Hypothalamic hormones Pituitary hormones Parathyroid hormone Assoc Prof
- Slides: 44
• Hypothalamic hormones • Pituitary hormones • Parathyroid hormone Assoc. Prof. Iv. Lambev E-mail: itlambev@mail. bg www. medpharm-sofia. eu
Hormones (from Greek hormaein – to set in motion) are chemical substances of intense biological activity. They are secreted by specific endocrine glands and are transported in the bloodstream to act on their distant target organs. Hormones regulate body functions and maintain homeostasis in the face of markedly variable external and internal environment. The natural hormones and their synthetic analogues (which in many cases may be more effective), are used as drugs for substitution therapy as well as for pharmacotherapy. In addition, hormone antagonists and hormone synthesis release inhibitors have significant therapeutic importance too.
Classification of hormones 1. Hypothalamic hormones Thyrotropin releasing hormone (TRH) – peptide Corticotropin releasing hormone (CRH) – peptide Gonadotropin releasing hormone (Gn. RH – Gonadorelin): LH-RH/FSH-RH – peptide Growth hormone releasing hormone: (GHRH) – peptide Prolactin releasing hormone (PRH): Unknown
2. Pituitary hormones a) Anterior Pituitary hormones (-tropins/-trop Growth hormone (GH) − Somatotropin Prolactin Adrenocorticotropic hormone (ACTH, Cortico Thyroid stimulating hormones (TSH, Thyrotro Gonadotropins - Follicle stimulating hormone (FSH) - Luteinizing hormone (LH) b) Posterior Pituitary hormones Oxytocin Antidiuretic hormone (ADH, Vasopressin)
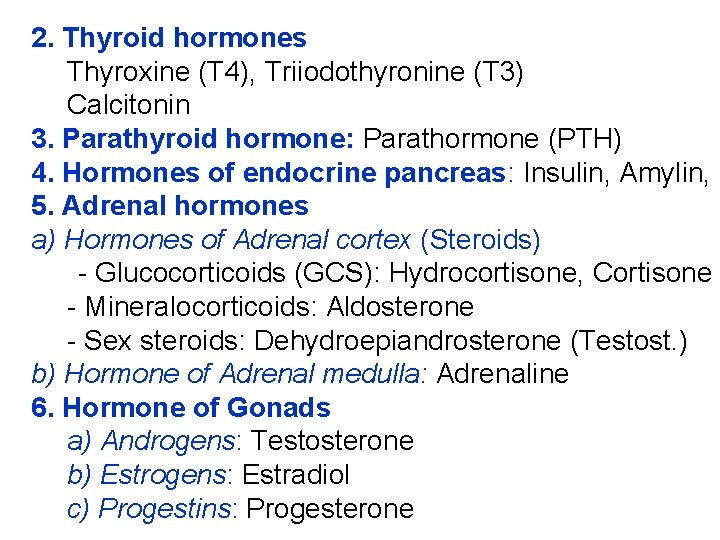
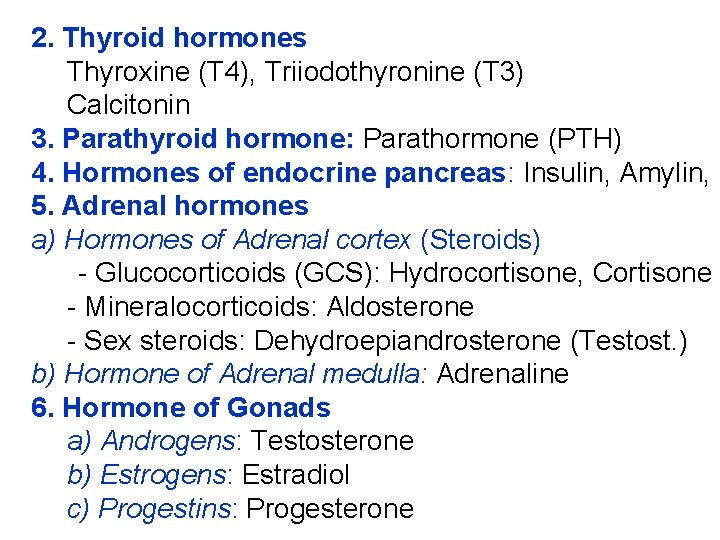
2. Thyroid hormones Thyroxine (T 4), Triiodothyronine (T 3) Calcitonin 3. Parathyroid hormone: Parathormone (PTH) 4. Hormones of endocrine pancreas: Insulin, Amylin, G 5. Adrenal hormones a) Hormones of Adrenal cortex (Steroids) - Glucocorticoids (GCS): Hydrocortisone, Cortisone - Mineralocorticoids: Aldosterone - Sex steroids: Dehydroepiandrosterone (Testost. ) b) Hormone of Adrenal medulla: Adrenaline 6. Hormone of Gonads a) Androgens: Testosterone b) Estrogens: Estradiol c) Progestins: Progesterone
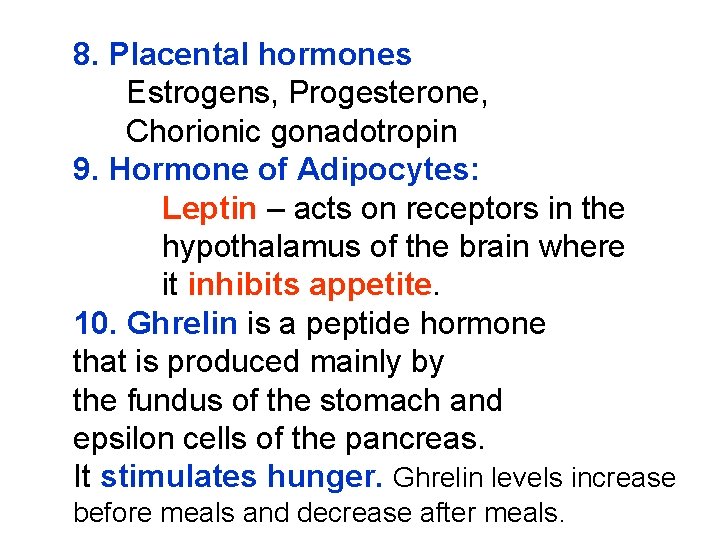
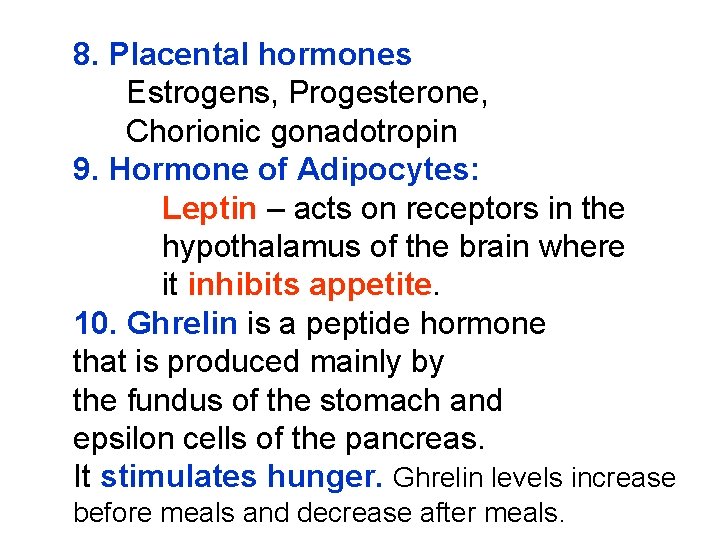
8. Placental hormones Estrogens, Progesterone, Chorionic gonadotropin 9. Hormone of Adipocytes: Leptin – acts on receptors in the hypothalamus of the brain where it inhibits appetite. 10. Ghrelin is a peptide hormone that is produced mainly by the fundus of the stomach and epsilon cells of the pancreas. It stimulates hunger. Ghrelin levels increase before meals and decrease after meals.
