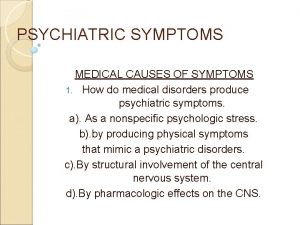
Creative Approaches for Differentiating Medical From Psychiatric Symptoms


























- Slides: 160
Creative Approaches for Differentiating Medical From Psychiatric Symptoms Using Physical Assessment Skills Mary Ann Foley-Mayer DMH, RN, APN, C Family Psychiatric Mental Health Nurse Practitioner
Disclosures l l l No affiliations to disclose The photos and video are from the internet and you tube and are all in public domain All names are fictional The case studies are from real client situations None of the photos are from actual patients
Objectives l l l Describe symptom analysis and how to formulate a differential diagnosis using physical assessment skills. Differentiate symptoms as medical or psychiatric based on case studies and visual aids Discuss physical symptoms that may be induced by psychotropic medication
Practical Objectives l l l Quickly assess the client who just doesn’t look right Utilize the practical physical assessment skills to decide if the situation is emergent Direct or provide the necessary care Plan ahead for emergencies Gain information you can use in your daily practice while enhancing your critical thinking skills
Have you even had a client walk into your office who: l l l Has chest pain Has an unexplained skin rash Has tremors or unusual movements Looks pale and shaky Has a seizure What do you do?
Topics l l l Cardiac vs anxiety/panic Skin rash vs rash from psychotropic medications Insomnia Neurologic topics: seizure vs Psychogenic Non Epileptic Seizure, change in mental status Medication induced physical symptoms
Physical Assessment l l l Health History Inspection Palpation Auscultation Percussion
Symptom Assessment Rule of Thumb l l l One symptom may not be serious The more symptoms the more likely the situation is serious Symptoms involving vital signs including blood pressure, pulse, respiration, acute pain, change in skin color are more serious
Develop an emergency plan l l l 911 What agency do you use for emergency services? Do you have a contact person in that agency? Develop a network of primary care referrals you can send clients to in an emergency Visit your local ED and crisis center to develop contacts
Cardiac vs. anxiety
Henry l l l 56 year old male treated for Major depression, grief related to the death of his wife and alcohol dependence in remission for the past year Meds include: Citalopram 20 mg and Quetiapine 50 mg daily at bedtime. He is complaining of a sharp pain in his left chest usually while sleeping.
Henry l l Is he having an MI? Could the pain be related to his psychotropic medication? Is this an emergency? Can we proceed with the psychiatric assessment or does he need acute medical treatment?
What if it’s cardiac? l l l l l A=airway B= breathing C=circulation Skin-pallor, color, cyanosis, diaphoresis, edema Question the client- chest pain, difficulty breathing, does he appear in distress, assess his ability to answer, any shortness of breath Vital signs Can the person focus and concentrate Assess pain Do I need to call 911?
Henry l l l His vital signs are normal and he is not in acute distress Proceed with taking a history of the pain Can continue with the psychiatric session as he is feeling well right now and is willing to continue
Henry l l He went to the ED 5 months ago for this sharp pain. Chest x-ray showed a nodule of the left chest. He saw his primary care practitioner and has an appointment for follow up He takes Motrin for pain He still has chest tightness and pain mainly at night and now is having headaches
Assessment of Symptoms l l l Chest tightness and pain usually while sleeping Possible causes Headache Related to chest pain? Look for the most logical or simplest causes
Henry l l Not likely an MI as he has no pain or symptoms now, he was seen in the ED and by his PCP and a work up is in progress Possible infection? Check blood work Suspicious nodule in left chest- lung lesions due to infection or cancerous tumor? Chest pain at night- possible GI etiology
Henry l Lung nodule determined benign and his practitioner is watching it. l He is now treated for GERD with relief of the night time chest pain His headache was from using an old pair of bifocals instead of getting new prescription trifocals He is doing well emotionally and denies feeling depressed By taking the time to review the symptoms and possible etiology with Henry he became calmer and we ruled out any emergent situation. l l l
Chest pain vs. Panic l l You are seeing a client for the first time for a psychiatric symptom and have very little information about the person This is how the client presents
What are your first thoughts? l l l Anxiety Panic Cardiac illness Asthma Physical illness

What are you priority assessments? l Airway, Breathing and Circulation l Is it necessary to call 911? Current complaints of pain? Does he/she look in distress? What are the vital signs? Conduct a pain assessment Order blood work and EKG? Send the patient to the ED? l l l
Is the patient having chest pain? l l l Is it a life threatening condition? Could it be pain from another system-pain from GI, musculoskeletal, respiratory, cardiac and pulmonary systems all transmit to the same spinal cord segments, T 1 -T 5. Life threatening illness includes MI, PE, pneumothorax and aortic dissection
Assessment of Pain l l l l Timing, onset, duration, frequency Anatomical location Character or quality Setting Severity or intensity-Rating scales of 1 -10 or happy and sad faces Aggravating or alleviating factors Associated symptoms Client’s perception of the meaning of the symptoms
Serious Symptoms involve vital organs l l l Abnormal blood pressure, temperature, pulse or respiration Cyanotic color changes Sudden change in level of consciousness or mental status Severe pain Sudden and intense agitation or lethargy These require immediate treatment
Assess l l l Vital signs Pain level Check the feet and ankles for edema Listen to the person’s lungs- assess for wheezing, crackles, rhonchi, absence of breath sounds. Auscultate for heart sounds
Sequence for Auscultating Begin with the diaphragm. l Note at each area: 1. rate & rhythm 2. identify S 1 and S 2 3. assess S 1 and S 2 separately 4. listen for extra heart sounds (ie. S 3, S 4) 5. listen for murmurs Repeat above using the bell. Listen for any irregular beats, skipped beats or tachycardia

