FETAL CIRCULATION IN HEALTH AND DISEASE Characteristics of



![Cardiac output and its distribution Fetal lamb § About 265 ml/mt [60%]passes through ductus Cardiac output and its distribution Fetal lamb § About 265 ml/mt [60%]passes through ductus](https://slidetodoc.com/presentation_image_h/288967fb98fa871bf782a1c0f7342b0a/image-9.jpg)







![Cardiac output and its distribution Fetal lamb § About 265 ml/mt [60%]passes through ductus Cardiac output and its distribution Fetal lamb § About 265 ml/mt [60%]passes through ductus](https://slidetodoc.com/presentation_image_h/288967fb98fa871bf782a1c0f7342b0a/image-44.jpg)






















- Slides: 107

FETAL CIRCULATION IN HEALTH AND DISEASE

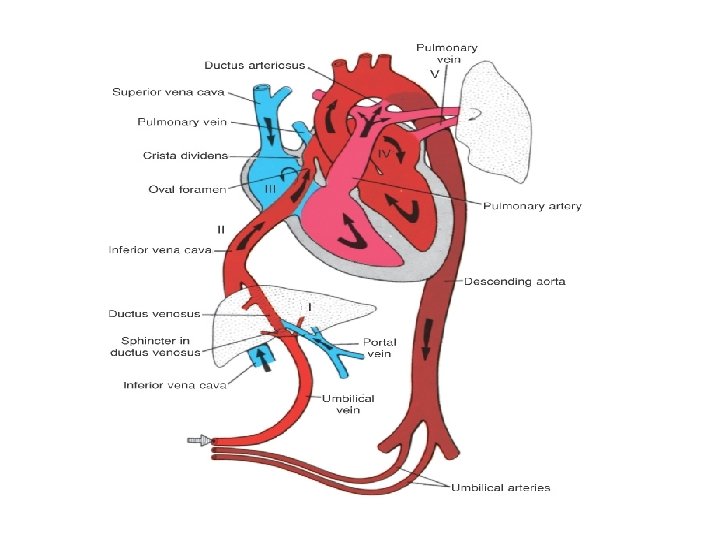
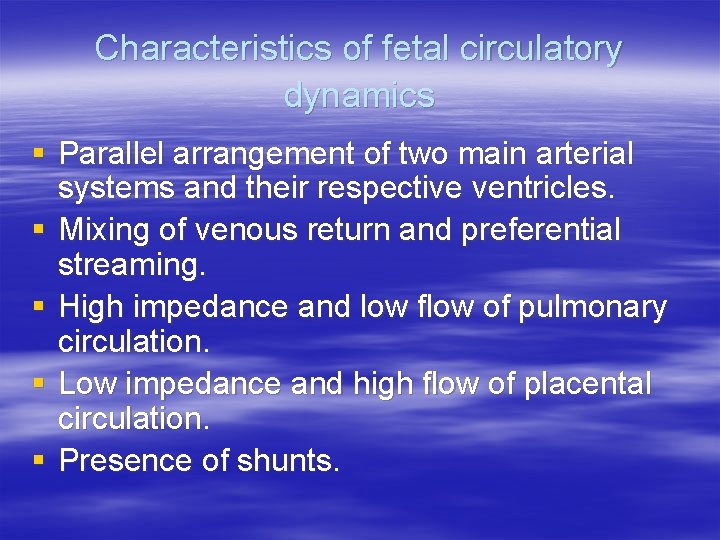
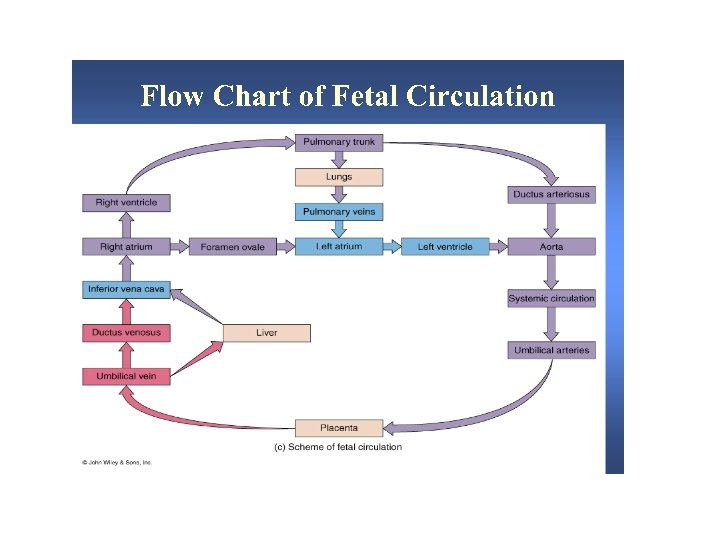
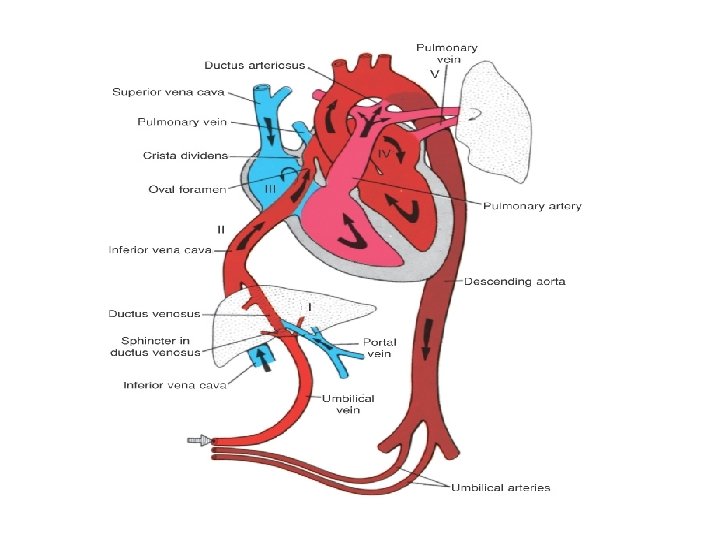
Characteristics of fetal circulatory dynamics § Parallel arrangement of two main arterial systems and their respective ventricles. § Mixing of venous return and preferential streaming. § High impedance and low flow of pulmonary circulation. § Low impedance and high flow of placental circulation. § Presence of shunts.

