Endocrine Disease and Anaesthesia 4 th year anaesthesia




- Slides: 48
Endocrine Disease and Anaesthesia 4 th year anaesthesia tutorial MBCh. B
Diabetes Mellitus • Excessive production of sweet urine • Caused by absolute or relative insulin deficiency • Increasingly common disease Diabetes Insipidus - excessive production of tasteless urine
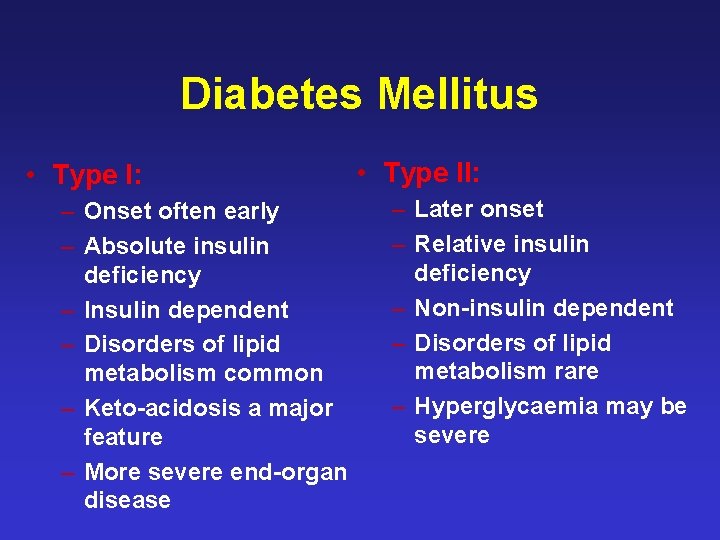
Diabetes Mellitus • Type I: – Onset often early – Absolute insulin deficiency – Insulin dependent – Disorders of lipid metabolism common – Keto-acidosis a major feature – More severe end-organ disease • Type II: – Later onset – Relative insulin deficiency – Non-insulin dependent – Disorders of lipid metabolism rare – Hyperglycaemia may be severe
Acute Consequences of Hyperglycaemia • Dehydration – Fluid deficit 5 - 6 litres • Fatigue & weight loss • Na+, K+ and Mg 2+ deficiency
Chronic Complications of Diabetes Mellitus • Microvascular – Retinopathy – Diabetic nephropathy • Macrovascular – Atherosclerosis • Neuropathic – Autonomic and peripheral neuropathies

Treatment • Insulin – Short acting – Intermediate – Long • Sulphonylureas • Biguanides • Other agents – Thiazolidinediones – Meglitinides – Alpha glucosidase inhibitors
Sulphonylureas • Enhance insulin secretion • Increase peripheral insulin sensitivity – May cause hypoglycaemia • Duration of action 6 - 24 hours
Biguanides Metformin • • Promote glucose utilisation Inhibit hepatic glucose production Less likely to cause hypoglycaemia Lactic acidosis: – Elderly – Renal / hepatic failure – Major surgery
The Surgical Challenge • Stress response evokes a hyperglycaemic response • If on insulin - Risk of hypoglycaemia due to interruption of food intake • Altered consciousness masking signs of hypoglycaemia • End-organ damage
Peri-operative Risks • • Coronary artery disease Diabetic cardiomyopathy Diabetic nephropathy Autonomic neuropathy Glycosylated collagen Decreased wound healing Increased infection
Coronary Heart Disease • Risk of CHD increased 4 - 5 times • Silent myocardial ischaemia
Diabetic Nephropathy • Commonest single cause of renal failure in USA • ACE inhibitors may decrease longterm risk • No effective “renal protective drugs” – Dopamine does not help • Moderate fluid loading is the best protective strategy
