Emergency Anaesthesia for the Head Injured Patient for




















- Slides: 93
"Emergency Anaesthesia for the Head Injured Patient for non head injury procedures" Dr. J. Balavenkat MD, DA Consultant Anaesthesiologist Ganga Hospital Coimbatore
Man kills Man … On the Roads!.
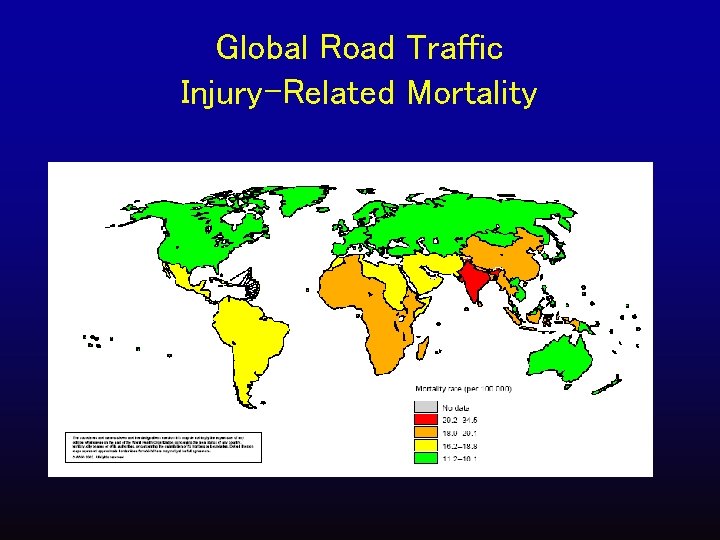
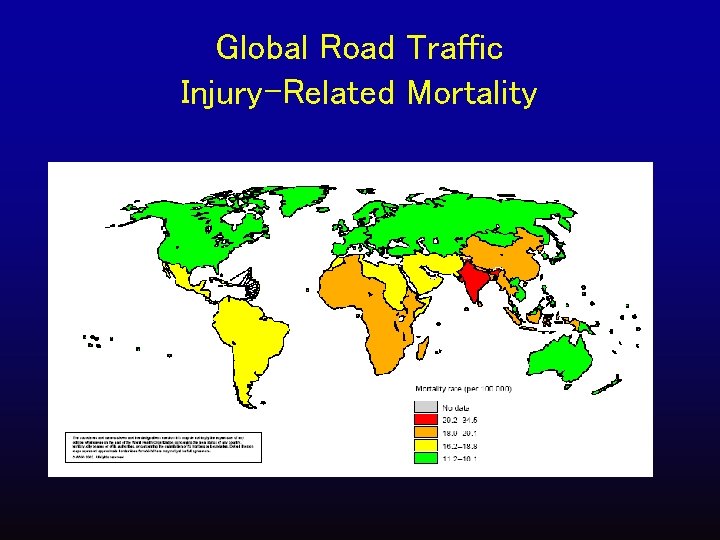
Global Road Traffic Injury-Related Mortality
By 2050, India will have the greatest number of automobiles on the planet, overtaking the United States
Before we coclude this two day meet about 500 people would have died and more than 5000 injured in India

If you are between 15 -45 years of age you have more chance of dying due to an accident than any other disease
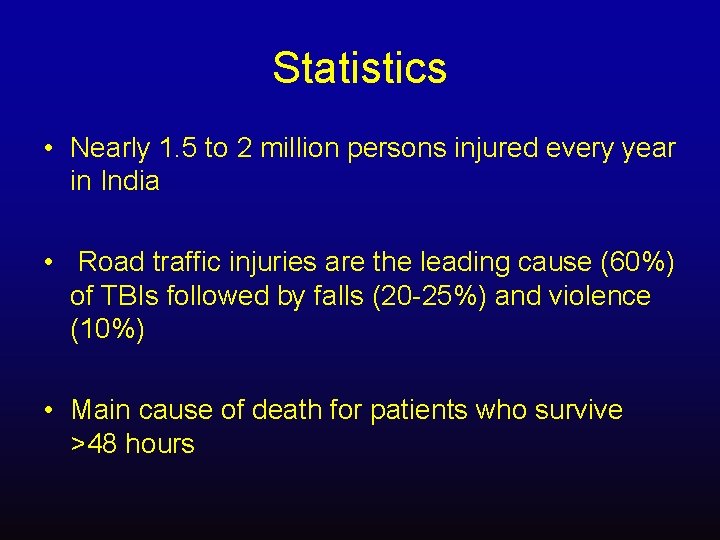
Statistics • Nearly 1. 5 to 2 million persons injured every year in India • Road traffic injuries are the leading cause (60%) of TBIs followed by falls (20 -25%) and violence (10%) • Main cause of death for patients who survive >48 hours
• Initial Resuscitation and Investigation protocol? • CT Scan : Timing in an unstable patient
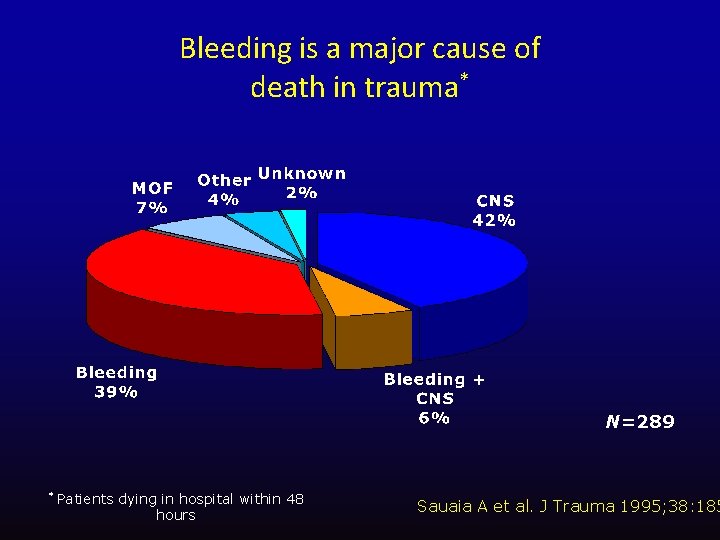
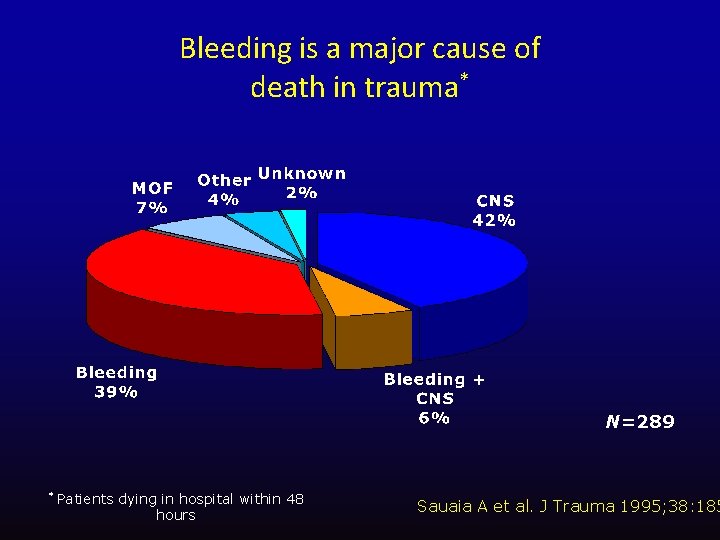
Bleeding is a major cause of death in trauma* N=289 * Patients dying in hospital within 48 hours Sauaia A et al. J Trauma 1995; 38: 185
Contentious Issues…. . • Role of hyperventilation • Role of hypothermia • Role of Glucose level in the neurological outcome • Best fluid to resuscitate • Cerebral protective strategies.
Pathophysiology of TBI is complex. But you do not need to know the details Simple, early and focussed interventions are effective in preventing secondary injury
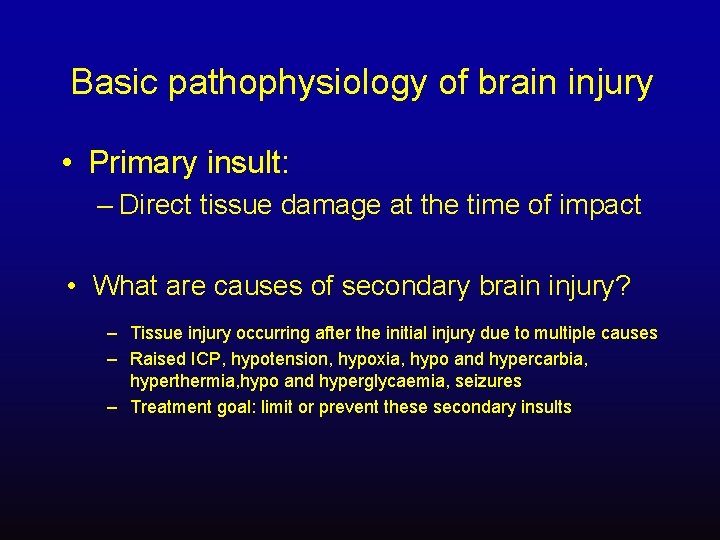
Basic pathophysiology of brain injury • Primary insult: – Direct tissue damage at the time of impact • What are causes of secondary brain injury? – Tissue injury occurring after the initial injury due to multiple causes – Raised ICP, hypotension, hypoxia, hypo and hypercarbia, hyperthermia, hypo and hyperglycaemia, seizures – Treatment goal: limit or prevent these secondary insults
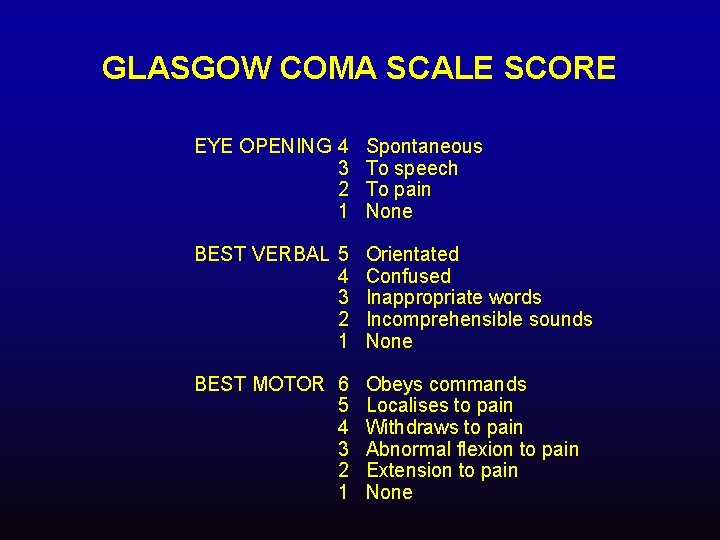
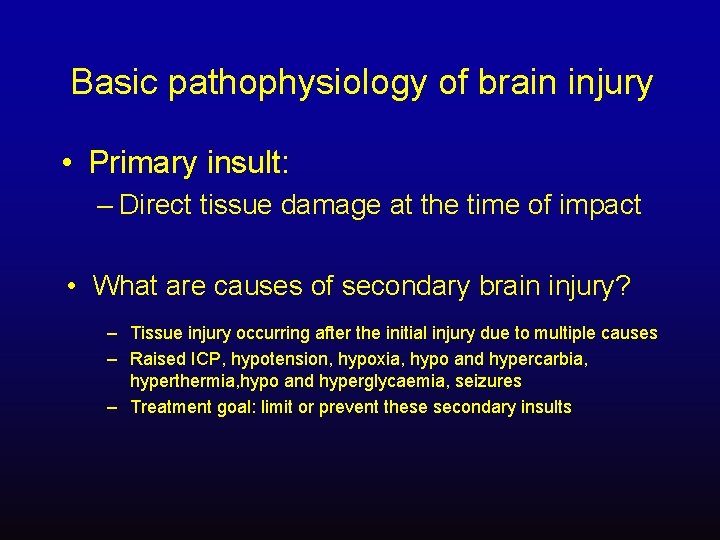
GLASGOW COMA SCALE SCORE EYE OPENING 4 3 2 1 Spontaneous To speech To pain None BEST VERBAL 5 4 3 2 1 Orientated Confused Inappropriate words Incomprehensible sounds None BEST MOTOR 6 5 4 3 2 1 Obeys commands Localises to pain Withdraws to pain Abnormal flexion to pain Extension to pain None
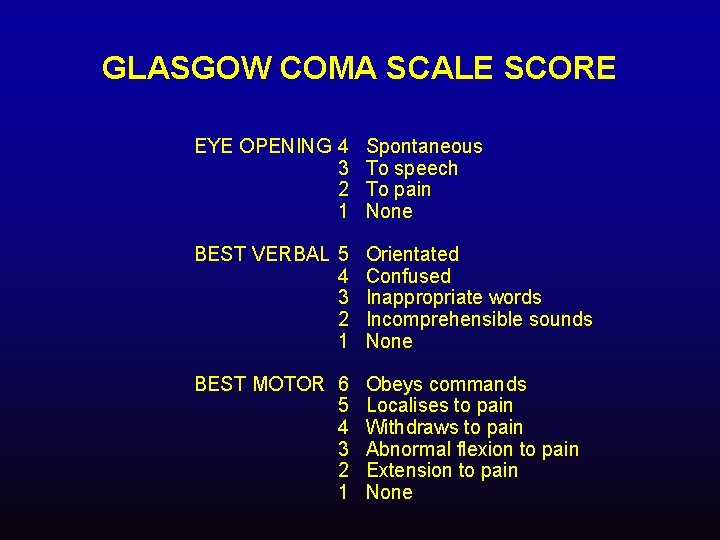
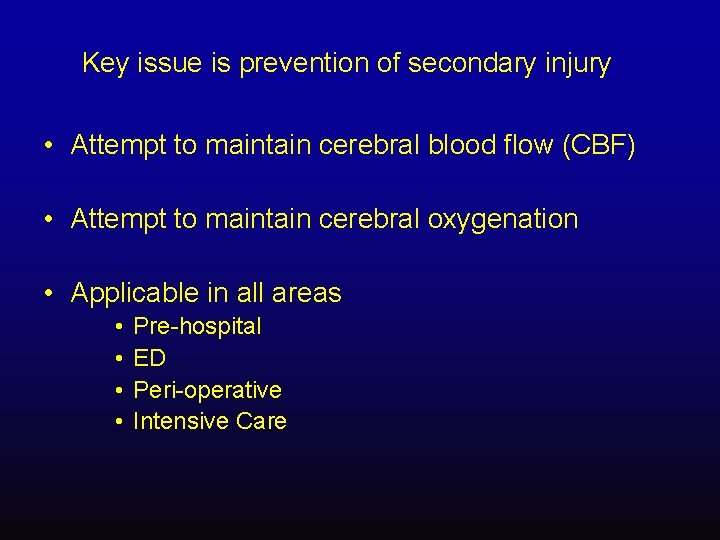
Key issue is prevention of secondary injury • Attempt to maintain cerebral blood flow (CBF) • Attempt to maintain cerebral oxygenation • Applicable in all areas • • Pre-hospital ED Peri-operative Intensive Care
Immediate management • A, B, C approach • Airway management must be with C-spine immobilisation and control • If GCS ≤ 8 should be intubated and ventilated to low normocapnia [4 -4. 5 k. Pa, 30 -35 mm. Hg] • A rapid sequence induction/intubation is appropriate, but avoid ICP ↑ • Circulation must be supported with IV volume loading and a MAP of 90 mm. Hg maintained
Intubation of the patient with Brain Injury • Record GCS and pupils before RSI • Rapid Sequence oro-tracheal intubation: – – – In line stabilization of C-spine Pre-oxygenation with 100% O 2 Induction agent? NMB: suxamethonium or rocuronium? OGT or NGT?

