The Heart Circulation Asst Prof Dr Ghaith Ali












![§ The [c] wave is synchronous with the pulse wave in carotid artery hence § The [c] wave is synchronous with the pulse wave in carotid artery hence](https://slidetodoc.com/presentation_image/c78e721071f7f59c21a03d21fdab3d4b/image-81.jpg)
![§ The [v] wave corresponds to the peak in the atrial pressure, which occurs § The [v] wave corresponds to the peak in the atrial pressure, which occurs](https://slidetodoc.com/presentation_image/c78e721071f7f59c21a03d21fdab3d4b/image-82.jpg)



- Slides: 117
The Heart & Circulation Asst. Prof. Dr. Ghaith Ali Jasim Al Zubaidy Ph. D Pharmacology MSc Physiology & Pharmacology dr. ghaithali@yahoo. com
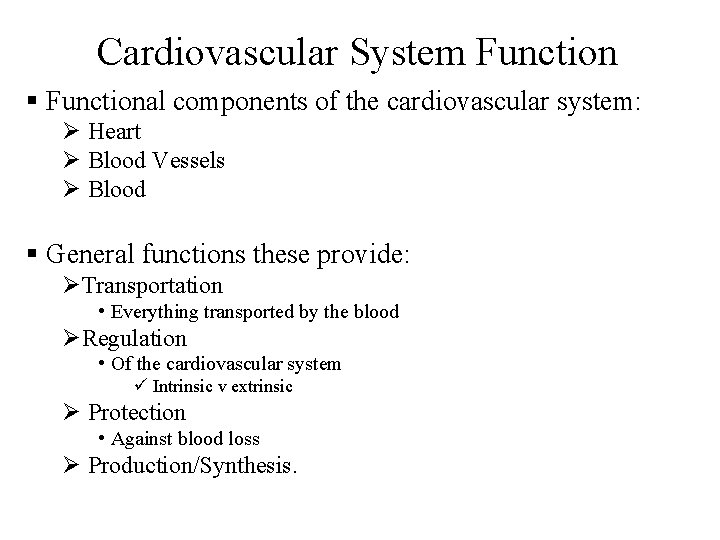
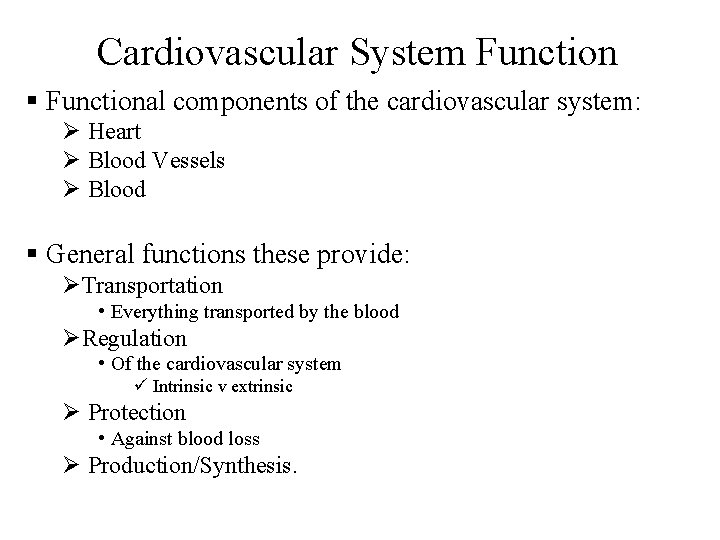
Cardiovascular System Function § Functional components of the cardiovascular system: Ø Heart Ø Blood Vessels Ø Blood § General functions these provide: ØTransportation • Everything transported by the blood ØRegulation • Of the cardiovascular system ü Intrinsic v extrinsic Ø Protection • Against blood loss Ø Production/Synthesis.
v To create the “pump” we have to examine the Functional Anatomy of: Ø Cardiac muscle Ø Chambers Ø Valves Ø Intrinsic Conduction System
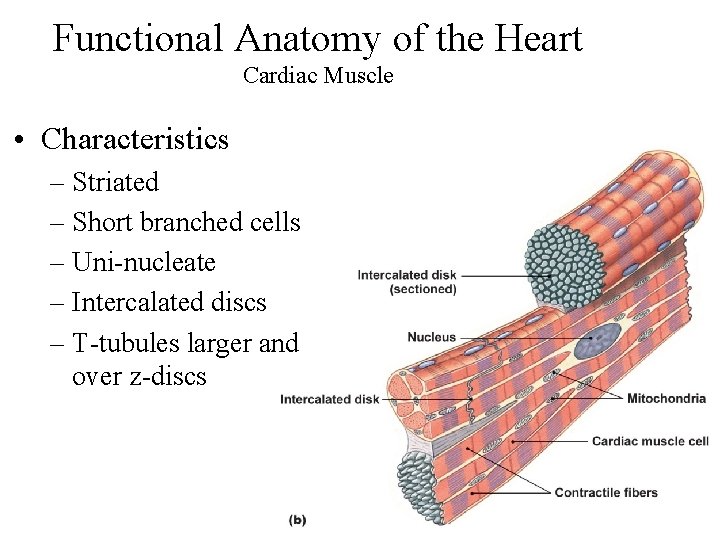
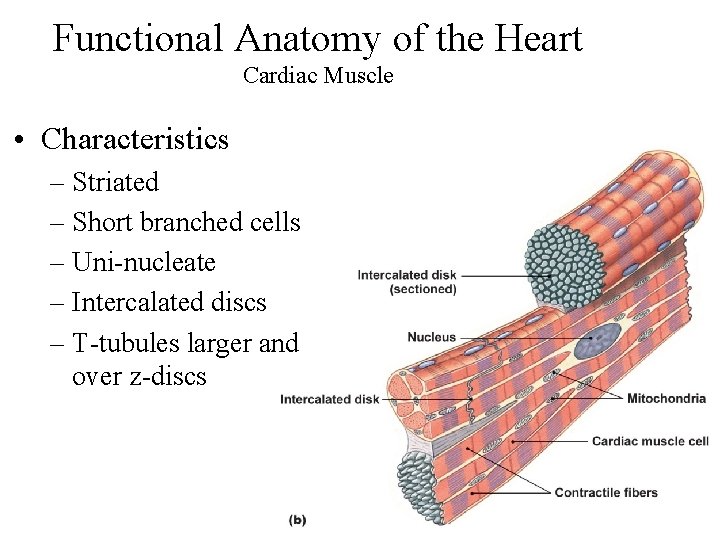
Functional Anatomy of the Heart Cardiac Muscle • Characteristics – Striated – Short branched cells – Uni nucleate – Intercalated discs – T tubules larger and over z discs
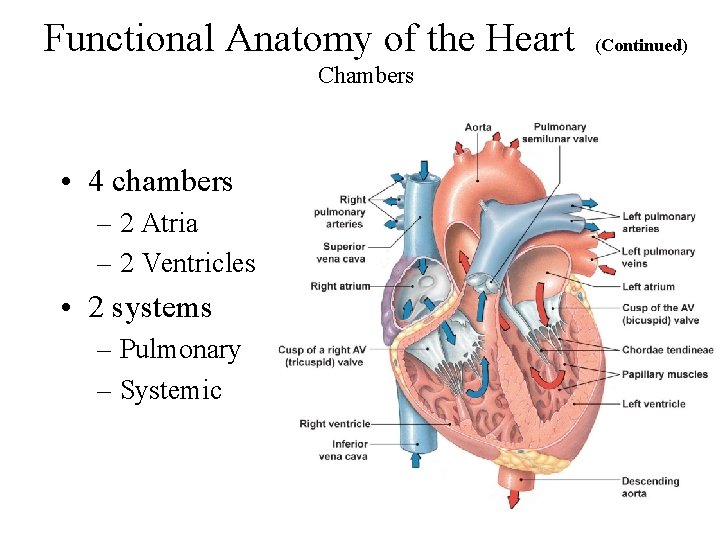
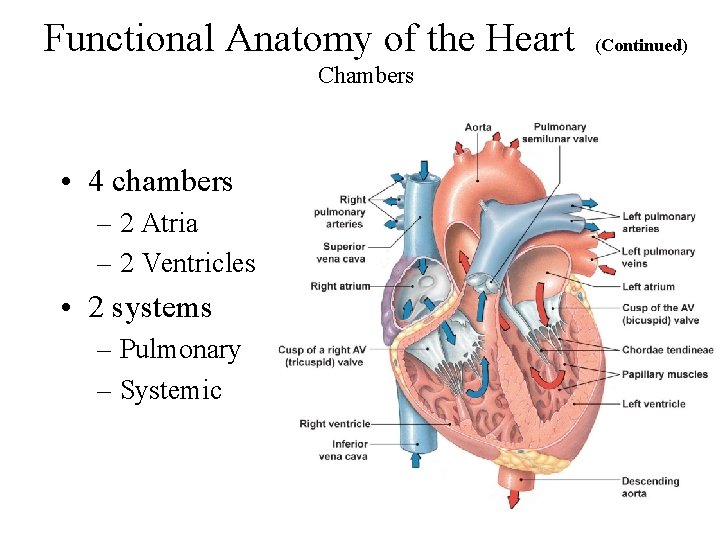
Functional Anatomy of the Heart Chambers • 4 chambers – 2 Atria – 2 Ventricles • 2 systems – Pulmonary – Systemic (Continued)
