Opportunistic Infections Associated with HIV Neelay Kothari MD

























- Slides: 71
Opportunistic Infections Associated with HIV Neelay Kothari, MD September 11 th , 2017
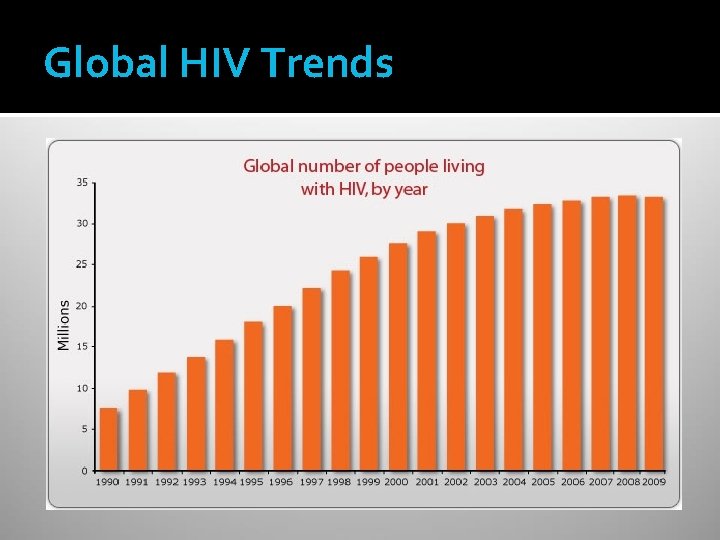
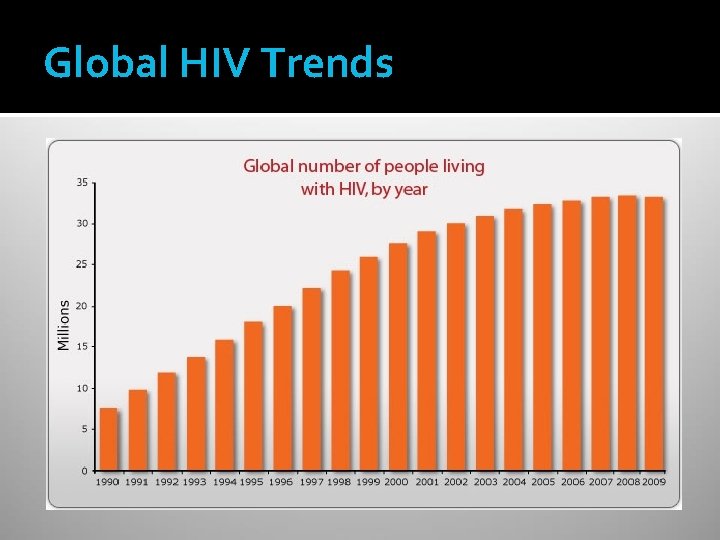
Global HIV Trends

HIV Epidemiology – United States Estimated 1. 1 million people living with HIV (2014) 15% believed to be unaware of their infection Males 75%, Females 25% Rates of infection 8 x higher amongst blacks than whites
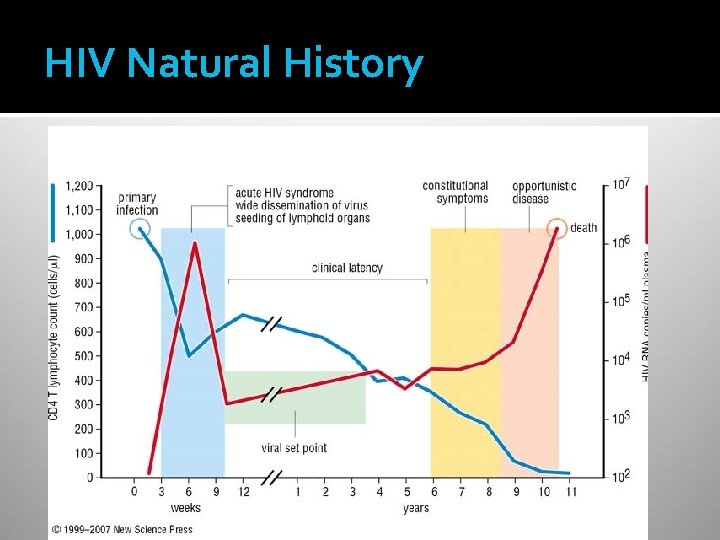
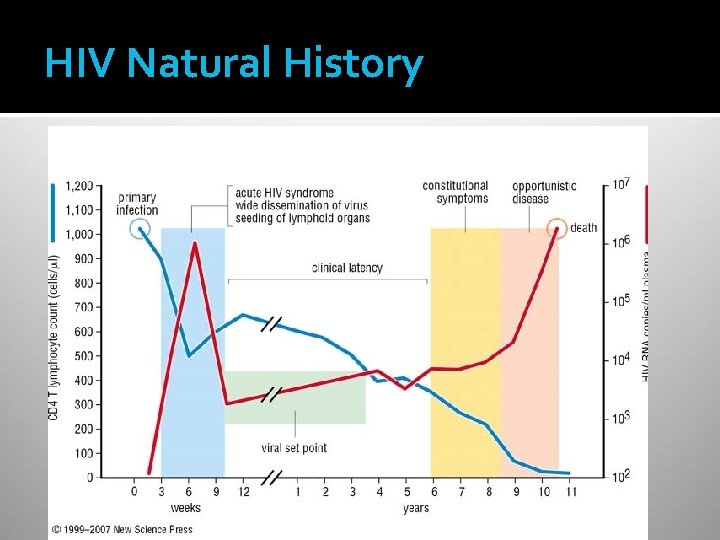
HIV Natural History
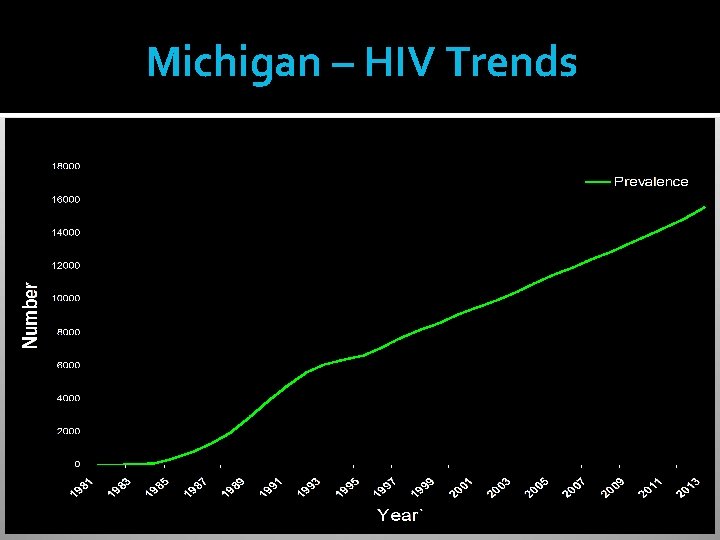
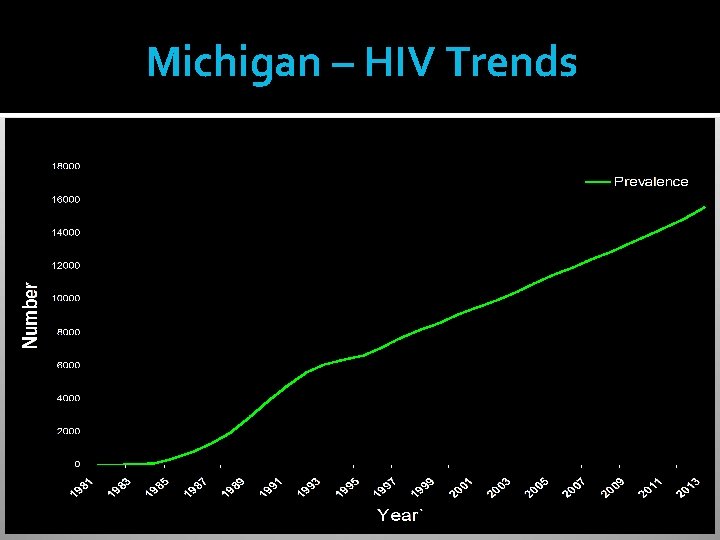
Michigan – HIV Trends

Question AIDS causes defects primarily in which component of the immune system? Granulocytes Cell-mediated Immunity Humoral Immunity Macrophage activation Mucosal protection
Question AIDS causes defects primarily in which component of the immune system? Granulocytes Cell-mediated Immunity Humoral Immunity Macrophage activation Mucosal protection
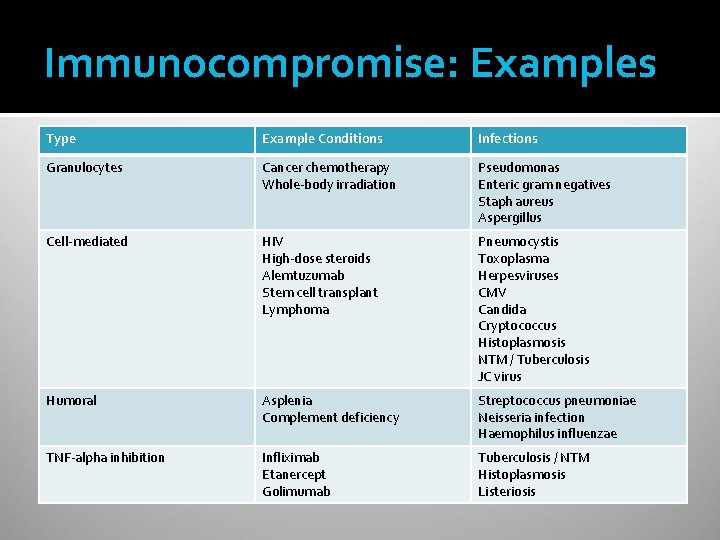
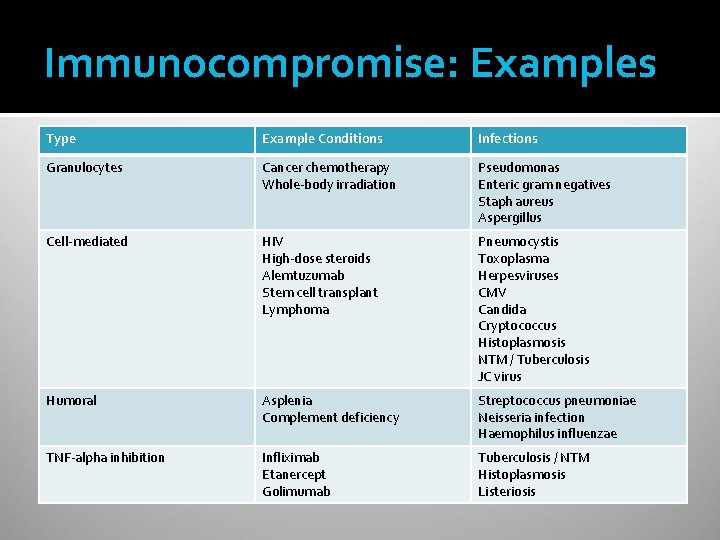
Immunocompromise: Examples Type Example Conditions Infections Granulocytes Cancer chemotherapy Whole-body irradiation Pseudomonas Enteric gram negatives Staph aureus Aspergillus Cell-mediated HIV High-dose steroids Alemtuzumab Stem cell transplant Lymphoma Pneumocystis Toxoplasma Herpesviruses CMV Candida Cryptococcus Histoplasmosis NTM / Tuberculosis JC virus Humoral Asplenia Complement deficiency Streptococcus pneumoniae Neisseria infection Haemophilus influenzae TNF-alpha inhibition Infliximab Etanercept Golimumab Tuberculosis / NTM Histoplasmosis Listeriosis

OI approach in HIV Reactivation of old infections Herpesviruses / CMV Tuberculosis Increased risk of exposure Hepatitis B and C STDs Increased risk of disease Pneumocystis JC virus

Case Presentation #1 34 year old Somali female with negative PMH Two month history of progressive dyspnea, dry cough, headache, loss of appetite Acutely worse over the past 3 days Exam (pertinent positives) Febrile to 102. 9 degrees Dyspneic and tachypneic Scattered crackles on lung exam

