REGIONAL ANALGESIA AND ANAESTHESIA DEPT OF ANAESTHESIA AND
















- Slides: 70
REGIONAL ANALGESIA AND ANAESTHESIA DEPT OF ANAESTHESIA AND ICU COLLEGE OF MEDICINE KING SAUD UNIVERSITY
HISTORY • • • 1885 Corning - First attempt with epidural cocaine 1891 Quincke - Describes the lumbar puncture technique 1921 Pagis - First lumbar anaesthesia for surgery 1947 Lidocaine commercially available 1949 Curbelo - First continuous lumbar analgesia with Touhy needle 1963 Bupivacaine commercially available 1979 Cousins - Epidural opioids provide analgesia 1983 Yaksh - Different spinal receptor systems mediating pain 1985 University of Keil, Germany, Anaesthesiology managed acute post-operative pain service Cousins & Bridenbaugh, 3 rd Edition
Regional/Neuraxial Anaesthesia A reversible loss of sensation in a specific area of the body. Bier block Axillary, Interscalene Spinal, Epidural Caudal Ankle block, metatarsal block Paracervical
Regional anaesthetic techniques categorized as follows • Epidural and spinal anaesthesia • Peripheral nerve blockades • IV regional anaesthesia
• SPINAL ANAESTHESIA • INTRATHECAL=administration of medication into subarachnoid space
• EPIDURAL ANAESTHESIA • EPIDURAL=administration of medication into epidural space
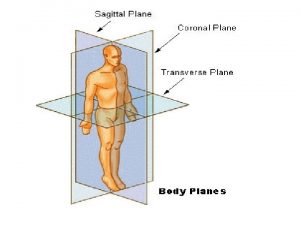
OVERVIEW OF THE SPINAL ANATOMY

SPINAL CORD • Located and protected within vertebral column • Extends from the foramen magnum to lower border 1 st L 1 (adult) S 2 (kids) • SC taper to a fibrous band - conus medullaris • Nerve root continue beyond the conus- cauda equina • Surrounded by the meninges (dura , arachnoid & pia mater. )

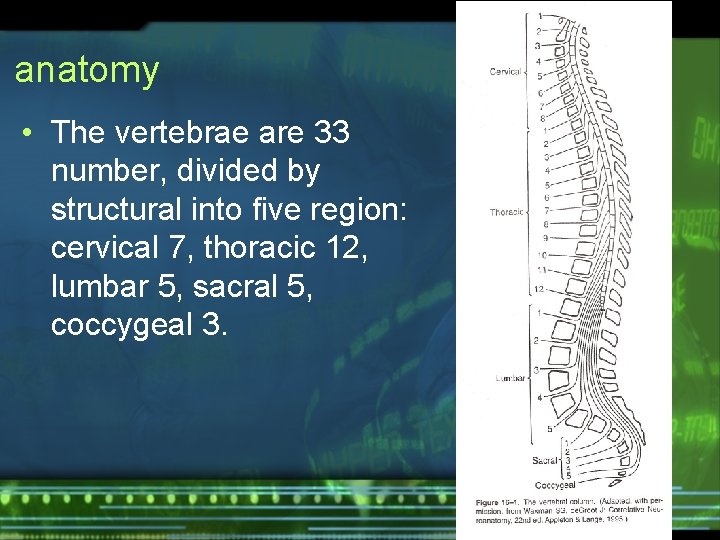
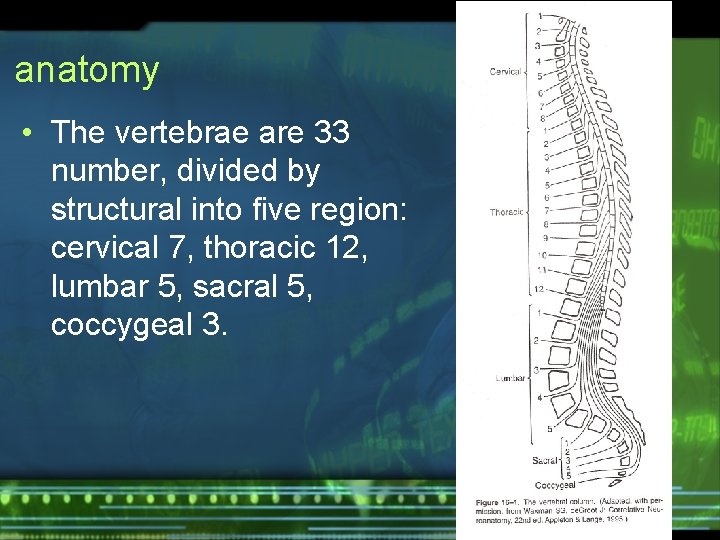
anatomy • The vertebrae are 33 number, divided by structural into five region: cervical 7, thoracic 12, lumbar 5, sacral 5, coccygeal 3.
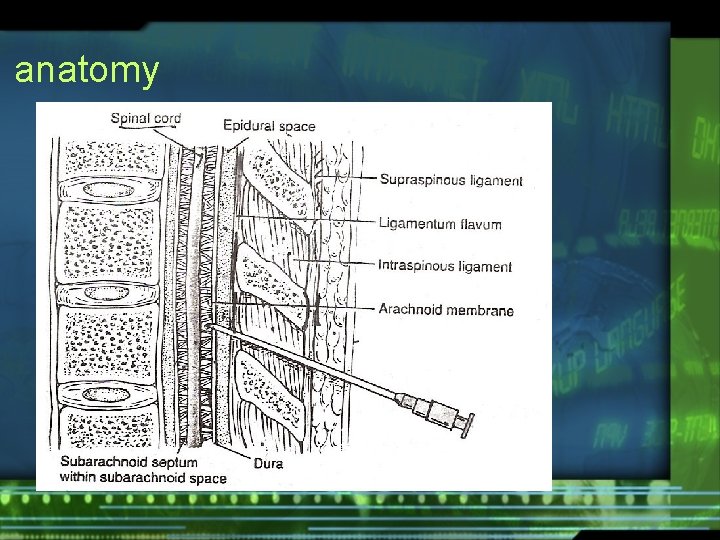
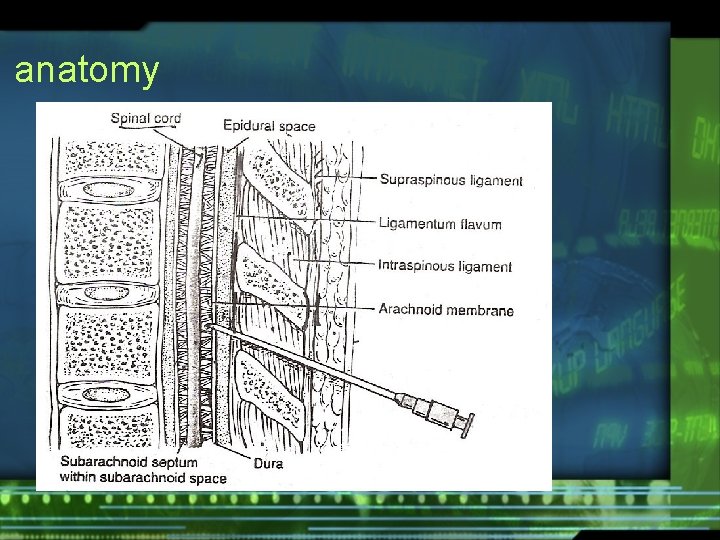
anatomy
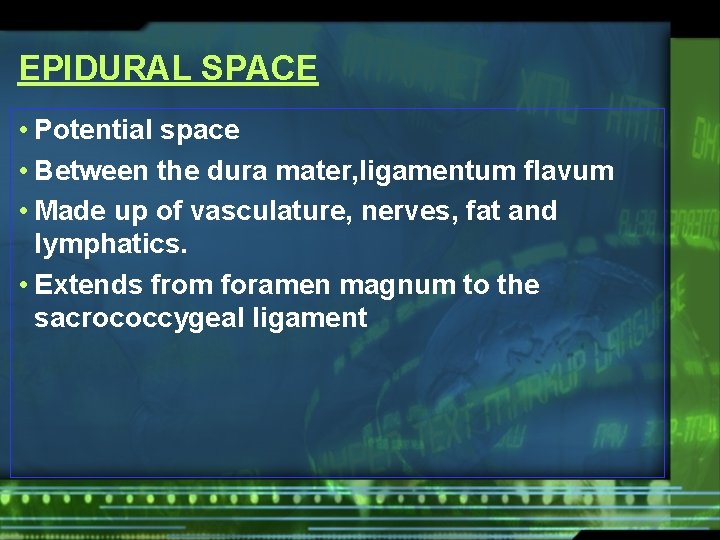
EPIDURAL SPACE • Potential space • Between the dura mater, ligamentum flavum • Made up of vasculature, nerves, fat and lymphatics. • Extends from foramen magnum to the sacrococcygeal ligament
Regional anaesthesia • Spinal lower extremities, lower abdomen, pelvis • Epidural cervical thoracic lumbar caudal
INDICATIONS § The objective of epidural analgesia is to relieve pain. Major surgery Trauma (# ribs) Palliative care (intractable pain) Labour and Delivery abd surgery Pelvic surgery lower lime surgery
CONTRAINDICATIONS ABSOLUTE CONTRAINDICATIONS • • • Patient refusal Known allergy to opioid or local anaesthetic Infection/abscess near the proposed injection site Hematological disorder Increase ICP
CONTRAINDICATIONS RELATIVE CONTRAINDICATIONS • Sepsis • Patient on anticoagulant • Hypotension • Hypovolemia • Spinal deformity • Neurological disorder.