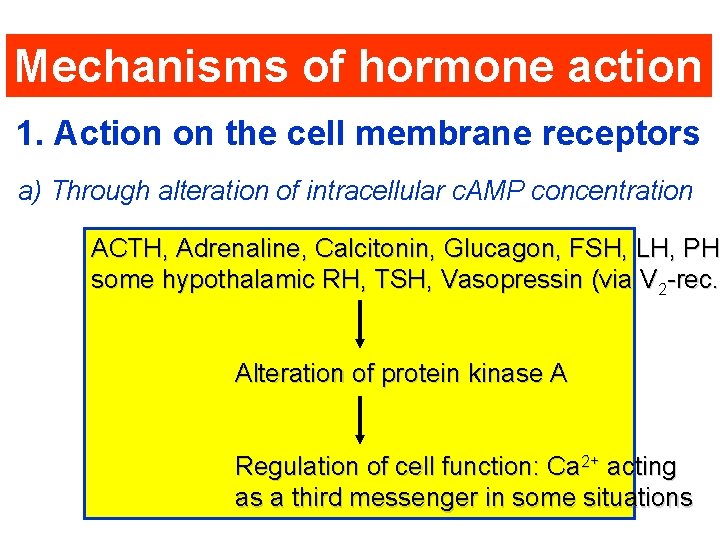
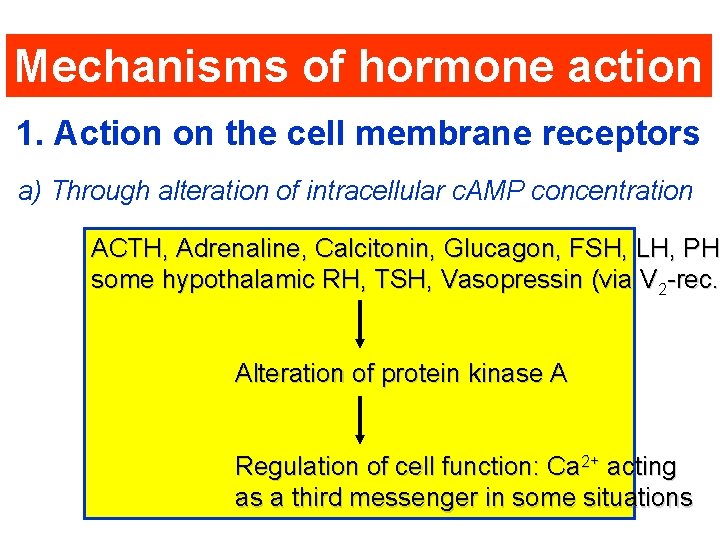
Mechanisms of hormone action 1. Action on the cell membrane receptors a) Through alteration of intracellular c. AMP concentration ACTH, Adrenaline, Calcitonin, Glucagon, FSH, LH, PHT PH some hypothalamic RH, TSH, Vasopressin (via V 2 -rec. ) -rec. Alteration of protein kinase A Regulation of cell function: Ca 2+ acting as a third messenger in some situations
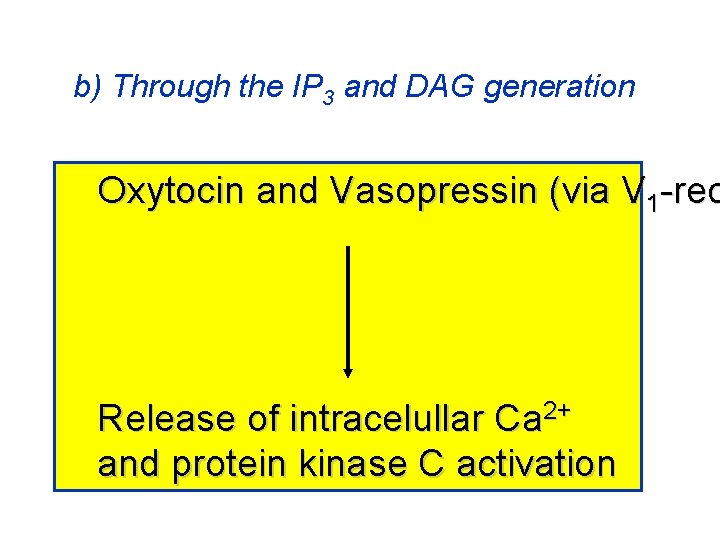
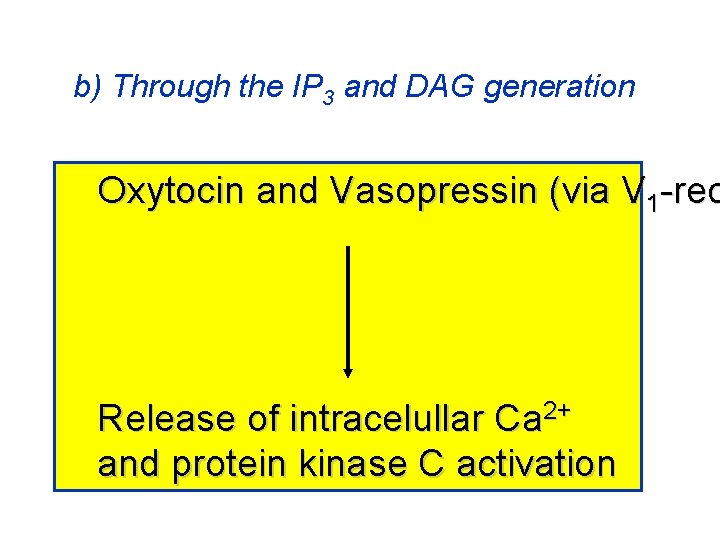
b) Through the IP 3 and DAG generation Oxytocin and Vasopressin (via V 1 -rec Release of intracelullar Ca 2+ and protein kinase C activation
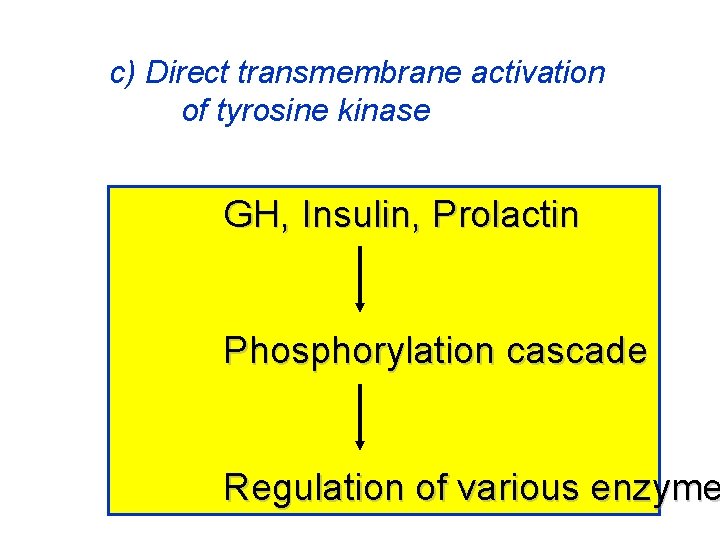
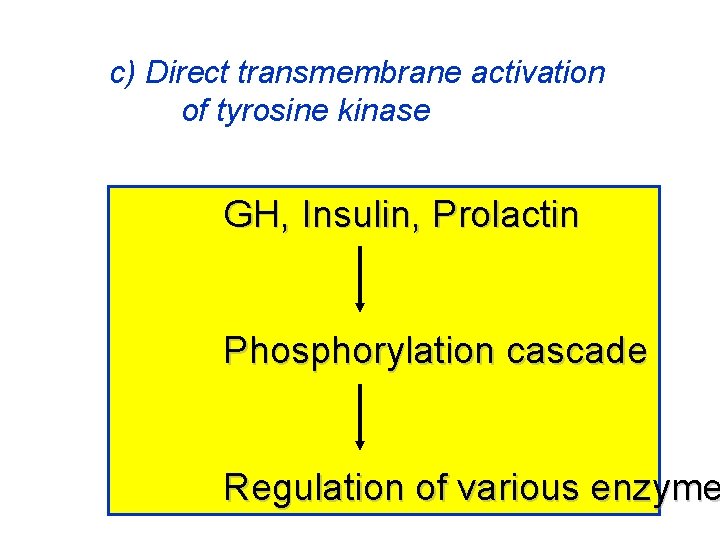
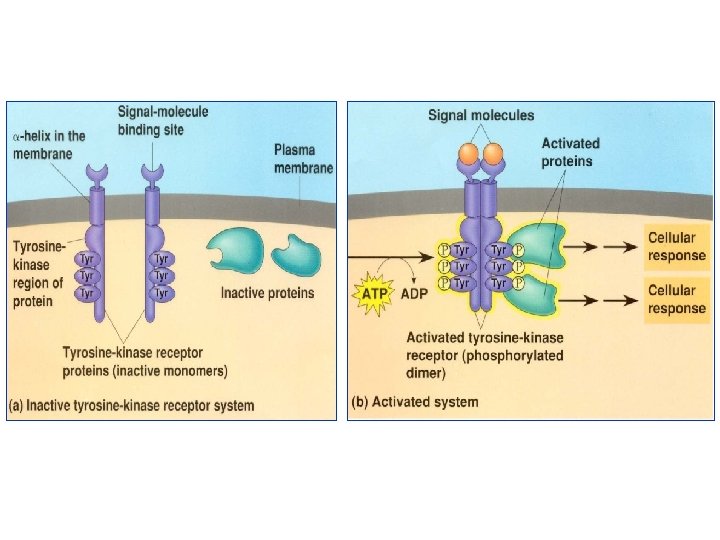
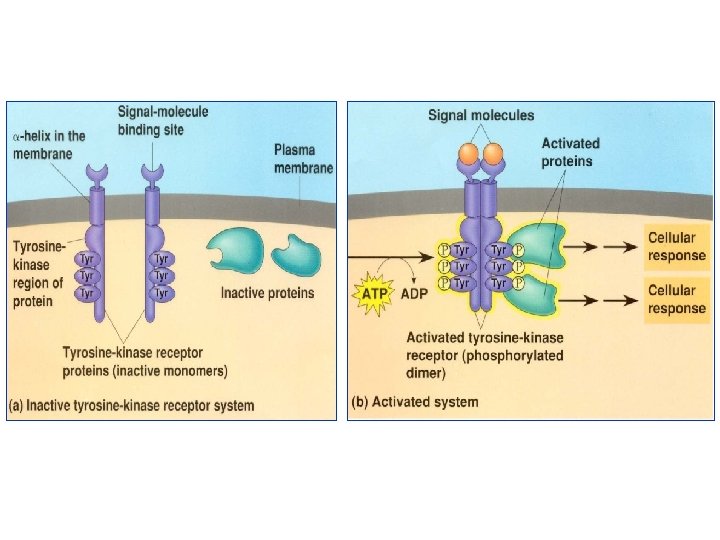
c) Direct transmembrane activation of tyrosine kinase GH, Insulin, Prolactin Phosphorylation cascade Regulation of various enzyme