Case Presentation #1 There is a very extensive diffuse hazy ground-glass opacity in virtually all the lungs, more severely involving the dependent portion of the lower lung fields, atelectases, as well as mild air bronchogram
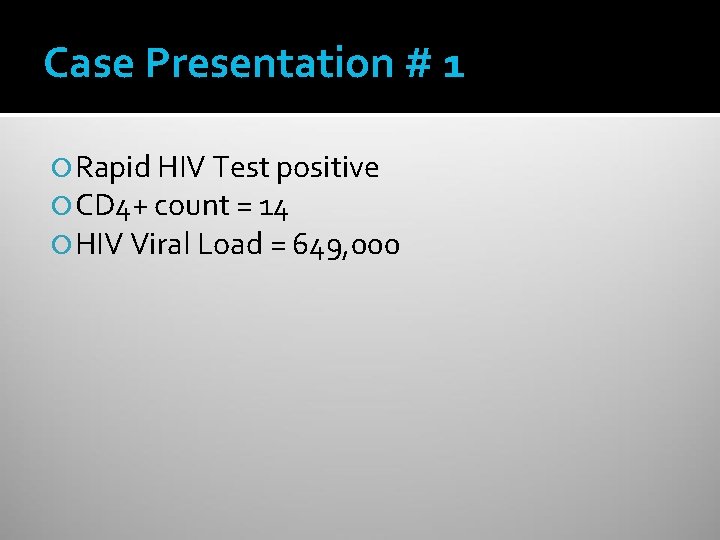
Case Presentation # 1 Rapid HIV Test positive CD 4+ count = 14 HIV Viral Load = 649, 000

Case # 1: Differential Diagnosis Which of the following is most likely? (A) Pulmonary tuberculosis (B) Pulmonary MAI infection (C) Pneumocystis infection (D) Toxoplasmosis pneumonia (E) Cryptococcal pneumonia
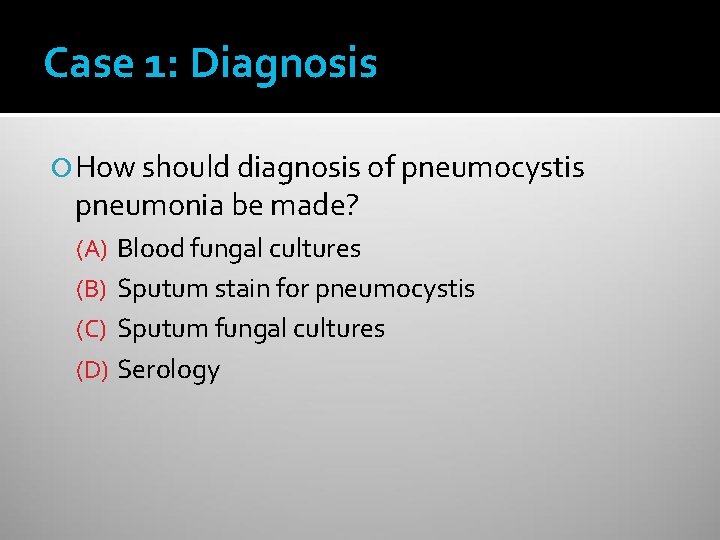
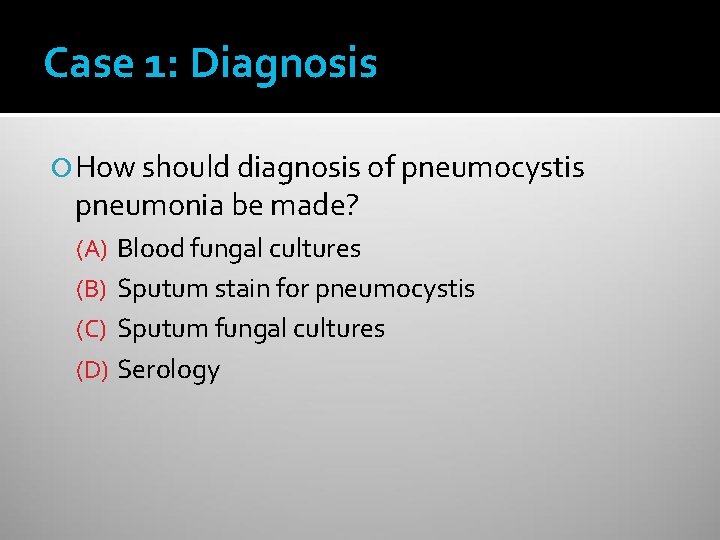
Case 1: Diagnosis How should diagnosis of pneumocystis pneumonia be made? (A) Blood fungal cultures (B) Sputum stain for pneumocystis (C) Sputum fungal cultures (D) Serology

Case Presentation #1 Sputum stain positive for pneumocystis organisms

PNEUMOCYSTIS JIROVECI (CARINII) PNEUMONIA CD 4 < 200 in 90%; Mean CD 4 = 79 Before HAART: 70 -80% got PCP without prophylaxis (mortality 20 -40%) Incidence markedly down with HAART Risk of relapse 65 % w/o secondary prophylaxis
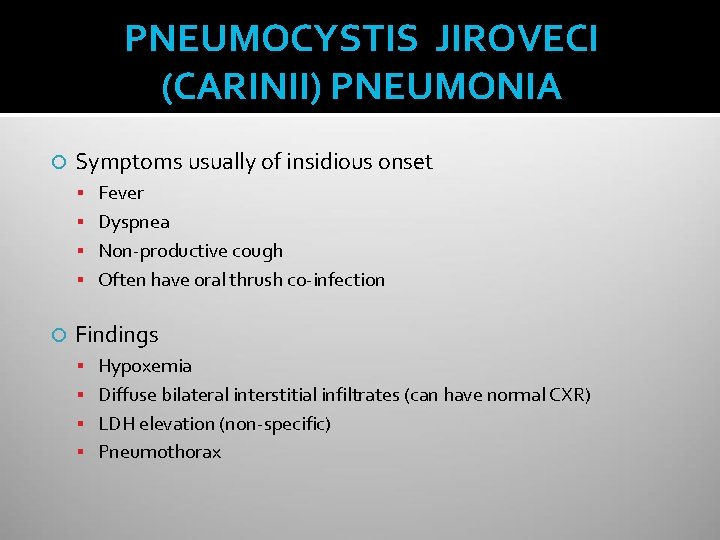
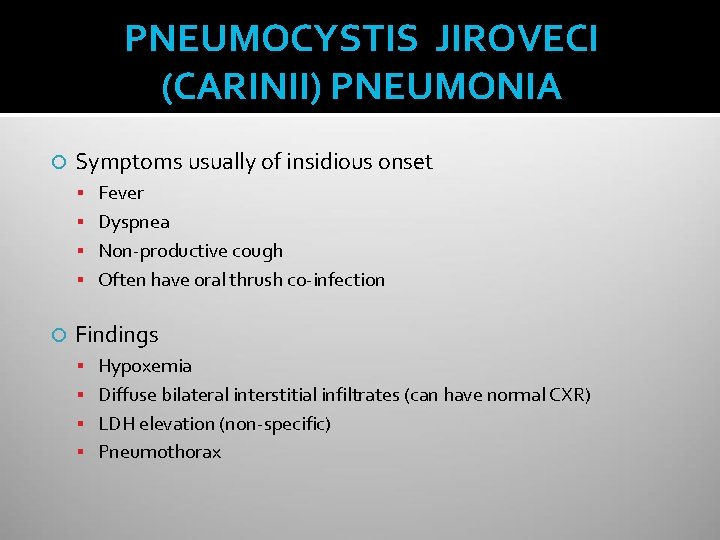
PNEUMOCYSTIS JIROVECI (CARINII) PNEUMONIA Symptoms usually of insidious onset Fever Dyspnea Non-productive cough Often have oral thrush co-infection Findings Hypoxemia Diffuse bilateral interstitial infiltrates (can have normal CXR) LDH elevation (non-specific) Pneumothorax
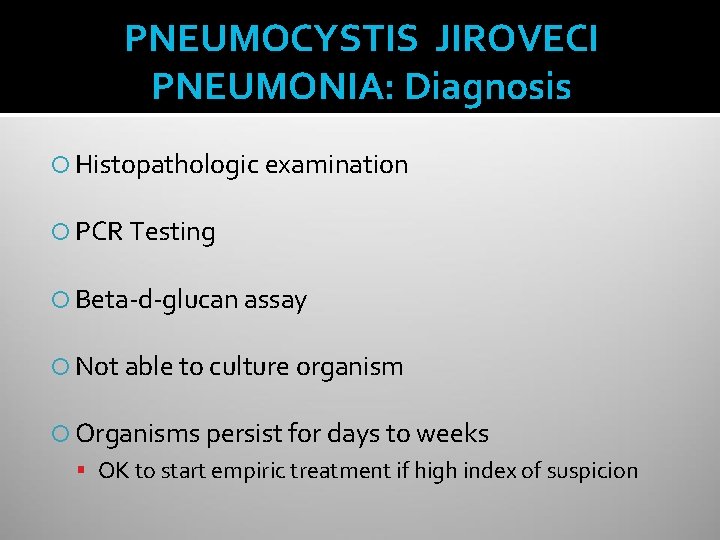
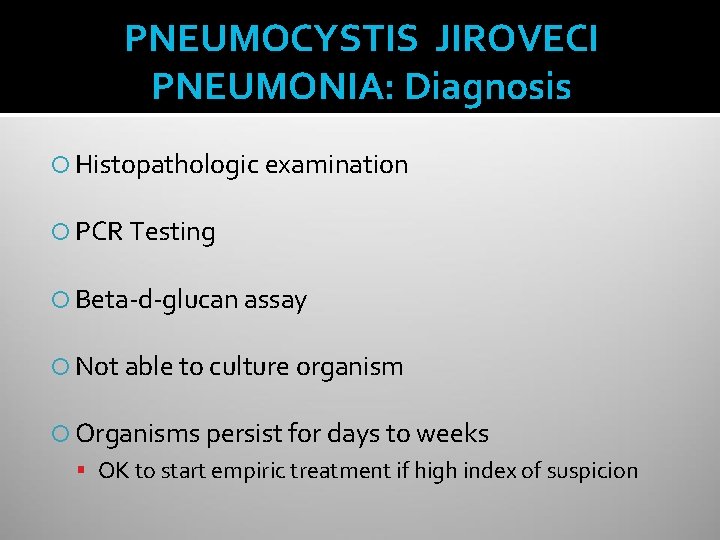
PNEUMOCYSTIS JIROVECI PNEUMONIA: Diagnosis Histopathologic examination PCR Testing Beta-d-glucan assay Not able to culture organism Organisms persist for days to weeks OK to start empiric treatment if high index of suspicion
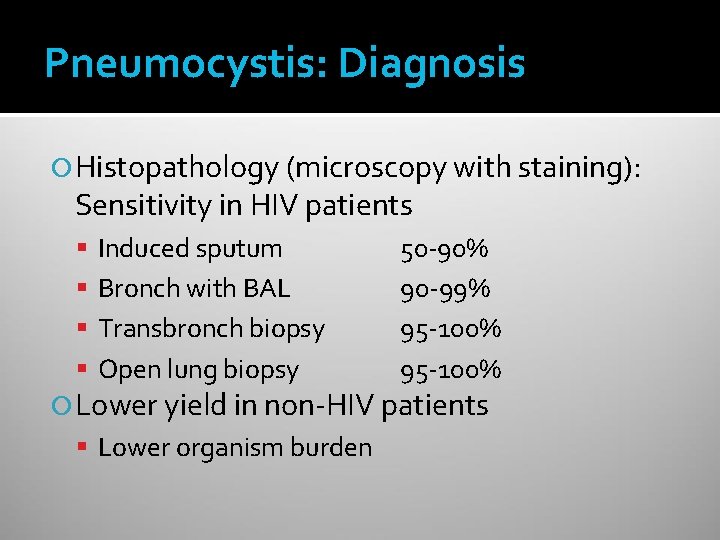
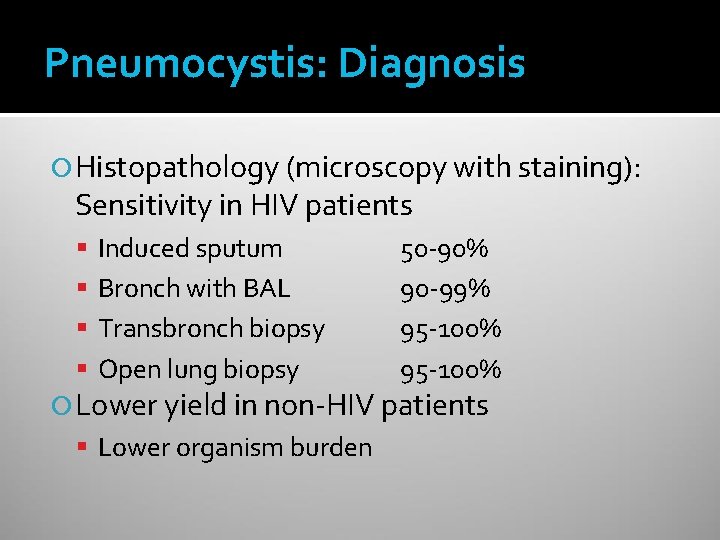
Pneumocystis: Diagnosis Histopathology (microscopy with staining): Sensitivity in HIV patients Induced sputum Bronch with BAL Transbronch biopsy Open lung biopsy 50 -90% 90 -99% 95 -100% Lower yield in non-HIV patients Lower organism burden