Autonomic Neuropathy • Commoner in Type I than Type II – 40 % vs. 15 % • Few patients are symptomatic • Impaired heart rate variability • Haemodynamic instability may occur – Risk increased in uraemic patients • Gastroparesis unresponsive to kinetic agents – May need RSI with cricoid pressure
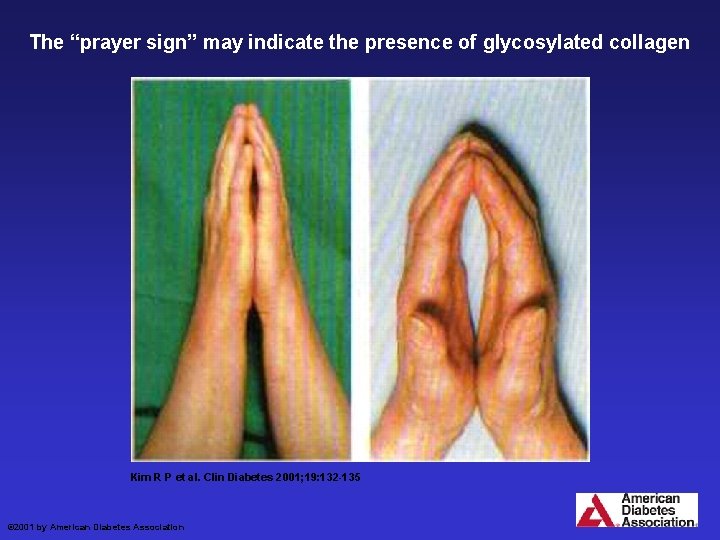
Glycosylated Collagen • • Stiff joint syndrome “Praying hands” sign May affect cervical mobility Possible difficult intubation – Minimal to moderate difficulty 5 % diabetics vs. 1 % in non-diabetics
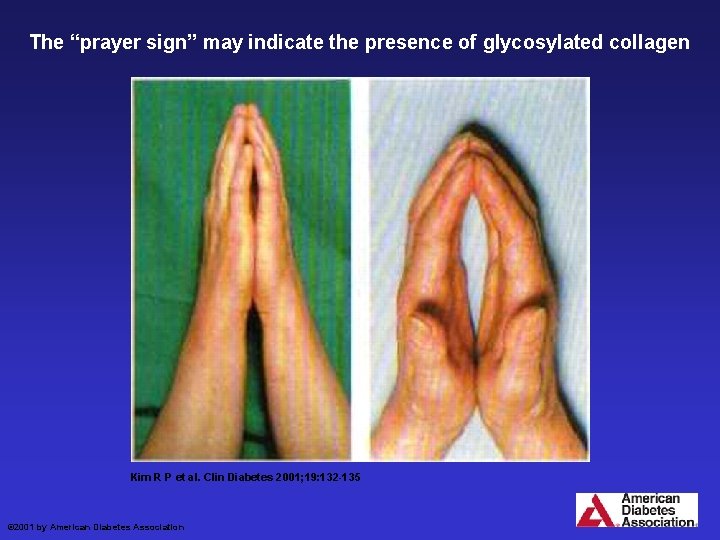
The “prayer sign” may indicate the presence of glycosylated collagen Kim R P et al. Clin Diabetes 2001; 19: 132 -135 © 2001 by American Diabetes Association
Wound Healing • Impaired in all diabetics – may be due to decreased neutrophil function • Improved by long-term glycaemic control • More prone to wound infection
Pre-operative Evaluation 1. Identify type of diabetes 2. Determine quality of control Glycosylated Hb 3. Evaluate end-organ dysfunction Neuropathies – autonomic + peripheral Renal function 4. Assess cardiovascular status BP, ischaemia (ECG)
Regional Anaesthetic • Reduced stress response • Better glycaemic control • Greater risk of hypoglycaemia • Awake patient • Risk of hypotension with autonomic dysfunction • Legal risk of neuropathy • Spinal and epidural abscess • No evidence of improved outcome
General Anaesthesia • May be increased risks of haemodynamic instability • Possible aspiration risk • Myocardial ischaemia • More difficult glycaemic control
Diabetics Minor Surgery • • Avoid hypoglycaemia Light snack before bed Omit insulin / oral agents in the morning Check blood sugar prior to induction Early on the list Regional anaesthetic if possible Restart intake and regular insulin as soon as possible
Diabetics Major Surgery • Convert to sliding scale insulin for 24 hours if poorly controlled • Omit morning dose and check blood sugar • Check blood sugar in theatre – On induction – Every hour • Insulin infusion or regular IV injections if indicated (watch K+) • Restart oral therapy as soon as possible
Intra-operative Insulin Therapy • Hourly sliding scale – Infusion with some dextrose – Infusion with some potassium – Regular IV insulin bolus • Measure blood glucose and electrolytes
Insulin and Crystalloid • Ringer’s lactate Previously discouraged as there is – Poor lactate handling in diabetics – Increased gluconeogenesis 0, 9 % saline thought to be preferable BUT Plasmalyte B or Ringer’s lactate is now preferred as it causes less acidosis!