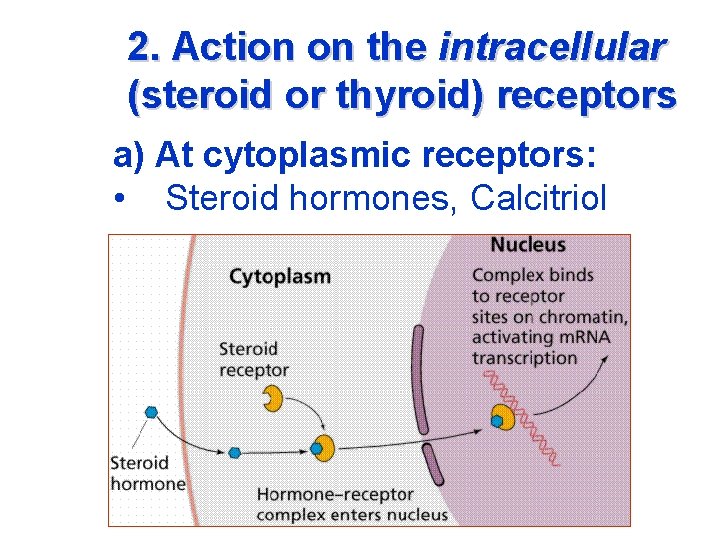
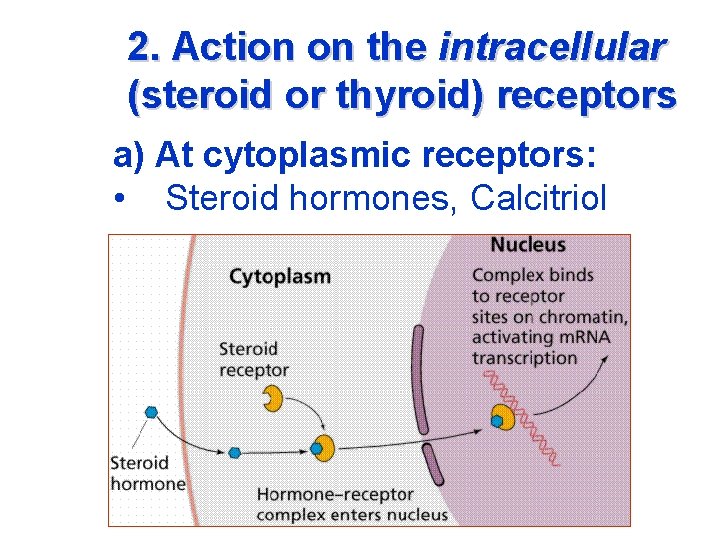
2. Action on the intracellular (steroid or thyroid) receptors a) At cytoplasmic receptors: • Steroid hormones, Calcitriol
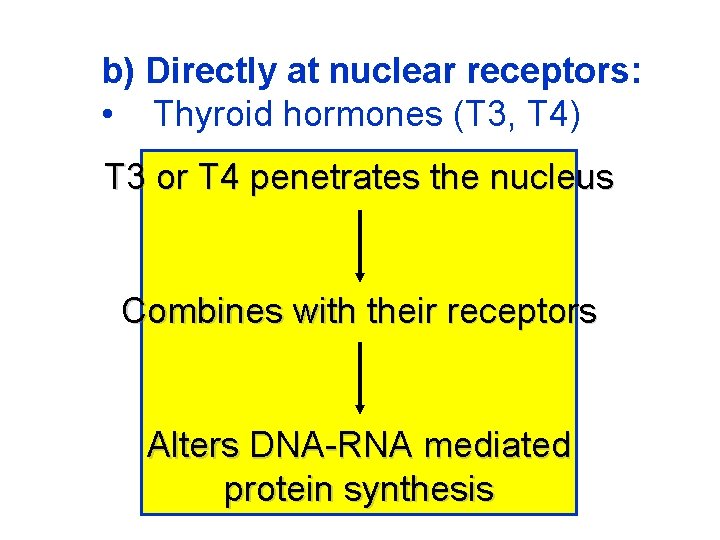
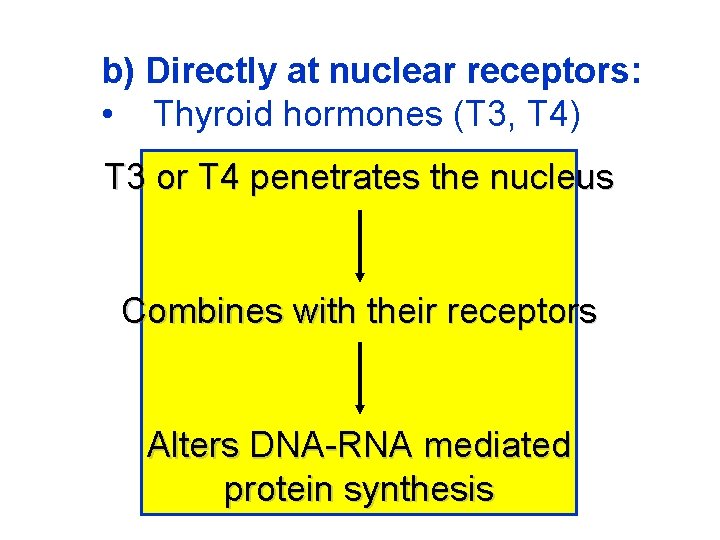
b) Directly at nuclear receptors: • Thyroid hormones (T 3, T 4) T 3 or T 4 penetrates the nucleus Combines with their receptors Alters DNA-RNA mediated protein synthesis
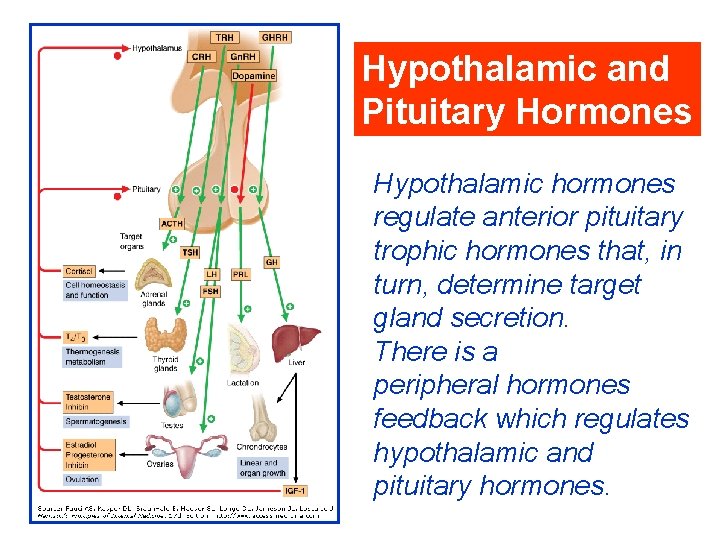
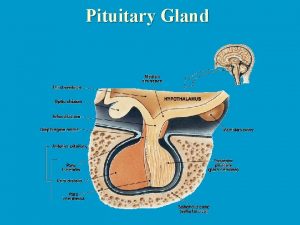
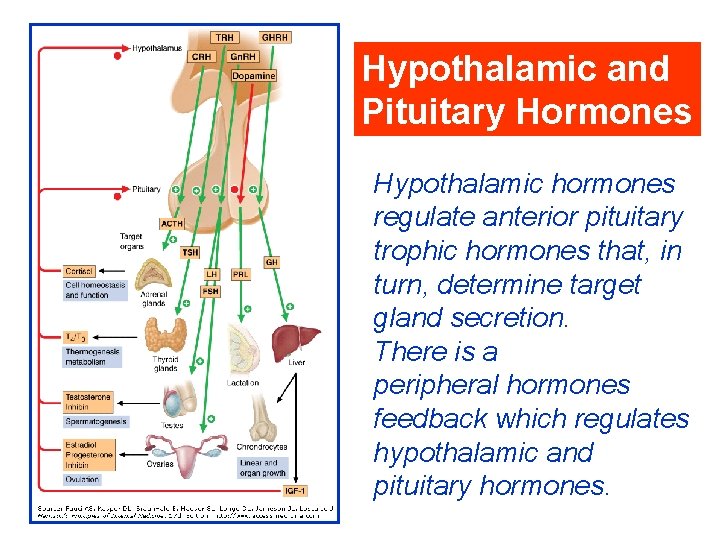
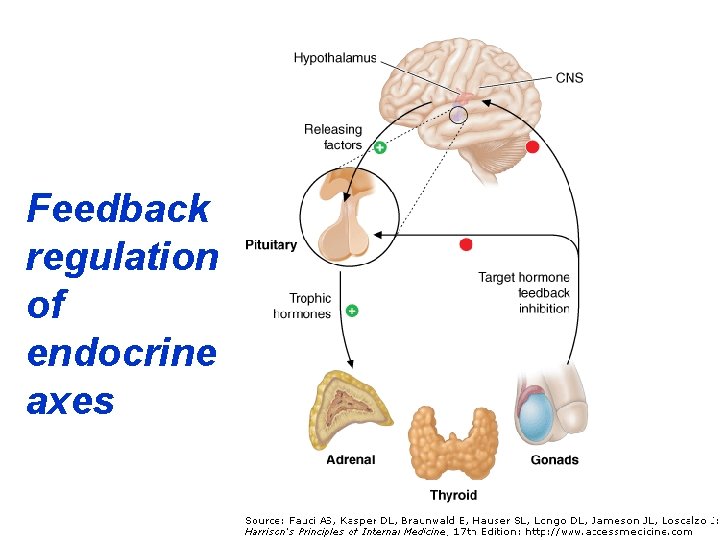
Hypothalamic and Pituitary Hormones Hypothalamic hormones regulate anterior pituitary trophic hormones that, in turn, determine target gland secretion. There is a peripheral hormones feedback which regulates hypothalamic and pituitary hormones.
