Pituitary Gland Disorders Pituitary Gland The pituitary is


- Slides: 80
Pituitary Gland Disorders
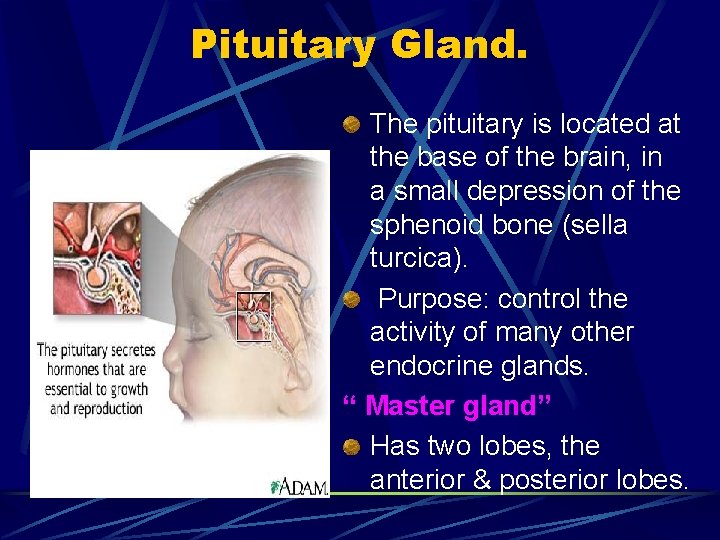
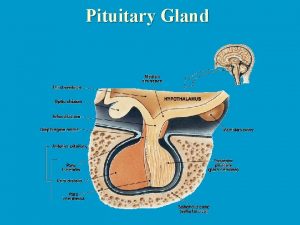
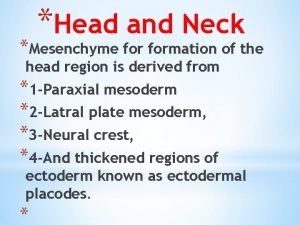
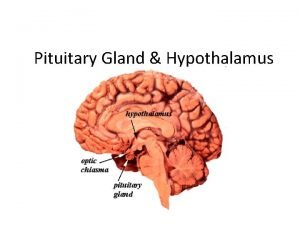
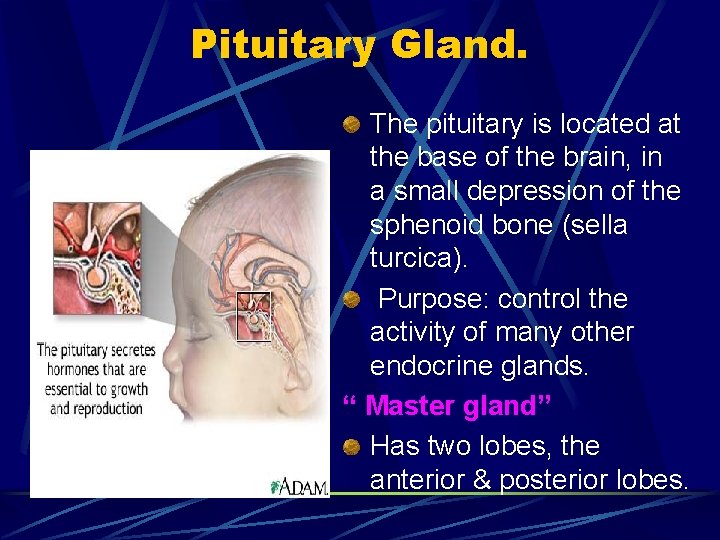
Pituitary Gland. The pituitary is located at the base of the brain, in a small depression of the sphenoid bone (sella turcica). Purpose: control the activity of many other endocrine glands. “ Master gland” Has two lobes, the anterior & posterior lobes.
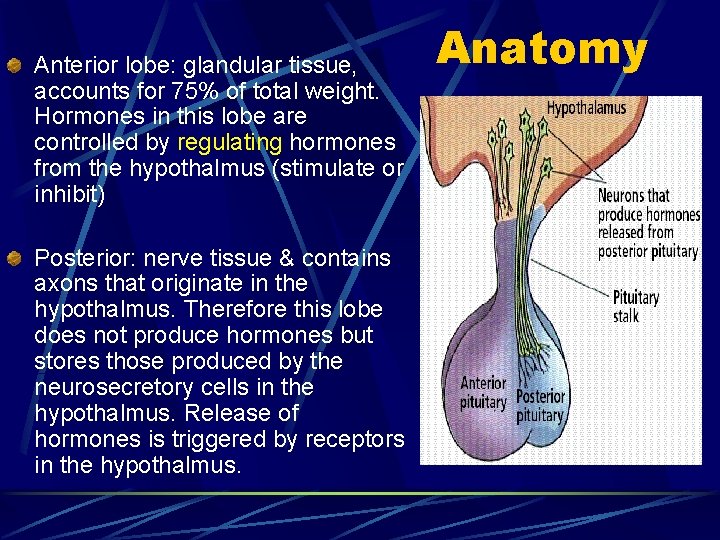
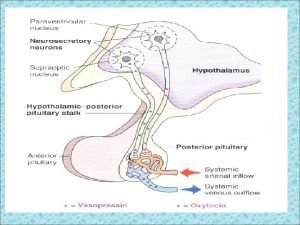
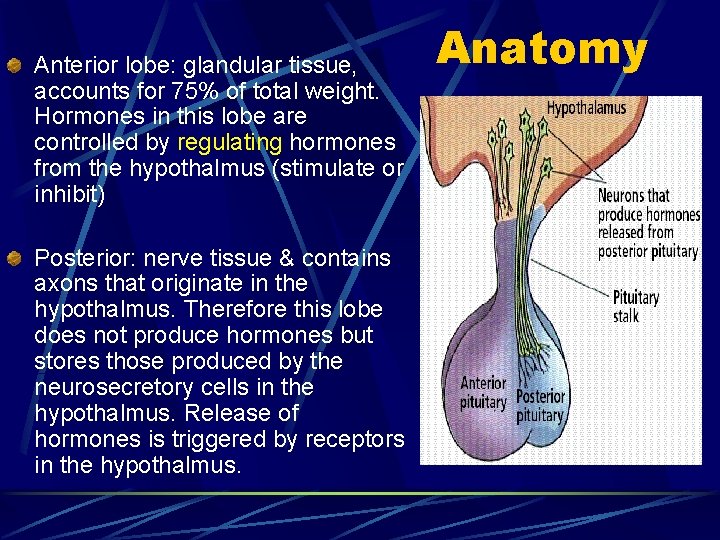
Anterior lobe: glandular tissue, accounts for 75% of total weight. Hormones in this lobe are controlled by regulating hormones from the hypothalmus (stimulate or inhibit) Posterior: nerve tissue & contains axons that originate in the hypothalmus. Therefore this lobe does not produce hormones but stores those produced by the neurosecretory cells in the hypothalmus. Release of hormones is triggered by receptors in the hypothalmus. Anatomy
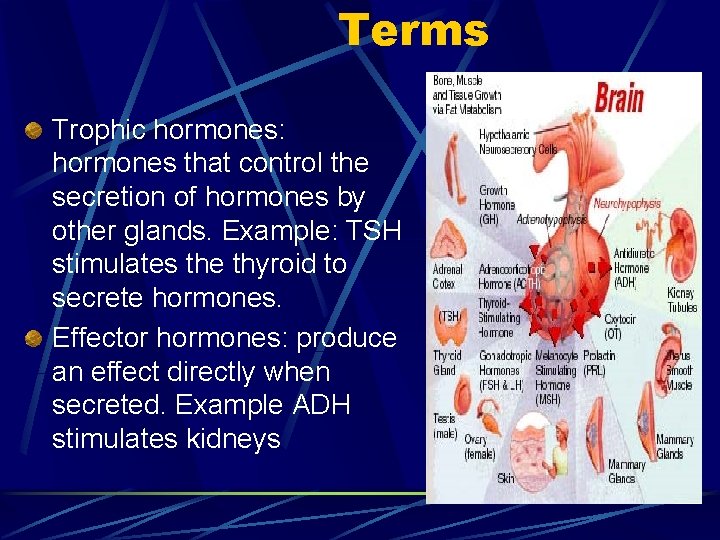
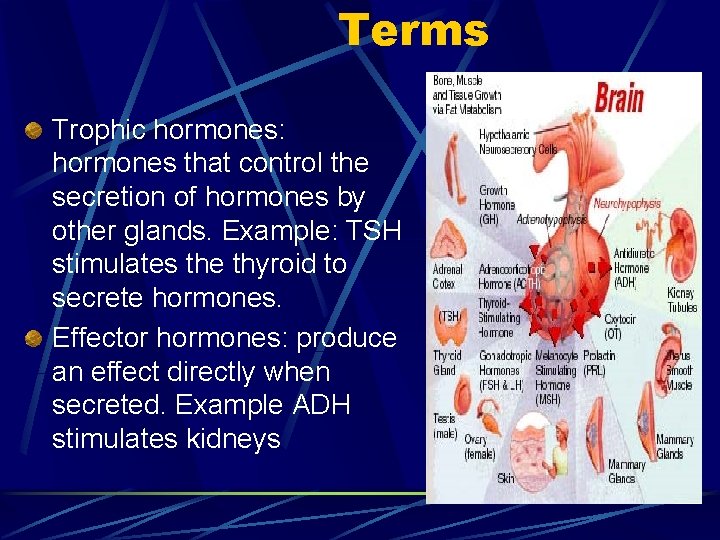
Terms Trophic hormones: hormones that control the secretion of hormones by other glands. Example: TSH stimulates the thyroid to secrete hormones. Effector hormones: produce an effect directly when secreted. Example ADH stimulates kidneys
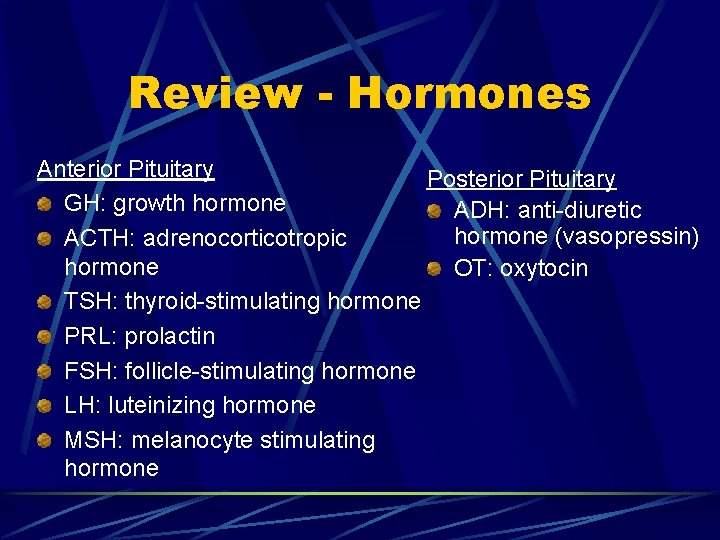
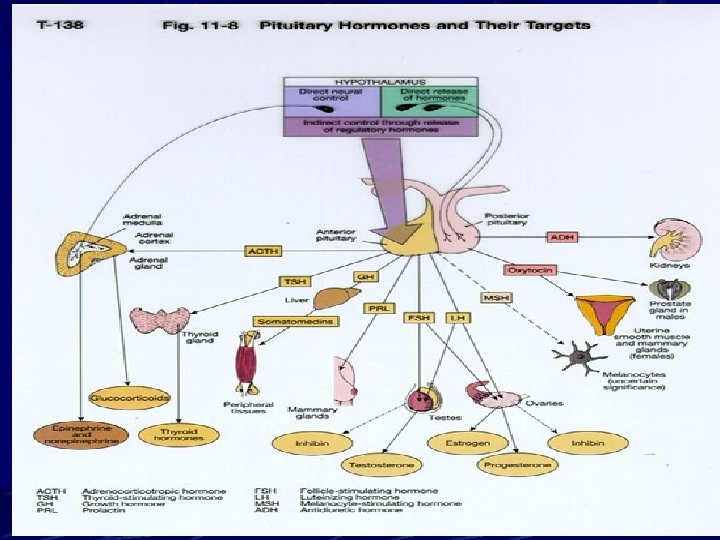
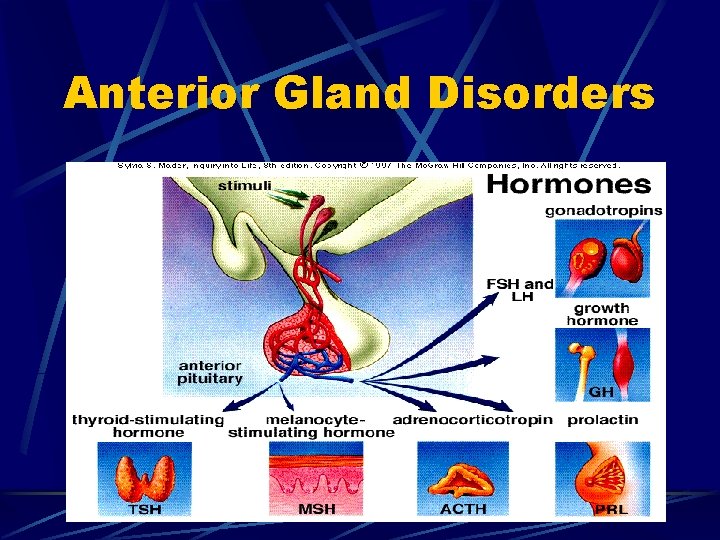
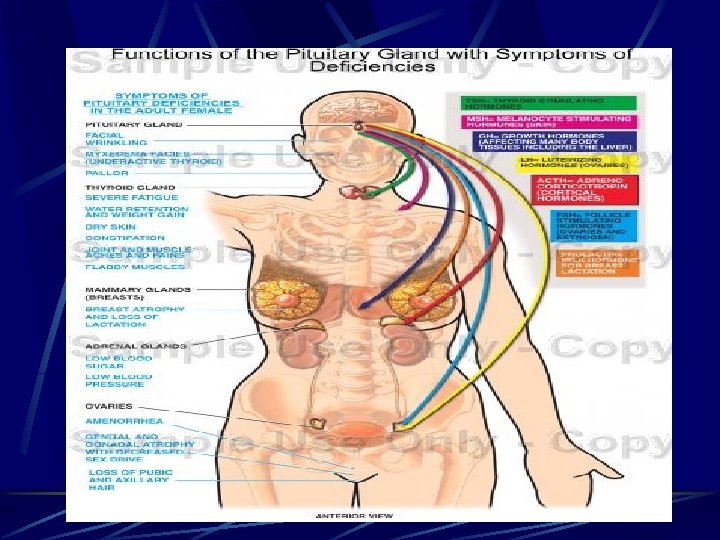