Pneumocystis: Diagnosis PCR testing Increased diagnostic yield, especially in non-HIV patients Beta-d-glucan in serum Up to 92% sensitivity Not specific for pneumocystis
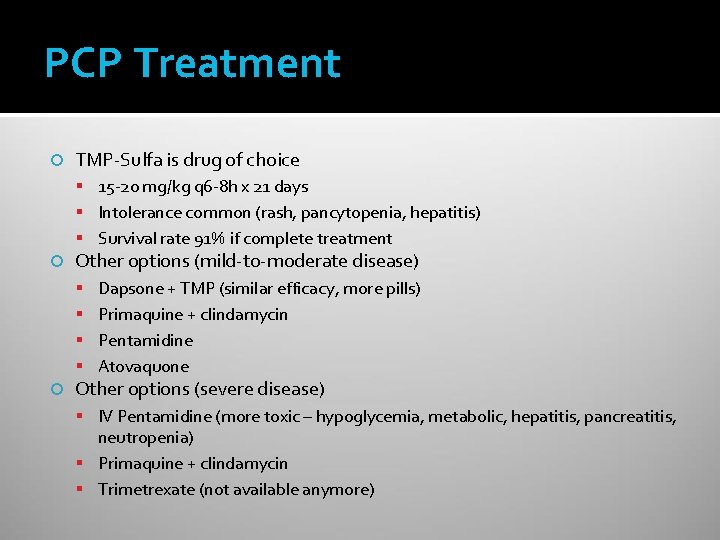
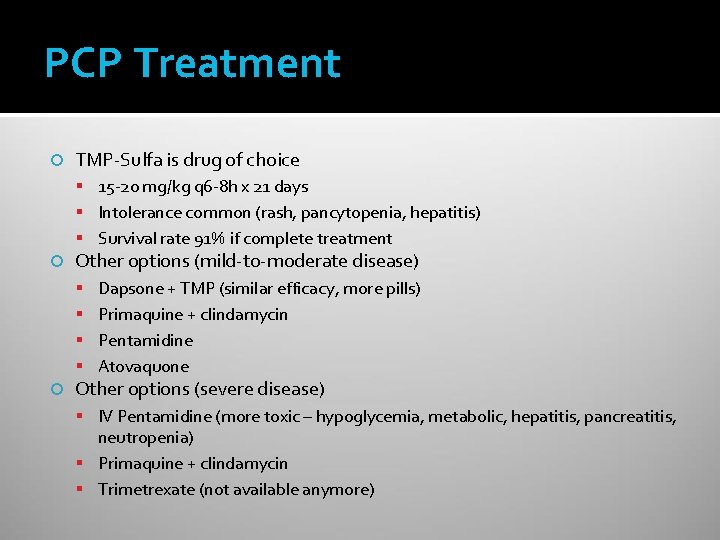
PCP Treatment TMP-Sulfa is drug of choice 15 -20 mg/kg q 6 -8 h x 21 days Intolerance common (rash, pancytopenia, hepatitis) Survival rate 91% if complete treatment Other options (mild-to-moderate disease) Dapsone + TMP (similar efficacy, more pills) Primaquine + clindamycin Pentamidine Atovaquone Other options (severe disease) IV Pentamidine (more toxic – hypoglycemia, metabolic, hepatitis, pancreatitis, neutropenia) Primaquine + clindamycin Trimetrexate (not available anymore)
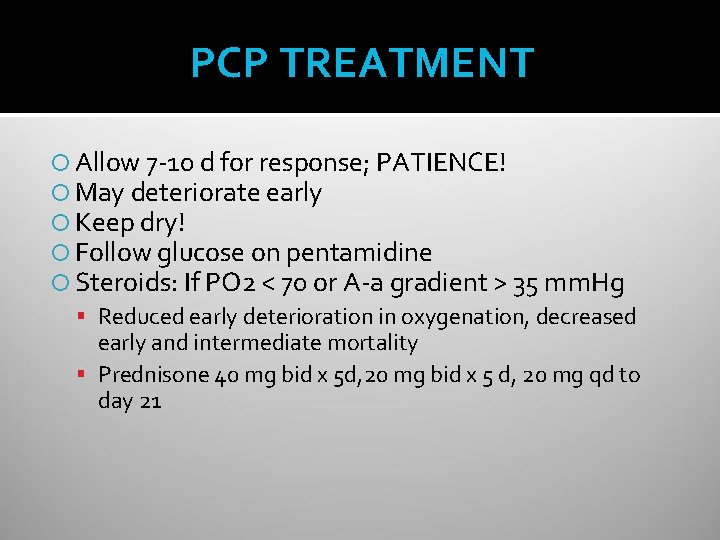
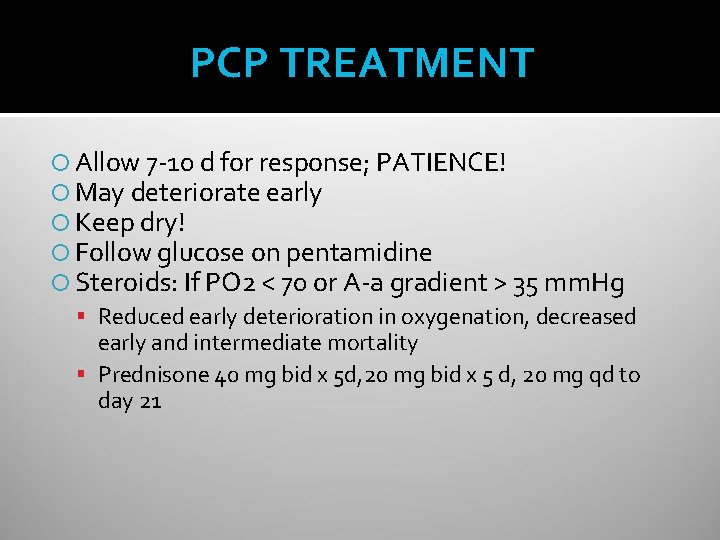
PCP TREATMENT Allow 7 -10 d for response; PATIENCE! May deteriorate early Keep dry! Follow glucose on pentamidine Steroids: If PO 2 < 70 or A-a gradient > 35 mm. Hg Reduced early deterioration in oxygenation, decreased early and intermediate mortality Prednisone 40 mg bid x 5 d, 20 mg bid x 5 d, 20 mg qd to day 21

PCP PROPHYLAXIS Indications for primary prophylaxis CD 4 < 200 (consider if 200 -250 and dropping fast) Oropharyngeal candidiasis CD 4 percentage < 14% AIDS-defining illness without ART / viral suppression Secondary prophylaxis History of pneumocystis Start immediately after completion of treatment regimen Discontinuation Once CD 4 > 200 for at least 3 months CD 4 100 -200 with consistent viral suppression for 3 -6 months
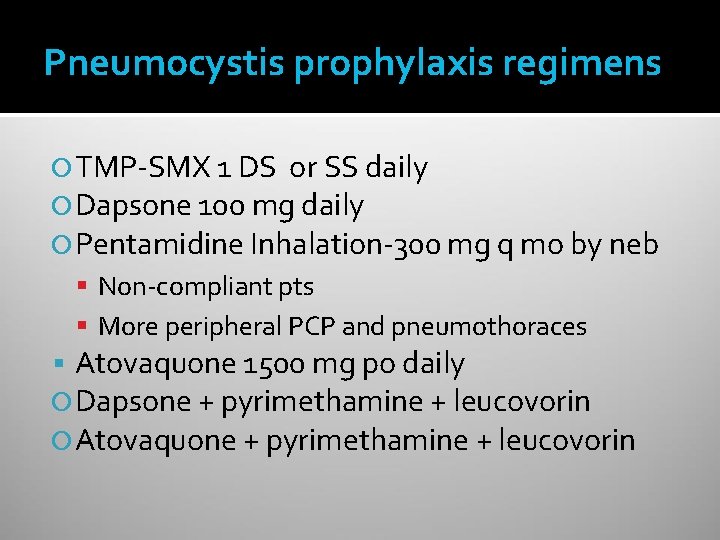
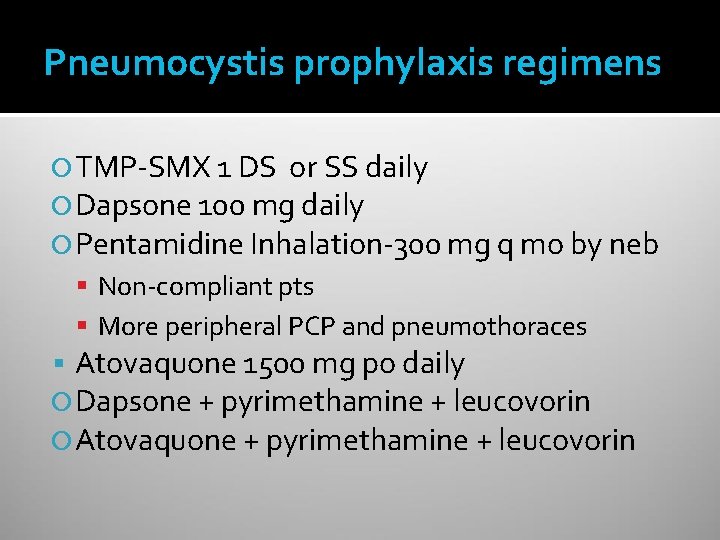
Pneumocystis prophylaxis regimens TMP-SMX 1 DS or SS daily Dapsone 100 mg daily Pentamidine Inhalation-300 mg q mo by neb Non-compliant pts More peripheral PCP and pneumothoraces Atovaquone 1500 mg po daily Dapsone + pyrimethamine + leucovorin Atovaquone + pyrimethamine + leucovorin
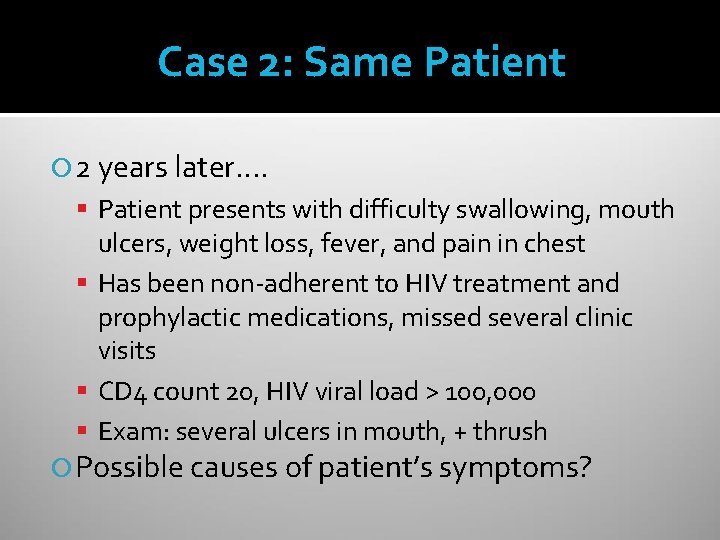
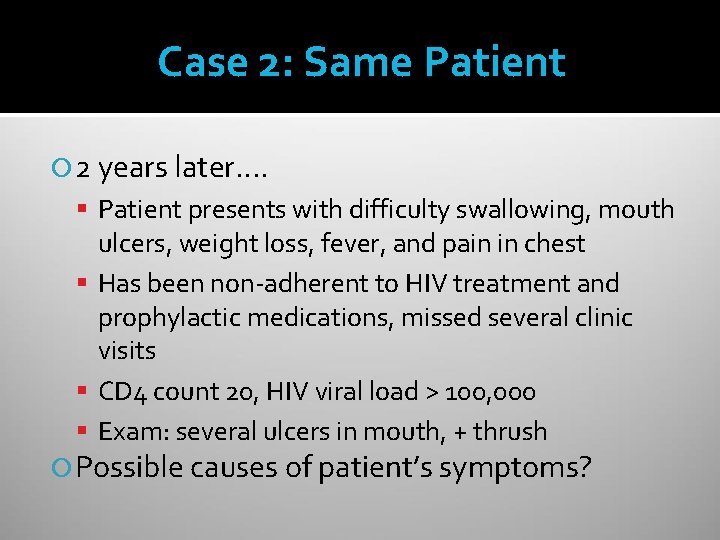
Case 2: Same Patient 2 years later…. Patient presents with difficulty swallowing, mouth ulcers, weight loss, fever, and pain in chest Has been non-adherent to HIV treatment and prophylactic medications, missed several clinic visits CD 4 count 20, HIV viral load > 100, 000 Exam: several ulcers in mouth, + thrush Possible causes of patient’s symptoms?
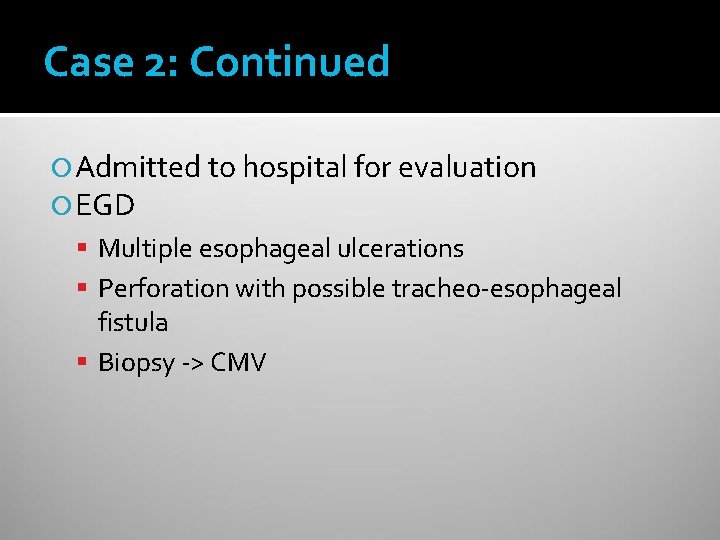
Case 2: Continued Admitted to hospital for evaluation EGD Multiple esophageal ulcerations Perforation with possible tracheo-esophageal fistula Biopsy -> CMV

