Starting ART in the Context of Opportunistic Infections



- Slides: 30
Starting ART in the Context of Opportunistic Infections HAIVN Harvard Medical School AIDS Initiative in Vietnam
Learning Objectives By the end of this session, participants should be able to: n Explain the best time and clinical conditions that an acute OI patient can start ART n Describe how to start ART in the context of acute OIs 2

Starting ARV in the Context of OIs: Advantages and Disadvantages Advantages n Recovery of immune system n Mortality reduction n Treatment of OI n Prevention of other OI and complications due to HIV disease Disadvantages n Risk of IRIS n Drug interactions n Drug adverse effects n Number of pills: adherence It’s never an emergency to start ART 3
General Principles (1) n Little data exist on best time to start ART when a patient is being treated for an OI • Clinical judgment must be used n Before starting ARV, patient should be: • Responding to OI therapy, clinically stable • Tolerating OI drugs with no side effects 4
General Principles (2) n n It’s important to know drug-drug interactions of all medications before they are prescribed If the patient is already on ART, do not stop • Continue ART and start OI treatment • Change ART regimen if necessary to avoid interactions with OI drugs 5

With Which OIs do you Need to Start ARVs Right Away?
OIs that Require ARVs to Resolve n n Diarrheal agents Kaposi Sarcoma Progressive Multifocal Leukoencephalopathy (PML) Non-infectious causes: • Malignancy • Autoimmune conditions • Skin conditions In these cases, ARVs should be started as soon as possible 7
With Which OIs Should You Delay the Start of ART?

OIs With Which ART Should Be Delayed n n n Tuberculosis and other mycobacterial infections Cerebral toxoplasmosis Pneumocystis Jiroveci Pneumonia (PCP) Cryptococcosis Penicillium marneffei Other fungal infections 9
Starting ARVs in the Context of an Acute OI
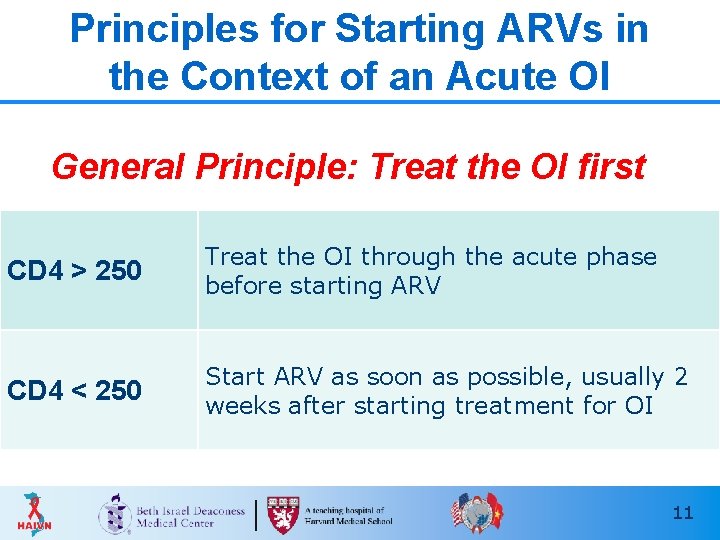
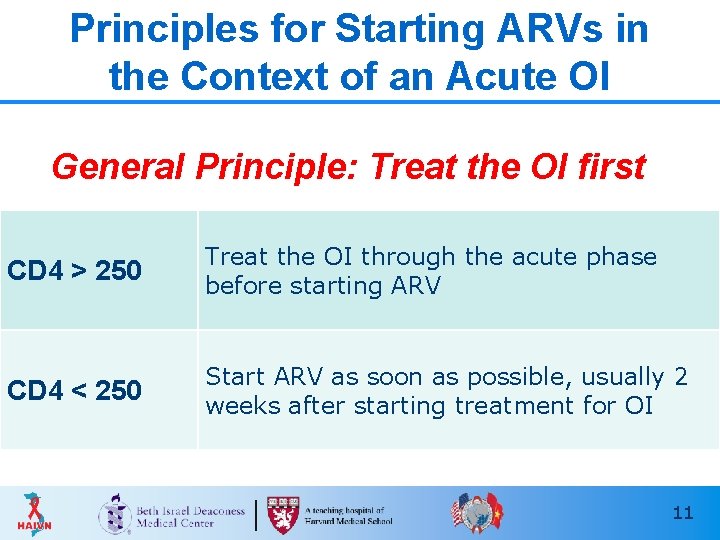
Principles for Starting ARVs in the Context of an Acute OI General Principle: Treat the OI first CD 4 > 250 Treat the OI through the acute phase before starting ARV CD 4 < 250 Start ARV as soon as possible, usually 2 weeks after starting treatment for OI 11
ART and Tuberculosis
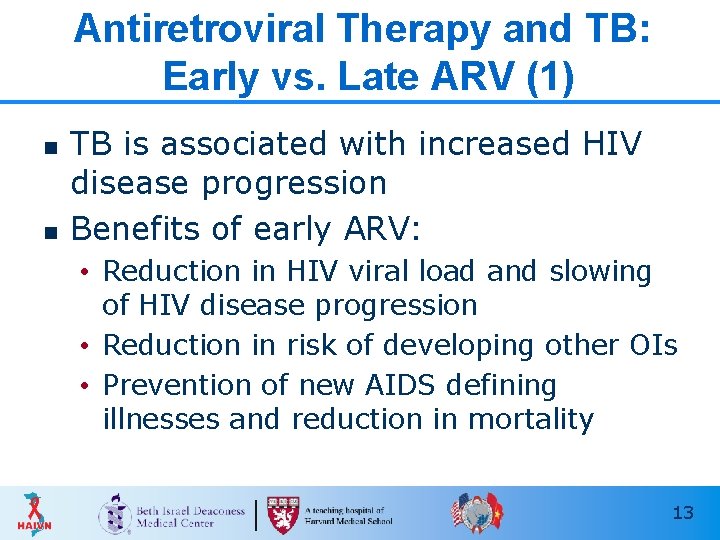
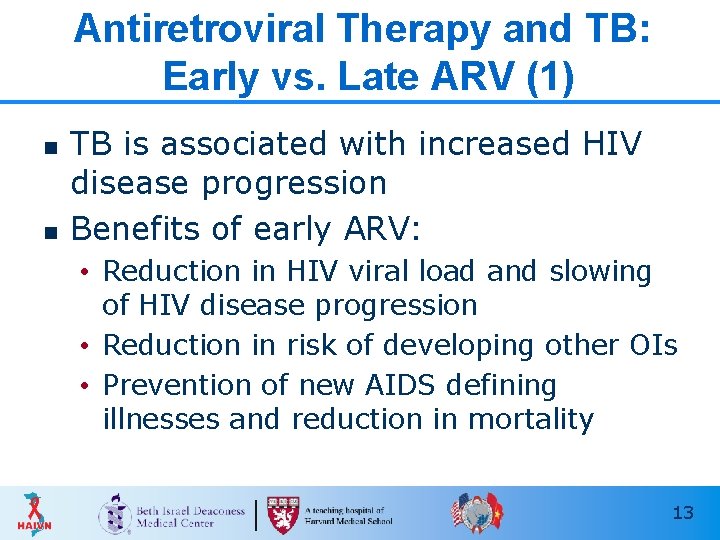
