Section Three Introduction Arterial Pressure Venous Circulation Microcirculation
- Slides: 99
Section Three Introduction Arterial Pressure Venous Circulation Microcirculation Blood Vessels
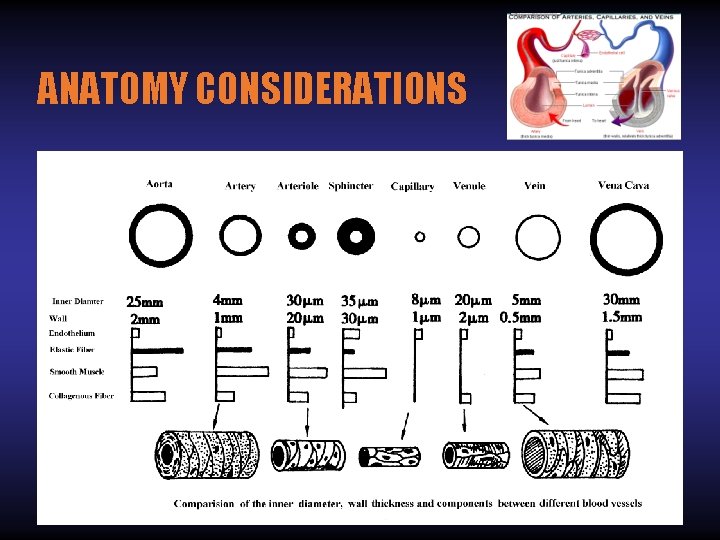
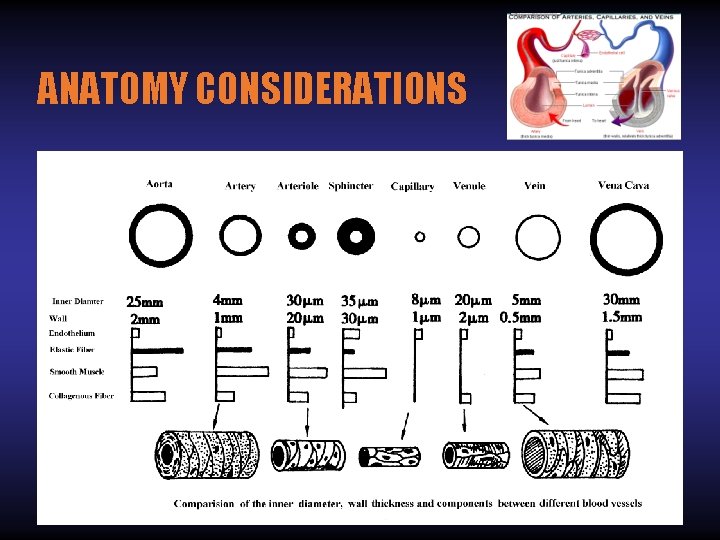
ANATOMY CONSIDERATIONS
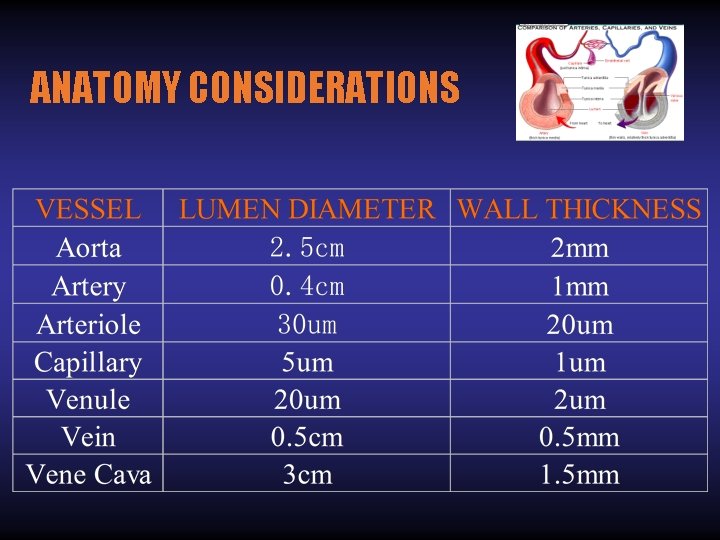
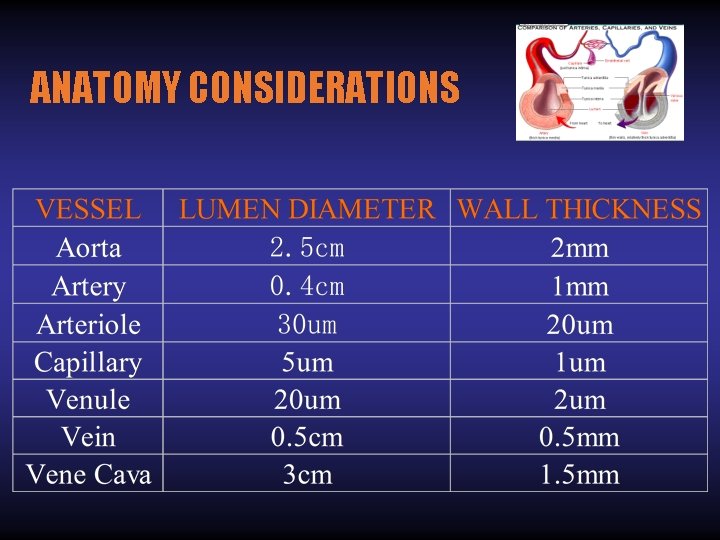
ANATOMY CONSIDERATIONS
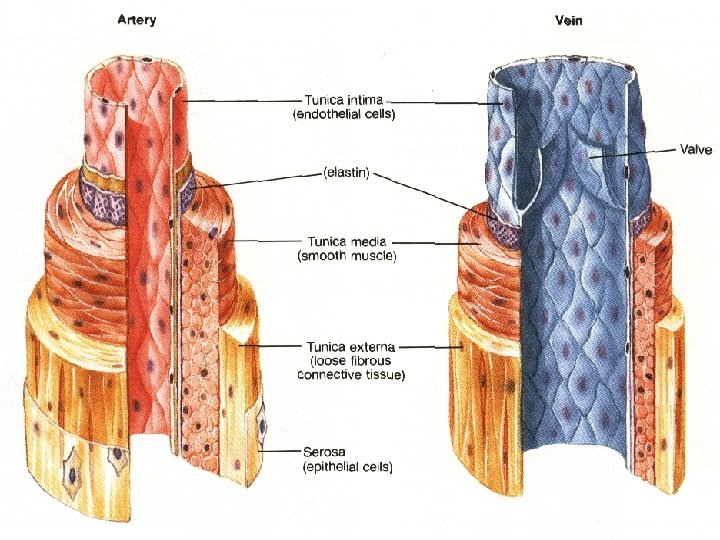
I. Physiological Classification of Blood Vessels
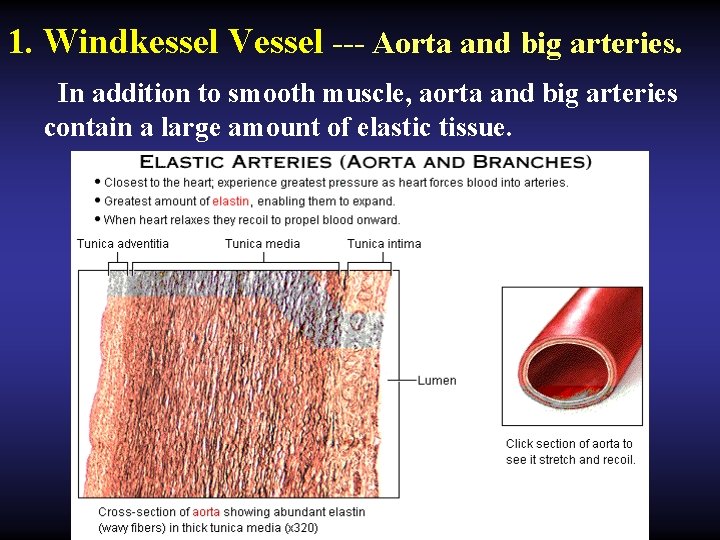
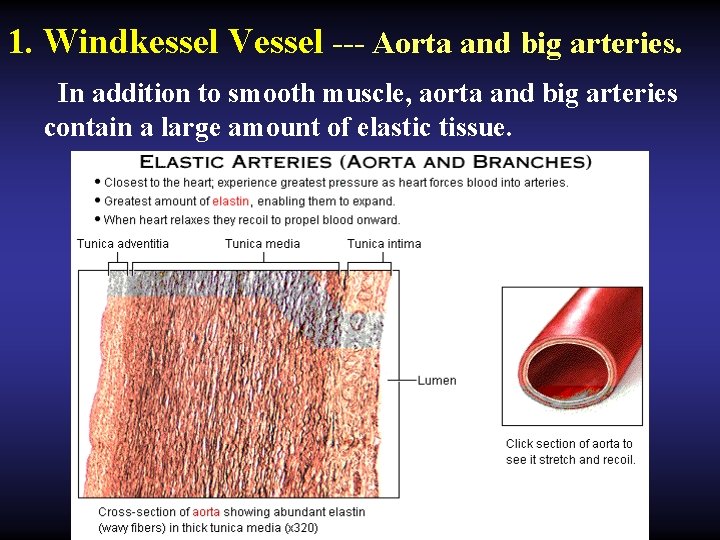
1. Windkessel Vessel --- Aorta and big arteries. In addition to smooth muscle, aorta and big arteries contain a large amount of elastic tissue.
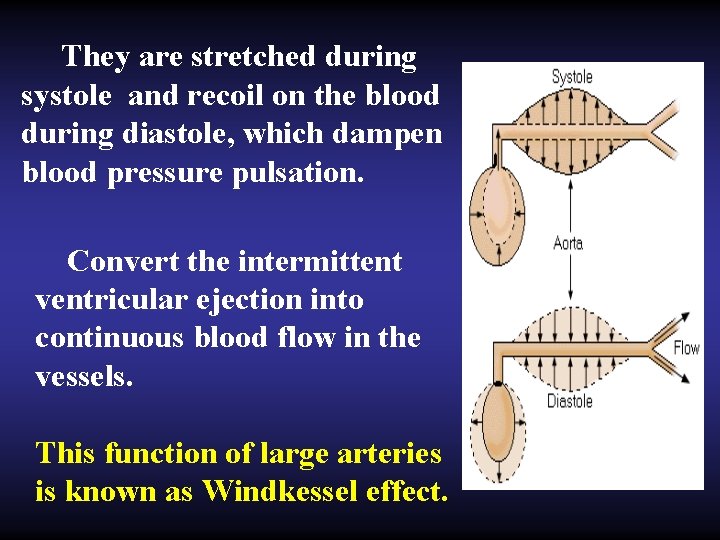
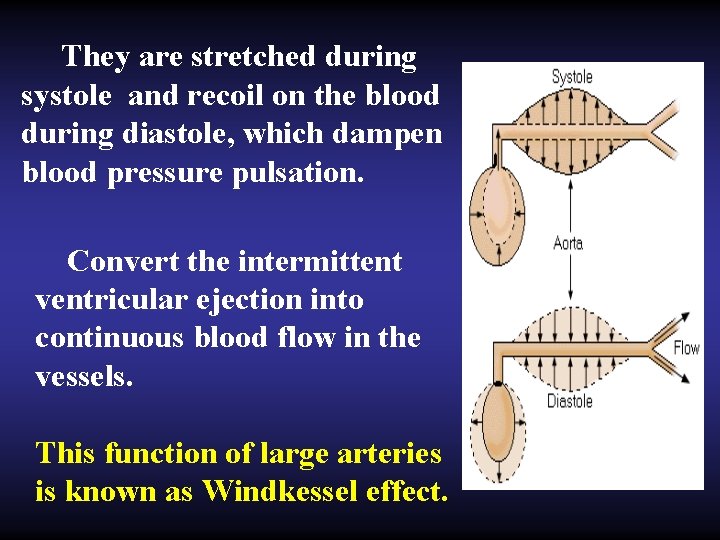
They are stretched during systole and recoil on the blood during diastole, which dampen blood pressure pulsation. Convert the intermittent ventricular ejection into continuous blood flow in the vessels. This function of large arteries is known as Windkessel effect.
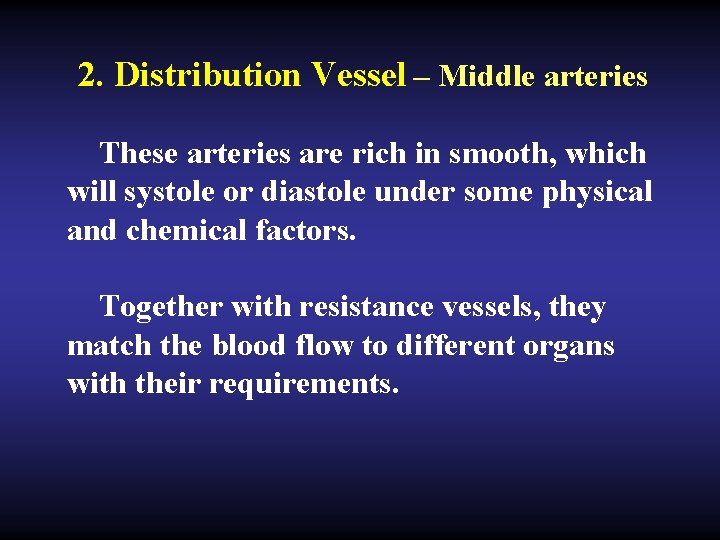
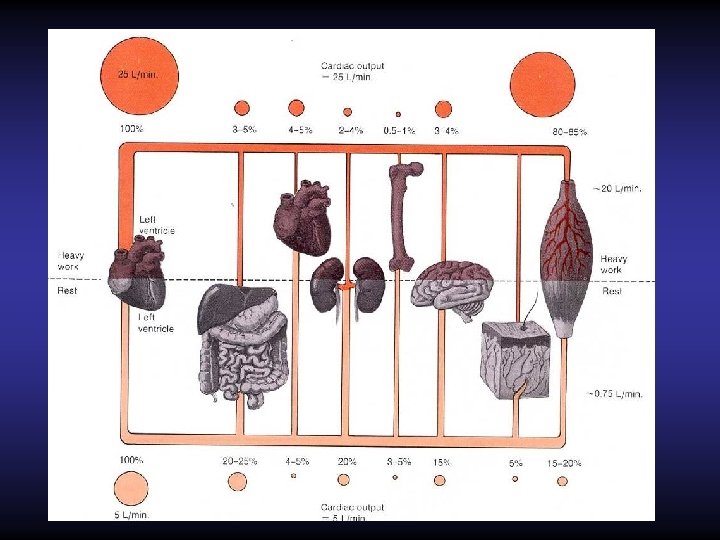
2. Distribution Vessel – Middle arteries These arteries are rich in smooth, which will systole or diastole under some physical and chemical factors. Together with resistance vessels, they match the blood flow to different organs with their requirements.
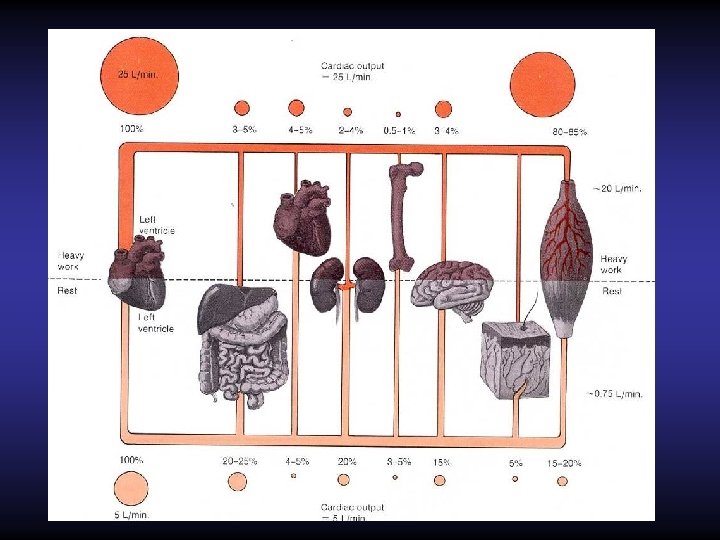
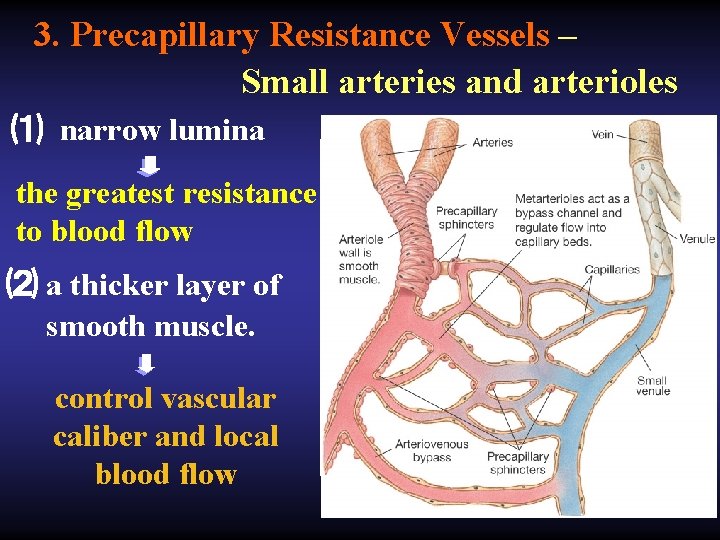
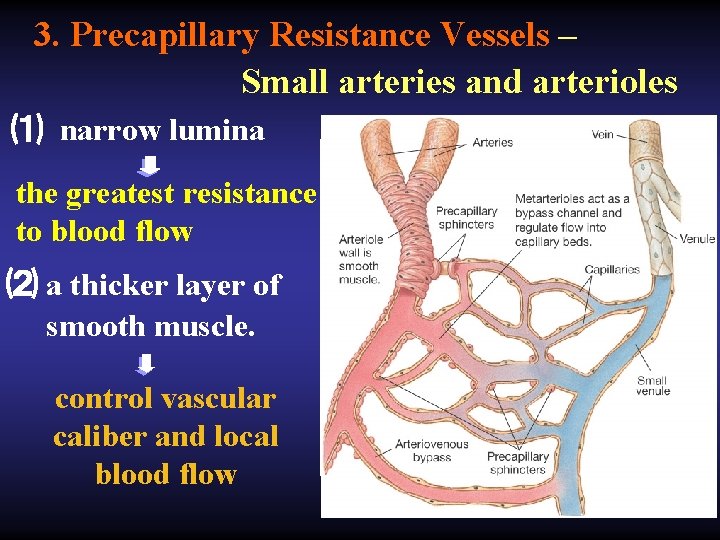
3. Precapillary Resistance Vessels – Small arteries and arterioles ⑴ narrow lumina the greatest resistance to blood flow ⑵ a thicker layer of smooth muscle. control vascular caliber and local blood flow
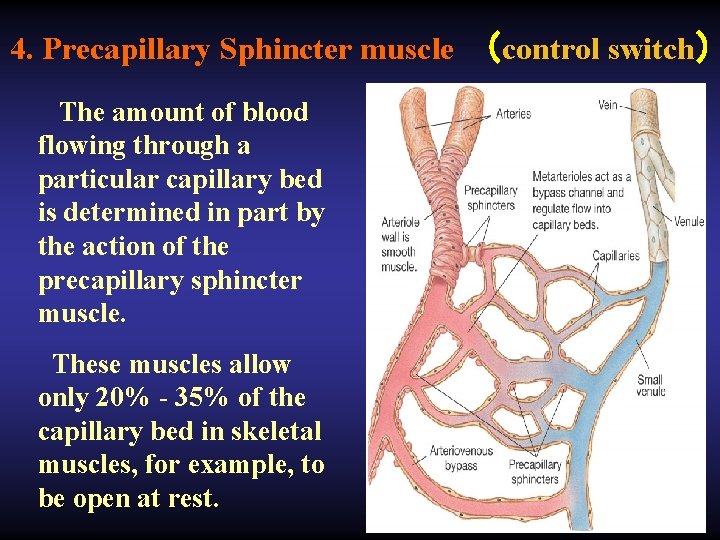
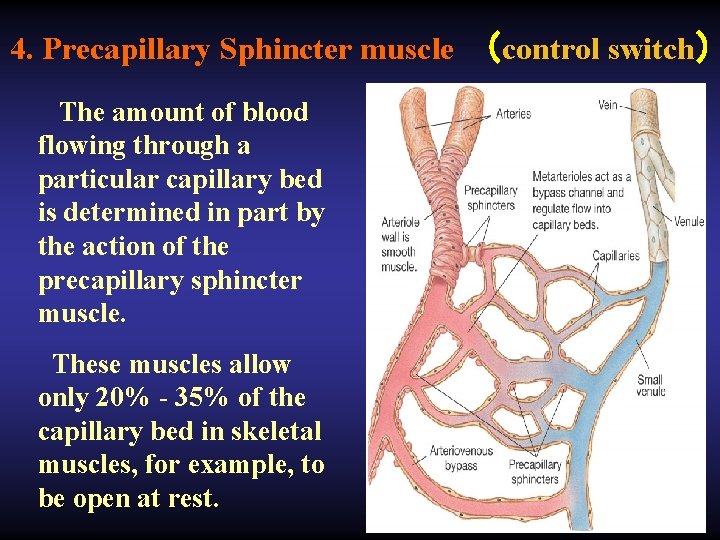
4. Precapillary Sphincter muscle (control switch) The amount of blood flowing through a particular capillary bed is determined in part by the action of the precapillary sphincter muscle. These muscles allow only 20% - 35% of the capillary bed in skeletal muscles, for example, to be open at rest.
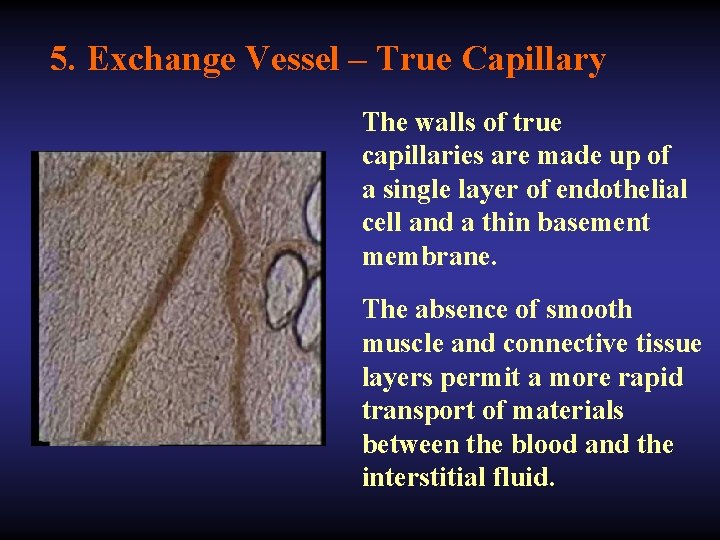
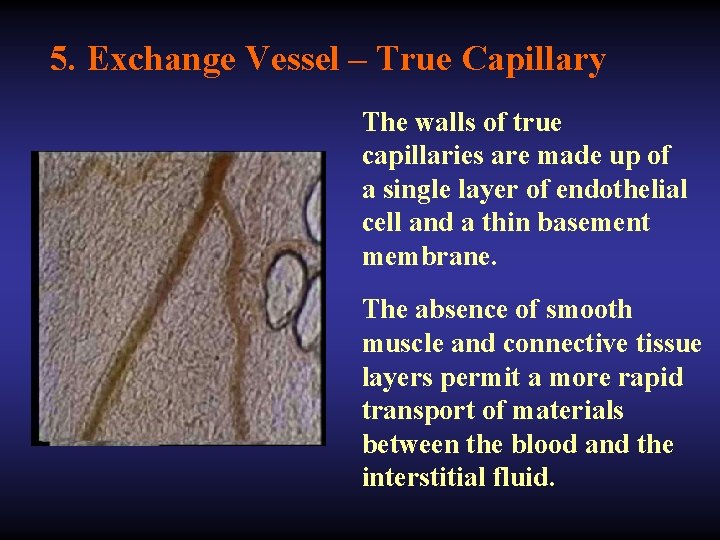
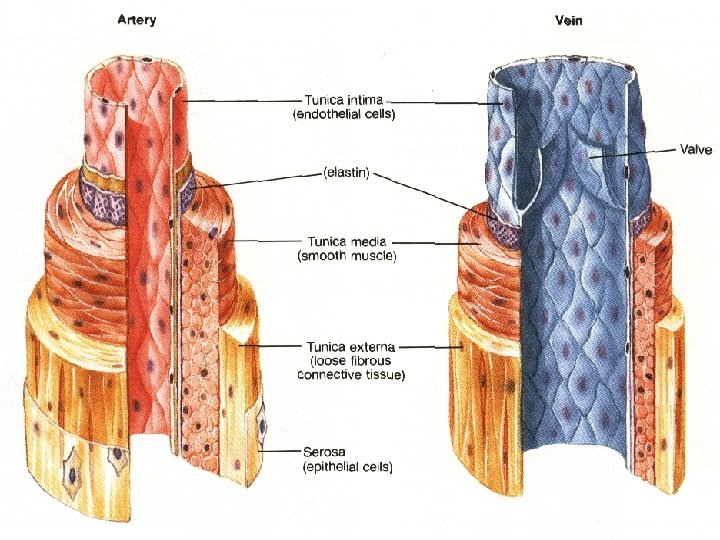
5. Exchange Vessel – True Capillary The walls of true capillaries are made up of a single layer of endothelial cell and a thin basement membrane. The absence of smooth muscle and connective tissue layers permit a more rapid transport of materials between the blood and the interstitial fluid.