Diabetic Ketoacidosis (DKA) May have a rapid onset - hours • Fluid resuscitation with Ringer’s lactate / Pasmalyte B to establish urine flow • Intravenous insulin 0, 1 U kg-1 loading 0, 1 U kg-1 hr-1 until blood sugar < 12 mmol l-1 • Check blood sugar, K+ & ketones hourly • Replace K+ and Mg 2+ as indicated, once urine output established • Bicarbonate only if p. H < 7, 1
Hyperosmolar Non-ketotic Hyperglycaemia (HONK) Usually a slow onset - days • Very high plasma osmolality • Fluid depleted • Replace fluids with isotonic fluids (not hypotonic fluid) • Gradual insulin administration • Lower blood sugar 3 - 5 mmol hr-1
Anaesthesia • • • Often require urgent surgery for sepsis Makes control difficult Do not anaesthetise until resuscitated Blood sugar < 20 mmol L-1 p. H > 7, 3 If possible ketosis controlled or at least improving
Postoperative • • Watch closely High mortality Insulin requirements can fluctuate Type II patients may need DVT prophylaxis • Potassium can drop precipitously • Fluid requirements can vary widely
Glucose Control • Tight glucose control (4 – 8 mmol L-1) decreases mortality in: – Cardiac anaesthesia – Brain injury – Trauma BUT Increases mortality from hypoglycaemia • Target 6 – 10 mmol L-1 • Treat < 4 or > 12 mmol L-1
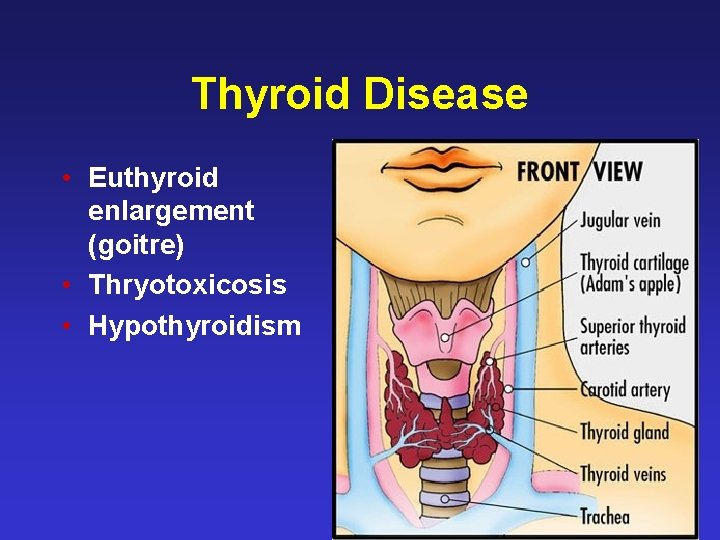
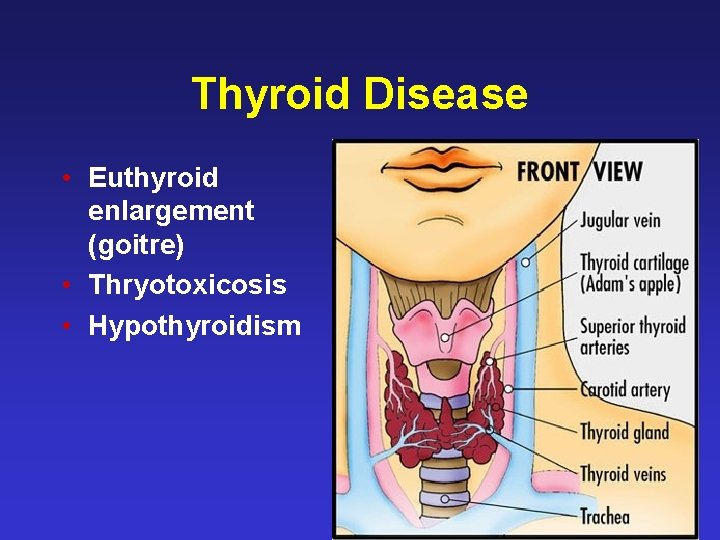
Thyroid Disease • Euthyroid enlargement (goitre) • Thryotoxicosis • Hypothyroidism

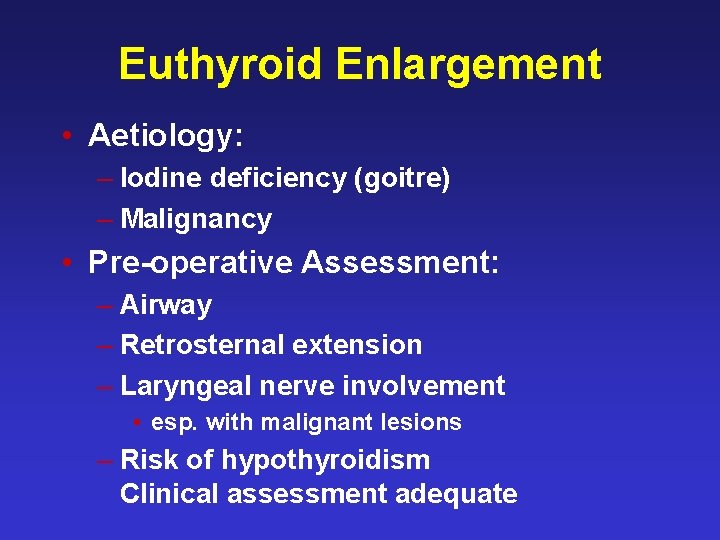
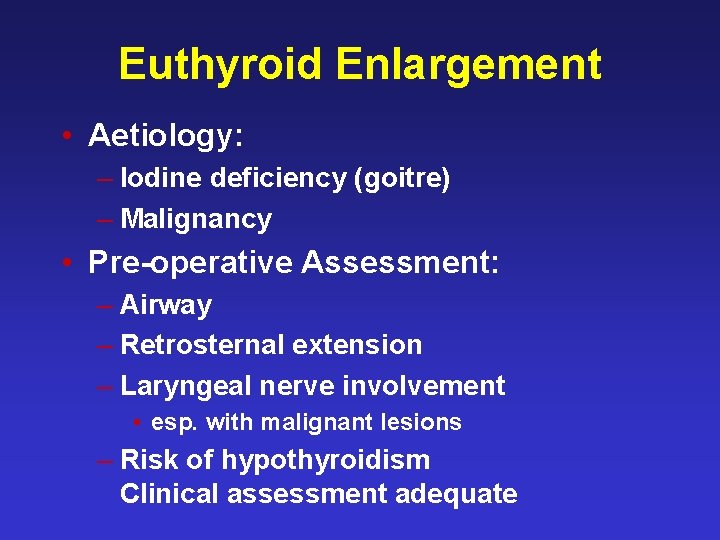