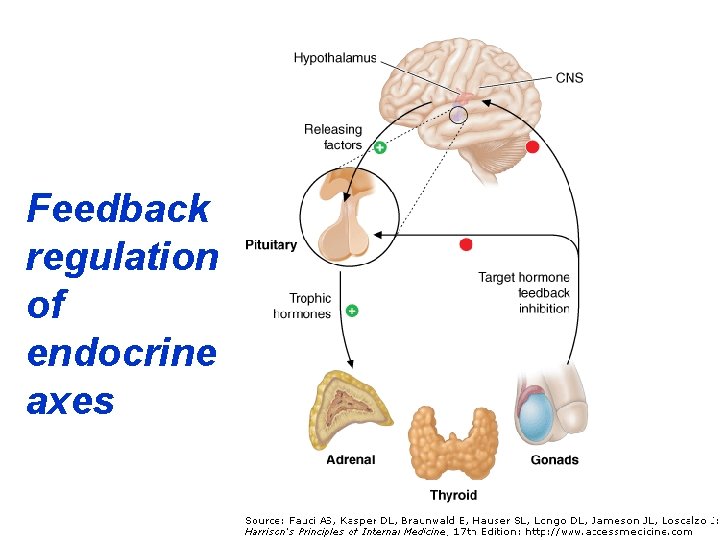
Feedback regulation of endocrine axes
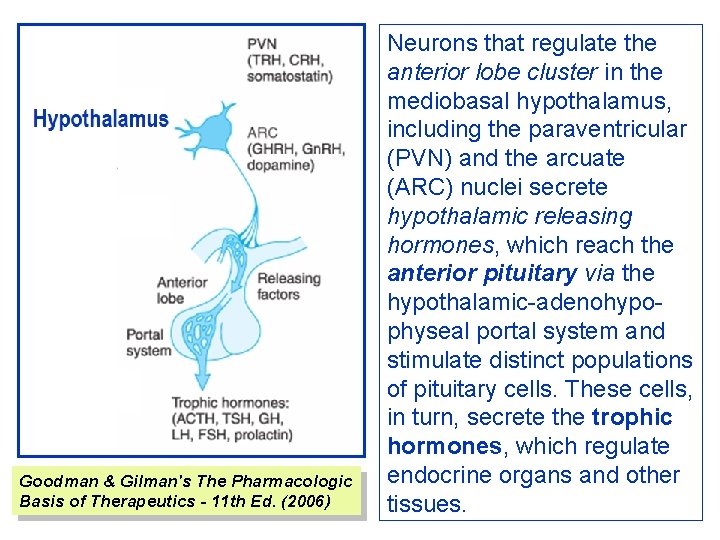
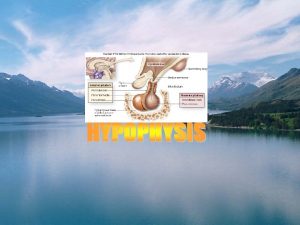
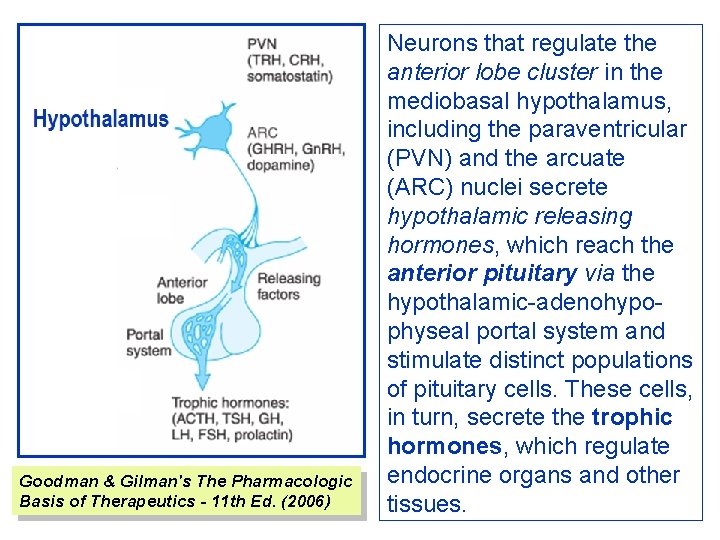
Goodman & Gilman's The Pharmacologic Basis of Therapeutics - 11 th Ed. (2006) Neurons that regulate the anterior lobe cluster in the mediobasal hypothalamus, including the paraventricular (PVN) and the arcuate (ARC) nuclei secrete hypothalamic releasing hormones, which reach the anterior pituitary via the hypothalamic-adenohypophyseal portal system and stimulate distinct populations of pituitary cells. These cells, in turn, secrete the trophic hormones, which regulate endocrine organs and other tissues.
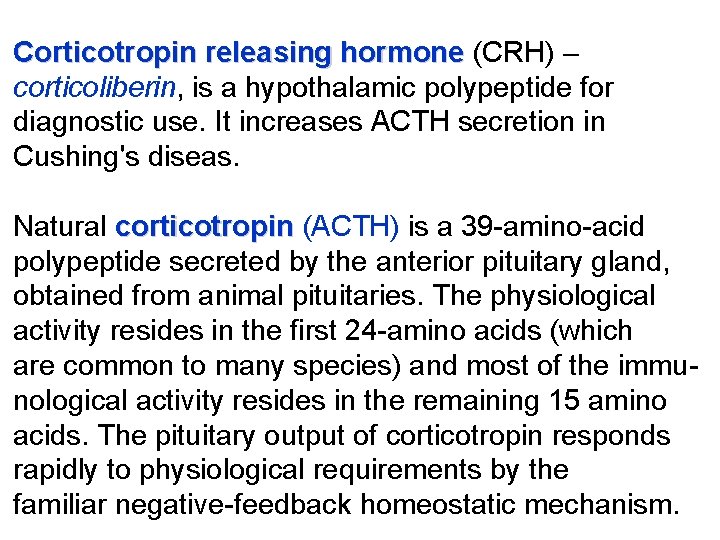
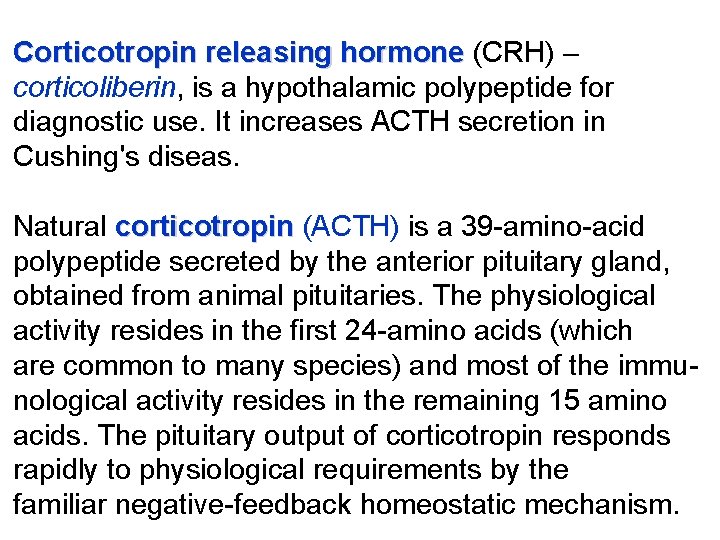
Corticotropin releasing hormone (CRH) – corticoliberin, is a hypothalamic polypeptide for diagnostic use. It increases ACTH secretion in Cushing's diseas. Natural corticotropin (ACTH) is a 39 -amino-acid polypeptide secreted by the anterior pituitary gland, obtained from animal pituitaries. The physiological activity resides in the first 24 -amino acids (which are common to many species) and most of the immunological activity resides in the remaining 15 amino acids. The pituitary output of corticotropin responds rapidly to physiological requirements by the familiar negative-feedback homeostatic mechanism.
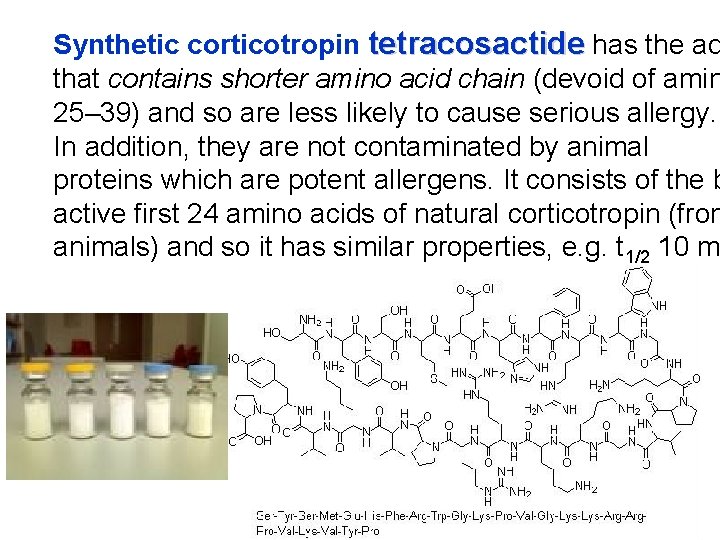
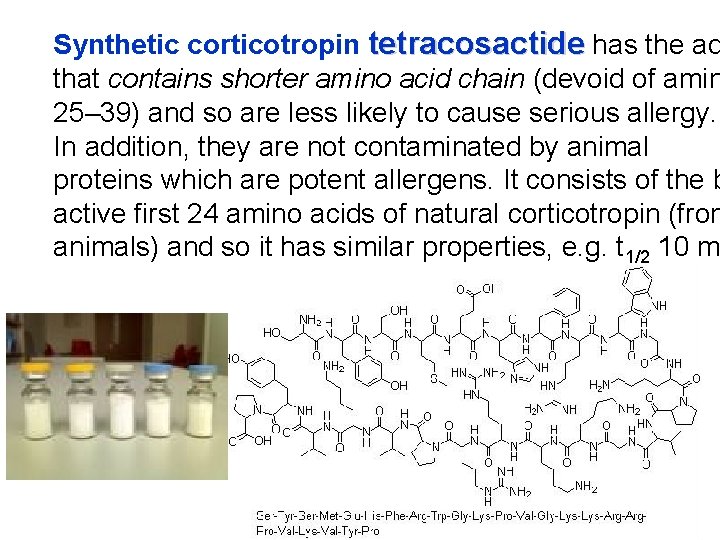
Synthetic corticotropin tetracosactide has the ad that contains shorter amino acid chain (devoid of amin 25– 39) and so are less likely to cause serious allergy. In addition, they are not contaminated by animal proteins which are potent allergens. It consists of the b active first 24 amino acids of natural corticotropin (from animals) and so it has similar properties, e. g. t 1/2 10 m
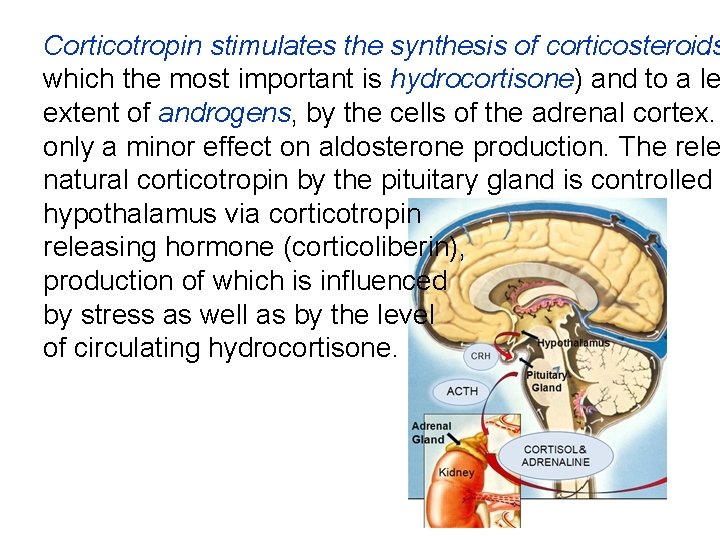
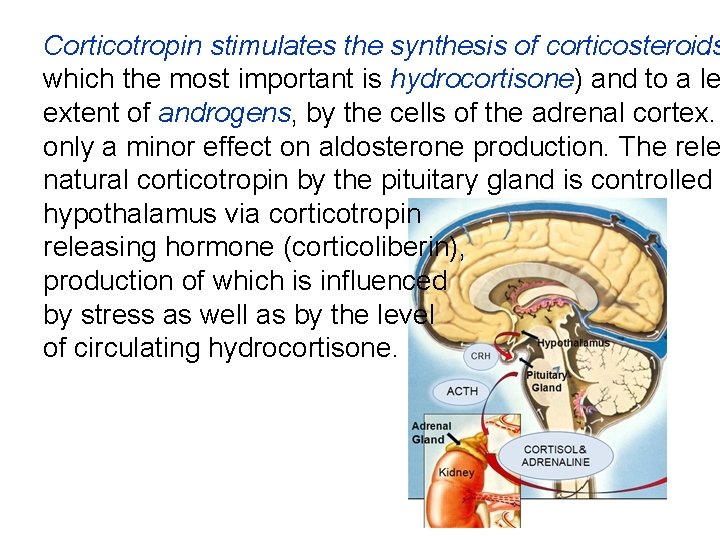
Corticotropin stimulates the synthesis of corticosteroids which the most important is hydrocortisone) and to a le extent of androgens, by the cells of the adrenal cortex. only a minor effect on aldosterone production. The rele natural corticotropin by the pituitary gland is controlled b hypothalamus via corticotropin releasing hormone (corticoliberin), production of which is influenced by stress as well as by the level of circulating hydrocortisone.