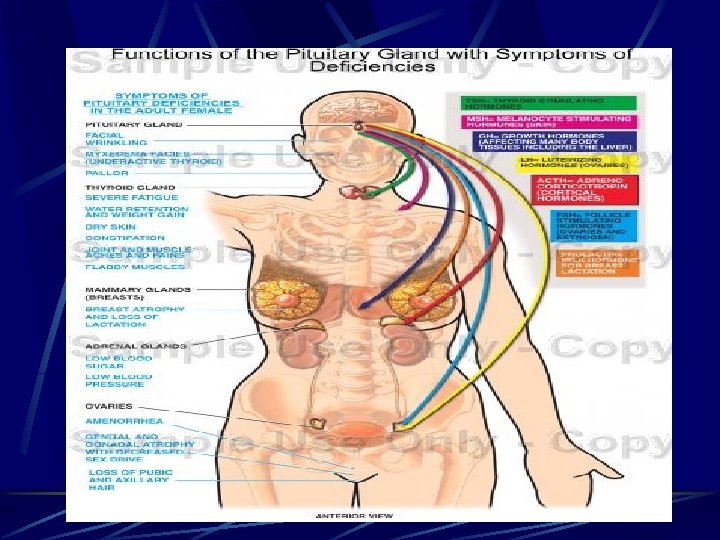
Review - Hormones Anterior Pituitary Posterior Pituitary GH: growth hormone ADH: anti-diuretic hormone (vasopressin) ACTH: adrenocorticotropic hormone OT: oxytocin TSH: thyroid-stimulating hormone PRL: prolactin FSH: follicle-stimulating hormone LH: luteinizing hormone MSH: melanocyte stimulating hormone
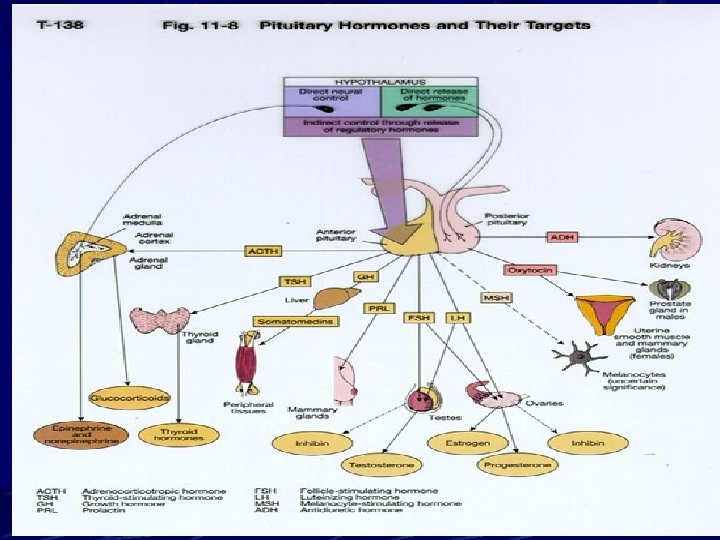
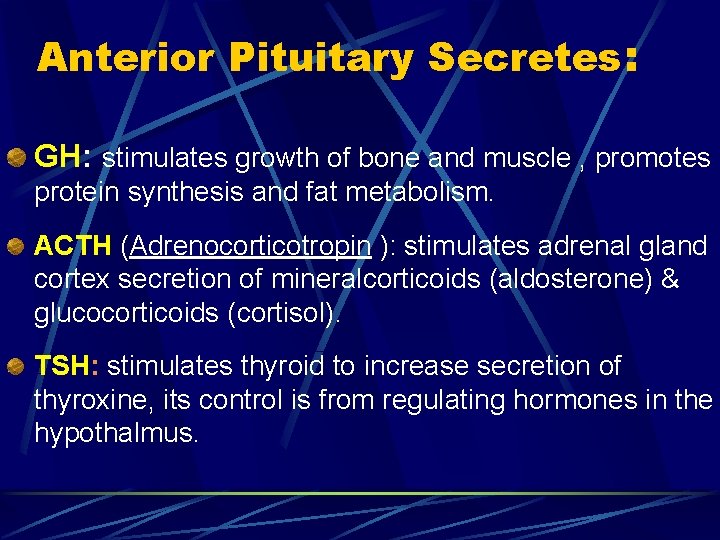
Anterior Pituitary Secretes: GH: stimulates growth of bone and muscle , promotes protein synthesis and fat metabolism. ACTH (Adrenocorticotropin ): stimulates adrenal gland cortex secretion of mineralcorticoids (aldosterone) & glucocorticoids (cortisol). TSH: stimulates thyroid to increase secretion of thyroxine, its control is from regulating hormones in the hypothalmus.
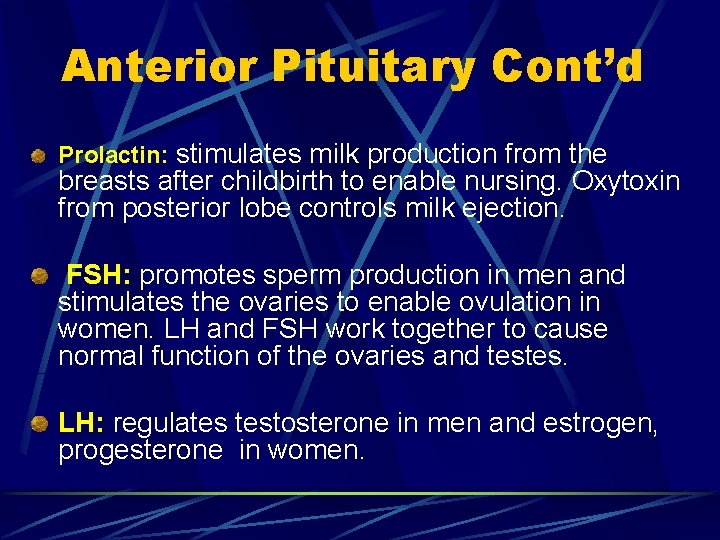
Anterior Pituitary Cont’d Prolactin: stimulates milk production from the breasts after childbirth to enable nursing. Oxytoxin from posterior lobe controls milk ejection. FSH: promotes sperm production in men and stimulates the ovaries to enable ovulation in women. LH and FSH work together to cause normal function of the ovaries and testes. LH: regulates testosterone in men and estrogen, progesterone in women.
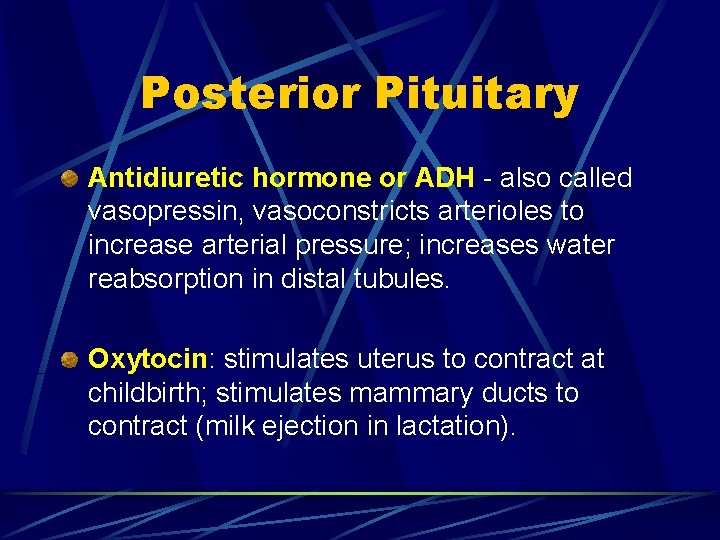
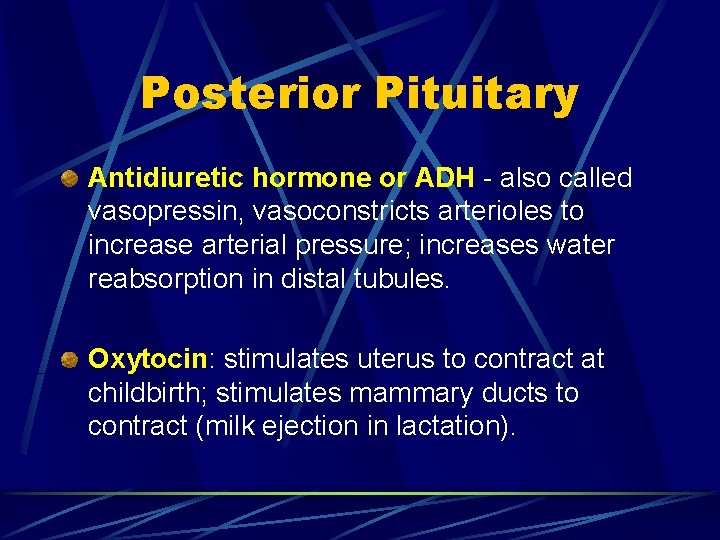
Posterior Pituitary Antidiuretic hormone or ADH - also called vasopressin, vasoconstricts arterioles to increase arterial pressure; increases water reabsorption in distal tubules. Oxytocin: stimulates uterus to contract at childbirth; stimulates mammary ducts to contract (milk ejection in lactation).
