PEDIATRIC INFECTIONS DISEASES Pediatric Exanthems 1 The exanthematous










- Slides: 75
PEDIATRIC INFECTIONS DISEASES Pediatric Exanthems 1
The exanthematous diseases of childhood were named according to the order in which they were reported: First disease: Measles (Rubeola) Second disease: Scarlet fever Third disease: German measles (rubella) Fourth disease: Duke’s Filatow disease (possible a scarlet fever variant) Fifth disease: Erythema infecciosum Sixth disease: Roseola 2
Rubella (German measles) Etiology: Is a Togavirus, a single stranded RNA virus Transmission: • Humans are the only host. • via infected respiratory droplets, where it replicates in the respiratory tract, and viremia follows 5 -7 days • Infected patients shed the virus 7 days prior to the exanthem to 7 days after. • They are contagious during the exanthem period • Transplacental transmission during viremia (first 16 weeks of pregnancy) deafness, cataracts, heart problems, and CNS abnormalities • Late winter – early spring • Incubation period: 14 -21 days 3
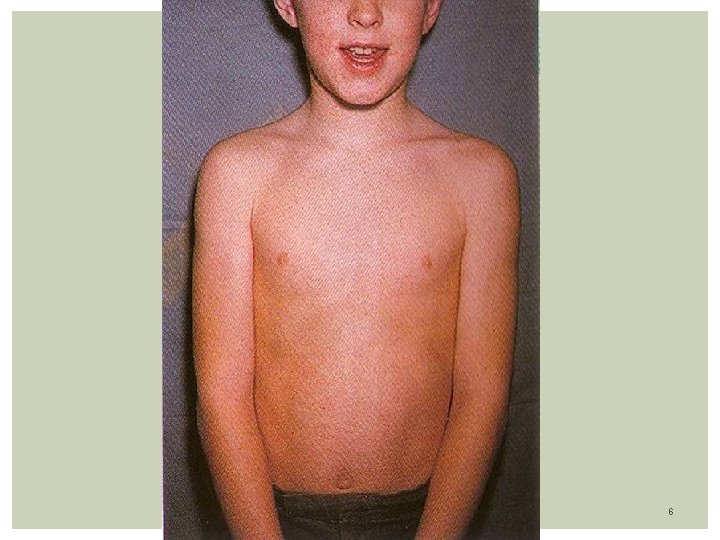
Rubella (German measles) Prodomal symptoms: Uncommon in children, mainly in Adolescents: Low fever, malaise 1 - 4 days, mild pharyngitis, Lymphadenopathy: Post-auricular, occipital Exanthem: Eruption generalized within 24 -48 hours Fine Pink (erythematous) maculopapules with discrete lesions Start in face/neck progressing in a cephalocaudal fashion By 3 rd day: Rash starts to fade in 3 days, signaling end of the viremia Rash on face disappeared Only extremities are involved Rash may disappear by end of 3 rd day No desquamation Others signs: Often transient polyarthralgia, polyarthritis, more in teens age 4

5
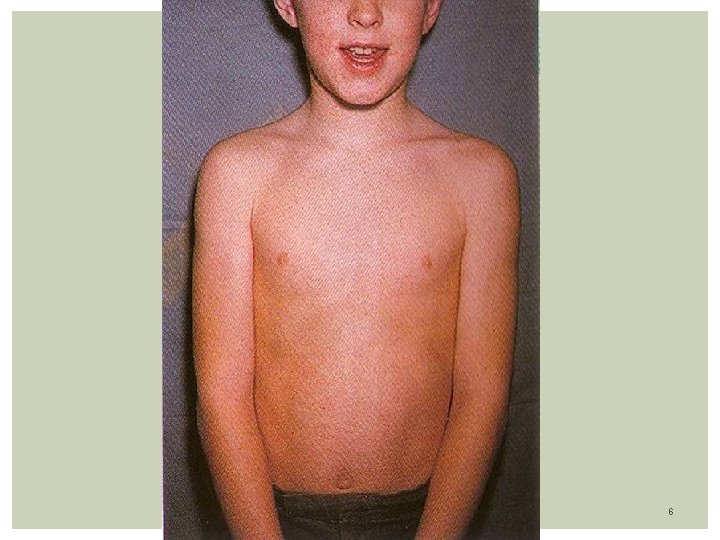
6
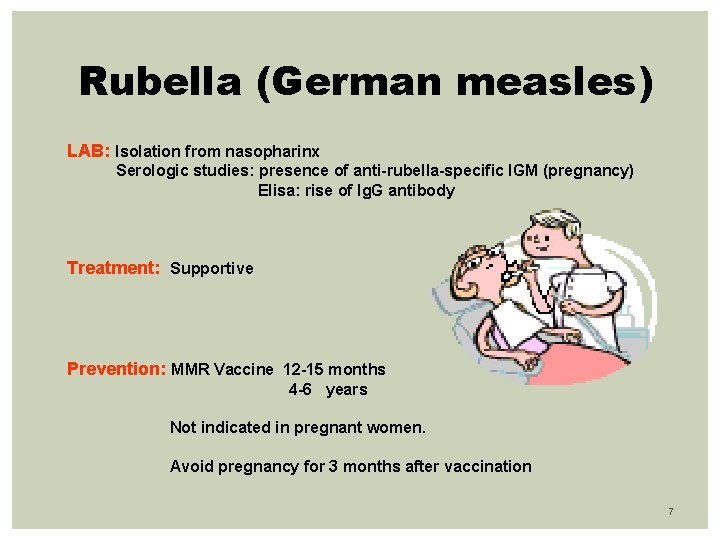
Rubella (German measles) LAB: Isolation from nasopharinx Serologic studies: presence of anti-rubella-specific IGM (pregnancy) Elisa: rise of Ig. G antibody Treatment: Supportive Prevention: MMR Vaccine 12 -15 months 4 -6 years Not indicated in pregnant women. Avoid pregnancy for 3 months after vaccination 7
Rubeola (Measles-First Disease) Highly contagious disease characterized byexanthem Etiology: Paramyxovirus, an RNA virus Rare in developing countries due to universal immunization Happens in Third world countries where can be fatal to malnourished children Transmission: Humans are the natural host and reservoir of the virus. Spread by respiratory droplets, primary replication of the virus occurs in the respiratory epithelial cells, where it replicates, later spreading to to the local lymphnodes, and then to the blood, resulting in a viremia Incubation period: 10 -21 days with average of 14 days Late winter – early spring 8
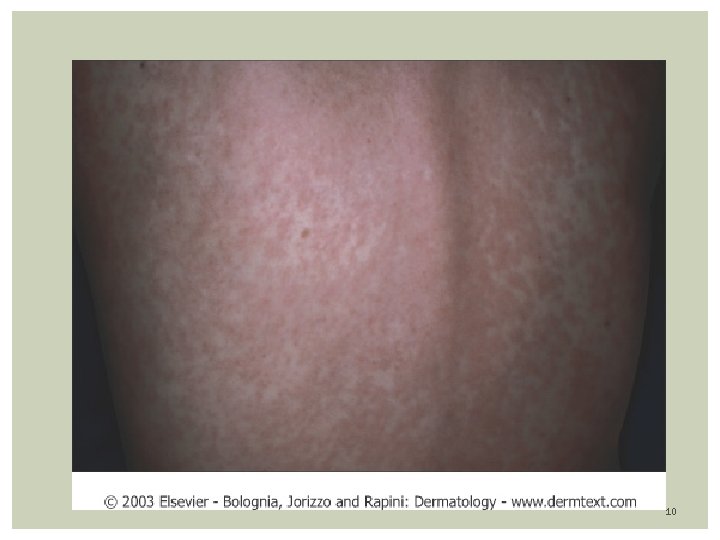
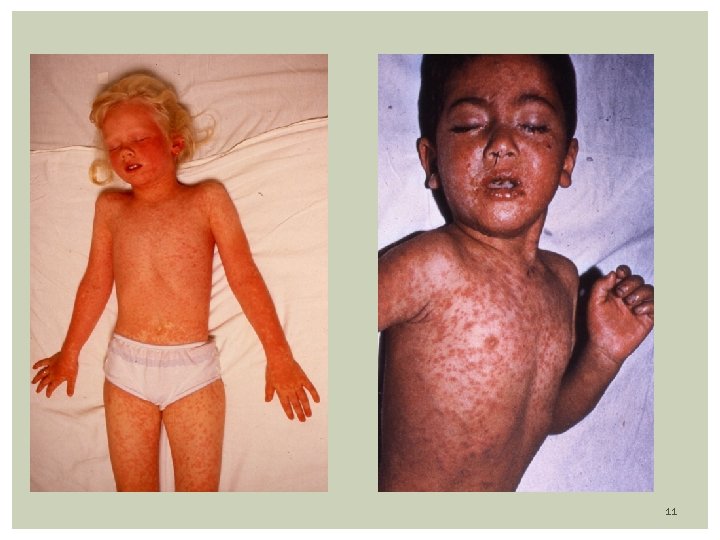
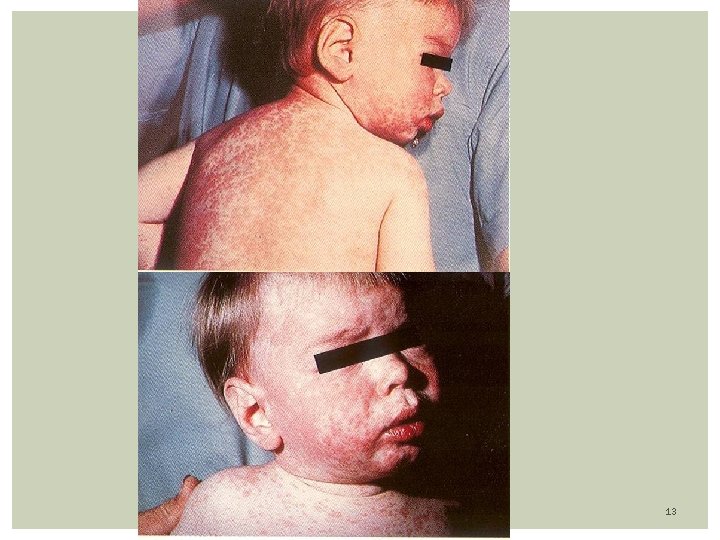
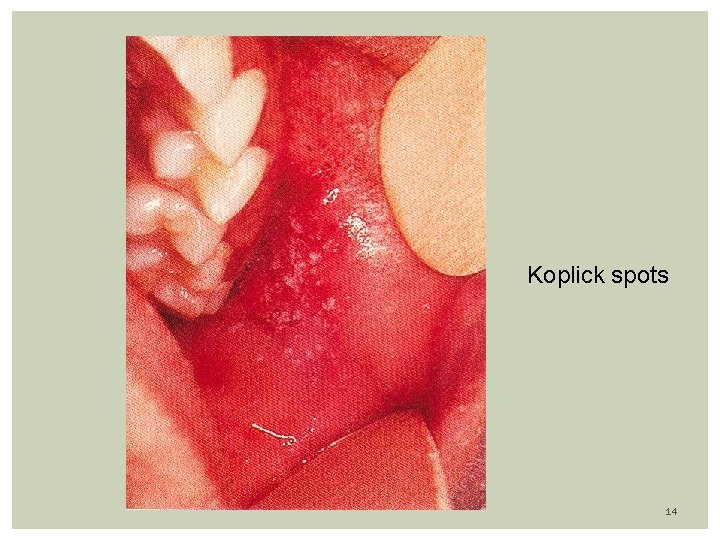
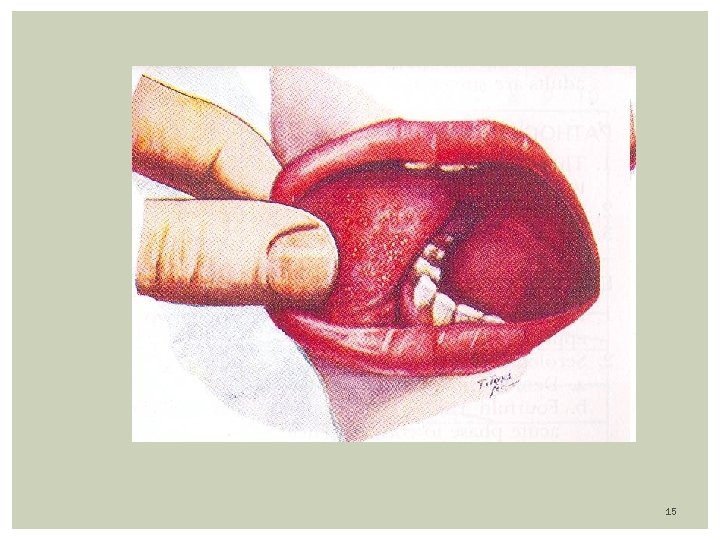
Rubeola (measles) Prodrome: high fever (104 F), malaise, anorexia followed by URI Three C’s: cough, coryza, conjunctivitis (exudative, photophobia) Exanthem: Appearance of macular-papular (confluent) rash on or about 3 th febrile day (coincides with peak of fever) Rash first of face/neck (hairline) with a cephalocaudal progression; fades in 5 days Mild desquamation and brown staining of skin Koplic Spots: White-Gray dots on erythematous buccal mucosa Seen 2 days before and 2 days after the rash appears Appears at: buccal mucosa opposite the lower molars 9