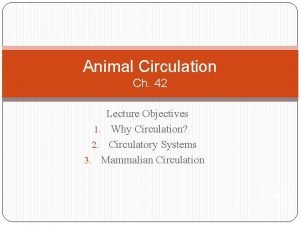
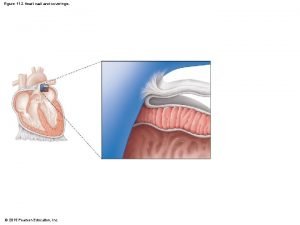
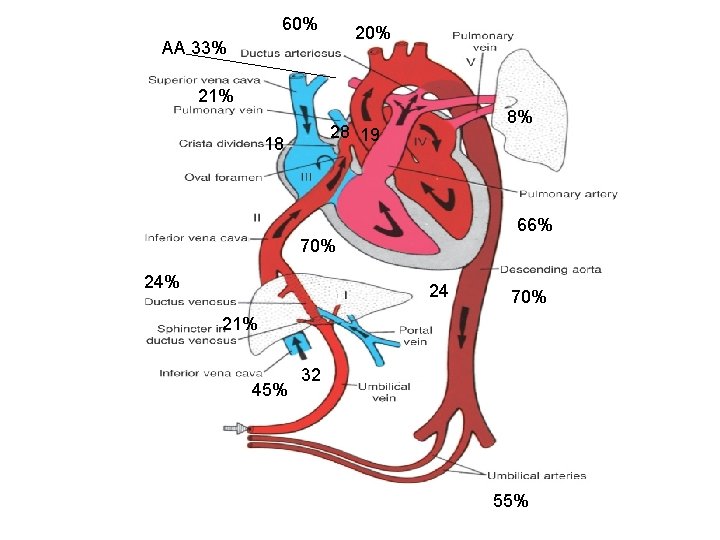
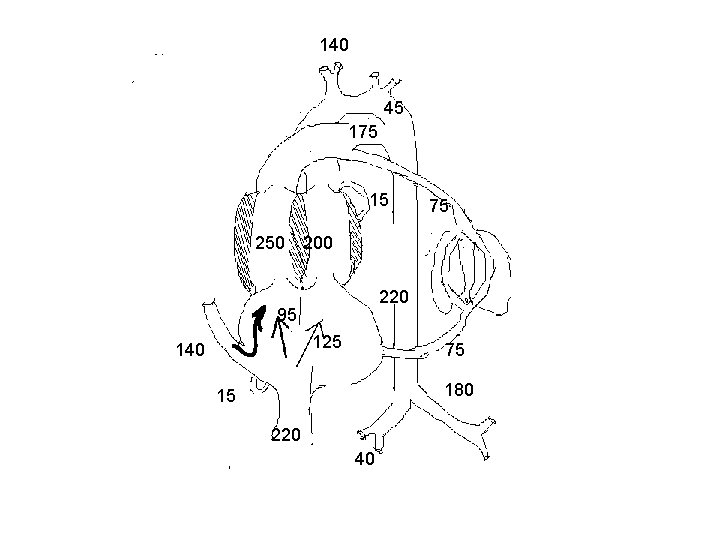
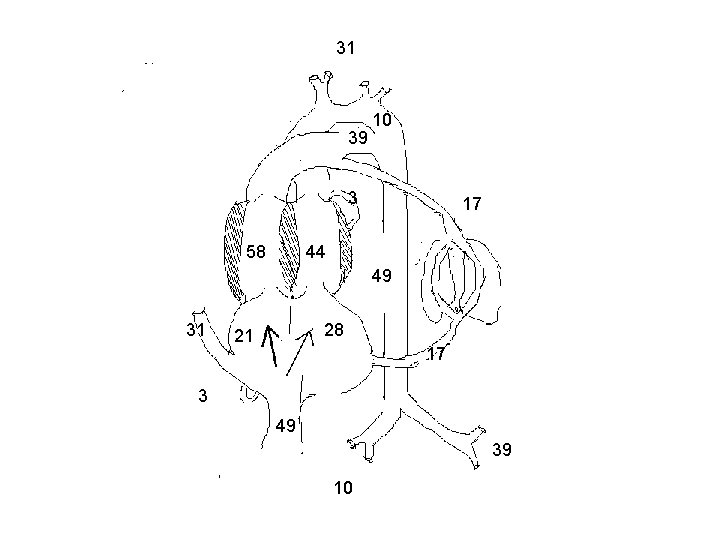
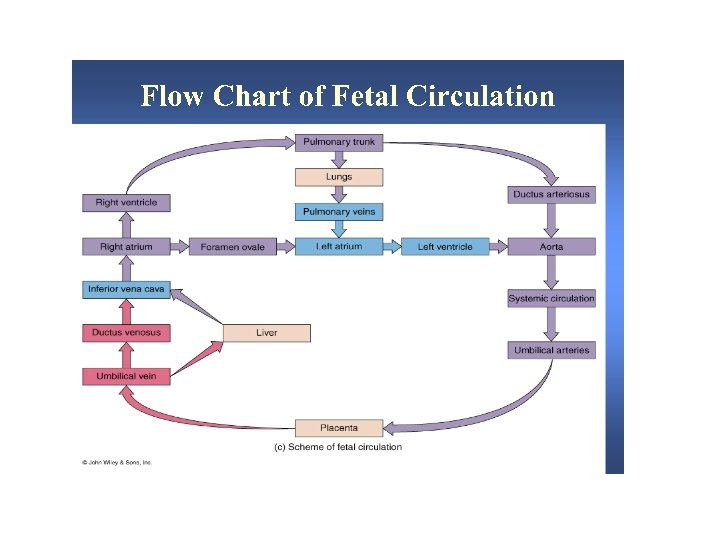
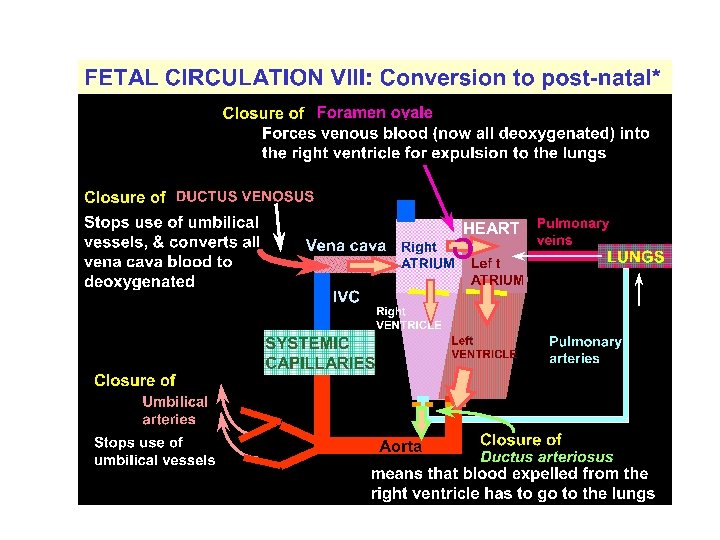
Cardiac output and its distribution Fetal lamb § § CVO is 450 ml/kg/wt RV ejects 2/3 and LV ejects 1/3 of CVO UV flow is 200 ml/mt/kg [45% of CVO] Of this, 110 ml/mt [24%] passes through DV and 90 ml/mt[21%] passes through hepatic circulation
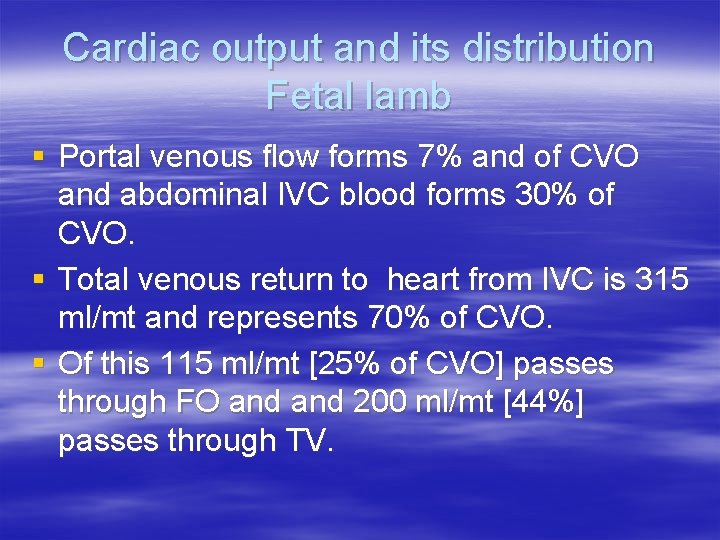
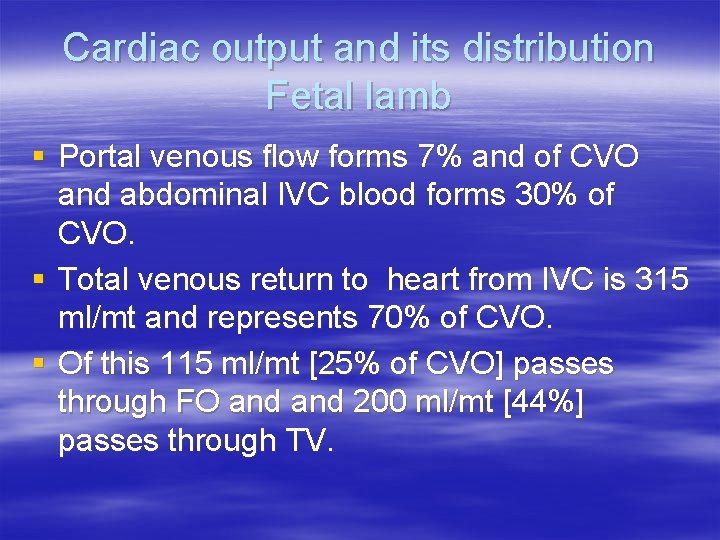
Cardiac output and its distribution Fetal lamb § Portal venous flow forms 7% and of CVO and abdominal IVC blood forms 30% of CVO. § Total venous return to heart from IVC is 315 ml/mt and represents 70% of CVO. § Of this 115 ml/mt [25% of CVO] passes through FO and 200 ml/mt [44%] passes through TV.
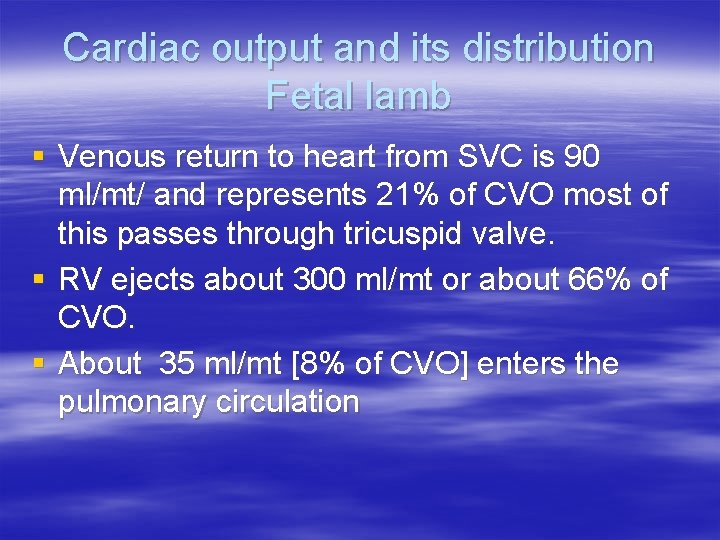
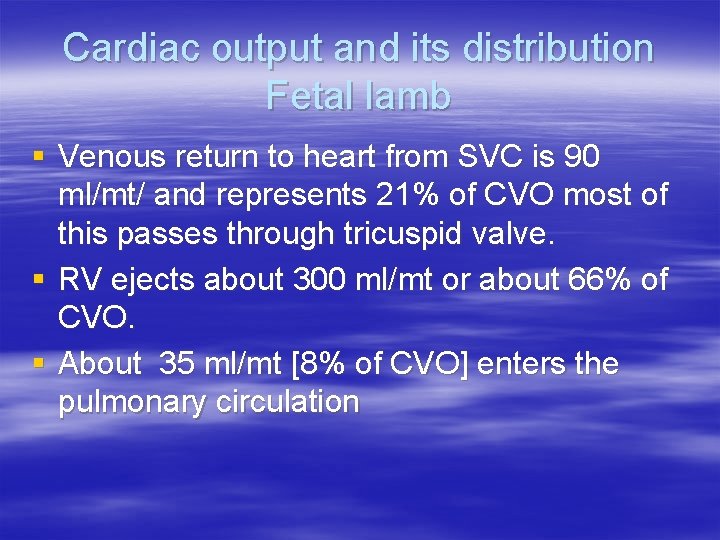
Cardiac output and its distribution Fetal lamb § Venous return to heart from SVC is 90 ml/mt/ and represents 21% of CVO most of this passes through tricuspid valve. § RV ejects about 300 ml/mt or about 66% of CVO. § About 35 ml/mt [8% of CVO] enters the pulmonary circulation
![Cardiac output and its distribution Fetal lamb About 265 mlmt 60passes through ductus Cardiac output and its distribution Fetal lamb § About 265 ml/mt [60%]passes through ductus](https://slidetodoc.com/presentation_image_h/288967fb98fa871bf782a1c0f7342b0a/image-9.jpg)
Cardiac output and its distribution Fetal lamb § About 265 ml/mt [60%]passes through ductus arteriosus. § LV ejects 150 ml/kg [ 33% ]. § Of this, 90 ml/mt [20%] distributed to head and upper half and 45 ml/mt [10%]passes through isthmus. § 3% of CVO enters coronary circulation.
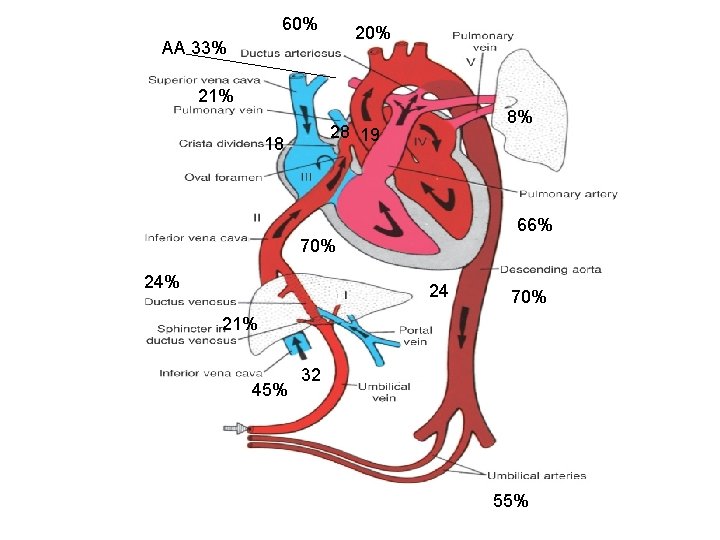
60% 20% AA 33% 21% 8% 28 19 18 66% 70% 24 70% 21% 45% 32 55%
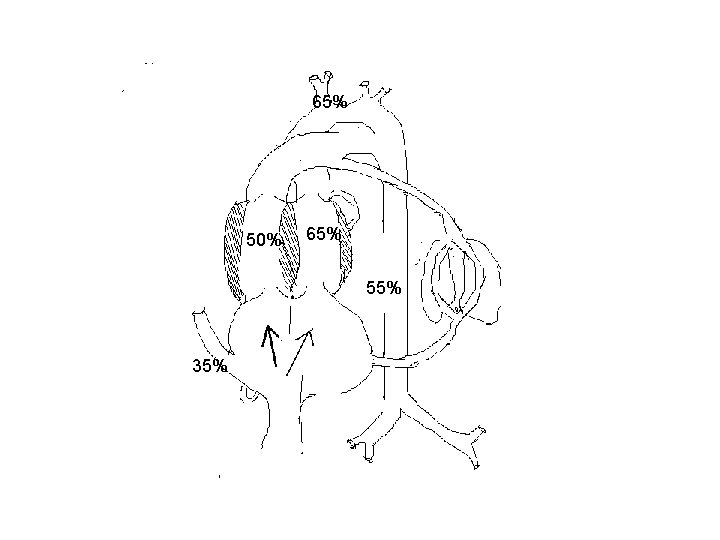
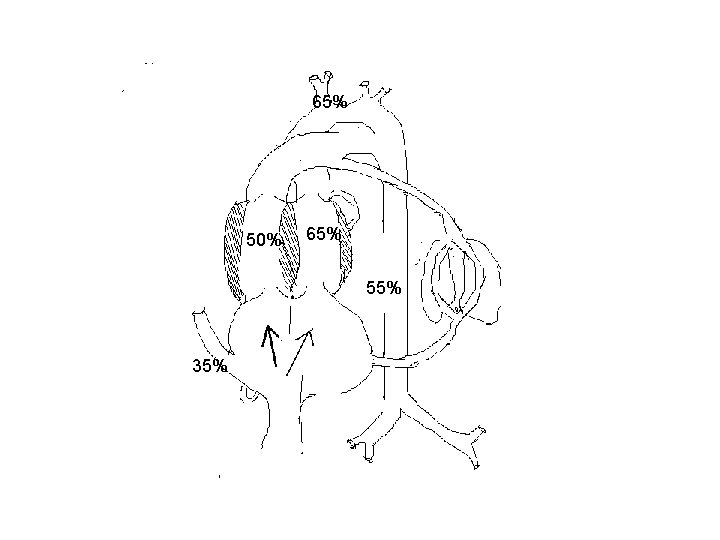
65% 50% 65% 55% 35%

