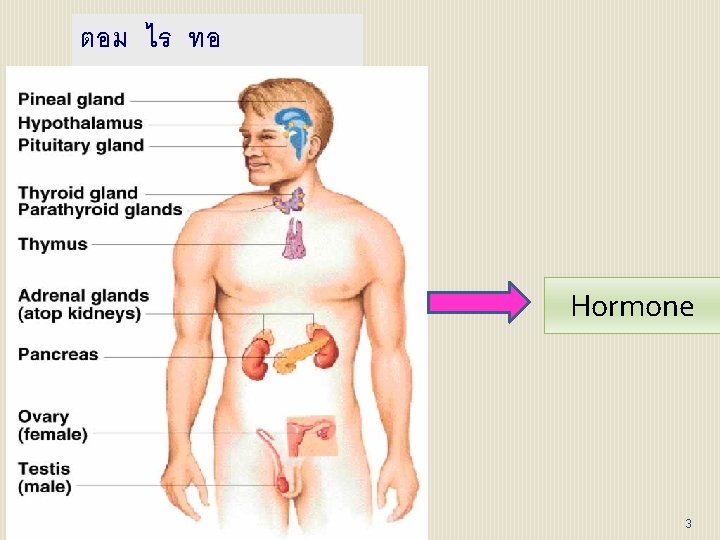
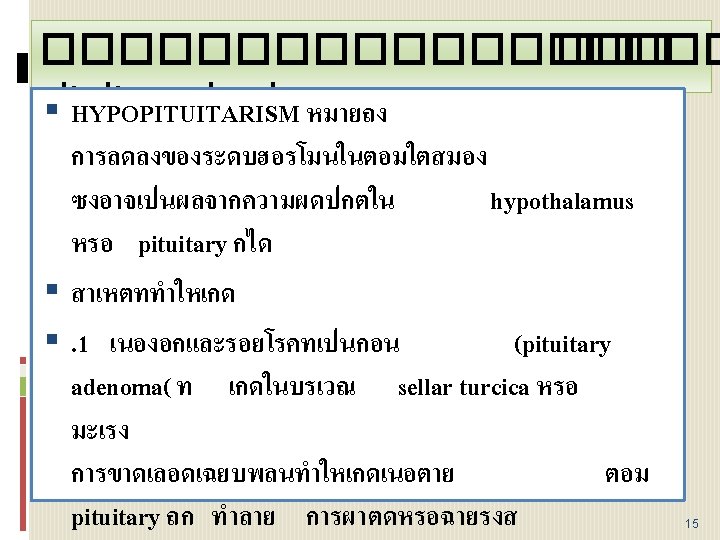
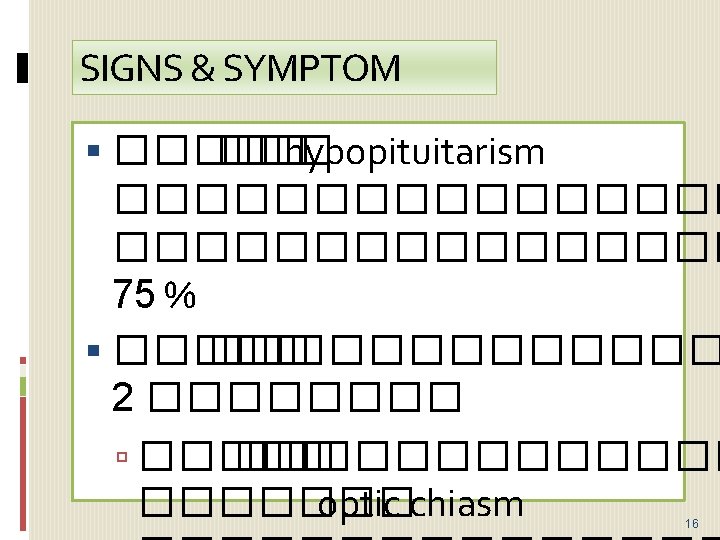
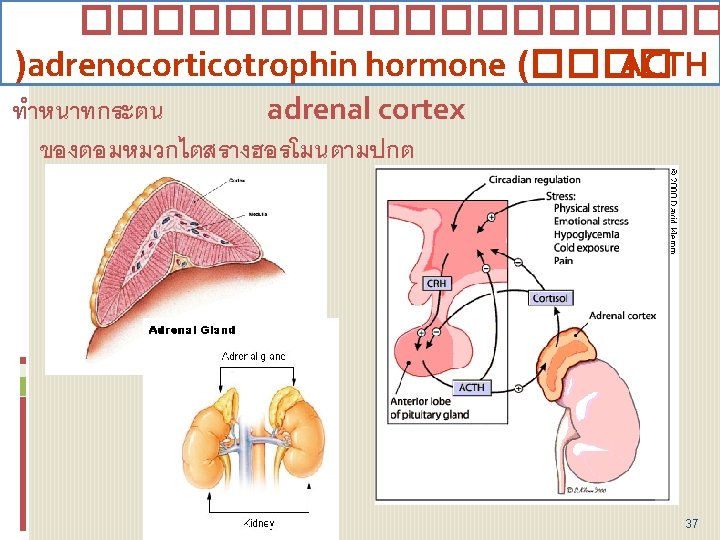
ENDOCRINE Hormone 3 Pituitary gland 11 Posterior pituitary

- Slides: 72
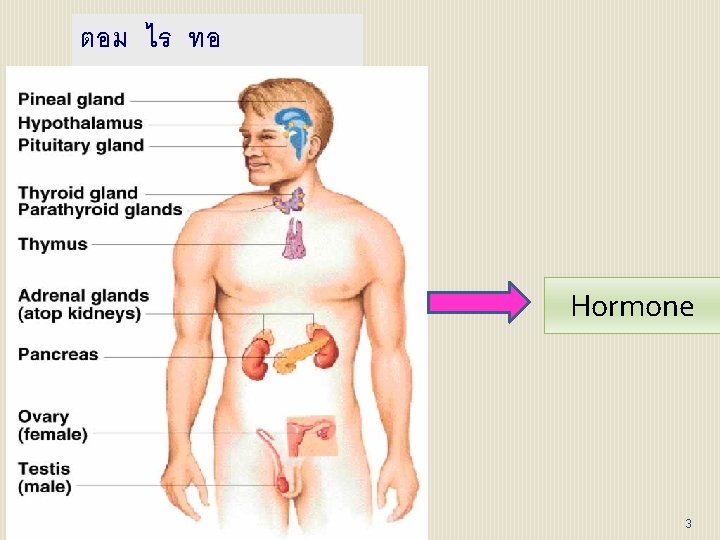
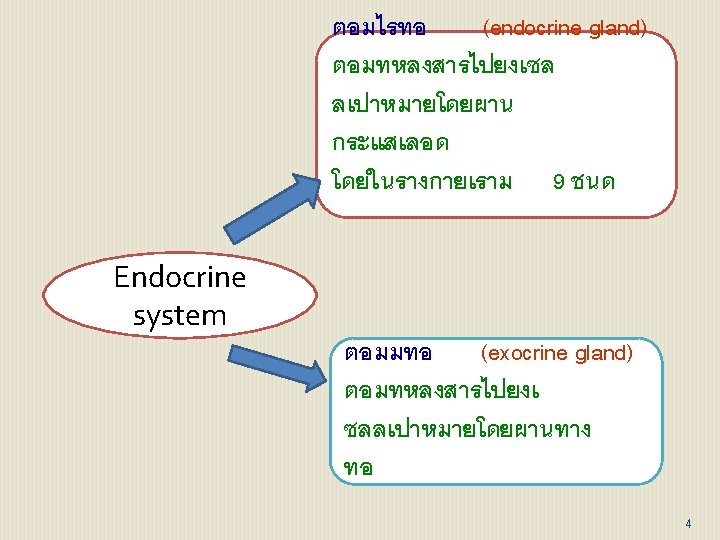
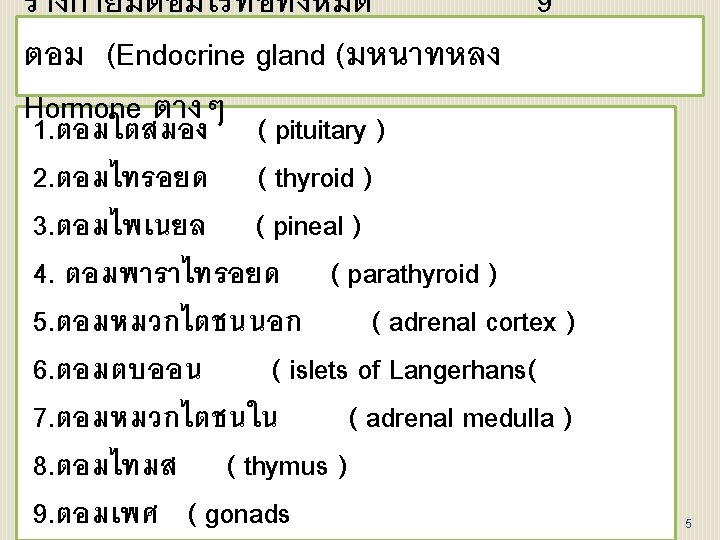
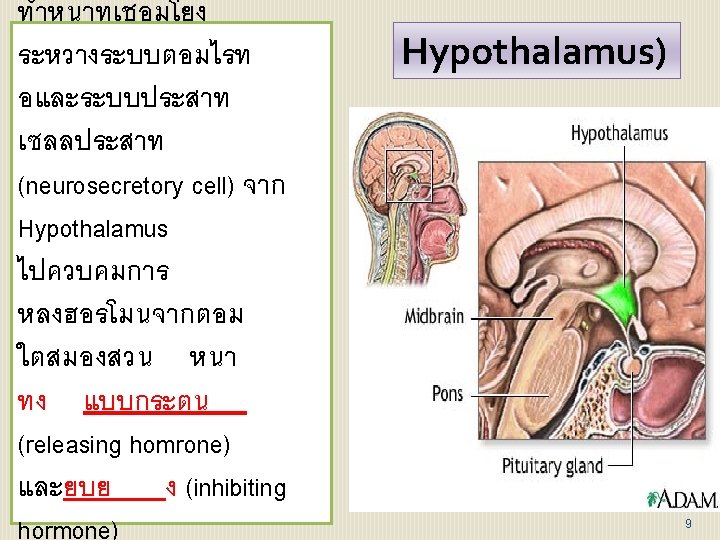
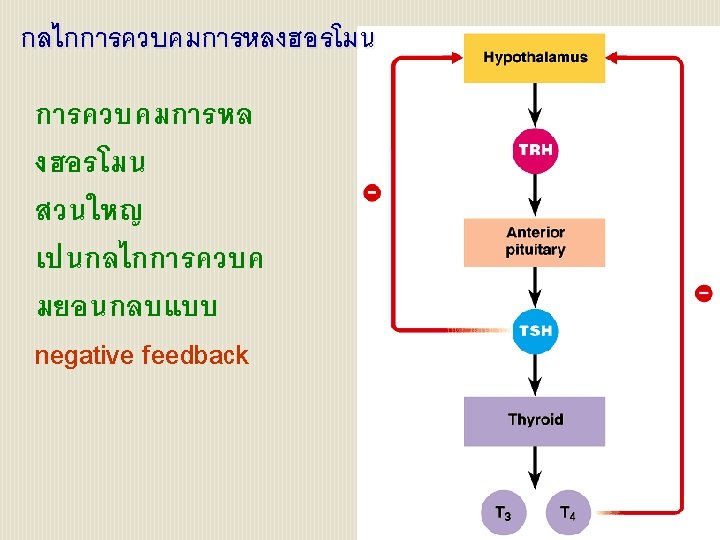
ตอม ไร ทอ (ENDOCRINE( Hormone 3
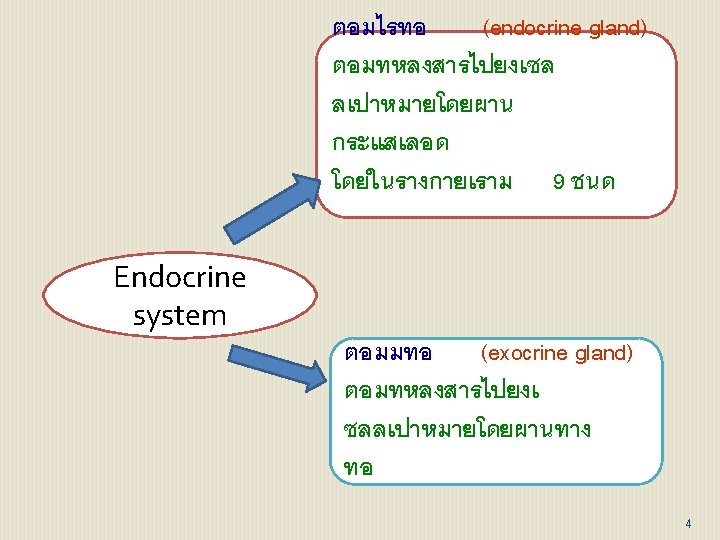
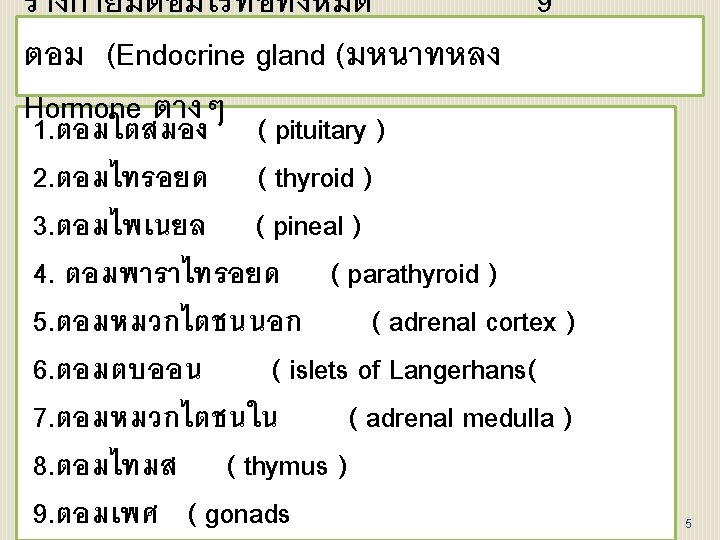
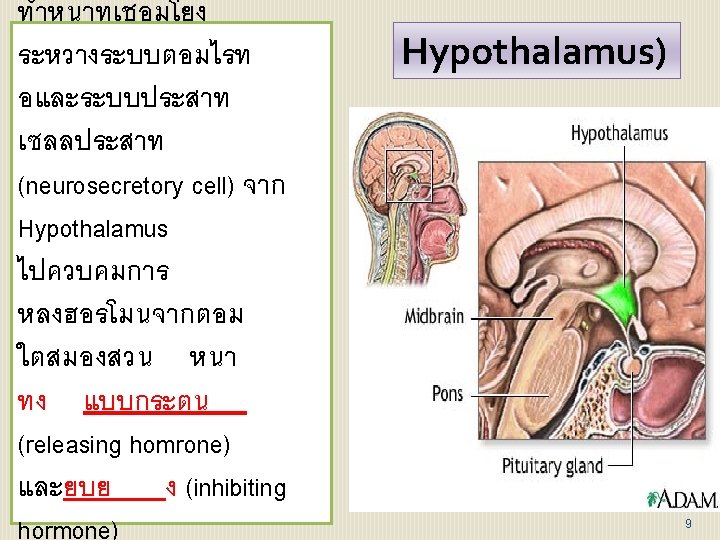
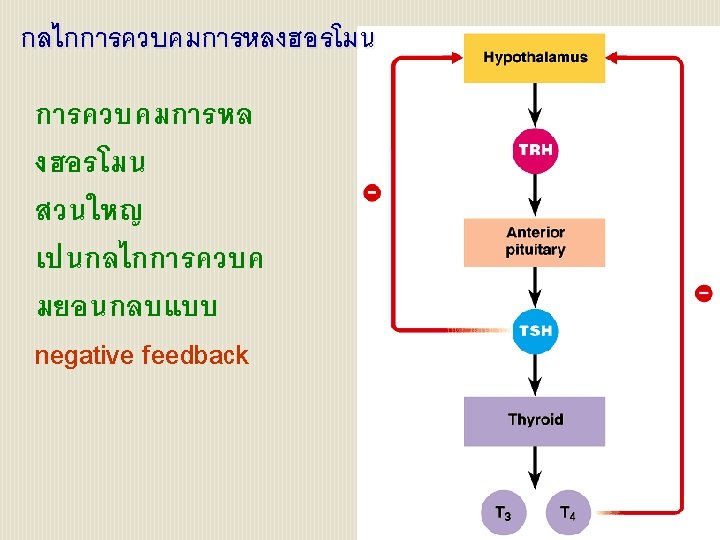
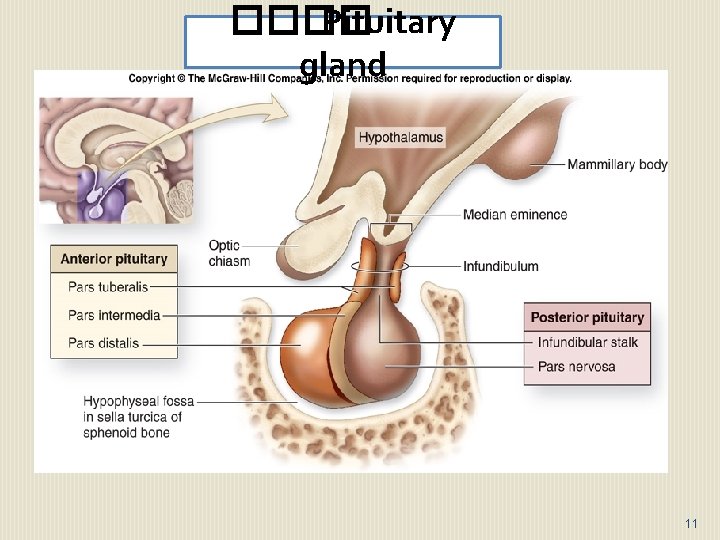
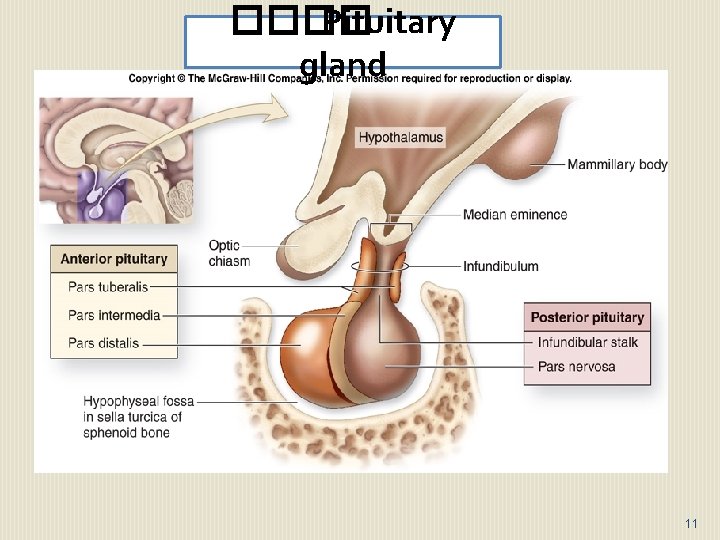
���� Pituitary gland 11
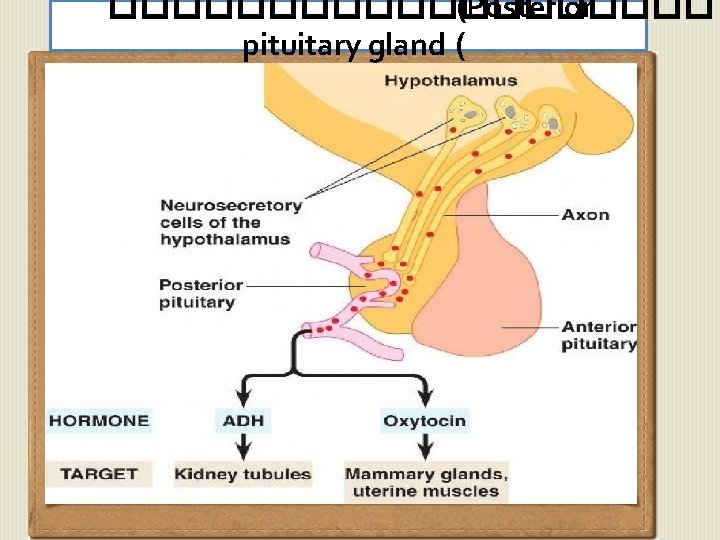
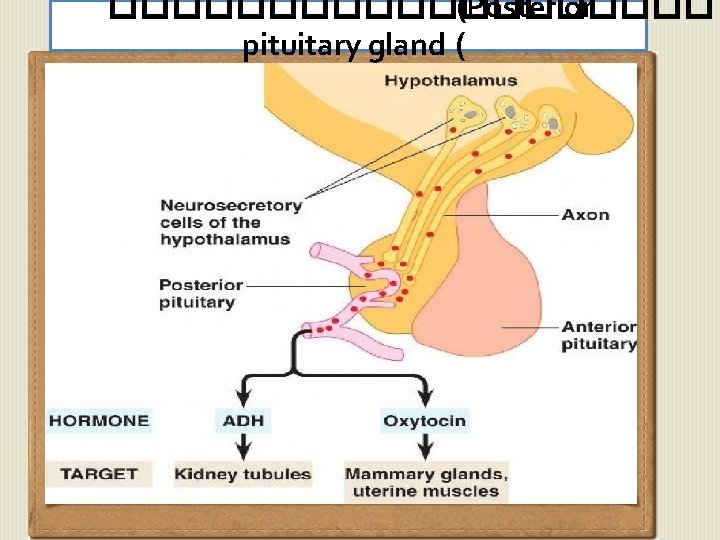
���������� (Posterior pituitary gland (
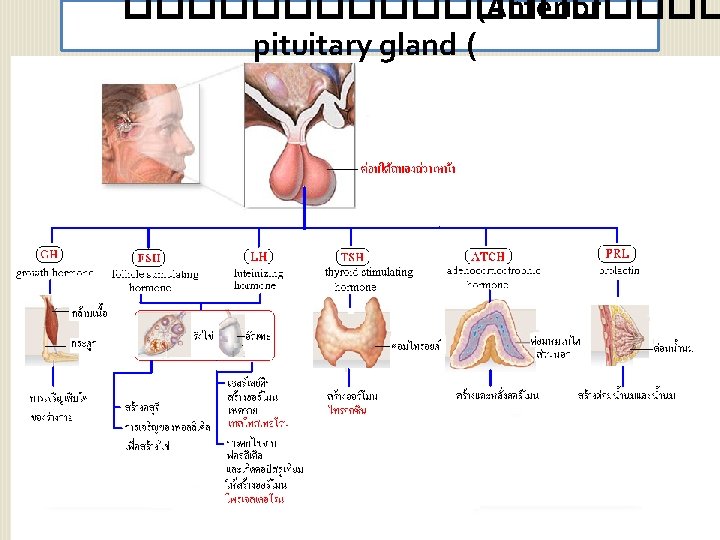
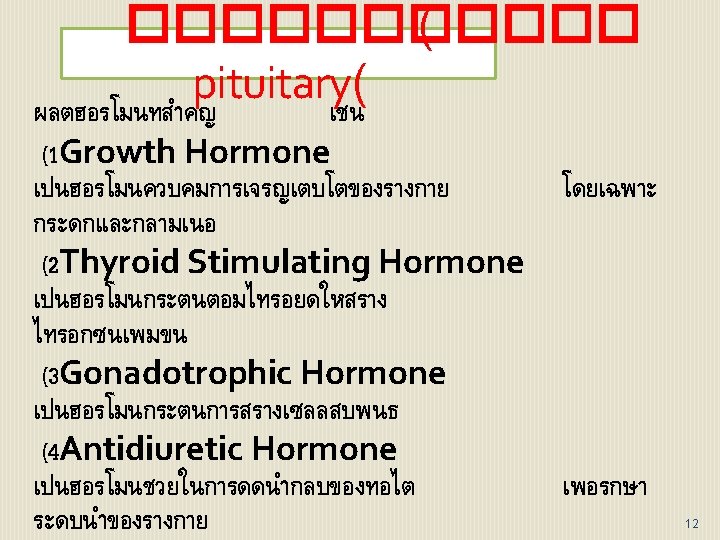
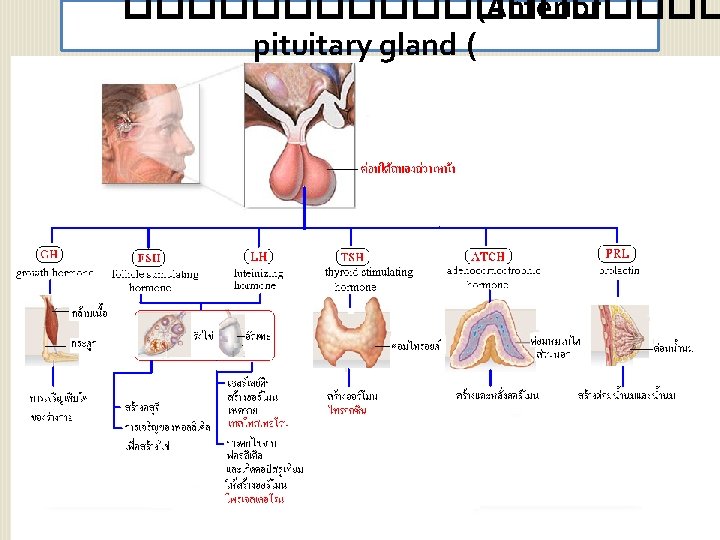
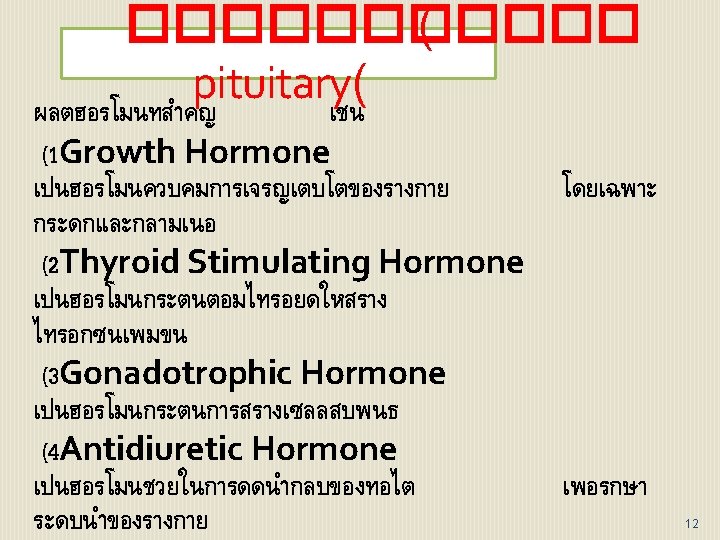
���������� (Anterior pituitary gland ( 14
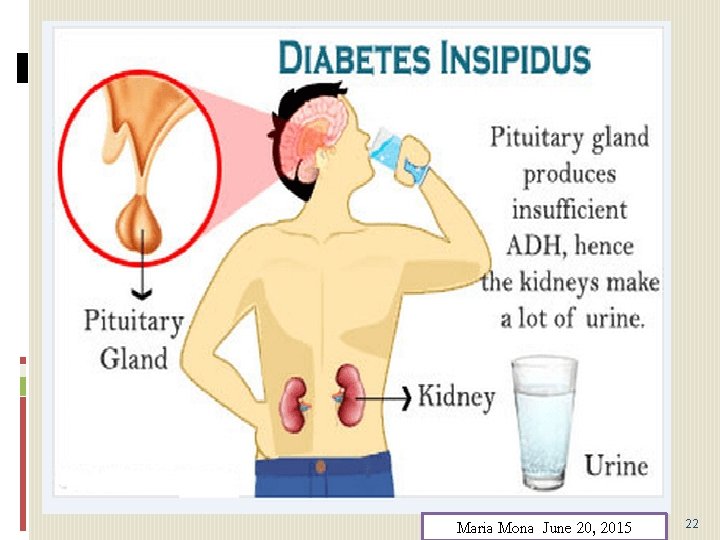
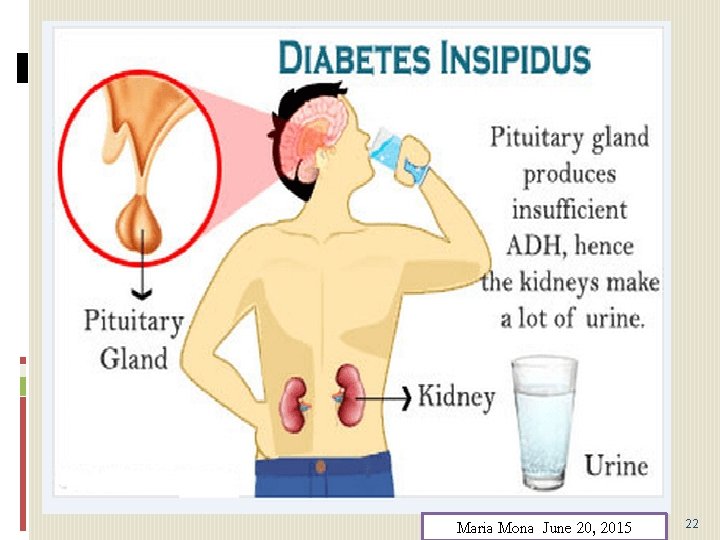
Maria Mona June 20, 2015 22
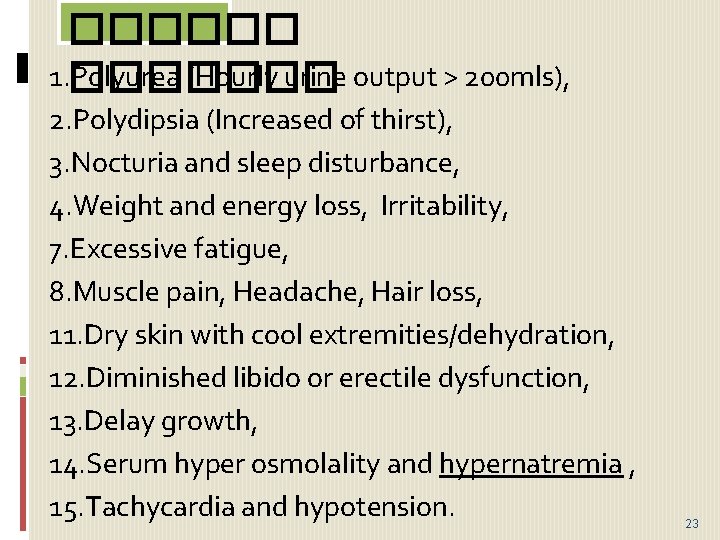
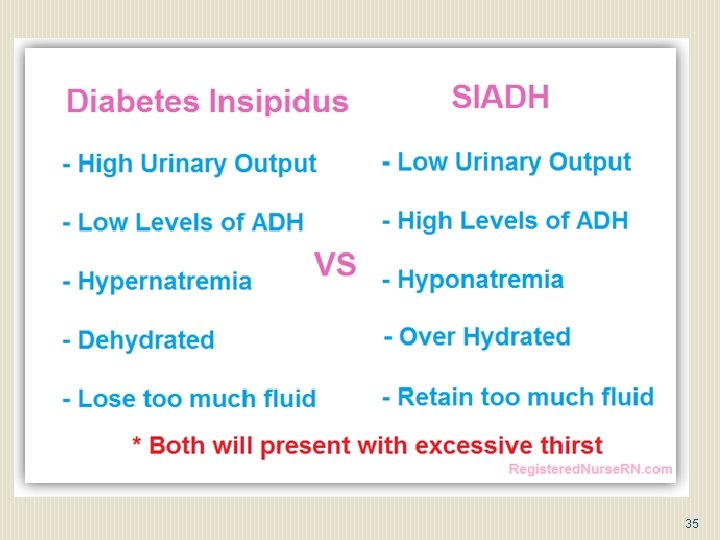
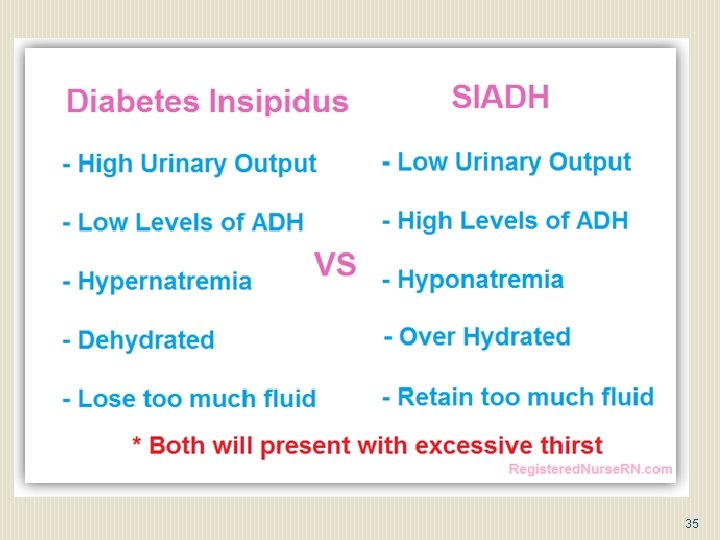
������ 1. Polyurea (Hourly urine output > 200 mls), ������� 2. Polydipsia (Increased of thirst), 3. Nocturia and sleep disturbance, 4. Weight and energy loss, Irritability, 7. Excessive fatigue, 8. Muscle pain, Headache, Hair loss, 11. Dry skin with cool extremities/dehydration, 12. Diminished libido or erectile dysfunction, 13. Delay growth, 14. Serum hyper osmolality and hypernatremia , 15. Tachycardia and hypotension. 23