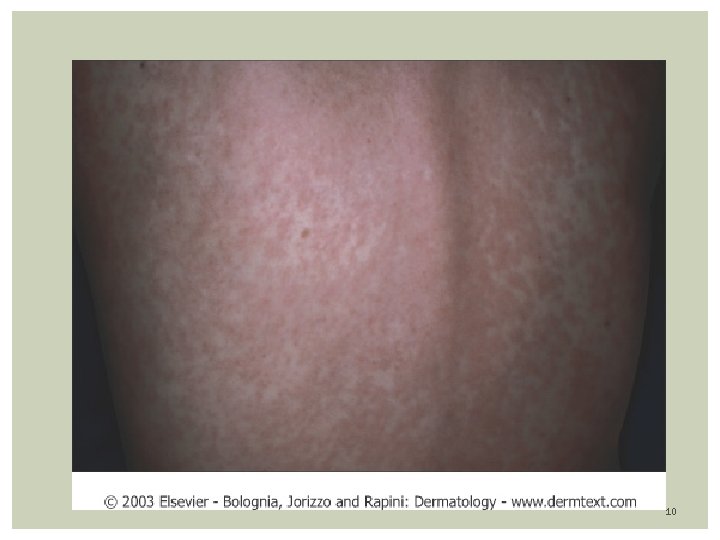
10
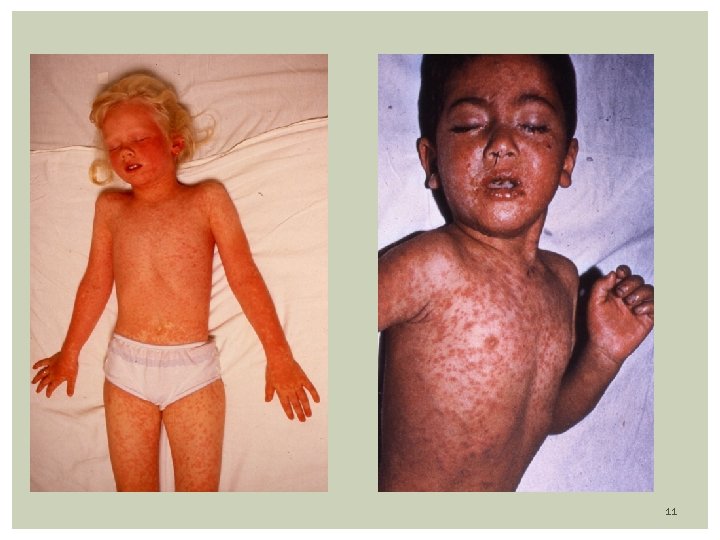
11
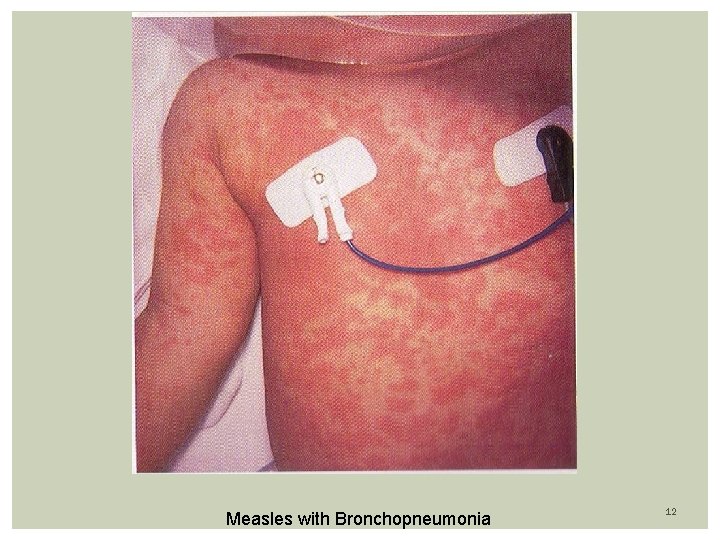
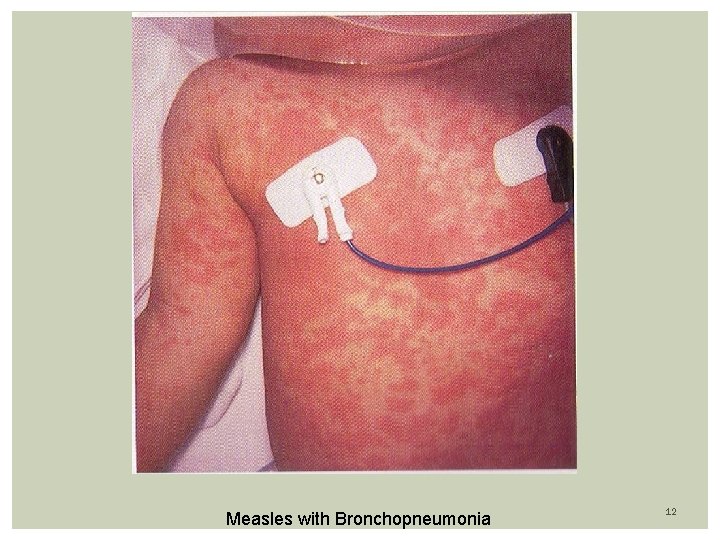
Measles with Bronchopneumonia 12
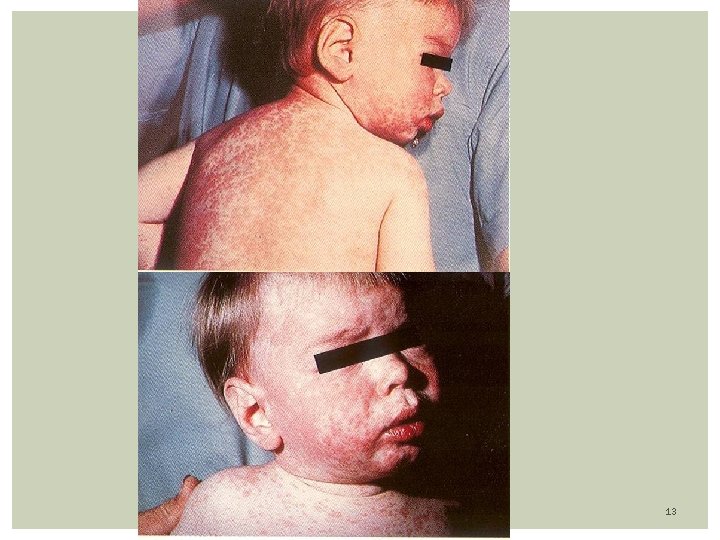
13
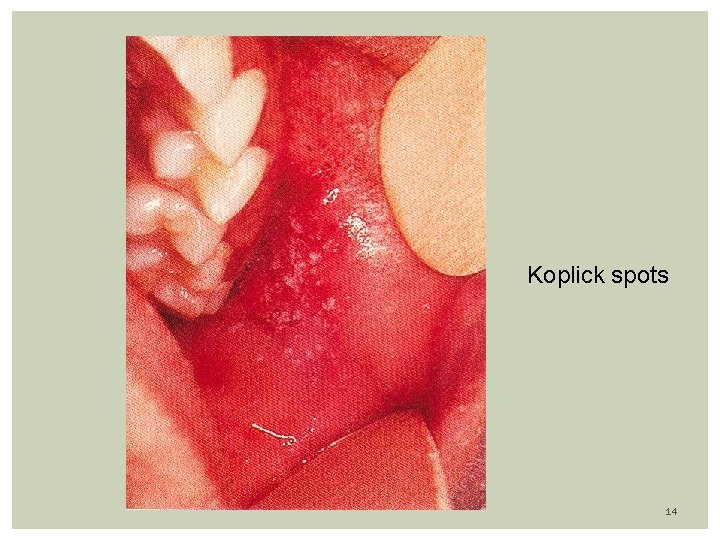
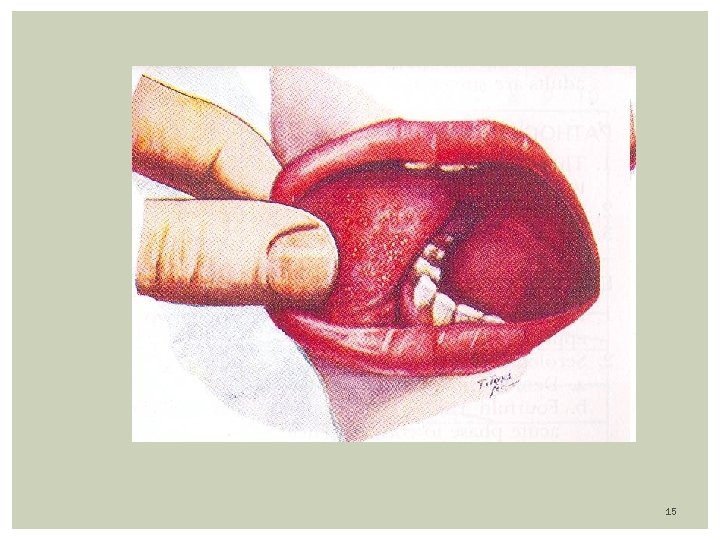
Koplick spots 14
15
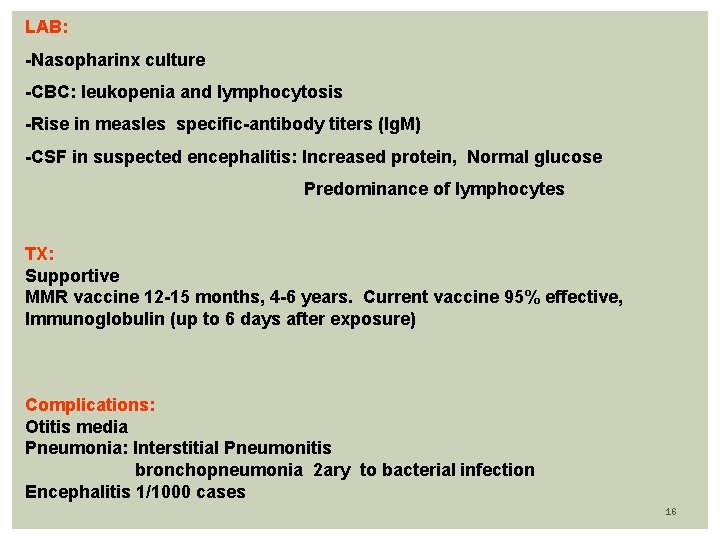
LAB: -Nasopharinx culture -CBC: leukopenia and lymphocytosis -Rise in measles specific-antibody titers (Ig. M) -CSF in suspected encephalitis: Increased protein, Normal glucose Predominance of lymphocytes TX: Supportive MMR vaccine 12 -15 months, 4 -6 years. Current vaccine 95% effective, Immunoglobulin (up to 6 days after exposure) Complications: Otitis media Pneumonia: Interstitial Pneumonitis bronchopneumonia 2 ary to bacterial infection Encephalitis 1/1000 cases 16
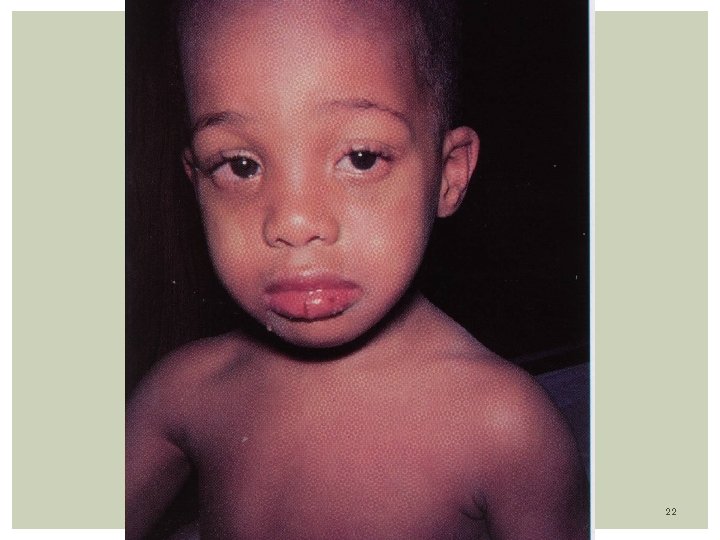
KAWASAKi DISEASE Is a febrile mucocutaneous lymph node syndrome. Systemic vasculitis with devastating cardiac sequelae Etiology: The exact cause is unknown. It is an immune-mediated disorder in a genetically predisposed child Epidemiology: Disease of young children, mainly boys Most of patients (80%) are less than 5 years of age, average 2 -3 years If child is older than 5 years old doubt the diagnosis Most common in Asians than whites, and least in blacks Most common in winter. Suspect of cases during spring months Pathogenesis: An unknown superantigen result in heavy cytokine release, being responsible for the multiple clinical findings. 17
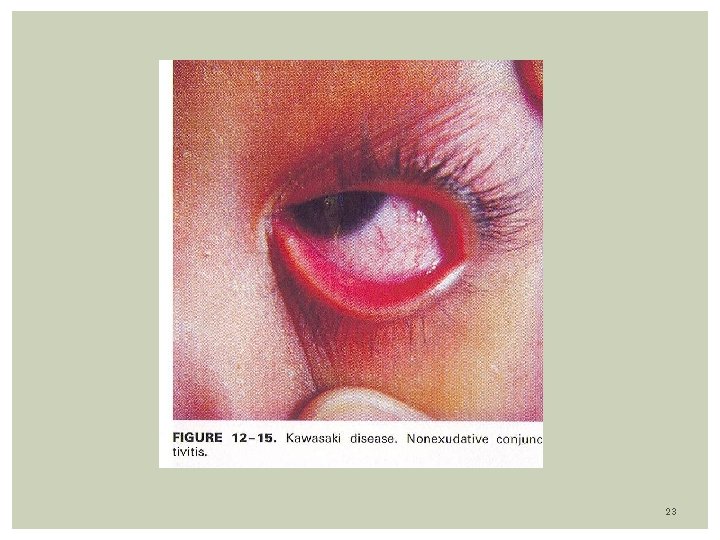
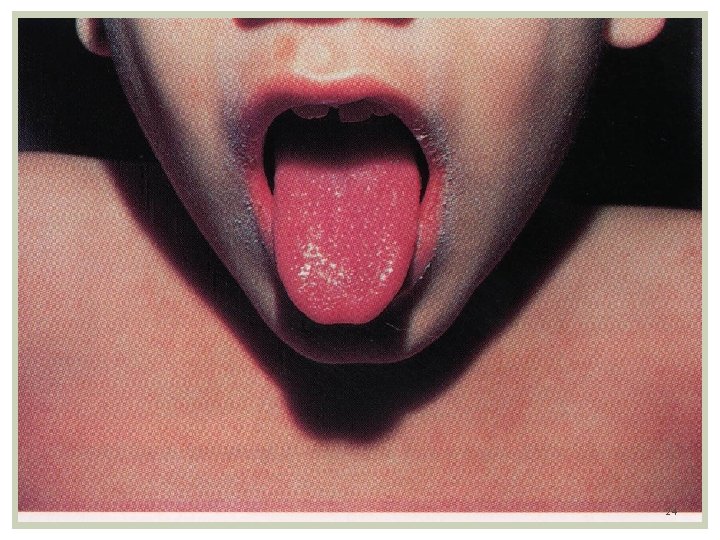
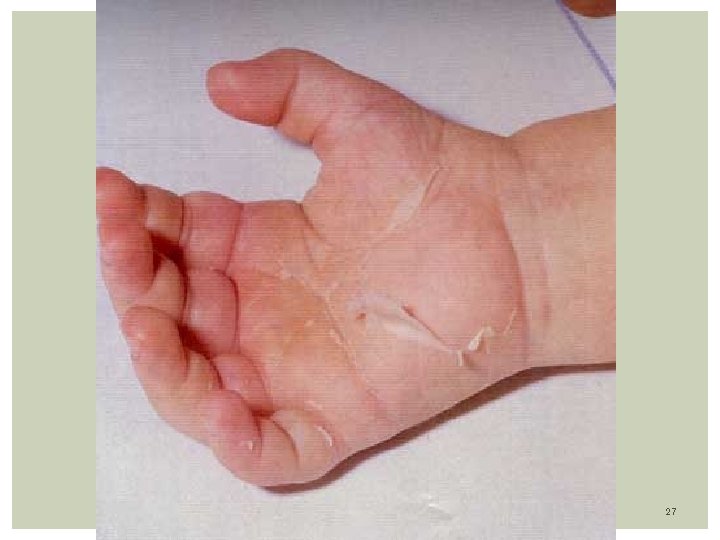
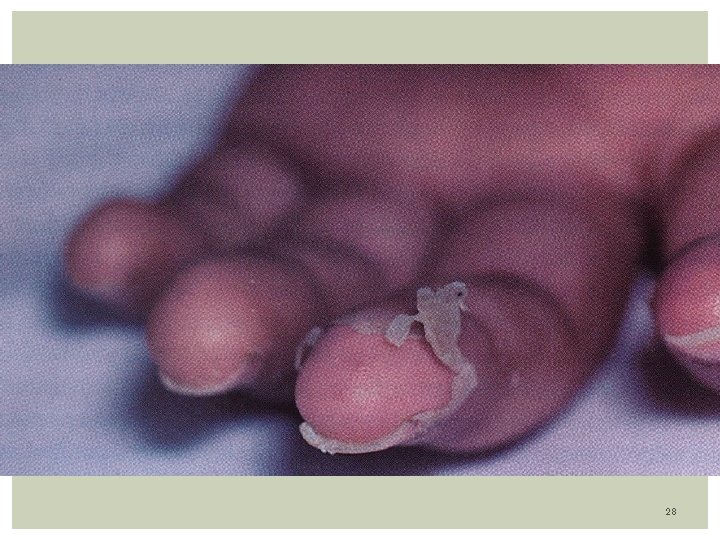
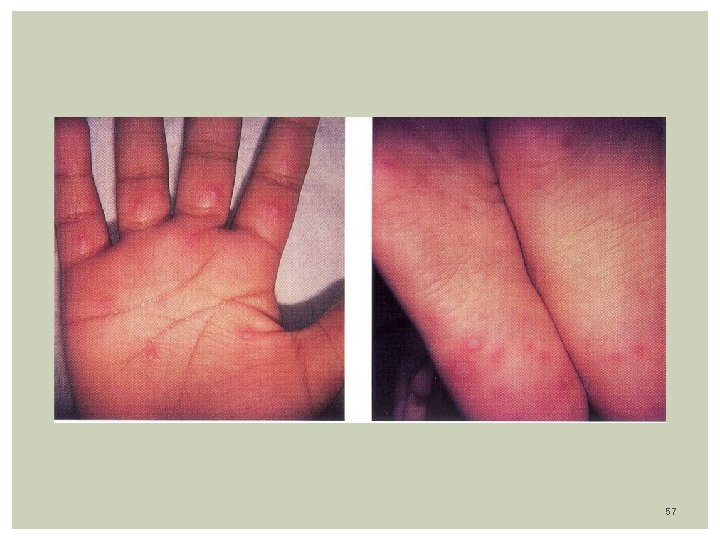
Clinical Features: Acute phase: Last 7 -14 days. Presence of 4/5 of the following: Fever- 104 F/39 C averaging 5 -10 days. Can persist up to 4 weeks Conjunctivitis- Dry eyes with dilated vessels (bulbar). Non purulent, non edema, non tearing, bilateral. Changes in oral mucosa: red strawberry tongue, pharyngeal erythema, dry red and cracked lip Extremity changes: edema hand/feet, erythema of palms/ sole precedes desquamation of fingers on palm and soles. The rash is erythematous, maculo-papular or morbiliform, scarlatiniform, non vesicular, affecting the groin and perineum. occurs on the trunk 3 days after fever. Also over buttocks Cervical lymphadenopathy: At least 1 node measuring 1. 5 cms. The node is unilateral, nontender / nonsuppurative 18
Subacute Phase: From day 14 to 25: - Decrease of fever. -Arthralgias occurs involving large and small joints. -Giant and painless skin desquamation occurs around day 14, in the fingertips, palms, soles, perineal areas (groin)!!! Convalescent Phase: Begins in day 21 -60: - In this phase, coronary artery aneurysms are detected by Echo - Arthritis may persist, but other Sx subside. - Beau Line in fingernails - Observe signs of cardiac insufficiency: Fatigue, chest pain, DOE - Control with weekly ECG. 19
