Hypothalamic Pituitary Hormones Dept of Pharmacology CIPS The

- Slides: 32
Hypothalamic Pituitary Hormones Dept. of Pharmacology, CIPS
The hypothalamic - pituitary axis: • The pituitary is connected to the hypothalamus by a stalk (the infundibulum) which carries axons to the neurohypophysis (posterior pituitary) as well as blood vessels to the adenohypophysis (anterior pituitary). • Most feedback loops run through this axis • HPA mediates Reproduction. Growth, Metabolism, Stress response,
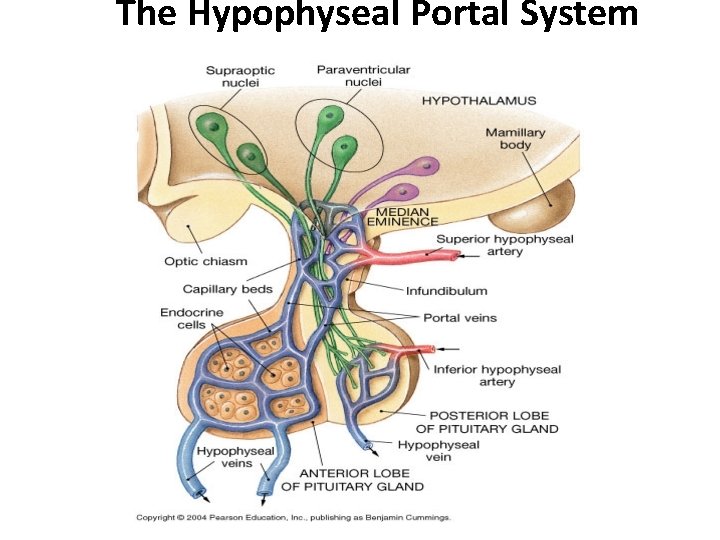
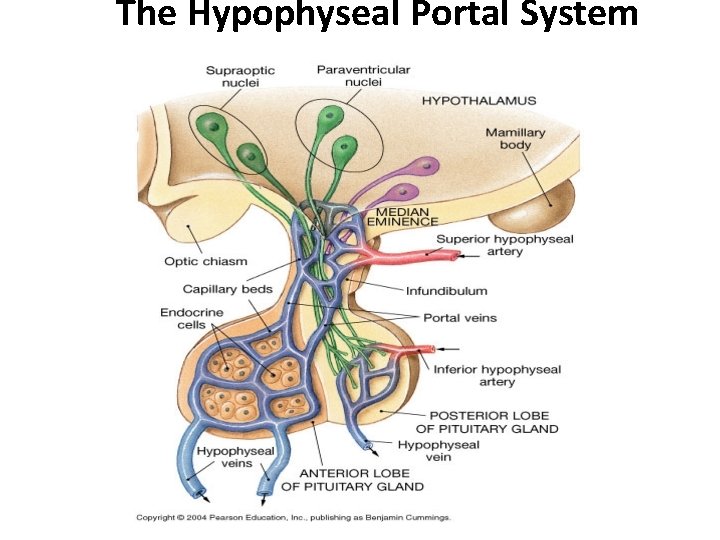
The Hypophyseal Portal System
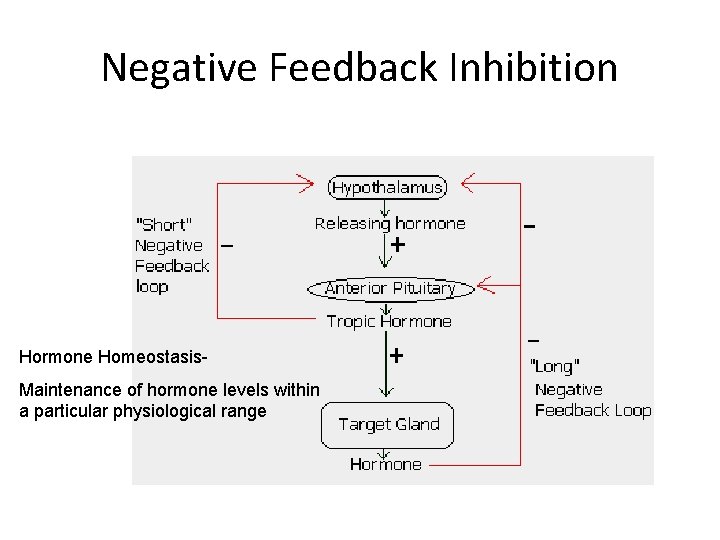
Characteristics of Hypothalamic releasing and inhibiting hormones • Hypothalamic releasing and inhibiting hormones are carried directly ONLY to the anterior pituitary gland via hypothalamic hypophyseal portal veins. • Secretion is pulsatile • They have short half lives so their actions on the pituitary are of short duration. • Their actions are limited by negative feedback mechanisms. • They stimulate release of anterior pituitary hormones. • They stimulate synthesis of anterior pituitary hormones. • They stimulate hyperplasia and hypertrophy of target cells.
