OPPORTUNISTIC MYCOSES Sevtap Arikan MD OPPORTUNISTIC MYCOSES General



- Slides: 28
OPPORTUNISTIC MYCOSES Sevtap Arikan, MD
OPPORTUNISTIC MYCOSES General features CAUSATIVE AGENTS Saprophyte in nature/found in normal flora HOST Immunosupressed /other risk factors
OPPORTUNISTIC MYCOSES 4 Candidiasis 4 Cryptococcosis 4 Aspergillosis 4 Zygomycosis 4 Other: Trichosporonosis, fusariosis, penicillosis…… ***ANY fungus found in nature may give rise to opportunistic mycoses ***
CANDIDIASIS 4 Most commonly encountered opportunistic mycoses worldwide 4 Cellular immunity protects against mucocutaneous candidiasis, neutrophiles protect against invasive candidiasis 4 Endogenous inf. 4 Etio: Candida spp. Most common: 1. C. albicans 2. C. tropicalis

MOST COMMONLY ISOLATED CANDIDA SPECIES 4 C. albicans 4 C. tropicalis 4 C. parapsilosis 4 C. kefyr 4 C. glabrata 4 C. krusei 4 C. guillermondii 4 C. lusitaniae
Candida MORPHOLOGICAL FEATURES 4 Micr. Budding yeast cells Pseudohyphae, true hyphae 4 Macr. Creamy yeast colonies (SDA) 4 Germ tube (C. albicans, C. dubliniensis) 4 Chlamydospore (C. albicans, C. dubliniensis) 4 Identification Germ tube, fermentation and assimilation reactions