Actions after tracheal intubation? • Confirm TT and gastric tube placement (clinical and CXR) • Ventilate, aiming for Pa. CO 2 4 -4. 5 k. Pa (30 -35 mm. Hg) • Oxygenate, using PEEP if necessary • Pa. O 2 > 13 k. Pa (97 mm. Hg) Sa. O 2 >94% • Cardiovascular assessment and stabilization • IV volume • MAP ≥ 70 -90 mm. Hg
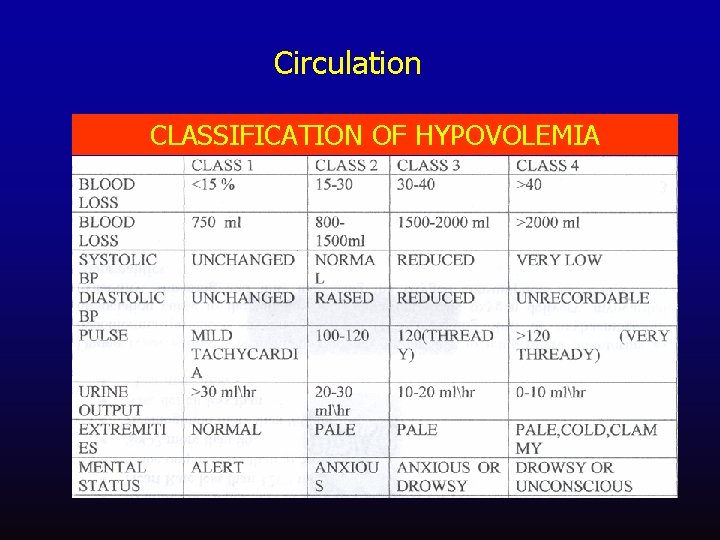
Circulation • • Hypotensive bleeding patients Early Vs Delayed Fluid Resuscitation Large Vs Small Volume resuscitation Crystalloids or colloids? To Transfuse blood and blood products early or late?
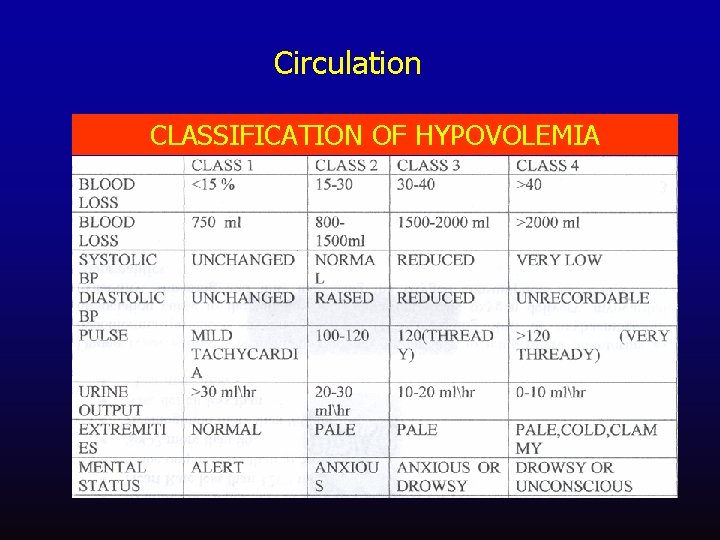
Circulation CLASSIFICATION OF HYPOVOLEMIA
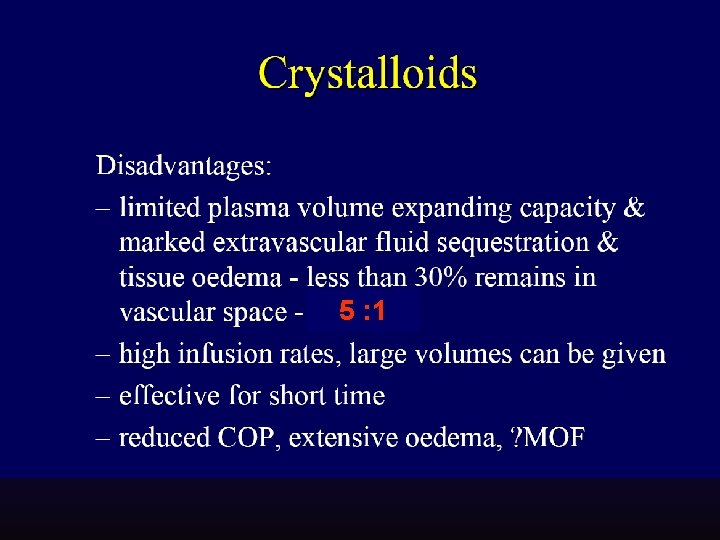
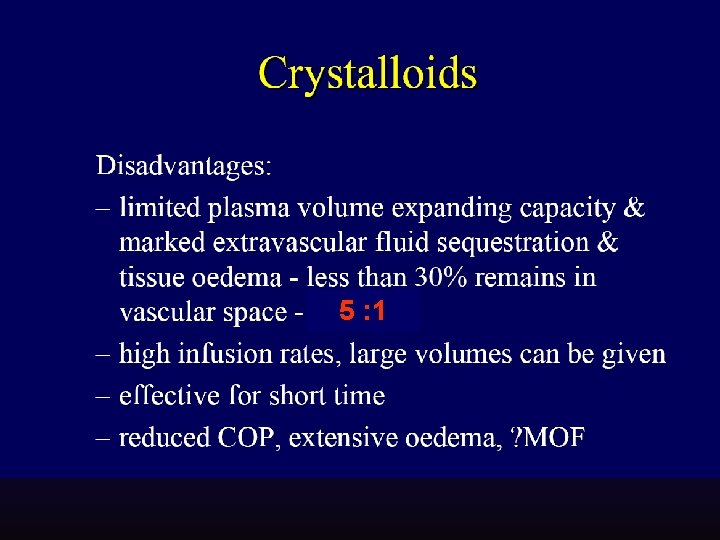
5 : 1
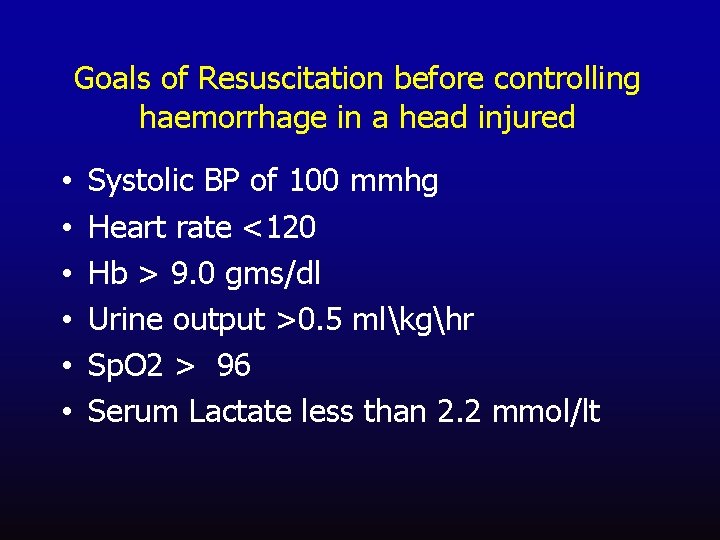
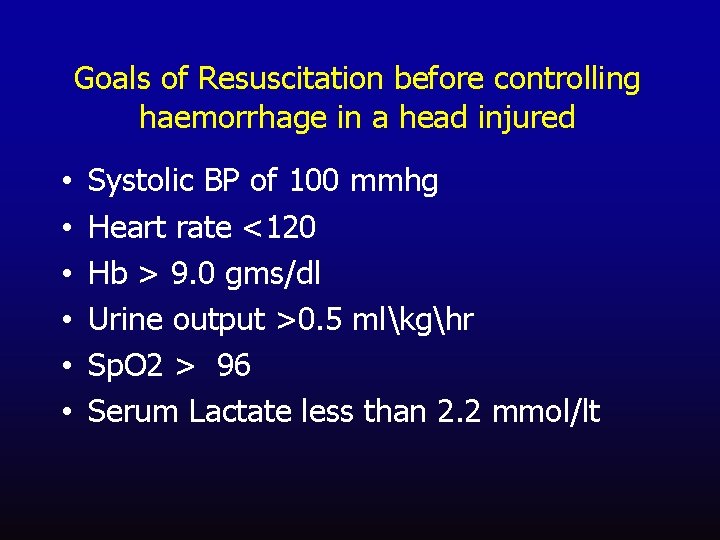
Goals of Resuscitation before controlling haemorrhage in a head injured • • • Systolic BP of 100 mmhg Heart rate <120 Hb > 9. 0 gms/dl Urine output >0. 5 mlkghr Sp. O 2 > 96 Serum Lactate less than 2. 2 mmol/lt
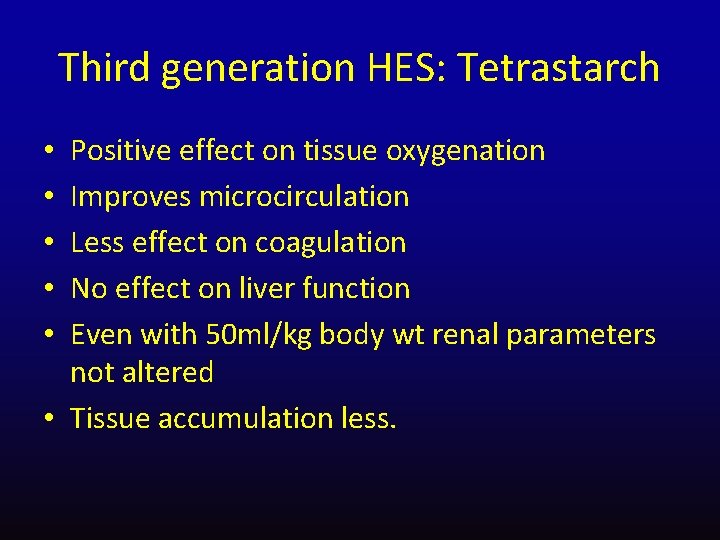
Third generation HES: Tetrastarch Positive effect on tissue oxygenation Improves microcirculation Less effect on coagulation No effect on liver function Even with 50 ml/kg body wt renal parameters not altered • Tissue accumulation less. • • •
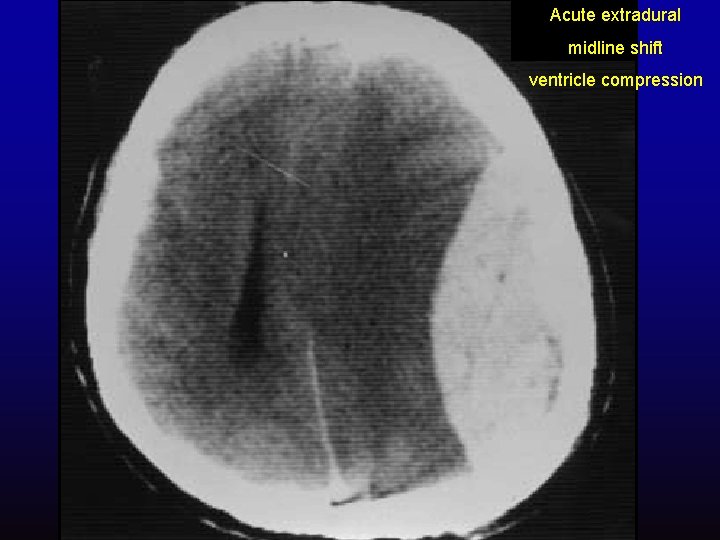
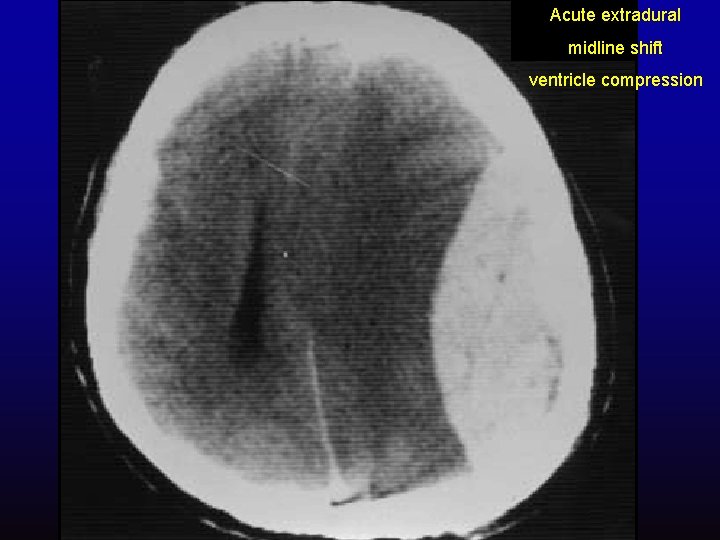
Acute extradural midline shift ventricle compression
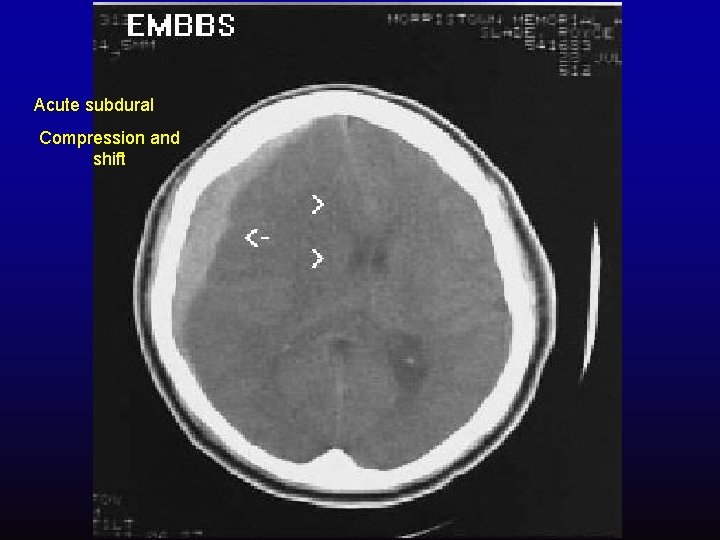
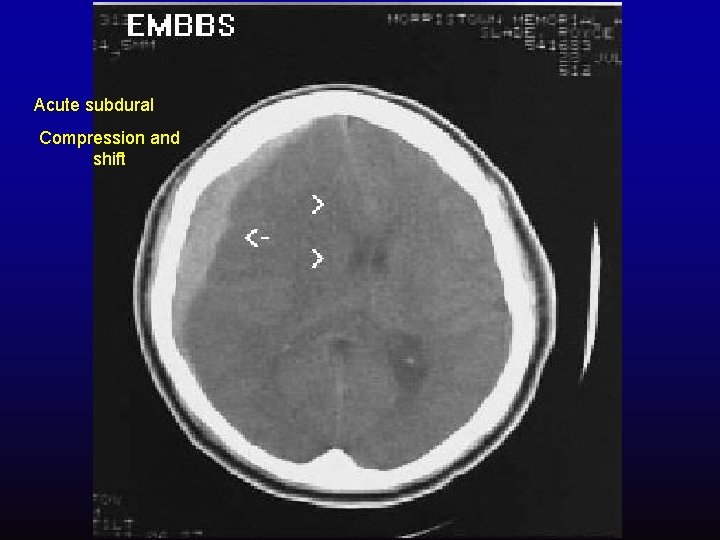
Acute subdural Compression and shift