Causes of an MI l l l Hypertension-causes chronic injury to the intimal lining of the coronary endothelium. Low-density lipoproteins (LDL) are the source of most lipids in atherosclerotic plaques. Diabetes, chemical irritants in tobacco smoke and infections cause injury to the lining of the coronary artery and plaque formation. Thrombosis related to damage to vessel walls The presence of damage to the intimal lining of the coronary artery changes the vessel size and interferes with homeostatic functions of the endothelium causing vasodilatation.
Causes of an MI l l Disruption of a plaque can produce thrombosis creating a lesion. This acute thrombus can produce complete or partial occlusion, which further impairs blood flow to the myocardium when coupled with vasospasm. Microvascular disease, endothelial dysfunction, or both may contribute to impaired blood flow to the myocardium. The duration and severity of blood flow impairment determines the severity of the acute coronary syndrome manifestations— unstable angina or myocardial infarction (MI).
MI Pathophysiology l l The major cause of MI is an atherosclerotic plaque impeding forward flow in a coronary artery. In women, however, chest pain and abnormal stress tests can occur without a critical, flow-limiting lesion. In the Women's Ischemia Syndrome Evaluation (WISE) study, nearly 60% of women with chest pain who underwent coronary angiography did not have a critical lesion (defined to be >50% luminal stenosis in a coronary artery). Merz CN, Kelsey SF, Pepine CJ, et al. The Women's Ischemia Syndrome Evaluation (WISE) study: protocol design, methodology and feasibility report. J Am Coll Cardiol 1999; 33: 1453– 1461.
MI Pathophysiology l l l In this study population, women without critical luminal narrowing had persistent symptoms despite usual therapy They had worse outcomes than age-matched controls during the follow -up period of 4 to 5 years. The persistence of symptoms coupled with abnormal stress test results has been attributed to endothelial dysfunction or microvascular disease. Women have smaller coronary arteries than men, even after correcting for body surface area. Women have been shown to be twice as likely as men to have plaque erosion with subsequent thrombus formation. Coronary vasospasm affects women more frequently than men.
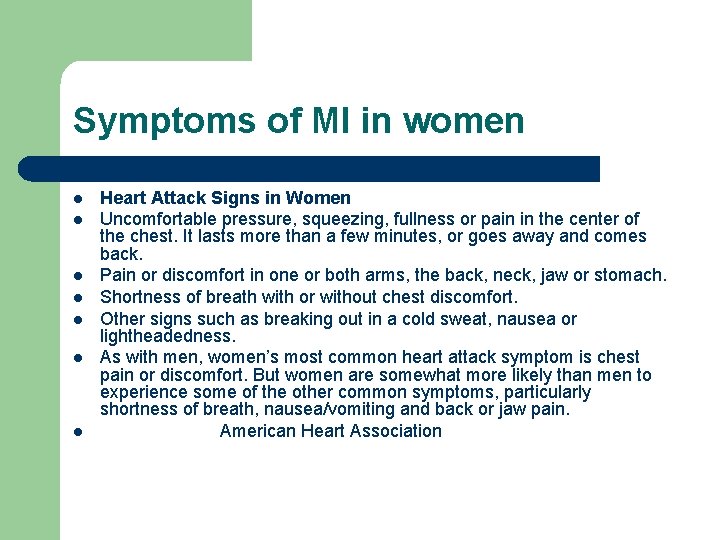
Symptoms of MI in women l l l l Heart Attack Signs in Women Uncomfortable pressure, squeezing, fullness or pain in the center of the chest. It lasts more than a few minutes, or goes away and comes back. Pain or discomfort in one or both arms, the back, neck, jaw or stomach. Shortness of breath with or without chest discomfort. Other signs such as breaking out in a cold sweat, nausea or lightheadedness. As with men, women’s most common heart attack symptom is chest pain or discomfort. But women are somewhat more likely than men to experience some of the other common symptoms, particularly shortness of breath, nausea/vomiting and back or jaw pain. American Heart Association
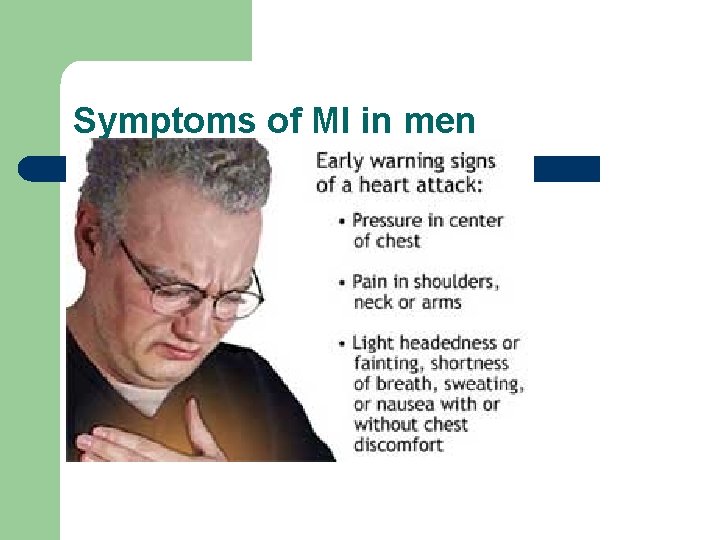
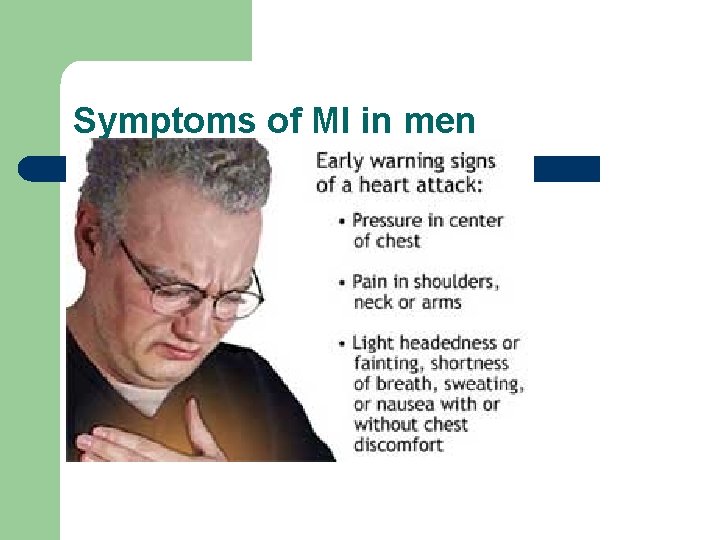
Symptoms of MI in men
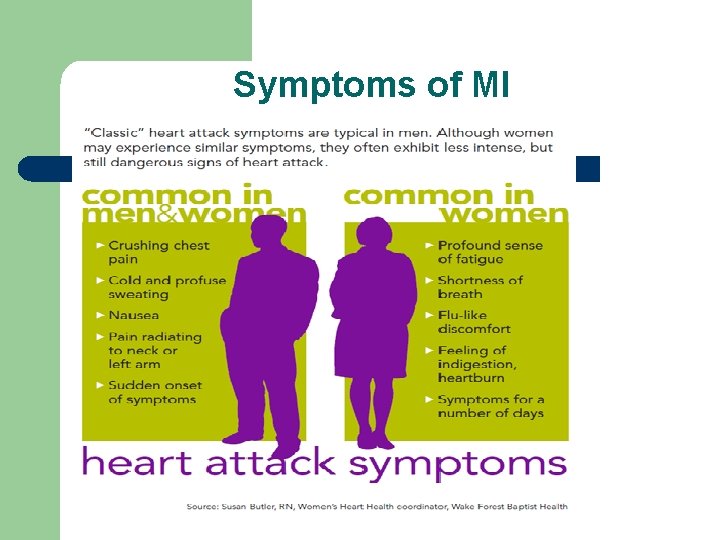
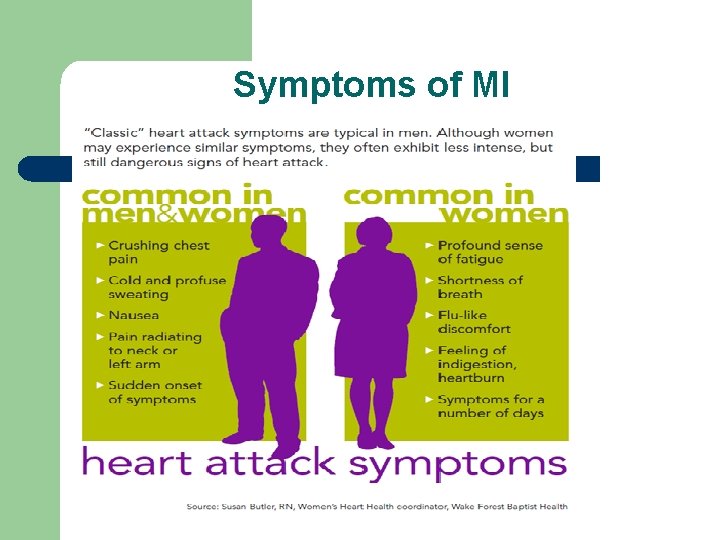
Symptoms of MI
Syncope
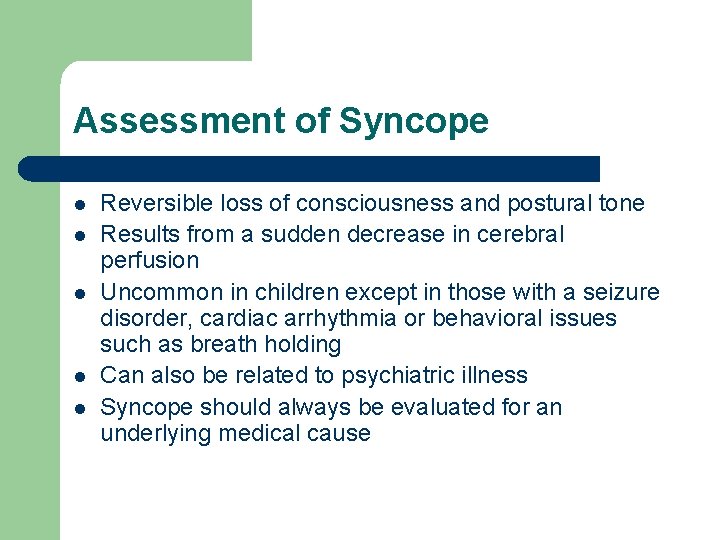
Assessment of Syncope l l l Reversible loss of consciousness and postural tone Results from a sudden decrease in cerebral perfusion Uncommon in children except in those with a seizure disorder, cardiac arrhythmia or behavioral issues such as breath holding Can also be related to psychiatric illness Syncope should always be evaluated for an underlying medical cause
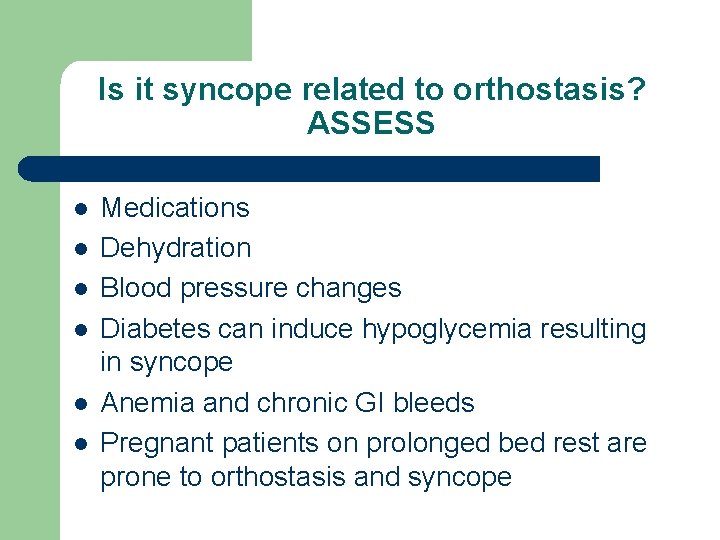
Is it syncope related to orthostasis? ASSESS l l l Medications Dehydration Blood pressure changes Diabetes can induce hypoglycemia resulting in syncope Anemia and chronic GI bleeds Pregnant patients on prolonged bed rest are prone to orthostasis and syncope
Is it syncope or “near syncope” l l l Did the person actually lose consciousness Was there dizziness, vertigo or pre-syncope (feel faint but not actually lose consciousness) Any prodromal symptoms – sweating, vertigo, nausea, yawning, aura (seizures and migraine headaches are often associated with an aura)
Psychiatric causes of Syncope l l l Psychogenic Panic and anxiety Somatization Major depression Substance abuse Physical exam is usually negative but psychiatric exam reveals symptoms
Syncope- What to do? l l l Determine if the person needs to go to the ED Ask the person what treatment they will accept- ie prefer to see own practitioner, no treatment If they refuse treatment but they are still having symptoms advise the person you are calling 911 to have him assessed and provide support.

Skin Rash
Skin Rashes l l Anxiety – causes stress and stress can cause a skin rash Negative stress releases cortisol and adrenalin into the circulation causing a skin rash. Stress also makes skin more sensitive to creams, sunscreen, and the sun causing skin rash. Stress causes skin conditions such as Psoriasis, Eczema, Acne, Rosacea and Herpes to worsen.
Skin rashes l l Anxiety producing May be serious or benign Can cause discomfort and fear May be related to medication
Skin Rashes-How to identify a drug related skin rash l l l l History Was it present in the past? Did it start when the drug was started? Did it improve when the medication was stopped? Where is the rash located? Is the person bothered by the rash? Could it be Stevens Johnson?
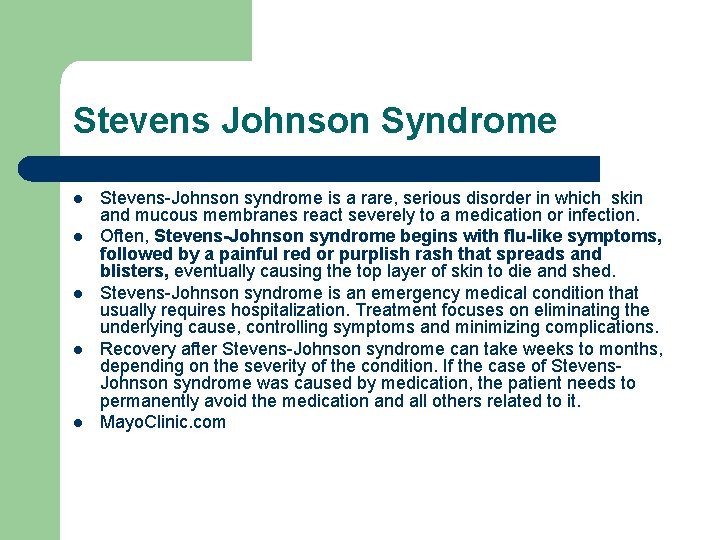
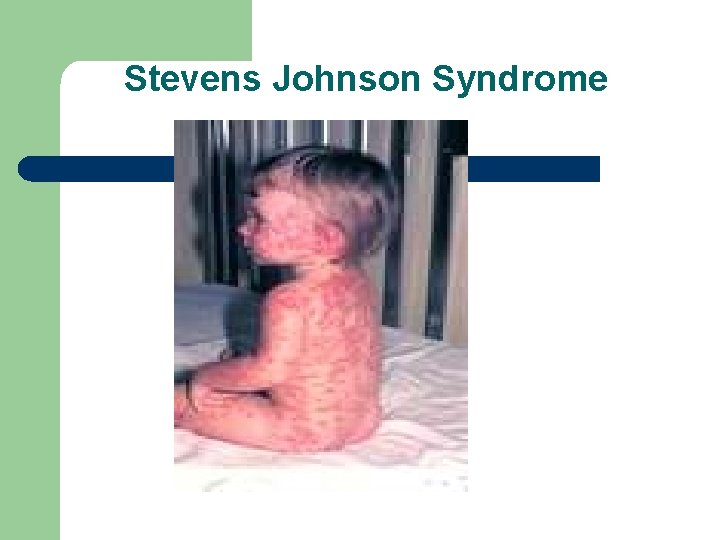
Stevens Johnson Syndrome l l l Stevens-Johnson syndrome is a rare, serious disorder in which skin and mucous membranes react severely to a medication or infection. Often, Stevens-Johnson syndrome begins with flu-like symptoms, followed by a painful red or purplish rash that spreads and blisters, eventually causing the top layer of skin to die and shed. Stevens-Johnson syndrome is an emergency medical condition that usually requires hospitalization. Treatment focuses on eliminating the underlying cause, controlling symptoms and minimizing complications. Recovery after Stevens-Johnson syndrome can take weeks to months, depending on the severity of the condition. If the case of Stevens. Johnson syndrome was caused by medication, the patient needs to permanently avoid the medication and all others related to it. Mayo. Clinic. com
Skin Rash l l l Identify the location and distribution of the lesions (localized, regional, generalized. ) Is it a primary lesion or a secondary lesion (resulting from change in the primary lesion) Identify the shape and arrangement of lesions Describe the color, borders, pigmentation and variations of the lesions Are there a few lesions or are they numerous and widespread They are more serious if they are widespread and have additional symptoms such as fever, itching, bulla, flu like symptoms