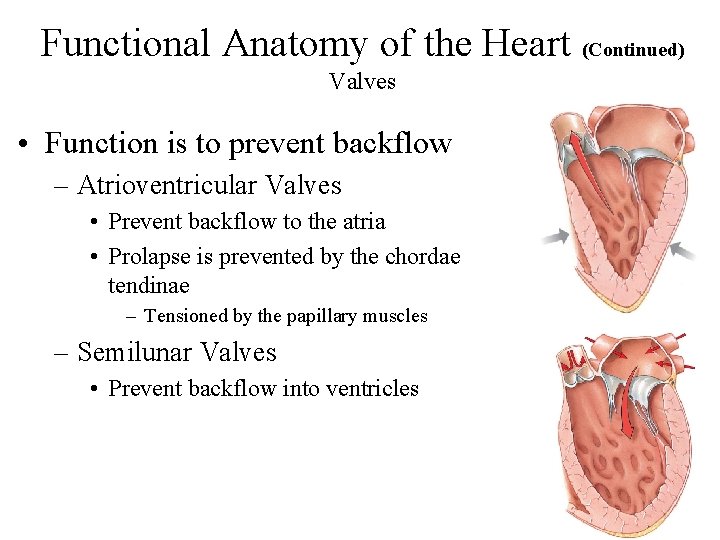
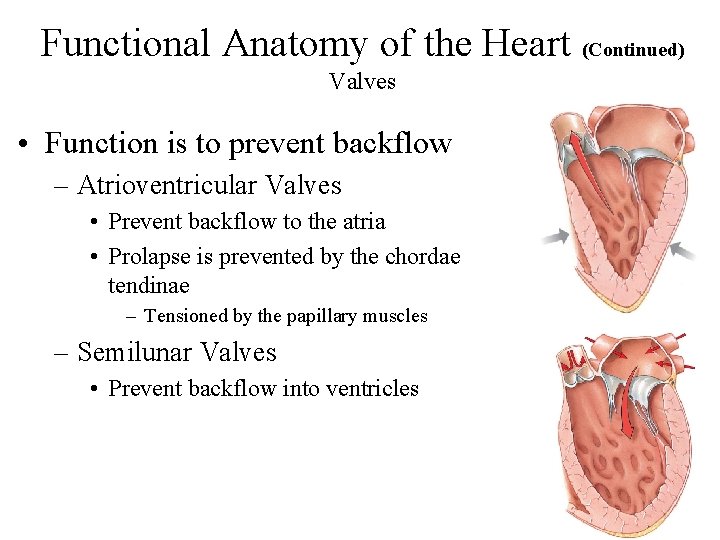
Functional Anatomy of the Heart (Continued) Valves • Function is to prevent backflow – Atrioventricular Valves • Prevent backflow to the atria • Prolapse is prevented by the chordae tendinae – Tensioned by the papillary muscles – Semilunar Valves • Prevent backflow into ventricles
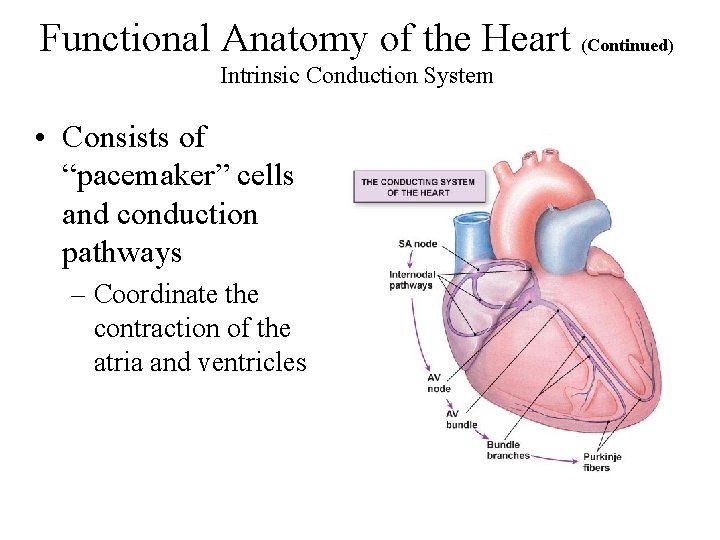
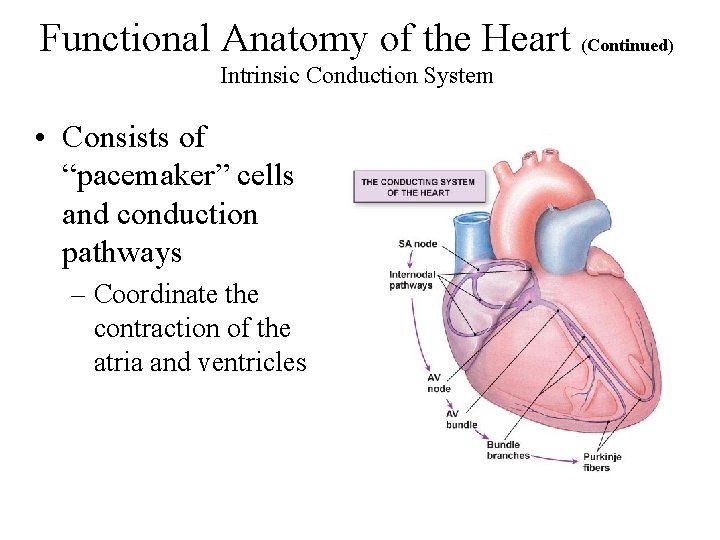
Functional Anatomy of the Heart (Continued) Intrinsic Conduction System • Consists of “pacemaker” cells and conduction pathways – Coordinate the contraction of the atria and ventricles
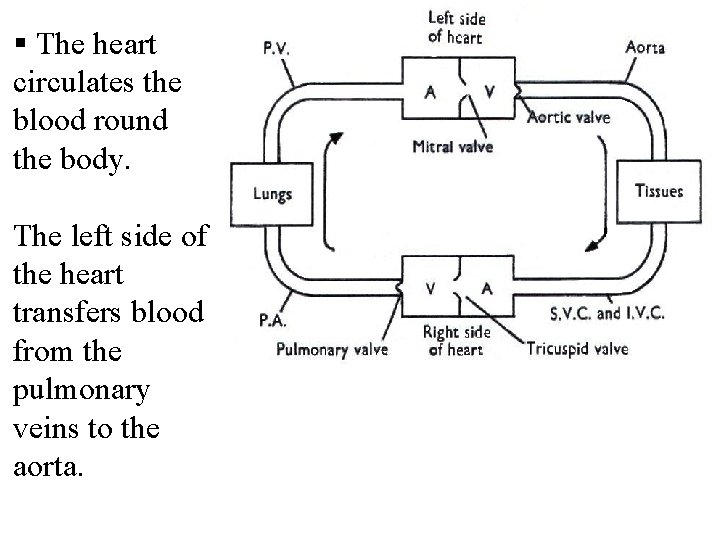
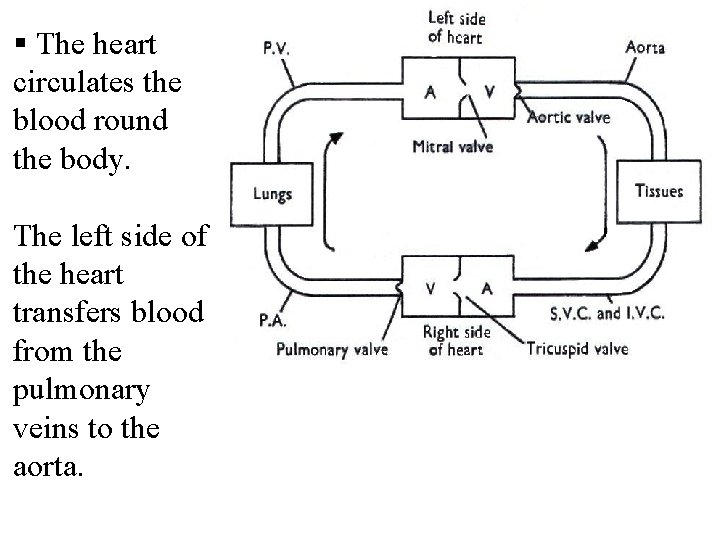
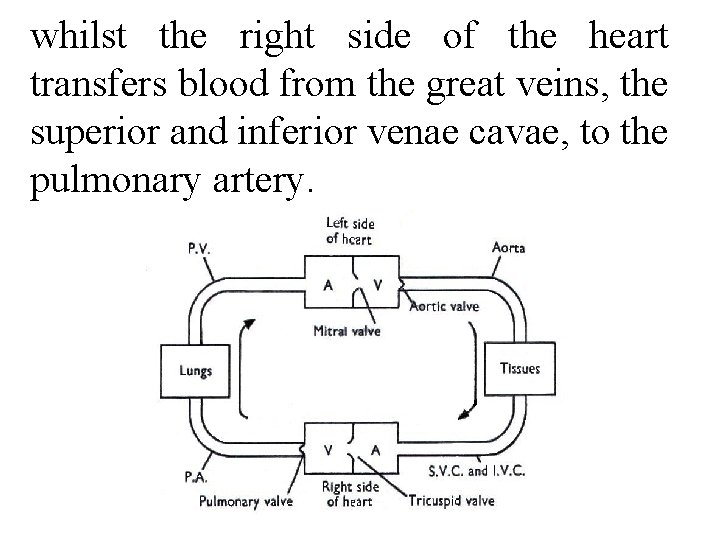
§ The heart circulates the blood round the body. The left side of the heart transfers blood from the pulmonary veins to the aorta.
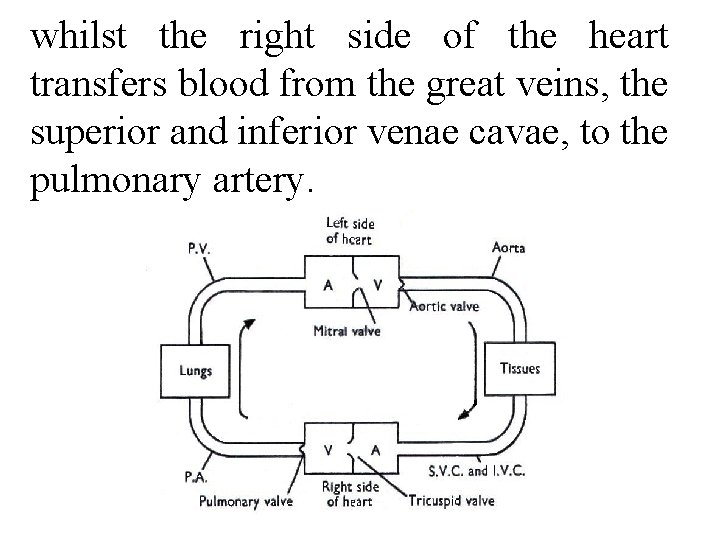
whilst the right side of the heart transfers blood from the great veins, the superior and inferior venae cavae, to the pulmonary artery.
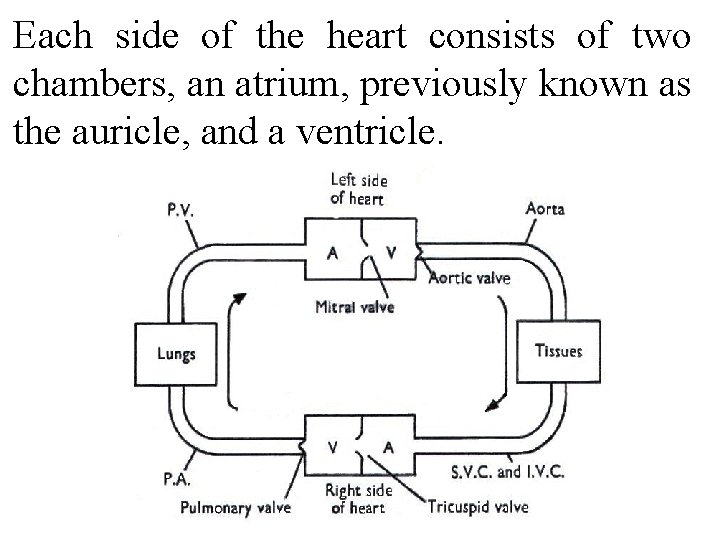
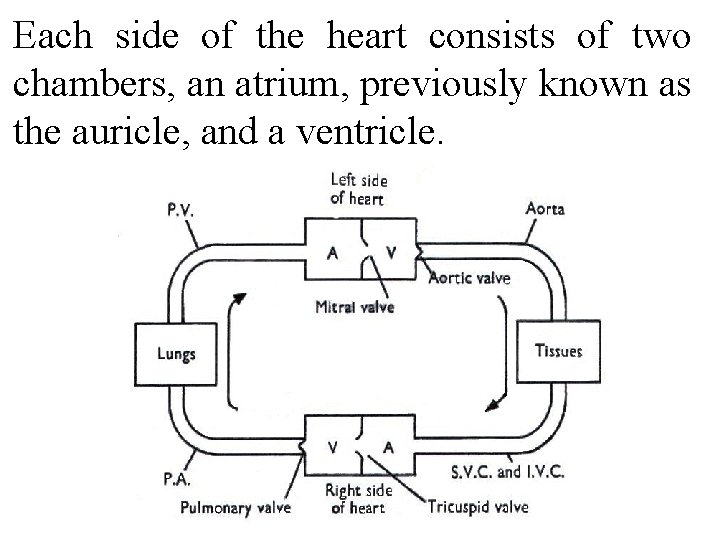
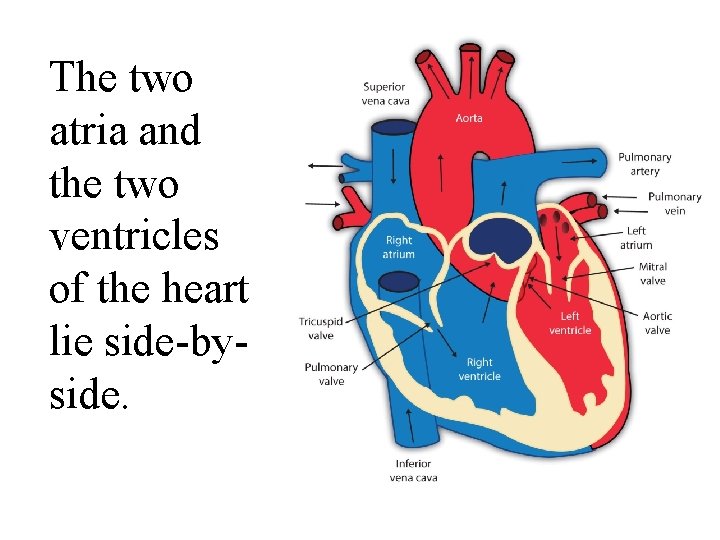
Each side of the heart consists of two chambers, an atrium, previously known as the auricle, and a ventricle.
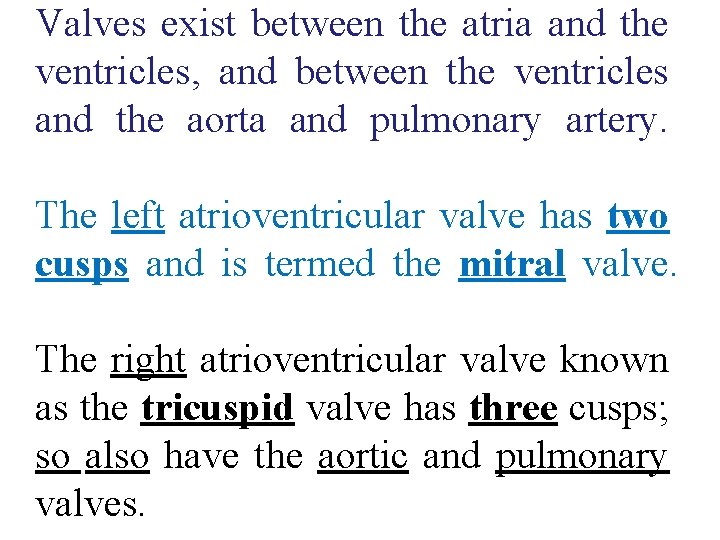
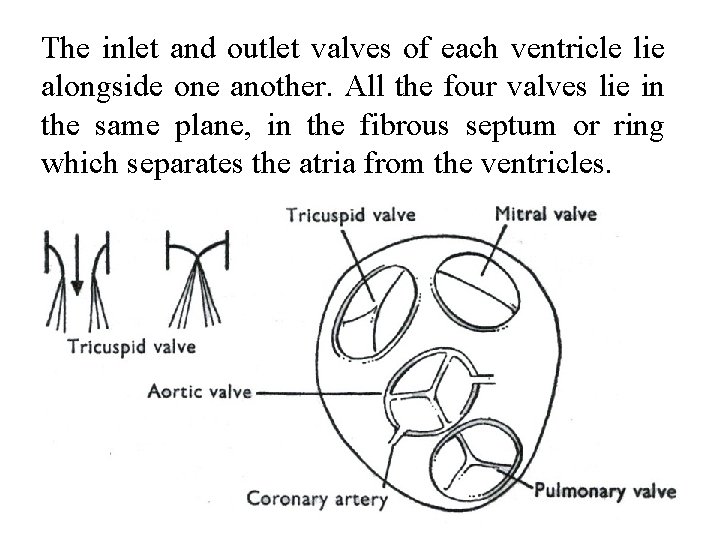
Valves exist between the atria and the ventricles, and between the ventricles and the aorta and pulmonary artery. The left atrioventricular valve has two cusps and is termed the mitral valve. The right atrioventricular valve known as the tricuspid valve has three cusps; so also have the aortic and pulmonary valves.

