Parathyroid hormoneParathormone Lecture NO 2 nd MBBS Dr
Parathyroid hormone(Parathormone) Lecture NO: 2 nd MBBS Dr Muhammad Ramzan
Parathyroid hormone (PTH) – the definition • A protein hormone (84 AA. ) from the Parathyroid gland that regulates the metabolism of : • Calcium and phosphorous in the body • It is also called as Parathormone (PTH) • www. merrium – webster. com
Parathormone (PTH) – the background ↑ Ca and↓PO 4 ions • PTH is important in bone remodeling via ongoing process of bone resorption and bone formation (Osteogenesis) • PTH elevates calcium level when it is low. • PTH excess causes bone/muscle pain and kidney stones • PTH deficiency produces muscle spasm; numbness in extremities, coagulation disorders and abnormal heart beats • www. webmd. com – www. wikipedia. com
PTH – the target organs - 3 Bone, kidney and Intestine • Target organs are the ones with PTH receptors and include bones, Kidneys (CNS) and Intestine • No receptors for Intestinal mucosa and Osteoclasts • PTH acts via Osteoblasts and Osteocytes • Activates Vit. D in Kidneys through 1 - α – hydroxylase to • Increase GIT Ca++ absorption • www. Labtestsonline. org
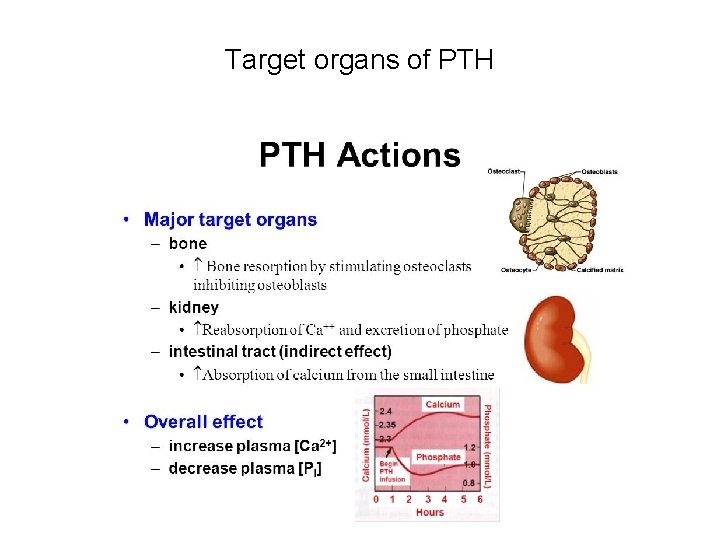
Target organs of PTH
Biosynthesis of PTH – As Pre Prohormone • PTH is synthesized as a Pre Prohormone in the RER of the Chief cells with 115 AAs • Pre-Pro PTH is cleaved by signal peptidase in RER to remove 25 AAs and is converted to Pro- PTH • Pro – PTH - 115 - 25 = 90 amino acids