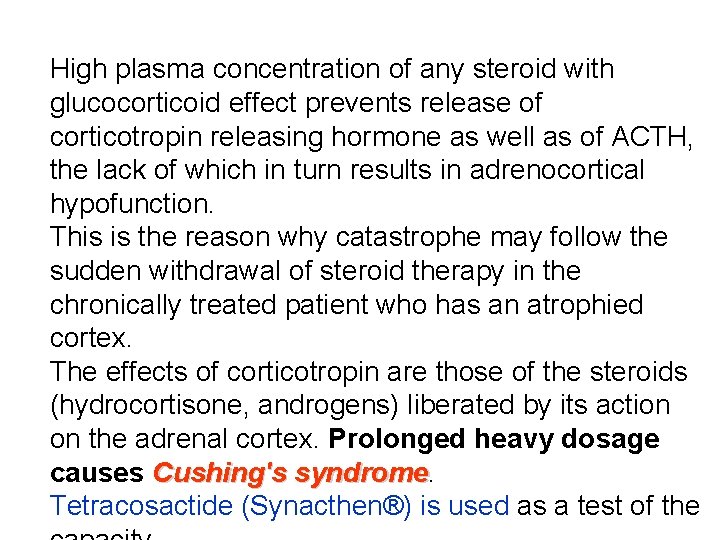
High plasma concentration of any steroid with glucocorticoid effect prevents release of corticotropin releasing hormone as well as of ACTH, the lack of which in turn results in adrenocortical hypofunction. This is the reason why catastrophe may follow the sudden withdrawal of steroid therapy in the chronically treated patient who has an atrophied cortex. The effects of corticotropin are those of the steroids (hydrocortisone, androgens) liberated by its action on the adrenal cortex. Prolonged heavy dosage causes Cushing's syndrome Tetracosactide (Synacthen®) is used as a test of the
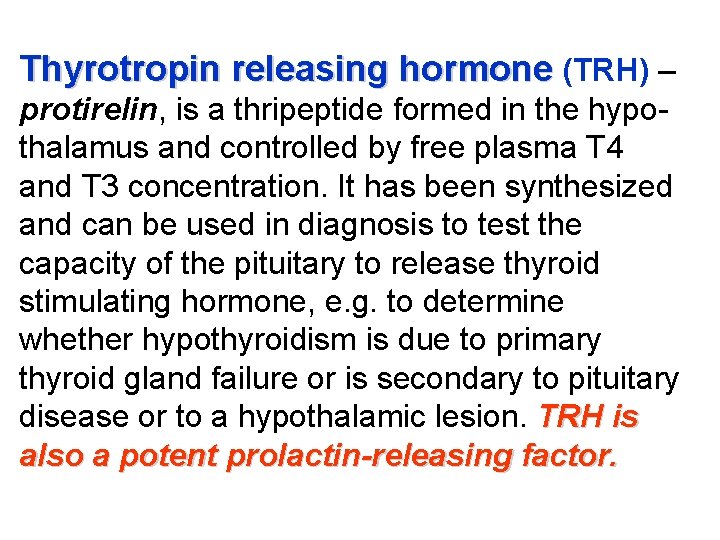
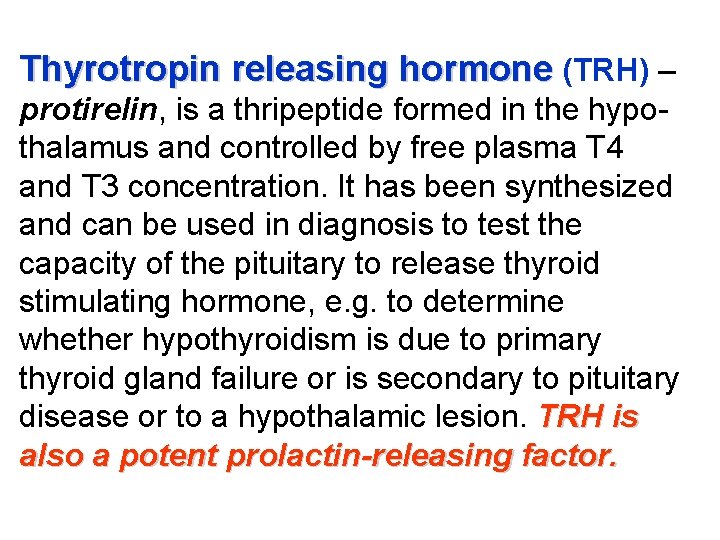
Thyrotropin releasing hormone (TRH) – protirelin, is a thripeptide formed in the hypothalamus and controlled by free plasma T 4 and T 3 concentration. It has been synthesized and can be used in diagnosis to test the capacity of the pituitary to release thyroid stimulating hormone, e. g. to determine whether hypothyroidism is due to primary thyroid gland failure or is secondary to pituitary disease or to a hypothalamic lesion. TRH is also a potent prolactin-releasing factor.
Thyroid stimulating hormone (TSH) thyrotr a glycoprotein of the anterior pituitary, controls the synthesis and release of thyroid hormone from the gland, and also the uptake iodide. There is a negative feedback of thyroid hormones on both the hypothalamic secretion TRH and pituitary secretion of TSH. Sermorelin is an analogue of the hypothalam growth hormone releasing hormone (somator It is used in a diagnostic test for growth hormo secretion from the pituitary.
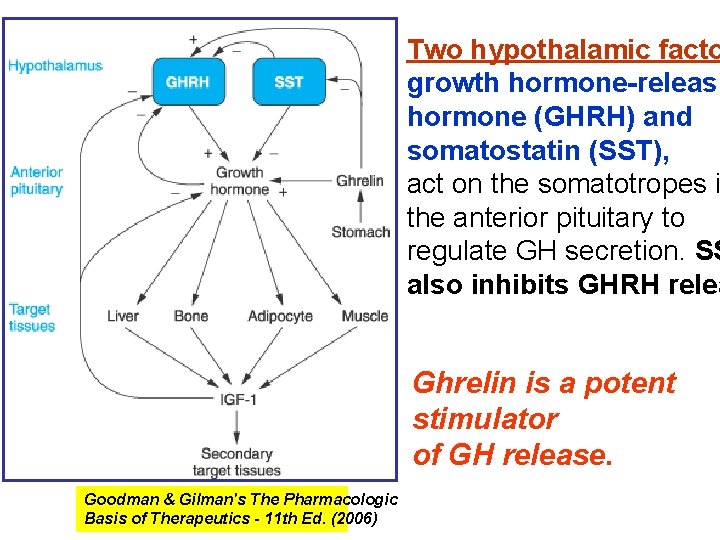
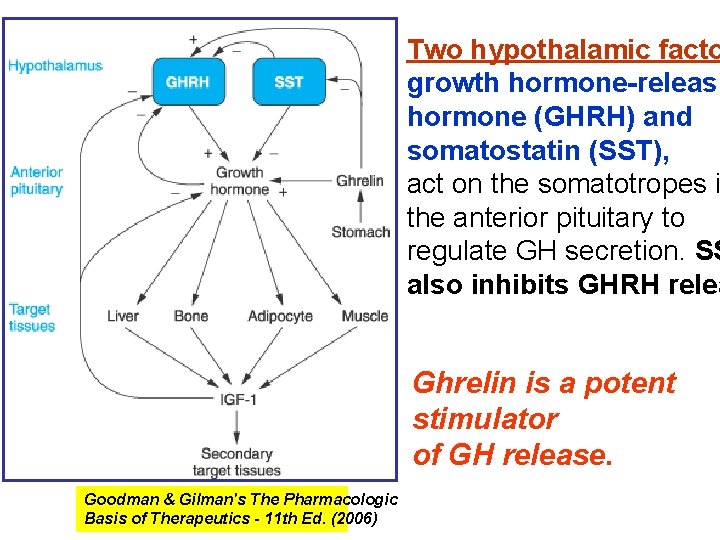
Two hypothalamic facto growth hormone-releasi hormone (GHRH) and somatostatin (SST), act on the somatotropes i the anterior pituitary to regulate GH secretion. SS also inhibits GHRH relea Ghrelin is a potent stimulator of GH release. Goodman & Gilman's The Pharmacologic Basis of Therapeutics - 11 th Ed. (2006)
Growth hormone (GH), one of the peptide hormones produced by the anterior pituitary, is required during childhood and adolescence for attainment of normal adult size and has important effects throughout postnatal life on lipid and carbohydrate metabolism, and on body mass. Its effects are primarily mediated via insulin-like growth factor 1 (IGF-1) and IGF-2 Individuals with congenital or acquired deficiency in GH during childhood or adolescence fail to reach their predicted adult height and have disproportionately increased body fat and decreased muscle mass. Adults with GH deficiency also have disproportionately small body mass.
