Premature Infants Adapted by Pam Jordan Ph D
Premature Infants Adapted by Pam Jordan, Ph. D, RNC from Susan Jones, MN, RNC
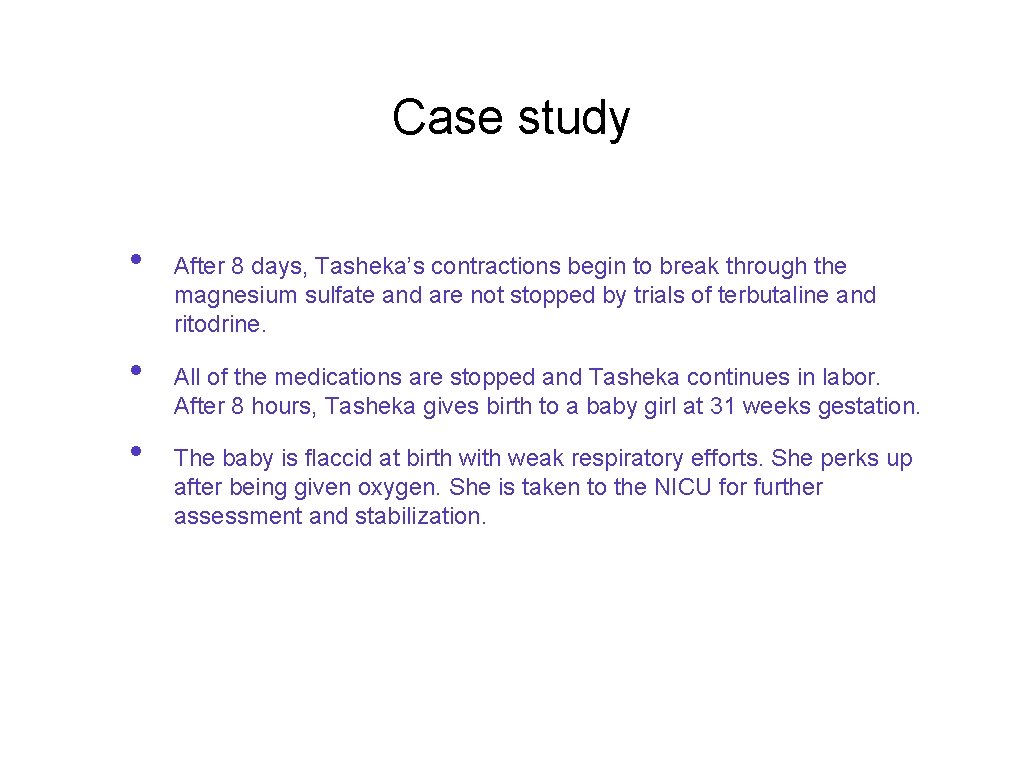
Case study • • • After 8 days, Tasheka’s contractions begin to break through the magnesium sulfate and are not stopped by trials of terbutaline and ritodrine. All of the medications are stopped and Tasheka continues in labor. After 8 hours, Tasheka gives birth to a baby girl at 31 weeks gestation. The baby is flaccid at birth with weak respiratory efforts. She perks up after being given oxygen. She is taken to the NICU for further assessment and stabilization.
![Troubling & Persistent Disparities in Rates of Preterm Birth [2010 statistics] Non-Hispanic Blacks 17. Troubling & Persistent Disparities in Rates of Preterm Birth [2010 statistics] Non-Hispanic Blacks 17.](http://slidetodoc.com/presentation_image/395425430aefe2e5f5ba993e81e24a19/image-3.jpg)
Troubling & Persistent Disparities in Rates of Preterm Birth [2010 statistics] Non-Hispanic Blacks 17. 15% Native Americans 13. 9% Hispanics 11. 97% Non-Hispanic Whites 10. 9% Asians 10. 9% Preterm birth is the leading cause of neonatal mortality and morbidity in the US.
Definitions Preterm birth refers only to gestational age at birth, regardless of birth weight. Very preterm=<32 weeks Moderately preterm=32 -34 weeks Late preterm=34 -36 weeks
![Definitions Low birth weight [LBW] refers only to birth weight regardless of gestational age. Definitions Low birth weight [LBW] refers only to birth weight regardless of gestational age.](http://slidetodoc.com/presentation_image/395425430aefe2e5f5ba993e81e24a19/image-5.jpg)