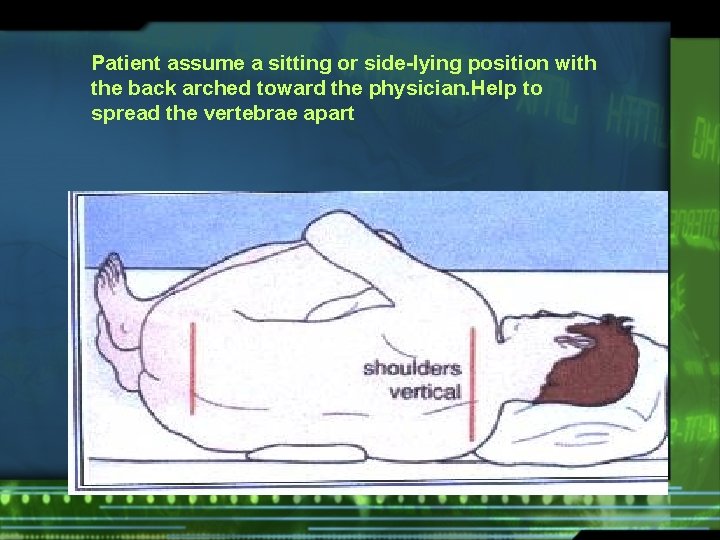
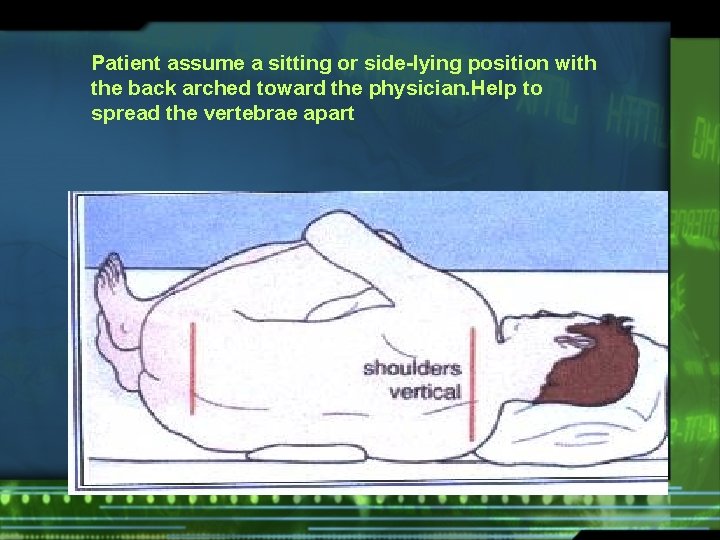
Patient assume a sitting or side-lying position with the back arched toward the physician. Help to spread the vertebrae apart
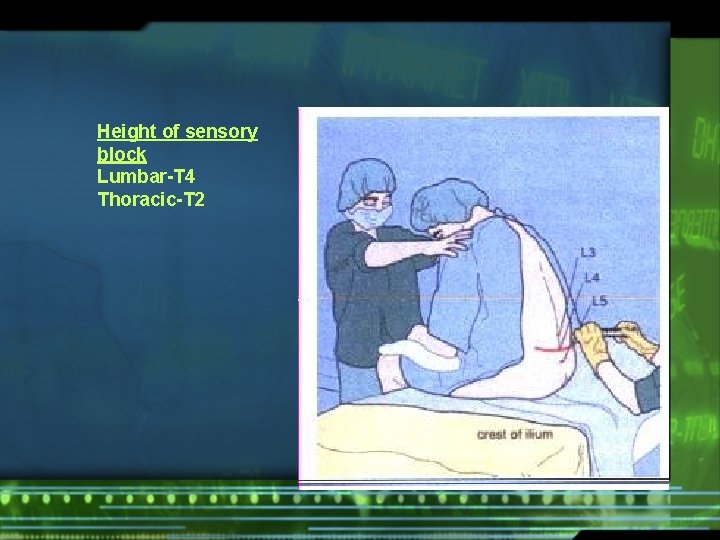
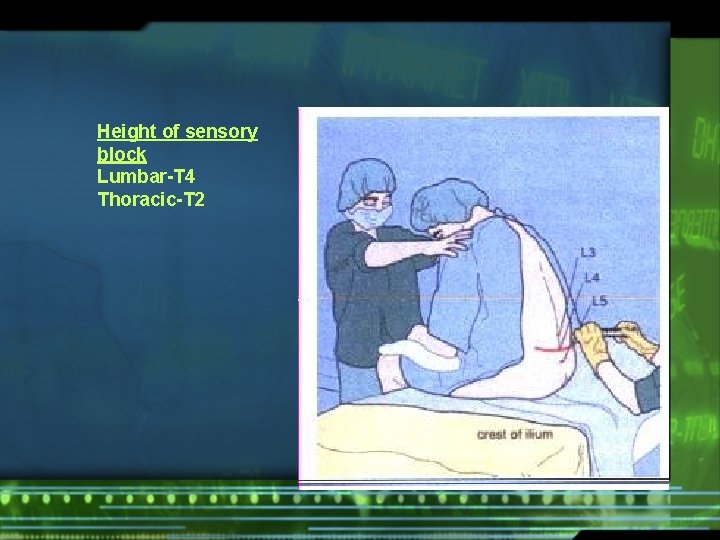
Height of sensory block Lumbar-T 4 Thoracic-T 2
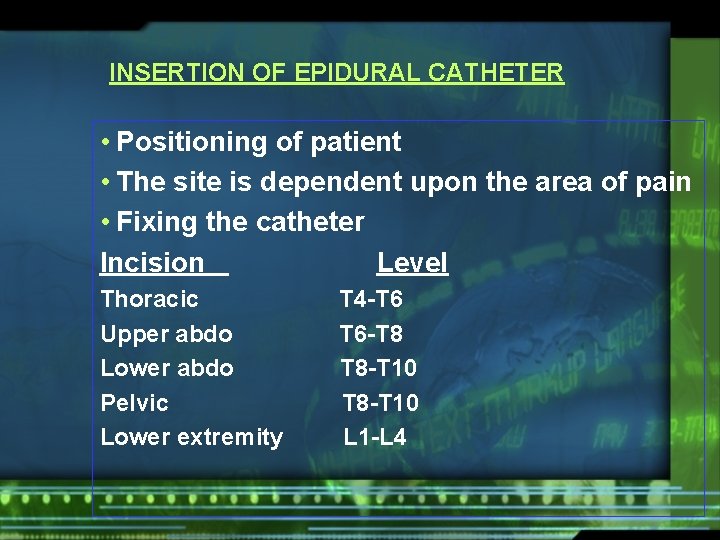
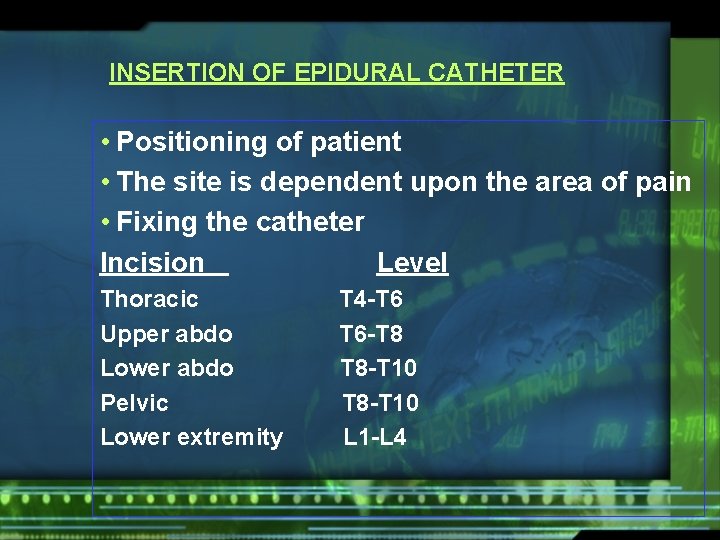
INSERTION OF EPIDURAL CATHETER • Positioning of patient • The site is dependent upon the area of pain • Fixing the catheter Incision Level Thoracic Upper abdo Lower abdo Pelvic Lower extremity T 4 -T 6 T 6 -T 8 T 8 -T 10 L 1 -L 4







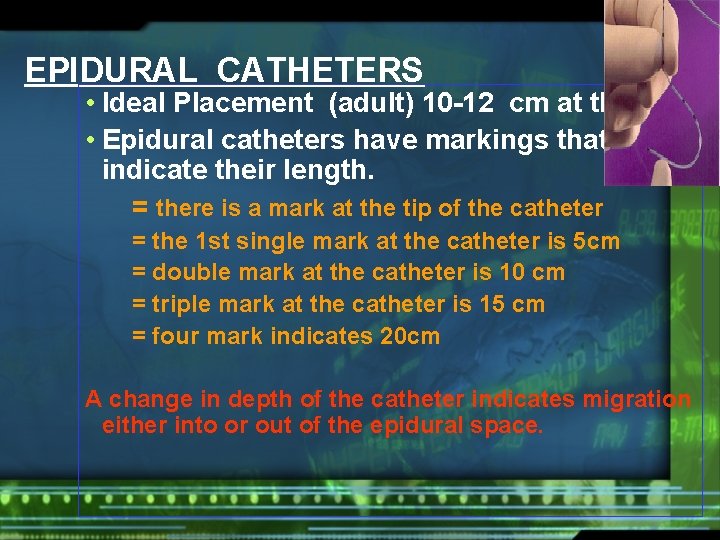
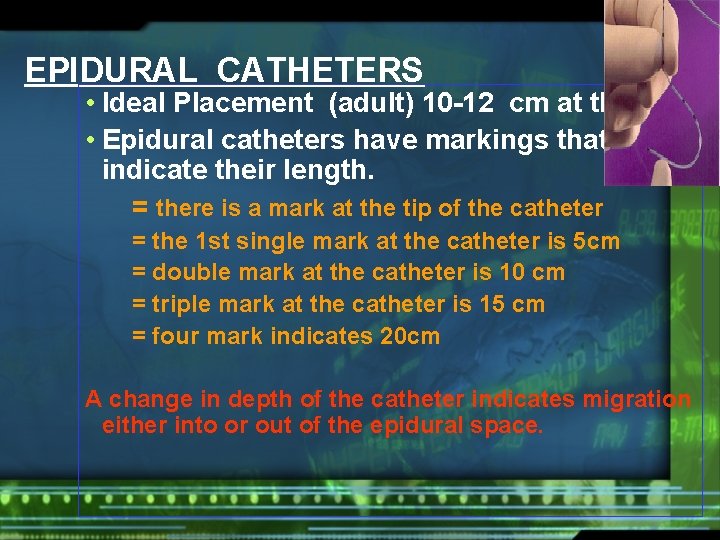
EPIDURAL CATHETERS • Ideal Placement (adult) 10 -12 cm at the skin • Epidural catheters have markings that indicate their length. = there is a mark at the tip of the catheter = the 1 st single mark at the catheter is 5 cm = double mark at the catheter is 10 cm = triple mark at the catheter is 15 cm = four mark indicates 20 cm A change in depth of the catheter indicates migration either into or out of the epidural space.