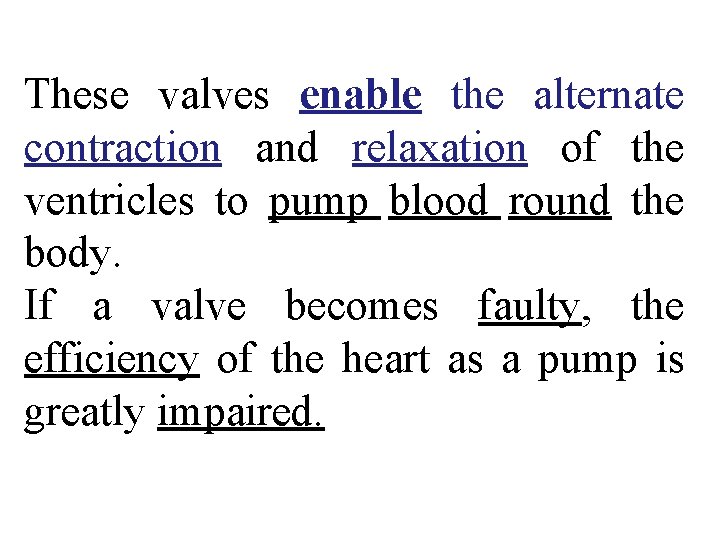
These valves enable the alternate contraction and relaxation of the ventricles to pump blood round the body. If a valve becomes faulty, the efficiency of the heart as a pump is greatly impaired.
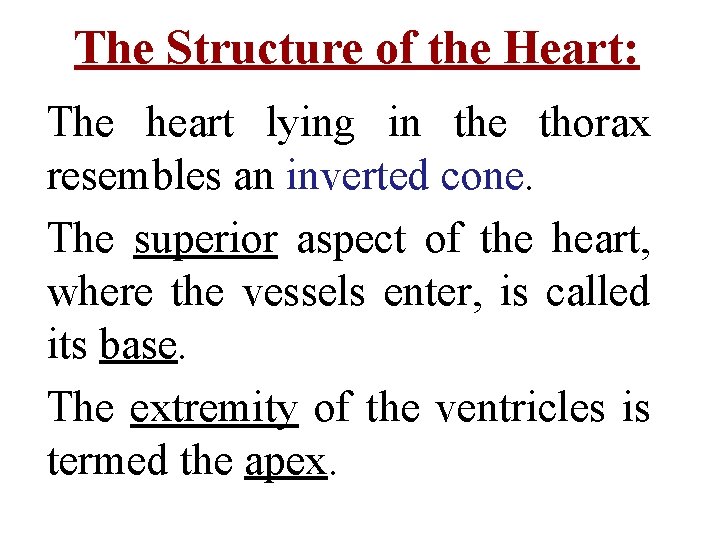
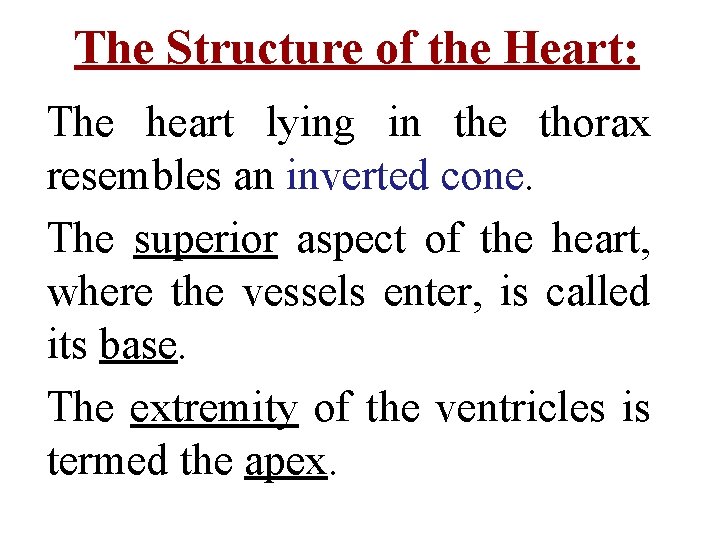
The Structure of the Heart: The heart lying in the thorax resembles an inverted cone. The superior aspect of the heart, where the vessels enter, is called its base. The extremity of the ventricles is termed the apex.
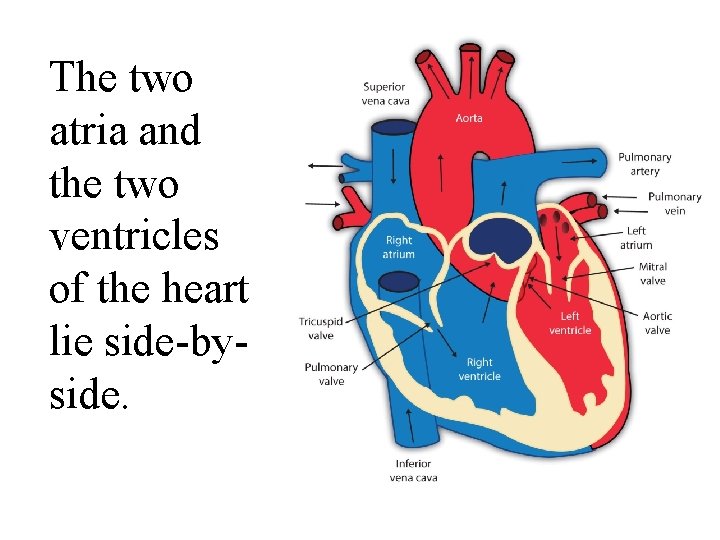
The two atria and the two ventricles of the heart lie side by side.
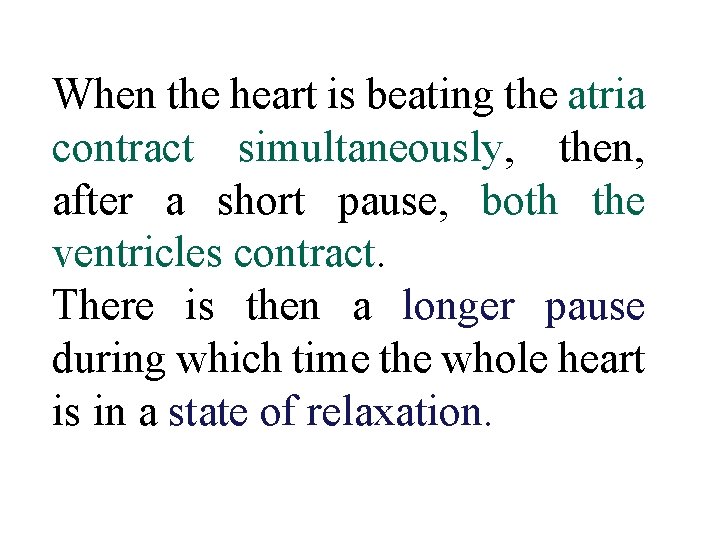
When the heart is beating the atria contract simultaneously, then, after a short pause, both the ventricles contract. There is then a longer pause during which time the whole heart is in a state of relaxation.
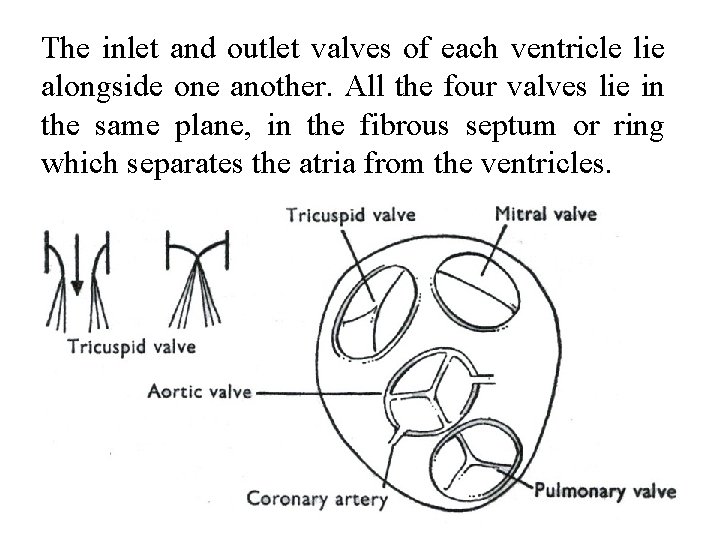
The inlet and outlet valves of each ventricle lie alongside one another. All the four valves lie in the same plane, in the fibrous septum or ring which separates the atria from the ventricles.
This property is developed to the greatest extent in a region known as the sino atrial node (S. A. node) which is situated in the wall of the right atrium near the entrance of the superior vena cava.
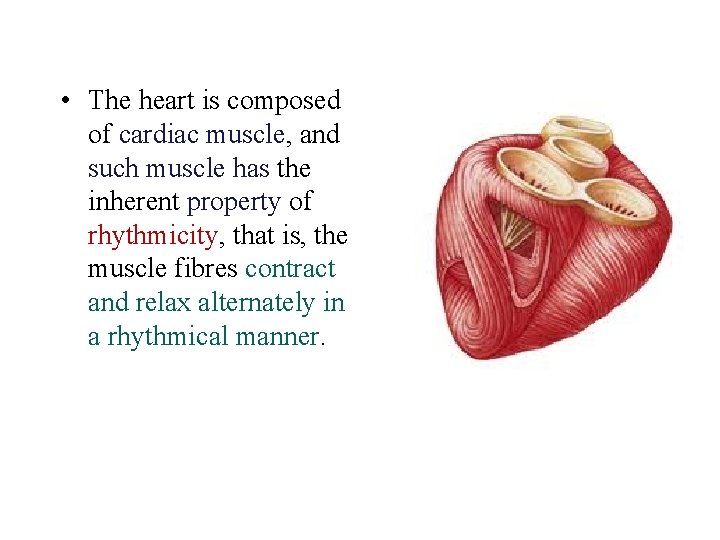
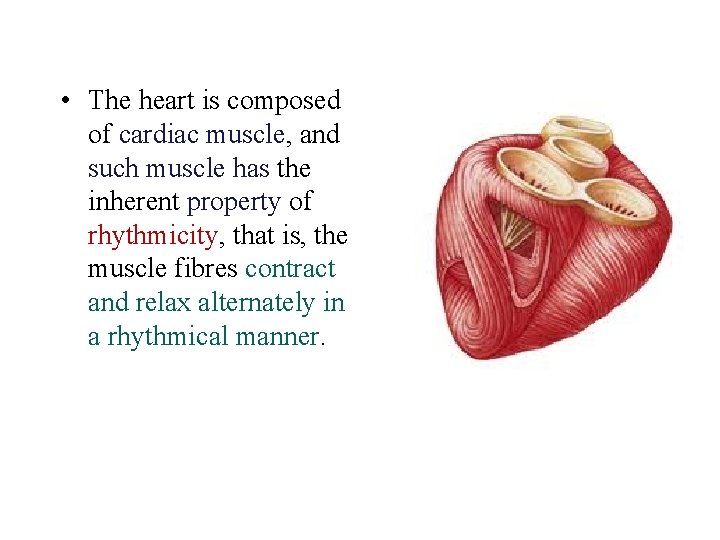
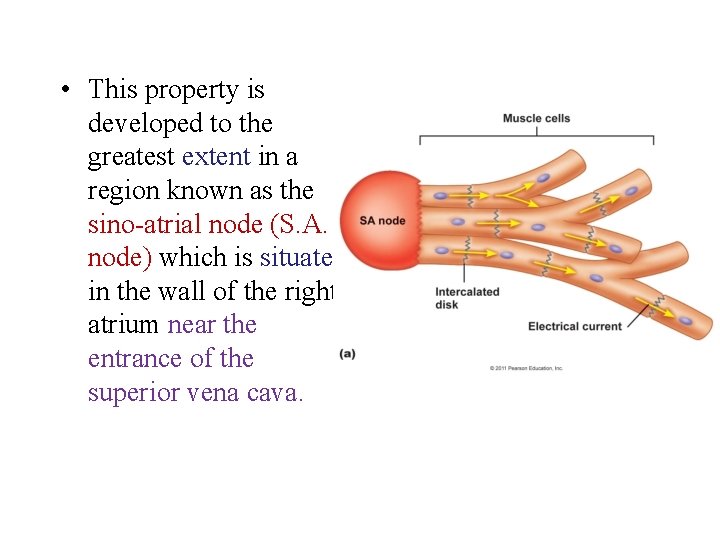
• The heart is composed of cardiac muscle, and such muscle has the inherent property of rhythmicity, that is, the muscle fibres contract and relax alternately in a rhythmical manner.
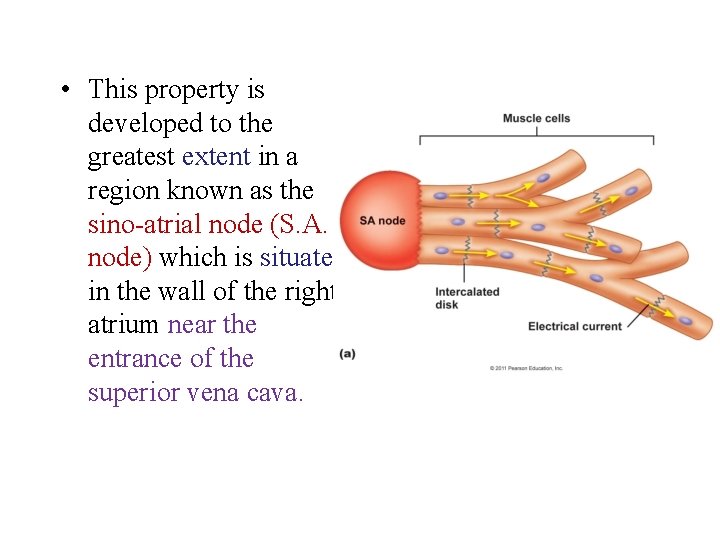
• This property is developed to the greatest extent in a region known as the sino atrial node (S. A. node) which is situated in the wall of the right atrium near the entrance of the superior vena cava.