Definitions Low birth weight [LBW] refers only to birth weight regardless of gestational age. Low birthweight <2500 g [5. 5 lbs] Very low birthweight <1500 g [3. 5 lbs] Extremely low birthweight <1000 g [2. 2 lbs]
Adverse Outcomes Associated with PTB • • • • Respiratory distress syndrome Transient tachypnea of the newborn Pulmonary infection Unspecified respiratory failure Recurrent apnea Temperature instability Jaundice Bilirubin-induced brain injury Rehospitalization for all causes Rehospitalization for dehydration Feeding difficulties Long term neurodevelopmental delay Periventricular leukomalacia
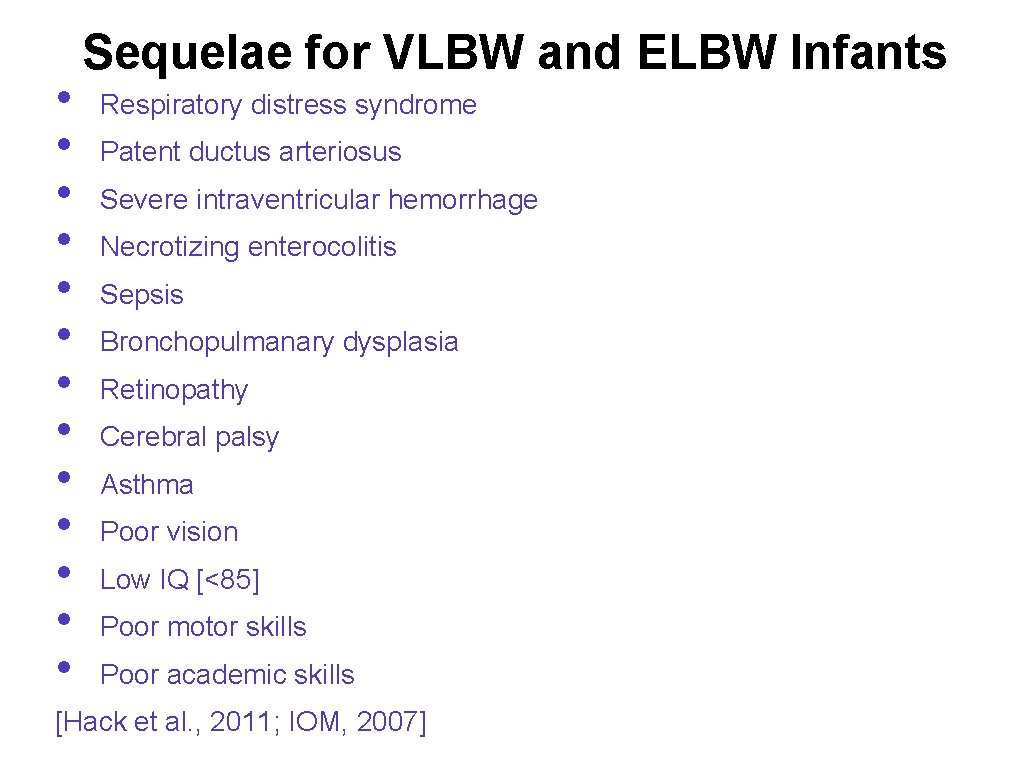
• • • • Sequelae for VLBW and ELBW Infants Respiratory distress syndrome Patent ductus arteriosus Severe intraventricular hemorrhage Necrotizing enterocolitis Sepsis Bronchopulmanary dysplasia Retinopathy Cerebral palsy Asthma Poor vision Low IQ [<85] Poor motor skills Poor academic skills [Hack et al. , 2011; IOM, 2007]
![Cost of PTB • • $26. 2 billion in US in 2005 [IOM, 2007] Cost of PTB • • $26. 2 billion in US in 2005 [IOM, 2007]](http://slidetodoc.com/presentation_image/395425430aefe2e5f5ba993e81e24a19/image-8.jpg)
Cost of PTB • • $26. 2 billion in US in 2005 [IOM, 2007] Costs to employers: • • $64, 713 for mother and baby compared to $15, 047 for uncomplicated birth and healthy newborn [Thomson Reuters, 2008]
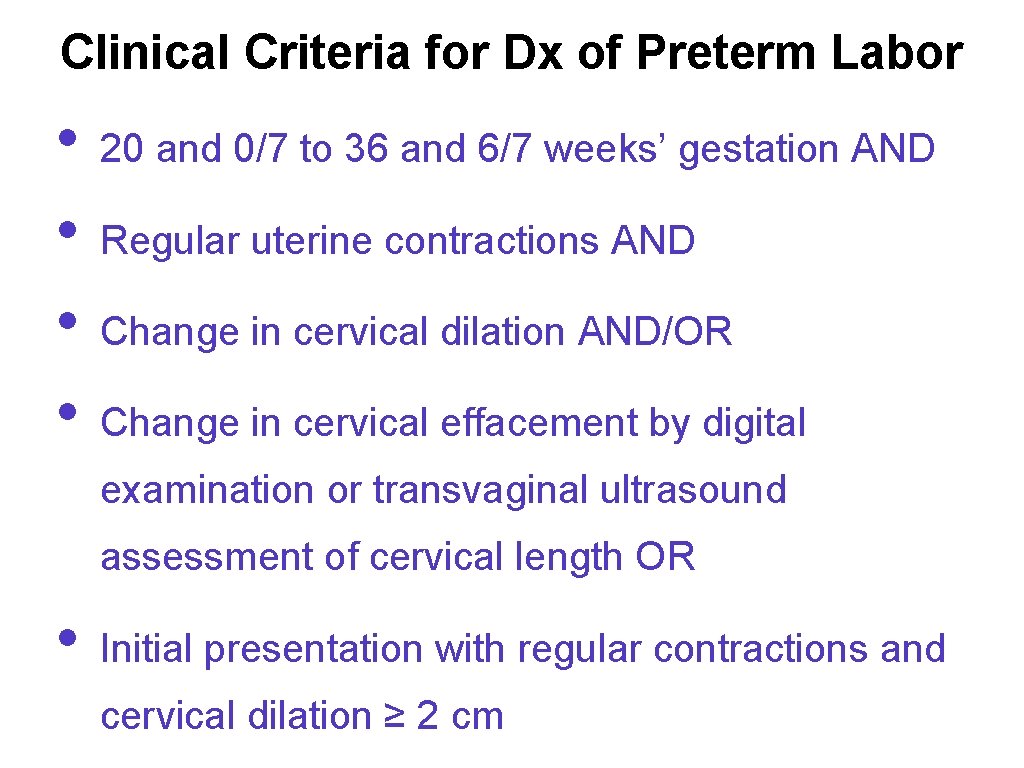