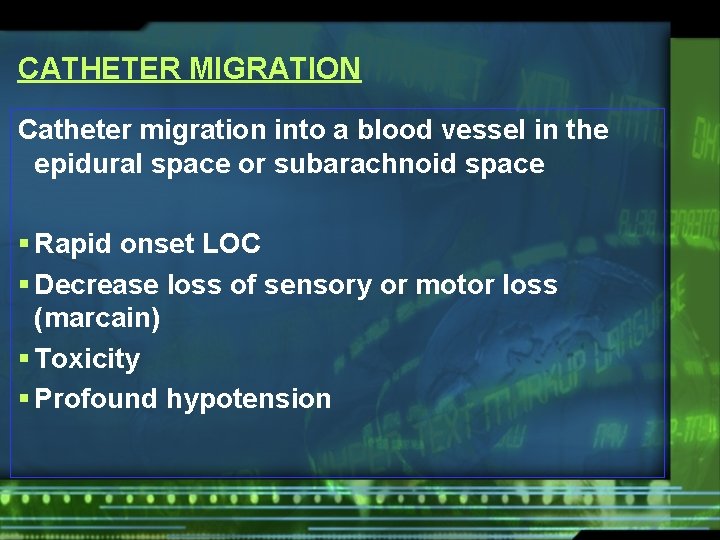
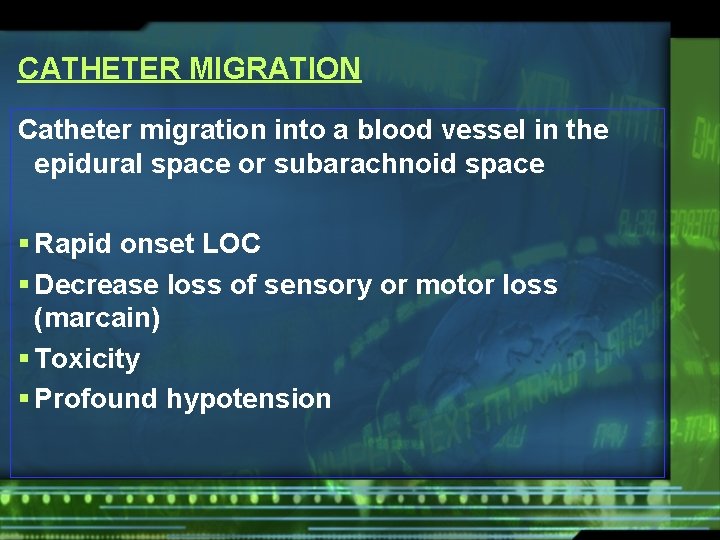
CATHETER MIGRATION Catheter migration into a blood vessel in the epidural space or subarachnoid space § Rapid onset LOC § Decrease loss of sensory or motor loss (marcain) § Toxicity § Profound hypotension
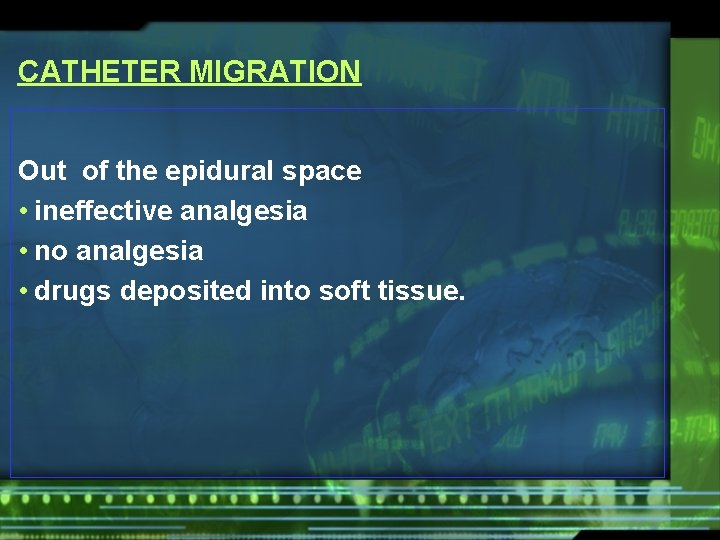
CATHETER MIGRATION Out of the epidural space • ineffective analgesia • no analgesia • drugs deposited into soft tissue.
Advantages/Disadvantages of Regional and Local Anaesthesia.
advantages • patient remains conscious • maintain his own airway • aspiration of gastric contents are unlikely • smooth recovery requiring less skilled nursing care as compared to general anaesthesia
advantages • postoperative analgesia • reduction in surgical stress • earlier discharge for outpatients • less expensive
Disadvantages: • patient may prefer to be asleep • practice and skill is required for the best results. • some blocks require up to 30 minutes or more to be fully effective • analgesia may not always be totally effectivepatient may require additional analgesics, IV sedation, or a light general anaesthetic
Disadvantages: • toxicity may occur if the local anaesthetic is given intravenously or if an overdose is injected • some operations are unsuitable for local anaesthetics, e. g. , thoracotomies
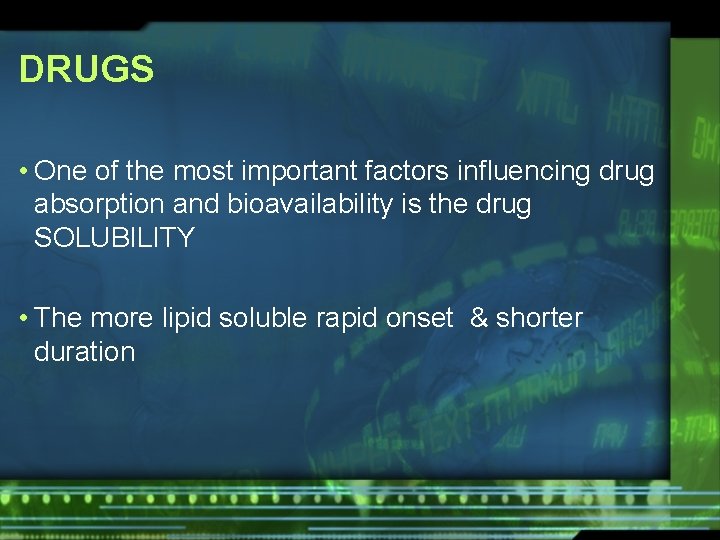
DRUGS • One of the most important factors influencing drug absorption and bioavailability is the drug SOLUBILITY • The more lipid soluble rapid onset & shorter duration