Complication of Diabetes Insipidus Disease: following: 1. Dry mouth and lips, 2. Sunken features (particularly the eyes), 3. Headaches, 4. Dizziness, 5. Confusion and irritability. Maria Mona June 20, 2015 24
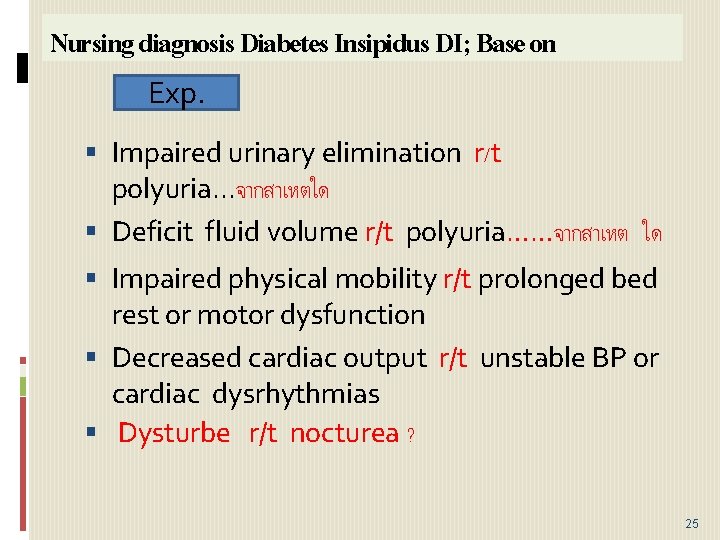
Nursing diagnosis Diabetes Insipidus DI; Base on Exp. Impaired urinary elimination r/t polyuria. . . จากสาเหตใด Deficit fluid volume r/t polyuria……จากสาเหต ใด Impaired physical mobility r/t prolonged bed rest or motor dysfunction Decreased cardiac output r/t unstable BP or cardiac dysrhythmias Dysturbe r/t nocturea ? 25
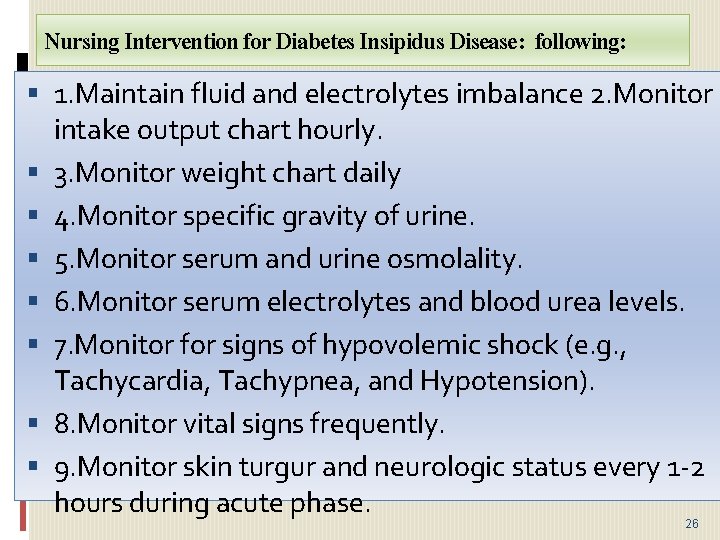
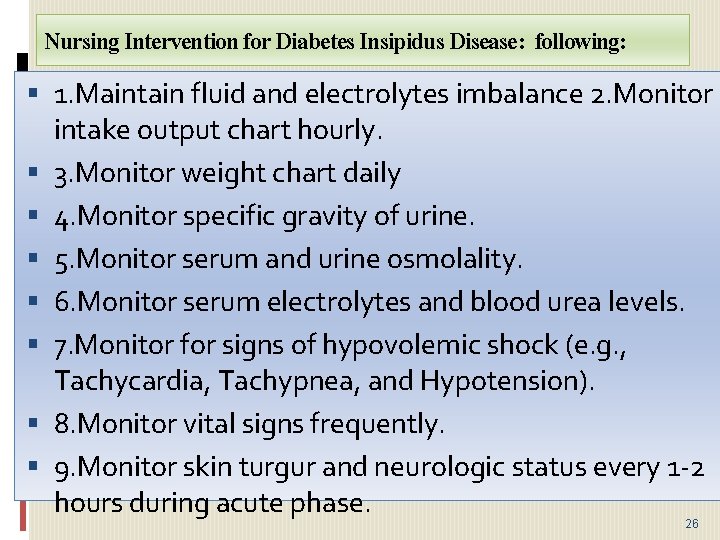
Nursing Intervention for Diabetes Insipidus Disease: following: 1. Maintain fluid and electrolytes imbalance 2. Monitor intake output chart hourly. 3. Monitor weight chart daily 4. Monitor specific gravity of urine. 5. Monitor serum and urine osmolality. 6. Monitor serum electrolytes and blood urea levels. 7. Monitor for signs of hypovolemic shock (e. g. , Tachycardia, Tachypnea, and Hypotension). 8. Monitor vital signs frequently. 9. Monitor skin turgur and neurologic status every 1 -2 hours during acute phase. 26
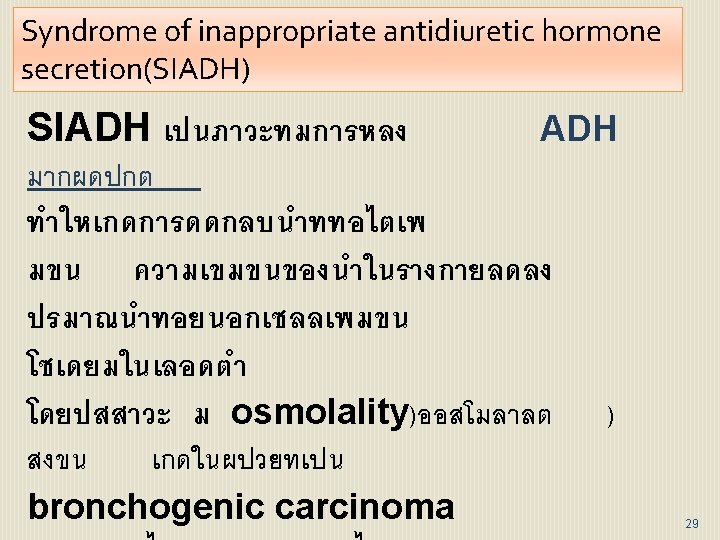
Syndrome of inappropriate antidiuretic hormone secretion (SIADH) 27
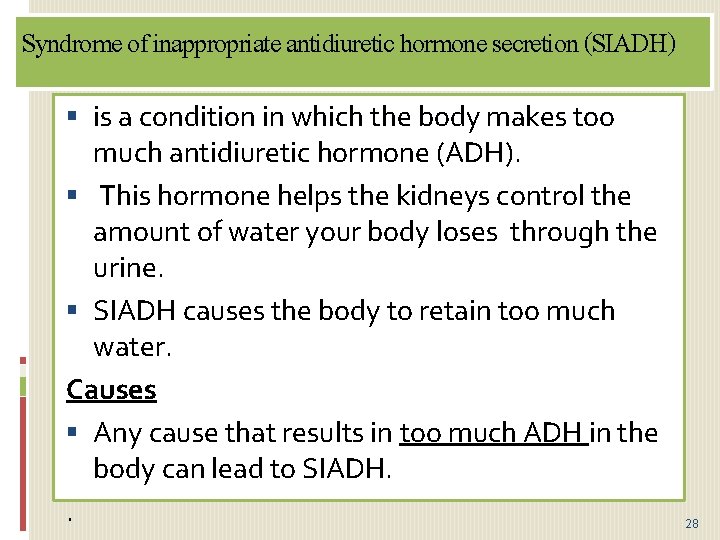
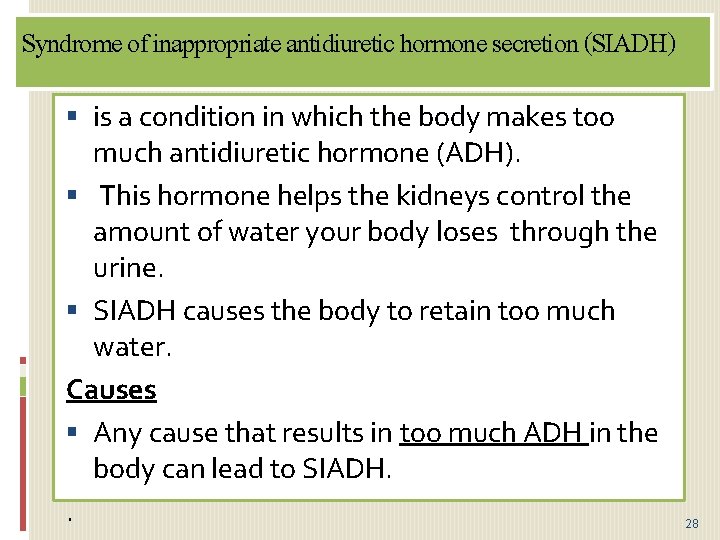
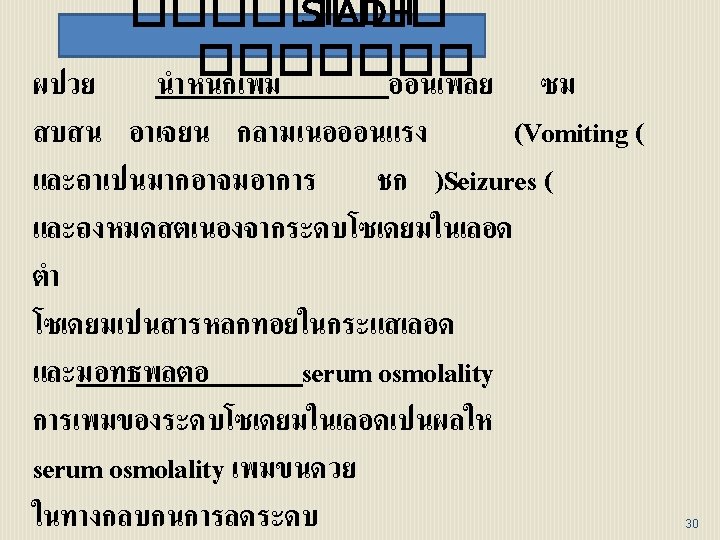
Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a condition in which the body makes too much antidiuretic hormone (ADH). This hormone helps the kidneys control the amount of water your body loses through the urine. SIADH causes the body to retain too much water. Causes Any cause that results in too much ADH in the body can lead to SIADH. . 28
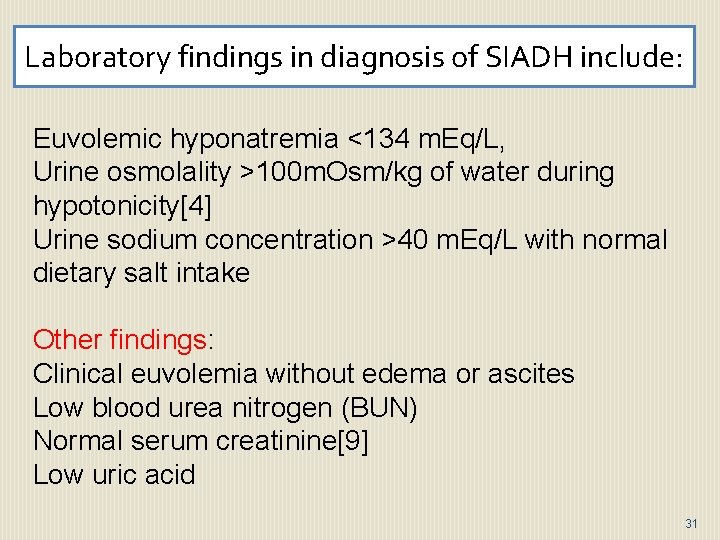
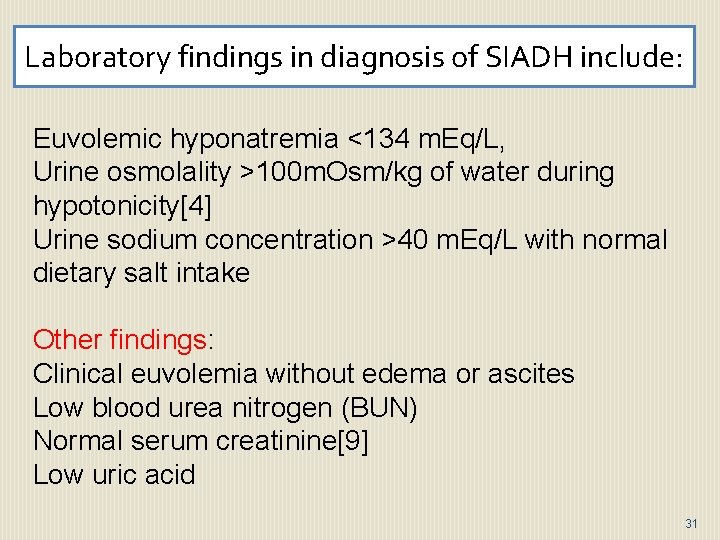