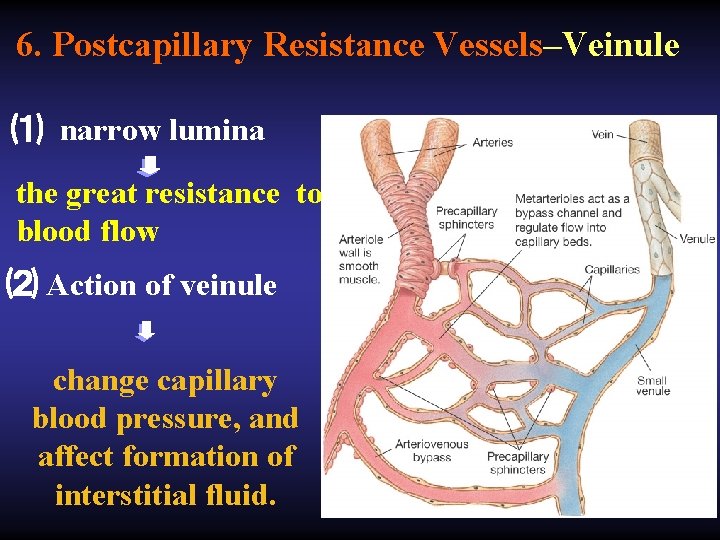
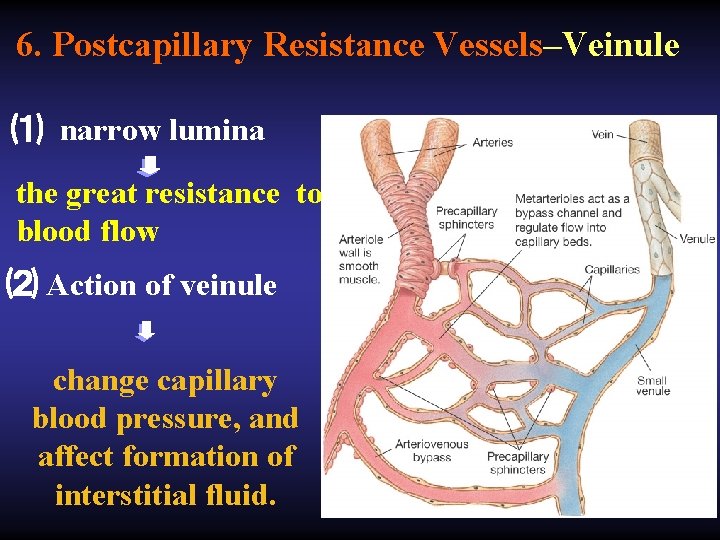
6. Postcapillary Resistance Vessels–Veinule ⑴ narrow lumina the great resistance to blood flow ⑵ Action of veinule change capillary blood pressure, and affect formation of interstitial fluid.
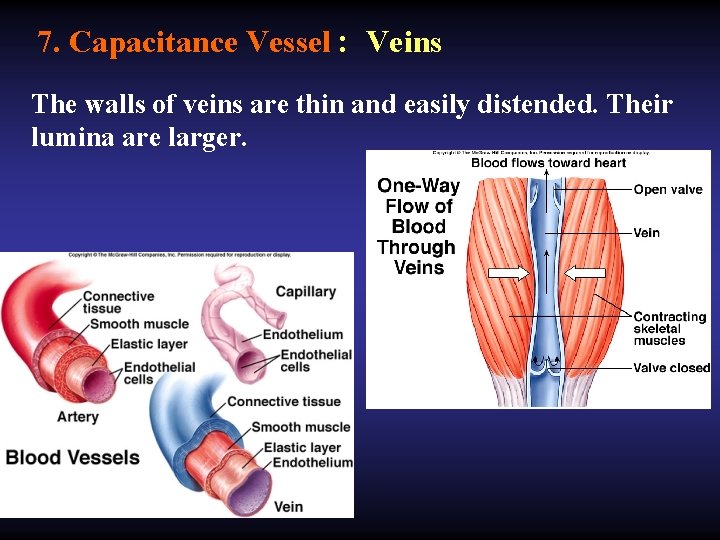
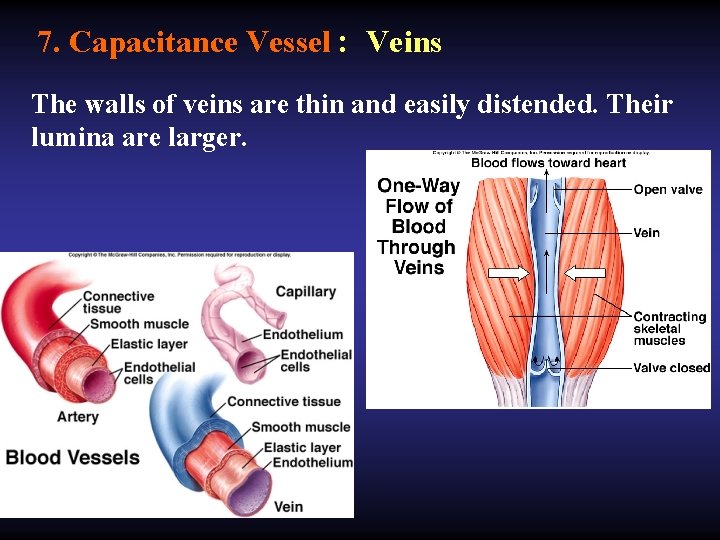
7. Capacitance Vessel : Veins The walls of veins are thin and easily distended. Their lumina are larger.
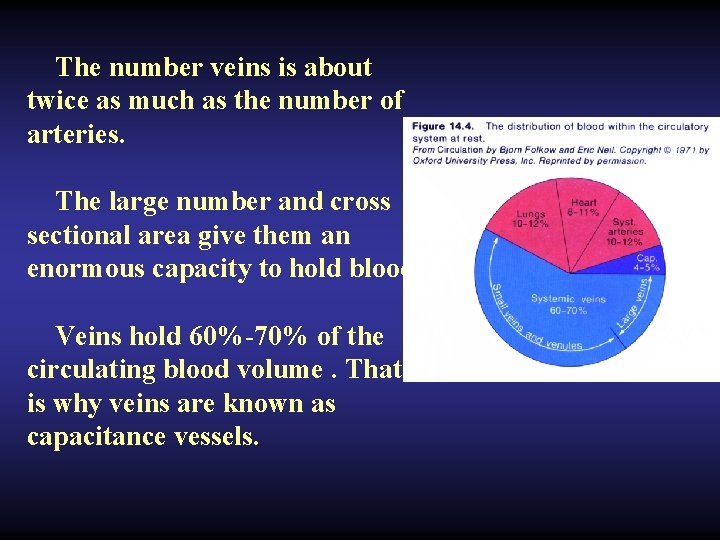
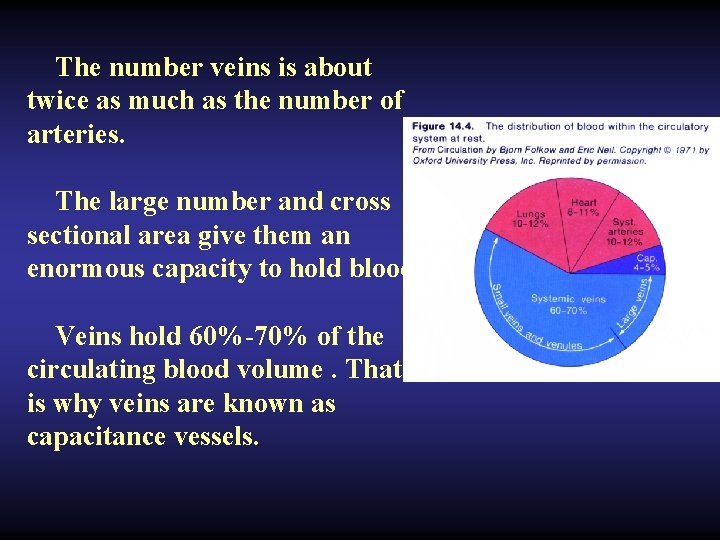
The number veins is about twice as much as the number of arteries. The large number and cross sectional area give them an enormous capacity to hold blood. Veins hold 60%-70% of the circulating blood volume. That is why veins are known as capacitance vessels.
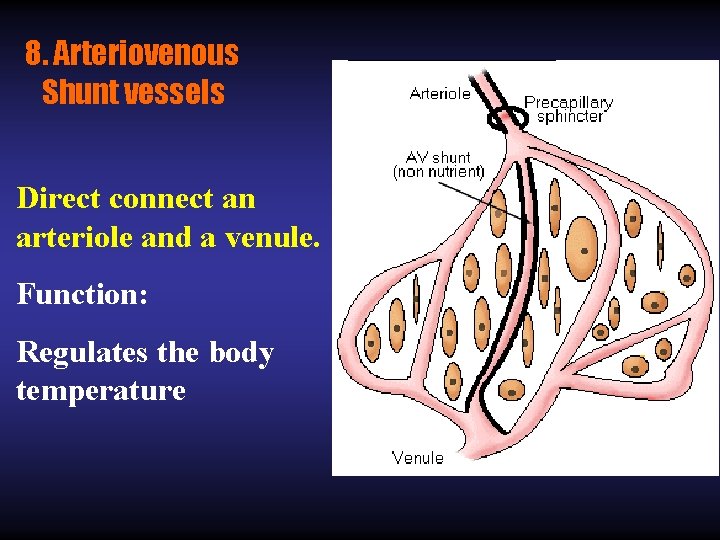
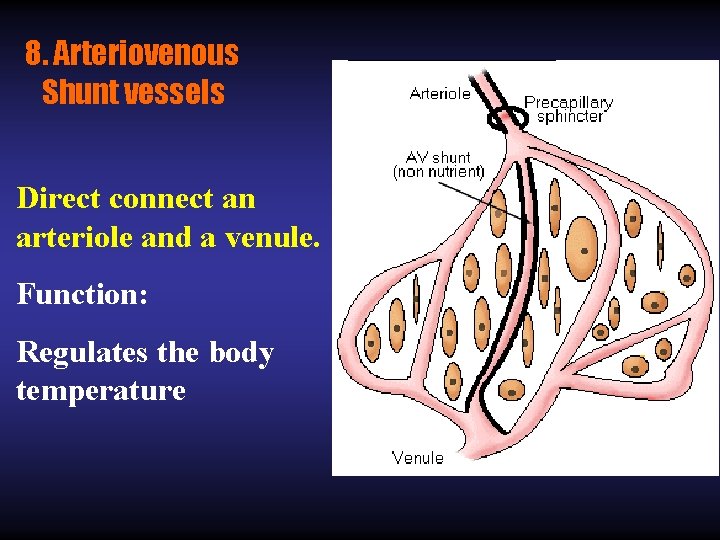
8. Arteriovenous Shunt vessels Direct connect an arteriole and a venule. Function: Regulates the body temperature
II Basic Concept of Hemodynamics: Blood Flow, Resistance of Blood Flow and Blood Pressure
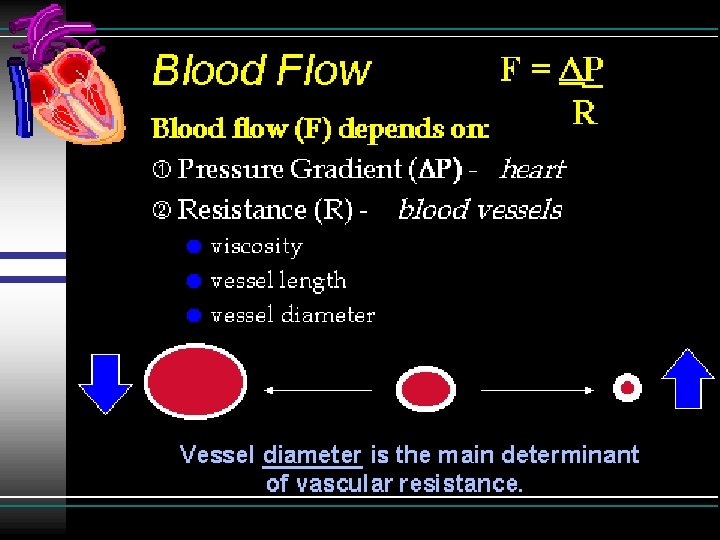
1. Blood Flow (Q) (1) Concept: The quantity of blood that passes through a cross section of blood vessel in unit time is called blood flow(also called volume velocity). (2) Velocity of blood flow(V) means line speed of a particle in the blood circulation. (3) Q ↑, V ↑ (4) Area of a cross section ↑, V ↓
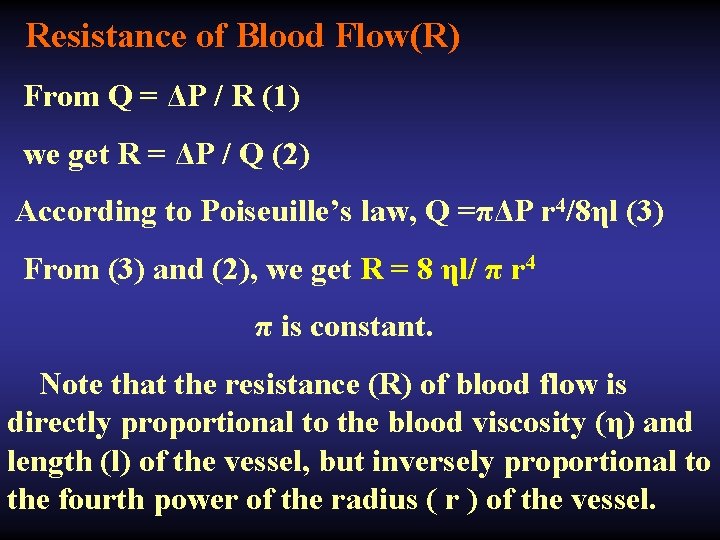
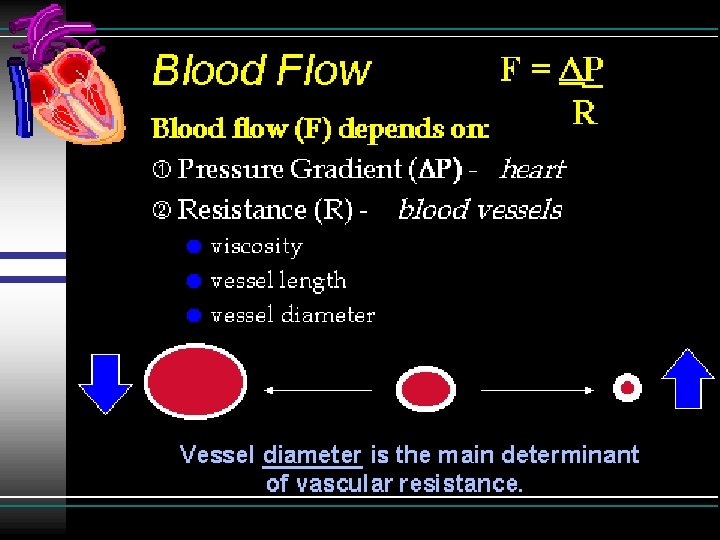
(2) Factors determining blood flow (interrelationships among blood flow, pressure and resistance. ) 1) ΔP: the pressure difference between the two ends of the vessels; 2) R: frictional force produced when blood flows through blood vessels. Q = ΔP / R Poiseuille’s law, Q =πΔP r 4/8ηl
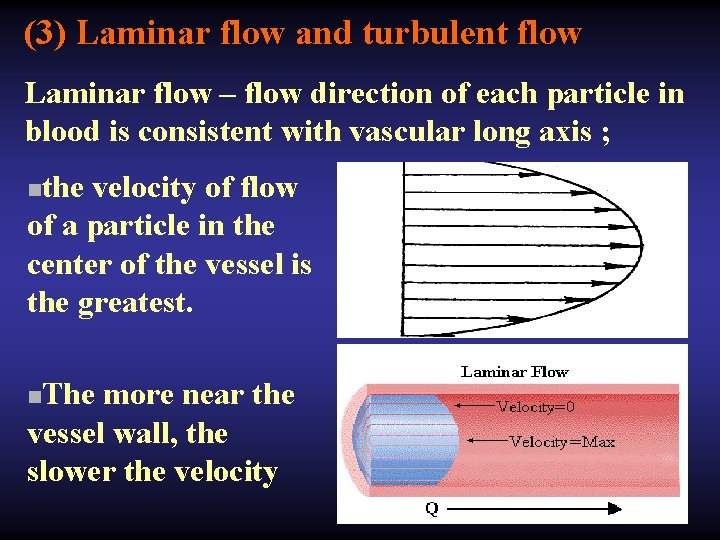
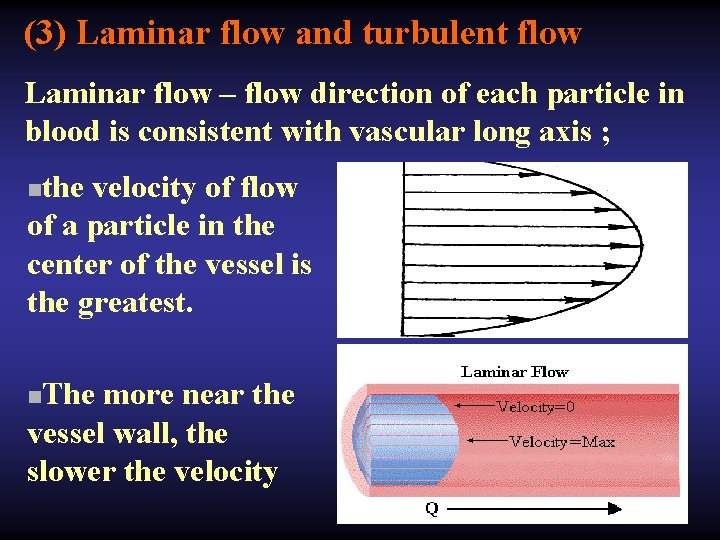
(3) Laminar flow and turbulent flow Laminar flow – flow direction of each particle in blood is consistent with vascular long axis ; the velocity of flow of a particle in the center of the vessel is the greatest. n The more near the vessel wall, the slower the velocity n
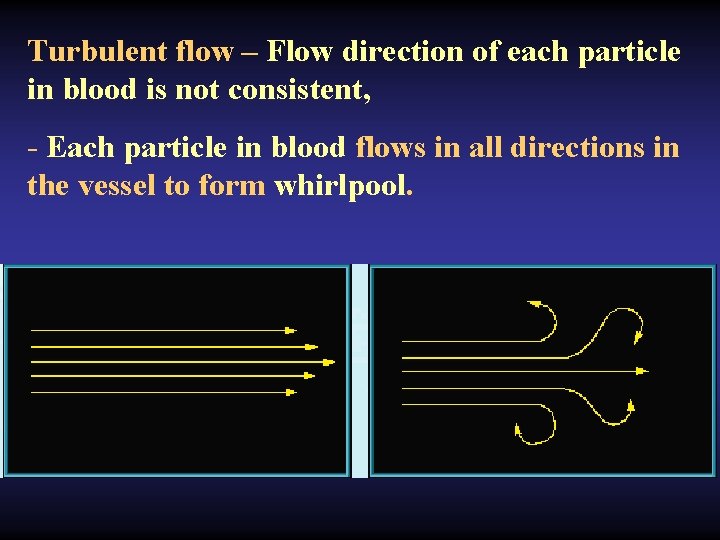
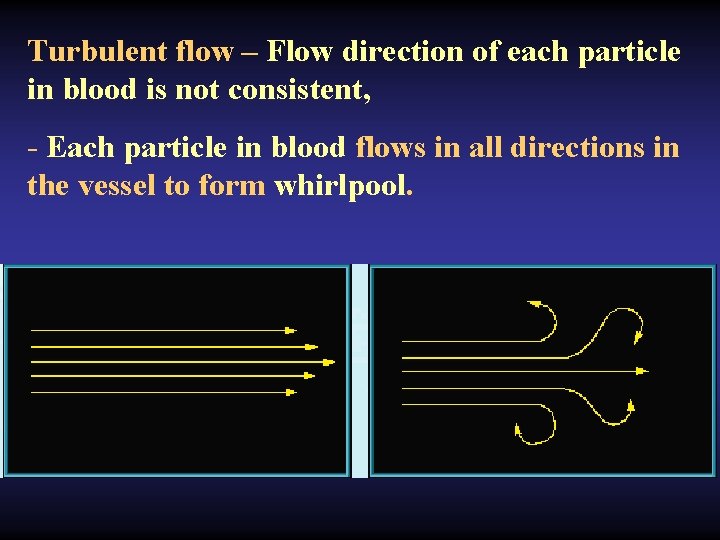
Turbulent flow – Flow direction of each particle in blood is not consistent, - Each particle in blood flows in all directions in the vessel to form whirlpool.
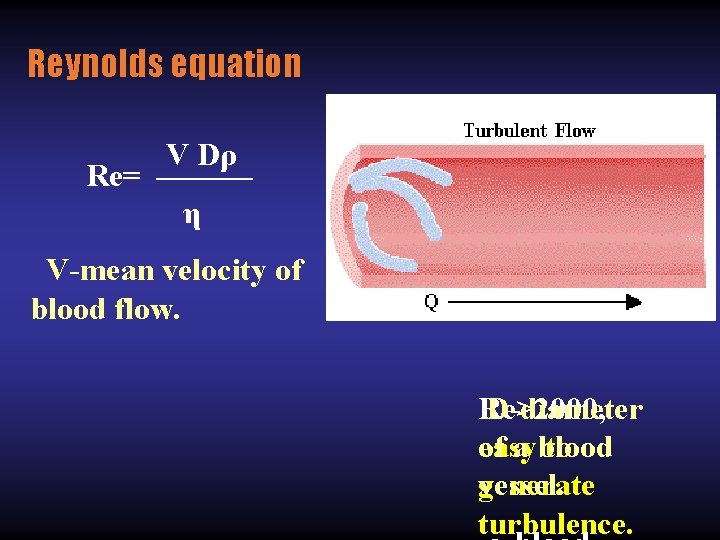
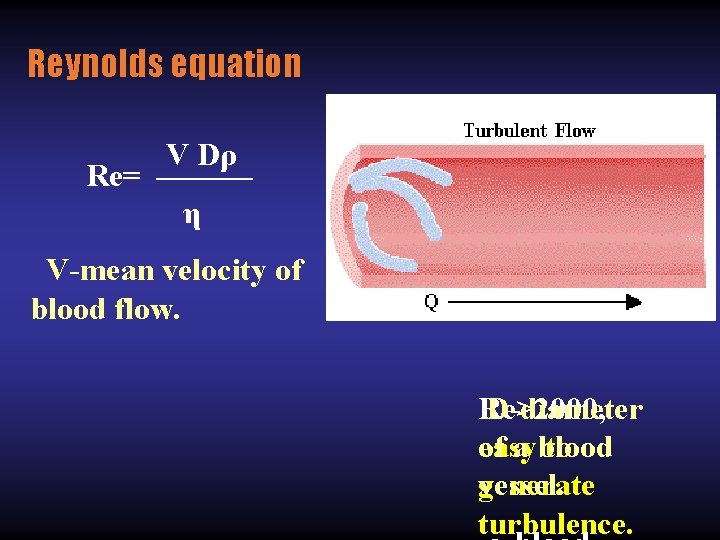
Reynolds equation V Dρ Re= ——— η V-mean velocity of blood flow. D-diameter Re>2000, of a blood easy to vessel. generate turbulence.
2. Resistance of Blood Flow(R) -Blood flowing within the vessel encountered resistance. -Friction between blood and blood vessel, and friction between blood components. - R of turbulent flow is greater than that in laminar flow.