Clinical Criteria for Dx of Preterm Labor • • 20 and 0/7 to 36 and 6/7 weeks’ gestation AND Regular uterine contractions AND Change in cervical dilation AND/OR Change in cervical effacement by digital examination or transvaginal ultrasound assessment of cervical length OR • Initial presentation with regular contractions and cervical dilation ≥ 2 cm
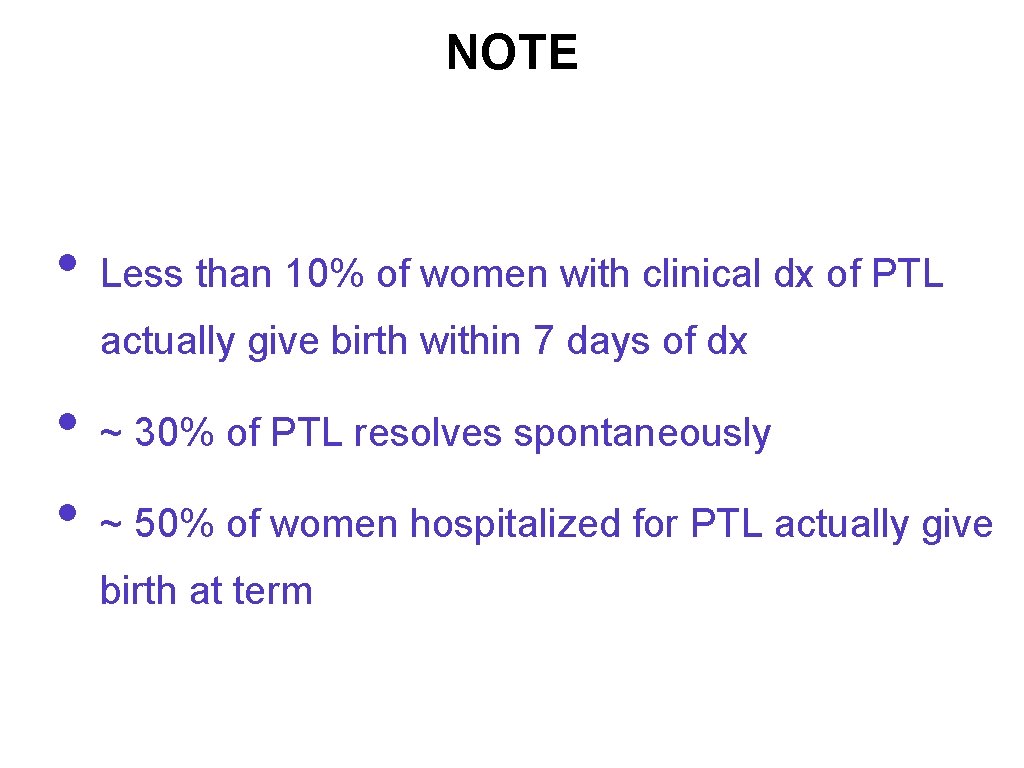
NOTE • Less than 10% of women with clinical dx of PTL actually give birth within 7 days of dx • • ~ 30% of PTL resolves spontaneously ~ 50% of women hospitalized for PTL actually give birth at term
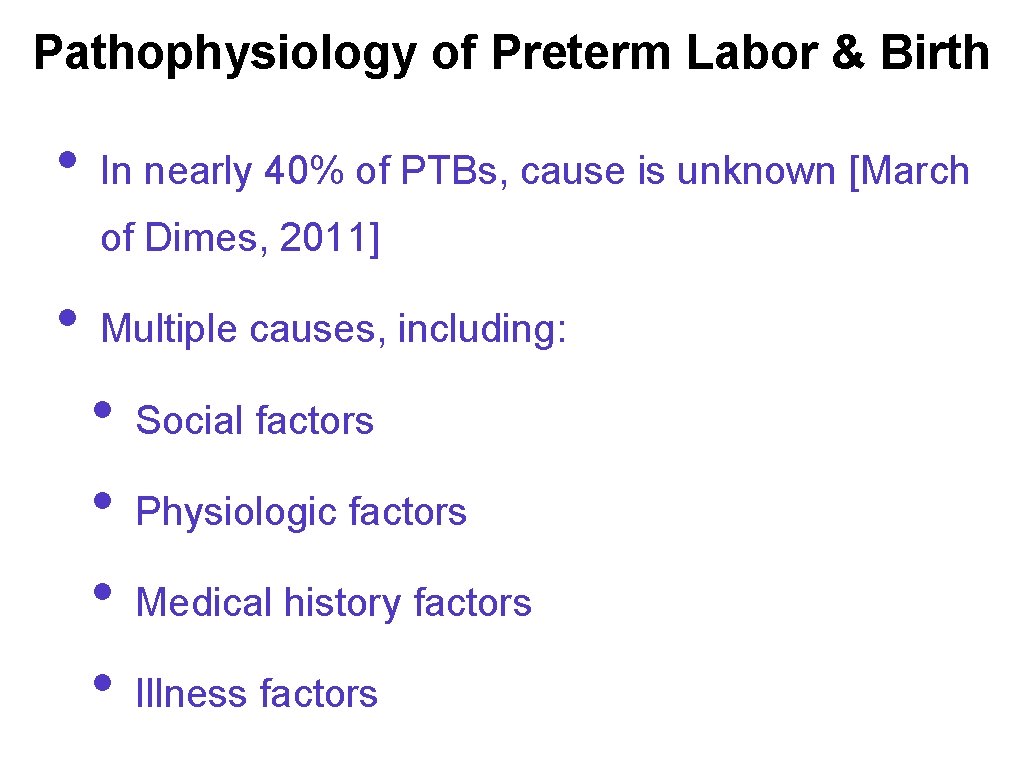
Pathophysiology of Preterm Labor & Birth • In nearly 40% of PTBs, cause is unknown [March of Dimes, 2011] • Multiple causes, including: • • Social factors Physiologic factors Medical history factors Illness factors
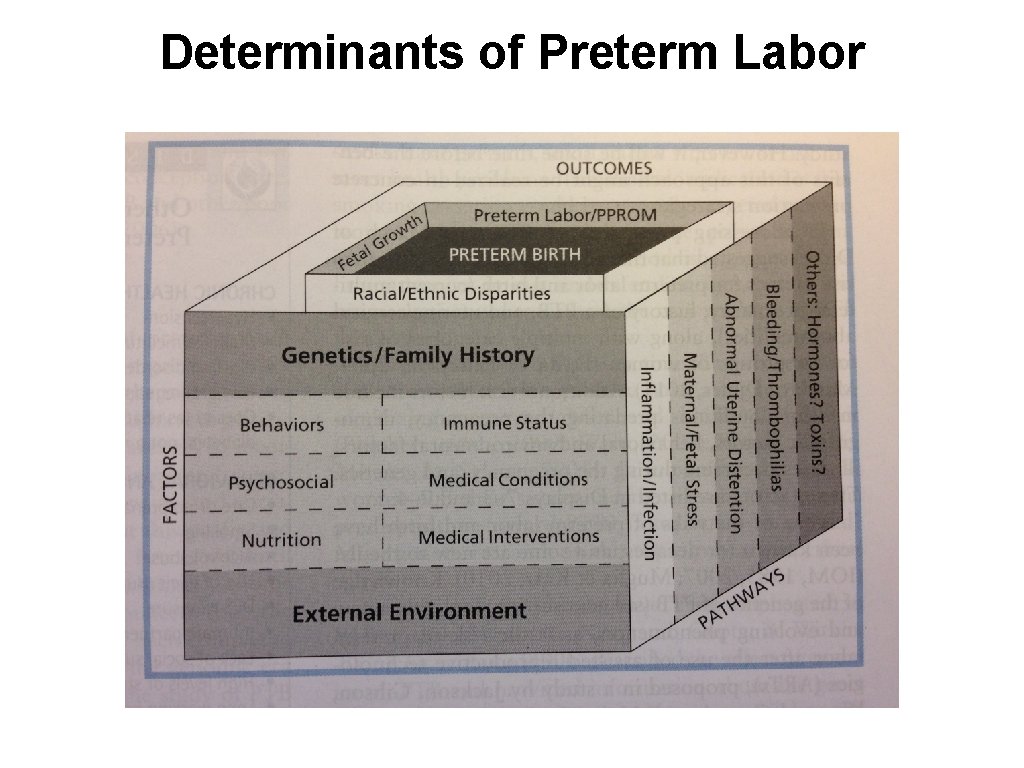
Determinants of Preterm Labor
![Four Main Routes Leading to PTL [March of Dimes, 2011] 1. Infections/inflammation: from genital Four Main Routes Leading to PTL [March of Dimes, 2011] 1. Infections/inflammation: from genital](http://slidetodoc.com/presentation_image/395425430aefe2e5f5ba993e81e24a19/image-13.jpg)
Four Main Routes Leading to PTL [March of Dimes, 2011] 1. Infections/inflammation: from genital and urinary tract, fetal membranes, periodontal disease 2. Maternal or fetal stress • Chronic psychosocial stress in mother or physical stress in fetus 3. Bleeding [placental abruption] 4. Uterine stretching [multiple gestation, polyhydramnios, uterine or placental abnormalities] ~25% of PTBs are intentional R/T health problems in mother or fetus ~another 25% of PTBs follow premature preterm rupture of membranes
Most Common Risk Factors for PTL/PTB • • • Current multifetal pregnancy History of preterm birth Uterine/cervical abnormalities