Laboratory findings in diagnosis of SIADH include: Euvolemic hyponatremia <134 m. Eq/L, Urine osmolality >100 m. Osm/kg of water during hypotonicity[4] Urine sodium concentration >40 m. Eq/L with normal dietary salt intake Other findings: Clinical euvolemia without edema or ascites Low blood urea nitrogen (BUN) Normal serum creatinine[9] Low uric acid 31
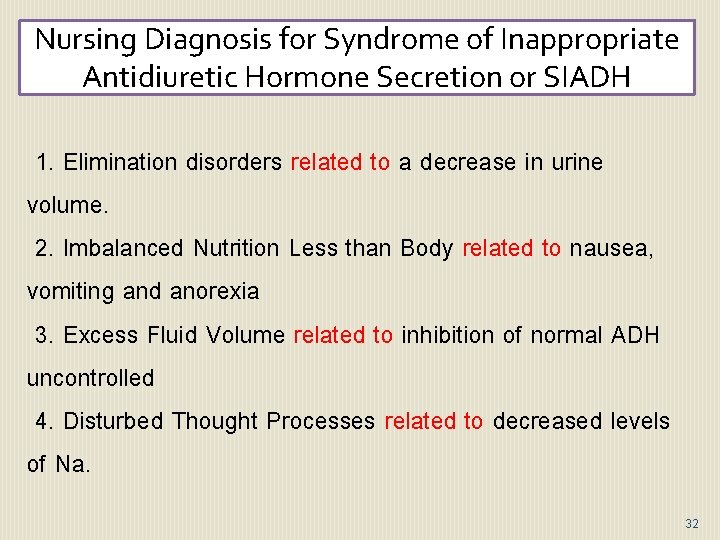
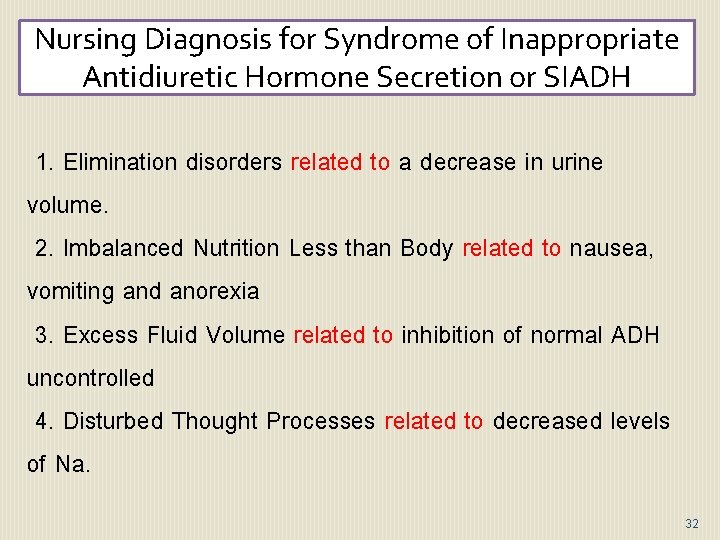
Nursing Diagnosis for Syndrome of Inappropriate Antidiuretic Hormone Secretion or SIADH 1. Elimination disorders related to a decrease in urine volume. 2. Imbalanced Nutrition Less than Body related to nausea, vomiting and anorexia 3. Excess Fluid Volume related to inhibition of normal ADH uncontrolled 4. Disturbed Thought Processes related to decreased levels of Na. 32
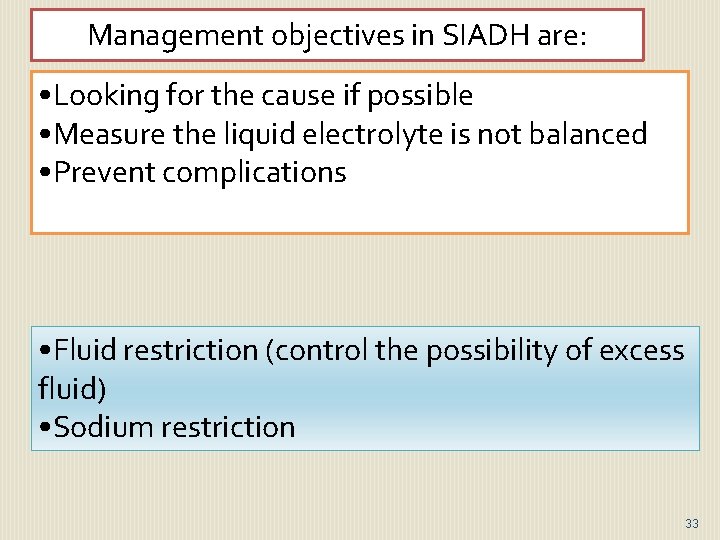
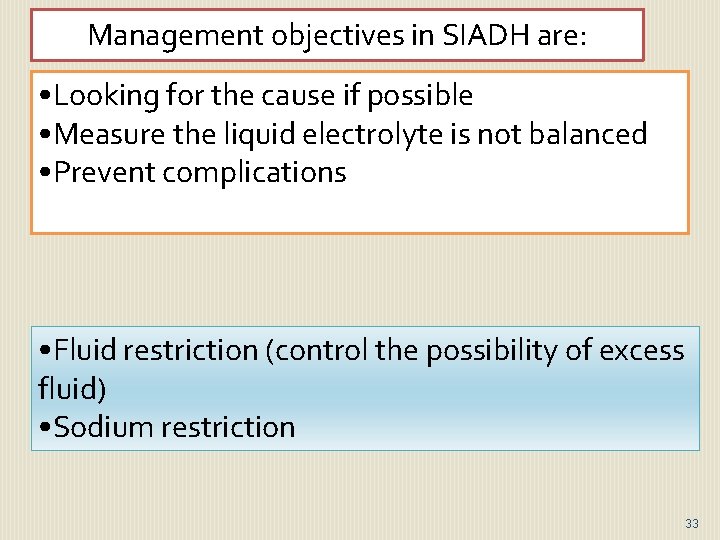
Management objectives in SIADH are: • Looking for the cause if possible • Measure the liquid electrolyte is not balanced • Prevent complications • Fluid restriction (control the possibility of excess fluid) • Sodium restriction 33
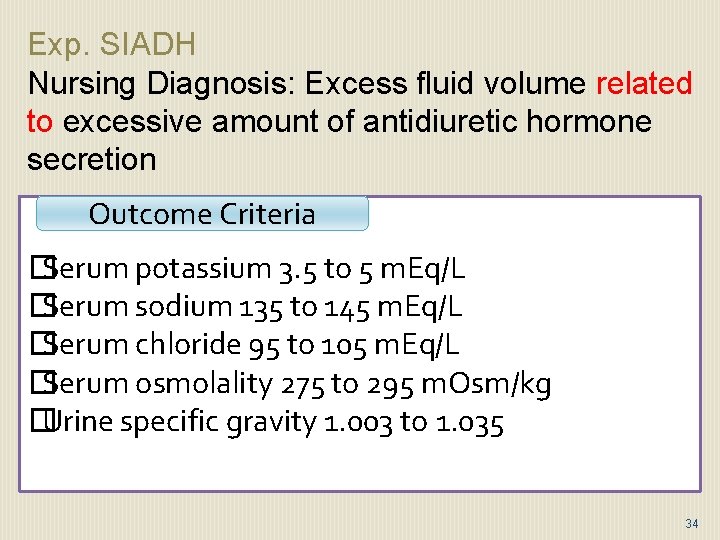
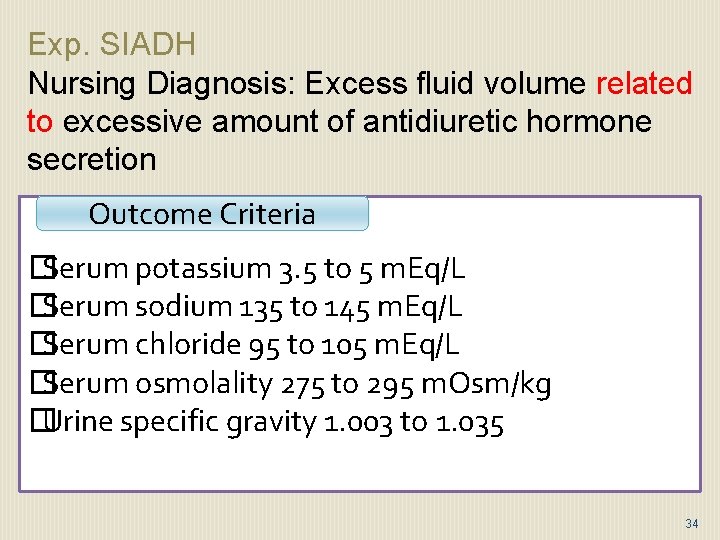
Exp. SIADH Nursing Diagnosis: Excess fluid volume related to excessive amount of antidiuretic hormone secretion Outcome Criteria � Serum potassium 3. 5 to 5 m. Eq/L � Serum sodium 135 to 145 m. Eq/L � Serum chloride 95 to 105 m. Eq/L � Serum osmolality 275 to 295 m. Osm/kg � Urine specific gravity 1. 003 to 1. 035 34
35
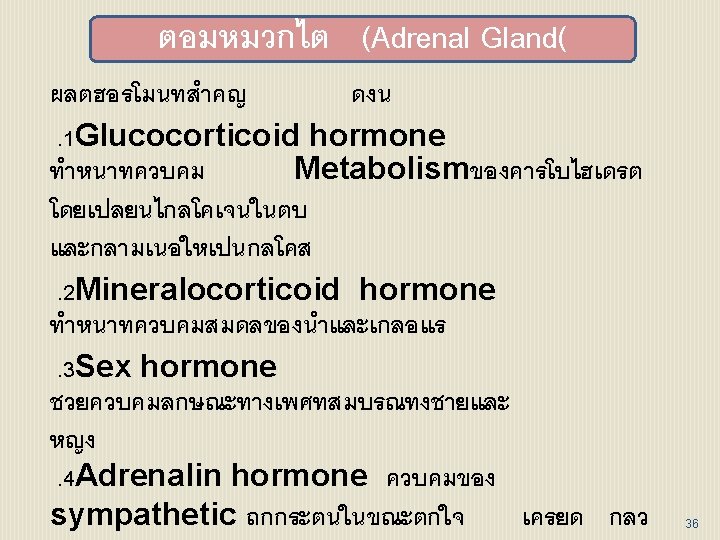
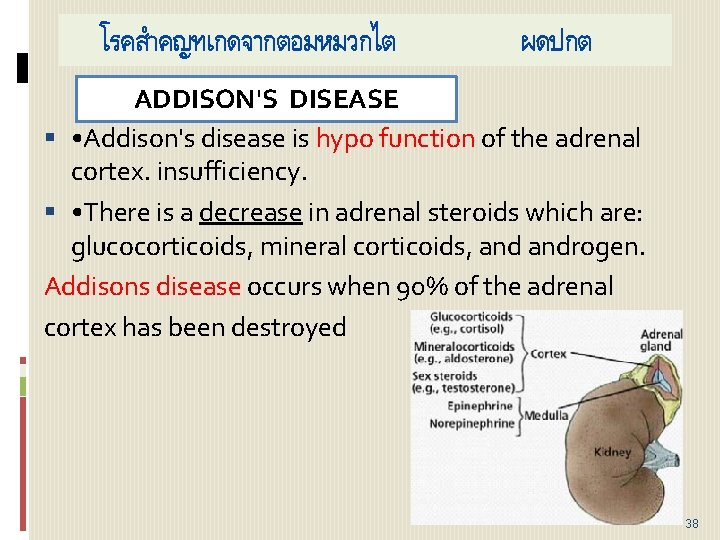
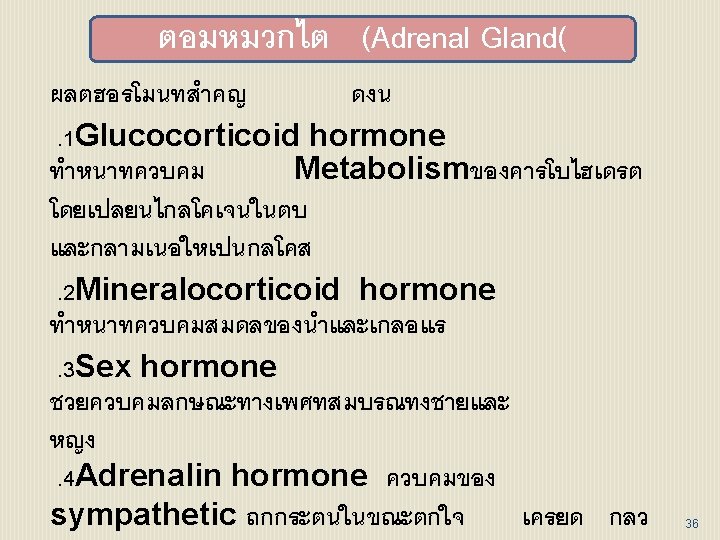
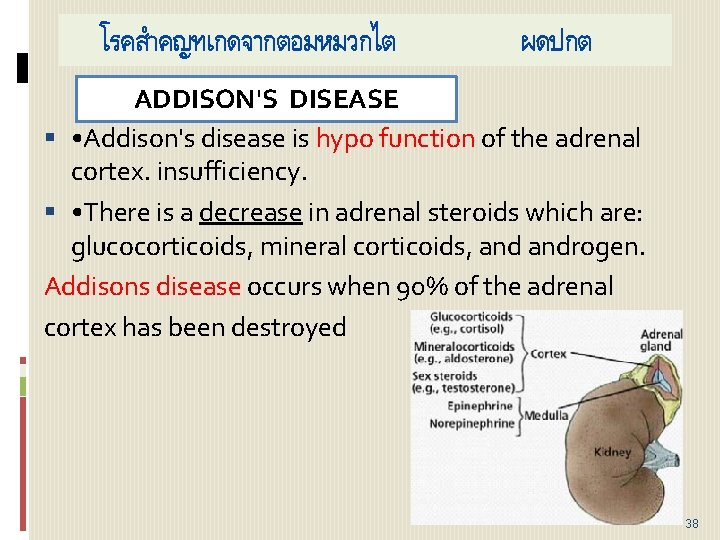