Candida PATHOGENICITY 4 Attachment (Germ tube is more adhesive than yeast cell) 4 Adherence to plastic surfaces (catheter, prosthetic valve. . ) 4 Protease 4 Phospholipase
CANDIDIASIS Risk factors 4 Physiological. Pregnancy, elderly, infancy 4 Traumatic. Burn, infection 4 Hematological. Cellular immune deficiency, AIDS, chronic granulamatous disease, aplastic anemia, leukemia, lymphoma. . . 4 Endocrinological. DM, hypoparathyroidism, Addison disease 4 Iatrogenic. Oral contraceptives, antibiotics, steroid, chemotherapy, catheter. . .
CANDIDIASIS Clinical manifestations-I 1. CUTANEOUS and SUBCUTANEOUS 4 Oral 4 Vaginal 4 Onychomycosis 4 Dermatitis 4 Diaper rash 4 Balanitis
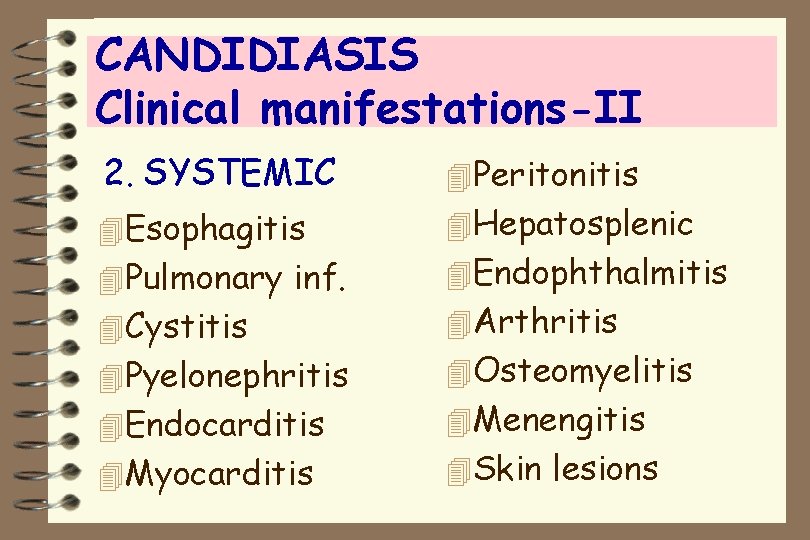
CANDIDIASIS Clinical manifestations-II 2. SYSTEMIC 4 Peritonitis 4 Esophagitis 4 Hepatosplenic 4 Pulmonary inf. 4 Cystitis 4 Pyelonephritis 4 Endocarditis 4 Myocarditis 4 Endophthalmitis 4 Arthritis 4 Osteomyelitis 4 Menengitis 4 Skin lesions
4 CANDIDIASIS Clinical manifestations-III 3. CHRONIC MUCOCUTANEOUS 4 Candida inf. of skin and mucous membranes 4 Verrucose lesions 4 Impaired cellular immunity 4 Autosomal recessive trait 4 Hypoparathyroidism, iron deficiency