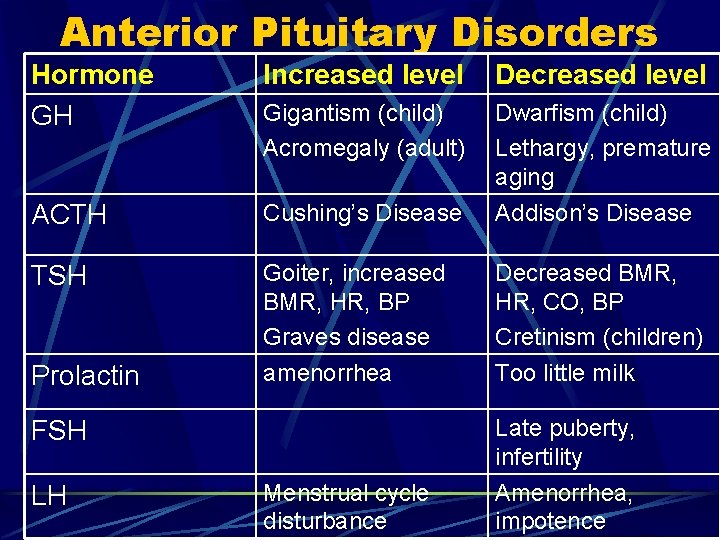
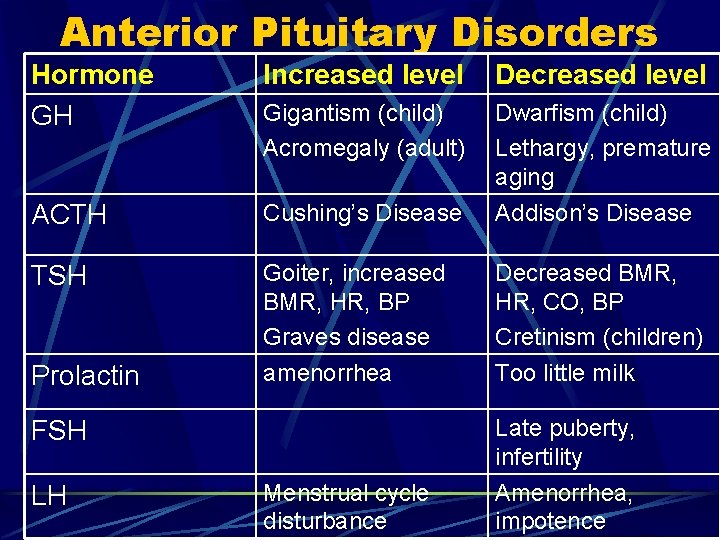
Anterior Pituitary Disorders Hormone GH Increased level Decreased level Gigantism (child) Acromegaly (adult) Dwarfism (child) Lethargy, premature aging ACTH Cushing’s Disease Addison’s Disease TSH Goiter, increased BMR, HR, BP Graves disease amenorrhea Decreased BMR, HR, CO, BP Cretinism (children) Too little milk Prolactin Late puberty, infertility FSH LH Menstrual cycle disturbance Amenorrhea, impotence
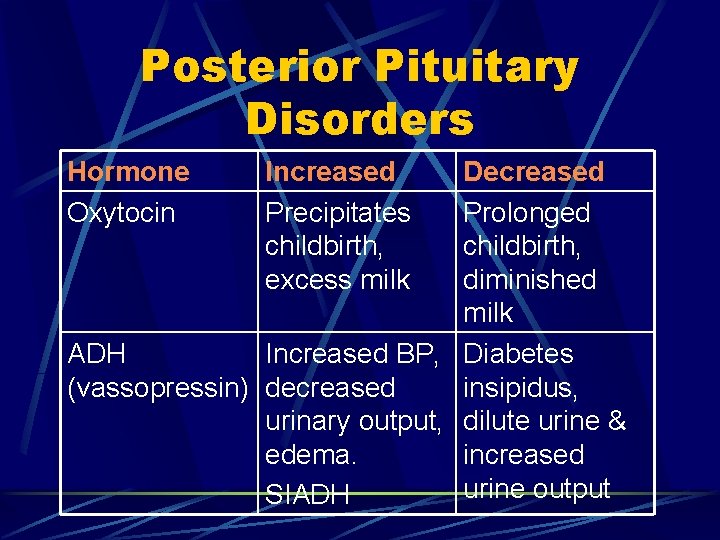
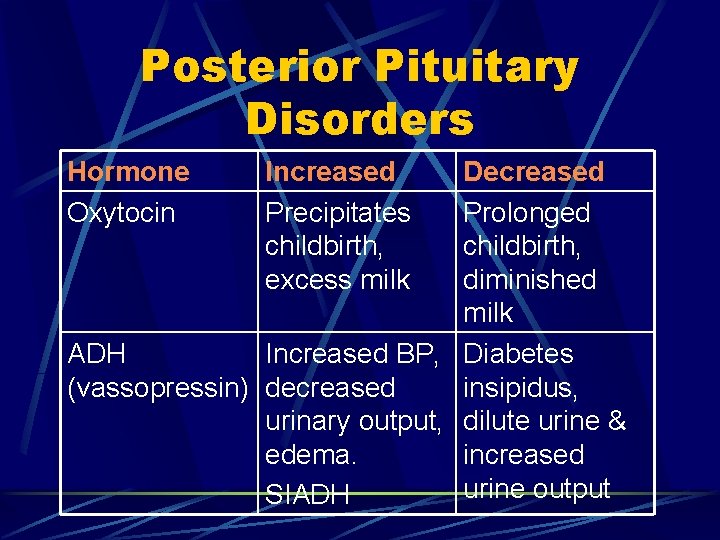
Posterior Pituitary Disorders Hormone Oxytocin Increased Precipitates childbirth, excess milk Decreased Prolonged childbirth, diminished milk ADH Increased BP, Diabetes (vassopressin) decreased insipidus, urinary output, dilute urine & edema. increased urine output SIADH
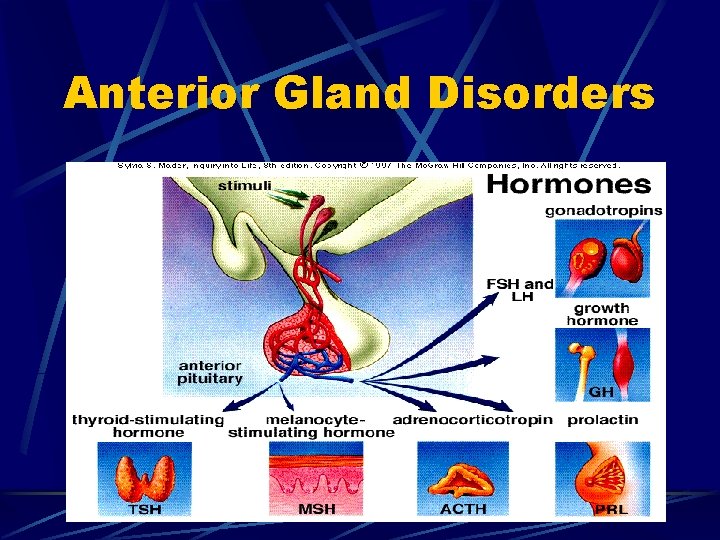
Anterior Gland Disorders
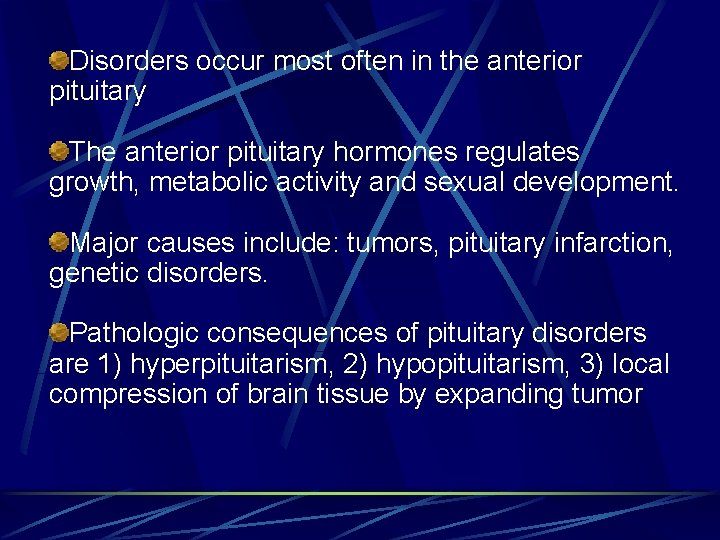
Disorders occur most often in the anterior pituitary The anterior pituitary hormones regulates growth, metabolic activity and sexual development. Major causes include: tumors, pituitary infarction, genetic disorders. Pathologic consequences of pituitary disorders are 1) hyperpituitarism, 2) hypopituitarism, 3) local compression of brain tissue by expanding tumor
Hyperpituitarism
Hyperfunction Results in excess production and secretion of one or more hormones such as GH, PRL, ACTH. Most common cause is a benign adenoma.
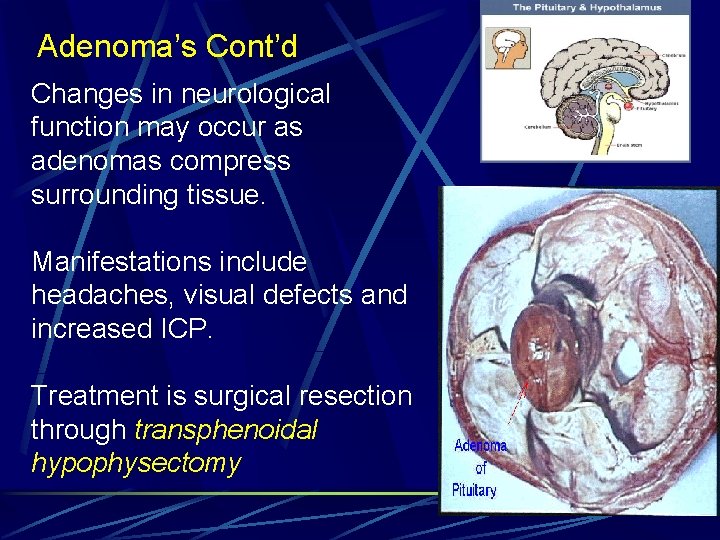
Pituitary Adenoma Anterior pituitary adenoma, a benign tumor which is classified according to size, degree of invasiveness and the hormone secreted. Prolactin and GH are the hormones most commonly over-produced by adenomas.
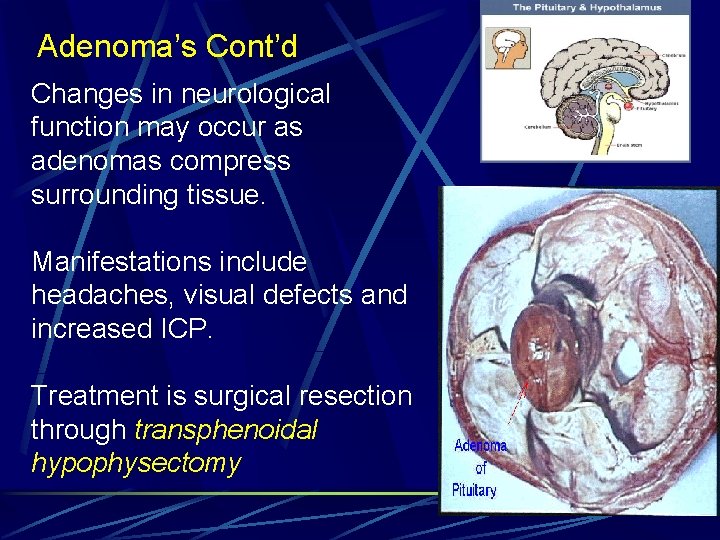
Adenoma’s Cont’d Changes in neurological function may occur as adenomas compress surrounding tissue. Manifestations include headaches, visual defects and increased ICP. Treatment is surgical resection through transphenoidal hypophysectomy
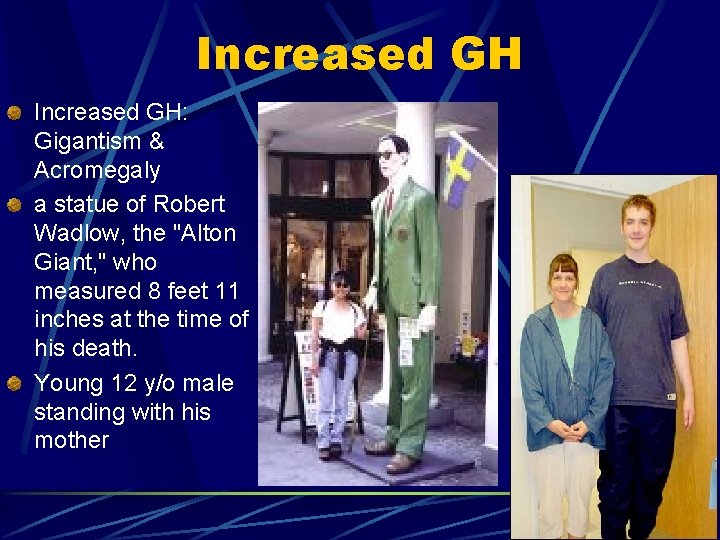
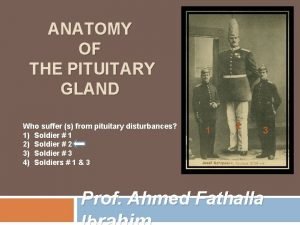
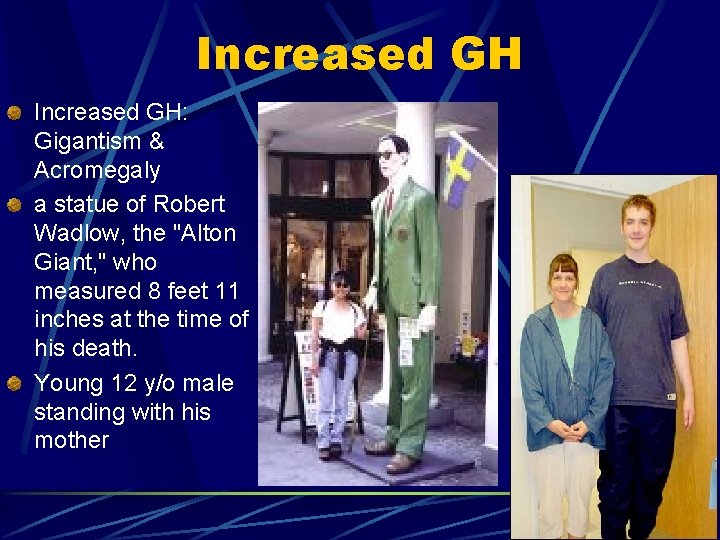
Increased GH: Gigantism & Acromegaly a statue of Robert Wadlow, the "Alton Giant, " who measured 8 feet 11 inches at the time of his death. Young 12 y/o male standing with his mother
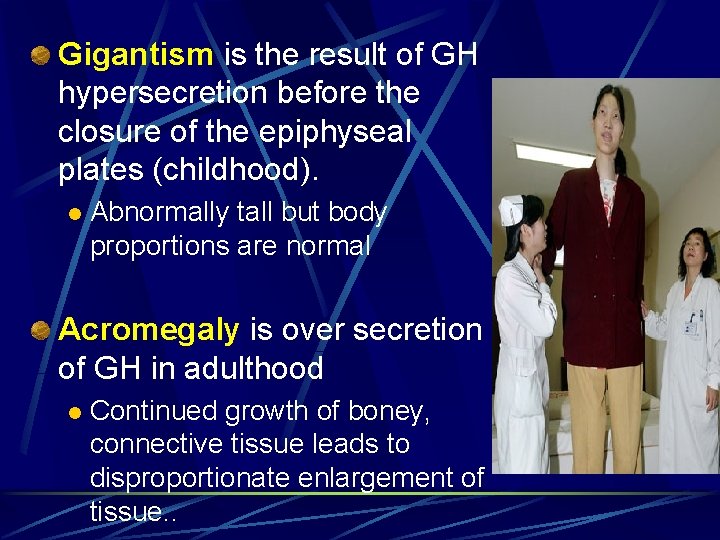
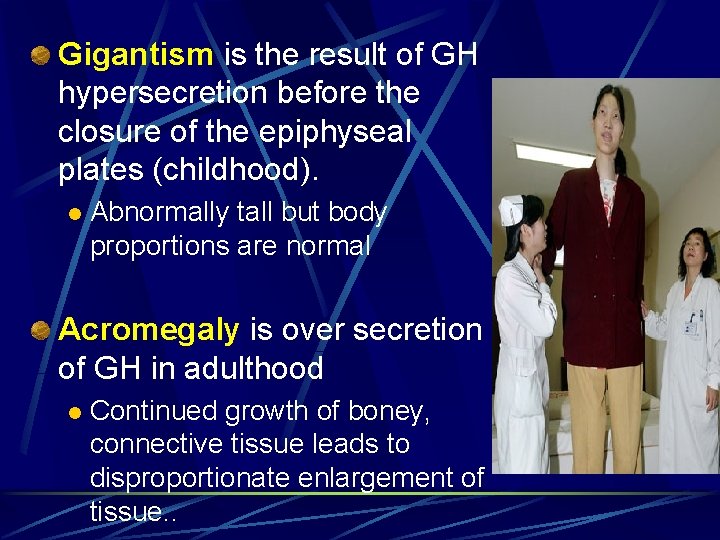
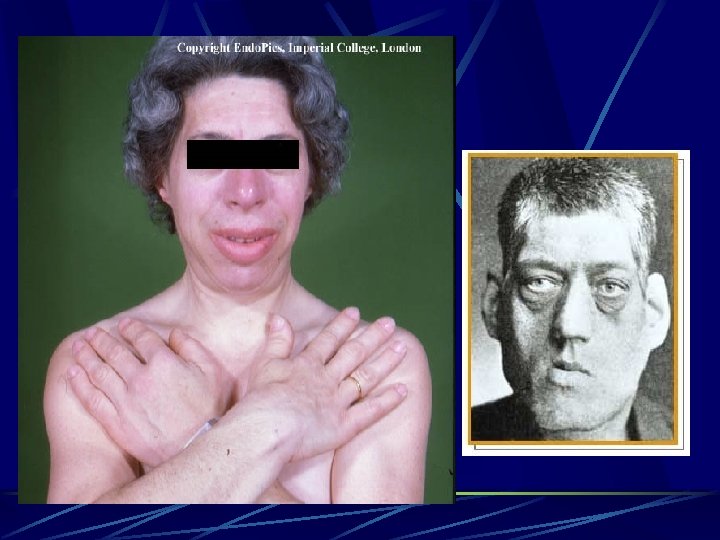
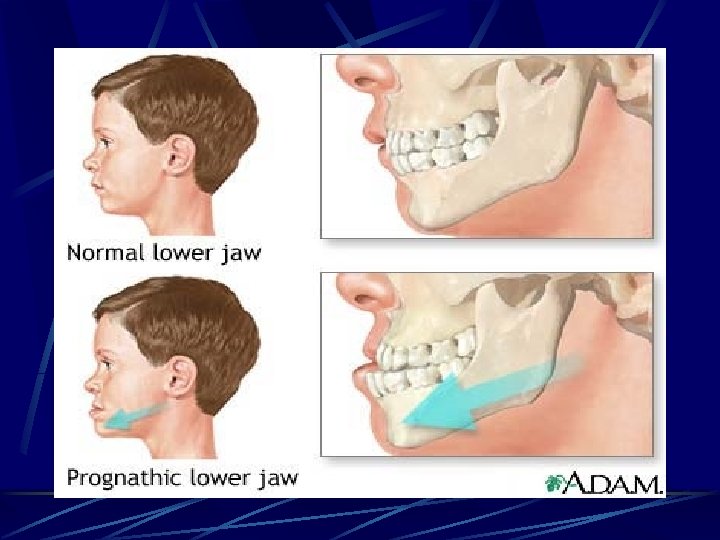
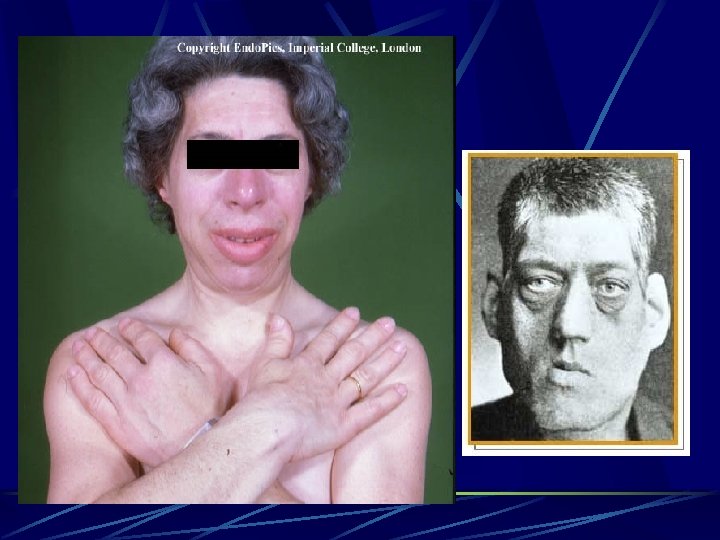
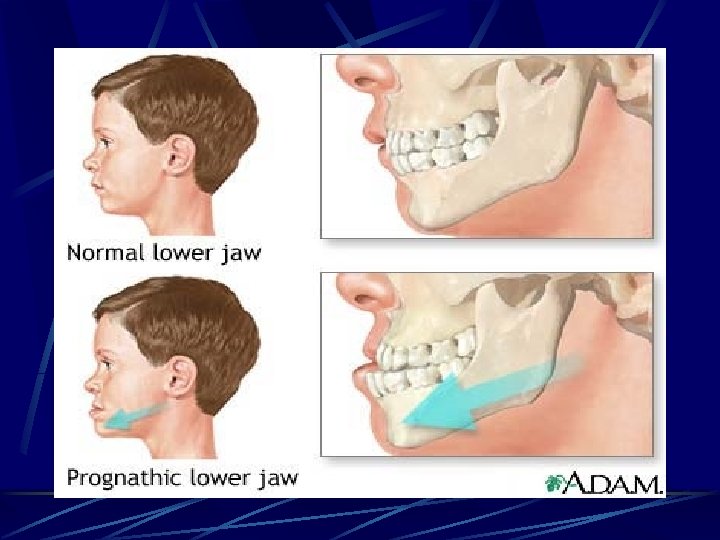
Gigantism is the result of GH hypersecretion before the closure of the epiphyseal plates (childhood). l Abnormally tall but body proportions are normal Acromegaly is over secretion of GH in adulthood l Continued growth of boney, connective tissue leads to disproportionate enlargement of tissue. .
Acromegaly Rare condition – develops between ages 30 -50 Symptoms: • Coarsening of facial features • Enlarged hands & feet • Carpel trunnel syndrome • Excessive sweating & oily skin • Headaches • Vision disturbance • Sleep apnea • General tiredness • Oligomenorrhea or amenorrhea • Impotence (adult males) • Decreased libido