The S. A node originates each heart beat. . . It is known as the pacemaker. Cardiac muscle cells, known as fibres, are cylindrical in shape with central nuclei and faint cross striations. The fibres branch to form a network or sheet of muscle in which it is difficult to see where one cell ends and another begins.

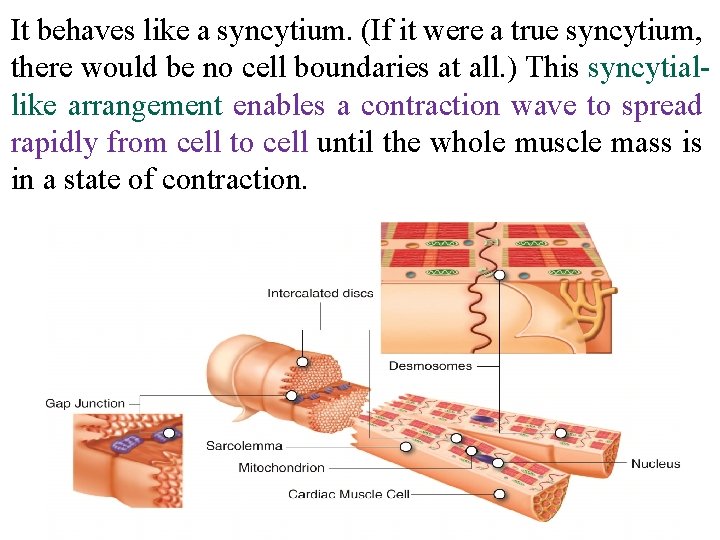
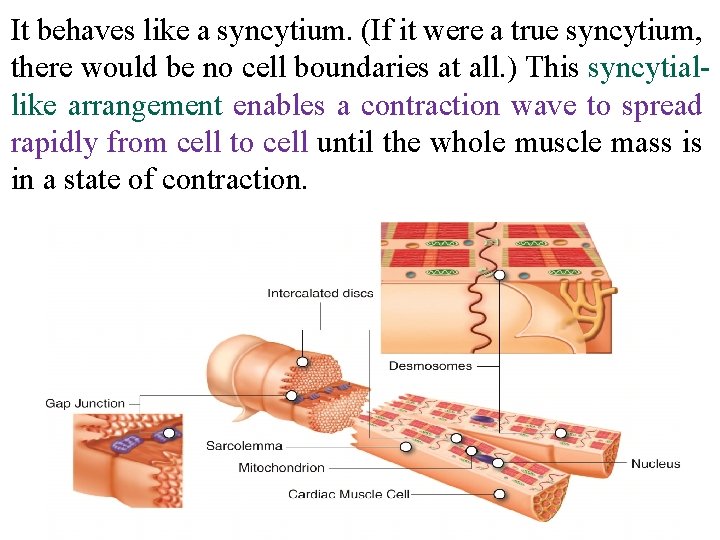
It behaves like a syncytium. (If it were a true syncytium, there would be no cell boundaries at all. ) This syncytial like arrangement enables a contraction wave to spread rapidly from cell to cell until the whole muscle mass is in a state of contraction.
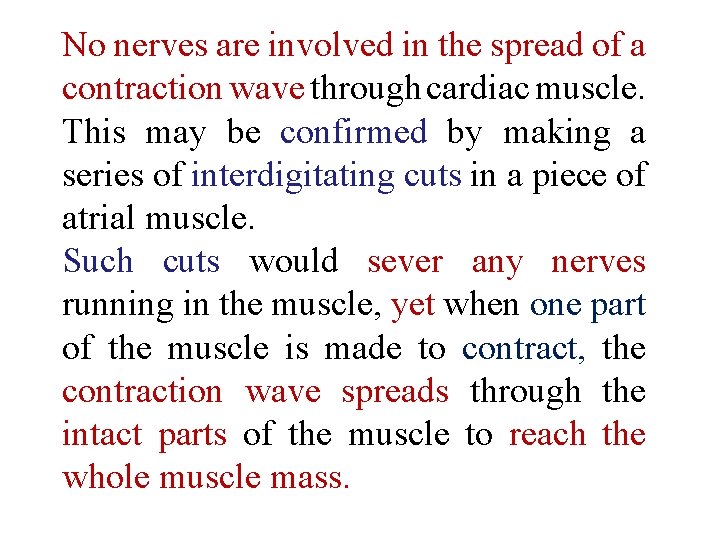
No nerves are involved in the spread of a contraction wave through cardiac muscle. This may be confirmed by making a series of interdigitating cuts in a piece of atrial muscle. Such cuts would sever any nerves running in the muscle, yet when one part of the muscle is made to contract, the contraction wave spreads through the intact parts of the muscle to reach the whole muscle mass.

Furthermore, in the embryo the heart beats before the nerves have developed. Although the two atria are separate chambers, the muscle fibres are arranged in rings round both atria.
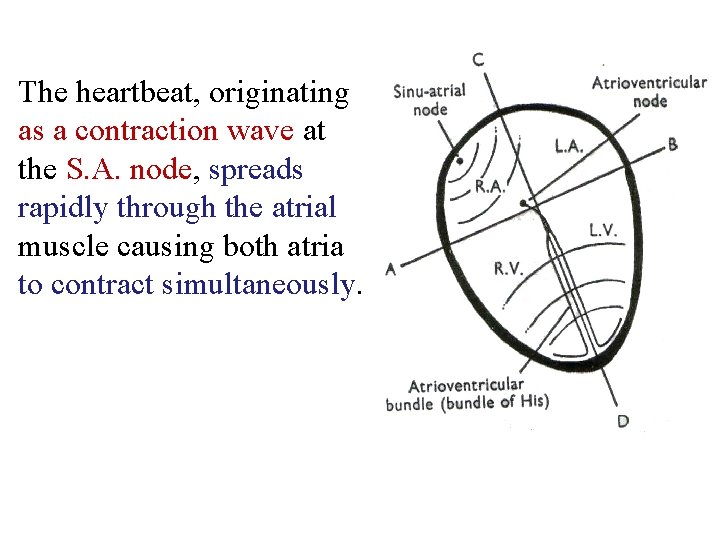
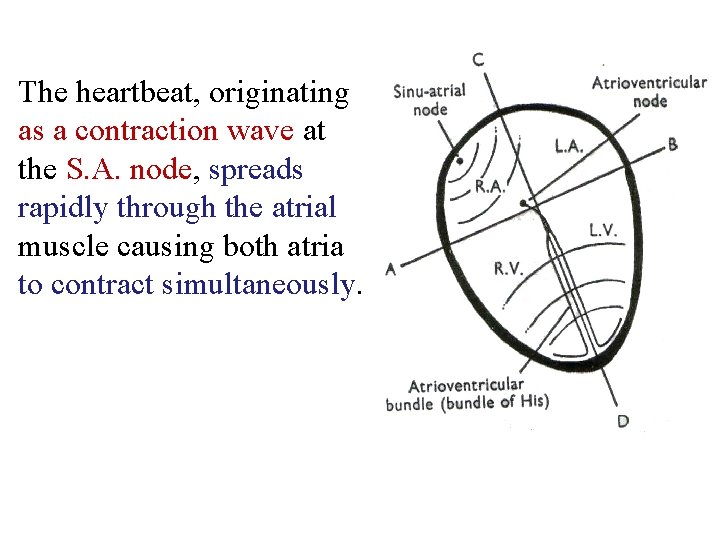
The heartbeat, originating as a contraction wave at the S. A. node, spreads rapidly through the atrial muscle causing both atria to contract simultaneously.
The blood in the atria is forced through the atrio ventricular valves into the ventricles. Rings of cardiac muscle around the entry of the superior and inferior venae cavae, and the pulmonary veins, close off the veins with a sphincter like action so that blood is not regurgitated back into the veins when the atria contract.
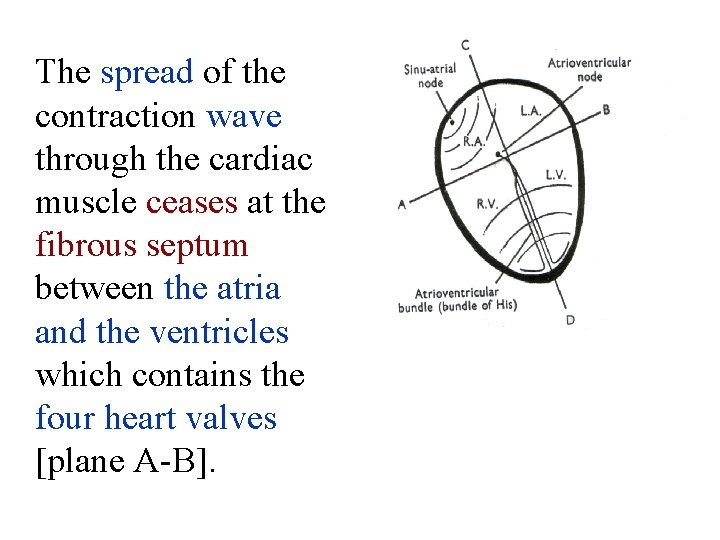
The spread of the contraction wave through the cardiac muscle ceases at the fibrous septum between the atria and the ventricles which contains the four heart valves [plane A B].
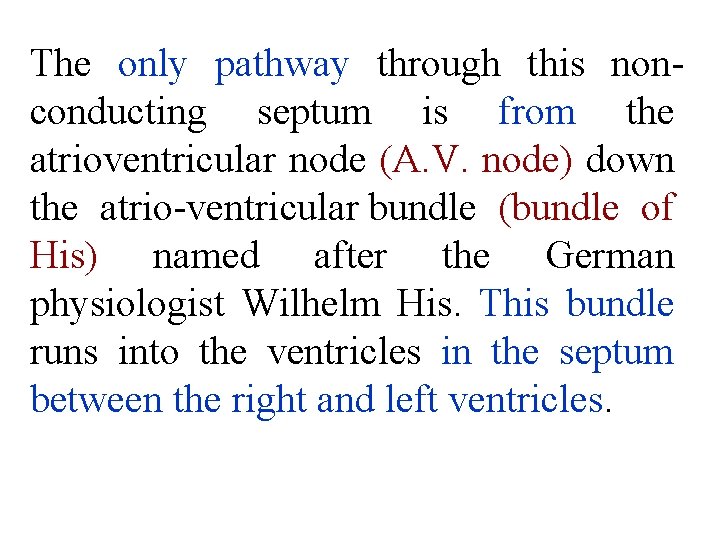
The only pathway through this non conducting septum is from the atrioventricular node (A. V. node) down the atrio ventricular bundle (bundle of His) named after the German physiologist Wilhelm His. This bundle runs into the ventricles in the septum between the right and left ventricles.

The passage of the contraction wave down this bundle of modified cardiac muscle is not visible from the surface of the heart, and there appears to be a slight pause following the atrial contraction, The contraction wave enters the ventricles near the apex and spreads upwards towards the base. The blood in the ventricles is forced upwards towards the base of the heart and out through the aortic and pulmonary valves.

Pericardium: The heart lies in a conical sac known as the pericardium. This consists of an inner serous pericardium and an outer fibrous pericardium. The inner serous pericardium is composed of two smooth layers, the visceral and parietal layers, one attached to the heart and the other to the fibrous sac. These two smooth layers allow the heart to beat in the mediastinum of the thorax with the minimum of friction.

The pericardium:

Thus when the ventricles contract, instead of the apex moving upwards towards the base, and particularly the atrio ventricular ring, descends towards the apex. This has the effect of increasing the size of the atria at the same time as blood is ejected from the ventricles.
Cardiac Cycle-The Heart as a Pump: The sequence of events may, therefore, be summarized as follows: The heart beat originates in the S. A. node, and shortly afterwards the atria contract. This is followed by a short pause whilst the contraction wave is moving down the bundle of His. Then the ventricles contract, the atrioventricular ring moves downwards and blood is ejected into the arteries. The ventricular muscle relaxes and the atrioventricular ring returns to its initial position. There is then a long pause, when all chambers are relaxed before the next beat occurs.
§ The ventricular contraction phase is termed systole (pro nounced sis'to. lee). It lasts for 0· 3 seconds. § The ventricular relaxation phase is termed diastole (pronounced dye. ess'to. lee) and this lasts for 0. 5 seconds. § The complete sequence of events, the cardiac cycle, lasts for 0. 8 seconds, so that there are: 60~70 cycles/minute. This is the heart rate. § The heart beats continuously for the whole of a person's life and its only period of rest is after each contraction, during diastole which becomes shorter.
The Heart Sounds § The valves in the heart close passively whenever there is a tendency for the blood to flow in the reverse direction. § Since blood flows from a region of high Pressure to a region of low pressure, it is the relative pressures in the atria, ventricles and arteries that will determine the opening and shutting of the valves.
Since the valves are passive structures and contain no contracting muscle, diseased valves may be replaced by mechanical valves (prosthetic valves) which have been specially designed with smooth surfaces to minimize the risk of blood clotting and red cell haemolysis.
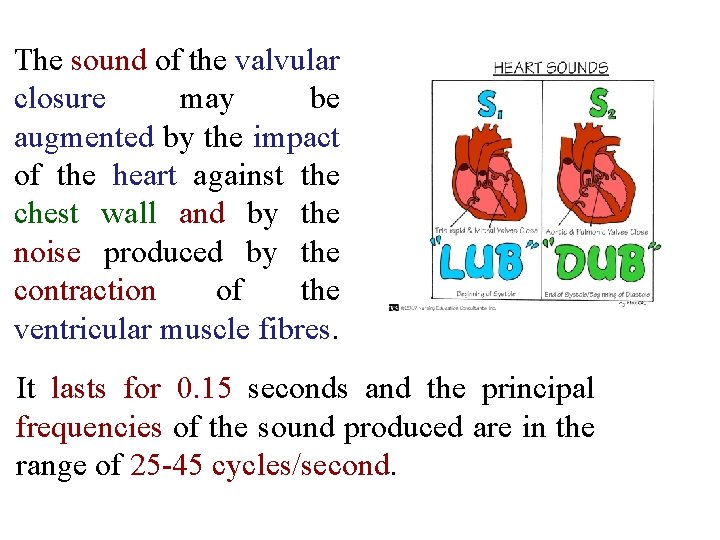
§ With the onset of ventricular systole, the pressure in the ventricles starts to rise. As soon as it exceeds that in the corresponding atrium, the A V valves will shut. This simultaneous closure of the mitral and tricuspid valves with the onset of systole can be heard by applying the ear to the chest wall of a subject (or by stethoscope). § The sound heard may be likened to the word 'lub' spoken very softly. It is termed the first heart sound
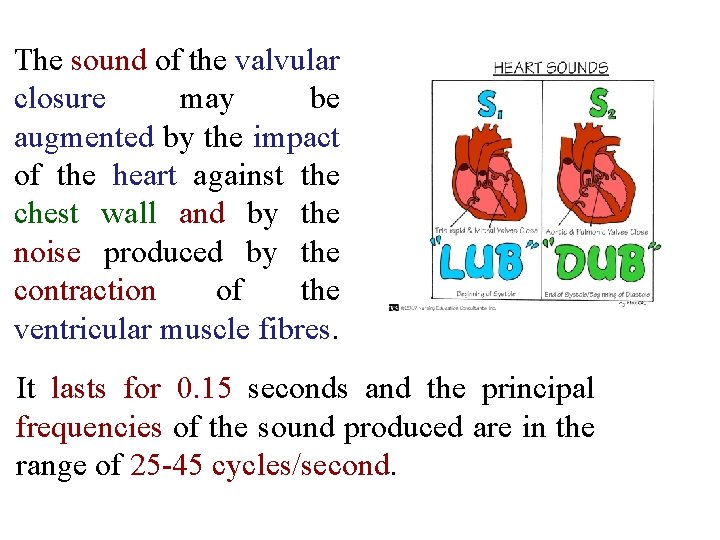
The sound of the valvular closure may be augmented by the impact of the heart against the chest wall and by the noise produced by the contraction of the ventricular muscle fibres. It lasts for 0. 15 seconds and the principal frequencies of the sound produced are in the range of 25 45 cycles/second.