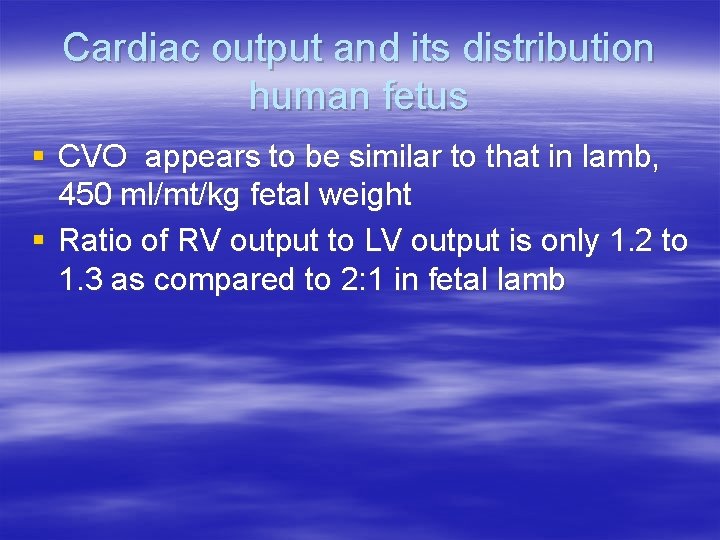
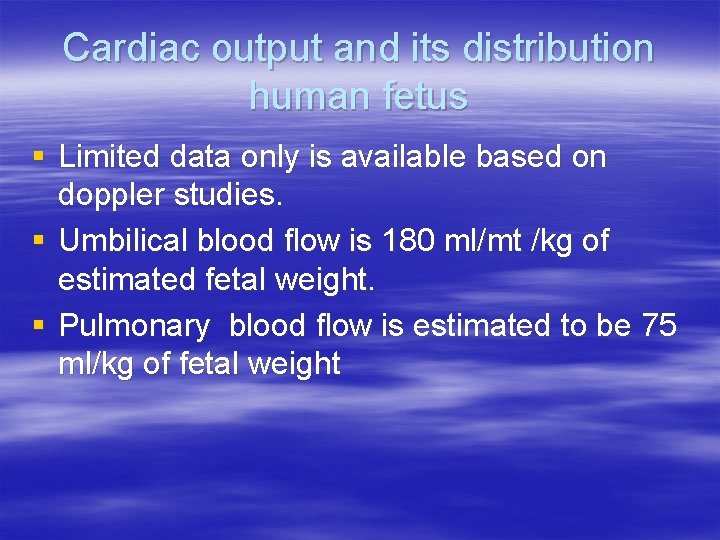
Cardiac output and its distribution human fetus § Limited data only is available based on doppler studies. § Umbilical blood flow is 180 ml/mt /kg of estimated fetal weight. § Pulmonary blood flow is estimated to be 75 ml/kg of fetal weight
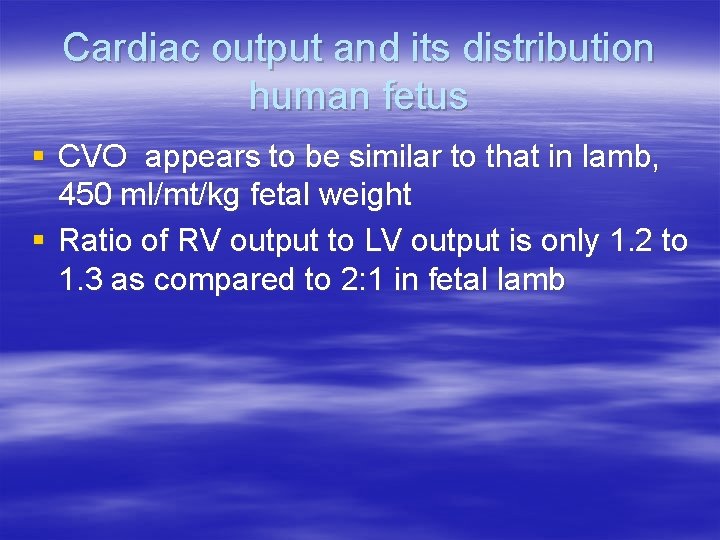
Cardiac output and its distribution human fetus § CVO appears to be similar to that in lamb, 450 ml/mt/kg fetal weight § Ratio of RV output to LV output is only 1. 2 to 1. 3 as compared to 2: 1 in fetal lamb
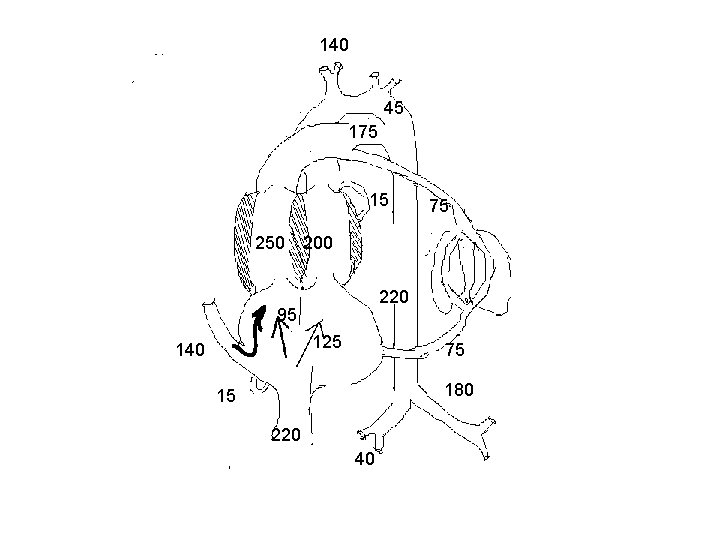
140 45 175 15 75 250 200 220 95 125 140 75 180 15 220 40
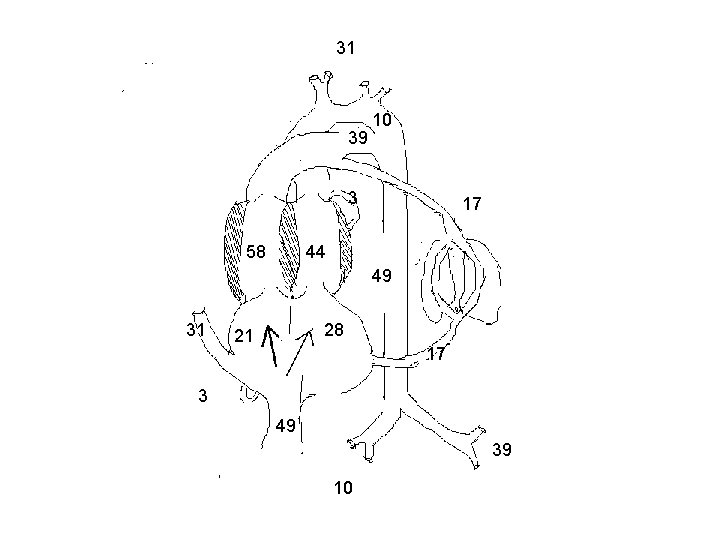
31 39 10 3 58 17 44 49 31 28 21 17 3 49 39 10
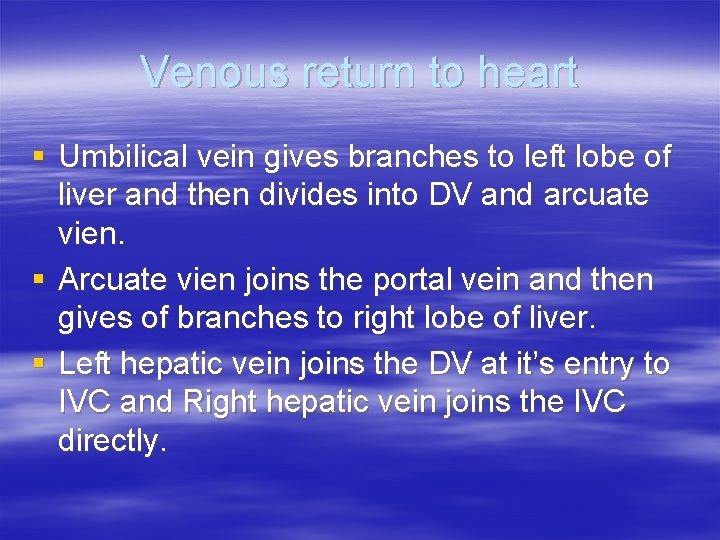
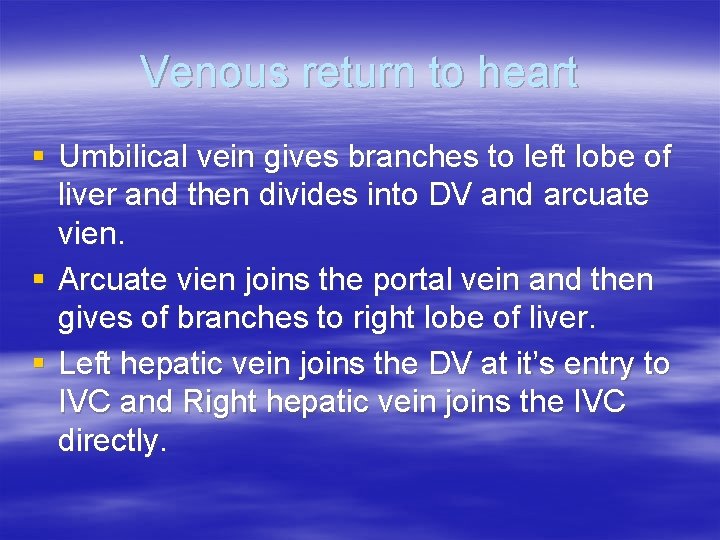
Venous return to heart § Umbilical vein gives branches to left lobe of liver and then divides into DV and arcuate vien. § Arcuate vien joins the portal vein and then gives of branches to right lobe of liver. § Left hepatic vein joins the DV at it’s entry to IVC and Right hepatic vein joins the IVC directly.
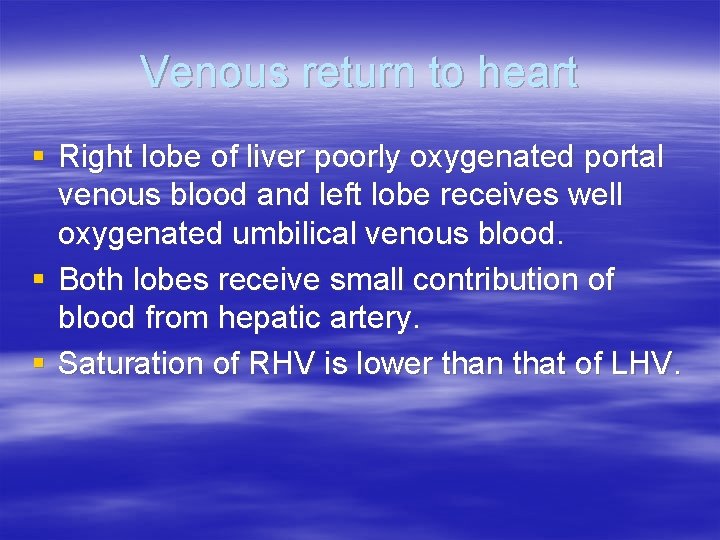
Venous return to heart § Right lobe of liver poorly oxygenated portal venous blood and left lobe receives well oxygenated umbilical venous blood. § Both lobes receive small contribution of blood from hepatic artery. § Saturation of RHV is lower than that of LHV.
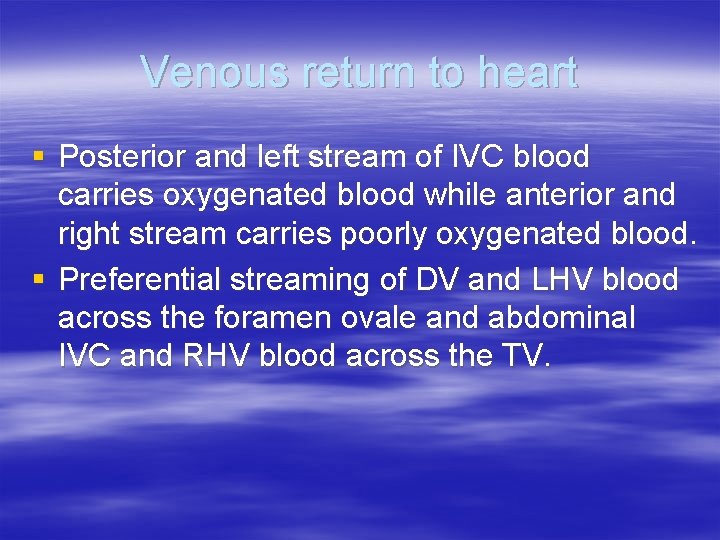
Venous return to heart § Posterior and left stream of IVC blood carries oxygenated blood while anterior and right stream carries poorly oxygenated blood. § Preferential streaming of DV and LHV blood across the foramen ovale and abdominal IVC and RHV blood across the TV.
Venous return to heart § Eustechian valve helps to direct the IVC blood to cross the foramen ovale. § The lower margin of septum secundum [christa dividens] helps to direct the left posterior stream to preferentially across the foramen ovale. § SVC blood is directed aross the TV.
Shunts in fetal circulation § Ductus venosus § Foramen ovale § Ductus arteriosus or aortic isthmus