Hypothalamic Neurohormones Seven neurohormones are made in the hypothalamus – Thyrotropin-releasing hormone (TRH) – Corticotropin-releasing hormone (CRH) – Gonadotropin-releasing hormone (Gn. RH) – Growth hormone-releasing hormone (GHRH) – Growth hormone-release inhibiting hormone (GHIH) or somatostatin – Prolactin-releasing factor (PRF) – Prolactin-inhibiting hormone (PIH)

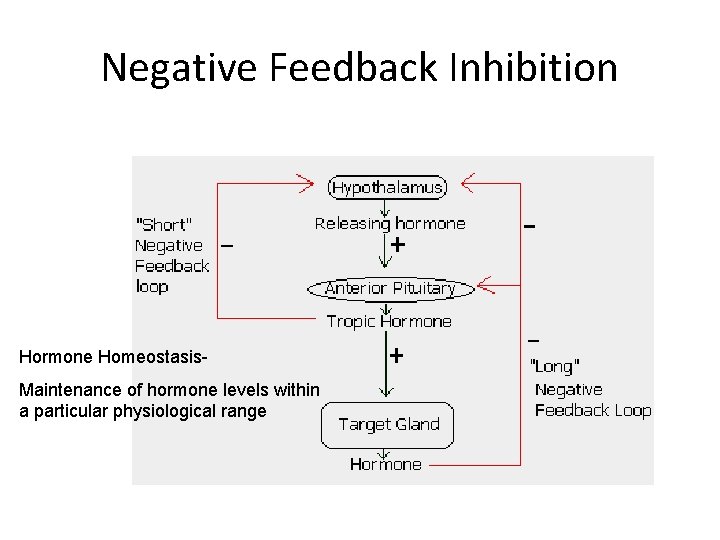
Negative Feedback Inhibition Hormone Homeostasis. Maintenance of hormone levels within a particular physiological range
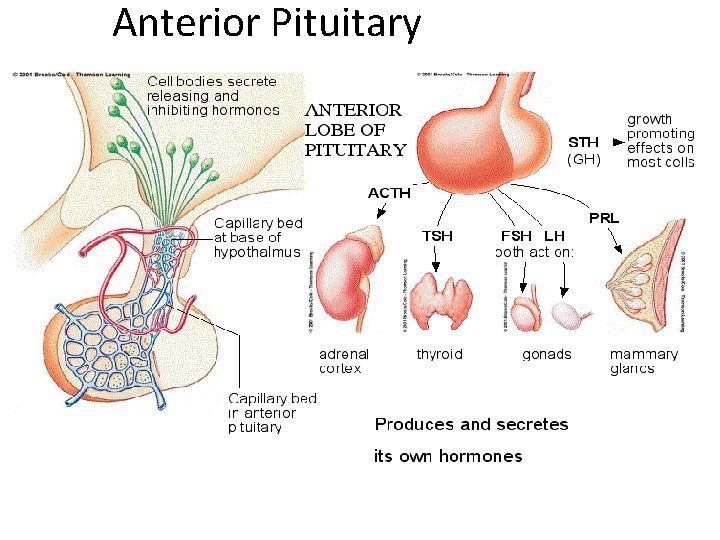
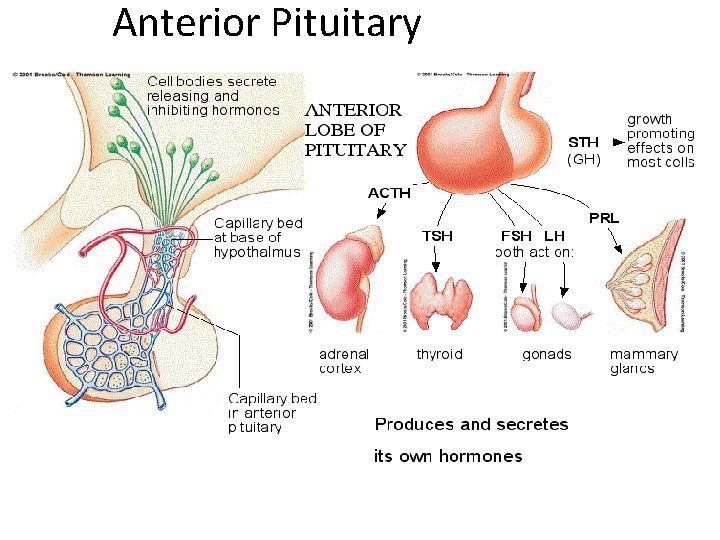
Anterior Pituitary
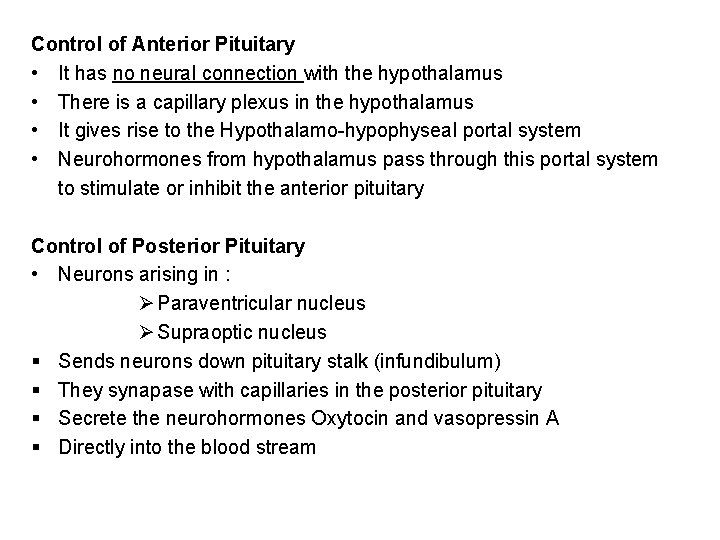
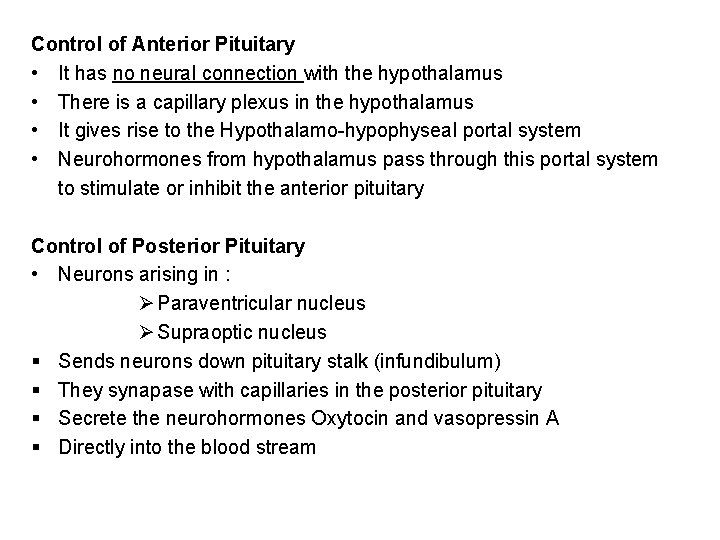
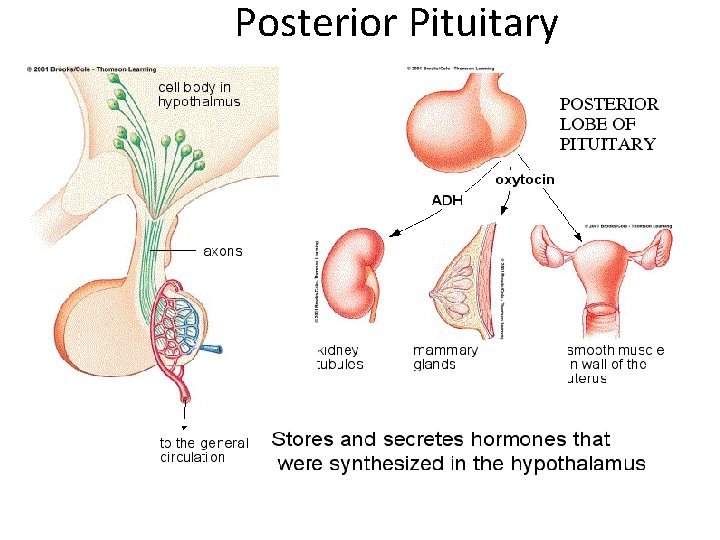