LAB: WBC: elevated with left shift. Greater than 20. 000 in 50% of cases ESR: Increased. Often greater than 40/50 mm or more CRP: Elevated, above 3 mg/d. L Albumin 3 g/d. L or less Platelet count: Increase after the 1 st week of illness. U/A: 10 wbc/hpf, Pyuria, proteinuria Elevation of alanine aminotransferase ECG: acute phase- prolonged PR interval, Flat T waves, ST changes CX-Ray: May show dilated heart during acute phase ECHO: Detection of aneurysm. Strict ECHO follow-up. DD: Scarlet- Throat CX Positive, Increase ASO Titer Measles- Increase Ig. G, Ig. M Titer EBV, TOXO, CMV- Saliva, U/A, Titers 20
TX: Bed Rest until 72 hours without fever IVIG: Intravenous Immunoglobulin- 2 g/kg one time over 10 hs Repeat to patients who fail to response the first shot. Aspirin: 80 -100 mg/kg/d in divided dosis, for 10 days, or until child 48 hours afebrile 3 -10 mg/kg/d for 6 -8 weeks after fever resolves or until platelets count returns to normal Descontinue if patient has varicella or Influenza Steroids: controversial Complications: coronary artery dilatation and aneurysms 21
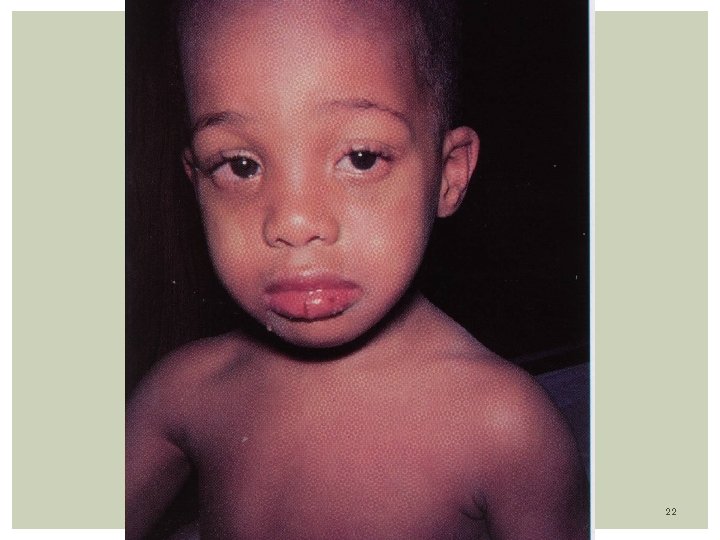
22
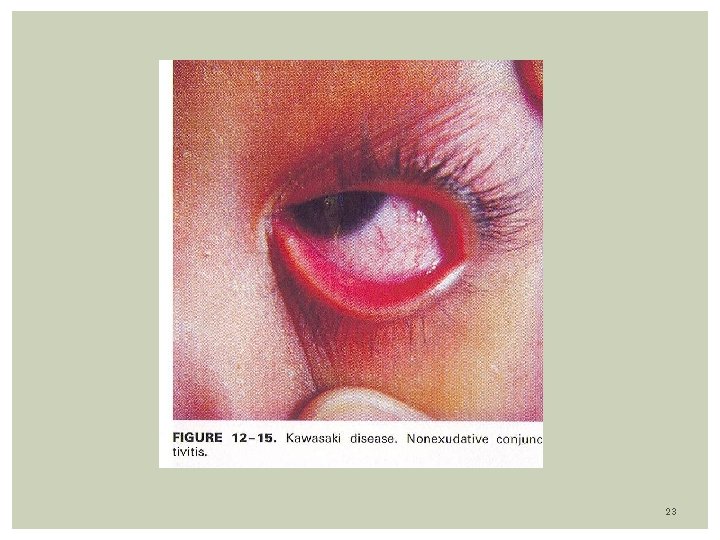
23
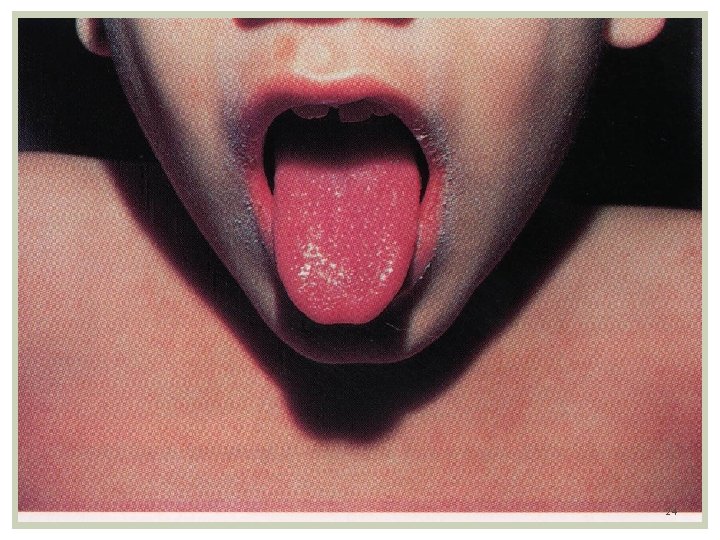
24

25

26
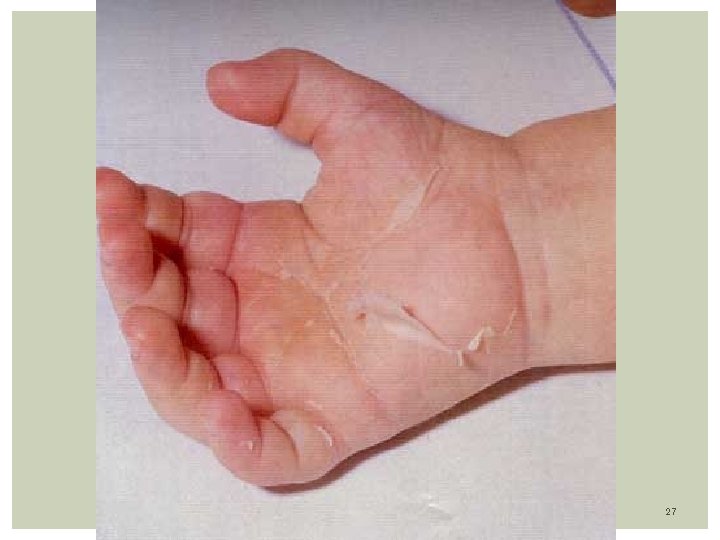
27
28
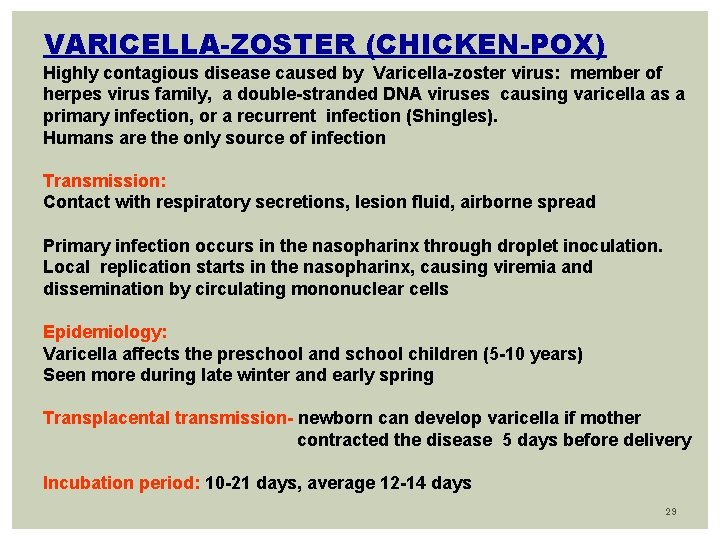
VARICELLA-ZOSTER (CHICKEN-POX) Highly contagious disease caused by Varicella-zoster virus: member of herpes virus family, a double-stranded DNA viruses causing varicella as a primary infection, or a recurrent infection (Shingles). Humans are the only source of infection Transmission: Contact with respiratory secretions, lesion fluid, airborne spread Primary infection occurs in the nasopharinx through droplet inoculation. Local replication starts in the nasopharinx, causing viremia and dissemination by circulating mononuclear cells Epidemiology: Varicella affects the preschool and school children (5 -10 years) Seen more during late winter and early spring Transplacental transmission- newborn can develop varicella if mother contracted the disease 5 days before delivery Incubation period: 10 -21 days, average 12 -14 days 29
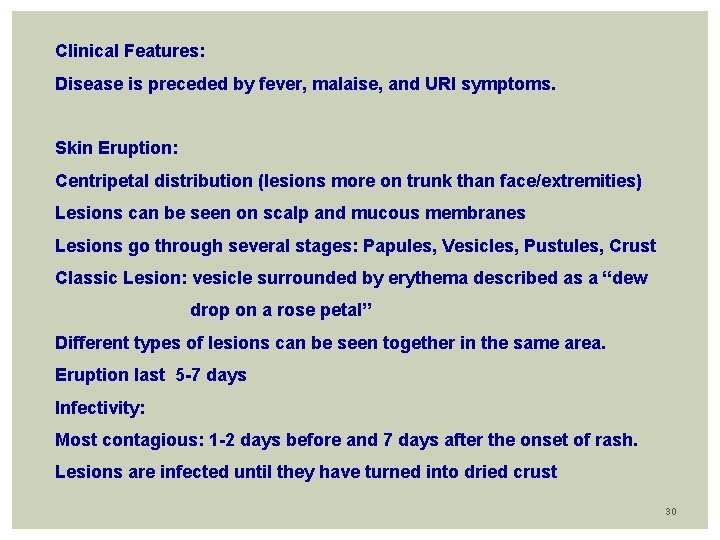
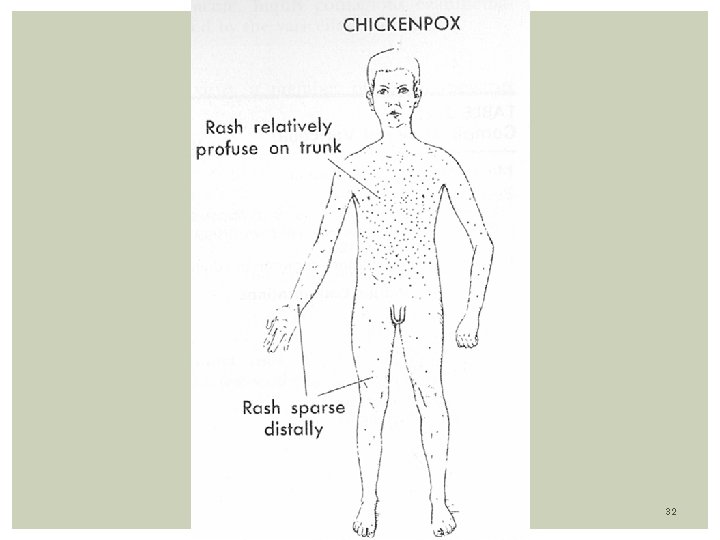
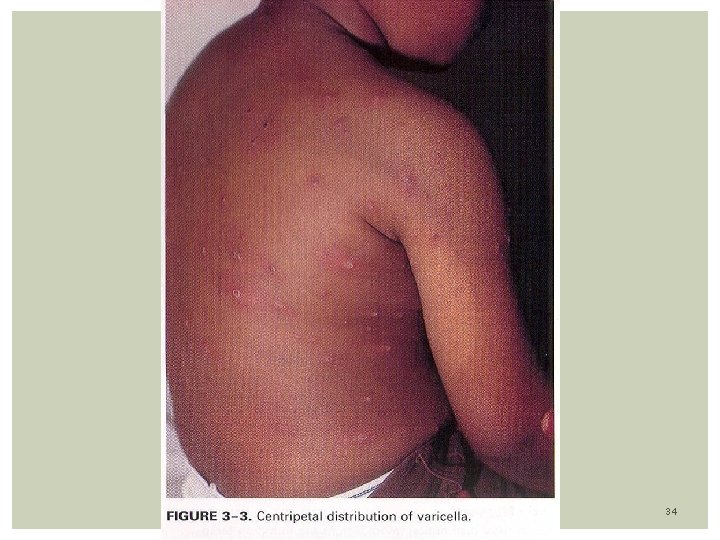
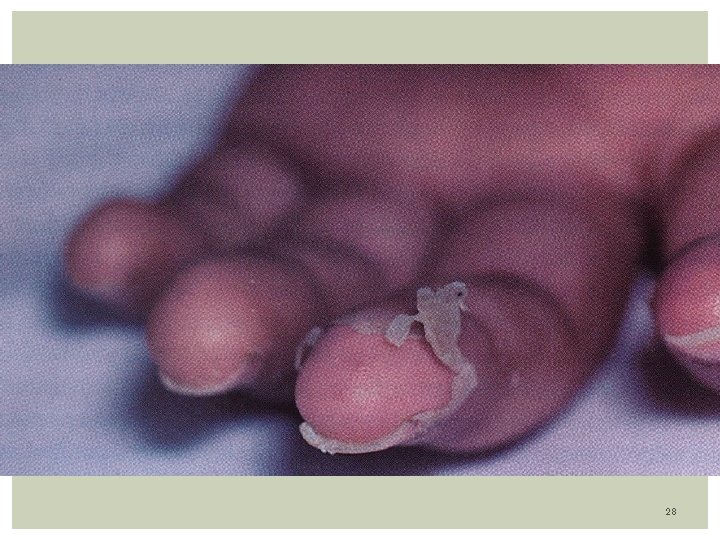
Clinical Features: Disease is preceded by fever, malaise, and URI symptoms. Skin Eruption: Centripetal distribution (lesions more on trunk than face/extremities) Lesions can be seen on scalp and mucous membranes Lesions go through several stages: Papules, Vesicles, Pustules, Crust Classic Lesion: vesicle surrounded by erythema described as a “dew drop on a rose petal” Different types of lesions can be seen together in the same area. Eruption last 5 -7 days Infectivity: Most contagious: 1 -2 days before and 7 days after the onset of rash. Lesions are infected until they have turned into dried crust 30
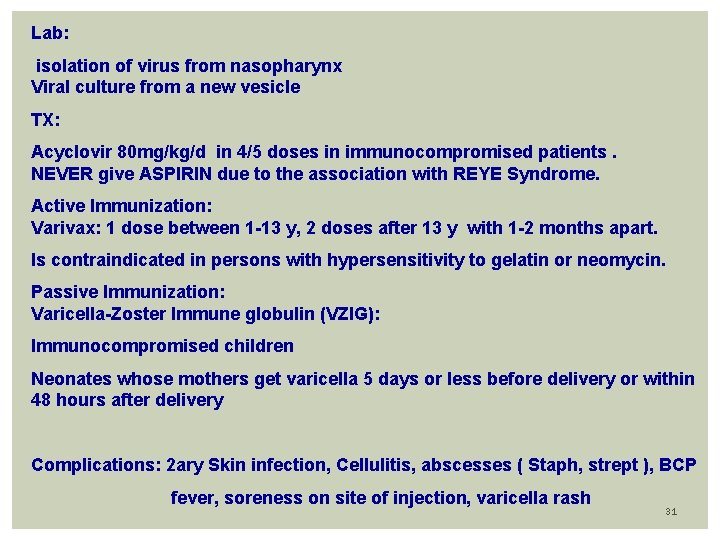
Lab: isolation of virus from nasopharynx Viral culture from a new vesicle TX: Acyclovir 80 mg/kg/d in 4/5 doses in immunocompromised patients. NEVER give ASPIRIN due to the association with REYE Syndrome. Active Immunization: Varivax: 1 dose between 1 -13 y, 2 doses after 13 y with 1 -2 months apart. Is contraindicated in persons with hypersensitivity to gelatin or neomycin. Passive Immunization: Varicella-Zoster Immune globulin (VZIG): Immunocompromised children Neonates whose mothers get varicella 5 days or less before delivery or within 48 hours after delivery Complications: 2 ary Skin infection, Cellulitis, abscesses ( Staph, strept ), BCP fever, soreness on site of injection, varicella rash 31