Shunts in fetal circulation § The blood returning to heart through venacavae and then redistributed to tissues without being delivered to placenta represents effective R to L shunt. § The blood which passes through DV and then reaches DA and goes to placenta without getting distributed to tissues represent effective L to R shunt. § Combined R to L and L to R shunts forms 33% of CVO.
PULMONARY CIRCULATION § Fetal lung does not serve gas exchange function. § PVR is high and PBF is low. § This helps to reduce workload of fetal heart.
PULMONARY CIRCULATION § MPA continues as Ductus and RPA and LPA arise as branches. § Medial layer is composed of smooth muscle predominantly in small pre acinar and large acinar level arteries. § Further branches have no muscular component.

PULMONARY CIRCULATION § PA pressure rises gradually paralleling the rise in aortic pressure. § TPR falls gradually but this fall when correlated with rise in lung weight, there is actually an increase in PVR towards term. § PBF increases gradually.
PULMONARY CIRCULATION § MPA has forward flow throughout systole with a short period of backflow at end of systole. § DA also has forward flow throughout systole. § BPA has forward flow only through initial one third of systole followed by back flow through rest of systole and diastole. § In humans forward flow is more prolonged.

PULMONARY CIRCULATION § Experiments show fetal PBF increases dramatically in response to increase in maternal PO 2. § This response is evident only in latter part of gestation. § Doppler studies indicate similar changes in humans as well.
PULMONARY CIRCULATION § Fetal pulmonary endothelium behaves in a similar fashion as adult endothelium to vasodilators. § Adrenomedullin has a potent and prolonged vasodilatory effect. § Leukotriens may be responsible for maintaining high fetal PVR.
PULMONARY CIRCULATION § Breathing at birth is associated with a marked fall in PVR and rise in PBF. § PA pressure does not fall as rapidly and remain elevated till the Ductus is widely patent. § Once the ductus is closed, PA pressure can vary independent of systemic pressure.
Oxygen exchange function § Higher hemoglobin level in fetus as compared to mother facilitates oxygen uptake by the fetus in the placenta. § Oxygen dissociation curve of fetal red cells is shifted to left as compared to adult red cells. § Hb. F has less affinity towards organic phosphates like 2, 3 DPG and ATP.
Oxygen exchange function § These phosphates that are present in red cells compete with oxygen for binding to hemoglobin. § Affinity of reduced hemoglobin to 2, 3 DPG is higher than that of oxyhemoglobin and this facilitates oxygen delivery at tissue site. § This is not significant in fetal hemoglobin.

Oxygen exchange function § As CO 2 crosses placenta from fetus to mother, it creates a local acidosis. § In the face of decreasing Ph, mothers hemoglobin shows less affinity towards Hb and oxygen release is enhanced. [Bohr effect] § This supports diffusion of more oxygen across the diffusion membrane to fetus.

Oxygen exchange function § As O 2 is released, maternal Hb acts as a buffer that removes H+ from local environment. § This encourages production of bicarbonate from H 2 O and CO 2 thereby reducing local PC 02 and facilitating diffusion of CO 2 from fetus.
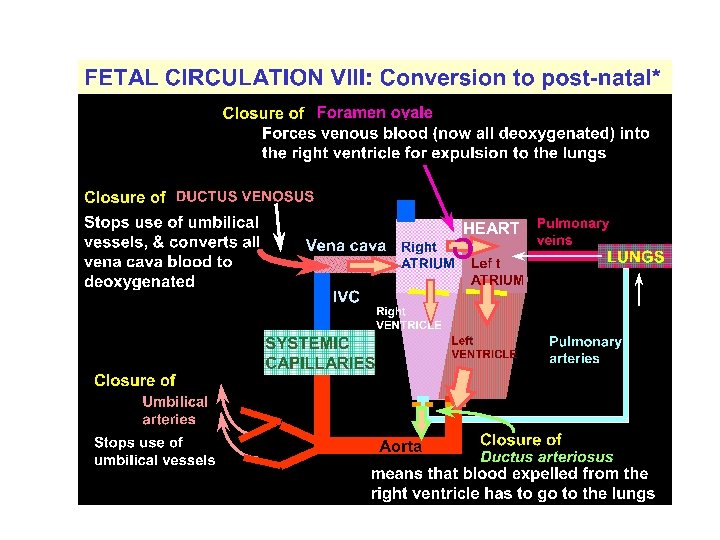
Post natal changes § Gas exchange function is transferred from placenta to the lungs. § Separation of systemic and pulmonary circulations § Increased metabolism to maintain body temperature and hence increased cardiac output.
Post natal changes in various circulatory beds § Coronary Blood flow decreases dramatically as the oxygen content increases. § Cerebral circulation also behaves in the same fashion as coronary circulation.
Post natal changes in various circulatory beds § Skin blood flow is high in utero as the vessels are dilated because the skin is exposed to warm amniotic fluid. § Cutaneous vasoconstriction occurs post natally as evaporation from skin starts. § Cutaneous flow falls and the vascular resistance increaes.
Post natal changes in various circulatory beds § Hepatic blood flow falls rapidly post natally with reduction in umbilical venous return and then increases as the GI flow is re established. § Hepatic blood flow progressively increases after birth and by 7 days after birth reaches a level of 250 ml/minute /100 g by which time there is no flow through ductus venosus.
Changes in Cardiac output § Oxygen consumption increases from 6 -8 ml/mt/kg body weight pre natally to 15 – 20 ml/mt/kg post natally. § CVO of fetal lamb is 450 ml/mt/kg. § C. O of neonatal lamb is 300 -425 ml/mt/kg. So the CVO will be 600 -850 ml/mt/kg. § So the increase is 1. 5 to 2 times.
Changes in Cardiac output Mechanisms § Neonate has to increase the metabolism to increase the body temperature as it is exposed to external temperature. § Improved diastolic function due to removal of compression by maternal organs and uterus causes increased cardiac filling and hence the cardiac output.
Characteristics of fetal circulatory dynamics § Parallel arrangement of two main arterial systems and their respective ventricles. § Mixing of venous return and preferential streaming. § High impedance and low flow of pulmonary circulation. § Low impedance and high flow of placental circulation. § Presence of shunts.