Urticaria- hives

Dermatitis

Rash from Amoxicillin

Varicella

Varicella-chicken Pox

Ringworm-Tinea Fungi

Psoriasis
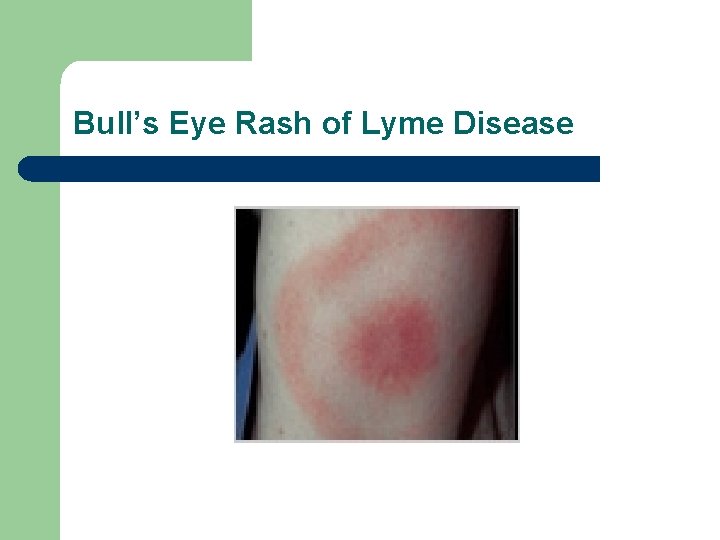
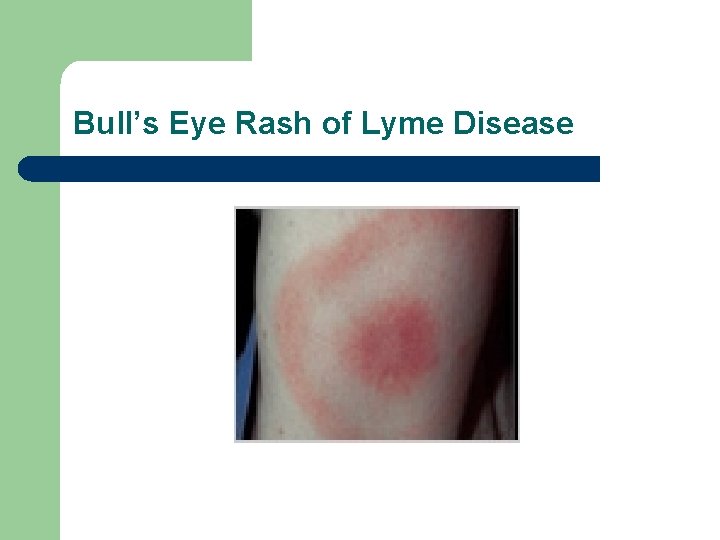
Bull’s Eye Rash of Lyme Disease
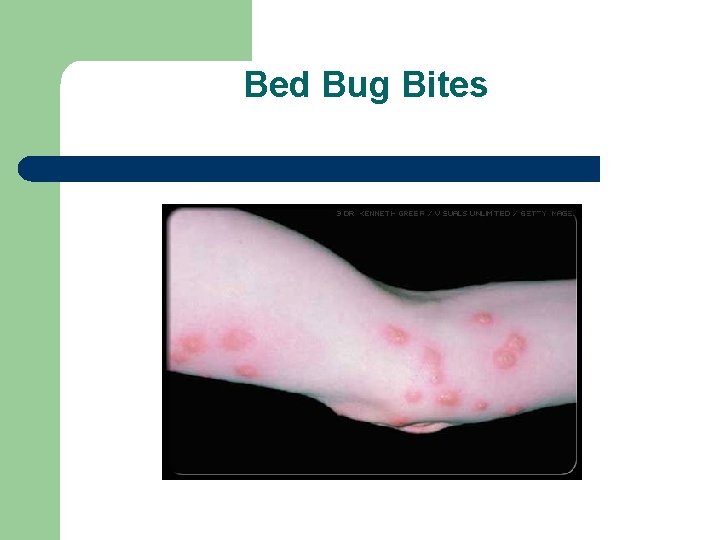
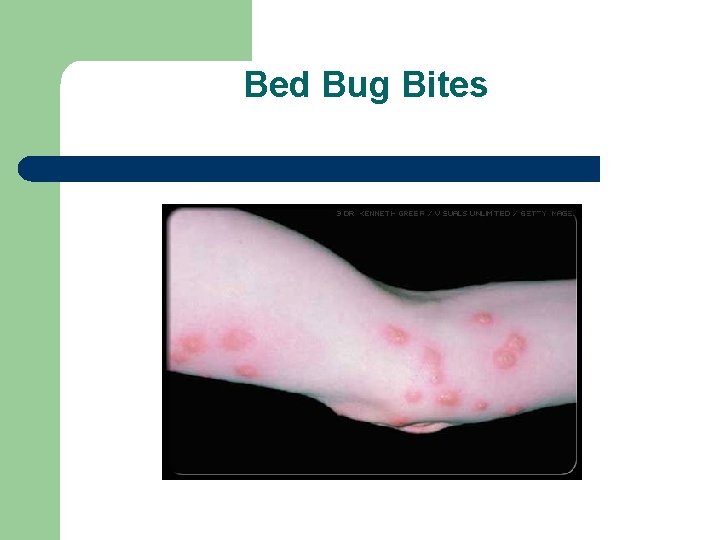
Bed Bug Bites

Shingles

Actinic Keratosis- on sun exposed skin
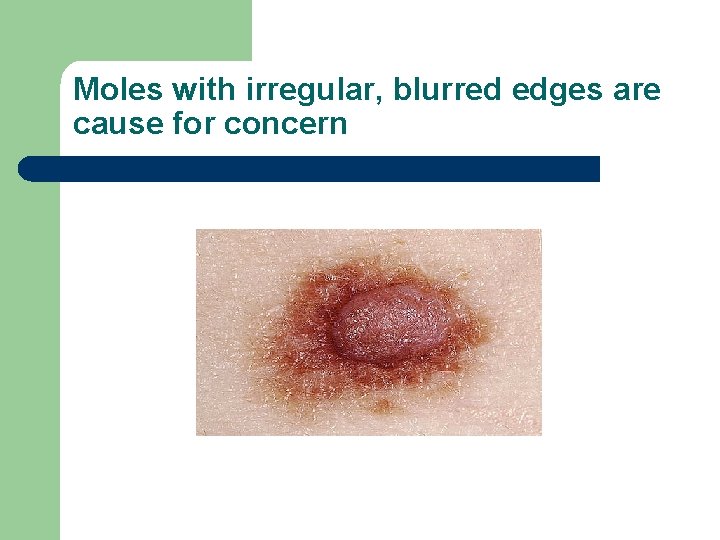
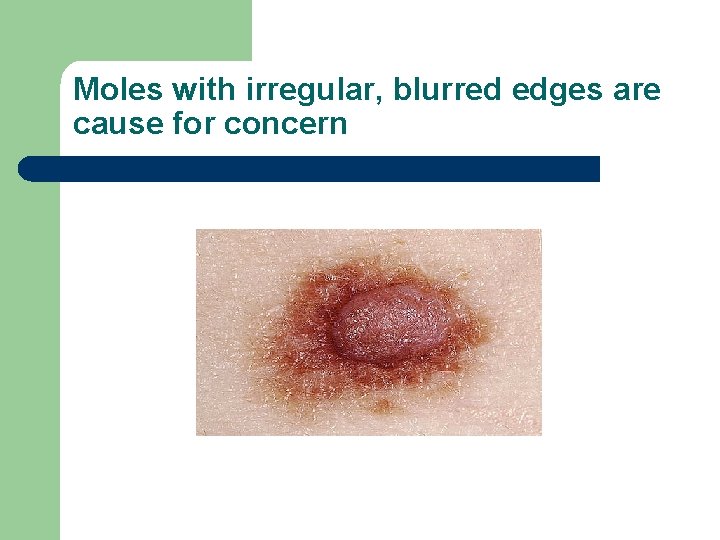
Moles with irregular, blurred edges are cause for concern
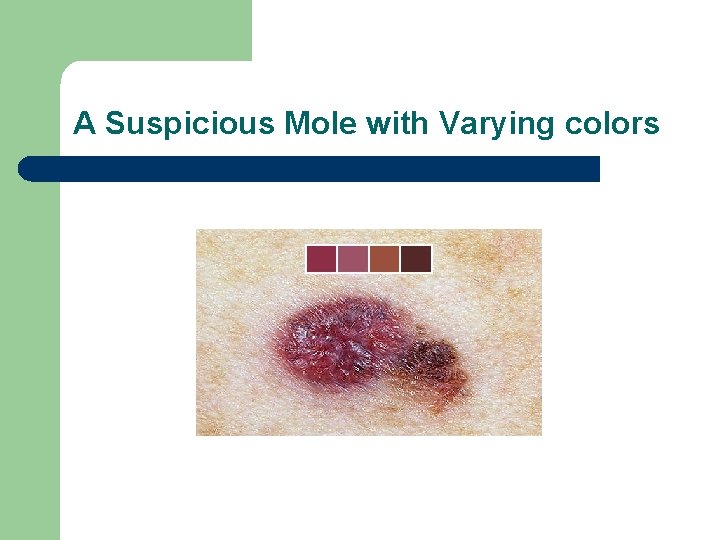
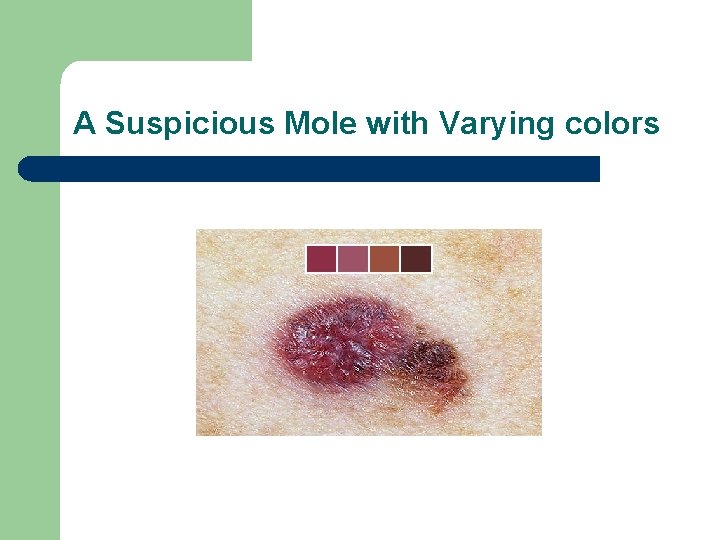
A Suspicious Mole with Varying colors
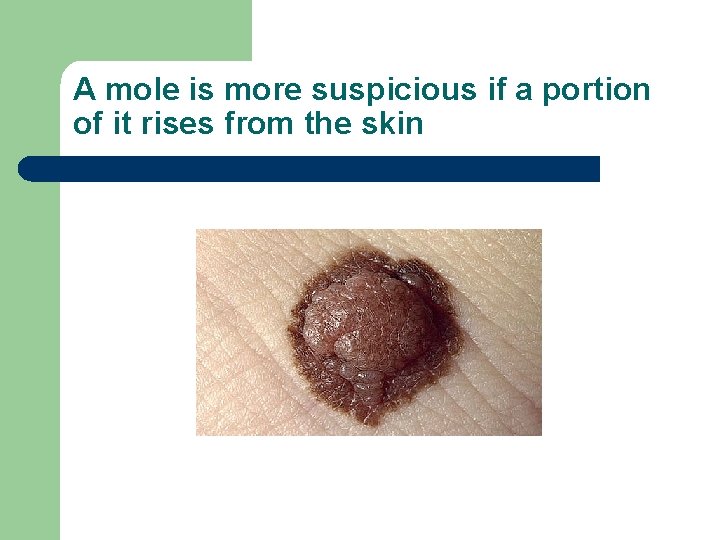
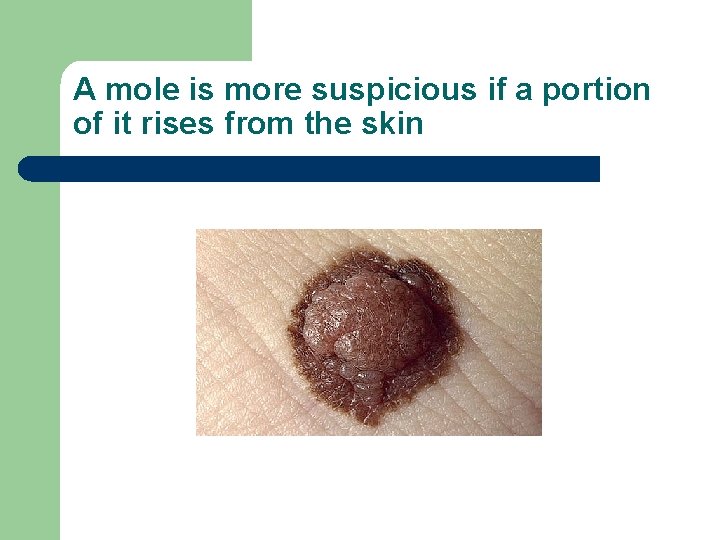
A mole is more suspicious if a portion of it rises from the skin
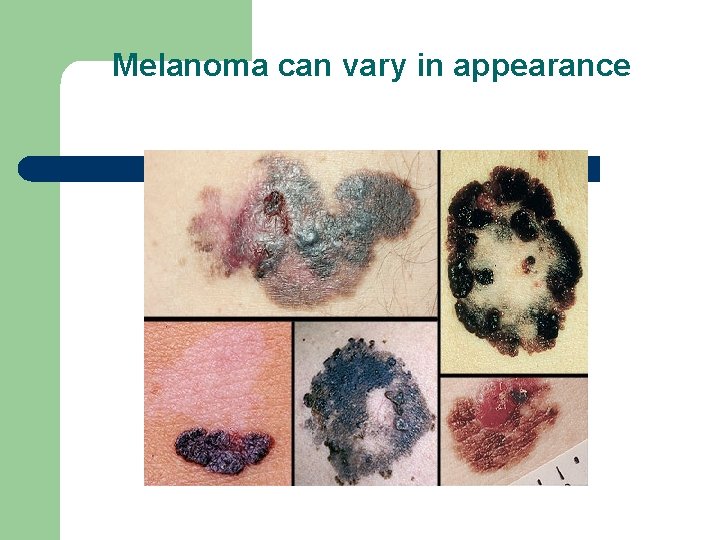
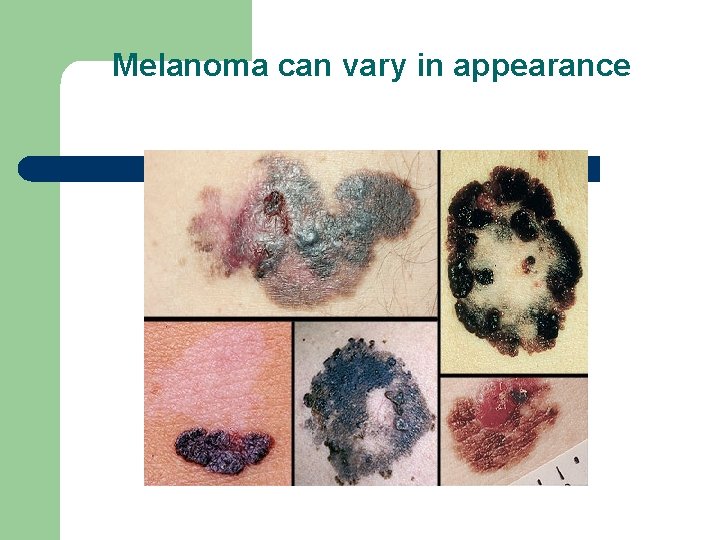
Melanoma can vary in appearance