CANDIDIASIS Diagnosis 4 Direct micr. ic examination Yeast cells, pseudohyphae, true hyphae 4 Culture SDA, routine bacteriological media 4 Serology Detection of mannan antigen (ELISA, RIA, IF, latex agglutination)

CANDIDIASIS Treatment 4 CUTANEOUS Topical antifungal: Ketoconazole, miconazole, nystatin 4 SYSTEMIC Amphotericin B Fluconazole, itraconazole 4 CHRONIC MUCOCUTANEOUS Amphotericin B Fluconazole, itraconazole Transfer factor
CRYPTOCOCCOSIS 4 Underlying cellular immunodeficiency (AIDS, lymphoma) 4 Exogenous inf. 4 Pathogenesis Inhalation of yeasts 4 Etio. Cryptococcus neoformans
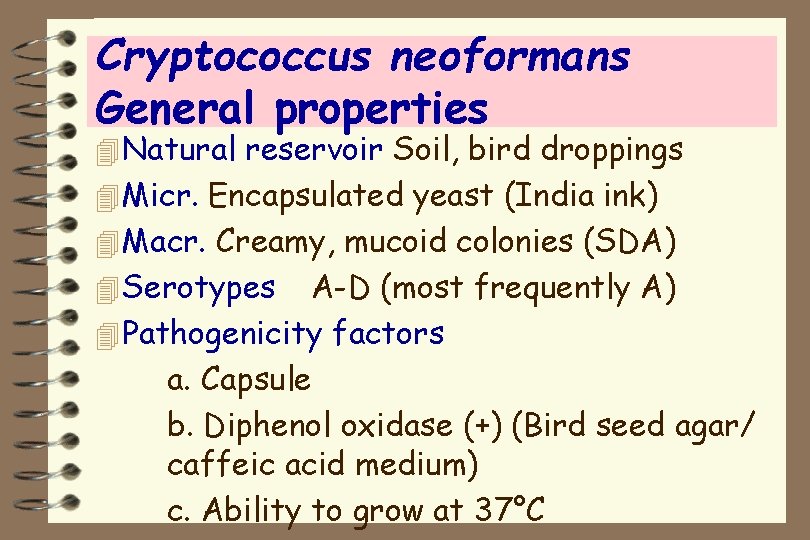
Cryptococcus neoformans General properties 4 Natural reservoir Soil, bird droppings 4 Micr. Encapsulated yeast (India ink) 4 Macr. Creamy, mucoid colonies (SDA) 4 Serotypes A-D (most frequently A) 4 Pathogenicity factors a. Capsule b. Diphenol oxidase (+) (Bird seed agar/ caffeic acid medium) c. Ability to grow at 37°C
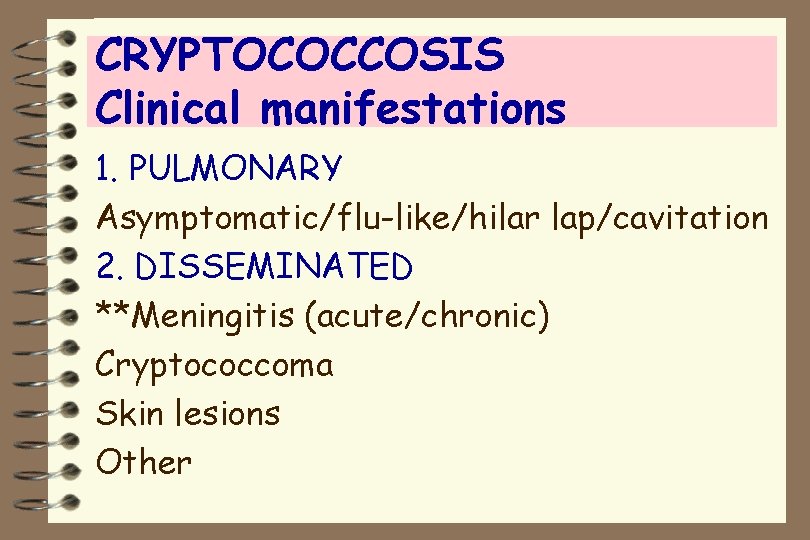
CRYPTOCOCCOSIS Clinical manifestations 1. PULMONARY Asymptomatic/flu-like/hilar lap/cavitation 2. DISSEMINATED **Meningitis (acute/chronic) Cryptococcoma Skin lesions Other
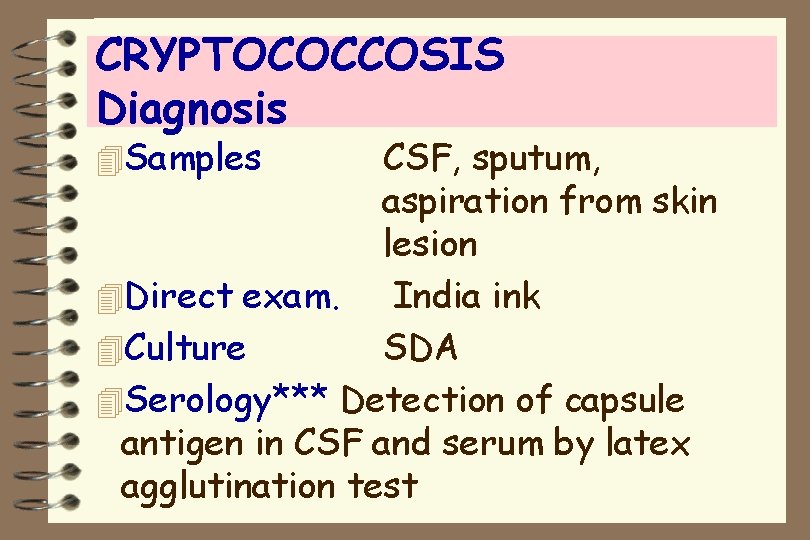
