Endocrine System Endocrine pharmacology vs endocrine physiology Hormones



![Parathyroid Hormone (PTH) Regulation of synthesis & release: ↑ [Ca++] → ↓ PTH; ↓ Parathyroid Hormone (PTH) Regulation of synthesis & release: ↑ [Ca++] → ↓ PTH; ↓](https://slidetodoc.com/presentation_image_h2/4ed5b004199d61801f352f945ecaabba/image-53.jpg)
![Disorders affecting the parathyroids: ** Hyposecretion (hypoparathyroidism): ↓ [Ca++] Causes: - Thyroidectomy (most common Disorders affecting the parathyroids: ** Hyposecretion (hypoparathyroidism): ↓ [Ca++] Causes: - Thyroidectomy (most common](https://slidetodoc.com/presentation_image_h2/4ed5b004199d61801f352f945ecaabba/image-59.jpg)
![** Hypersecretion (hyperparathyroidism): ↑ [Ca++] Causes: - 1º hyperparathyroidism (adenomas) - 2º hyperparathyroidism 2º ** Hypersecretion (hyperparathyroidism): ↑ [Ca++] Causes: - 1º hyperparathyroidism (adenomas) - 2º hyperparathyroidism 2º](https://slidetodoc.com/presentation_image_h2/4ed5b004199d61801f352f945ecaabba/image-61.jpg)


- Slides: 132
Endocrine System
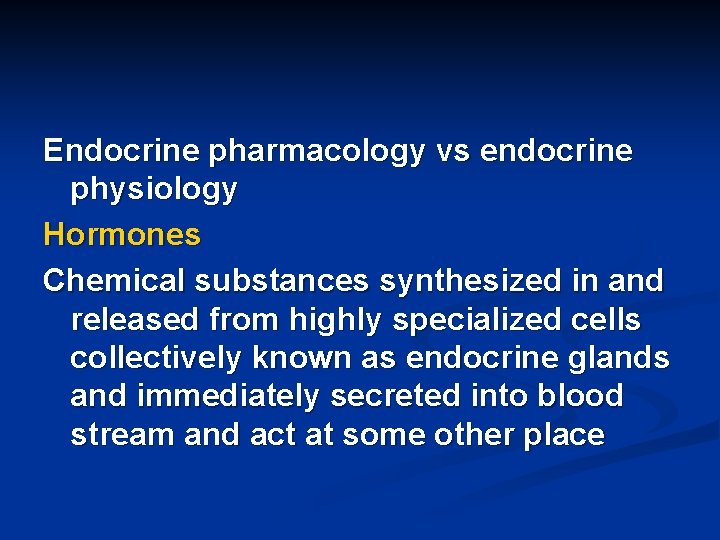
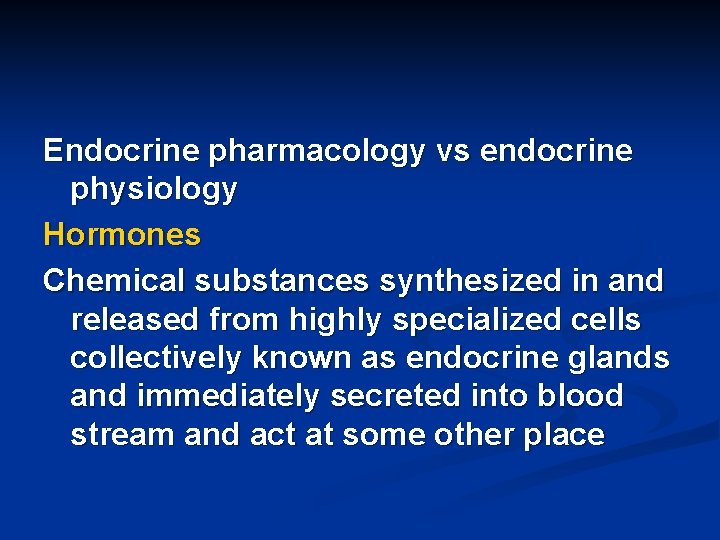
Endocrine pharmacology vs endocrine physiology Hormones Chemical substances synthesized in and released from highly specialized cells collectively known as endocrine glands and immediately secreted into blood stream and act at some other place

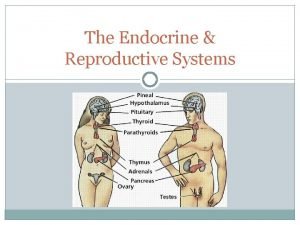
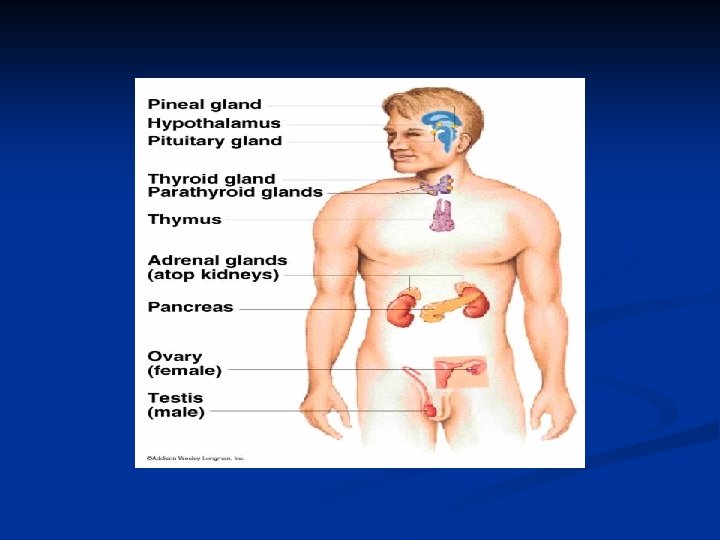
** Glands Ductless Hypothalamus Pituitary Thyroid Parathyroid Pancreas Adrenals Ovaries testes
Hormonal regulation ↑↓ is important for: - Growth & development - Reproduction, fertility, sexual function - Response to environmental situations (stress. . ) - Maintenance of normal homeostasis
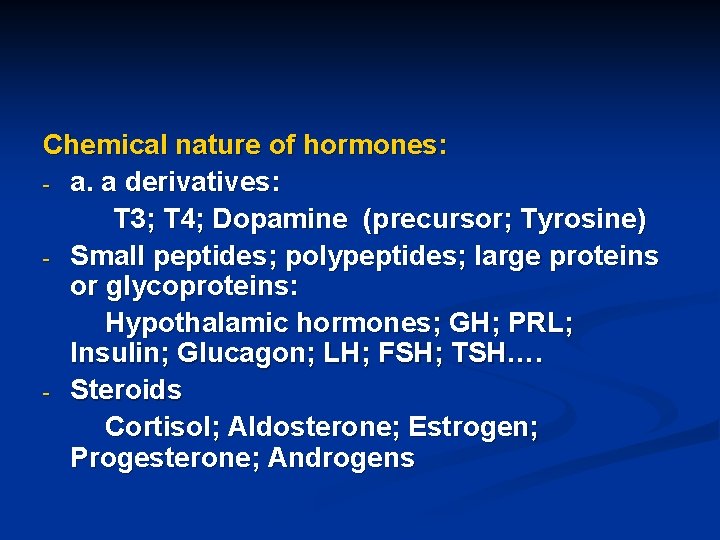
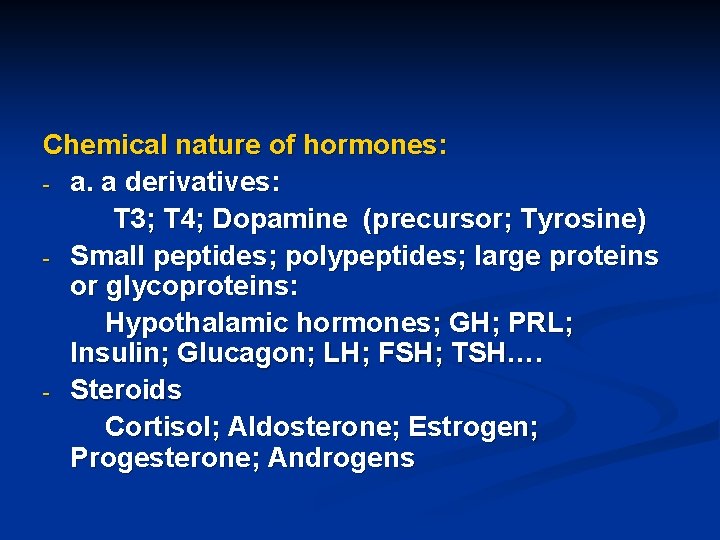
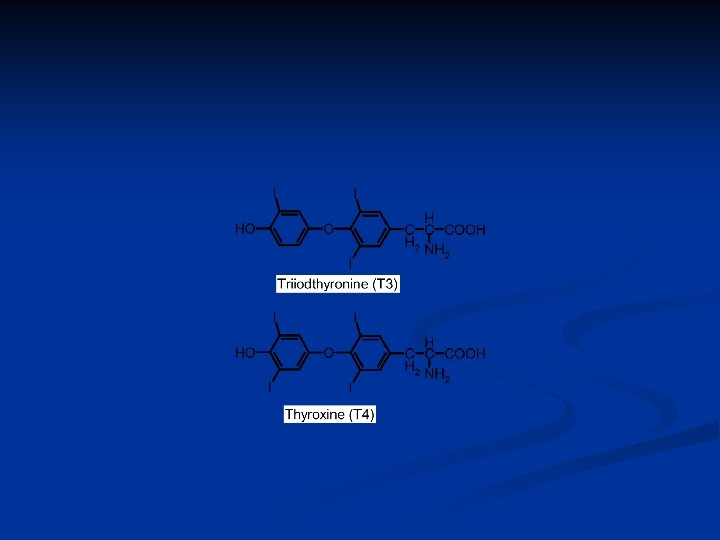
Chemical nature of hormones: - a. a derivatives: T 3; T 4; Dopamine (precursor; Tyrosine) - Small peptides; polypeptides; large proteins or glycoproteins: Hypothalamic hormones; GH; PRL; Insulin; Glucagon; LH; FSH; TSH…. - Steroids Cortisol; Aldosterone; Estrogen; Progesterone; Androgens
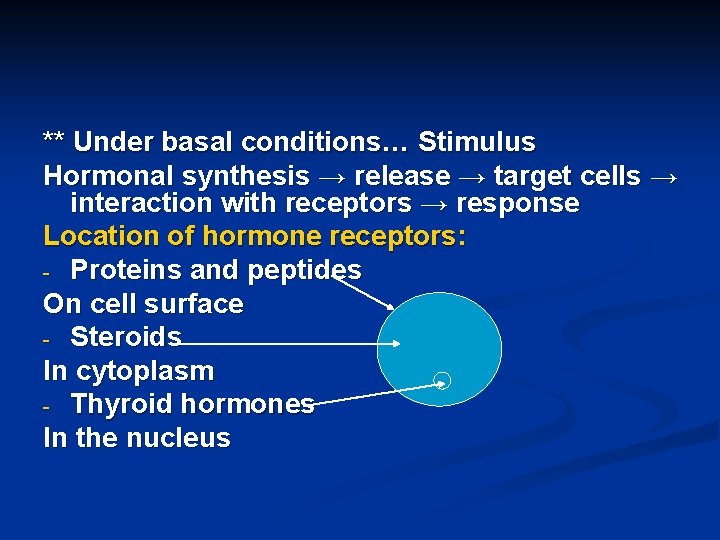
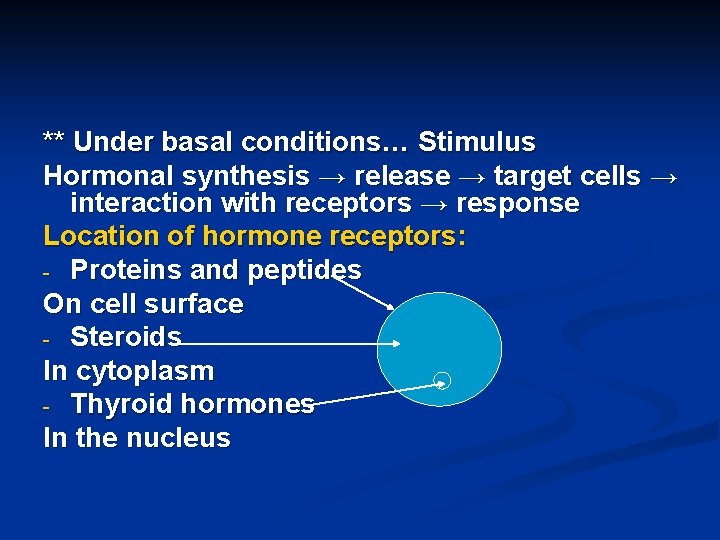
** Under basal conditions… Stimulus Hormonal synthesis → release → target cells → interaction with receptors → response Location of hormone receptors: - Proteins and peptides On cell surface - Steroids In cytoplasm - Thyroid hormones In the nucleus
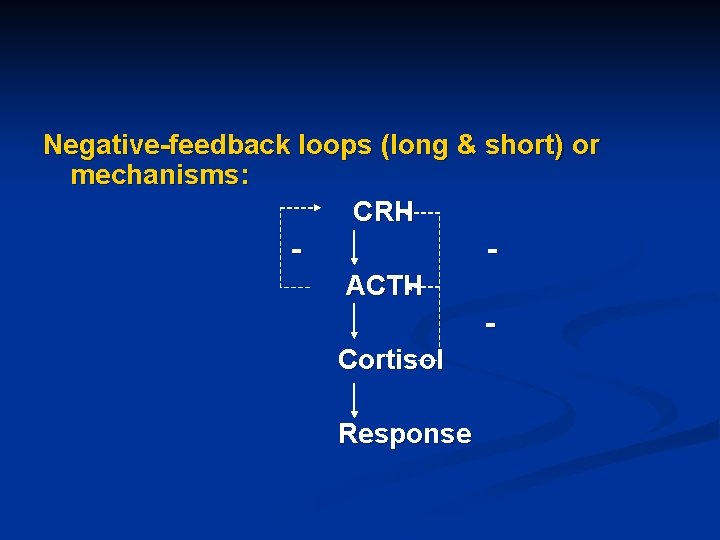
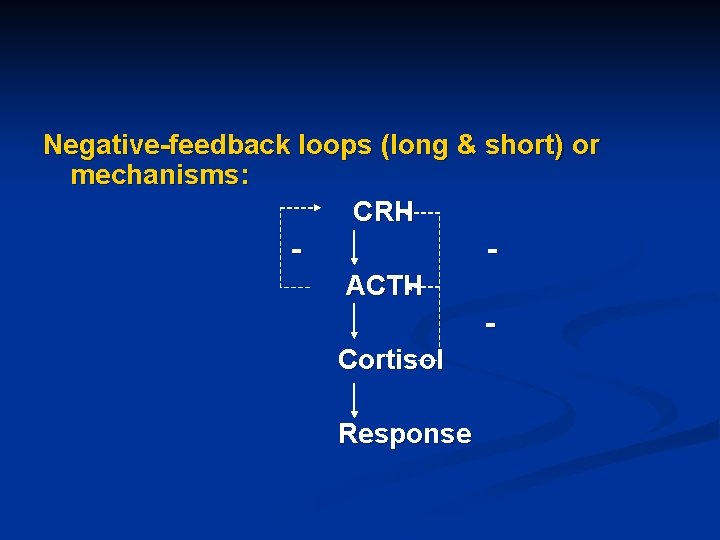
Negative-feedback loops (long & short) or mechanisms: CRH ACTH Cortisol Response
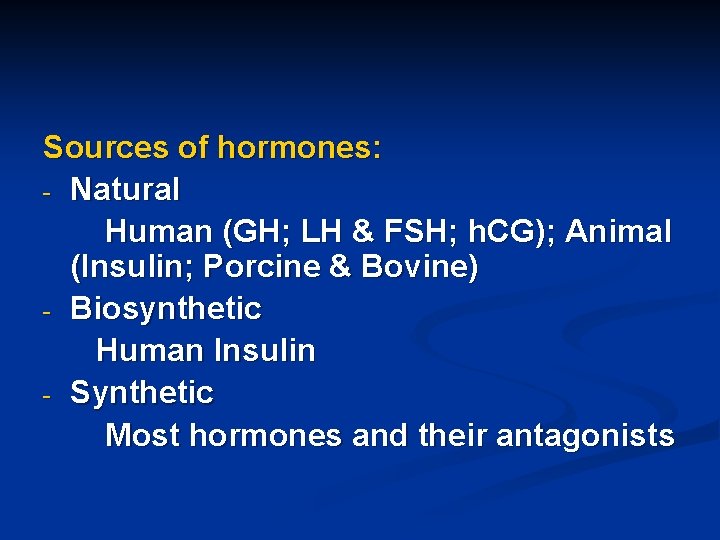
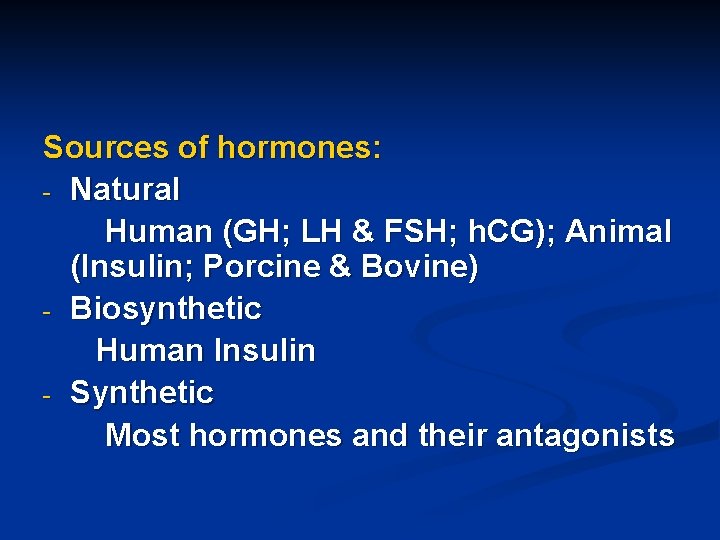
Sources of hormones: - Natural Human (GH; LH & FSH; h. CG); Animal (Insulin; Porcine & Bovine) - Biosynthetic Human Insulin - Synthetic Most hormones and their antagonists
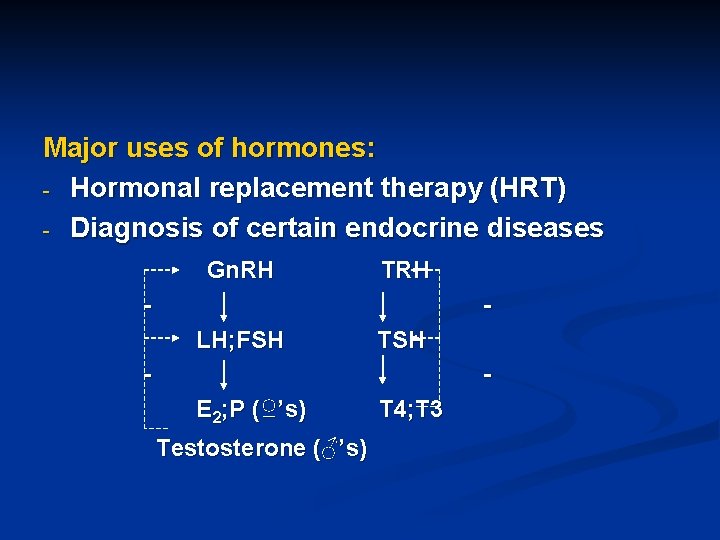
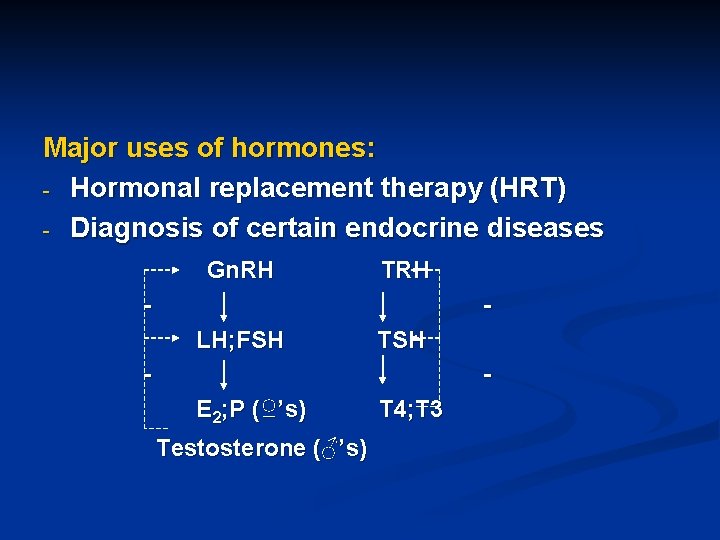
Major uses of hormones: - Hormonal replacement therapy (HRT) - Diagnosis of certain endocrine diseases Gn. RH TRH - LH; FSH TSH - E 2; P (♀’s) Testosterone (♂’s) T 4; T 3
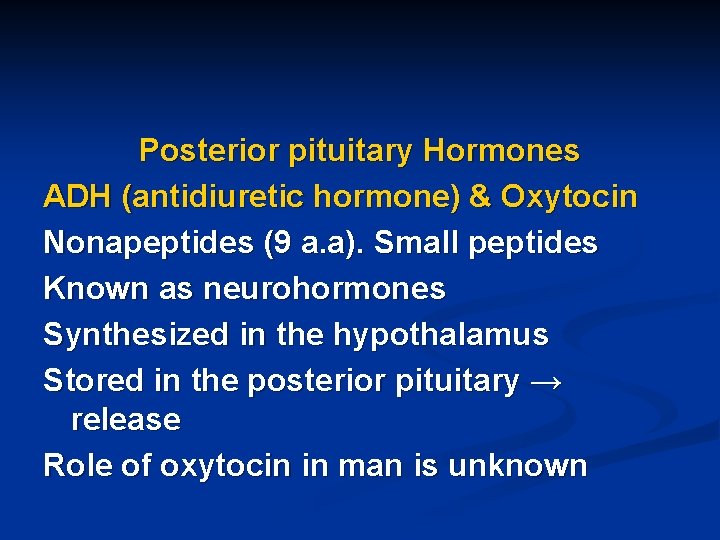
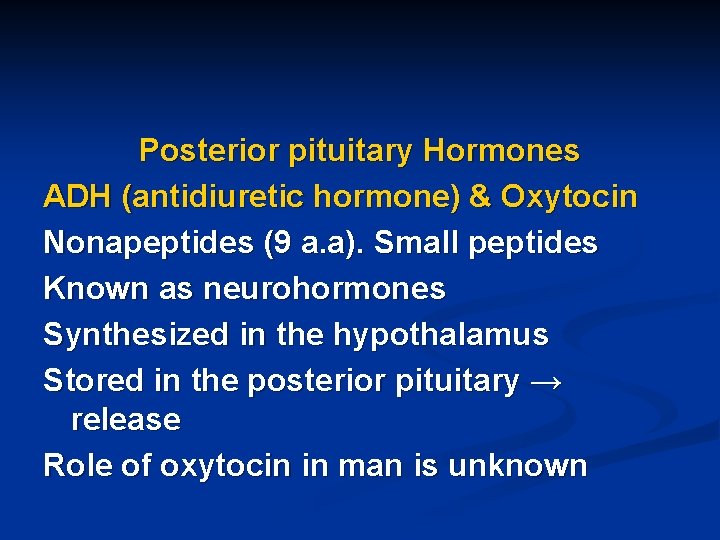
Posterior pituitary Hormones ADH (antidiuretic hormone) & Oxytocin Nonapeptides (9 a. a). Small peptides Known as neurohormones Synthesized in the hypothalamus Stored in the posterior pituitary → release Role of oxytocin in man is unknown
ADH ( Vasopressin) Physiological and pharmacological actions: - ↑ reabsorption of H 2 O from kidney tubules or collecting ducts - Large doses lead to vasoconstriction - Increase synthesis of certain clotting factors - Has Oxytocin-like activity
Clinical uses to ADH: - Deficiency of ADH → diabetes isipidus (DI) - Bleeding esophageal varices (ADH infusion) - Hemophilia - Nocturnal enuresis (intranasal Desmopressin; Minirin®) - + local anaesthetic as a vasoconstrictor
ADH preparations: - Natural human ADH (Pitressin) Given I. M, S. C, has short half-life (15 min) Synthetic preparations: - Lypressin ( synthetic, porcine source) Given intranasally, I. V, I. M, has short DOA (4 hrs) - Desmopressin (synthetic ADH-like drug) Given intranasally, S. C Most widely used preparation, has long DOA (12 hrs)
