI) Vision impairment 1. 70 (1. 01 to 2. 85) Infection 2. 96 (1. 42 to 6. 15) Age over 65 3. 03 (1. 19 to 7. 71) Illness severity (APACHE) 3. 49 (1. 48 to 8. 23) Age over 80 Cognitive impairment Fracture on admission 5. 22 (2. 61 to 10. 44) 6. 30 (2. 89 to 13. 74) 6. 57 (2. 23 to 19. 33) *National Institute for Health and Clinical Excellence. DELIRIUM: diagnosis, prevention and management Clinical Guideline 103. Regent’s Park, London: National Clinical Guideline Centre, 2010. Copyright 2016 Nash

Pathophysiology of Delirium • Anatomical Deficits • Anterior thalamus, basal ganglia and temporal‐occipital cortex implicated • Prefrontal and nondominant posterior parietal regions are implicated by f. MRI, PET and SPECT • Neurotransmitter Imbalances • • Dopamine excess Acetylcholine and Melatonin deficiencies Likely, increased GABA, NE, Glutamine, 5 HT Eventual global dysfunction of cerebral metabolism http: //www. mc. vanderbilt. edu/icudelirium/overview. html Copyright 2016 Nash
Psychiatric Symptoms amenable to treatment with medications • • • Paranoia and delusions Hallucinations Depression Sometimes anxiety Pain ? agitation? Copyright 2016 Nash

Symptoms not usually amenable to medications • • Wandering Calling out (not related to pain) Repetitive questions Anxiety related to having memory loss Psychomotor agitation Sleep problems ? agitation? Copyright 2016 Nash
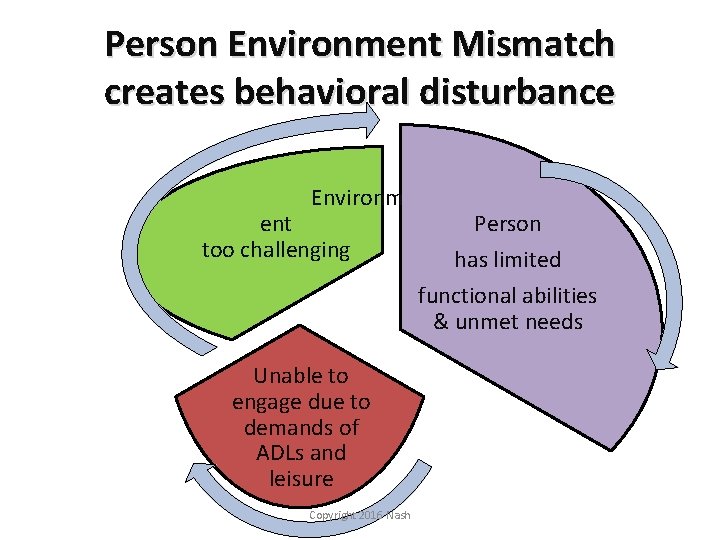
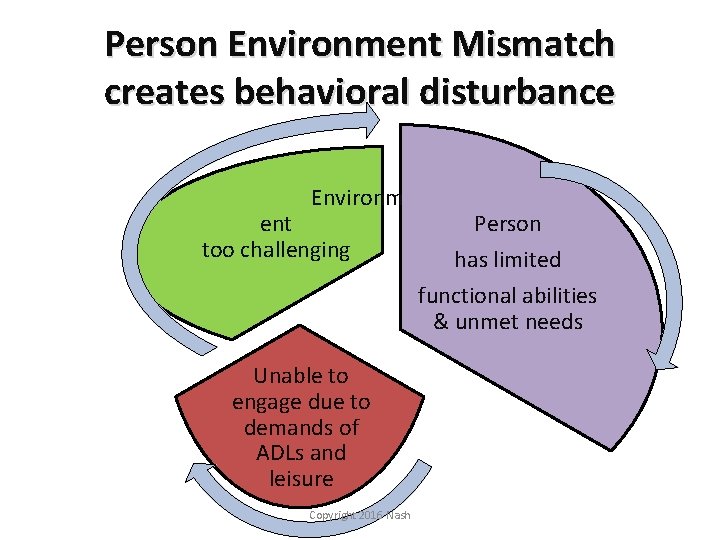
Person Environment Mismatch creates behavioral disturbance Environm ent too challenging Unable to engage due to demands of ADLs and leisure Copyright 2016 Nash Person has limited functional abilities & unmet needs
How do you find delirium?