CMV Typically causes disease with CD 4 < 50 Chorioretinitis 30% incidence in AIDS patients (before HAART) Initially unilateral – will spread to other eye Floaters, visual loss, decreased acuity Diagnosis: clinical ophthalmology evaluation Treatment: systemic and local (val)ganciclovir Esophagitis / colitis Fever, weight loss, diarrhea, odynophagia Can have hemorrhage / perforation rarely Neurologic disease: dementia, ventriculoencephalitis, ascending polyradiculomyelopathy Pulmonary disease: significance often unclear
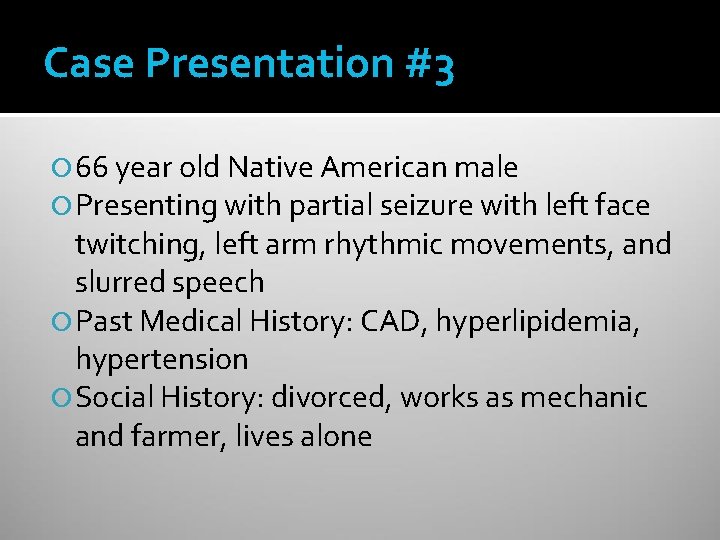
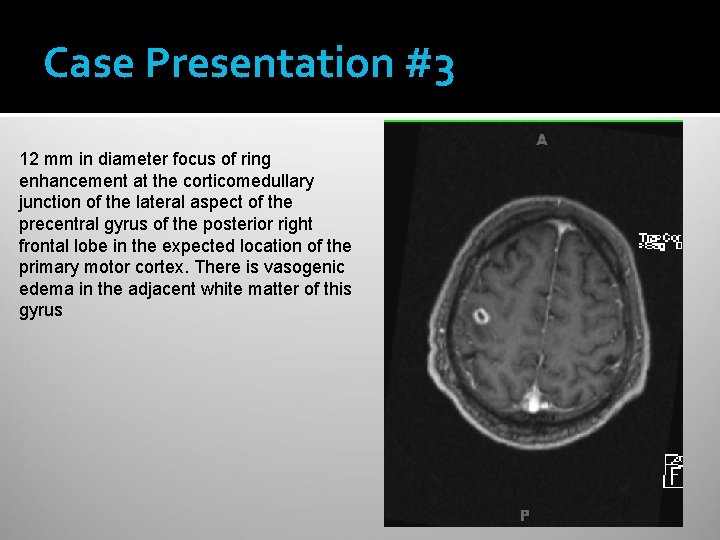
Case Presentation #3 66 year old Native American male Presenting with partial seizure with left face twitching, left arm rhythmic movements, and slurred speech Past Medical History: CAD, hyperlipidemia, hypertension Social History: divorced, works as mechanic and farmer, lives alone
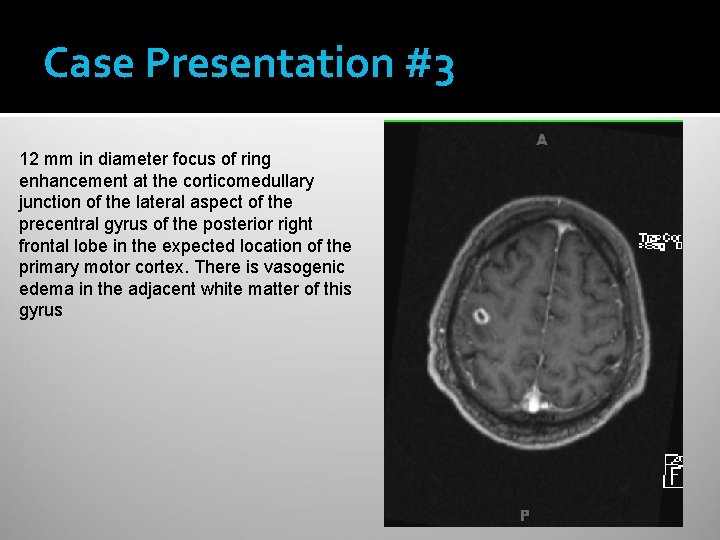
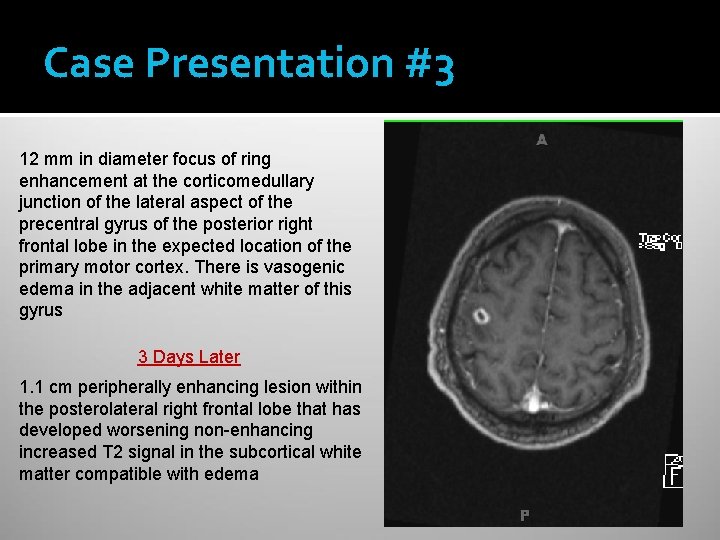
Case Presentation #3 12 mm in diameter focus of ring enhancement at the corticomedullary junction of the lateral aspect of the precentral gyrus of the posterior right frontal lobe in the expected location of the primary motor cortex. There is vasogenic edema in the adjacent white matter of this gyrus
Case 3: Differential Diagnosis? Further workup?
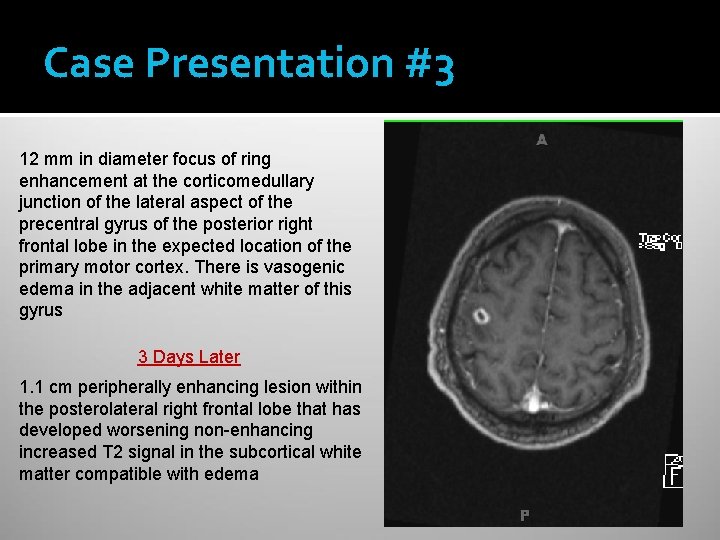
Case Presentation #3 12 mm in diameter focus of ring enhancement at the corticomedullary junction of the lateral aspect of the precentral gyrus of the posterior right frontal lobe in the expected location of the primary motor cortex. There is vasogenic edema in the adjacent white matter of this gyrus 3 Days Later 1. 1 cm peripherally enhancing lesion within the posterolateral right frontal lobe that has developed worsening non-enhancing increased T 2 signal in the subcortical white matter compatible with edema
Case Presentation #3 Laboratory Evaluation HIV antibody POSITIVE CD 4 count = 32 HIV viral load = 315, 000 Toxoplasma Ig. G POSITIVE

TOXOPLASMOSIS EPIDEMIOLOGY Variable seroprevalence CLINICAL Disease risk 11% in United States CD 4 count usually < 50 50 -75% in parts of Europe 33% will get disease without Transmission Undercooked meat with tissue cysts Oocysts in cat feces (sporulation requires 24 hours) Not person-to-person prophylaxis Symptoms Focal encephalitis Headache, confusion, focal motor weakness Fever Seizures Extra. CNS disease rare