Cardiac output and its distribution Fetal lamb § § CVO is 450 ml/kg/wt RV ejects 2/3 and LV ejects 1/3 of CVO UV flow is 200 ml/mt/kg [45% of CVO] Of this, 110 ml/mt [24%] passes through DV and 90 ml/mt[21%] passes through hepatic circulation
Cardiac output and its distribution Fetal lamb § Portal venous flow forms 7% and of CVO and abdominal IVC blood forms 30% of CVO. § Total venous return to heart from IVC is 315 ml/mt and represents 70% of CVO. § Of this 115 ml/mt [25% of CVO] passes through FO and 200 ml/mt [44%] passes through TV.
Cardiac output and its distribution Fetal lamb § Venous return to heart from SVC is 90 ml/mt/ and represents 21% of CVO most of this passes through tricuspid valve. § RV ejects about 300 ml/mt or about 66% of CVO. § About 35 ml/mt [8% of CVO] enters the pulmonary circulation
![Cardiac output and its distribution Fetal lamb About 265 mlmt 60passes through ductus Cardiac output and its distribution Fetal lamb § About 265 ml/mt [60%]passes through ductus](https://slidetodoc.com/presentation_image_h/288967fb98fa871bf782a1c0f7342b0a/image-44.jpg)
Cardiac output and its distribution Fetal lamb § About 265 ml/mt [60%]passes through ductus arteriosus. § LV ejects 150 ml/kg [ 33% ]. § Of this, 90 ml/mt [20%] distributed to head and upper half and 45 ml/mt [10%]passes through isthmus. § 3% of CVO enters coronary circulation.
Cardiac output and its distribution human fetus § Limited data only is available based on doppler studies. § Umbilical blood flow is 180 ml/mt /kg of estimated fetal weight. § Pulmonary blood flow is estimated to be 75 ml/kg of fetal weight

Cardiac output and its distribution human fetus § CVO appears to be similar to that in lamb, 450 ml/mt/kg fetal weight § Ratio of RV output to LV output is only 1. 2 to 1. 3 as compared to 2: 1 in fetal lamb
Venous return to heart § Umbilical vein gives branches to left lobe of liver and then divides into DV and arcuate vien. § Arcuate vien joins the portal vein and then gives of branches to right lobe of liver. § Left hepatic vein joins the DV at it’s entry to IVC and Right hepatic vein joins the IVC directly.
Venous return to heart § Right lobe of liver poorly oxygenated portal venous blood and left lobe receives well oxygenated umbilical venous blood. § Both lobes receive small contribution of blood from hepatic artery. § Saturation of RHV is lower than that of LHV.
Venous return to heart § Posterior and left stream of IVC blood carries oxygenated blood while anterior and right stream carries poorly oxygenated blood. § Preferential streaming of DV and LHV blood across the foramen ovale and abdominal IVC and RHV blood across the TV.
Venous return to heart § Eustechian valve helps to direct the IVC blood to cross the foramen ovale. § The lower margin of septum secundum [christa dividens] helps to direct the left posterior stream to preferentially across the foramen ovale. § SVC blood is directed aross the TV.

Shunts in fetal circulation § Ductus venosus § Foramen ovale § Ductus arteriosus or aortic isthmus

Shunts in fetal circulation § The blood returning to heart through venacavae and then redistributed to tissues without being delivered to placenta represents effective R to L shunt. § The blood which passes through DV and then reaches DA and goes to placenta without getting distributed to tissues represent effective L to R shunt. § Combined R to L and L to R shunts forms 33% of CVO.
PULMONARY CIRCULATION § Fetal lung does not serve gas exchange function. § PVR is high and PBF is low. § This helps to reduce workload of fetal heart.

PULMONARY CIRCULATION § MPA continues as Ductus and RPA and LPA arise as branches. § Medial layer is composed of smooth muscle predominantly in small pre acinar and large acinar level arteries. § Further branches have no muscular component.
PULMONARY CIRCULATION § PA pressure rises gradually paralleling the rise in aortic pressure. § TPR falls gradually but this fall when correlated with rise in lung weight, there is actually an increase in PVR towards term. § PBF increases gradually.
PULMONARY CIRCULATION § MPA has forward flow throughout systole with a short period of backflow at end of systole. § DA also has forward flow throughout systole. § BPA has forward flow only through initial one third of systole followed by back flow through rest of systole and diastole. § In humans forward flow is more prolonged.
PULMONARY CIRCULATION § Experiments show fetal PBF increases dramatically in response to increase in maternal PO 2. § This response is evident only in latter part of gestation. § Doppler studies indicate similar changes in humans as well.
PULMONARY CIRCULATION § Fetal pulmonary endothelium behaves in a similar fashion as adult endothelium to vasodilators. § Adrenomedullin has a potent and prolonged vasodilatory effect. § Leukotriens may be responsible for maintaining high fetal PVR.
PULMONARY CIRCULATION § Breathing at birth is associated with a marked fall in PVR and rise in PBF. § PA pressure does not fall as rapidly and remain elevated till the Ductus is widely patent. § Once the ductus is closed, PA pressure can vary independent of systemic pressure.
Oxygen exchange function § Higher hemoglobin level in fetus as compared to mother facilitates oxygen uptake by the fetus in the placenta. § Oxygen dissociation curve of fetal red cells is shifted to left as compared to adult red cells. § Hb. F has less affinity towards organic phosphates like 2, 3 DPG and ATP.

Oxygen exchange function § These phosphates that are present in red cells compete with oxygen for binding to hemoglobin. § Affinity of reduced hemoglobin to 2, 3 DPG is higher than that of oxyhemoglobin and this facilitates oxygen delivery at tissue site. § This is not significant in fetal hemoglobin.

Oxygen exchange function § As CO 2 crosses placenta from fetus to mother, it creates a local acidosis. § In the face of decreasing Ph, mothers hemoglobin shows less affinity towards Hb and oxygen release is enhanced. [Bohr effect] § This supports diffusion of more oxygen across the diffusion membrane to fetus.
Oxygen exchange function § As O 2 is released, maternal Hb acts as a buffer that removes H+ from local environment. § This encourages production of bicarbonate from H 2 O and CO 2 thereby reducing local PC 02 and facilitating diffusion of CO 2 from fetus.
Post natal changes § Gas exchange function is transferred from placenta to the lungs. § Separation of systemic and pulmonary circulations § Increased metabolism to maintain body temperature and hence increased cardiac output.
Post natal changes in various circulatory beds § Coronary Blood flow decreases dramatically as the oxygen content increases. § Cerebral circulation also behaves in the same fashion as coronary circulation.
Post natal changes in various circulatory beds § Skin blood flow is high in utero as the vessels are dilated because the skin is exposed to warm amniotic fluid. § Cutaneous vasoconstriction occurs post natally as evaporation from skin starts. § Cutaneous flow falls and the vascular resistance increaes.
Post natal changes in various circulatory beds § Hepatic blood flow falls rapidly post natally with reduction in umbilical venous return and then increases as the GI flow is re established. § Hepatic blood flow progressively increases after birth and by 7 days after birth reaches a level of 250 ml/minute /100 g by which time there is no flow through ductus venosus.
Changes in Cardiac output § Oxygen consumption increases from 6 -8 ml/mt/kg body weight pre natally to 15 – 20 ml/mt/kg post natally. § CVO of fetal lamb is 450 ml/mt/kg. § C. O of neonatal lamb is 300 -425 ml/mt/kg. So the CVO will be 600 -850 ml/mt/kg. § So the increase is 1. 5 to 2 times.
Changes in Cardiac output Mechanisms § Neonate has to increase the metabolism to increase the body temperature as it is exposed to external temperature. § Improved diastolic function due to removal of compression by maternal organs and uterus causes increased cardiac filling and hence the cardiac output.
Changes in Cardiac output Mechanisms § Perinatal but not post natal increase in thyroid hormones is the principal mechanism for increase in cardiac output. § Improvement in myocardial growth and maturation brought about by cortisol may also play important role.

Changes in hemoglobin and tissue oxygen delivery § Human new born has a high hemoglobin level (about 16 g/dl) so that the oxygen carrying capacity is quiet high and the total amount of oxygen transported to tissues is quiet high. § Since the Hb F levels are still high facilitation at tissue site is not as great as in adults. § Over the first 8 -10 weeks after the birth, Hb concentration falls to 10 -11 g/dl. This is accompanied by loss of Hb F and almost 100% is adult type.
Regulation of fetal circulation § Arterial baroreceptors are funtional in fetus from early in the gestation § Near term, it is as sensitive as adults in fetal lambs. § Chemoreceptors are active only in latter part of gestation.

Fetal circulation in pathological conditions
Fetal circulation in pathological conditions § Development of a structural abnormality will modify the fetal circulation. § This will affect the development of other components and can lead to other defects. § The impact of a defect will depend on it’s severity and time of gestation at which it occurs.

Fetal circulation in pathological conditions § Many of the defects, though it modifies the circulation, will not significantly affect fetal perfusion and hence the growth and development. § This is because of the presence of shunts and mixing of blood. § Fetus tolerates the obstructive lesions very much. § Fetal circulation is jeopardized by regurgitant lesions and myocardial disease.

Septal defects § They in general do not modify the fetal circulation significantly. § VSD may have a transient left to right shunt in systole. § In OP ASD, due to close proximity of defect with TV, more than normal amount of SVC blood may enter the LA.

Septal defects § In atrioventricular septal defects, the obligatory flow from LV to RA will result in decrease in LV output and an increase in RV output. § This will reduce the flow across the isthmus and can predispose to coarctation. § It is the degree of severity of AV valve lesion and regurgitation which will determine the outcome.