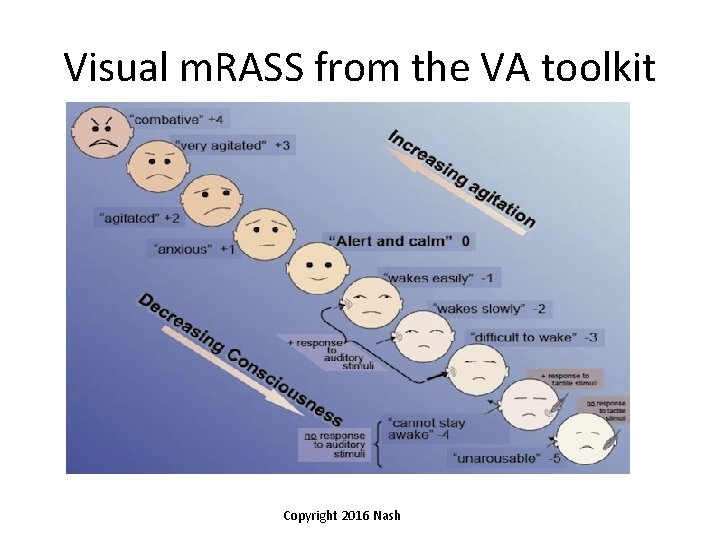
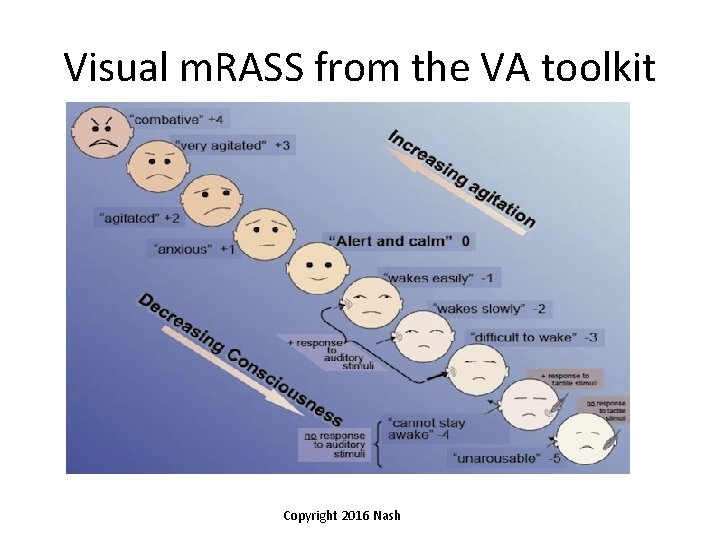
Visual m. RASS from the VA toolkit Copyright 2016 Nash
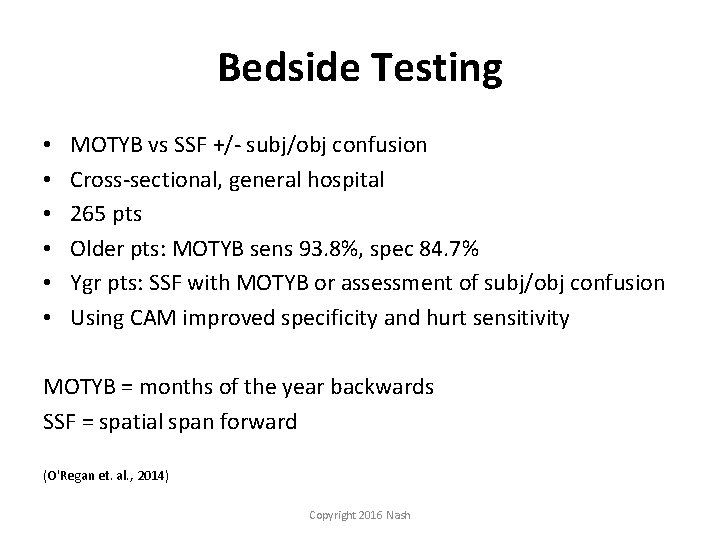
Bedside Testing • • • MOTYB vs SSF +/‐ subj/obj confusion Cross‐sectional, general hospital 265 pts Older pts: MOTYB sens 93. 8%, spec 84. 7% Ygr pts: SSF with MOTYB or assessment of subj/obj confusion Using CAM improved specificity and hurt sensitivity MOTYB = months of the year backwards SSF = spatial span forward (O'Regan et. al. , 2014) Copyright 2016 Nash
Can you prevent or decrease the risk of delirium?