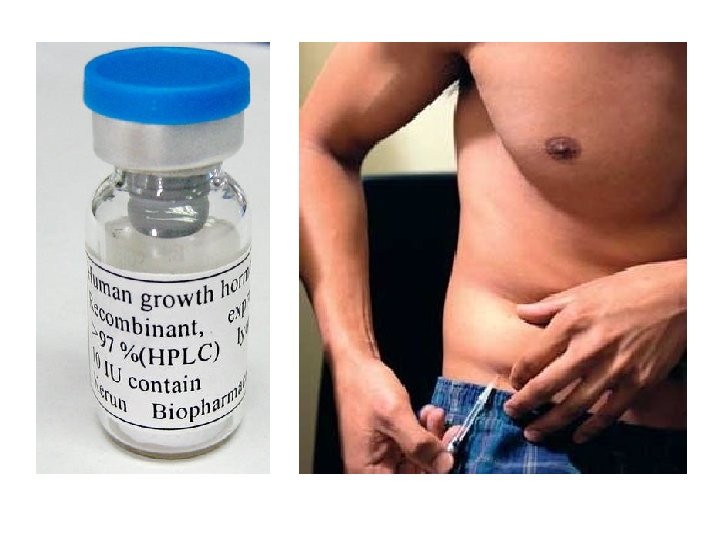
GH is a 191 -amino-acid peptide. Two types of recombinant human growth hormone (rh. GH) are approved for clinical use: Somatropin (identical with the native form of human GH) and Somatrem (with an extra methionine residue at the amino terminal end). The drugs are used in children with growth horm deficiency, while the bone epiphyses are still open, to prevent dwarfism (underdevelopment of the body) and provide normal growth. Treatment improves exercise performance and increases lean body mass. It may improve overall quality of life.
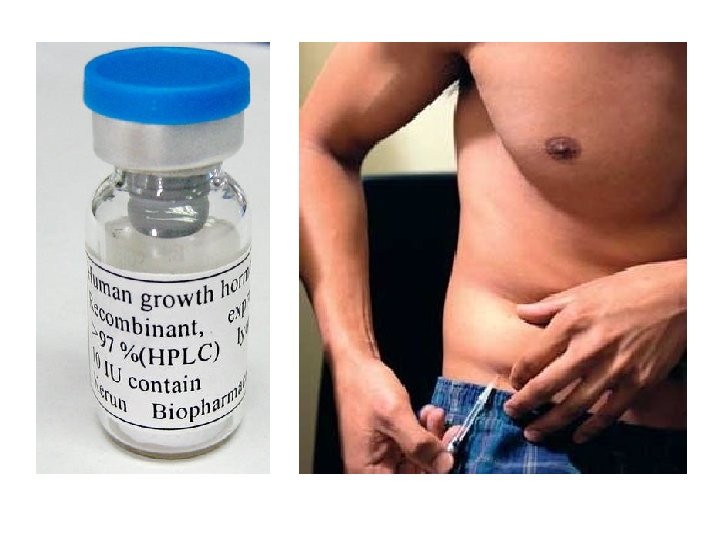
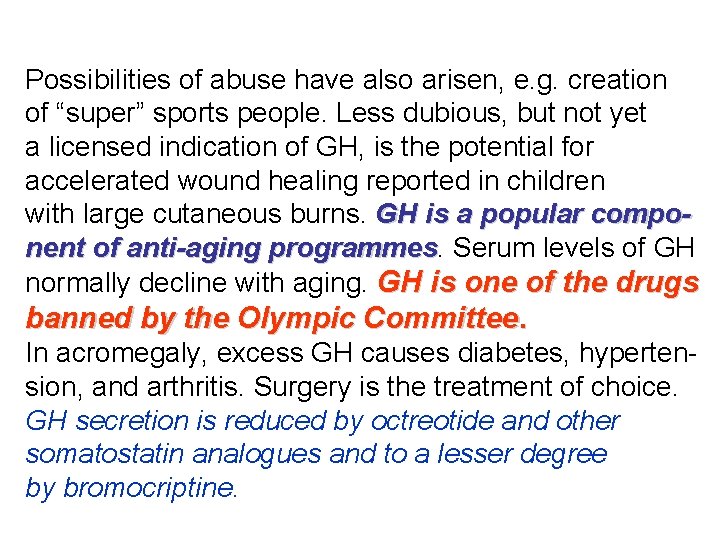
Possibilities of abuse have also arisen, e. g. creation of “super” sports people. Less dubious, but not yet a licensed indication of GH, is the potential for accelerated wound healing reported in children with large cutaneous burns. GH is a popular component of anti-aging programmes Serum levels of GH normally decline with aging. GH is one of the drugs banned by the Olympic Committee. In acromegaly, excess GH causes diabetes, hypertension, and arthritis. Surgery is the treatment of choice. GH secretion is reduced by octreotide and other somatostatin analogues and to a lesser degree by bromocriptine.
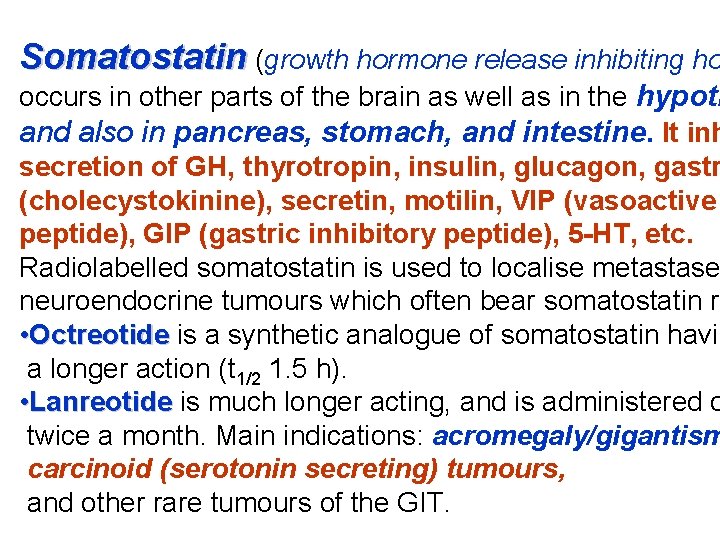
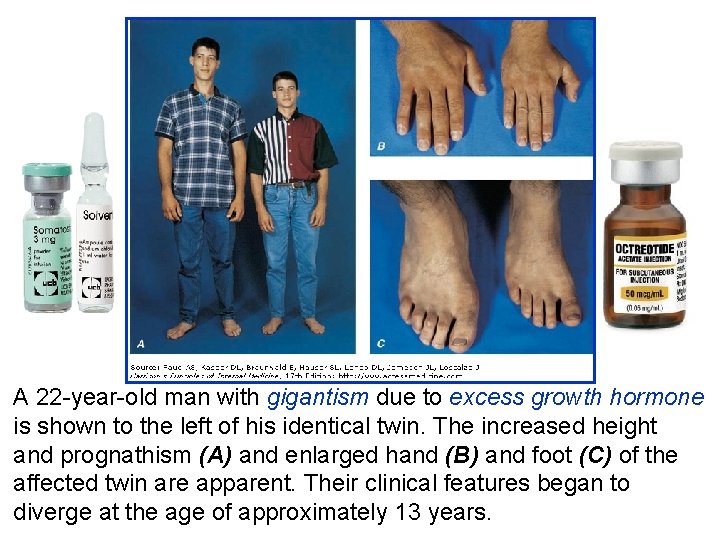
Somatostatin (growth hormone release inhibiting ho occurs in other parts of the brain as well as in the hypoth and also in pancreas, stomach, and intestine. It inh secretion of GH, thyrotropin, insulin, glucagon, gastr (cholecystokinine), secretin, motilin, VIP (vasoactive peptide), GIP (gastric inhibitory peptide), 5 -HT, etc. Radiolabelled somatostatin is used to localise metastase neuroendocrine tumours which often bear somatostatin re • Octreotide is a synthetic analogue of somatostatin havin a longer action (t 1/2 1. 5 h). • Lanreotide is much longer acting, and is administered o twice a month. Main indications: acromegaly/gigantism carcinoid (serotonin secreting) tumours, and other rare tumours of the GIT.
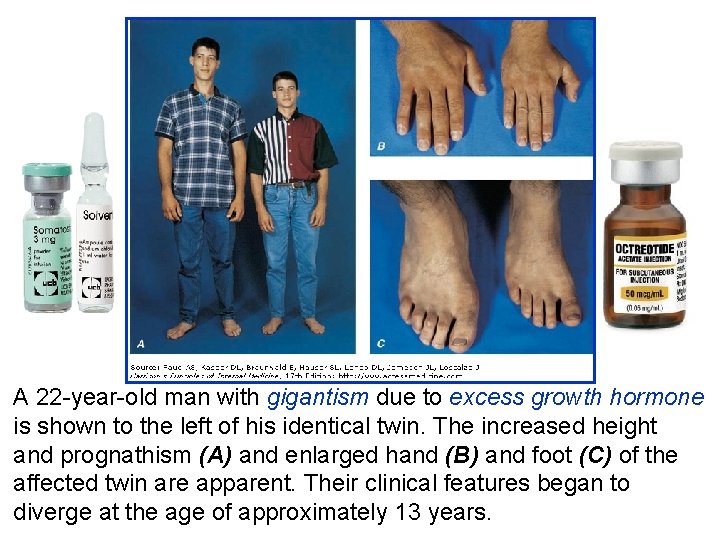
A 22 -year-old man with gigantism due to excess growth hormone is shown to the left of his identical twin. The increased height and prognathism (A) and enlarged hand (B) and foot (C) of the affected twin are apparent. Their clinical features began to diverge at the age of approximately 13 years.