LVOT Obstruction § Severe obstruction developing early result in a small LV with an increased mass. § RV is able to compensate fully if LVOTO develops slowly.
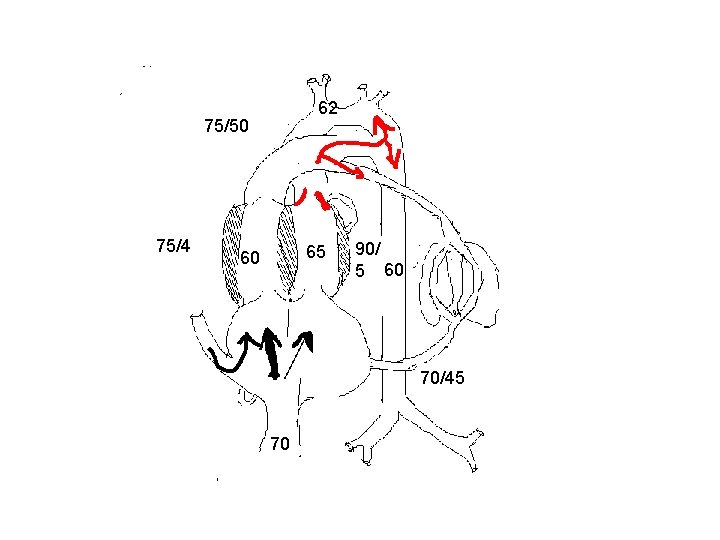
LVOT Obstruction § SVC flow courses normally. § Majority of IVC blood flow crosses TV to RV. § Flow across the ductus increases. § PBF has higher than normal saturation.
LVOT obstruction § Decrease in saturation between DA and AA. § LV systolic pressure increases slightly but not EDP. § A retrograde flow in arch and ascending aorta indicates severe obstruction.
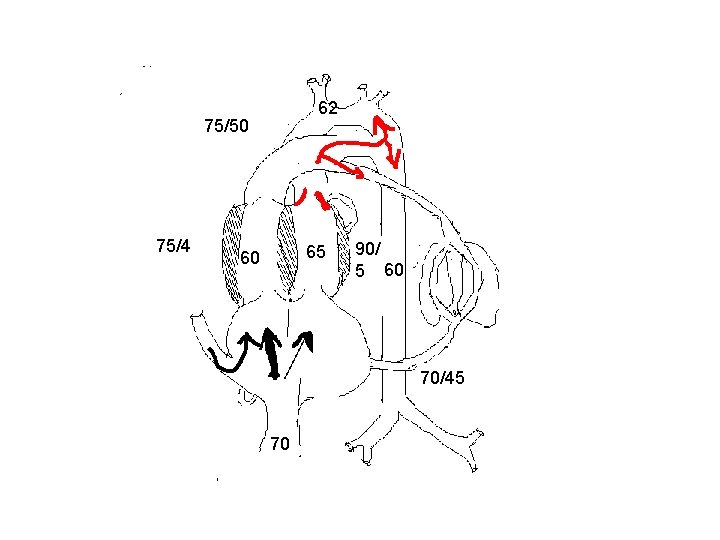
62 75/50 75/4 65 60 90/ 5 60 70/45 70
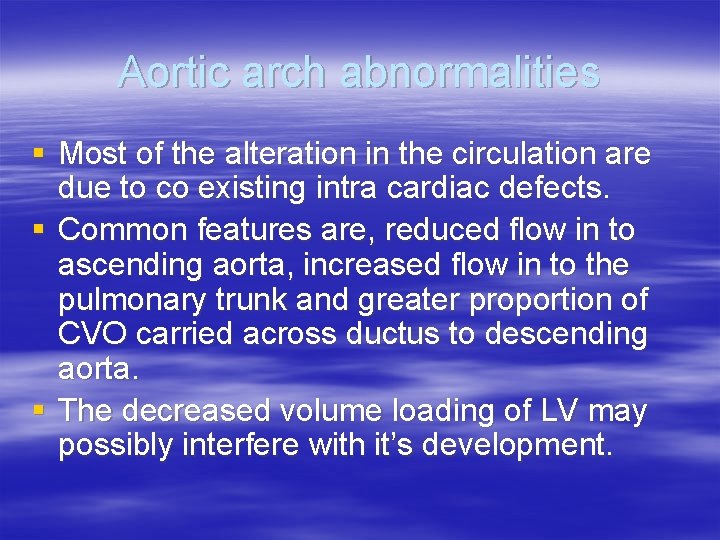
Aortic arch abnormalities § Most of the alteration in the circulation are due to co existing intra cardiac defects. § Common features are, reduced flow in to ascending aorta, increased flow in to the pulmonary trunk and greater proportion of CVO carried across ductus to descending aorta. § The decreased volume loading of LV may possibly interfere with it’s development.
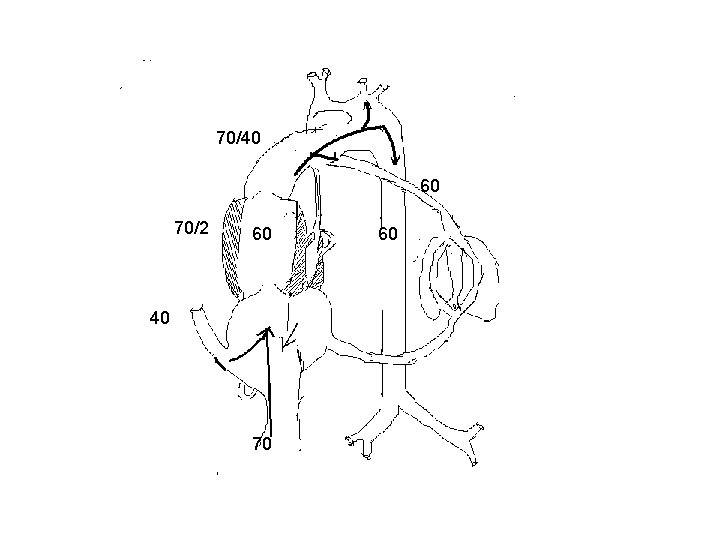
Mitral and aortic atresia § All blood must pass through RV and ductus has to provide for both AA and DA blood flow. § Complete mixing of blood occurs in RA and saturation in PA, AA and DA are all same. § If the foramen ovale is sufficiently large and ductus accomodates whole of systemic blood flow, there will be no significant interference with intrauterine development and survival.
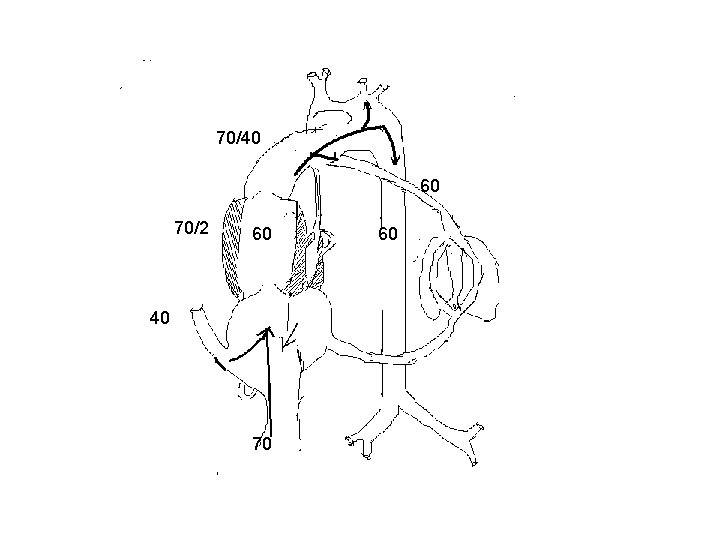
70/40 60 70/2 60 40 70 60
Mitral and aortic atresia § If the foramen ovale is restrictve, severe pulmonary venous hypertension develops. § If the ductus does not enlarge to accommodate the whole of systemic blood flow increased blood flow to lungs and pulmonary hypertension develops. § Both these can lead to increased development of smooth muscle in the pulmonary vasculature.

RVOTO with intact IVS § In rapidly developing RVOTO, RV and LV cannot compensate for and the CVO falls. § If RVOTO developing slowly, both LV and RV can compensate for and CVO is maintained. § In pulmonary atresia, total cardiac output is carried by the left heart.