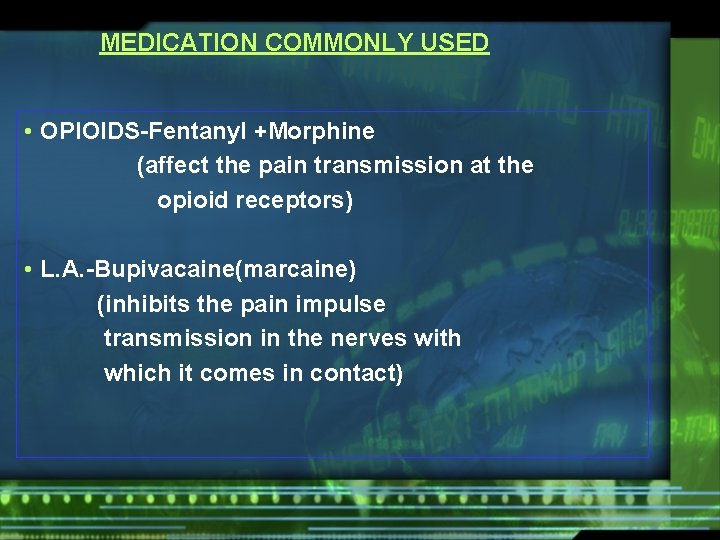
MEDICATION COMMONLY USED • OPIOIDS-Fentanyl +Morphine (affect the pain transmission at the opioid receptors) • L. A. -Bupivacaine(marcaine) (inhibits the pain impulse transmission in the nerves with which it comes in contact)
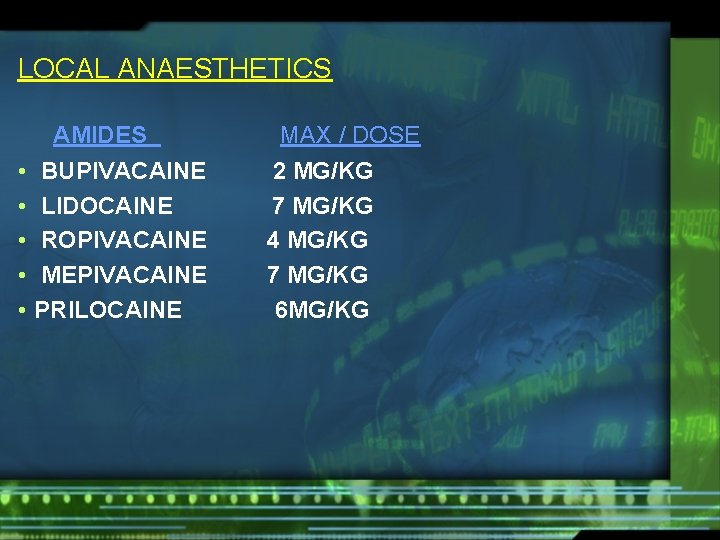
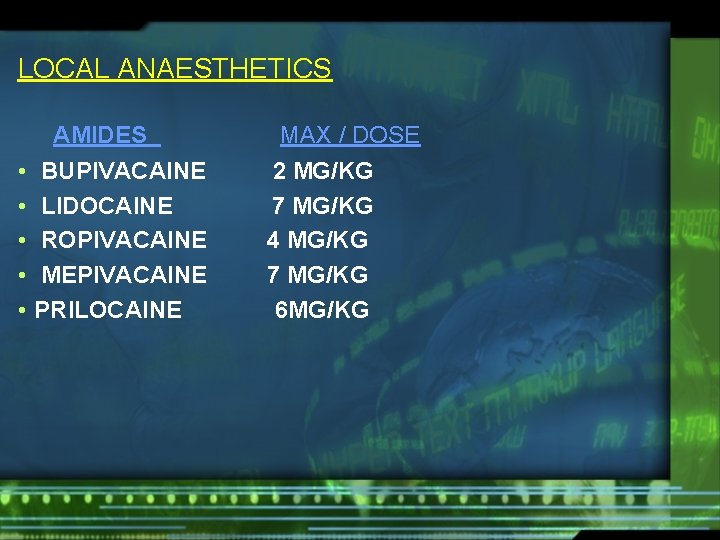
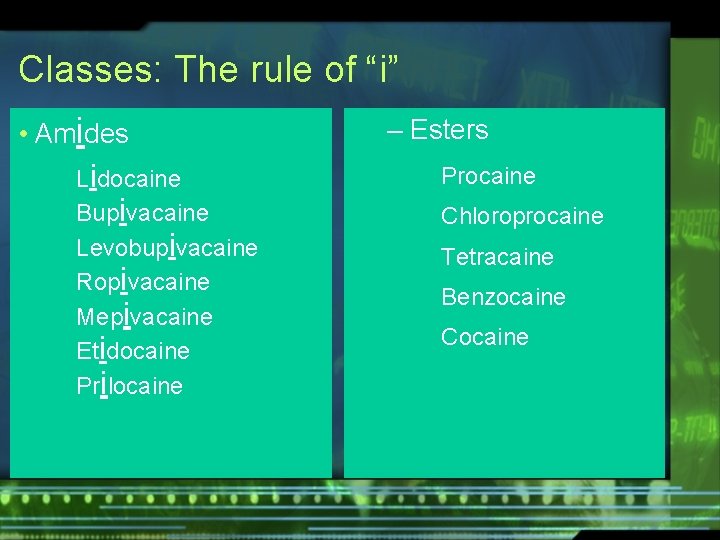
LOCAL ANAESTHETICS AMIDES • • • BUPIVACAINE LIDOCAINE ROPIVACAINE MEPIVACAINE PRILOCAINE MAX / DOSE 2 MG/KG 7 MG/KG 4 MG/KG 7 MG/KG 6 MG/KG
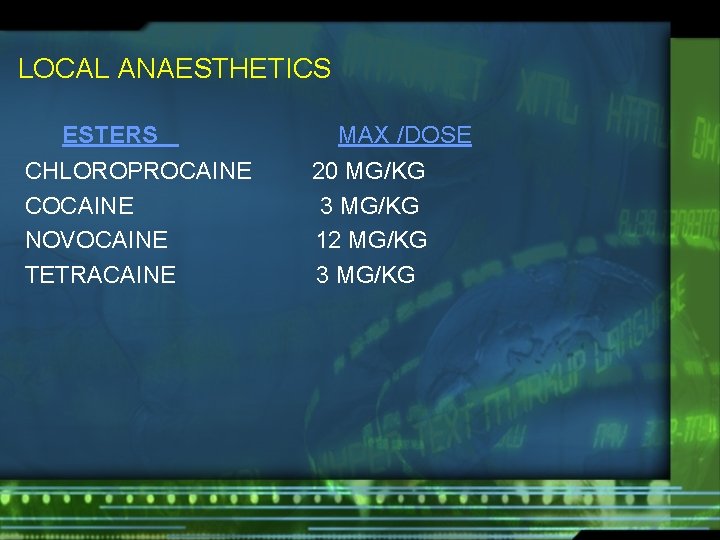
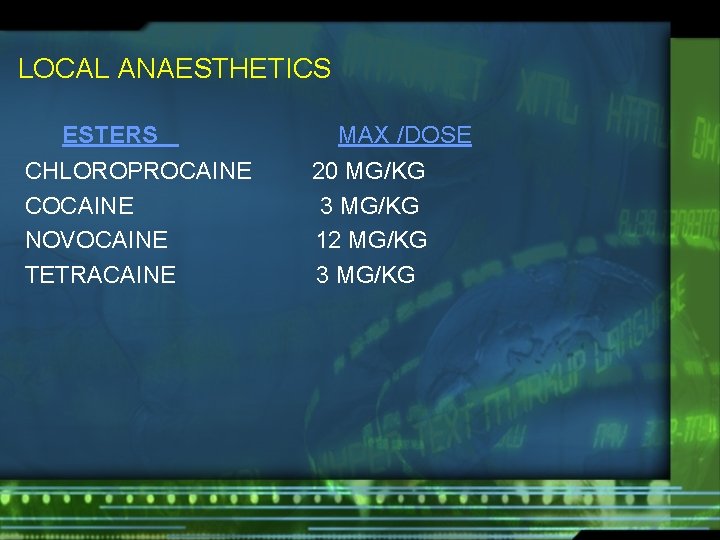
LOCAL ANAESTHETICS ESTERS CHLOROPROCAINE COCAINE NOVOCAINE TETRACAINE MAX /DOSE 20 MG/KG 3 MG/KG 12 MG/KG 3 MG/KG
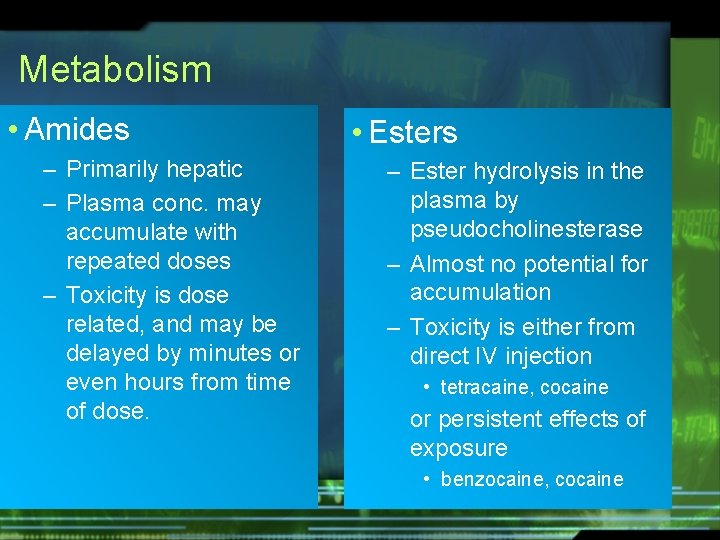
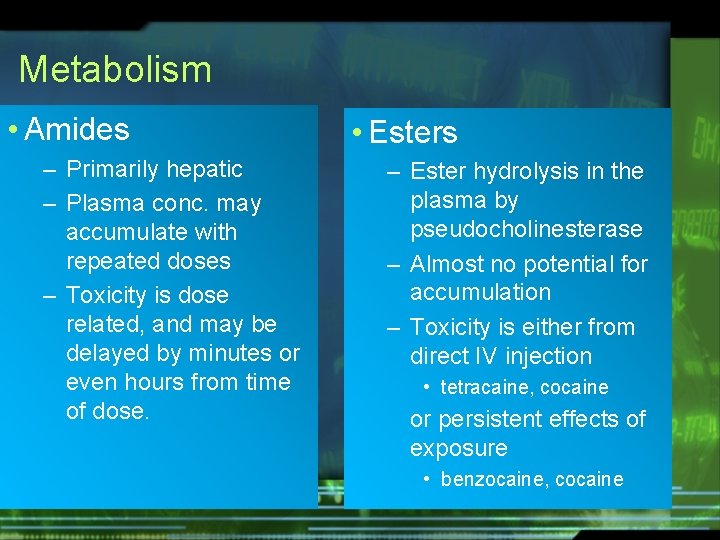
Metabolism • Amides – Primarily hepatic – Plasma conc. may accumulate with repeated doses – Toxicity is dose related, and may be delayed by minutes or even hours from time of dose. • Esters – Ester hydrolysis in the plasma by pseudocholinesterase – Almost no potential for accumulation – Toxicity is either from direct IV injection • tetracaine, cocaine or persistent effects of exposure • benzocaine, cocaine
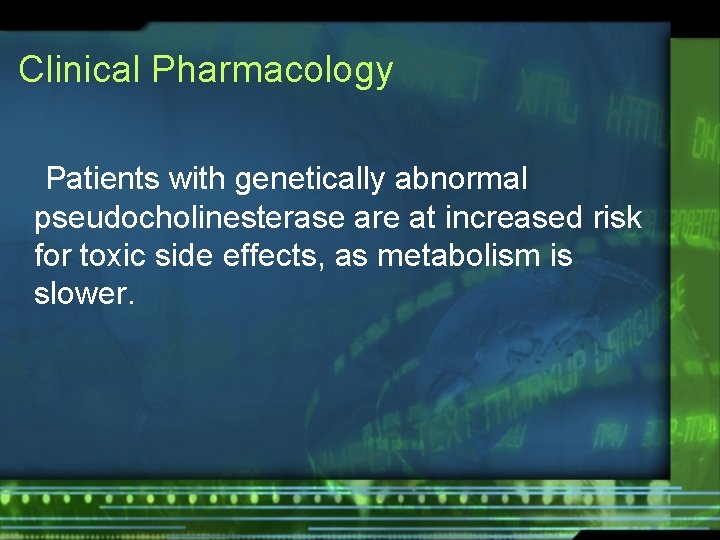
Clinical Pharmacology Patients with genetically abnormal pseudocholinesterase are at increased risk for toxic side effects, as metabolism is slower.