Antiretroviral Therapy and TB: Early vs. Late ARV (1) n n TB is associated with increased HIV disease progression Benefits of early ARV: • Reduction in HIV viral load and slowing of HIV disease progression • Reduction in risk of developing other OIs • Prevention of new AIDS defining illnesses and reduction in mortality 13
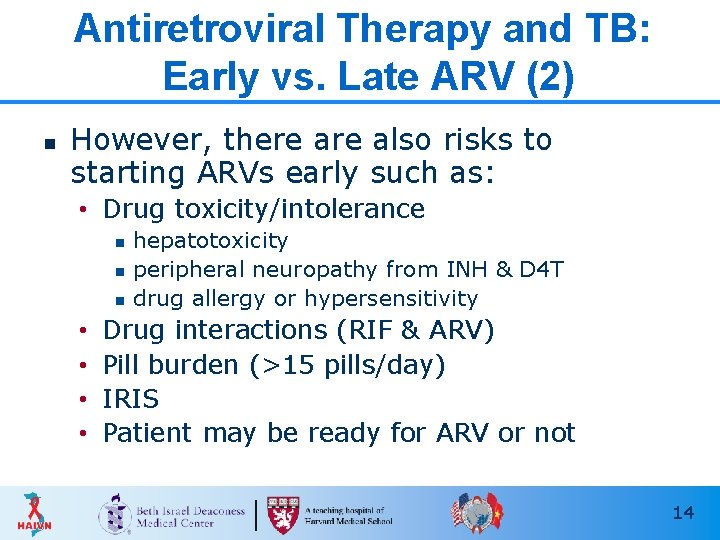
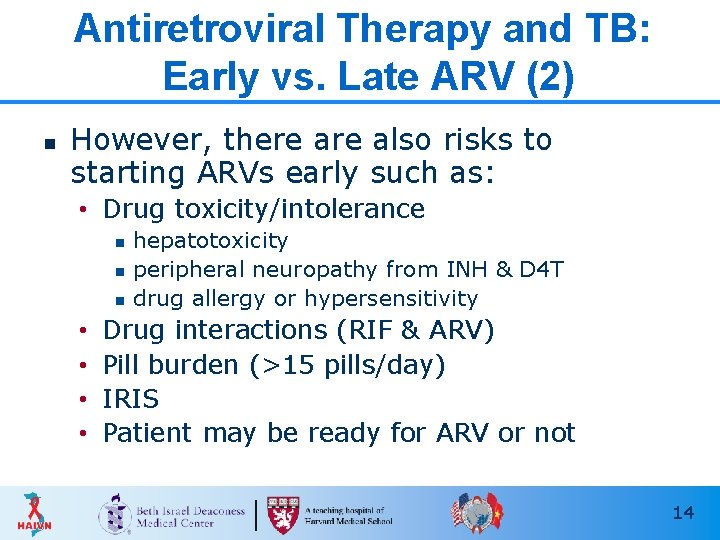
Antiretroviral Therapy and TB: Early vs. Late ARV (2) n However, there also risks to starting ARVs early such as: • Drug toxicity/intolerance n n n • • hepatotoxicity peripheral neuropathy from INH & D 4 T drug allergy or hypersensitivity Drug interactions (RIF & ARV) Pill burden (>15 pills/day) IRIS Patient may be ready for ARV or not 14
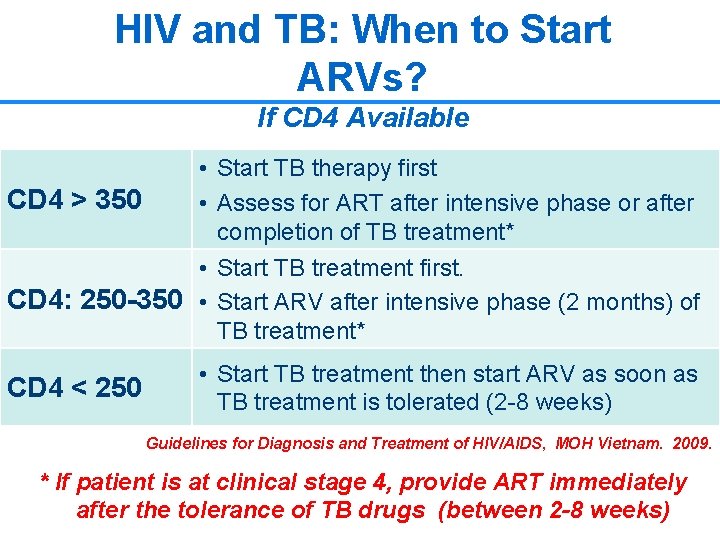
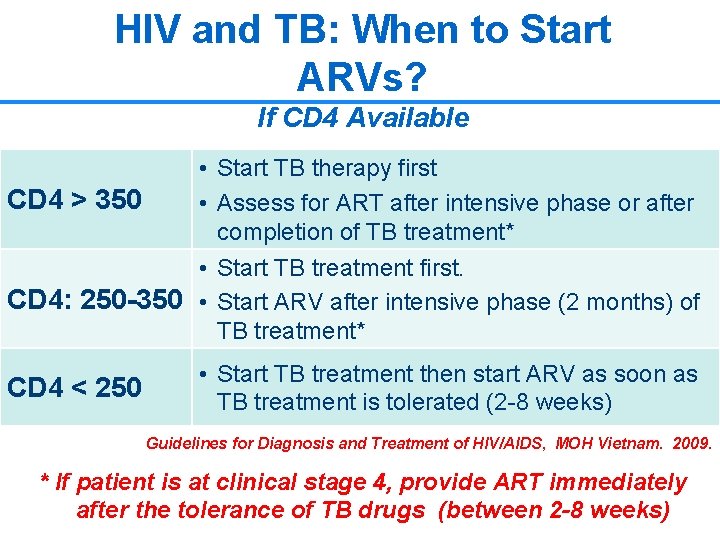
HIV and TB: When to Start ARVs? If CD 4 Available • Start TB therapy first CD 4 > 350 • Assess for ART after intensive phase or after completion of TB treatment* • Start TB treatment first. CD 4: 250 -350 • Start ARV after intensive phase (2 months) of TB treatment* CD 4 < 250 • Start TB treatment then start ARV as soon as TB treatment is tolerated (2 -8 weeks) Guidelines for Diagnosis and Treatment of HIV/AIDS, MOH Vietnam. 2009. * If patient is at clinical stage 4, provide ART immediately after the tolerance of TB drugs (between 2 -8 weeks) 15