โรคสำคญทเกดจากตอมหมวกไต ผดปกต ADDISON'S DISEASE • Addison's disease is hypo function of the adrenal cortex. insufficiency. • There is a decrease in adrenal steroids which are: glucocorticoids, mineral corticoids, androgen. Addisons disease occurs when 90% of the adrenal cortex has been destroyed 38
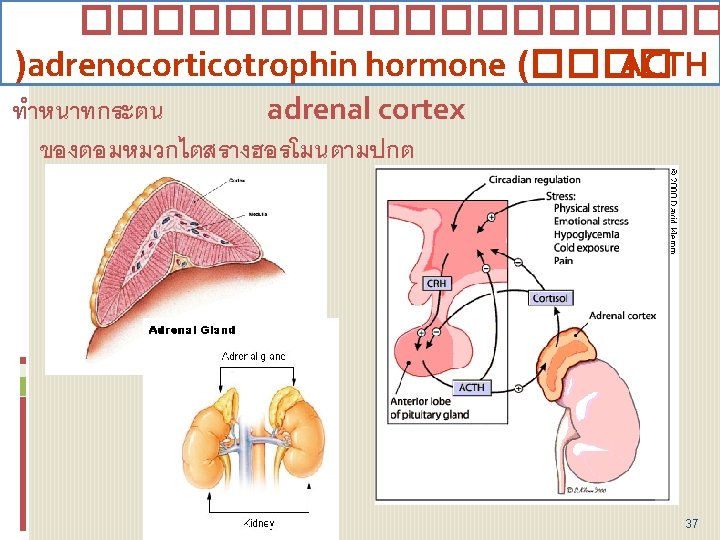
CAUSES • Autoimmune or idiopathic atrophy of the adrenal glands is responsible for 80% to 90% of cases. • Surgical removal of both adrenal glands • Infection of the adrenal glands • Tuberculosis and histoplasmosis are the most • Inadequate secretion of ACTH from the pituitary. By: Claudia Martinez Cynthia Diaz Courtney Hipp 39
SIGNS AND SYMPTOMS • Early signs: Tiredness, Weakness Loss of appetite , Weight loss Dizziness when standing Muscle aches Nausea, vomiting Diarrhea Depression Late signs: Sharp pain in the abdomen, or legs Loss of too much fluid from body (Dehydration) Hypotension 40
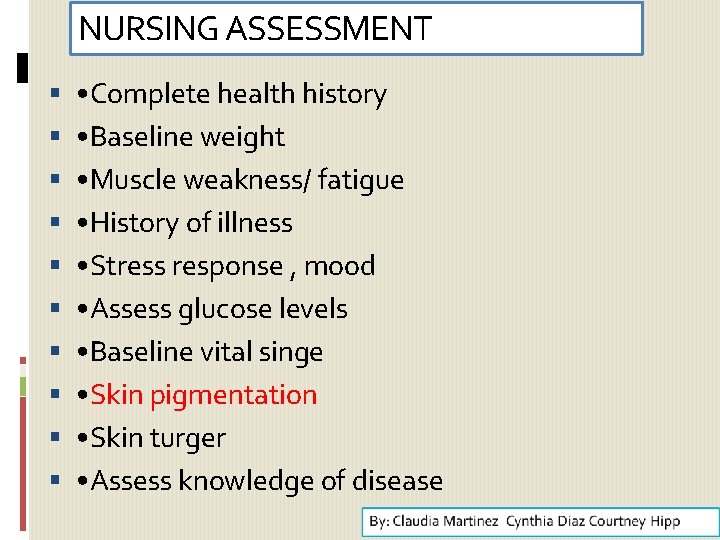
NURSING ASSESSMENT • Complete health history • Baseline weight • Muscle weakness/ fatigue • History of illness • Stress response , mood • Assess glucose levels • Baseline vital singe • Skin pigmentation • Skin turger • Assess knowledge of disease 41
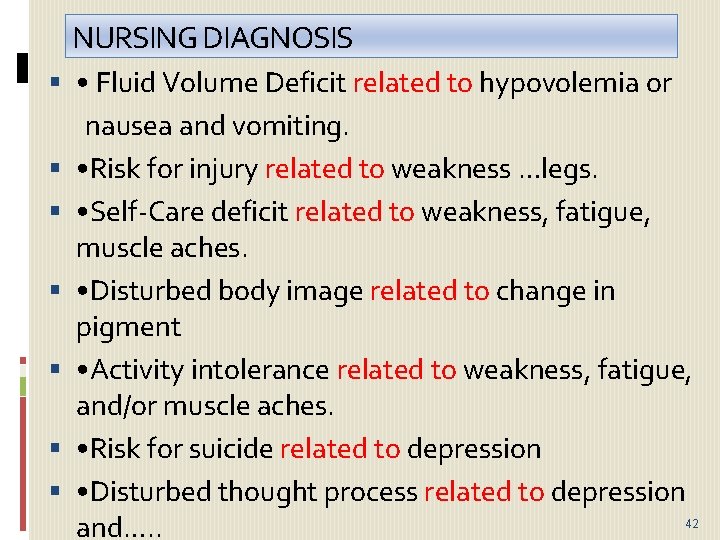
NURSING DIAGNOSIS • Fluid Volume Deficit related to hypovolemia or nausea and vomiting. • Risk for injury related to weakness …legs. • Self-Care deficit related to weakness, fatigue, muscle aches. • Disturbed body image related to change in pigment • Activity intolerance related to weakness, fatigue, and/or muscle aches. • Risk for suicide related to depression • Disturbed thought process related to depression 42 and…. .
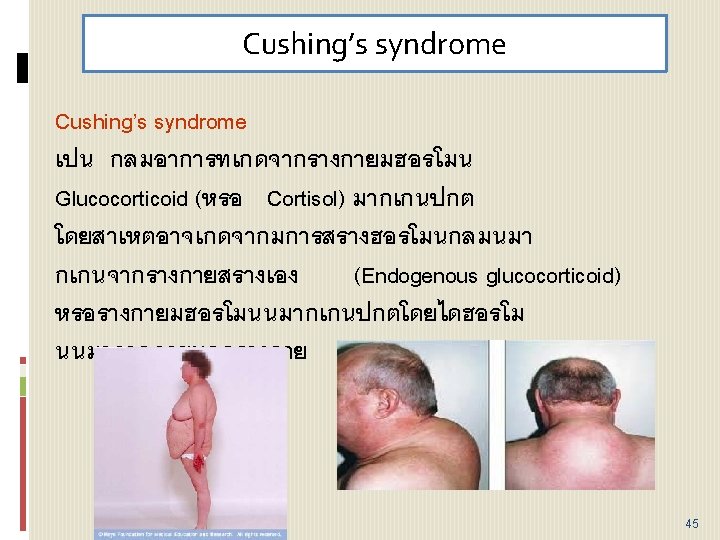
Cushing’s syndrome 43
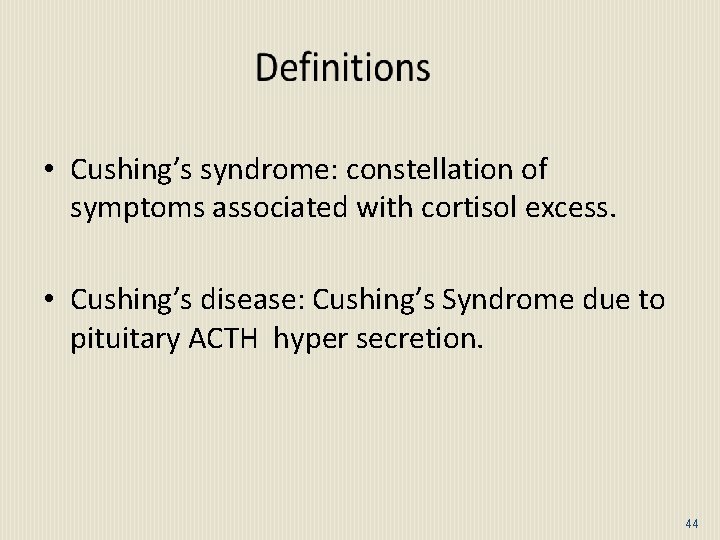