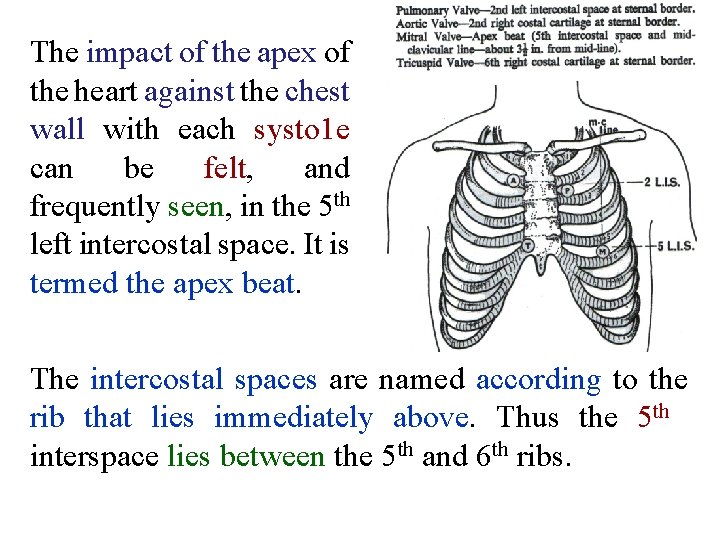
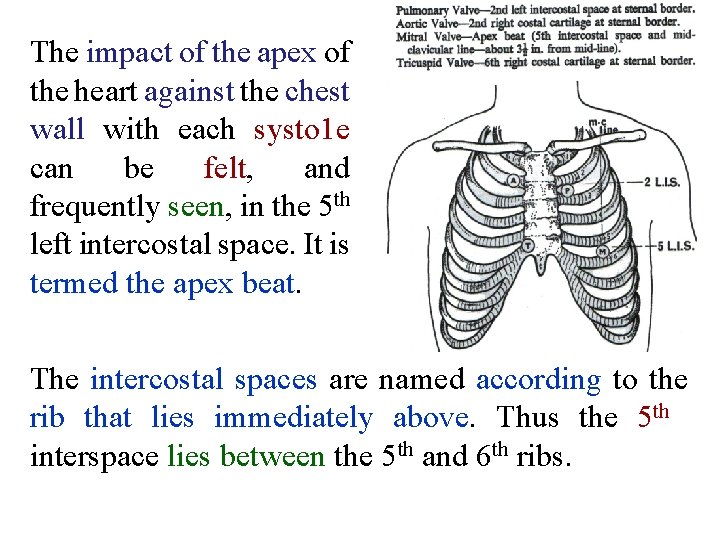
The impact of the apex of the heart against the chest wall with each systo 1 e can be felt, and frequently seen, in the 5 th left intercostal space. It is termed the apex beat. The intercostal spaces are named according to the rib that lies immediately above. Thus the 5 th interspace lies between the 5 th and 6 th ribs.

§The apex beat lies about 3 3. 5 in. from the midline. A line through the apex beat to the midline passes through the middle of the clavicle (mid clavicular line). §As soon as the ventricular pressures exceed those in the aorta and the pulmonary artery, the aortic and pulmonary valves will open.
§ The opening of the valves does not produce any detectable sound. (A clapping sound is produced when we bring our bands sharply together, but there is no sound when we take them apart again). § During the short interval of time, between the closure of the mitral valve and the opening of the aortic valve, the left ventricle is a closed chamber.
• At the same time the right ventricle will be closed off by the closure of the tricuspid and pulmonary valves. • Blood is incompressible and although the contraction of the ventricular muscle is increasing the pressure in the ventricles there is no actual change in volume during this phase. It is known as the isometric contraction phase.
§ As soon as the aortic and pulmonary valves open, the ventricles decrease in size as the blood is ejected into the aorta and pulmonary artery. § At the end of ventricular systole the pressure in the ventricles drops and the aortic and pulmonary valves close since the pressure in these vessels now exceeds that in the ventricles.
There is a short isometric relaxation phase during which time the ventricles are once again closed chambers, but as soon as the ventricu 1 ar pressure has fall to below that in the atria the mitral and tricuspid valves will open.
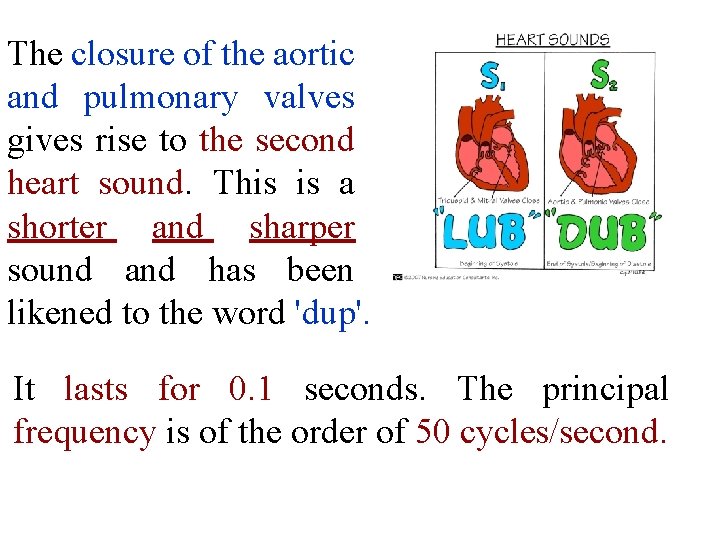
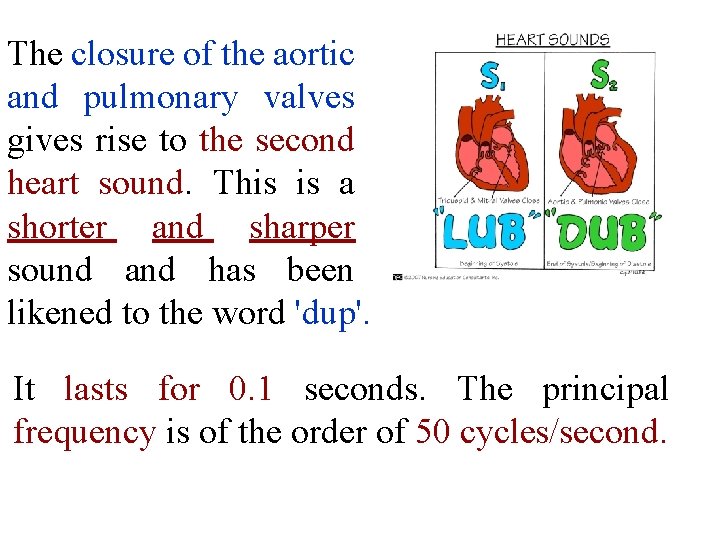
The closure of the aortic and pulmonary valves gives rise to the second heart sound. This is a shorter and sharper sound and has been likened to the word 'dup'. It lasts for 0. 1 seconds. The principal frequency is of the order of 50 cycles/second.
Since systole is shorter than diastole the rhythm when listening to the heart is: 'LUB' I 'DUP' II Pause 'LUB' 'DUP' I II Pause with a shorter interval between the first and next second heart sound than between the second and next first sound.
§ Under suitable conditions a 3 rd heart sound can be heard. This is caused by the blood rushing into the ventricles during diastole. § The third heart sound is probably due to vibrations of the mitral valve cusps since it is no longer heard in patients with prosthetic mitral valves.
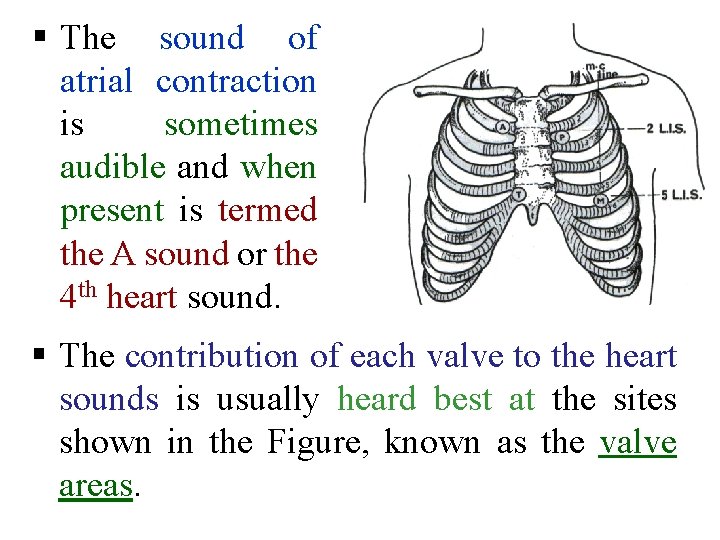
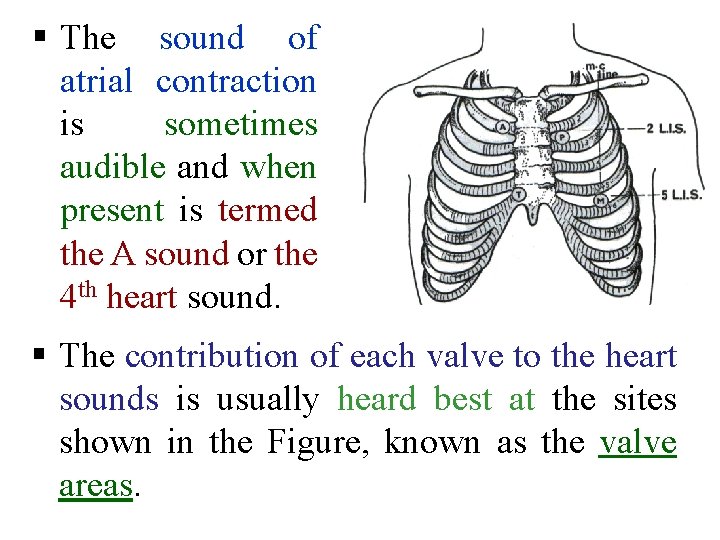
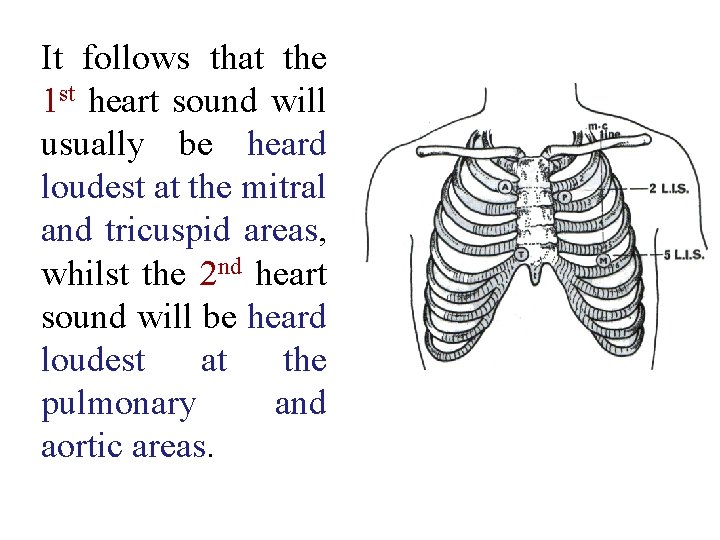
§ The sound of atrial contraction is sometimes audible and when present is termed the A sound or the 4 th heart sound. § The contribution of each valve to the heart sounds is usually heard best at the sites shown in the Figure, known as the valve areas.
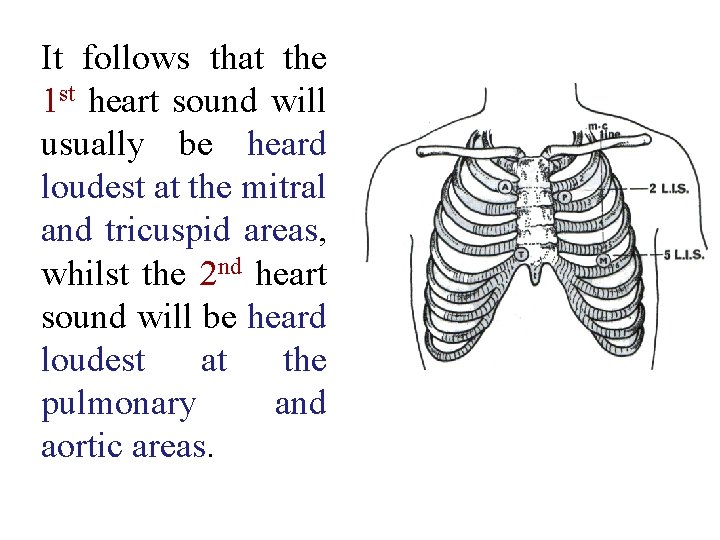
It follows that the 1 st heart sound will usually be heard loudest at the mitral and tricuspid areas, whilst the 2 nd heart sound will be heard loudest at the pulmonary and aortic areas.