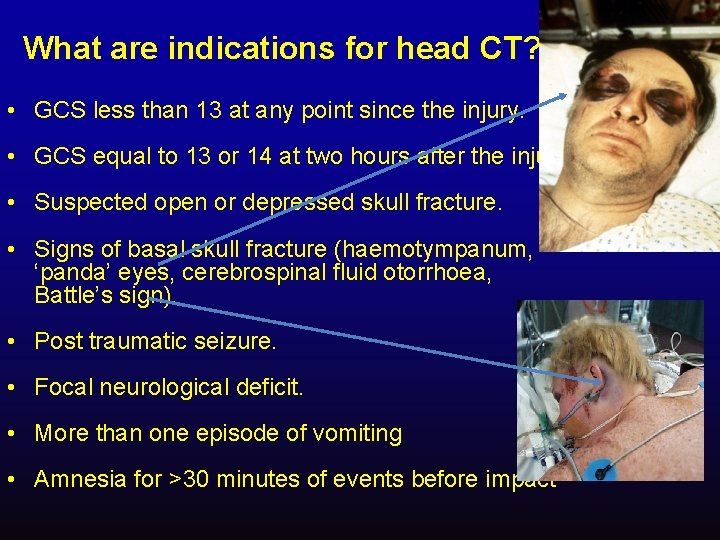
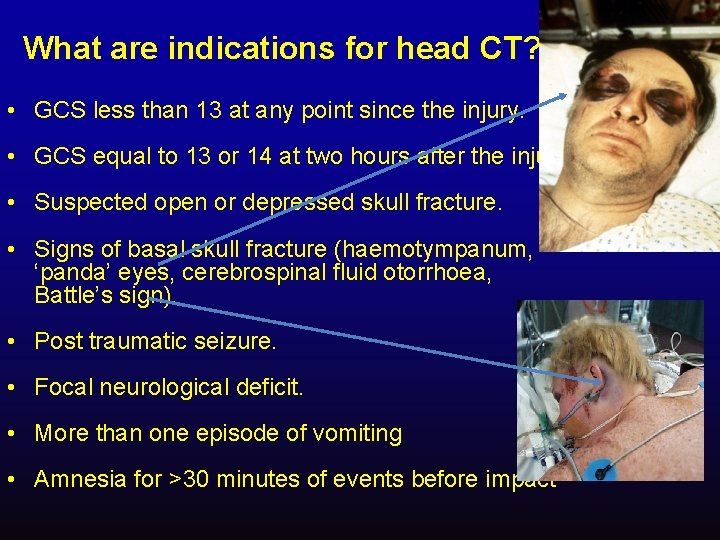
What are indications for head CT? • GCS less than 13 at any point since the injury. • GCS equal to 13 or 14 at two hours after the injury. • Suspected open or depressed skull fracture. • Signs of basal skull fracture (haemotympanum, ‘panda’ eyes, cerebrospinal fluid otorrhoea, Battle’s sign). • Post traumatic seizure. • Focal neurological deficit. • More than one episode of vomiting • Amnesia for >30 minutes of events before impact
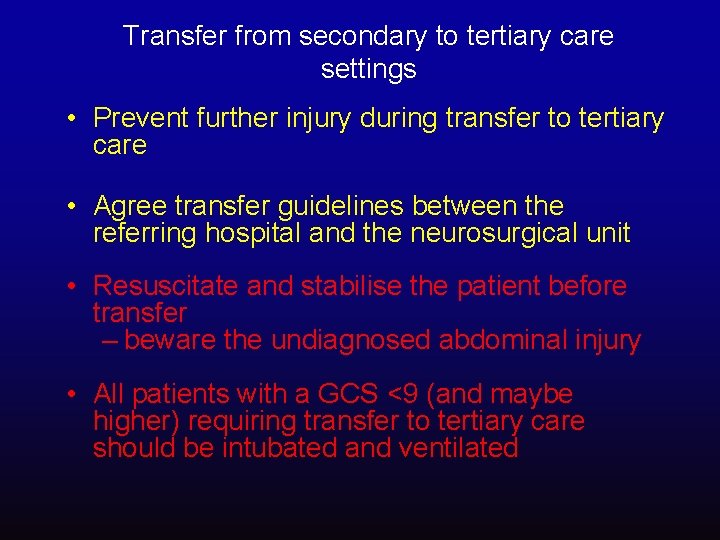
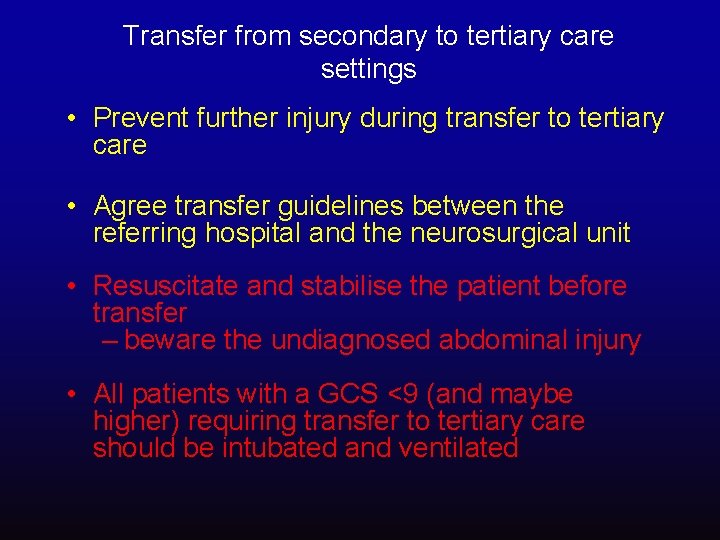
Transfer from secondary to tertiary care settings • Prevent further injury during transfer to tertiary care • Agree transfer guidelines between the referring hospital and the neurosurgical unit • Resuscitate and stabilise the patient before transfer – beware the undiagnosed abdominal injury • All patients with a GCS <9 (and maybe higher) requiring transfer to tertiary care should be intubated and ventilated
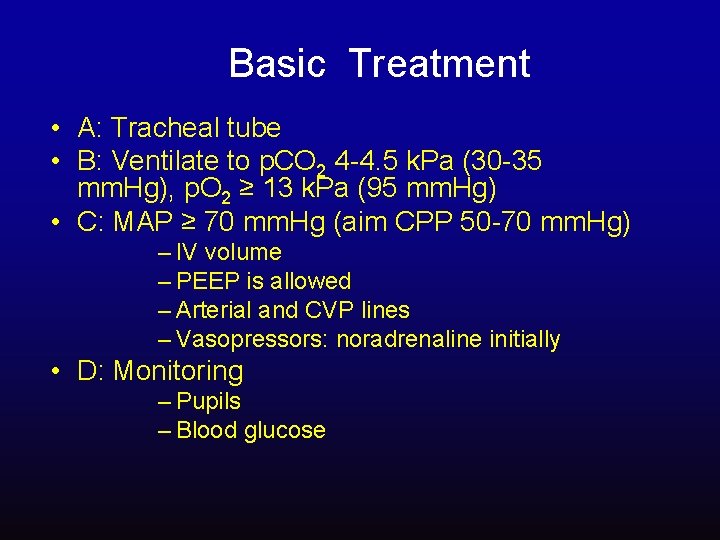
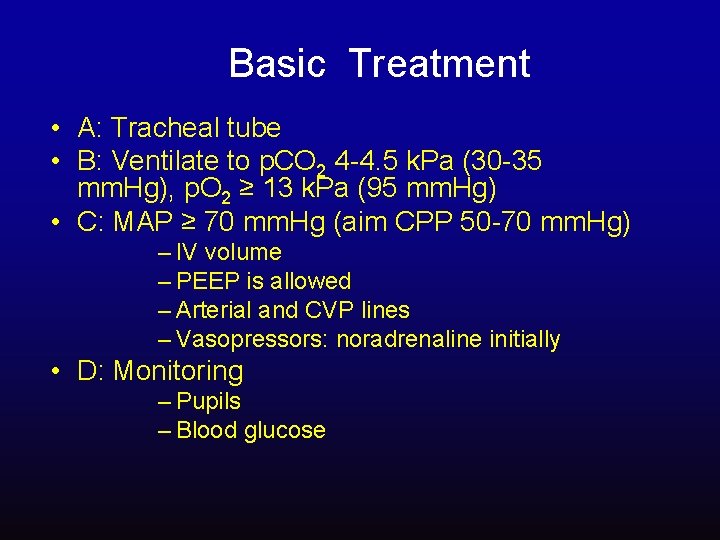
Basic Treatment • A: Tracheal tube • B: Ventilate to p. CO 2 4 -4. 5 k. Pa (30 -35 mm. Hg), p. O 2 ≥ 13 k. Pa (95 mm. Hg) • C: MAP ≥ 70 mm. Hg (aim CPP 50 -70 mm. Hg) – IV volume – PEEP is allowed – Arterial and CVP lines – Vasopressors: noradrenaline initially • D: Monitoring – Pupils – Blood glucose
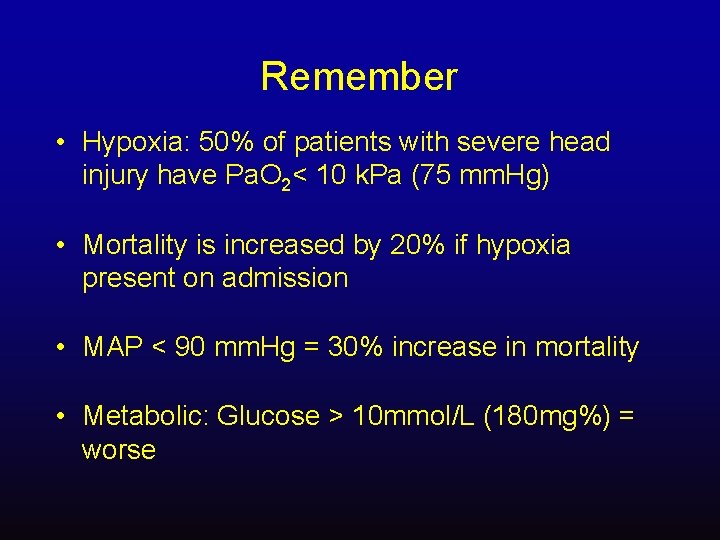
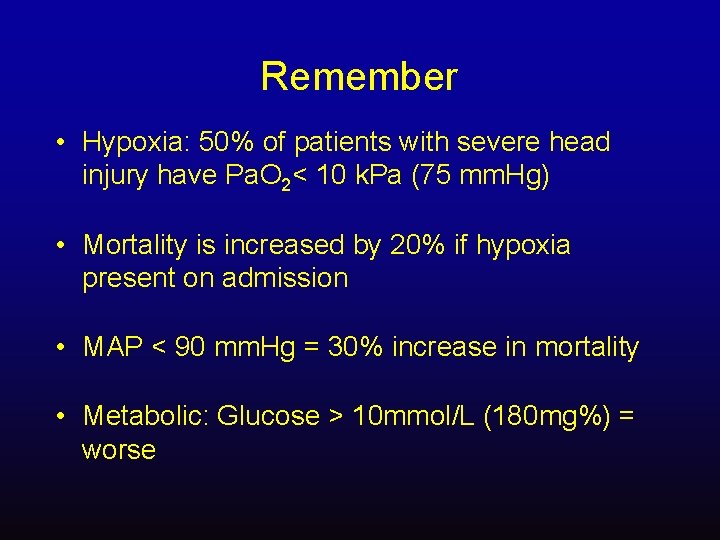
Remember • Hypoxia: 50% of patients with severe head injury have Pa. O 2< 10 k. Pa (75 mm. Hg) • Mortality is increased by 20% if hypoxia present on admission • MAP < 90 mm. Hg = 30% increase in mortality • Metabolic: Glucose > 10 mmol/L (180 mg%) = worse
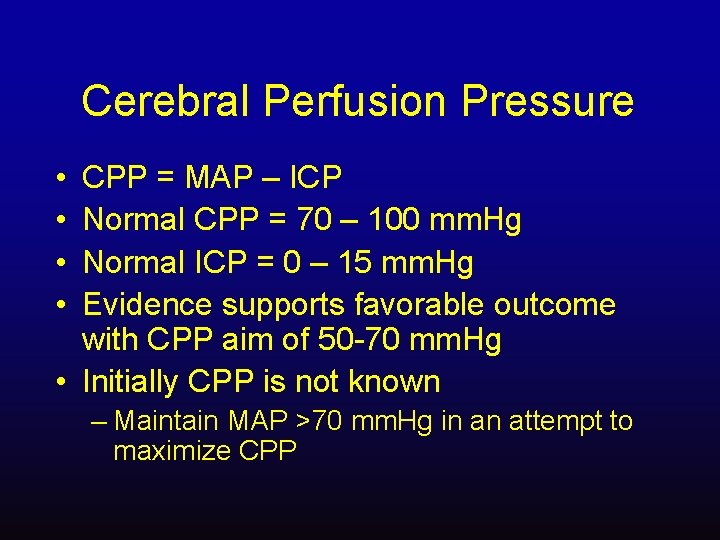
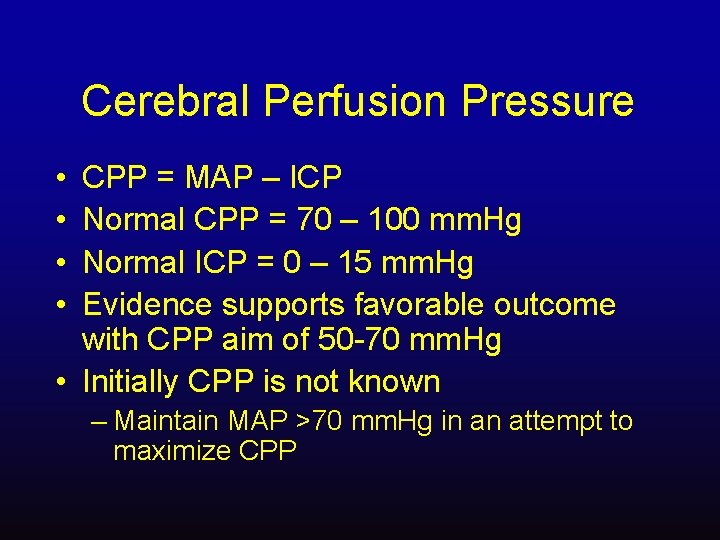
Cerebral Perfusion Pressure • • CPP = MAP – ICP Normal CPP = 70 – 100 mm. Hg Normal ICP = 0 – 15 mm. Hg Evidence supports favorable outcome with CPP aim of 50 -70 mm. Hg • Initially CPP is not known – Maintain MAP >70 mm. Hg in an attempt to maximize CPP
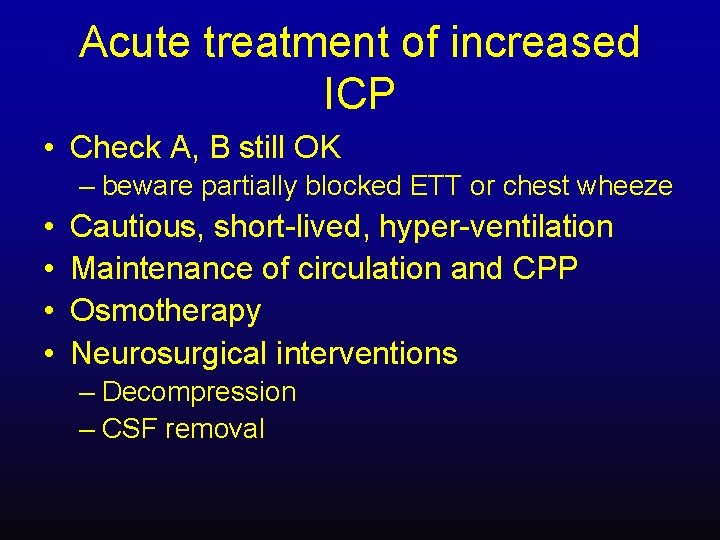
Acute treatment of increased ICP • Check A, B still OK – beware partially blocked ETT or chest wheeze • • Cautious, short-lived, hyper-ventilation Maintenance of circulation and CPP Osmotherapy Neurosurgical interventions – Decompression – CSF removal
Hyperventilation • Theory: ICP via constriction of cerebral vasculature and reduced brain volume • Change: 2 - 4% in cerebral blood flow with every 1 mm. Hg change in p. CO 2 • Pa. O 2 below 60 mm. Hg (8 k. Pa) is the second most powerful predictor of poor outcome • Pa. CO 2 <4 k. Pa (30 mm. Hg) may increase ischaemic damage due to cerebral vasoconstriction • Severe vasoconstriction with p. CO 2 < 25 mm. Hg (3. 5 k. Pa) • Evidence suggest hyperventilation is harmful
Hyperventilation: Recommendations • Brain Trauma Foundation: 1) Prophylactic hyperventilation is to be avoided 2) Hyperventilate for brief periods when there is acute neurologic deterioration 3) Hyperventilate for ICP that is refractory to sedation, paralysis, cerebral spinal fluid (CSF) drainage, and osmotic diuretics