• Cushing’s syndrome: constellation of symptoms associated with cortisol excess. • Cushing’s disease: Cushing’s Syndrome due to pituitary ACTH hyper secretion. 44
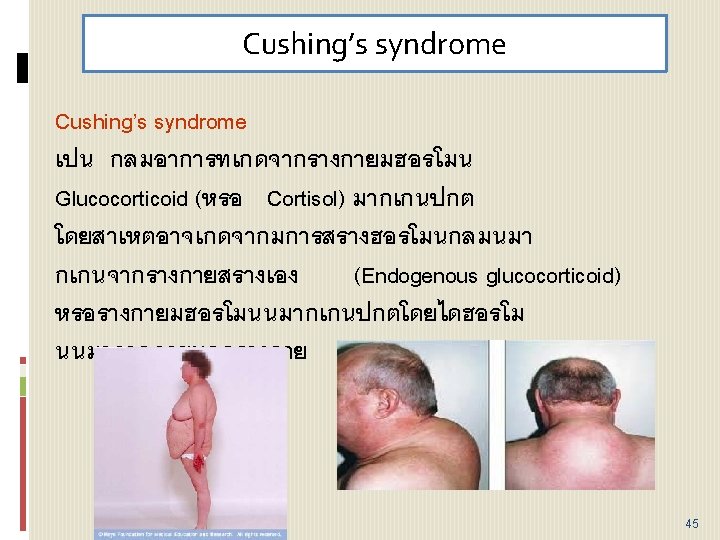
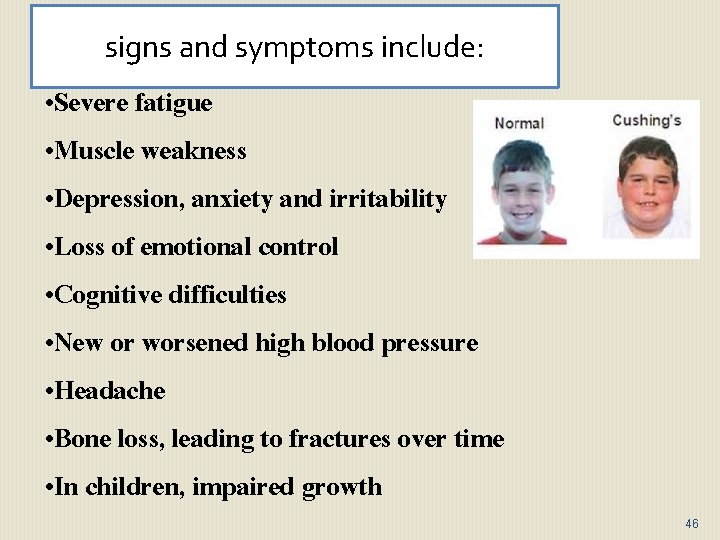
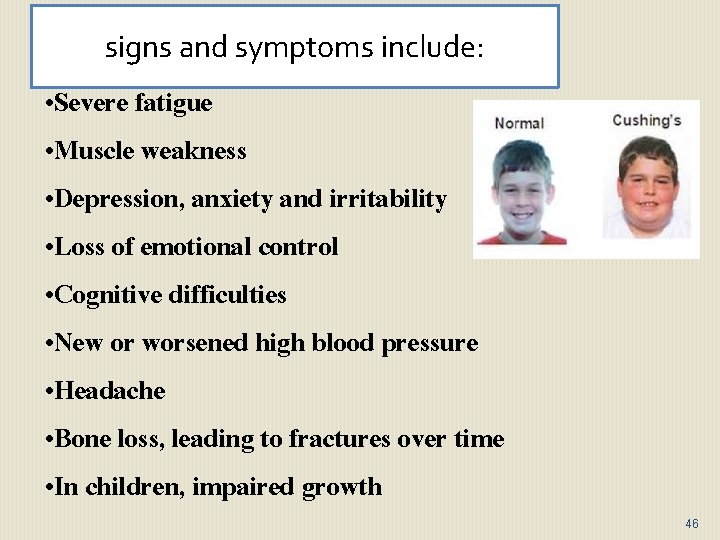
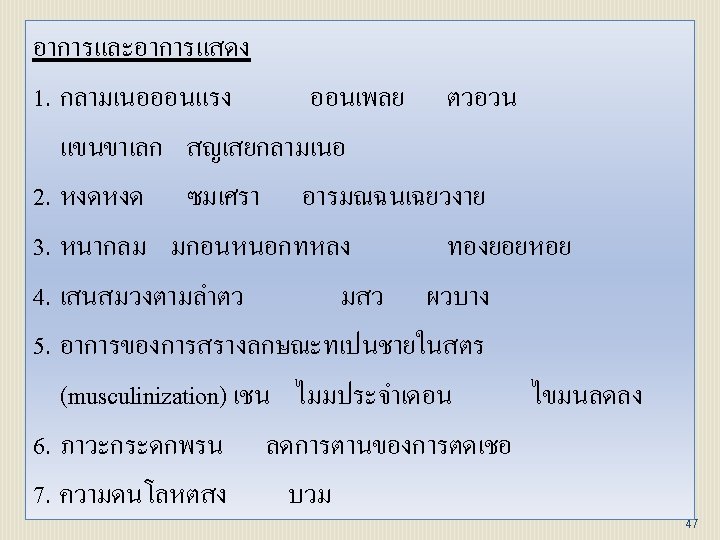
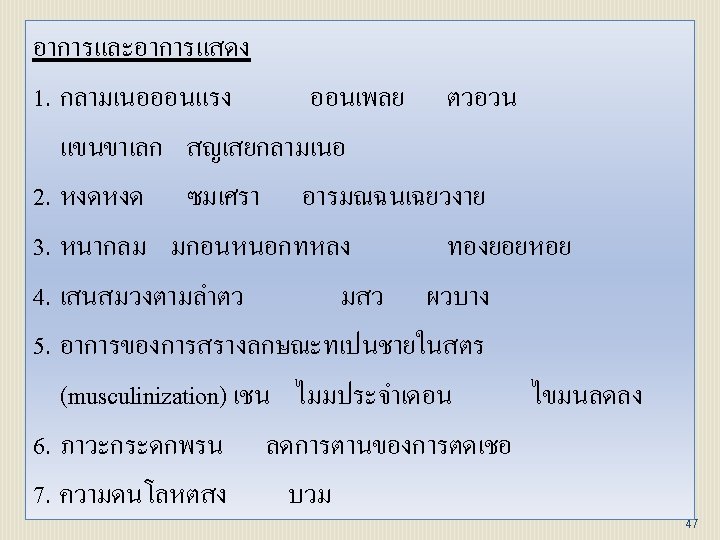
: signs and symptoms include: • Severe fatigue • Muscle weakness • Depression, anxiety and irritability • Loss of emotional control • Cognitive difficulties • New or worsened high blood pressure • Headache • Bone loss, leading to fractures over time • In children, impaired growth 46
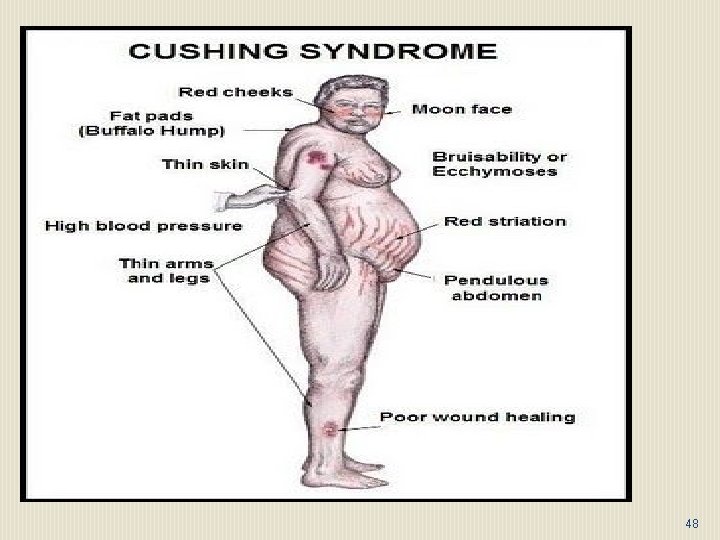
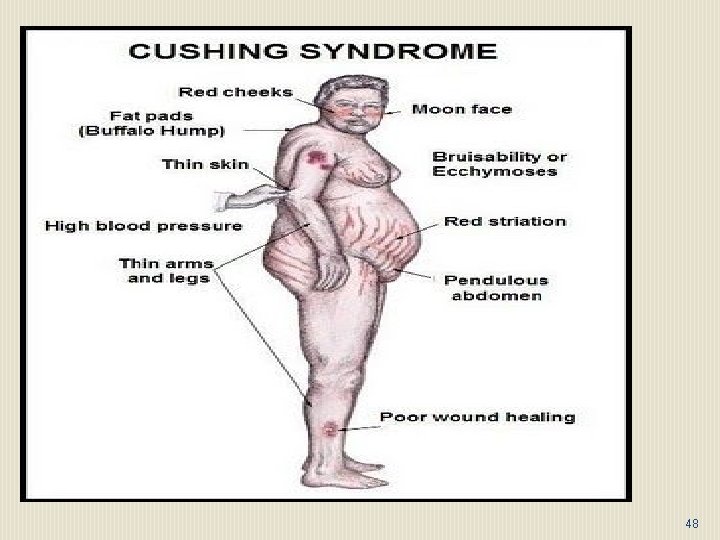
48
Because cortisol is responsible for many functions in the body, qsuch as helping to maintain blood pressure, qreducing inflammation, qbalancing the effects of insulin and regulating metabolism, qan excessive amount produces various symptoms. 49
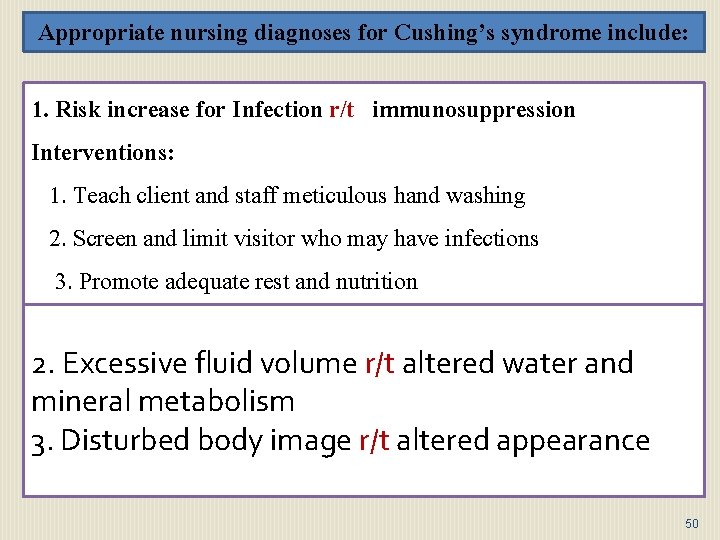
Appropriate nursing diagnoses for Cushing’s syndrome include: 1. Risk increase for Infection r/t immunosuppression Interventions: 1. Teach client and staff meticulous hand washing 2. Screen and limit visitor who may have infections 3. Promote adequate rest and nutrition 2. Excessive fluid volume r/t altered water and mineral metabolism 3. Disturbed body image r/t altered appearance 50
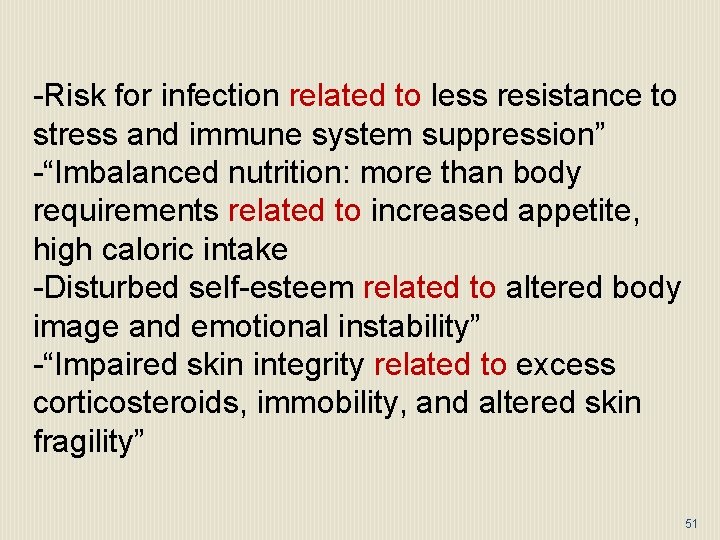
-Risk for infection related to less resistance to stress and immune system suppression” -“Imbalanced nutrition: more than body requirements related to increased appetite, high caloric intake -Disturbed self-esteem related to altered body image and emotional instability” -“Impaired skin integrity related to excess corticosteroids, immobility, and altered skin fragility” 51
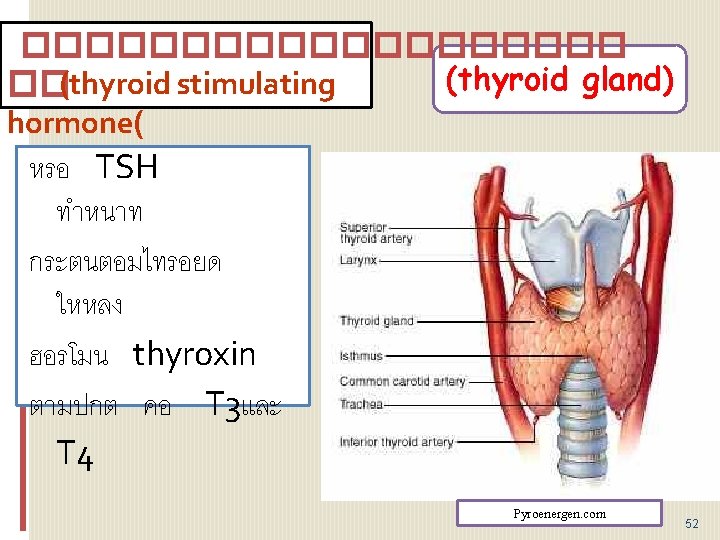