Other Possible Risk Factors for PTL Chronic health problems • • • Hypertension Diabetes mellitus Clotting disorders/thrombophilia Low prepregnancy weight Obesity [as related to comorbidities, such as HTN, DM, not a risk factor for spontaneous preterm labor
Other Possible Risk Factors for PTL Behavioral and environmental factors • • • Late or no prenatal care Smoking Alcohol abuse Use of illicit drugs DES exposure Intimate partner violence Lack of social support High levels of stress Long working hours Long periods of standing
Other Possible Risk Factors for PTL Demographic risks • • Non-Hispanic black race Age <17 years Age >35 years Low socioeconomic status
Other Possible Risk Factors for PTL Genetics-assisted reproductive technologies Medical risks in current pregnancy • • Infection [esp. genitourinary] Short interpregnancy interval Fetal anomalies Preterm premature rupture of membranes Vaginal bleeding, esp in the second trimester or in more than one trimester Periodontal disease Being underweight prior to pregnancy
• • Objectives: apply your knowledge of term infants and compare and contrast with premature newborns Discuss the following subjects: • How would this preterm baby’s transition to extrauterine life differ from that of a term infant? • • Thermoregulation Respiratory Cardiac GI/Nutrition/Fluids Immune function Neurologic Skin How can you support Tasheka and BJ while their daughter is in the NICU?
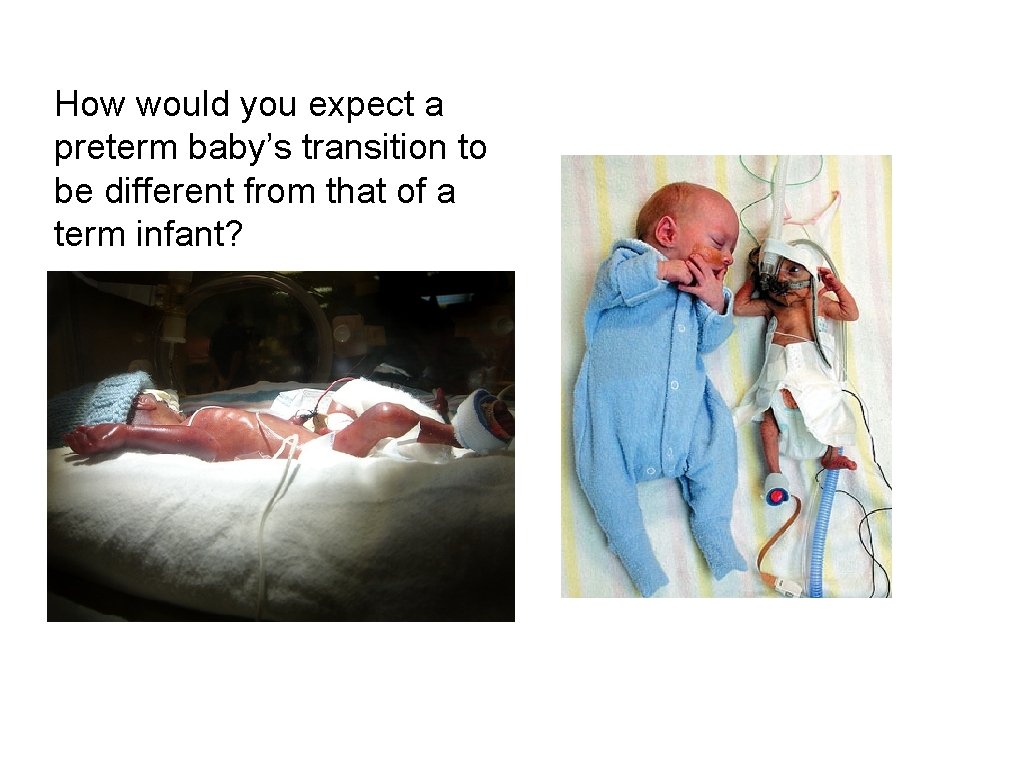
How would you expect a preterm baby’s transition to be different from that of a term infant?