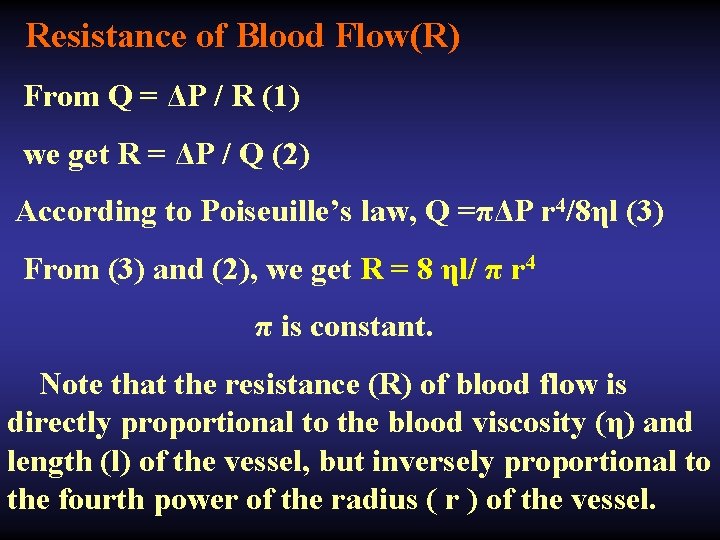
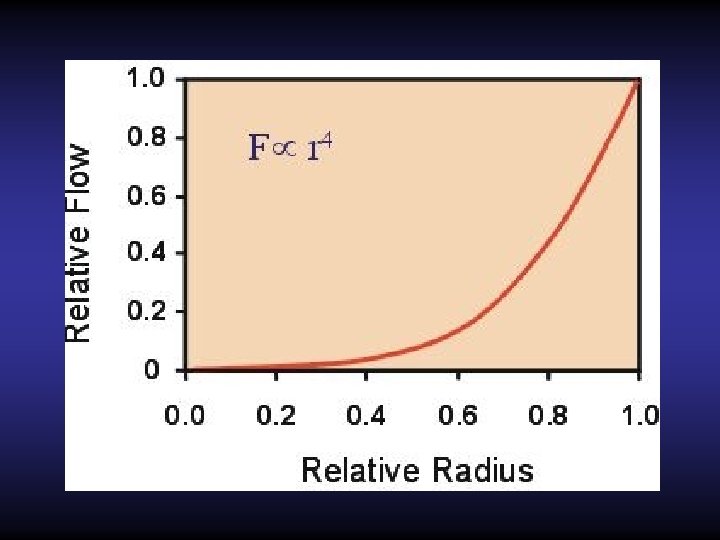
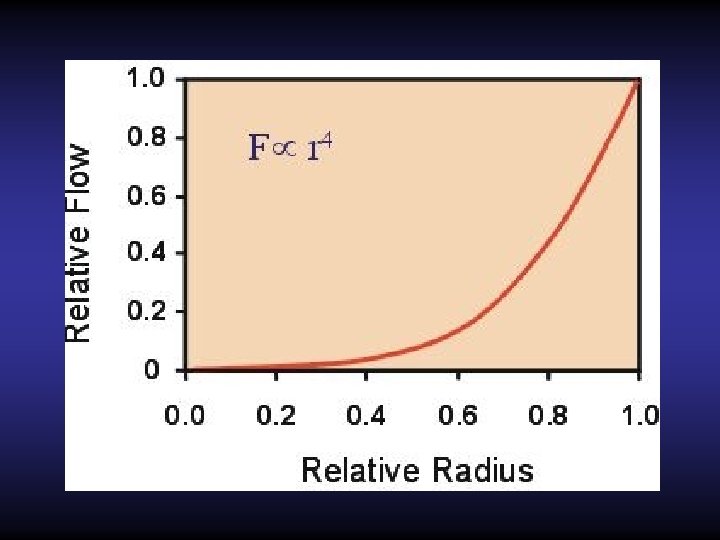
Resistance of Blood Flow(R) From Q = ΔP / R (1) we get R = ΔP / Q (2) According to Poiseuille’s law, Q =πΔP r 4/8ηl (3) From (3) and (2), we get R = 8 ηl/ π r 4 π is constant. Note that the resistance (R) of blood flow is directly proportional to the blood viscosity (η) and length (l) of the vessel, but inversely proportional to the fourth power of the radius ( r ) of the vessel.
Normally, L and η have no change or almost no change. Therefore, the radius of a blood vessel plays the greatest role in determining the resistance ( R ) of blood flow.
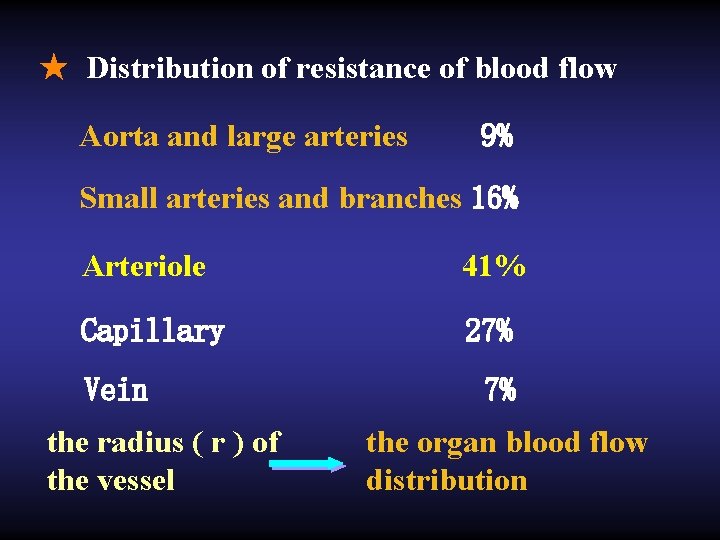
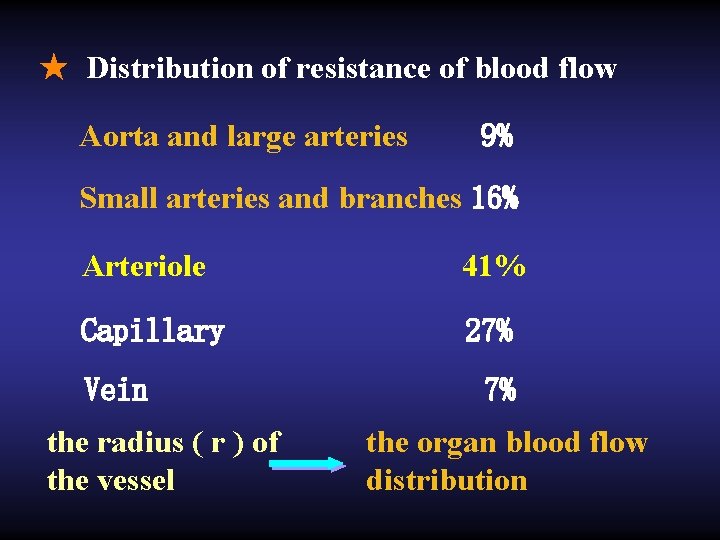
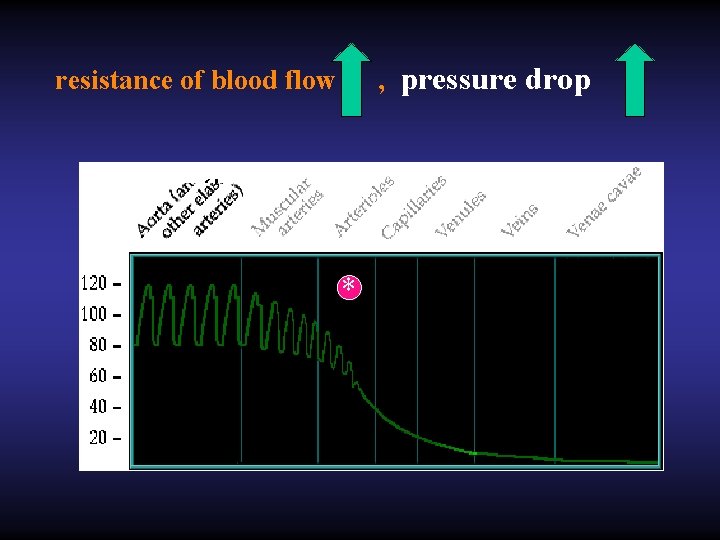
★ Distribution of resistance of blood flow Aorta and large arteries 9% Small arteries and branches 16% Arteriole 41% Capillary 27% Vein the radius ( r ) of the vessel 7% the organ blood flow distribution
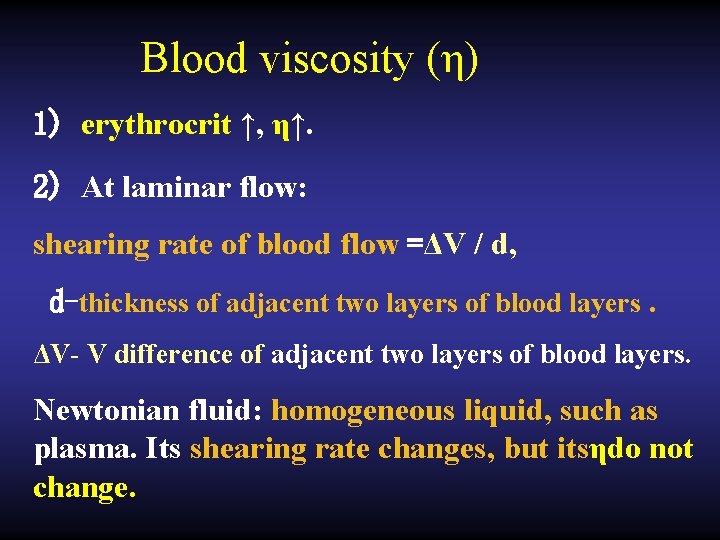
Blood viscosity (η) 1) erythrocrit ↑, η↑. 2) At laminar flow: shearing rate of blood flow =ΔV / d, d-thickness of adjacent two layers of blood layers. ΔV- V difference of adjacent two layers of blood layers. Newtonian fluid: homogeneous liquid, such as plasma. Its shearing rate changes, but itsηdo not change.
Non-Newtonian fluid: Non homogeneous liquid, such as blood. Its shearing rate changes ↓, its η↑. Axial flow- when blood flows in the form of laminar flow, red cells have a trend of moving to central axis. When shearing rate is higher, axial flow phenomenon is more obvious, its η is lower.
3) Calibre of blood vessel: Fahraeus-Lindqvist effect. If calibre of blood vessel is smaller than 0. 2~0. 3 mm, shearing rate of blood is enough high, within a certain range, decrease inηaccompanys with calibre of blood vessel becoming smaller. 4)Temperature ↓, η↑.
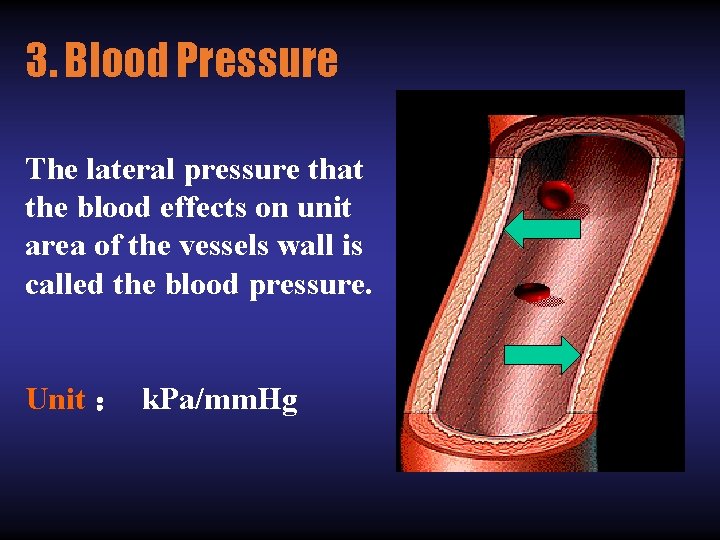
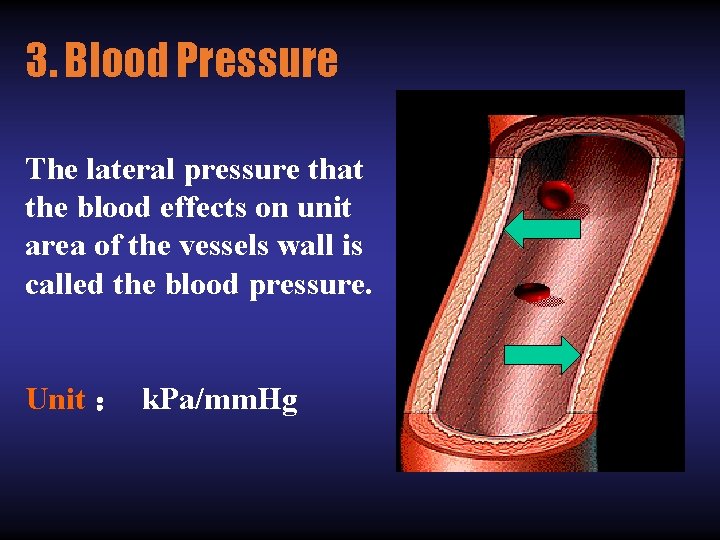
3. Blood Pressure The lateral pressure that the blood effects on unit area of the vessels wall is called the blood pressure. Unit : k. Pa/mm. Hg
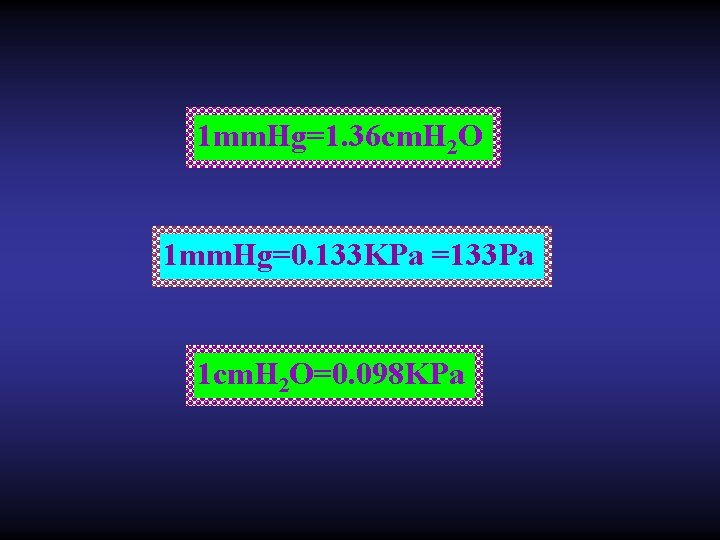
1 mm. Hg=1. 36 cm. H 2 O 1 mm. Hg=0. 133 KPa =133 Pa 1 cm. H 2 O=0. 098 KPa
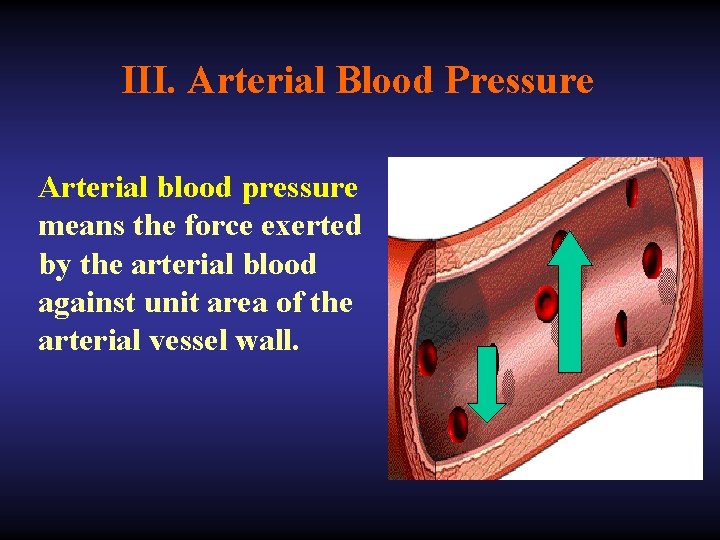
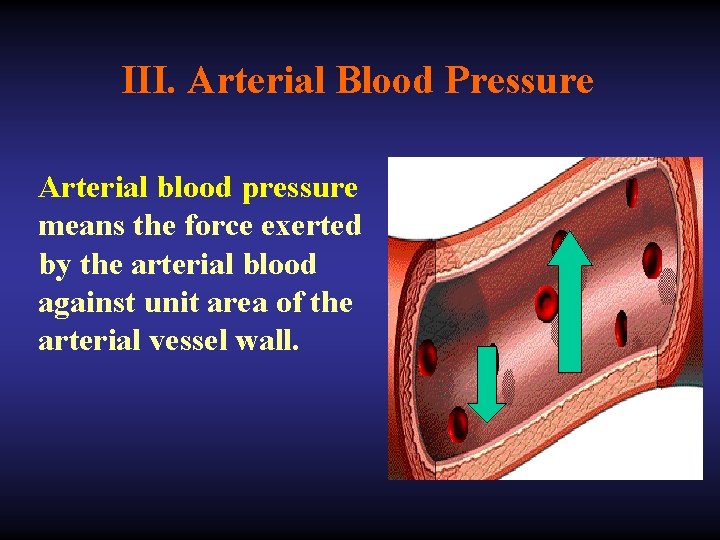
III. Arterial Blood Pressure Arterial blood pressure means the force exerted by the arterial blood against unit area of the arterial vessel wall.
Formation Of Arterial Pressure Conditions: + There is a enough blood in the cardiovascular system. + cardiac pumping and peripheral resistance + windkessel of aorta and big arteries
+ There is a enough blood in the cardiovascular system. Mean circulatory filling pressure (MCFP): when heart beat is stopped, the pressure in any point of cardiovascular system is equal. This pressure is called MCFP. systemic circulation, 7 mm. Hg; pulmonary circulation, 10 mm. Hg.
+ cardiac pumping and peripheral resistance Energy released from heart contraction is transferred into two parts, 1) kinetic energy (1% of the total), 2) 2) potential energy (pressure) (99% of the total). 3) That means most part of energy used to create the blood pressure. There is a resistance of blood flow in the blood vessels, especially in small arteries and arterioles.