Felypressin (synthetic ADH-like drug) has strong vasoconstrictor activity mainly used in dentistry with L. A as vasoconstrictor ADH side effects: - Pallor - ↑ B. P and anginal pain (coronary artery vasospasm) - Allergy - H 2 O intoxication - Abdominal pain in ♀’s (oxytocin-like activity, massive doses) -
Oxytocin (9 a. a peptide) - Contracts the myoepithelial cells of the breast → milk letdown; milk ejection Major stimuli, baby cry, suckling - Contracts the uterus → delivery The uterus is insensitive to oxytocin in early pregnancy but its sensitivity increases with advanced pregnancy reaching maximum at time of delivery - Has slight ADH-like activity
Clinical uses to oxytocin (Syntocinon): - Induction of labor Drug of choice to induce labor Synthetic oxytocin (Syntocinon) is used and given in units in an I. V infusion in gradually increasing units (2, 4, 6…) Monitoring of uterine contraction, general condition of mother and the fetus is essential
- - - Abortifacient (induce abortion) In 2 nd trimester ≥ 20 weeks of gestation, ineffective in 1 st trimester. Also given in an I. V infusion Postpartum hemorrhage, I. M. Ergot alkaloids are better (ergonovine, methylergonovine) but oxytocin could be used and even a preparation containing oxytocin and ergometrine is available and given I. M, Syntometrine® (oxytocin+ ergometrine) Breast engorgement, intranasally
Side effects to oxytocin: - Rupture of the uterus Major and most serious side effect - H 2 O intoxication and hypertension Due to its ADH-like activity Specific oxytocin antagonist: Atosiban, effective in the management of premature delivery

Anterior Pituitary Hormones n ACTH (adrenocorticotropin hormone) A peptide, stimulates cortisol secretion from adrenal gland Under – ve feedback by cortisol Tetracosactrin Synthetic ACTH Used I. M or I. V as a diagnostic tool to assess the function of adrenal gland also in certain cases of cortisol deficiency 2 o to ACTH deficiency
TSH (thyroid stimulating hormone) A glycoprotein stimulates thyroid hormones synthesis and release Used to test thyroid function n Growth hormone (GH) A protein stimulates growth and development of soft tissues and bones It increases blood sugar level n
GH is under stimulation and inhibition by hypothalamus Deficiency of GH results in dwarfism Rx replacement therapy with synthetic recombinant human GH (Somatrem) Somatrem is usually given S. C daily at night until closure of epiphyseal plate
Excessive production of GH leads to: Gigantism in children Acromegaly in adults Rx: - Surgery - Bromocriptine; DA agonist inhibits GH release given orally - Somatostatin; a hypothalamic inhibitory hormone to GH
Octreotide Synthetic somatostatin used in cases: - Acromegaly - Carcinoid syndrome; tumor characterized by excessive production of serotonin (5 HT) that results in severe diarrhea Octreotide inhibits release of serotonin and given S. C
Prolactin A protein that stimulates milk production and growth of breast at time of puberty and during pregnancy It is under predominant inhibition by the hypothalamus Its inhibitory hormone is Dopamine (DA) So DA agonists e. g. Bromocriptine inhibit prolactin release from ant. Pit. n
Prolactin also inhibits LH & FSH release from the ant. Pit. → infertility in ♂’s and ♀’s Bromocriptine: DA agonist given orally Inhibits prolactin and GH release Major clinical uses: 1. Hyperprolactinemia (a major cause of infertility; amenorrhea in ♀’s and impotency in ♂’s) 2. Supression of lactation 3. Parkinson’s disease 4. Acromegaly
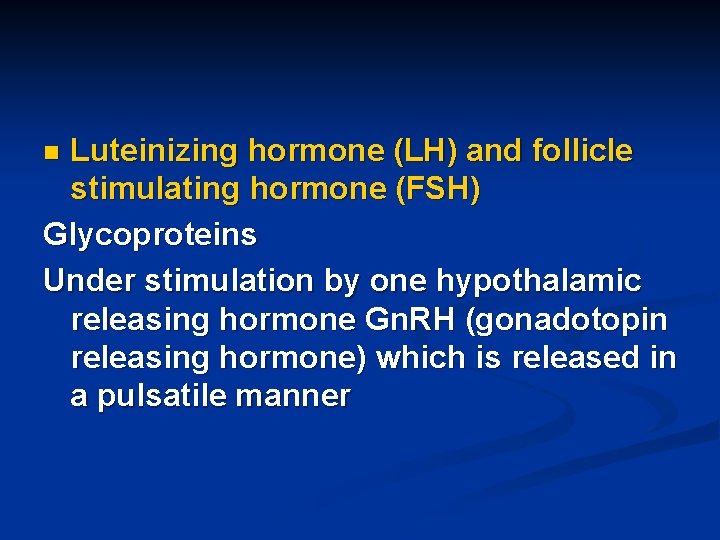
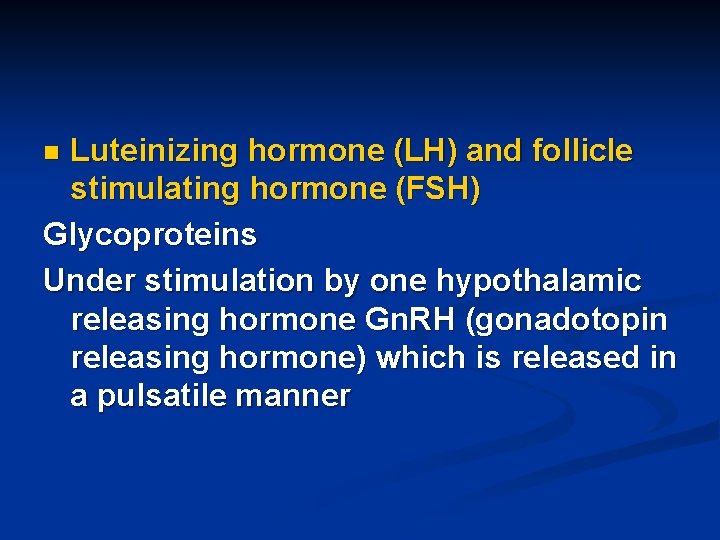
Luteinizing hormone (LH) and follicle stimulating hormone (FSH) Glycoproteins Under stimulation by one hypothalamic releasing hormone Gn. RH (gonadotopin releasing hormone) which is released in a pulsatile manner n
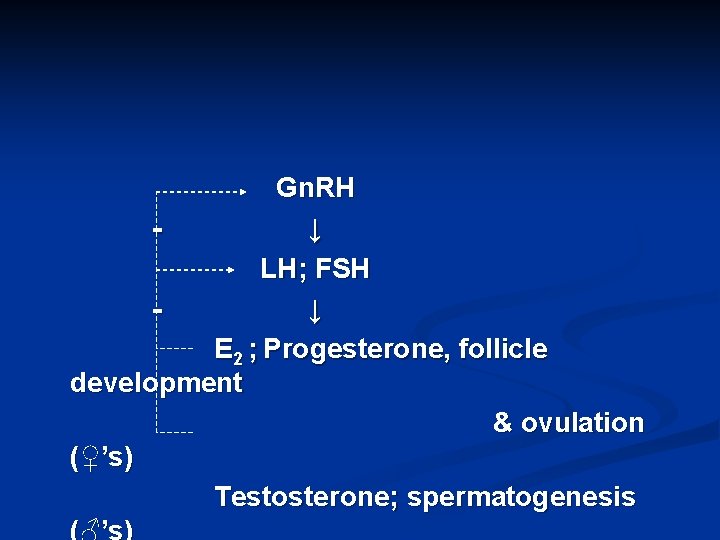
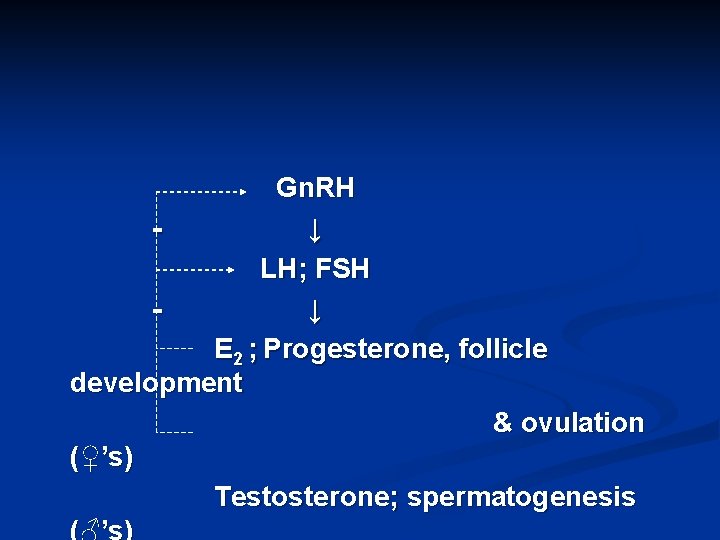
Gn. RH ↓ LH; FSH ↓ E 2 ; Progesterone, follicle development & ovulation (♀’s) Testosterone; spermatogenesis (♂’s)

Source of LH & FSH: Urine of postmenopausal females (human) Clinical uses of LH & FSH - Treatment of LH & FSH deficiency in ♂’s & ♀’s (Rx of infertility) - IVF Given by I. M injection Menotropin A drug containing LH & FSH in 1: 1 ratio
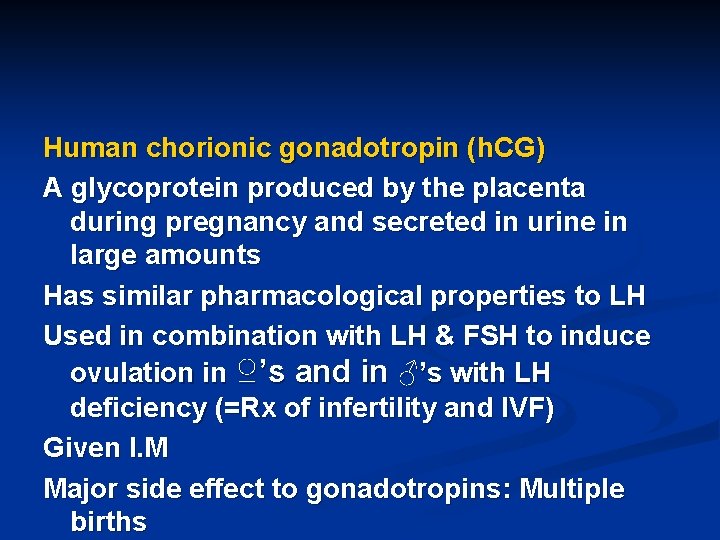