TOXOPLASMOSIS-DIAGNOSIS Clinical presentation Serology 95 % sensitive CT or MRI-Multiple, bilateral, hypodense, ring -enhancing mass lesions with predilection for B. G. and corticomedullary junction Commonest cause of focal brain lesion in AIDS Reduced in HAART Era Clinical and radiographic response to Rx Usually better in 2 wks
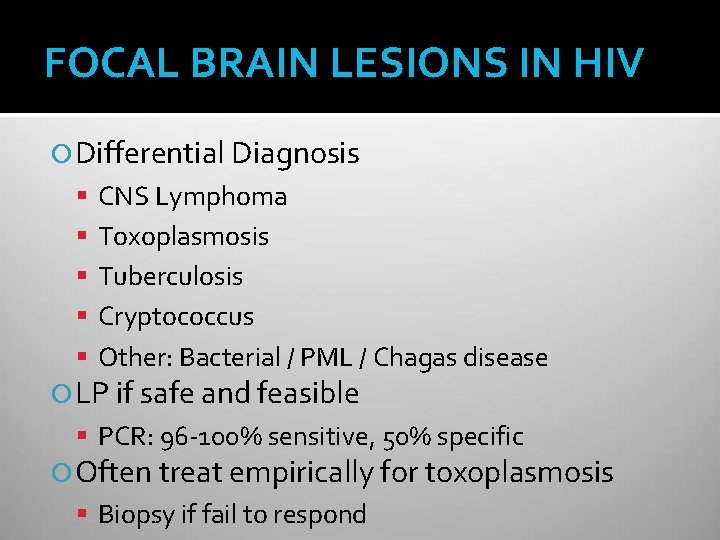
FOCAL BRAIN LESIONS IN HIV Differential Diagnosis CNS Lymphoma Toxoplasmosis Tuberculosis Cryptococcus Other: Bacterial / PML / Chagas disease LP if safe and feasible PCR: 96 -100% sensitive, 50% specific Often treat empirically for toxoplasmosis Biopsy if fail to respond
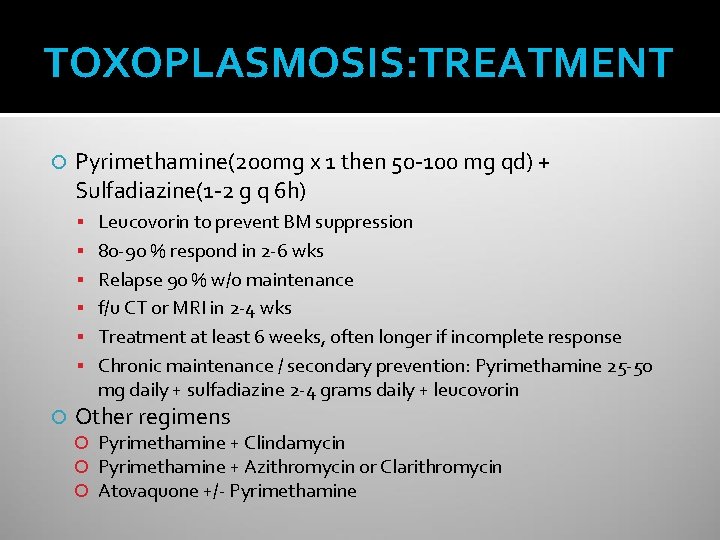
TOXOPLASMOSIS: TREATMENT Pyrimethamine(200 mg x 1 then 50 -100 mg qd) + Sulfadiazine(1 -2 g q 6 h) Leucovorin to prevent BM suppression 80 -90 % respond in 2 -6 wks Relapse 90 % w/o maintenance f/u CT or MRI in 2 -4 wks Treatment at least 6 weeks, often longer if incomplete response Chronic maintenance / secondary prevention: Pyrimethamine 25 -50 mg daily + sulfadiazine 2 -4 grams daily + leucovorin Other regimens Pyrimethamine + Clindamycin Pyrimethamine + Azithromycin or Clarithromycin Atovaquone +/- Pyrimethamine
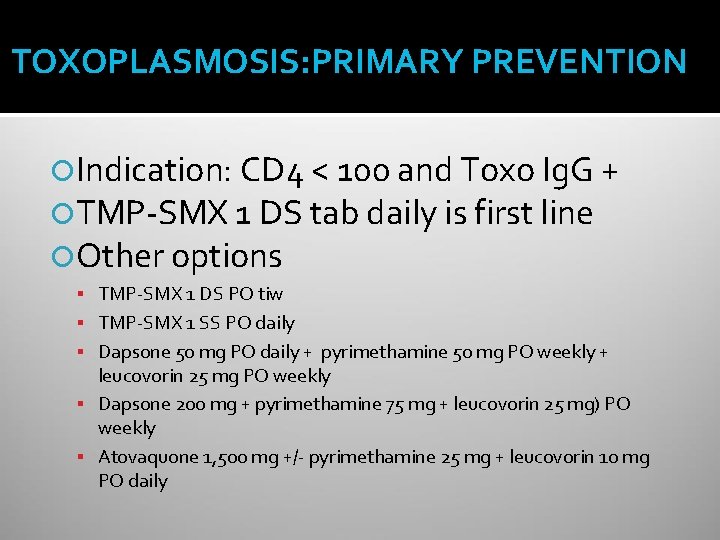
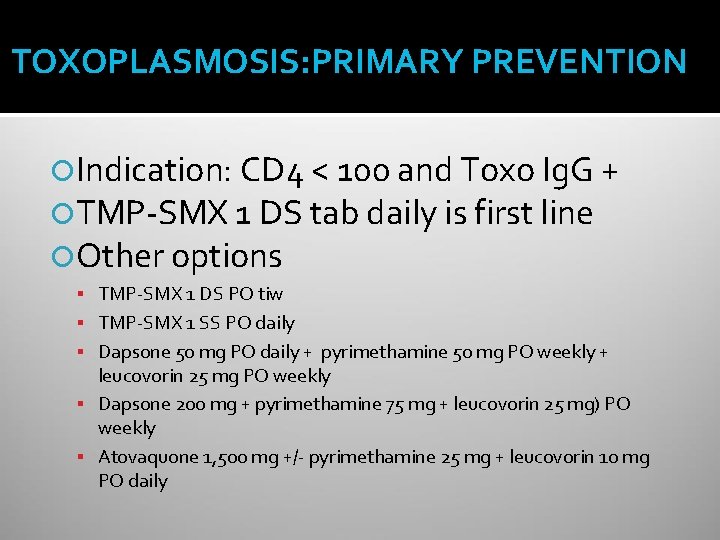
TOXOPLASMOSIS: PRIMARY PREVENTION Indication: CD 4 < 100 and Toxo Ig. G + TMP-SMX 1 DS tab daily is first line Other options TMP-SMX 1 DS PO tiw TMP-SMX 1 SS PO daily Dapsone 50 mg PO daily + pyrimethamine 50 mg PO weekly + leucovorin 25 mg PO weekly Dapsone 200 mg + pyrimethamine 75 mg + leucovorin 25 mg) PO weekly Atovaquone 1, 500 mg +/- pyrimethamine 25 mg + leucovorin 10 mg PO daily
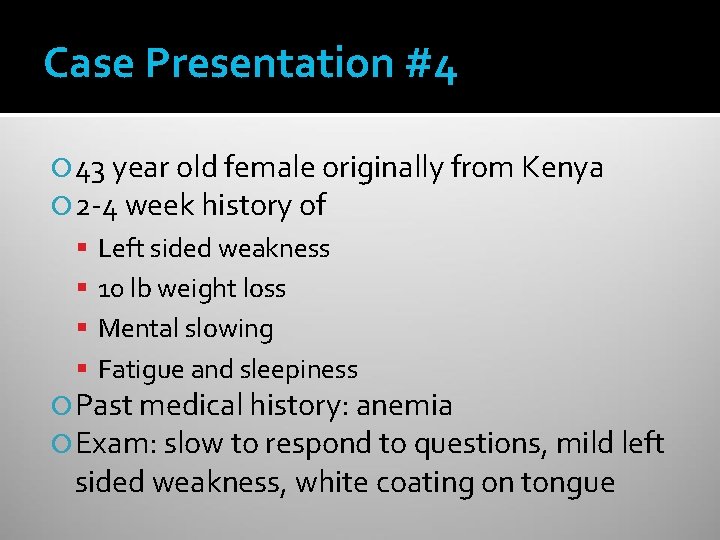
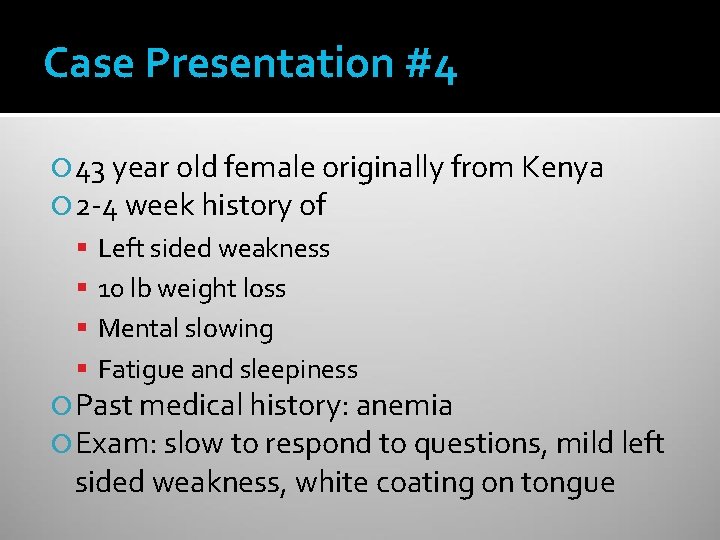
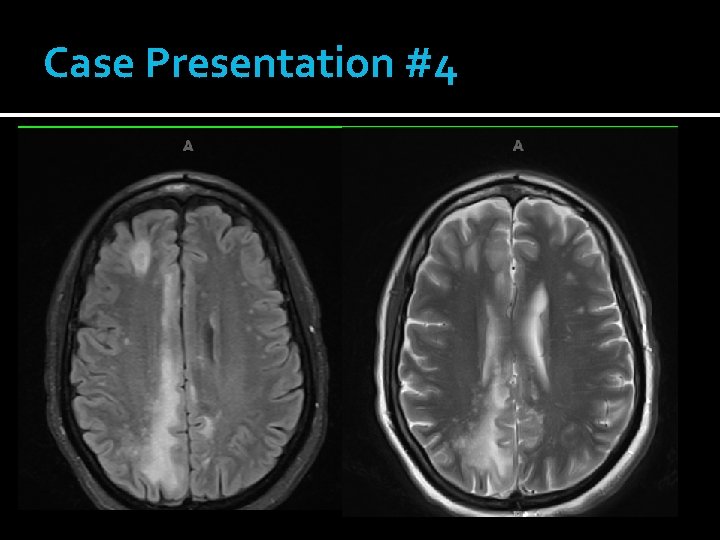
Case Presentation #4 43 year old female originally from Kenya 2 -4 week history of Left sided weakness 10 lb weight loss Mental slowing Fatigue and sleepiness Past medical history: anemia Exam: slow to respond to questions, mild left sided weakness, white coating on tongue
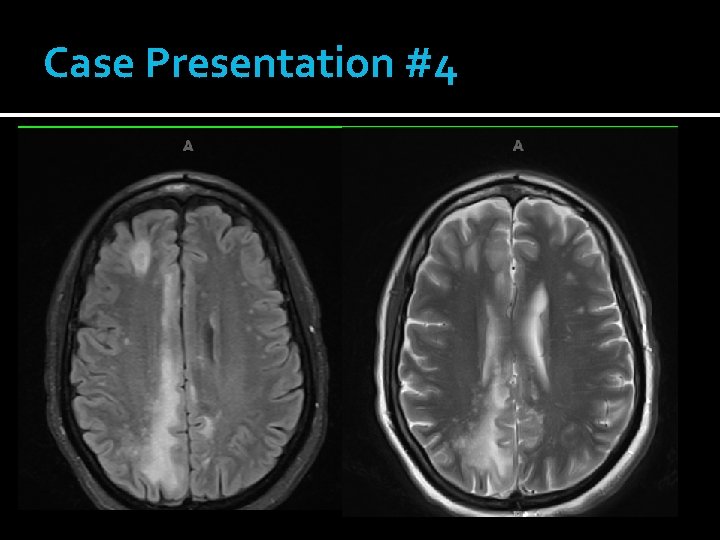
Case Presentation #4
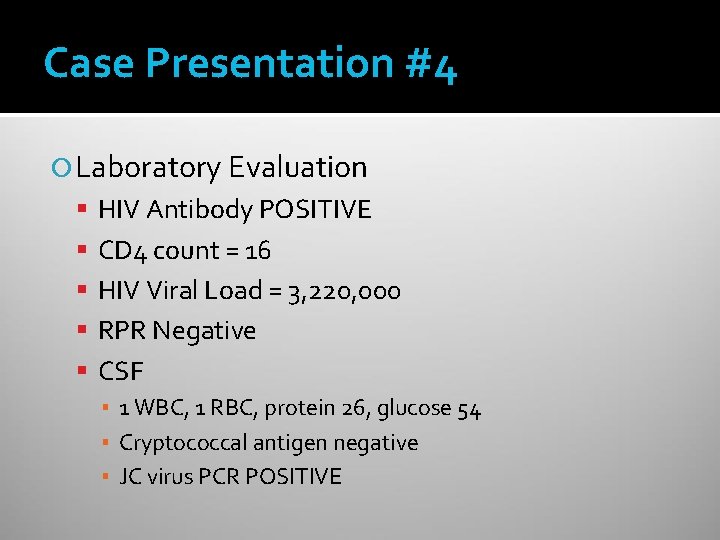
Case Presentation #4 Laboratory Evaluation HIV Antibody POSITIVE CD 4 count = 16 HIV Viral Load = 3, 220, 000 RPR Negative CSF ▪ 1 WBC, 1 RBC, protein 26, glucose 54 ▪ Cryptococcal antigen negative ▪ JC virus PCR POSITIVE
Case # 4: Clinical Course Patient was started on HIV treatment Unfortunately her mental status continued to deteriorate Transitioned to comfort care and died
PROGRESSIVE MULTIFOCAL LEUKOENCEPHALOPATHY JC Virus – 85% of population seropositive CD 4+ count usually < 100 Clinical Presentation Demyelinating lesions Focal neurologic deficits Progressive over weeks to months Seizures in 20% Imaging: Multiple nonenhancing white matter lesions No mass effect CSF analysis: PCR positive in 70 -90% if not on HAART
PROGRESSIVE MULTIFOCAL LEUKOENCEPHALOPATHY Treatment No specific treatment Reverse immunosuppression ▪ Start HAART immediately Prognosis High morbidity and mortality Half get better with HAART, though often have residual deficits Lower CD 4 count at presentation associated with poor outcome

Immune Reconstitution Inflammatory Syndrome (IRIS) Parodoxical clinical worsening after starting HAART despite improved immune function Due to inflammatory response against infectious antigen CD 4 count usually < 50 Usually within 6 weeks, though can be several months Common pathogens: MAC, TB, CMV, cryptococcus, pneumocystis, JC virus Can have atypical presentation Treatment: continue HAART if possible, treat infection, anti-inflammatory therapy
Case Presentation #5 46 year old male previously healthy Chief complaint: headache Present for approximately one month Sudden onset, with gradual worsening since Bilateral, retro-orbital and into top of head Initially seen in Minute Clinic Presumed sinusitis, prescribed amoxicillin Not better, prescribed azithromycin Not better, then prescribed Vicodin 6 days prior to admission
Case Presentation #5 Associated symptoms Nausea and vomiting x 2 weeks 15 pound weight loss Brief 30 -60 second episodes of dizziness Intermittent photophobia Ringing sensation in right ear Feels somewhat depressed Per family Slow mentation and speech Increased sleepiness