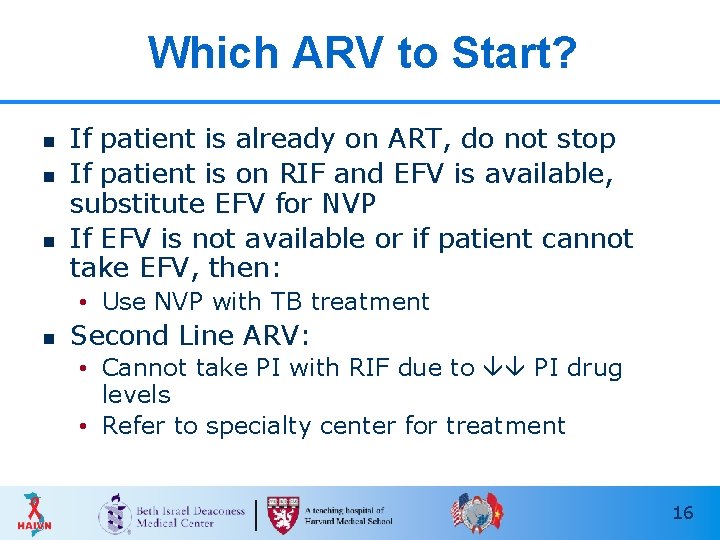
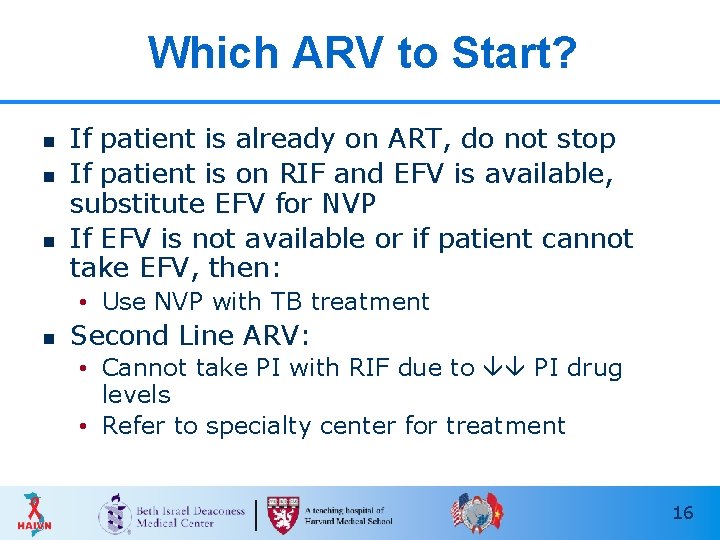
Which ARV to Start? n n n If patient is already on ART, do not stop If patient is on RIF and EFV is available, substitute EFV for NVP If EFV is not available or if patient cannot take EFV, then: • Use NVP with TB treatment n Second Line ARV: • Cannot take PI with RIF due to PI drug levels • Refer to specialty center for treatment 16
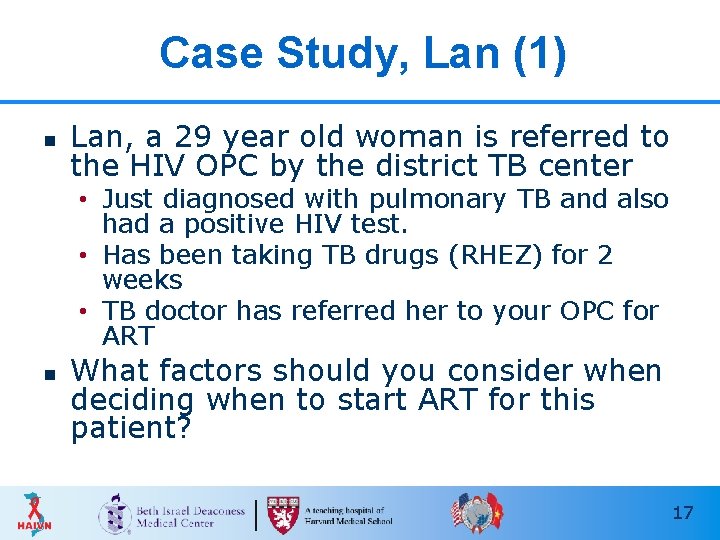
Case Study, Lan (1) n Lan, a 29 year old woman is referred to the HIV OPC by the district TB center • Just diagnosed with pulmonary TB and also had a positive HIV test. • Has been taking TB drugs (RHEZ) for 2 weeks • TB doctor has referred her to your OPC for ART n What factors should you consider when deciding when to start ART for this patient? 17
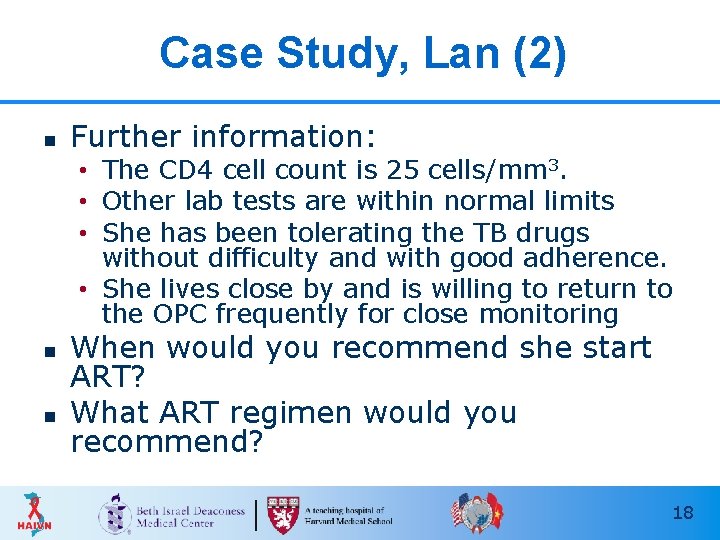
Case Study, Lan (2) n Further information: • The CD 4 cell count is 25 cells/mm 3. • Other lab tests are within normal limits • She has been tolerating the TB drugs without difficulty and with good adherence. • She lives close by and is willing to return to the OPC frequently for close monitoring n n When would you recommend she start ART? What ART regimen would you recommend? 18
ART and Cryptococcus Meningitis