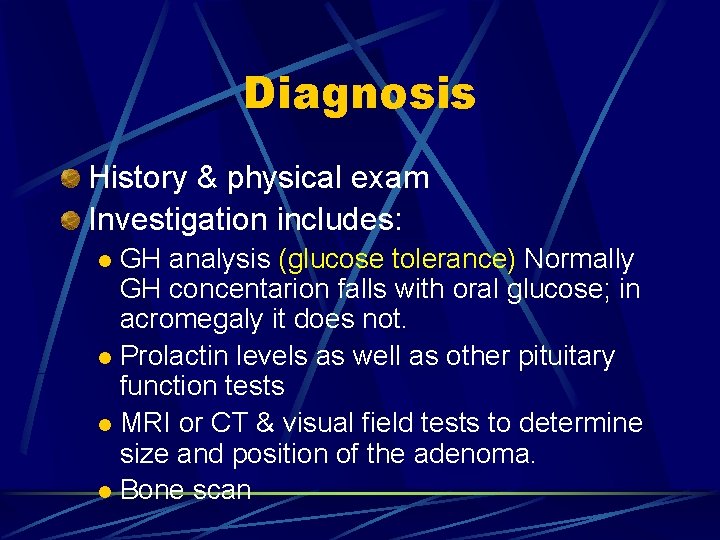
Diagnosis History & physical exam Investigation includes: GH analysis (glucose tolerance) Normally GH concentarion falls with oral glucose; in acromegaly it does not. l Prolactin levels as well as other pituitary function tests l MRI or CT & visual field tests to determine size and position of the adenoma. l Bone scan l
Treatment Surgery (primary choice) Radiotherapy Drug treatment – when surgery is not feasible Combinations of above
Drug treatment of Acromegaly Dopamine agonists: Dopamine agonists work on specialist markers (dopamine receptors) on the surface of the tumor to inhibit GH release from the tumour (Parlodel). Somatostatin: growth hormone receptor antagonist decreases the action of GH on target tissues. (octreocide acetate) Dopamine agonists are taken by mouth but in general are less effective than somatostatin analogues, which have to be injected.
Hypopituitarism
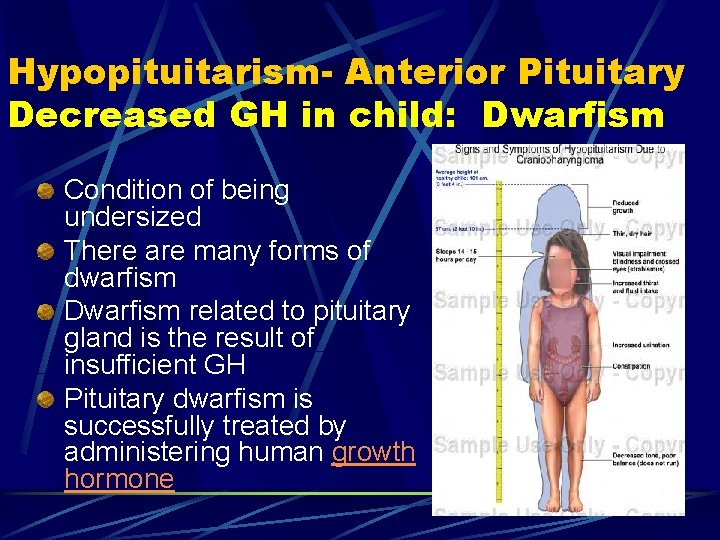
Hypopituitarism- Anterior Pituitary Decreased GH in child: Dwarfism Condition of being undersized There are many forms of dwarfism Dwarfism related to pituitary gland is the result of insufficient GH Pituitary dwarfism is successfully treated by administering human growth hormone
Hypopituitarism (Adult)- GH Lack of GH leads to: l Increased CV disease l Excessive tiredness l Anxiety l Depression l Reduced “quality of life” l Possible premature death
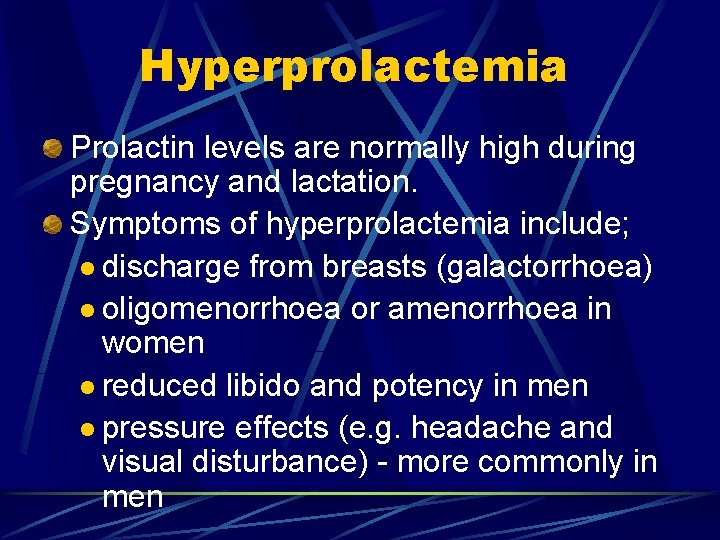
Hyperprolactemia Prolactin levels are normally high during pregnancy and lactation. Symptoms of hyperprolactemia include; l discharge from breasts (galactorrhoea) l oligomenorrhoea or amenorrhoea in women l reduced libido and potency in men l pressure effects (e. g. headache and visual disturbance) - more commonly in men
Treatment is surgery, radiation, or medical therapy with drugs that will suppress the production of prolactin l Urgent: deterioration in vision l Important: l successful RX. results in restoration of fertility l Patients may be predisposed to problems related to osteoporosis l Ask about erectile function & reassure client that it is part of the disease and can be treated.
Increased ACTH: Cushing’s Disease Cushing's is a disorder in which the adrenal glands are producing too much cortisol (hypercotisolism). If the source of the problem is the pituitary gland, then the correct name is Cushing's Disease whereas, if it originates anywhere else (adrenal tumors, long term steroid administration) then the correct name is Cushing's Syndrome. Cushing’s Disease is caused by pituitary hypersecretion of ACTH.
Etiology - Hypercortisolism Iatrogenic hypercortisolism resulting from medical intervention is most common cause of Cushing Syndrome. Pituitary hyper secretion and pituitary tumors account for 70% of Cushing’s Disease. Adrenal tumors account for 30%. Ectopic secretion of ACTH by tumors located outside the pituitary gland are rare cause of the syndrome and associated with increased morbidity/mortality (ie oat cell ca).