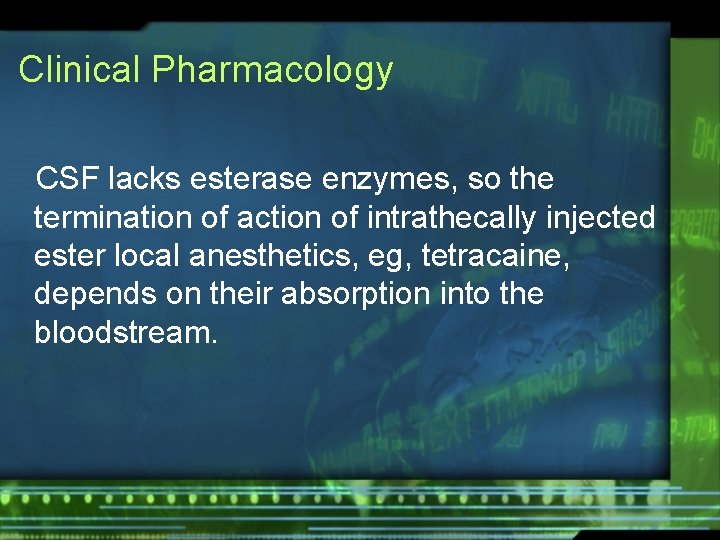
Clinical Pharmacology CSF lacks esterase enzymes, so the termination of action of intrathecally injected ester local anesthetics, eg, tetracaine, depends on their absorption into the bloodstream.
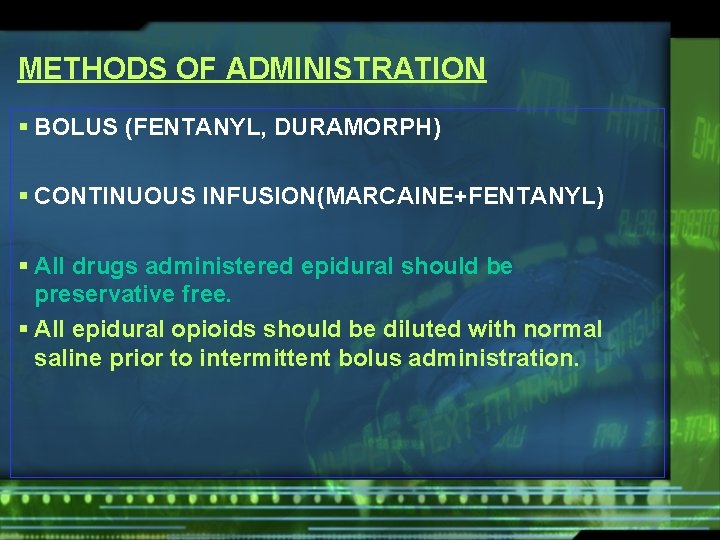
METHODS OF ADMINISTRATION § BOLUS (FENTANYL, DURAMORPH) § CONTINUOUS INFUSION(MARCAINE+FENTANYL) § All drugs administered epidural should be preservative free. § All epidural opioids should be diluted with normal saline prior to intermittent bolus administration.
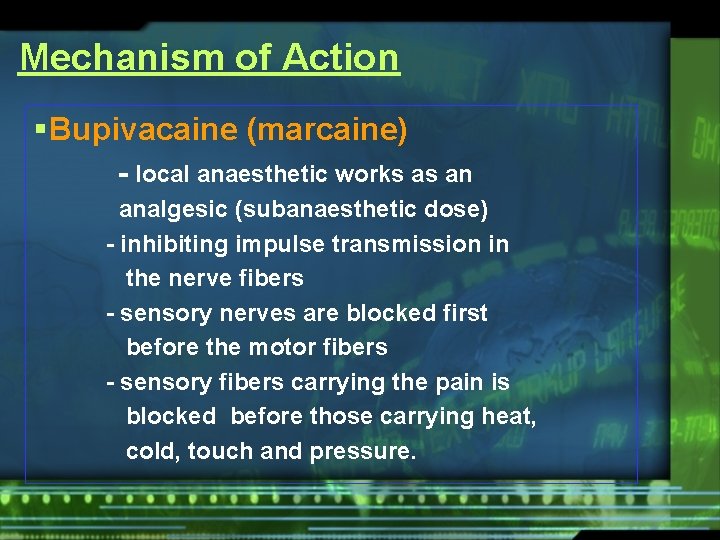
Mechanism of Action § Bupivacaine (marcaine) - local anaesthetic works as an analgesic (subanaesthetic dose) - inhibiting impulse transmission in the nerve fibers - sensory nerves are blocked first before the motor fibers - sensory fibers carrying the pain is blocked before those carrying heat, cold, touch and pressure.
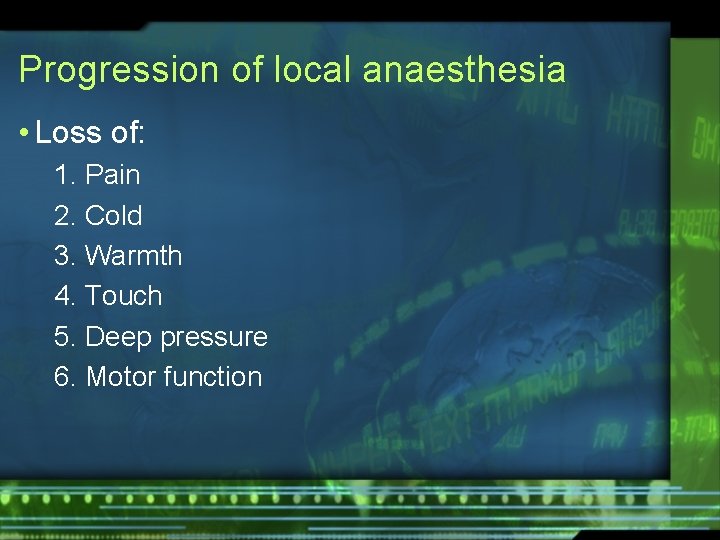
Progression of local anaesthesia • Loss of: 1. Pain 2. Cold 3. Warmth 4. Touch 5. Deep pressure 6. Motor function
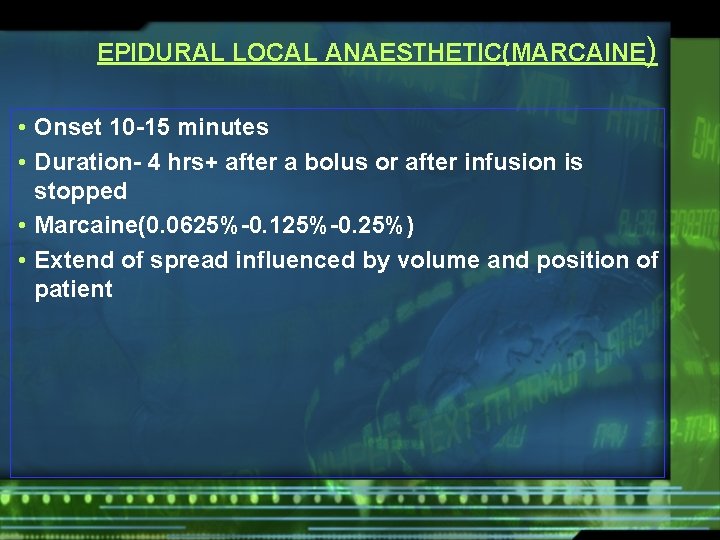
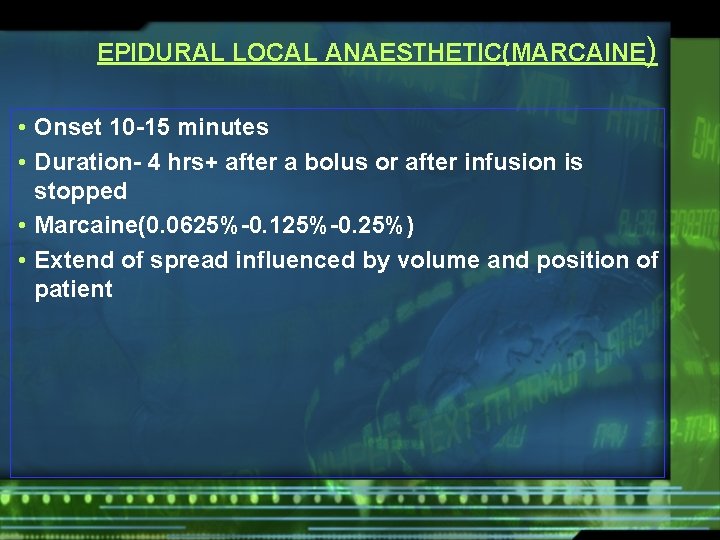
EPIDURAL LOCAL ANAESTHETIC(MARCAINE) • Onset 10 -15 minutes • Duration- 4 hrs+ after a bolus or after infusion is stopped • Marcaine(0. 0625%-0. 125%-0. 25%) • Extend of spread influenced by volume and position of patient
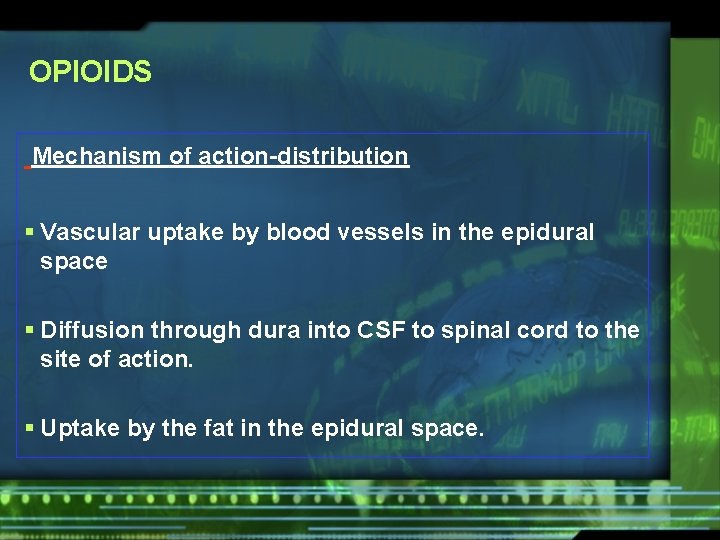
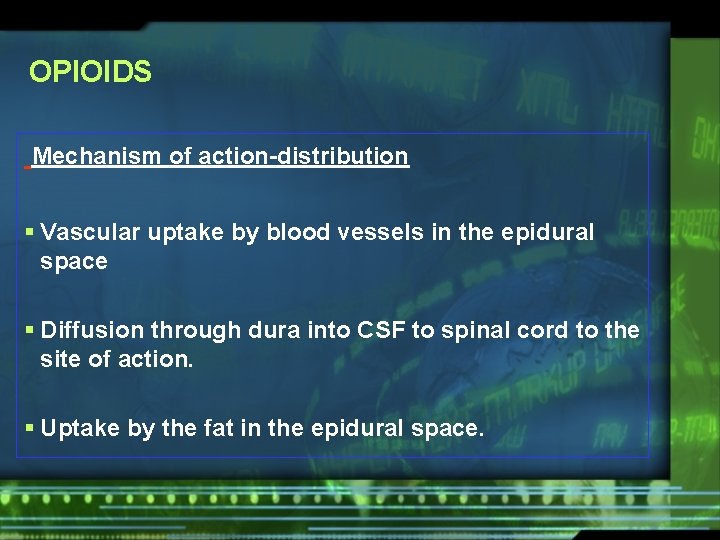
OPIOIDS Mechanism of action-distribution § Vascular uptake by blood vessels in the epidural space § Diffusion through dura into CSF to spinal cord to the site of action. § Uptake by the fat in the epidural space.