Pro - PTH is transferred to Golgi 6 AAs are removed • Pro - PTH is transferred to the Golgi Complex and 6 AAs are removed by Clipase for PTH = 84 AAs • PTH is packed/stored as secretary vesicles in Chief cells • Hormone Is released to the circulation in response to a proper physiological stimulus like: • Low Ca++ level in serum/ ECF
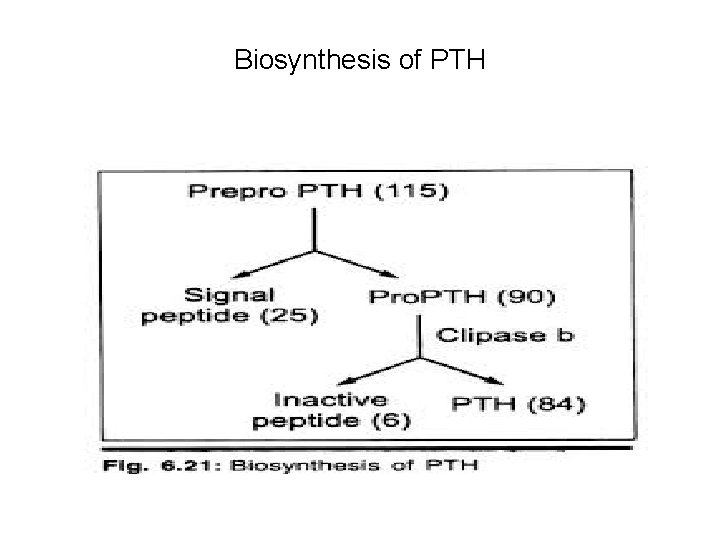
Biosynthesis of PTH
Regulation of PTH – 2 pathways • PTH is regulated through negative feed back mechanism • Regulation is through 2 pathways • Direct and • Indirect
Regulation of PTH – Direct pathway No role of Calcitonin • It is the interaction B/W Ca++ level and PTH secretion • Low free calcium (Ions) in ECF is sensed by the Calcium sensory receptors - Integral membrane proteins • It ↑ the secretion of PTH that elevates Ca++ level by its action on the target organs (bones and Kidneys) • There is no role of Calcitonin • www. vivo. colostate. com
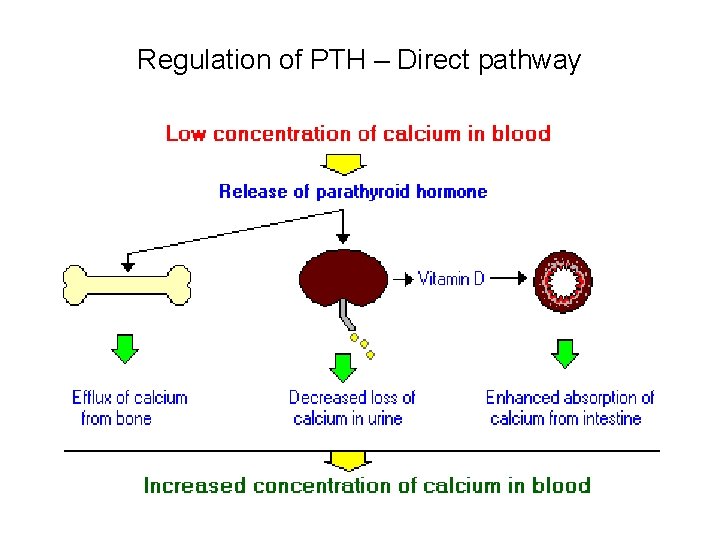
Regulation of PTH – Direct pathway
PTH Regulation – Indirect pathway ↑ Ca, PTH and Calcitonin • It is interaction B/w high serum Ca++, PTH and Calcitonin • High serum Ca++ Induces the following changes • 1. ↓Transcription of m. RNA for PTH (synthesis) • 2. Auto degradation of the preformed PTH secretary granules • Secretion of Calcitonin reduces the Ca++ by promoting its renal excretion and bone formation