Lamictal rash vs drug rash from Penicillin

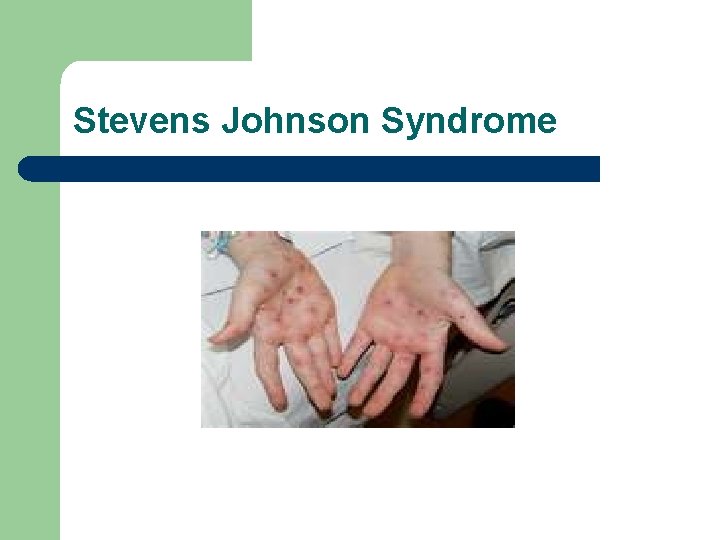
Stevens Johnson skin rash
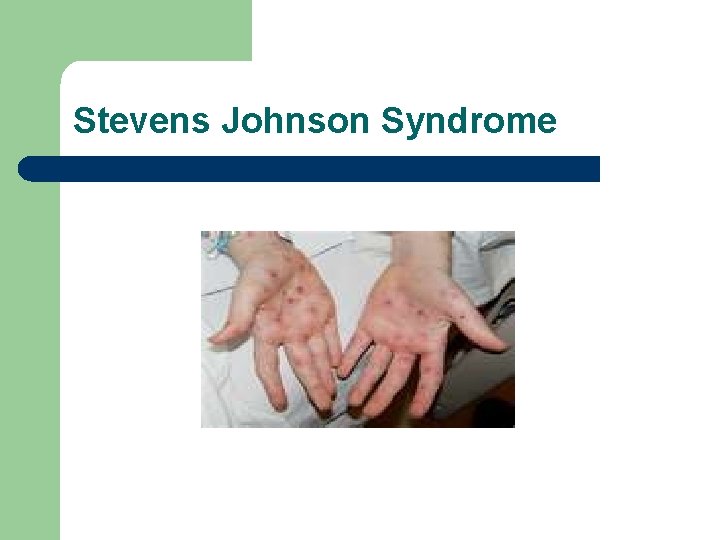
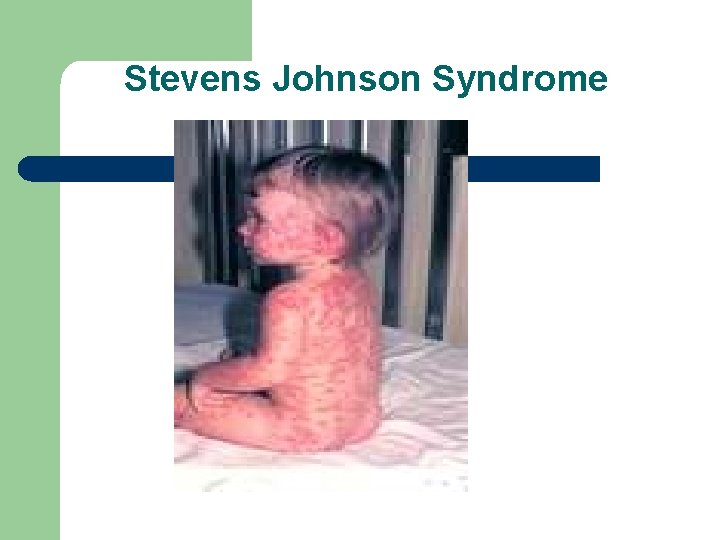
Stevens Johnson Syndrome
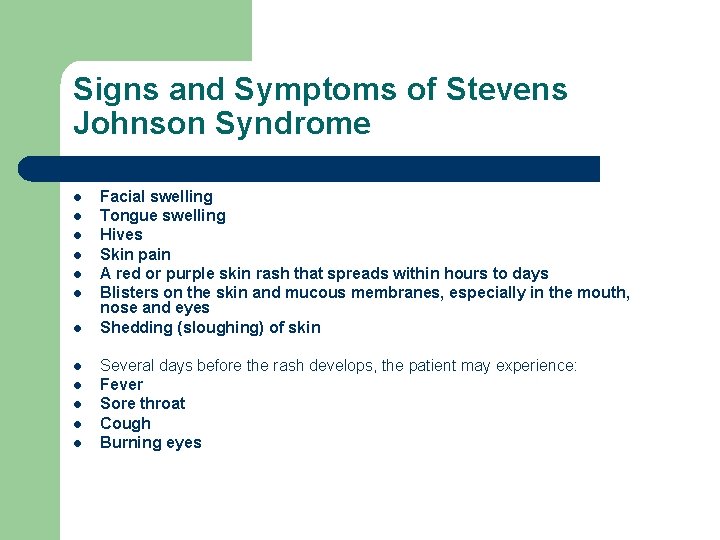
Signs and Symptoms of Stevens Johnson Syndrome l l l Facial swelling Tongue swelling Hives Skin pain A red or purple skin rash that spreads within hours to days Blisters on the skin and mucous membranes, especially in the mouth, nose and eyes Shedding (sloughing) of skin Several days before the rash develops, the patient may experience: Fever Sore throat Cough Burning eyes
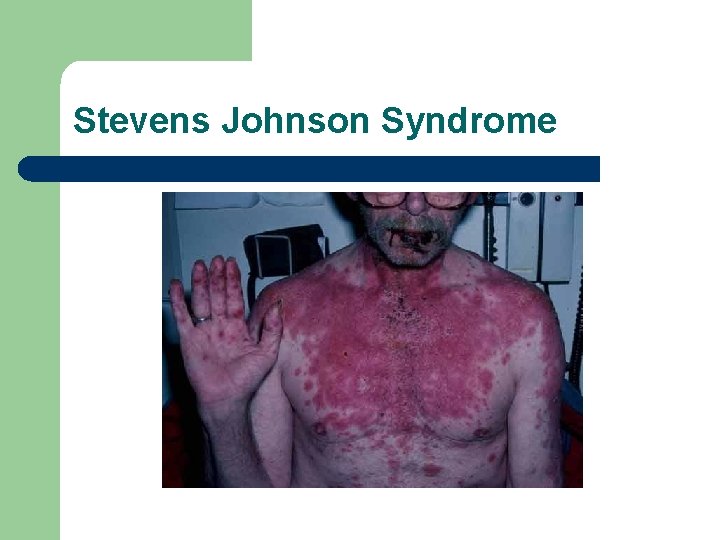
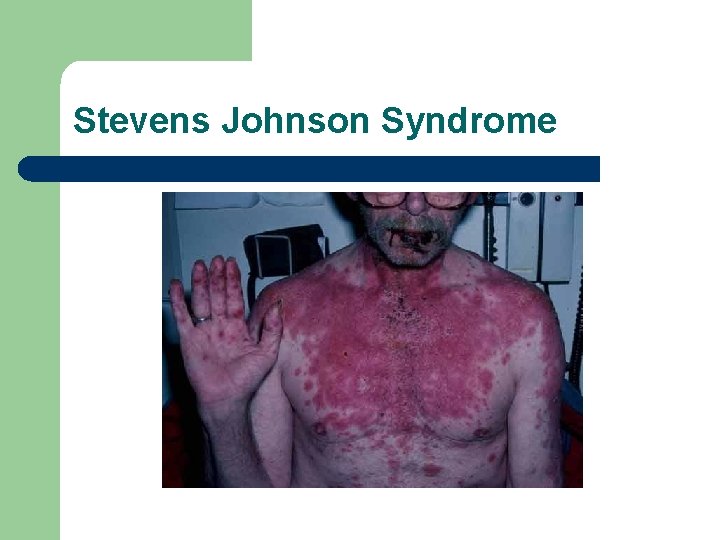
Stevens Johnson Syndrome
Causes of Stevens Johnson Syndrome l l l l The exact cause of Stevens-Johnson syndrome can't always be identified. Usually, the condition is an allergic reaction in response to medication, infection or illness. Medication causes Medications are most often the cause of Stevens-Johnson syndrome. Drugs commonly associated with Stevens-Johnson syndrome include: Anti-gout medications, such as allopurinol Nonsteroidal anti-inflammatory drugs (NSAIDs) Sulfonamides and penicillins, which are used to treat infections Anticonvulsants, which are used to treat seizures Infectious causes Infections that can cause Stevens-Johnson syndrome include: Herpes (herpes simplex or herpes zoster) Influenza HIV Diphtheria Typhoid Hepatitis Other causes In some cases, Stevens-Johnson syndrome may be caused by physical stimuli, such as radiation therapy or ultraviolet light.
Risk Factors l l l Stevens-Johnson syndrome is a rare and unpredictable reaction. No test is available to help predict who is at greater risk. Some factors, however, may increase the risk of developing Stevens. Johnson syndrome: Existing medical conditions. Viral infections, diseases that decrease immunity such as human immunodeficiency virus (HIV) and systemic lupus erythematosis. Genetics. Carrying a gene called HLA-B 12 may make a person more susceptible to Stevens-Johnson syndrome.
Complications l l l Secondary skin infection (cellulitis). This acute infection of the skin can lead to life-threatening complications, including meningitis. Sepsis occurs when bacteria from a massive infection enter the bloodstream and spread throughout the body. Sepsis is a rapidly progressing, life-threatening condition that can cause shock and organ failure. Eye problems. The rash caused by Stevens-Johnson syndrome can lead to inflammation in the eyes. In mild cases, this may cause irritation and dry eyes. In severe cases, it can lead to extensive tissue damage and scarring within the eyes that can result in blindness. Damage to internal organs. Stevens-Johnson syndrome can cause lesions of the internal organs, which can result in inflammation of the lungs (pneumonitis), heart (myocarditis), kidney (nephritis) and liver (hepatitis). Permanent skin damage. When the skin grows back following Stevens. Johnson syndrome, it may have abnormal bumps and pigmentation. Scars may remain on the skin. Hair may fall out, and fingernails and toenails may not grow normally.
Stevens Johnson Syndrome
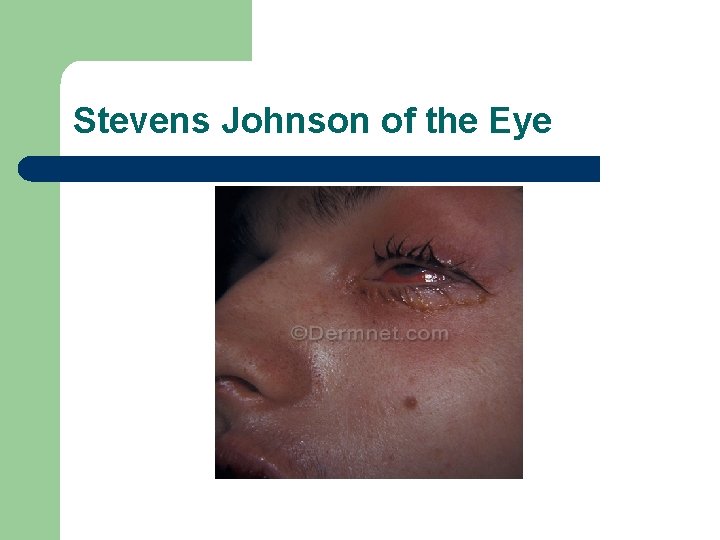
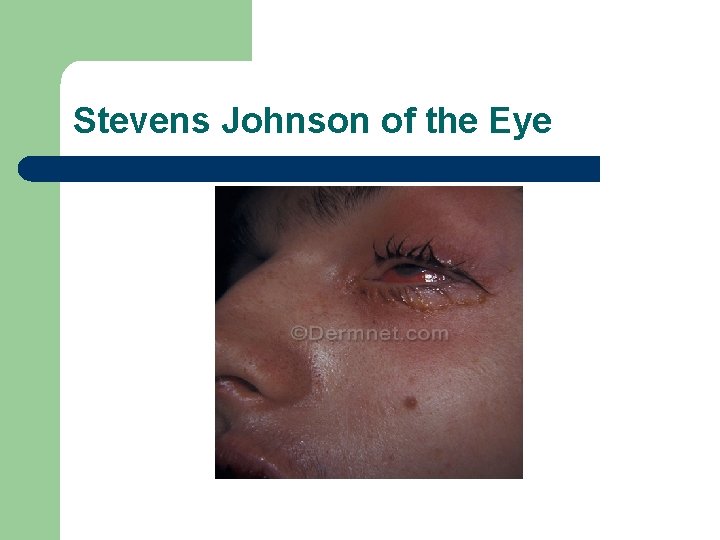
Stevens Johnson of the Eye