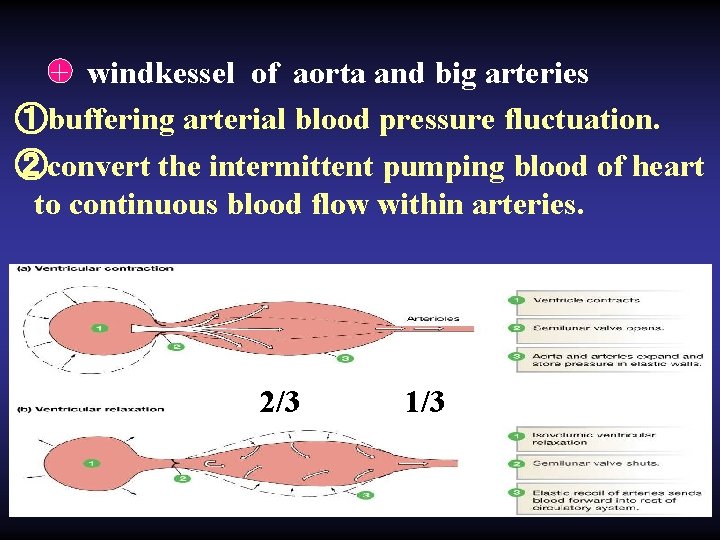
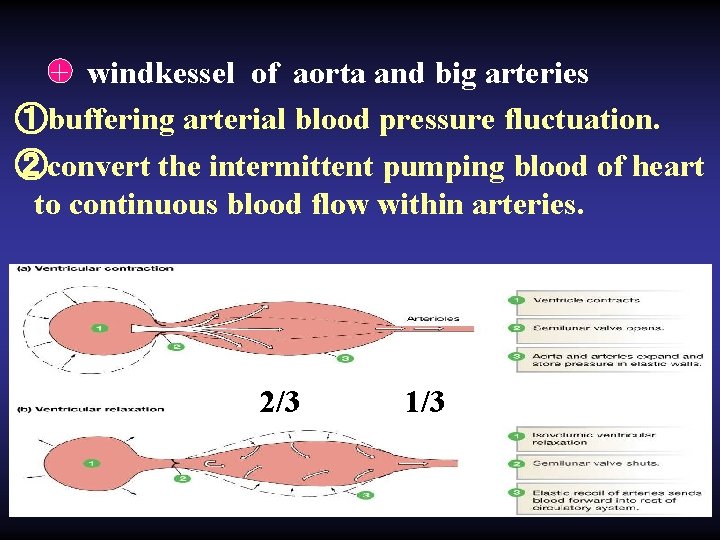
+ windkessel of aorta and big arteries ①buffering arterial blood pressure fluctuation. ②convert the intermittent pumping blood of heart to continuous blood flow within arteries. 2/3 1/3
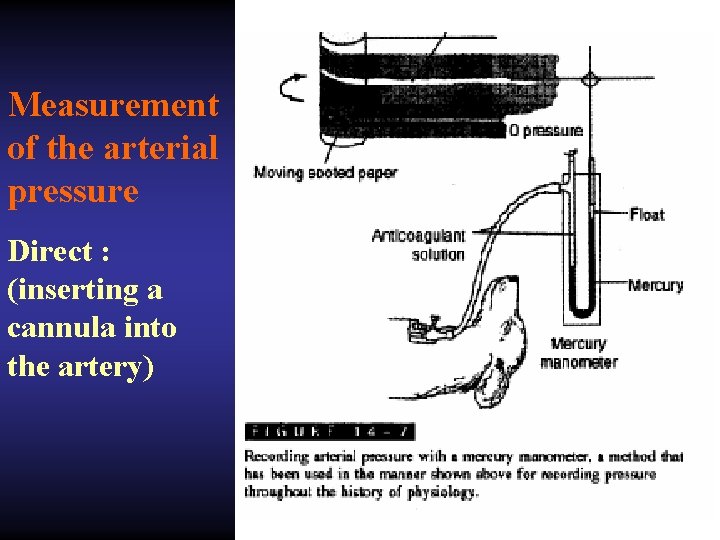
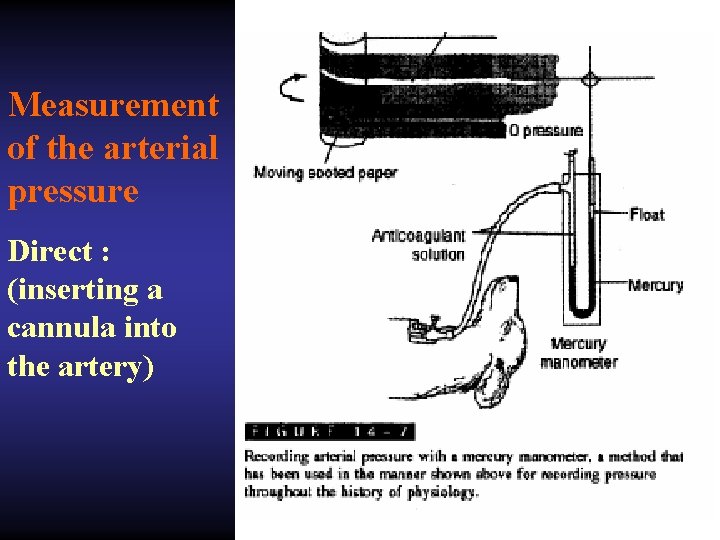
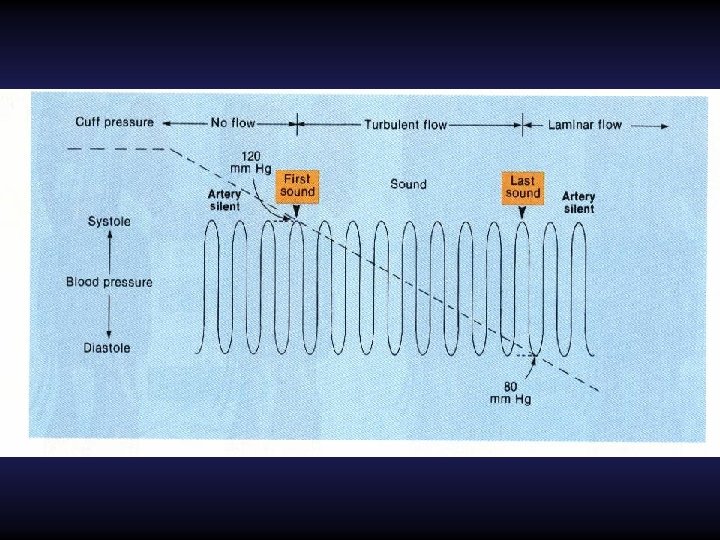
Measurement of the arterial pressure Direct : (inserting a cannula into the artery)
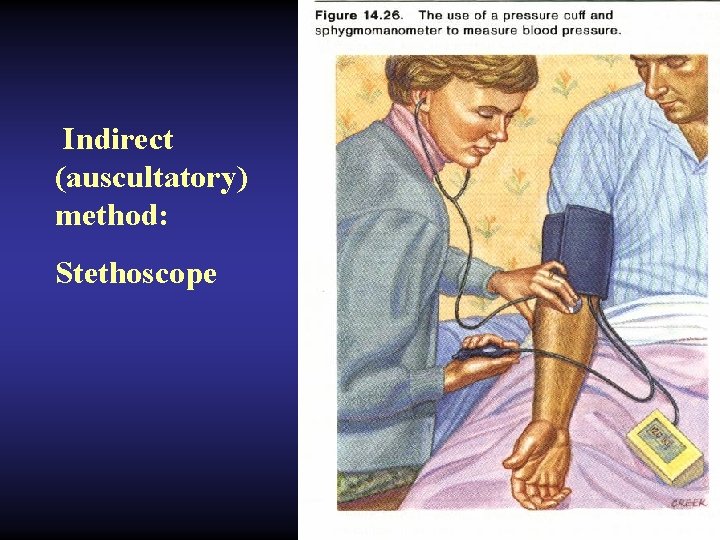
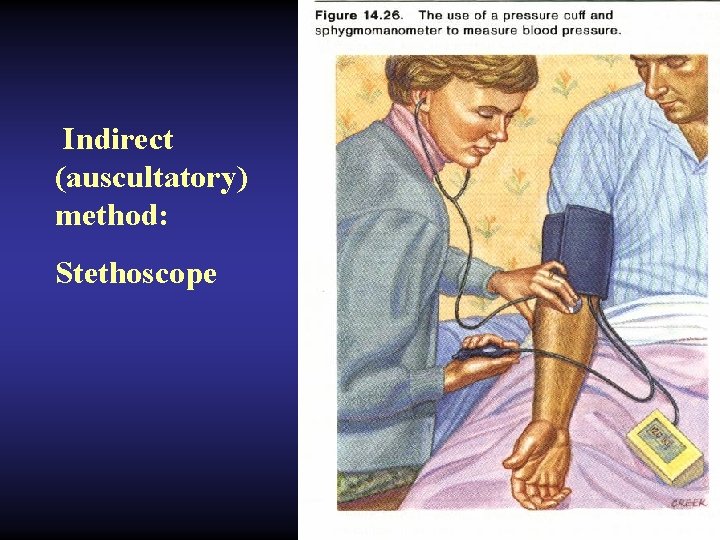
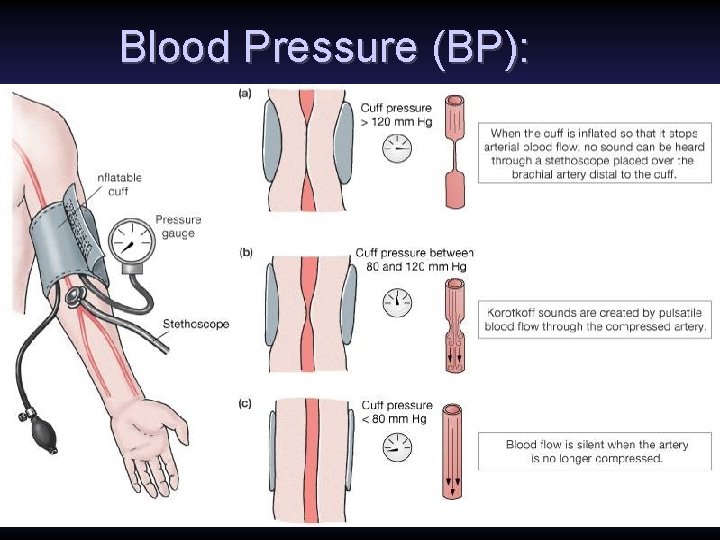
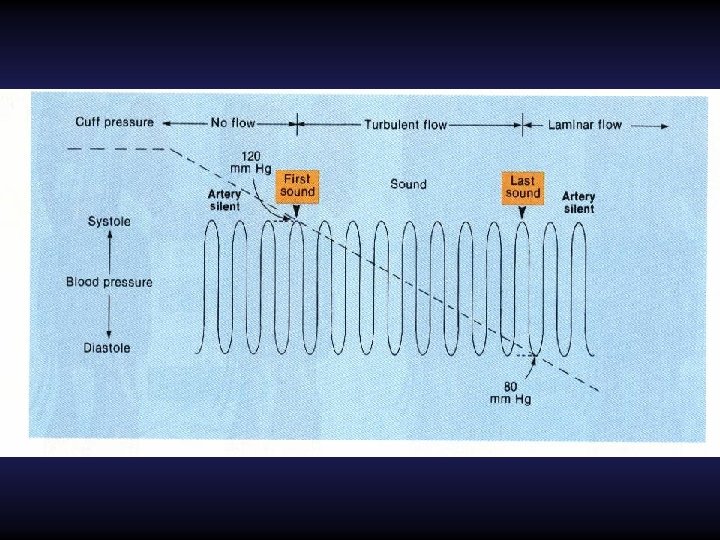
Indirect (auscultatory) method: Stethoscope
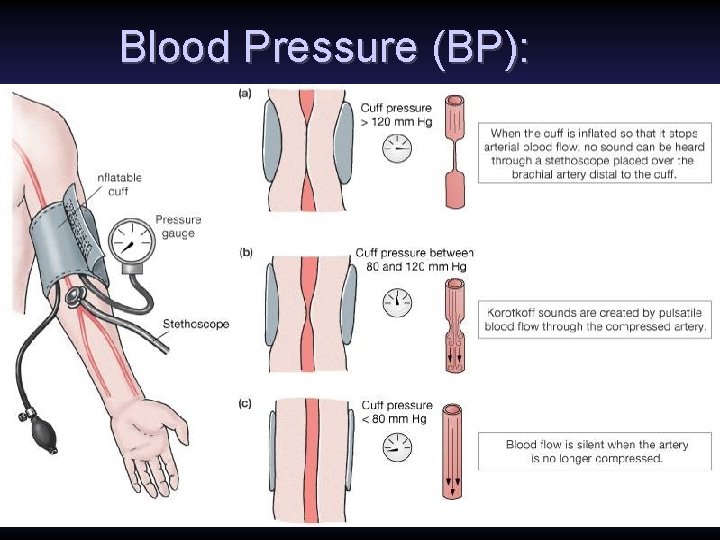
Blood Pressure (BP):
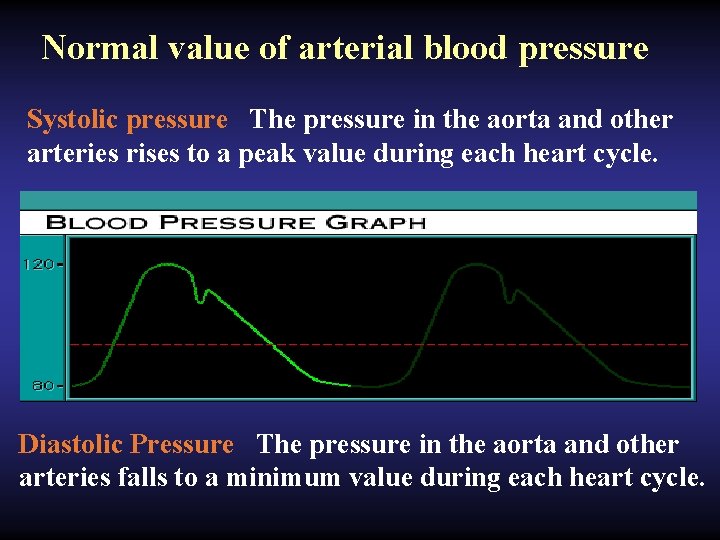
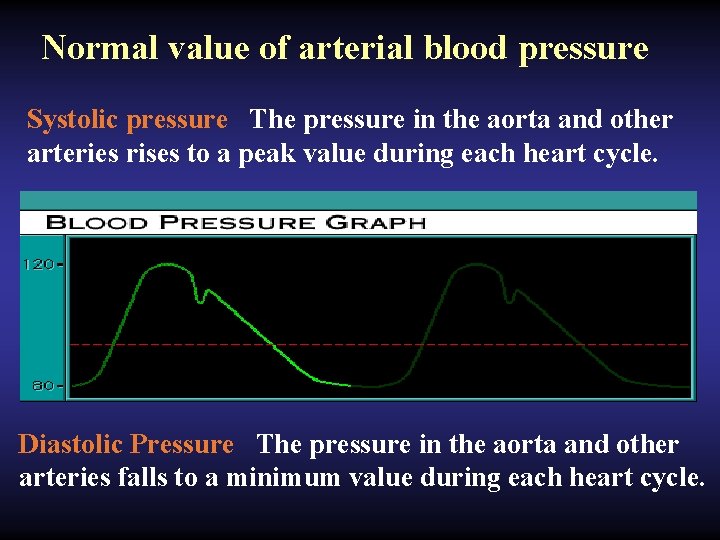
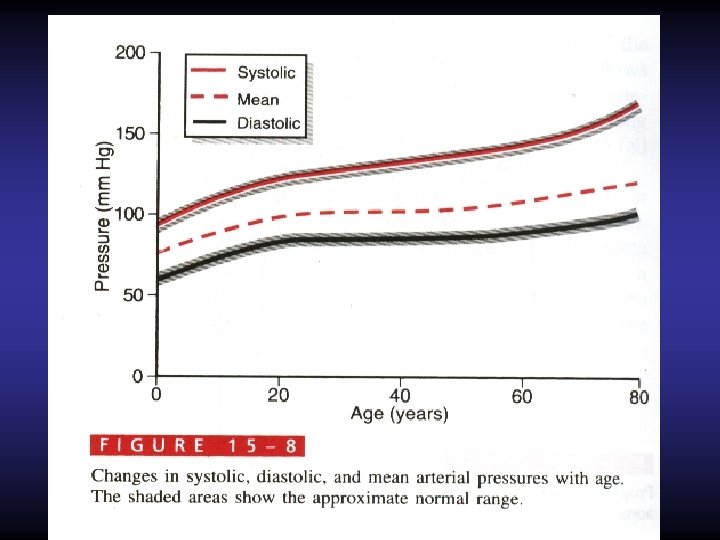
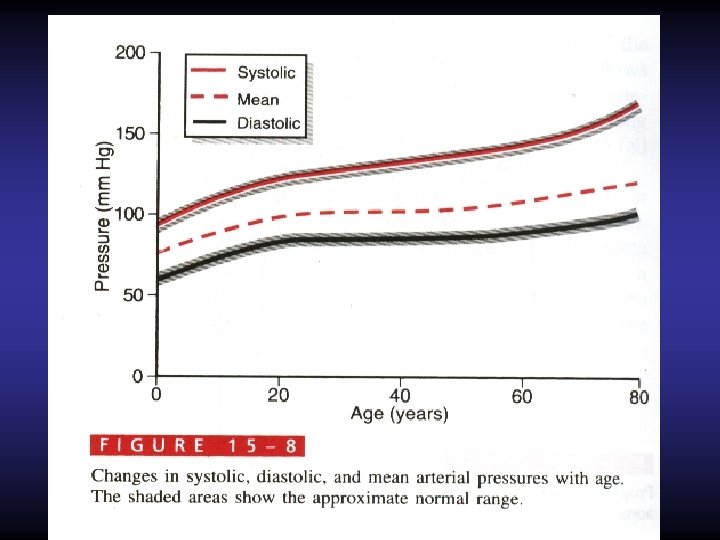
Normal value of arterial blood pressure Systolic pressure The pressure in the aorta and other arteries rises to a peak value during each heart cycle. Diastolic Pressure The pressure in the aorta and other arteries falls to a minimum value during each heart cycle.
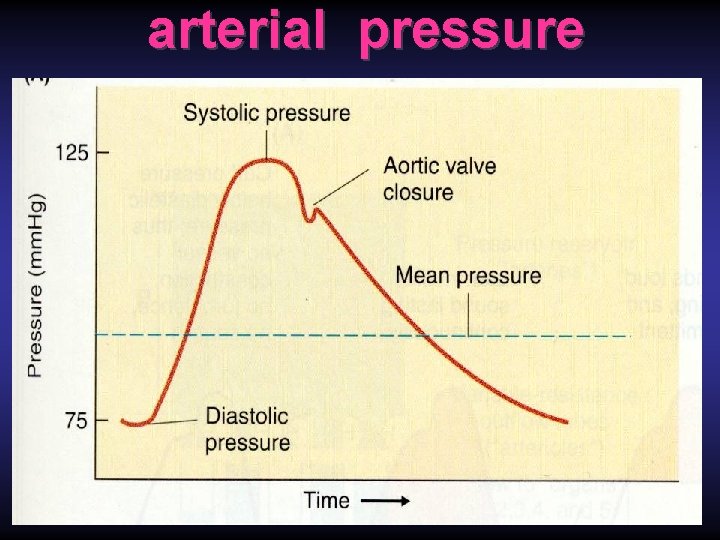
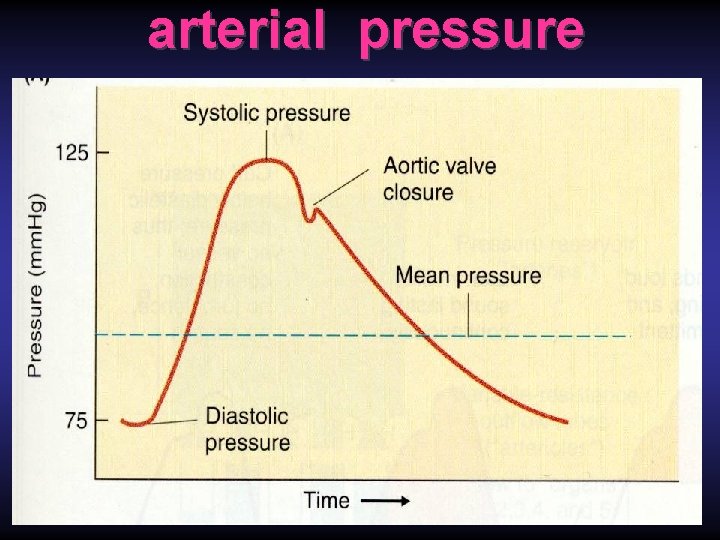
arterial pressure
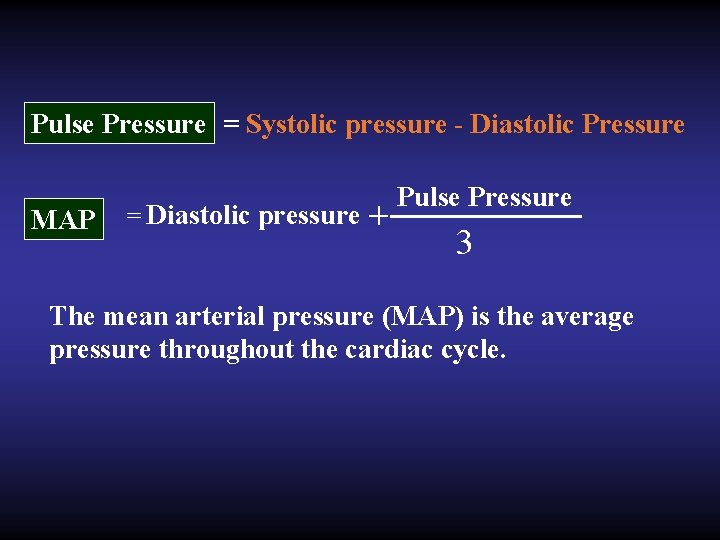
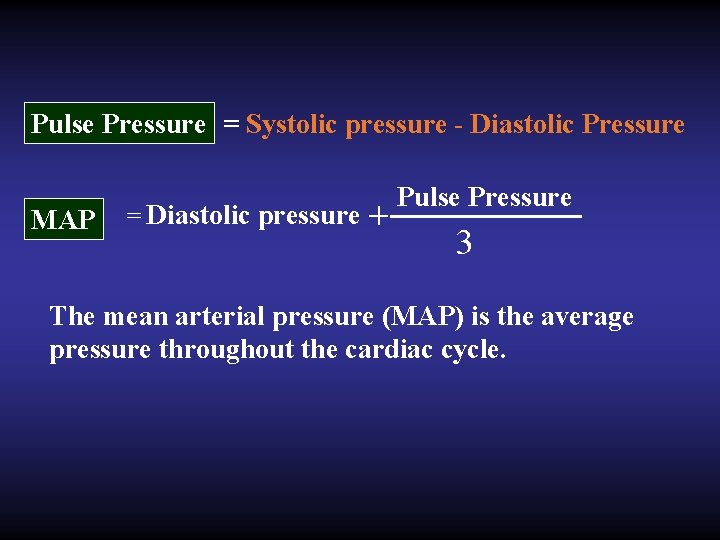
Pulse Pressure = Systolic pressure - Diastolic Pressure MAP = Diastolic pressure + Pulse Pressure 3 The mean arterial pressure (MAP) is the average pressure throughout the cardiac cycle.
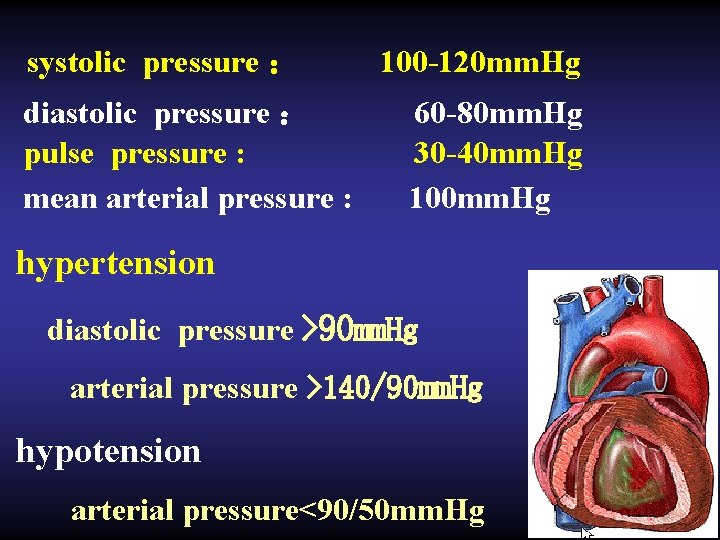
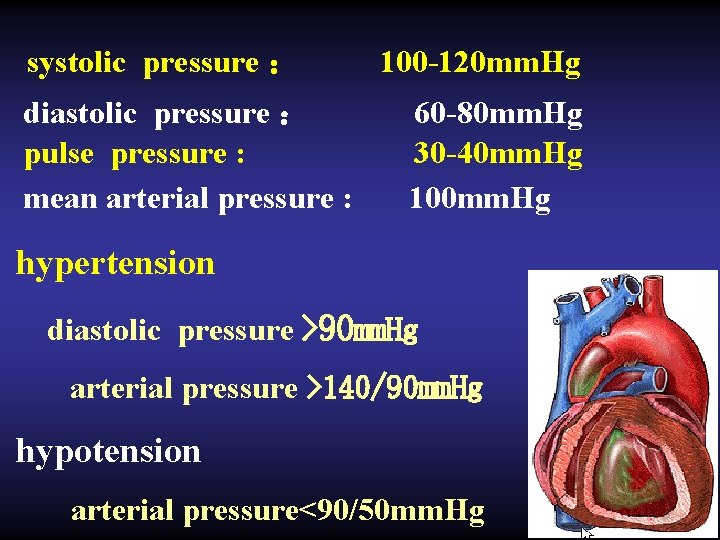
systolic pressure : diastolic pressure : pulse pressure : mean arterial pressure : 100 -120 mm. Hg 60 -80 mm. Hg 30 -40 mm. Hg 100 mm. Hg hypertension diastolic pressure >90 mm. Hg arterial pressure >140/90 mm. Hg hypotension arterial pressure<90/50 mm. Hg
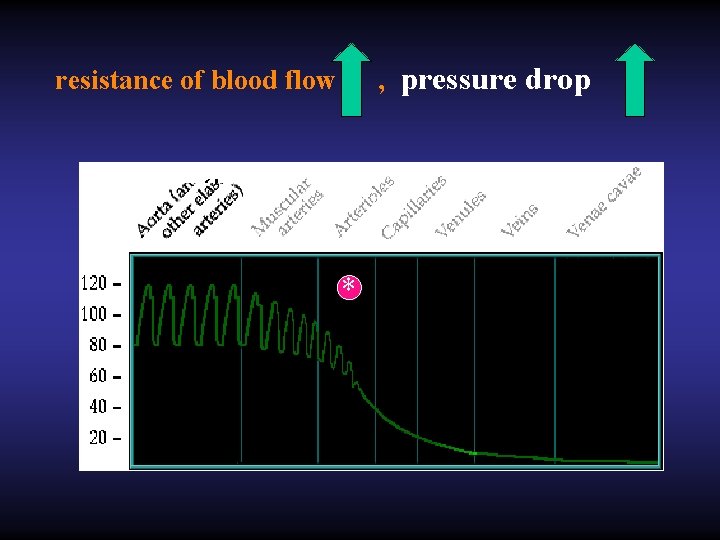
, pressure drop resistance of blood flow *
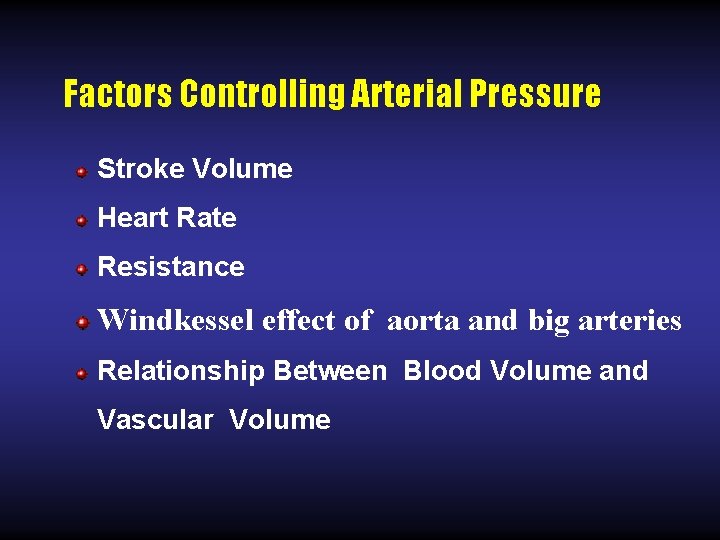
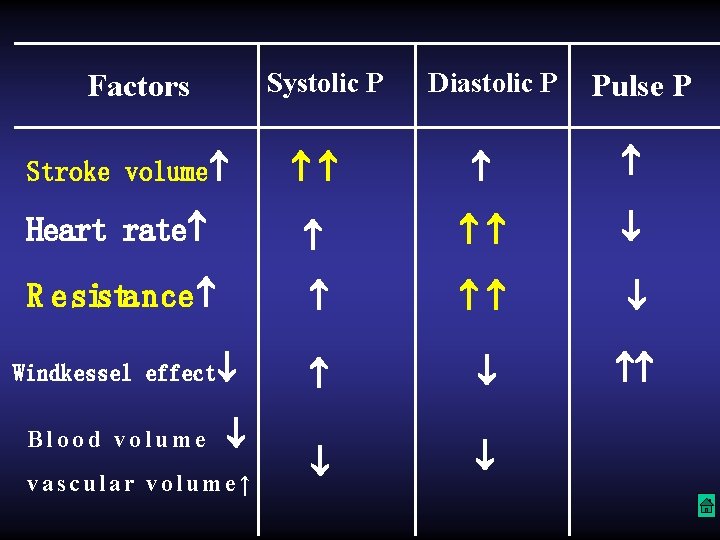
Factors Controlling Arterial Pressure Stroke Volume Heart Rate Resistance Windkessel effect of aorta and big arteries Relationship Between Blood Volume and Vascular Volume
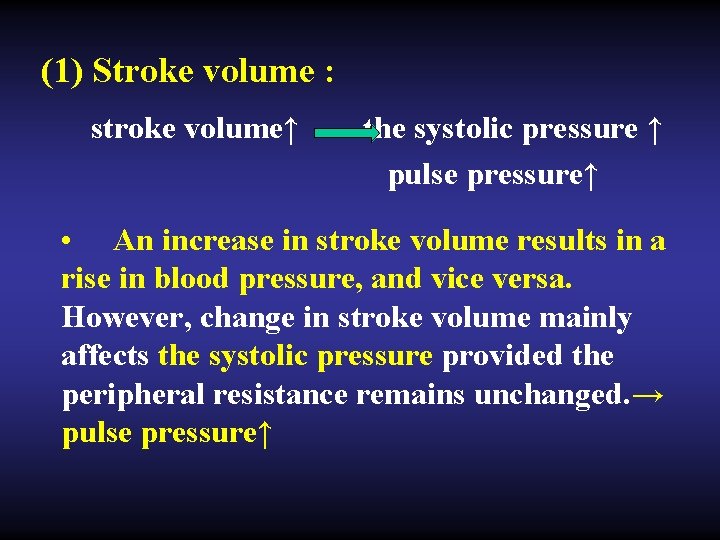
(1) Stroke volume : stroke volume↑ the systolic pressure ↑ pulse pressure↑ • An increase in stroke volume results in a rise in blood pressure, and vice versa. However, change in stroke volume mainly affects the systolic pressure provided the peripheral resistance remains unchanged. → pulse pressure↑
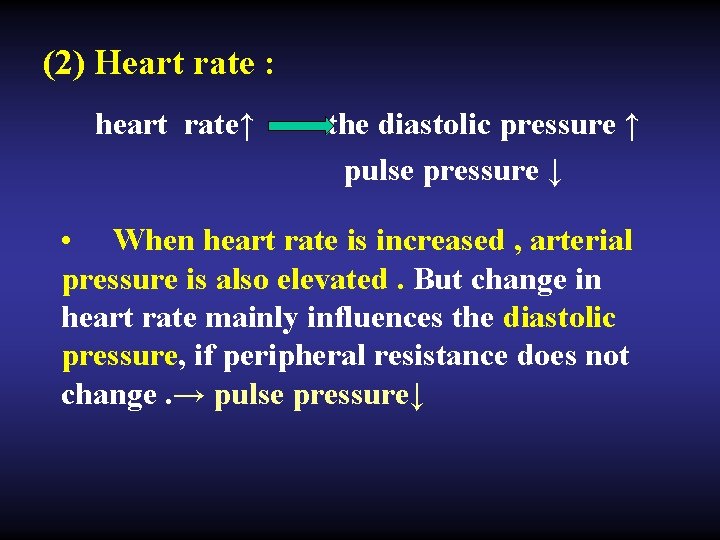
(2) Heart rate : heart rate↑ the diastolic pressure ↑ pulse pressure ↓ • When heart rate is increased , arterial pressure is also elevated. But change in heart rate mainly influences the diastolic pressure, if peripheral resistance does not change. → pulse pressure↓
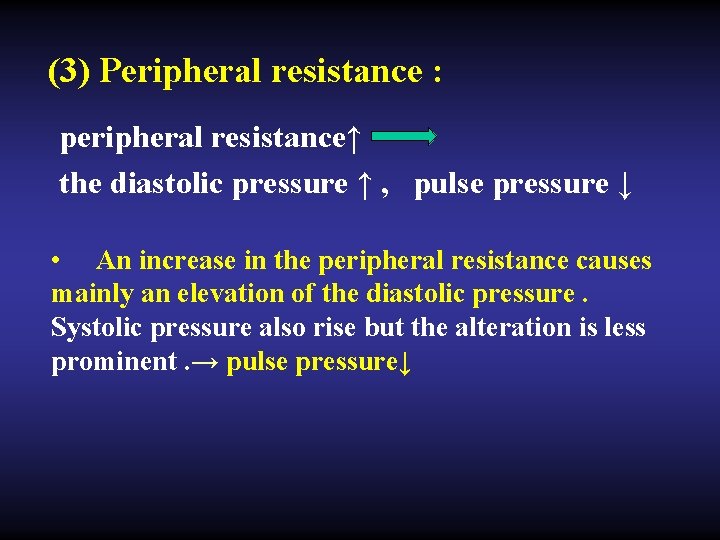
(3) Peripheral resistance : peripheral resistance↑ the diastolic pressure ↑ , pulse pressure ↓ • An increase in the peripheral resistance causes mainly an elevation of the diastolic pressure. Systolic pressure also rise but the alteration is less prominent. → pulse pressure↓
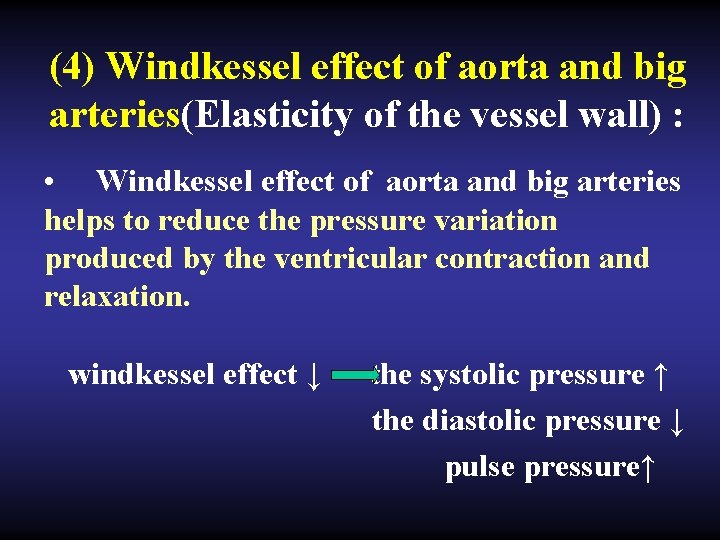
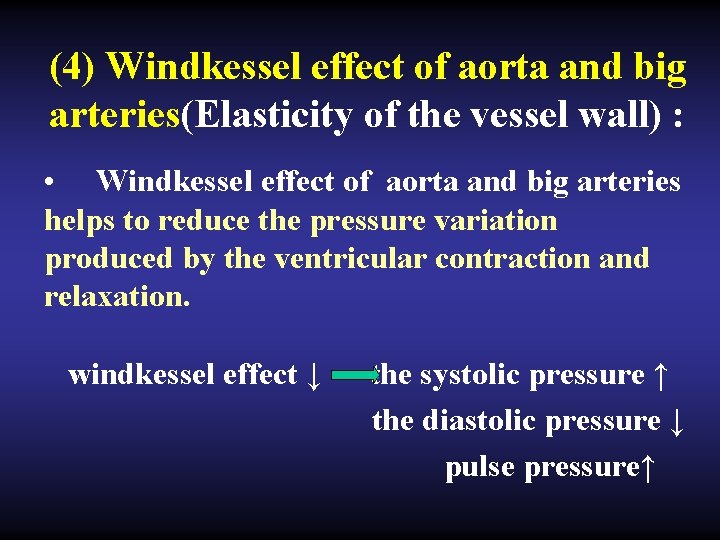