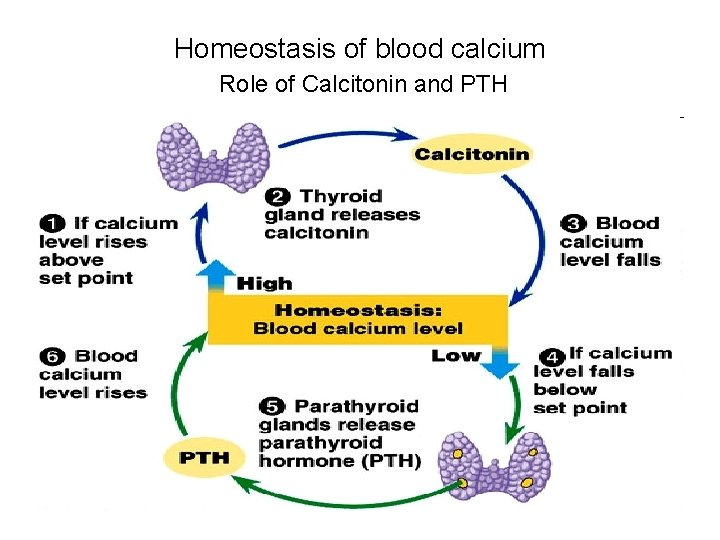
Homeostasis of blood calcium Role of Calcitonin and PTH
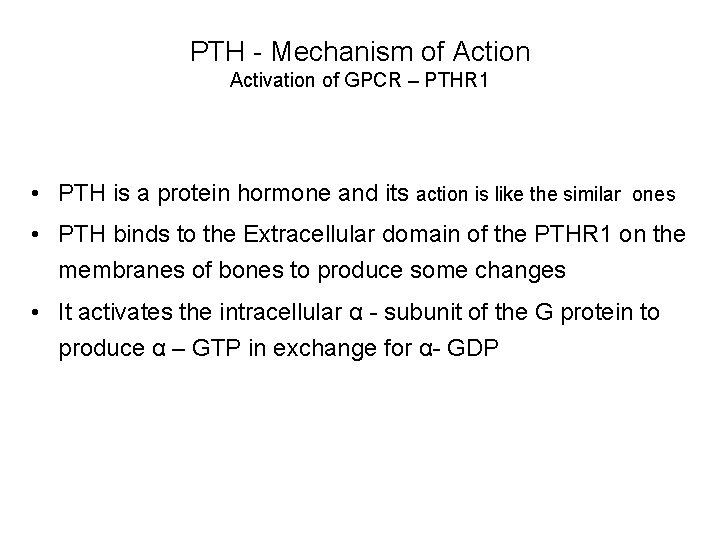
PTH - Mechanism of Action Activation of GPCR – PTHR 1 • PTH is a protein hormone and its action is like the similar ones • PTH binds to the Extracellular domain of the PTHR 1 on the membranes of bones to produce some changes • It activates the intracellular α - subunit of the G protein to produce α – GTP in exchange for α- GDP
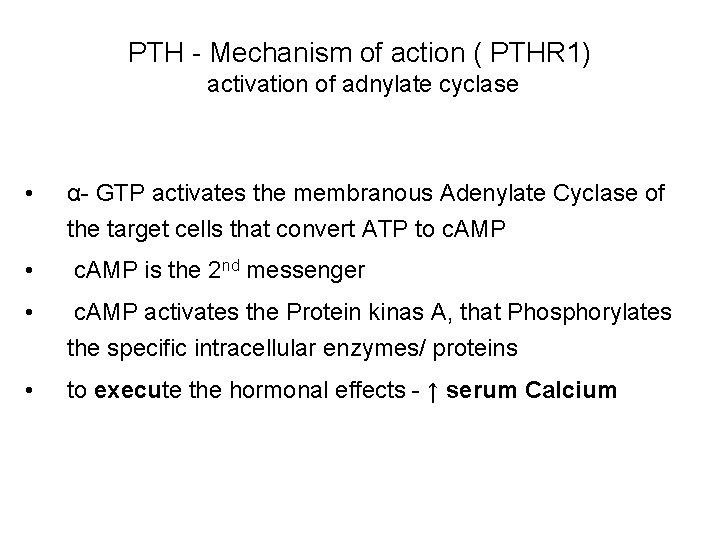
PTH - Mechanism of action ( PTHR 1) activation of adnylate cyclase • α- GTP activates the membranous Adenylate Cyclase of the target cells that convert ATP to c. AMP • c. AMP is the 2 nd messenger • c. AMP activates the Protein kinas A, that Phosphorylates the specific intracellular enzymes/ proteins • to execute the hormonal effects - ↑ serum Calcium
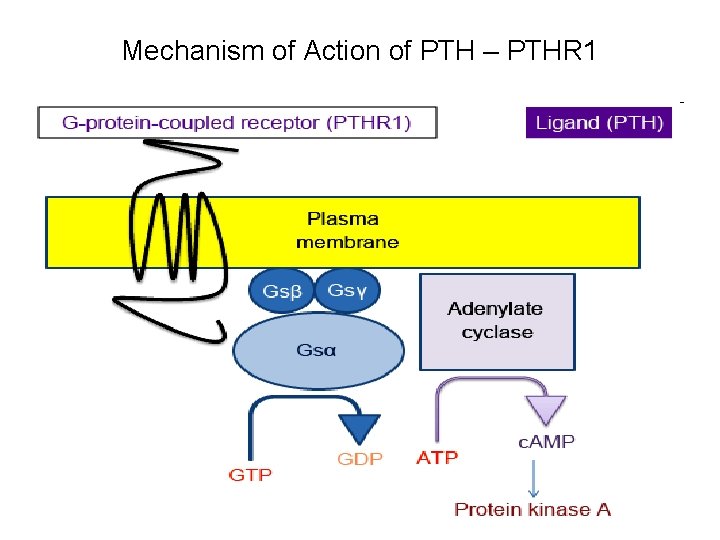
Mechanism of Action of PTH – PTHR 1
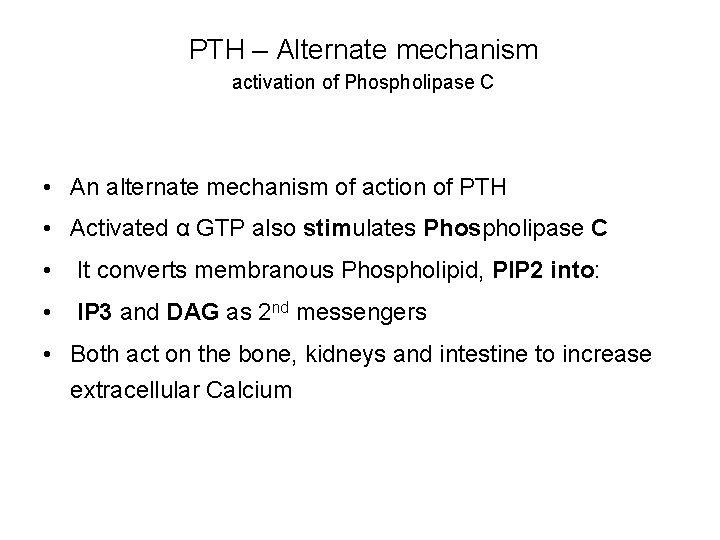
PTH – Alternate mechanism activation of Phospholipase C • An alternate mechanism of action of PTH • Activated α GTP also stimulates Phospholipase C • It converts membranous Phospholipid, PIP 2 into: • IP 3 and DAG as 2 nd messengers • Both act on the bone, kidneys and intestine to increase extracellular Calcium
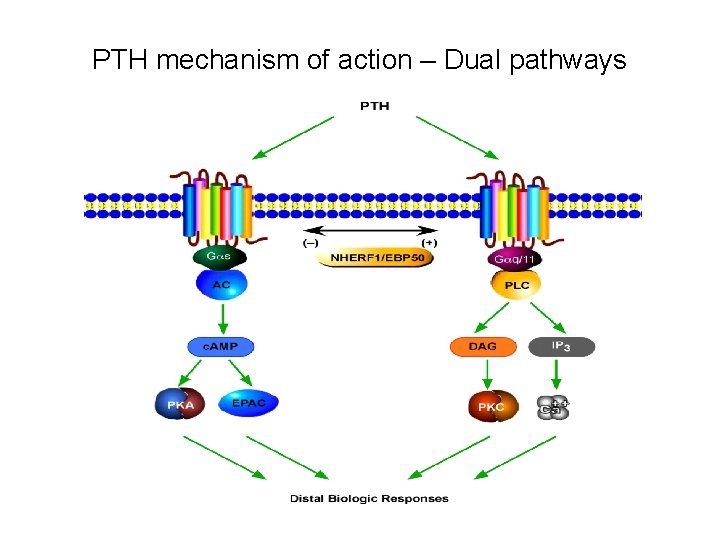
PTH mechanism of action – Dual pathways