Osmotherapy • Mannitol • Hypertonic saline
Mannitol • Lowers ICP and Increases MAP – 1) plasma expander: increases cerebral blood flow and cerebral oxygen delivery – 2) Delayed effect (30 minute - 6 hour): osmotic agent • Cardiovascular collapse if volume depleted • May increase bleeding • Renal failure: if serum osmolarity > 320 m. Osm • Concentrated in brain tissue with prolonged infusion
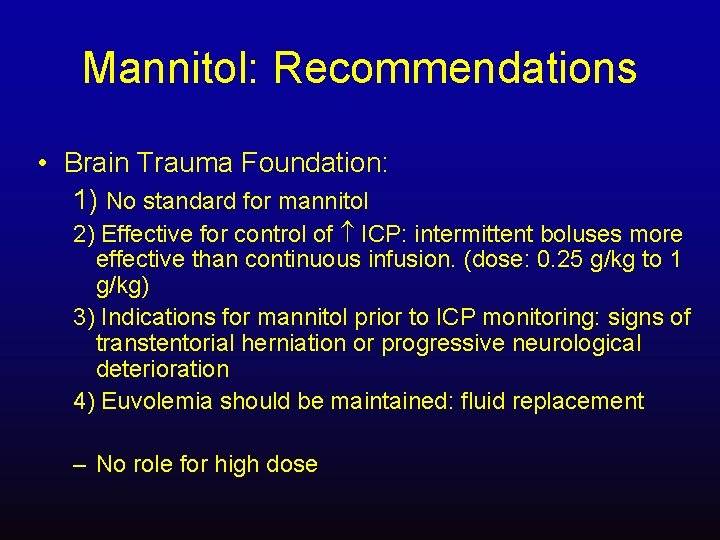
Mannitol: Recommendations • Brain Trauma Foundation: 1) No standard for mannitol 2) Effective for control of ICP: intermittent boluses more effective than continuous infusion. (dose: 0. 25 g/kg to 1 g/kg) 3) Indications for mannitol prior to ICP monitoring: signs of transtentorial herniation or progressive neurological deterioration 4) Euvolemia should be maintained: fluid replacement – No role for high dose
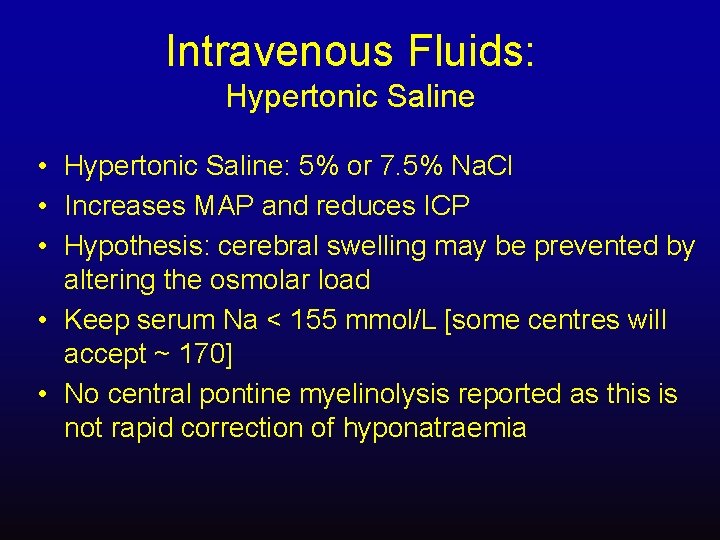
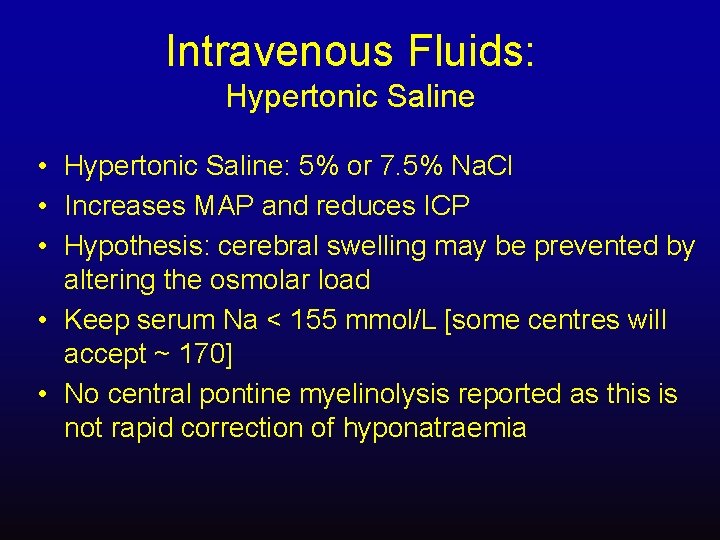
Intravenous Fluids: Hypertonic Saline • Hypertonic Saline: 5% or 7. 5% Na. Cl • Increases MAP and reduces ICP • Hypothesis: cerebral swelling may be prevented by altering the osmolar load • Keep serum Na < 155 mmol/L [some centres will accept ~ 170] • No central pontine myelinolysis reported as this is not rapid correction of hyponatraemia
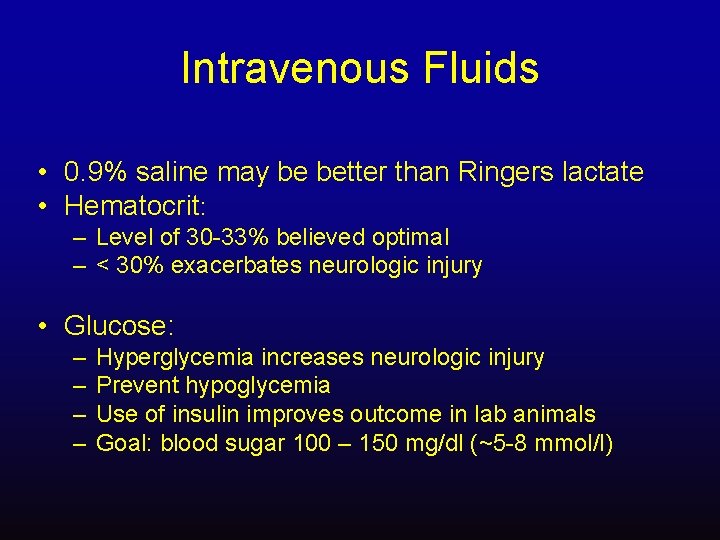
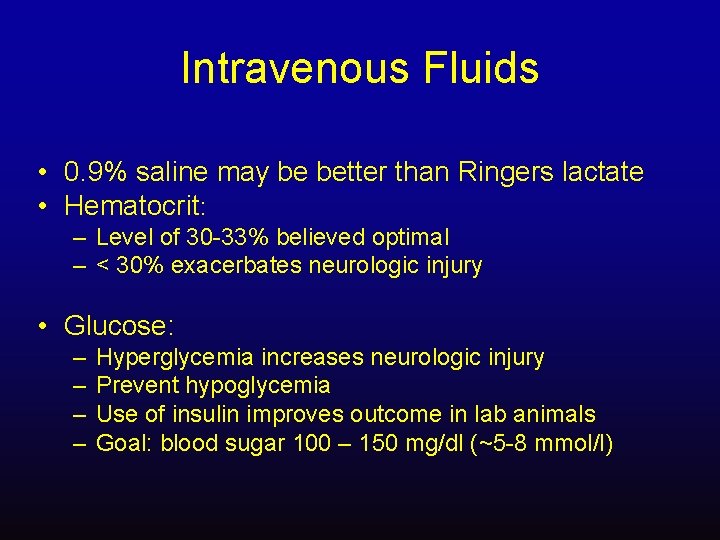
Intravenous Fluids • 0. 9% saline may be better than Ringers lactate • Hematocrit: – Level of 30 -33% believed optimal – < 30% exacerbates neurologic injury • Glucose: – – Hyperglycemia increases neurologic injury Prevent hypoglycemia Use of insulin improves outcome in lab animals Goal: blood sugar 100 – 150 mg/dl (~5 -8 mmol/l)
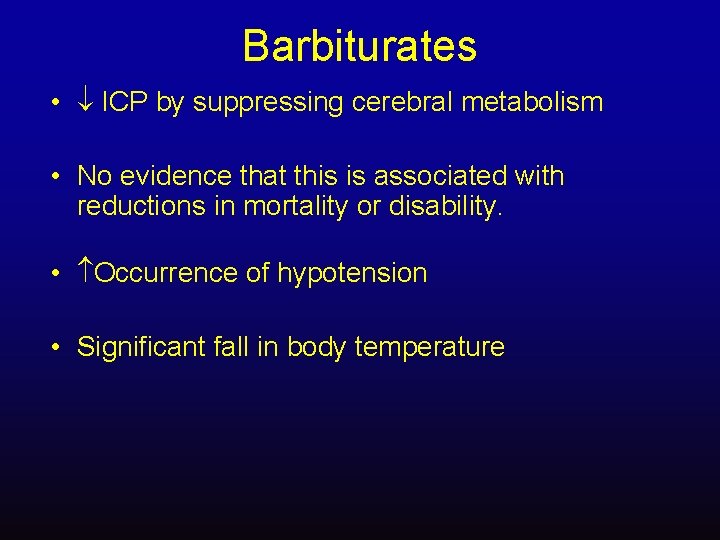
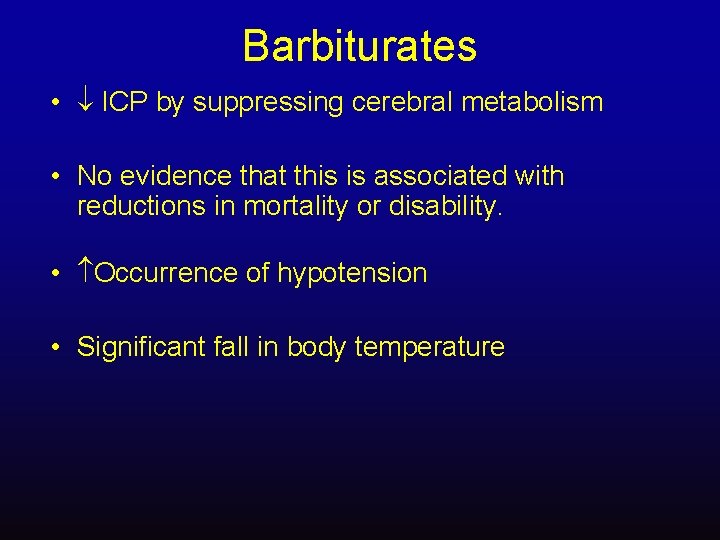
Barbiturates • ICP by suppressing cerebral metabolism • No evidence that this is associated with reductions in mortality or disability. • Occurrence of hypotension • Significant fall in body temperature
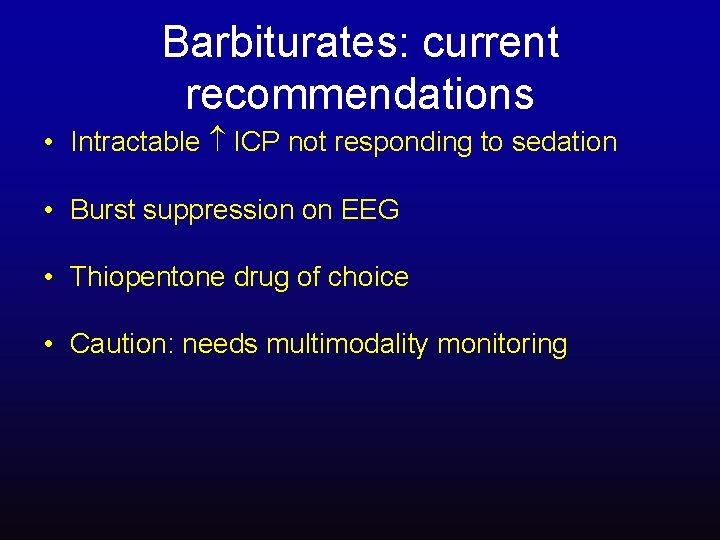
Barbiturates: current recommendations • Intractable ICP not responding to sedation • Burst suppression on EEG • Thiopentone drug of choice • Caution: needs multimodality monitoring

Associated Injuries…. . • • • Spinal Cord Injury Faciomaxillary Injury Thoracic Injury Abdominal Injury Pelvic Injury Musculoskeletal Injury
Spinal Cord Injury • Hypotension (neurogenic shock) – characterized by bradycardia rather than tachycardia (due to loss of cardiac accelerator function and unopposed parasympathetic tone) may be difficult to distinguish from hypotension due to acute hemorrhage. • The hypotensive trauma patient is always assumed to be bleeding, until this possibility is definitively ruled out.

Early Need for a Surgical Airway…. . • • • Head injury/coma Face or neck injury Cervical Spine injury Chest injury: rib fractures Haemo-pneumothorax


Rib Fractures • Ribs 1 -3 major force to break : associated injuries • Ribs 4 -9 Lung contusions : Haemothorax/pneumothorax • Ribs 10 -12 Intra-abdominal injuries
What are the causes of life threatening chest trauma? Primary survey • Airway obstruction • Tension pneumothorax • Open pneumothorax • Massive haemothorax • Flail chest • Cardiac tamponade
Blunt Abdominal Trauma (BAT) • Delicate organs in an expandable cavity with little bony protection • May be the source of occult fatal exsanguination • Injury is sometimes obvious (evisceration) but usually occult. • Clinical signs are unreliable and occur late (expanding abdomen) • Difficult to assess existence or extent of injury on clinical grounds alone. • If suspicious, ORGAN INJURY MUST BE EXCLUDED.
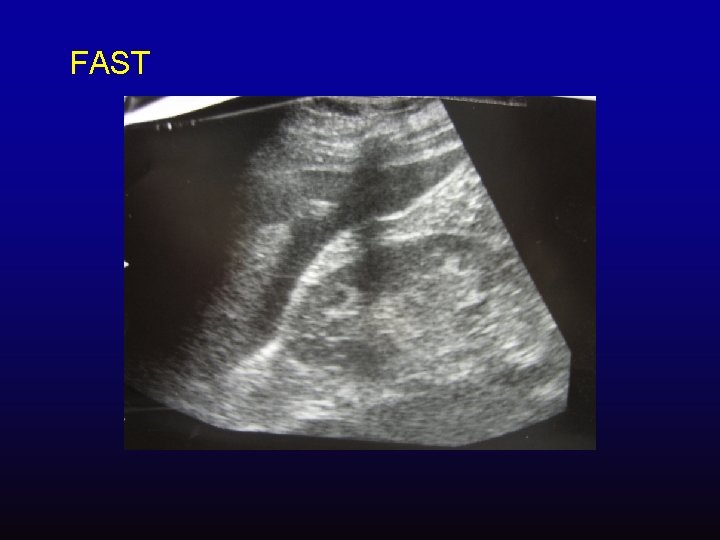
FAST