63 63 63 100/4 63 70/3 40 70

RVOTO with intact IVS § In pulmonary atresia, all systemic venous blood is carried to left side through foramen ovale and all blood supply to DA is provided through isthmus. § Larger than normal foramen ovale, left sided chambers, AA and aortic isthmus.
RVOTO with intact IVS § If severe RVOTO develops early in gestation, the flow through the ductus is reversed and carries only 8 to 10 % of cardiac output. § The ductus will be narrower and will make an acute inferior angle with aorta. § The ductus will remain patent for longer than normal duration.
RVOTO with intact IVS § If the fetus develops significant TR, RV pressure remains low and myocardial sinusoids and coronary fistulae do not develop. § If TR does not develop, significant RV systolic pressure develops and if occurs early in gestation, intramyocardial sinusoids and coronary fistulae develop.
TAPVC § Usually does not affect the development of fetus. § If whole of PV return drains to SVC, LV will be totally free of PV blood and hence will be of higher saturation. § Left atrium and left ventricle will be relatively small in TAPVC.
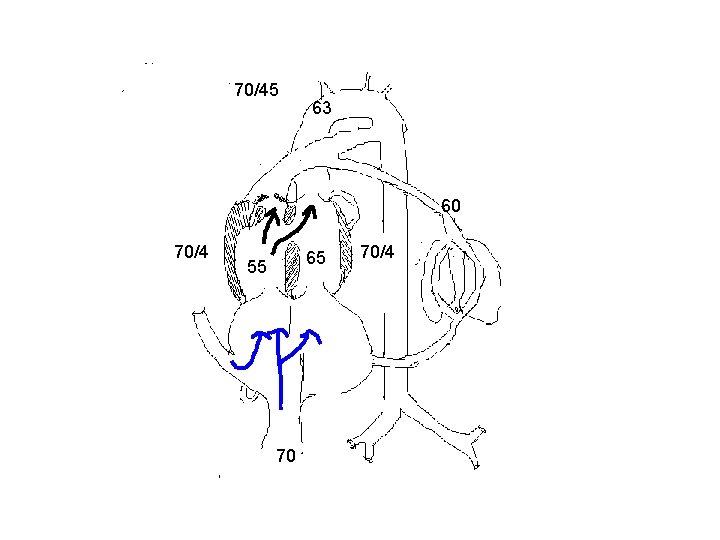
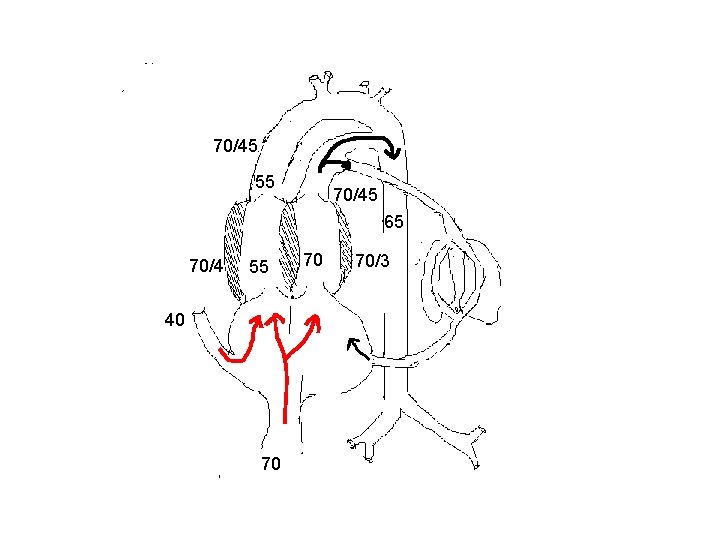
TOF and related disorders § Does not appear to affect fetal circulation adversely. § The volume and direction of flow across the PA and ductus are dependant on the severity of obstruction. § Total flow through the ductus will be reduced considerably.
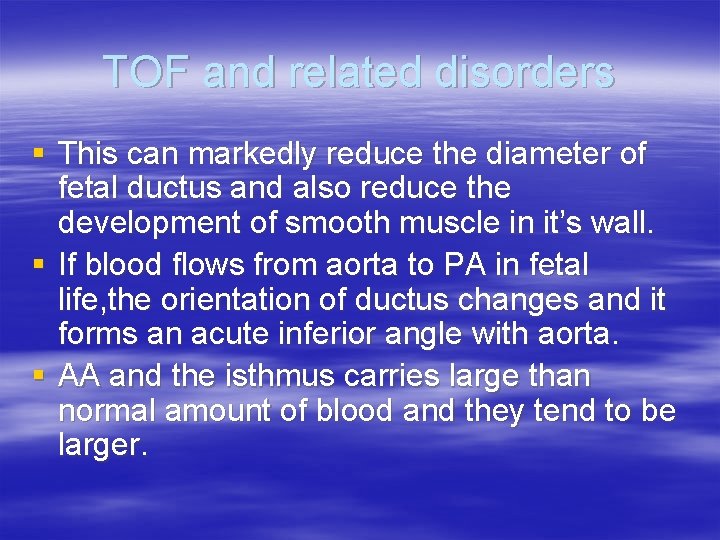
TOF and related disorders § This can markedly reduce the diameter of fetal ductus and also reduce the development of smooth muscle in it’s wall. § If blood flows from aorta to PA in fetal life, the orientation of ductus changes and it forms an acute inferior angle with aorta. § AA and the isthmus carries large than normal amount of blood and they tend to be larger.
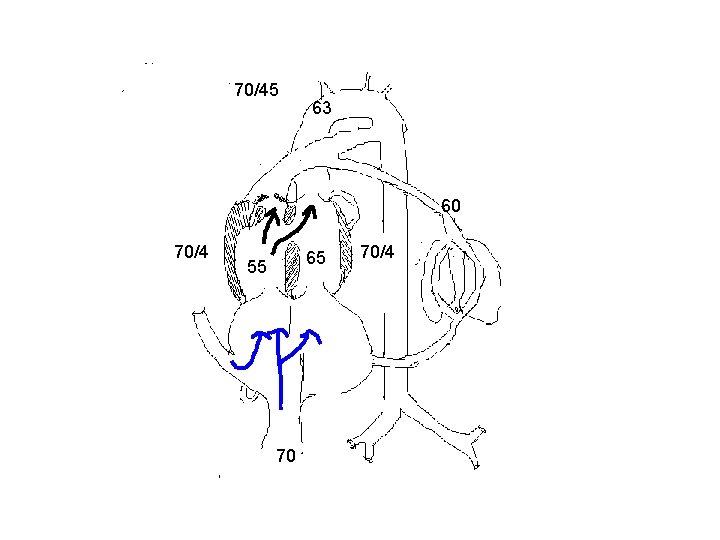
70/45 63 60 70/4 65 55 70 70/4
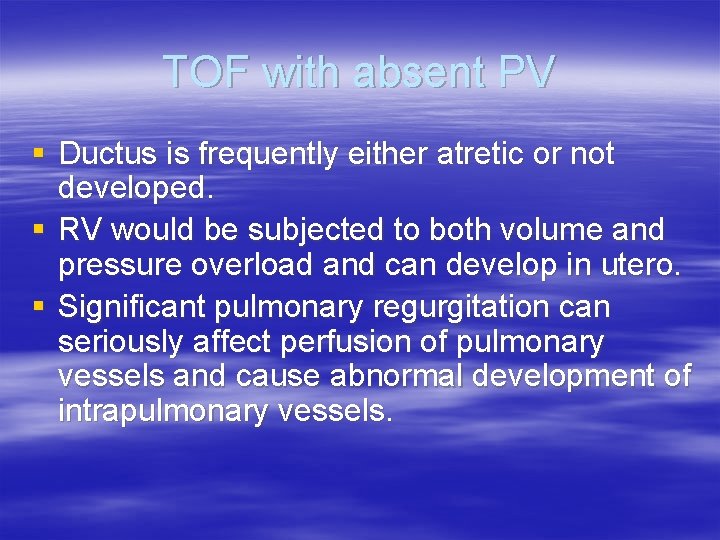
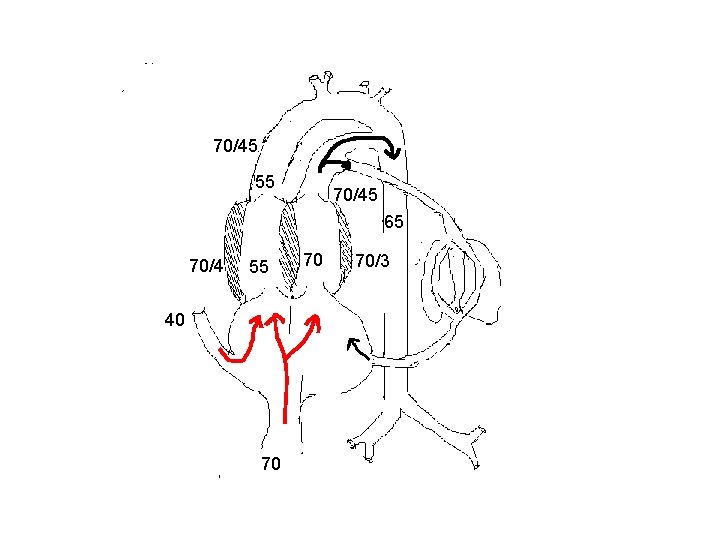
TOF with absent PV § Ductus is frequently either atretic or not developed. § RV would be subjected to both volume and pressure overload and can develop in utero. § Significant pulmonary regurgitation can seriously affect perfusion of pulmonary vessels and cause abnormal development of intrapulmonary vessels.

Aortopulmonary transposition § Compatible with fetal survival and normal intrauterine development. § Does not affect the pattern of venous return. § Blood with higher oxygen saturation will go to lungs. This will reduce the PVR and hence increase in PBF.

Aortopulmonary transposition § This will reduce the blood flow across the ductus and increases the flow across the isthmus. § Blood with lower oxygen saturation perfuses coronary and cerebral circulation. § Hence cerebral and coronary blood flow are increased considerably.
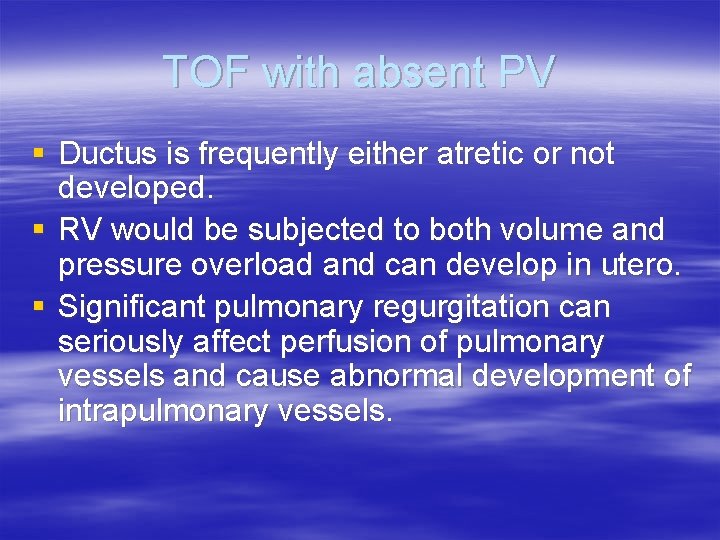
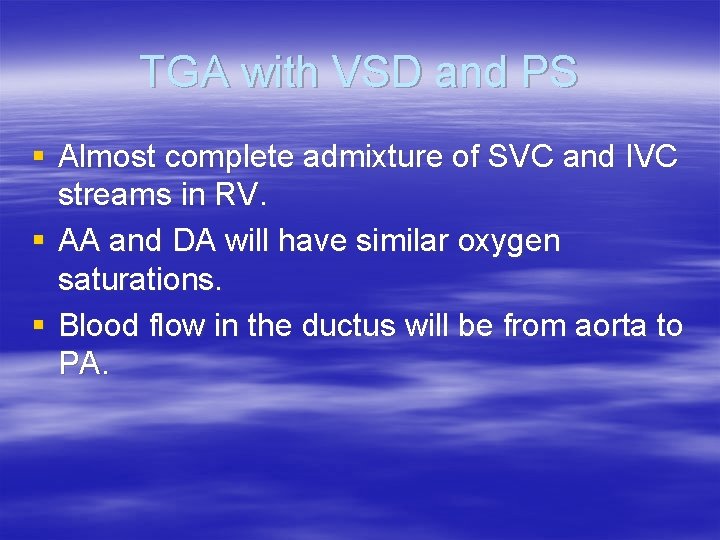
70/45 55 70/45 65 70/4 55 40 70 70 70/3

TGA with VSD § Bi directional shunting occur depending on after load of each ventricle. § The difference in saturation between AA and DA will be lesser.
TGA with VSD and PS § Almost complete admixture of SVC and IVC streams in RV. § AA and DA will have similar oxygen saturations. § Blood flow in the ductus will be from aorta to PA.