Case Presentation #5 Works as nail technician, unable to work recently No tobacco, occasional cigar, occasional alcohol (2 drinks per week), denies other drug use Travel: recent travel to England No pets, animal or tick exposures, sick contacts Enjoys gardening

Case Presentation #5 VS Temp 98. 1, P 75, R 16, BP 131/90 Weight 130 lb General: flat and depressed affect, slow speech HEENT: whitish patches on tongue Skin: 3 -4 mm skin colored papules present on forehead, shoulder, sternum Remainder of exam unremarkable

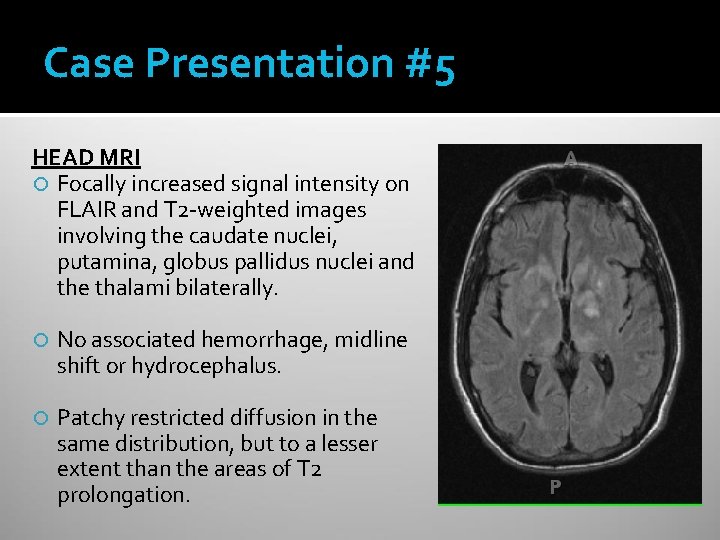
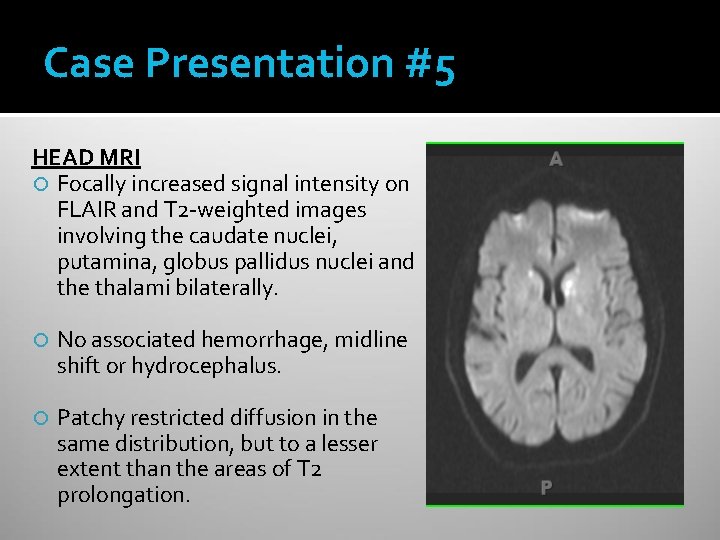
Case Presentation #5 HEAD MRI Focally increased signal intensity on FLAIR and T 2 -weighted images involving the caudate nuclei, putamina, globus pallidus nuclei and the thalami bilaterally. No associated hemorrhage, midline shift or hydrocephalus. Patchy restricted diffusion in the same distribution, but to a lesser extent than the areas of T 2 prolongation.

Case Presentation #5 HEAD MRI Focally increased signal intensity on FLAIR and T 2 -weighted images involving the caudate nuclei, putamina, globus pallidus nuclei and the thalami bilaterally. No associated hemorrhage, midline shift or hydrocephalus. Patchy restricted diffusion in the same distribution, but to a lesser extent than the areas of T 2 prolongation.
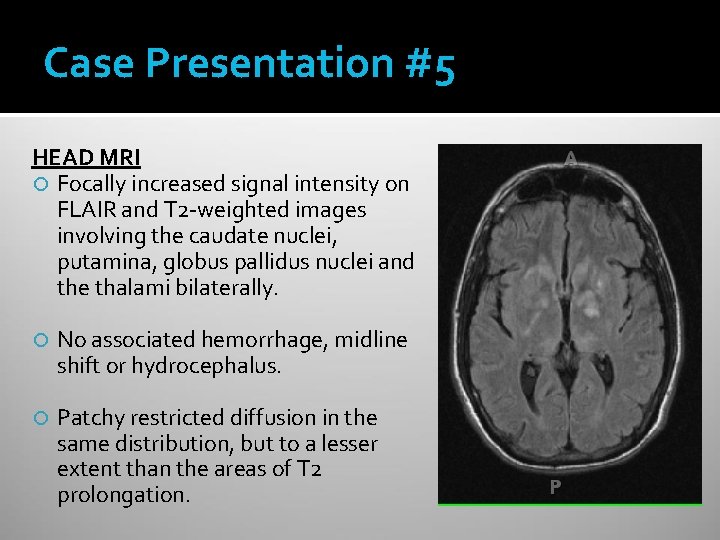
Case Presentation #5 HEAD MRI Focally increased signal intensity on FLAIR and T 2 -weighted images involving the caudate nuclei, putamina, globus pallidus nuclei and the thalami bilaterally. No associated hemorrhage, midline shift or hydrocephalus. Patchy restricted diffusion in the same distribution, but to a lesser extent than the areas of T 2 prolongation.
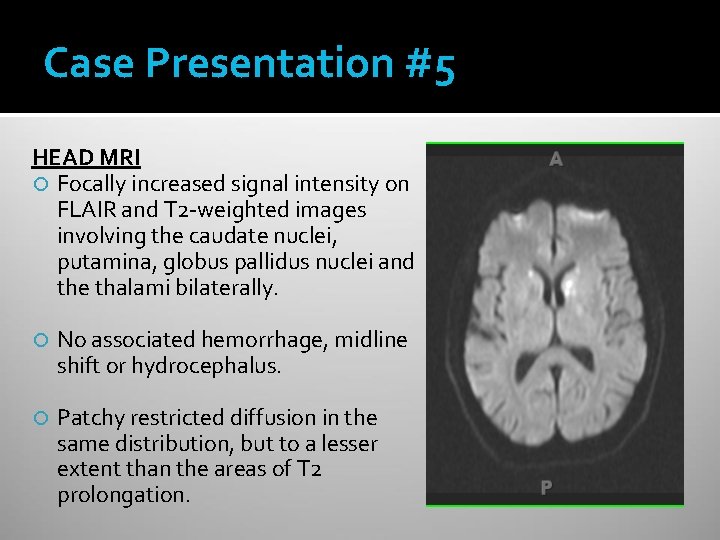
Case Presentation #5 HEAD MRI Focally increased signal intensity on FLAIR and T 2 -weighted images involving the caudate nuclei, putamina, globus pallidus nuclei and the thalami bilaterally. No associated hemorrhage, midline shift or hydrocephalus. Patchy restricted diffusion in the same distribution, but to a lesser extent than the areas of T 2 prolongation.
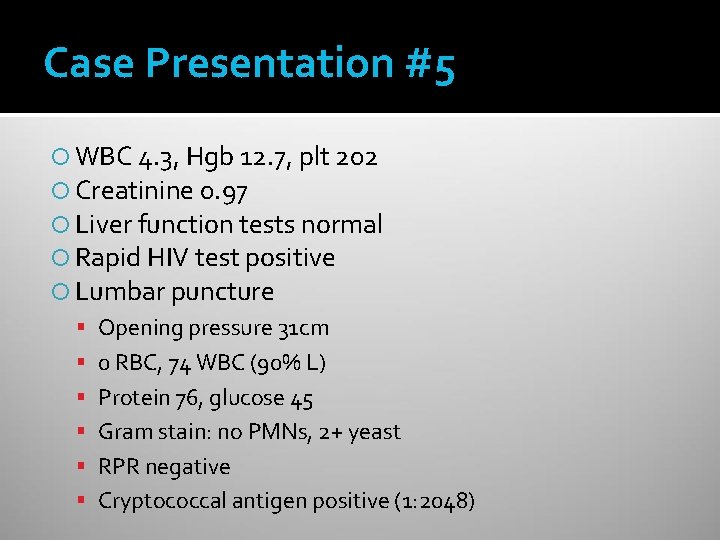
Case Presentation #5 WBC 4. 3, Hgb 12. 7, plt 202 Creatinine 0. 97 Liver function tests normal Rapid HIV test positive Lumbar puncture Opening pressure 31 cm 0 RBC, 74 WBC (90% L) Protein 76, glucose 45 Gram stain: no PMNs, 2+ yeast RPR negative Cryptococcal antigen positive (1: 2048)