Human chorionic gonadotropin (h. CG) A glycoprotein produced by the placenta during pregnancy and secreted in urine in large amounts Has similar pharmacological properties to LH Used in combination with LH & FSH to induce ovulation in ♀’s and in ♂’s with LH deficiency (=Rx of infertility and IVF) Given I. M Major side effect to gonadotropins: Multiple births
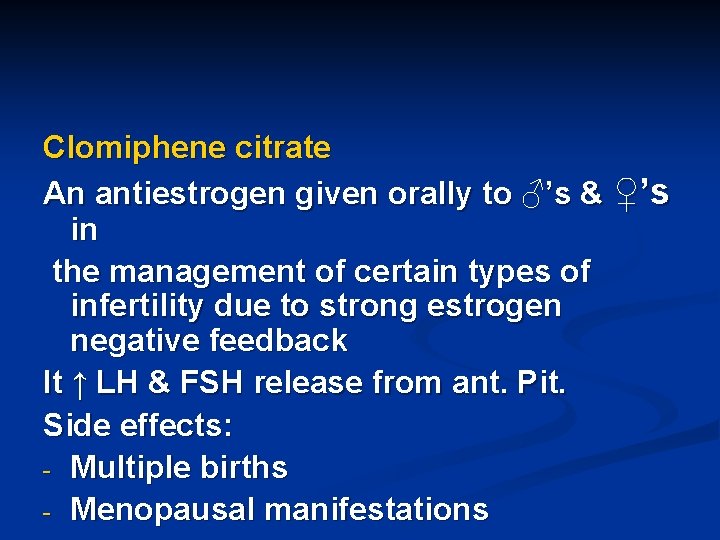
Clomiphene citrate An antiestrogen given orally to ♂’s & ♀’s in the management of certain types of infertility due to strong estrogen negative feedback It ↑ LH & FSH release from ant. Pit. Side effects: - Multiple births - Menopausal manifestations
Thyroid Gland Hormones
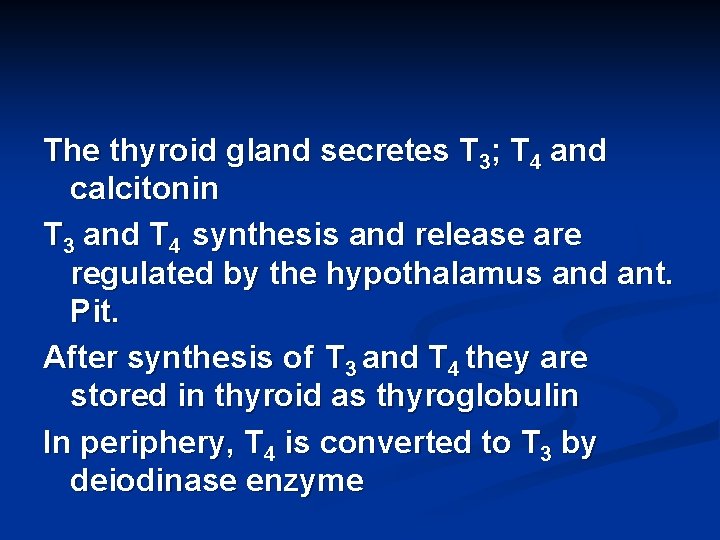
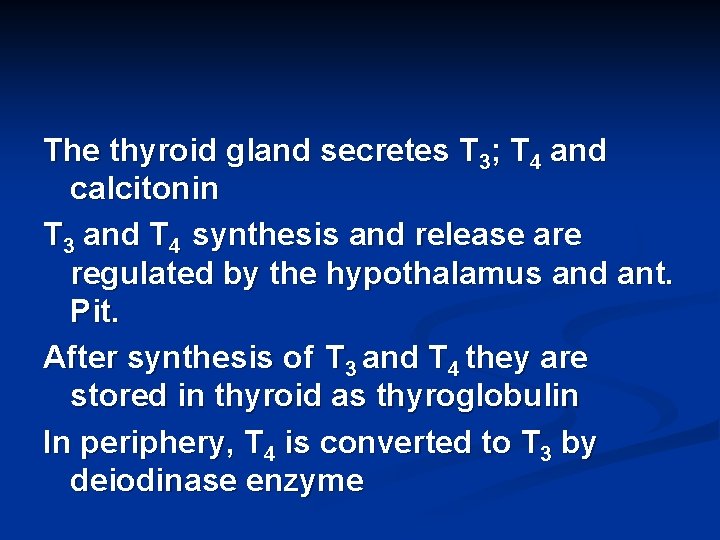
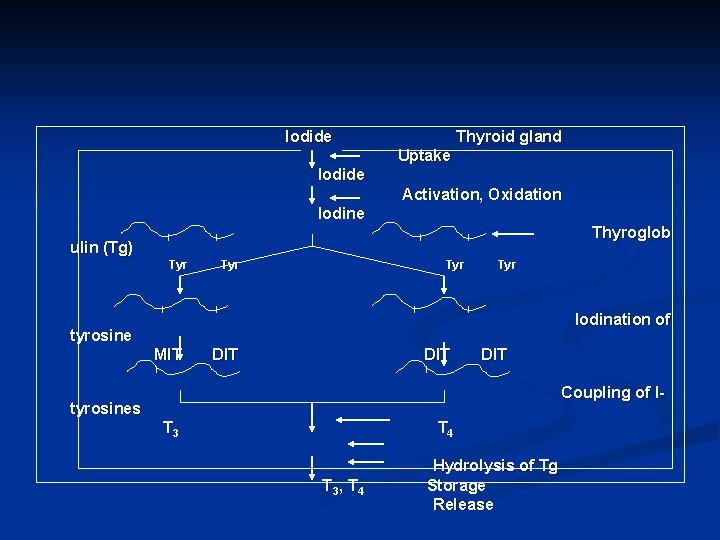
The thyroid gland secretes T 3; T 4 and calcitonin T 3 and T 4 synthesis and release are regulated by the hypothalamus and ant. Pit. After synthesis of T 3 and T 4 they are stored in thyroid as thyroglobulin In periphery, T 4 is converted to T 3 by deiodinase enzyme
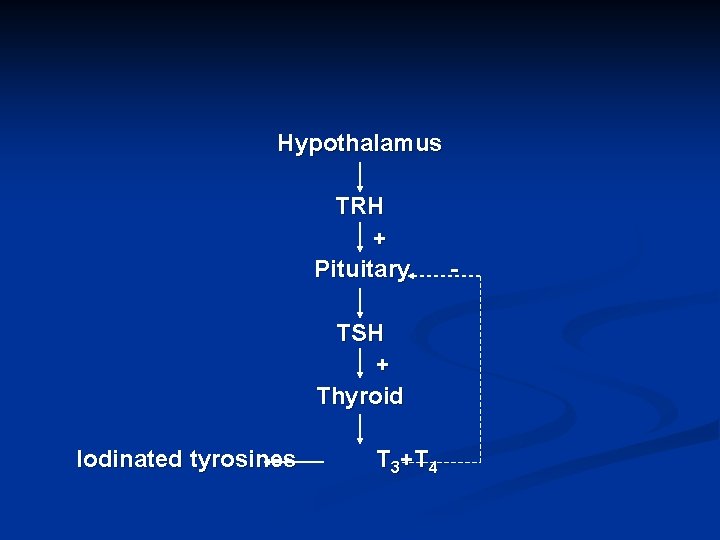
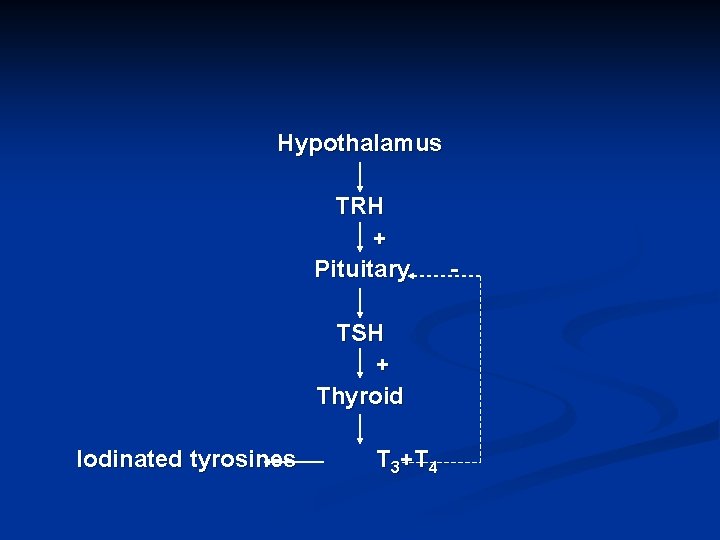
Hypothalamus TRH + Pituitary TSH + Thyroid Iodinated tyrosines T 3+T 4 -
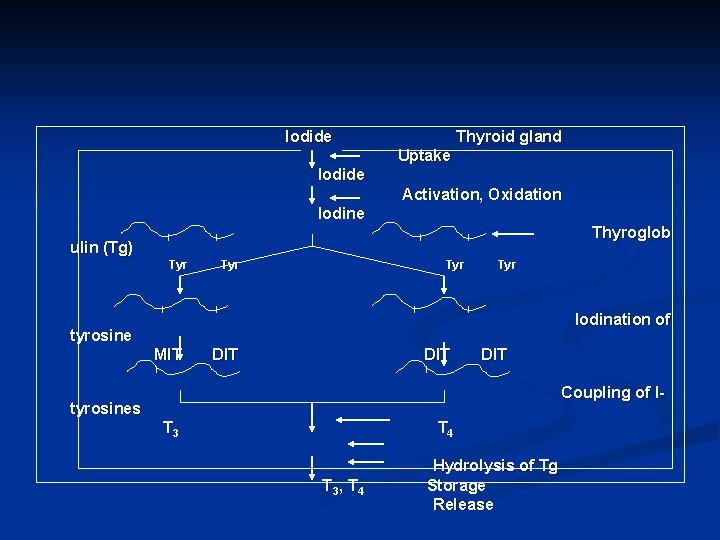
Iodide Thyroid gland Uptake Iodide Activation, Oxidation Iodine Thyroglob ulin (Tg) Tyr Tyr Iodination of tyrosine MIT DIT DIT Coupling of I- tyrosines T 3 T 4 T 3, T 4 Hydrolysis of Tg Storage Release
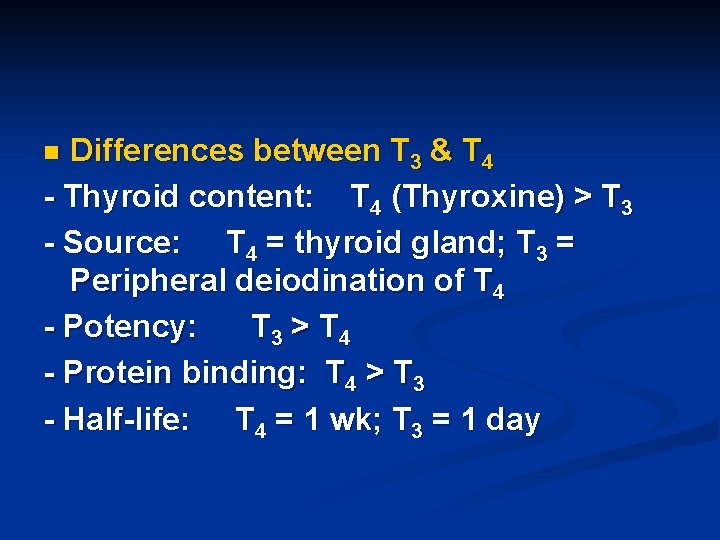
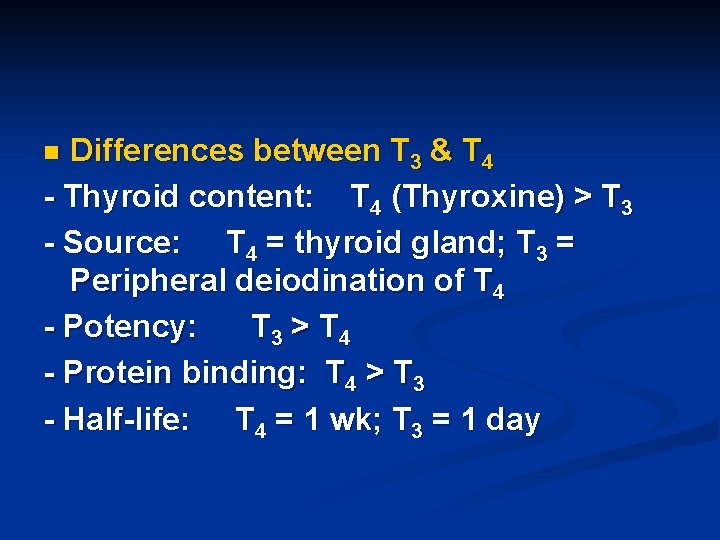
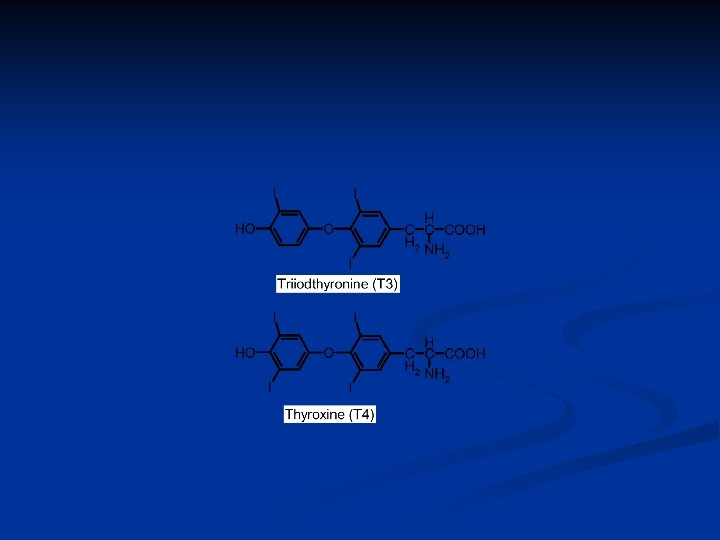
Differences between T 3 & T 4 - Thyroid content: T 4 (Thyroxine) > T 3 - Source: T 4 = thyroid gland; T 3 = Peripheral deiodination of T 4 - Potency: T 3 > T 4 - Protein binding: T 4 > T 3 - Half-life: T 4 = 1 wk; T 3 = 1 day n
General effects of thyroid hormones: - Promote growth & development - Calorigenic effect: ↑ BMR; ↑ O 2 consumption; ↑ metabolism - ↑ lipolysis - ↓ Cholesterol blood level - ↑ β-adrenergic receptors in most tissues → sweating, tachycardia (AF), palpitation, anxiety, nervousness… n
Disorders affecting the thyroid gland: ** Hypothyroidism (deficiency of thyroid hormones) In Children → Cretinism In adults → Myxedema Primary hypothyroidism – symptoms Cold intolerance, lethargy, constipation Slowing of mental function and motor activity Weight gain but appetite decreased, abnormal menses, dry/thick skin, hair loss, and hoarse voice Stroke volume and heart rate decreased R : HRT (hormonal replacement therapy) n
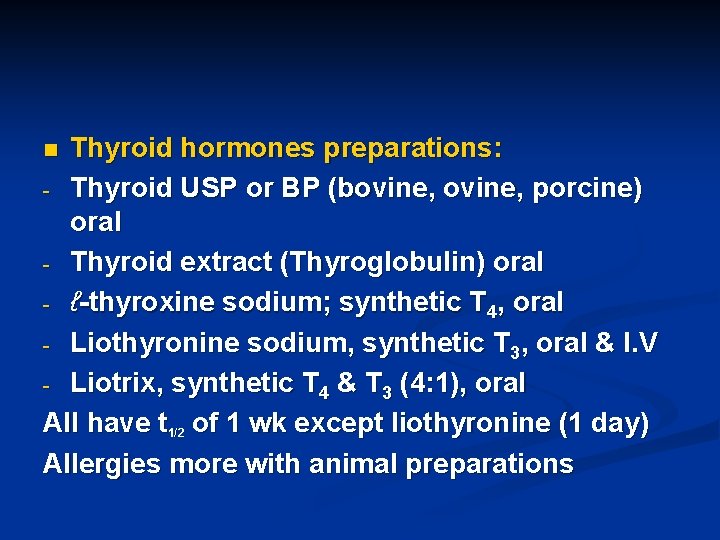
Thyroid hormones preparations: - Thyroid USP or BP (bovine, porcine) oral - Thyroid extract (Thyroglobulin) oral - ℓ-thyroxine sodium; synthetic T 4, oral - Liothyronine sodium, synthetic T 3, oral & I. V - Liotrix, synthetic T 4 & T 3 (4: 1), oral All have t 1/2 of 1 wk except liothyronine (1 day) Allergies more with animal preparations n
Clinical uses to thyroid hormones: - Hypothyroidism(Cretinism & Myxedema) Most widely used preparation: ℓ-thyroxine sodium; synthetic T 4 - Thyroid cancer - Wt. reduction (abuse!!!) Side effects to thyroid hormones: - Hyperthyroidism - Allergic reactions
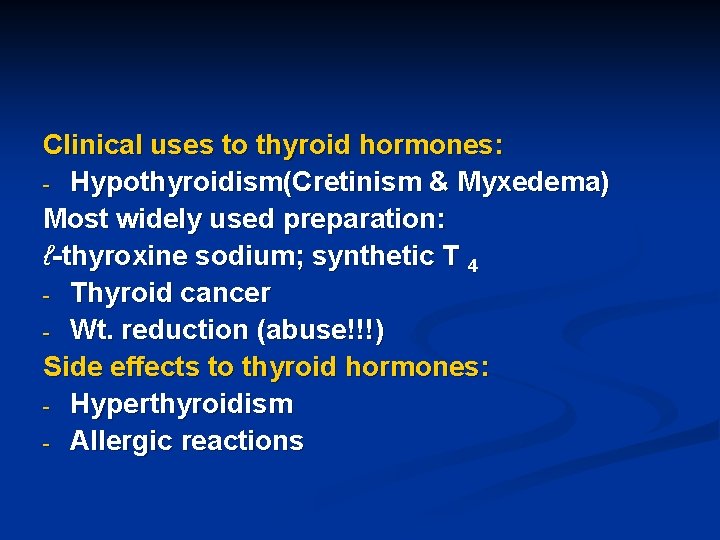
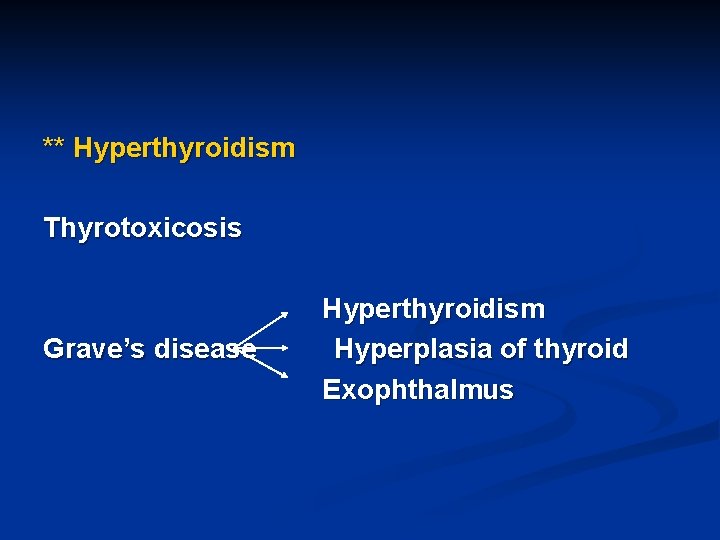
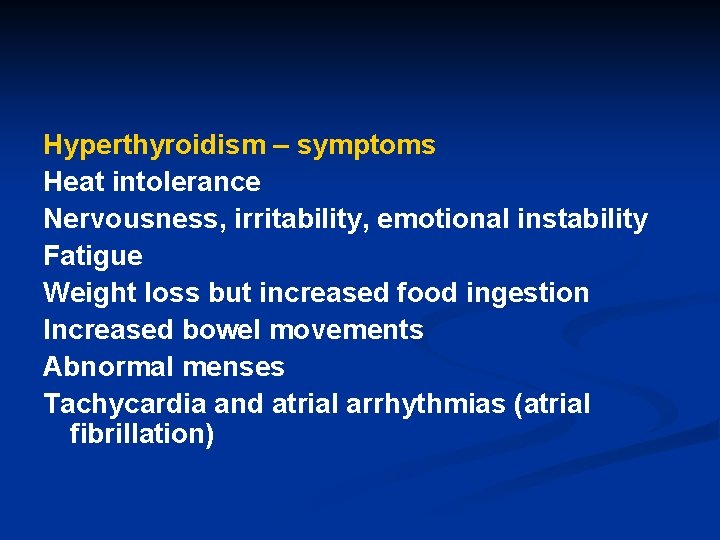
** Hyperthyroidism Thyrotoxicosis Grave’s disease Hyperthyroidism Hyperplasia of thyroid Exophthalmus
Hyperthyroidism – symptoms Heat intolerance Nervousness, irritability, emotional instability Fatigue Weight loss but increased food ingestion Increased bowel movements Abnormal menses Tachycardia and atrial arrhythmias (atrial fibrillation)
Rx of hyperthyroidism: - Propranolol - Antityroid drugs - Surgery Propranolol controls the manifestations of thyrotoxicosis It has no antithyroid activity
Antithyroid drugs: 1. Thiourea derivatives (Thioamides) Methimazole, Carbimazole, Propylthiouracil Potency: Methi. > Carbi. > Propyl. All effective orally MOA: Interfere with synthesis of T 4 & T 3 n
Side effects to thioamides: - Allergy - Hepatic dysfunction - Agranulocytosis Disadvantages: - Prolong Rx - Delayed onset of action (12 -18 hrs) - Side effects - High relapse rate - Contraindicated during pregnancy
2. Iodide (K+ or Na+); Lugol’s iodine: Solution and oral tab. MOA: ↓ synthesis, ↓ release of T 4 & T 3, ? ↓ uptake Major side effects: Allergy ( test for iodide hypersensitivity) Widely used before thyroid surgeries to ↓ vascularity of the thyroid gland