CRYPTOCOCCOSIS Diagnosis 4 Samples CSF, sputum, aspiration from skin lesion 4 Direct exam. India ink 4 Culture SDA 4 Serology*** Detection of capsule antigen in CSF and serum by latex agglutination test
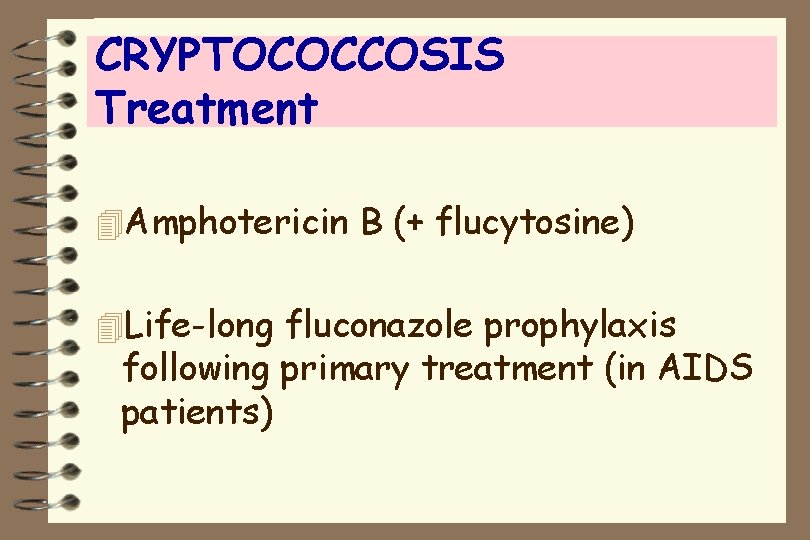
CRYPTOCOCCOSIS Treatment 4 Amphotericin B (+ flucytosine) 4 Life-long fluconazole prophylaxis following primary treatment (in AIDS patients)
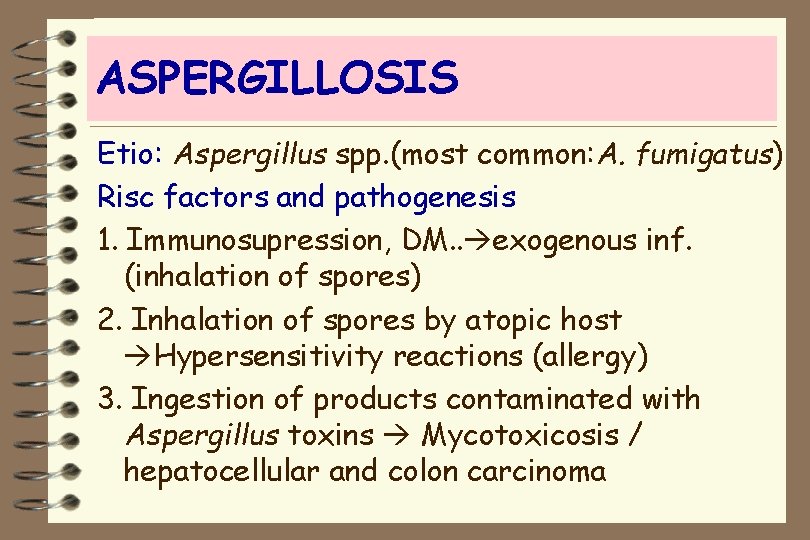
ASPERGILLOSIS Etio: Aspergillus spp. (most common: A. fumigatus) Risc factors and pathogenesis 1. Immunosupression, DM. . exogenous inf. (inhalation of spores) 2. Inhalation of spores by atopic host Hypersensitivity reactions (allergy) 3. Ingestion of products contaminated with Aspergillus toxins Mycotoxicosis / hepatocellular and colon carcinoma
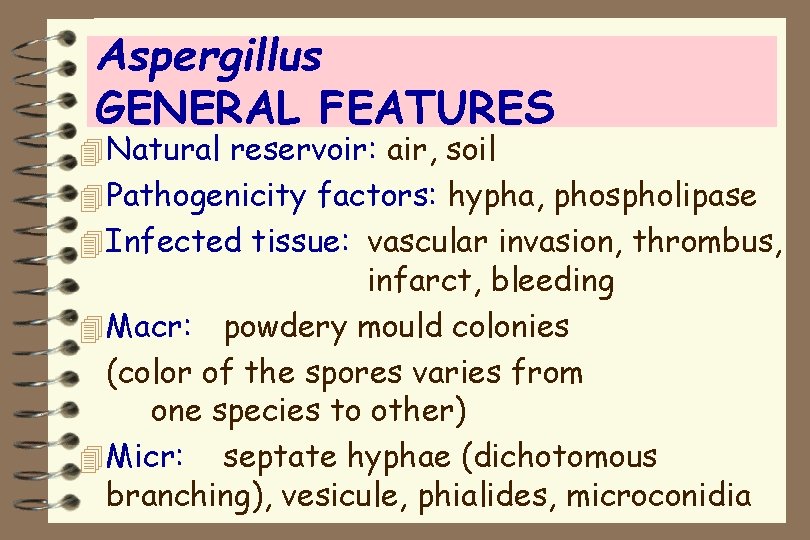
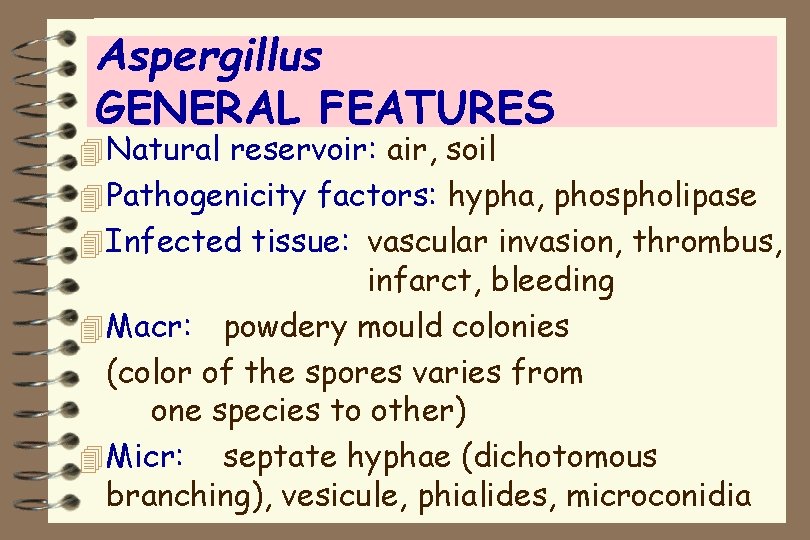
Aspergillus GENERAL FEATURES 4 Natural reservoir: air, soil 4 Pathogenicity factors: hypha, phospholipase 4 Infected tissue: vascular invasion, thrombus, infarct, bleeding 4 Macr: powdery mould colonies (color of the spores varies from one species to other) 4 Micr: septate hyphae (dichotomous branching), vesicule, phialides, microconidia