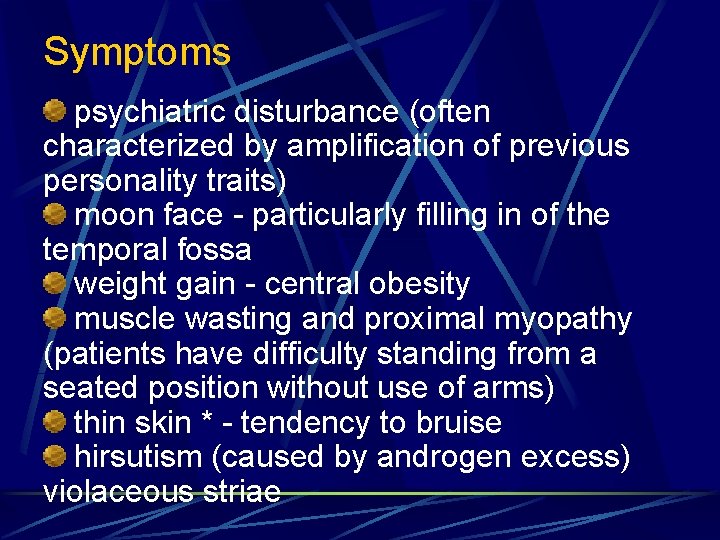
Symptoms psychiatric disturbance (often characterized by amplification of previous personality traits) moon face - particularly filling in of the temporal fossa weight gain - central obesity muscle wasting and proximal myopathy (patients have difficulty standing from a seated position without use of arms) thin skin * - tendency to bruise hirsutism (caused by androgen excess) violaceous striae
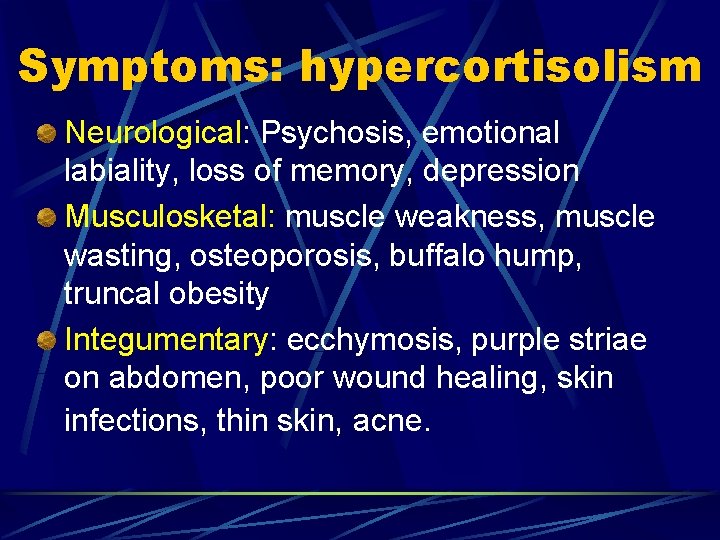
Symptoms: hypercortisolism Neurological: Psychosis, emotional labiality, loss of memory, depression Musculosketal: muscle weakness, muscle wasting, osteoporosis, buffalo hump, truncal obesity Integumentary: ecchymosis, purple striae on abdomen, poor wound healing, skin infections, thin skin, acne.
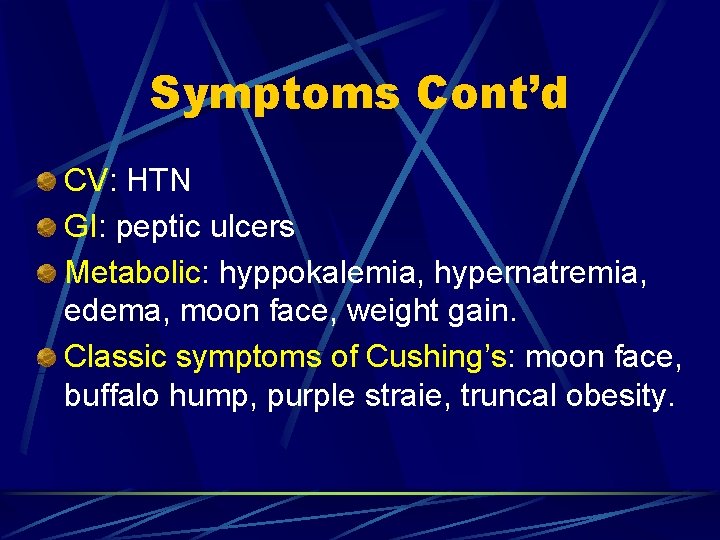
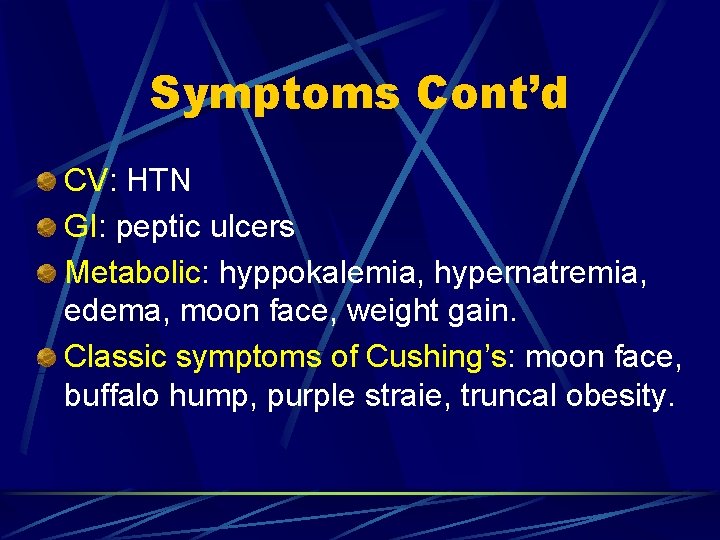
Symptoms Cont’d CV: HTN GI: peptic ulcers Metabolic: hyppokalemia, hypernatremia, edema, moon face, weight gain. Classic symptoms of Cushing’s: moon face, buffalo hump, purple straie, truncal obesity.
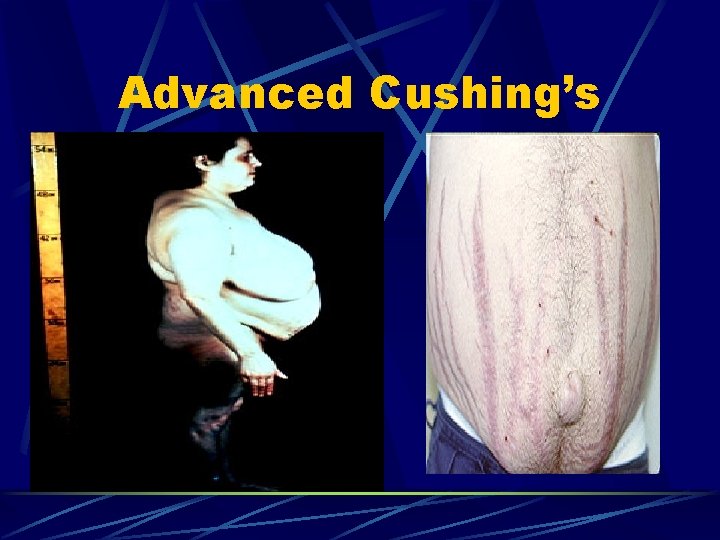
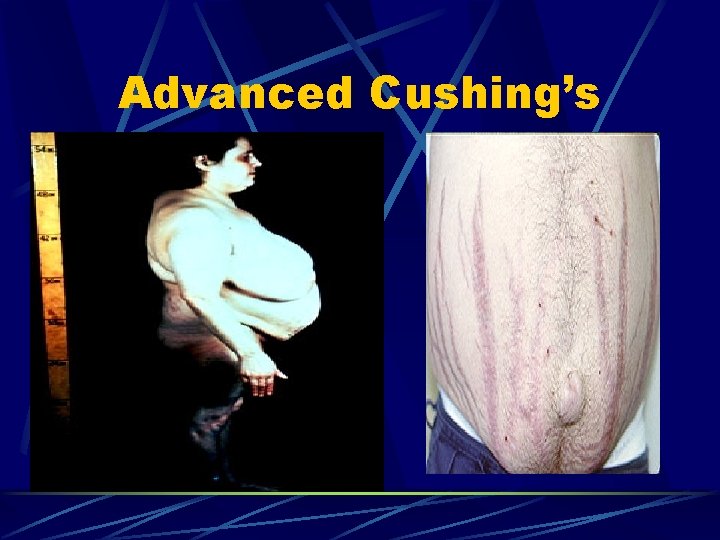
Advanced Cushing’s
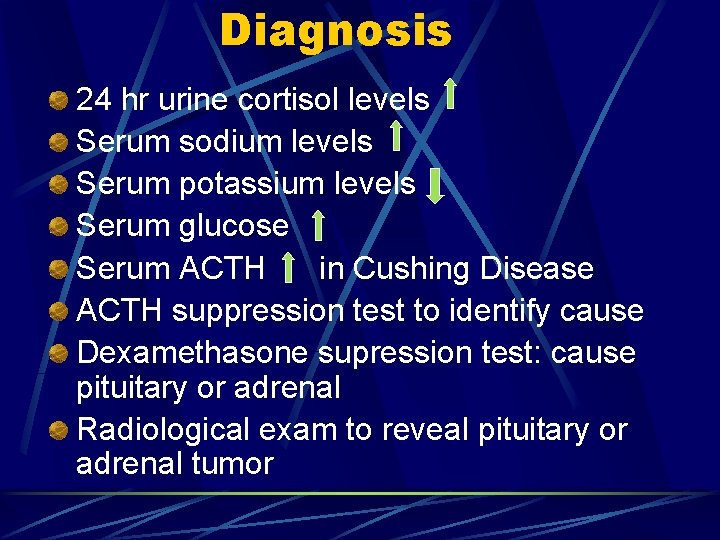
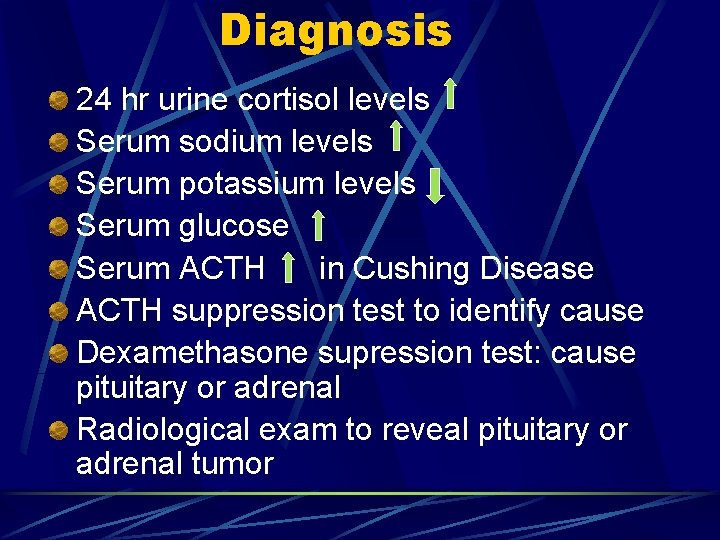
Diagnosis 24 hr urine cortisol levels Serum sodium levels Serum potassium levels Serum glucose Serum ACTH in Cushing Disease ACTH suppression test to identify cause Dexamethasone supression test: cause pituitary or adrenal Radiological exam to reveal pituitary or adrenal tumor
Treatment Transphenoidal surgery if the condition is due to a pituitary tumor Where surgery is contraindicated or fails to reduce cortisol levels, adrenalectomy and/or pituitary radiation may be necessary. Adrenocortical Inhibitors: (metapyrone, aminogluthimide) are only effective short-term. Diet: low calorie, carbohydrate & salt. High potassium.

Priority Nursing Diagnoses Fluid volume excess Risk for infection Risk for injury Activity intolerance Anxiety Knowledge deficit Risk for impaired tissue integrity
Teaching Diet Medications Medic alert bracelet Hormone levels and stress Signs of excessive or deficient adrenal hormones
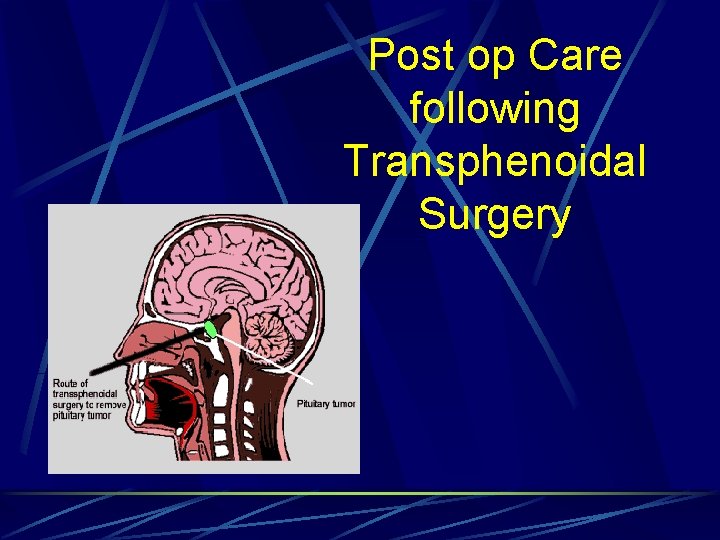
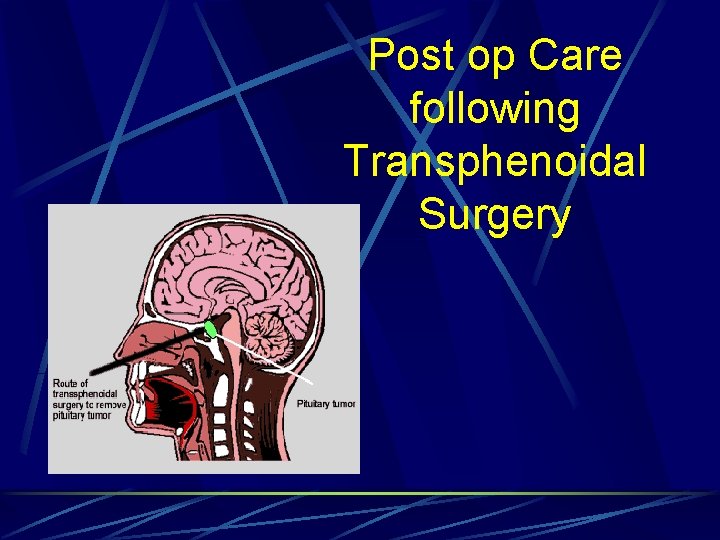
Post op Care following Transphenoidal Surgery
Post op care for cranial surgery (CSF leak, ICP etc. ) Hydrocortisone therapy, some on a longterm basis If surgery results in hypopituitarism, longterm hormone replacement therapy will be required Moods swings and depression may be a serious problem that may take months to treat
Hypopituitarism – Addison’s Disease To be covered under adrenal dysfunction
Posterior Pituitary Disorders
Deficiency or excess of ADH • Diabetes insipidus • SIADH
Posterior Lobe Disorders SIADH & diabetes insipidus are major disorders of the posterior pituitary……however Even if posterior lobe becomes damaged, hormonal deficiencies usually do not develop because……? ?