Severe Stevens Johnson
Let’s test your assessment skills with shin rashes

Stevens Johnson and drug rash

Dermatitis and drug rash

Drug rash from Tegretol and bed bug bites

Bed Bug Bites vs. shingles

Lamictal rash vs. rash from Penicillin
Neurologic illness and changes in mental status l l Seizures Change in mental status

Psychogenic Non Epileptic Seizures (PNES) l l l Psychogenic seizures are caused by subconscious thoughts, emotions or negative stress They are not caused by abnormal electrical activity in the brain as are epileptic seizures They are psychological in nature, but the person is not faking the seizure and is usually not aware of them nor can they control them. The term "pseudo seizures" has also been used They can be caused by negative life events such as childhood abuse, or any severe stressful event
Psychogenic Non Epileptic Seizures l l l Psychogenic non epileptic seizures are common. About 20% of the patients referred to comprehensive epilepsy centers for Video-EEG monitoring are found to have non epileptic seizures. About 1 in 6 of patients with PNES also has epileptic seizures or has had them in the past. 70% of the cases develop between the age of 20 -40 but they also can occur in children and the elderly. They are three times more common in females. Video-EEG monitoring is the best way of diagnosing non epileptic seizures
Psychogenic Non Epileptic Seizures l l The seizures may look like complex partial or tonic-clonic (grand mal) seizures. Certain kinds of movements are more common in psychogenic non epileptic seizures than in seizures caused by epilepsy. Epileptic seizure- loss or change in consciousness, jerking or spasm movement of limbs usually in a repetitive motion, movement is more synchronized rather then thrashing. PNES- violent thrashing of all four limbs, arms and legs move in various directions, may have pelvic jerking, consciousness varies