Metabolic actions of PTH • PTH acts to maintain serum/ECF Calcium between • 9. 5 - 11 mg/dl and Po 4 B/W 3 - 4. 5 mg/dl • PTH has significant metabolic actions on : • Bones, Kidneys and Intestine
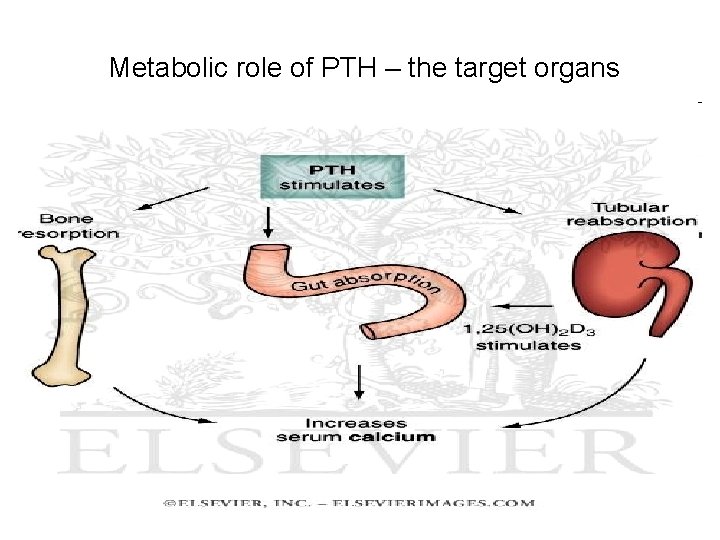
Metabolic role of PTH – the target organs
PTH - Metabolic actions on bone • Bone is a large reservoir of Calcium • PTH enhances the release of Ca and Po 4 from the bone by Osteolysis via Osteoclasts - a normal process • Osteolysis is also supported by the : • 1. Membranous Calcium pump activated by PTH • 2. Elevated Phosphatases around Osteoclasts
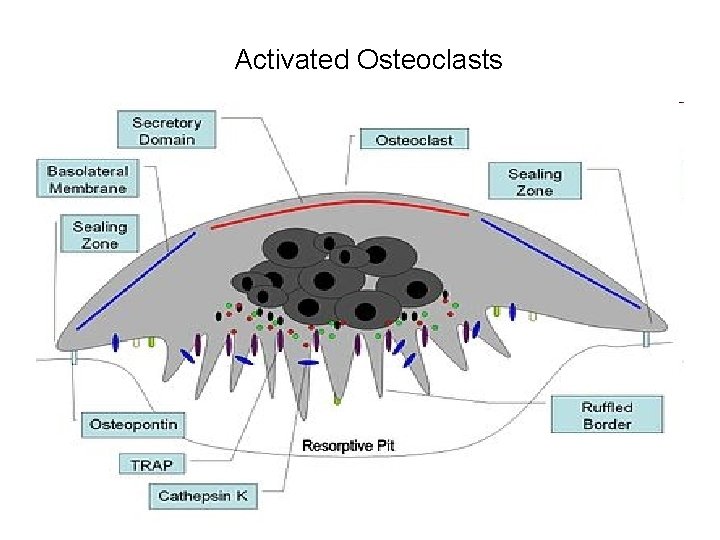
Activated Osteoclasts
Membranous Calcium pump – How it works • Calcium pump causes rapid removal of calcium phosphate from the sites near these cells (Osteoclasts) • Calcium phosphate salts are transported to ECF as: • It alters the permeability of Osteocytes to calcium
Metabolic action on Kidneys ↑ Cal. Resorption and Po 4 excretion • PTH promotes renal excretion of Phosphates to decrease its plasma level and • 1 Enhances active resorption of Ca and Mg from the distal tubules and ascending loop of Henley 2 • This increases Calcium phosphate ratio (3: 11) and more free Ca++ ions in circulation