• Laparotomy: splenic injury/ liver laceration splenectomy, packing abdomen, Temporary Closure with Vac dressing
Evidence-based… Intra-abdominal Hypertension Ivatury RR: Supranormal trauma resuscitation and abdominal compartment syndrome. Arch Surg 2004; 139: 225.
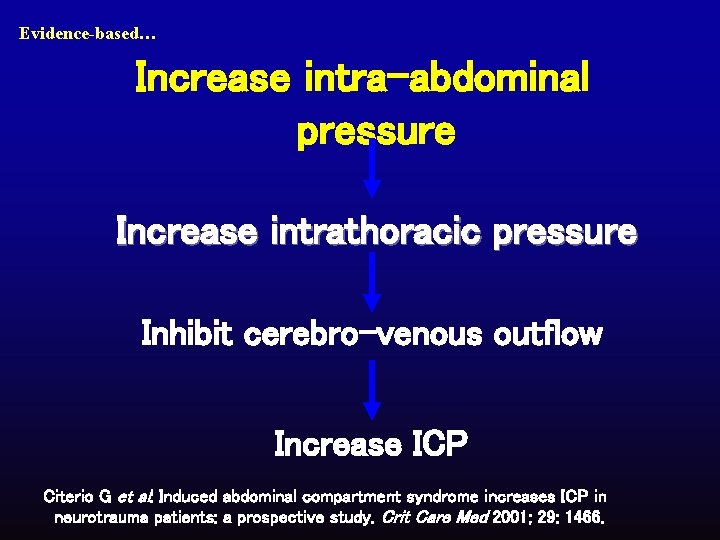
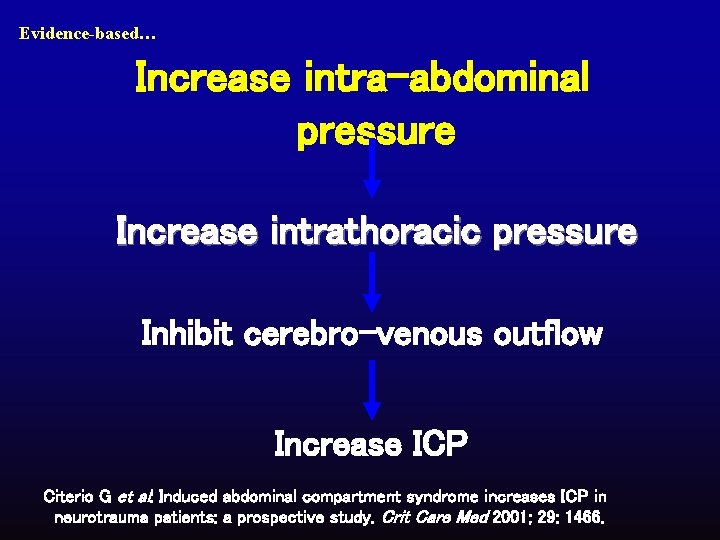
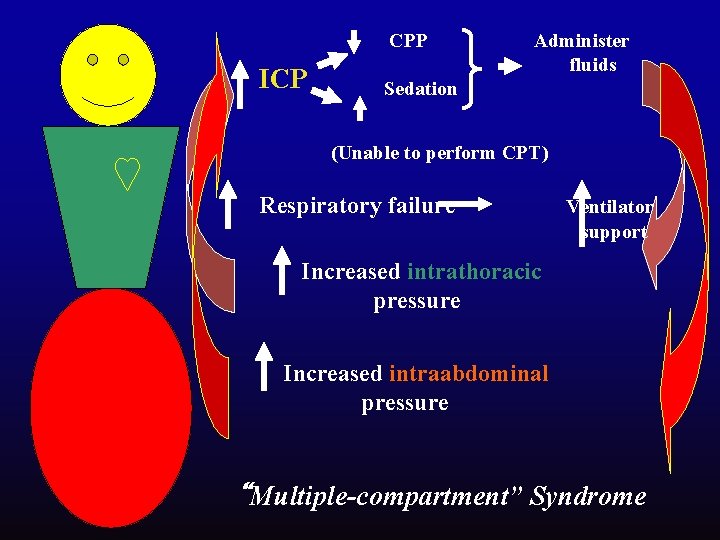
Evidence-based… Increase intra-abdominal pressure Increase intrathoracic pressure Inhibit cerebro-venous outflow Increase ICP Citerio G et al: Induced abdominal compartment syndrome increases ICP in neurotrauma patients: a prospective study. Crit Care Med 2001; 29: 1466.
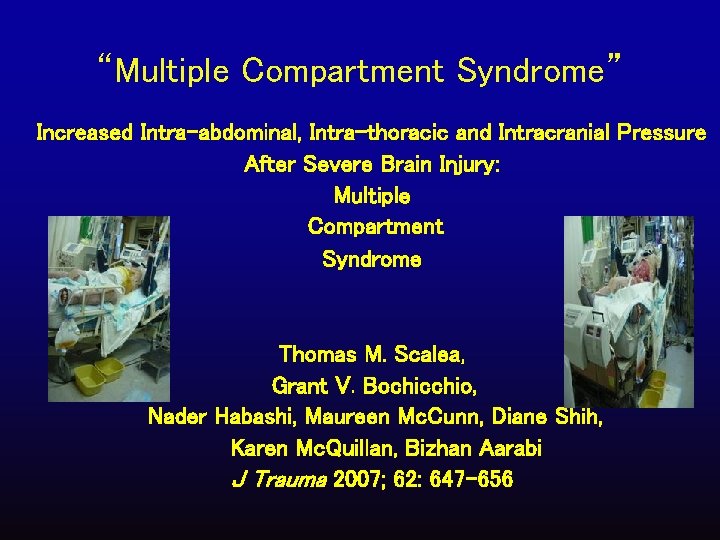
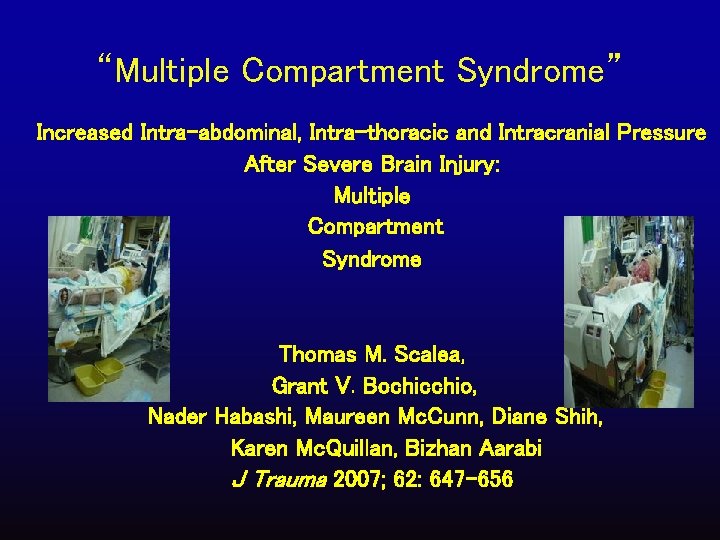
“Multiple Compartment Syndrome” Increased Intra-abdominal, Intra-thoracic and Intracranial Pressure After Severe Brain Injury: Multiple Compartment Syndrome Thomas M. Scalea, Grant V. Bochicchio, Nader Habashi, Maureen Mc. Cunn, Diane Shih, Karen Mc. Quillan, Bizhan Aarabi J Trauma 2007; 62: 647 -656
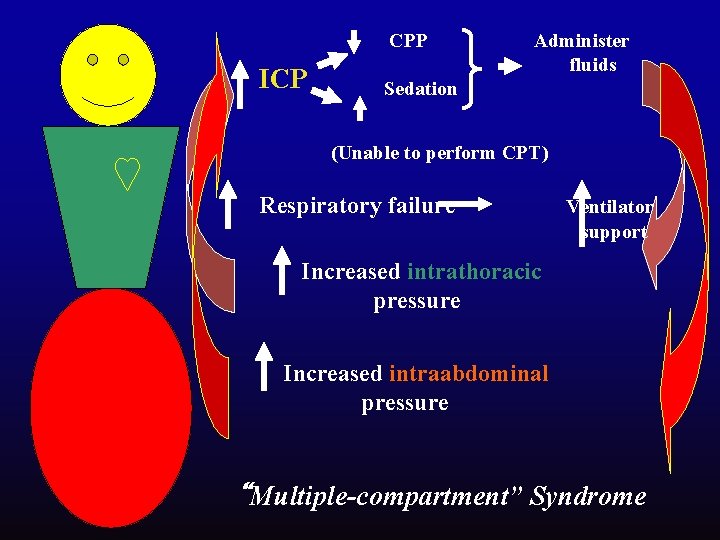
CPP ICP Administer fluids Sedation (Unable to perform CPT) Respiratory failure Ventilator support Increased intrathoracic pressure Increased intraabdominal pressure “Multiple-compartment” Syndrome
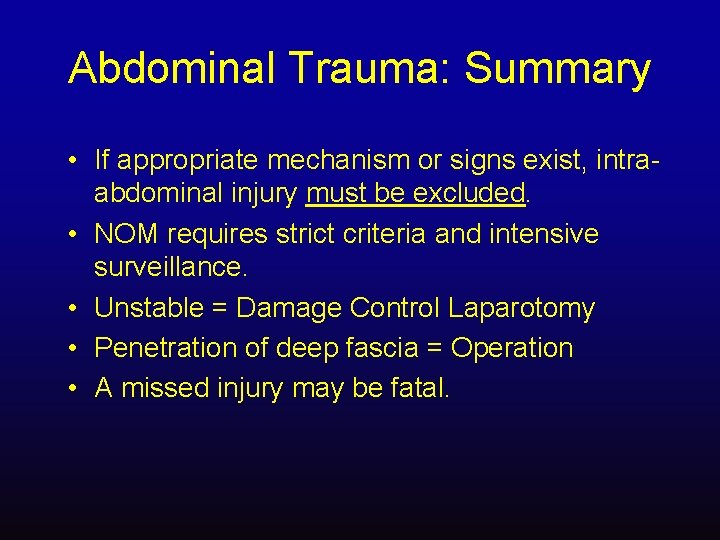
Abdominal Trauma: Summary • If appropriate mechanism or signs exist, intraabdominal injury must be excluded. • NOM requires strict criteria and intensive surveillance. • Unstable = Damage Control Laparotomy • Penetration of deep fascia = Operation • A missed injury may be fatal.

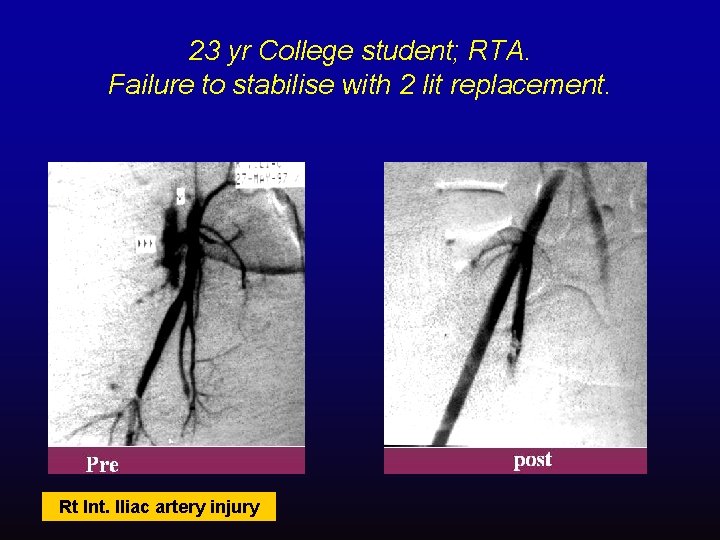
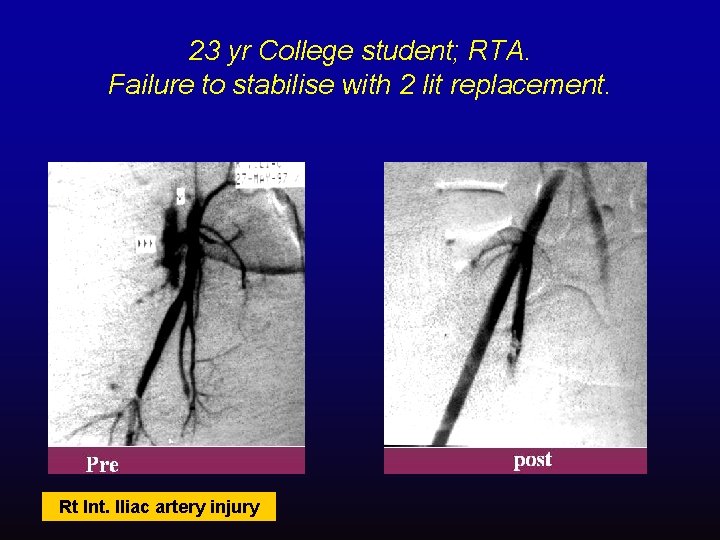
23 yr College student; RTA. Failure to stabilise with 2 lit replacement. Rt Int. Iliac artery injury
Musculoskeletal Trauma • Common, may be life-threatening • Often indicate major trauma and associated with others injuries • Result in haemorrhage, compartment syndrome, rhabdomyolysis, and fat embolism are limb and life-threatening problems