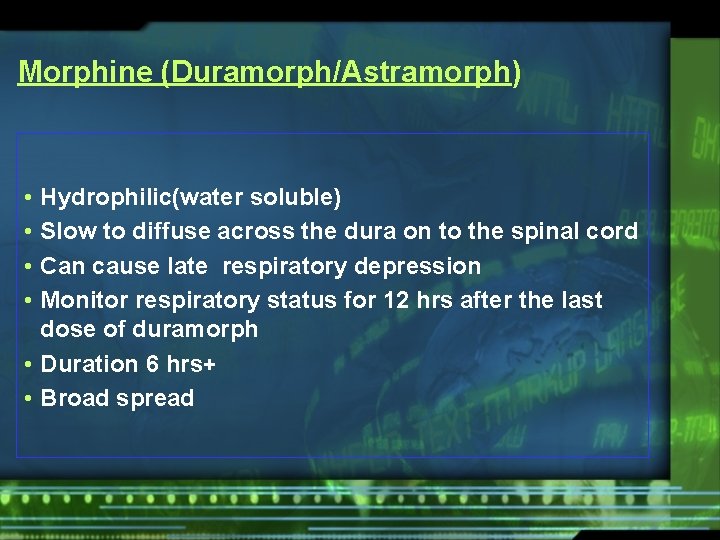
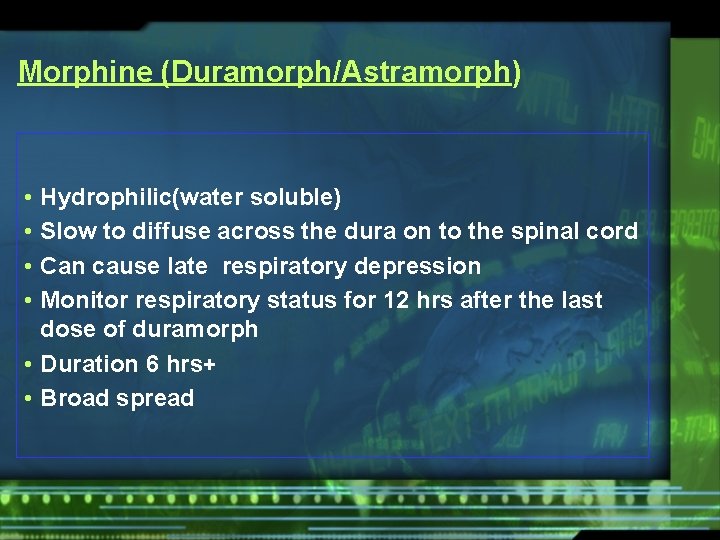
Morphine (Duramorph/Astramorph) • • Hydrophilic(water soluble) Slow to diffuse across the dura on to the spinal cord Can cause late respiratory depression Monitor respiratory status for 12 hrs after the last dose of duramorph • Duration 6 hrs+ • Broad spread
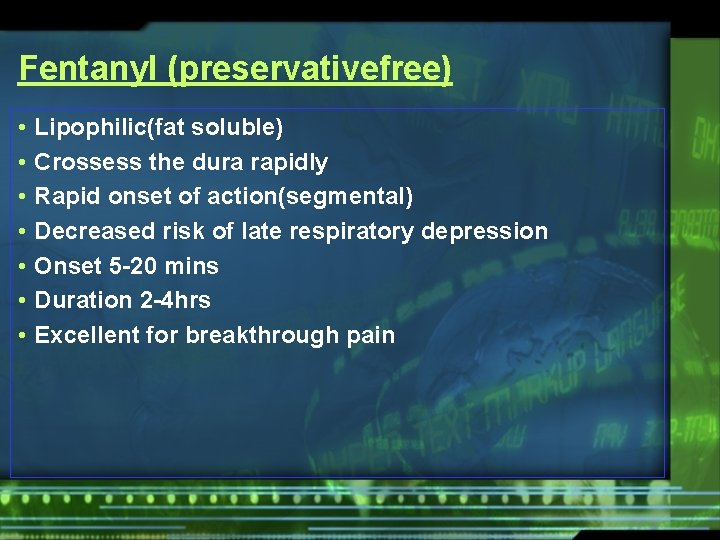
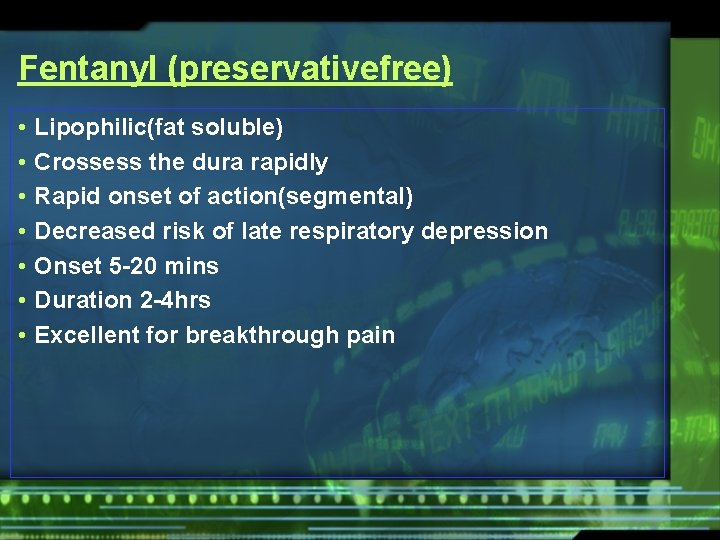
Fentanyl (preservativefree) • • Lipophilic(fat soluble) Crossess the dura rapidly Rapid onset of action(segmental) Decreased risk of late respiratory depression Onset 5 -20 mins Duration 2 -4 hrs Excellent for breakthrough pain
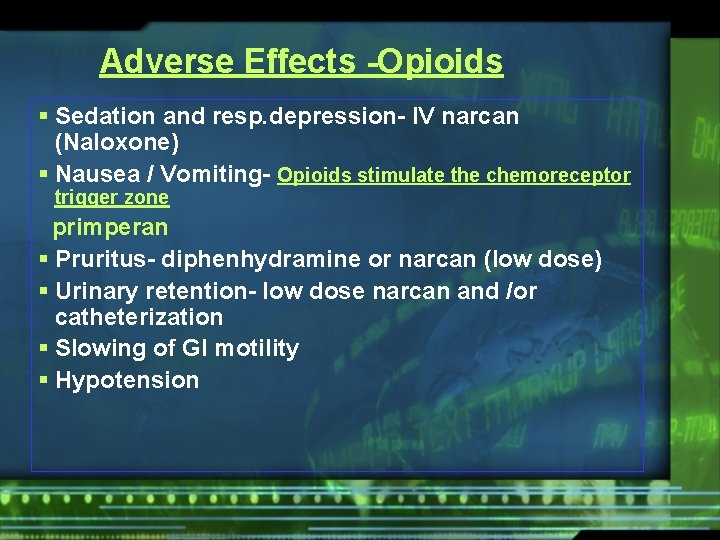
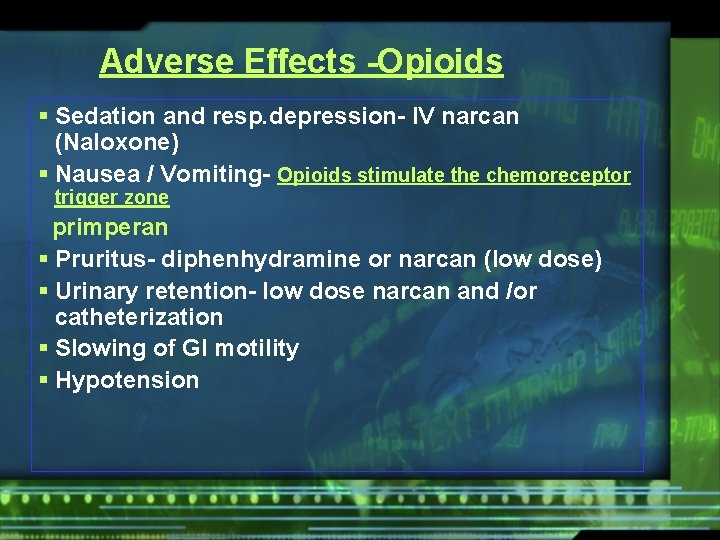
Adverse Effects -Opioids § Sedation and resp. depression- IV narcan (Naloxone) § Nausea / Vomiting- Opioids stimulate the chemoreceptor trigger zone primperan § Pruritus- diphenhydramine or narcan (low dose) § Urinary retention- low dose narcan and /or catheterization § Slowing of GI motility § Hypotension