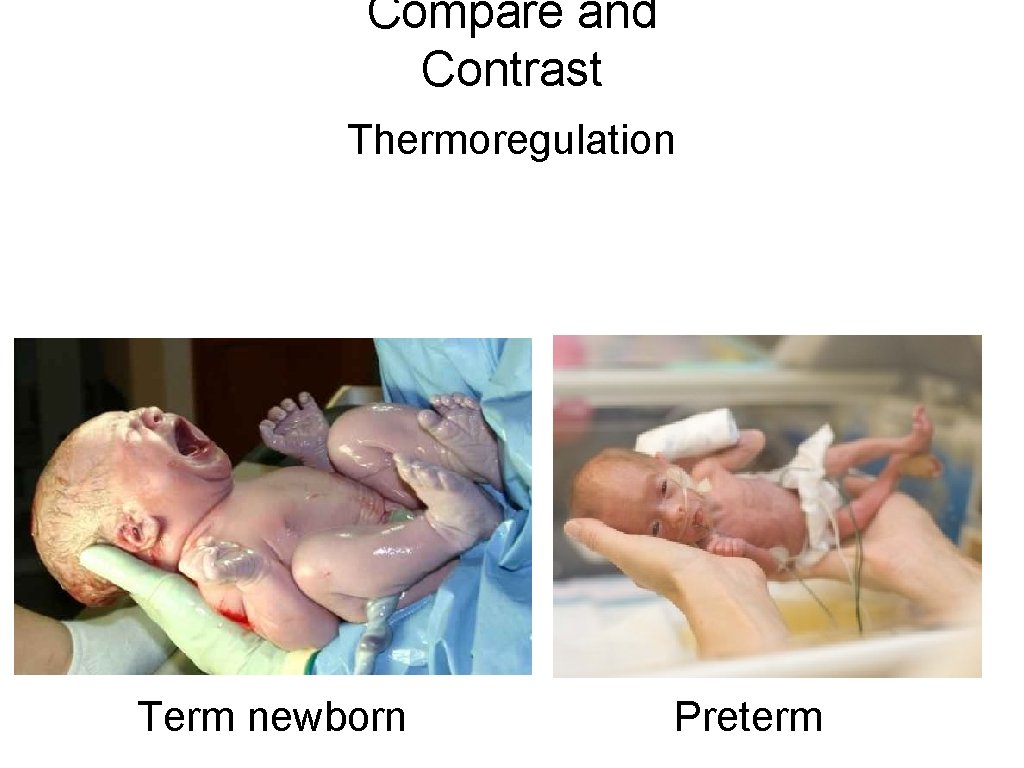
Compare and Contrast Thermoregulation Term newborn Preterm
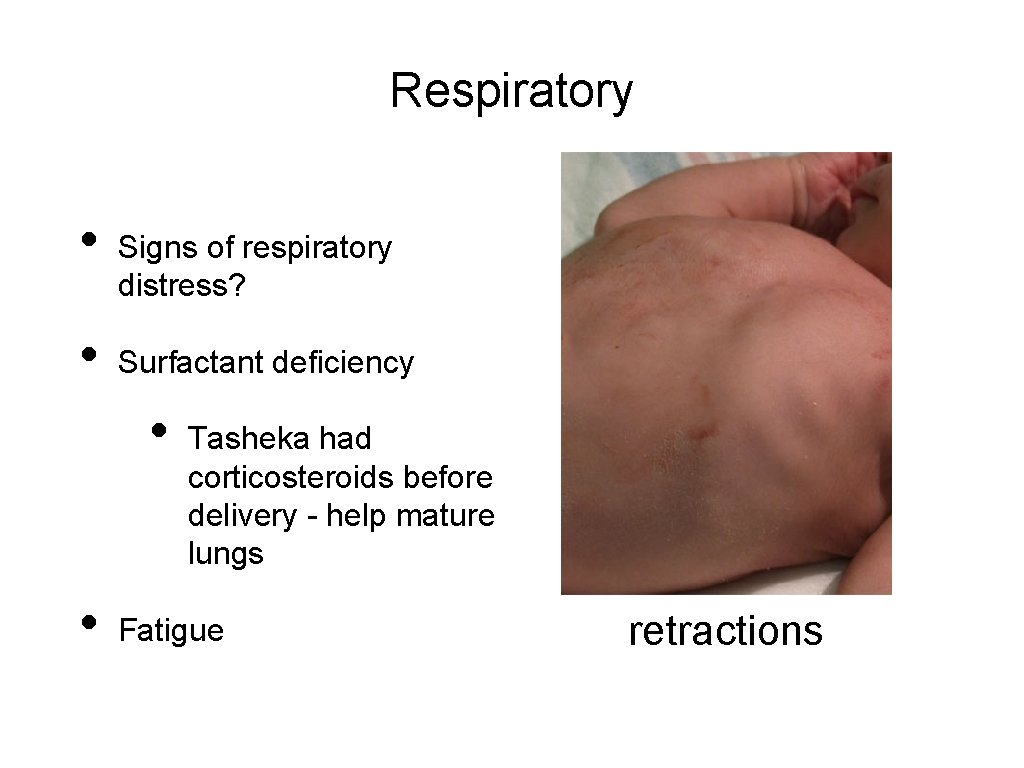
Respiratory • • Signs of respiratory distress? Surfactant deficiency • • Tasheka had corticosteroids before delivery - help mature lungs Fatigue retractions
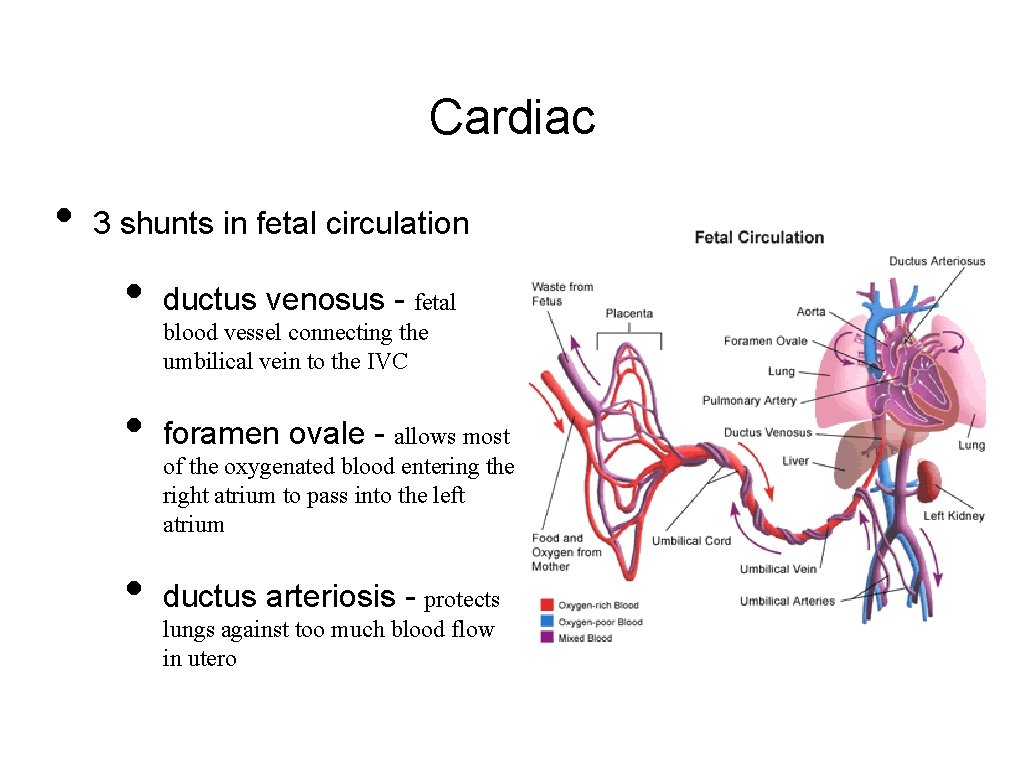
Cardiac • 3 shunts in fetal circulation • ductus venosus - fetal • foramen ovale - allows most • ductus arteriosis - protects blood vessel connecting the umbilical vein to the IVC of the oxygenated blood entering the right atrium to pass into the left atrium lungs against too much blood flow in utero
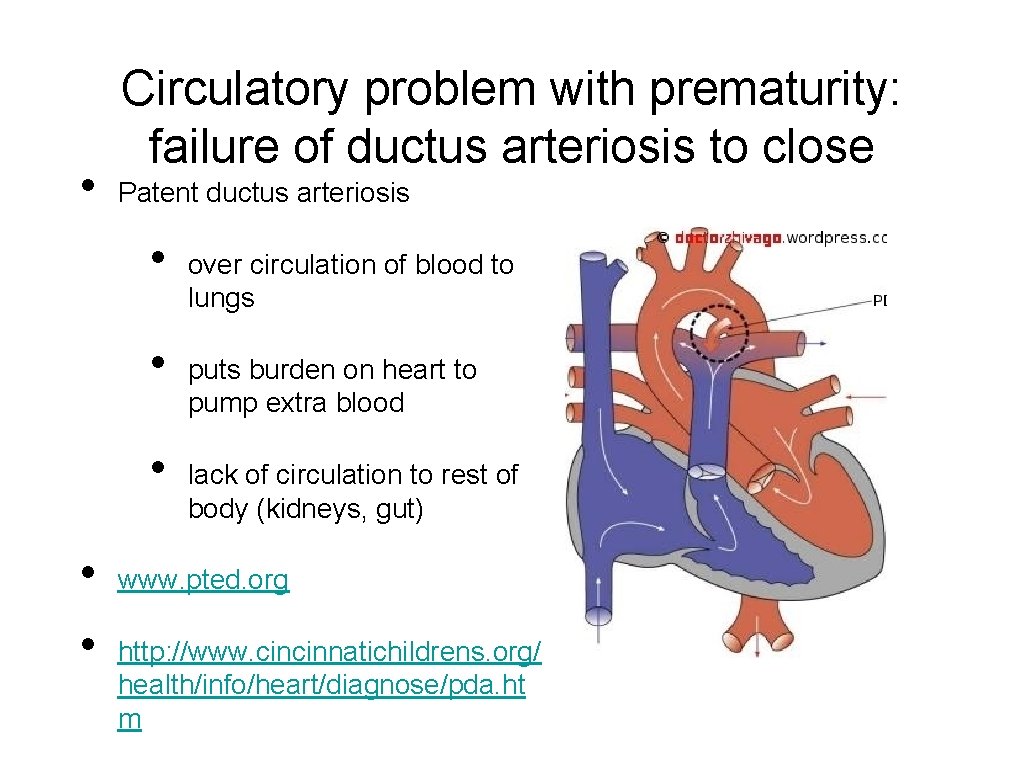