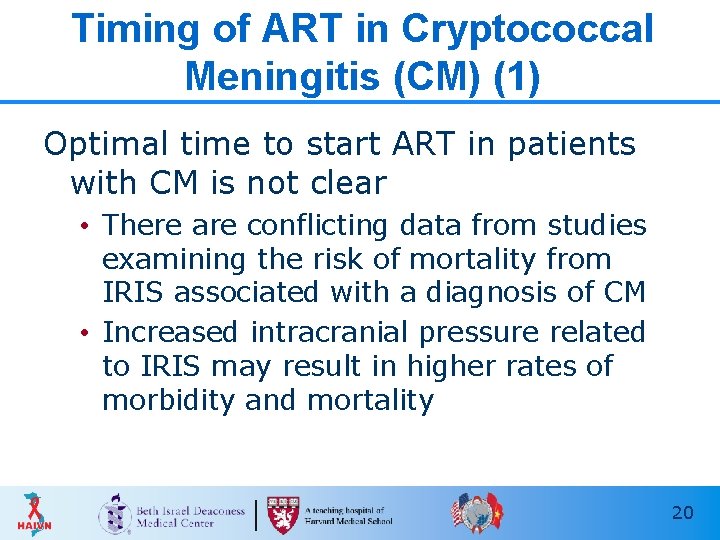
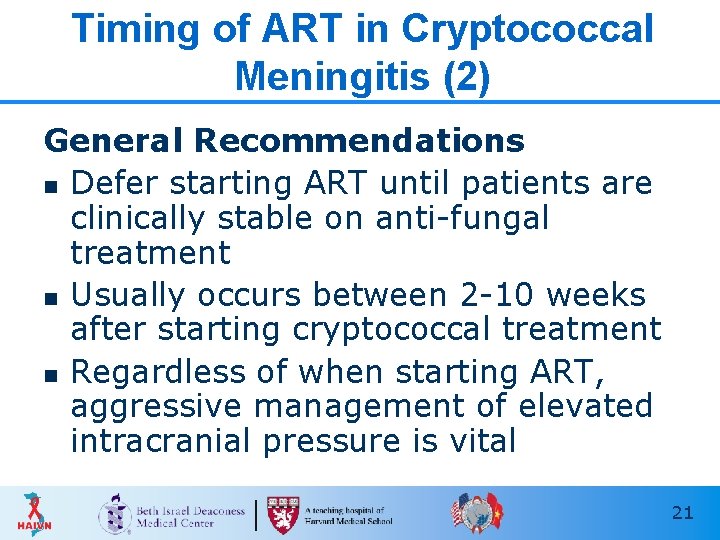
Timing of ART in Cryptococcal Meningitis (CM) (1) Optimal time to start ART in patients with CM is not clear • There are conflicting data from studies examining the risk of mortality from IRIS associated with a diagnosis of CM • Increased intracranial pressure related to IRIS may result in higher rates of morbidity and mortality 20
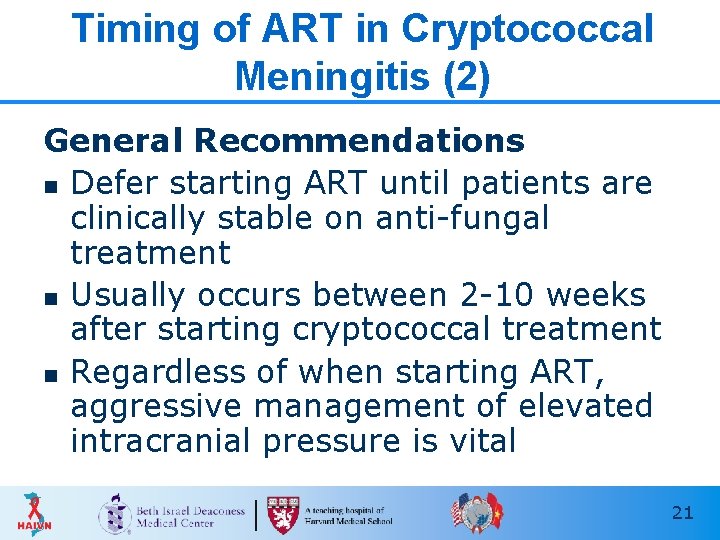
Timing of ART in Cryptococcal Meningitis (2) General Recommendations n Defer starting ART until patients are clinically stable on anti-fungal treatment n Usually occurs between 2 -10 weeks after starting cryptococcal treatment n Regardless of when starting ART, aggressive management of elevated intracranial pressure is vital 21
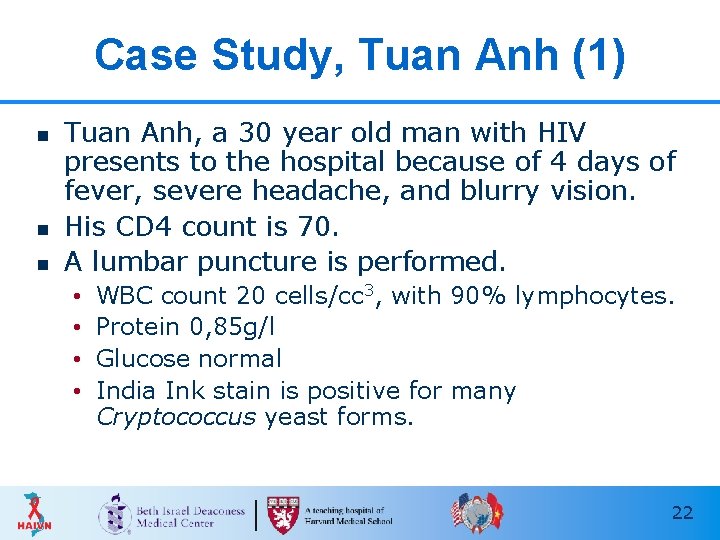
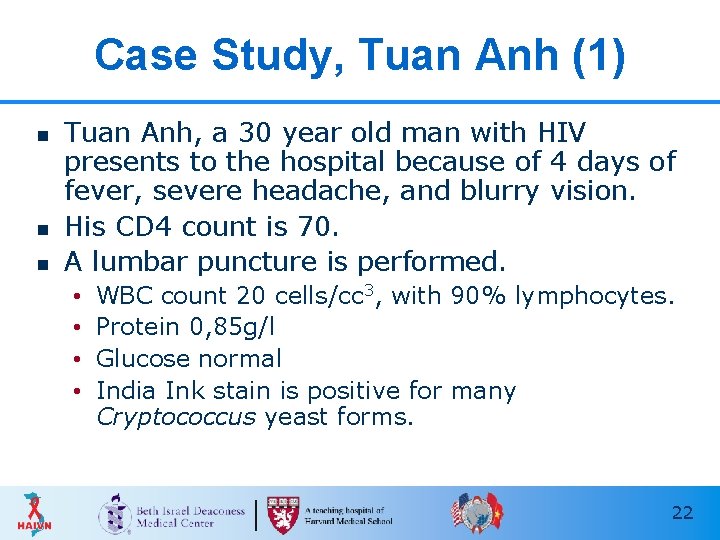
Case Study, Tuan Anh (1) n n n Tuan Anh, a 30 year old man with HIV presents to the hospital because of 4 days of fever, severe headache, and blurry vision. His CD 4 count is 70. A lumbar puncture is performed. • • WBC count 20 cells/cc 3, with 90% lymphocytes. Protein 0, 85 g/l Glucose normal India Ink stain is positive for many Cryptococcus yeast forms. 22
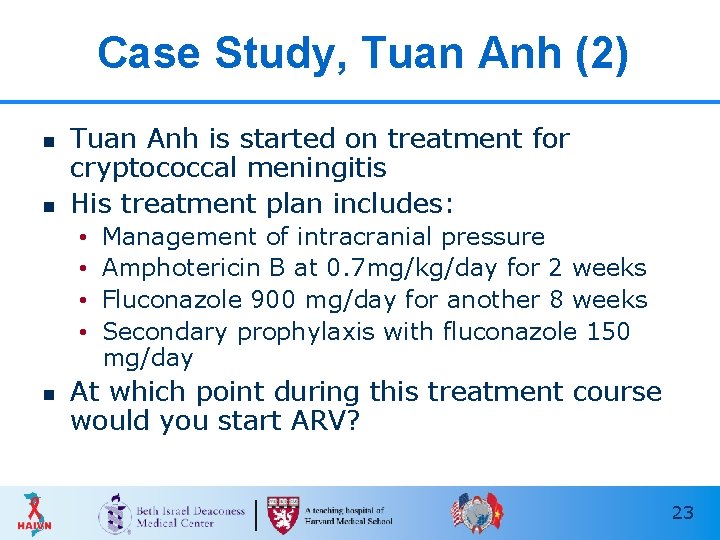