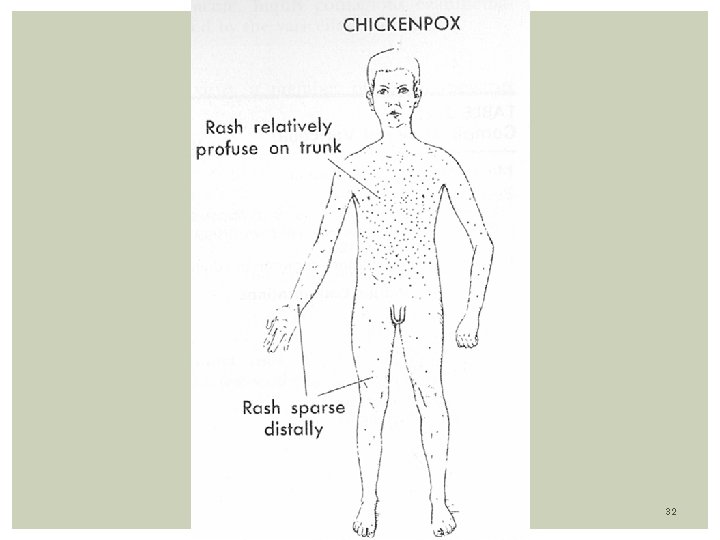
32
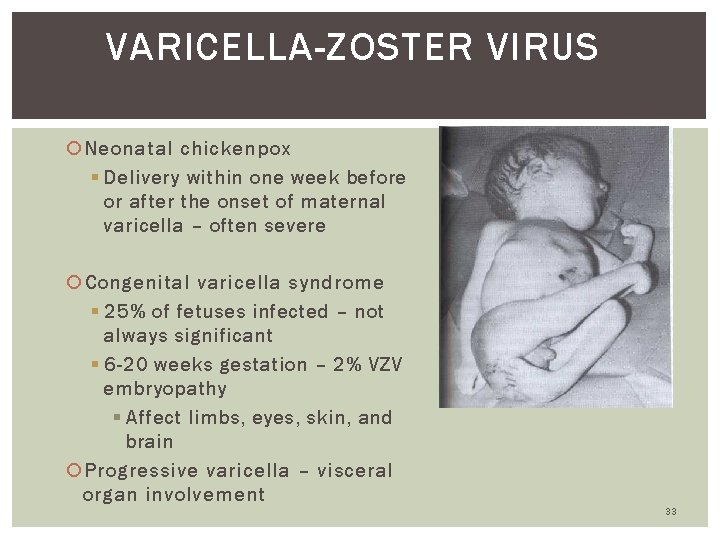
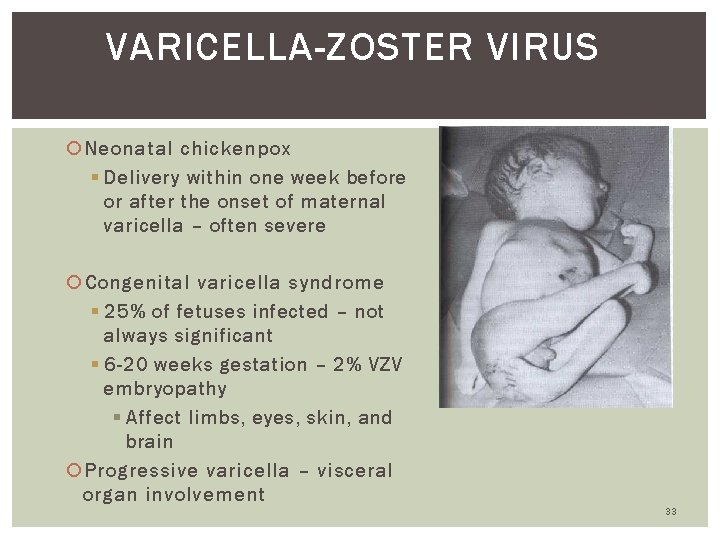
VARICELLA-ZOSTER VIRUS Neonatal chickenpox § Delivery within one week before or after the onset of maternal varicella – often severe Congenital varicella syndrome § 25% of fetuses infected – not always significant § 6 -20 weeks gestation – 2% VZV embryopathy § Affect limbs, eyes, skin, and brain Progressive varicella – visceral organ involvement 33
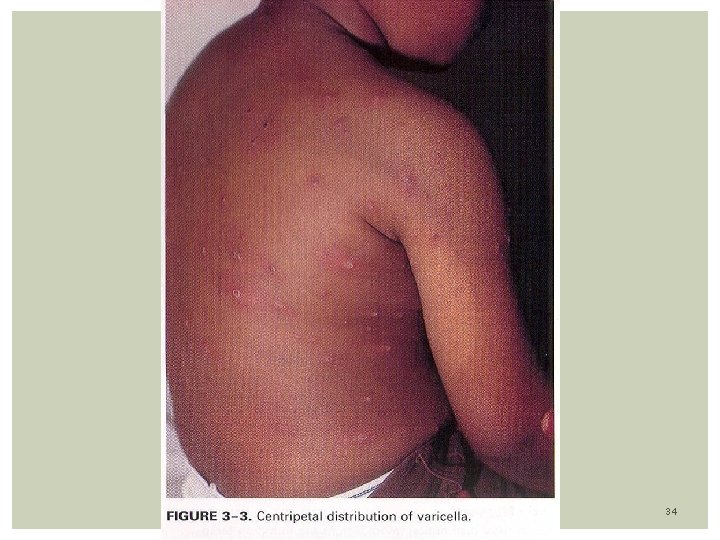
34

35

36
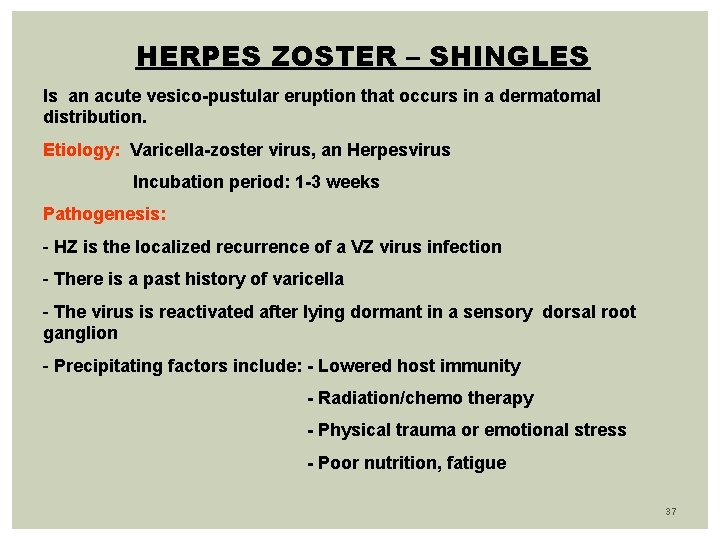
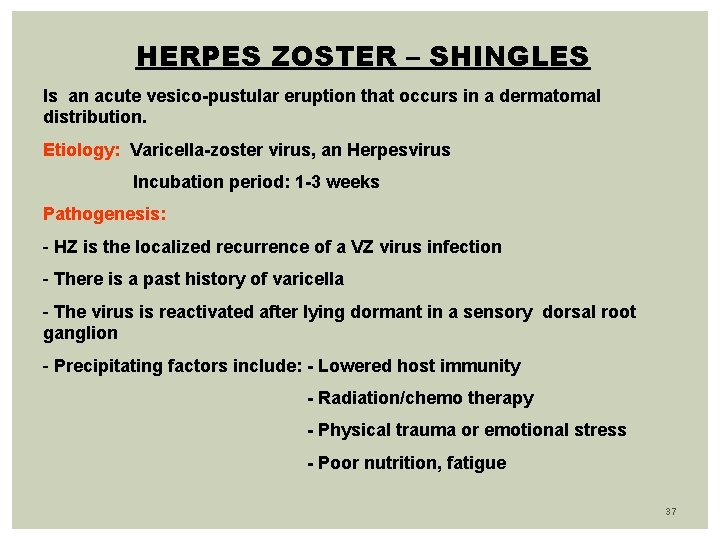
HERPES ZOSTER – SHINGLES Is an acute vesico-pustular eruption that occurs in a dermatomal distribution. Etiology: Varicella-zoster virus, an Herpesvirus Incubation period: 1 -3 weeks Pathogenesis: - HZ is the localized recurrence of a VZ virus infection - There is a past history of varicella - The virus is reactivated after lying dormant in a sensory dorsal root ganglion - Precipitating factors include: - Lowered host immunity - Radiation/chemo therapy - Physical trauma or emotional stress - Poor nutrition, fatigue 37
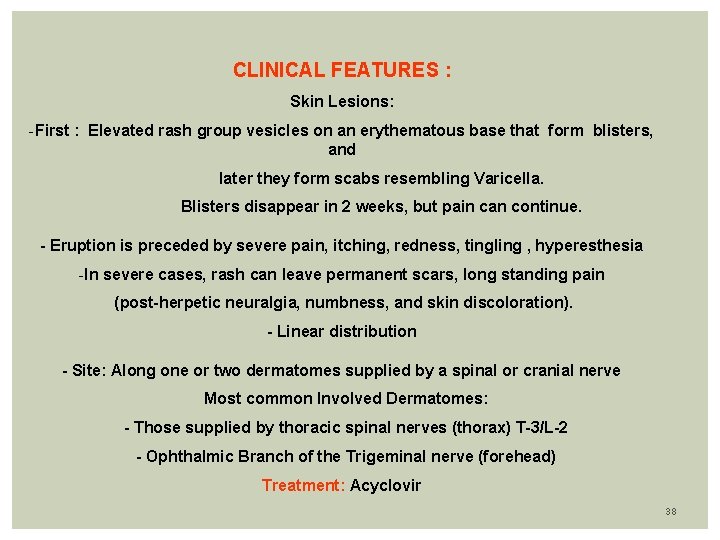
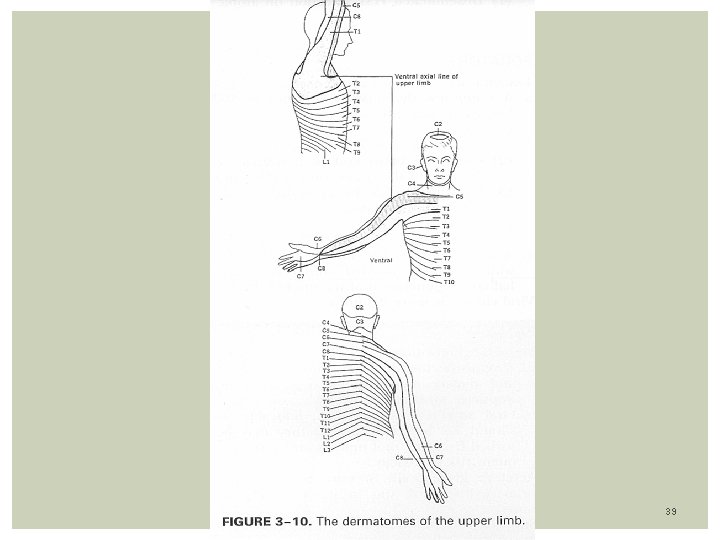
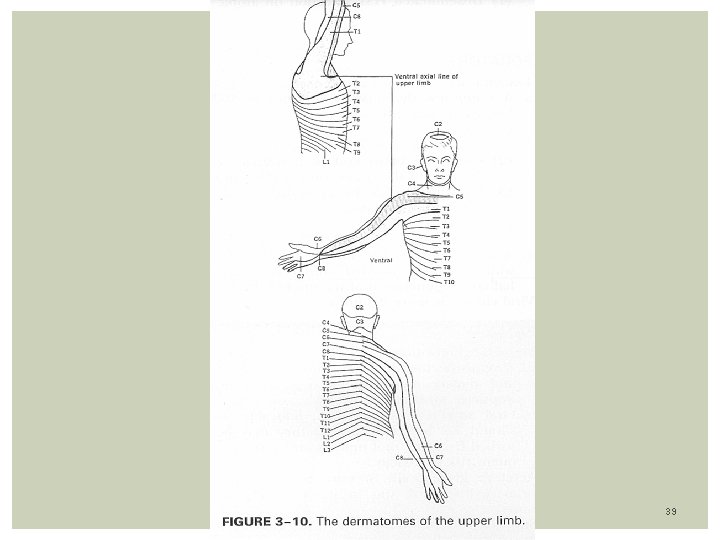
CLINICAL FEATURES : Skin Lesions: -First : Elevated rash group vesicles on an erythematous base that form blisters, and later they form scabs resembling Varicella. Blisters disappear in 2 weeks, but pain can continue. - Eruption is preceded by severe pain, itching, redness, tingling , hyperesthesia -In severe cases, rash can leave permanent scars, long standing pain (post-herpetic neuralgia, numbness, and skin discoloration). - Linear distribution - Site: Along one or two dermatomes supplied by a spinal or cranial nerve Most common Involved Dermatomes: - Those supplied by thoracic spinal nerves (thorax) T-3/L-2 - Ophthalmic Branch of the Trigeminal nerve (forehead) Treatment: Acyclovir 38
39
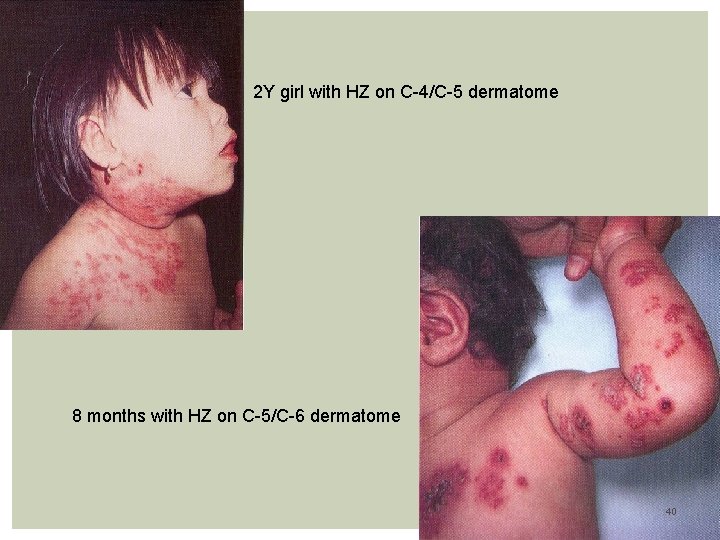
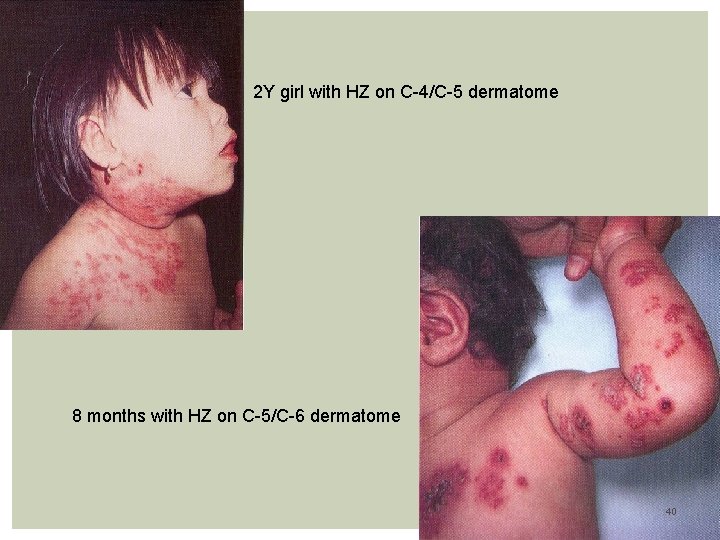
2 Y girl with HZ on C-4/C-5 dermatome 8 months with HZ on C-5/C-6 dermatome 40

Neurocutaneous pathway on the trunk HZ in the T-1 dermatome 41
HERPES SIMPLEX Caused by the Herpes-virus hominis, which consists of 2 related viruses: Herpes simplex virus type 1 (HSV-1) / Herpes simplex virus type-2 (HSV-2) produce infections involving mucocutaneous surfaces, the CNS. 42
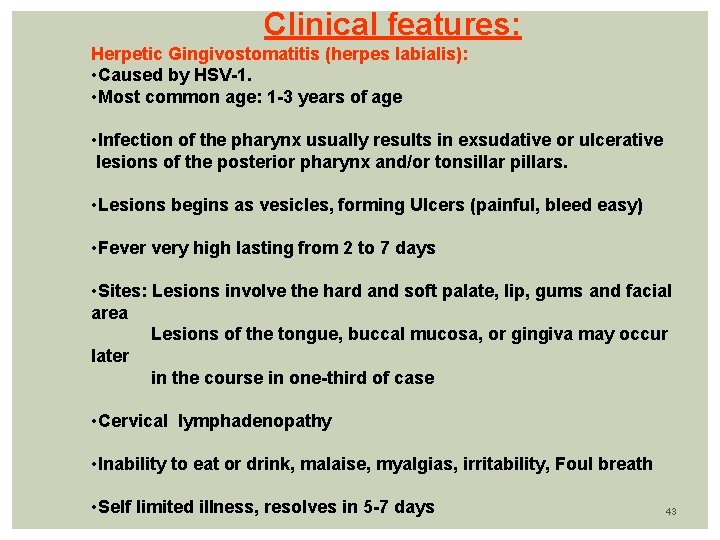
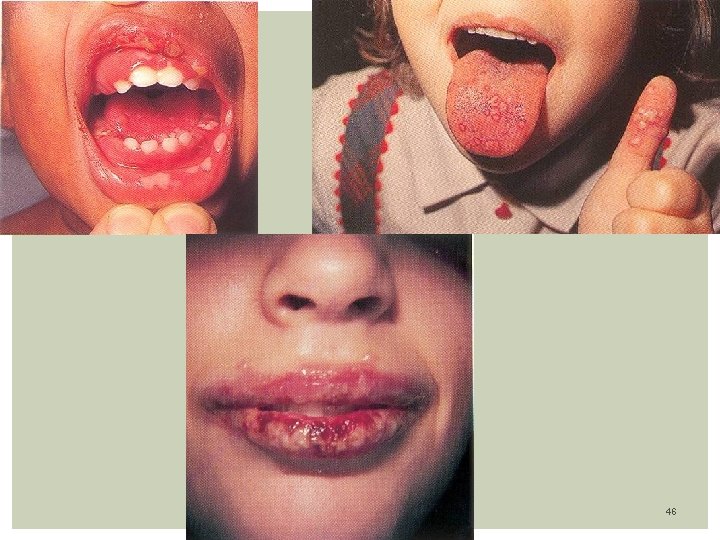
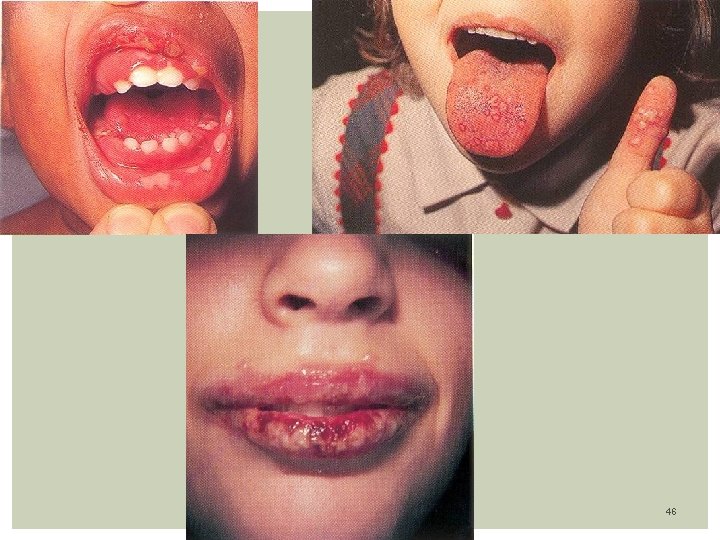
Clinical features: Herpetic Gingivostomatitis (herpes labialis): • Caused by HSV-1. • Most common age: 1 -3 years of age • Infection of the pharynx usually results in exsudative or ulcerative lesions of the posterior pharynx and/or tonsillar pillars. • Lesions begins as vesicles, forming Ulcers (painful, bleed easy) • Fever very high lasting from 2 to 7 days • Sites: Lesions involve the hard and soft palate, lip, gums and facial area Lesions of the tongue, buccal mucosa, or gingiva may occur later in the course in one-third of case • Cervical lymphadenopathy • Inability to eat or drink, malaise, myalgias, irritability, Foul breath • Self limited illness, resolves in 5 -7 days 43