Blood Flow Round the Circulation * With each systole 70 ml. of blood are ejected from each ventricle. * This quantity is termed the stroke volume. * The aorta and large arteries are elastic vessels and they accommodate this blood with a relatively small rise in pressure. During the ensuing diastole, there is no output from the heart, and the pressure in the arteries falls. The blood now in the arteries is pulsatile, and if an artery is cut, the blood shoots out in spurts.
* The blood flow to the tissues is maintained by the elastic recoil of the arterial walls, and by the time the capillaries have been reached, the flow has ceased to be pulsatile; the steady flow of blood through these vessels shows no variation in systole or diastole.
§ The blood returns to the heart along the veins, and the venous flow is a steady one. If a vein is cut the blood oozes out from the distal end without any pulsation. § On approaching the heart, the flow again becomes pulsatile as the ventricles are unable to receive the venous blood during systole
Function of the Atria: *The blood returning to the heart during ventricular diastole passes through the atria and enters the ventricles. *The blood returning during systole is unable to do this as the A V valves are closed. *The atria act as a storage reservoir for this blood until the end of systole when the A V valves open. With the opening of these valves the ventricles fill rapidly with the waiting blood.
*Further filling occurs as blood returns during diastole. One-tenth of a second before the onset of systole, when the ventricles are already 70% full of blood, the atria contract and complete the filling of the ventricles by adding the remaining 30%. *Atrial contraction is not essential for life, but the heart is a much more efficient pump when the atria are contracting. *The flow of blood through the lungs and tissues is continued but the flow is intermittent through the heart.
Pressure Changes In The Heart: § Although the pressures could be expressed in dyne/cm. 2 or lb. per in. 2, it is usual to express blood pressure in terms of the height of a corresponding column of mercury measured in millimeters. The units are mm. Hg. § These pressures are measured with reference to the atmospheric pressure.
§ The pressure in the intra thoracic part of the circulation may be less than the atmospheric pressure. This is due to the elastic recoil of the lungs. § The pressure in the atria, for example, may be 755 mm. Hg (absolute) whilst the outside barometric pressure is 760 mm. Hg. Such a pressure is denoted as 5 mm. Hg meaning 5 mm. Hg less than atmospheric. Such a pressure is referred to as a negative pressure.
§The atria are thin walled vessels and the pressure of blood in them is never very far from the pressure outside in the surrounding mediastinum. § This pressure is slightly negative ( 2 mm. Hg) and it becomes more negative when breathing in ( 8 mm. Hg).
v Respiratory variations in atrial pressure are seen in records of atrial pressure which are obtained with the chest closed by passing a catheter along the veins into the heart and into the right atrium. They disappear when the chest is opened as, for example, in thoracic surgery.
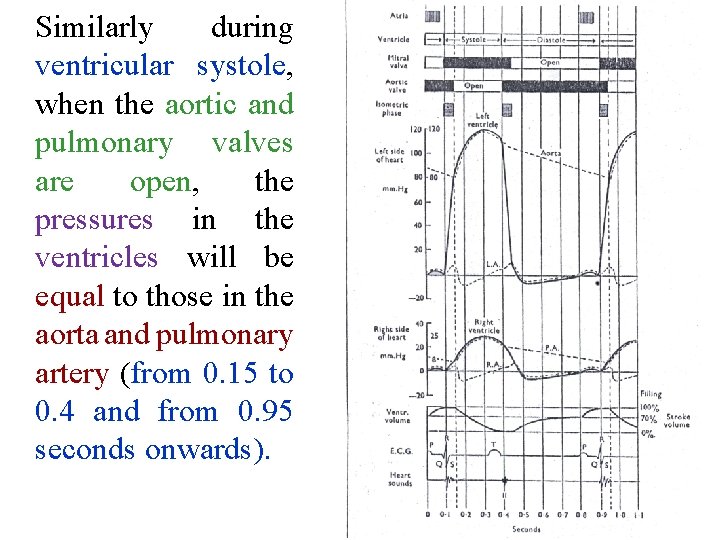
v. When the A V valves (mitral and tricuspid) are open during diastole (up to 0. 1 and from 0. 45 to 0. 9 seconds), the atrial pressure is very slightly greater than the ventricular pressure, otherwise the blood would not enter the ventricles. But to all intents and purposes the atrial and ventricular pressures are identical during this phase.
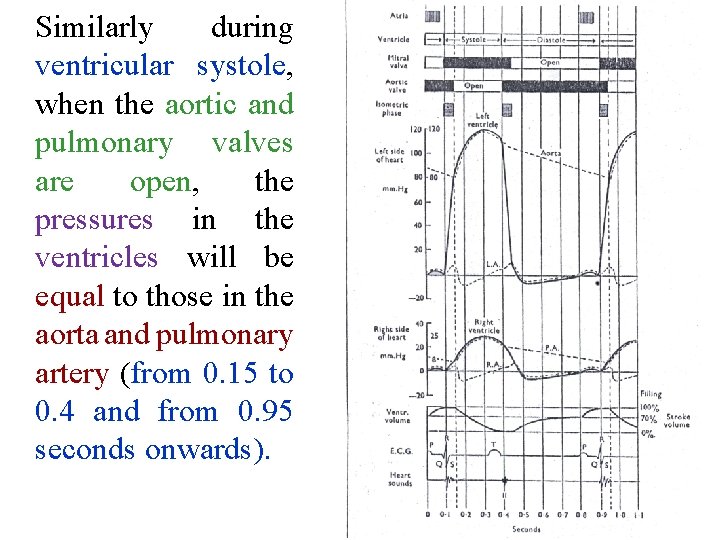
Similarly during ventricular systole, when the aortic and pulmonary valves are open, the pressures in the ventricles will be equal to those in the aorta and pulmonary artery (from 0. 15 to 0. 4 and from 0. 95 seconds onwards).
Ventricular Pressure Changes: § The left ventricle develops a maximum pressure of 120 mm. Hg during systole and therefore the aortic pressure reaches the same peak value. § During diastole the ventricular pressure falls to that in the thorax which is approximately 0 mm. Hg (atmospheric pressure). The ventricular changes are thus 120/0 mm. Hg.
§ The pressure in the aorta, however, is maintained by the elastic recoil of the arterial walls. Due to this elastic recoil the pressure in the aorta has only fallen to 80 mm. Hg by the time the next systole occurs. § Thus the pressure in the aorta fluctuates between 120 mm. Hg and 80 mm. Hg. These changes are denoted as 120/80 mm. Hg.
§ The right ventricle pumps out exactly the same quantity of blood as the left ventricle but at a much lower pressure. § The right ventricle develops a maximum pressure of 25 mm. Hg. The pressure falls to 0 mm. Hg in diastole and the right ventricle pressure changes are 25/0 mm. Hg. § The pressure in the pulmonary artery falls to 8 mm. Hg during diastole and the pressure changes in this vessel are, therefore 25/8 mm. Hg.
Atrial Pressure Changes § The atrial pressure tracing follows a complex pattern due to the interplay of several factors. § Atrial contraction (atrial systole) is associated with a pressure rise in the atria. It lasts for only 0. 1 seconds (time 0 to o. 1 and 0. 8 to 0. 9 seconds). § For the reminder of the cardiac cycle the atrial muscle is in u state or relaxation (atrial diastole).
§ The isometric contraction of the ventricles causes the mitral and tricuspid valves to bulge into the atria causing a further increase in atrial pressure (time 0. 1 to 0. 15 and 0. 9 to 0. 95 seconds). § However, as soon as the aortic and pulmonary valves open, the ventricular volumes decrease rapidly.
§ The A V ring descends increasing the volume of the atria. The atrial pressure falls sharply. § Blood returning to the heart cannot now enter the ventricles and the pressure in the atria builds up (time 0. 2 to 0. 45 seconds).
§ With the relaxation of the ventricles the atrioventricular ring moves upwards towards the base of the heart decreasing the volume of the atria and causing the atrial pressure to rise further (just before 0. 45 seconds).
§ With the opening of the mitral and tricuspid valves at time 0. 45 seconds the pressures in the atria and ventricles fall. § Blood returning to the heart enters the atria and ventricles and their pressures build up together till time 0. 8 seconds is reached when another atrial contraction occurs.

Venous Pressure Changes: § The veins near the heart show similar pressure waves to those in the right atrium. § Since the veins and atria are in communication at all times except during the brief atrial systole, the atrial pressure changes will be transmitted back to the veins.
§ There are three maxima in each cardiac cycle lettered a, c and v. § The [a] wave is caused by atrial systole. The sphincter like action of the atrial muscle round the entry of the veins prevents this being due simply to a transmission of atrial systole to the veins. § The pressure builds up because the veins are unable to empty their blood into the atria.
![The c wave is synchronous with the pulse wave in carotid artery hence § The [c] wave is synchronous with the pulse wave in carotid artery hence](https://slidetodoc.com/presentation_image/c78e721071f7f59c21a03d21fdab3d4b/image-81.jpg)
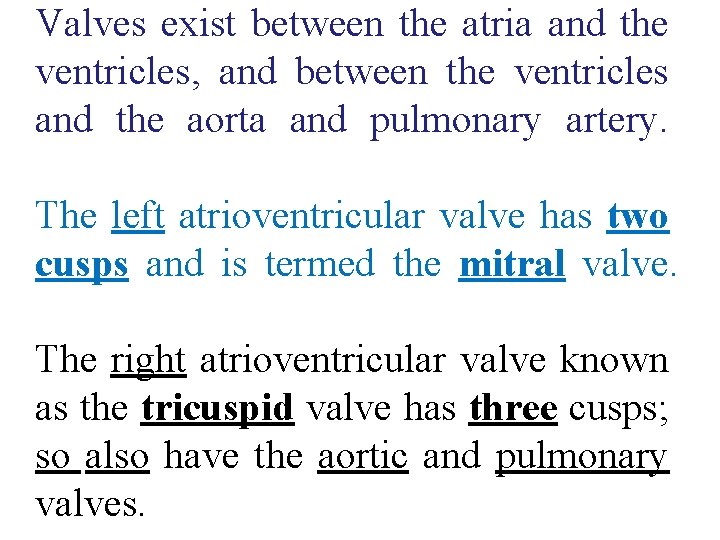
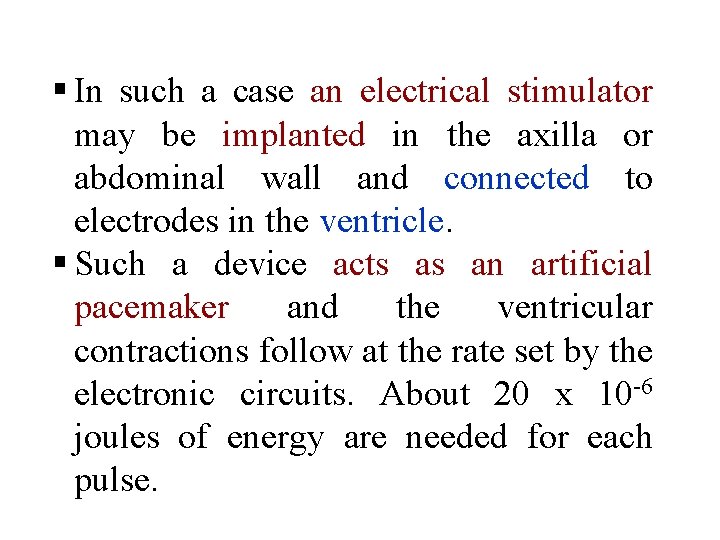
§ The [c] wave is synchronous with the pulse wave in carotid artery hence the letter c. § It corresponds to the atrial pressure peaks occurring at 0. 15 and 0. 95 seconds and is duo to the bulging of the A V valves during the isometric contraction phase.
![The v wave corresponds to the peak in the atrial pressure which occurs § The [v] wave corresponds to the peak in the atrial pressure, which occurs](https://slidetodoc.com/presentation_image/c78e721071f7f59c21a03d21fdab3d4b/image-82.jpg)
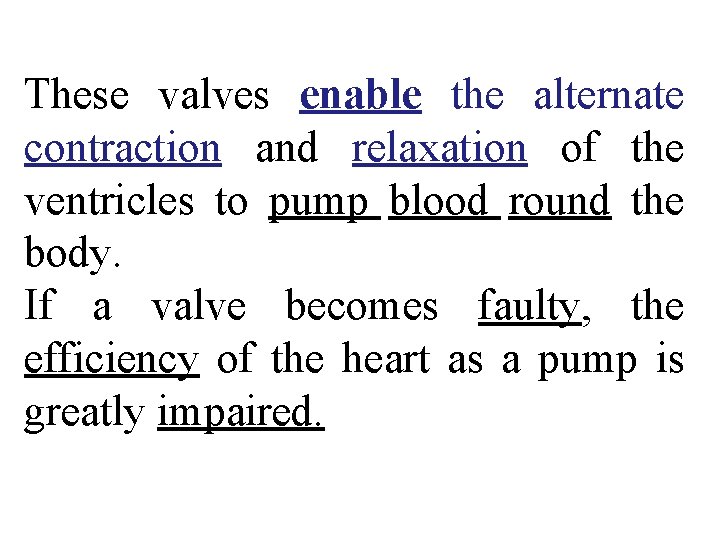
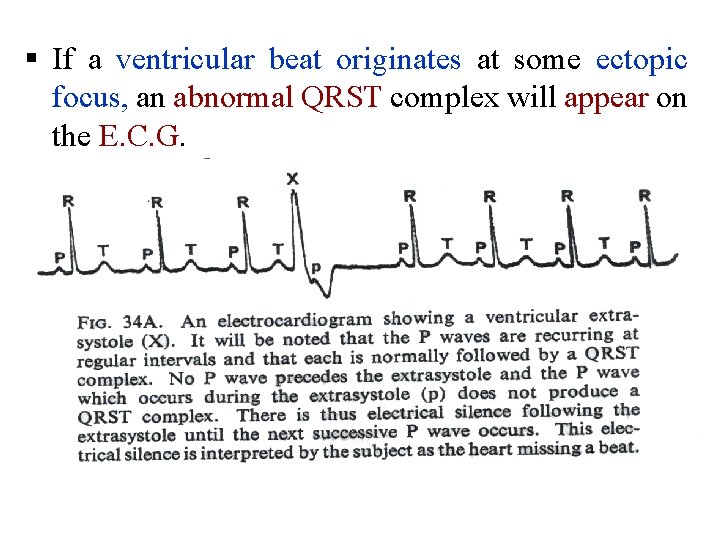
§ The [v] wave corresponds to the peak in the atrial pressure, which occurs just before 0. 45 seconds and is due to the filling of the atria whilst the A V valves are shut and the upward movement of the A V ring at the end of ventricular systole. § These pressure changes in the veins produce the venous pulse which is visible in the neck veins when the subject is lying down.
§All veins above the sternal angle are usually collapsed because their pressure is sub atmospheric. § No pulsations are therefore visible in the neck veins in the upright posture unless venous congestion is present.
§ The venous pulsations are seen best in the right external jugular vein which is in direct continuity with the superior vena cava and the right atrium. § The venous pressure changes are too small to be palpable.
Ventricular Volume Changes § The ventricular volume is constant during both the isometric contraction phase and the isometric relaxation phase. § Thus with the onset of systole, for the first 0. 05 second there is reduction in volume.