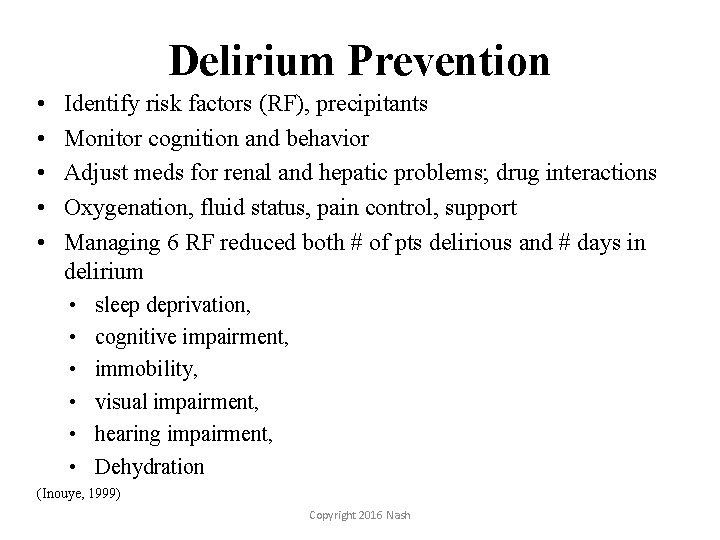
Delirium Prevention • • • Identify risk factors (RF), precipitants Monitor cognition and behavior Adjust meds for renal and hepatic problems; drug interactions Oxygenation, fluid status, pain control, support Managing 6 RF reduced both # of pts delirious and # days in delirium • • • sleep deprivation, cognitive impairment, immobility, visual impairment, hearing impairment, Dehydration (Inouye, 1999) Copyright 2016 Nash
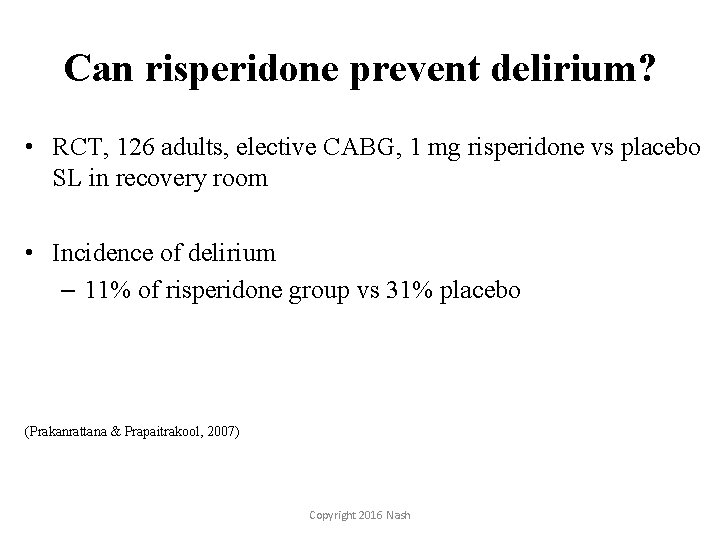
Can risperidone prevent delirium? • RCT, 126 adults, elective CABG, 1 mg risperidone vs placebo SL in recovery room • Incidence of delirium – 11% of risperidone group vs 31% placebo (Prakanrattana & Prapaitrakool, 2007) Copyright 2016 Nash
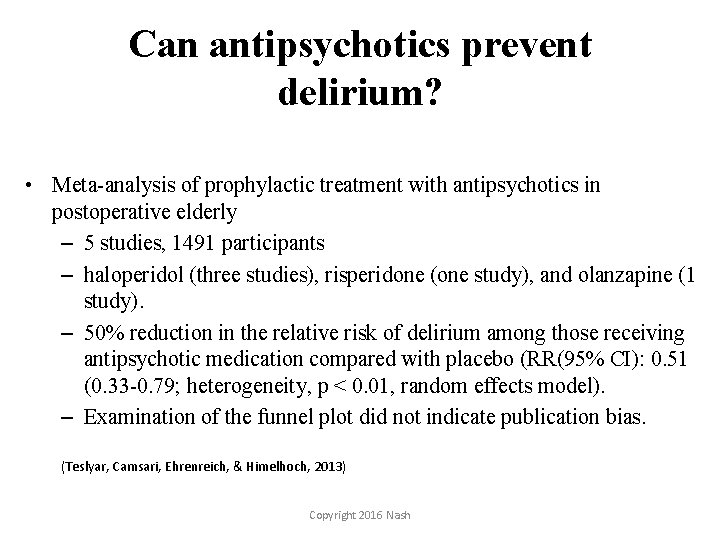
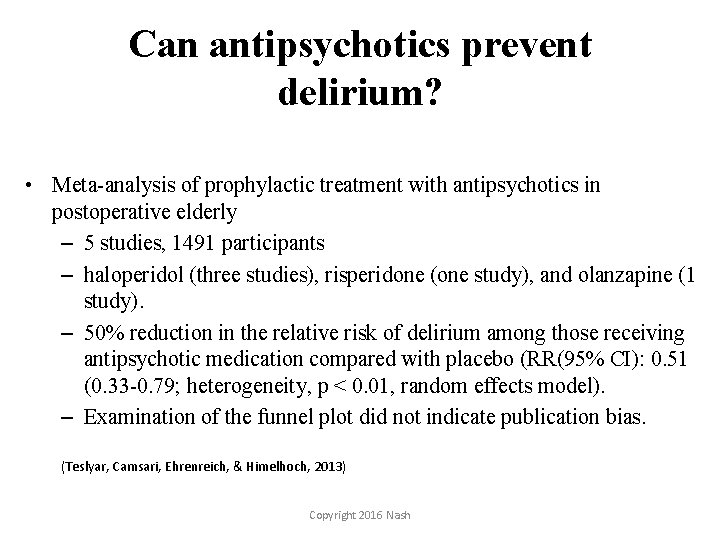
Can antipsychotics prevent delirium? • Meta-analysis of prophylactic treatment with antipsychotics in postoperative elderly – 5 studies, 1491 participants – haloperidol (three studies), risperidone (one study), and olanzapine (1 study). – 50% reduction in the relative risk of delirium among those receiving antipsychotic medication compared with placebo (RR(95% CI): 0. 51 (0. 33 -0. 79; heterogeneity, p < 0. 01, random effects model). – Examination of the funnel plot did not indicate publication bias. (Teslyar, Camsari, Ehrenreich, & Himelhoch, 2013) Copyright 2016 Nash

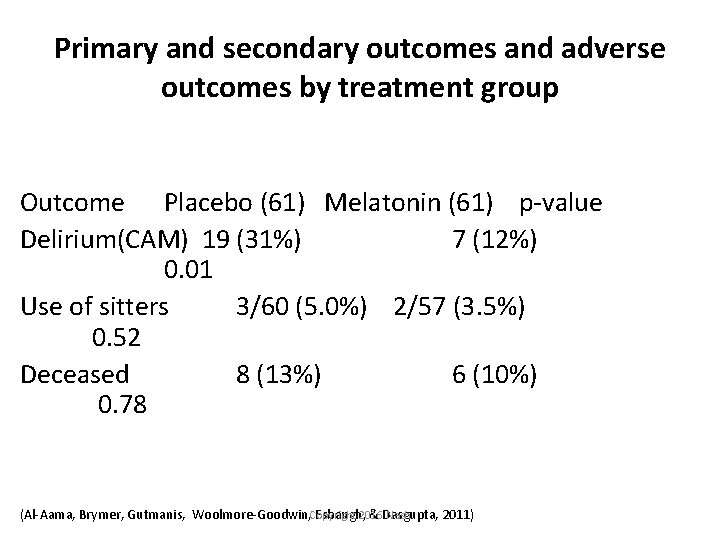
Melatonin to decrease delirium • 145 pts, 65+ yo admitted through the emergency department at tertiary care hospital • Tx: 0. 5 mg of melatonin vs placebo every night for 14 days or until discharge. (Al‐Aama, Brymer, Gutmanis, Woolmore‐Goodwin, Esbaugh, & Dasgupta, 2011) Copyright 2016 Nash
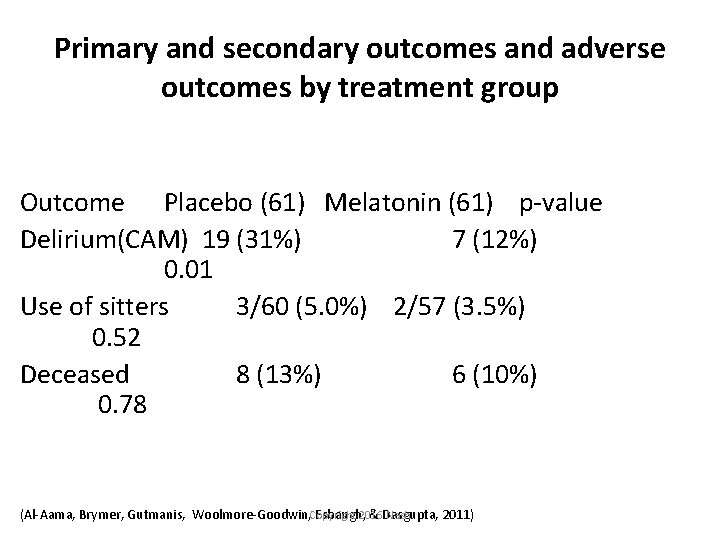
Primary and secondary outcomes and adverse outcomes by treatment group Outcome Placebo (61) Melatonin (61) p‐value Delirium(CAM) 19 (31%) 7 (12%) 0. 01 Use of sitters 3/60 (5. 0%) 2/57 (3. 5%) 0. 52 Deceased 8 (13%) 6 (10%) 0. 78 2016 Nash (Al‐Aama, Brymer, Gutmanis, Woolmore‐Goodwin, Copyright Esbaugh, & Dasgupta, 2011)

Helpful websites • Vanderbilt ICU delirium information for providers and lay persons alike – www. icudelirium. org • Delirium Toolkit based on a Quality Improvement project in VA system – www. heartbrain. com/delirium • Ontario, CA website with education, protocols etc – www. seniorfriendlyhospitals. ca Copyright 2016 Nash