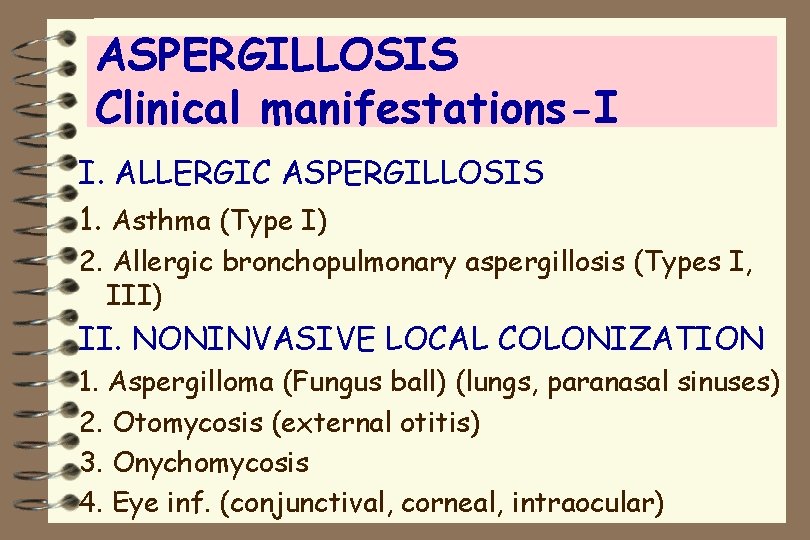
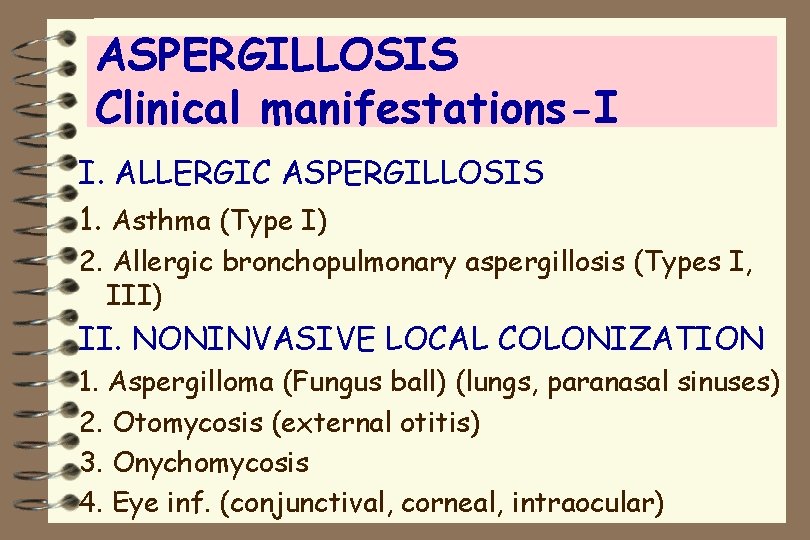
ASPERGILLOSIS Clinical manifestations-I I. ALLERGIC ASPERGILLOSIS 1. Asthma (Type I) 2. Allergic bronchopulmonary aspergillosis (Types I, III) II. NONINVASIVE LOCAL COLONIZATION 1. Aspergilloma (Fungus ball) (lungs, paranasal sinuses) 2. Otomycosis (external otitis) 3. Onychomycosis 4. Eye inf. (conjunctival, corneal, intraocular)

ASPERGILLOSIS Clinical manifestations-II III. INVASIVE ASPERGILLOSIS 1. Pulmonary 2. Disseminated: GIT, brain, liver, kidney, heart, skin, eye IV. MYCOTOXICOSIS
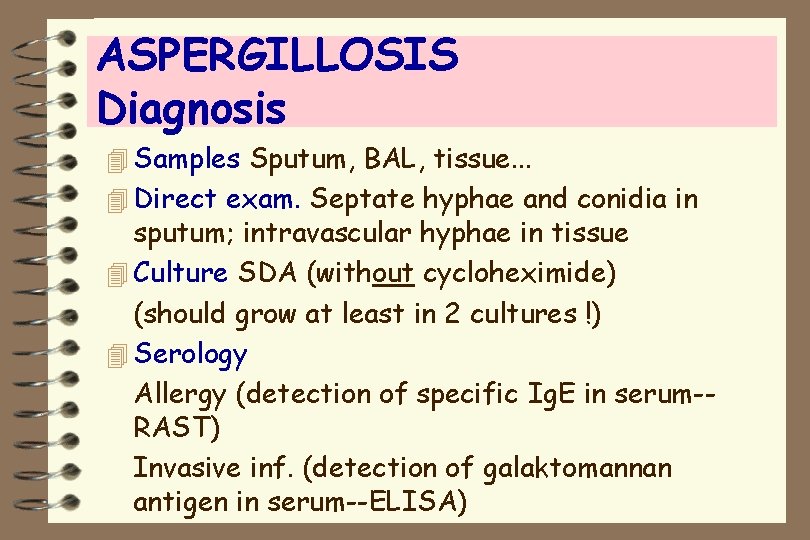
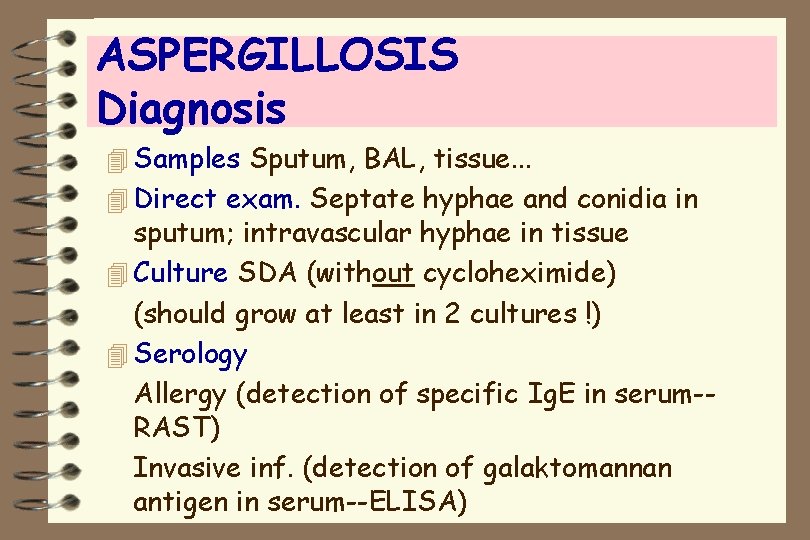
ASPERGILLOSIS Diagnosis 4 Samples Sputum, BAL, tissue. . . 4 Direct exam. Septate hyphae and conidia in sputum; intravascular hyphae in tissue 4 Culture SDA (without cycloheximide) (should grow at least in 2 cultures !) 4 Serology Allergy (detection of specific Ig. E in serum-RAST) Invasive inf. (detection of galaktomannan antigen in serum--ELISA)
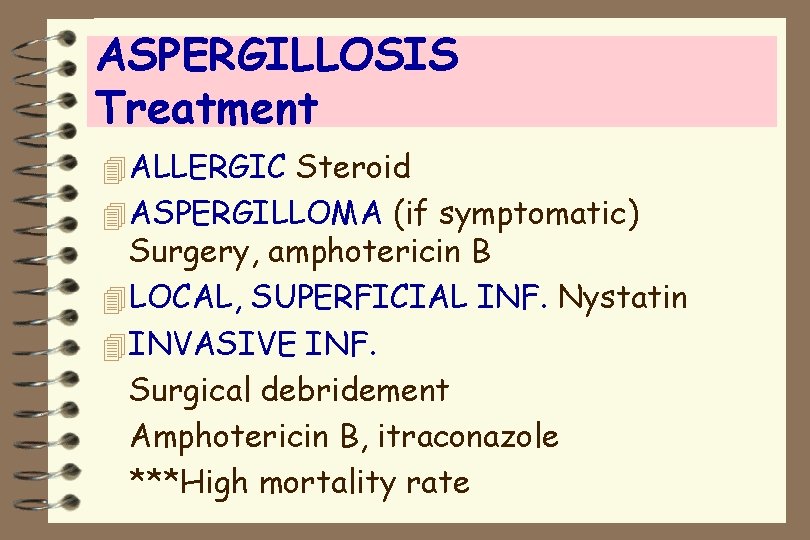
ASPERGILLOSIS Treatment 4 ALLERGIC Steroid 4 ASPERGILLOMA (if symptomatic) Surgery, amphotericin B 4 LOCAL, SUPERFICIAL INF. Nystatin 4 INVASIVE INF. Surgical debridement Amphotericin B, itraconazole ***High mortality rate