Herpetic Vulvovaginitis: Caused by HSV-2 Genital herpes is characterized by fever, headache, malaise, and myalgias. Pain, itching, dysuria, vaginal and urethral discharge, and tender inguinal lymphadenopathy are the predominant local symptoms. Lesions may be present in varying stages, including vesicles, pustules, or painful erythematous ulcers. The cervix and urethra are involved in >80% of women with firstepisode infections. May result from sexual abuse 44
LAB: Molecular techniques are the gold standard. HSV infection is best confirmed in the lab by isolation of the virus in tissue culture or by demonstration of HSV antigens or DNA in scrapings from lesions. PCR is being used for the detection of HSV DNA TX: Supportive therapy: antipyretics, diet (cold drinks, soft diet) Acyclovir, Valacyclovir, Famciclovir (act on viral replication, causing chain termination of the viral DNA ) topical vidarabine, and cidofovir Idoxuridine ophtalmic drops when lesions are near the eye 45
46
Roseola It is an acute infection of infants characterized by a rash that appears after 3 -4 days of high fever Etiology: Human herpes virus 6 or 7, double stranded DNA virus Self-limited benign disease Epidemiology: Affects 6 months to 36 months infants. Peak 6 -7 months Incubation period 7 -15 days Transmission: Saliva, airbone Lab: Serology: Anti-HHV-6 Ig. M, Anti-HHV-7 Ig. M Polymerase chain reaction of HHV-6 DNA Complication: Febrile seizures during the prodromal stage TX: Supportive 47
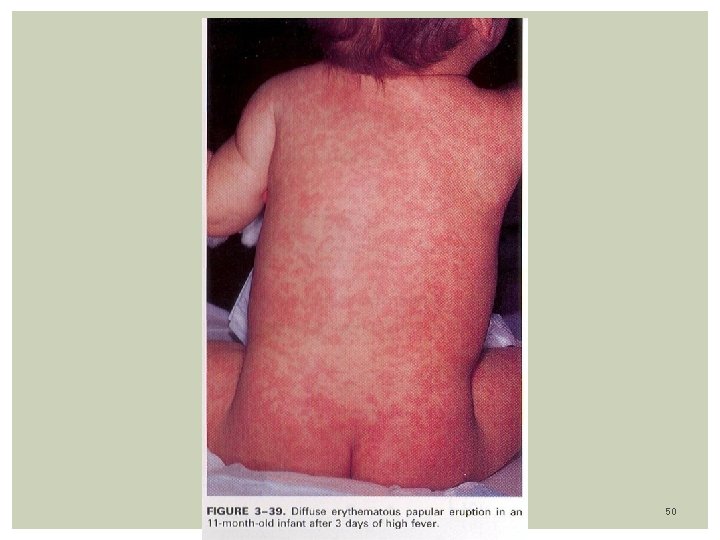
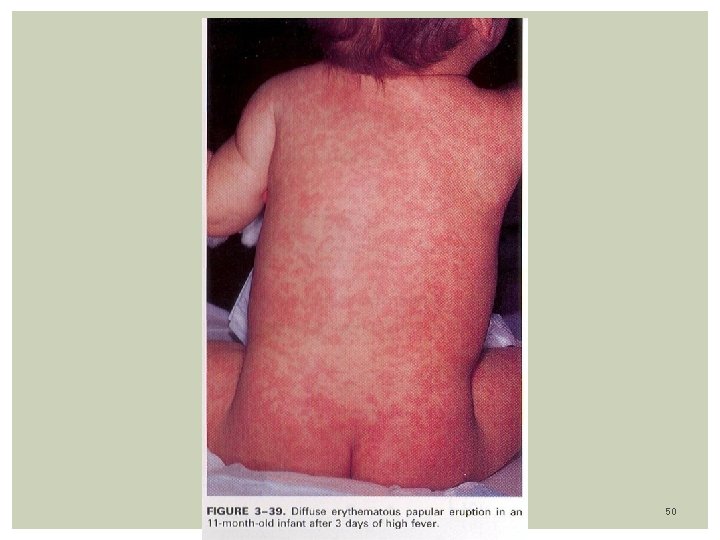
Clinical features: Incubation period 7 -15 days Sudden onset of fever lasting 1 -6 days, average of 4 days ( high as 40. 0 C) Infant looks well Mild irritability despite fevers Exam: reveal cervical adenopathy (posterior cervical & occipital) tonsillar, pharyngeal and erythematous tonsil 1/3 with diarrhea & vomiting Bulging anterior fontanel in 26% of patients Rash: Appears after Temp. drops suddenly on 4 th – 5 th day Rarely rash appears before fever has subsided completely Diffuse blanching pink morbiliform maculopapules rash Distribution on Trunk, Neck, Extremities, spares the face It last hours to 2 -3 days Clears without any pigmentation or desquamation 48

ROSEOLA 49
50
Erythema infectiosum (fifth disease) Etiology: Human Parvovirus B-19 Smallest human DNA virus (single strand of DNA) Transmission: Respiratory secretions Transplacental (higher risk at second trimester) Complications: Arthralgyas, Fetal hydrops in pregnants, anemia with low Reticulocytes ( aplastic crises) TX: Supportive 51
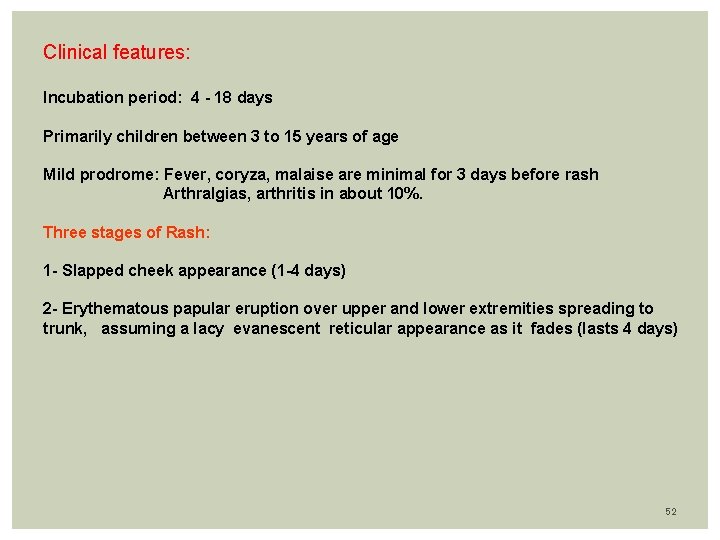
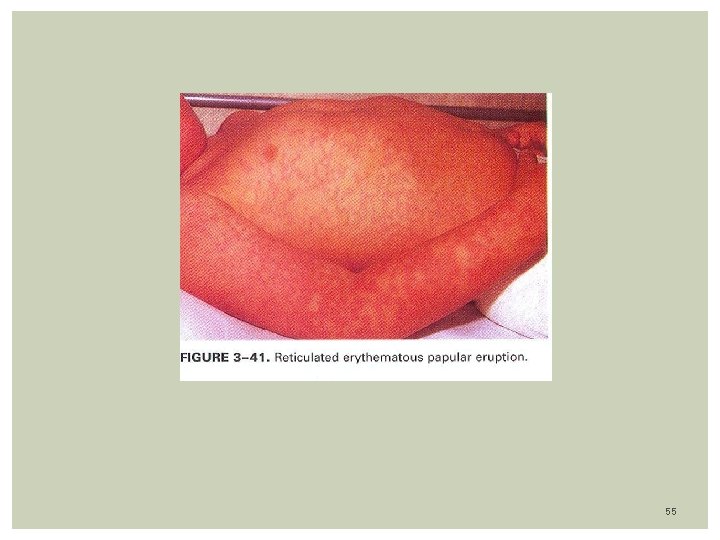
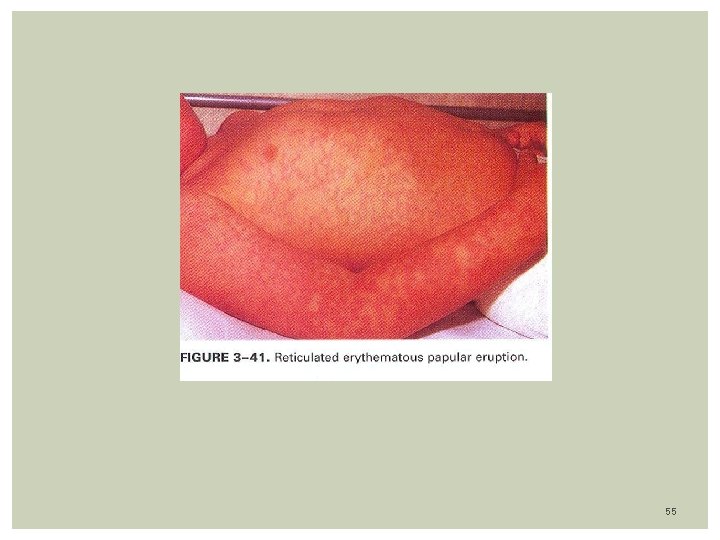
Clinical features: Incubation period: 4 - 18 days Primarily children between 3 to 15 years of age Mild prodrome: Fever, coryza, malaise are minimal for 3 days before rash Arthralgias, arthritis in about 10%. Three stages of Rash: 1 - Slapped cheek appearance (1 -4 days) 2 - Erythematous papular eruption over upper and lower extremities spreading to trunk, assuming a lacy evanescent reticular appearance as it fades (lasts 4 days) 52