3. Radioactive iodine (131 I): Sol. , Caps. - Diagnostic use (small dose) - Rx of hyperthyroidism and Grave’s disease (intermediate dose) - Rx of thyroid Ca (large doses) Side effects: - Pulmonary fibrosis - Teratogenicity and carcinogenicity
4. Lithium carbonate: Oral and S. R tab. Has similar MOA to iodide Has narrow therapeutic window Also the drug of choice to treat manic depressive psychosis Side effects: Nausea, diarrhea, drowsiness, blurred vision Ataxia, tinnitus and diabetes insipidus
5. Iodinated contrast media: e. g. Ipodate Given orally Contain iodine+ Inhibit peripheral conversion of T 4 to T 3 Inhibit release of T 4 & T 3 Similar side effects to iodide Allergic reactions
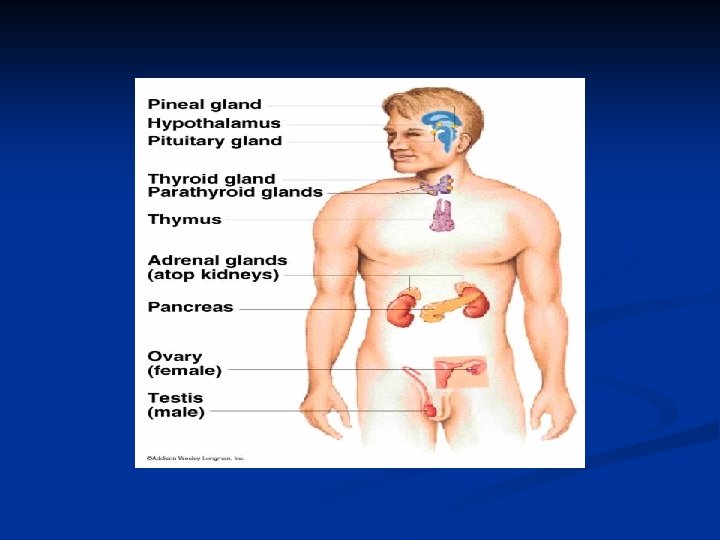
Parathyroid Gland & Calcium Metabolism
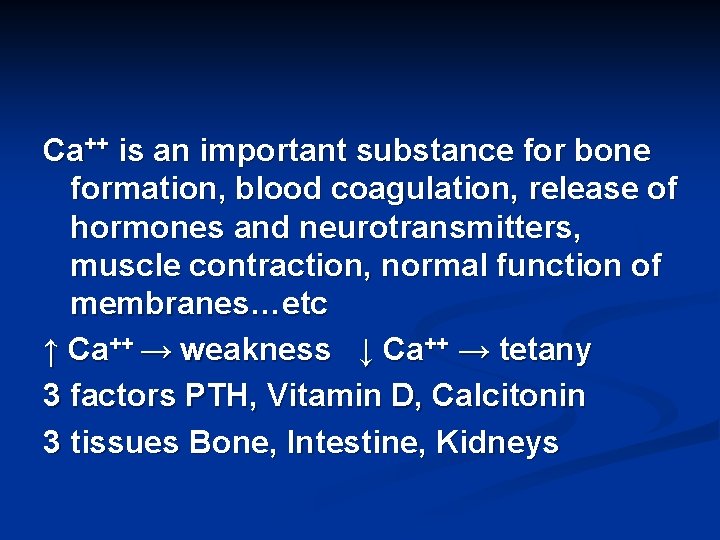
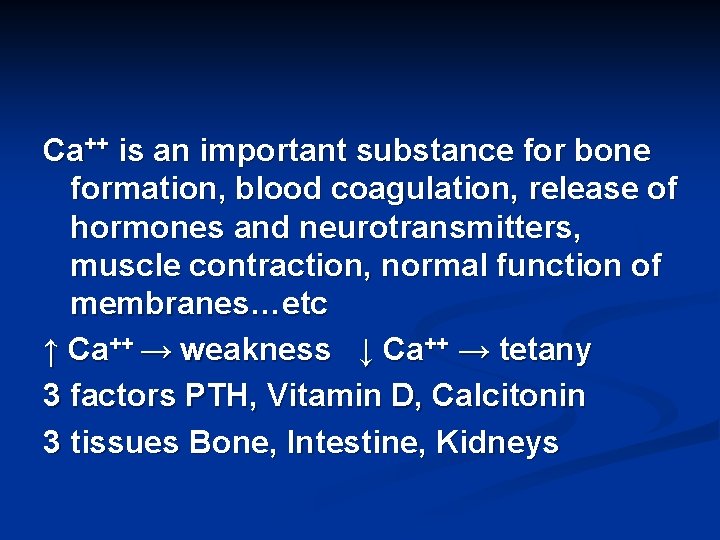
Ca++ is an important substance for bone formation, blood coagulation, release of hormones and neurotransmitters, muscle contraction, normal function of membranes…etc ↑ Ca++ → weakness ↓ Ca++ → tetany 3 factors PTH, Vitamin D, Calcitonin 3 tissues Bone, Intestine, Kidneys
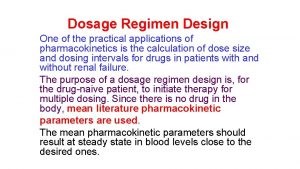
![Parathyroid Hormone PTH Regulation of synthesis release Ca PTH Parathyroid Hormone (PTH) Regulation of synthesis & release: ↑ [Ca++] → ↓ PTH; ↓](https://slidetodoc.com/presentation_image_h2/4ed5b004199d61801f352f945ecaabba/image-53.jpg)
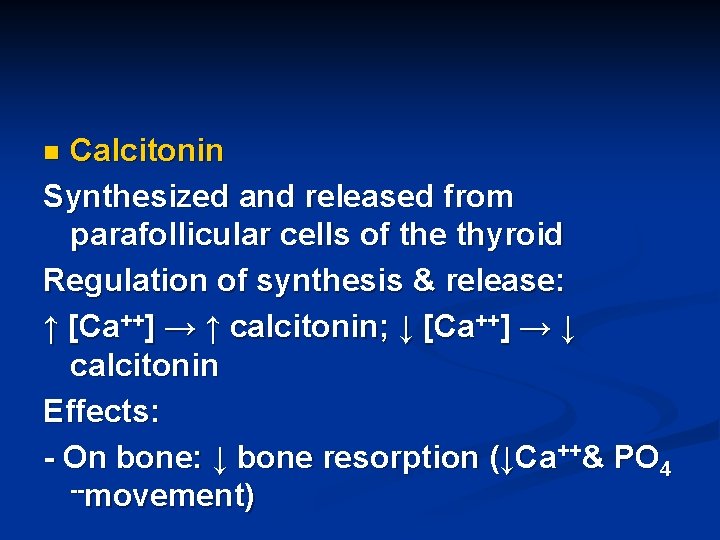
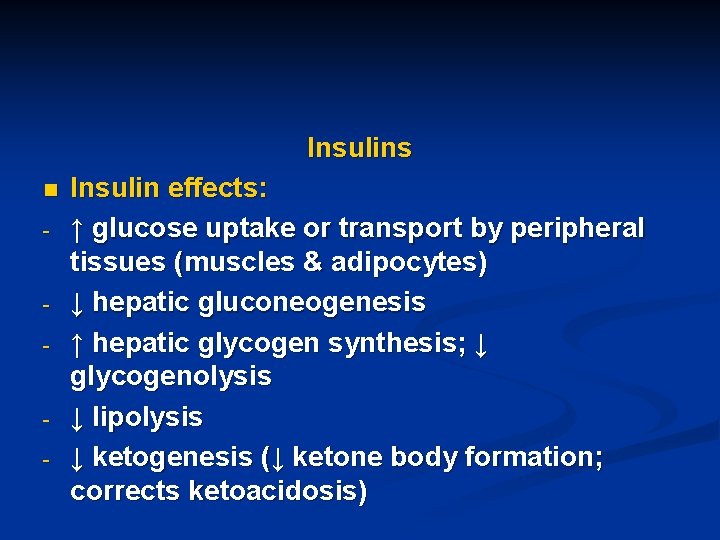
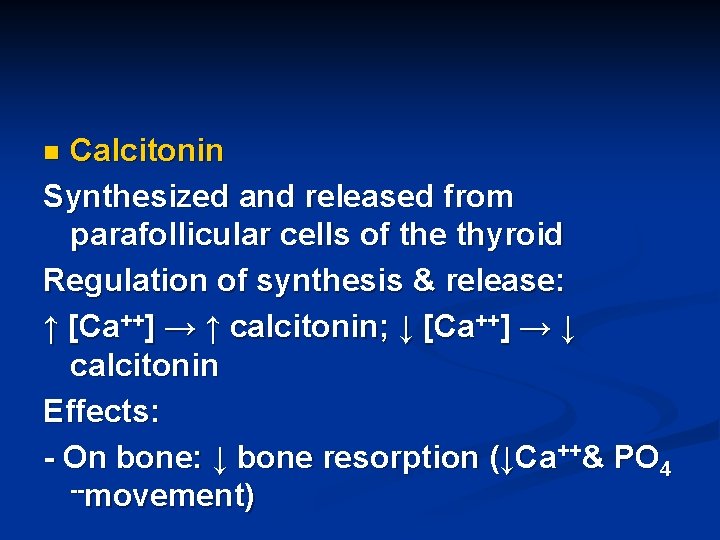
Parathyroid Hormone (PTH) Regulation of synthesis & release: ↑ [Ca++] → ↓ PTH; ↓ [Ca++] → ↑ PTH Little if any regulation by PO 4 -Effects of PTH: - On bone (1º target tissue): PTH ↑ resorption of Ca++& PO 4 -- (↑ movement of Ca++& PO 4 -- from bone to blood) (c. AMP) mediated effect n
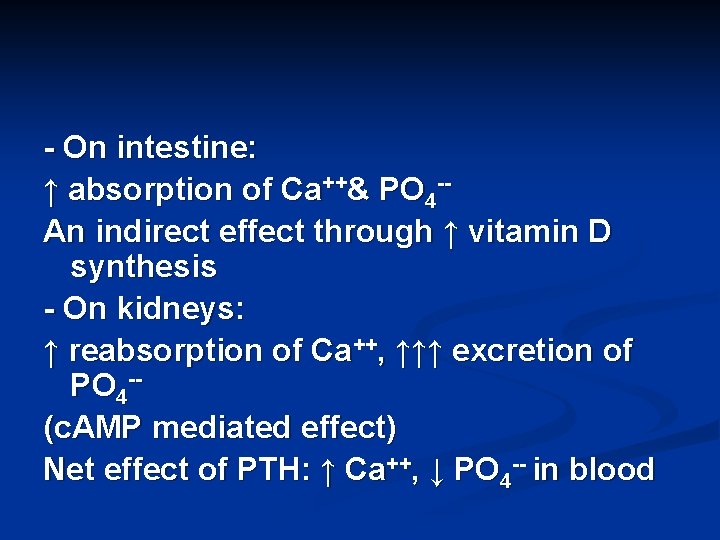
- On intestine: ↑ absorption of Ca++& PO 4 -An indirect effect through ↑ vitamin D synthesis - On kidneys: ↑ reabsorption of Ca++, ↑↑↑ excretion of PO 4 -(c. AMP mediated effect) Net effect of PTH: ↑ Ca++, ↓ PO 4 -- in blood
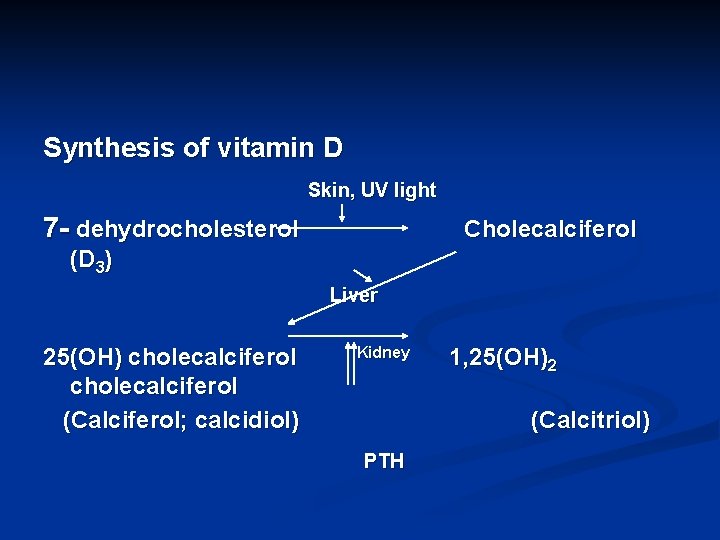
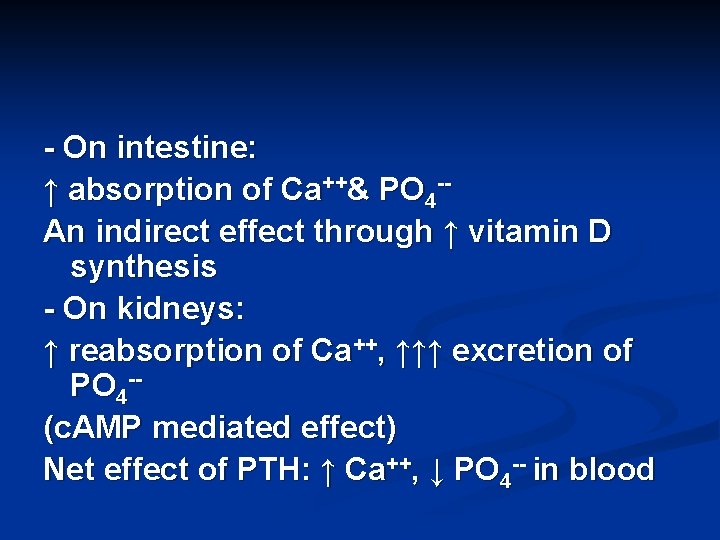
Synthesis of vitamin D Skin, UV light 7 - dehydrocholesterol Cholecalciferol (D 3) Liver 25(OH) cholecalciferol (Calciferol; calcidiol) Kidney 1, 25(OH)2 (Calcitriol) PTH
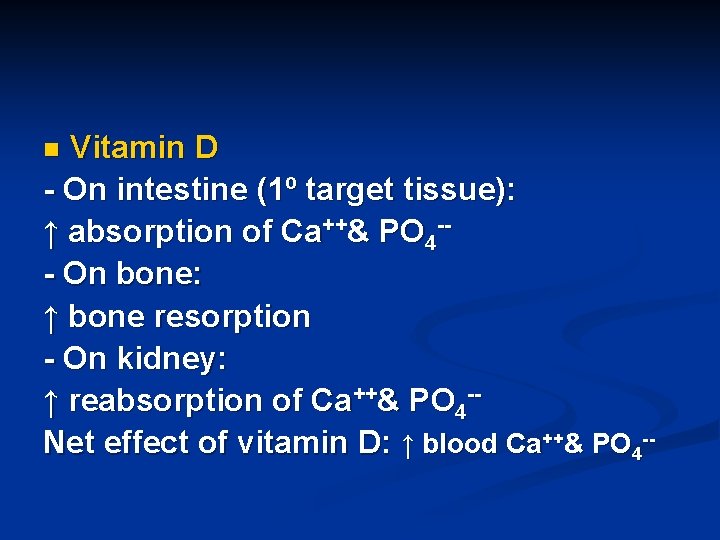
Vitamin D - On intestine (1º target tissue): ↑ absorption of Ca++& PO 4 -- On bone: ↑ bone resorption - On kidney: ↑ reabsorption of Ca++& PO 4 -Net effect of vitamin D: ↑ blood Ca++& PO 4 -n
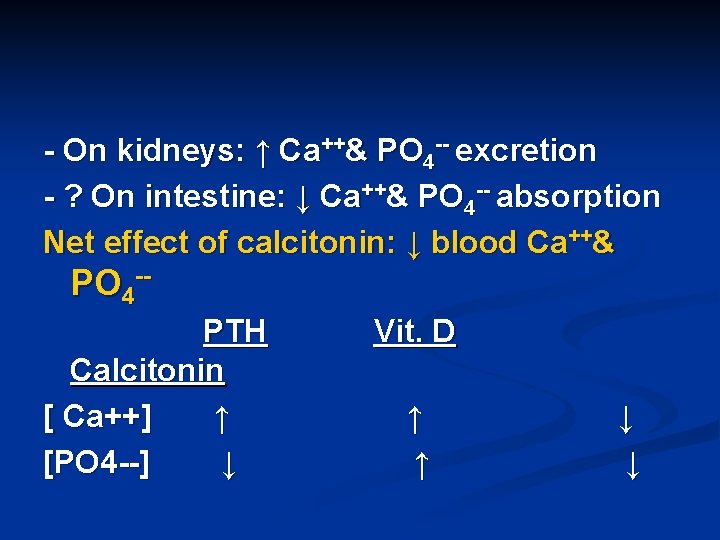
Calcitonin Synthesized and released from parafollicular cells of the thyroid Regulation of synthesis & release: ↑ [Ca++] → ↑ calcitonin; ↓ [Ca++] → ↓ calcitonin Effects: - On bone: ↓ bone resorption (↓Ca++& PO 4 --movement) n
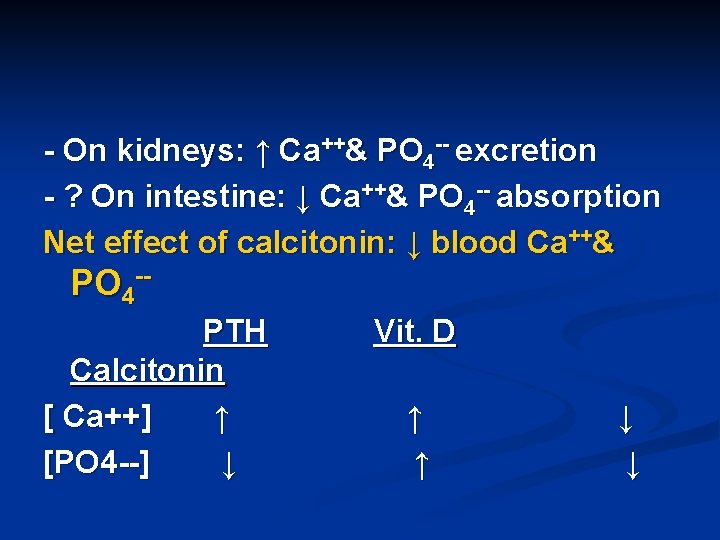
- On kidneys: ↑ Ca++& PO 4 -- excretion - ? On intestine: ↓ Ca++& PO 4 -- absorption Net effect of calcitonin: ↓ blood Ca++& PO 4 -PTH Calcitonin [ Ca++] ↑ [PO 4 --] ↓ Vit. D ↑ ↑ ↓ ↓
![Disorders affecting the parathyroids Hyposecretion hypoparathyroidism Ca Causes Thyroidectomy most common Disorders affecting the parathyroids: ** Hyposecretion (hypoparathyroidism): ↓ [Ca++] Causes: - Thyroidectomy (most common](https://slidetodoc.com/presentation_image_h2/4ed5b004199d61801f352f945ecaabba/image-59.jpg)
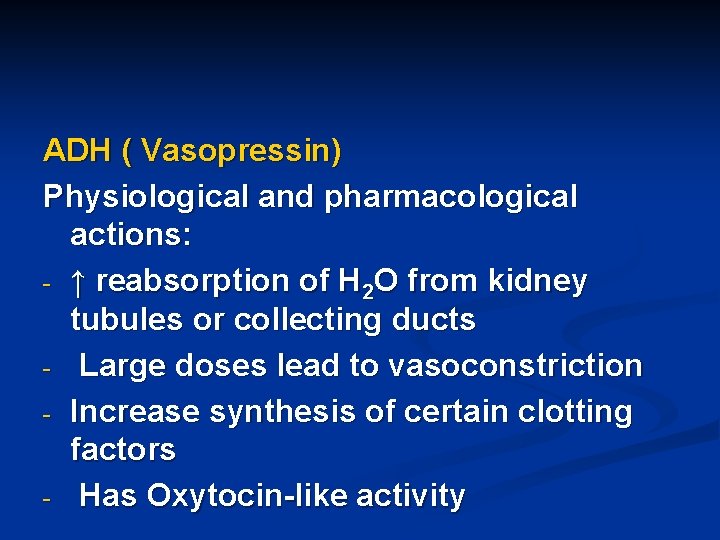
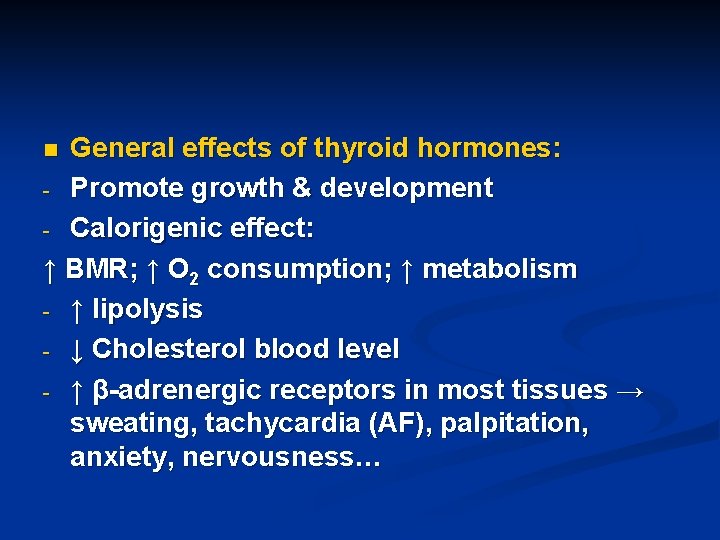
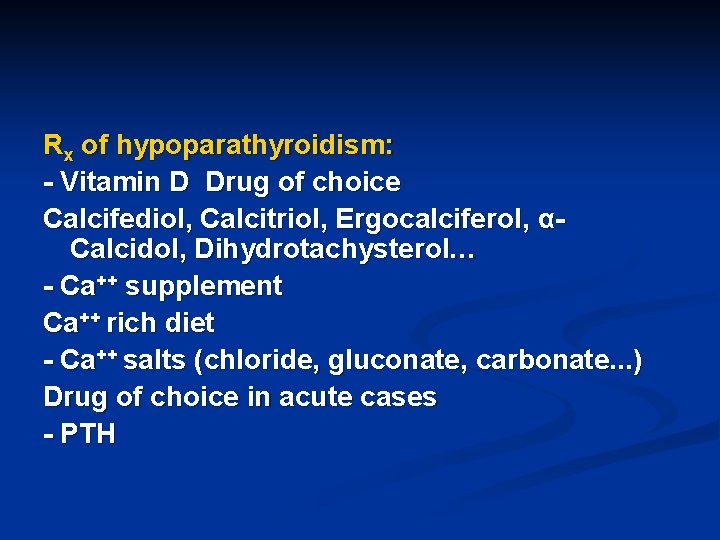
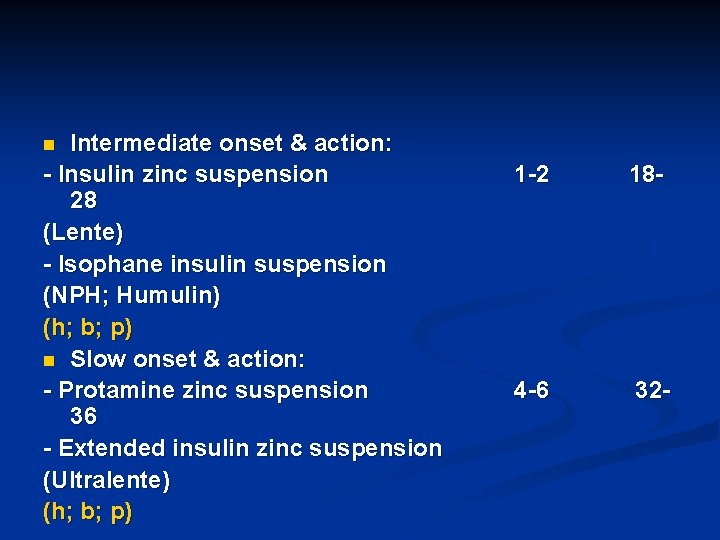
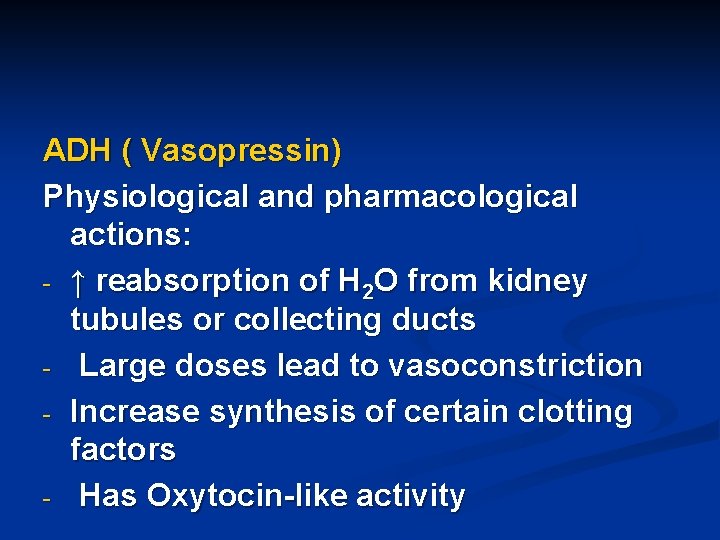
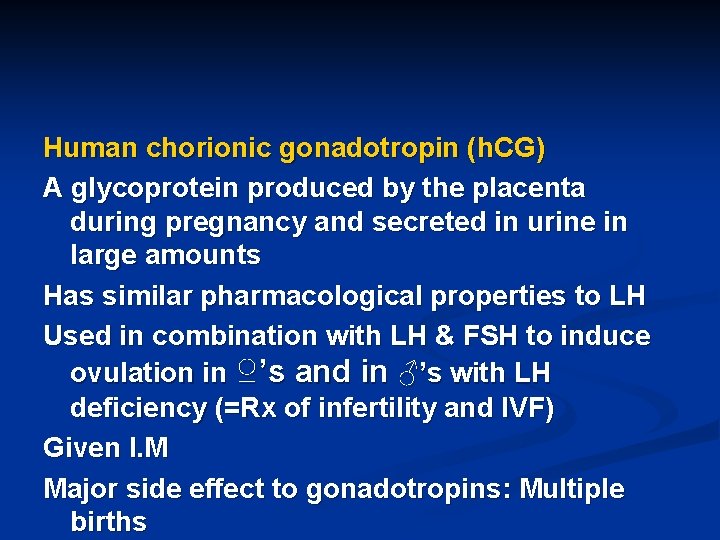
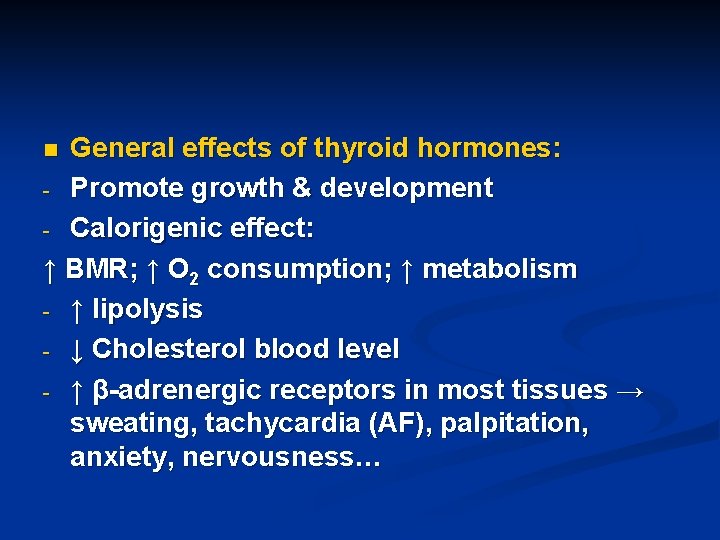
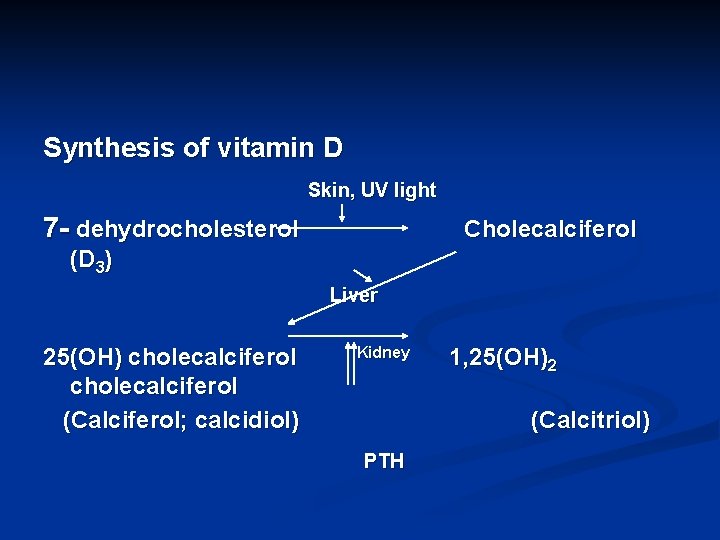
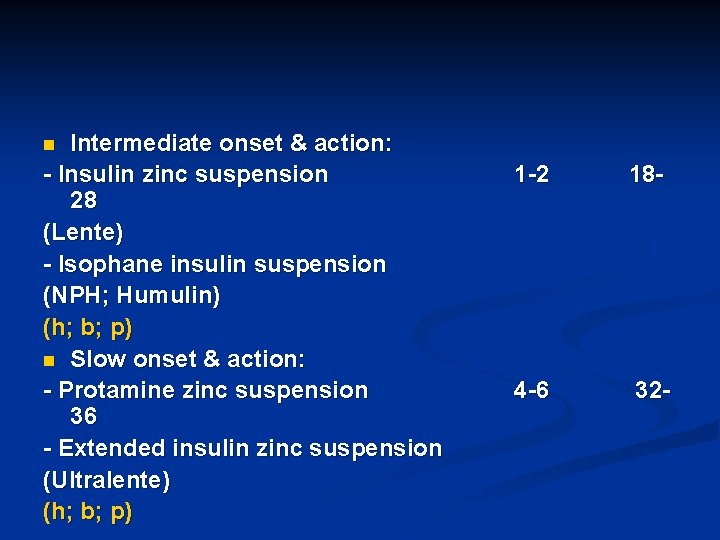
Disorders affecting the parathyroids: ** Hyposecretion (hypoparathyroidism): ↓ [Ca++] Causes: - Thyroidectomy (most common cause) - Idiopathic - ↓ sensitivity of target tissues to PTH (pseudohypoparathyroidism) n
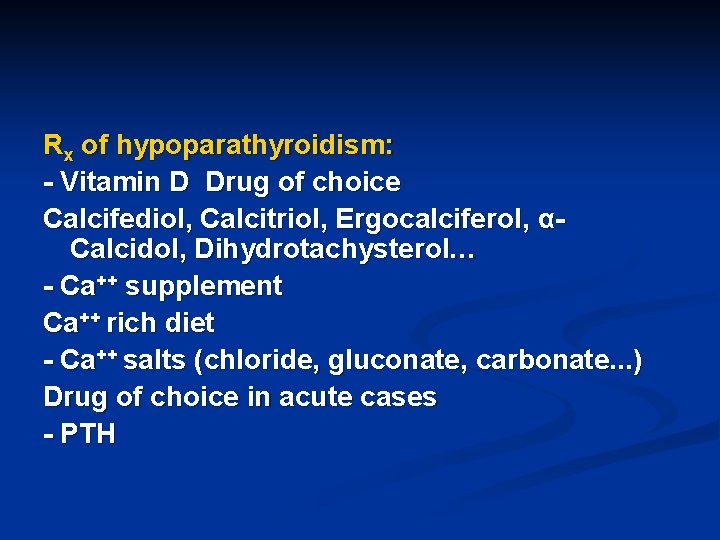
Rx of hypoparathyroidism: - Vitamin D Drug of choice Calcifediol, Calcitriol, Ergocalciferol, αCalcidol, Dihydrotachysterol… - Ca++ supplement Ca++ rich diet - Ca++ salts (chloride, gluconate, carbonate. . . ) Drug of choice in acute cases - PTH