Metabolic actions on Kidneys cont. Activation of Vit. D for GIT • PTH promote activation of Vitamin D to 1 -25 Dihydroxy Cholecalceferol in kidneys via 1 - α- hydroxylase • Vita. D promotes calcium absorption from GIT • It is facilitated by Calbindin (Ca binding protein) • No PTH receptors are present on Intestinal mucosa • PTH has no significant effect on Po 4 absorption by GIT
PTH - secretion abnormalities • Parathormone may be secreted in excess or there may be deficiency of PTH secretion • Both abnormalities lead to significant clinical conditions
PTH excess - hyperparathyroidism • Excessive PTH secretion is classified as : • Primary and secondary • Primary one is the result of diseases of parathyroid and is due to tumour of the gland • Results in hypercalcemia, kidney stones and osteoporosis
Hyperparathyroidism - Secondary • Secondary one is due to causes out side the parathyroid • Common cause is the: • 1. Renal disease/ failure as it is unable to reabsorb Calcium and there is fall in blood Ca. • 2. Malnutrition for Calcium and Vit. D produces : • Decalcification of bone leading to rubber bones, • pathological fractures and cyst formation
PTH deficiency – Hyoparathyroidism • It refers to the condition when PTH is produced less than the body requirements. Caused by: • Inborn error of metabolism and autoimmune disorders. • Hyoparathyroidism results in : • 1. Reduction of Serum calcium • 2. Defects in muscle contraction and • 3. Tetany
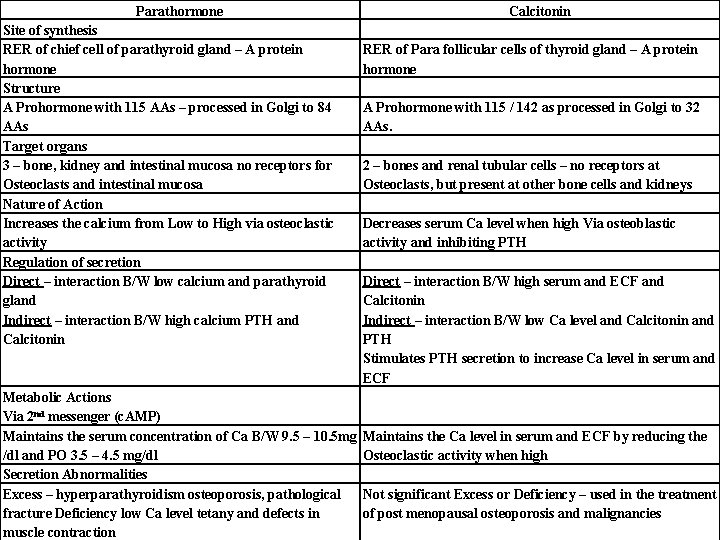