Control of Anterior Pituitary • It has no neural connection with the hypothalamus • There is a capillary plexus in the hypothalamus • It gives rise to the Hypothalamo-hypophyseal portal system • Neurohormones from hypothalamus pass through this portal system to stimulate or inhibit the anterior pituitary Control of Posterior Pituitary • Neurons arising in : Ø Paraventricular nucleus Ø Supraoptic nucleus § Sends neurons down pituitary stalk (infundibulum) § They synapase with capillaries in the posterior pituitary § Secrete the neurohormones Oxytocin and vasopressin A § Directly into the blood stream
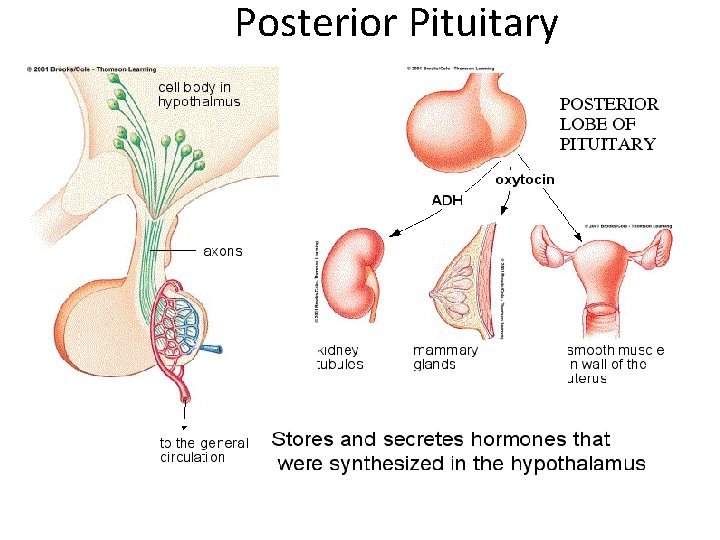
Posterior Pituitary
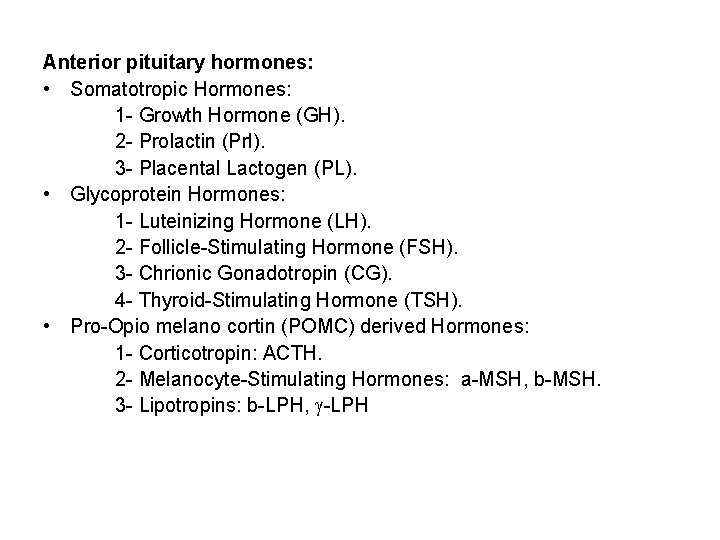
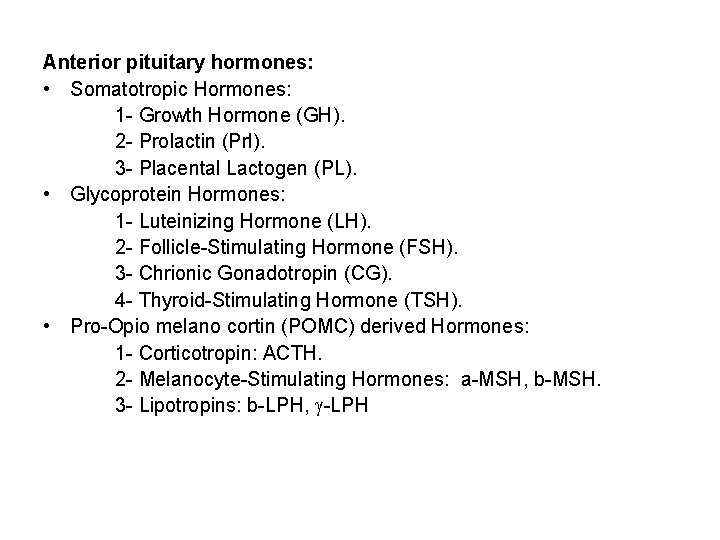
Anterior pituitary hormones: • Somatotropic Hormones: 1 - Growth Hormone (GH). 2 - Prolactin (Prl). 3 - Placental Lactogen (PL). • Glycoprotein Hormones: 1 - Luteinizing Hormone (LH). 2 - Follicle-Stimulating Hormone (FSH). 