![Hypersecretion hyperparathyroidism Ca Causes 1º hyperparathyroidism adenomas 2º hyperparathyroidism 2º ** Hypersecretion (hyperparathyroidism): ↑ [Ca++] Causes: - 1º hyperparathyroidism (adenomas) - 2º hyperparathyroidism 2º](https://slidetodoc.com/presentation_image_h2/4ed5b004199d61801f352f945ecaabba/image-61.jpg)
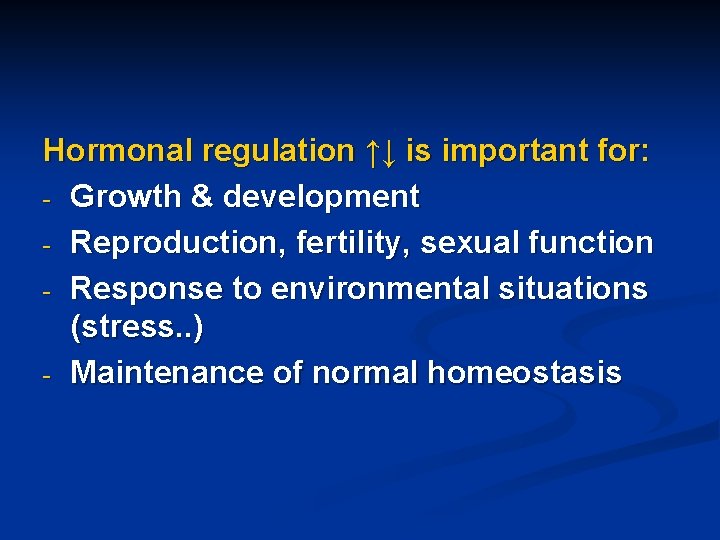
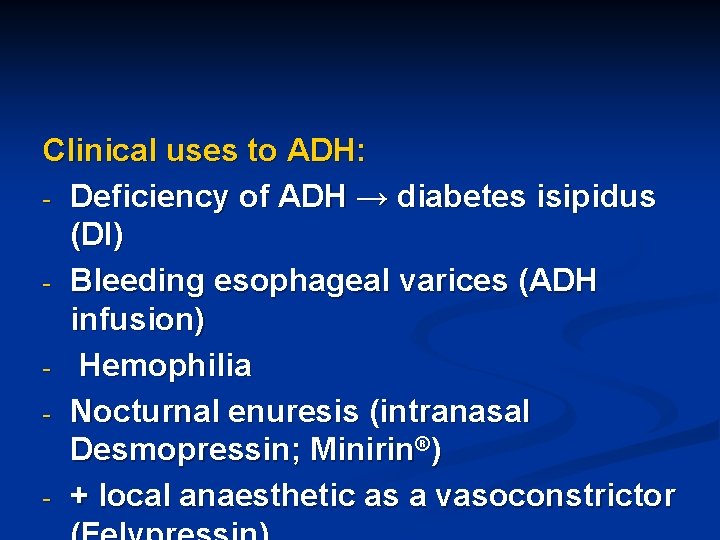
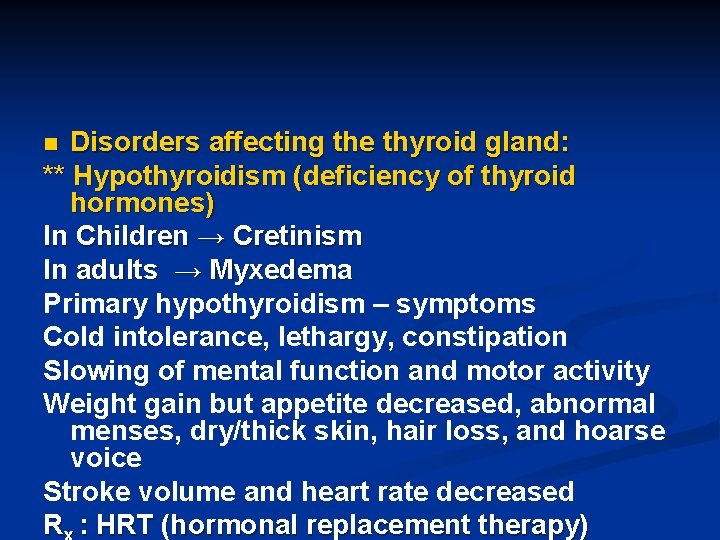
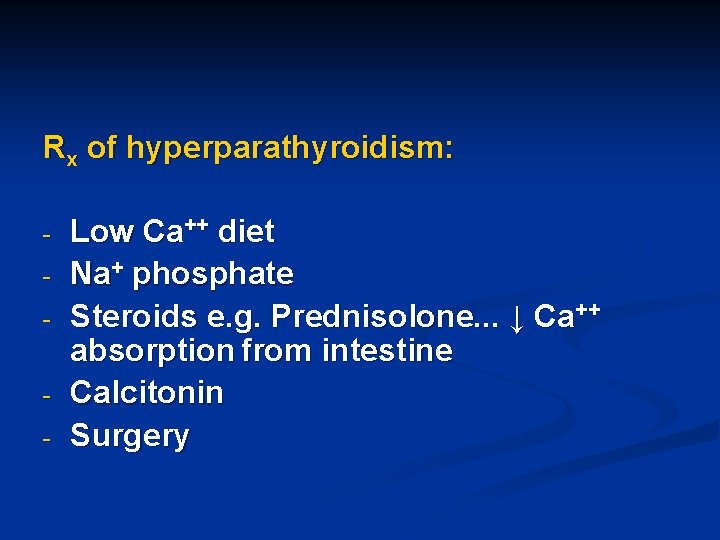
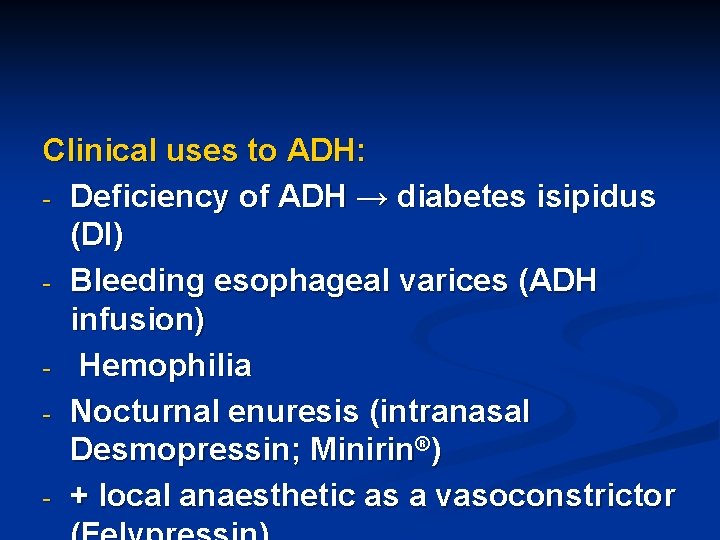
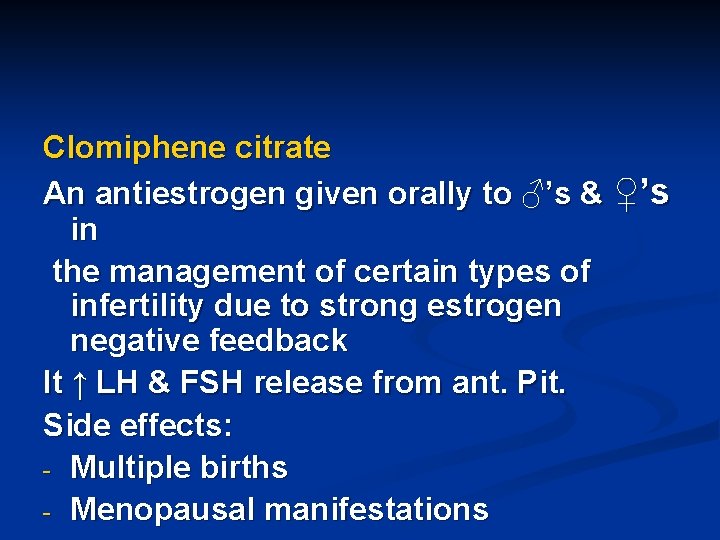
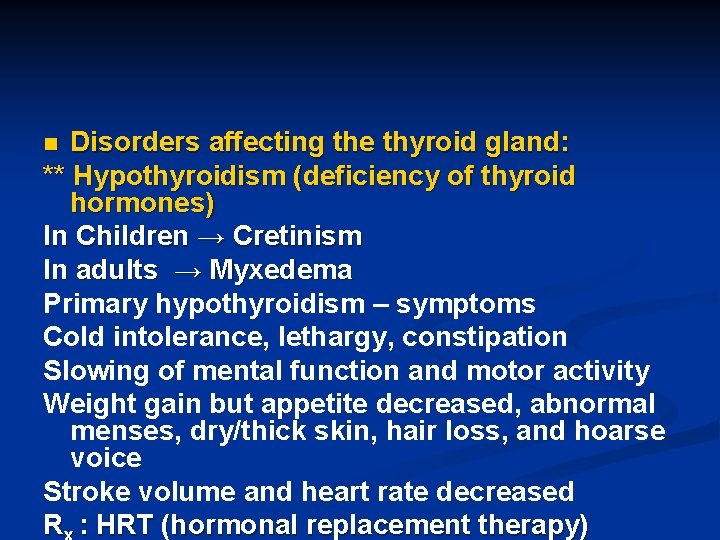
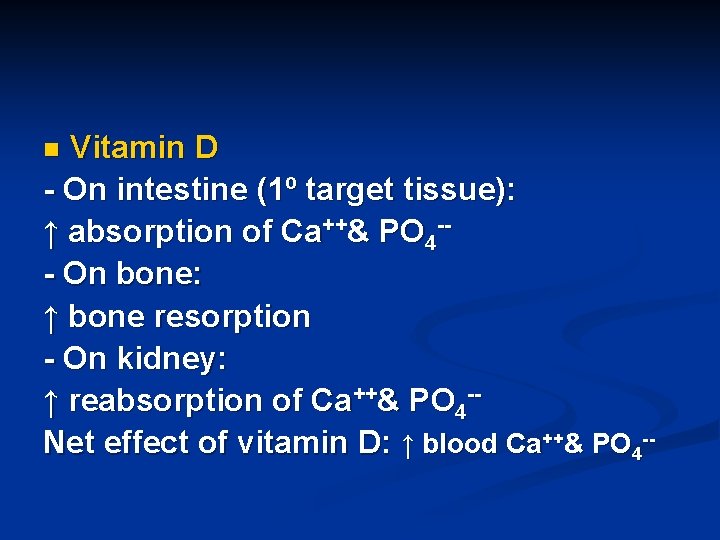
** Hypersecretion (hyperparathyroidism): ↑ [Ca++] Causes: - 1º hyperparathyroidism (adenomas) - 2º hyperparathyroidism 2º to any cause of hypocalcemia e. g. malabsorption syndrome, renal disease…
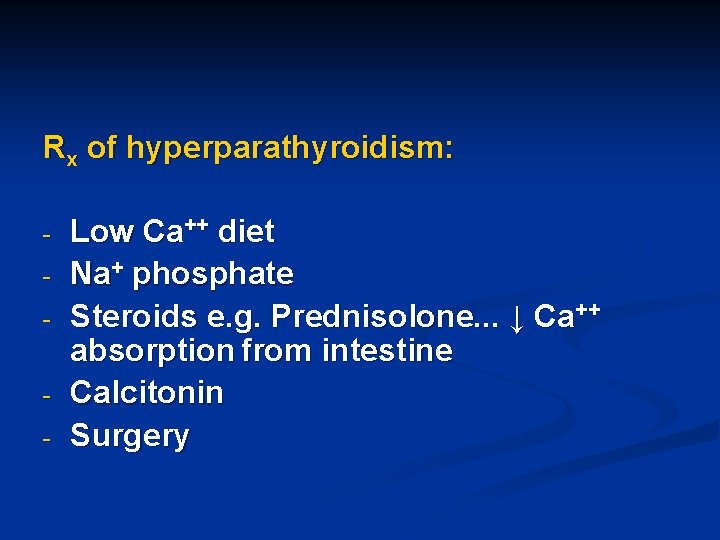
Rx of hyperparathyroidism: - Low Ca++ diet Na+ phosphate Steroids e. g. Prednisolone. . . ↓ Ca++ absorption from intestine Calcitonin Surgery
Paget’s disease Rare bone disorder characterized by demineralization of bone, disorganized bone formation, ↑ bone resorption, fractures, spinal cord injuries, deafness… R x: - Salmon calcitonin (drug of choice), S. C, I. M. Effective in all cases of hypercalcemia irrespective of its causes - Biophosphanates, orally Etidronate, alendronate, residronate, pamidronate… n
Adrenal Steroids Mineralocorticoids & Glucocorticoids
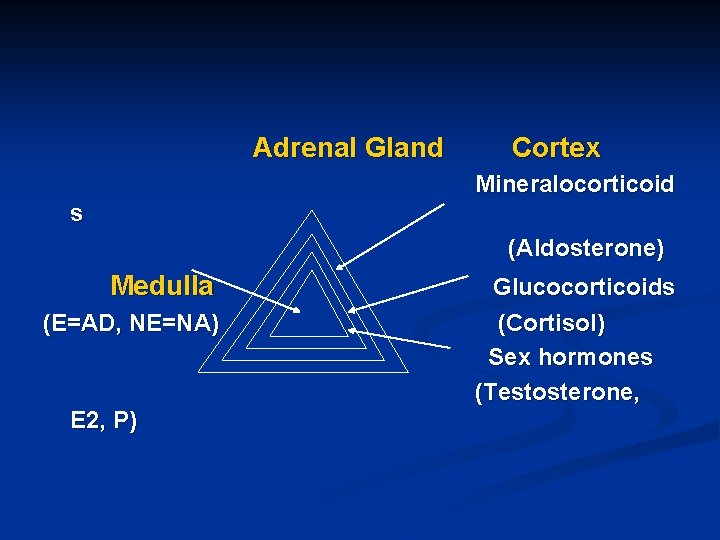
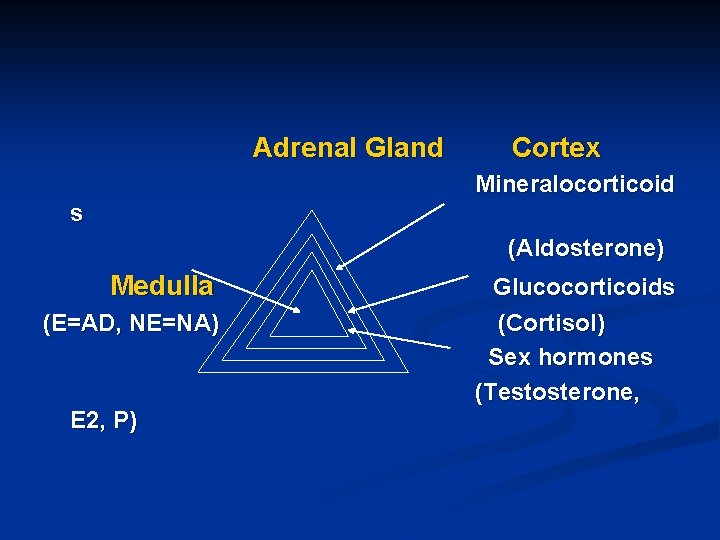
Adrenal Gland Cortex Mineralocorticoid s (Aldosterone) Medulla (E=AD, NE=NA) E 2, P) Glucocorticoids (Cortisol) Sex hormones (Testosterone,
Mineralocorticoids (Aldosterone) Synthesis: From cholesterol Synthesis and release are under the control of renin –angiotensin aldosterone system Aldosterone effects: ↑ reabsorption of Na+ and H 2 O from kidney tubules → ↑ BP, ↑ excretion of K+ → hypokalemia Aldosterone is not used clinically n
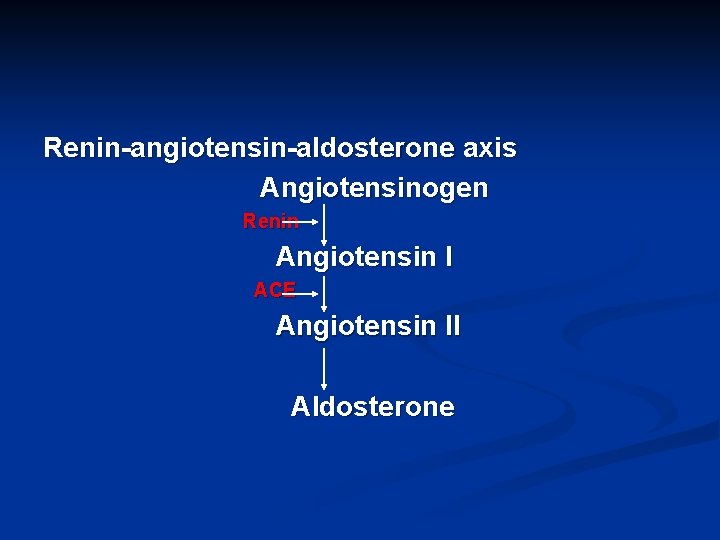
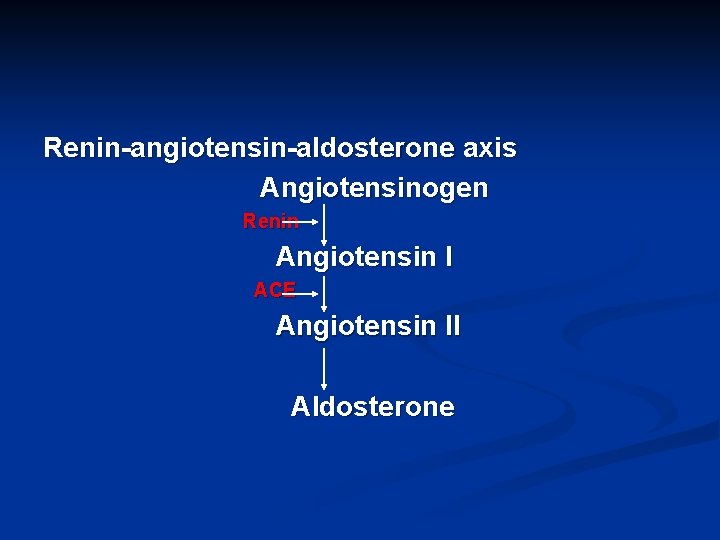
Renin-angiotensin-aldosterone axis Angiotensinogen Renin Angiotensin I ACE Angiotensin II Aldosterone
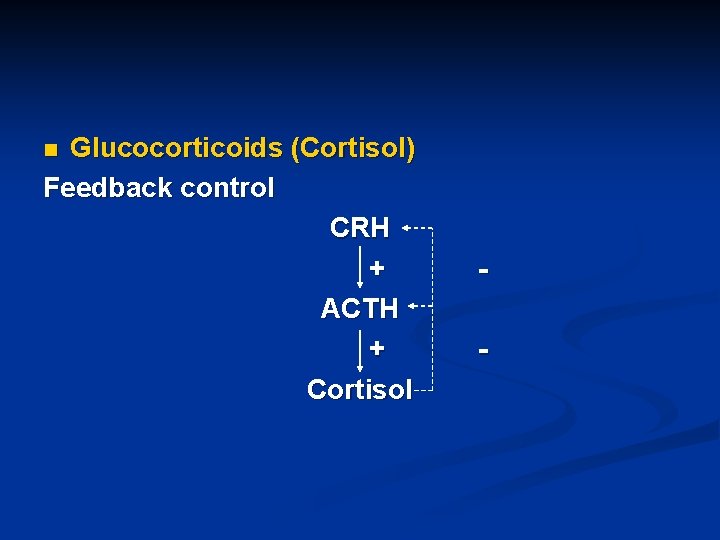
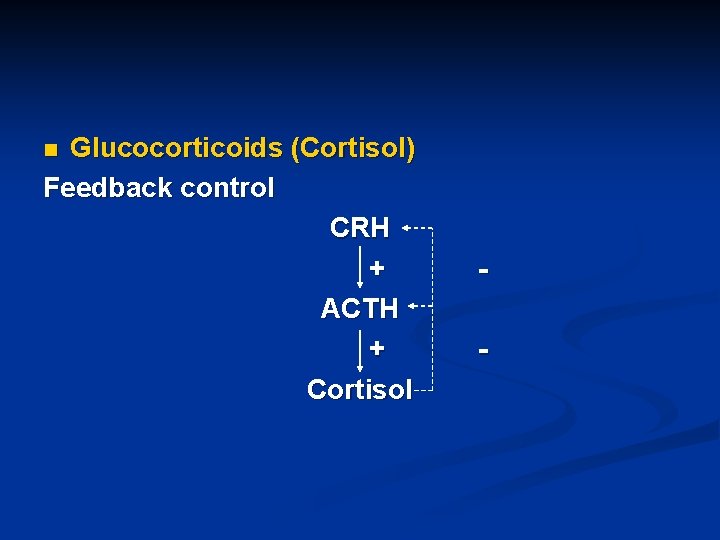
Glucocorticoids (Cortisol) Feedback control CRH + ACTH + Cortisol n -
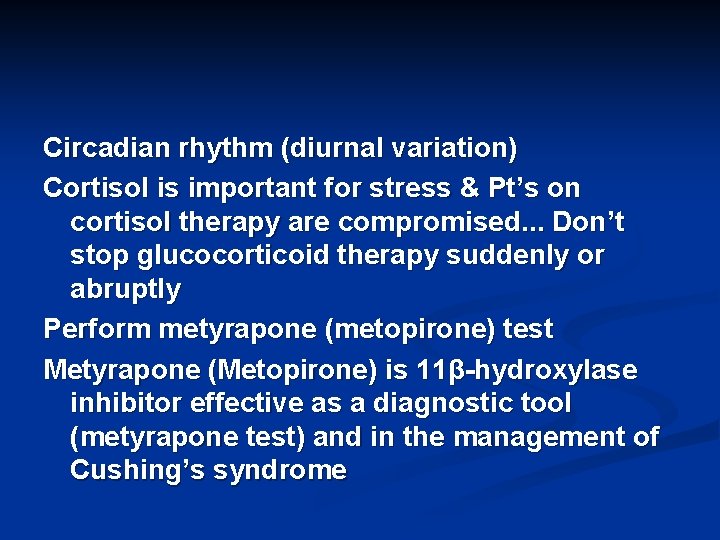
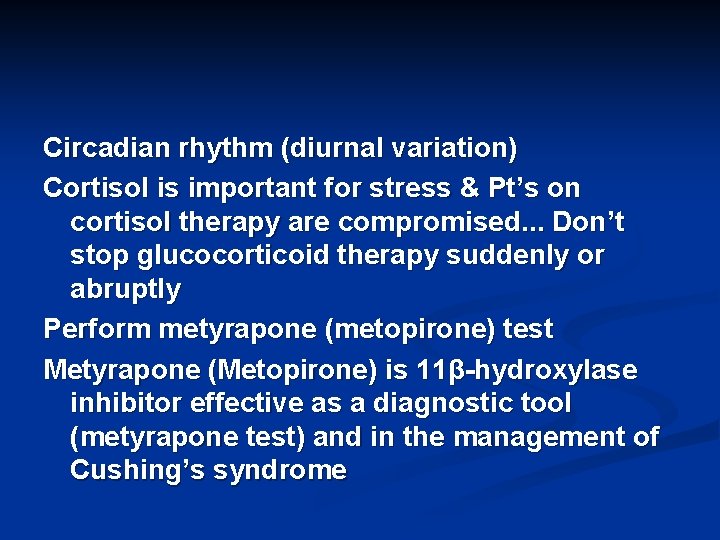
Circadian rhythm (diurnal variation) Cortisol is important for stress & Pt’s on cortisol therapy are compromised. . . Don’t stop glucocorticoid therapy suddenly or abruptly Perform metyrapone (metopirone) test Metyrapone (Metopirone) is 11β-hydroxylase inhibitor effective as a diagnostic tool (metyrapone test) and in the management of Cushing’s syndrome
Cortisol synthesis (from cholesterol)
Pharmacological effects/side effects to cortisol: - On proteins ↑ Catabolism ↓ anabolism → Osteoporosis; steroid myopathy; delayed wound healing; delayed peptic ulcer healing…) - On CHO ↑ blood sugar level ( ↑ gluconeogenesis; ↓ peripheral utilization of glucose)
On lipids ↑ lipolysis Fat redistribution (moon face; abdominal obesity…) - On electrolytes Aldosterone-like effect (↑ Na+; ↓ K+) ↓ Ca++ absorption from intestine ↑ Ca++ excretion by kidney ↑ uric acid excretion -
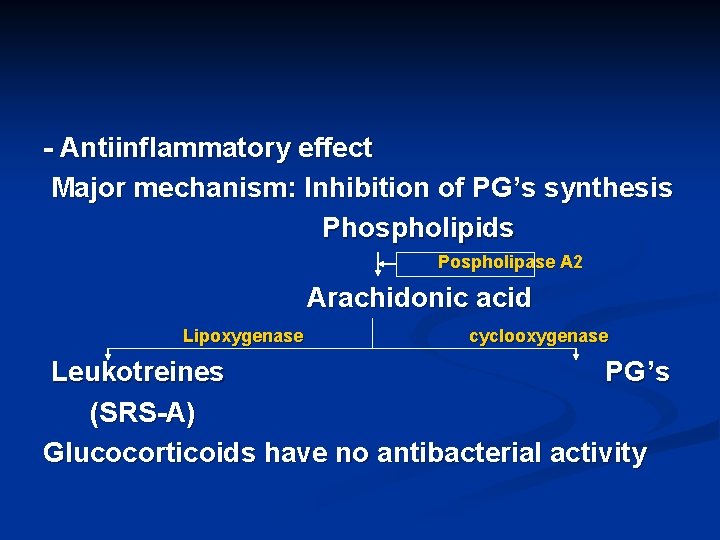
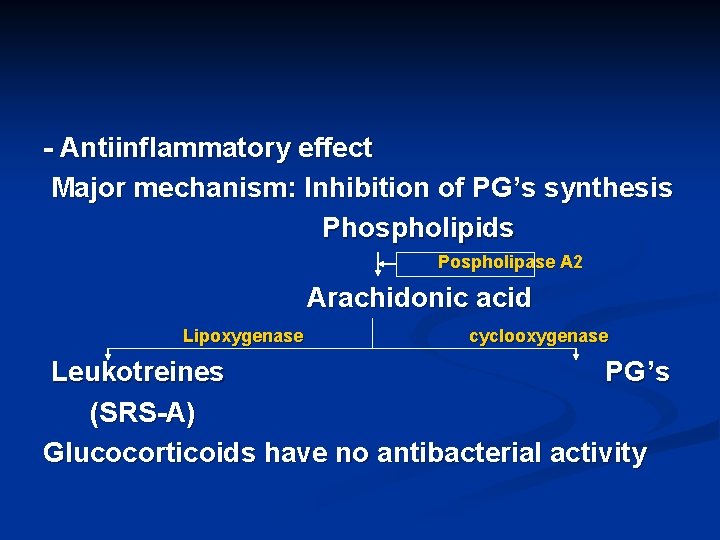
- Antiinflammatory effect Major mechanism: Inhibition of PG’s synthesis Phospholipids Pospholipase A 2 Arachidonic acid Lipoxygenase cyclooxygenase Leukotreines PG ’s (SRS-A) Glucocorticoids have no antibacterial activity
Immunosuppressant effect - Antiallergic effect; suppress allergic response ↓ histamine release - Ulcerogenic effect Gastric and duodenal ulcers - CNS manifestations Euphoria; psychosis… - cataract -
Clinical uses to glucocorticoids: - Adrenal insufficiency (HRT): (acute; chronic, Addisonian crisis, Addison’s disease. . . ) - Inflammatory conditions: (rheumatoid arthritis, SLE, arteritis, dermatomycosis, cerebral edema, ulcerative colitis, rheumatic carditis, active chronic hepatitis, proctitis, acute gout. . . ) - Allergic reactions: drug-induced allergy, hay fever, eczema, dermatitis, bronchial asthma, status asthmaticus