(4) Windkessel effect of aorta and big arteries(Elasticity of the vessel wall) : • Windkessel effect of aorta and big arteries helps to reduce the pressure variation produced by the ventricular contraction and relaxation. windkessel effect ↓ the systolic pressure ↑ the diastolic pressure ↓ pulse pressure↑
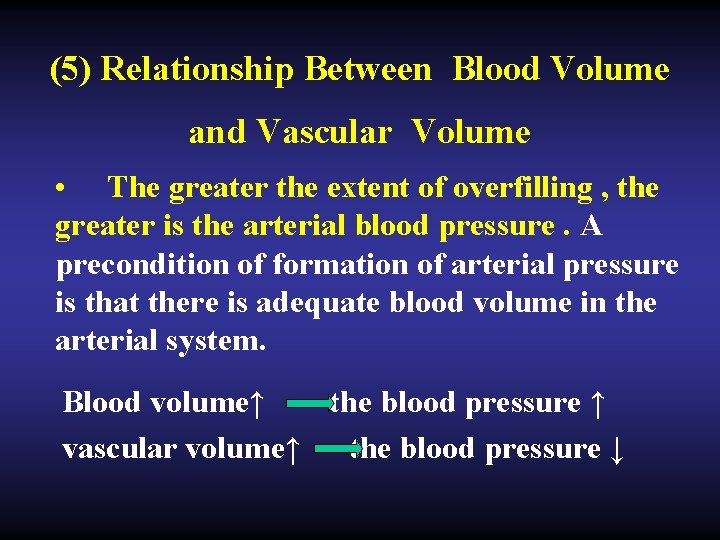
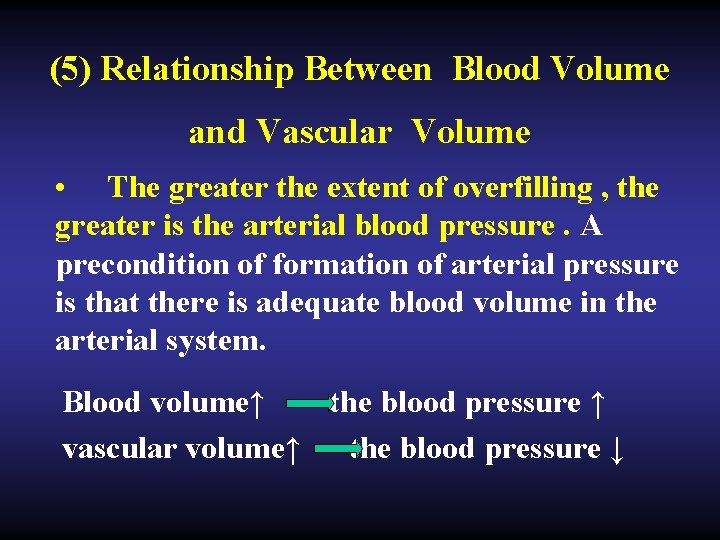
(5) Relationship Between Blood Volume and Vascular Volume • The greater the extent of overfilling , the greater is the arterial blood pressure. A precondition of formation of arterial pressure is that there is adequate blood volume in the arterial system. Blood volume↑ the blood pressure ↑ vascular volume↑ the blood pressure ↓
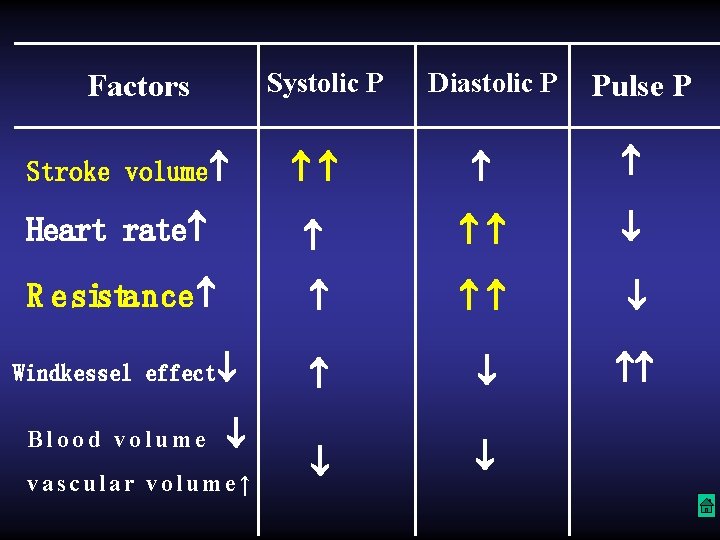
Systolic P Factors Diastolic P Pulse P Heart rate R esistance Windkessel effect Stroke volume Blood volume vascular volume↑
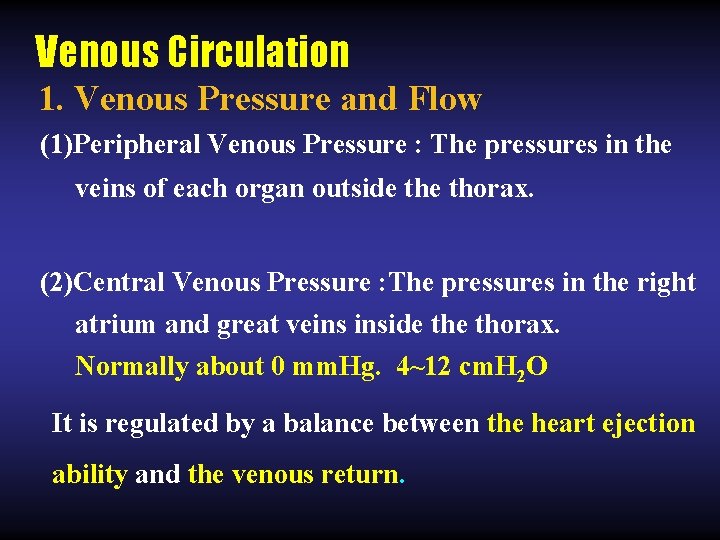
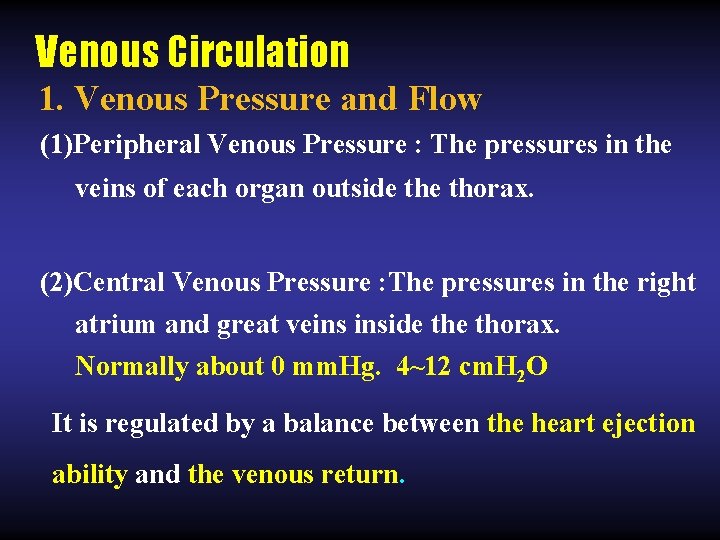
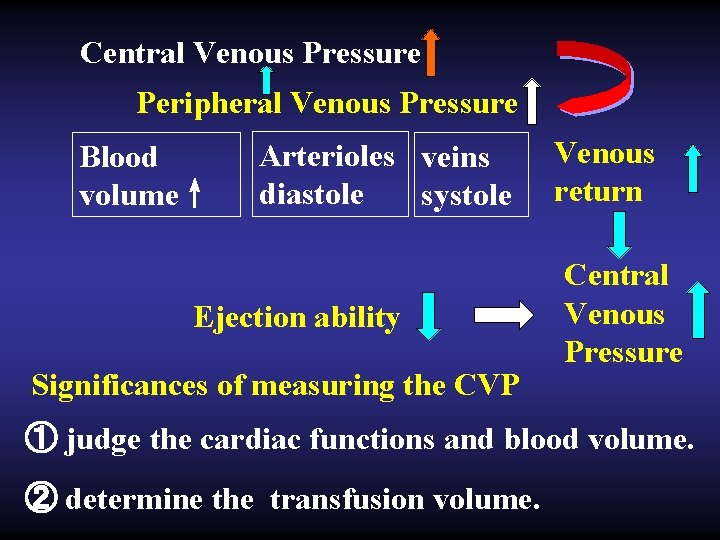
Venous Circulation 1. Venous Pressure and Flow (1)Peripheral Venous Pressure : The pressures in the veins of each organ outside thorax. (2)Central Venous Pressure : The pressures in the right atrium and great veins inside thorax. Normally about 0 mm. Hg. 4~12 cm. H 2 O It is regulated by a balance between the heart ejection ability and the venous return.
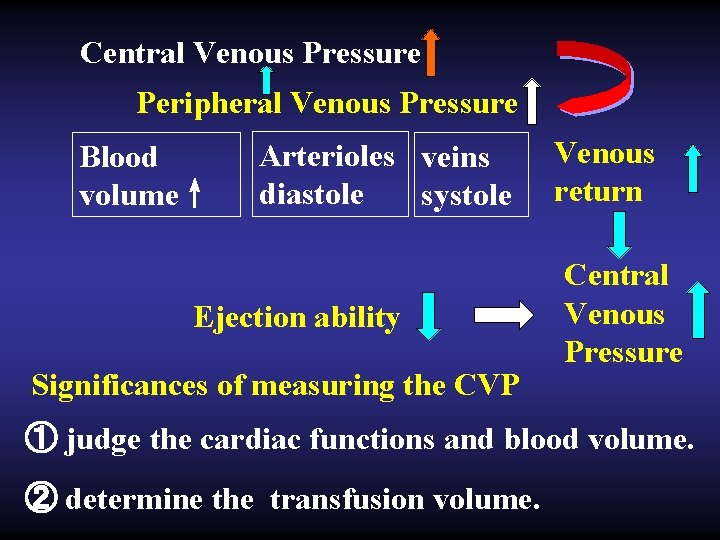
Central Venous Pressure Peripheral Venous Pressure Blood volume↑ Arterioles veins diastole systole Ejection ability Significances of measuring the CVP Venous return Central Venous Pressure ① judge the cardiac functions and blood volume. ② determine the transfusion volume.
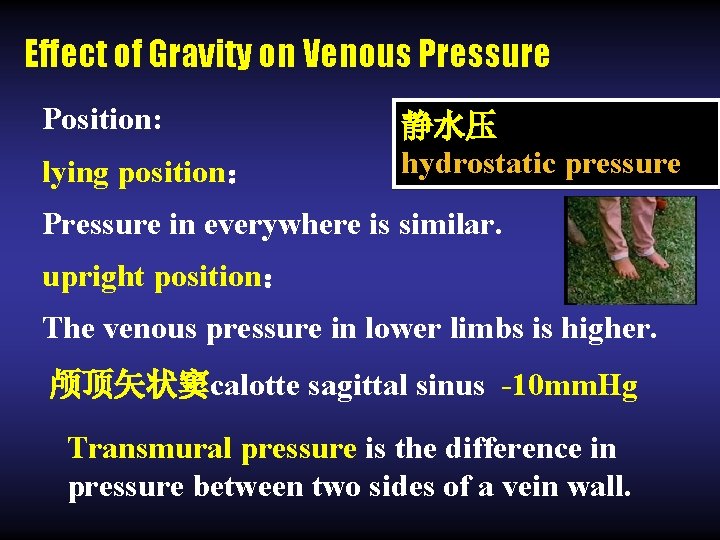
Effect of Gravity on Venous Pressure Position: lying position: 静水压 hydrostatic pressure Pressure in everywhere is similar. upright position: The venous pressure in lower limbs is higher. 颅顶矢状窦calotte sagittal sinus -10 mm. Hg Transmural pressure is the difference in pressure between two sides of a vein wall.
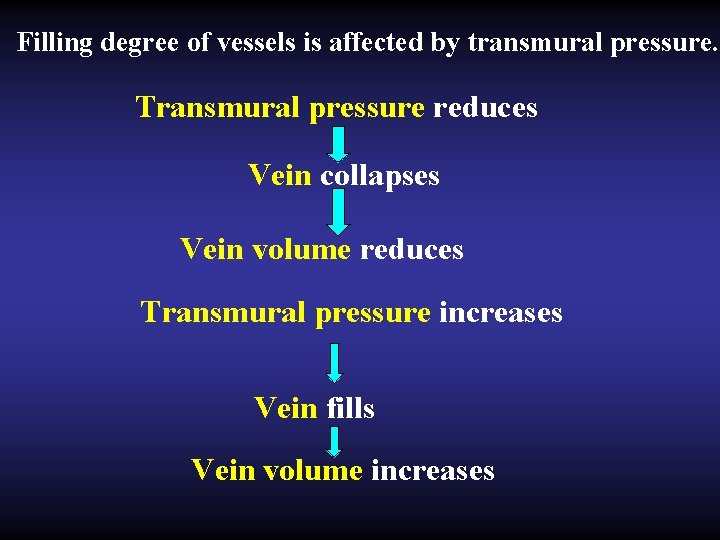
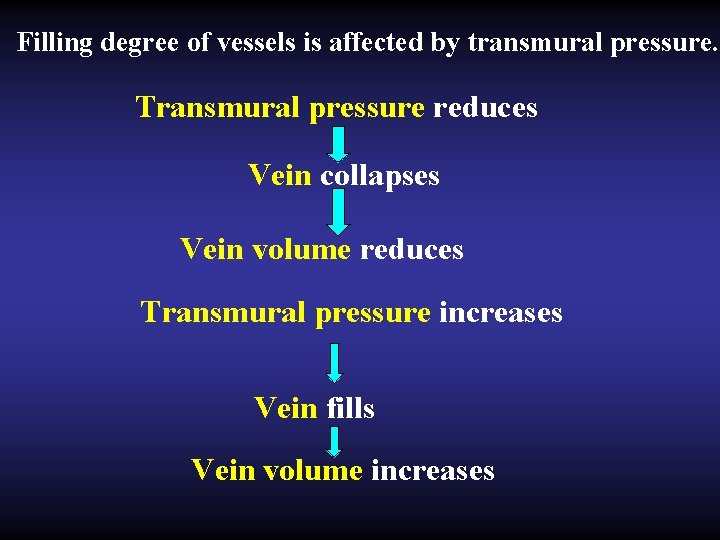
Filling degree of vessels is affected by transmural pressure. Transmural pressure reduces Vein collapses Vein volume reduces Transmural pressure increases Vein fills Vein volume increases
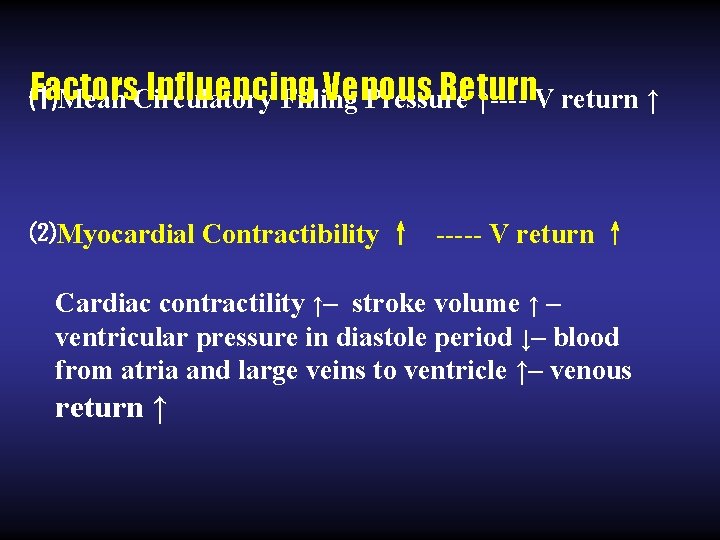
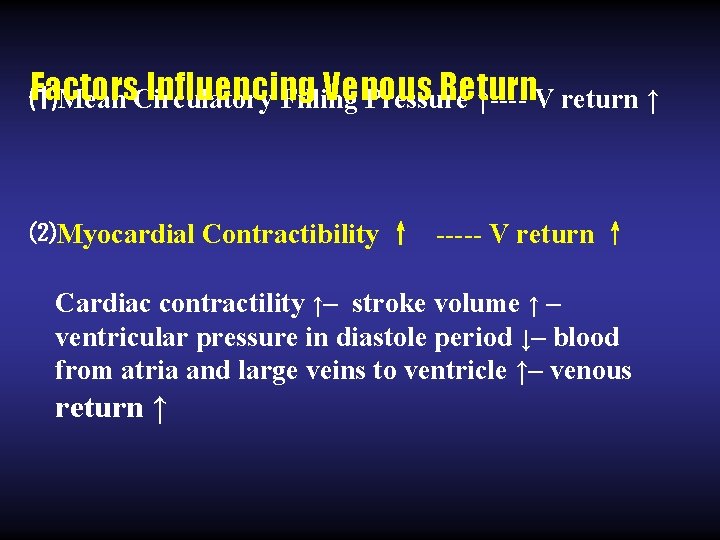
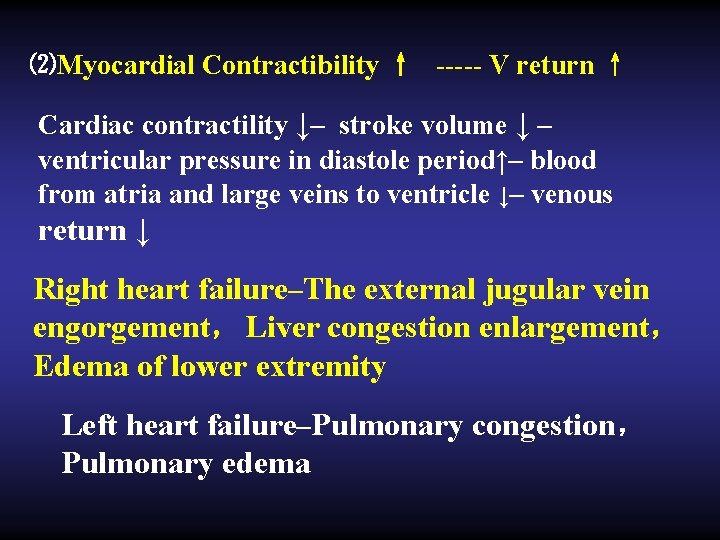
Factors. Circulatory Influencing Venous Return ⑴Mean Filling Pressure ↑---- V return ↑ ⑵Myocardial Contractibility ↑ ----- V return ↑ Cardiac contractility ↑– stroke volume ↑ – ventricular pressure in diastole period ↓– blood from atria and large veins to ventricle ↑– venous return ↑
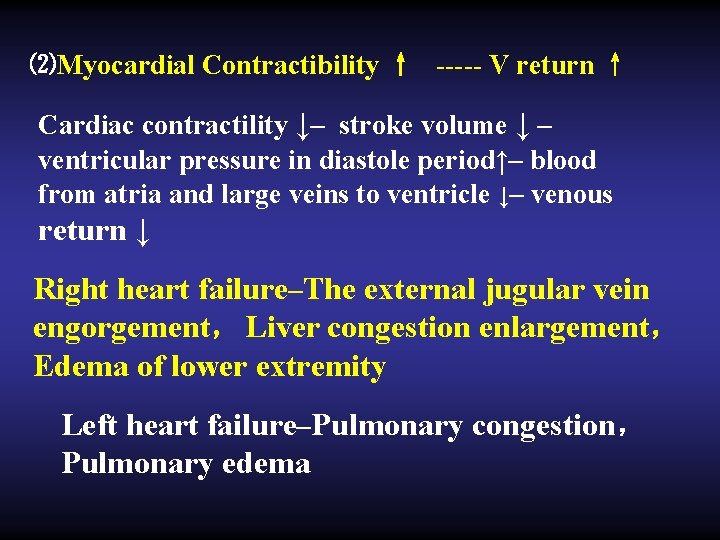
⑵Myocardial Contractibility ↑ ----- V return ↑ Cardiac contractility ↓– stroke volume ↓ – ventricular pressure in diastole period↑– blood from atria and large veins to ventricle ↓– venous return ↓ Right heart failure–The external jugular vein engorgement, Liver congestion enlargement, Edema of lower extremity Left heart failure–Pulmonary congestion, Pulmonary edema
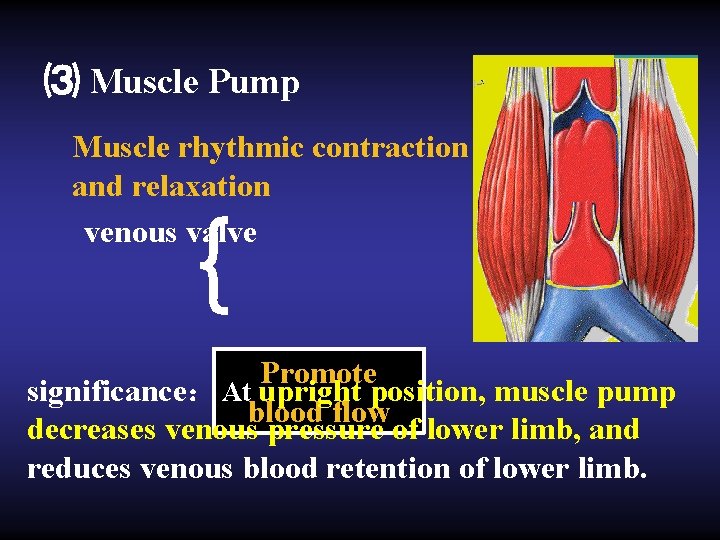
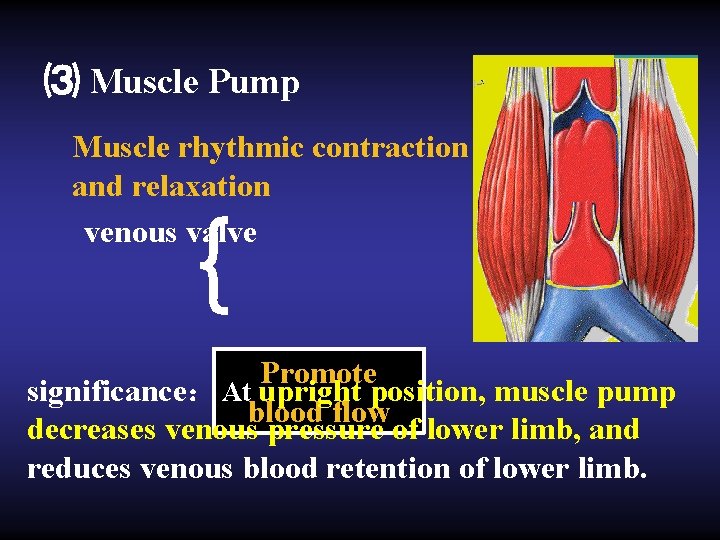
⑶ Muscle Pump Muscle rhythmic contraction and relaxation venous valve { Promote significance: At upright position, muscle pump blood flow decreases venous pressure of lower limb, and reduces venous blood retention of lower limb.