Cryptococcus: Clinical Manifestations Can infect any organ Most common sites of infection Lungs: nodules, masslike infiltrate, adenopathy, lung cavitation, lobar infiltrates CNS: subacute meningitis or meningoencephalitis Skin: papules with soft or ulcerated center
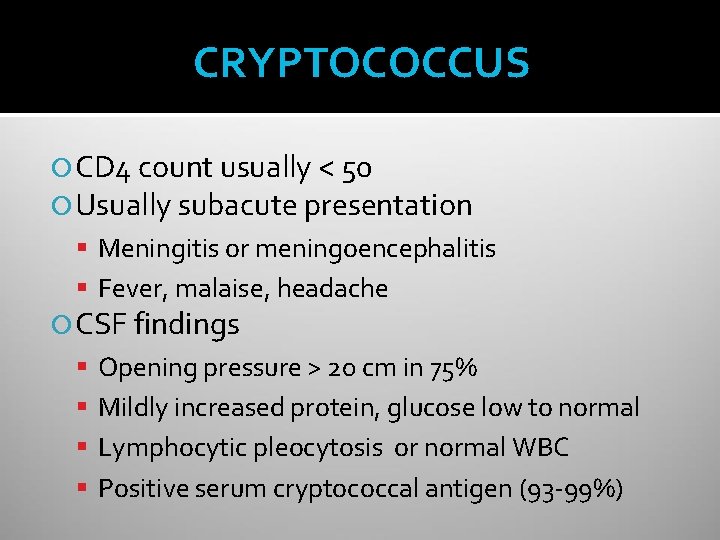
CRYPTOCOCCUS CD 4 count usually < 50 Usually subacute presentation Meningitis or meningoencephalitis Fever, malaise, headache CSF findings Opening pressure > 20 cm in 75% Mildly increased protein, glucose low to normal Lymphocytic pleocytosis or normal WBC Positive serum cryptococcal antigen (93 -99%)
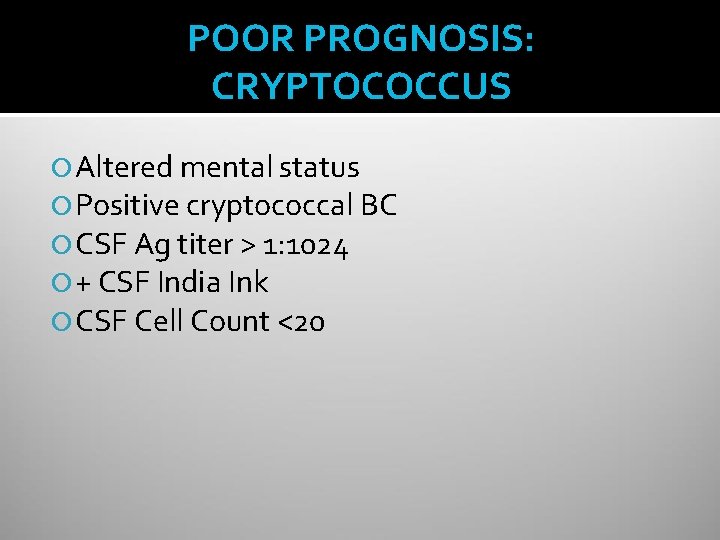
POOR PROGNOSIS: CRYPTOCOCCUS Altered mental status Positive cryptococcal BC CSF Ag titer > 1: 1024 + CSF India Ink CSF Cell Count <20
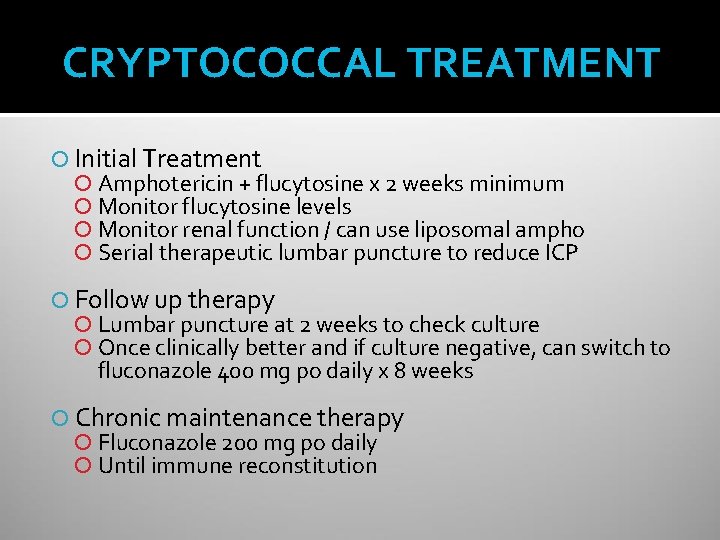
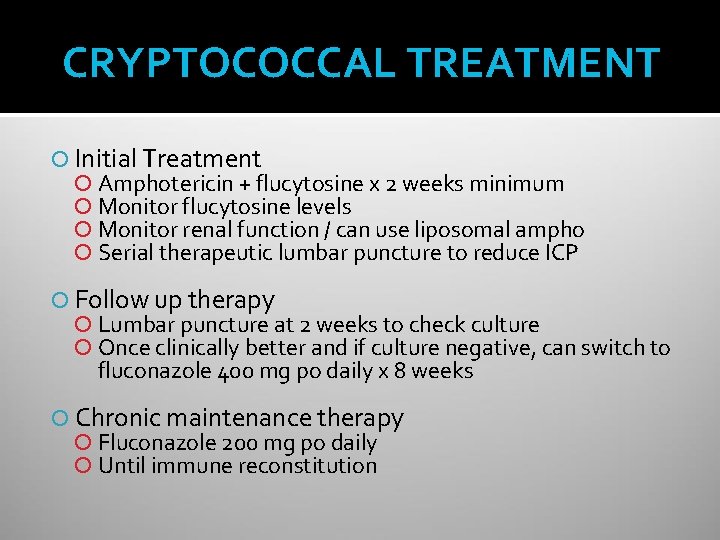
CRYPTOCOCCAL TREATMENT Initial Treatment Amphotericin + flucytosine x 2 weeks minimum Monitor flucytosine levels Monitor renal function / can use liposomal ampho Serial therapeutic lumbar puncture to reduce ICP Follow up therapy Lumbar puncture at 2 weeks to check culture Once clinically better and if culture negative, can switch to fluconazole 400 mg po daily x 8 weeks Chronic maintenance therapy Fluconazole 200 mg po daily Until immune reconstitution
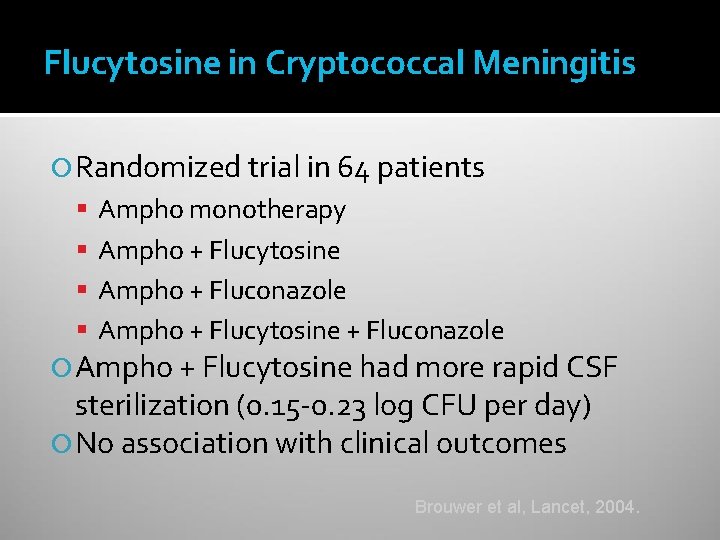
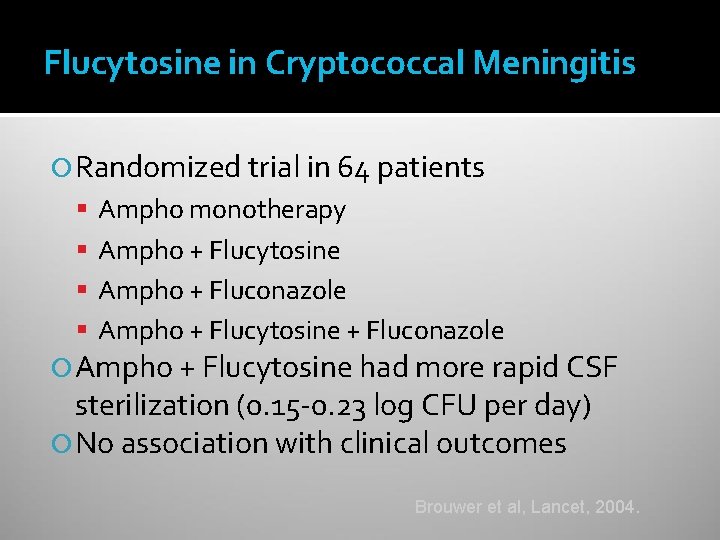
Flucytosine in Cryptococcal Meningitis Randomized trial in 64 patients Ampho monotherapy Ampho + Flucytosine Ampho + Fluconazole Ampho + Flucytosine had more rapid CSF sterilization (0. 15 -0. 23 log CFU per day) No association with clinical outcomes Brouwer et al, Lancet, 2004.
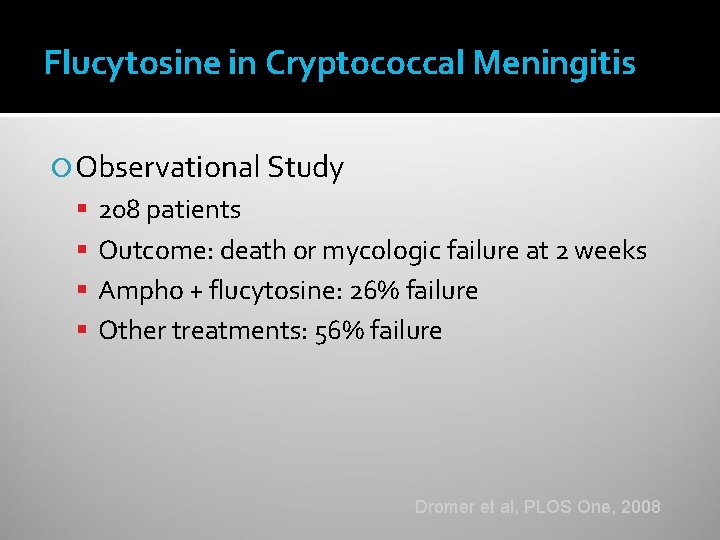
Flucytosine in Cryptococcal Meningitis Observational Study 208 patients Outcome: death or mycologic failure at 2 weeks Ampho + flucytosine: 26% failure Other treatments: 56% failure Dromer et al, PLOS One, 2008
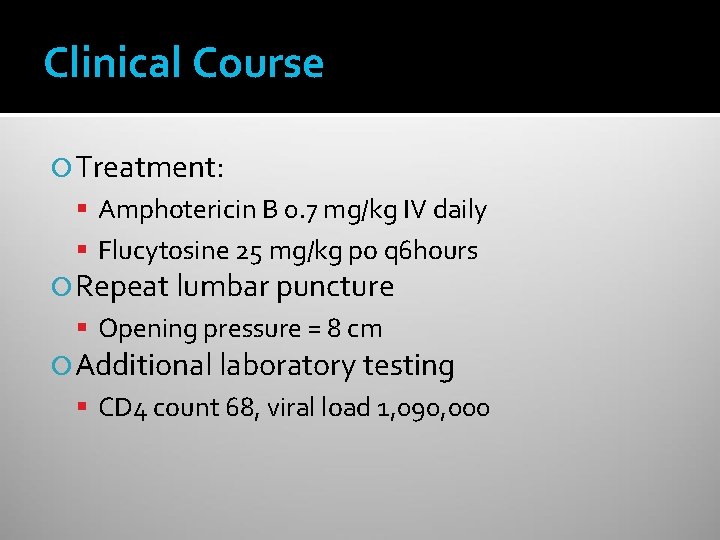
Clinical Course Treatment: Amphotericin B 0. 7 mg/kg IV daily Flucytosine 25 mg/kg po q 6 hours Repeat lumbar puncture Opening pressure = 8 cm Additional laboratory testing CD 4 count 68, viral load 1, 090, 000

Clinical Course After 4 days of therapy, creatinine increased from 0. 97 to 1. 92 Changed amphotericin to Abelcet 5 mg / kg Creatinine subsequently improved gradually Subsequently developed severe nausea, vomiting, and bloody diarrhea
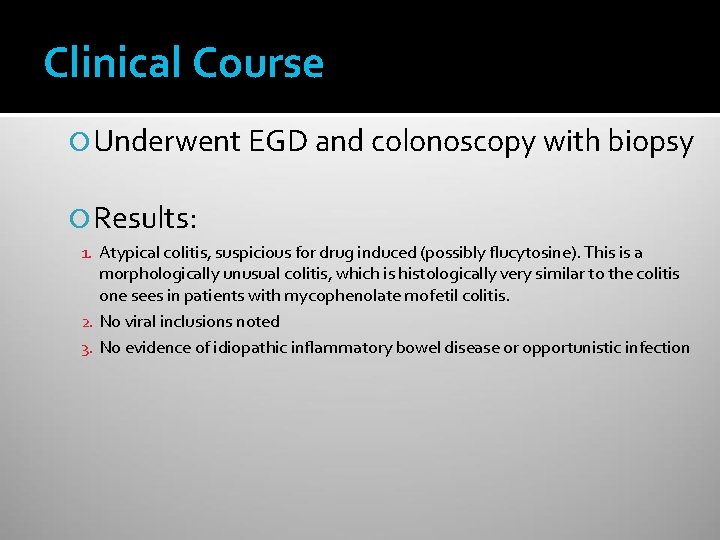
Clinical Course Underwent EGD and colonoscopy with biopsy Results: 1. Atypical colitis, suspicious for drug induced (possibly flucytosine). This is a morphologically unusual colitis, which is histologically very similar to the colitis one sees in patients with mycophenolate mofetil colitis. 2. No viral inclusions noted 3. No evidence of idiopathic inflammatory bowel disease or opportunistic infection

Clinical Course Headache improved, mentation improved Repeat lumbar puncture at ~2 weeks Cryptococcal antigen 1: 256 Culture with 1+ cryptococcus ▪ Fluconazole MIC = 16 ▪ Flucytosine MIC > 32 (RESISTANT) Antifungal therapy was changed to fluconazole
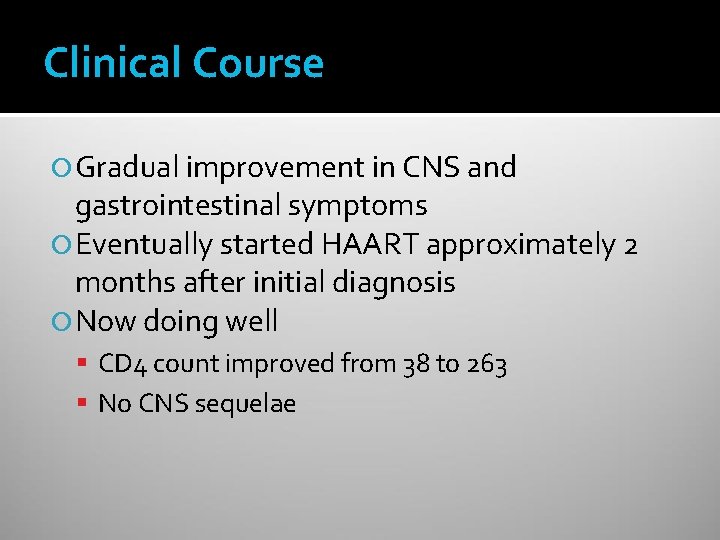
Clinical Course Gradual improvement in CNS and gastrointestinal symptoms Eventually started HAART approximately 2 months after initial diagnosis Now doing well CD 4 count improved from 38 to 263 No CNS sequelae
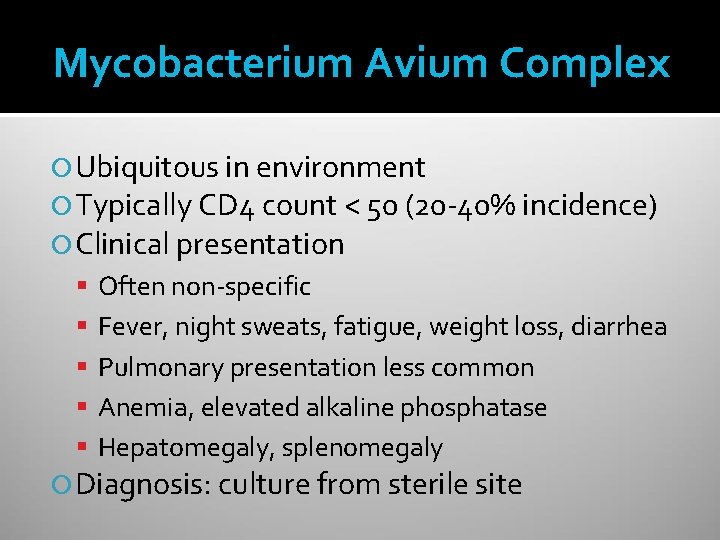
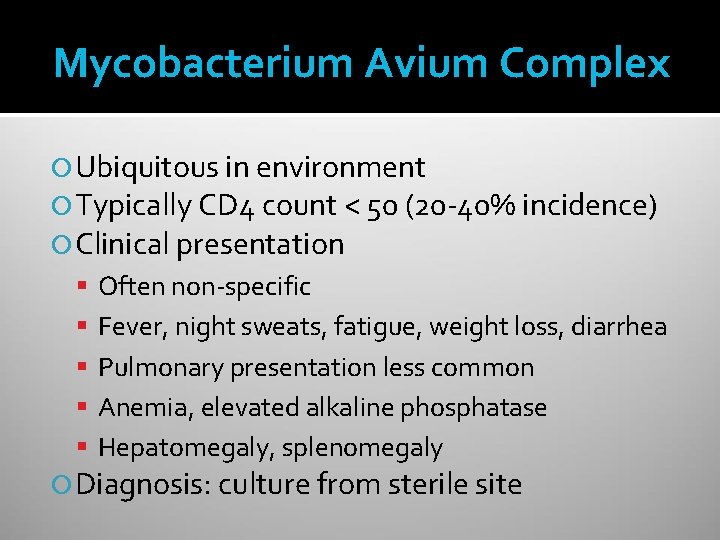
Mycobacterium Avium Complex Ubiquitous in environment Typically CD 4 count < 50 (20 -40% incidence) Clinical presentation Often non-specific Fever, night sweats, fatigue, weight loss, diarrhea Pulmonary presentation less common Anemia, elevated alkaline phosphatase Hepatomegaly, splenomegaly Diagnosis: culture from sterile site