Behavior Oriented what the evidence says Techniques to directly decrease or change behavior Example Modalities: Differential reinforcement, Redirection Typical Target Behaviors: Agitation, sexual inappropriate behaviors, wandering (O'Neil et al. , 2011) Copyright 2016 Nash
Cognitive Oriented Language based modalities including skills training, cognitive training, and reality training No evidence for efficacy or use in patients in the moderate to severe category Cognitive stimulation is efficacious for MCI or healthy aging – Word games, reading, current events, puzzles, trivia Copyright 2016 Nash
Environmental Strategies Treatment modalities that stimulate or deescalate that are external to the patient Examples: • • • caregiver education simplifying environment Removing barriers, accessibility lowering stimulation Programming: Montessori, Intergenerational, Eden’s alternative Typical target behaviors: wandering, disruptive behavior, agitation, pain Copyright 2016 Nash (Cooper et. al. 2012; Kverno et al 2009; O'Neil et al. , 2011; Spijker et al. 2008)
Sun Downing and Sleep • Late day confusion associated with dementia • Poor sleep pattern (reverse day and nights) • Disturbance in circadian rhythms • Interventions – Avoid sleep medications – Adjust schedule of the day (People with dementia are not living on everyone else’s schedules) – Avoid large meals at night – Provide plenty of light and fresh air during the day – Monitor fatigue – Proactively treat pain – Look for sensory triggers – Establish a comforting routine – Provide caregiver support (What happens at 4? ) Copyright 2016 Nash
Communication Strategies • Nonverbal vs. Verbal • Don’t ask questions • Remember the spatial orientation is impaired (middle temporal lobe, occipital, parietal) • Identify the world in which they live, avoid reality orientation Supportive Communication – Listen for the message, not the content – Watch for emotions, not words – Validate feelings – Redirect with purposeful activity – Do not ask questions, provide simple information Copyright 2016 Nash