Compartment Syndrome


Myoglobinuria
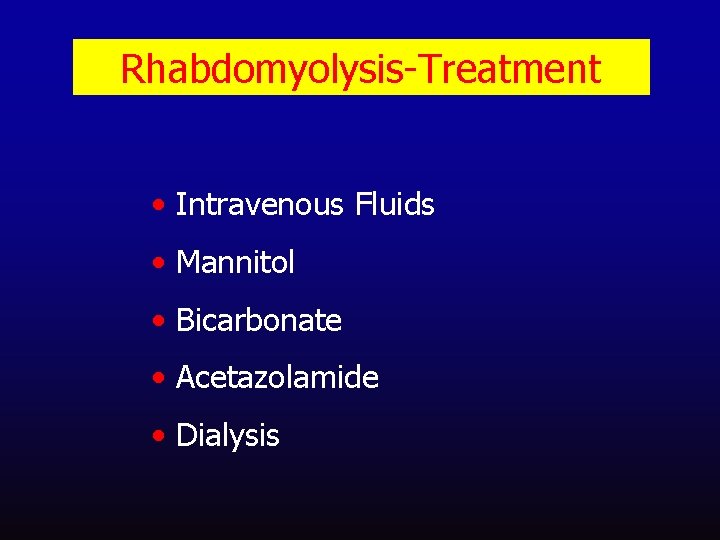
Rhabdomyolysis-Treatment • Intravenous Fluids • Mannitol • Bicarbonate • Acetazolamide • Dialysis
How far to allow the surgeon to proceed? Early Total Care or Damage Control
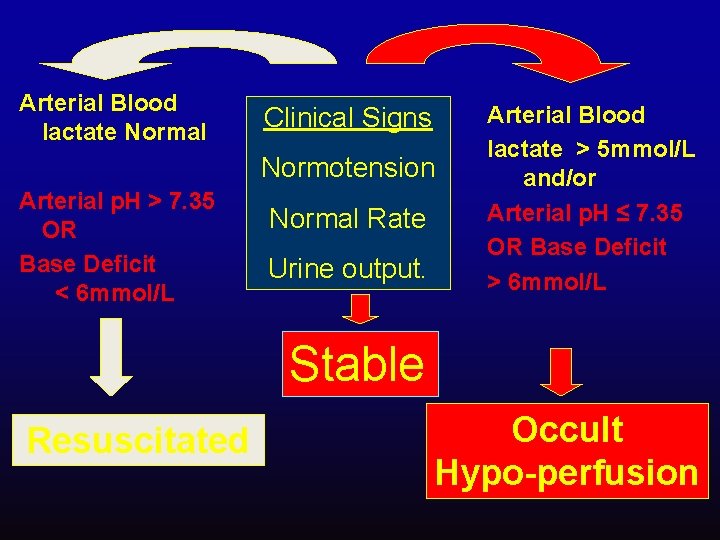
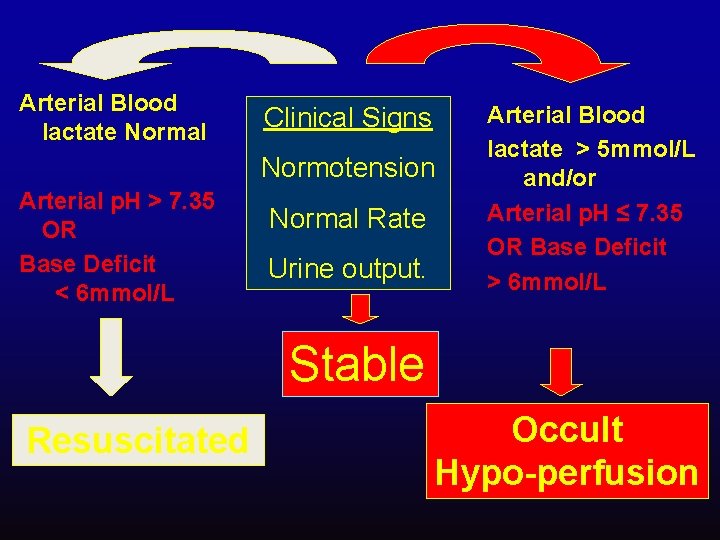
Arterial Blood lactate Normal Clinical Signs Normotension Arterial p. H > 7. 35 OR Base Deficit < 6 mmol/L Normal Rate Urine output. Arterial Blood lactate > 5 mmol/L and/or Arterial p. H ≤ 7. 35 OR Base Deficit > 6 mmol/L Stable Resuscitated Occult Hypo-perfusion
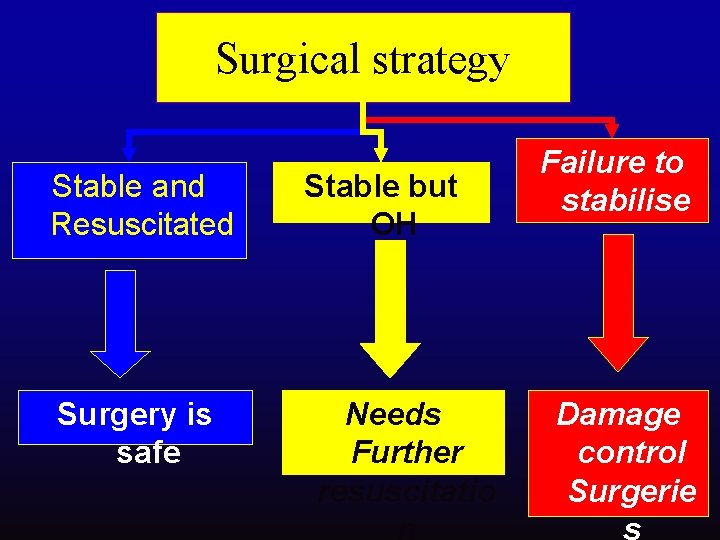
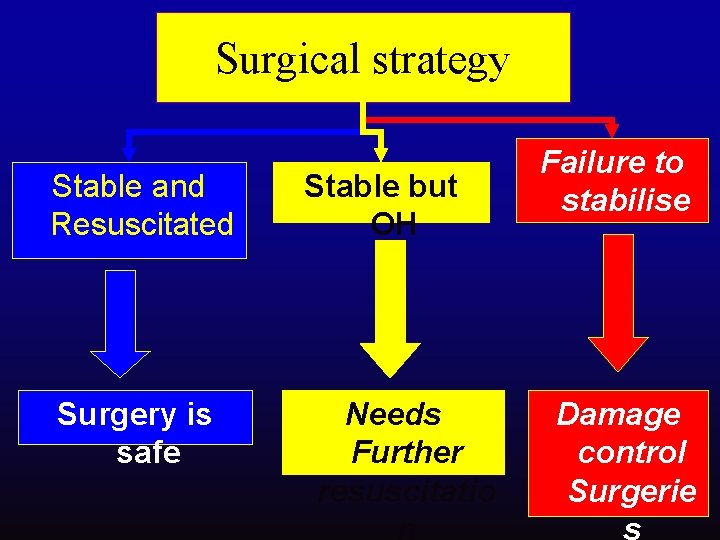
Surgical strategy Stable and Resuscitated Surgery is safe Stable but OH Needs Further resuscitatio n Failure to stabilise Damage control Surgerie s
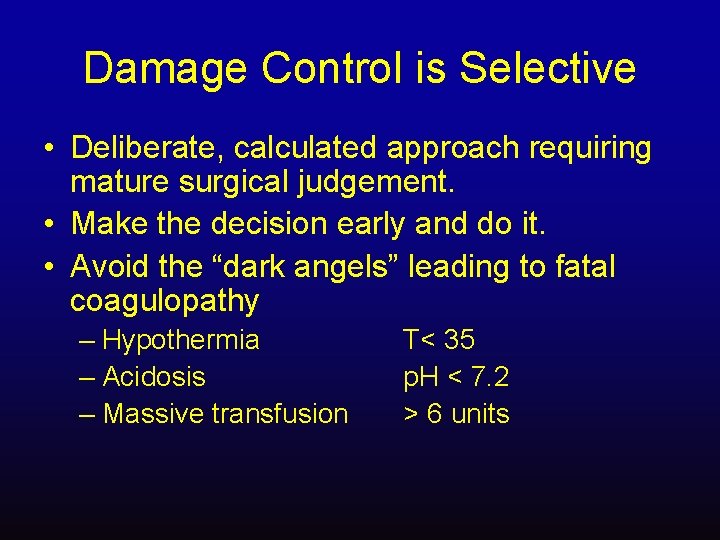
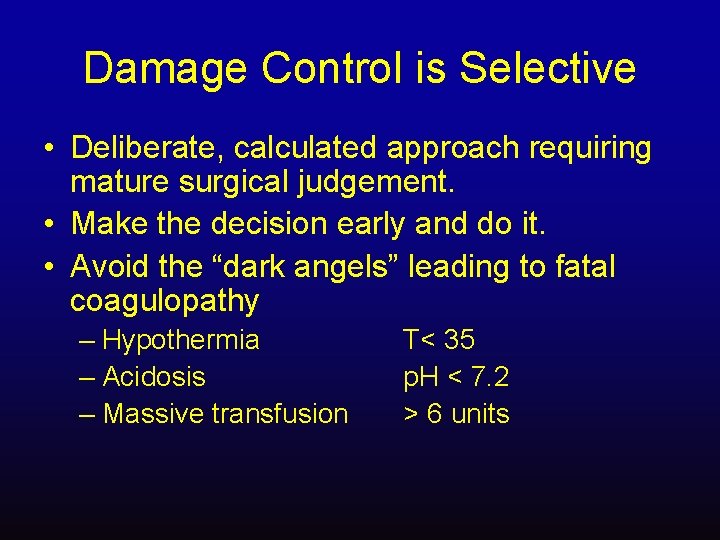
Damage Control is Selective • Deliberate, calculated approach requiring mature surgical judgement. • Make the decision early and do it. • Avoid the “dark angels” leading to fatal coagulopathy – Hypothermia – Acidosis – Massive transfusion T< 35 p. H < 7. 2 > 6 units
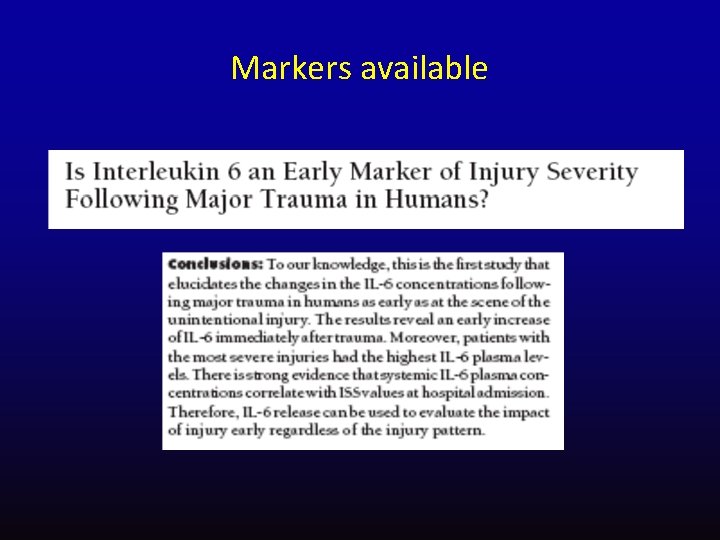
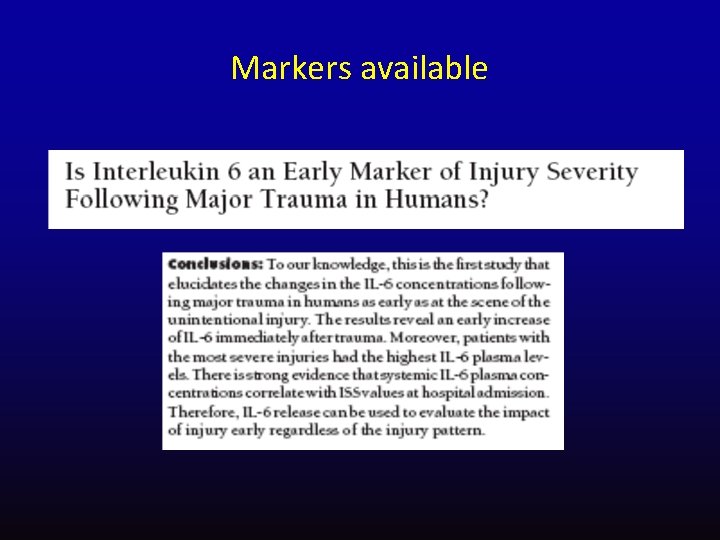
Markers available
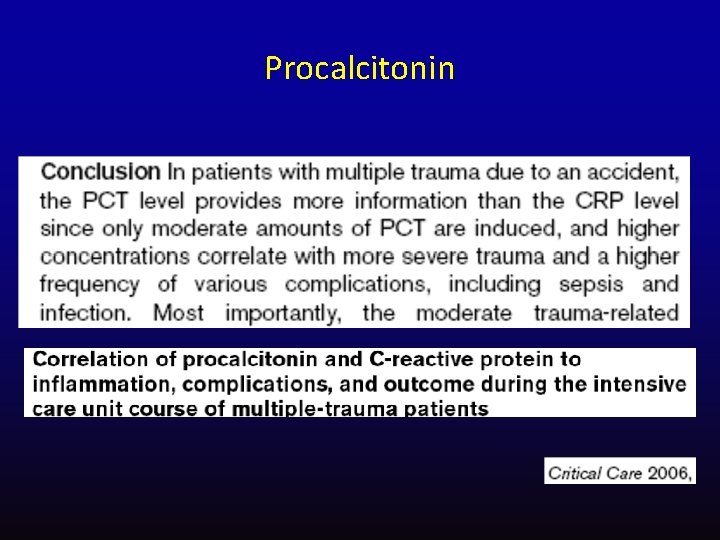
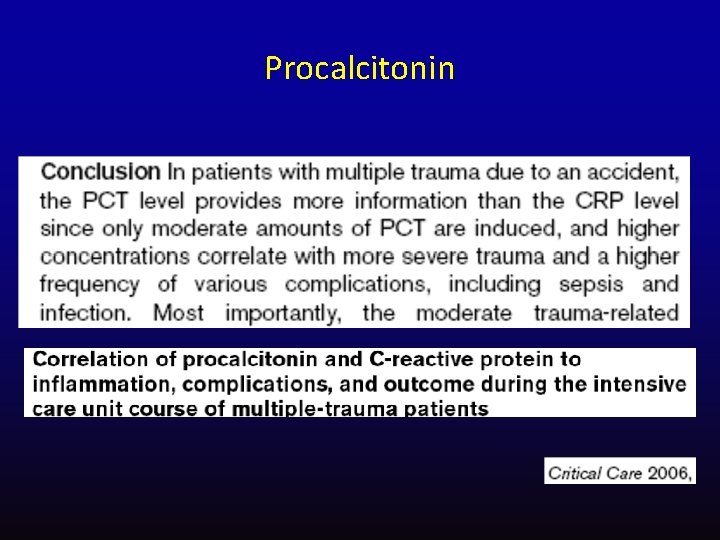
Procalcitonin
• • Pain relief strategies in head injured trauma patient
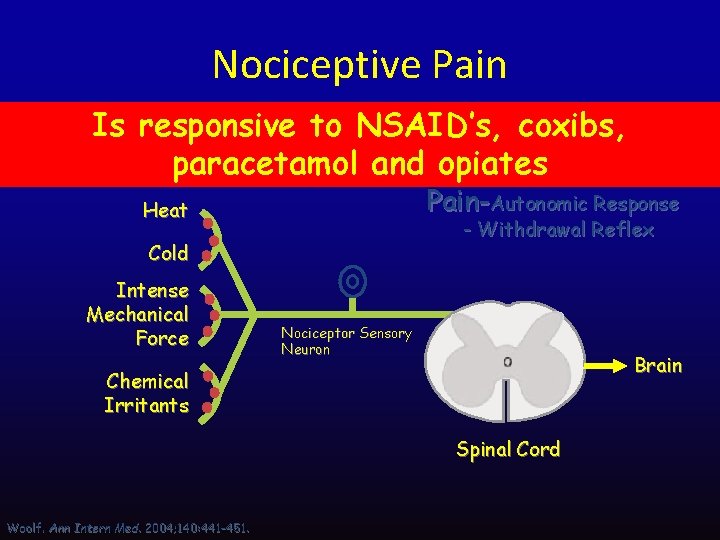
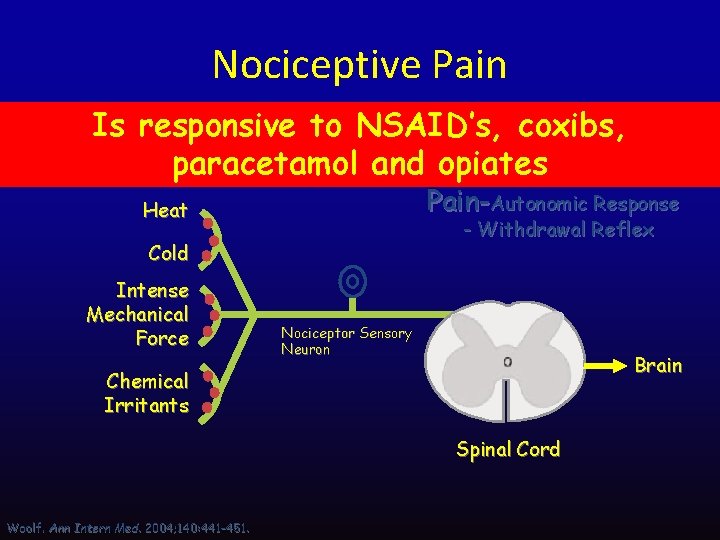
Nociceptive Pain Is responsive to NSAID’s, coxibs, paracetamol and opiates Noxious Peripheral Stimuli Pain-Autonomic Response Heat - Withdrawal Reflex Cold Intense Mechanical Force Nociceptor Sensory Neuron Brain Chemical Irritants Spinal Cord Woolf. Ann Intern Med. 2004; 140: 441 -451.
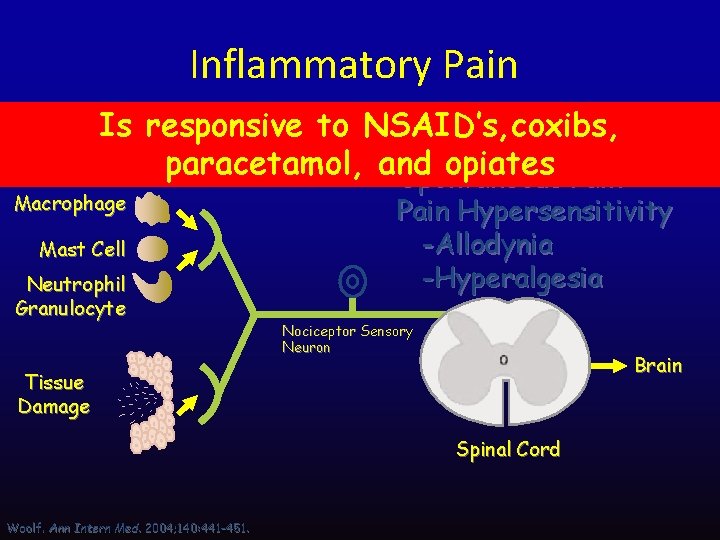
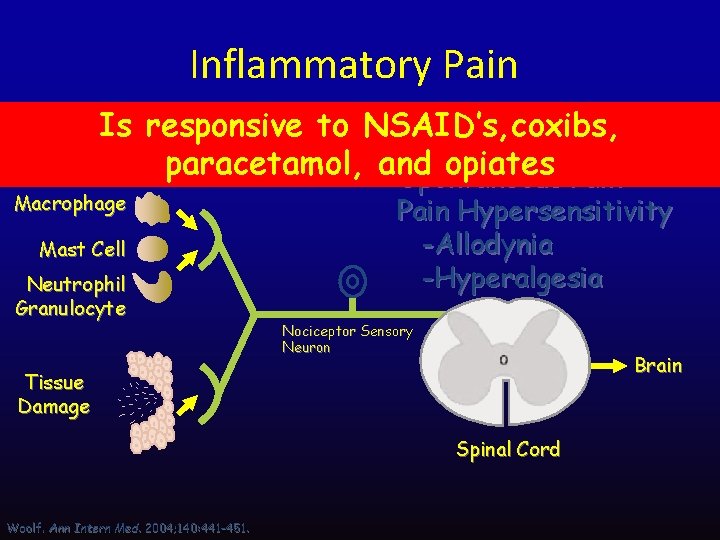
Inflammatory Pain Is responsive to NSAID’s, coxibs, paracetamol, and opiates Pain Inflammation Spontaneous Macrophage Mast Cell Neutrophil Granulocyte Pain Hypersensitivity -Allodynia -Hyperalgesia Nociceptor Sensory Neuron Brain Tissue Damage Spinal Cord Woolf. Ann Intern Med. 2004; 140: 441 -451.
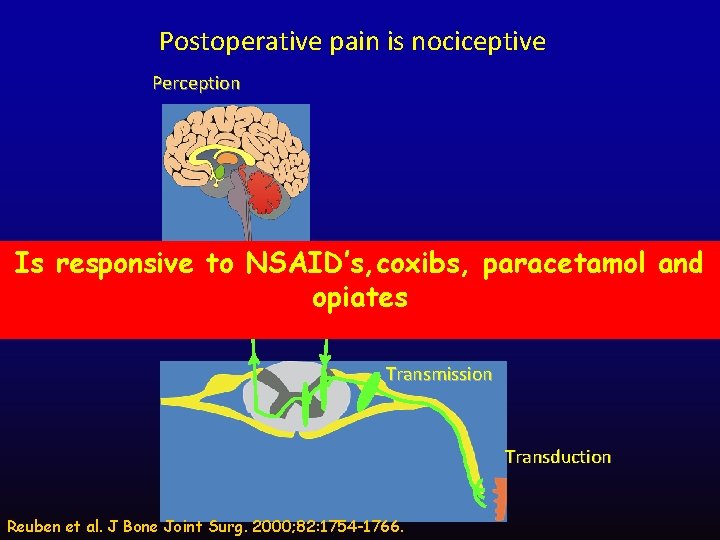
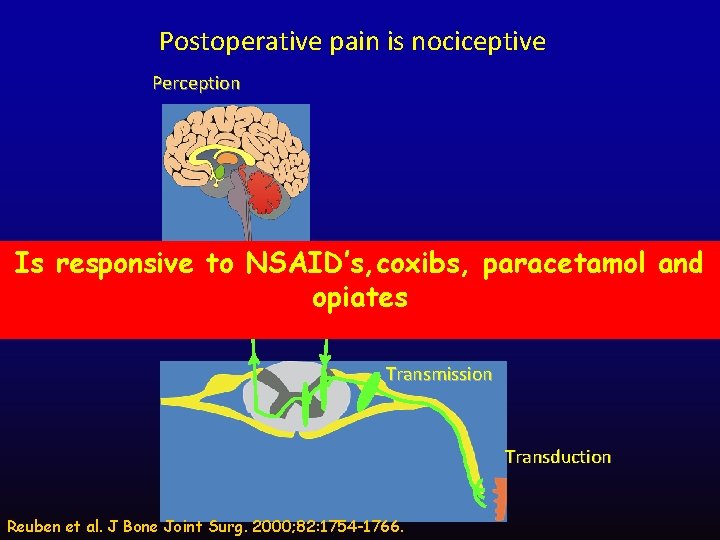
Postoperative pain is nociceptive Perception Modulation Is responsive to NSAID’s, coxibs, paracetamol and opiates Transmission Transduction Reuben et al. J Bone Joint Surg. 2000; 82: 1754 -1766.
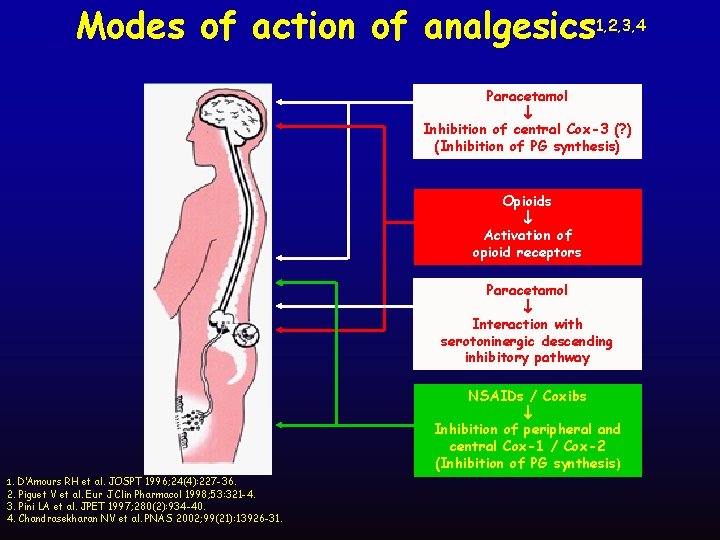
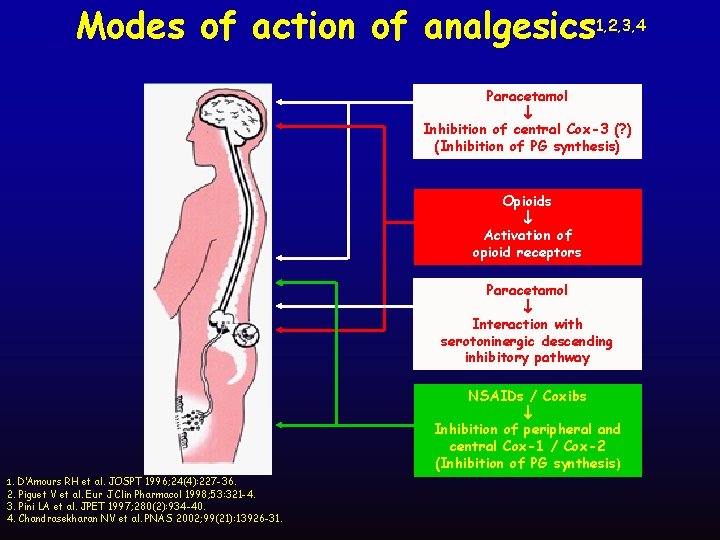
Modes of action of analgesics 1, 2, 3, 4 Paracetamol Inhibition of central Cox-3 (? ) (Inhibition of PG synthesis) Opioids Activation of opioid receptors Paracetamol Interaction with serotoninergic descending inhibitory pathway NSAIDs / Coxibs Inhibition of peripheral and central Cox-1 / Cox-2 (Inhibition of PG synthesis) 1. D’Amours RH et al. JOSPT 1996; 24(4): 227 -36. 2. Piguet V et al. Eur J Clin Pharmacol 1998; 53: 321 -4. 3. Pini LA et al. JPET 1997; 280(2): 934 -40. 4. Chandrasekharan NV et al. PNAS 2002; 99(21): 13926 -31.
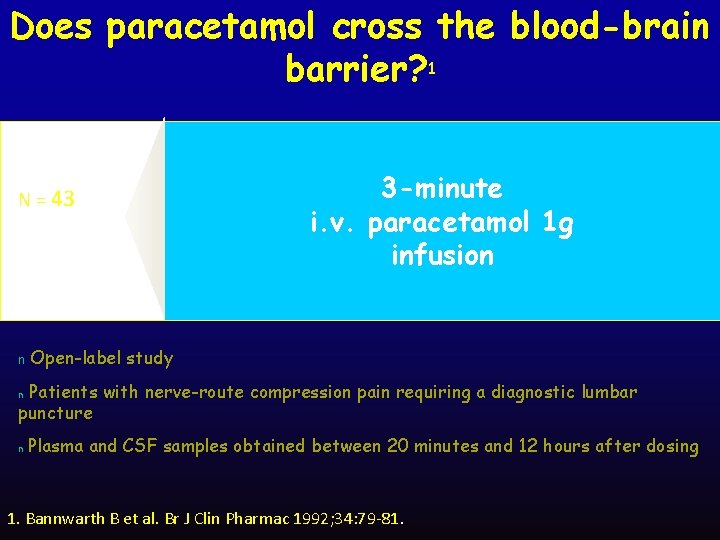
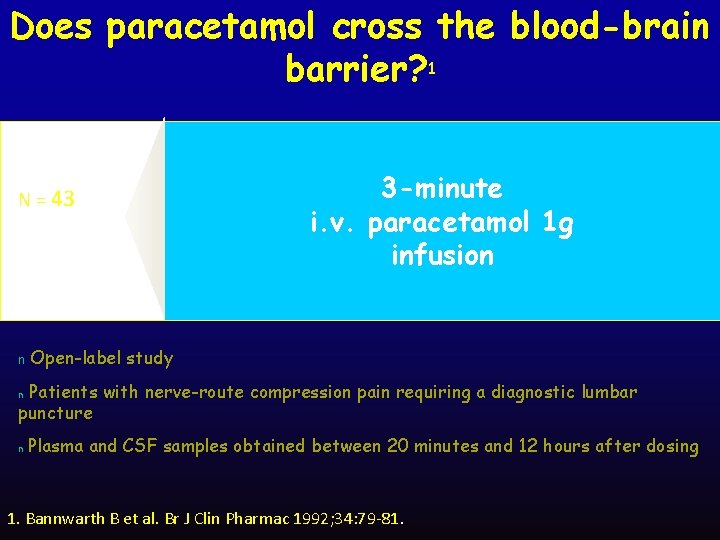
Does paracetamol cross the blood-brain barrier? 1 N = 43 n 3 -minute i. v. paracetamol 1 g infusion Open-label study Patients with nerve-route compression pain requiring a diagnostic lumbar puncture n Plasma and CSF samples obtained between 20 minutes and 12 hours after dosing n 1. Bannwarth B et al. Br J Clin Pharmac 1992; 34: 79 -81.
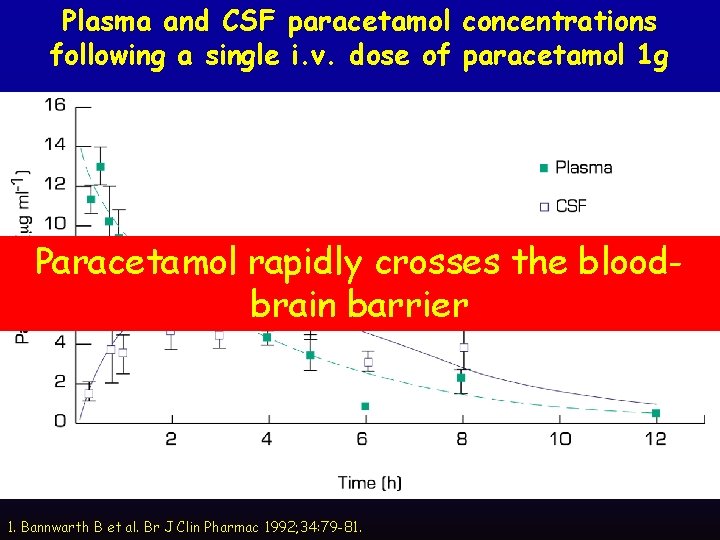
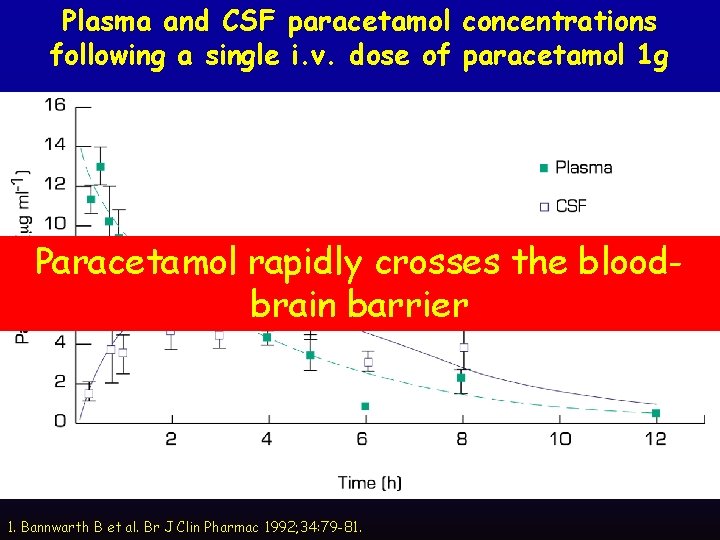
Plasma and CSF paracetamol concentrations following a single i. v. dose of paracetamol 1 g 43) Paracetamol rapidly crosses the(n=bloodbrain barrier 1. Bannwarth B et al. Br J Clin Pharmac 1992; 34: 79 -81.
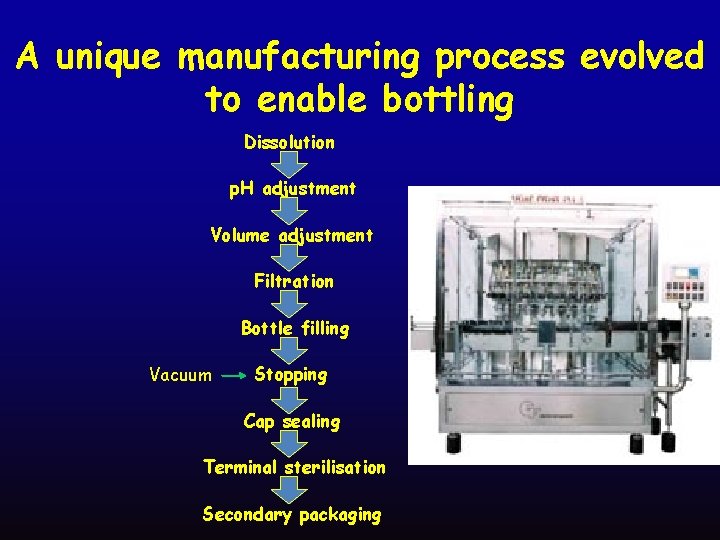
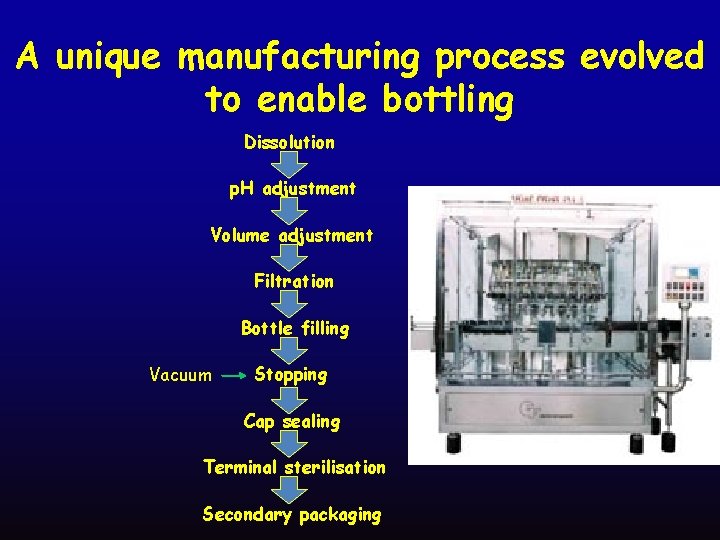
A unique manufacturing process evolved to enable bottling Dissolution p. H adjustment Volume adjustment Filtration Bottle filling Vacuum Stopping Cap sealing Terminal sterilisation Secondary packaging
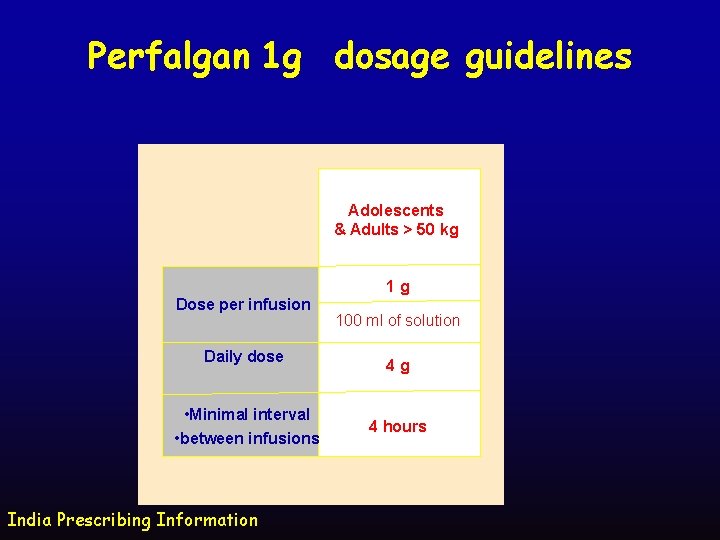
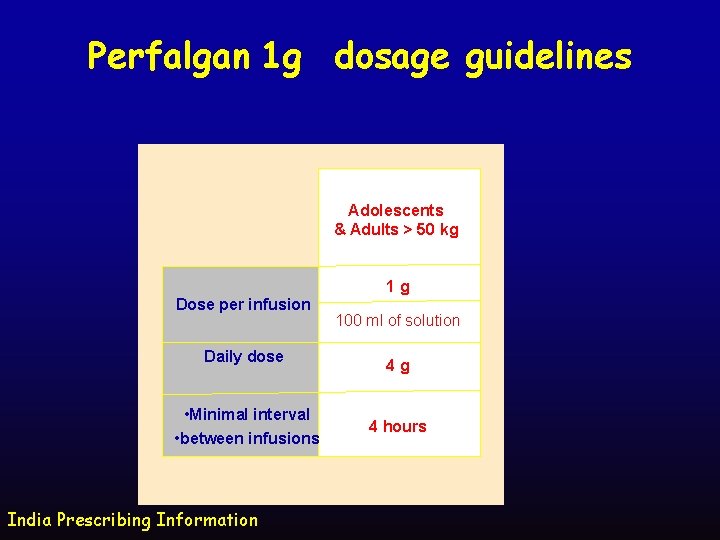
Perfalgan 1 g dosage guidelines Adolescents & Adults > 50 kg 1 g Dose per infusion Daily dose • Minimal interval • between infusions India Prescribing Information 100 ml of solution 4 g 4 hours