Is precipitated by: Hot showers, vigorous exercise, sunlight 3 -Papular Purpuric Gloves and Socks syndrome (only hands and feet affected) Parvovirus B-19, usually teenagers, lasts 7 -14 days. Fever, rash and arthralgias. 53

54
55
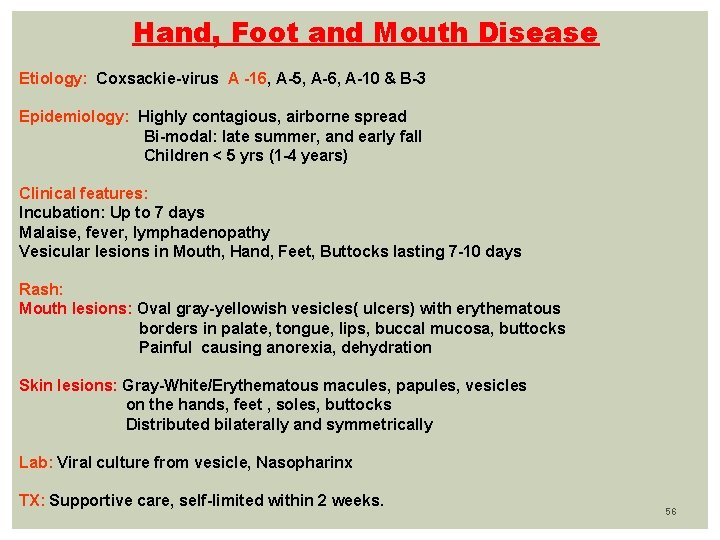
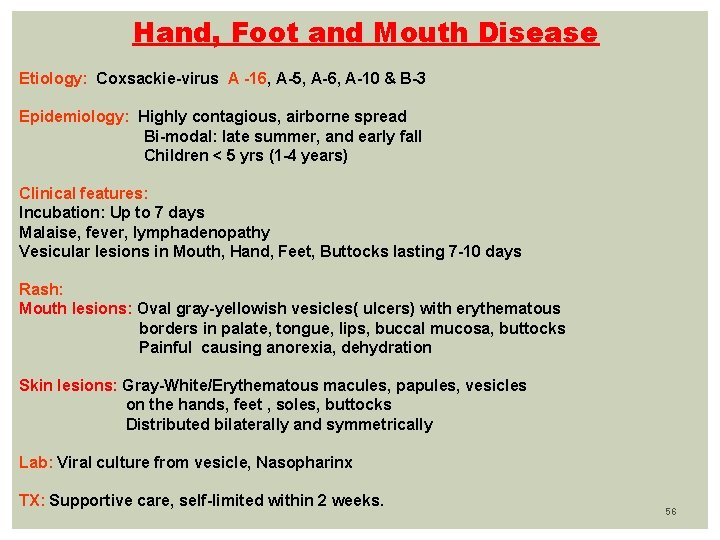
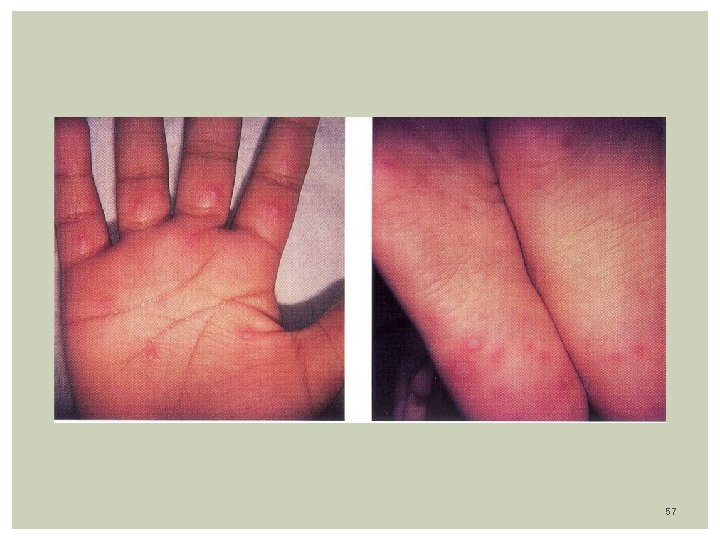
Hand, Foot and Mouth Disease Etiology: Coxsackie-virus A -16, A-5, A-6, A-10 & B-3 Epidemiology: Highly contagious, airborne spread Bi-modal: late summer, and early fall Children < 5 yrs (1 -4 years) Clinical features: Incubation: Up to 7 days Malaise, fever, lymphadenopathy Vesicular lesions in Mouth, Hand, Feet, Buttocks lasting 7 -10 days Rash: Mouth lesions: Oval gray-yellowish vesicles( ulcers) with erythematous borders in palate, tongue, lips, buccal mucosa, buttocks Painful causing anorexia, dehydration Skin lesions: Gray-White/Erythematous macules, papules, vesicles on the hands, feet , soles, buttocks Distributed bilaterally and symmetrically Lab: Viral culture from vesicle, Nasopharinx TX: Supportive care, self-limited within 2 weeks. 56
57
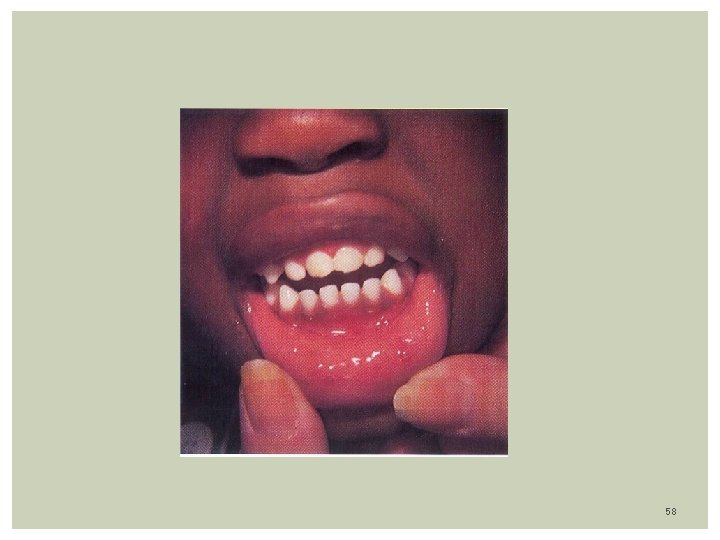
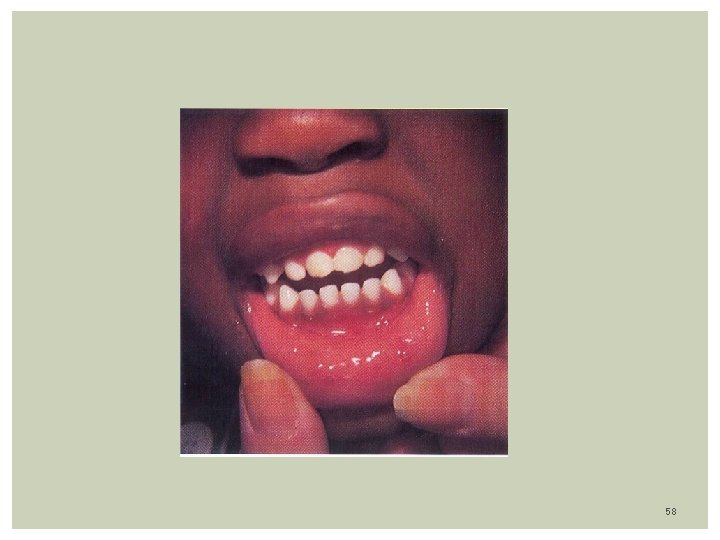
58

59
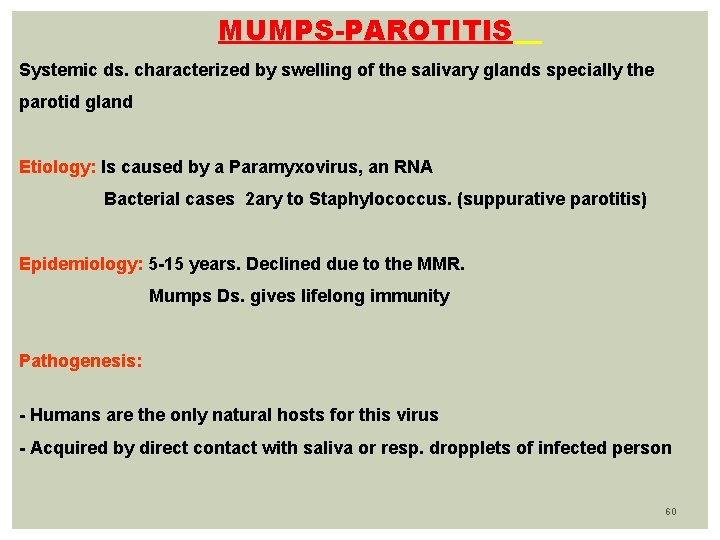
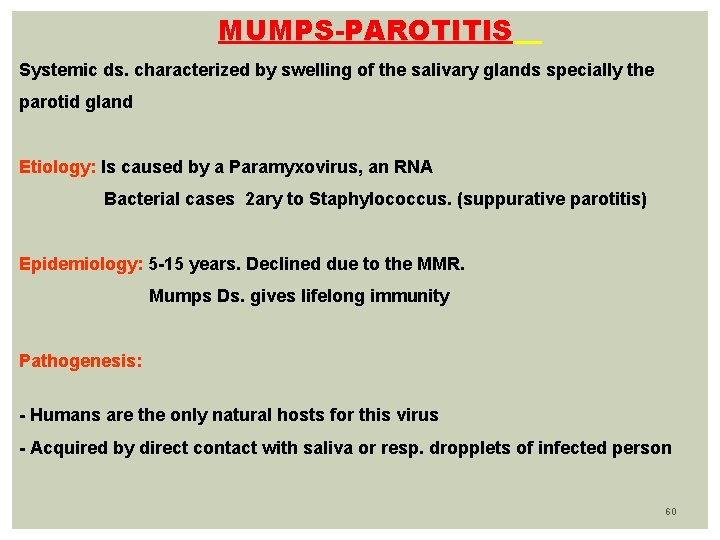
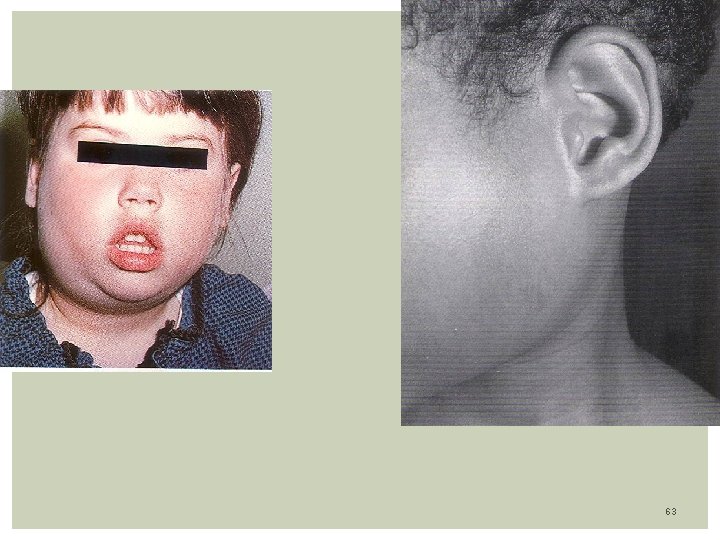
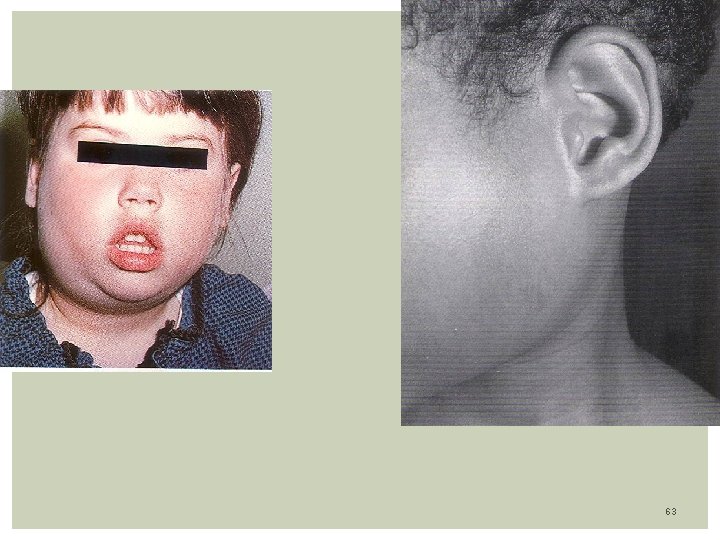
MUMPS-PAROTITIS Systemic ds. characterized by swelling of the salivary glands specially the parotid gland Etiology: Is caused by a Paramyxovirus, an RNA Bacterial cases 2 ary to Staphylococcus. (suppurative parotitis) Epidemiology: 5 -15 years. Declined due to the MMR. Mumps Ds. gives lifelong immunity Pathogenesis: - Humans are the only natural hosts for this virus - Acquired by direct contact with saliva or resp. dropplets of infected person 60
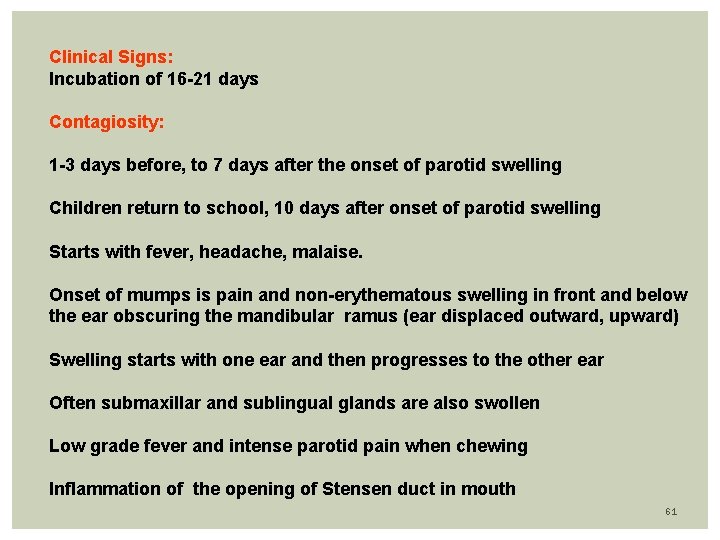
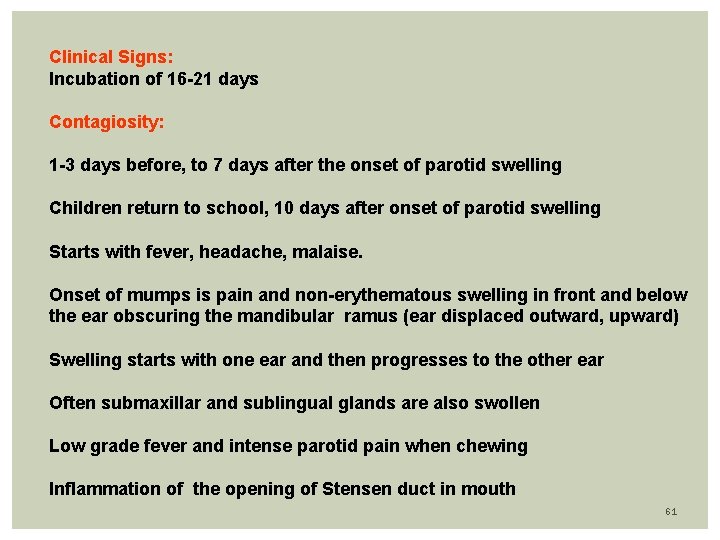
Clinical Signs: Incubation of 16 -21 days Contagiosity: 1 -3 days before, to 7 days after the onset of parotid swelling Children return to school, 10 days after onset of parotid swelling Starts with fever, headache, malaise. Onset of mumps is pain and non-erythematous swelling in front and below the ear obscuring the mandibular ramus (ear displaced outward, upward) Swelling starts with one ear and then progresses to the other ear Often submaxillar and sublingual glands are also swollen Low grade fever and intense parotid pain when chewing Inflammation of the opening of Stensen duct in mouth 61
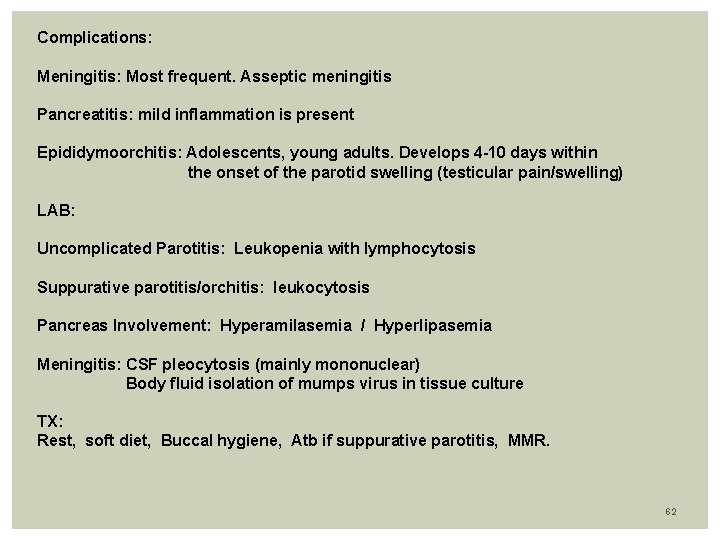
Complications: Meningitis: Most frequent. Asseptic meningitis Pancreatitis: mild inflammation is present Epididymoorchitis: Adolescents, young adults. Develops 4 -10 days within the onset of the parotid swelling (testicular pain/swelling) LAB: Uncomplicated Parotitis: Leukopenia with lymphocytosis Suppurative parotitis/orchitis: leukocytosis Pancreas Involvement: Hyperamilasemia / Hyperlipasemia Meningitis: CSF pleocytosis (mainly mononuclear) Body fluid isolation of mumps virus in tissue culture TX: Rest, soft diet, Buccal hygiene, Atb if suppurative parotitis, MMR. 62
63