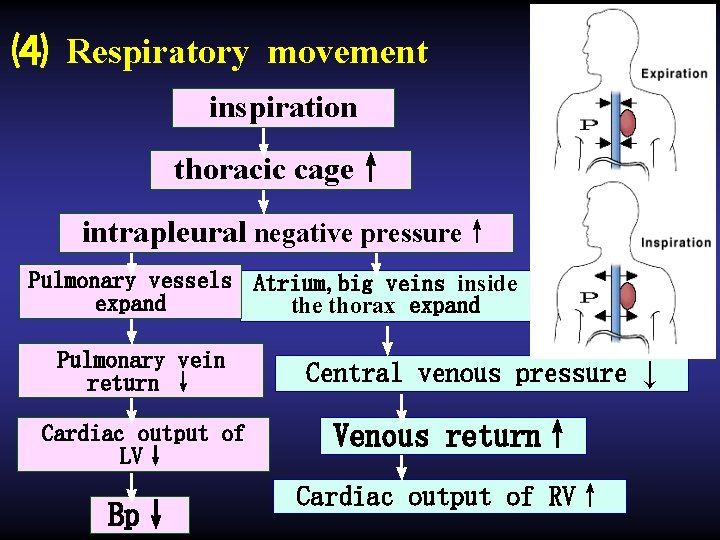
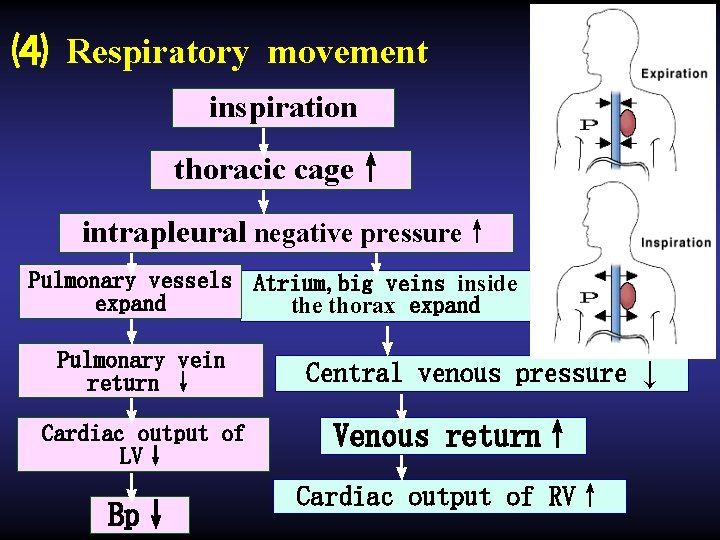
⑷ Respiratory movement inspiration ↓ thoracic cage↑ ↓ intrapleural negative pressure↑ ↓ ↓ Pulmonary vessels expand ↓ Pulmonary vein return ↓ ↓ Cardiac output of LV↓ ↓ Bp↓ Atrium, big veins inside thorax expand ↓ Central venous pressure ↓ ↓ Venous return↑ ↓ Cardiac output of RV↑
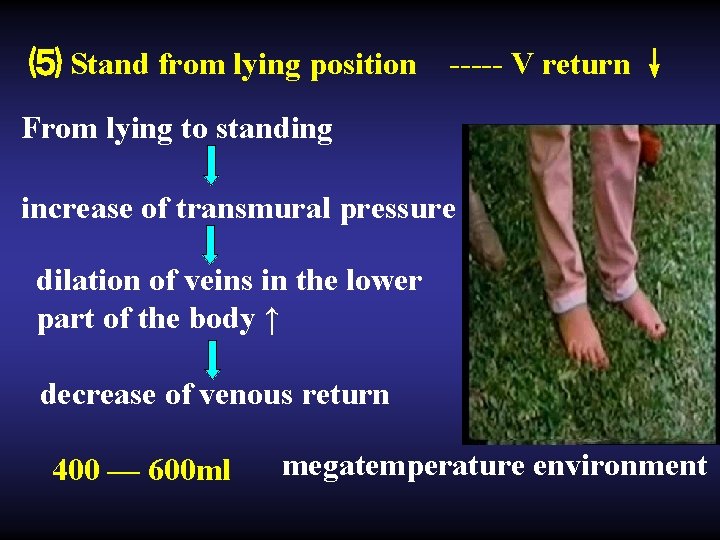
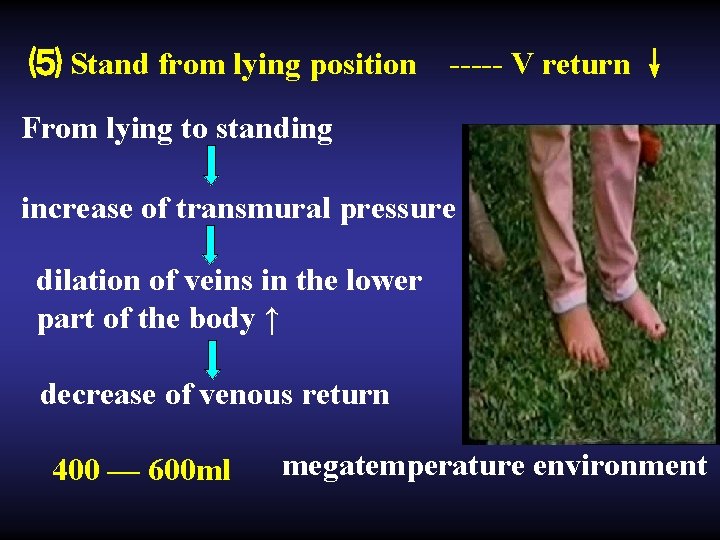
⑸ Stand from lying position ----- V return ↓ From lying to standing increase of transmural pressure dilation of veins in the lower part of the body ↑ decrease of venous return 400 — 600 ml megatemperature environment
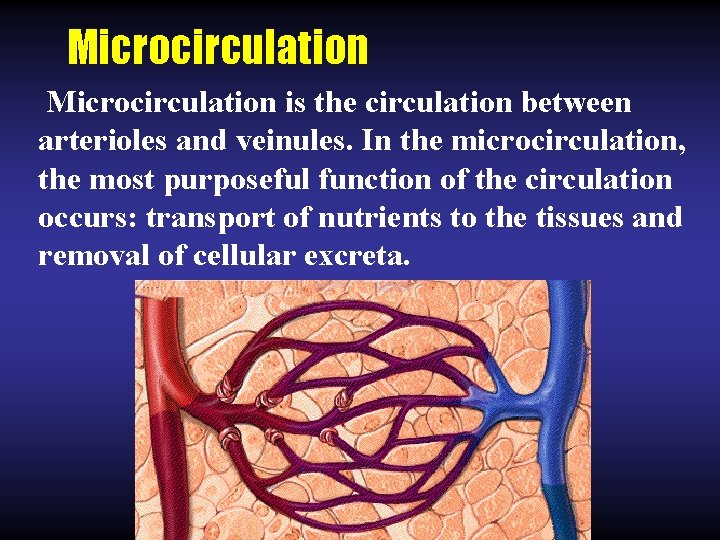
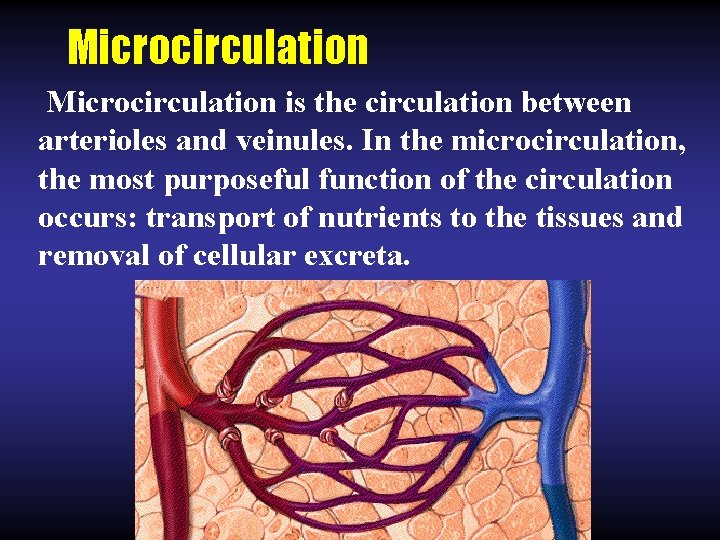
Microcirculation is the circulation between arterioles and veinules. In the microcirculation, the most purposeful function of the circulation occurs: transport of nutrients to the tissues and removal of cellular excreta.
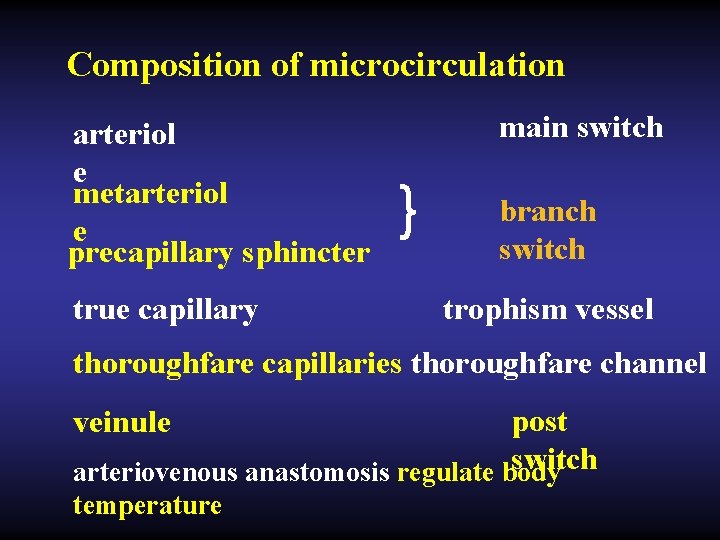
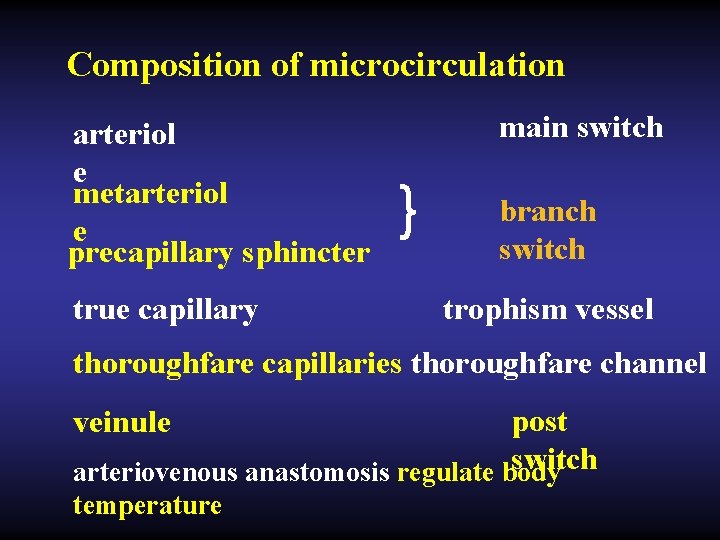
Composition of microcirculation arteriol e metarteriol e precapillary sphincter true capillary main switch } branch switch trophism vessel thoroughfare capillaries thoroughfare channel post switch arteriovenous anastomosis regulate body veinule temperature
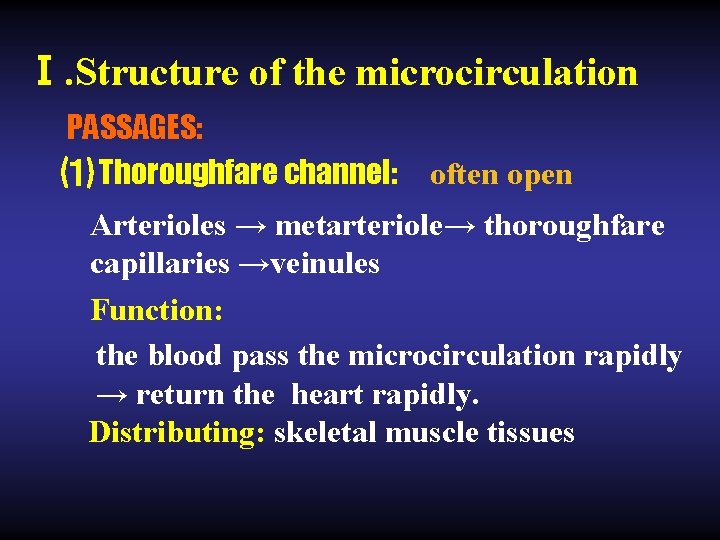
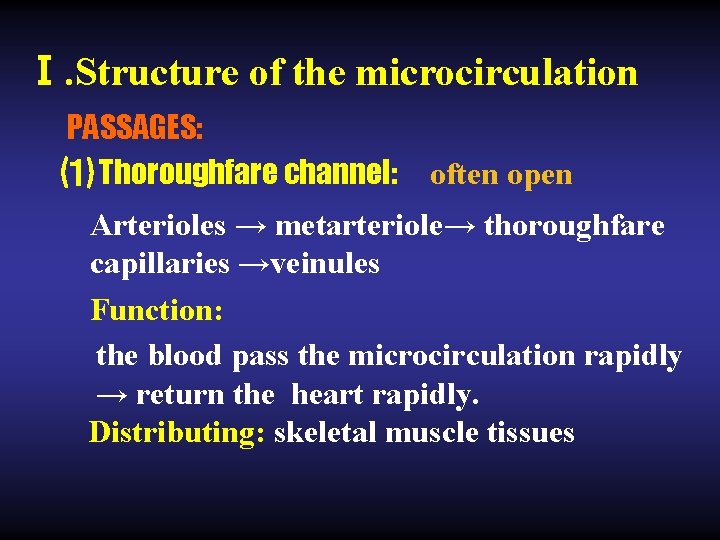
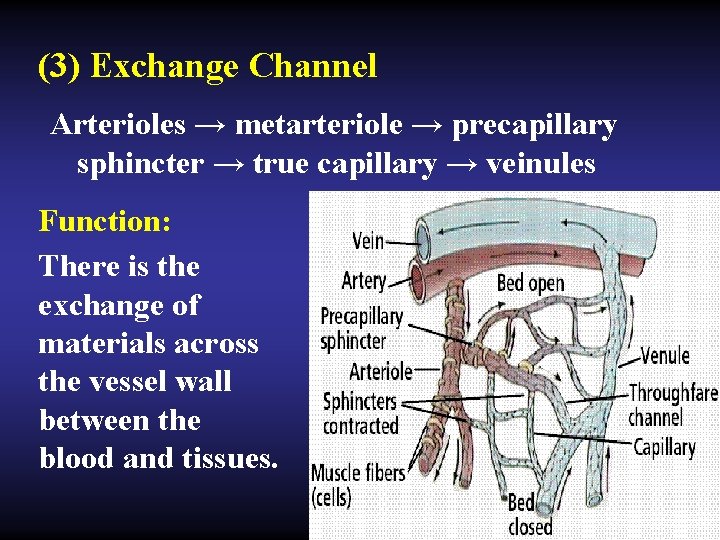
Ⅰ. Structure of the microcirculation PASSAGES: ⑴ Thoroughfare channel: often open Arterioles → metarteriole→ thoroughfare capillaries →veinules Function: the blood pass the microcirculation rapidly → return the heart rapidly. Distributing: skeletal muscle tissues
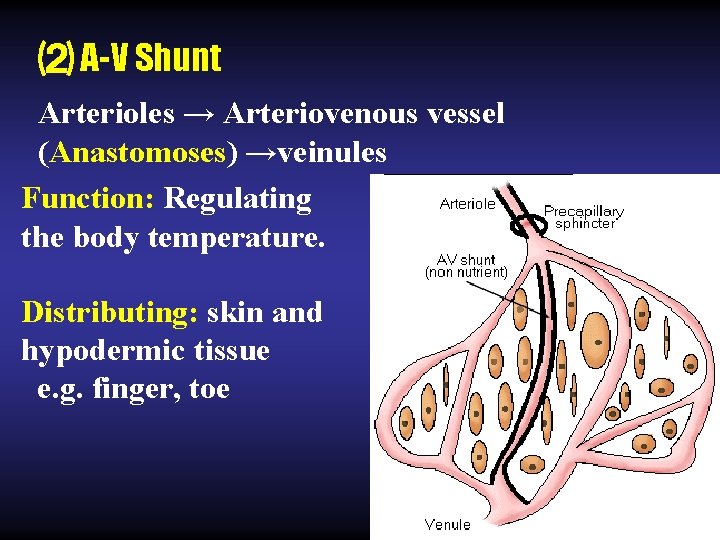
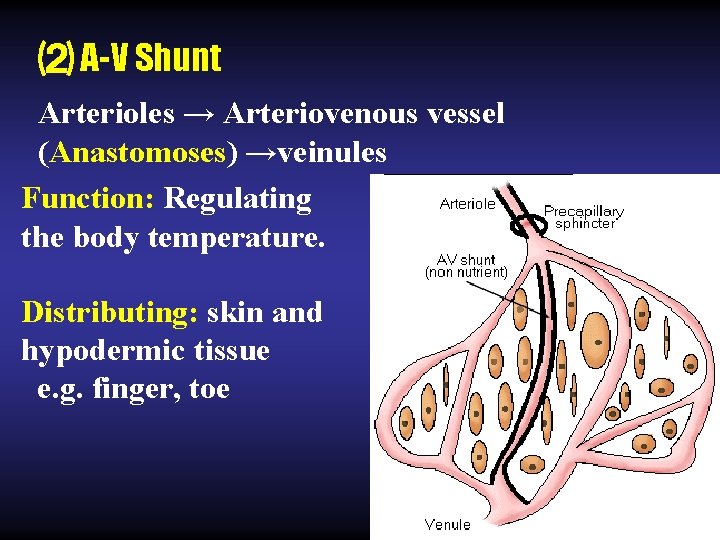
⑵ A-V Shunt Arterioles → Arteriovenous vessel (Anastomoses) →veinules Function: Regulating the body temperature. Distributing: skin and hypodermic tissue e. g. finger, toe
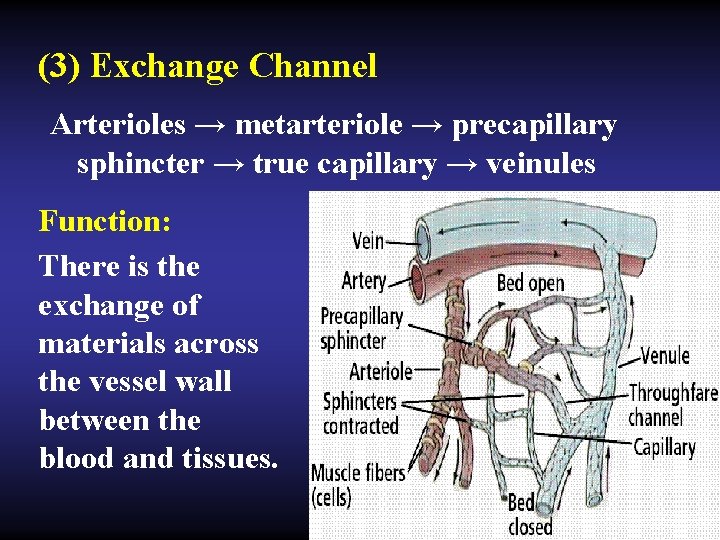
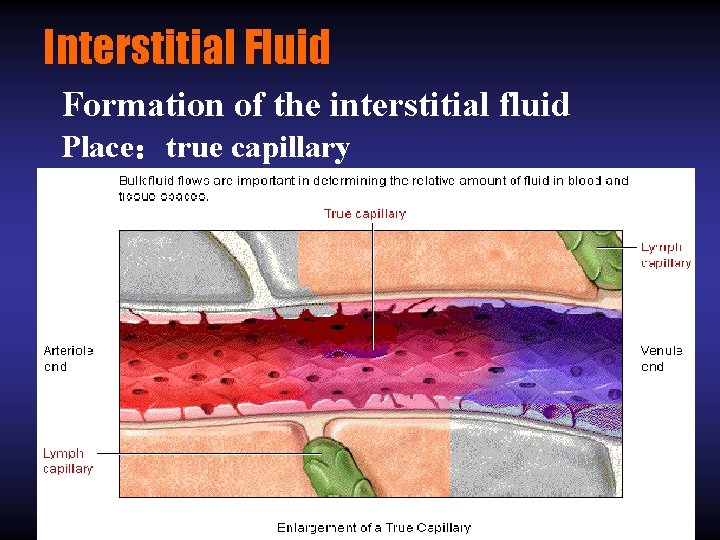
(3) Exchange Channel Arterioles → metarteriole → precapillary sphincter → true capillary → veinules Function: There is the exchange of materials across the vessel wall between the blood and tissues.