Mycobacterium Avium Complex Treatment: multi-drug therapy Clarithromycin (or azithromycin) Ethambutol Rifabutin Prophylaxis – rule out active infection first Azithromycin 1200 mg weekly is preferred Rifabutin is an option ▪ More drug interactions ▪ Rule out active TB
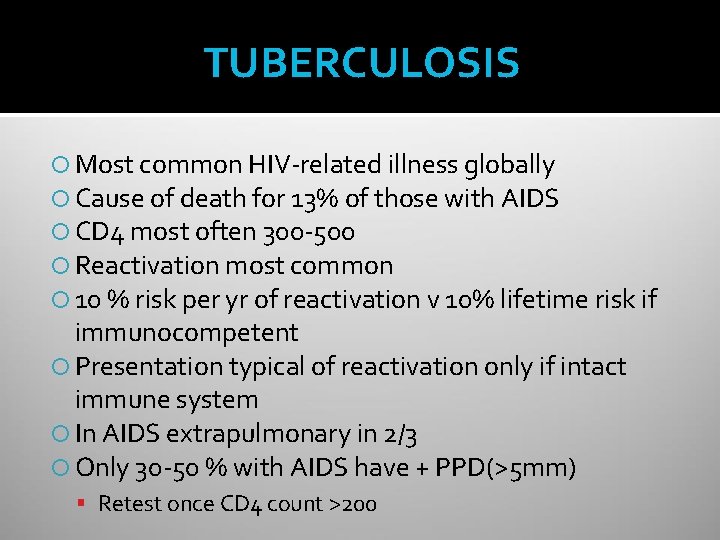
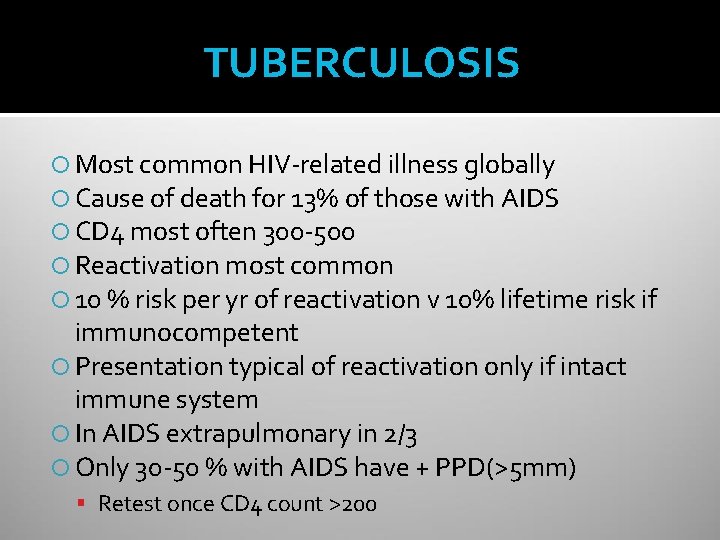
TUBERCULOSIS Most common HIV-related illness globally Cause of death for 13% of those with AIDS CD 4 most often 300 -500 Reactivation most common 10 % risk per yr of reactivation v 10% lifetime risk if immunocompetent Presentation typical of reactivation only if intact immune system In AIDS extrapulmonary in 2/3 Only 30 -50 % with AIDS have + PPD(>5 mm) Retest once CD 4 count >200

KAPOSI’S SARCOMA Most common neoplasm in AIDS Usually gay males HHV-8 -DNA + > 90% HIV + KS Localized or widespread visceral disease GI, Lung, LN Violaceous lesions Bx-mimics BA Rx = IFN, Vinblastine, VCR, VP-16, Adriamycin Responses Poor HAART-good responses, sometimes complete remission

OPPORTUNISTIC INFECTIONS AND CD 4 200 -350 Candida Tuberculosis HSV Zoster Pneumococcus CD 4 100 -200 PCP Cryptosporidiosis CD 4 < 100 NHL PML Toxoplasmosis Cryptococcus CMV MAI Wasting Syndrome HIV Encephalopathy Recurrent PCP
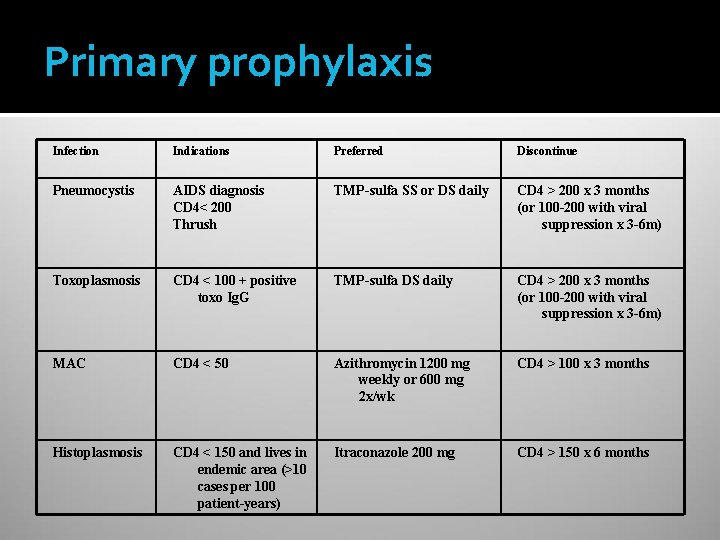
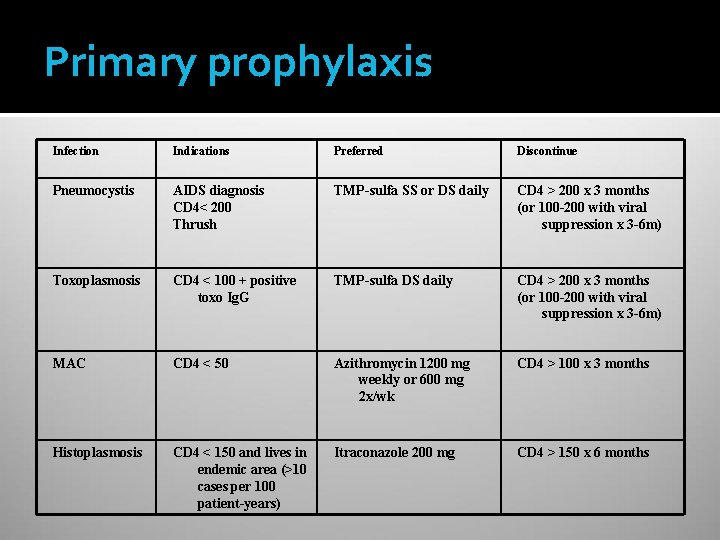
Primary prophylaxis Infection Indications Preferred Discontinue Pneumocystis AIDS diagnosis CD 4< 200 Thrush TMP-sulfa SS or DS daily CD 4 > 200 x 3 months (or 100 -200 with viral suppression x 3 -6 m) Toxoplasmosis CD 4 < 100 + positive toxo Ig. G TMP-sulfa DS daily CD 4 > 200 x 3 months (or 100 -200 with viral suppression x 3 -6 m) MAC CD 4 < 50 Azithromycin 1200 mg weekly or 600 mg 2 x/wk CD 4 > 100 x 3 months Histoplasmosis CD 4 < 150 and lives in endemic area (>10 cases per 100 patient-years) Itraconazole 200 mg CD 4 > 150 x 6 months

Summary Opportunistic infections are often the initial presentation of persons with undiagnosed HIV infection Important to recognize syndromes, test for HIV infection when indicated Treatment of HIV infection reduces risk for opportunistic infections
 Opportunistic infections
Opportunistic infections Opportunistic infections
Opportunistic infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Name the five lesions associated with hiv/aids chapter 17
Name the five lesions associated with hiv/aids chapter 17 Opportunistic approach adalah model proses
Opportunistic approach adalah model proses Nation and macalister language curriculum design
Nation and macalister language curriculum design Phagocytr
Phagocytr Bone and joint infections
Bone and joint infections Johnson and johnson botnet infections
Johnson and johnson botnet infections Classification of acute gingival infections
Classification of acute gingival infections Neurosiphyllis
Neurosiphyllis Genital infections
Genital infections Storch infections
Storch infections Eye infections
Eye infections Amber blumling
Amber blumling Storch infections
Storch infections Postpartum infections
Postpartum infections Methotrexate and yeast infections
Methotrexate and yeast infections Hiv
Hiv Hiv test results example
Hiv test results example Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Ciclo do hiv
Ciclo do hiv Hiv vaccinr
Hiv vaccinr Phdp in hiv
Phdp in hiv Viral integration
Viral integration Patogenesis hiv
Patogenesis hiv Hiv patologia
Hiv patologia Dr shabani
Dr shabani Hiv lifecycle
Hiv lifecycle Risk of receiving unprotected oral
Risk of receiving unprotected oral Hiv treatments
Hiv treatments Iris syndrome
Iris syndrome Hiv retrovirus
Hiv retrovirus Asante hiv-1 rapid recency assay
Asante hiv-1 rapid recency assay Hiv in adults
Hiv in adults Hiv
Hiv Test wiedzy o hiv i aids z odpowiedziami
Test wiedzy o hiv i aids z odpowiedziami Hiv roga lakshana
Hiv roga lakshana Hiv
Hiv Hiv test window period
Hiv test window period Vidas hiv duo ultra package insert
Vidas hiv duo ultra package insert Hiv test window period
Hiv test window period Leukopenia
Leukopenia Stadium hiv
Stadium hiv Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Abcde hiv
Abcde hiv Objawy hiv
Objawy hiv Global hiv prevention coalition
Global hiv prevention coalition Phagocytosis ap bio
Phagocytosis ap bio Syptoms of hiv
Syptoms of hiv Kuchecheudzwa
Kuchecheudzwa Cytomegalavirus
Cytomegalavirus Nefropatia hiv
Nefropatia hiv Hiv
Hiv Hiv
Hiv Hiv virus
Hiv virus How does hiv get into the urethra
How does hiv get into the urethra Causative organism of hiv/aids
Causative organism of hiv/aids Hiv
Hiv Hiv
Hiv Fiebig hiv
Fiebig hiv Cdc hiv testing
Cdc hiv testing Hiv
Hiv Kasus hiv aids
Kasus hiv aids Approche index testing
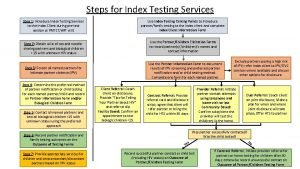
Approche index testing Hiv meaning
Hiv meaning Profilaksis pasca pajanan hiv
Profilaksis pasca pajanan hiv Hiv stool color
Hiv stool color Hiv lifecycle
Hiv lifecycle Stadium hiv menurut who
Stadium hiv menurut who Basic hiv course
Basic hiv course