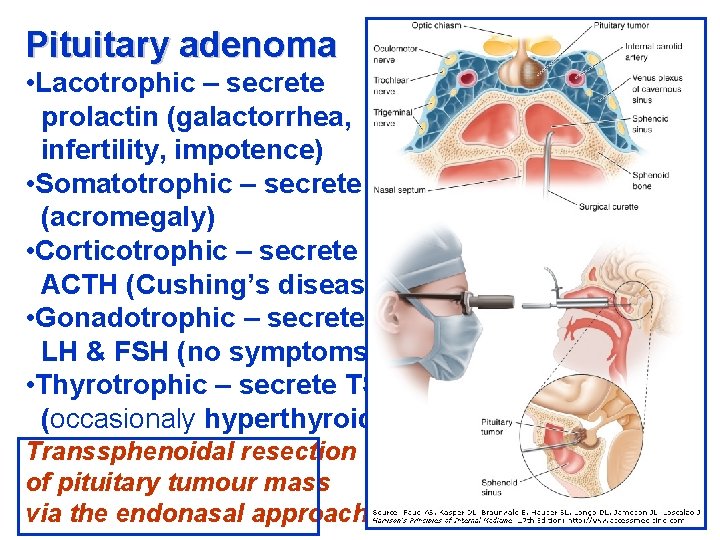
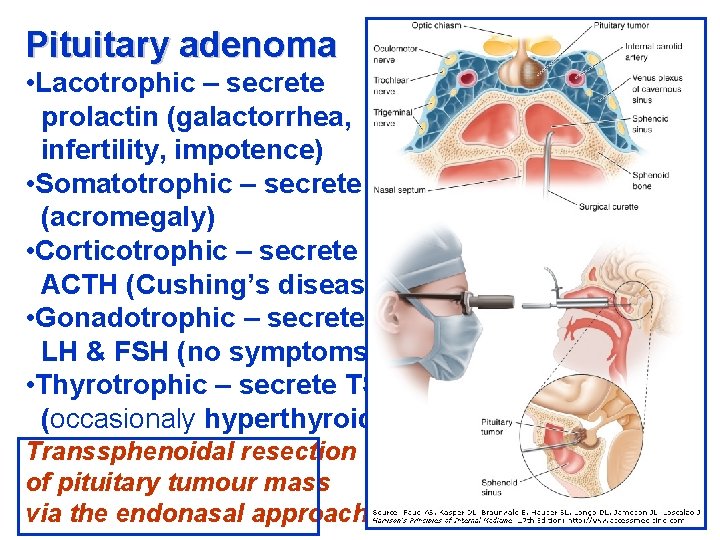
Pituitary adenoma • Lacotrophic – secrete prolactin (galactorrhea, infertility, impotence) • Somatotrophic – secrete GH (acromegaly) • Corticotrophic – secrete ACTH (Cushing’s disease) • Gonadotrophic – secrete LH & FSH (no symptoms) • Thyrotrophic – secrete TSH (occasionaly hyperthyroidism) Transsphenoidal resection of pituitary tumour mass via the endonasal approach
Gonadorelin (gonadotropin releasing hormone – Gn. RH) releases luteinising hormone (LH) and follicle-stimulating hormone (FSH). It has use in the assessment of pituitary function. Intermittent pulsatile administration evokes secretion of gonadotropins (LH and FSH) and is used to treat infertility. But continuous use evokes tachyphylaxis due to down-regulation of its receptors, i. e. gonadotropin release and therefore gonadal secretions are reduced. Longer-acting analogues – agonists of Gn. RH (buserelin, goserelin, nafarelin, deslorelin, and leupro are used to suppress androgen secretion in prostatic carcinoma.
Other uses may include endometriosis, precocious puberty, and contraception. All these drugs need to be administered by a parenteral route, by i. m. injection or intranasally. Follicle stimulating hormone (FSH) stimulates the development of ova and of spermatozoa. It is prepared from the urine of postmenopausal women. Urofollitropin (Metrodin®) contains FSH. Menotropins (Pergonal®) contains FSH and LH. These drugs are used in female and male hypopituitary infertility. Chorionic gonadotropin (human chorionic gonadotropin – h. CG) is secreted by the placenta and is obtained from the urine of pregnant women.
The predominant action of h. CG is that of LH. It induces progesterone production by the corpus luteum and, in the male – gonadal testosterone production. It is used in hypopituitary anovular and other infertility in both sexes. It is also used for cryptorchidism in prepubertal boys (6 years of age; if it fails to induce testicular descent, there is time for surgery before puberty to provide maximal possibility of a full functional testis). It may also precipitate puberty in men where this is delayed.
Prolactin is secreted by the lactotroph cells of the anterior pituitary gland. Its control is by tonic hypothalamic inhibition through prolactin inhibitory factor (PIF), probably dopamine, opposed by a prolactin releasing factor (PRF) in both women and, despite its name, it influences numerous biological functions. Prolactin secretion is controlled by an inhibitory dopaminergic path. Hyperprolactinaemia may be caused by drugs (with antidopaminergic actions e. g. metoclopramide), hypothyroidism, or prolactin secreting adenomas. Medical treatment is with bromocriptine, cabergoline or quinagolide at bedtime.
In hypopituitarism there is a partial or complete deficiency of hormones secreted by the anterior lobe of the pituitary. The posterior lobe hormones may also be deficient in a few cases, e. g. when a tumour has destroyed the pituitary. Patients suffering from hypopituitarism may present in coma, in which case treatment is for a severe acute adrenal insufficiency. Maintenance therapy is required, using hydrocortisone, thyroxine, oestradiol, and progesterone (in women) and testosterone (in men), or GH analogues (somatropin or somatrem).
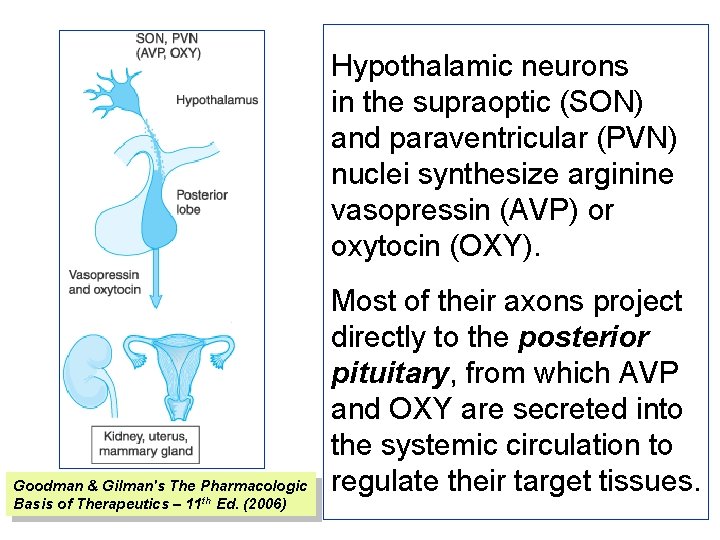
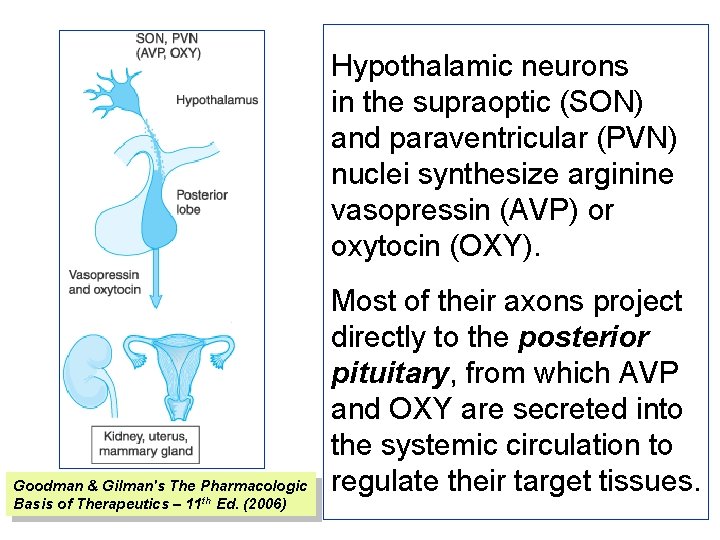
Hypothalamic neurons in the supraoptic (SON) and paraventricular (PVN) nuclei synthesize arginine vasopressin (AVP) or oxytocin (OXY). Goodman & Gilman's The Pharmacologic Basis of Therapeutics – 11 th Ed. (2006) Most of their axons project directly to the posterior pituitary, from which AVP and OXY are secreted into the systemic circulation to regulate their target tissues.
Vasopressin is a nonapeptide (t 1/2 20 min) with two separate G-protein coupled target receptors responsible for its two roles. The V 1 receptor on vascular smooth muscle is coupled to calcium entry. This receptor is not usually stimulated by physiological concentrations of the hormone. The V 2 receptor is coupled to adenylyl cyclase, and regulates opening of the water channel, aquaporin, in cells of the renal collecting duct. Secretion of the antidiuretic hormone is stimulated by any increase in the osmotic pressure of the blood supplying the hypothalamus and by a variety of drugs, notably nicotine. Secretion is inhibited by a fall in blood osmotic pressure and by alcohol.
In large nonphysiological doses (pharmacotherapy) vasopressin causes contraction of all smooth muscle, raising the blood pressure and causing intestinal colic. The smooth-muscle stimulant effect provides an example of tachyphylaxis (frequently repeated doses give progressively less effect). It is not only inefficient when used to raise the blood pressure, but is also dangerous, since it causes constriction of the coronary arteries and sudden death has occurred following its use. For replacement therapy of pituitary diabetes insipidus the longer acting analogue desmopressin is used.
Desmopressin (des-amino-D-arginine vasopressin) (DDAVP) has two major advantages: the vasoconstrictor effect has been reduced to near insignificance and the duration of action with nasal instillation, spray or s. c. injection, is 8– 20 h (t 1/2 75 min) so that, using it once to twice daily, patients are not inconvenienced by frequent recurrence of polyuria during their waking hours and can also expect to spend the night continuously in bed. The adult dose for intranasal administration is 10– 20 micrograms daily. The dose for children is about half that for adults. The bioavailability of intranasal DDAVP is 10%. It is also the only peptide for which an oral formulation is available, with a bioavailability of only 1%.