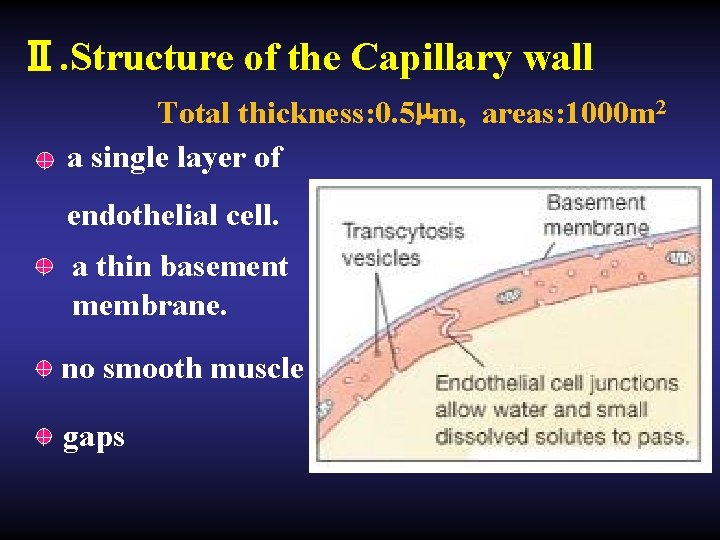
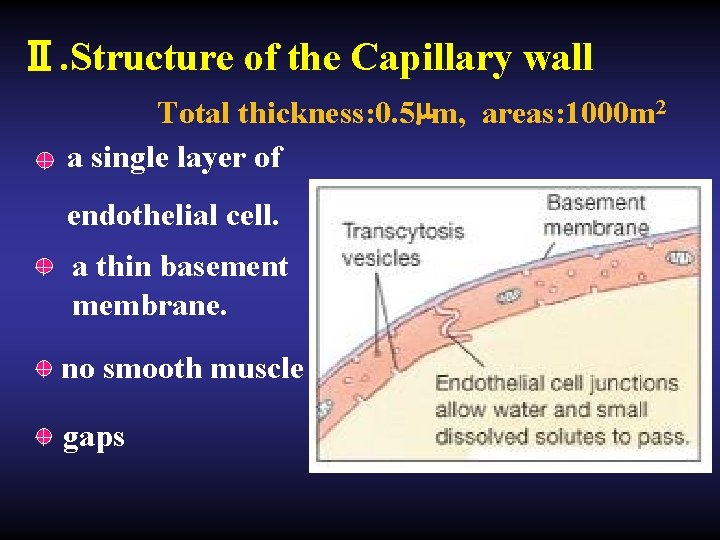
Ⅱ. Structure of the Capillary wall Total thickness: 0. 5µm, areas: 1000 m 2 + a single layer of endothelial cell. + a thin basement membrane. + no smooth muscle + gaps
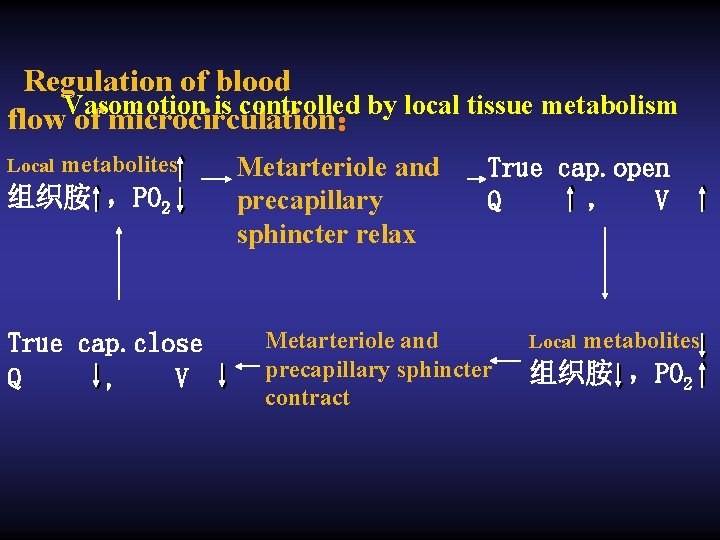
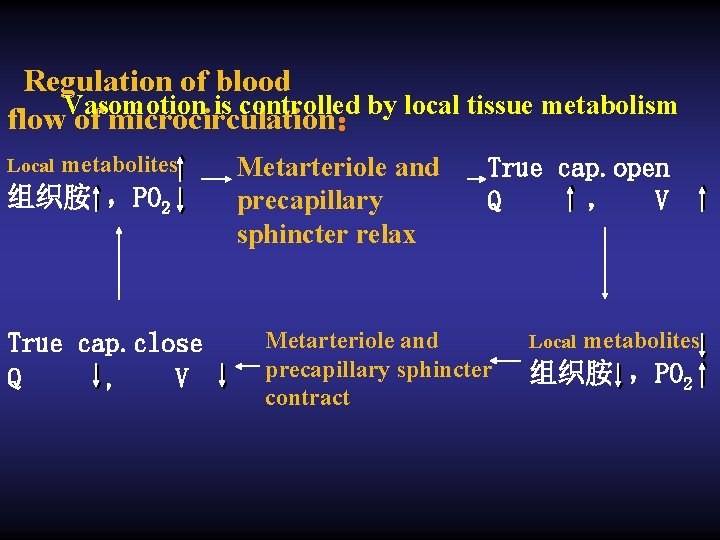
Regulation of blood Vasomotion is controlled by local tissue metabolism flow of microcirculation: Local metabolites 组织胺 ,PO 2 True cap. close Q , V Metarteriole and precapillary sphincter relax True cap. open Q , V Metarteriole and precapillary sphincter contract Local metabolites 组织胺 ,PO 2
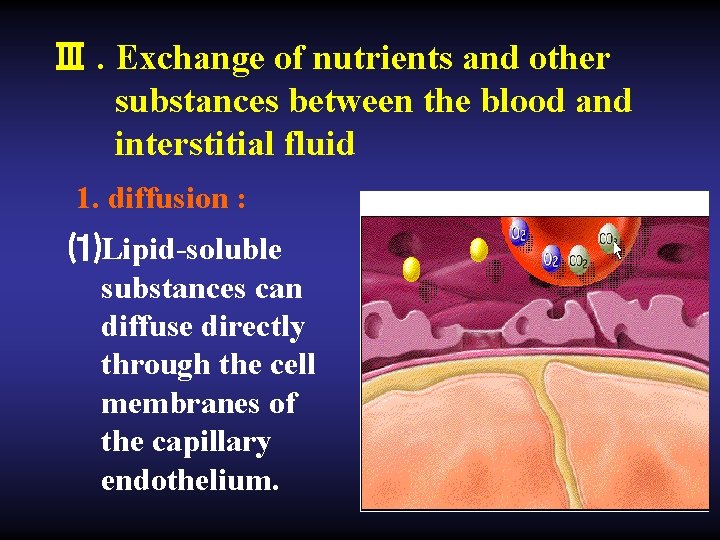
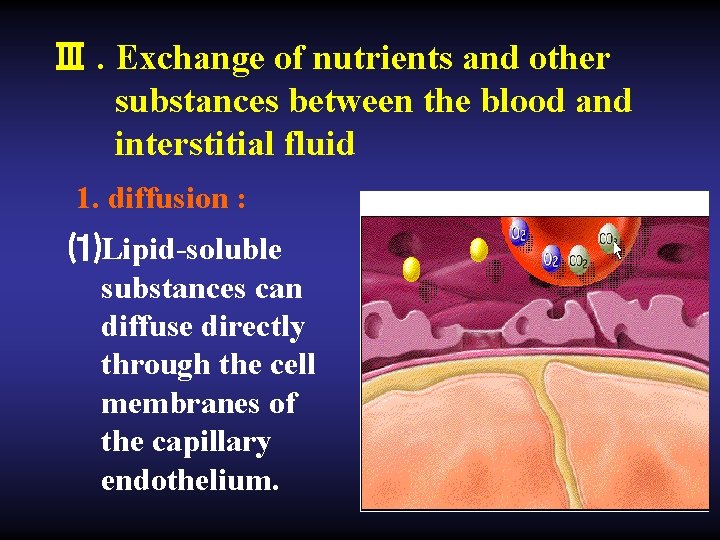
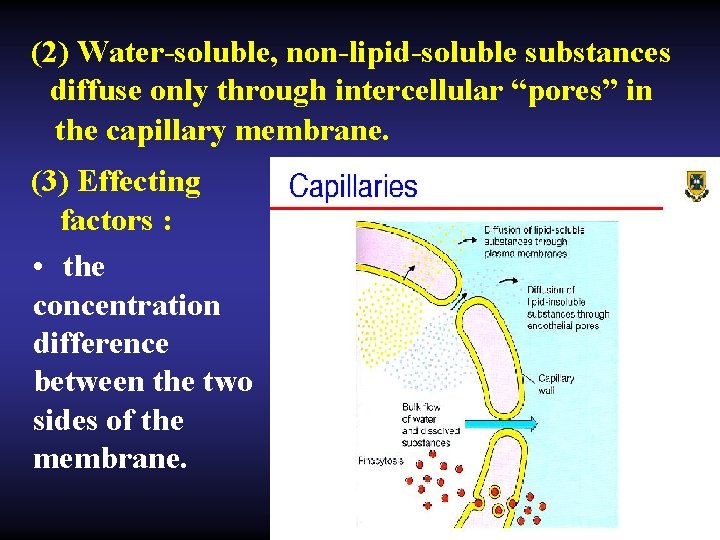
Ⅲ. Exchange of nutrients and other substances between the blood and interstitial fluid 1. diffusion : ⑴Lipid-soluble substances can diffuse directly through the cell membranes of the capillary endothelium.
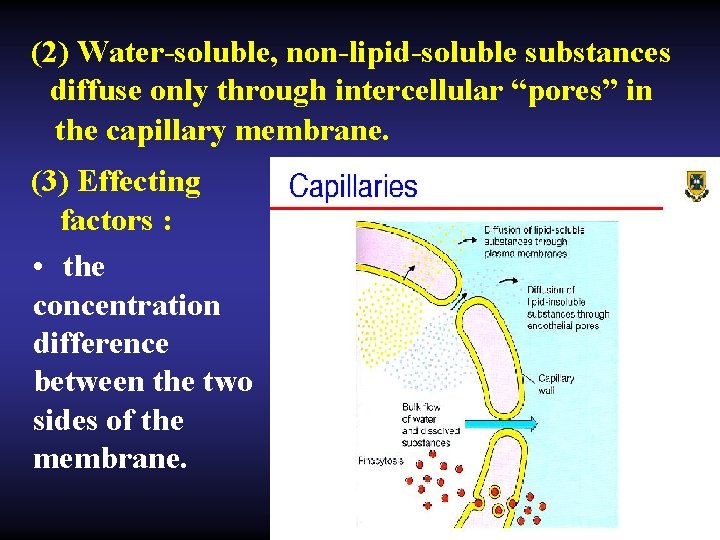
(2) Water-soluble, non-lipid-soluble substances diffuse only through intercellular “pores” in the capillary membrane. (3) Effecting factors : • the concentration difference between the two sides of the membrane.
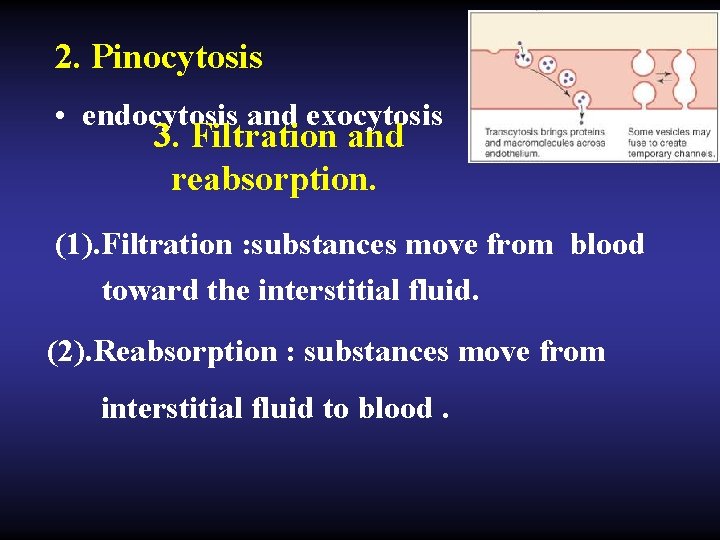
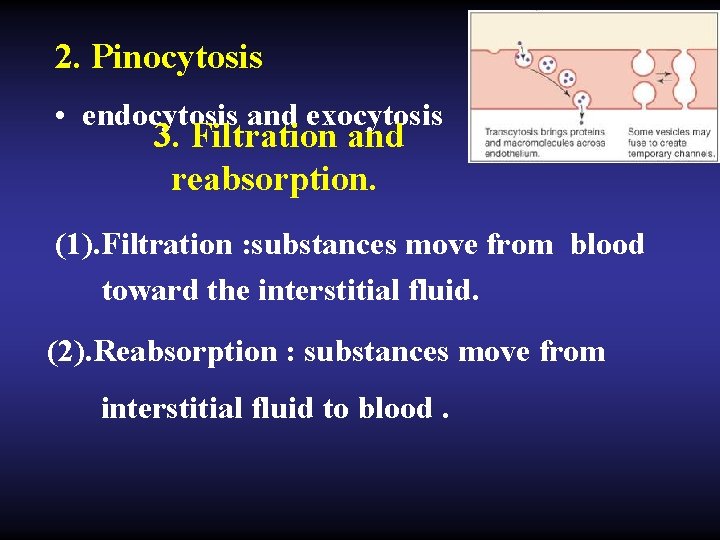
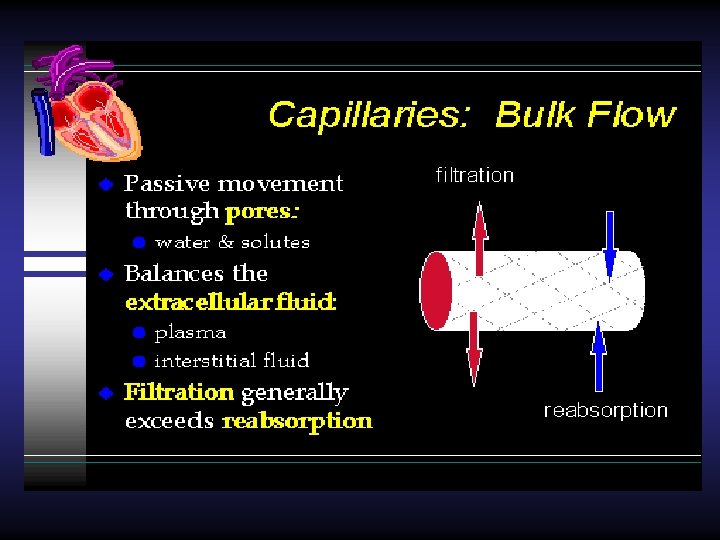
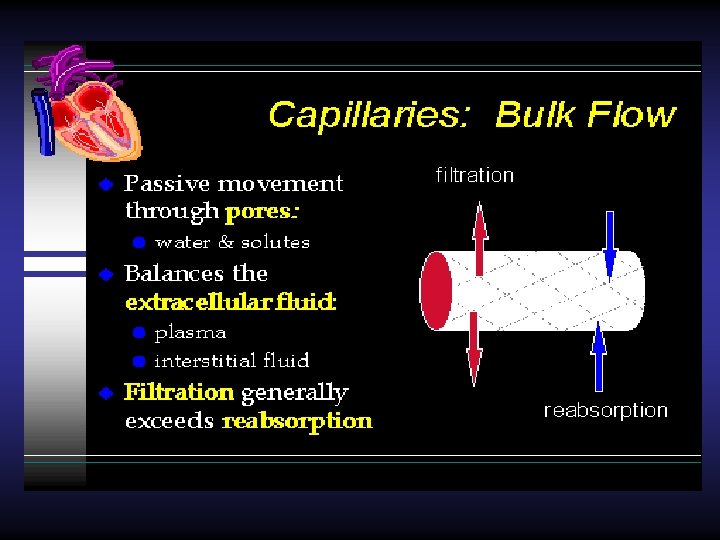
2. Pinocytosis • endocytosis and exocytosis 3. Filtration and reabsorption. (1). Filtration : substances move from blood toward the interstitial fluid. (2). Reabsorption : substances move from interstitial fluid to blood.
Ⅳ. Interstitial fluid Water within the body accounts for 60% of the total body weight (body fluid). 2/3 intracellular compartment 1/3 extracellular compartment (75%, interstitial fluid; 25%, blood plasma)
• The interstitial fluid is derived by filtration and diffusion from the capillaries, it contains almost the same constituents as plasma except for proteins because proteins do not pass outward through the pores of the capillaries with ease.
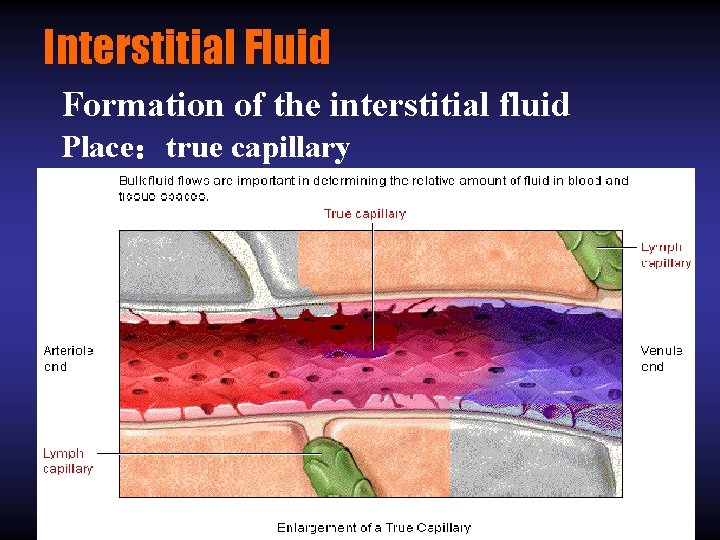
Interstitial Fluid Formation of the interstitial fluid Place:true capillary
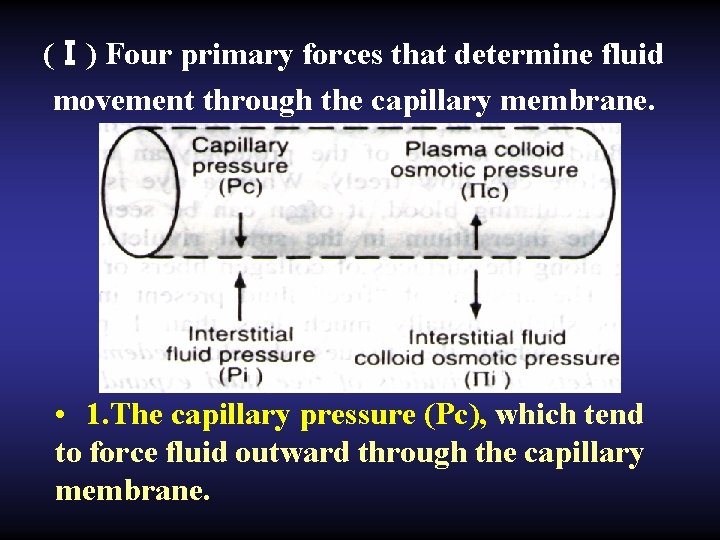
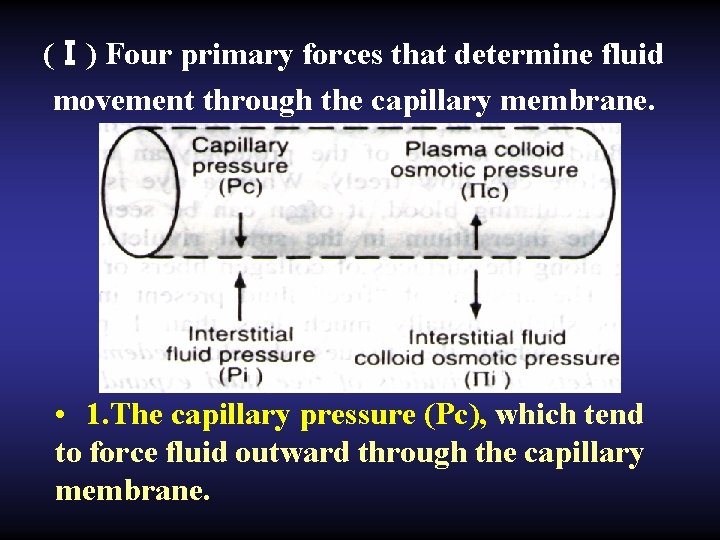
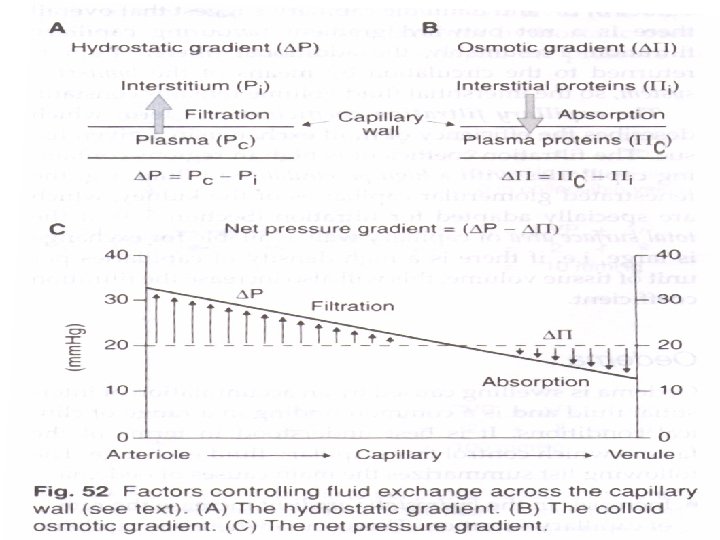
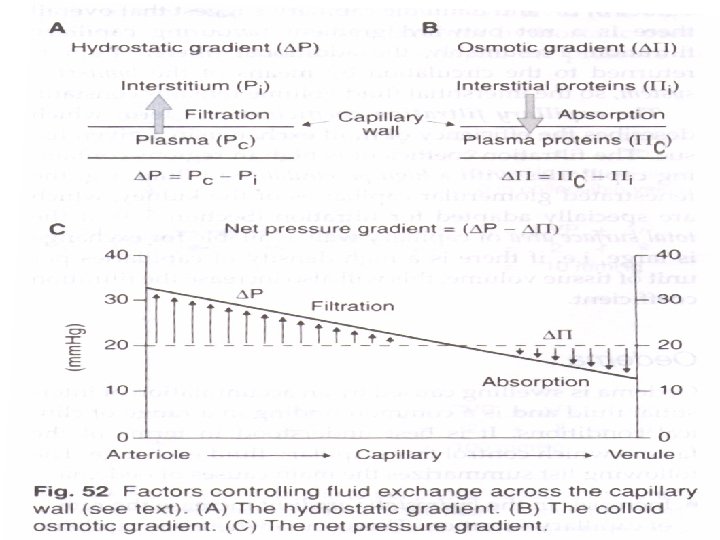
(Ⅰ) Four primary forces that determine fluid movement through the capillary membrane. • 1. The capillary pressure (Pc), which tend to force fluid outward through the capillary membrane.
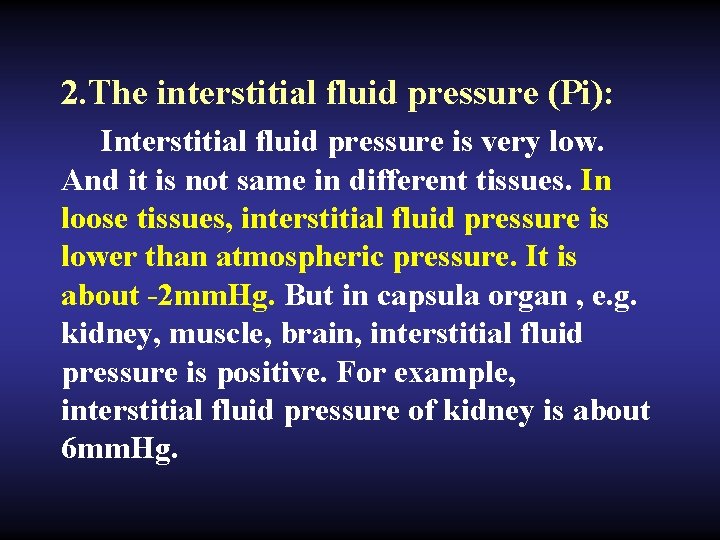
2. The interstitial fluid pressure (Pi): Interstitial fluid pressure is very low. And it is not same in different tissues. In loose tissues, interstitial fluid pressure is lower than atmospheric pressure. It is about -2 mm. Hg. But in capsula organ , e. g. kidney, muscle, brain, interstitial fluid pressure is positive. For example, interstitial fluid pressure of kidney is about 6 mm. Hg.
• When Pi is positive, it tends to force fluid inward through the capillary membrane. But when Pi is negative. it tends to force fluid outward.
3. The plasma colloid osmotic pressure ( πc): The plasma colloid osmotic pressure is formed by plasma proteins. Its normal value is about 25 mm. Hg. Ions diffuse rapidly across the capillary wall but proteins do not, so colloid osmotic pressure of plasma plays an important role in determining the balance of distribution of fluid between extravascular and intravascular spaces and maintaining normal blood volume.
• Fluid always flows from a region of low osmotic pressure to a region of high osmotic pressure. So the plasma colloid osmotic pressure tends to cause osmosis of fluid inward through the capillary membrane.
4. The interstitial fluid colloid osmotic pressure (πi ) , which tends to cause osmosis of fluid outward through the capillary membrane. It is about 10 mm. Hg.
(Ⅱ) Exchange of fluid volume through the capillary membrane
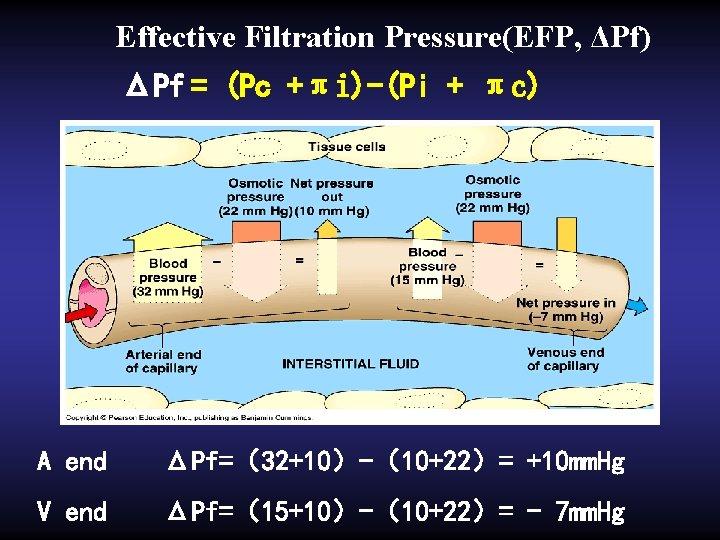
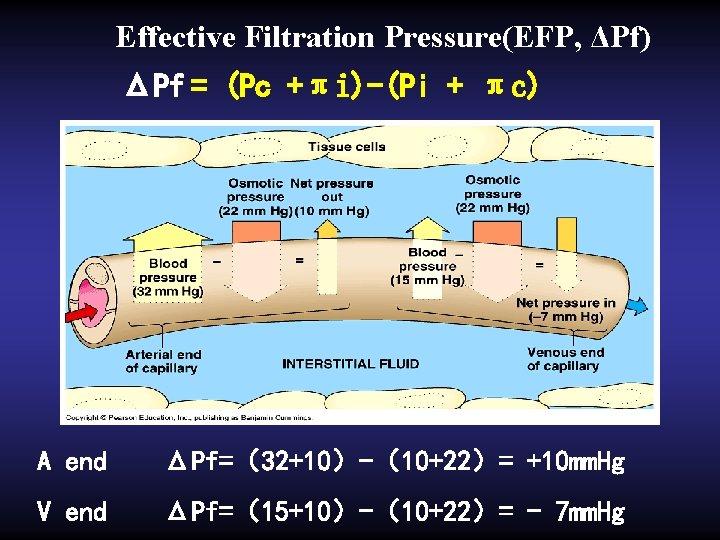
Effective Filtration Pressure(EFP, ΔPf) ΔPf = (Pc +πi)-(Pi + πc) A end ΔPf=(32+10)-(10+22)= +10 mm. Hg V end ΔPf=(15+10)-(10+22)= - 7 mm. Hg
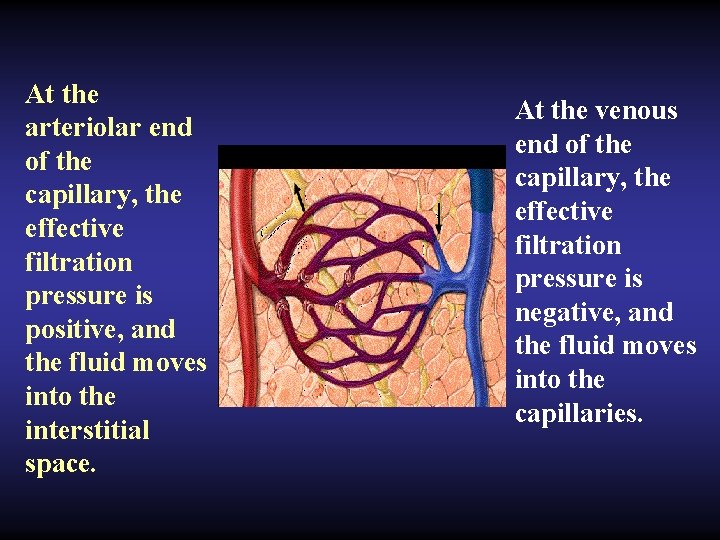
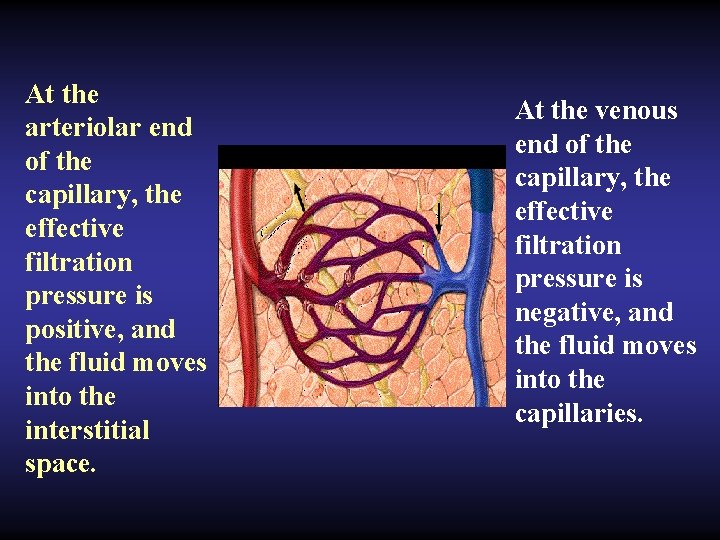
At the arteriolar end of the capillary, the effective filtration pressure is positive, and the fluid moves into the interstitial space. At the venous end of the capillary, the effective filtration pressure is negative, and the fluid moves into the capillaries.