Hyper – Posterior Pituitary
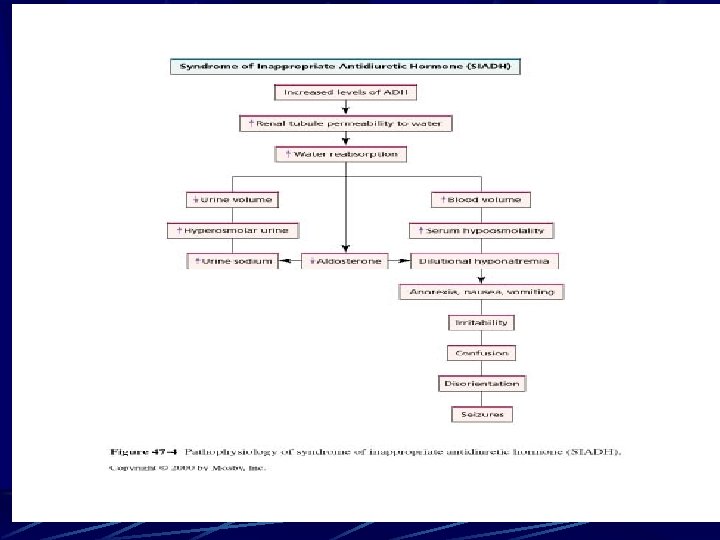
SIADH Syndrome of Inappropriate Anti-Diuretic Hormone Too much ADH produced or secreted. SIADH commonly results from malignancies, CHF, & CVA - resulting in damage to the hypothalamus or pituitary which causes failure of the feedback loop that regulates ADH. Client retains water causing dilutional hyponaetremia & decreased osmolality. Decreased serum osmolality cause water to move into cells
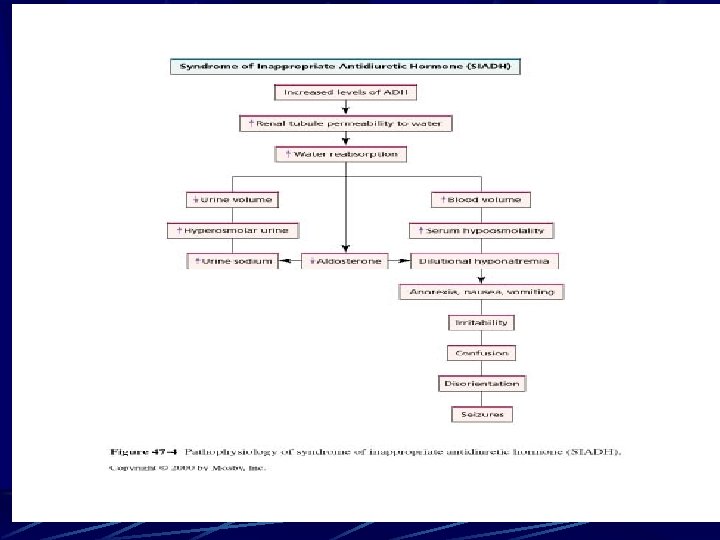
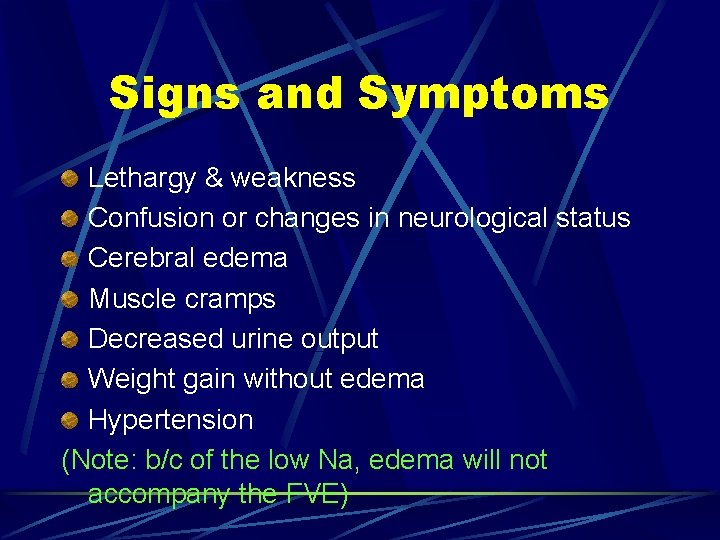
Signs and Symptoms Lethargy & weakness Confusion or changes in neurological status Cerebral edema Muscle cramps Decreased urine output Weight gain without edema Hypertension (Note: b/c of the low Na, edema will not accompany the FVE)
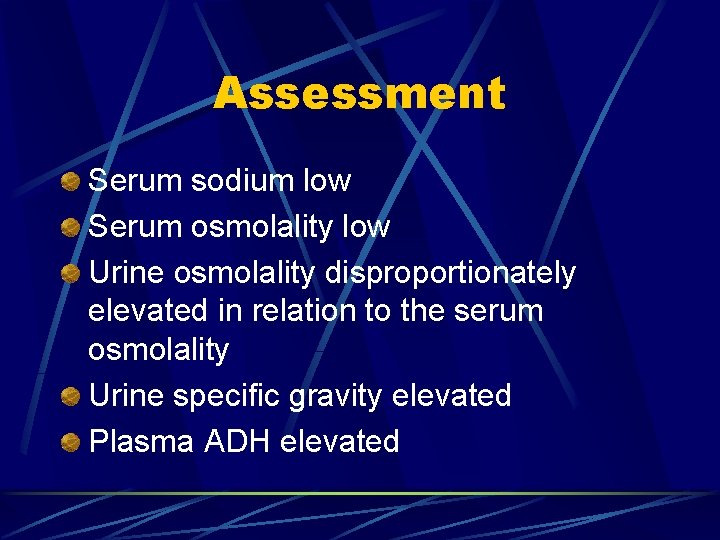
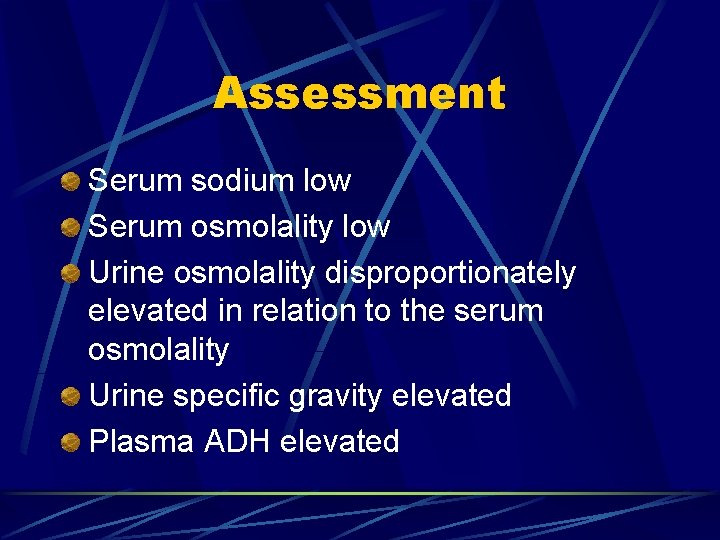
Assessment Serum sodium low Serum osmolality low Urine osmolality disproportionately elevated in relation to the serum osmolality Urine specific gravity elevated Plasma ADH elevated
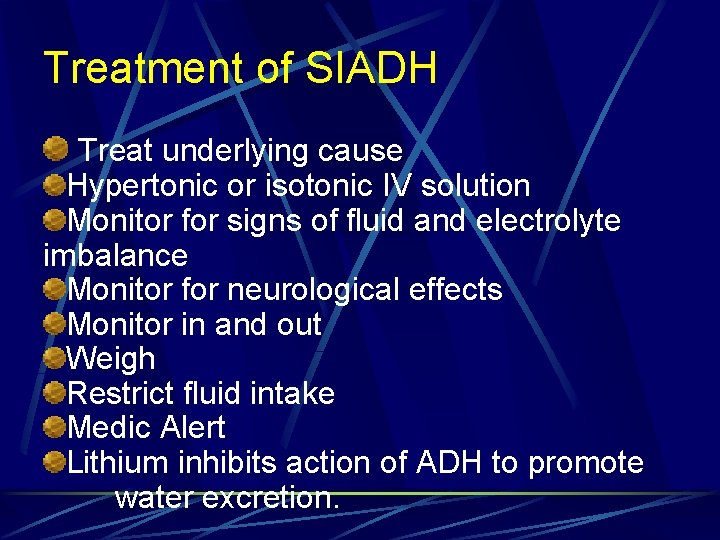
Treatment of SIADH Treat underlying cause Hypertonic or isotonic IV solution Monitor for signs of fluid and electrolyte imbalance Monitor for neurological effects Monitor in and out Weigh Restrict fluid intake Medic Alert Lithium inhibits action of ADH to promote water excretion.
Hypofunction – Posterior pituitary
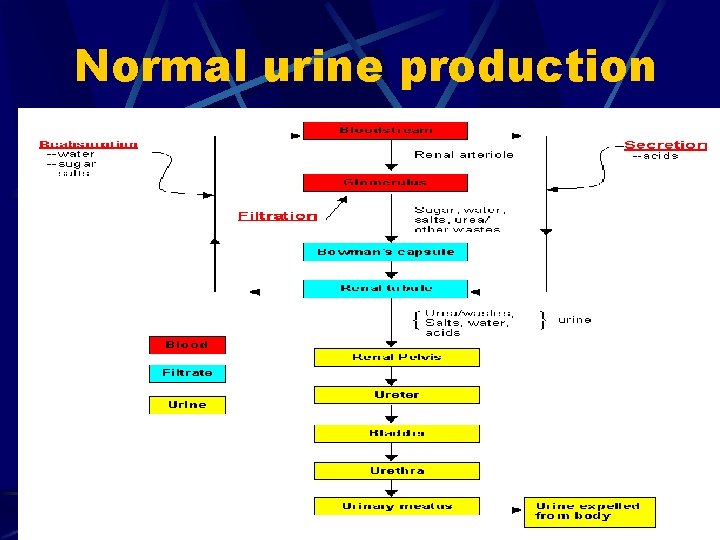
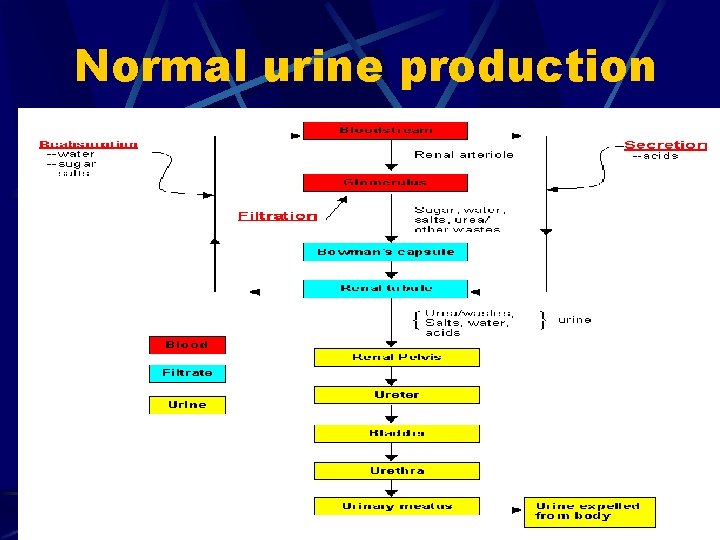
Normal urine production
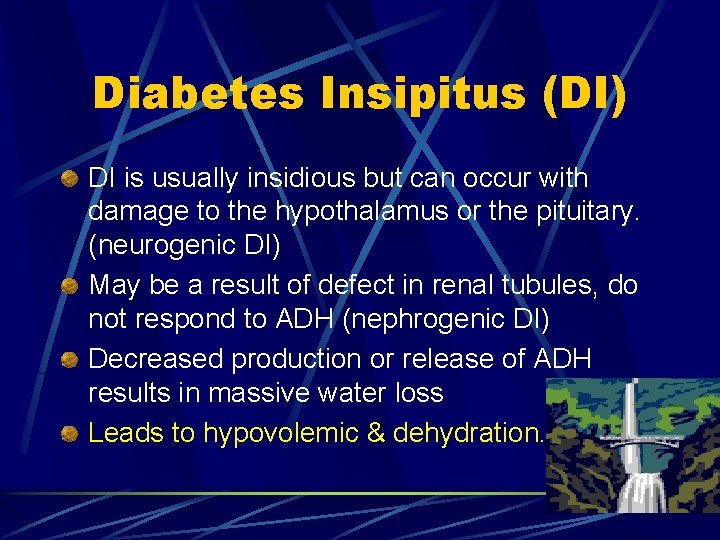
Diabetes Insipitus (DI) DI is usually insidious but can occur with damage to the hypothalamus or the pituitary. (neurogenic DI) May be a result of defect in renal tubules, do not respond to ADH (nephrogenic DI) Decreased production or release of ADH results in massive water loss Leads to hypovolemic & dehydration.