Psychogenic Non Epileptic Seizures. Treatment l l l Psychiatric evaluation to determine if there is an underlying psychiatric problem. A diagnoses of psychogenic seizures does not necessarily mean that a person has a serious psychiatric disorder. Sometimes the episodes stop when the person learns that they are psychological. Can learn how to control the events with behavioral techniques such as relaxation therapy or other forms of cognitive behavioral therapy. Medication management to treat any psychiatric disorder People who have both epilepsy and psychogenic non epilepsy seizures will require an anticonvulsant medication as well as treatments for the psychogenic events. A person with PNES without epilepsy does not need anticonvulsant medication.
Case Study Janice l l 48 y o woman with a history of mild cognitive impairment, history of major depressive disorder with psychotic symptoms She lives in a group home and is able to attend program 5 days per week, goes on trips with the group home and can do her own self care She has a history of seizure disorder. She came to the office for her medication management
What to Do? l l l Is it a psychogenic or epileptic seizure? How do we treat it? What emergency measures are needed?
Change in Mental Status l l l Confusion Mood and Behavior Changes New psychiatric symptoms New Medications Physical illness
Assessment l l l l Complete health history from the patient if possible and from the family Level of orientation Symptom assessment Recent falls or trauma, infections Use of drugs or alcohol Suicidal thoughts or statements New medications Bereavement
Assessment l l l l Any fever or recent illness Difficulty in walking, tremors Loss of appetite, nausea or vomiting Interest in activities History of mental illness History of chronic illnesses Correct doses of medications
Psychopathology l l l Substance abuse Pharmacologic induced adverse events Dementia Mood disorder Psychosis Suicide ideation and attempt
Acute Confusional State l l l l Hospitalization or surgery Electrolyte imbalance Organ failure Polypharmacy Nutritional deficiency Systemic infection Cerebral insufficiency-TIA or CVA Substances
Confusion l l l Delirium Dementia Depression
Delirium l l l l Symptom of a medical condition Alteration in brain metabolism Acute onset, change in level of consciousness, may include aggression Disorganized thought process with disorientation. Difficulty with focus and concentration Disturbance in the sleep/wake cycle May include psychotic symptoms, usually visual hallucinations or delusions
Dementia l l l Gradual onset of confusion Chronic impairment of brain function Thinking and reasoning affected Level of consciousness is unaffected Memory deficits, impaired concentration May be reversible, modifiable or irreversible
Dementia l l l l Impairment of intellectual function Language (aphasia) Memory Visuospatial disturbance (apraxia-cannot complete motor activities, agnosia-does not recognize what was familiar) Emotional, behavioral or personality changes Impaired cognition Problems with calculation, abstraction, and judgment
Depression l l l l Can produce confusion in the elderly Persistent sad mood Anhedonia Change in appetite and sleep Lack of motivation Self care deficits May have suicidal thoughts or thoughts of giving up
Pharmacologic-induced adverse events that can alter mental status l l l Agranulocytosis-Absence of polymorphonuclear leukocytes, relative lymphopenia, WBC count of 2, 000/cu mm or less Hpyotension and cardiac conditions Lithium toxicity Anticholinergic psychosis Hypertensive crisis
Hypotension and Cardiac conditions l l Some Neuroleptics and antidepressants can lower BP Tricyclic antidepressants can cause heart block, brady and tachy arrhythmias and conduction delays Tricyclics and antipsychotics can prolong the QT interval with resulting ventricular arrhythmias Risk of seizures
Lithium Toxicity l l l GI complaints Ataxia Slurred speech Delirium Coma
Anticholinergic Psychosis: A toxic confusional state in which auditory, visual or tactile hallucinations, irritability and assaultiveness accompany delirium l l l Antidepressants Low-potency antipsychotics Anticholinergic antiparkinsonian agents Demerol Atropine Over the counter analgesic/antihistamine combinations, “PM” medications
Anticholinergic Psychosis: Symptoms l l l l Dry mouth Constipation Paralytic ileus Vertigo Urinary retention Increased intraocular pressure Cardiac arrhythmias Tactile hallucinations
Treatment Options l l l Reduce polypharmacy Warn about OTC medications Importance of medical follow-up Importance of therapy for depression and anxiety and other psychiatric disorders Non-pharmacologic interventions Nutrition and exercise
Case Study- change in mental status l l l Annette is a 42 year old AA woman who is married with two children age 16 and 18. She has a history of post partum depression with her second child She has a college education and works part time in retail PMH: Hypertension and GERD PPH: Depression treated with Sertraline 50 mg daily in the past
Annette l l Annette is 37 weeks pregnant Delivery was induced due to pregnancy induced hypertension Seen by Psychiatric/Mental Health APN the day after delivery due to her history of recent depression and past post partum depression She was not on any psychotropic medication during the pregnancy
Annette l l l She was awake, alert and oriented She reported her mood as mildly depressed but more overwhelmed She felt tired as she has not been sleeping well She did not want to resume her antidepressant at this time She was interested in the baby and was holding her
Annette l l l 4 days post partum she returned to the ED due to persistent hypertension and change in mental status. ED physician thought she might be depressed Psychiatry was called due to her current mood change and past history of depression Annette was sitting on the stretcher with a flat affect, little eye contact, crying, slow speech with poverty of content
Annette- Initial Impression l l l Major Depression with possible catatonic state Post partum depression Medical delirium due to possible electrolyte imbalance, infection
Neurological Exam l l l Mental Status Cranial Nerves Cerebellar Testing Motor Strength Testing Sensory Testing Deep Tendon Reflexes
Mental Status Exam l l l AA&O, little eye contact, crying silently, staring behavior, blank look No weakness, able to walk, able to sit up and not fall over She tried to cooperative with questioning Blood work and EKG all WNL BP 156/92, P=104 R=18 Pulse ox 98% on room air. What else would you test?
Mental Status Exam l l l Able to spell WORLD forward but not backward Unable to calculate serial 7’s She tried serial 5’s but was unable Count backward from 100 - she tried but was unable. What does this tell you?
Annette l l l Annette is a college graduate- she may have trouble with serial 7’s due to depression or anxiety and maybe would have trouble with serial 5’s But she should be able to count backward from 100 Even a depressed person who is trying to cooperate as Annette was should be able to count backwards from 100
Diagnosis l l l Delirium from a medical illness- etiology to be determined While she may be depressed this current illness is medical and not related to depression Annette had a medical work up including an MRI of her head.
She had an intracerebral hemorrhage (ICH) l l l ICH accounts for a substantial portion of pregnancyrelated mortality. The risk of ICH associated with pregnancy is greatest in the postpartum period. Advanced maternal age, African American race, hypertensive diseases, coagulopathy, and tobacco abuse were all independent risk factors for pregnancy-related ICH. Intracerebral hemorrhage in pregnancy B. T. Bateman, MD, et al Neurology August 8, 2006 vol. 67 no. 3 424 -429
Conclusion l l l Annette was admitted to the ICU and treated successfully Her family took care of the baby and the other children Annette was transferred to a sub acute rehab and made slow but steady progress
Sleep Disturbances. Assessment, Diagnosis and Treatment
I can’t sleep! l l l Is this an emergency? Is it related to a medical illness? Medication related? Substance related? Before you prescribe the sleeping pills… Take the time to determine the underlying cause
Sleepiness- Regulated by two primary processes l l The body’s circadian rhythm Physiologic need for sleep Sleep is often disturbed in people with mental and physical illness Sleep may also be disturbed by poor sleep hygiene
Sleep Hygiene l l l l Avoid napping during the day. It disturbs the normal pattern of sleep and wakefulness. Avoid stimulants such as caffeine, nicotine, and alcohol too close to bedtime. Alcohol can initially induce sleep but it disrupts sleep later as the body begins to metabolize the alcohol, causing arousal. Exercise can promote good sleep. Vigorous exercise should be taken in the morning or late afternoon. Relaxing exercise, like yoga, can be helpful to induce rest and sleep. Food can be disruptive right before sleep. Avoid large meals, caffeine and sugary foods near bedtime. Ensure adequate exposure to natural light. Light exposure helps maintain a healthy sleep-wake cycle. Establish a regular relaxing bedtime routine. Avoid emotionally upsetting conversations and activities before trying to go to sleep. Don't dwell on, or bring your problems to bed. Associate your bed with sleep and sexual activity. It's not a good idea to use your bed to watch TV or listen to the radio as that can be stimulating. Reading or listening to soothing music can help induce sleep
Types of Insomnia l . There used to be two types of insomnia: primary insomnia and secondary insomnia. Now it is all Insomnia disorders Primary insomnia: sleep problems that are not directly associated with any other health condition or problem. Secondary insomnia: sleep problems related to a health condition such as depression, anxiety, asthma, pain, or due to a medication of substance such as alcohol.
Insomnia l l l Acute insomnia can last from one night to a few weeks. Chronic insomnia occurs when a person has insomnia at least three nights a week for a month or longer. Need dissatisfaction with sleep and sleep dysfunction for the diagnosis of insomnia
Obtain a comprehensive sleep history l l l l Describe the sleep problem Difficulty falling asleep, staying asleep or falling asleep during the day Restless legs Obstructive Sleep apnea-snoring, stop breathing Food, stimulants, drugs, ETOH use Sleep hygiene Lifestyle related Ask about PTSD as most people with PTSD have sleep disturbance
Key Indicators for Insomnia l l l If the person has a good nights sleep does he feel much better the next day? If the answer is “Yes” it’s probably a diagnosis of Insomnia If the answer is “No” the sleep disturbance is more likely related to a psychiatric/mental health illness
Insomnia l l Not Age related-older people do not necessarily have insomnia Conditioned insomnia- associate the bedroom with difficulty sleeping, able to fall asleep in front of the TV but not in bed Sleepwalking Secondary to illness or medication-GERD, COPD, peptic ulcer disease, CHF, DM, prostatic hypertrophy, PTSD
Physical Exam l l l Vital signs, height and weight Inspect the ears for infection Inspect the nose for obstruction, secretion Inspect the mouth, throat and neck- for narrow pharyngeal space, enlarged tonsils or uvula. A heavy or thick neck is a risk factor for sleep apnea. Auscultate the lungs- wheezing, congestion Palpate the abdomen- abdominal pain, distended bladder
Laboratory and Diagnostic Tests l l l Sleep diary Sleep studies- for sleep apnea Blood work
Treatment l l l l Sleep diary Improved sleep hygiene Cognitive Behavioral techniques Relaxation techniques Lifestyle changes Change in food, fluid, alcohol and drug use Medication
Medication l l l Prazosin- research evidence for it’s benefit in treating nightmares in PTSD and also useful for non-PTSD nightmares Trazodone- doses over 100 mg can cause orthostasis Remeron- warn client of weight gain Gapapentin- can help with sleep by reducing anxiety- BID dosing more useful. 300 -600 mg or higher is usually well tolerated Orexin antagonist- brand name of Belsomra (suvorexant)- new class of med for insomnia Caution with Klonopin for sleep- half life is 40 hours- person is prone to daytime drowsiness and impaired function
Movement Disorders
Differential Diagnosis l l l Tourette Syndrone Cerebral palsy Parkinson disease Stroke Restless leg syndrome Essential tremor
What is Essential Tremor? l l Essential tremor is a neurological disorder that causes a rhythmic shaking. It can affect almost any part of the body, but the trembling occurs most often in hands — especially when drinking from a glass, tying shoelaces, writing or shaving. Essential tremor may also cause a rhythmic head movement and change in voice. Essential tremor worsens over time and can be severe in some people. It isn't caused by other diseases, although it's sometimes confused with Parkinson's disease. Essential tremor can occur at any age but is most common in people age 40 and over.
Essential Tremors l l l Begin gradually Worsen with movement Usually occur in the hands first, affecting one hand or both hands Can include a "yes-yes" or "no-no" motion of the head May be aggravated by emotional stress, fatigue, caffeine or extremes of temperature.
Essential Tremors l l l Essential tremor vs. Parkinson's disease Many people associate tremors with Parkinson's disease, but the two conditions differ in key ways: Timing of tremors. Essential tremor of the hands are intention tremors- they occur with use of the extremity. Tremors from Parkinson's disease are most prominent at rest. Associated conditions. Essential tremor is not usually associated with other symptoms but Parkinson's disease is associated with a stooped posture, slow movement and a shuffling gait. However, people with essential tremor may sometimes develop ataxia. Parts of body affected. Essential tremor mainly involves hands, head and voice. Parkinson's disease tremors usually start in hands, and may affect legs, chin and other parts of the body. Mayo clinic. org
Causes of Essential tremor l l l About half of essential tremor cases appear to result from a genetic mutation. This form is referred to as familial tremor. It isn't clear what causes essential tremor in people without a known genetic mutation. Research has found that changes in specific areas of the brain may contribute to essential tremor. Mayoclinic. org
Treatment for Essential Tremor l l l Beta blockers. propranolol (Inderal) help relieve tremors in some people. Other beta blockers that may be used include atenolol (Tenormin), and metoprolol (Lopressor), Beta blockers are not an option for people with asthma or certain heart problems. Side effects may include fatigue, lightheadedness or heart problems. Anti-seizure medications. Epilepsy drugs, such as primidone (Mysoline), may be effective in people who don't respond to beta blockers. Other medications that may be prescribed include gabapentin (Neurontin) and topiramate (Topamax). . Benzodiazepines such as alprazolam (Xanax) and clonazepam (Klonopin) to treat people whose tremors are made worse by tension or anxiety. Onabotulinumtoxin. A (Botox) injections. Botox injections may be useful in treating some types of tremors, especially head and voice tremors. Botox injections can improve tremors for up to three months at a time. However, if Botox is used to treat hand tremors, it can cause weakness in hand fingers. If it's used to treat voice tremors, it can cause a hoarse voice and difficulty swallowing.
Extrapyramidal Symptoms l l Akathisia- difficulty controlling movement Dystonia Pseudoparkinsonism Dyskinesia- difficulty initiating movement


Cause of EPS l l l The most common cause of EPS is from antipsychotics. Other anti-dopainergic drugs like the antiemetic metoclopramide (Reglan) or prochlorperazine (Compazine) or the tetracyclic antidepressant amoxapine (Asendin) can also cause extrapyramidal side-effects. Another common cause are SSRI’s, which indirectly decrease dopamine via 5 -HT 2 and 5 -HT 3 postsynaptic serotonin neurotransmission. Akathesia is the most common EPS symptom from SSRI’s Extrapyramidal symptoms can also be caused by brain damage, as in cerebral palsy, encephalitis and meningitis.
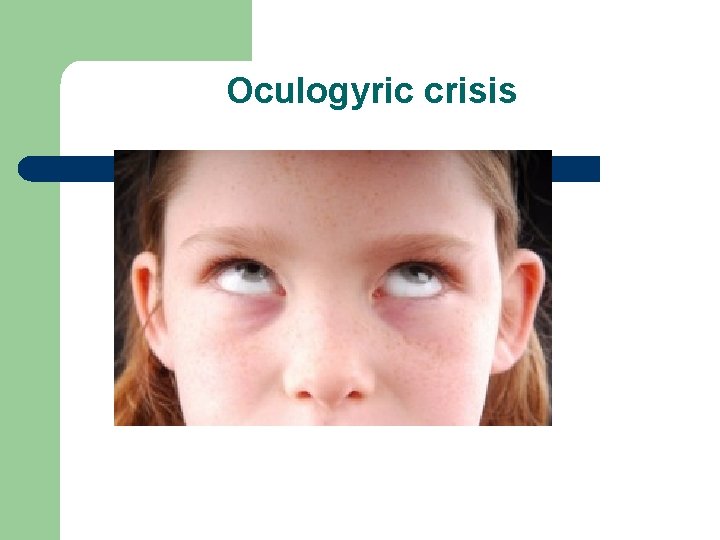
EPS l l l Acute dystonic reactions- muscular spasms of neck (torticollis), eyes (oculogyric crisis), tongue, or jaw; more frequent in children Akathisia: A feeling of motor restlessness Pseudoparkinsonism: drug-induced parkinsonism (cogwheel rigidity, bradykinesia/akinesia, resting tremor, and postural instability; more frequent in adults and the elderly). Although Parkinson’s disease is primarily a disease of the nigrostriatal pathway and not the extrapyramidal system, loss of dopaminergic neurons in the substantia nigra leads to dysregulation of the extrapyramidal system. Since this system regulates posture and skeletal muscle tone, a result is the characteristic bradykinesia of Parkinson's. Tardive dyskinsia: involuntary asymmetrical movements of the muscles, a long term chronic condition associated with long term use of antipsychotics.
Akathisia l l l Inner motor restlessness Feels anxious, impaired concentration Can be describes as “anxiety” Pacing, marching, shuffling, foot-tapping, rocking, shifting body weight from leg to leg. Restlessness can be in one body area or generalized over the body
Dystonic Reactions l l Involuntary muscle contraction of head, neck, trunk, extremities Most often affected areas are the head and neck including tongue, throat face, eyes and jaw. Voice may be hoarse, tongue stiff or thick Medical emergency if it causes laryngeal or pharyngeal spasms and potential obstruction
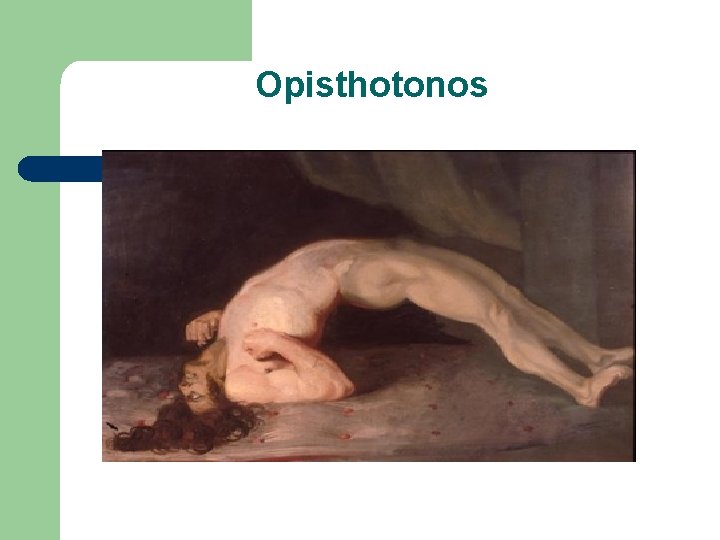
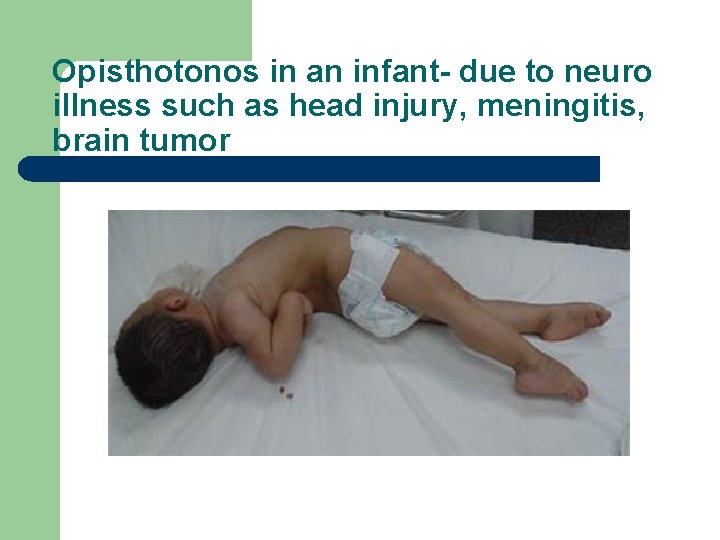
Dystonic Reactions l l l Torticollis- contorting or twisting for cervical spine muscle Oculogyric crisis- rolling of the eyes in a locked upward position Opisthotonos- a severe form of back arching