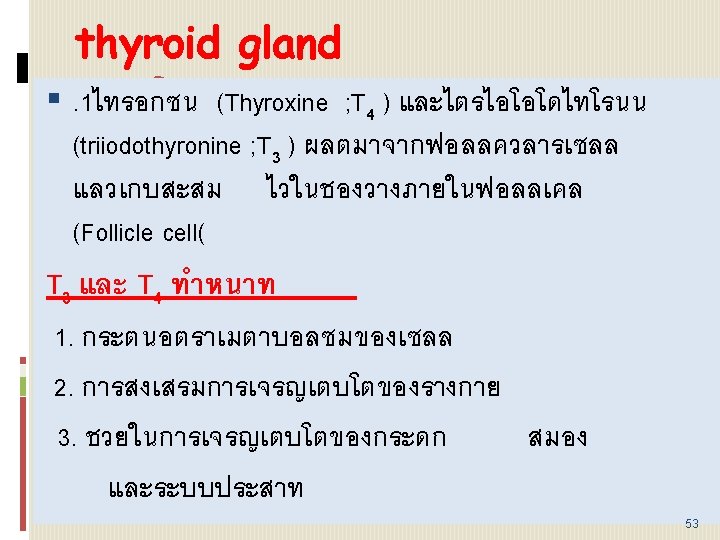
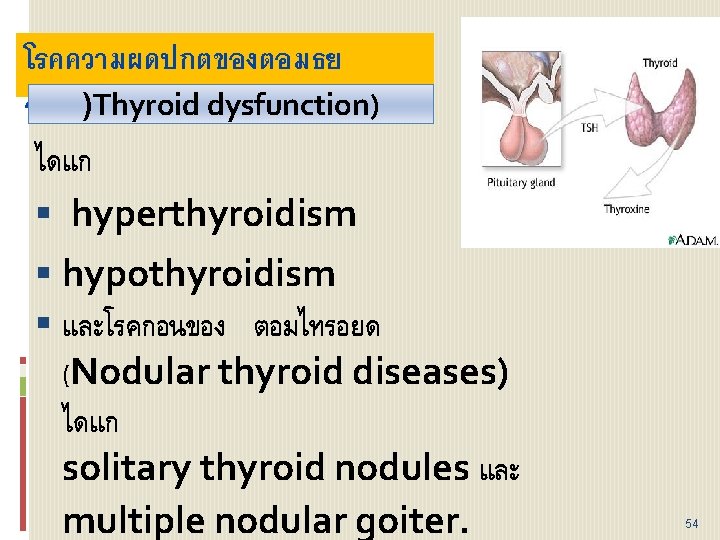
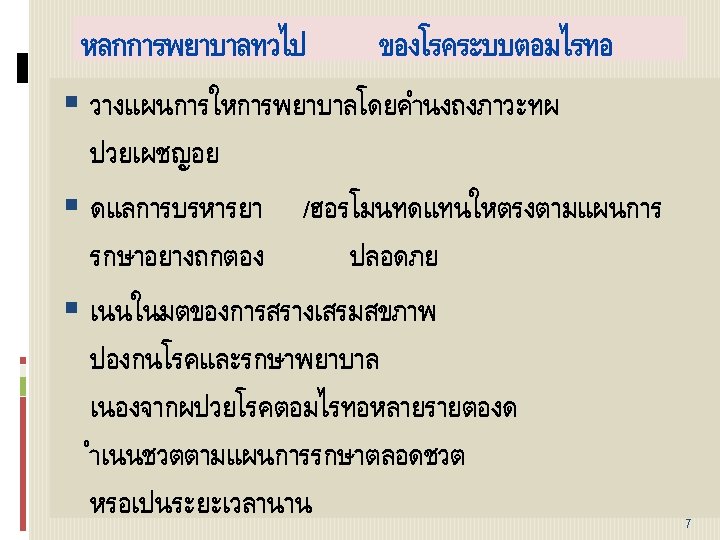
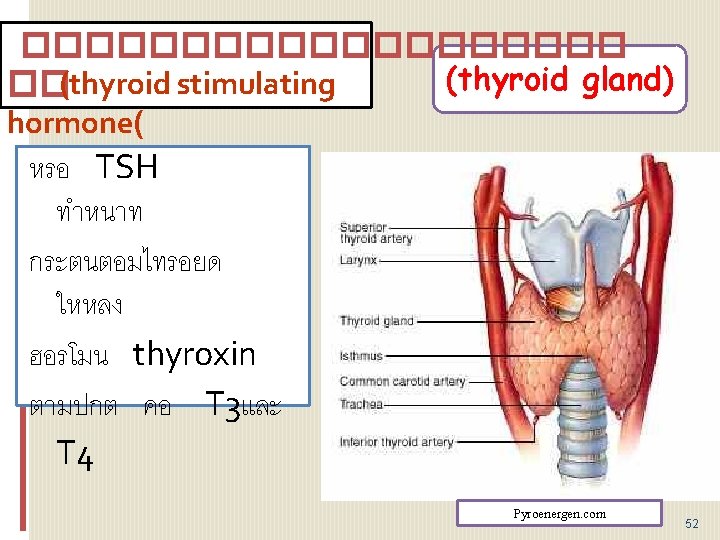
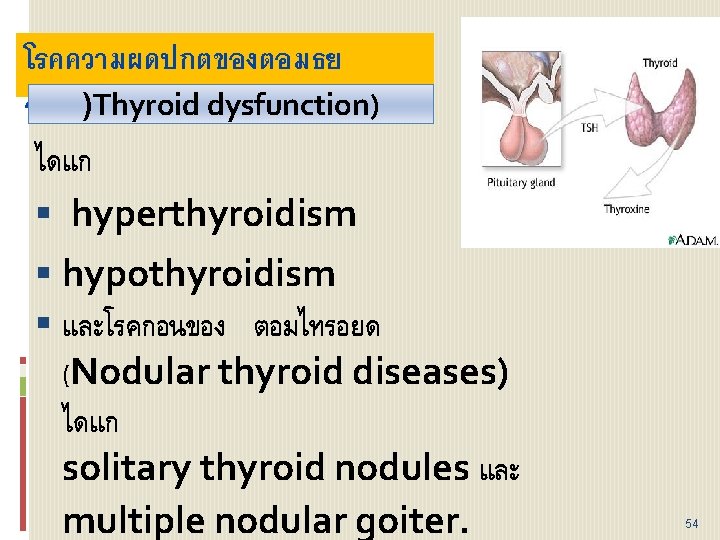
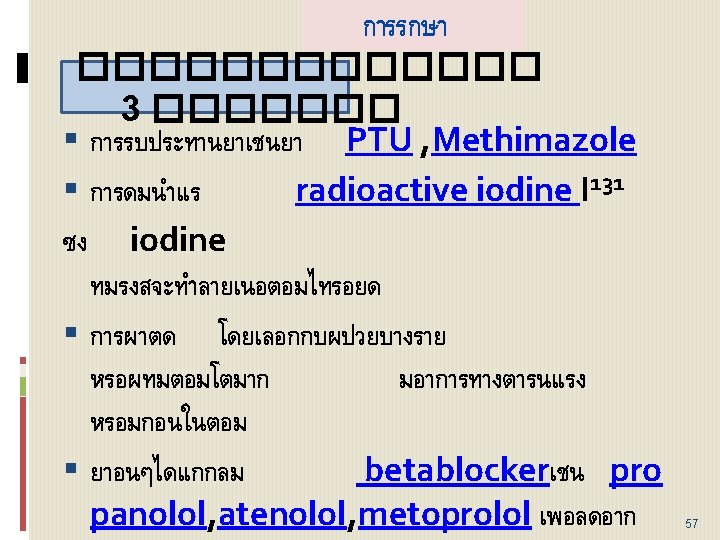
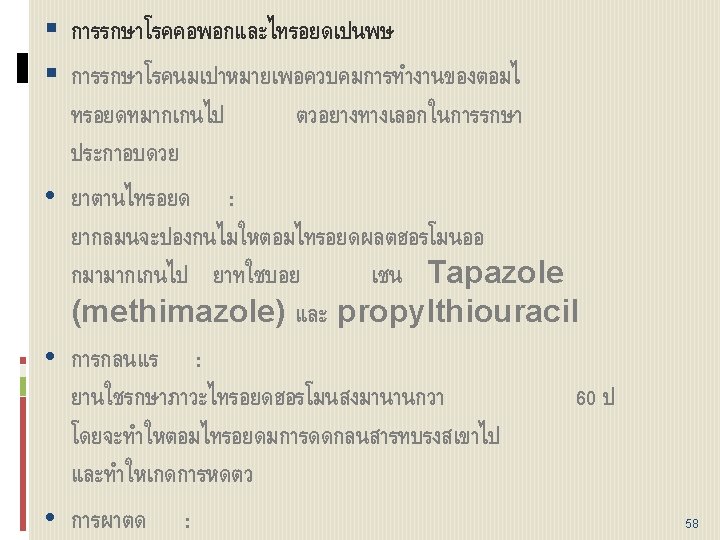
โรคความผดปกตของตอมธย รอยด)Thyroid dysfunction) ไดแก hyperthyroidism hypothyroidism และโรคกอนของ ตอมไทรอยด (Nodular thyroid diseases) ไดแก solitary thyroid nodules และ multiple nodular goiter. 54
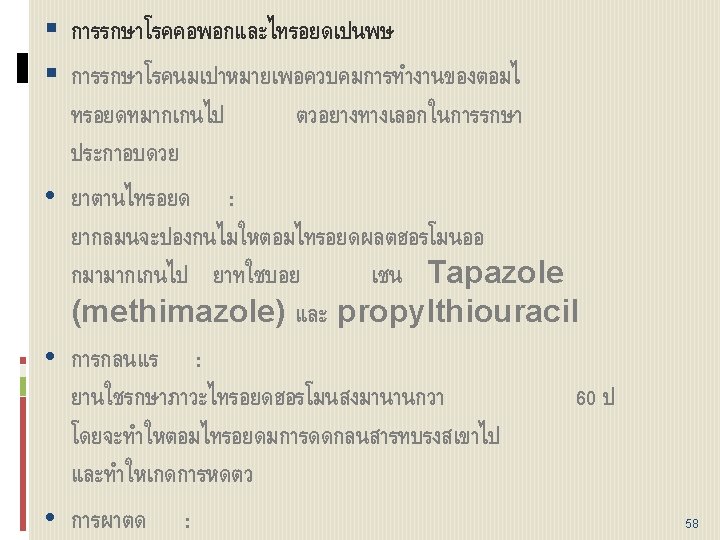
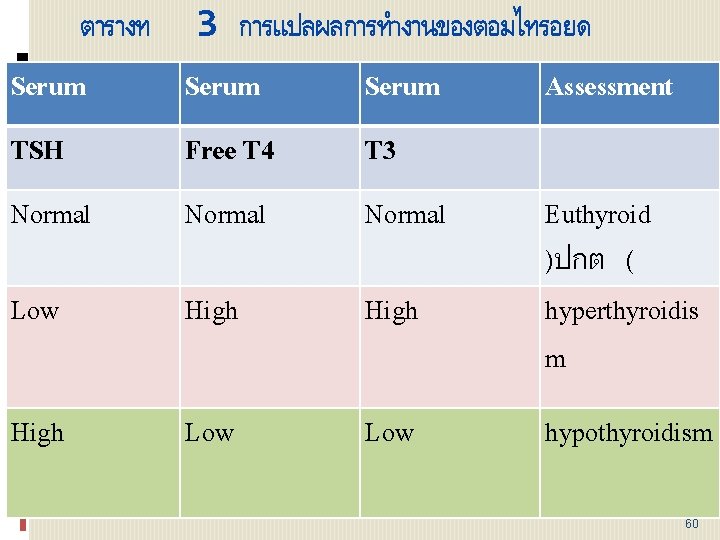
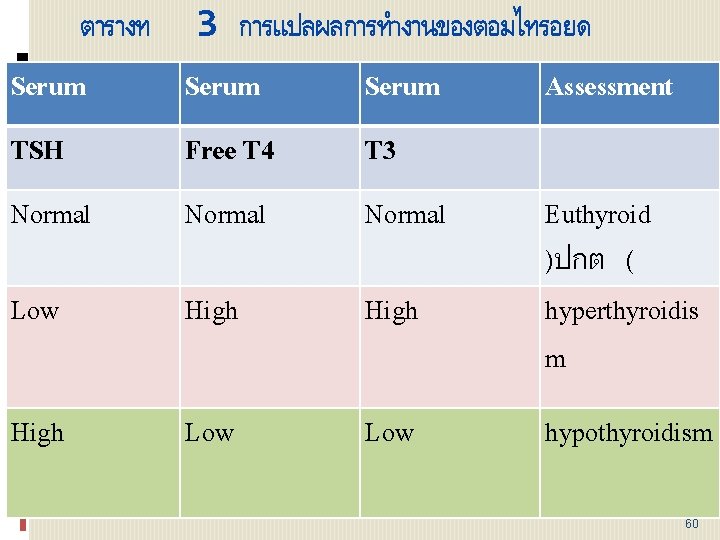
ตารางท 3 การแปลผลการทำงานของตอมไทรอยด Serum Assessment TSH Free T 4 T 3 Normal Low High Low Euthyroid )ปกต ( hyperthyroidis m hypothyroidism 60
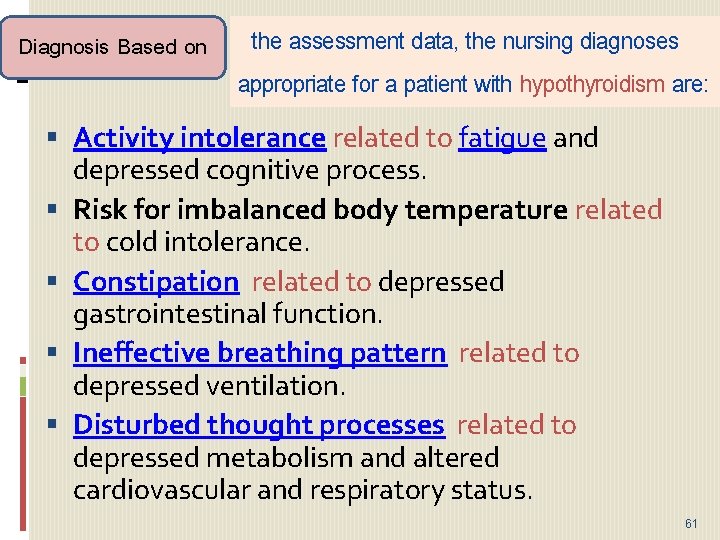
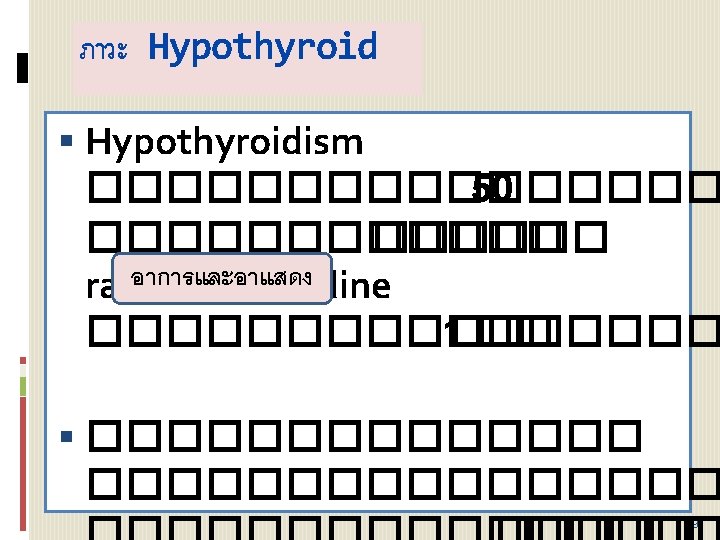
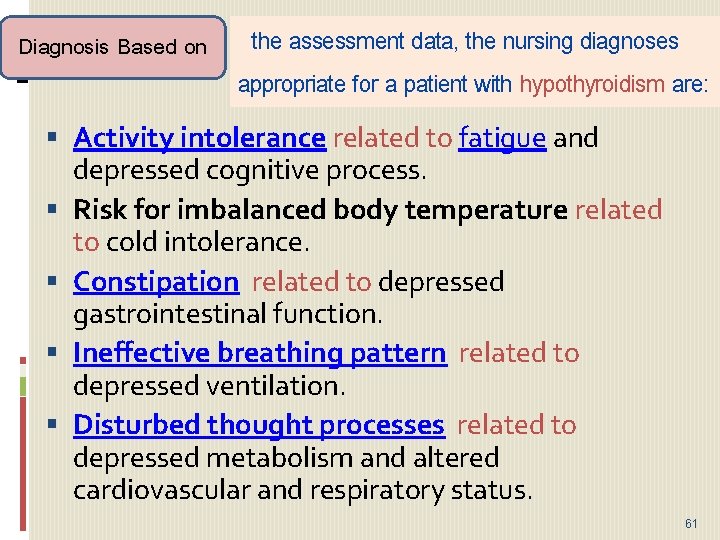
Diagnosis Based on the assessment data, the nursing diagnoses appropriate for a patient with hypothyroidism are: Activity intolerance related to fatigue and depressed cognitive process. Risk for imbalanced body temperature related to cold intolerance. Constipation related to depressed gastrointestinal function. Ineffective breathing pattern related to depressed ventilation. Disturbed thought processes related to depressed metabolism and altered cardiovascular and respiratory status. 61
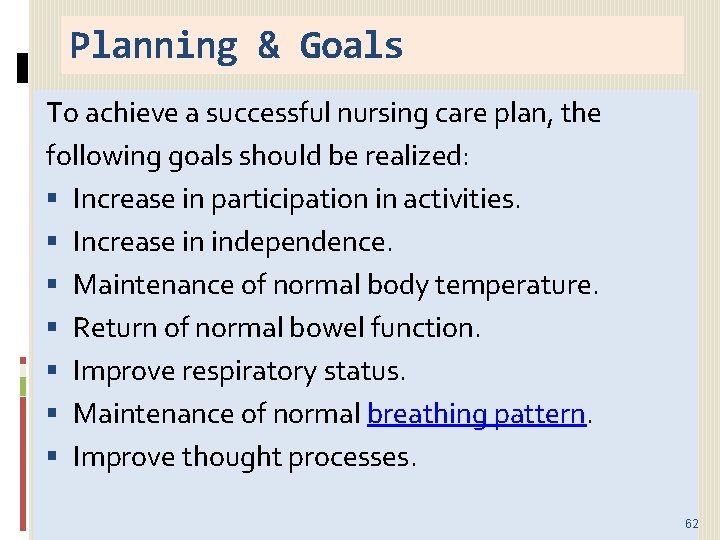
Planning & Goals To achieve a successful nursing care plan, the following goals should be realized: Increase in participation in activities. Increase in independence. Maintenance of normal body temperature. Return of normal bowel function. Improve respiratory status. Maintenance of normal breathing pattern. Improve thought processes. 62
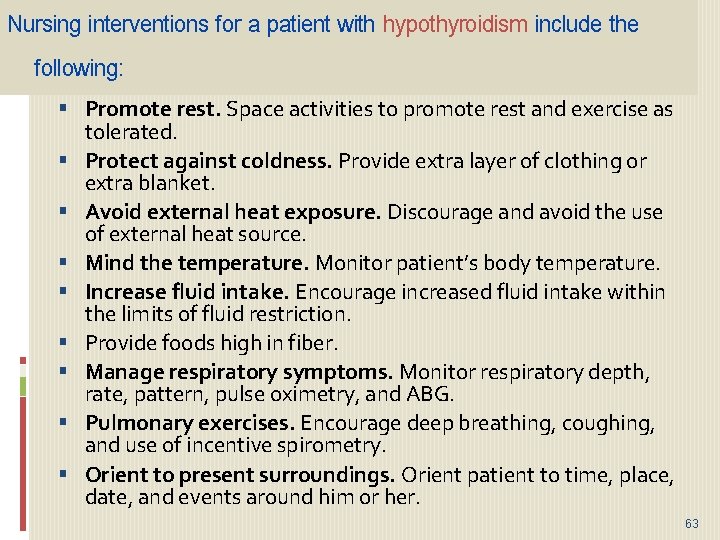