The main complication of DDAVP is hyponatraemia which can be prevented by allowing the patient to develop some polyuria for a short period during each week. The requirement for DDAVP may decrease during intercurrent illness. Terlipressin is an analogue of vasopressin used in NA-resistant septic shock and esophageal varices. Oxytocin is a peptide hormone of the posterior pituitary gland. It stimulates the contractions of the pregnant uterus, which becomes much more sensitive to it at term. Patients with posterior pituitary disease (diabetes insipidus) can, however, go into labour norma
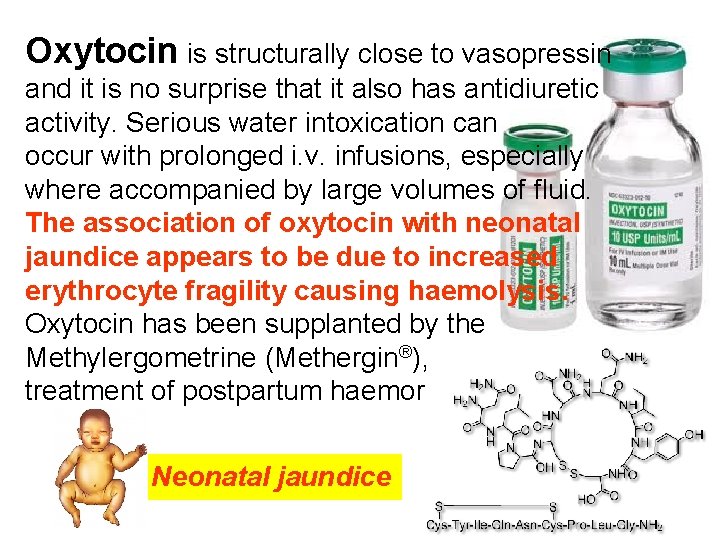
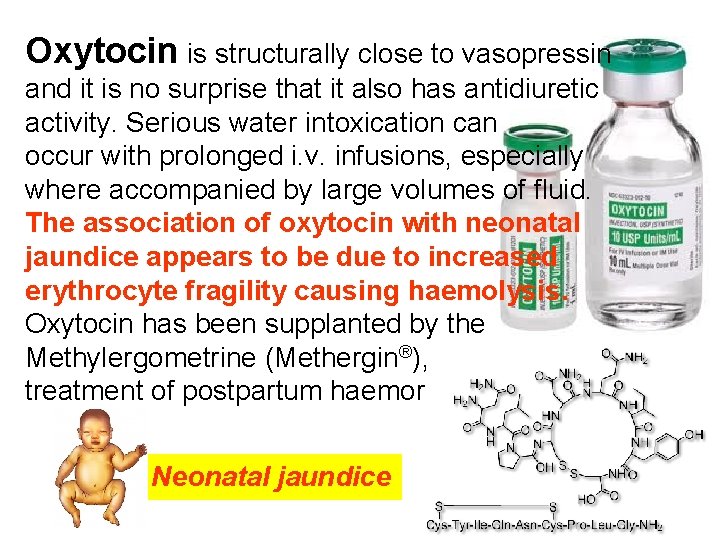
Oxytocin is structurally close to vasopressin and it is no surprise that it also has antidiuretic activity. Serious water intoxication can occur with prolonged i. v. infusions, especially where accompanied by large volumes of fluid. The association of oxytocin with neonatal jaundice appears to be due to increased erythrocyte fragility causing haemolysis. Oxytocin has been supplanted by the Methylergometrine (Methergin®), as the prime treatment of postpartum haemorrhage. Neonatal jaundice
Oxytocin is reflexly released from the pituitary following suckling (also by manual stimulation of the nipple) and causes almost immediate contraction of the myoepithelium of the breast; it can be used to enhance milk ejection (nasal spray). Oxytocin is used i. v. in the induction of labour. It produces, almost immediately, rhythmic contractions with relaxation between, i. e. it mimics normal uterine activity. The decision to use oxytocin requires s skill. It has a t 1/2 of 6 min and is given by i. v. infusion using a pump; it must be closely supervised; the dose is adjusted by the results; overdose can cause uter tetany and even rupture.
Atosiban is a modified form of oxytocin that the action of this hormone on the uterus, leadi a cessation of contractions. It is used i. v. as a tocolytic to halt premature labor. Barusiban is three to four times more poten antagonist than atosiban with higher affinity an selectivity for the oxytocin receptor.
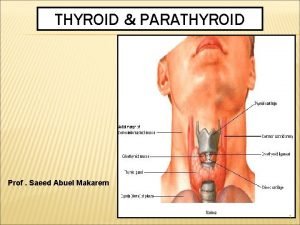
Parathyroid hormone (PTH) PTH acts chiefly on the kidney increasing renal tubular reabsorption and bone resorptio calcium; it increases calcium absorption from the gut, indirectly, by stimulating the renal synthesis of 25 -hydroxycholecalciferol (calcifediol). It increases the rate of bone remodelling (mineral and collagen) and osteocyte activity with, at high doses, an overall balance in favour of resorption (osteoclast activity) with a rise in plasma calcium concentration (and fall in phosphate); but, at low doses, the balance favours bone formation (osteoblast activity).
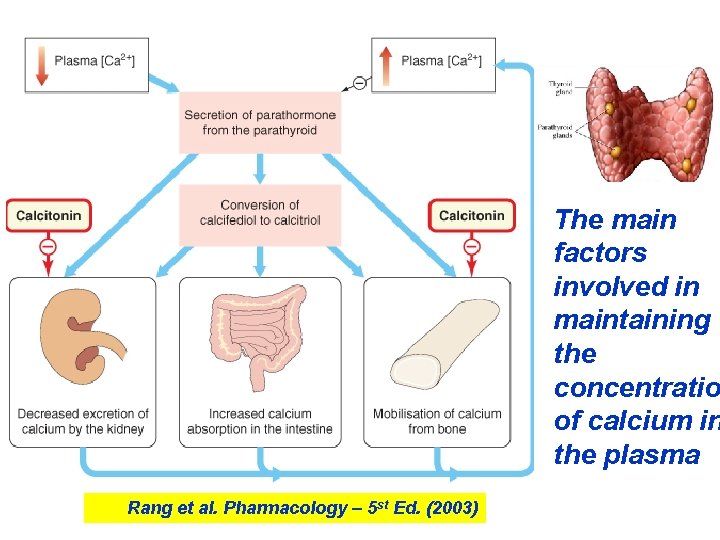
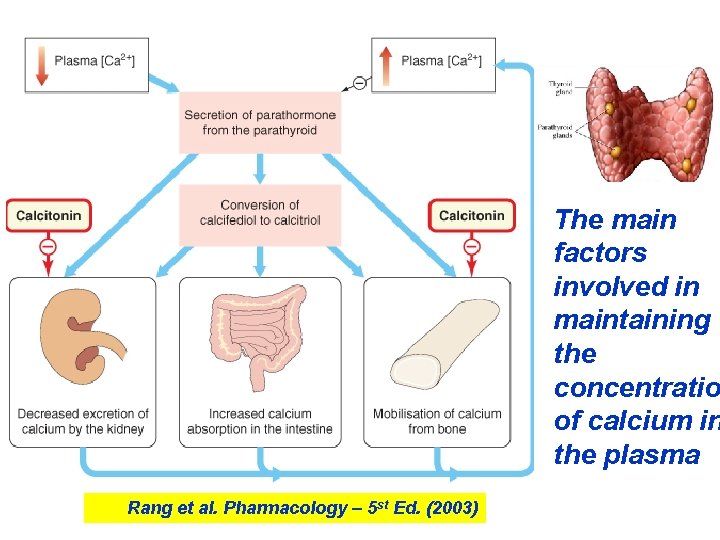
The main factors involved in maintaining the concentratio of calcium in the plasma Rang et al. Pharmacology – 5 st Ed. (2003)
 Hypothalamic pituitary portal system
Hypothalamic pituitary portal system What are the tropic hormones
What are the tropic hormones Adenohypophisis
Adenohypophisis Hypothalamic hormones
Hypothalamic hormones Pth hormone
Pth hormone Phycatri
Phycatri Parathyroid gland image
Parathyroid gland image Pth
Pth Pituitary hormones and their targets
Pituitary hormones and their targets Anterior pituitary hormones
Anterior pituitary hormones Hypophysis
Hypophysis Structure of hypothalamus and pituitary gland
Structure of hypothalamus and pituitary gland Pituitary gland hormones
Pituitary gland hormones Common lisp sort
Common lisp sort Angus gestation calculator
Angus gestation calculator Reproductive system conclusion
Reproductive system conclusion Mechanisms of hypothalamic control over endocrine function
Mechanisms of hypothalamic control over endocrine function Parathyroid gland pharyngeal pouch
Parathyroid gland pharyngeal pouch Histological structure of parathyroid gland
Histological structure of parathyroid gland Neurohypophsis
Neurohypophsis Parathyroid gland location
Parathyroid gland location A thyroidea ima
A thyroidea ima Thyroid class 11
Thyroid class 11 Hypothalamus
Hypothalamus Isthmus size
Isthmus size Pituitary adenoma
Pituitary adenoma Pituitary gland disorders
Pituitary gland disorders Thyoid gland
Thyoid gland Hashitoxicosis
Hashitoxicosis Blood supply of pituitary gland
Blood supply of pituitary gland Division of pituitary gland
Division of pituitary gland Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Hypothalamus hormones
Hypothalamus hormones Dictalie
Dictalie Anterior pituitary
Anterior pituitary Evolution of pituitary gland
Evolution of pituitary gland Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Propothiouracil
Propothiouracil Difference between anterior and posterior pituitary
Difference between anterior and posterior pituitary Positive feedback mechanism
Positive feedback mechanism Nystagmus unidirectional
Nystagmus unidirectional Difference between anterior and posterior pituitary
Difference between anterior and posterior pituitary Diaphragm sella
Diaphragm sella Pituitary gland
Pituitary gland Reproductive organ system
Reproductive organ system