• Circulatory problem with prematurity: failure of ductus arteriosis to close Patent ductus arteriosis • • • over circulation of blood to lungs puts burden on heart to pump extra blood lack of circulation to rest of body (kidneys, gut) www. pted. org http: //www. cincinnatichildrens. org/ health/info/heart/diagnose/pda. ht m
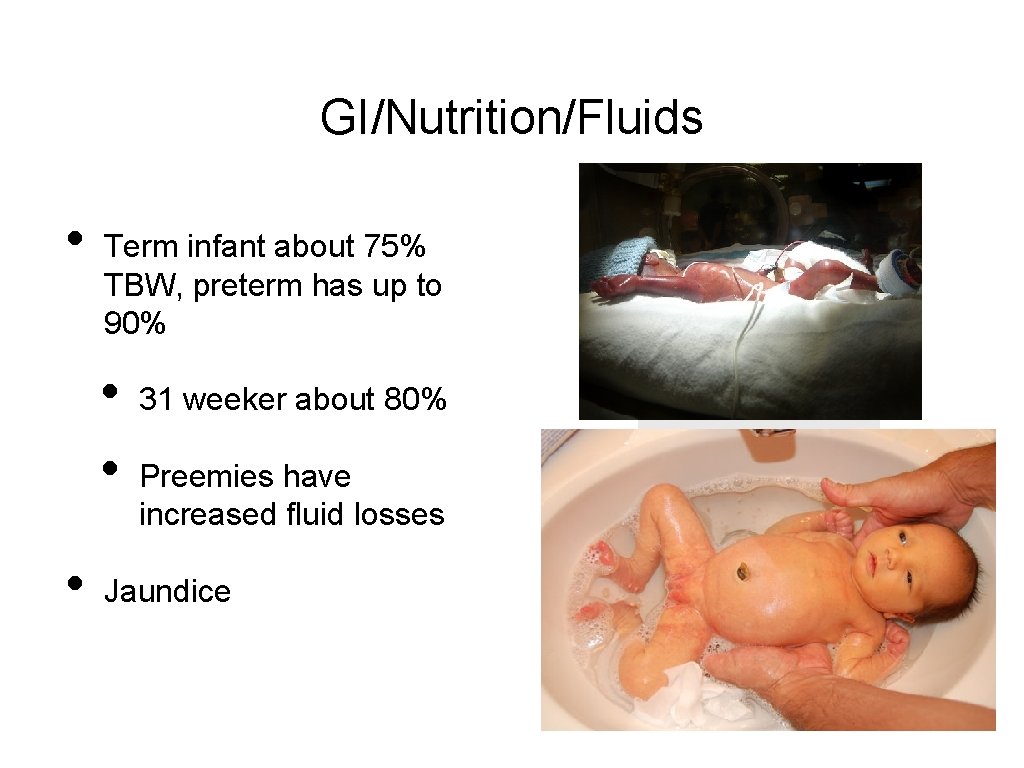
GI/Nutrition/Fluids • Term infant about 75% TBW, preterm has up to 90% • • • 31 weeker about 80% Preemies have increased fluid losses Jaundice
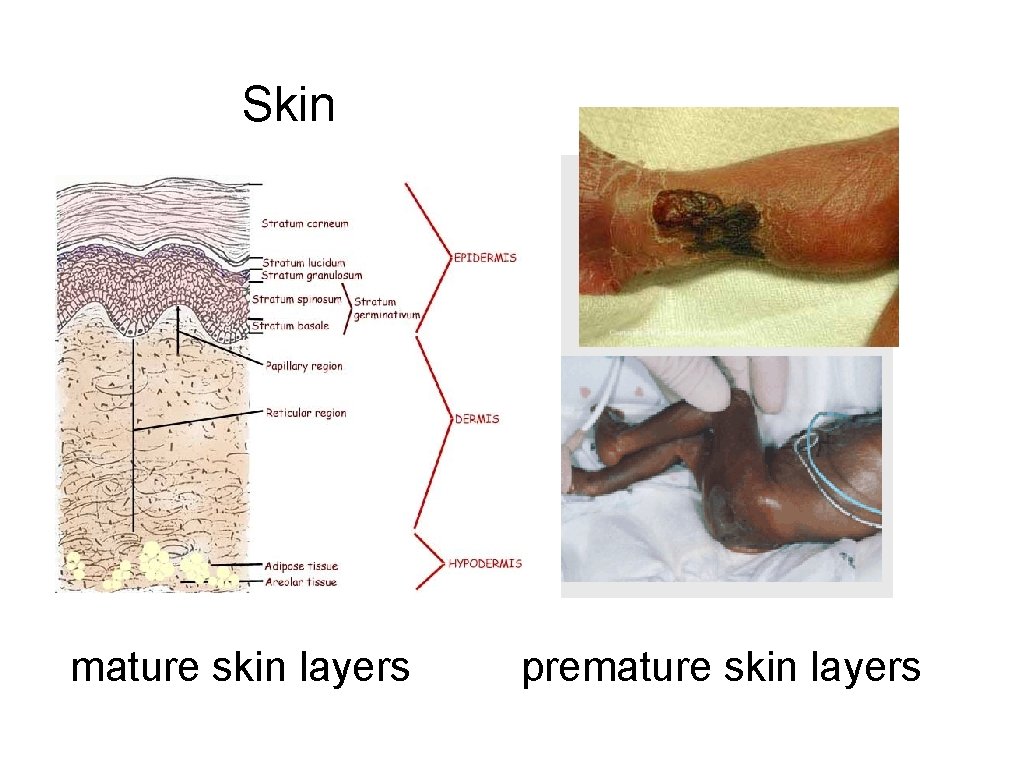
Skin mature skin layers premature skin layers
Immune Function • Placental transfer of immunity (Ig. G) • Breast milk • premature milk higher in protein first 3 weeks • immunologic factors • • secretory immunoglobulin A (Ig. A) leukocytes