Euthyroid Enlargement • Aetiology: – Iodine deficiency (goitre) – Malignancy • Pre-operative Assessment: – Airway – Retrosternal extension – Laryngeal nerve involvement • esp. with malignant lesions – Risk of hypothyroidism Clinical assessment adequate


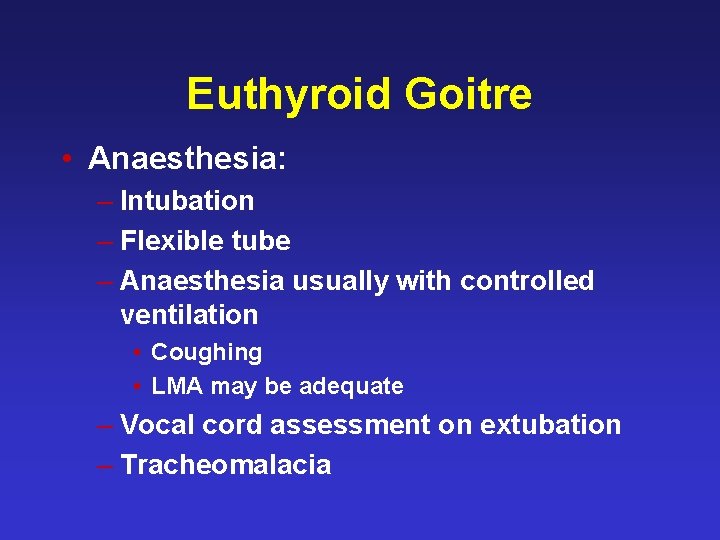
Euthyroid Goitre • Anaesthesia: – Intubation – Flexible tube – Anaesthesia usually with controlled ventilation • Coughing • LMA may be adequate – Vocal cord assessment on extubation – Tracheomalacia
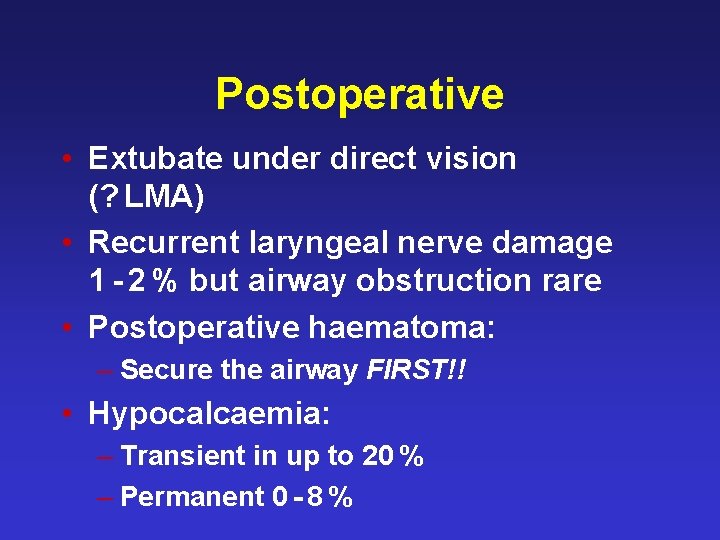
Postoperative • Extubate under direct vision (? LMA) • Recurrent laryngeal nerve damage 1 - 2 % but airway obstruction rare • Postoperative haematoma: – Secure the airway FIRST!! • Hypocalcaemia: – Transient in up to 20 % – Permanent 0 - 8 %
Thyrotoxicosis • Common condition affecting 2 % of women and 0, 2 % of men • Modern drugs make anaesthesia in thyrotoxicosis a rare event • Crisis usually follows another event e. g. pregnancy or malignancy • Do not anaesthetise until euthyroid
Thyroid Storm • May be precipitated by: – Anaesthesia – Surgery – Pregnancy – Systemic illness (esp. infection) – Radio-active iodine therapy • Usually occurs late (hours) after the precipitating event
Management • Oxygen • Cooling • Intravenous fluids – Ringer’s or plamalyte B – 0, 9 % saline may worsen acidosis – Add dextrose
-blockade • Usually treatment of choice – Control heart rate – Inhibit conversion of T 4 to T 3 – High doses may be needed • Non-cardioselective agents preferred – Esmolol initially to establish dose range – Propranolol • Use with caution if cardiac failure or bronchospasm are present