3 - Chrionic Gonadotropin (CG). 4 - Thyroid-Stimulating Hormone (TSH). • Pro-Opio melano cortin (POMC) derived Hormones: 1 - Corticotropin: ACTH. 2 - Melanocyte-Stimulating Hormones: a-MSH, b-MSH. 3 - Lipotropins: b-LPH, -LPH
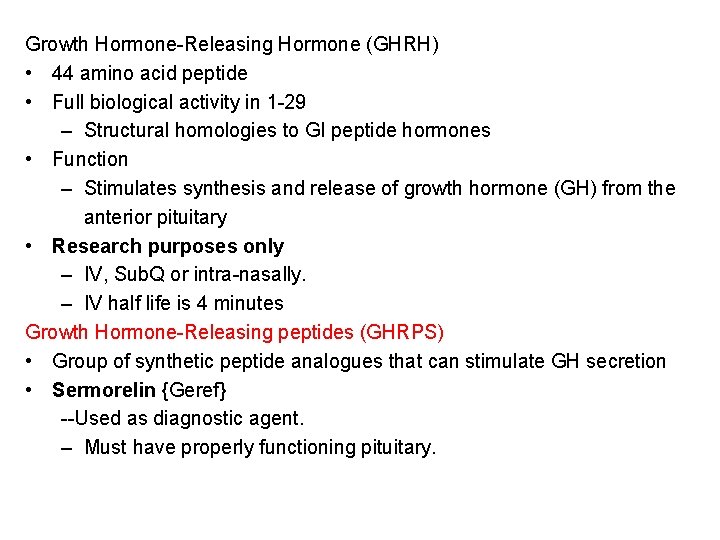
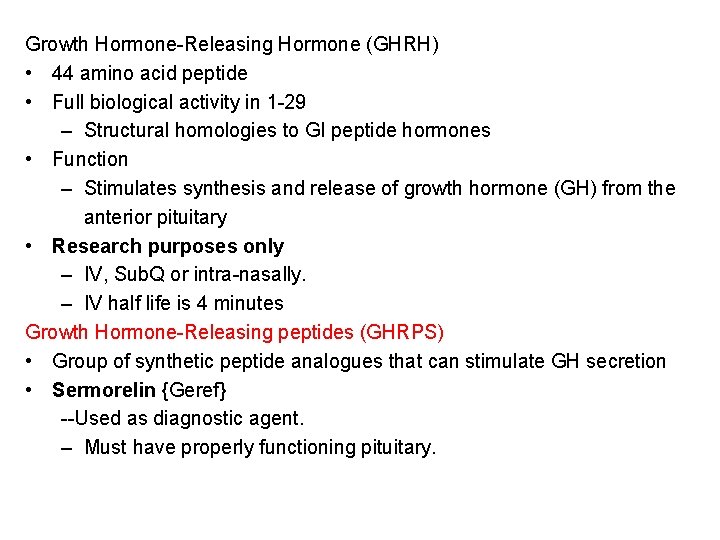
Growth Hormone-Releasing Hormone (GHRH) • 44 amino acid peptide • Full biological activity in 1 -29 – Structural homologies to GI peptide hormones • Function – Stimulates synthesis and release of growth hormone (GH) from the anterior pituitary • Research purposes only – IV, Sub. Q or intra-nasally. – IV half life is 4 minutes Growth Hormone-Releasing peptides (GHRPS) • Group of synthetic peptide analogues that can stimulate GH secretion • Sermorelin {Geref} --Used as diagnostic agent. – Must have properly functioning pituitary.