- - - Immunosuppressant effect (organ transplantation, hemolytic anemia, leukemias, many tumors. . . ) Hypercalcemia associated with Vit. D intoxication or sarcoidosis or cancer or hyperparathyroidism. . . ) Many eye, ear, and skin diseases (allergic or inflammatory)
Glucocorticoids dosage forms Available in all dosage forms Available in many preparations Structure activity relationship Major objective: Good antiinflammatory effect, less or no aldosterone-like activity Metabolism: In the liver by reduction and conjugation (9095%); little hydroxylation reactions (5%)
Glucocorticoid preparations: Corisol; Hydrocortisone; Cortisone; Prednisolone; Prednisone; Fludrocortisone; Corticosterone; Triamcinolone; Dexamethasone… Differ in pharmacokinetic parameters
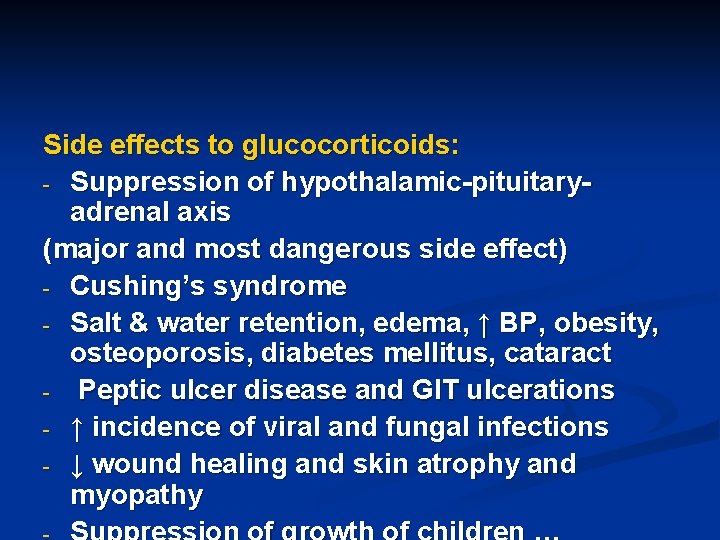
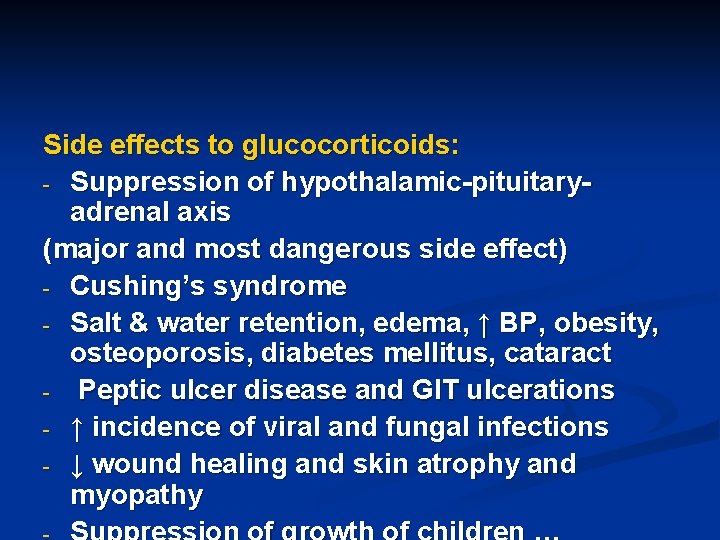
Side effects to glucocorticoids: - Suppression of hypothalamic-pituitaryadrenal axis (major and most dangerous side effect) - Cushing’s syndrome - Salt & water retention, edema, ↑ BP, obesity, osteoporosis, diabetes mellitus, cataract - Peptic ulcer disease and GIT ulcerations - ↑ incidence of viral and fungal infections - ↓ wound healing and skin atrophy and myopathy
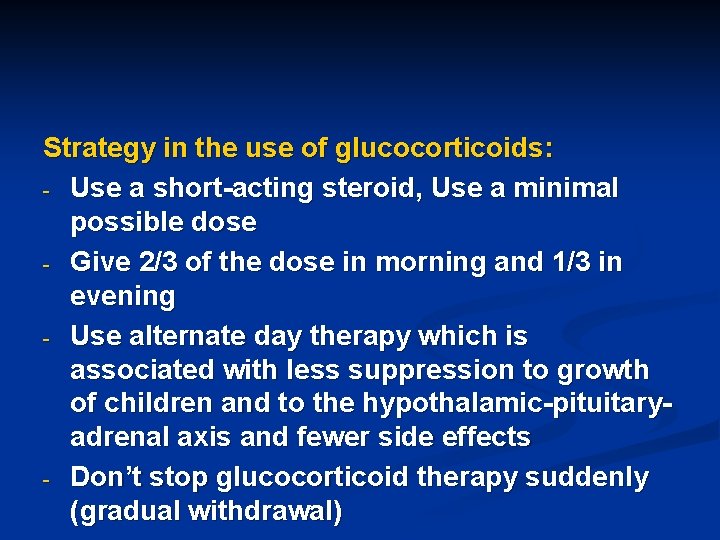
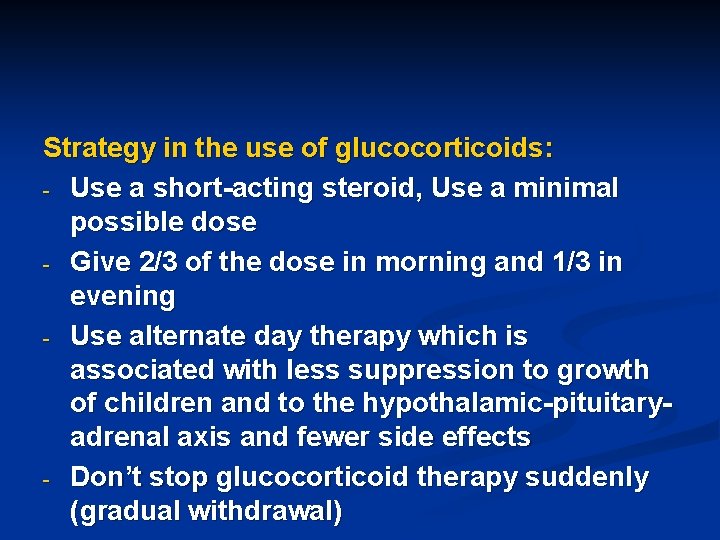
Strategy in the use of glucocorticoids: - Use a short-acting steroid, Use a minimal possible dose - Give 2/3 of the dose in morning and 1/3 in evening - Use alternate day therapy which is associated with less suppression to growth of children and to the hypothalamic-pituitaryadrenal axis and fewer side effects - Don’t stop glucocorticoid therapy suddenly (gradual withdrawal)
Pancreatic Hormones
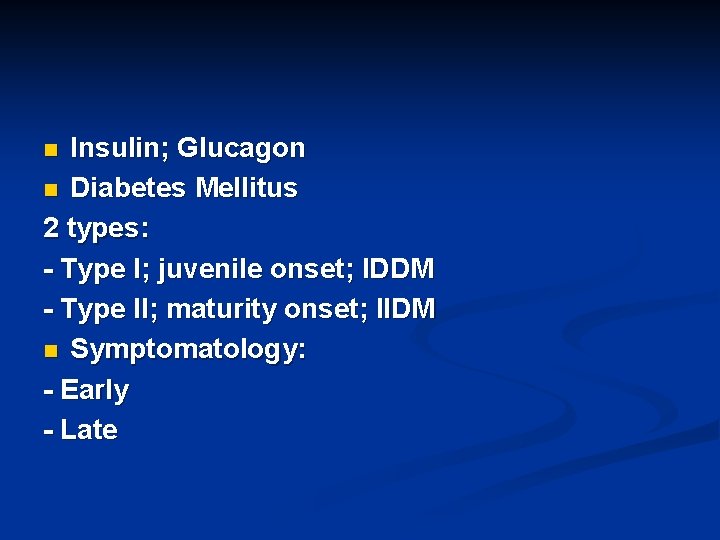
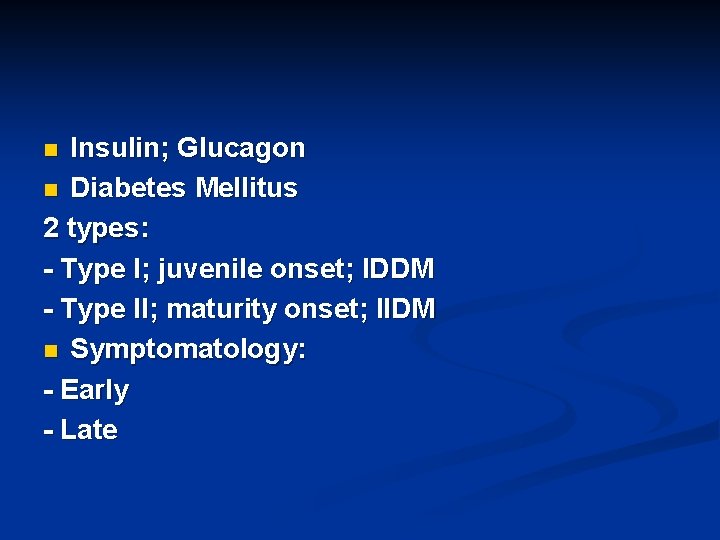
Insulin; Glucagon n Diabetes Mellitus 2 types: - Type I; juvenile onset; IDDM - Type II; maturity onset; IIDM n Symptomatology: - Early - Late n
Early manifestations: Polyuria Polydipsia Polyphagia Ketoacidosis (type I) Diet & insulin correct immediately these symptoms n
Late complications: Atherosclerosis & IHD Retinopathy Nephropathy Neuropathy ? Insulin will prevent these symptoms Strong evidence suggests that good control of DM will at least delay onset of such symptoms n
Diagnosis: - Clinical manifestations - Lab. Tests: Random blood sugar (RBS) Fasting blood sugar Glycosylated hemoglobin Glucose tolerance test n
Management: - Type I: Diet + Insulin therapy Oral hypoglycemic agents are ineffective - Type II: Diet & exercise ± Oral hypoglycemic agents ± Insulin (insulin resistance; pre-receptor; post-receptor mechanisms) n
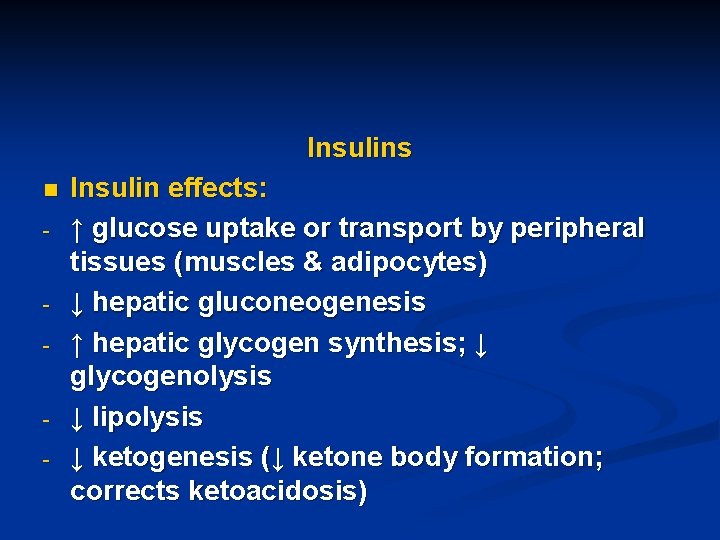
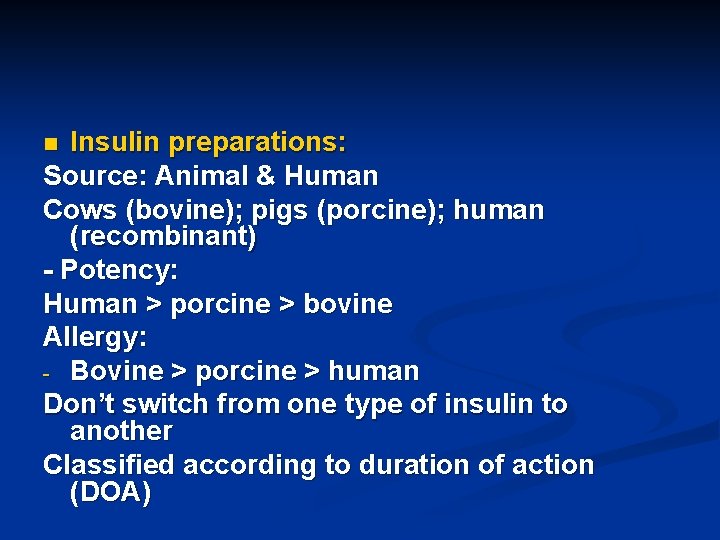
Insulins n - - - Insulin effects: ↑ glucose uptake or transport by peripheral tissues (muscles & adipocytes) ↓ hepatic gluconeogenesis ↑ hepatic glycogen synthesis; ↓ glycogenolysis ↓ lipolysis ↓ ketogenesis (↓ ketone body formation; corrects ketoacidosis)
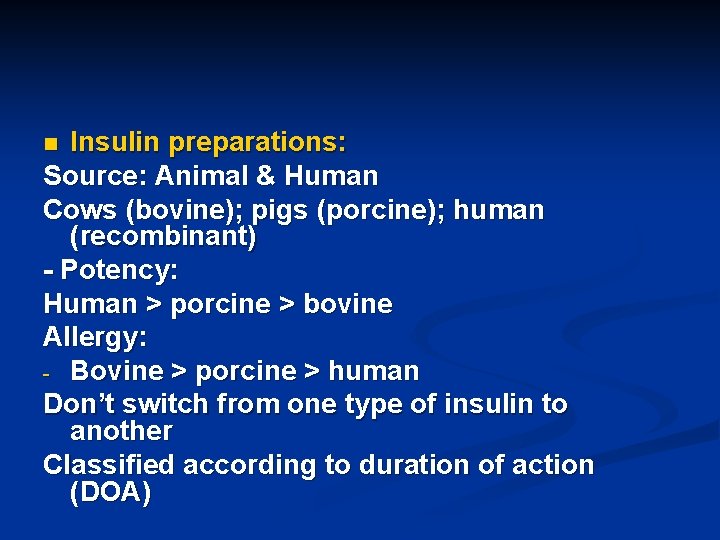
Insulin preparations: Source: Animal & Human Cows (bovine); pigs (porcine); human (recombinant) - Potency: Human > porcine > bovine Allergy: - Bovine > porcine > human Don’t switch from one type of insulin to another Classified according to duration of action (DOA) n
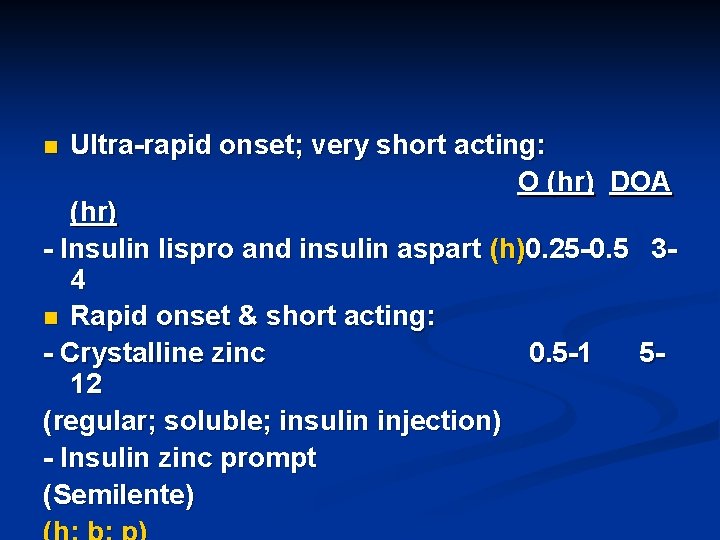
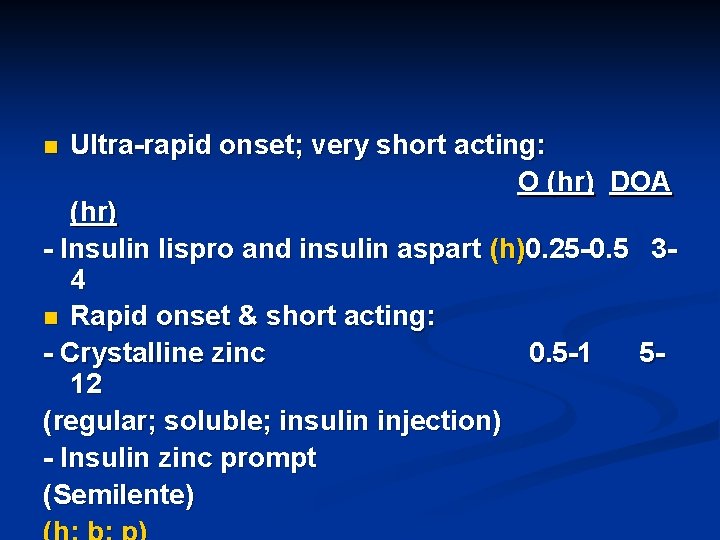
Ultra-rapid onset; very short acting: O (hr) DOA (hr) - Insulin lispro and insulin aspart (h)0. 25 -0. 5 34 n Rapid onset & short acting: - Crystalline zinc 0. 5 -1 512 (regular; soluble; insulin injection) - Insulin zinc prompt (Semilente) n
Intermediate onset & action: - Insulin zinc suspension 28 (Lente) - Isophane insulin suspension (NPH; Humulin) (h; b; p) n Slow onset & action: - Protamine zinc suspension 36 - Extended insulin zinc suspension (Ultralente) (h; b; p) n 1 -2 18 - 4 -6 32 -

Insulin Glargine (h) 24 -36 (peakless insulin) Insulin detemir (h) 24 -36 n Mixed insulins: Int. + short 20 -24 Int. + long 22 -24 (h; b; p) 1 -2 0. 5 -1 2 -4
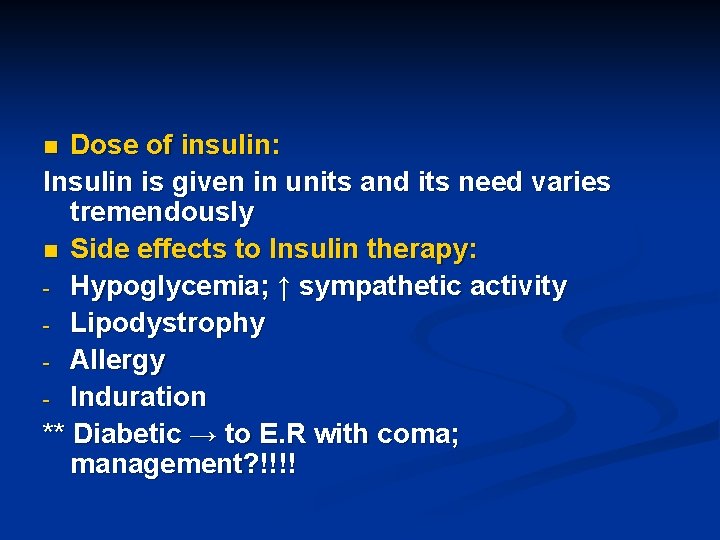
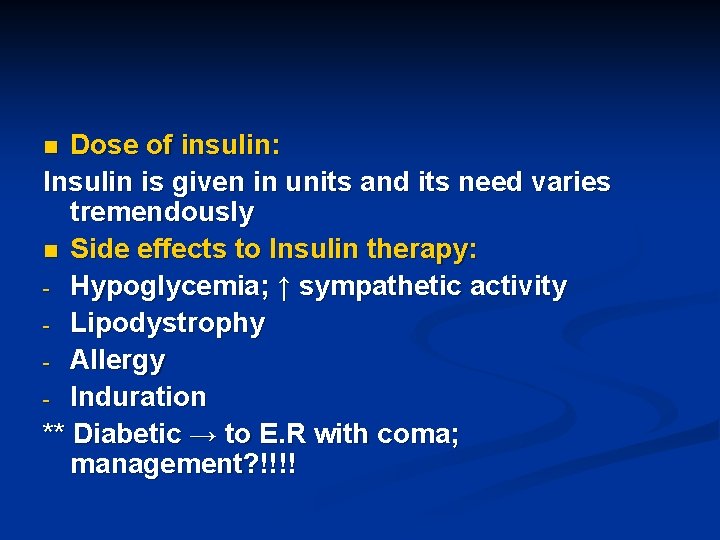
Dose of insulin: Insulin is given in units and its need varies tremendously n Side effects to Insulin therapy: - Hypoglycemia; ↑ sympathetic activity - Lipodystrophy - Allergy - Induration ** Diabetic → to E. R with coma; management? !!!! n
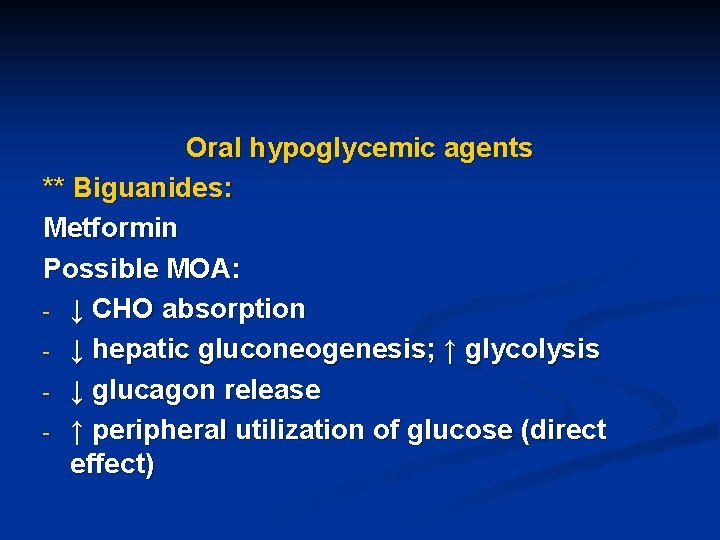