§ As soon as the aortic valve has opened the ventricular volume decreases as blood is ejected into the aorta. The ejection is rapid at first. Late in systole the ejection rate is reduced. § For the first 0. 05 second of diastole there is again no ventricular volume change as the ventricular muscle fibers relax isometrically.
§ As soon as the mitral valve opens the blood rushes into the ventricle, the ventricular volume increases rapidly at first and later more slowly. § By the time 0. 4 of the 0. 5 second of diastole has elapsed the filling has been such that the ventricular volume has increased by 50 m 1= 70% of the next stroke volume. § Atrial contraction in the last 0. 1 second of ventricular diastole completes the filling by the addition of a further 20 ml.
Murmurs § Murmurs are sounds heard during the cardiac cycle in addition to the normal heart sounds. § Those occurring during systole are known as systolic murmurs. Those occurring during diastole are termed diastolic murmurs. § They are caused by turbulence in the blood as it flows through the valve.
§ Valvular disease may prevent adequate closure of the valves, so that blood regurgitates back through the partially closed valves. § This will occur during systole in a case of mitral or tricuspid incompetence, giving rise to a systolic murmur. It will occur during diastole if the aortic or pulmonary valve is faulty giving a diastolic murmur.
§ Murmurs are also caused by a narrowing of the valve orifice which is known as a stenosis. The murmur will occur during the rapid passage of blood through the valve. § Thus, mitral and tricuspid stenosis will give rise to a diastolic murmur which will reach a maximum during late diastole when atrial contraction forces blood through the valve into the ventricle. § Aortic and pulmonary stenosis will give rise to a systolic murmur.
§ If the turbulence produces vibrations of the chest wall with low frequency components, the vibrations can be felt when the flat of the hand (or the ulnar border of the hand) is applied to the chest wall. Such a palpable murmur is termed a thrill. § In general, low frequencies can be felt rather than heard, whilst high frequencies can be heard rather than felt.
Heart Block § The duration of the P Q, or as it is often called the P R, interval is a measure of the conduction time in the bundle. It is normally (0. 15 0. 2) seconds. § Any longer time denotes delay in the transmission along the bundle and maybe the forerunner of complete failure of conduction along the bundle known as heart block.
§ Complete heart block occurs when the ventricles will be cut off from the pacemaker and will stop beating. § However, they may restart at a slow independent rate due to the inherent rhythmicity of the ventricular muscle. § The rate (about 30 beats/minute) is often too slow for an efficient circulation.
§ In all probability the S. A. node and atria will continue at their original rate of 70 beats/minute. § Atrial contractions will cease to be effective in aiding the circulation as many will occur whilst the A V valves are shut. § The ECG will show numerous P waves but few abnormal QRS complexes and there will be no time correlation between them.
§ In such a case an electrical stimulator may be implanted in the axilla or abdominal wall and connected to electrodes in the ventricle. § Such a device acts as an artificial pacemaker and the ventricular contractions follow at the rate set by the electronic circuits. About 20 x 10 6 joules of energy are needed for each pulse.
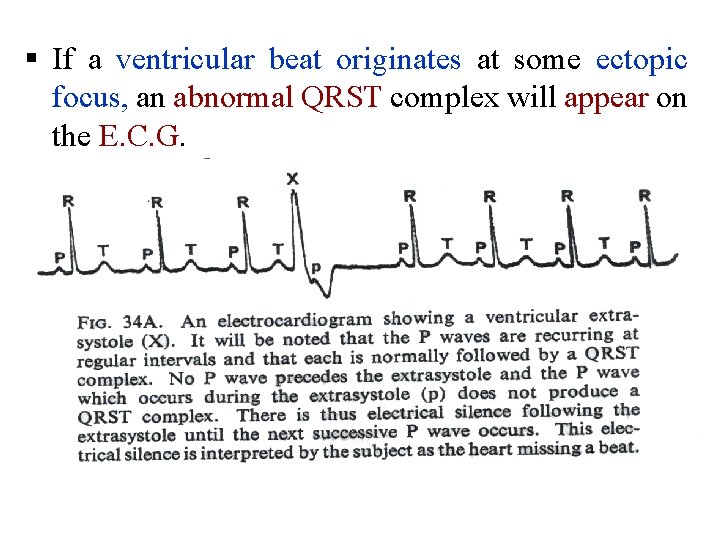
§ If a ventricular beat originates at some ectopic focus, an abnormal QRST complex will appear on the E. C. G.
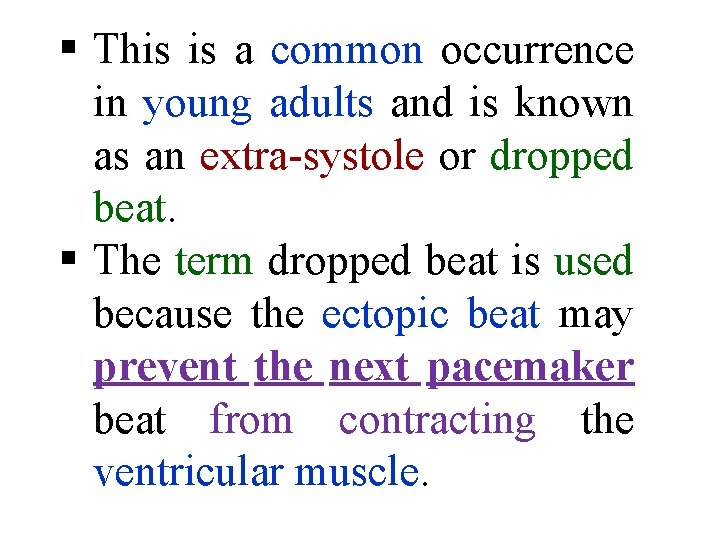
§ This is a common occurrence in young adults and is known as an extra systole or dropped beat. § The term dropped beat is used because the ectopic beat may prevent the next pacemaker beat from contracting the ventricular muscle.
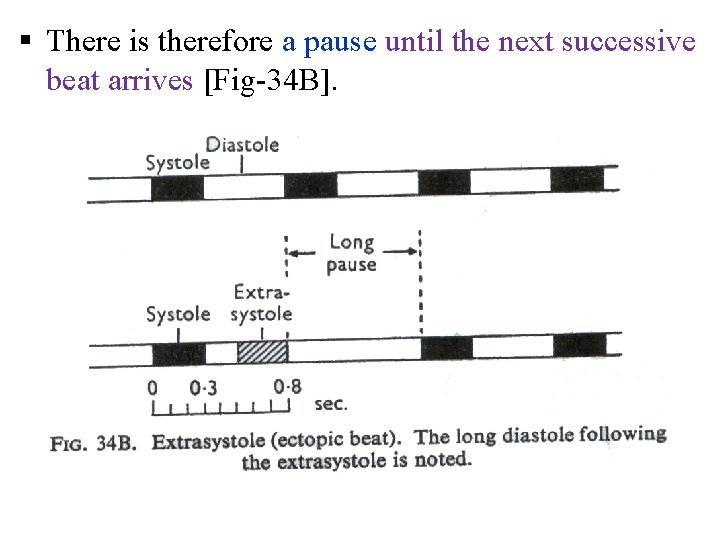
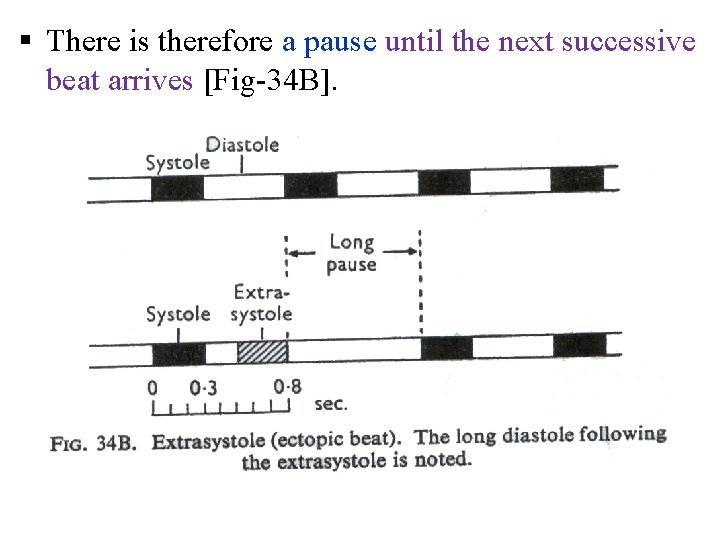
§ There is therefore a pause until the next successive beat arrives [Fig 34 B].
Atrial Fibrillation § Atrial fibrillation occurs when the increased excitability of the atrial muscle leads to abnormal beats arising from ectopic loci in the atria. § As a result, different parts of the atria are contracting and relaxing out of phase with one another.
§ The general appearance of the atria during fibrillation has been described as resembling a bag of wriggling worms. § The atria never empty and the atrial wall becomes a quivering sheet of muscle.
§ In atrial fibrillation the atria cease to pump blood into the ventricles. § In addition, the beat originated by the pacemaker is not transmitted to the ventricles. § Instead, impulses down the bundle of His in a haphazard fashion at a rate too fast for the ventricle to respond to each impulse.
§ The ventricular contractions which do occur are irregular both in rate and amplitude. § A proportion of these beats fail to develop sufficient pressure to open the aortic valve. § As a result the radial pulse is "irregularly irregular" and the heart rate measured at the heart may be higher than if it is measured by the pulse at the wrist. This is known as a pulse deficit.
Ventricular Fibrillation § Should the ventricular muscle fibrillate, the circulation stops immediately. Unless immediate cardiac massage is carried out, life will cease. § Under suitable conditions ventricular fibrillation may be stopped by passing an electric current through the heart. § The apparatus is termed a cardiac defibrillator.
The Electro. Cardio. Gram (E. C. G) § The invasion of the cardiac muscle by the contraction wave is associated with electrical changes. § These potentials may be recorded at points remote from the heart and after electronic amplification may be displayed on a pen recorder or a cathode ray oscilloscope. § The wave form obtained is termed ECG. § The various waves present in the waveform are lettered starting with the letter P.
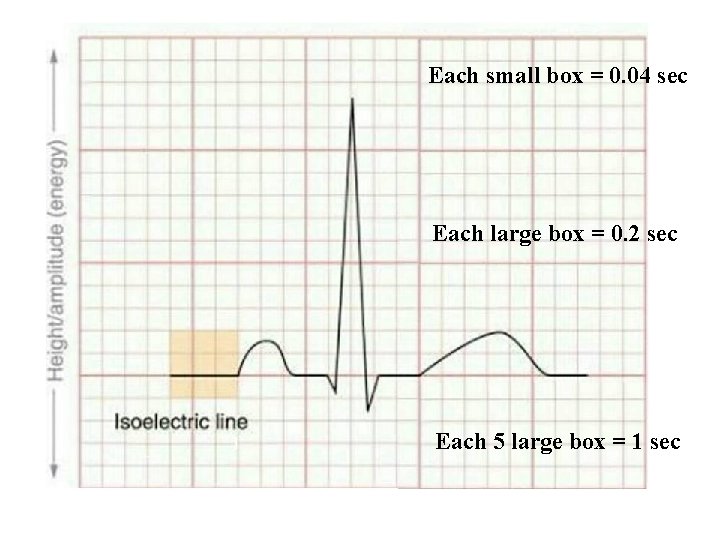
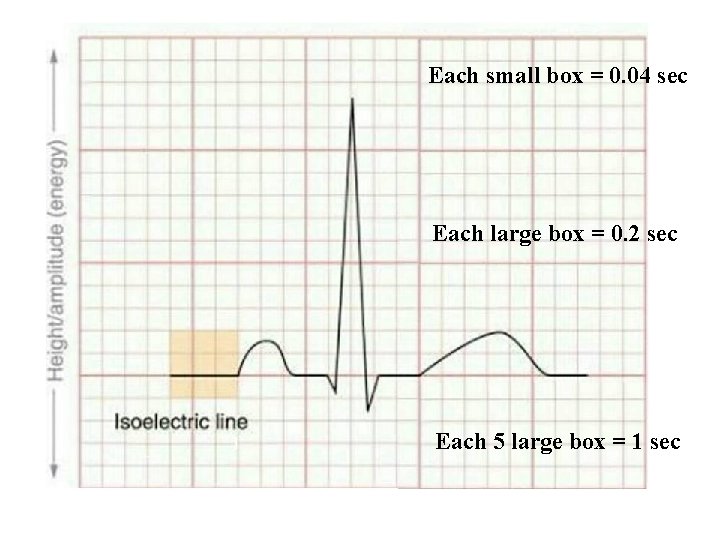
Each small box = 0. 04 sec Each large box = 0. 2 sec Each 5 large box = 1 sec