Clinical Manifestations Polyuria of more than 3 litres per 24 hours in adults (may be up to 20!) Urine specific gravity low Polydipsia (excessive drinking) Weight loss Dry skin & mucous membranes Possible hypovolemia, hypotension, electrolyte imbalance
Diagnostic Tests Serum sodium Urine specific gravity Serum osmolality Urine osmolality Serum ADH levels Vasopressin test and water deprivation test: increased hyperosmolality is diagnostic for DI.
Management Medical management includes Rehydration IV fluids (hypotonic) Symptom management ADH replacement (vasopressin) For nephrogenic DI: thiazide diuretics, mild salt depletion, prostaglandin inhibitors (i. e. ibuprophen)
Nursing 1. Monitor for signs of fluid and electrolyte imbalance 2. Monitor in and out 3. Daily weight 4. Monitor for excessive thirst or output 5. Assess serum and urine values (decreased SG, decreased urine osmolality, high serum osmolality are early indicators
POSSIBLE NURSING DIAGNOSIS Fluid Volume Deficit Risk for Injury r/t altered LOC Risk for Altered Health Maintenance Sleep Pattern Disturbance r/t urinary frequency or anxiety Altered Urinary Elimination r/t excess urinary output Body Image Altered sexuality
Panhypopituitarism When both the anterior and posterior fail to secrete hormones, the condition is called panhypopituitarism. Causes include tumors, infection, injury, iatrogenic (radiation, surgery), infarction Manifestations don’t occur until 75% of pituitary has been obliterated. Treatment involves removal of cause and hormone replacement (adrenaocortical insufficiency, thyroid hormone, sex hormones)
Know The what these conditions are & difference b/t a) Cushings’ Disease & Cushings’ Syndrome b) Giantism &Acromegaly c) Dwarfism d) Diabetes Insipidus vs. Diabetes Mellitus Consider Nursing Diagnosis related to these conditions
What role does the pituitary gland play in fluid and electrolyte balance?
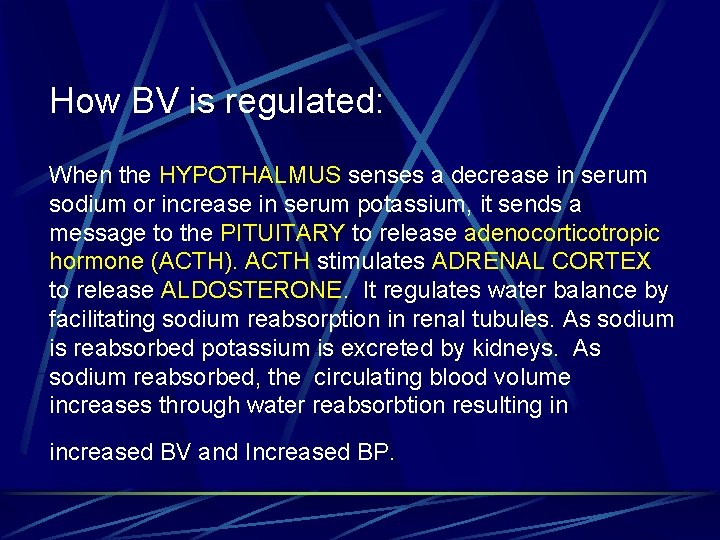
How BV is regulated: When the HYPOTHALMUS senses a decrease in serum sodium or increase in serum potassium, it sends a message to the PITUITARY to release adenocorticotropic hormone (ACTH). ACTH stimulates ADRENAL CORTEX to release ALDOSTERONE. It regulates water balance by facilitating sodium reabsorption in renal tubules. As sodium is reabsorbed potassium is excreted by kidneys. As sodium reabsorbed, the circulating blood volume increases through water reabsorbtion resulting in increased BV and Increased BP.
Endocrine system and sodium balance?
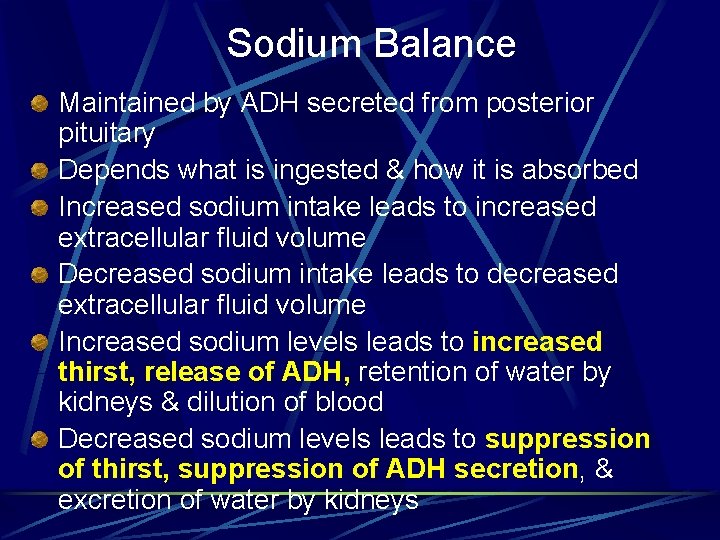
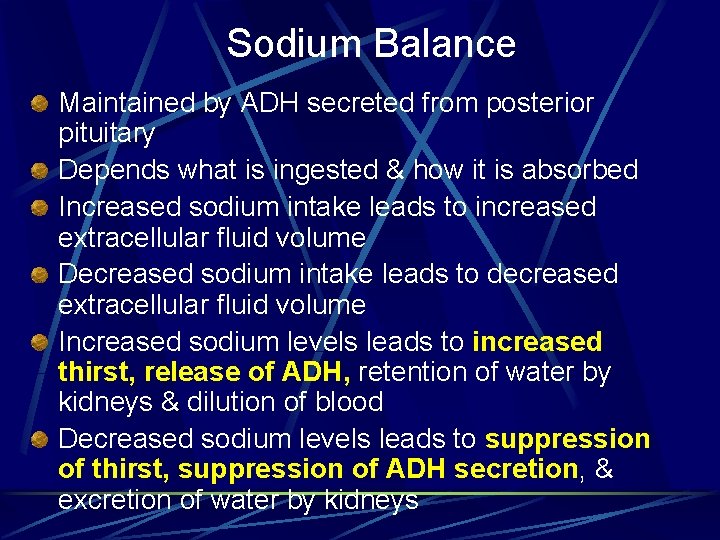
Sodium Balance Maintained by ADH secreted from posterior pituitary Depends what is ingested & how it is absorbed Increased sodium intake leads to increased extracellular fluid volume Decreased sodium intake leads to decreased extracellular fluid volume Increased sodium levels leads to increased thirst, release of ADH, retention of water by kidneys & dilution of blood Decreased sodium levels leads to suppression of thirst, suppression of ADH secretion, & excretion of water by kidneys
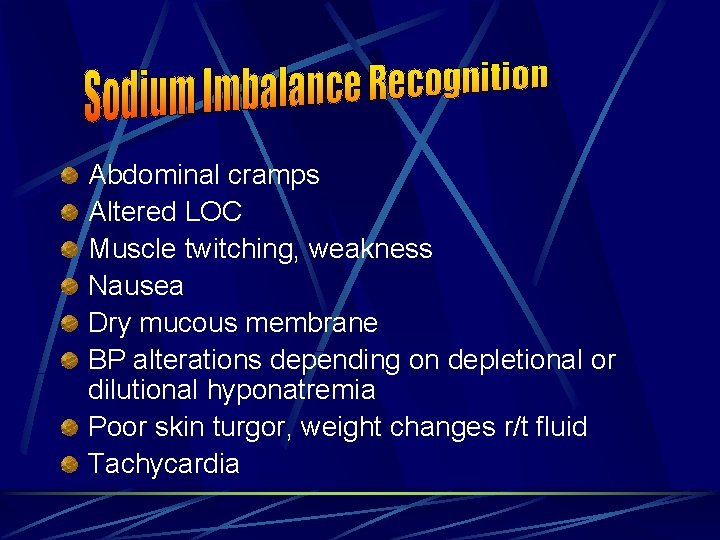
Abdominal cramps Altered LOC Muscle twitching, weakness Nausea Dry mucous membrane BP alterations depending on depletional or dilutional hyponatremia Poor skin turgor, weight changes r/t fluid Tachycardia
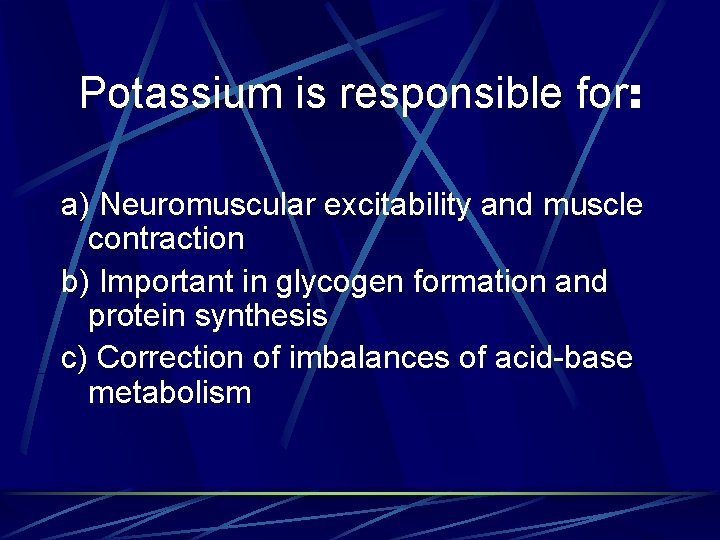
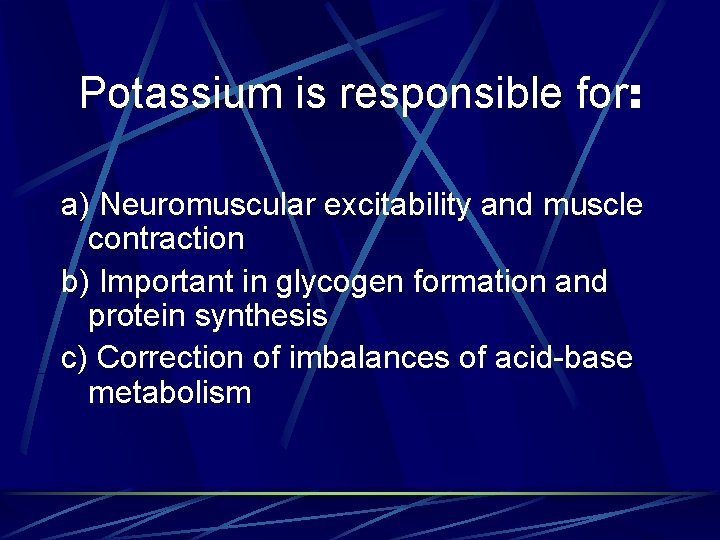
Potassium is responsible for: a) Neuromuscular excitability and muscle contraction b) Important in glycogen formation and protein synthesis c) Correction of imbalances of acid-base metabolism
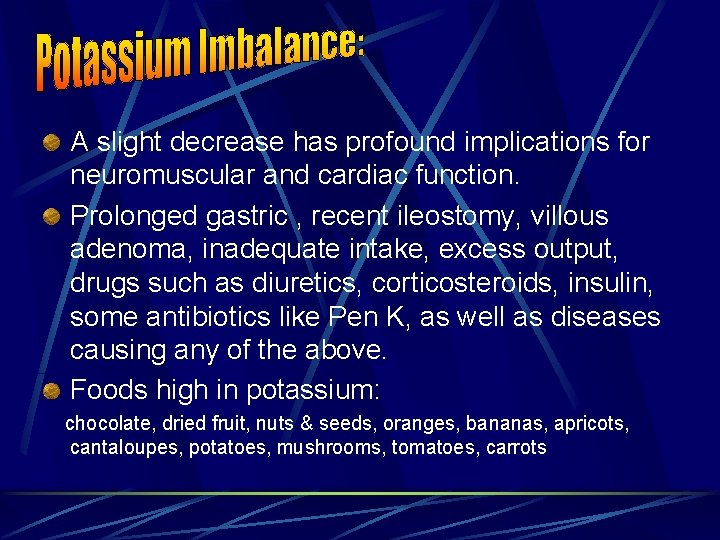
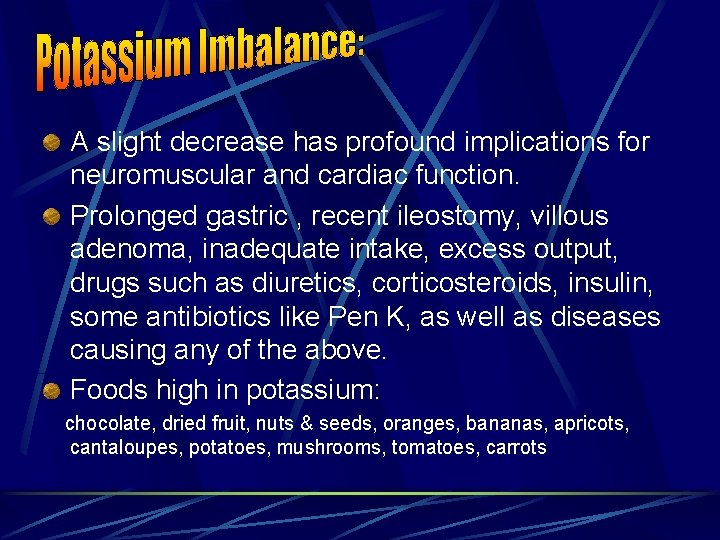
A slight decrease has profound implications for neuromuscular and cardiac function. Prolonged gastric , recent ileostomy, villous adenoma, inadequate intake, excess output, drugs such as diuretics, corticosteroids, insulin, some antibiotics like Pen K, as well as diseases causing any of the above. Foods high in potassium: chocolate, dried fruit, nuts & seeds, oranges, bananas, apricots, cantaloupes, potatoes, mushrooms, tomatoes, carrots
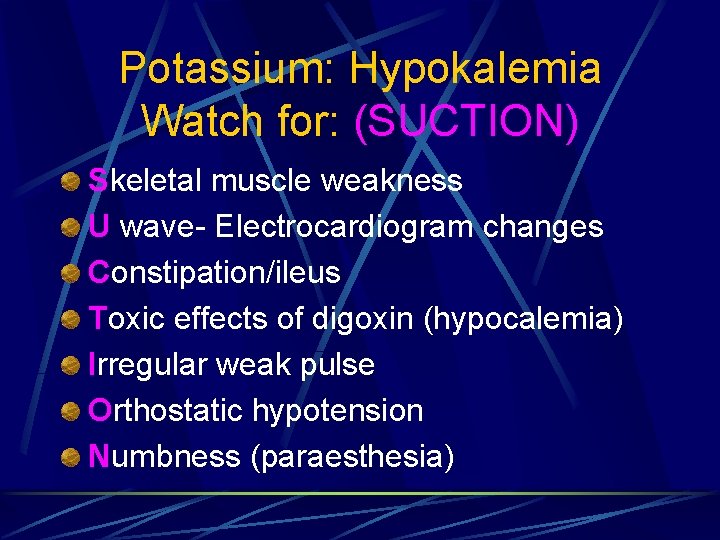
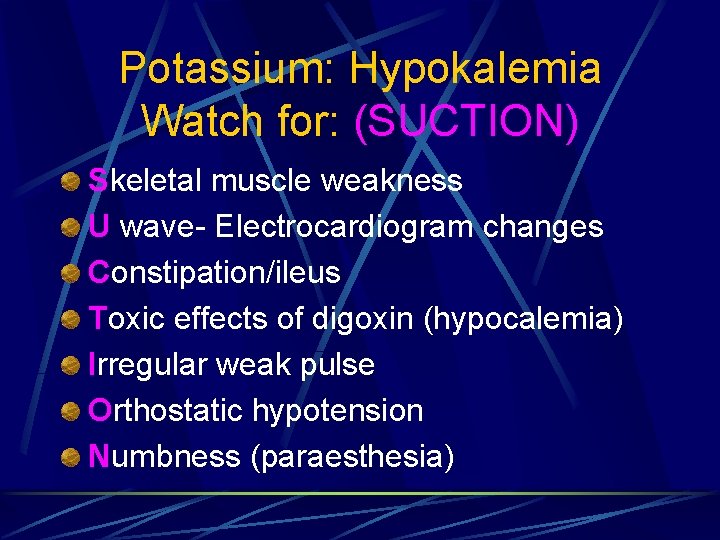
Potassium: Hypokalemia Watch for: (SUCTION) Skeletal muscle weakness U wave- Electrocardiogram changes Constipation/ileus Toxic effects of digoxin (hypocalemia) Irregular weak pulse Orthostatic hypotension Numbness (paraesthesia)