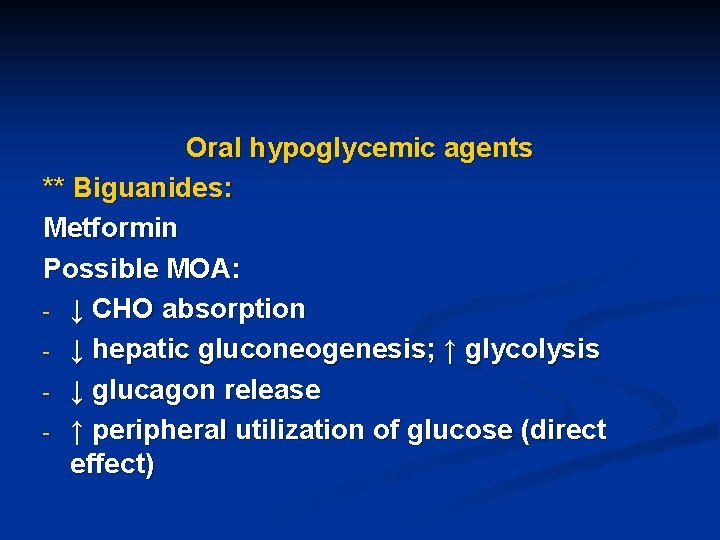
Oral hypoglycemic agents ** Biguanides: Metformin Possible MOA: - ↓ CHO absorption - ↓ hepatic gluconeogenesis; ↑ glycolysis - ↓ glucagon release - ↑ peripheral utilization of glucose (direct effect)
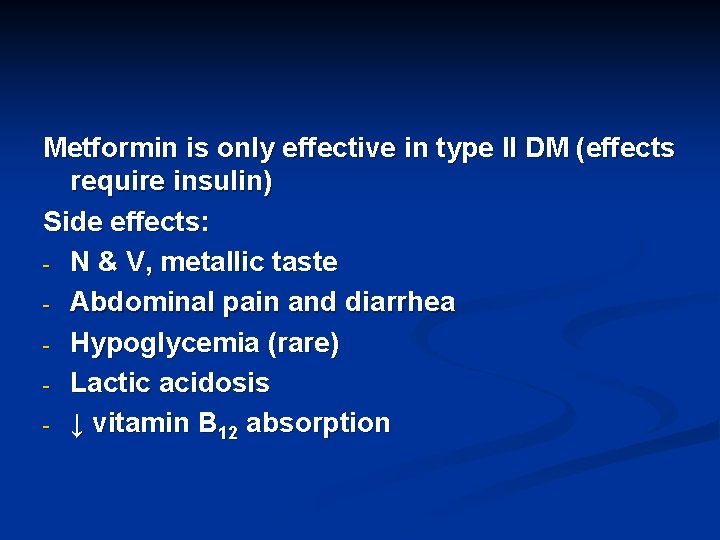
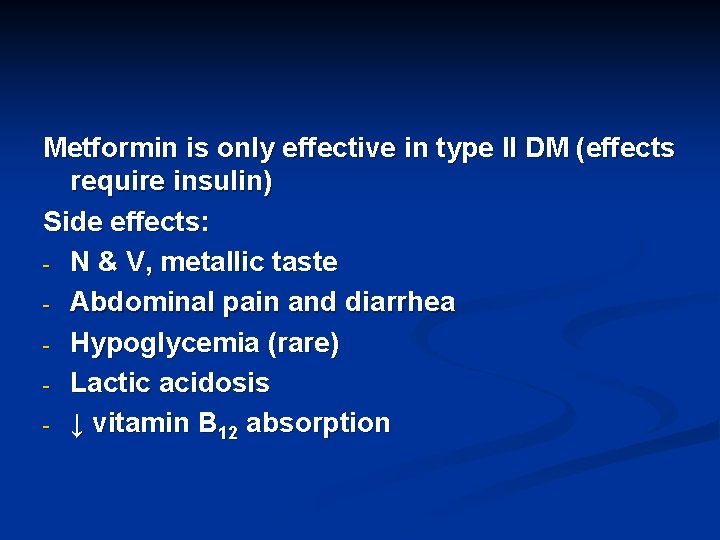
Metformin is only effective in type II DM (effects require insulin) Side effects: - N & V, metallic taste - Abdominal pain and diarrhea - Hypoglycemia (rare) - Lactic acidosis - ↓ vitamin B 12 absorption
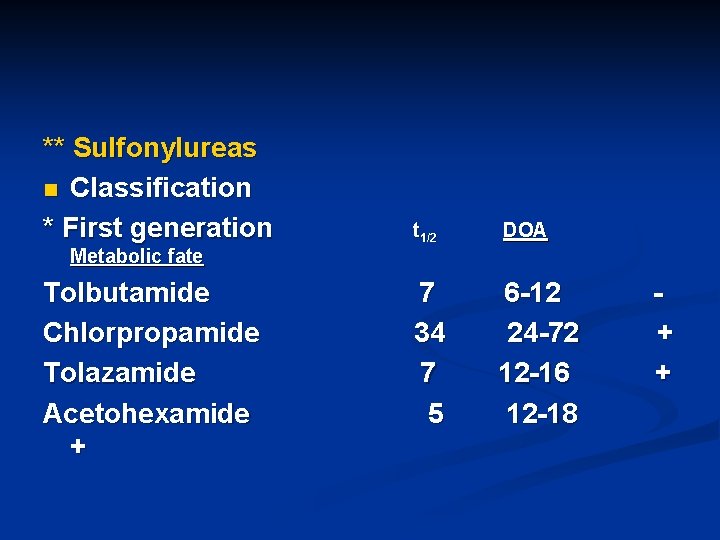
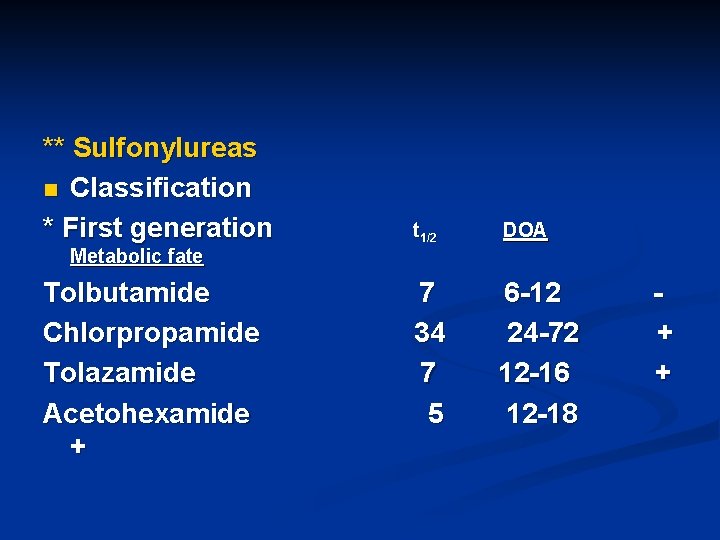
** Sulfonylureas n Classification * First generation t 1/2 DOA 7 34 7 5 6 -12 24 -72 12 -16 12 -18 Metabolic fate Tolbutamide Chlorpropamide Tolazamide Acetohexamide + + +

* Second generation t 1/2 DOA 4 3 20 -24 14 -16 8 10 -15 5 18 -22 Metabolic fate Glyburide (Glibenclamide) Glipizide – Gliclazide – Glimeperide ± ±
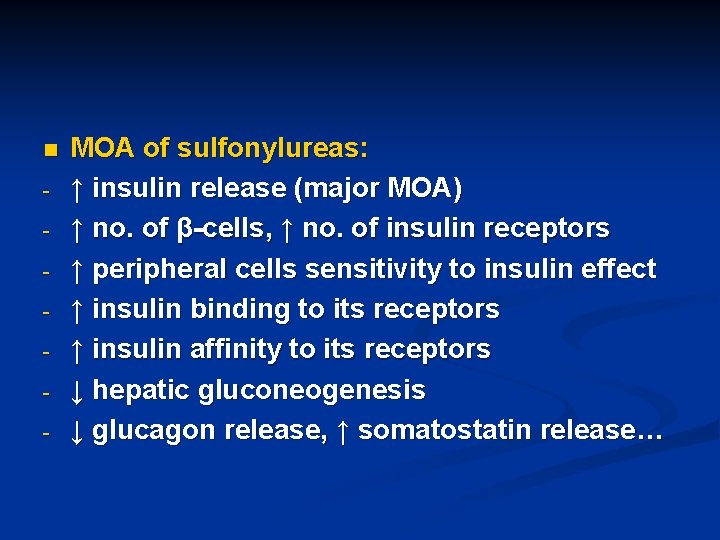
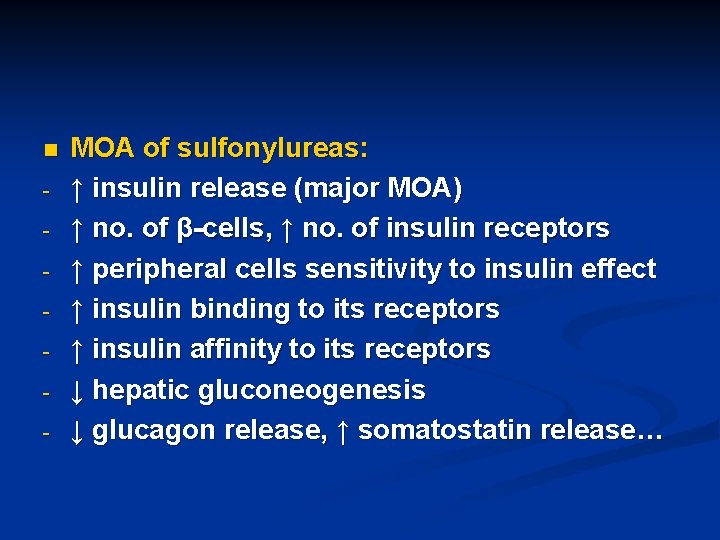
n - MOA of sulfonylureas: ↑ insulin release (major MOA) ↑ no. of β-cells, ↑ no. of insulin receptors ↑ peripheral cells sensitivity to insulin effect ↑ insulin binding to its receptors ↑ insulin affinity to its receptors ↓ hepatic gluconeogenesis ↓ glucagon release, ↑ somatostatin release…
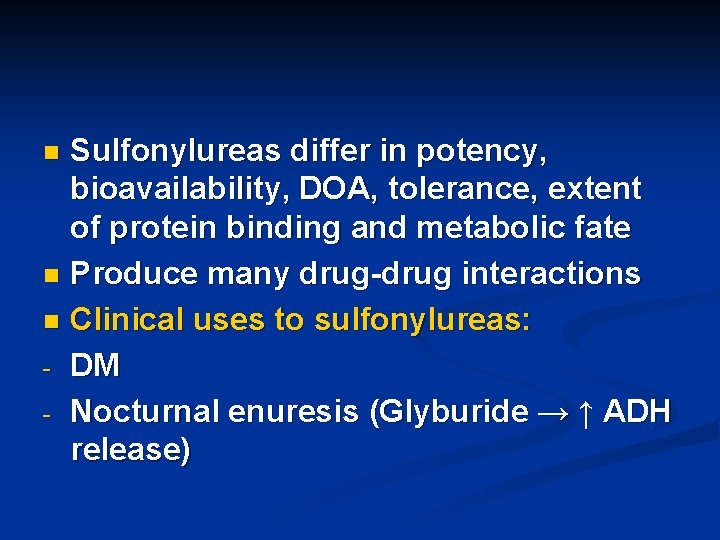
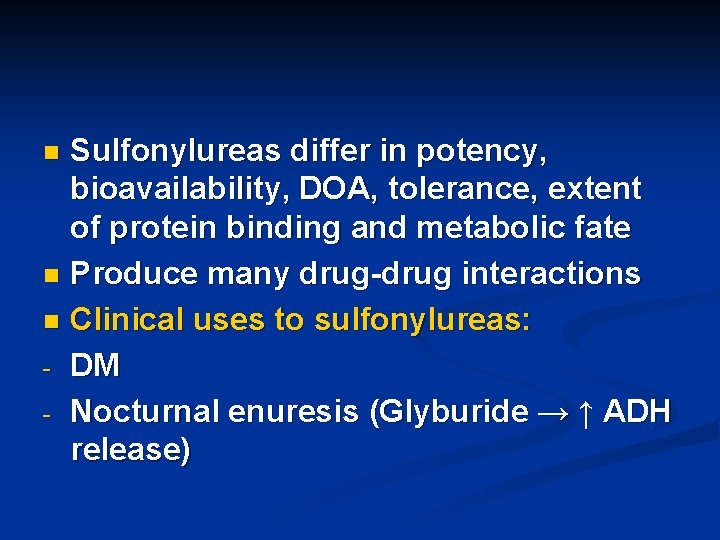
Sulfonylureas differ in potency, bioavailability, DOA, tolerance, extent of protein binding and metabolic fate n Produce many drug-drug interactions n Clinical uses to sulfonylureas: - DM - Nocturnal enuresis (Glyburide → ↑ ADH release) n
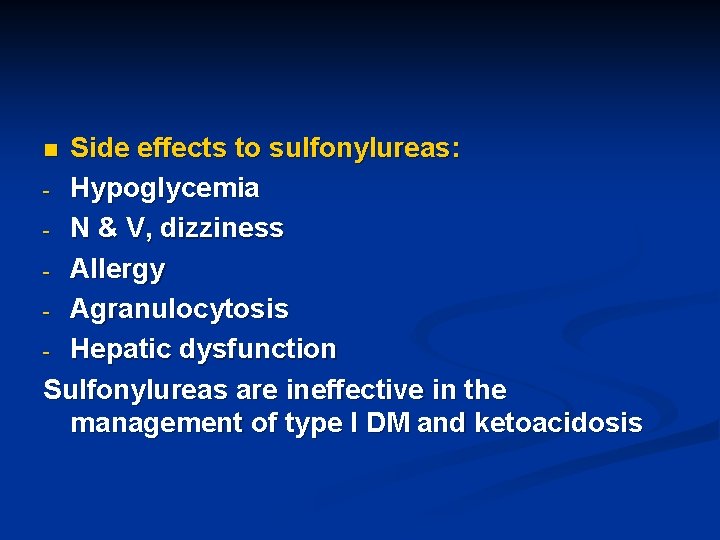
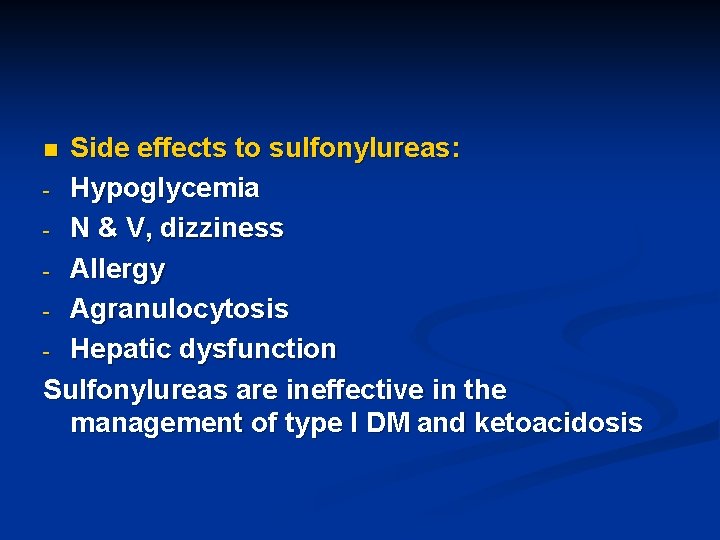
Side effects to sulfonylureas: - Hypoglycemia - N & V, dizziness - Allergy - Agranulocytosis - Hepatic dysfunction Sulfonylureas are ineffective in the management of type I DM and ketoacidosis n
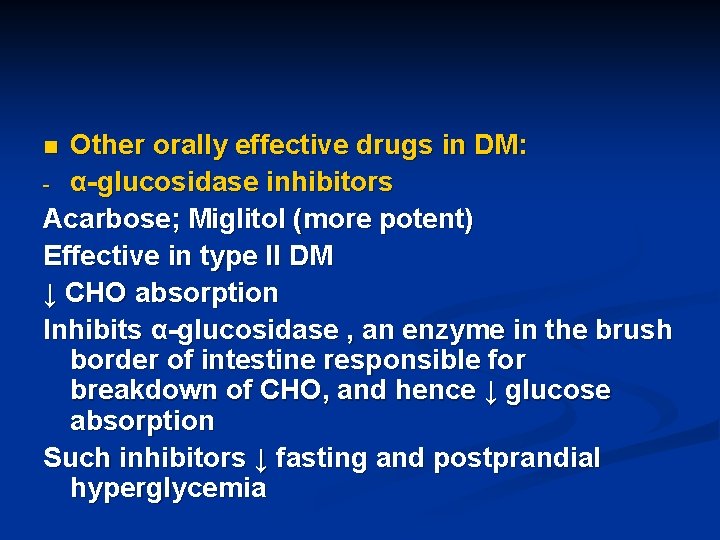
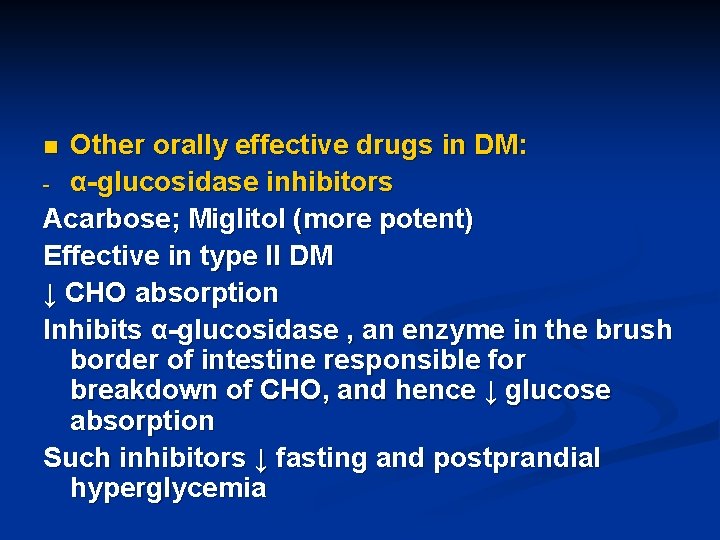
Other orally effective drugs in DM: - α-glucosidase inhibitors Acarbose; Miglitol (more potent) Effective in type II DM ↓ CHO absorption Inhibits α-glucosidase , an enzyme in the brush border of intestine responsible for breakdown of CHO, and hence ↓ glucose absorption Such inhibitors ↓ fasting and postprandial hyperglycemia n
α-glucosidase inhibitors also ↓ insulin secretion following administration sparing βcells Its been found that these inhibitors reduce incidence or risk of atherosclerosis in diabetics Taken before or with meals Could be given with insulin and sulfonylureas Side effects: Abdominal pain and diarrhea
Prandial glucose regulators: Repaglinide; Nateglinide (has faster OOA) ↑ insulin release Hypoglycemia is infrequent Taken before meals (every meal) Could be taken with metformin or insulin Hypoglycemia is infrequent -
Thiazolidinediones: Rosiglitazone; Pioglitazone (has shorter t 1/2) New drugs recently approved by FDA to be used in NIDDM who have insulin resistance (only) ↑ sensitivity of peripheral tissues to insulin effect ↓ glucose exit or output from the liver ↓insulin resistance Good to patients with ↑ insulin levels which are believed to be responsible for ↑ B. P, ↑ lipids and atherosclerosis in patients with insulin -
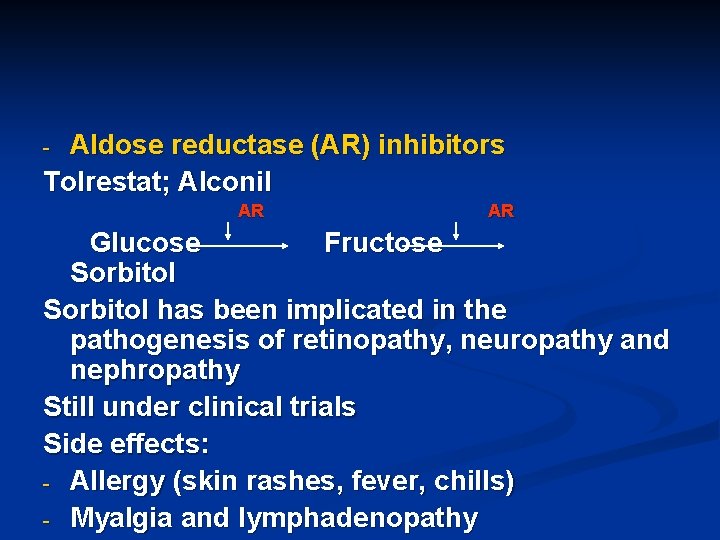
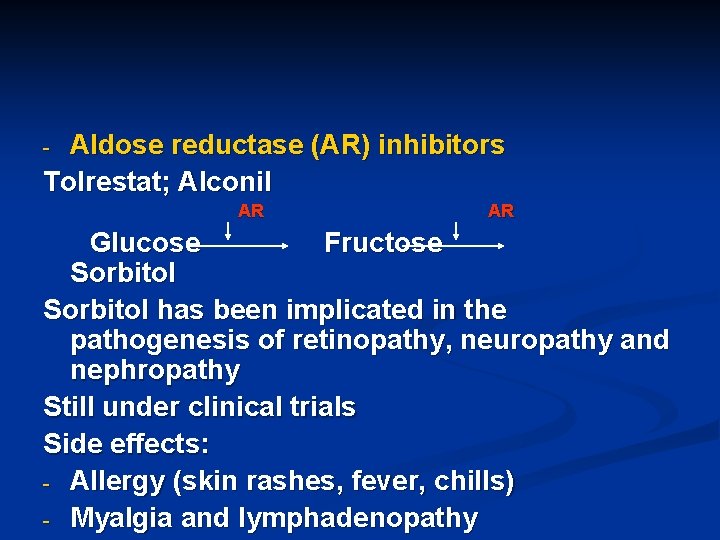
Aldose reductase (AR) inhibitors Tolrestat; Alconil - AR AR Glucose Fructose Sorbitol has been implicated in the pathogenesis of retinopathy, neuropathy and nephropathy Still under clinical trials Side effects: - Allergy (skin rashes, fever, chills) - Myalgia and lymphadenopathy
Somatostatin In low doses → ↓ glucagon release Under evaluation ** Pancreatic transplantation and gene therapy ** Role of Glucagon in diabetics? !!! ** Streptozotocin (Streptozocin) -
Goals of DM treatment!!=Control n Ensure good Pt. -clinic relationship n Control symptoms n Prevent acute metabolic crisis of KA & hypoglycemia n Maintain normal growth & BW n Encourage self-reliance & self-care n Eliminate risk factors Smoking, ↑ BP, ↑ lipids…
Cont. goals: n Prevent psychological complications - Accept restrictions on life - Diet control - Monitoring blood glucose & insulin adjustment - Know manifestations of hypoglycemia & how avoiding them n Early treatment of complications Photocoagulation, foot care advices. . .