Spasmodic Torticollis
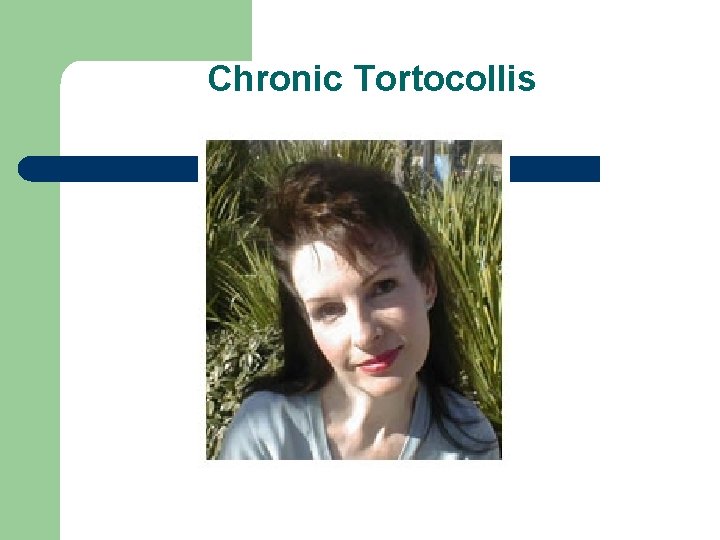
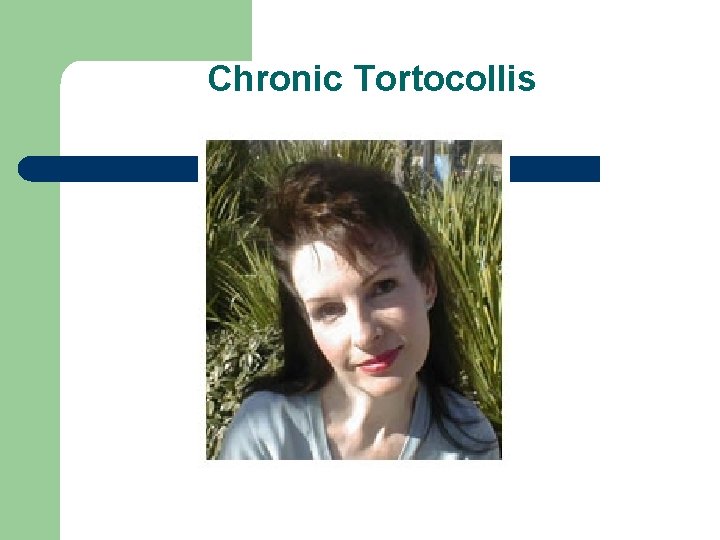
Chronic Tortocollis
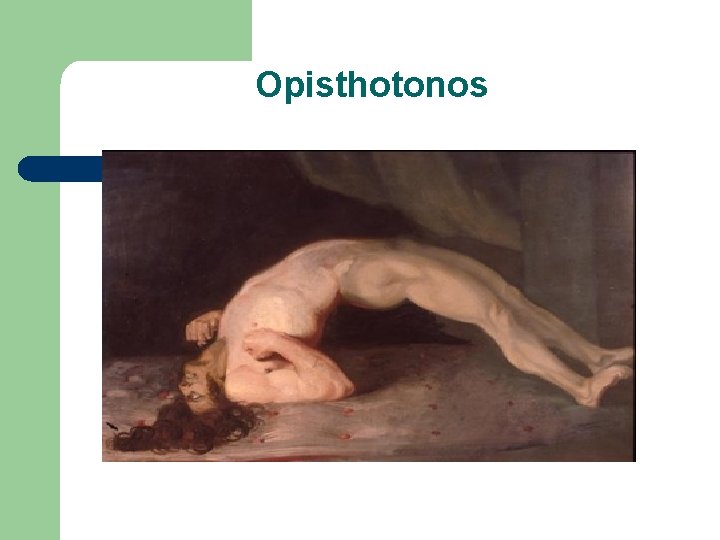
Opisthotonos
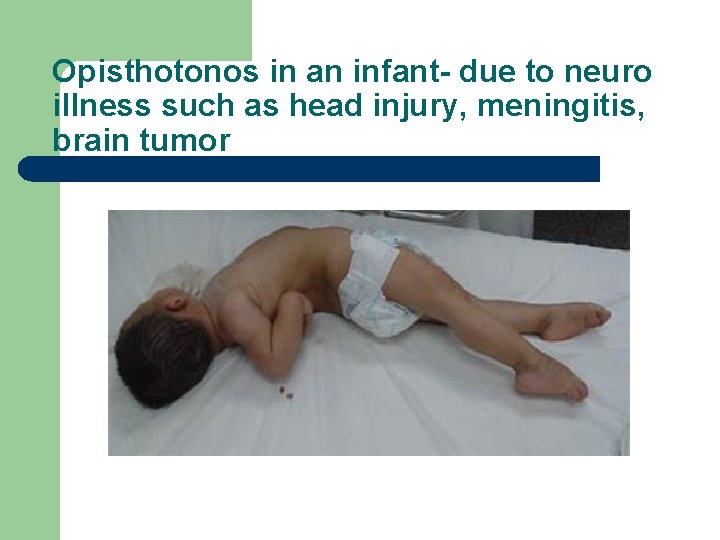
Opisthotonos in an infant- due to neuro illness such as head injury, meningitis, brain tumor
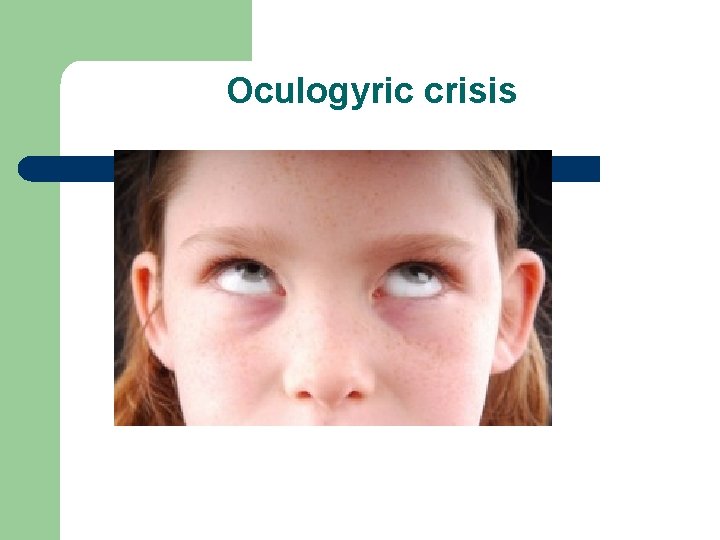
Oculogyric crisis
Case Study- Jane l l l Jane is a 28 year old female with mild developmental disabilities She has Bipolar disorder and takes Lithium and Clozaril She lives in a group home On a routine visit she told me her eyes are at times “rolling back in my head” The staff of the group home thought she was making this up so did not report it. What do you think?
Pseudoparkinsonism l l l Pill rolling finger tremors Mask like facial expression Weakened voice Absence of arm swing Stiff stooped posture Shuffling gait
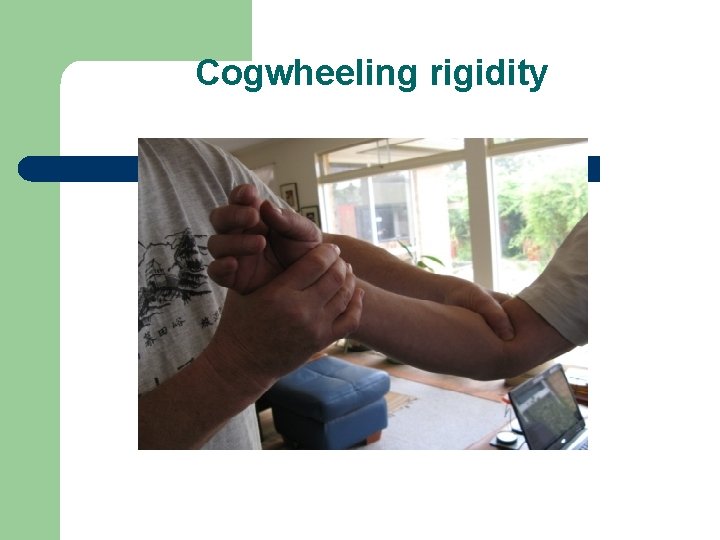
Pseudoparkinsonism l l l Cogwheeling rigidity Bradyphenia- slowed ability to think through familiar situations Rabbit syndrome- tremor of the lip and a constant chewing motion. Usually from prolonged use of an antipsychostic
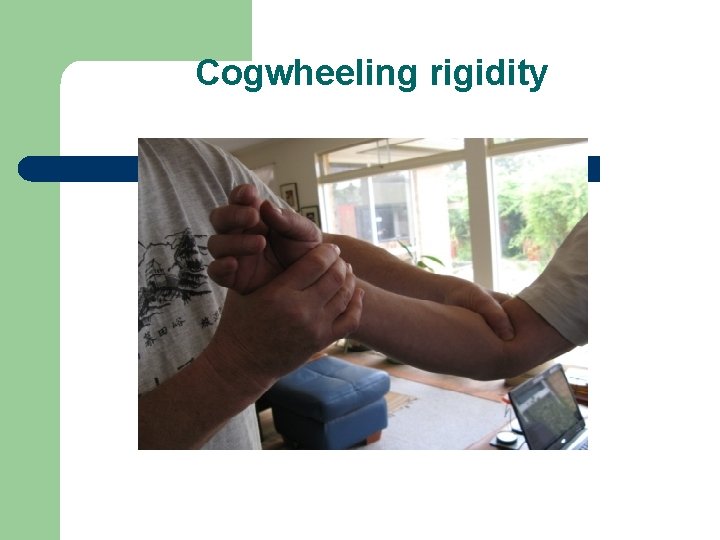
Cogwheeling rigidity