70/45 65 65 70/4 55 40 70 65

Truncus arteriosus § Various degree of mixing occurs just above the semilunar valve. § Degree of mixing depends on morphology. In type 1, there is differential streaming of blood and in others there will be complete mixing. § Ductus is usually small or absent and increased flow traverses through isthmus and it is large.
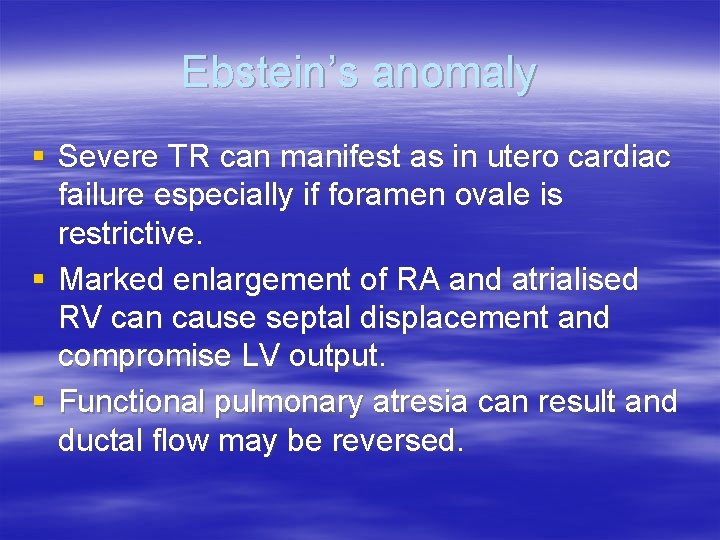
Ebstein’s anomaly § Severe TR can manifest as in utero cardiac failure especially if foramen ovale is restrictive. § Marked enlargement of RA and atrialised RV can cause septal displacement and compromise LV output. § Functional pulmonary atresia can result and ductal flow may be reversed.
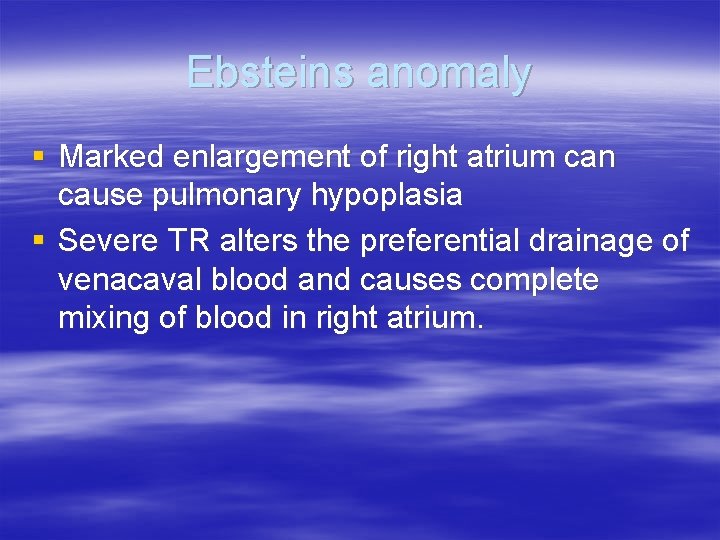
Ebsteins anomaly § Marked enlargement of right atrium can cause pulmonary hypoplasia § Severe TR alters the preferential drainage of venacaval blood and causes complete mixing of blood in right atrium.

Tricuspid atresia § All of the venous return traverses foramen ovale and it is considerably larger than normal. § Complete admixture of blood in the left atrium § It is compatible with normal intrauterine development and survival.
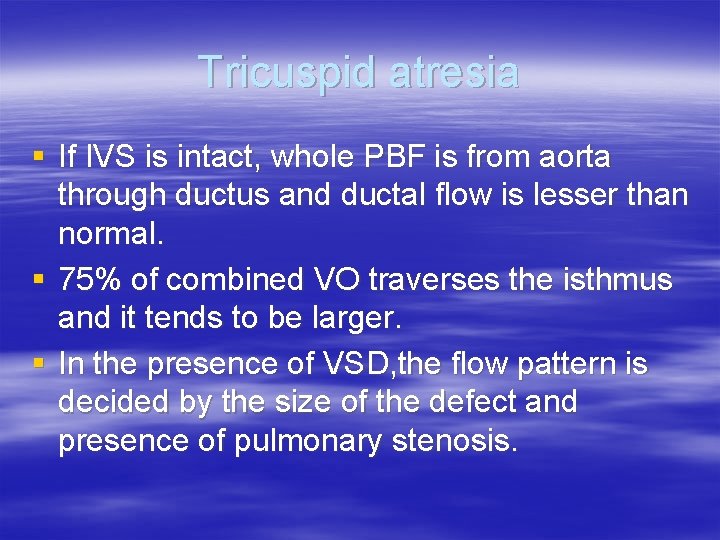
Tricuspid atresia § If IVS is intact, whole PBF is from aorta through ductus and ductal flow is lesser than normal. § 75% of combined VO traverses the isthmus and it tends to be larger. § In the presence of VSD, the flow pattern is decided by the size of the defect and presence of pulmonary stenosis.

 Single vs double circulatory system
Single vs double circulatory system Single circulation and double circulation
Single circulation and double circulation Alveoli
Alveoli Placental circulation flow chart
Placental circulation flow chart Fetal circulation flow chart
Fetal circulation flow chart 3 shunts of fetal circulation
3 shunts of fetal circulation Fetal circulation definition
Fetal circulation definition Fetal circulation
Fetal circulation Fetal circulation ppt flowchart
Fetal circulation ppt flowchart Bharathi viswanathan
Bharathi viswanathan Health promotion and levels of disease prevention
Health promotion and levels of disease prevention Health promotion and levels of disease prevention
Health promotion and levels of disease prevention Romanticism is disease classicism is health
Romanticism is disease classicism is health The human body in health and disease chapter 2 answer key
The human body in health and disease chapter 2 answer key Biomedical concept of health
Biomedical concept of health Introduction to community medicine
Introduction to community medicine The human body in health and disease chapter 2 answer key
The human body in health and disease chapter 2 answer key Chapter 2 the human body in health and disease
Chapter 2 the human body in health and disease Conclusion of health and safety
Conclusion of health and safety Conclusion of health and disease
Conclusion of health and disease Chapter 37 respiration circulation and excretion
Chapter 37 respiration circulation and excretion Vorticity and circulation
Vorticity and circulation Chapter 14 circulation and blood vessels
Chapter 14 circulation and blood vessels Triple response and cutaneous circulation
Triple response and cutaneous circulation Micro and macro circulation
Micro and macro circulation Chapter 42 circulation and gas exchange
Chapter 42 circulation and gas exchange Chapter 21 blood vessels and circulation
Chapter 21 blood vessels and circulation Bat characteristics
Bat characteristics Health and social care component 3 health and wellbeing
Health and social care component 3 health and wellbeing Two circulation syndrome
Two circulation syndrome Blood flow circuit
Blood flow circuit Circulatory pathway
Circulatory pathway Circulation of air masses
Circulation of air masses Portal blood circulation
Portal blood circulation Plan de circulation usine
Plan de circulation usine Teeth of herbivorous animals
Teeth of herbivorous animals Deportation definition ap human geography
Deportation definition ap human geography Types of vertical circulation
Types of vertical circulation Hepatic acinus
Hepatic acinus Circulation extracorporelle
Circulation extracorporelle Secretion of bicarbonate ions
Secretion of bicarbonate ions Phylum fish
Phylum fish Figure 12-2 layers of the heart wall
Figure 12-2 layers of the heart wall Estuary circulation
Estuary circulation Estuary circulation
Estuary circulation Single cell model of atmospheric circulation
Single cell model of atmospheric circulation Components of the bile
Components of the bile Chapter 34 circulation in humans concept mapping answer key
Chapter 34 circulation in humans concept mapping answer key Function of arterioles
Function of arterioles Figure 11-7 veins labeled
Figure 11-7 veins labeled Chapter 11 the cardiovascular system figure 11-10 answers
Chapter 11 the cardiovascular system figure 11-10 answers Circulates air between 60-90 latitudes
Circulates air between 60-90 latitudes Convection circulation
Convection circulation Internal energy formula
Internal energy formula A. profunda brachii
A. profunda brachii One pipe circulation
One pipe circulation Confidential not for circulation
Confidential not for circulation Circulation cells
Circulation cells Circulation sanguine
Circulation sanguine Guest circulation pattern
Guest circulation pattern Atmospheric circulation
Atmospheric circulation Chapter 34 section 2 the respiratory system
Chapter 34 section 2 the respiratory system Salur darah
Salur darah Figure 11-9 is a diagram of the hepatic portal circulation
Figure 11-9 is a diagram of the hepatic portal circulation Mojo magazine circulation
Mojo magazine circulation Vacate hyperemia
Vacate hyperemia Arteries of the systemic circulation
Arteries of the systemic circulation Worm like amphibian
Worm like amphibian A airway b breathing c circulation
A airway b breathing c circulation Cross circulation drying
Cross circulation drying Characterstics of leadership
Characterstics of leadership Poiseuille's law in blood flow
Poiseuille's law in blood flow Arteries of the systemic circulation
Arteries of the systemic circulation Arteries of the systemic circulation
Arteries of the systemic circulation Arteries of the systemic circulation
Arteries of the systemic circulation Human blood circulation
Human blood circulation Clavipectoral fascia
Clavipectoral fascia Ekman pumping
Ekman pumping Circulation practitioner
Circulation practitioner Magazine circulation software
Magazine circulation software Loeffler boiler
Loeffler boiler Functional circulation
Functional circulation Posterior tibial pulse location
Posterior tibial pulse location Disadvantages of short tube evaporator
Disadvantages of short tube evaporator Forced circulation reboiler
Forced circulation reboiler Structure of blood vessels
Structure of blood vessels Types of circulation in the body
Types of circulation in the body Heart cycle animation
Heart cycle animation Coronary circulation of heart
Coronary circulation of heart Yakima herald republic circulation
Yakima herald republic circulation Normal walker circulation
Normal walker circulation Zonation and succession
Zonation and succession Atlantic meridional overturning circulation
Atlantic meridional overturning circulation Systemic artery
Systemic artery Porifera excretion
Porifera excretion Precapillary sphincter
Precapillary sphincter Circulation 511
Circulation 511 Circulation in amphibians
Circulation in amphibians Circulation in reptiles
Circulation in reptiles Global circulation patterns
Global circulation patterns Weebly
Weebly The thermohaline circulation belt _____.
The thermohaline circulation belt _____. Pulmonary circuit and systemic circuit
Pulmonary circuit and systemic circuit Abcde ehbo
Abcde ehbo Neuroendocrine reflex
Neuroendocrine reflex Small saphenous vein
Small saphenous vein Schma
Schma Signe du flot genou
Signe du flot genou