Androgens (anabolic steroids) Testosterone: ♂ sex hormone Important for - 1 o & 2 o sexual characteristics of ♂’s - Spermatogenesis - Growth (growth promoting properties = Anabolic effect)
Testosterone clinical uses: - Deficiency states; aging Mesteronolone orally - Osteoporosis Nandrolone phenylpropionate I. M - Breast cancer Testolactone orally Testosterone side effects: Hirsutism; jaundice, acne, salt & water retention
Antiandrogens Estrogens; Progesterone (Progestins); Flutamide; Spironolactone; Gossypol Clinical uses: - Acne and hirsutism Spironolactone - Ca of prostate Cyproterone acetate (progestin); Diethylstilbesterol (DES) (estrogen); Flutamide - ? ♂ contraceptive Gossypol ( frequent use in China) ? Efficacy not sure and associated with many side effects
Female sex hormones
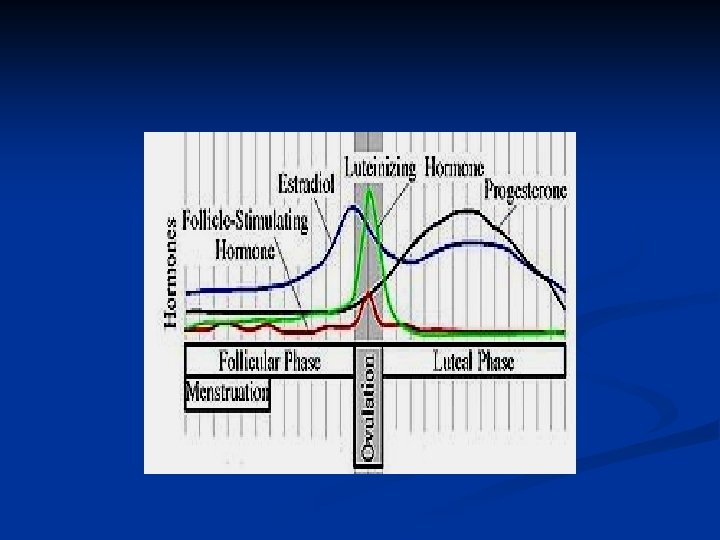
Estrogens and progestins Menstrual cycle. . . Changes and hormonal events Estrogens Natural estrogens: Estadiol >> Estrone > Estriol Natural estrogens are ineffective orally Synthesis: From cholesterol
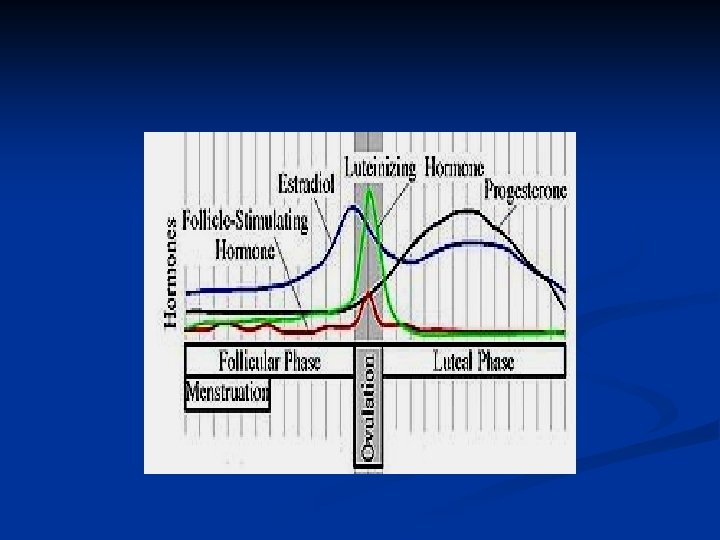
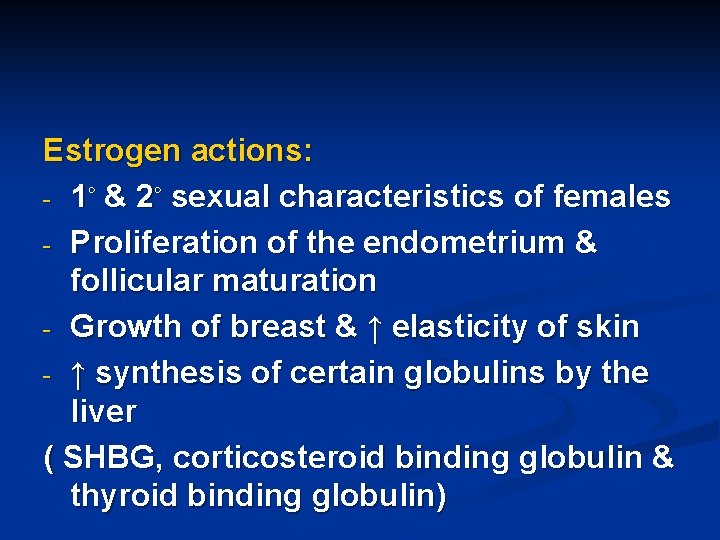
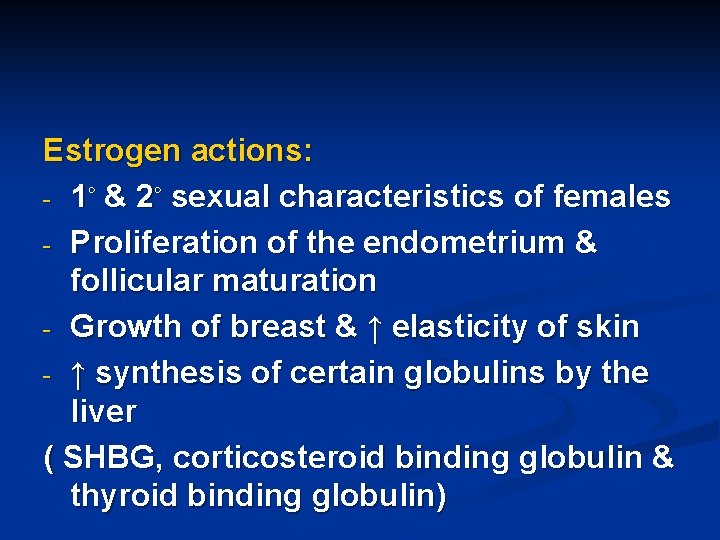
Estrogen actions: - 1◦ & 2◦ sexual characteristics of females - Proliferation of the endometrium & follicular maturation - Growth of breast & ↑ elasticity of skin - ↑ synthesis of certain globulins by the liver ( SHBG, corticosteroid binding globulin & thyroid binding globulin)
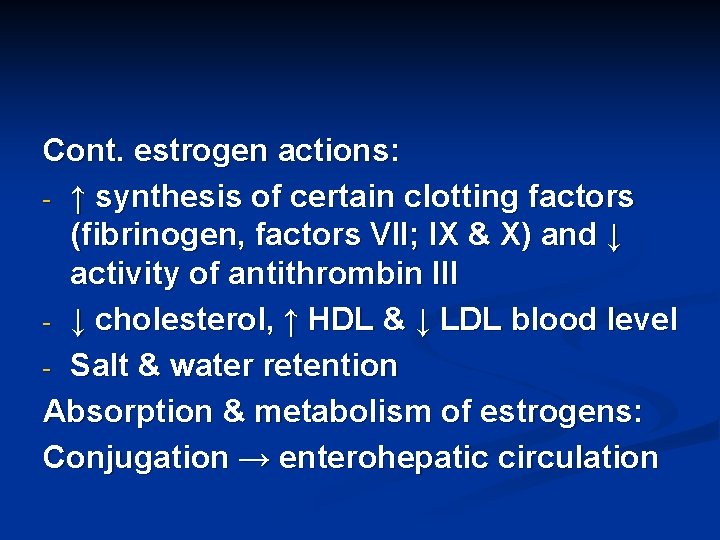
Cont. estrogen actions: - ↑ synthesis of certain clotting factors (fibrinogen, factors VII; IX & X) and ↓ activity of antithrombin III - ↓ cholesterol, ↑ HDL & ↓ LDL blood level - Salt & water retention Absorption & metabolism of estrogens: Conjugation → enterohepatic circulation
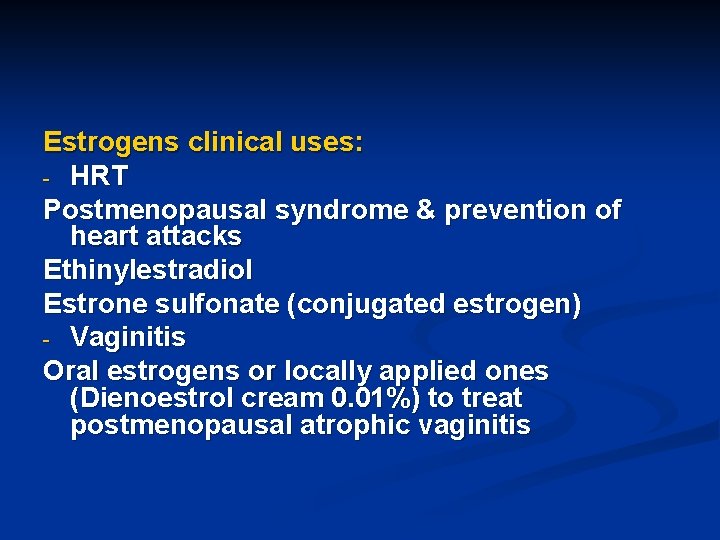
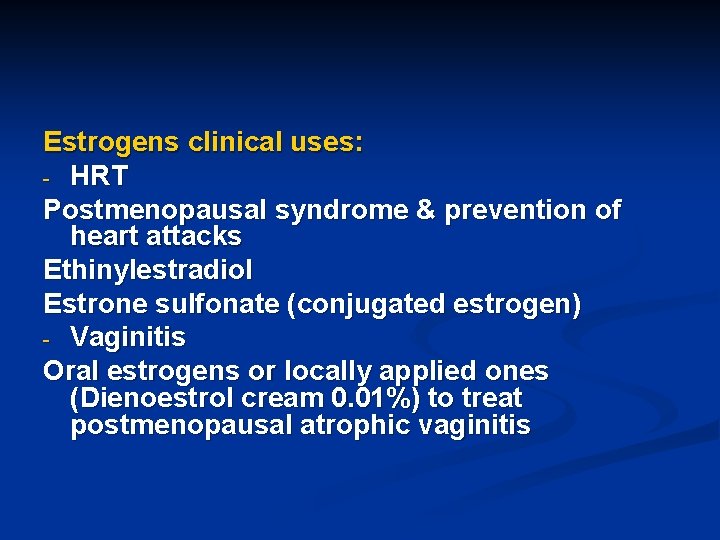
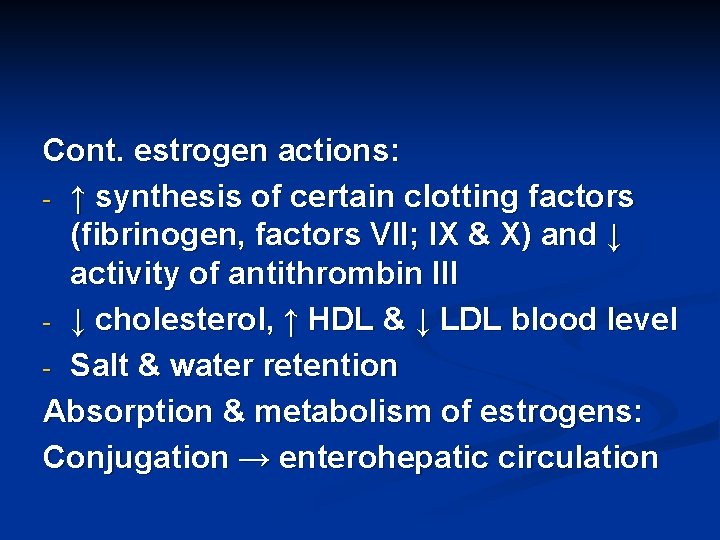
Estrogens clinical uses: - HRT Postmenopausal syndrome & prevention of heart attacks Ethinylestradiol Estrone sulfonate (conjugated estrogen) - Vaginitis Oral estrogens or locally applied ones (Dienoestrol cream 0. 01%) to treat postmenopausal atrophic vaginitis
Cont. estrogen clinical uses: - Osteoporosis Tibolone Synthetic estrogen highly effective to control osteoporosis Skin patches of estrogen are also available - Components of OCP’s - Prostate Ca (Diethylstilbesterol), certain types of breast Ca, endometrial cancer + progesterone
Cont. estrogen clinical uses: - Dysmenorrhea - Infertility - Acne, hirsutism Estrogen side effects: - Nausea, vomiting, dizziness, weight gain - Headache, migranous headache - Salt & water retention → ↑ BP - ↑ risk of thromboembolism and endometrial cancer - Teratogenic effect
Antiestrogens ** Competitive antagonists at estrogen receptors: Tamoxifen & clomiphene citrate Orally effective in the management of certain cases of infertility (in ♂’s and ♀’s) & in certain cases of breast cancer
** Selective estrogen receptor modulators (SERM’s): Nonhormonal pharmacological agents that bind estrogen receptors producing agonistic activity in certain tissues (in bone) and estrogen antagonistic effect at other tissues (breast and endometrium) Raloxifene Orally effective SERM widely used in the management of osteoporosis (prophylactic and Rx) in postmenopausal women
Progesterone (progestins)
Physiological & Pharmacological effects: - Endometrial differentiation, growth and development. Sudden withdrawal → bleeding (menses) - Maintenance of pregnancy - Breast development - Vagina: ↓ cornification, ↑ mucus content - Cervix: ↑ viscosity ↓ Na. Cl content - Thermogenic effect - Weak aldosterone-like effect
Progesterone clinical uses: - Components of OCP’s Norethindrone; Norgestrel; Megesterol - Dysfunctional uterine bleeding Medroxyprogesterone I. M or oral - Endometrial Ca + estrogens; breast & prostate Ca Cyproterone acetate oral - Abortion or maintaining pregnancy Dydrogesterone (IVF) oral
Progesterone side effects: Depression; weight gain; salt-water retention Antiprogestins Mifepristone Given orally Clinical uses: - Abortifacient + PG - Induction of labor + PG - Progesterone-dependent cancer - Cushing’s syndrome
Contraception
I. Male contraception: 1. Behavioral 2. Mechanical (e. g condoms) ± spermicidal agent (nonoxynol-9) 3. Drugs Estrogens; progestins; danazol; Gn. RH agonists & antagonists; spermicidal agents; gossypol 4. Surgical procedures e. g vasectomy
II. Female contraception: 1. Behavioral 2. Mechanical Diaphrams; condoms ± spermicidal agents; IUD’s ± progestins (progestasert) 3. Drugs - Estrogen alone Morning after pill or postcoital pill Ethinylestradiol; DES; mestranol…. . × 5
- Progesterone alone The minipill * Norethisteron. . . Tab * I. M medroxyprogesterone Depo-provera (effect lasts in 3 -6 months) * Subdermal progesterone implants Levonorgesrel (effect lasts in 5 -6 years)
4. Sequential Estrogen followed by progesterone 5. Combined oral contraceptive pills (COCP’s) ethinylestradiol or mestranol + Norgestrel ethinylestradiol or mestranol + Norethisterone * Estrogen + progesterone in different ratios (lowest E highest P to achieve
n MOA of OCP’s: Inhibition of ovulation (major mechanism) At the level of the pituitary (-ve feedback) - ↑ viscosity of cervical mucus - Change in Fallopian tube motility -
n - - OCP’s side effects: Nausea, vomiting, dizziness, headache, migraine, nervousness, depression Salt & water retention → ↑ BP Thromboembolic disease, embolism, MI Vaginal yeast growth Postpill amenorrhea and infertility
OCP’s contraindications: - Ladies > 35 years old - History of thromboembolic disease or ↑ BP - Severe headache - Severe nausea & vomiting - Liver dysfunction - Pregnancy - Abnormal menstrual cycles n
 A hormone
A hormone Hormones
Hormones Pharmacology of drugs acting on respiratory system
Pharmacology of drugs acting on respiratory system Endocrine system and reproductive system
Endocrine system and reproductive system Endocrine system and nervous system
Endocrine system and nervous system Lympathic
Lympathic Amino acid-based hormones
Amino acid-based hormones Adh function
Adh function Pharmacology and venipuncture
Pharmacology and venipuncture Potentiation example
Potentiation example Ion trapping
Ion trapping What is ion trapping in pharmacology
What is ion trapping in pharmacology Glucouronide
Glucouronide Chapter 30 principles of pharmacology
Chapter 30 principles of pharmacology First pass effect drugs
First pass effect drugs What is pharmacology
What is pharmacology Drug excretion
Drug excretion Factors affecting absorption of drug
Factors affecting absorption of drug Receptors in pharmacology
Receptors in pharmacology First pass metabolism definition pharmacology
First pass metabolism definition pharmacology Basic principles of pharmacology
Basic principles of pharmacology What is pharmacology
What is pharmacology Pharmacology introduction
Pharmacology introduction Competitive antagonist
Competitive antagonist What is ion trapping in pharmacology
What is ion trapping in pharmacology What is pharmacology
What is pharmacology Chapter 15 diagnostic procedures and pharmacology
Chapter 15 diagnostic procedures and pharmacology Pharmacology for nurses: a pathophysiological approach
Pharmacology for nurses: a pathophysiological approach Respiratory pharmacology quiz
Respiratory pharmacology quiz Pharmacology module
Pharmacology module First pass metabolism definition pharmacology
First pass metabolism definition pharmacology Clinical pharmacology powered by clinicalkey
Clinical pharmacology powered by clinicalkey Pharmacology pay
Pharmacology pay Pharmacology definition
Pharmacology definition Toxicology and applied pharmacology
Toxicology and applied pharmacology Rationale meaning in pharmacology
Rationale meaning in pharmacology Pharmacology chapter 1
Pharmacology chapter 1 Pharmacology tutor anderson
Pharmacology tutor anderson Clinical pharmacology
Clinical pharmacology Basic & clinical pharmacology
Basic & clinical pharmacology Dopamine synthesis
Dopamine synthesis Branches of pharmacology
Branches of pharmacology Fundamentals of pharmacology for veterinary technicians
Fundamentals of pharmacology for veterinary technicians Analglesia
Analglesia Clinical pharmacology residency
Clinical pharmacology residency Annual review of pharmacology and toxicology
Annual review of pharmacology and toxicology Dopamine pharmacology
Dopamine pharmacology Define pharmacology
Define pharmacology Concept of essential drugs
Concept of essential drugs Reductinist
Reductinist Glomerular filtration
Glomerular filtration Relative bioavailability
Relative bioavailability Estado estable
Estado estable Difference between tolerance and tachyphylaxis
Difference between tolerance and tachyphylaxis Therapeutic index
Therapeutic index Apparent volume of distribution
Apparent volume of distribution Fish pharmacology
Fish pharmacology Pharmacology definition
Pharmacology definition Loading dose
Loading dose Maintenance dose formula
Maintenance dose formula Guaifenasin
Guaifenasin Clinical pharmacology seminar
Clinical pharmacology seminar Adrenal drugs pharmacology
Adrenal drugs pharmacology Spremicides
Spremicides Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals Lomotib
Lomotib Computational pharmacology
Computational pharmacology Tactcardia
Tactcardia Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Tidal volume
Tidal volume Human respiratory system
Human respiratory system Anterior surface of scapula
Anterior surface of scapula Chapter 16 endocrine system
Chapter 16 endocrine system Adenohypophysis
Adenohypophysis Differences between nervous system and endocrine
Differences between nervous system and endocrine Comparison of endocrine and nervous system
Comparison of endocrine and nervous system Gonads glands
Gonads glands Facts about the endocrine system
Facts about the endocrine system Rat internal organs
Rat internal organs Pearson
Pearson Endocrine and nervous system comparison
Endocrine and nervous system comparison 7:13 endocrine system
7:13 endocrine system Mammillary body
Mammillary body Figure of endocrine system
Figure of endocrine system Chapter 11 endocrine system
Chapter 11 endocrine system Biology 30 endocrine system
Biology 30 endocrine system Pak pandani
Pak pandani Chapter 23 the endocrine system
Chapter 23 the endocrine system Endocrine system analogy
Endocrine system analogy Introduction of endocrine system
Introduction of endocrine system Classification of hormones
Classification of hormones T3.taktak
T3.taktak Endocrine system
Endocrine system Endocrine system
Endocrine system Pancreas in endocrine system
Pancreas in endocrine system Glands of the endocrine system
Glands of the endocrine system Endocrine system
Endocrine system Chapter 16 lesson 2 the male reproductive system
Chapter 16 lesson 2 the male reproductive system Endocrine system regents questions
Endocrine system regents questions Endocrine system regents questions
Endocrine system regents questions Endocrine tissues
Endocrine tissues Chapter 18: the endocrine system answer key
Chapter 18: the endocrine system answer key Steroid hormone lipid
Steroid hormone lipid Amino acid derivative hormones
Amino acid derivative hormones Steroid hormone biosynthesis
Steroid hormone biosynthesis Auxins and gibberellins
Auxins and gibberellins Amiformes
Amiformes Hormones definition psychology
Hormones definition psychology Amine hormone
Amine hormone Prolactin target
Prolactin target Hypothalamus hormones
Hypothalamus hormones Lipid soluble hormones
Lipid soluble hormones Lipid soluble hormones examples
Lipid soluble hormones examples Gonadal hormones
Gonadal hormones Abreviation
Abreviation Bioflix activity homeostasis hormones and homeostasis
Bioflix activity homeostasis hormones and homeostasis What is a tropic hormone
What is a tropic hormone Amino acid-based hormones
Amino acid-based hormones Hypothalmus
Hypothalmus Tropic hormones
Tropic hormones Tropic vs nontropic hormones
Tropic vs nontropic hormones Four classes of hormones
Four classes of hormones Tropic casade
Tropic casade Hormones during pregnancy
Hormones during pregnancy Autocrine hormones
Autocrine hormones Hormones after sex
Hormones after sex Where is trh produced
Where is trh produced Hypothalamic hormones
Hypothalamic hormones Hunger motivation ap psychology
Hunger motivation ap psychology Male and female hormones
Male and female hormones Hypothalamus and pituitary gland connection
Hypothalamus and pituitary gland connection Thyroxine binding prealbumin
Thyroxine binding prealbumin What is that?
What is that?