Hypothyroidism • Aetiology: – Thyroiditis, radiation or surgery – Antithyroid drugs – Malignancy – Pituitary failure • Symptoms: – Mental changes: ‘slowing’ – Hypertension, bradycardia, CCF – Anaemia, muscle dysfunction
Hypothyroidism • Diagnosis: – TSH always elevated except in pituitary failure – T 3 and T 4 confirmatory • Preparation: – If severe, establish euthyroid state with SLOW administration of thyroxine • May precipitate myocardial ischaemia – Monitor TSH
Anaesthesia in Hypothyroidism • Sensitivity to drugs: – Anaesthetic agents – Opiates • Careful fluid balance • Ensure adequate reversal of neuromuscular blockade • Control hypoglycaemia and hypothermia
Phaeochromocytoma, Addison’s Disease Conn’s Syndrome • Very high risk • Specialist care • “Do not touch”
Endocrine Disease in Anaesthesia • Diabetes is a very common problem • Goitre is common, but not a major problem • Other endocrine diseases are rare and require specialised care
Obesity
Obesity • Not an endocrine disease per se, but a result of many contributing factors – Diet, exercise, genetics • In a small minority there may be an endocrine aetiology, e. g. Cushing’s • Conversely, obesity may cause type II diabetes and Syndrome X in susceptible individuals
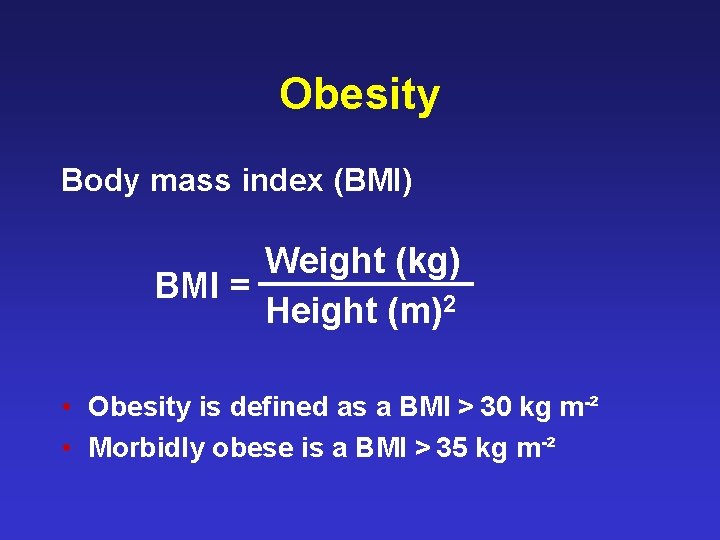
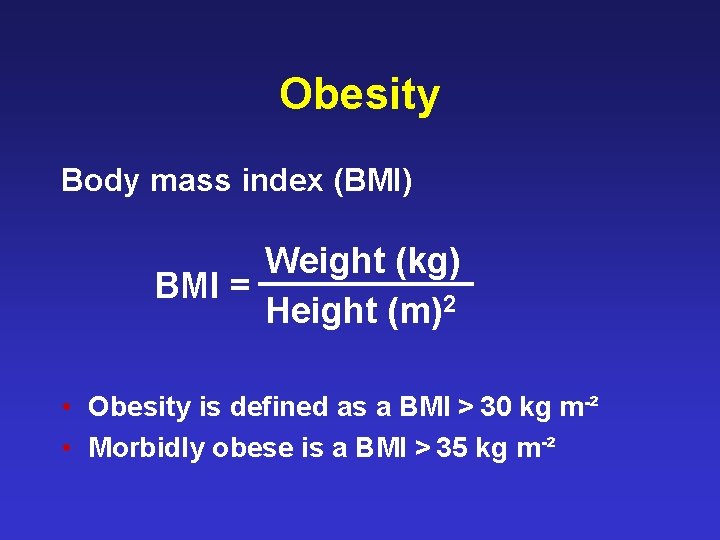
Obesity Body mass index (BMI) Weight (kg) BMI = Height (m)2 • Obesity is defined as a BMI > 30 kg m-² • Morbidly obese is a BMI > 35 kg m-²