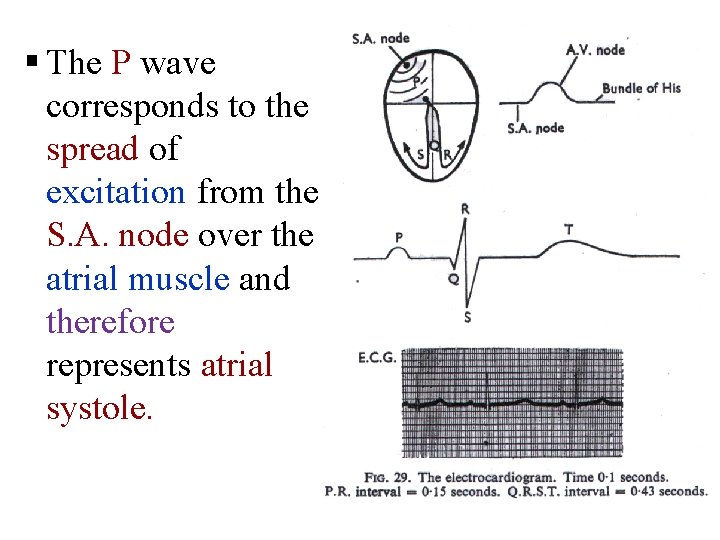
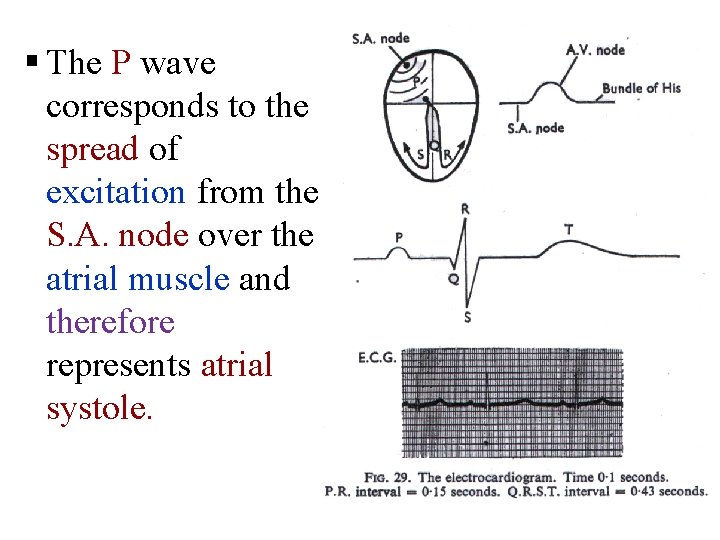
§ The P wave corresponds to the spread of excitation from the S. A. node over the atrial muscle and therefore represents atrial systole.
§ The propagation of the contraction wave down the bundle of His does not produce any detectable external electrical change. It is denoted on the E. C. G. by the iso-electric P Q interval where there is no deflection. § The QRS complex at the commencement of the ventricular excitation, and the T wave at the end are all that remain of this algebraic summation. The relaxation phase T P is iso-electric.
Leads I, Ill, a. VR, a. VL and a. VF § The detailed waveform depends on the site of the recording electrodes. § To record the standard limb leads, electrodes are applied to the left arm, right arm, and left leg. These electrodes usually consist of a metal plate which is strapped over the flat part of the limb. § Electrode fluid or jelly is used between the electrode and the skin to ensure a good electrical connexion.
§ The right leg is not used for recording the ECG, but a further electrode is often applied to this limb to 'earth' the subject, and thus minimize interference from the mains and electrical apparatus. § In order to make a recording, two input connexions must be made to the amplifier and there is usually a switch on the electrocardiograph apparatus which makes the appropriate connexions internally when a particular lead is chosen.
§ When the switch is set at Lead I, the electrodes on the right and left arms are connected to the amplifier. The amplifier then records the potential difference between the right arm and the left arm. § When the switch is set to Lead II, the potential difference between the right arm and left leg is recorded. §When set to Lead III, the potential difference between the left arm and left leg is recorded.
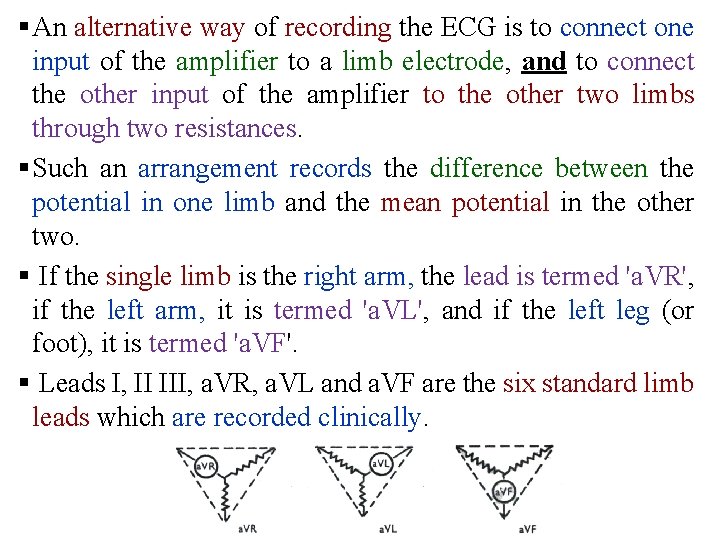
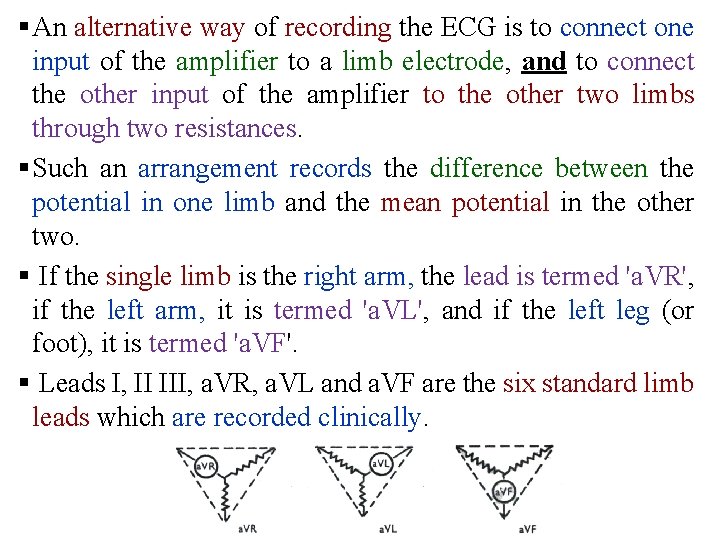
§ An alternative way of recording the ECG is to connect one input of the amplifier to a limb electrode, and to connect the other input of the amplifier to the other two limbs through two resistances. § Such an arrangement records the difference between the potential in one limb and the mean potential in the other two. § If the single limb is the right arm, the lead is termed 'a. VR', if the left arm, it is termed 'a. VL', and if the left leg (or foot), it is termed 'a. VF'. § Leads I, II III, a. VR, a. VL and a. VF are the six standard limb leads which are recorded clinically.
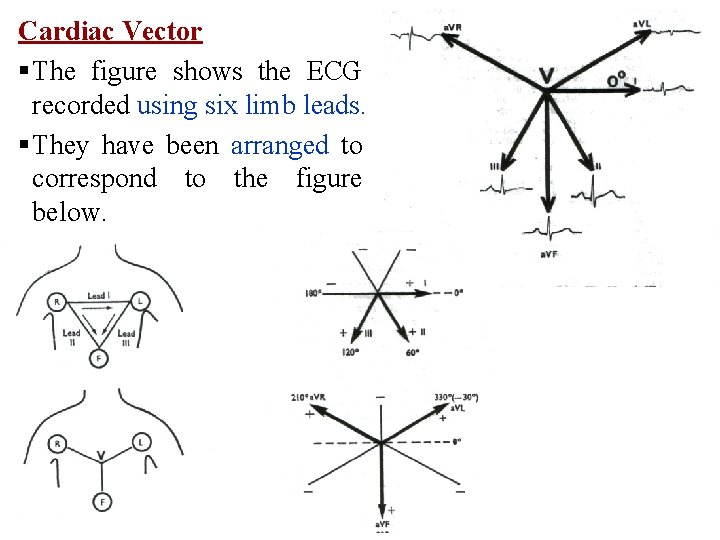
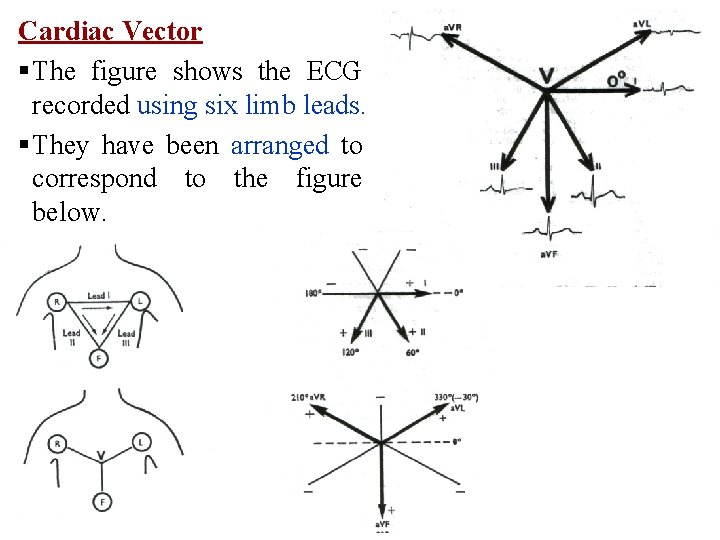
Cardiac Vector § The figure shows the ECG recorded using six limb leads. § They have been arranged to correspond to the figure below.
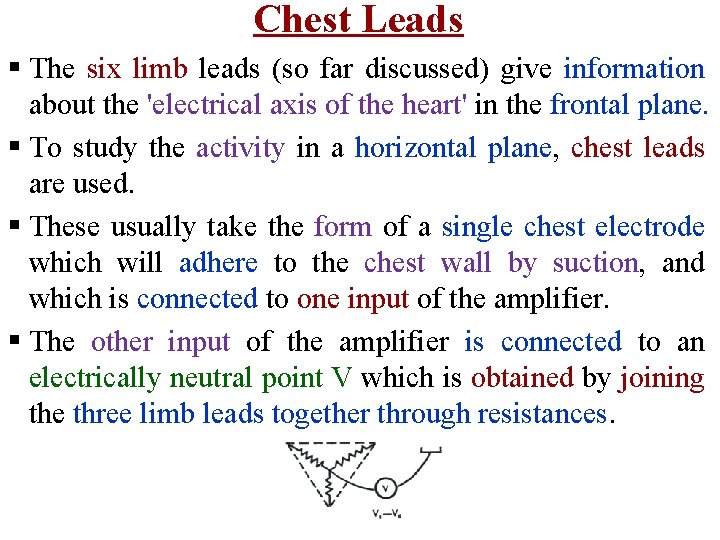
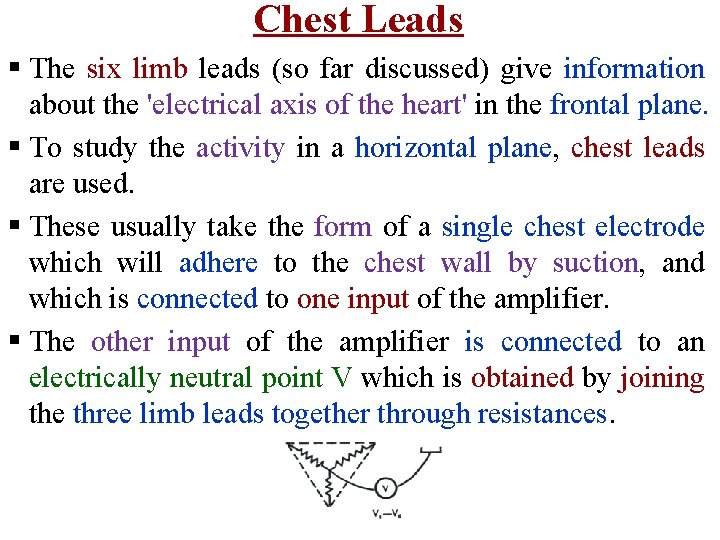
Chest Leads § The six limb leads (so far discussed) give information about the 'electrical axis of the heart' in the frontal plane. § To study the activity in a horizontal plane, chest leads are used. § These usually take the form of a single chest electrode which will adhere to the chest wall by suction, and which is connected to one input of the amplifier. § The other input of the amplifier is connected to an electrically neutral point V which is obtained by joining the three limb leads together through resistances.
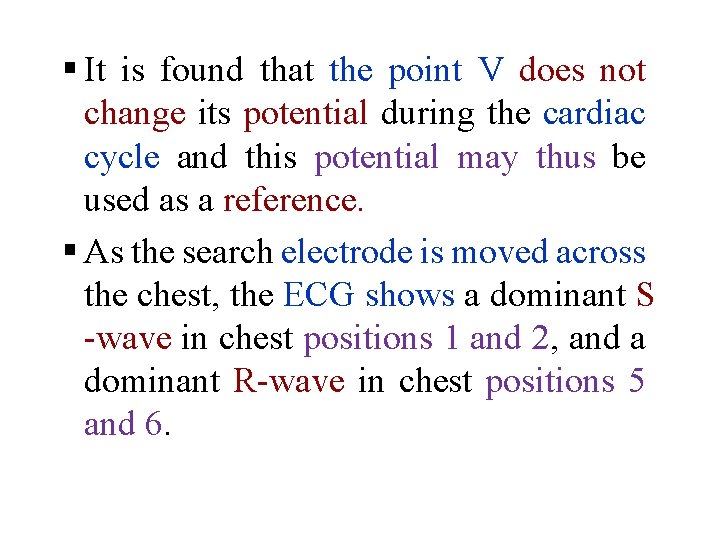
§ It is found that the point V does not change its potential during the cardiac cycle and this potential may thus be used as a reference. § As the search electrode is moved across the chest, the ECG shows a dominant S wave in chest positions 1 and 2, and a dominant R wave in chest positions 5 and 6.