People with dementia cannot changebut you can • Respect personal preference, keep normal patterns • Reframe “bad behaviors” – look to meet needs • Gather information about occupational and personal history • Stop, Look, and Listen: Be present • “Sensing is Believing” • Retain composure, non reactive responses • Never argue; use distraction • Model positive mood Copyright 2016 Nash

Caregiver’s influence on Environment • Physical contact • Impact on level of stimulation • Therapeutic use of self/ Intentional Presence • Amounts of redirection • Purpose of interaction • Familiarity with each individual Copyright 2016 Nash
Millie has lived in an ALF for years. Recently Millie has become verbally hostile, including scratching and biting with care. When I met her, Millie screams every time someone enters room for care. She refuses all interaction, medication, and care. Copyright 2016 Nash
Cleopatra • 92 yo Female • Referred for increasing aggression towards caregivers and peers at AFH – biting, hitting, kicking • Family gave history of abrupt decline since surgery 4 weeks ago • Preexisting dementia but previously independent in ADLs Copyright 2016 Nash
Major steps to take with all patients • Avoid benzodiazepines (lorazepam, diazepam, oxazepam…) • Avoid anticholinergic medications (diphenhydramine, metoclopramide…) • Normalize sleep/wake cycle • Frequent reorientation • Avoid dehydration, encourage po intake=FEED patients Copyright 2016 Nash

Treatment Copyright 2016 Nash
Treating Delirium • Aggressively search for underlying cause and treat it • Consider drug withdrawal (alcohol, benzodiazepines), Otherwise, avoid BZDs if at all possible • Lower anticholinergic load • Check medication levels (digoxin, VPA etc) • Dose medications for renal impairment • Antipsychotic medications – (haloperidol if < 70 yo, otherwise risperidone Mtab, ziprasidone IM) Copyright 2016 Nash
Double-Blind Trial of Risperidone vs Haloperidol for the Treatment of Delirium • 28 patients with delirium • flexible-dose regimen of haloperidol or risperidone over 7 days • Severity assessed - Memorial Delirium Assessment Scale • Scores for each group decreased significantly over the study period. • No significant differences in mean scores between groups • The group-by-time effect was not significant. • There was no significant difference in the frequency of response to the drugs between the two groups. • One patient in the haloperidol group experienced mild akathisia, but no other patients reported clinically significant side effects Han, Chang-Su, Kim, Yong-Ku. Psychosomatics 2004 45: 297 -301 Copyright 2016 Nash