Obesity • Patients are at increased risk of: – Hypertension – Ischaemic heart disease – Type II diabetes – Peripheral vascular disease – Hiatus hernia and – Gastro-oesophageal reflux
 Bharathi viswanathan
Bharathi viswanathan Rods airway
Rods airway Nasal trumpet measurement
Nasal trumpet measurement Spinal anaesthesia site
Spinal anaesthesia site Spinal anesthesia structures pierced
Spinal anesthesia structures pierced Classification of inhalational agents
Classification of inhalational agents Balanced anesthesia components
Balanced anesthesia components Spinal anaesthesia position
Spinal anaesthesia position Spinal anaesthesia position
Spinal anaesthesia position Contraindications of spinal anesthesia
Contraindications of spinal anesthesia Appherensive
Appherensive Dose of lidocaine
Dose of lidocaine Bromage scale
Bromage scale Balanced anaesthesia ppt
Balanced anaesthesia ppt Anaesthesia information management system
Anaesthesia information management system Leavers poem primary school
Leavers poem primary school Hyperthyroidea
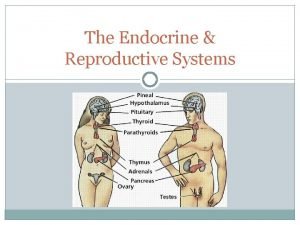
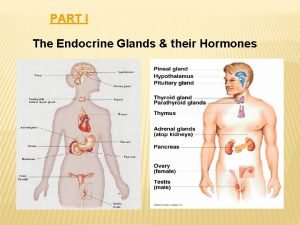
Hyperthyroidea Major endocrine glands male and female
Major endocrine glands male and female Chapter 16 matching question 6-10
Chapter 16 matching question 6-10 Endocrine system and reproductive system
Endocrine system and reproductive system The body's speedy electrochemical communication network
The body's speedy electrochemical communication network Comparison of endocrine and nervous system
Comparison of endocrine and nervous system Difference between endocrine and exocrine glands