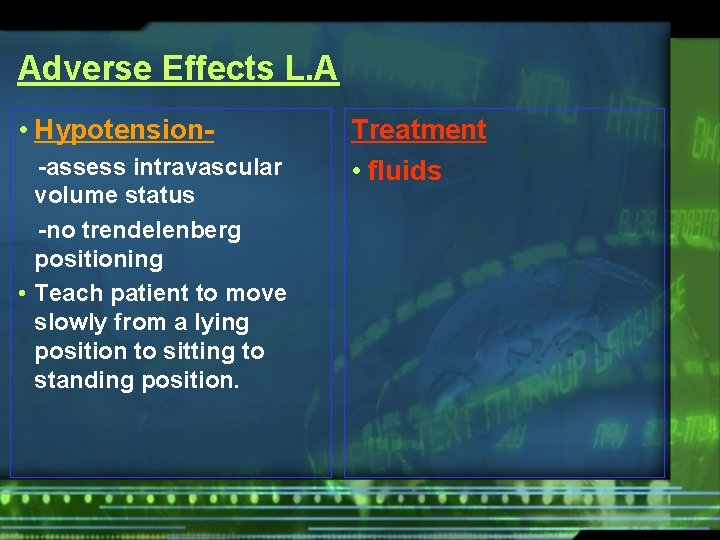
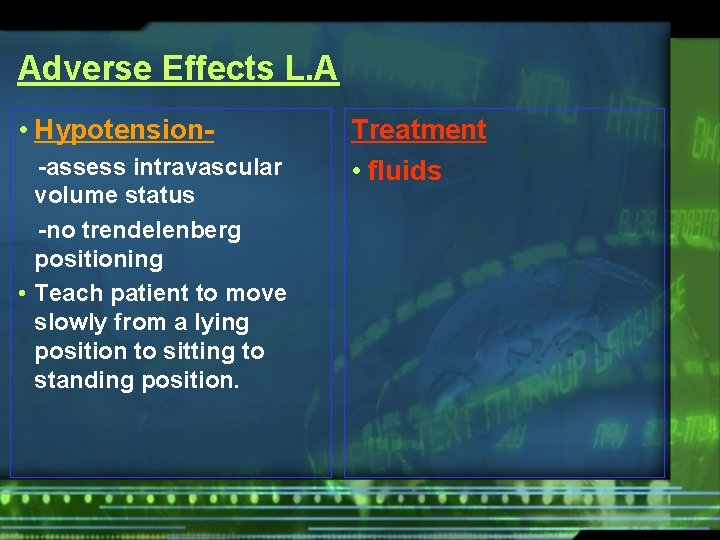
Adverse Effects L. A • Hypotension-assess intravascular volume status -no trendelenberg positioning • Teach patient to move slowly from a lying position to sitting to standing position. Treatment • fluids
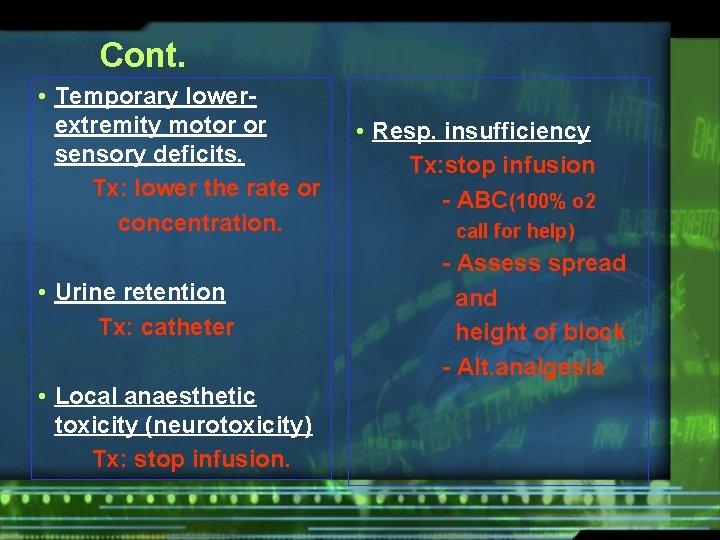
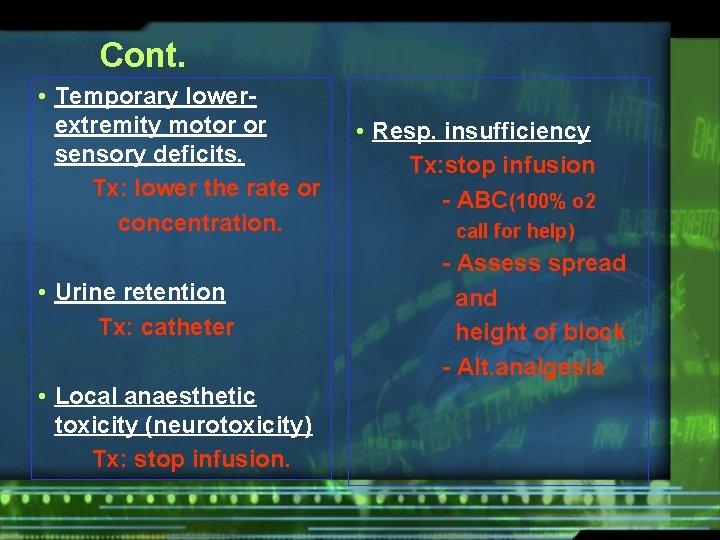
Cont. • Temporary lowerextremity motor or sensory deficits. Tx: lower the rate or concentration. • Urine retention Tx: catheter • Local anaesthetic toxicity (neurotoxicity) Tx: stop infusion. • Resp. insufficiency Tx: stop infusion - ABC(100% o 2 call for help) - Assess spread and height of block - Alt. analgesia
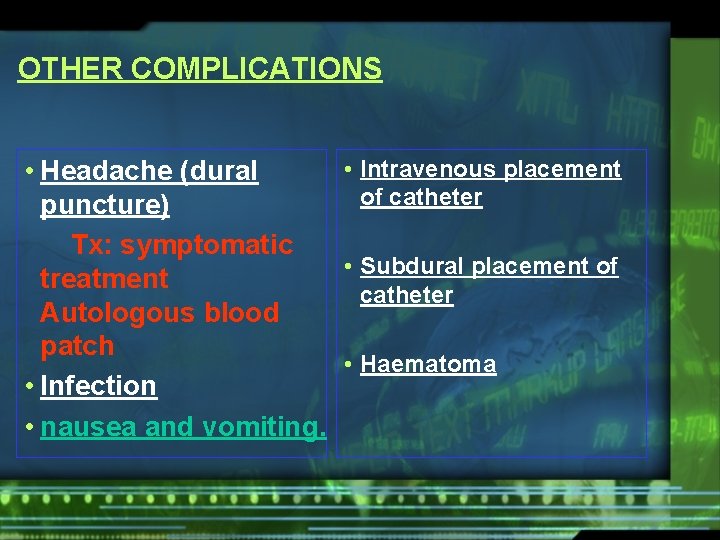
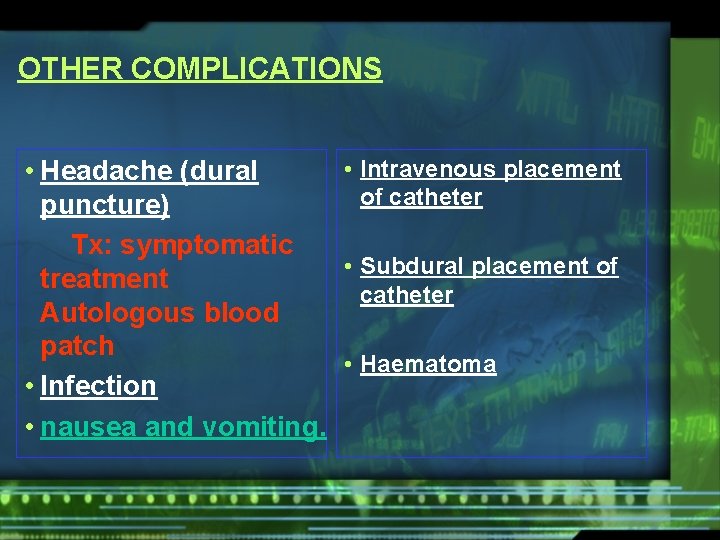
OTHER COMPLICATIONS • Intravenous placement • Headache (dural of catheter puncture) Tx: symptomatic • Subdural placement of treatment catheter Autologous blood patch • Haematoma • Infection • nausea and vomiting.