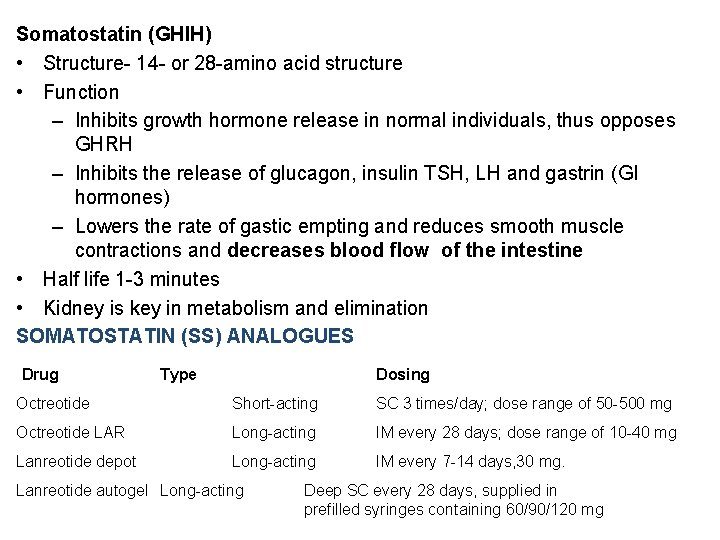
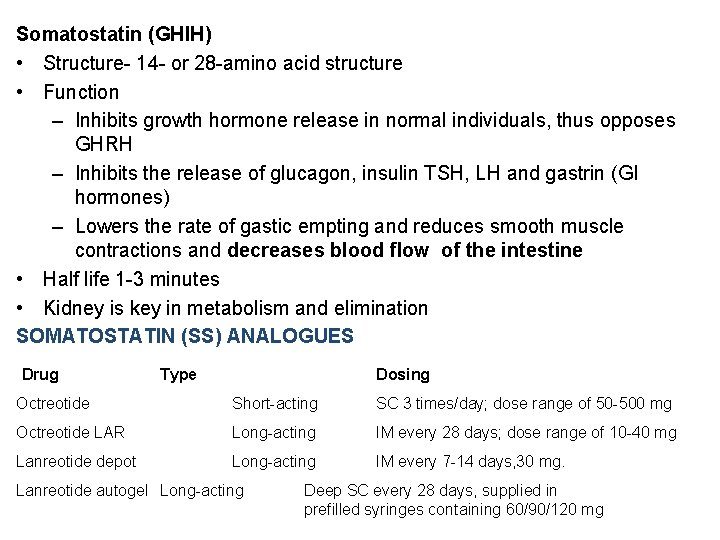
Somatostatin (GHIH) • Structure- 14 - or 28 -amino acid structure • Function – Inhibits growth hormone release in normal individuals, thus opposes GHRH – Inhibits the release of glucagon, insulin TSH, LH and gastrin (GI hormones) – Lowers the rate of gastic empting and reduces smooth muscle contractions and decreases blood flow of the intestine • Half life 1 -3 minutes • Kidney is key in metabolism and elimination SOMATOSTATIN (SS) ANALOGUES Drug Type Dosing Octreotide Short-acting SC 3 times/day; dose range of 50 -500 mg Octreotide LAR Long-acting IM every 28 days; dose range of 10 -40 mg Lanreotide depot Long-acting IM every 7 -14 days, 30 mg. Lanreotide autogel Long-acting Deep SC every 28 days, supplied in prefilled syringes containing 60/90/120 mg
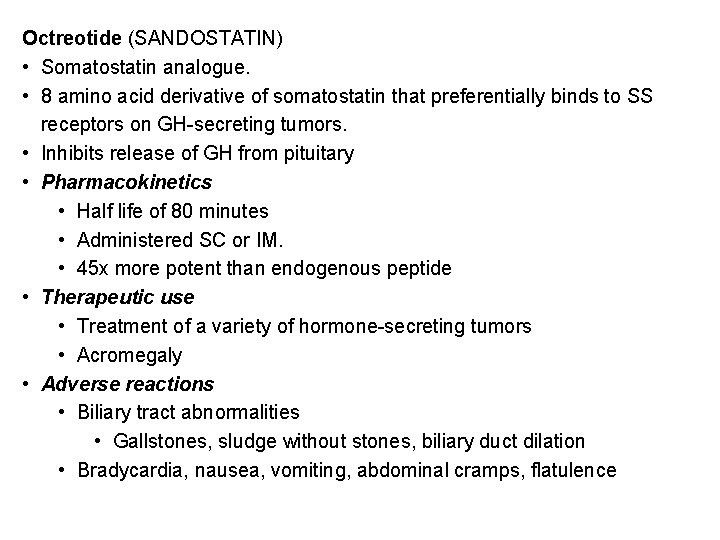
Octreotide (SANDOSTATIN) • Somatostatin analogue. • 8 amino acid derivative of somatostatin that preferentially binds to SS receptors on GH-secreting tumors. • Inhibits release of GH from pituitary • Pharmacokinetics • Half life of 80 minutes • Administered SC or IM. • 45 x more potent than endogenous peptide • Therapeutic use • Treatment of a variety of hormone-secreting tumors • Acromegaly • Adverse reactions • Biliary tract abnormalities • Gallstones, sludge without stones, biliary duct dilation • Bradycardia, nausea, vomiting, abdominal cramps, flatulence
• Induces lipolysis in adipose tissue and growth in skeletal muscle – Binding to its receptor (direct) • Adipose tissue stimulated to break down triglyceride and stops the uptake of circulating lipids – Insulin-like growth factor-1 (indirect) • Stimulates the liver to release IGF-1 target tissues>produces growth at open epiphyses • Lanreotide (SOMATULINE-LA) slow release, long-acting octapeptide causes • prolonged GH suppression. Most effective for patients with nonpituitary tumours
Growth Hormone (GH): • Structure: It is a single polypeptide chain composed of 191 amino acid residues. It has two disulfide bonds. • Secretion: Somatotropes of the Anterior Pituitary. • Level: High in children Maximal during adolescence Lowest during adulthood. • Measurments: During 24 hours After stimulation • Regulation: Stimulation: By Growth Hormone Releasing Hormone (GHRH). Inhibition: By Somatostatin. • Direct Effects: 1 - Stimulation of Lipolyses (Hydrolyses of Triglycerides). 2 - Stimulation of Hepatic glucose output. 3 - Production of Insulin-like growth factors (IGF’s, Somatomedins) • Indirect Effects: Mediated by IGF-1: 1 - Increase cell numbers. 2 - Positive Nitrogen balance. 3 - Increase Protein synthesis.