Parathormone Site of synthesis RER of chief cell of parathyroid gland – A protein hormone Structure A Prohormone with 115 AAs – processed in Golgi to 84 AAs Target organs 3 – bone, kidney and intestinal mucosa no receptors for Osteoclasts and intestinal mucosa Nature of Action Increases the calcium from Low to High via osteoclastic activity Regulation of secretion Direct – interaction B/W low calcium and parathyroid gland Indirect – interaction B/W high calcium PTH and Calcitonin Metabolic Actions Via 2 nd messenger (c. AMP) Maintains the serum concentration of Ca B/W 9. 5 – 10. 5 mg /dl and PO 3. 5 – 4. 5 mg/dl Secretion Abnormalities Excess – hyperparathyroidism osteoporosis, pathological fracture Deficiency low Ca level tetany and defects in muscle contraction Calcitonin RER of Para follicular cells of thyroid gland – A protein hormone A Prohormone with 115 / 142 as processed in Golgi to 32 AAs. 2 – bones and renal tubular cells – no receptors at Osteoclasts, but present at other bone cells and kidneys Decreases serum Ca level when high Via osteoblastic activity and inhibiting PTH Direct – interaction B/W high serum and ECF and Calcitonin Indirect – interaction B/W low Ca level and Calcitonin and PTH Stimulates PTH secretion to increase Ca level in serum and ECF Maintains the Ca level in serum and ECF by reducing the Osteoclastic activity when high Not significant Excess or Deficiency – used in the treatment of post menopausal osteoporosis and malignancies
- Slides: 30