Signs and Symptoms of Local/Regional Anaesthesia Toxicity • CNS • Cardiovascular
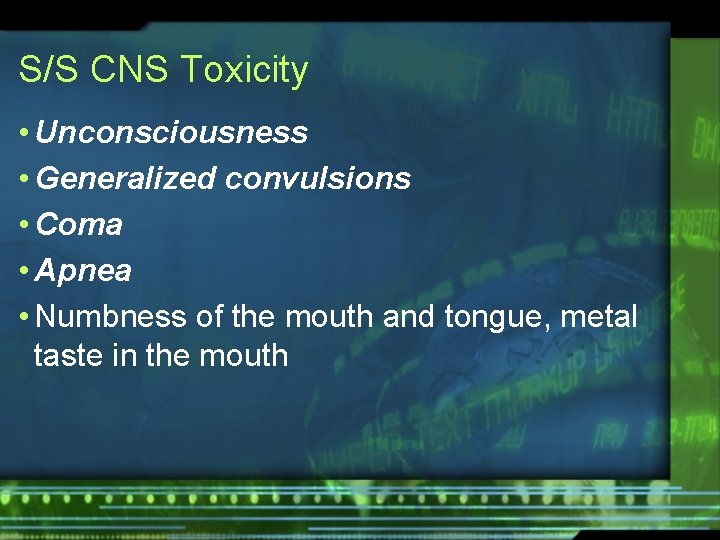
S/S CNS Toxicity • Unconsciousness • Generalized convulsions • Coma • Apnea • Numbness of the mouth and tongue, metal taste in the mouth
S/S CNS Toxicity • Light-headedness • Tinnitus • Visual disturbance • Muscle twitching
Cardiovascular toxicity • slowing of the conduction in the myocardium • myocardial depression • peripheral vasodilatation
Prevention and Treatment of Local/Regional Anaesthesia Toxicity
prevention • Always use the recommended dose • Aspirate through the needle or catheter before injecting the local anesthetic. Intravascular injection can have catastrophic results. • If a large quantity of a drug is required, use a drug of low toxicity and divide the dose into small increments, increasing the total injection time • always inject slowly (<10 ml/min) and communicate with the pt
treatment • All necessary equipment to perform resuscitation, induction, and intubation should be on hand before injection of local/regional anesthetics • Manage airway and give oxygen • Stop convulsions if they continue for more than 15 to 20 seconds – Thiopental 100 mg to 150 mg IV – or Diazepam 5 mg to 20 mg IV
OTHER BLOCKS
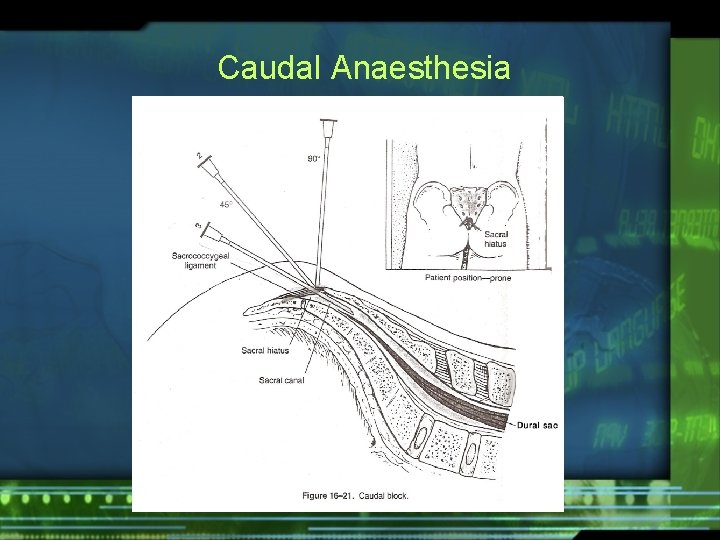
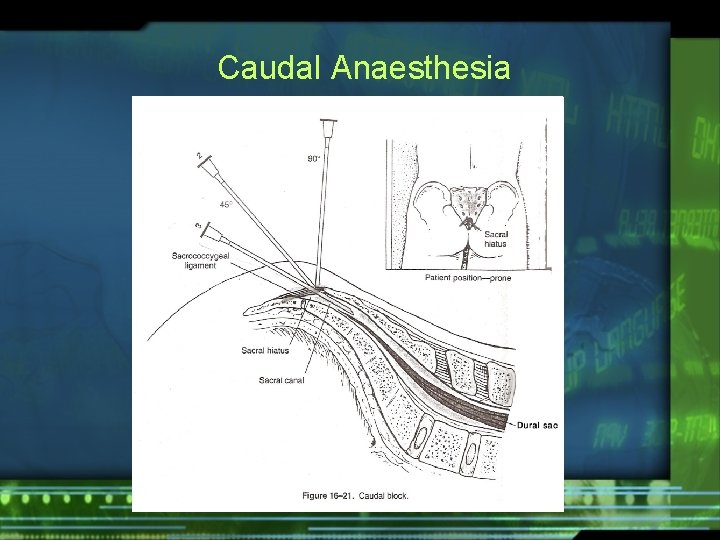
Caudal Anaesthesia

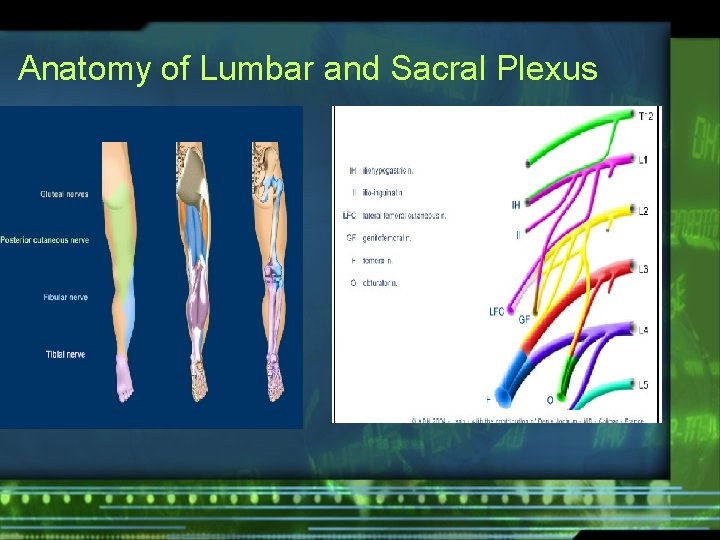
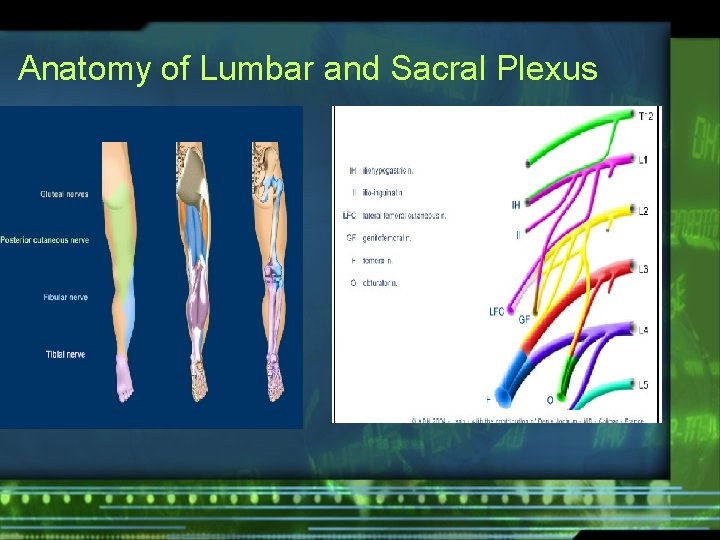
Anatomy of Lumbar and Sacral Plexus





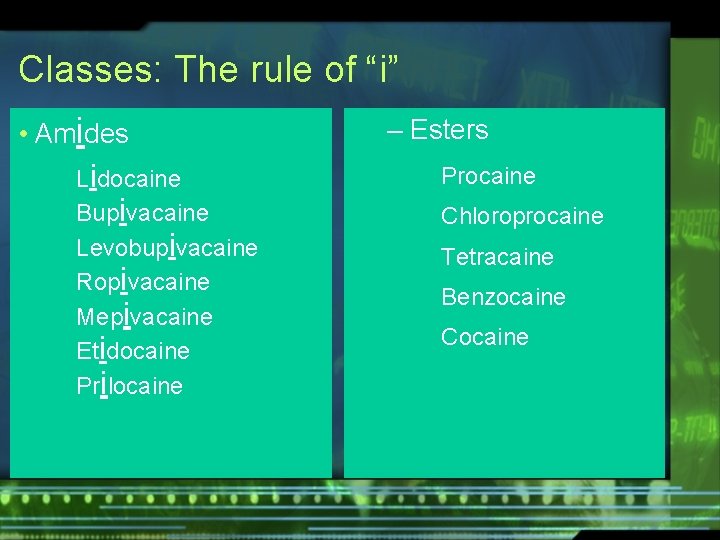
Classes: The rule of “i” • Amides Lidocaine Bupivacaine Levobupivacaine Ropivacaine Mepivacaine Etidocaine Prilocaine – Esters Procaine Chloroprocaine Tetracaine Benzocaine Cocaine

 Analgesia sistemica
Analgesia sistemica Scala di bromage
Scala di bromage Dept of finance and administration
Dept of finance and administration Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Difficult airway algorithm
Difficult airway algorithm Head tilt chin lift jaw thrust
Head tilt chin lift jaw thrust Anesthesia
Anesthesia Paramedian epidural layers
Paramedian epidural layers Components of anaesthesia
Components of anaesthesia Balanced anesthesia components
Balanced anesthesia components Dr pradnya joshi
Dr pradnya joshi Structures pierced in spinal anaesthesia
Structures pierced in spinal anaesthesia Contraindications of spinal anaesthesia
Contraindications of spinal anaesthesia Calcium displacement theory of local anaesthesia
Calcium displacement theory of local anaesthesia Local anesthesia
Local anesthesia Blood patch procedure
Blood patch procedure Balanced anaesthesia ppt
Balanced anaesthesia ppt Anaesthesia information management system
Anaesthesia information management system Dept nmr spectroscopy
Dept nmr spectroscopy Organizational structure of finance department
Organizational structure of finance department Worcester plumbing inspector
Worcester plumbing inspector Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) Mn dept of education
Mn dept of education Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) Employment first ohio
Employment first ohio Poster affiliation
Poster affiliation Vaginal dept
Vaginal dept Gome dept
Gome dept Gome dept
Gome dept Gome dept
Gome dept Gome dept
Gome dept Hoe dept
Hoe dept Lafd interview questions
Lafd interview questions Maine dept of agriculture
Maine dept of agriculture Dept of education
Dept of education Dept a
Dept a Central islip fire dept
Central islip fire dept Dss rowan county
Dss rowan county Dept of education
Dept of education Tabella nmr
Tabella nmr Pt dept logistik
Pt dept logistik Nys dept of homeland security
Nys dept of homeland security La dept of revenue
La dept of revenue La revenue dept
La revenue dept Rewley house continuing education library
Rewley house continuing education library Nebraska dept of agriculture
Nebraska dept of agriculture Iit
Iit Dept ind onegov
Dept ind onegov Albany county dept of social services
Albany county dept of social services Covert prestige and overt prestige
Covert prestige and overt prestige Disadvantages of regional integration
Disadvantages of regional integration Regional and social dialect
Regional and social dialect Position of the body
Position of the body Prograde and retrograde metamorphism venn diagram
Prograde and retrograde metamorphism venn diagram Regional variation linguistics
Regional variation linguistics Indigenized dialect examples
Indigenized dialect examples Chelsea adam and eve regional buyer
Chelsea adam and eve regional buyer Gummy bear lab anatomy
Gummy bear lab anatomy How is specialization connected to interdependence?
How is specialization connected to interdependence? Regional write up head face and neck
Regional write up head face and neck Regional and transregional interactions
Regional and transregional interactions Ministry of regional development and public works
Ministry of regional development and public works Ministry of regional development and public works
Ministry of regional development and public works Entrepreneurship and regional development
Entrepreneurship and regional development Regional and transregional interactions
Regional and transregional interactions Regional area network
Regional area network Neck anatomical term
Neck anatomical term Va roanoke regional loan center
Va roanoke regional loan center Universidad de panama azuero
Universidad de panama azuero