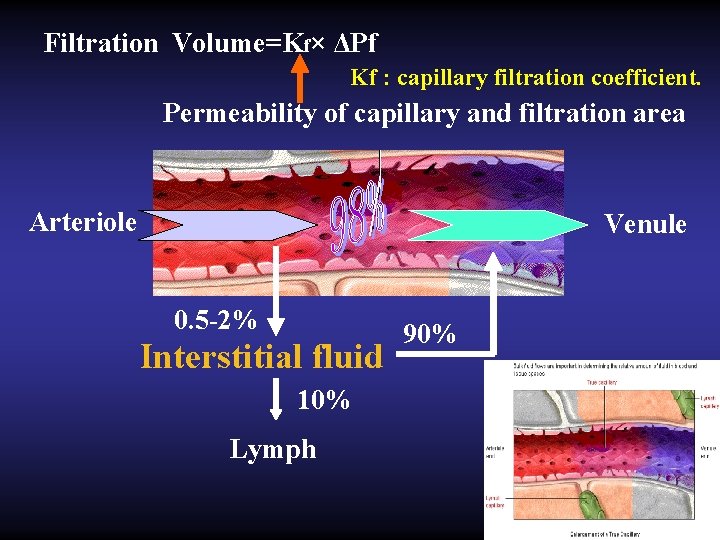
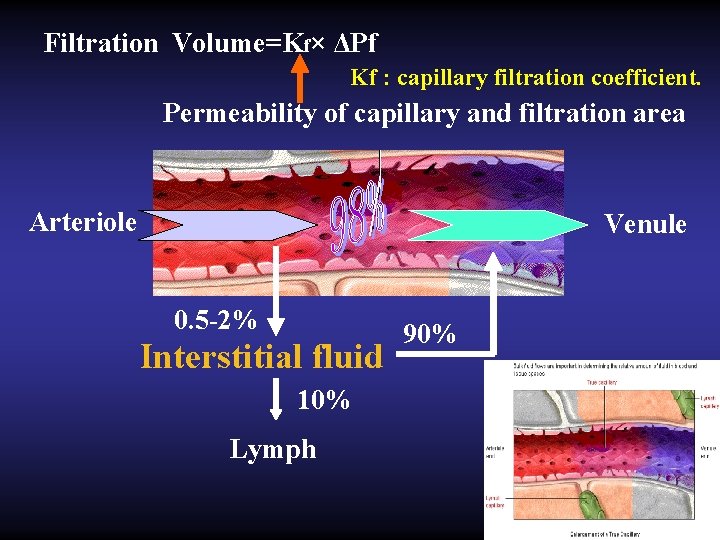
Filtration Volume=Kf× ΔPf Kf : capillary filtration coefficient. Permeability of capillary and filtration area Arteriole Venule 0. 5 -2% Interstitial fluid 10% Lymph 90%
• Most of the fluid filtering from the blood capillaries flows among the cells and finally is reabsorbed back into the venous ends of the blood capillaries; • but on the average, about 1/10 of the fluid instead enters the lymphatic capillaries and returns to the blood system through the lymphatic system. • The total quantity of this lymph is normally only 2 to 4 liters each day.
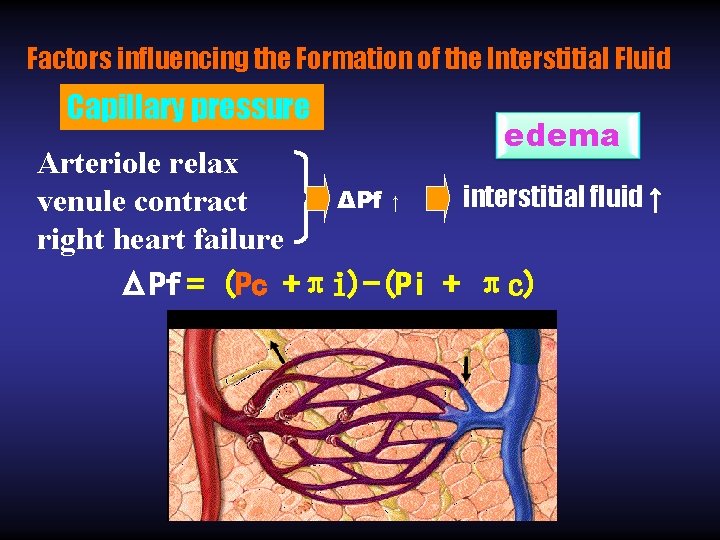
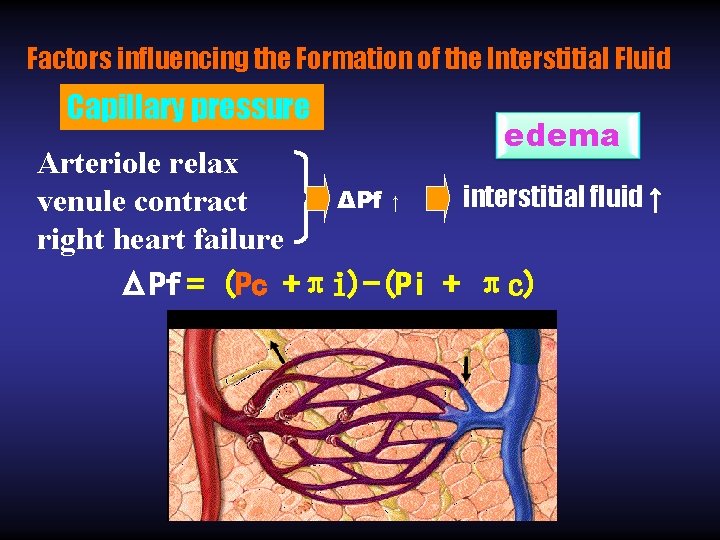
Factors influencing the Formation of the Interstitial Fluid Capillary pressure edema Arteriole relax interstitial fluid ↑ ΔPf ↑ venule contract right heart failure ΔPf = (Pc +πi)-(Pi + πc)
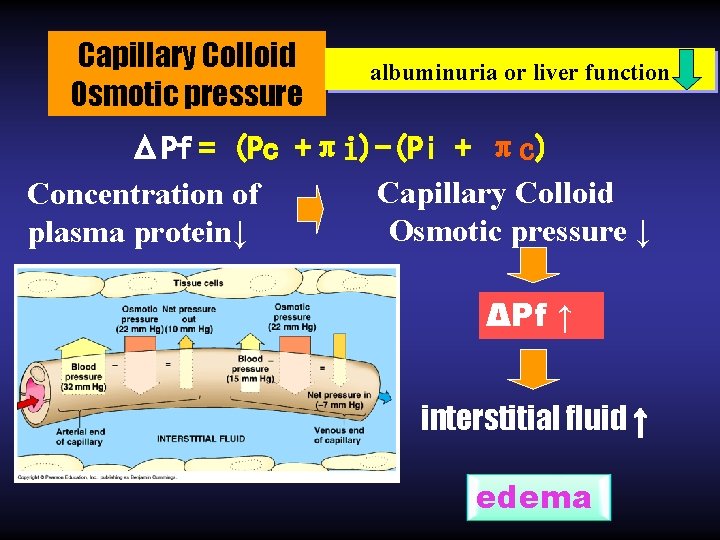
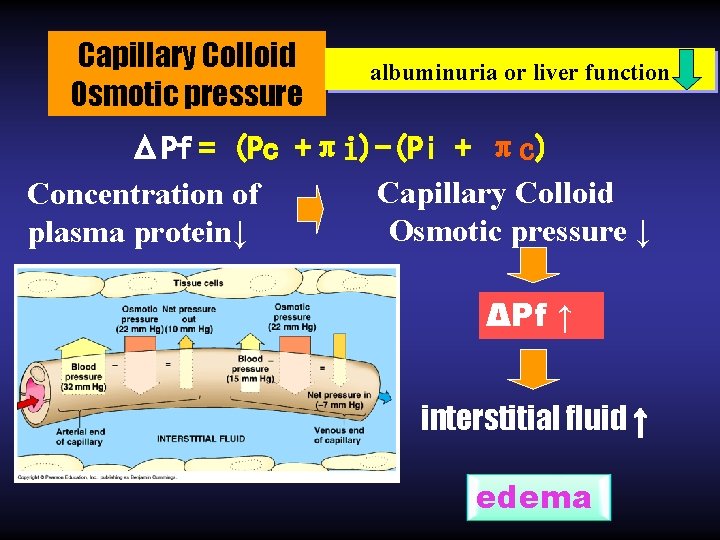
Capillary Colloid Osmotic pressure albuminuria or liver function ΔPf = (Pc +πi)-(Pi + πc) Capillary Colloid Concentration of Osmotic pressure ↓ plasma protein↓ ΔPf ↑ interstitial fluid ↑ edema
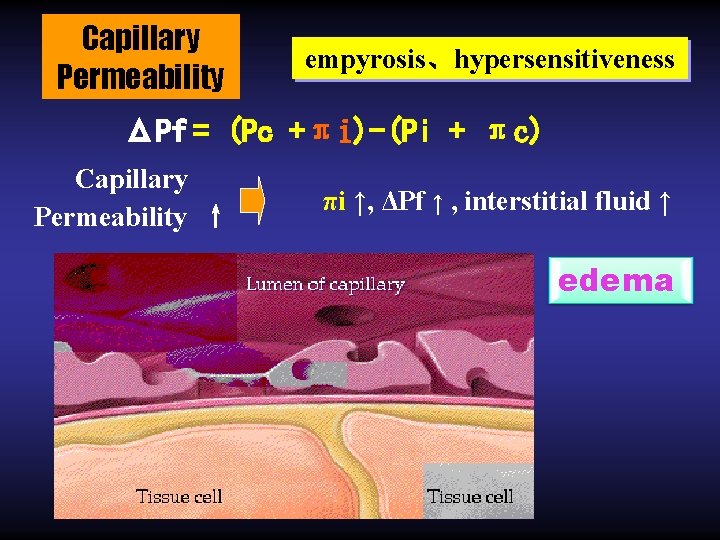
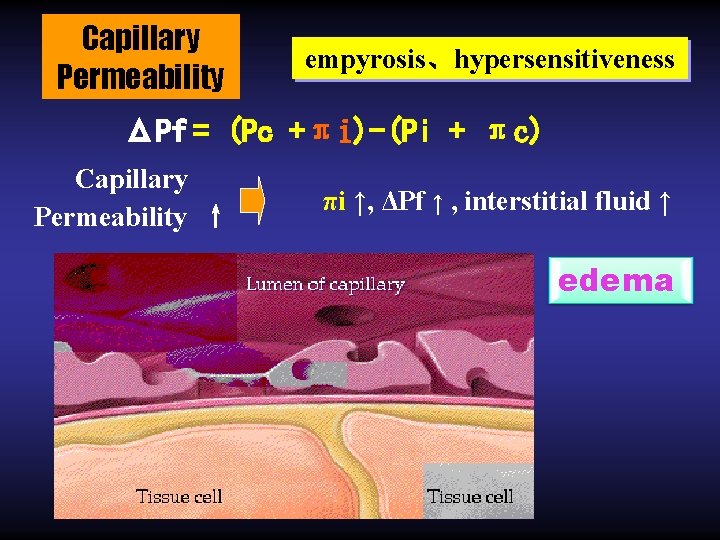
Capillary Permeability empyrosis、hypersensitiveness ΔPf = (Pc +πi)-(Pi + πc) Capillary Permeability ↑ πi ↑, ΔPf ↑ , interstitial fluid ↑ edema
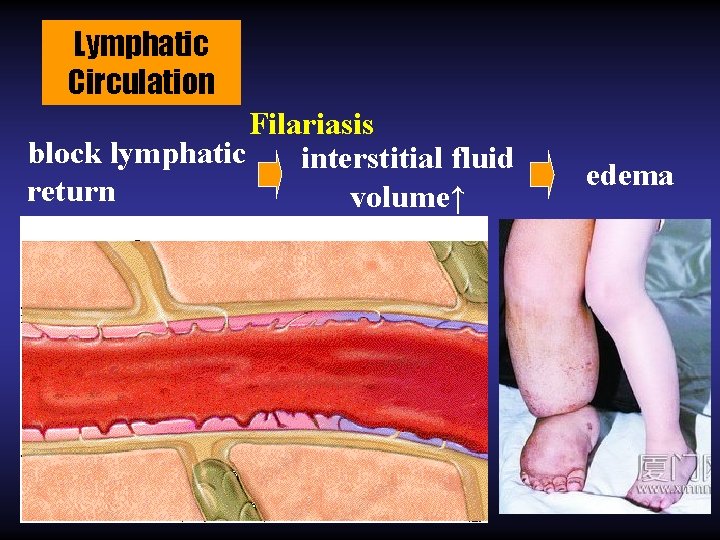
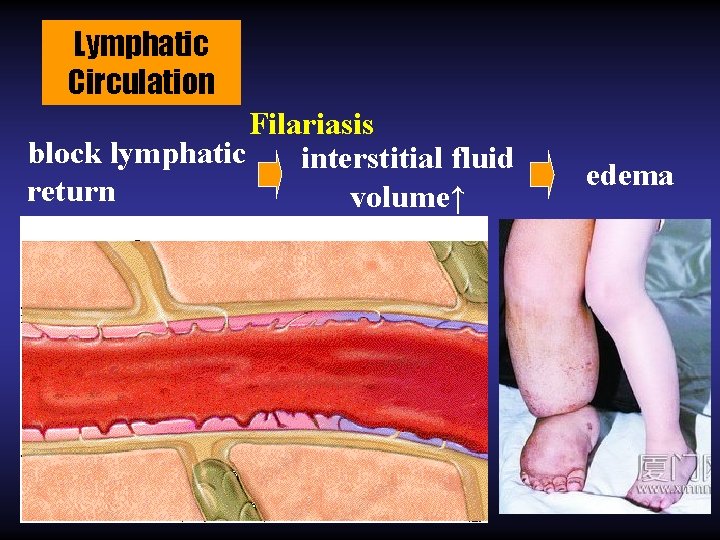
Lymphatic Circulation Filariasis block lymphatic interstitial fluid return volume↑ edema
Ⅴ. Lymphatic system The lymphatic system represents an accessory route by which interstitial fluid can flow from the interstitial spaces into the blood vessels. Its function is very important.
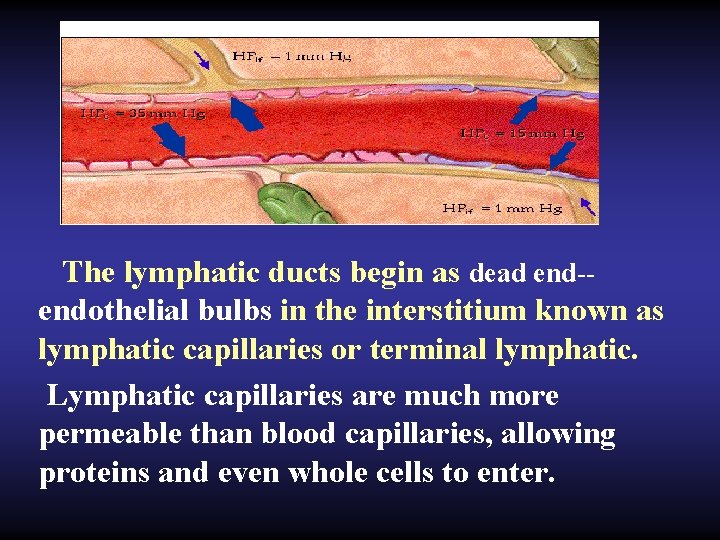
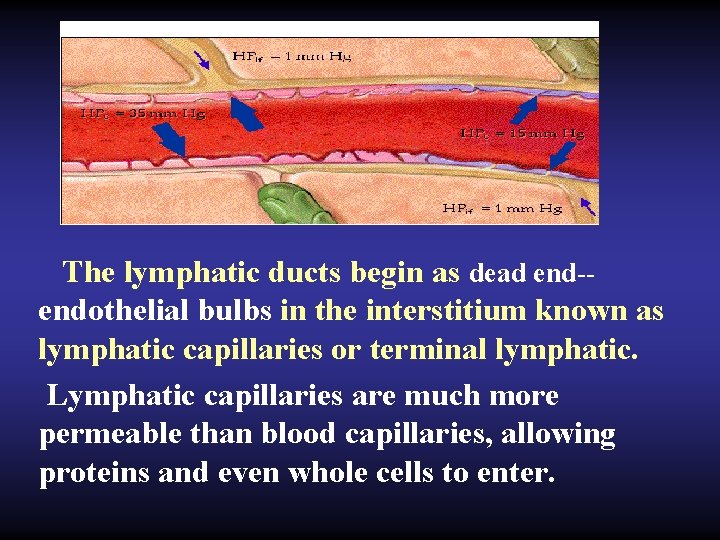
The lymphatic ducts begin as dead end-endothelial bulbs in the interstitium known as lymphatic capillaries or terminal lymphatic. Lymphatic capillaries are much more permeable than blood capillaries, allowing proteins and even whole cells to enter.
• Tissue fluid can flow into the lymphatics. Then the tissue fluid in the lymphatics is called lymph. • Lymph passes into capillary lymphatic ducts and collecting lymphatic ducts. • Eventually the lymph empties into the central veins by the right lymphatic duct and the thoracic duct. • The total quantity of the lymph is normally 2 to 4 liters each day at rest. • Lymph flow is unidirectional from lymphatic ducts to the blood vessels because of valves in lymphatic ducts.
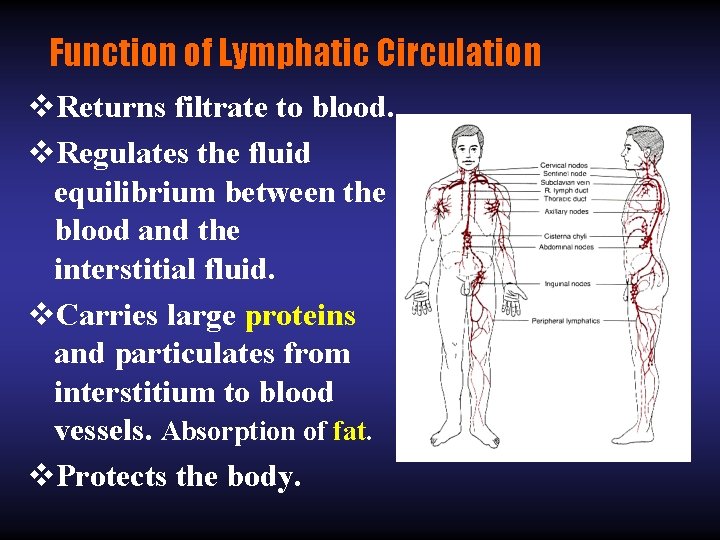
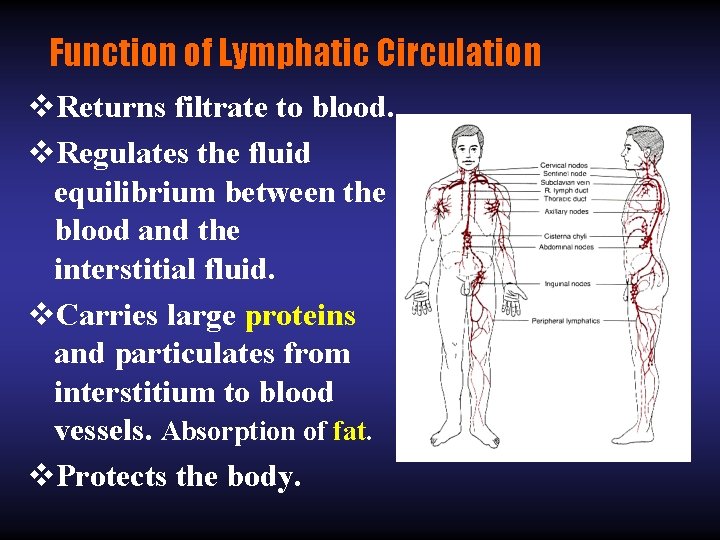
Function of Lymphatic Circulation v. Returns filtrate to blood. v. Regulates the fluid equilibrium between the blood and the interstitial fluid. v. Carries large proteins and particulates from interstitium to blood vessels. Absorption of fat. v. Protects the body.
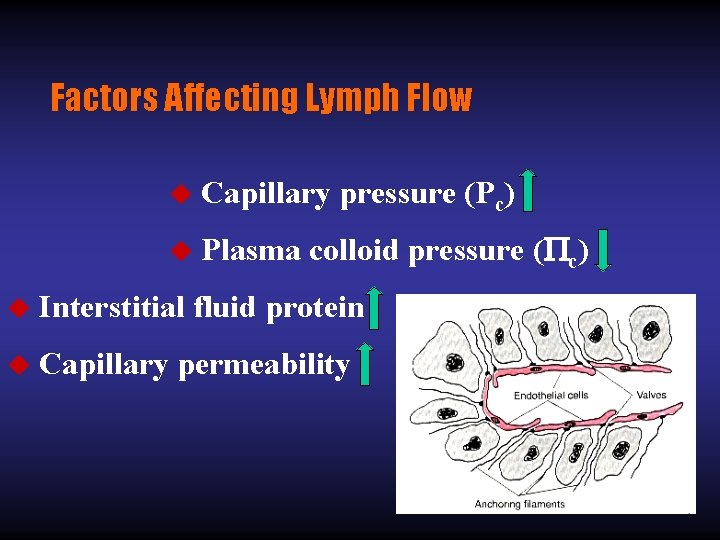
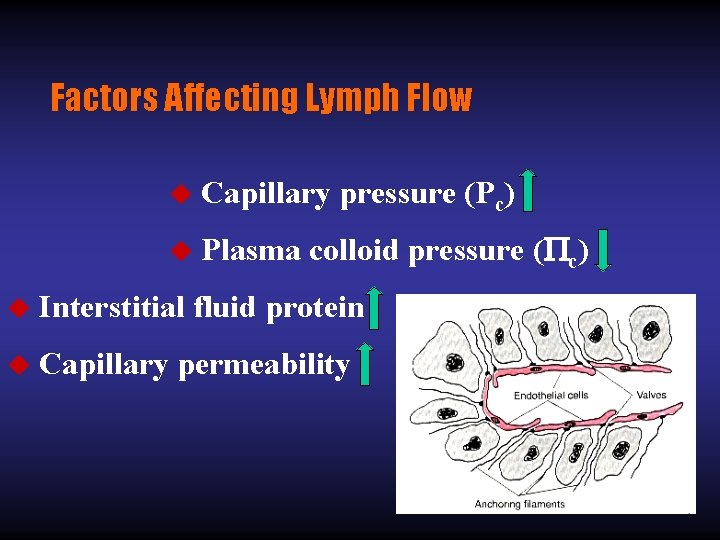
Factors Affecting Lymph Flow u Capillary pressure (Pc) u Plasma colloid pressure ( c) u Interstitial fluid protein u Capillary permeability