Disease Conditions Related to GH: • Deficiency: * Dwarfism. • Excessive Secretion: * Giantism: Due to tumor in somatotrpes in young children or adolescents. * Acromegaly: Rare disease (3/Million). Causes: 1 - Benign tumor of Pituitary gland (90%). 2 - Tumors of pancreas, lung or adrenal Symptoms: Enlargements of extremities. • Uses of Growth Hormone: * Replacement therapy for children with GH deficiency. * Administered by intramuscular or subcutaneous. • Sources: * Recombinant DNA technology.
Treatment of GH insufficiency (all SC or IM) : GH SUPPLEMENTATION Somatropins GH preparations whose sequence matches native h. GH. Somatrem: GH derivative with an additional methionine at the amino terminus. For Children • To mimic the normal pattern of secretion, they typically are administered to GH-deficient children in a dose of 40 mg/kg per day subcutaneously in the evening; • Higher daily doses (e. g. , 50 mg/kg) are employed for patients with Turner's syndrome, who have partial GH resistance. • In children with overt GH deficiency, measurements of serum IGF-1 levels are used to monitor initial response and compliance; long-term response is monitored by close evaluation of height For adults, the FDA recommends a starting dose of 3 to 4 mg/kg, given once daily by subcutaneous injection, with a maximum dose of 25 mg/kg in patients £ 35 years old and 12. 5 mg/kg in older patients.
Side Effects of GH Therapy: In children: • GH therapy is associated with remarkably few side effects. • Rarely, intracranial hypertension, visual changes, headache, nausea, and/or vomiting. • Leukemia has been reported in some children receiving GH therapy; and conditions associated with GH deficiency (e. g. , Down's syndrome, cranial irradiation for CNS tumors) probably explain the apparent increased incidence of leukemia. • An increased incidence of type 2 diabetes mellitus has been reported. In adults • Side effects associated with the initiation of GH therapy include Peripheral edema, carpal tunnel syndrome, arthralgia, and myalgia. • These symptoms, which occur most frequently in patients who are older or more obese, generally respond to a decrease in dose.
IGF-1 THERAPY For Pts with GH Receptor mutation Mecasermin: complex of recombinant human IGF-1 (rh. IGF-1) and recombinant human insulin-like growth factor-binding protein-3 (rh. IGFBP-3). Clinical response is monitored Serum IGF-1 levels. Treatment of Acromegaly: Trans-sphenoidal surgery to remove tumor. Radiation therapy usually follow the surgery. Drug Therapy: 1 - Dopaminergic Agonists: Bromocriptine 2 - Synthetic Somatostatin analogs: Octeroide (Sandostatin).
Growth Hormone Receptor Antagonist: • Binds to GH receptors, blocks GH-stimulated, hepatic production of IGF-1 • Pegvisomant {Somavert} • Injection, SC. • Treatment of – Acromegaly • Increased growth hormone in adults • Adverse reactions – Pain/redness/itching at the injection site, diarrhea, or nausea may occur. – Liver toxicity, yellowing of the skin, abdominal pain, dark urine, vomiting – Allergic reactions • CI – Liver disease
Prolactin: • 198 amino acid peptide with three disulfide bonds • Lactation • Recombinant agents not available • Hypothalamic dopamine inhibits the secretion and release of prolactin. • Major function of prolactin is milk production – oxytocin stimulates ejection • Release is tonically inhibited by PIH (dopamine) • Suckling response inhibits PIH release Other Physiological Roles of Prolactin: – important for reproduction - female – produced in uterine – endometrium during menstrual cycle – male – absence decreases fertility – involved in immune system – involved in T lymphocyte differentiation
Hyperprolactinemia • Galactorrhea • Amenorrhea • Male impotence • Associated with autoimmune diseases: multiple sclerosis, lupus Dopamine Agonists: • Decrease prolactin secretion through a dopamine-mimic action • Bromocriptine –D 2 receptor agonist, D 1 anta. • Pergolide • Cabergoline • Quinagolide –Non ergot dopamine agonist. Oral administration Treatment of Prolactin secreting adenomas Acromegaly Parkinson’s disease Adverse reactions Headache, light headedness, fatigue, Psychotic reactions
Glycoprotein hormones: Ø LH, FSH, TSH and h. CG Ø a and b subunits Ø Each subunit encoded by different gene Ø a subunit is identical for all hormones Ø b subunit are unique and provide biological specificity Gonadotropin-Releasing Hormone – Pulsatile Gn. RH secretion stimulates the gonadotroph cells in the anterior pituitary to produce and release LH & FSH • Sustained non-pulsatile administration inhibits the release of FSH and LH by the pituitary in both males and females
Gonadorelin {Factrel}: • Synthetic Gn. RH - Small peptide • Diagnostic purpose only • Portable pump system - Male and female infertility • Administered SC and IV Gn. RH Analogs: • Synthesized by selective substitution of amino acids • Leuprolide {Eligrad} – Highly effective at decreasing estrogen levels – Given IM/SC. • Nafarelin {Synrel} – Nasal spray • Goserelin {Zoladex} – Implantable cylinders Histrelin, Triptorelin.