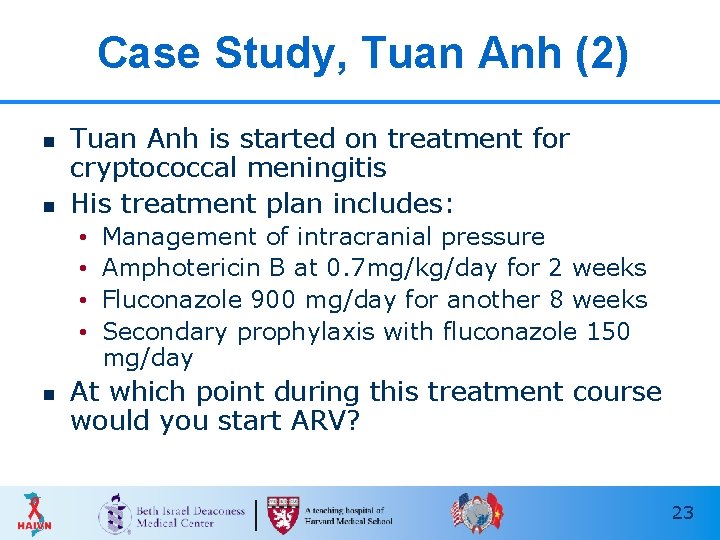
Case Study, Tuan Anh (2) n n Tuan Anh is started on treatment for cryptococcal meningitis His treatment plan includes: • • n Management of intracranial pressure Amphotericin B at 0. 7 mg/kg/day for 2 weeks Fluconazole 900 mg/day for another 8 weeks Secondary prophylaxis with fluconazole 150 mg/day At which point during this treatment course would you start ARV? 23
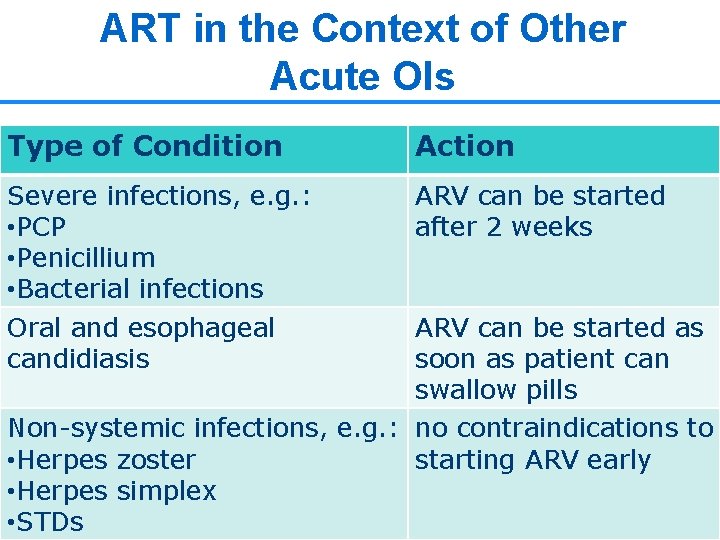
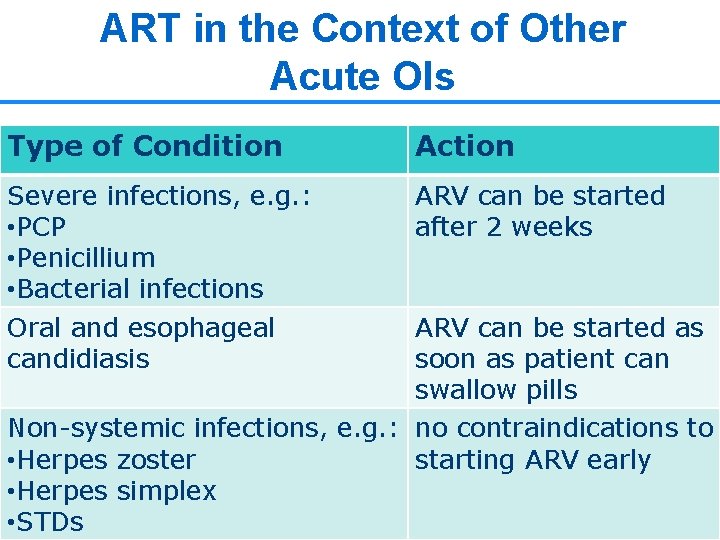
ART in the Context of Other Acute OIs Type of Condition Action Severe infections, e. g. : • PCP • Penicillium • Bacterial infections Oral and esophageal candidiasis ARV can be started after 2 weeks ARV can be started as soon as patient can swallow pills Non-systemic infections, e. g. : no contraindications to • Herpes zoster starting ARV early • Herpes simplex 24 • STDs
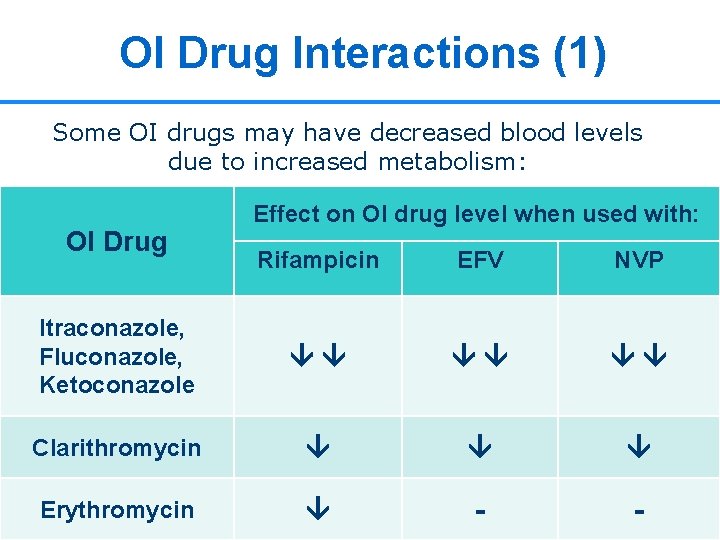
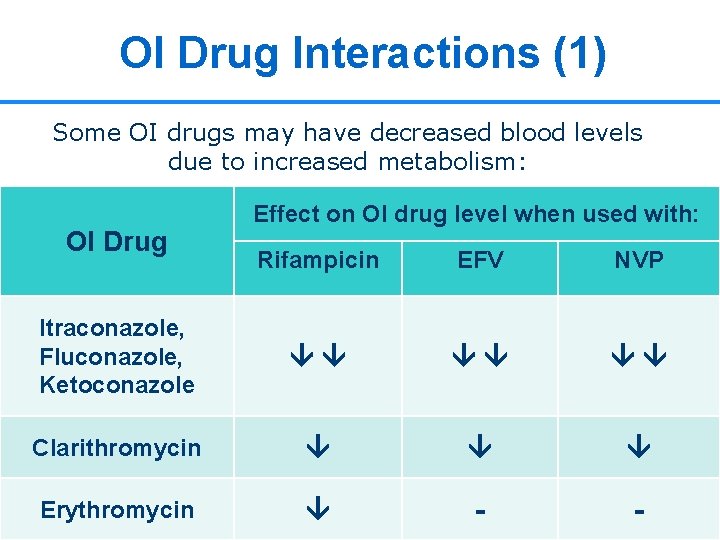
OI Drug Interactions (1) Some OI drugs may have decreased blood levels due to increased metabolism: OI Drug Effect on OI drug level when used with: Rifampicin EFV NVP Itraconazole, Fluconazole, Ketoconazole Clarithromycin Erythromycin - - 25
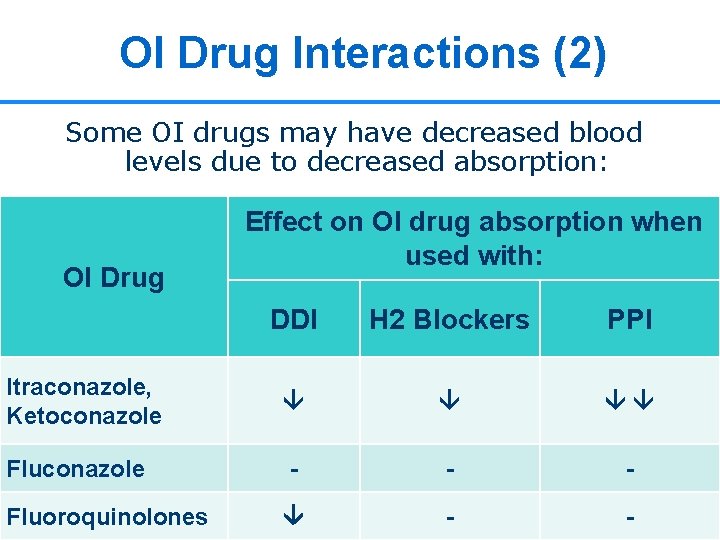