Promote breastfeeding • • • How? Why? Immature gut - risks? Feeding ability - oral? NG?
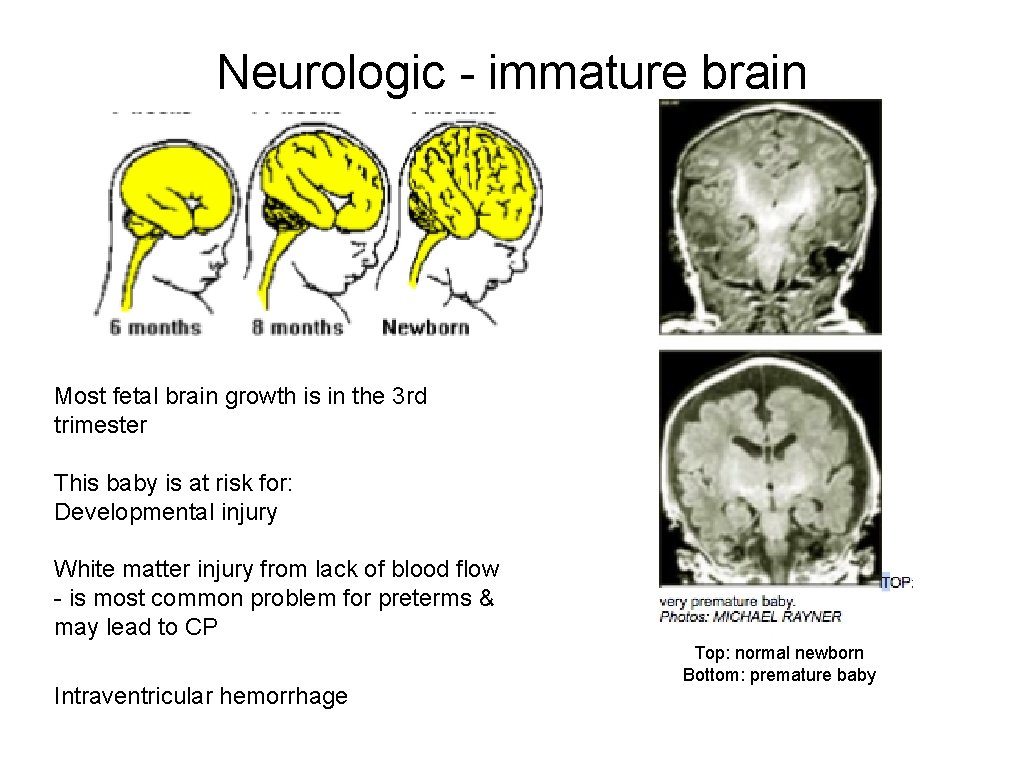
Neurologic - immature brain Most fetal brain growth is in the 3 rd trimester This baby is at risk for: Developmental injury White matter injury from lack of blood flow - is most common problem for preterms & may lead to CP Intraventricular hemorrhage Top: normal newborn Bottom: premature baby

Compare tone
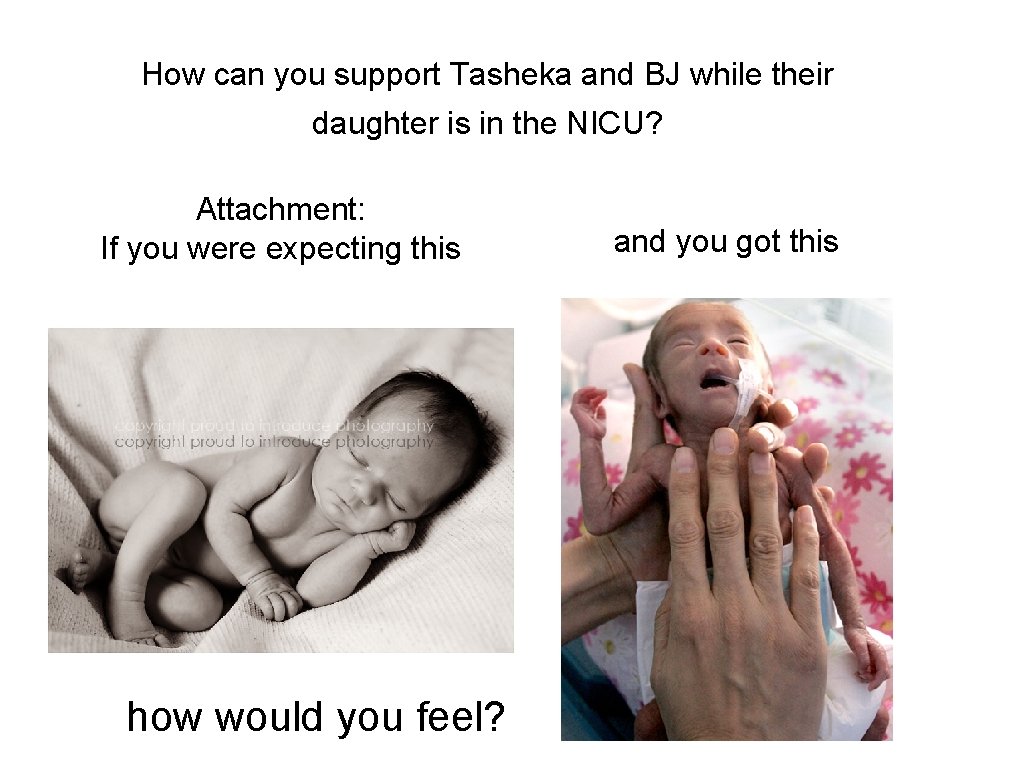
How can you support Tasheka and BJ while their daughter is in the NICU? Attachment: If you were expecting this how would you feel? and you got this