Nursing interventions for a patient with hypothyroidism include the following: Promote rest. Space activities to promote rest and exercise as tolerated. Protect against coldness. Provide extra layer of clothing or extra blanket. Avoid external heat exposure. Discourage and avoid the use of external heat source. Mind the temperature. Monitor patient’s body temperature. Increase fluid intake. Encourage increased fluid intake within the limits of fluid restriction. Provide foods high in fiber. Manage respiratory symptoms. Monitor respiratory depth, rate, pattern, pulse oximetry, and ABG. Pulmonary exercises. Encourage deep breathing, coughing, and use of incentive spirometry. Orient to present surroundings. Orient patient to time, place, date, and events around him or her. 63
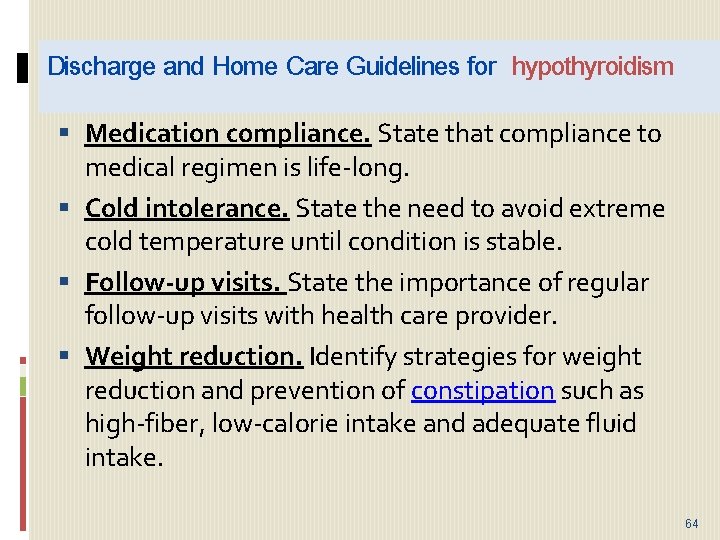
Discharge and Home Care Guidelines for hypothyroidism Medication compliance. State that compliance to medical regimen is life-long. Cold intolerance. State the need to avoid extreme cold temperature until condition is stable. Follow-up visits. State the importance of regular follow-up visits with health care provider. Weight reduction. Identify strategies for weight reduction and prevention of constipation such as high-fiber, low-calorie intake and adequate fluid intake. 64
Nursing Diagnosis Risk for Decreased Cardiac Output Risk factors may include Uncontrolled hyperthyroidism, hyper metabolic state Increasing cardiac workload Changes in venous return and systemic vascular resistance Alterations in rate, rhythm, conduction 65
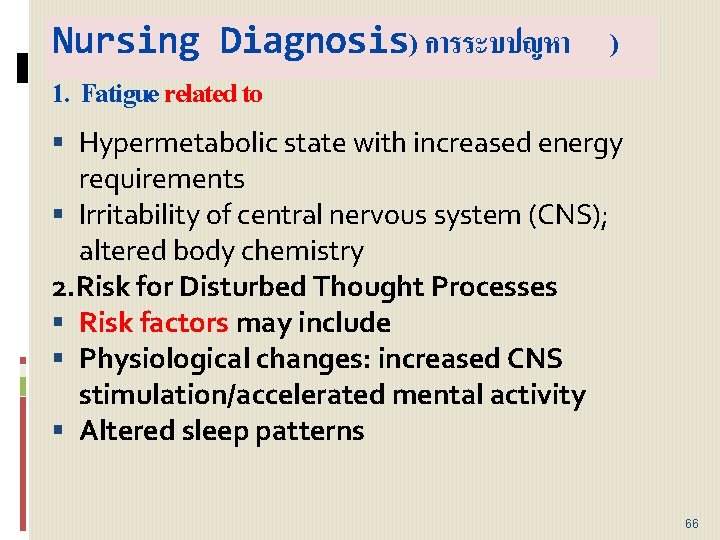