• Treatment of – Endometriosis and Uterine fibroids – Breast cancer – Prostate cancer – Central precocious puberty – Male and female infertility • Adverse reactions – Hot flashes, acne, depression, vaginal bleeding – Tachycardia, lightheadedness, ED • Gn. RH Antagonist • Binds to pituitary Gn. RH receptors without activation – Blocks secretion and release of LH and at high doses FSH – Immediate suppression of LH • Ganirelix {Antagon} • Cetrorelix {Cetrotide}
• Treatment of – In vitro fertilization – Endometriosis and uterine fibroids • Advantage – Decrease risk of LH surge • Injectables SC. • Adverse reactions – Nausea – HRs. – Vaginal bleeding Follicle Stimulating Hormone: • Glycoprotein hormone consisting of two chains • Produced by gonadotroph cells in the anterior pituitary • Stimulates gametogenesis and follicular development in women and spermatogenesis in males • Stimulates androgen conversion into estrogen
Menotropin {Humegon}: • Commercially available since 1960 s • human Menopausal Gonadotropins (h. MG) – Purified from urine of post-menopausal females • Combination of FSH and LH • MENOPAUSE happens when no follicles remain in the ovaries – ESTROGEN and PROGESTERONE are no longer made, thus leading to high levels of circulating FSH and LH Urofollitropin {Bravelle} • Purified FSH • Derived from post-menopausal females Follitropin Beta {Follistim} • 1996, recombinant technology • Batch to batch consistency, and highly pure • Cost 3 x as much as h. MG • Injectables, SC. • Treatment: Anovulatory females; Pituitary and hypothalamic hypogonadism with infertility
• Adverse reactions – Abdominal pain, vaginal bleeding, ovarian cysts – Injection site pain, rash • Risk of multiple births Luteinizing Hormone • Glycoprotein consisting of two chains • Regulation of gonadal steroid production • No LH clinically available • human Chorionic Gonadotropin (h. CG) – IM injection – Half life of 8 hours Human Chorionic Gonadotropin (h. CG): • Diagnostic use • Treatment of infertility – Induce ovulation • Adverse reactions – Headache – Depression
ACTH is made up of 39 amino acids Ø Regulates adrenal cortex and synthesis of adrenocorticosteroids Ø a-MSH resides in first 13 AA of ACTH Ø a-MSH stimulates melanocytes and can darken skin Ø Overproduction of ACTH may accompany increased pigmentation due to a-MSH. Regulation of ACTH: • Stimulation of release – CRH and ADH – Stress – Hypoglycemia • CRH and ADH both synthesized in hypothalamus – ADH is released by posertior pituitary and reaches anterior pituitary via inferior hypophyseal artery.