Dyskinesia l l Rapid, repetitive, involuntary movements of the face, trunk, respiratory muscles and extremities. Facial movements can include protruding or rolling tongue, lip smacking, grimacing, frowning, sucking or kissing motions, and facial distortions. It is a late appearing side effect of antipsychostic medications. The symptoms may be irreversible.
Clinical management l l Identify the symptoms Reduce the dose of the antipsychotic- may help with symptoms other then tardive dyskinesia Change medications Akathisia usually responds to discontinuation of the medication and addition of a Benzodiazepine
Clinical management of EPS l l l Benzodiazepines- Lorazepam, Diazepam or Alprazolam, Clonazepam Beta blockers- Propranolol Pramipexole (Mirapax) – dopamine agaonist. Reverses the symptoms of extrapyramidal side effects caused by antipsychotics or other drugs that either directly or indirectly inhibit dopaminergic neurotransmission.
Anticholinergic and Antiparkinson agents l l l Diphenhydramine (Benadryl), 25 -50 mg PO TID-QID or 2550 mg IM or IV for acute symtpoms Benztropine mesylate (Cogentin), 1 -3 mg PO BID or 1 -2 mg IM or IV Bromocriptione mesylate (Parlodel), 1. 25 -2 mg IM or IV Trihexyphenidyl (Artane) 2 -5 mg PO TID Reserpine- anti hypertensive also used for acute agitation in psychiatric disorder and may be used for the agitated movements of EPS- dose 0. 1 to 1 mg daily Botox
In conclusion l l Use your critical thinking skills to rapidly assess the patient who presents with unusual symptoms The more symptoms the more likely it is serious Use physical assessment skills to do a quick evaluation. Use your team to access treatment
The diagnostic process-symptom assessment l l l l Timing, onset, duration, frequency Anatomical location Character or quality Setting in which they occur Severity or intensity Aggravating or alleviating factors Associated symptoms Client’s perception of the meaning of the symptoms
References l l l Benbadis, S; Lutsep, H. Psychogenic Nonepileptic Seizures. Medscape. March 19, 2013: 1 -6. Courey, Tamra c. Detection, Prevention, and Management of Extrapyramidal Symptoms. Journal of Nurse Practitioners. 2007; 3(7)” 464 -469. Dains, Joyce E; Baumann, Linda C; Scheibel, Pamela. Advanced Health Assessment and Clinical Diagnosis in Primary Care. 3 rd ed. 2007. Mosby –Elsevier. Freudenreich, Oliver. Differential Diagnosis of Psychotic Symptoms: Medical “Mimics. ” Psychiatric Times. Dec. 3, 2012 Griffith, D. Pseudoseizures: Evaluation and Treatment. Medscape Psychiatry and Mental Health e. Journal. 1997: 2(2). Amp.
References l l l Madhusudanan, M. Psychiatric Symptoms in Neurological Practice. Annals of Indian Academy of Neurology. 2006; 9: 72 -89. http: //www. annalsofian. org/text. asp? 2006/9/2/72/25979. Panegyres, P; Graves, A. ; Frencham, K. The Clinical Differentiation of Fronto-Temporal Dementia from Psychiatric Disease. Neuropsychiatric Disease Treatment. Oct. 2007: 3(5): 637 -645 Pringsheim, Tamara et al. Treatment Recommendations for Extrapyramidal side Effects Associated with Second Generation Antipsychotic use in Children and Youth. Paediatrics and Child Health. Nov 2011; 16(9): 590 -598. Virani, A, et al. Clinical Handbook of Psychotroptic Drugs 19 th ed. Hogrefe Publisher: 2012 Winkelman, J. Psychopharmacology and Sleep Disorders. Massachusetts General Psychiatry Academy, 38 th Annual Psychopharmacology Conference. Oct. 24 -26, 2014
References l l l l Mayo clinic. org American Heart Assn. , www. heart. org Epilepsy foundation, Epilepsy. com Non epileptic seizure www. youtube. com/watch? v=GVIr. GYSYi. Zk search: Dystonic reaction video on you tube Recognizing Extrapyramidal symptoms video part 1 and 2. You tube. com Slide show for skin rashes http: //www. mayoclinic. org/skin-rash/SLS-20077087
 Tender nipples sign of pregnancy
Tender nipples sign of pregnancy Differentiating factors in constructing market indexes
Differentiating factors in constructing market indexes Differentiating process examples
Differentiating process examples Differentiate trigonometric functions
Differentiate trigonometric functions The chain rule
The chain rule Scaffolding vs differentiation
Scaffolding vs differentiation Contoh differentiating competencies
Contoh differentiating competencies Knapps relationship stages
Knapps relationship stages Differentiating factors in constructing market indexes
Differentiating factors in constructing market indexes Differentiating acceleration
Differentiating acceleration Contoh differentiating competencies
Contoh differentiating competencies Differentiating process examples
Differentiating process examples How to find derivative of inverse function
How to find derivative of inverse function Ethical issues in psychiatric nursing
Ethical issues in psychiatric nursing American psychiatric association annual meeting 2020
American psychiatric association annual meeting 2020 Assessment skills
Assessment skills Psychiatric disorders
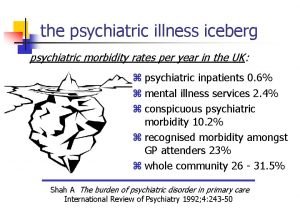
Psychiatric disorders Sleep disorders
Sleep disorders Psychiatric emergency
Psychiatric emergency Psychiatric security review board
Psychiatric security review board Northeast florida state hospital
Northeast florida state hospital Cmc psychiatric hospital
Cmc psychiatric hospital Ethical and legal issues in psychiatric nursing
Ethical and legal issues in psychiatric nursing Psychiatric emergency
Psychiatric emergency Psychiatric rehabilitation
Psychiatric rehabilitation Nursing care plan evaluation examples
Nursing care plan evaluation examples Liberty hill academy
Liberty hill academy Role of psychiatric nurse
Role of psychiatric nurse Calgary family assessment model
Calgary family assessment model American nurses association illinois
American nurses association illinois Mental health definition in nursing
Mental health definition in nursing History of psychiatric nursing
History of psychiatric nursing Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Southern psychiatric association
Southern psychiatric association Chapter 22 psychiatric emergencies
Chapter 22 psychiatric emergencies Vätsketryck formel
Vätsketryck formel Uppställning multiplikation
Uppställning multiplikation Rbk-mätning
Rbk-mätning Elektronik för barn
Elektronik för barn Särskild löneskatt för pensionskostnader
Särskild löneskatt för pensionskostnader Borra hål för knoppar
Borra hål för knoppar Tack för att ni har lyssnat
Tack för att ni har lyssnat Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Bris för vuxna
Bris för vuxna Trög för kemist
Trög för kemist Vad är ett minoritetsspråk
Vad är ett minoritetsspråk Indikation för kejsarsnitt på moderns önskan
Indikation för kejsarsnitt på moderns önskan Delegerande ledarskap
Delegerande ledarskap Toppslätskivling effekt
Toppslätskivling effekt Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Redogör för vad psykologi är
Redogör för vad psykologi är Skapa med geometriska former
Skapa med geometriska former Claes martinsson
Claes martinsson Bra mat för unga idrottare
Bra mat för unga idrottare Ledarskapsteorier
Ledarskapsteorier Publik sektor
Publik sektor Tidbok för yrkesförare
Tidbok för yrkesförare Datorkunskap för nybörjare
Datorkunskap för nybörjare Kvinnlig mantel i antikens rom
Kvinnlig mantel i antikens rom Fspos
Fspos Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Steg för steg rita
Steg för steg rita Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Jätte råtta
Jätte råtta Tillitsbaserad ledning
Tillitsbaserad ledning Bat mitza
Bat mitza Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Romarriket tidslinje
Romarriket tidslinje Klassens tjejtjusare rim
Klassens tjejtjusare rim Mästare lärling modell
Mästare lärling modell Shingelfrisyren
Shingelfrisyren Borstål, egenskaper
Borstål, egenskaper Shaktismen
Shaktismen Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Cellorov
Cellorov I gullregnens månad
I gullregnens månad A gastrica
A gastrica Stig kerman
Stig kerman Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning Novell typiska drag
Novell typiska drag Relativ standardavvikelse formel
Relativ standardavvikelse formel Ledningssystem för verksamhetsinformation
Ledningssystem för verksamhetsinformation Tack för att ni har lyssnat
Tack för att ni har lyssnat Treserva lathund
Treserva lathund Cks
Cks Läkarutlåtande för livränta
Läkarutlåtande för livränta Påbyggnader för flakfordon
Påbyggnader för flakfordon Tack för att ni lyssnade
Tack för att ni lyssnade Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Egg för emanuel
Egg för emanuel En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Tack för att ni har lyssnat
Tack för att ni har lyssnat Rutin för avvikelsehantering
Rutin för avvikelsehantering Var finns arvsanlagen
Var finns arvsanlagen Myndigheten för delaktighet
Myndigheten för delaktighet Presentera för publik crossboss
Presentera för publik crossboss Densitet vatten
Densitet vatten Att skriva en debattartikel
Att skriva en debattartikel Var 1721 för stormaktssverige
Var 1721 för stormaktssverige Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Mall för referat
Mall för referat Epiteltyper
Epiteltyper Verifikationsplan
Verifikationsplan Brant karttecken
Brant karttecken Gbmc medical records
Gbmc medical records Difference between medical report and medical certificate
Difference between medical report and medical certificate Torrance memorial outpatient lab
Torrance memorial outpatient lab California medical license application
California medical license application Cartersville medical center medical records
Cartersville medical center medical records Queer theory in literary criticism ppt
Queer theory in literary criticism ppt General pricing approaches
General pricing approaches English
English A ray of light approaches a jar of honey
A ray of light approaches a jar of honey Rules based approach to corporate governance
Rules based approach to corporate governance Direct or expository approach
Direct or expository approach Activity planning in software project management
Activity planning in software project management 7 branding approaches
7 branding approaches The structural approach
The structural approach A comparison of approaches to large-scale data analysis
A comparison of approaches to large-scale data analysis Applying critical approaches to literary analysis
Applying critical approaches to literary analysis Marketing research approaches to demand estimation
Marketing research approaches to demand estimation Basic approaches to leadership
Basic approaches to leadership Approaches to psychology
Approaches to psychology Three approaches to ethics
Three approaches to ethics Initial approach fix
Initial approach fix Cost approaches and techniques in suppler assessment
Cost approaches and techniques in suppler assessment Basic approaches to leadership
Basic approaches to leadership Discourse and register analysis approaches
Discourse and register analysis approaches Outline critical approaches to interpreting text
Outline critical approaches to interpreting text Approaches to literary criticism
Approaches to literary criticism Approaches of industrial relations
Approaches of industrial relations Three approaches to probability
Three approaches to probability Approaches meets masters
Approaches meets masters Synchronic and diachronic linguistics
Synchronic and diachronic linguistics Approaches to decision making
Approaches to decision making Approaches to develop physical factors
Approaches to develop physical factors Pedagogical approaches to teaching math
Pedagogical approaches to teaching math Critical approaches to poetry
Critical approaches to poetry Pricing considerations and approaches
Pricing considerations and approaches Brand-based comparative approaches
Brand-based comparative approaches External locus of control psychology definition
External locus of control psychology definition The two dominant agile approaches are
The two dominant agile approaches are Pendekatan kontemporer adalah
Pendekatan kontemporer adalah The pearl chapter 3
The pearl chapter 3 Message authentication code requirements
Message authentication code requirements Content based task based and participatory approaches
Content based task based and participatory approaches Approaches to measuring performance
Approaches to measuring performance Similarities and differences of wid/wad and gad
Similarities and differences of wid/wad and gad Dualistic development thesis
Dualistic development thesis Gdp forumla
Gdp forumla Species diversity
Species diversity Moralist approach examples
Moralist approach examples Distributed shared memory
Distributed shared memory What is expressive criticism
What is expressive criticism Learning approaches theory and practice
Learning approaches theory and practice Approaches to develop emotional factors
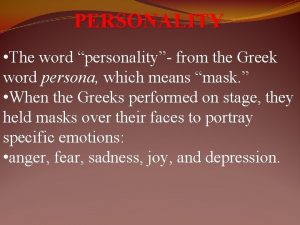
Approaches to develop emotional factors Greek word for personality
Greek word for personality The main approaches to forecasting exchange rates are
The main approaches to forecasting exchange rates are Individual approaches to stress management
Individual approaches to stress management Approaches to systems development
Approaches to systems development