INFECTIOUS MONONUCLEOSIS Lymphoproliferative self-limited disease caused by the Epstein-Barr virus. Etiology: EBV, a DNA virus, belongs to the Herpes group virus Epidemiology: Occurs in all age groups, predominates in adolescents and young adults. Mild cases can be seen in children Incubation: 30 -50 days EBV spreads via respiratory droplets, coughing, kissing Pathophysiology: EBV replicates in oropharyngeal epithelium Selective infection of B-lymphocytes occurs, resulting in proliferation of cells in tonsils, lymph nodes, spleen 64
Clinical Features: Incubation period of 30 -50 days Low grade fever, sore throat, coryza, malaise, Exsudative pharyngitis (50%) with palatal petecchia Cervical Lymphadenopathy- Enlarged, usually nontender Hepatomegaly Splenomegaly: moderate enlargement (50%) Skin rash: Seen in 10 -15%. Increase to 40% if penicillin derivatives is used CNS features: Encephalitis, aseptic meningitis, Guillain-Barre syndrome Classic illness is characterized by: fatigue, low grade fever, malaise, tonsillopharyngitis (often exsudative) adenopathy, hepatosplenomegaly (may persist for months) 65
LAB: CBC: > 10% of atypical lymphocytes (greater than 50% lymphocytes), Leukocytosis Liver enzymes: Mild hepatitis is found, jaundice is rare EBV serology: Elisa (Monospot): rapid slide agglutinin test for heterophile antibodies: Often negative in children under 5 years old Detects 90% of cases in adolescents Anti-VCA Ig. G/Ig. M (viral capsid antigen) recent/past infection EBNA: Ebstein Barr Nuclear Antigen- positive means no latent infection 66
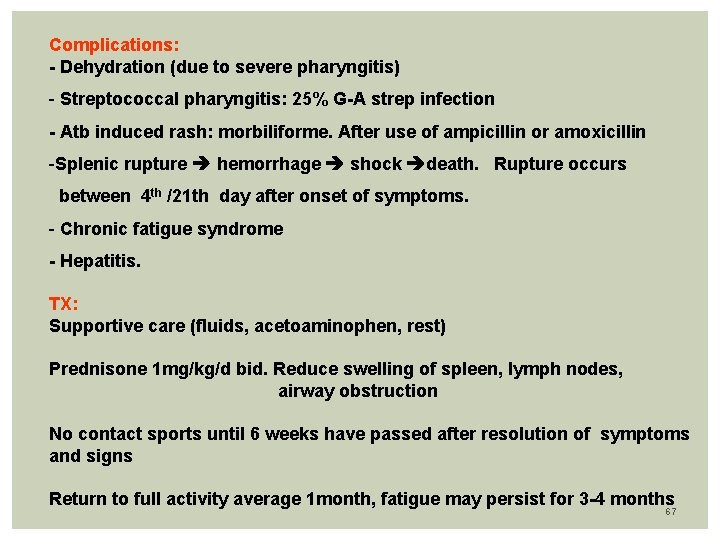
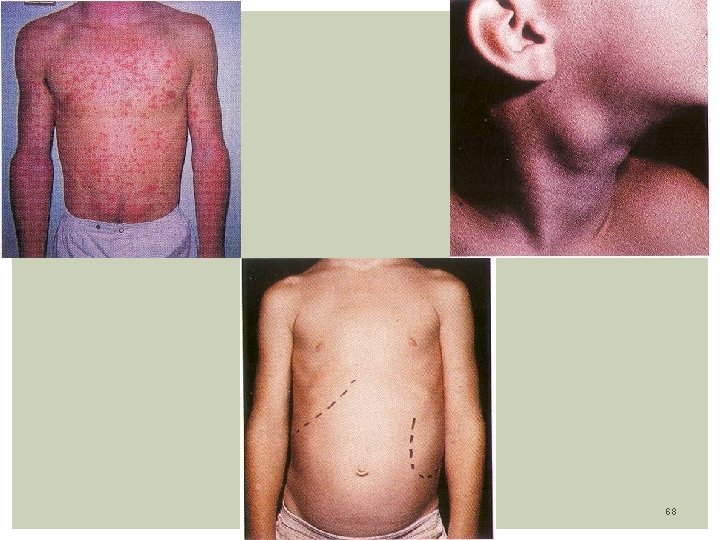
Complications: - Dehydration (due to severe pharyngitis) - Streptococcal pharyngitis: 25% G-A strep infection - Atb induced rash: morbiliforme. After use of ampicillin or amoxicillin -Splenic rupture hemorrhage shock death. Rupture occurs between 4 th /21 th day after onset of symptoms. - Chronic fatigue syndrome - Hepatitis. TX: Supportive care (fluids, acetoaminophen, rest) Prednisone 1 mg/kg/d bid. Reduce swelling of spleen, lymph nodes, airway obstruction No contact sports until 6 weeks have passed after resolution of symptoms and signs Return to full activity average 1 month, fatigue may persist for 3 -4 months 67
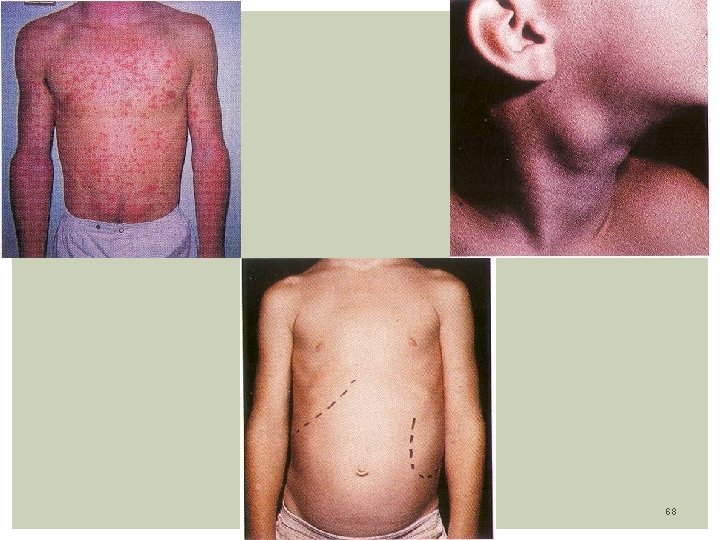
68
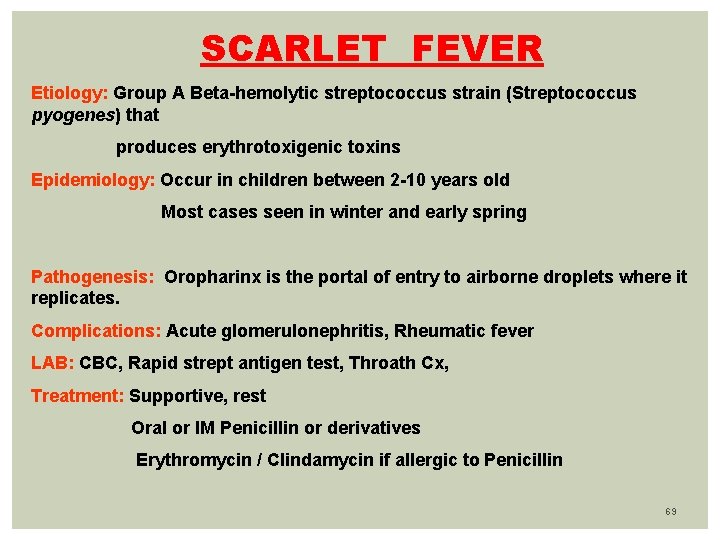
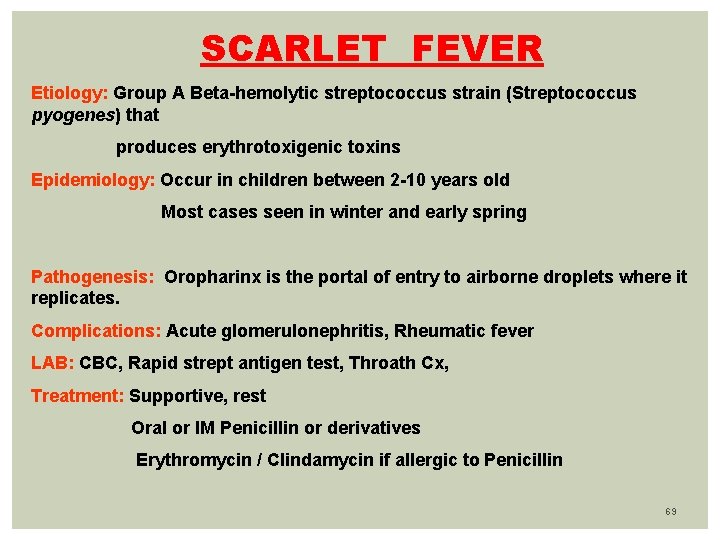
SCARLET FEVER Etiology: Group A Beta-hemolytic streptococcus strain (Streptococcus pyogenes) that produces erythrotoxigenic toxins Epidemiology: Occur in children between 2 -10 years old Most cases seen in winter and early spring Pathogenesis: Oropharinx is the portal of entry to airborne droplets where it replicates. Complications: Acute glomerulonephritis, Rheumatic fever LAB: CBC, Rapid strept antigen test, Throath Cx, Treatment: Supportive, rest Oral or IM Penicillin or derivatives Erythromycin / Clindamycin if allergic to Penicillin 69
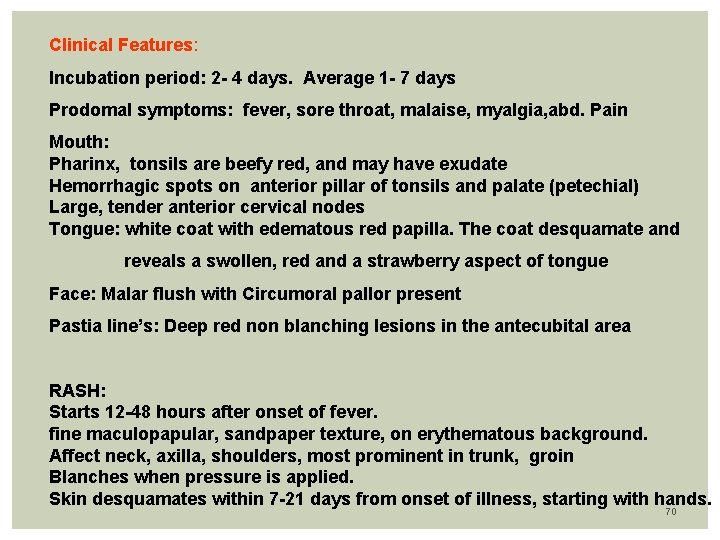
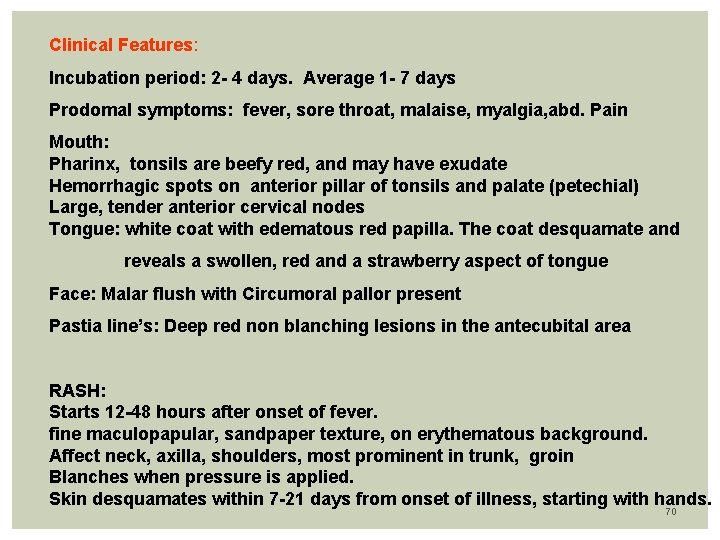
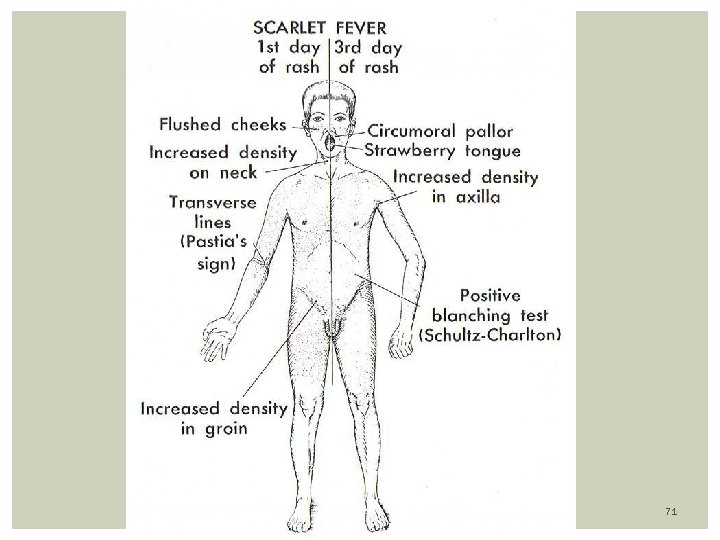
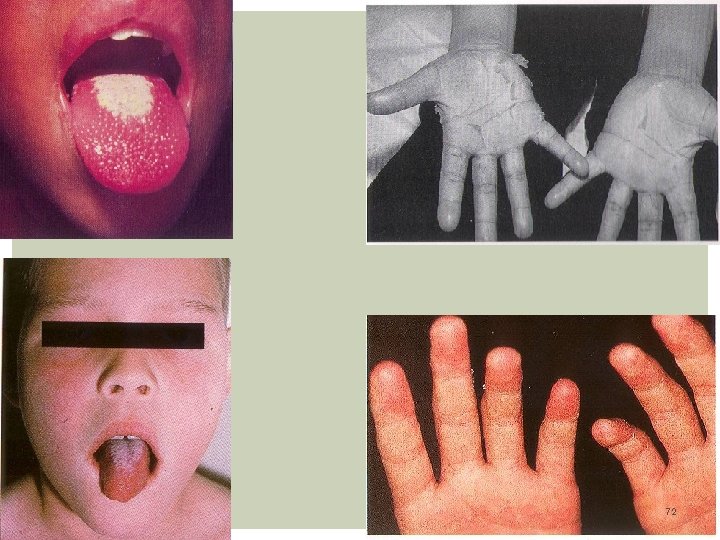
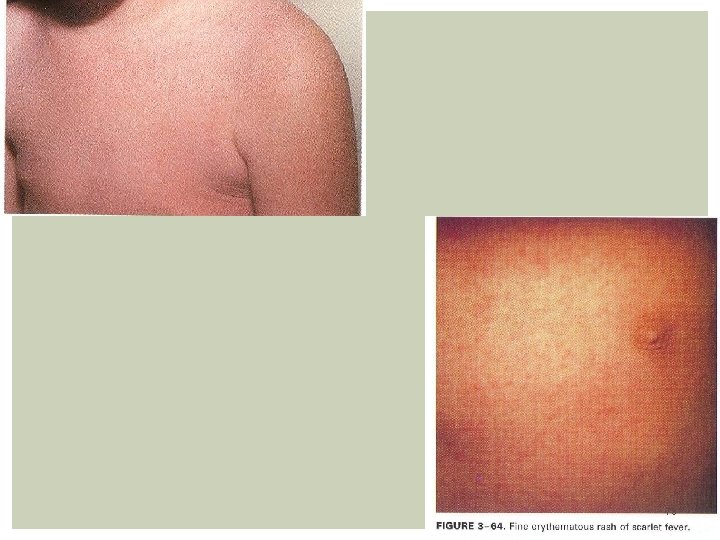
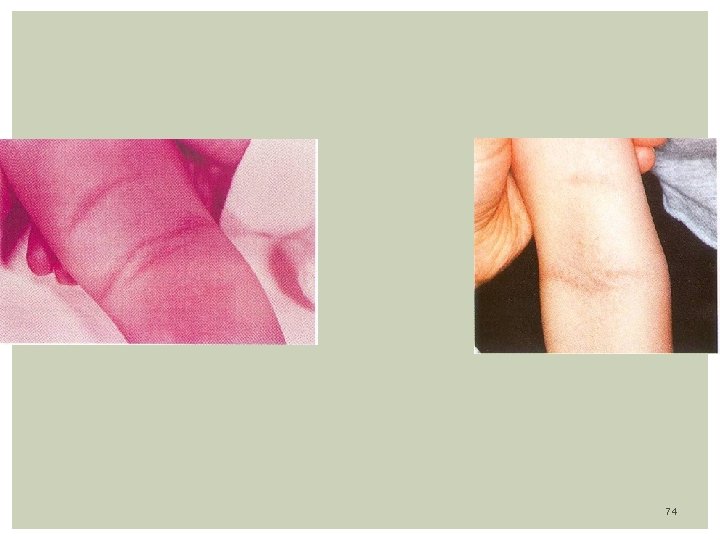
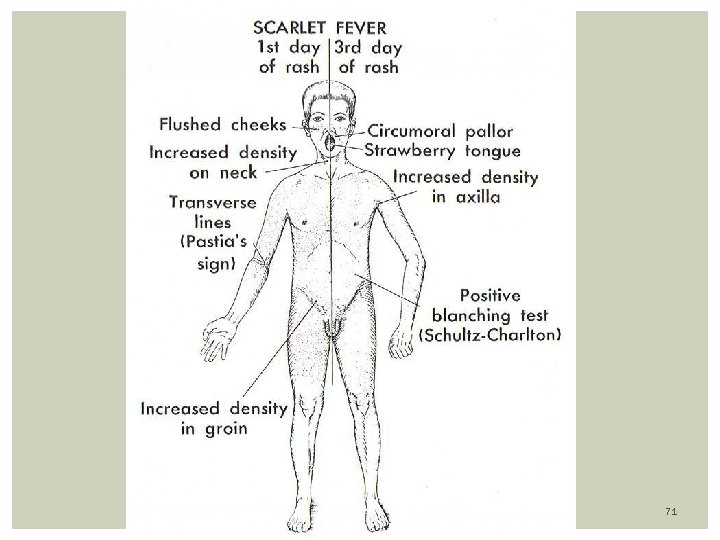
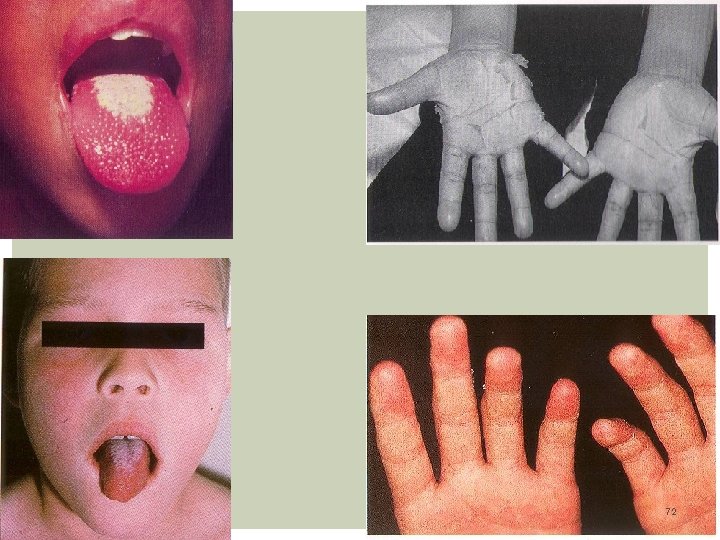
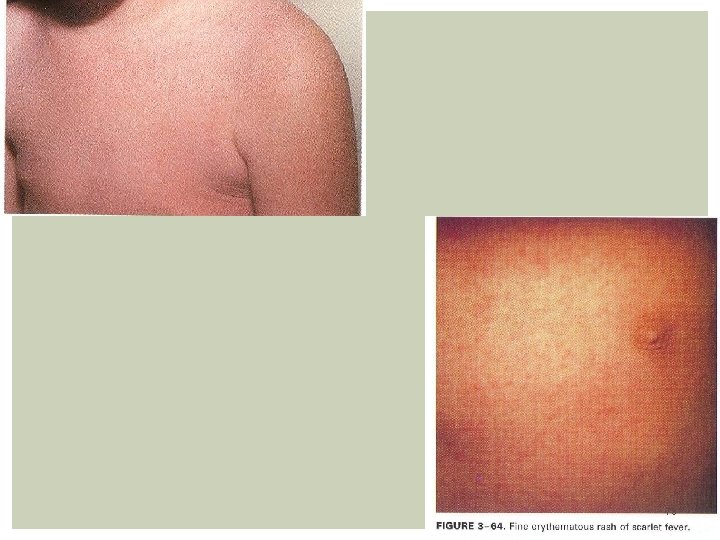