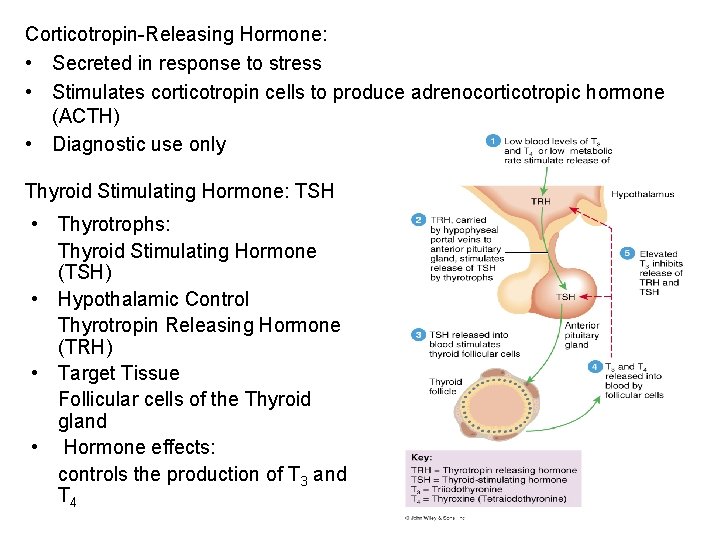
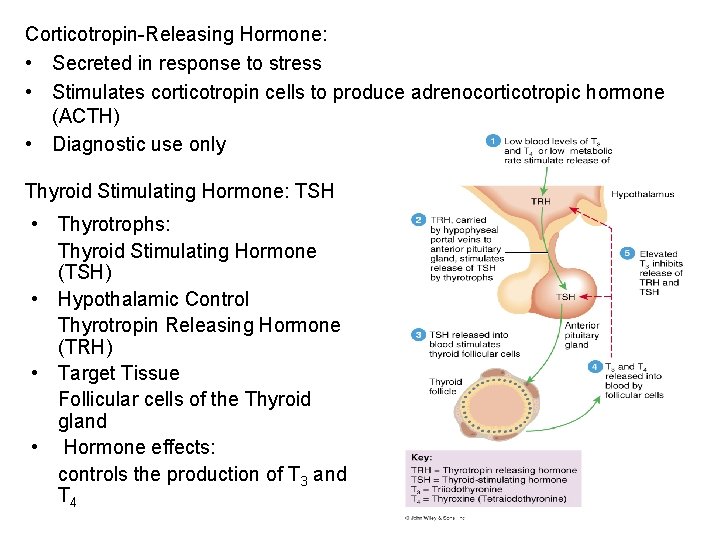
Corticotropin-Releasing Hormone: • Secreted in response to stress • Stimulates corticotropin cells to produce adrenocorticotropic hormone (ACTH) • Diagnostic use only Thyroid Stimulating Hormone: TSH • Thyrotrophs: Thyroid Stimulating Hormone (TSH) • Hypothalamic Control Thyrotropin Releasing Hormone (TRH) • Target Tissue Follicular cells of the Thyroid gland • Hormone effects: controls the production of T 3 and T 4
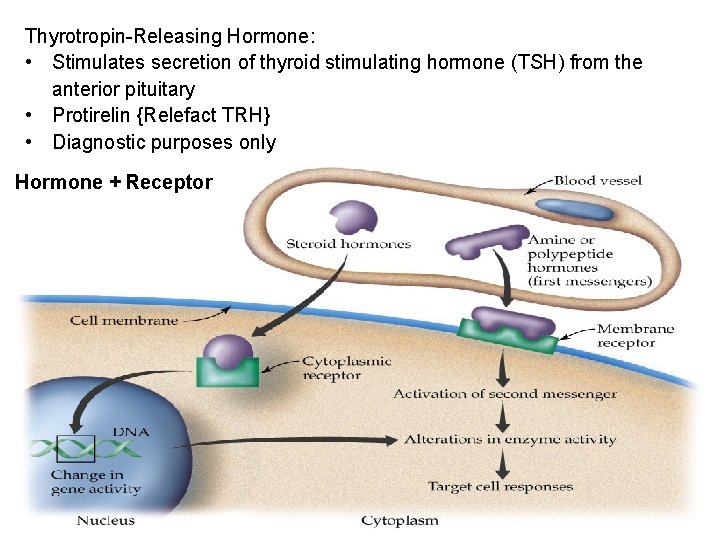
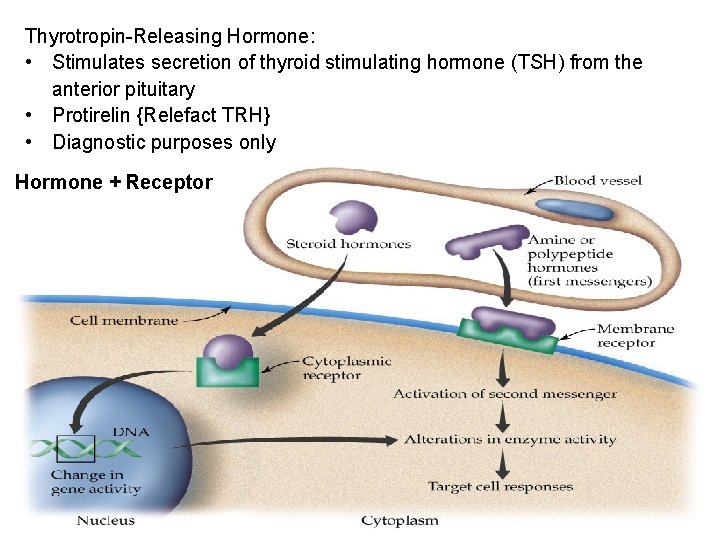
Thyrotropin-Releasing Hormone: • Stimulates secretion of thyroid stimulating hormone (TSH) from the anterior pituitary • Protirelin {Relefact TRH} • Diagnostic purposes only Hormone + Receptor
 Hypothalamohypophyseal
Hypothalamohypophyseal Vasopresine
Vasopresine Hypothalamic hormones
Hypothalamic hormones What are the tropic hormones
What are the tropic hormones Hypophysis
Hypophysis Anterior pituitary hormones
Anterior pituitary hormones Pituitary gland hormones
Pituitary gland hormones Pituitary hormones and their targets
Pituitary hormones and their targets Neurotransimitters
Neurotransimitters Mechanisms of hypothalamic control over endocrine function
Mechanisms of hypothalamic control over endocrine function Female reproductive system conclusion
Female reproductive system conclusion Cips dcvg
Cips dcvg Cips undp
Cips undp Sonji clarke
Sonji clarke Cips procurement process
Cips procurement process Cips dubai
Cips dubai Cips code of ethics and professional conduct
Cips code of ethics and professional conduct Pmms consulting
Pmms consulting Mini cips
Mini cips Co-destiny relationship
Co-destiny relationship Cips challenge
Cips challenge Finance dept structure
Finance dept structure Dept ind onegov
Dept ind onegov Pt dept logistik
Pt dept logistik Micah ennis
Micah ennis La city fire interview
La city fire interview Ms department of finance and administration
Ms department of finance and administration Hjdkdkd
Hjdkdkd Rewley house continuing education library
Rewley house continuing education library Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Horizontal
Horizontal Worcester ma building department
Worcester ma building department Albany county dept of social services
Albany county dept of social services