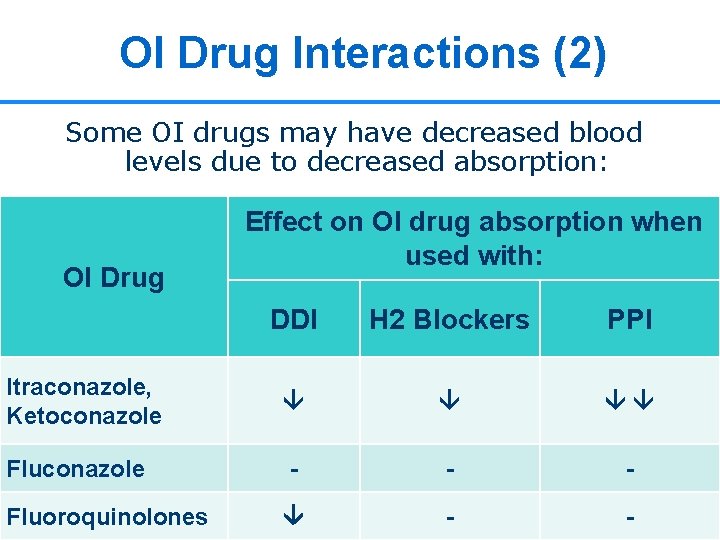
OI Drug Interactions (2) Some OI drugs may have decreased blood levels due to decreased absorption: OI Drug Effect on OI drug absorption when used with: DDI H 2 Blockers PPI Itraconazole, Ketoconazole Fluconazole - - - Fluoroquinolones - - 26
Case Study, Phuong (1) n n n Phuong, a 25 year old woman with HIV comes to the OPC with recurrent fever and skin lesions 2 months ago she was diagnosed with penicilliosis She improved quickly after treatment with Itraconazole 200 mg twice daily 27
Case Study, Phuong (2) n n n Now, however, symptoms have returned 4 weeks ago she started on ART (D 4 T, 3 TC, NVP) 2 weeks ago she decreased her Itraconazole dose to 200 mg daily for maintenance therapy What are possible explanations for Phuong’s recurrent penicilliosis symptoms? How might you manage this situation? 28
Key Points n n n For patient with an acute OI, start ART when patient is clinically stable and tolerating OI treatment Patients with more advanced immunosuppression (CD 4<250) should be started on ART as soon as possible (between 2 -8 weeks) Clinicians should be aware of potential interactions between OI drugs and ARV 29
Thank You Questions?
 Opportunistic infections
Opportunistic infections Opportunistic infections
Opportunistic infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Opportunistic approach adalah model proses
Opportunistic approach adalah model proses Designing language curriculum
Designing language curriculum Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Johnson and johnson botnet infections
Johnson and johnson botnet infections Storch infections
Storch infections Storch infections
Storch infections Bone and joint infections
Bone and joint infections Infections opportunistes digestives
Infections opportunistes digestives Bacterial vaginosis
Bacterial vaginosis Postpartum infections
Postpartum infections Genital infections
Genital infections Genital infections
Genital infections Cell lysis complement system
Cell lysis complement system Acute gingival infections
Acute gingival infections High context vs low context culture ppt
High context vs low context culture ppt Communicating across generational differences
Communicating across generational differences Linguistic context examples
Linguistic context examples Soal essay komunikasi nonverbal
Soal essay komunikasi nonverbal Context of art
Context of art Context of art
Context of art Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Hát lên người ơi
Hát lên người ơi