Family support
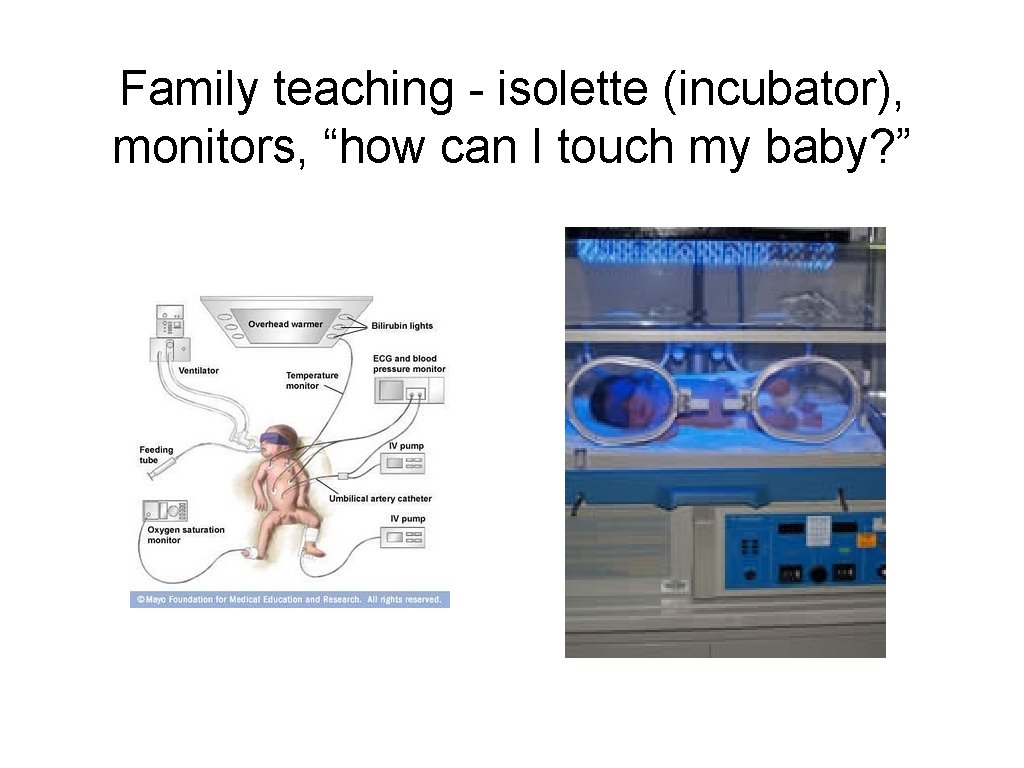
Family teaching - isolette (incubator), monitors, “how can I touch my baby? ”

Facilitated Tuck with Dad’s Hands
Helpful websites • http: //www. meriter. com/living/preemie/ • www. marchofdimes. com/aboutus/ttmm m • http: //newborns. stanford. edu/Photo. Gall ery/ • www. prematurity. org (careful with blogs and forums - lots of misinformation) • www. nann. org (NICU RN professional organization)
Primary source: Reedy, N. J. (2014). Preterm labor and birth. In Simpson, K. R. & Creehan, P. A. (Eds. ), Perinatal nursing (4 th edition) (pp. 166 -202). Philadelphia, PA: Wolters Kluwer/Lippincott, Williams, & Wilkins.
- Slides: 36