ZYGOMYCOSIS 4 Causative agents Rhizopus, Rhizomucor, Mucor. . . 4 Natural reservoir Air, water, soil 4 Risk factors Diabetic ketoacidosis, immunosuppression 4 Pathogenesis Inhalation of sporangiospores 4 Infected tissue vascular invasion, thrombus, infarct, bleeding
ZYGOMYCOSIS Clinical manifestations I. RHINOCEREBRAL 4 Nose, paranasal sinuses, eye, brain and meninges are involved 4 Orbital cellulitis II. THORACIC 4 Pulmonary lesions, parenchymal necrosis III. LOCAL 4 Posttraumatic kidney inf. 4 Skin inf. following burn or surgery
ZYGOMYCOSIS Diagnosis 4 Samples Sputum, BAL, biopsy of paranasal sinuses. . 4 Direct exam. Nonseptate, ribbon-like hyphae which branch at right angles, sporangium 4 Culture SDA (cotton candy appearence)
ZYGOMYCOSIS Treatment 4 Surgical debridement 4 Amphotericin B ***High mortality rate
 Sevtap yasin
Sevtap yasin Michael chekhov oyuncuya
Michael chekhov oyuncuya Mustafa arikan
Mustafa arikan Elisa arikan
Elisa arikan Berkay arıkan
Berkay arıkan Selma arıkan
Selma arıkan Irem arikan
Irem arikan Deniz cemgil arıkan
Deniz cemgil arıkan Cutaneous mycoses
Cutaneous mycoses Inscryption ringworm
Inscryption ringworm Systemic mycoses
Systemic mycoses Mycoses
Mycoses Classification of mycoses ppt
Classification of mycoses ppt Opportunistic infections
Opportunistic infections Environment analysis in language curriculum design
Environment analysis in language curriculum design Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Opportunistic infections
Opportunistic infections Opportunistic approach adalah model proses untuk
Opportunistic approach adalah model proses untuk Where did general lee surrender to general grant?
Where did general lee surrender to general grant? Diferencia entre gran plano general y plano general
Diferencia entre gran plano general y plano general General mechanics
General mechanics Objetivo general de la pobreza
Objetivo general de la pobreza Specific problem example
Specific problem example General organizational resources
General organizational resources Diseños curriculares relacionales
Diseños curriculares relacionales How to write general and specific objectives in research
How to write general and specific objectives in research Balance day adjustments
Balance day adjustments General taso
General taso Acotacion de chaflanes
Acotacion de chaflanes