Antipsychotics used to treat Delirium • Haloperidol up to 10 mg IM (usually 0. 5 -2 mg); 0. 55 mg IV (max 20 mg daily, though 10 mg/24 hrs occupies 90% of D 2 receptors) • Ziprasidone (Geodon) 10 IM mg q 2 hours to max 40 mg daily • Quick disintegrating oral preparations – Risperidone (Risperdal) M tab 0. 5, 1, 2 mg orally Copyright 2016 Nash

Meds theoretically less likely to be helpful • Olanzepine • anticholinergic at > 10 mg / 24 hr • Quetiapine • anticholinergic at > 150 mg / 24 hr Copyright 2016 Nash
Non-pharmacologic Management • • Private room Observer Remove dangers Family education Familiar objects Calendar, clock Re-orient frequently Visitation • Respiratory care • PT/OT for physical and mental activity • Explanations, reassurance • Avoid restraints • Physical restraints may be better than chemical in the short term (especially if chemical already overused) (Fann, Eyler) Copyright 2016 Nash

CASES
Cleopatra • 92 yo Female • Referred for increasing aggression towards caregivers and peers at AFH – biting, hitting, kicking • Family gave history of abrupt decline since surgery 4 weeks ago • Preexisting dementia but previously independent in ADLs Copyright 2016 Nash

Associated symptoms • Poor po intake with 15# weight loss • Clearly paranoid and responding to internal stimuli • Treatment for Dementia with Behavior Disturbance helped maybe 10% • Quite aggressive with staff on psych unit • Treatment regimen: eliminate anticholinergics, start low dose risperidone, start memantine Copyright 2016 Nash
Hospital Course • PO intake < 20%, would only eat a little when family travelled from Corvallis to feed her • Dehydrated • POLST not consistent with IVF • No side effects from risperidone • Discussion with family: – Treat as a severe delirium with decent dose of antipsychotic or dc to ICF with hospice and let pt die while she was psychotic and suffering Copyright 2016 Nash
Outcome • Increased risperidone to 1 mg tid Mtab with IM olanzepine 2. 5 mg IM backup • Within 48 hours pt began to eat 30% of meals • Hallucinations faded • Within 5 days, pt smiling, pleasant, 100% cooperative, no aggression at all • Discharged to AFH Copyright 2016 Nash