CRASH 2 TRIAL: ROLE OF TRANEXAMIC ACID IN TRAUMA
A large randomised controlled trial among trauma patients with significant haemorrhage, of the effects of antifibrinolytic treatment on death and transfusion requirement
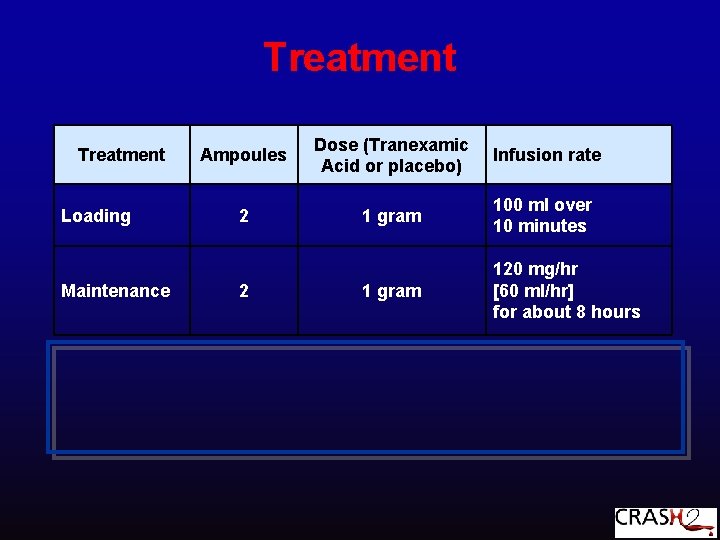
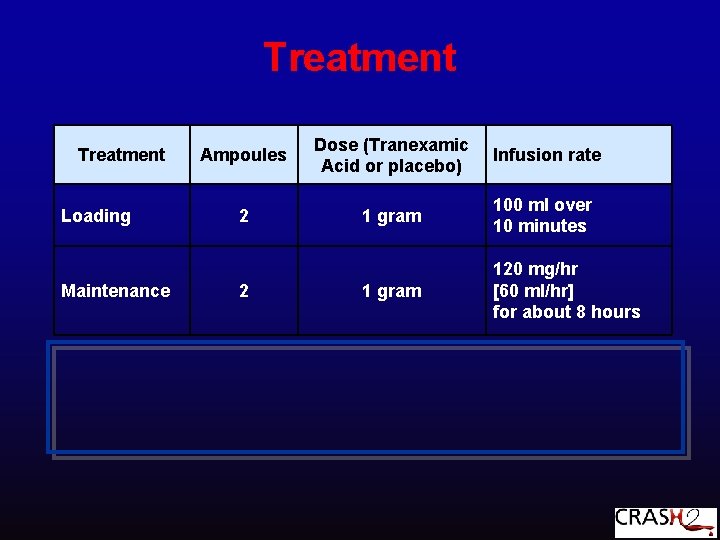
Treatment Loading Maintenance Ampoules Dose (Tranexamic Acid or placebo) Infusion rate 2 1 gram 100 ml over 10 minutes 1 gram 120 mg/hr [60 ml/hr] for about 8 hours 2