Difference between endocrine and exocrine glands Chapter 46 digestive and endocrine disorders
Chapter 46 digestive and endocrine disorders Chapter 45 hormones and the endocrine system
Chapter 45 hormones and the endocrine system Section 39-4 fertilization and development
Section 39-4 fertilization and development Chapter 29 endocrine and metabolic disorders
Chapter 29 endocrine and metabolic disorders Chapter 19 endocrine and hematologic emergencies
Chapter 19 endocrine and hematologic emergencies Exocrine glands are ductless
Exocrine glands are ductless Whats the difference between endocrine and exocrine glands
Whats the difference between endocrine and exocrine glands Endocrine system and nervous system
Endocrine system and nervous system Endocrine system vs nervous system
Endocrine system vs nervous system Hormones
Hormones Endokrin dan eksokrin
Endokrin dan eksokrin Adenohypophysis
Adenohypophysis Portal circulation
Portal circulation Endocrine anatomy
Endocrine anatomy Endocrine molecules
Endocrine molecules Endocrine system fact
Endocrine system fact Lymphatic system vs endocrine system
Lymphatic system vs endocrine system Rat external anatomy
Rat external anatomy Humoral neural and hormonal stimuli
Humoral neural and hormonal stimuli 7:13 endocrine system
7:13 endocrine system Mammillary body
Mammillary body Lamina propria of tongue
Lamina propria of tongue Stimulus humoral
Stimulus humoral Follicular epithelium
Follicular epithelium Endocrine axis
Endocrine axis 30 / 4
30 / 4