Inpatient Medicine Consult • 87 yo F with L sided CVA & post CVA sz • Tx with fosphenytoin for sz – then pt had hypotensive episode and CVA symptoms worsened. • Nearly constant yelling out & severe psychomotor agitation • Aggressive with nursing staff during cares • Could not carry on a conversation • Poor po, little sleep • Per PCP records she was on fluoxetine 80 mg daily which was restarted 2 days prior to consulting psychiatry Copyright 2016 Nash
• PMH: – moderate to severe aortic stenosis, htn, DM, ASCVD S/P LAD stent, obesity • History from family: – Likely preexisting short term memory problems – Problems functioning independently though lived alone – Likely not taking medications as prescribed for a number of years Copyright 2016 Nash
Initial interview 7 am • • • Restless constant movement in hospital bed Did not focus on me or her family in room Yelling loudly“I want, I want bayyyyy” R sided neglect Did not maintain eye contact Severe expressive and receptive aphasia Copyright 2016 Nash

Initial Interventions • DC fluoxetine – Serotonergic load, akithisia, worsened confusion due to high dose, likely noncompliance • Give scheduled risperidone M tab 0. 5 mg tid • PRN ziprasidone 10 mg IM q 6 hrs prn severe agitation • Order not to check VS between 10 pm and 5 am unless there is a clinical need to do so. • Make sure to feed patient frequently throughout the day • Use IVF to keep her hydrated Copyright 2016 Nash
Next interview 6 pm same day • Lying quietly in bed • Reached out her hand seemed to try to engage in conversation • Nonsense speech but tone, volume, cadence normal • Just after I left the room she began to call out again, nonsense speech but at a low volume, minimal psychomotor agitation Copyright 2016 Nash

Next interventions • Continue previous orders • Mirtazapine 7. 5 mg po qhs for sleep • Donepezil 5 mg po daily after a meal • Memantine 5 mg po bid Copyright 2016 Nash
Follow up • 2 months later I saw the neurologist who had consulted me on the case • “It was a miracle” within 48 hours • Pt able to participate with PT/OT and do some rehabilitation • Pt able to recognize and communicate with her family Copyright 2016 Nash