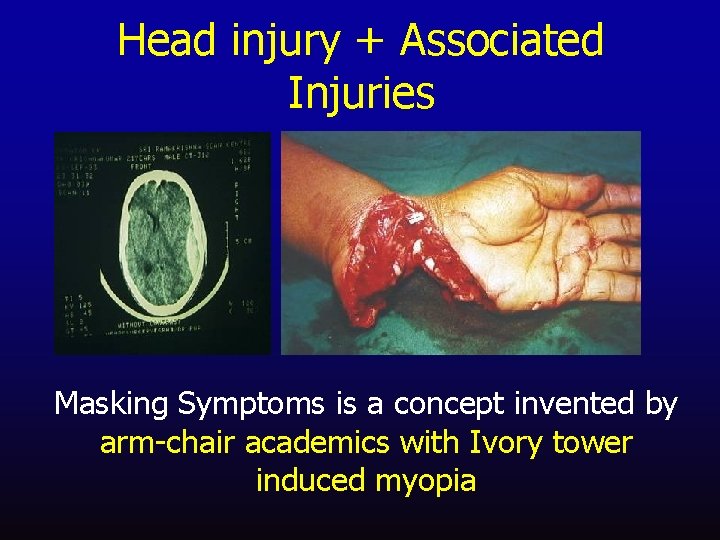
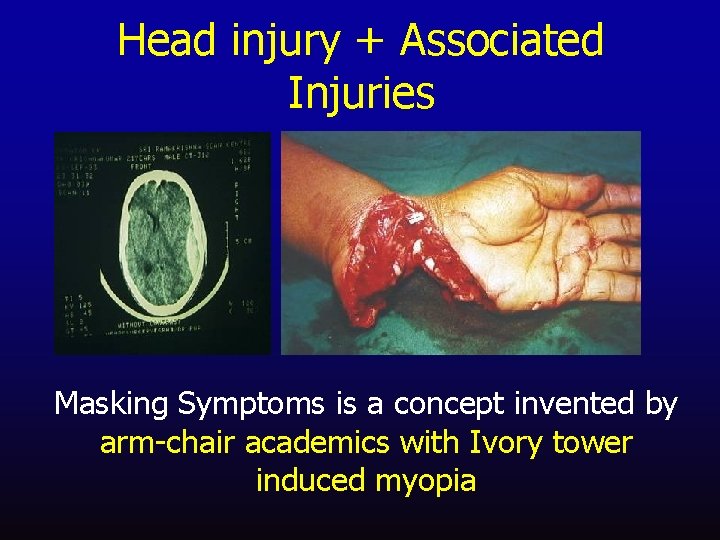
Head injury + Associated Injuries Masking Symptoms is a concept invented by arm-chair academics with Ivory tower induced myopia
DVT prophylaxis • High risk: spinal injury, pelvic or lower limb fractures, brain injury. • Use compression stockings early. • Institute medical prophylaxis once early bleeding controlled and stable. • Encourage early mobilisation. • Also: Tetanus and post-splenectomy immunisation in appropriate patients.
• Timing of tracheostomy in a head injured patient
• Nutrition in Head Injured patient : important tips
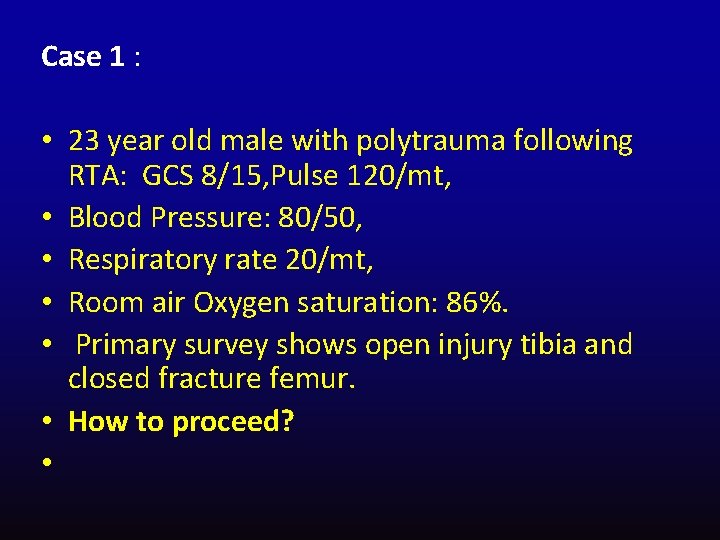
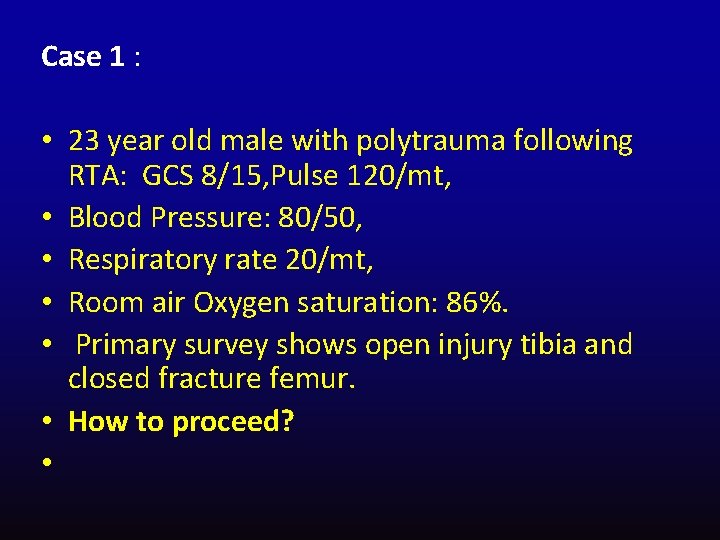
Case 1 : • 23 year old male with polytrauma following RTA: GCS 8/15, Pulse 120/mt, • Blood Pressure: 80/50, • Respiratory rate 20/mt, • Room air Oxygen saturation: 86%. • Primary survey shows open injury tibia and closed fracture femur. • How to proceed? •


Team Work

Thank You
 Multiply injured patient
Multiply injured patient Which is preferred when moving equipment and patients?
Which is preferred when moving equipment and patients? Structures pierced in spinal anaesthesia
Structures pierced in spinal anaesthesia Airway assessment in anaesthesia
Airway assessment in anaesthesia Blood patch procedure
Blood patch procedure Vrg
Vrg Contraindications of spinal anesthesia
Contraindications of spinal anesthesia Nasal trumpet measurement
Nasal trumpet measurement Anaesthesia information management system
Anaesthesia information management system Balanced anaesthesia ppt
Balanced anaesthesia ppt What is anesthesia
What is anesthesia Calcium displacement theory of local anaesthesia
Calcium displacement theory of local anaesthesia Baricity of local anesthetics
Baricity of local anesthetics Spinal anaesthesia position
Spinal anaesthesia position Mechanism of local anesthesia
Mechanism of local anesthesia Structures pierced spinal anaesthesia
Structures pierced spinal anaesthesia Patient 2 patient
Patient 2 patient It is an immediate and temporary
It is an immediate and temporary At night you see a pedestrian wearing reflective
At night you see a pedestrian wearing reflective Juan continued playing although he injured his knee
Juan continued playing although he injured his knee We can wait here until carlo calls us
We can wait here until carlo calls us Hammock carry first aid
Hammock carry first aid Flooded suction vs suction lift
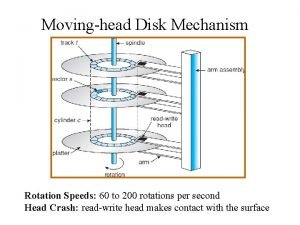
Flooded suction vs suction lift Moving head disk mechanism
Moving head disk mechanism Moving head disk mechanism in os
Moving head disk mechanism in os Biceps femoris short head
Biceps femoris short head Dividing head formula
Dividing head formula Parts of the chest
Parts of the chest The attacking firm goes head-to-head with its competitor.
The attacking firm goes head-to-head with its competitor. The tone unit
The tone unit What is tonic syllable
What is tonic syllable Tagi html
Tagi html V cc
V cc Thể thơ truyền thống
Thể thơ truyền thống Chúa yêu trần thế
Chúa yêu trần thế Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu đại từ thay thế
đại từ thay thế Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Công thức tính thế năng
Công thức tính thế năng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Phản ứng thế ankan
Phản ứng thế ankan Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Phối cảnh
Phối cảnh điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Lp html
Lp html Sơ đồ cơ thể người
Sơ đồ cơ thể người Bảng số nguyên tố lớn hơn 1000
Bảng số nguyên tố lớn hơn 1000 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Tư thế ngồi viết
Tư thế ngồi viết Cái miệng nó xinh thế
Cái miệng nó xinh thế Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết Läkarutlåtande för livränta
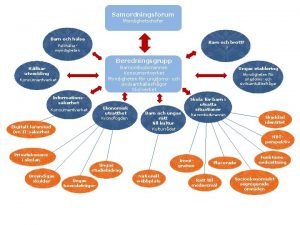
Läkarutlåtande för livränta Klassificeringsstruktur för kommunala verksamheter
Klassificeringsstruktur för kommunala verksamheter Myndigheten för delaktighet
Myndigheten för delaktighet Att skriva debattartikel
Att skriva debattartikel Tack för att ni lyssnade
Tack för att ni lyssnade En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Egg för emanuel
Egg för emanuel Tack för att ni har lyssnat
Tack för att ni har lyssnat Verifikationsplan
Verifikationsplan Biologiska arvet
Biologiska arvet Presentera för publik crossboss
Presentera för publik crossboss Rbk fuktmätning
Rbk fuktmätning Var 1721 för stormaktssverige
Var 1721 för stormaktssverige Förklara densitet för barn
Förklara densitet för barn Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Tack för att ni har lyssnat
Tack för att ni har lyssnat Referatmarkering
Referatmarkering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Karttecken tät skog
Karttecken tät skog