Clinical Features: Incubation period: 2 - 4 days. Average 1 - 7 days Prodomal symptoms: fever, sore throat, malaise, myalgia, abd. Pain Mouth: Pharinx, tonsils are beefy red, and may have exudate Hemorrhagic spots on anterior pillar of tonsils and palate (petechial) Large, tender anterior cervical nodes Tongue: white coat with edematous red papilla. The coat desquamate and reveals a swollen, red and a strawberry aspect of tongue Face: Malar flush with Circumoral pallor present Pastia line’s: Deep red non blanching lesions in the antecubital area RASH: Starts 12 -48 hours after onset of fever. fine maculopapular, sandpaper texture, on erythematous background. Affect neck, axilla, shoulders, most prominent in trunk, groin Blanches when pressure is applied. Skin desquamates within 7 -21 days from onset of illness, starting with hands. 70
71
72
73
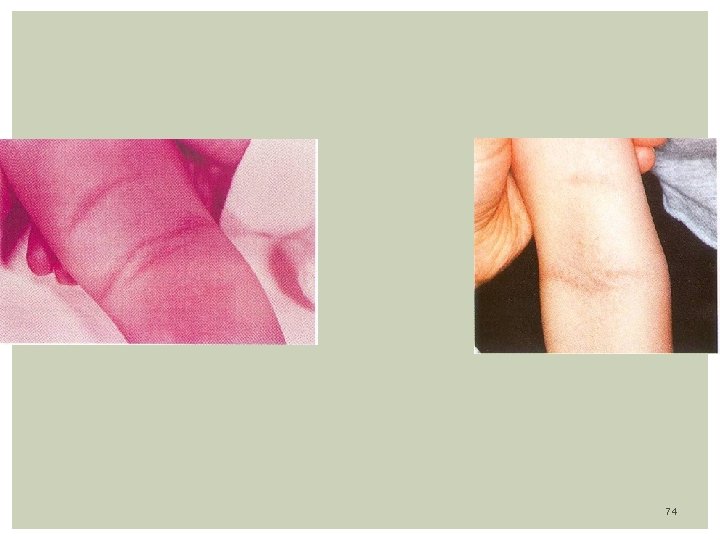
74

THANK YOU 75
 Genital infections
Genital infections Storch infections
Storch infections Postpartum infections
Postpartum infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Nosocomial infections
Nosocomial infections Bone and joint infections
Bone and joint infections Opportunistic infections
Opportunistic infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Understanding the mirai botnet
Understanding the mirai botnet Infections opportunistes digestives
Infections opportunistes digestives Methotrexate yeast infection
Methotrexate yeast infection Genital infections
Genital infections Acute gingival infections
Acute gingival infections Storch infections
Storch infections Eye infections
Eye infections Opportunistic infections
Opportunistic infections Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Dot
Dot điện thế nghỉ
điện thế nghỉ Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Phản ứng thế ankan
Phản ứng thế ankan Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Ng-html
Ng-html Hệ hô hấp
Hệ hô hấp Bảng số nguyên tố
Bảng số nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Thang điểm glasgow
Thang điểm glasgow ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Thẻ vin
Thẻ vin Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Bổ thể
Bổ thể Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết V cc cc
V cc cc Thể thơ truyền thống
Thể thơ truyền thống Phép trừ bù
Phép trừ bù Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào Diễn thế sinh thái là
Diễn thế sinh thái là đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công thức tính thế năng
Công thức tính thế năng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Diseases caused by bacteria
Diseases caused by bacteria Abcsses
Abcsses Glott medical term
Glott medical term What are periradicular tissues
What are periradicular tissues Chapter 23 lesson 1 understanding communicable diseases
Chapter 23 lesson 1 understanding communicable diseases Std
Std Myth and fallacies about non-communicable diseases
Myth and fallacies about non-communicable diseases Nutritional diseases
Nutritional diseases Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Public health entomology certificate
Public health entomology certificate Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases Migrants
Migrants What is natural history of disease
What is natural history of disease Examples of communicable diseases
Examples of communicable diseases Different types of diseases
Different types of diseases Flaccid gingiva
Flaccid gingiva Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Gingival diseases
Gingival diseases