Nursing Diagnosis) การระบปญหา ) 1. Fatigue related to Hypermetabolic state with increased energy requirements Irritability of central nervous system (CNS); altered body chemistry 2. Risk for Disturbed Thought Processes Risk factors may include Physiological changes: increased CNS stimulation/accelerated mental activity Altered sleep patterns 66
Nursing Diagnosis Out come Maintain usual reality orientation. Recognize changes in thinking/behavior and causative factors. 67
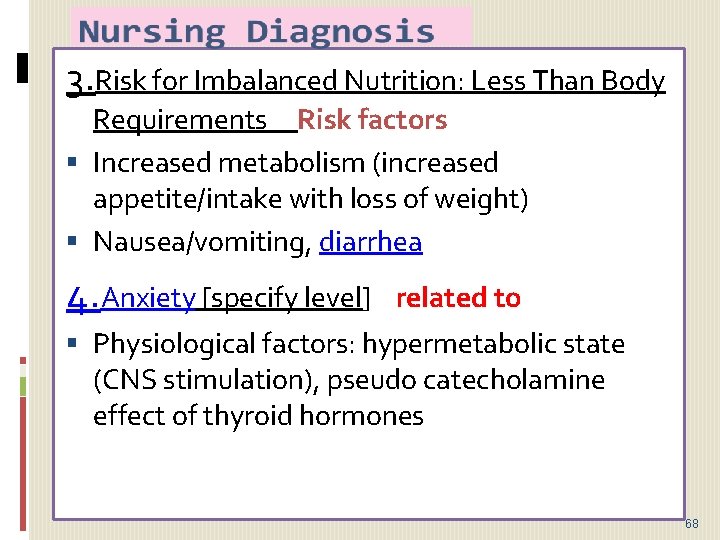
3. Risk for Imbalanced Nutrition: Less Than Body Requirements Risk factors Increased metabolism (increased appetite/intake with loss of weight) Nausea/vomiting, diarrhea 4. Anxiety [specify level] related to Physiological factors: hypermetabolic state (CNS stimulation), pseudo catecholamine effect of thyroid hormones 68
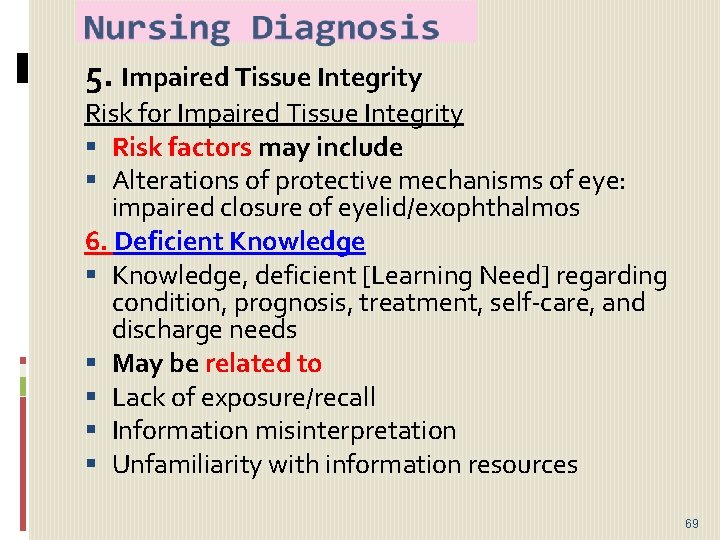
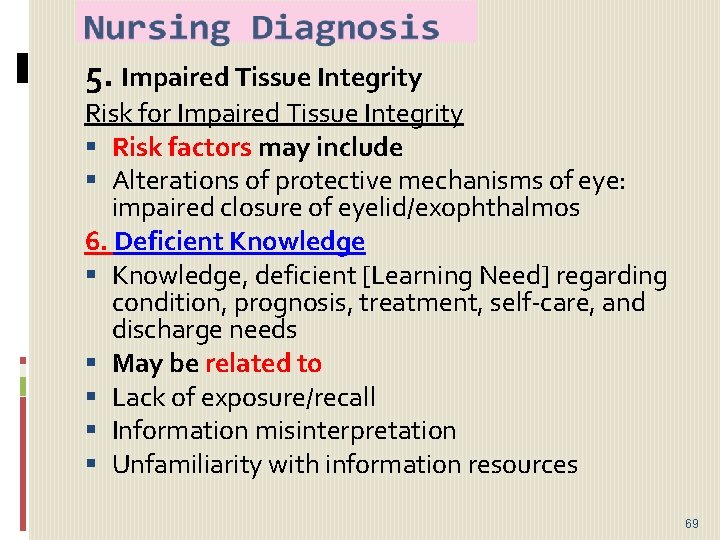
5. Impaired Tissue Integrity Risk for Impaired Tissue Integrity Risk factors may include Alterations of protective mechanisms of eye: impaired closure of eyelid/exophthalmos 6. Deficient Knowledge, deficient [Learning Need] regarding condition, prognosis, treatment, self-care, and discharge needs May be related to Lack of exposure/recall Information misinterpretation Unfamiliarity with information resources 69
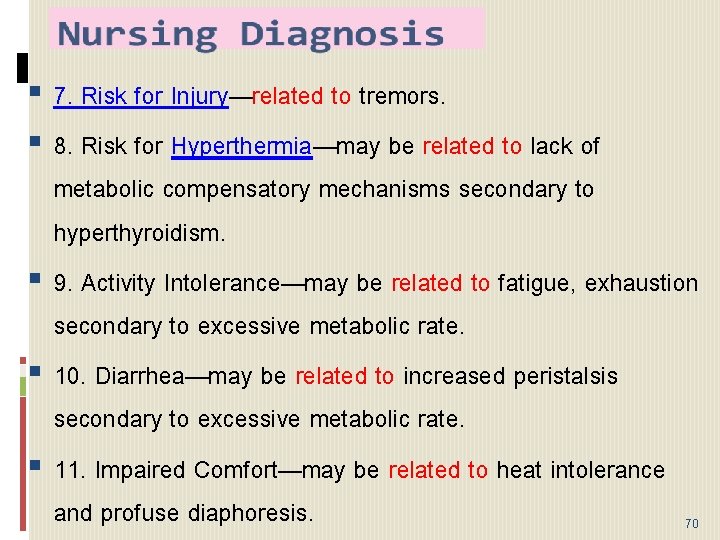
7. Risk for Injury—related to tremors. 8. Risk for Hyperthermia—may be related to lack of metabolic compensatory mechanisms secondary to hyperthyroidism. 9. Activity Intolerance—may be related to fatigue, exhaustion secondary to excessive metabolic rate. 10. Diarrhea—may be related to increased peristalsis secondary to excessive metabolic rate. 11. Impaired Comfort—may be related to heat intolerance and profuse diaphoresis. 70
12. Risk for Impaired Tissue Integrity: Corneal— may be related to inability to close eyelids secondary to exophthalmos. 71

THANK YOU 72