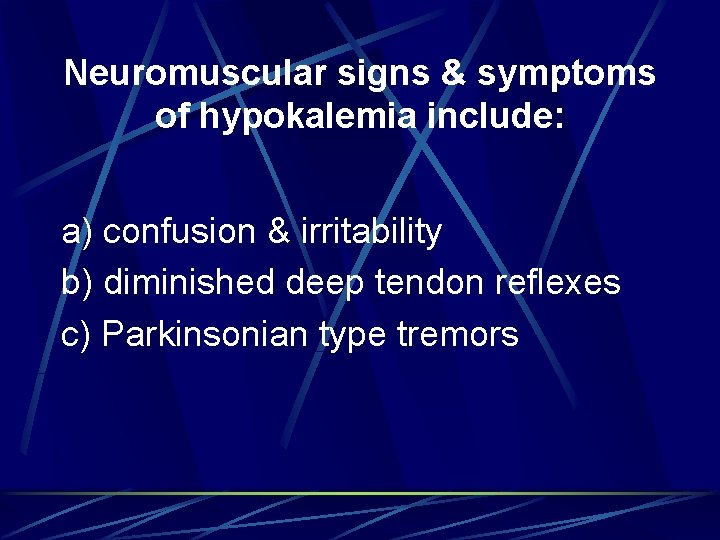
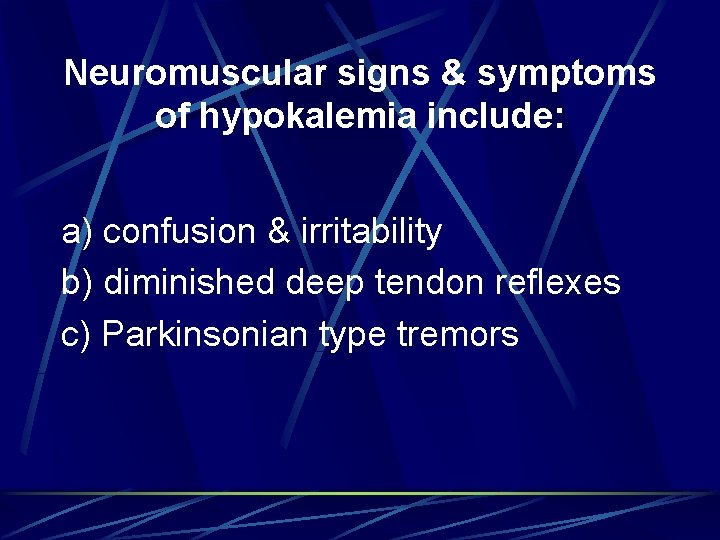
Neuromuscular signs & symptoms of hypokalemia include: a) confusion & irritability b) diminished deep tendon reflexes c) Parkinsonian type tremors
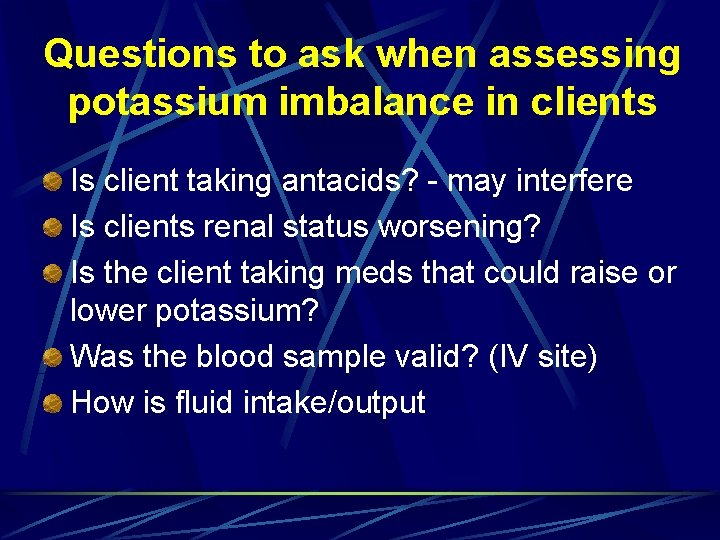
Questions to ask when assessing potassium imbalance in clients Is client taking antacids? - may interfere Is clients renal status worsening? Is the client taking meds that could raise or lower potassium? Was the blood sample valid? (IV site) How is fluid intake/output
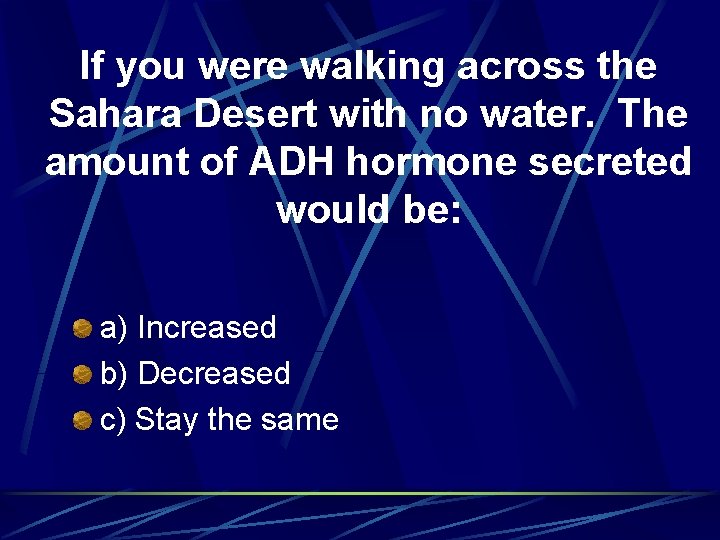
If you were walking across the Sahara Desert with no water. The amount of ADH hormone secreted would be: a) Increased b) Decreased c) Stay the same
Giving a hypertonic IV solution to a client may cause too much fluid to be: a) pulled from cells into the bloodstream b) pulled out of the bloodstream into the cells c) pushed out of the bloodstream into extravascular space
Thirst Eating highly salty foods and losing fluids lead to an increase in extracellular fluid osmolality. This leads to drying of mucous membrane, which stimulates the thirst center in hypothalamus. This mechanism is less effective in elderly, thus they are more prone to dehydration. Also it takes a while for this response to occur. Anticipate!
Great web site http: //www. emc. maricopa. edu/faculty/far abee/BIOBK/Bio. Book. ENDOCR. html
 Pituitary gland disorders
Pituitary gland disorders Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Thyoid gland
Thyoid gland Ceolocant
Ceolocant Posterior abdominal wall nerves
Posterior abdominal wall nerves Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Endocrine organ
Endocrine organ Anterior pituitary gland
Anterior pituitary gland Morphology of pituitary gland
Morphology of pituitary gland Claivus
Claivus Human body
Human body Tuberculum impar
Tuberculum impar Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Sketch of pituitary gland
Sketch of pituitary gland Origin of posterior pituitary gland
Origin of posterior pituitary gland Htpothalamus
Htpothalamus Pituitary gland hormones
Pituitary gland hormones Pituitary gland division
Pituitary gland division Function of pituitary gland in points
Function of pituitary gland in points Putery gland
Putery gland Acromegaly before and after
Acromegaly before and after Pituitary gland
Pituitary gland Hormoni hidrosolubili
Hormoni hidrosolubili Brainstem glioma
Brainstem glioma Nerve supply to pituitary gland
Nerve supply to pituitary gland Histology of pituitary gland
Histology of pituitary gland Anterior pituitary hormones
Anterior pituitary hormones Hashitoxicosis
Hashitoxicosis Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Follicular epithelium
Follicular epithelium Hypothalamus hormones
Hypothalamus hormones Salivary gland disorders classification
Salivary gland disorders classification Thế nào là giọng cùng tên
Thế nào là giọng cùng tên Thể thơ truyền thống
Thể thơ truyền thống Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Hươu thường đẻ mỗi lứa mấy con
Hươu thường đẻ mỗi lứa mấy con đại từ thay thế
đại từ thay thế Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Cong thức tính động năng
Cong thức tính động năng Phép trừ bù
Phép trừ bù Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Môn thể thao bắt đầu bằng từ đua
Môn thể thao bắt đầu bằng từ đua Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ độ dài liên kết
độ dài liên kết Chó sói
Chó sói Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Sơ đồ cơ thể người
Sơ đồ cơ thể người Frameset trong html5
Frameset trong html5 Số.nguyên tố
Số.nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Tư thế worm breton là gì
Tư thế worm breton là gì ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Tư thế ngồi viết
Tư thế ngồi viết Cái miệng nó xinh thế
Cái miệng nó xinh thế Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Bổ thể
Bổ thể Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết Difference between anterior and posterior pituitary
Difference between anterior and posterior pituitary Pineal and pituitary glands
Pineal and pituitary glands Pituitary dwarfism
Pituitary dwarfism Pituitary
Pituitary Anterior pituitary
Anterior pituitary Propothiouracil
Propothiouracil Galactorrehea
Galactorrehea